Attached files
| file | filename |
|---|---|
| EX-12.1 - EXHIBIT 12.1 - CONSOLIDATED EDISON INC | ed-20170930xex121.htm |
| EX-32.2.2 - EXHIBIT 32.2.2 - CONSOLIDATED EDISON INC | ed-20170930xex3222.htm |
| EX-32.2.1 - EXHIBIT 32.2.1 - CONSOLIDATED EDISON INC | ed-20170930xex3221.htm |
| EX-31.2.2 - EXHIBIT 31.2.2 - CONSOLIDATED EDISON INC | ed-20170930xex3122.htm |
| EX-31.2.1 - EXHIBIT 31.2.1 - CONSOLIDATED EDISON INC | ed-20170930xex3121.htm |
| EX-12.2 - EXHIBIT 12.2 - CONSOLIDATED EDISON INC | ed-20170930xex122.htm |
| EX-32.1.2 - EXHIBIT 32.1.2 - CONSOLIDATED EDISON INC | ed-20170930xex3212.htm |
| EX-32.1.1 - EXHIBIT 32.1.1 - CONSOLIDATED EDISON INC | ed-20170930xex3211.htm |
| EX-31.1.2 - EXHIBIT 31.1.2 - CONSOLIDATED EDISON INC | ed-20170930xex3112.htm |
| EX-31.1.1 - EXHIBIT 31.1.1 - CONSOLIDATED EDISON INC | ed-20170930xex3111.htm |
| EX-10.1.2 - EXHIBIT 10.1.2 - CONSOLIDATED EDISON INC | ed-20170930xex1012.htm |
| EX-10.1.1 - EXHIBIT 10.1.1 - CONSOLIDATED EDISON INC | ed-20170930xex1011.htm |
| 10-Q - 10-Q - CONSOLIDATED EDISON INC | ed-20170930x10q.htm |
Exhibit 10.2.1
Consolidated Edison Company
of New York
SUPPLEMENTAL MEDICAL BENEFITS
EFFECTIVE DATE: January 1, 2017
CN007
3331910
This document printed in February, 2017 takes the place of any documents previously issued to you which described your benefits.
Printed in U.S.A.
Exhibit 10.2.1
Exhibit 10.2.1
Table of Contents
Certification......................................................................................................................................4
Important Notices............................................................................................................................6
How To File Your Claim..................................................................................................................9
Eligibility – Effective Date..............................................................................................................9
Supplemental Medical Benefits.....................................................................................................11
Covered Expenses................................................................................................................................11
General Limitations.......................................................................................................................15
Payment of Benefits.......................................................................................................................15
Termination of Supplemental Medical Benefits..........................................................................16
Employees...........................................................................................................................................16
Dependents..........................................................................................................................................16
Continuation........................................................................................................................................17
Rescissions..........................................................................................................................................18
Medical Benefits Extension Upon Policy Cancellation..............................................................19
Federal Requirements...................................................................................................................19
Qualified Medical Child Support Order (QMCSO)...............................................................................19
Special Enrollment Rights Under the Health Insurance Portability & Accountability Act (HIPAA)....20
Effect of Section 125 Tax Regulations on This Plan..............................................................................21
Eligibility for Coverage for Adopted Children.......................................................................................22
Coverage for Maternity Hospital Stay....................................................................................................22
Women’s Health and Cancer Rights Act (WHCRA)..............................................................................22
Group Plan Coverage Instead of Medicaid.............................................................................................22
Requirements of Medical Leave Act of 1993 (as amended) (FMLA)....................................................22
Uniformed Services Employment and Re-Employment Rights Act of 1994 (USERRA)......................23
Claim Determination Procedures under ERISA.....................................................................................23
COBRA Continuation Rights Under Federal Law.................................................................................24
ERISA Required Information.................................................................................................................27
Notice of an Appeal or a Grievance.......................................................................................................29
When You Have A Concern Or Complaint.................................................................................29
Definitions......................................................................................................................................33
Exhibit 10.2.1
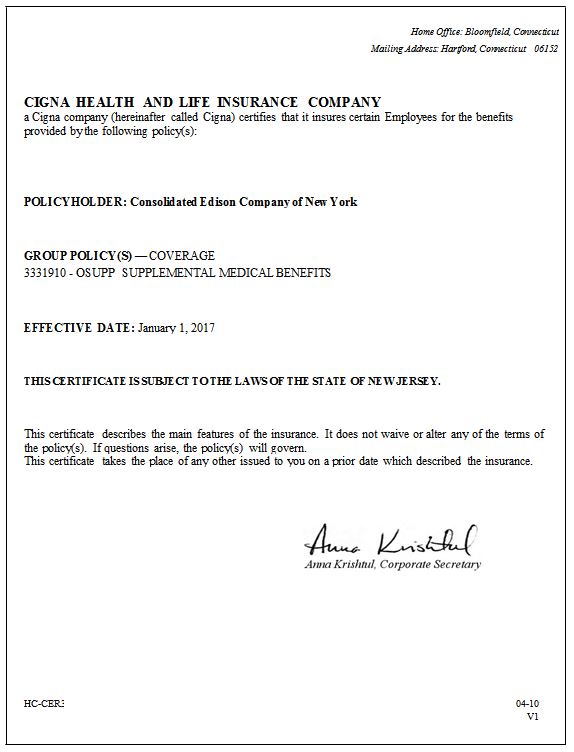
Exhibit 10.2.1
Explanation of Terms
You will find terms starting with capital letters throughout your certificate. To help you understand your benefits, most of these terms are defined in the Definitions section of your certificate.
Exhibit 10.2.1

_____________________________________________________________________________________________
Important Notices
Notice of Grandfathered Plan Status
This plan is being treated as a “grandfathered health plan” under the Patient Protection and Affordable Care Act (the Affordable Care Act). As permitted by the Affordable Care Act, a grandfathered health plan can preserve certain basic health coverage that was already in effect when that law was enacted. Being a grandfathered health plan means that your coverage may not include certain consumer protections of the Affordable Care Act that apply to other plans, for example, the requirement for the provision of preventive health services without any cost sharing. However, grandfathered health plans must comply with certain other consumer protections in the Affordable Care Act, for example, the elimination of lifetime limits on benefits.
Questions regarding which protections apply and which protections do not apply to a grandfathered health plan and what might cause a plan to change from grandfathered health plan status can be directed to the plan administrator at the phone number or address provided in your plan documents, to your employer or plan sponsor or an explanation can be found on Cigna’s website at http://www.Cigna.com/sites/healthcare_reform/customer.html.
If your plan is subject to ERISA, you may also contact the Employee Benefits Security Administration, U.S. Department of Labor at 1-866-444-3272 or www.dol.gov/ebsa/healthreform. This website has a table summarizing which protections do and do not apply to grandfathered health plans.
If your plan is a nonfederal government plan or a church plan, you may also contact the U.S. Department of Health and Human Services at www.healthcare.gov.
HC-NOT4 | 01-11 | |||
Important Information
Mental Health Parity and Addiction Equity Act The Certificate is amended as stated below:
In the event of a conflict between the provisions of your plan documents and the provisions of this notice, the provisions that provide the better benefit shall apply.
The Schedule and Mental Health and Substance Abuse Covered Expenses:
Partial Hospitalization charges for Mental Health and Substance Abuse will be paid at the Outpatient level. Covered Expenses are changed as follows:
Mental Health and Substance Abuse Services
Mental Health Services are services that are required to treat a disorder that impairs the behavior, emotional reaction or thought processes. In determining benefits payable, charges made for the treatment of any physiological conditions related to Mental Health will not be considered to be charges made for treatment of Mental Health.
Substance Abuse is defined as the psychological or physical dependence on alcohol or other mind-altering drugs that requires diagnosis, care, and treatment. In determining benefits payable, charges made for the treatment of any physiological conditions related to rehabilitation services for alcohol or drug abuse or addiction will not be considered to be charges made for treatment of Substance Abuse.
Inpatient Mental Health Services
Services that are provided by a Hospital while you or your Dependent is Confined in a Hospital for the treatment and evaluation of Mental Health. Inpatient Mental Health Services include Mental Health Residential Treatment Services.
Mental Health Residential Treatment Services are services provided by a Hospital for the evaluation and treatment of the psychological and social functional disturbances that are a result of subacute Mental Health conditions.
Mental Health Residential Treatment Center means an institution which specializes in the treatment of psychological and social disturbances that are the result of Mental Health conditions; provides a subacute, structured, psychotherapeutic treatment program, under the supervision of Physicians; provides 24-hour care, in which a person lives in an open setting; and is licensed in accordance with the laws of the appropriate legally authorized agency as a residential treatment center.
A person is considered confined in a Mental Health Residential Treatment Center when she/he is a registered bed patient in a Mental Health Residential Treatment Center upon the recommendation of a Physician.
Outpatient Mental Health Services are Services of Providers who are qualified to treat Mental Health when treatment is provided on an outpatient basis, while you or your Dependent is not Confined in a Hospital, or for Partial Hospitalization sessions, and is provided in an individual, group or Mental Health Intensive Outpatient Therapy Program. Covered services include, but are not limited to, outpatient treatment of conditions such as: anxiety or depression which interfere with daily functioning; emotional adjustment or concerns related to chronic conditions, such as psychosis or depression; emotional reactions associated with marital problems or divorce; child/adolescent problems of conduct or poor impulse control; affective disorders; suicidal or homicidal threats or acts; eating
_____________________________________________________________________________________________________________
6 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
disorders; or acute exacerbation of chronic Mental Health conditions (crisis intervention and relapse prevention) and outpatient testing and assessment.
Partial Hospitalization sessions are services that are provided for not less than 4 hours and not more than 12 hours in any 24- hour period.
Inpatient Substance Abuse Rehabilitation Services
Services provided for rehabilitation, while you or your Dependent is Confined in a Hospital, when required for the diagnosis and treatment of abuse or addiction to alcohol and/or drugs. Inpatient Substance Abuse Services include Residential Treatment services.
Substance Abuse Residential Treatment Services are services provided by a Hospital for the evaluation and treatment of the psychological and social functional disturbances that are a result of subacute Substance Abuse conditions.
Substance Abuse Residential Treatment Center means an institution which specializes in the treatment of psychological and social disturbances that are the result of Substance Abuse; provides a subacute, structured, psychotherapeutic treatment program, under the supervision of Physicians; provides 24- hour care, in which a person lives in an open setting; and is licensed in accordance with the laws of the appropriate legally authorized agency as a residential treatment center.
A person is considered confined in a Substance Abuse Residential Treatment Center when she/he is a registered bed patient in a Substance Abuse Residential Treatment Center upon the recommendation of a Physician.
Outpatient Substance Abuse Rehabilitation Services
Services provided for the diagnosis and treatment of abuse or addiction to alcohol and/or drugs, while you or your Dependent is not Confined in a Hospital, including outpatient rehabilitation in an individual, or a Substance Abuse Intensive Outpatient Therapy Program and for Partial Hospitalization sessions.
Partial Hospitalization sessions are services that are provided for not less than 4 hours and not more than 12 hours in any 24- hour period.
A Substance Abuse Intensive Outpatient Therapy Program consists of distinct levels or phases of treatment that are provided by a certified/licensed Substance Abuse program. Intensive Outpatient Therapy Programs provide a combination of individual, family and/or group therapy in a day, totaling nine, or more hours in a week.
Substance Abuse Detoxification Services
Detoxification and related medical ancillary services are provided when required for the diagnosis and treatment of addiction to alcohol and/or drugs. Cigna will decide, based on
the Medical Necessity of each situation, whether such services will be provided in an inpatient or outpatient setting.
Mental Health and Substance Abuse Exclusions:
The following exclusion is hereby deleted and no longer applies:
• | any court ordered treatment or therapy, or any treatment or therapy ordered as a condition of parole, probation or custody or visitation evaluations unless Medically Necessary and otherwise covered under this policy or agreement. |
Terms within the agreement:
The term “mental retardation” within your Certificate is hereby changed to “intellectual disabilities”.
Visit Limits:
Any health care service billed with a Mental Health or Substance Abuse diagnosis, will not incur a visit limit, including but not limited to genetic counseling and nutritional evaluation/counseling.
HC-NOT69 | 12-14 | |||
Discrimination is Against the Law
Cigna complies with applicable Federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability or sex. Cigna does not exclude people or treat them differently because of race, color, national origin, age, disability or sex.
Cigna:
• | Provides free aids and services to people with disabilities to communicate effectively with Cigna, such as qualified sign language interpreters and written information in other formats (large print, audio, accessible electronic formats, other formats). |
• | Provides free language services to people whose primary language is not English, such as qualified interpreters and information written in other languages. |
If you need these services, contact Customer Service/Member Services at the toll-free phone number shown on your ID card, and ask an associate for assistance.
If you believe that Cigna has failed to provide these services or discriminated in another way on the basis of race, color, national origin, age, disability or sex, you can file a grievance by sending an email to ACAGrievance@cigna.com or by writing to the following address: Cigna, Nondiscrimination Complaint Coordinator, P.O. Box 188016, Chattanooga, TN 37422.
_____________________________________________________________________________________________________________
7 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
If you need assistance filing a written grievance, please call the toll-free phone shown on your ID card or send an email to ACAGrievance@cigna.com.
You can also file a civil rights complaint with the U.S. Department of Health and Human Services, Office for Civil Rights electronically through the Office for Civil Rights Complaint Portal, available at https://ocrportal.hhs.gov/ocr/portal/lobby.jsf, or by mail at:
U.S. Department of Health and Human Services, 200 Independence Avenue, SW, Room 509F, HHH Building, Washington, D.C. 20201; or by phone at 1-800-368-1019, 800-537-7697 (TDD).
Complaint forms are available at http://www.hhs.gov/ocr/office/file/index.html.
HC-NOT76 | 10-16 | |||
Proficiency of Language Assistance Services
ATTENTION: Language assistance services, free of charge, are available to you. For current Cigna customers, call the number on the back of your ID card. Otherwise, call 1-800- 244-6224 (TTY: Dial 711).
Spanish
ATENCIÓN: tiene a su disposición servicios gratuitos de asistencia lingüística. Si es un cliente actual de Cigna, llame al número que figura en el reverso de su tarjeta de identificación. Si no lo es, llame al 1-800-244-6224 (los usuarios de TTY deben llamar al 711).
Chinese
Vietnamese
CHÚ Ý: Có dịch vụ hỗ trợ ngôn ngữ miễn phí dành cho bạn. Dành cho khách hàng hiện tại của Cigna, gọi số ở mặt sau thẻ Hội viên. Các trýờng hợp khác xin gọi số 1- 800-244-6224 (TTY: Quay số 711).
Korean
Tagalog
PAUNAWA: Makakakuha ka ng mga serbisyo sa tulong sa wika nang libre. Para sa mga kasalukuyang customer ng Cigna, tawagan ang numero sa likuran ng iyong ID card. O kaya, tumawag sa 1-800-244-6224 (TTY: I-dial ang 711).
Russian
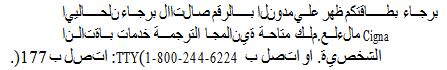
Arabic
French Creole
ATANSYON: Gen sèvis èd nan lang ki disponib gratis pou ou. Pou kliyan Cigna yo, rele nimewo ki dèyè kat ID ou.
Sinon, rele nimewo 1-800-244-6224 (TTY: Rele 711). French
ATTENTION: des services d’aide linguistique vous sont proposés gratuitement. Si vous êtes un client actuel de Cigna, veuillez appeler le numéro indiqué au verso de votre carte d’identité. Sinon, veuillez appeler le numéro 1-800-244-6224 (ATS: composez le numéro 711).
Portuguese
ATENÇÃO: Tem ao seu dispor serviços de assistência linguística, totalmente gratuitos. Para clientes Cigna atuais, ligue para o número que se encontra no verso do seu cartão de identificação. Caso contrário, ligue para 1-800-244-6224 (Dispositivos TTY: marque 711).
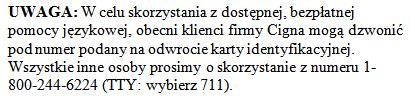
Polish
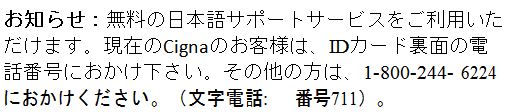
Japanese
Italian
ATTENZIONE: sono disponibili servizi di assistenza linguistica gratuiti. Per i clientI Cigna attuali, chiamare il
_____________________________________________________________________________________________________________
8 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
numero sul retro della tessera ID. In caso contrario, chiamare il numero 1-800-244-6224 (utenti TTY: chiamare il numero 711).
German
Achtung: Die Leistungen der Sprachunterstützung stehen Ihnen kostenlos zur Verfügung. Für gegenwärtige Cigna- Kunden, Bitte rufen Sie die Nummer auf der Rückseite Ihres Personalausweises. Sonst, rufen Sie 1-800-244-6224 (TTY: Wählen Sie 711).
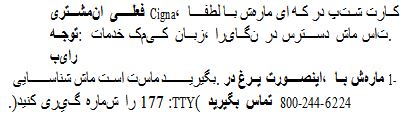
Persian (Farsi)
HC-NOT77 | 10-16 | |||
How To File Your Claim
Claims can be submitted by the provider if the provider is able and willing to file on your behalf. If the provider is not submitting on your behalf, you must send your completed claim form and itemized bills to the claims address listed on the claim form.
You may get the required claim forms from the website listed on your identification card or by calling Member Services using the toll-free number on your identification card.
CLAIM REMINDERS
• | BE SURE TO USE YOUR MEMBER ID AND ACCOUNT/GROUP NUMBER WHEN YOU FILE CIGNA’S CLAIM FORMS, OR WHEN YOU CALL YOUR CIGNA CLAIM OFFICE. |
YOUR MEMBER ID IS THE ID SHOWN ON YOUR BENEFIT IDENTIFICATION CARD.
YOUR ACCOUNT/GROUP NUMBER IS SHOWN ON YOUR BENEFIT IDENTIFICATION CARD.
• | BE SURE TO FOLLOW THE INSTRUCTIONS LISTED ON THE BACK OF THE CLAIM FORM CAREFULLY WHEN SUBMITTING A CLAIM TO CIGNA. |
Timely Filing of Out-of-Network Claims
Cigna will consider claims for coverage under our plans when proof of loss (a claim) is submitted within one year (365 days) after services are rendered. If services are rendered on consecutive days, such as for a hospital confinement, the limit will be counted from the last date of service. If claims are not submitted within one year, the claim will not be considered valid and will be denied. However, if proof of loss is not given
in the time period stated in the paragraph, the claim will not be invalidated nor reduced if it is shown that proof of loss
was given as soon as reasonably possible.
WARNING: Any person who knowingly files a statement of claim containing any false or misleading information is subject to criminal and civil penalties. Any person who includes any false or misleading information on an application for an insurance policy is subject to criminal and civil penalties.
HC-CLM1 | 04-10 | |||
V6 | ||||
Eligibility - Effective Date
Eligibility for Employee Insurance
You will become eligible for Supplemental Medical Benefits on the day you are eligible under your Employer-Sponsored Medical and Vision Benefits Plans if you are in a Class of Eligible Employees.
Eligibility for Dependent Insurance
You will become eligible for Supplemental Medical Benefits for Dependents on the later of:
• | the day you become eligible for yourself; or |
• | the day you acquire your first Dependent. |
Classes of Eligible Employees
Each Employee
Employee Supplemental Medical Benefits
This Plan is offered to you as an Employee.
Effective Date of Your Supplemental Medical Benefits
You will become insured on the date you elect the insurance by signing an approved payroll deduction form (if required), but no earlier than the date you become eligible.
Dependent Supplemental Medical Benefits
For your Dependents to be insured, you may have to pay part of the cost of Dependent Supplemental Medical Benefits.
Effective Date of Your Supplemental Medical Benefits for Your Dependents
Supplemental Medical Benefits for your Dependents will become effective on the date you elect them by signing an approved payroll deduction form (if required), but no earlier than the date you become eligible for them. All of your Dependents as defined by the terms of your Employer- Sponsored Medical and Vision Benefits Plans will be included.
_____________________________________________________________________________________________________________
9 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
Your Dependents will be insured only if you are insured.
HC-ELG2 | 04-10 | |||
V1 | ||||
_____________________________________________________________________________________________________________
10 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
Supplemental Medical Benefits
If you or any one of your Dependents, while insured for Supplemental Medical Benefits, incurs Covered Expenses as defined below, Cigna will pay 100% of the amount of Covered Expenses so incurred. The amount of Supplemental Medical Benefits payable will be subject to the Maximum Benefit Provision.
Maximum Benefit Provision
The total amount of Supplemental Medical Benefits payable for all expenses incurred for you and your Dependents, if any, in a calendar year will not exceed $2,700 per individual and
$5,200 per family, per calendar year.
Covered Expenses
The term Covered Expenses means expenses incurred by or on behalf of you or any one of your Dependents. for the charges below. Expenses are considered Covered Expenses to the extent that the services or supplies provided are recommended by a Physician. Covered Expenses will include only those expenses incurred for charges made:
• | for medical services and supplies to the extent that no benefits are payable under your Employer's medical insurance plan solely because of: Coinsurance factors or Deductibles; dollar limits; or limits on the number of days for which benefits are payable. |
• | for or in connection with cosmetic surgery when: a person receives an Injury which results in bodily damage requiring the surgery; it qualifies as reconstructive surgery following a mastectomy, including surgery and reconstruction of the other breast to achieve symmetry; it qualifies as reconstructive surgery performed on a person following surgery, and both the surgery and the reconstructive surgery are essential and medically necessary; or it is performed to correct a congenital abnormality on one of your Dependents who has not reached skeletal maturity. |
• | for eye examinations and eyeglasses, including contact lenses. |
• | for hearing examinations and hearing aids. |
• | for routine physical examinations and immunizations. |
• | for dental services and supplies provided by a Dentist to the extent that no benefits are payable under your Employer's dental plan solely because of: Coinsurance factors or Deductibles; or dollar limits. |
• | for orthodontia. |
• | for or in connection with in vitro fertilization, artificial insemination or similar procedures. |
• | for charges made for or in connection with tired, weak or strained feet for which treatment consists of routine foot care, including but not limited to, the removal of calluses and corns or the trimming of toenails. |
Limitations
No payment will be made for expenses incurred to the extent that you or your Dependents are entitled to receive payment for such expenses under any other Group Health Plan sponsored by your Employer.
See the section in this certificate entitled General Limitations
for additional restrictions that apply to these benefits.
Extension Of Supplemental Medical Benefits
Covered Expenses incurred after a person's Supplemental Medical Benefits cease, but within one year, will be deemed to be incurred while he is insured if such expense is for an Injury or a Sickness which causes him to be Totally Disabled from the day his insurance ceases until that expense is incurred.
This Extension of Supplemental Medical Benefits will not apply to a child born as a result of a pregnancy which exists when these benefits cease.
General
There is no Conversion Privilege applicable to Supplemental Medical Benefits once insurance under the Policy ceases.
HC-MRP1 | 04-10 | |||
V1 | ||||
Covered Expenses
The term Covered Expenses means the expenses incurred by or on behalf of a person for the charges listed below if they are incurred after he becomes insured for these benefits. Expenses incurred for such charges are considered Covered Expenses to the extent that the services or supplies provided are recommended by a Physician, and are Medically Necessary for the care and treatment of an Injury or a Sickness, as determined by Cigna. Any applicable Copayments, Deductibles or limits are shown in The Schedule.
Covered Expenses
• | charges made by a Hospital, on its own behalf, for Bed and Board and other Necessary Services and Supplies; except that for any day of Hospital Confinement, Covered Expenses will not include that portion of charges for Bed and Board which is more than the Bed and Board Limit shown in The Schedule. |
• | charges for licensed ambulance service to or from the nearest Hospital where the needed medical care and treatment can be provided. |
_____________________________________________________________________________________________________________
11 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
• | charges made by a Hospital, on its own behalf, for medical care and treatment received as an outpatient. |
• | charges made by a Free-Standing Surgical Facility, on its own behalf for medical care and treatment. |
• | charges made on its own behalf, by an Other Health Care Facility, including a Skilled Nursing Facility, a Rehabilitation Hospital or a subacute facility for medical care and treatment; except that for any day of Other Health Care Facility confinement, Covered Expenses will not include that portion of charges which are in excess of the Other Health Care Facility Daily Limit shown in The Schedule. |
• | charges made for Emergency Services and Urgent Care. |
• | charges made by a Physician or a Psychologist for professional services. |
• | charges made by a Nurse, other than a member of your family or your Dependent's family, for professional nursing service. |
• | charges made for anesthetics and their administration; diagnostic x-ray and laboratory examinations; x-ray, radium, and radioactive isotope treatment; chemotherapy; blood transfusions; oxygen and other gases and their administration. |
• | charges made for a baseline mammogram for women between the ages of 35 and 40; an annual mammogram for women age 40 and over; and mammograms at any time if ordered by a woman’s health care provider for women with a family history of breast cancer or other breast cancer risk factors. |
• | charges made for an annual Papanicolaou laboratory screening test. Pap smear coverage includes an initial pap smear and any confirmatory tests, when Medically Necessary, as ordered by the attending Physician, including all associated laboratory tests. |
• | charges made for an annual prostate-specific antigen test (PSA), including a digital rectal examination, for men age 50 and over who are asymptomatic and for men age 40 and over with a family history of prostate cancer, or other prostate cancer risk factors. |
• | charges made for laboratory services, radiation therapy and other diagnostic and therapeutic radiological procedures. |
• | abortion when a Physician certifies in writing that the pregnancy would endanger the life of the mother, or when the expenses are incurred to treat medical complications due to abortion. |
• | charges made for the following preventive care services (detailed information is available at www.healthcare.gov.): |
(1) | evidence-based items or services that have in effect a rating of “A” or “B” in the current recommendations of the United States Preventive Services Task Force; |
(2) | immunizations that have in effect a recommendation from the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention with respect to the Covered Person involved; |
(3) | for infants, children, and adolescents, evidence- informed preventive care and screenings provided for in the comprehensive guidelines supported by the Health Resources and Services Administration; |
(4) | for women, such additional preventive care and screenings not described in paragraph (1) as provided for in comprehensive guidelines supported by the Health Resources and Services Administration. |
• | charges made for Preventive Care consisting of the following health and wellness tests and services delivered or supervised by a Physician, in keeping with prevailing medical standards: |
• | for all persons 20 years of age and older, annual tests to determine blood hemoglobin, blood pressure, blood glucose level, and blood cholesterol level or, instead, low- density lipoprotein (LDL) level and blood high-density lipoprotein (HDL) level; for all persons 35 years of age or older, a glaucoma eye test every five years; for all persons 40 years of age or older, an annual stool examination for presence of blood; for all persons 45 years of age or older, a left-sided colon examination of 35 to 60 centimeters every five years; for all women 20 years of age and older; a Pap smear as recommended by a Physician; for all women 40 years and older, a mammogram annually; for all adults, recommended immunizations; and all persons 20 years of age and older, an annual consultation with a health care provider to discuss lifestyle behaviors that promote health and well-being including, but not limited to, smoking control, nutrition and diet recommendations, exercise plans, lower back protection, weight control, immunization practices, breast self-examination, testicular self-exam and seat belt usage in motor vehicles; excluding any charges for: |
• | services for which benefits are otherwise provided under this Medical Benefits section; |
• | services for which benefits are not payable according to the Expenses Not Covered section. |
Other wellness tests and time schedules will be covered upon the recommendation of a Physician. Any In-Network deductible will be waived for these preventive care services.
_____________________________________________________________________________________________________________
12 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
Additionally, Covered Expenses include charges for childhood immunizations as recommended by the Advisory Committee on Immunization practices of the U.S. Public Health Service, the Department of Health and the New Jersey Department of Health and Senior Services for a Dependent child during that child’s lifetime. Any In- Network deductible will be waived for childhood immunizations.
• | charges for the following screening examinations and laboratory tests for colorectal cancer screening in average- risk adults, beginning at age 50: annual guaiac-based fecal occult blood test (gFOBT) with high tests sensitivity for cancer; annual immunochemical-based fecal occult blood test (FIT) with high test sensitivity for cancer; stool DNA (sDNA) test with high test sensitivity for cancer; flexible sigmoidoscopy every five years; colonoscopy every ten years; double contract barium enema every five years; computed tomography colonography (virtual colonoscopy) every five years. |
• | charges for maternity benefits to include 48 hours of inpatient care following a vaginal delivery and 96 hours of inpatient care following a cesarean section for a mother and her newborn child in a licensed health care facility if requested by the mother or determined by the attending Physician to be Medically Necessary. |
• | charges for screening by blood lead measurement for lead poisoning for children, including: confirmatory blood lead testing, medical evaluation, and any necessary medical follow-up and treatment for lead poisoning for children. |
• | charges for therapeutic treatment of inherited metabolic diseases, when diagnosed by a Physician and deemed to be medically necessary. Treatment includes the purchase of medical foods and low protein modified food products. Inherited metabolic diseases means a disease caused by an inherited abnormality of body chemistry. A low protein modified food product is one that is specially formulated to have less than one gram of protein per serving. It is intended to be used under the direction of a Physician for the dietary treatment of an inherited metabolic disease, but does not include a (natural) food that is naturally low in protein. |
Medical food means one that is intended for the dietary treatment of a disease or condition for which nutritional requirements are established by medical evaluation and is formulated to be consumed or administered enterally under the direction of a Physician.
• | charges for screening for newborn hearing loss by electrophysiologic screening measures and periodic monitoring. Any deductible will be waived for newborn and infant hearing screening. |
• | charges for or in connection with a drug that has been prescribed for a treatment for which it has not been |
approved by the Food and Drug Administration (FDA). Such drug must be covered, provided: it is recognized as medically appropriate for that specific treatment in one of the following reference compendia: the American Medical Association Drug Evaluations; the American Hospital Formulary Service Drug Information; the United States Pharmacopeia Drug Information; or it is recommended by a clinical study or review article in a major peer-reviewed professional journal; and the drug has not been contraindicated by the FDA for the use prescribed.
• | charges for insulin, insulin syringes, prefilled insulin cartridges for the blind, glucose test strips, visual reading strips and urine test strips, lancets, alcohol swabs and oral blood sugar control agents which are recommended or prescribed by a Physician, nurse practitioner or clinical nurse specialist for the treatment of diabetes. Diabetic pharmaceuticals are payable at the same Deductible and Coinsurance as any other Covered Expense. |
• | charges for blood glucose monitors (including monitors for the blind), insulin pumps, infusion devices and related accessories. Charges for these items are not subject to the Durable Medical Equipment Maximum shown in The Schedule. |
• | charges for the diagnosis and treatment of autism and other developmental disabilities. |
For a primary diagnosis of autism or another developmental disability, Cigna provides coverage for the following medically necessary therapies as prescribed through a treatment plan:
• | occupational therapy where occupational therapy refers to treatment to develop a covered person’s ability to perform the ordinary tasks of daily living; |
• | physical therapy where physical therapy refers to treatment to develop a covered person’s physical function; and |
• | speech therapy where speech therapy speech therapy refers to treatment of a speech impairment. |
If a covered person’s primary diagnosis is autism, and the covered person is under 21 years of age, in addition to coverage for the therapy services as described above, Cigna also covers Medically Necessary behavioral interventions based on the principles of applied behavioral analysis and related structured behavioral programs as prescribed through a treatment plan. Except as stated below, such coverage of medically necessary behavioral interventions based on the principles of applied behavioral analysis and related structured behavioral programs is subject to a
$36,000 maximum benefit per calendar year for each year through 2011. (Thereafter the maximum benefit shall be adjusted by New Jersey regulation.)
_____________________________________________________________________________________________________________
13 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
Exception: If the Employer providing coverage under the Contract is subject to the Federal law governing parity in mental health and substance use disorder benefits the maximum benefit does not apply.
The treatment plan(s) referred to above must be in writing, signed by the treating physician, and must include: a diagnosis, proposed treatment by type, frequency and duration; the anticipated outcomes stated as goals; and the frequency by which the treatment plan will be updated.
Cigna may request additional information if necessary to determine the coverage under this plan. Cigna may require the submission of an updated treatment plan once every six months unless Cigna and the treating physician agree to more frequent updates.
Clinical Trials
Charges made for routine patient services associated with cancer clinical trials approved and sponsored by the federal government. In addition the following criteria must be met:
• | the cancer clinical trial is listed on the NIH web site www.clinicaltrials.gov as being sponsored by the federal government; |
• | the trial investigates a treatment for terminal cancer and: the person has failed standard therapies for the disease; cannot tolerate standard therapies for the disease; or no effective nonexperimental treatment for the disease exists; |
• | the person meets all inclusion criteria for the clinical trial and is not treated “off-protocol”; |
• | the trial is approved by the Institutional Review Board of the institution administering the treatment. |
Routine patient services do not include, and reimbursement will not be provided for:
• | the investigational service or supply itself; |
• | services or supplies listed herein as Exclusions; |
• | services or supplies related to data collection for the clinical trial (i.e., protocol-induced costs); |
• | services or supplies which, in the absence of private health care coverage, are provided by a clinical trial sponsor or other party (e.g., device, drug, item or service supplied by manufacturer and not yet FDA approved) without charge to the trial participant. |
Genetic Testing
Charges made for genetic testing that uses a proven testing method for the identification of genetically-linked inheritable disease. Genetic testing is covered only if:
• | a person has symptoms or signs of a genetically-linked inheritable disease; |
• | it has been determined that a person is at risk for carrier status as supported by existing peer-reviewed, evidence- |
based, scientific literature for the development of a genetically-linked inheritable disease when the results will impact clinical outcome; or
• | the therapeutic purpose is to identify specific genetic mutation that has been demonstrated in the existing peer- reviewed, evidence-based, scientific literature to directly impact treatment options. |
Pre-implantation genetic testing, genetic diagnosis prior to embryo transfer, is covered when either parent has an inherited disease or is a documented carrier of a genetically- linked inheritable disease.
Genetic counseling is covered if a person is undergoing approved genetic testing, or if a person has an inherited disease and is a potential candidate for genetic testing. Genetic counseling is limited to 3 visits per calendar year for both pre- and post-genetic testing.
Nutritional Evaluation
Charges made for nutritional evaluation and counseling when diet is a part of the medical management of a documented organic disease.
Internal Prosthetic/Medical Appliances
Charges made for internal prosthetic/medical appliances that provide permanent or temporary internal functional supports for nonfunctional body parts are covered. Medically Necessary repair, maintenance or replacement of a covered appliance is also covered.
Diabetic Services
Charges made for diabetic services, provided an official diagnosis of diabetes has been made by a Physician. Diabetic services include:
• | coverage for an annual screening via dilated eye examinations by a Physician for person with diabetes; |
• | glycohemoglobin A1c blood testing determination whenever needed to assess and achieve near-normal glycemia; and |
•microalbumin/urinalysis screening annually. Additional diabetic services include:
• | coverage for Medically Necessary fitting of therapeutic molded or depth-inlay shoes, replacement inserts, preventive devices and shoe modifications; |
• | calluses and nail trimming; |
• | complex evaluation of sensory loss; and |
• | treatment of ulcerations with total contact casting. |
_____________________________________________________________________________________________________________
14 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
Diabetic services will also include inpatient and outpatient
self-management training services provided by a Physician, by a certified diabetes educator, or by a registered pharmacist qualified to provide management education for diabetes:
• | according to standards established under New Jersey Department of Health and Senior Services regulations upon diagnosis of diabetes; or |
• | when a Physician certifies that a change in self-management is needed due to a change in symptoms or conditions, or that new medication, therapy or retraining is Medically Necessary. |
Covered training will also include nutrition therapy by a licensed, certified dietician or nutritionist and must be supervised and certified as completed successfully by a Physician.
Second Surgical Opinion Benefits
Covered Expenses will include expenses incurred for charges made for a second surgical opinion if, as a result of an Injury or a Sickness, you or any one of your Dependents, while insured for these benefits and prior to the performance of an Elective Surgical Procedure recommended by a surgeon, asks for an opinion from another Physician who is qualified to diagnose and treat that Injury or Sickness. Covered Expenses will also include any diagnostic laboratory or x-ray examinations asked for by the Physician who gives that opinion.
Payment will be made whether or not the Surgical Procedure is performed.
Third Surgical Opinion Benefits
If your second surgical opinion does not confirm that an Elective Surgical Procedure is medically advisable, a third surgical opinion will also be covered.
Limitations
No payment will be made for expenses incurred in connection with:
• | cosmetic or dental Surgical Procedures not covered under the policy; |
• | minor Surgical Procedures that are routinely performed in a Physician's office, such as incision and drainage for abscess or excision of benign lesions; |
• | an opinion rendered by the Physician who performs the Surgical Procedure. |
• | other limitations shown in the General Limitations section. |
No payment will be made under any other section to the extent that benefits are payable for incurred expenses under this section.
Elective Surgical Procedure
The term Elective Surgical Procedure means a Surgical Procedure which is not considered emergency in nature and which may be avoided without undue risk to the individual.
HC-COV42 | 04-10 | |||
V1 | ||||
General Limitations Supplemental Medical Benefits
No payment will be made for expenses incurred for you or any one of your Dependents for:
• | cosmetic surgery which does not meet any of the requirements listed under Covered Expenses. |
• | electrolysis or other hair removal procedures. |
• | illegal operations or treatments. |
• | controlled substances, including, but not limited to, marijuana or laetrile. |
• | nursing services for a normal, healthy infant. |
• | weight-loss programs for general health, even if a Physician prescribes the program. |
• | over-the-counter drugs or medications or any drug or medication that does not require a Physician's prescription for use, if used for general well-being or for purely cosmetic purposes. |
• | nicotine gum or nicotine patches. |
HC-MRP2 | 04-10 | |||
V1 | ||||
Payment of Benefits
To Whom Payable
Medical Benefits are assignable to the provider. When you assign benefits to a provider, you have assigned the entire amount of the benefits due on that claim. If the provider is overpaid because of accepting a patient’s payment on the charge, it is the provider’s responsibility to reimburse the patient. Because of Cigna’s contracts with providers, all claims from contracted providers should be assigned.
Cigna may, at its option, make payment to you for the cost of any Covered Expenses even if benefits have been assigned. When benefits are paid to you or your Dependent, you or your Dependents are responsible for reimbursing the provider.
_____________________________________________________________________________________________________________
15 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
If any person to whom benefits are payable is a minor or, in the opinion of Cigna is not able to give a valid receipt for any payment due him, such payment will be made to his legal guardian. If no request for payment has been made by his legal guardian, Cigna may, at its option, make payment to the person or institution appearing to have assumed his custody and support.
When one of our participants passes away, Cigna may receive notice that an executor of the estate has been established. The executor has the same rights as our insured and benefit payments for unassigned claims should be made payable to the executor.
Payment as described above will release Cigna from all liability to the extent of any payment made.
Time of Payment
Benefits will be paid by Cigna within 30 days after it receives a proper claim by electronic means and within 40 days after it receives a proper claim by other than electronic means. A claim will be considered to be properly submitted if it is an eligible claim for a health care service provided by a Physician to an insured; the claim has no material defect such as missing substantiating documentation or incorrect coding; there is no dispute regarding the amount of the claim; Cigna has no reason to believe the claim is fraudulent; and the claim requires no special treatment that prevents timely payment. If the claim is in whole or in part denied, ineligible, incomplete of substantiating documentation, miscoded or contains misinformation, the amount is in dispute, or requires special treatment, Cigna will in writing or by electronic means as appropriate, give an explanation of: denial, what documentation is needed to perfect a claim, a disputed claim amount, or a claim requiring extra time to process. Cigna will give notice of receipt of a claim by electronic means no later than two working days following receipt of the transmission of the claim. An overdue payment shall bear simple interest at the rate of 12% per annum.
Recovery of Overpayment
When an overpayment has been made by Cigna, Cigna will have the right, as permitted by New Jersey law, to: recover that overpayment from the person to whom or on whose behalf it was made; or offset the amount of that overpayment from a future claim payment.
Calculation of Covered Expenses
Cigna, in its discretion, will calculate Covered Expenses following evaluation and validation of all provider billings in accordance with:
• | the methodologies in the most recent edition of the Current Procedural terminology, |
• | the methodologies as reported by generally recognized professionals or publications. |
HC-POB3 | 04-10 | |||
V1 | ||||
Termination of Supplemental Medical Benefits
Employees
Your Supplemental Medical Benefits will cease on the earliest date below:
• | The date you cease to be in a Class of Eligible Employees or cease to qualify for the insurance. |
• | The date your coverage under the Employer's Group Medical Benefits Plan ceases. |
• | The date the Supplemental Medical Benefits policy is canceled. |
• | The date your Active Service ends except as described below. |
Any continuation of insurance must be based on a plan which precludes individual selection.
Temporary Layoff or Leave of Absence
If your Active Service ends due to temporary layoff or leave of absence, your insurance will be continued until the date your Employer: stops paying premium for you; or otherwise cancels your insurance. However, your insurance will not be continued for more than 60 days past the date your Active Service ends.
Injury or Sickness
If your Active Service ends due to an Injury or Sickness, your insurance will be continued while you remain totally and continuously disabled as a result of the Injury or Sickness.
However, your insurance will not continue past the date your Employer stops paying premium for you or otherwise cancels your insurance.
Dependents
Your Supplemental Medical Benefits for all of your Dependents will cease on the earliest date below:
• | The date you cease to be in a Class of Eligible Employees or cease to qualify for the insurance. |
• | The date your coverage under the Employer's Group Medical Benefits Plan ceases. |
• | The date the Supplemental Medical Benefits policy is canceled. |
_____________________________________________________________________________________________________________
16 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
The insurance for any one of your Dependents will cease on the date that Dependent no longer qualifies as a Dependent, as defined under the Employer's Group Medical Benefits Plan.
Any continuation of insurance with premium waiver set forth in the Employer-Sponsored Medical Benefits Plan will not apply to the insurance under this Supplemental Medical Benefits policy.
HC-TRM2 | 04-10 | |||
VI | ||||
Continuation
Special Continuation of Medical Insurance - Total Disability
If your insurance would otherwise cease due to total disability, and if you have been insured for at least three consecutive months under the policy, and if you pay your Employer the required premium, your Medical Insurance will be continued until the earliest of:
• | the last day for which you have paid the required premium; |
• | the date you become employed and eligible for similar insurance under another group policy for medical and dental benefits; |
• | the date the policy is canceled. |
Within 31 days after the date the insurance would otherwise cease, you may elect such continuation by completing a continuation notification and by paying the required premium to your Employer.
If your insurance is being continued as outlined above, the Medical Insurance for any of your Dependents insured on the date your insurance would otherwise cease may be continued, subject to the above provisions. The Dependent Medical Insurance will be continued until the earlier of:
• | the date your insurance ceases; or |
• | with respect to any one Dependent, the date that Dependent no longer qualifies as a Dependent. |
This option will not operate to reduce any continuation of insurance otherwise provided.
Continuation of Coverage for Dependent Children under New Jersey Law
A Dependent child of a Covered Person who meets the limiting age for coverage of a Dependent, is eligible to continue coverage for himself until his 31st birthday, provided he meets all of the following “Special Eligibility Criteria” for this continuation coverage:
• | is a Covered Person’s child by blood or by law; and |
• | has reached the limiting age as specified under his parents’ policy, but has not yet reached his 31st birthday; and |
• | is unmarried; and |
• | has no Dependents of his own; and |
• | is either a resident of New Jersey OR is enrolled as a full- time student at an accredited public or private institution of higher education; and |
• | is not covered under any other group or individual health benefits plan, and is not entitled to benefits under Medicare. |
To obtain continued coverage under this provision, the Dependent child must make a written election for continuation coverage as a Dependent, complete any necessary enrollment forms and pay the premium, at any of the following times:
• | within 30 days prior to the termination of coverage at the specific age provided in this Plan; or |
• | within 30 days after meeting the “Special Eligibility Criteria” requirements, when coverage for the Dependent under this Plan previously terminated; or |
• | during an open enrollment period, if provided in the Plan, if the Dependent child meets the “Special Eligibility Criteria” during the open enrollment period; or |
• | for the initial 12 months after the effective date of this legislation, from 5/12/2006 to 5/11/2007 only, a Dependent child meeting the “Special Eligibility Criteria” whose coverage as a Dependent under a Covered Person’s policy terminated prior to 5/12/2006 due to attainment of limiting age under such Covered Person’s policy. |
A Dependent child is only entitled to make an election for continued coverage if the Dependent child was actually covered under his parent’s Plan on the date he reached the limiting age and was terminated due to reaching such limiting age.
To continue group health benefits, the Dependent child must meet all of the requirements specified in this section and must make written election to us. The effective date of the Dependent child’s continued coverage will be the later of: the date the Dependent child requests continued coverage with us; or the date the Dependent meets all of the “Special Eligibility Criteria.” This continued coverage is conditional upon the Dependent child completing the required enrollment form and sending us the first month’s premium due. The Dependent child covered under this continuation benefit must pay subsequent premiums monthly, in advance, at the times and in the manner specified by us. Premium payments, other than the first premium payment, will be considered timely if payment is made no later than 30 days of the date such premium payment is due.
For a Dependent child whose coverage has not yet terminated due to the attainment of the limiting age as specified under this Plan, the written election must be made within 30 days prior to
_____________________________________________________________________________________________________________
17 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
termination of coverage due to the attainment of the limiting age.
For a Dependent child who did not qualify for this continued coverage because he fails to meet all the “Special Eligibility Criteria,” but who subsequently meets all of the “Special Eligibility Criteria,” written election must be made within 30 days after the Dependent child first subsequently meets all of the requirements.
This election opportunity for the Dependent child is explained in greater detail as follows:
• | If a Dependent child did not qualify because he or she was married, the notice must be given within 30 days of the date he or she is no longer married. |
• | If a Dependent child did not qualify because he had a Dependent of his own, the election must be made within 30 days of the date he no longer has a Dependent. |
• | If a Dependent child did not qualify because he either was not a resident of New Jersey or was not a full-time student at an accredited school, the election must be made within 30 days of the date he becomes a resident of New Jersey, or becomes a full-time student at an accredited school. |
• | If a Dependent child did not qualify because he was covered under any other group or individual health benefits plan, group health plan, church plan or health benefits plan, or was entitled to Medicare, the election must be made within 30 days of the date he is no longer covered under any other group or individual health benefits plan, group health plan, church plan or health benefits plan, or is no longer entitled to Medicare. |
Each year, there will be an Open Enrollment Period as specified under this Plan during which a Dependent child who previously did not elect to continue coverage, may make an election to continue coverage.
A Dependent child who qualifies for this continuation coverage as of May 12, 2006, having reached the limiting age under his parents’ plan and lost coverage prior to May 12, 2006 due to reaching such limiting age, may give written notice of an election for continued coverage at any time beginning May 12, 2006 and continuing until May 11, 2007.
A Dependent child who was covered under prior Creditable Coverage that terminated no more than 90 days prior to making an election for continuation under this section will be given credit for the time he was covered under the Creditable Coverage toward the application of the Pre-Existing Conditions Exclusion under the Policy.
The continued coverage shall be identical to the coverage provided to the Dependent child continuant’s parent who is covered as an Employee under this Plan. If coverage is modified for Dependents who are under the limiting age as specified in this Plan, the coverage for Dependent child
continuants shall also be modified in the same manner. Evidence of insurability is not required for the continued coverage.
The Group is required to notify the Dependent child in writing of the option to continue coverage and the duties of continuing coverage at the following times:
• | on/before the coverage of the Dependent terminates due to reaching the limiting age; and |
• | at the time coverage terminates because the Dependent child no longer meets the “Special Eligibility Criteria”, except |
that notice is not required when the Dependent child turns 30 or has a dependent of his own; and
• | before any open enrollment period; and |
• | immediately following 5/12/2006, for the subsequent 12 months. |
Continuation of coverage under this section will end on the earliest of the following dates:
• | the date ending the period for which premium has been paid for the Dependent child continuant, subject to the Grace Period for such payment; or |
• | the date the Group ceases to provide coverage to the Covered Person, who is the Dependent child’s parent; or |
• | the date the Plan under which the Dependent child continuing coverage is amended to delete coverage for Dependents; or |
• | the date the Dependent child ceases to continue to meet any of the “Special Eligibility Criteria” requirements; or |
• | the date the Dependent child’s parent who is covered as an Employee under this Plan waives Dependent coverage. Except, if the Employee has no other Dependents, the Dependent child continuant’s coverage will not end as a result of the Employee waiving Dependent coverage. |
HC-TRM12 | 04-10 | |||
VI | ||||
Rescissions
Your coverage may not be rescinded (retroactively terminated) by Cigna or the plan sponsor unless the plan sponsor or an individual (or a person seeking coverage on behalf of the individual) performs an act, practice or omission that constitutes fraud; or the plan sponsor or individual (or a person seeking coverage on behalf of the individual) makes an intentional misrepresentation of material fact.
HC-TRM80 | 01-11 | |||
_____________________________________________________________________________________________________________
18 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
Medical Benefits Extension Upon Policy Cancellation
If the Medical Benefits under this plan cease for you or your Dependent due to cancellation of the policy, and you are or you Dependent is Totally Disabled on that date due to an Injury or Sickness, Medical Benefits will be paid for Covered Expenses incurred in connection with that Injury or Sickness. However, no benefits will be paid after the earliest of:
• | the date you exceed the Maximum Benefit, if any, shown in the Schedule; |
• | the date you are covered for medical benefits under another group policy; |
• | the date you are no longer Totally Disabled (but only if benefits for that disabling condition are being paid for you under the replacing policy); |
• | 12 months from the date your Medical Benefits cease; or |
• | 12 months from the date the policy is canceled. |
Totally Disabled
You will be considered Totally Disabled if, because of an Injury or a Sickness:
• | you are unable to perform the basic duties of your occupation; and |
• | you are not performing any other work or engaging in any other occupation for wage or profit. |
Your Dependent will be considered Totally Disabled if, because of an Injury or a Sickness:
• | he is unable to engage in the normal activities of a person of the same age, sex and ability; or |
• | in the case of a Dependent who normally works for wage or profit, he is not performing such work. |
Please Note: The terms of this Medical Benefits Extension will not apply to a child born as a result of a pregnancy which exists when you or your Dependent's Medical Benefits cease.
HC-BEX10 | 04-10 | |||
V1 | ||||
Federal Requirements
The following pages explain your rights and responsibilities under federal laws and regulations. Some states may have similar requirements. If a similar provision appears elsewhere in this booklet, the provision which provides the better benefit will apply.
HC-FED1 | 10-10 | |||
Qualified Medical Child Support Order (QMCSO)
Eligibility for Coverage Under a QMCSO
If a Qualified Medical Child Support Order (QMCSO) is issued for your child, that child will be eligible for coverage as required by the order and you will not be considered a Late Entrant for Dependent Insurance.
You must notify your Employer and elect coverage for that child, and yourself if you are not already enrolled, within 31 days of the QMCSO being issued.
Qualified Medical Child Support Order Defined
A Qualified Medical Child Support Order is a judgment, decree or order (including approval of a settlement agreement) or administrative notice, which is issued pursuant to a state domestic relations law (including a community property law), or to an administrative process, which provides for child support or provides for health benefit coverage to such child and relates to benefits under the group health plan, and satisfies all of the following:
• | the order recognizes or creates a child’s right to receive group health benefits for which a participant or beneficiary is eligible; |
• | the order specifies your name and last known address, and the child’s name and last known address, except that the name and address of an official of a state or political subdivision may be substituted for the child’s mailing address; |
• | the order provides a description of the coverage to be provided, or the manner in which the type of coverage is to be determined; |
• | the order states the period to which it applies; and |
• | if the order is a National Medical Support Notice completed in accordance with the Child Support Performance and Incentive Act of 1998, such Notice meets the requirements above. |
The QMCSO may not require the health insurance policy to provide coverage for any type or form of benefit or option not otherwise provided under the policy, except that an order may require a plan to comply with State laws regarding health care coverage.
_____________________________________________________________________________________________________________
19 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
Payment of Benefits
Any payment of benefits in reimbursement for Covered Expenses paid by the child, or the child’s custodial parent or legal guardian, shall be made to the child, the child’s custodial parent or legal guardian, or a state official whose name and address have been substituted for the name and address of the child.
HC-FED4 | 10-10 | |||
Special Enrollment Rights Under the Health Insurance Portability & Accountability Act (HIPAA)
If you or your eligible Dependent(s) experience a special enrollment event as described below, you or your eligible Dependent(s) may be entitled to enroll in the Plan outside of a designated enrollment period upon the occurrence of one of the special enrollment events listed below. If you are already enrolled in the Plan, you may request enrollment for you and your eligible Dependent(s) under a different option offered by the Employer for which you are currently eligible. If you are not already enrolled in the Plan, you must request special enrollment for yourself in addition to your eligible Dependent(s). You and all of your eligible Dependent(s) must be covered under the same option. The special enrollment events include:
• | Acquiring a new Dependent. If you acquire a new Dependent(s) through marriage, birth, adoption or placement for adoption, you may request special enrollment for any of the following combinations of individuals if not already enrolled in the Plan: Employee only; spouse only; Employee and spouse; Dependent child(ren) only; Employee and Dependent child(ren); Employee, spouse and Dependent child(ren). Enrollment of Dependent children is limited to the newborn or adopted children or children who became Dependent children of the Employee due to marriage. |
• | Loss of eligibility for State Medicaid or Children’s Health Insurance Program (CHIP). If you and/or your Dependent(s) were covered under a state Medicaid or CHIP plan and the coverage is terminated due to a loss of eligibility, you may request special enrollment for yourself and any affected Dependent(s) who are not already enrolled in the Plan. You must request enrollment within 60 days after termination of Medicaid or CHIP coverage. |
• | Loss of eligibility for other coverage (excluding continuation coverage). If coverage was declined under this Plan due to coverage under another plan, and eligibility for the other coverage is lost, you and all of your eligible |
Dependent(s) may request special enrollment in this Plan. If required by the Plan, when enrollment in this Plan was
previously declined, it must have been declined in writing with a statement that the reason for declining enrollment was due to other health coverage. This provision applies to loss of eligibility as a result of any of the following:
• | divorce or legal separation; |
• | cessation of Dependent status (such as reaching the limiting age); |
• | death of the Employee; |
• | termination of employment; |
• | reduction in work hours to below the minimum required for eligibility; |
• | you or your Dependent(s) no longer reside, live or work in the other plan’s network service area and no other coverage is available under the other plan; |
• | you or your Dependent(s) incur a claim which meets or exceeds the lifetime maximum limit that is applicable to all benefits offered under the other plan; or |
• | the other plan no longer offers any benefits to a class of similarly situated individuals. |
• | Termination of employer contributions (excluding continuation coverage). If a current or former employer ceases all contributions toward the Employee’s or Dependent’s other coverage, special enrollment may be requested in this Plan for you and all of your eligible Dependent(s). |
• | Exhaustion of COBRA or other continuation coverage. Special enrollment may be requested in this Plan for you and all of your eligible Dependent(s) upon exhaustion of COBRA or other continuation coverage. If you or your Dependent(s) elect COBRA or other continuation coverage following loss of coverage under another plan, the COBRA or other continuation coverage must be exhausted before any special enrollment rights exist under this Plan. An individual is considered to have exhausted COBRA or other continuation coverage only if such coverage ceases: due to failure of the employer or other responsible entity to remit premiums on a timely basis; when the person no longer resides or works in the other plan’s service area and there is no other COBRA or continuation coverage available under the plan; or when the individual incurs a claim that would meet or exceed a lifetime maximum limit on all benefits and there is no other COBRA or other continuation coverage available to the individual. This does not include termination of an employer’s limited period of contributions toward COBRA or other continuation coverage as provided under any severance or other agreement. |
• | Eligibility for employment assistance under State Medicaid or Children’s Health Insurance Program |
_____________________________________________________________________________________________________________
20 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
(CHIP). If you and/or your Dependent(s) become eligible for assistance with group health plan premium payments under a state Medicaid or CHIP plan, you may request special enrollment for yourself and any affected Dependent(s) who are not already enrolled in the Plan. You must request enrollment within 60 days after the date you are determined to be eligible for assistance.
Except as stated above, special enrollment must be requested within 30 days after the occurrence of the special enrollment event. If the special enrollment event is the birth or adoption of a Dependent child, coverage will be effective immediately on the date of birth, adoption or placement for adoption. Coverage with regard to any other special enrollment event will be effective no later than the first day of the first calendar month following receipt of the request for special enrollment.
Domestic Partners and their children (if not legal children of the Employee) are not eligible for special enrollment.
HC-FED71 | 12-14 | |||
VI | ||||
Effect of Section 125 Tax Regulations on This Plan
Your Employer has chosen to administer this Plan in accordance with Section 125 regulations of the Internal Revenue Code. Per this regulation, you may agree to a pretax salary reduction put toward the cost of your benefits.
Otherwise, you will receive your taxable earnings as cash (salary).
A.Coverage Elections
Per Section 125 regulations, you are generally allowed to enroll for or change coverage only before each annual benefit period. However, exceptions are allowed if your Employer agrees and you enroll for or change coverage within 30 days of the following:
• | the date you meet the Special Enrollment criteria described above; or |
• | the date you meet the criteria shown in the following Sections B through H. |
B. | Change of Status |
A change in status is defined as:
• | change in legal marital status due to marriage, death of a spouse, divorce, annulment or legal separation; |
• | change in number of Dependents due to birth, adoption, placement for adoption, or death of a Dependent; |
• | change in employment status of Employee, spouse or Dependent due to termination or start of employment, strike, lockout, beginning or end of unpaid leave of absence, including under the Family and Medical Leave Act (FMLA), or change in worksite; |
• | changes in employment status of Employee, spouse or Dependent resulting in eligibility or ineligibility for coverage; |
• | change in residence of Employee, spouse or Dependent to a location outside of the Employer’s network service area; and |
• | changes which cause a Dependent to become eligible or ineligible for coverage. |
C. | Court Order |
A change in coverage due to and consistent with a court order of the Employee or other person to cover a Dependent.
D. | Medicare or Medicaid Eligibility/Entitlement |
The Employee, spouse or Dependent cancels or reduces coverage due to entitlement to Medicare or Medicaid, or enrolls or increases coverage due to loss of Medicare or Medicaid eligibility.
E. | Change in Cost of Coverage |
If the cost of benefits increases or decreases during a benefit period, your Employer may, in accordance with plan terms, automatically change your elective contribution.
When the change in cost is significant, you may either increase your contribution or elect less-costly coverage. When a significant overall reduction is made to the benefit option you have elected, you may elect another available benefit option. When a new benefit option is added, you may change your election to the new benefit option.
F.Changes in Coverage of Spouse or Dependent Under Another Employer’s Plan
You may make a coverage election change if the plan of your spouse or Dependent: incurs a change such as adding or deleting a benefit option; allows election changes due to Special Enrollment, Change in Status, Court Order or Medicare or Medicaid Eligibility/Entitlement; or this Plan and the other plan have different periods of coverage or open enrollment periods.
G. | Reduction in work hours |
If an Employee’s work hours are reduced below 30 hours/week (even if it does not result in the Employee losing eligibility for the Employer’s coverage); and the Employee (and family) intend to enroll in another plan that provides Minimum Essential Coverage (MEC). The new coverage must be effective no later than the 1st day of the 2nd month following the month that includes the date the original coverage is revoked.
_____________________________________________________________________________________________________________
21 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
H. Enrollment in Qualified Health Plan (QHP)
The Employee must be eligible for a Special Enrollment Period to enroll in a QHP through a Marketplace or the Employee wants to enroll in a QHP through a Marketplace during the Marketplace’s annual open enrollment period; and the disenrollment from the group plan corresponds to the intended enrollment of the Employee (and family) in a QHP through a Marketplace for new coverage effective beginning no later than the day immediately following the last day of the original coverage.
HC-FED70 | 12-14 | |||
Eligibility for Coverage for Adopted Children
Any child who is adopted by you, including a child who is placed with you for adoption, will be eligible for Dependent Insurance, if otherwise eligible as a Dependent, upon the date of placement with you. A child will be considered placed for adoption when you become legally obligated to support that child, totally or partially, prior to that child’s adoption.
If a child placed for adoption is not adopted, all health coverage ceases when the placement ends, and will not be continued.
The provisions in the “Exception for Newborns” section of this document that describe requirements for enrollment and effective date of insurance will also apply to an adopted child or a child placed with you for adoption.
HC-FED67 | 09-14 | |||
Coverage for Maternity Hospital Stay
Under federal law, group health plans and health insurance issuers offering group health insurance coverage generally may not restrict benefits for any hospital length of stay in connection with childbirth for the mother or newborn child to less than 48 hours following a vaginal delivery, or less than 96 hours following a delivery by cesarean section. However, the plan or issuer may pay for a shorter stay if the attending provider (e.g., your physician, nurse midwife, or physician assistant), after consultation with the mother, discharges the mother or newborn earlier.
Also, under federal law, plans and issuers may not set the level of benefits or out-of-pocket costs so that any later portion of the 48-hour (or 96-hour) stay is treated in a manner less favorable to the mother or newborn than any earlier portion of the stay.
In addition, a plan or issuer may not, under federal law, require that a physician or other health care provider obtain authorization for prescribing a length of stay of up to 48 hours (or 96 hours). However, to use certain providers or facilities, or to reduce your out-of-pocket costs, you may be required to obtain precertification. For information on precertification, contact your plan administrator.
HC-FED10 | 10-10 | |||
Women’s Health and Cancer Rights Act (WHCRA)
Do you know that your plan, as required by the Women’s Health and Cancer Rights Act of 1998, provides benefits for mastectomy-related services including all stages of reconstruction and surgery to achieve symmetry between the breasts, prostheses, and complications resulting from a mastectomy, including lymphedema? Call Member Services at the toll free number listed on your ID card for more information.
HC-FED12 | 10-10 | |||
Group Plan Coverage Instead of Medicaid
If your income and liquid resources do not exceed certain limits established by law, the state may decide to pay premiums for this coverage instead of for Medicaid, if it is cost effective. This includes premiums for continuation coverage required by federal law.
HC-FED13 | 10-10 | |||
Requirements of Medical Leave Act of 1993 (as amended) (FMLA)
Any provisions of the policy that provide for: continuation of insurance during a leave of absence; and reinstatement of insurance following a return to Active Service; are modified by the following provisions of the federal Family and Medical Leave Act of 1993, as amended, where applicable:
Continuation of Health Insurance During Leave
Your health insurance will be continued during a leave of absence if:
• | that leave qualifies as a leave of absence under the Family and Medical Leave Act of 1993, as amended; and |
_____________________________________________________________________________________________________________
22 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
• | you are an eligible Employee under the terms of that Act. |
The cost of your health insurance during such leave must be paid, whether entirely by your Employer or in part by you and your Employer.
Reinstatement of Canceled Insurance Following Leave
Upon your return to Active Service following a leave of absence that qualifies under the Family and Medical Leave Act of 1993, as amended, any canceled insurance (health, life or disability) will be reinstated as of the date of your return.
You will not be required to satisfy any eligibility or benefit waiting period to the extent that they had been satisfied prior to the start of such leave of absence.
Your Employer will give you detailed information about the Family and Medical Leave Act of 1993, as amended.
HC-FED17 | 10-10 | |||
Uniformed Services Employment and Re- Employment Rights Act of 1994 (USERRA)
The Uniformed Services Employment and Re-employment Rights Act of 1994 (USERRA) sets requirements for continuation of health coverage and re-employment in regard to an Employee’s military leave of absence. These requirements apply to medical and dental coverage for you and your Dependents. They do not apply to any Life, Short- term or Long-term Disability or Accidental Death & Dismemberment coverage you may have.
Continuation of Coverage
For leaves of less than 31 days, coverage will continue as described in the Termination section regarding Leave of Absence.
For leaves of 31 days or more, you may continue coverage for yourself and your Dependents as follows:
You may continue benefits by paying the required premium to your Employer, until the earliest of the following:
• | 24 months from the last day of employment with the Employer; |
• | the day after you fail to return to work; and |
• | the date the policy cancels. |
Your Employer may charge you and your Dependents up to 102% of the total premium.
Reinstatement of Benefits (applicable to all coverages)
If your coverage ends during the leave of absence because you do not elect USERRA at the expiration of USERRA and you are reemployed by your current Employer, coverage for you and your Dependents may be reinstated if you gave your
Employer advance written or verbal notice of your military service leave, and the duration of all military leaves while you are employed with your current Employer does not exceed 5 years.
You and your Dependents will be subject to only the balance of a waiting period that was not yet satisfied before the leave began. However, if an Injury or Sickness occurs or is aggravated during the military leave, full Plan limitations will apply.
If your coverage under this plan terminates as a result of your eligibility for military medical and dental coverage and your order to active duty is canceled before your active duty service commences, these reinstatement rights will continue to apply.
HC-FED18 | 10-10 | |||
Claim Determination Procedures under ERISA
The following complies with federal law. Provisions of applicable laws of your state may supersede.
Procedures Regarding Medical Necessity Determinations
In general, health services and benefits must be Medically Necessary to be covered under the plan. The procedures for determining Medical Necessity vary, according to the type of service or benefit requested, and the type of health plan.
Medical Necessity determinations are made on a preservice, concurrent, or postservice basis, as described below:
Certain services require prior authorization in order to be covered. The Certificate describes who is responsible for obtaining this review. You or your authorized representative (typically, your health care professional) must request prior authorization according to the procedures described below, in the Certificate, and in your provider’s network participation documents as applicable.
When services or benefits are determined to be not covered, you or your representative will receive a written description of the adverse determination, and may appeal the determination. Appeal procedures are described in the Certificate, in your provider’s network participation documents as applicable, and in the determination notices.
Preservice Determinations
When you or your representative requests a required prior authorization, Cigna will notify you or your representative of the determination within 15 days after receiving the request. However, if more time is needed due to matters beyond Cigna’s control, Cigna will notify you or your representative within 15 days after receiving your request. This notice will include the date a determination can be expected, which will be no more than 30 days after receipt of the request. If more
_____________________________________________________________________________________________________________
23 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
time is needed because necessary information is missing from the request, the notice will also specify what information is needed, and you or your representative must provide the specified information to Cigna within 45 days after receiving the notice. The determination period will be suspended on the date Cigna sends such a notice of missing information, and the determination period will resume on the date you or your representative responds to the notice.
If the determination periods above would seriously jeopardize your life or health, your ability to regain maximum function, or in the opinion of a health care professional with knowledge of your health condition, cause you severe pain which cannot be managed without the requested services, Cigna will make the preservice determination on an expedited basis. Cigna's reviewer, in consultation with the treating health care professional, will decide if an expedited determination is necessary. Cigna will notify you or your representative of an expedited determination within 72 hours after receiving the request.
However, if necessary information is missing from the request, Cigna will notify you or your representative within 24 hours after receiving the request to specify what information is needed. You or your representative must provide the specified information to Cigna within 48 hours after receiving the notice. Cigna will notify you or your representative of the expedited benefit determination within 48 hours after you or your representative responds to the notice. Expedited determinations may be provided orally, followed within 3 days by written or electronic notification.
If you or your representative fails to follow Cigna’s procedures for requesting a required preservice determination, Cigna will notify you or your representative of the failure and describe the proper procedures for filing within 5 days (or 24 hours, if an expedited determination is required, as described above) after receiving the request. This notice may be provided orally, unless you or your representative requests written notification.
Concurrent Determinations
When an ongoing course of treatment has been approved for you and you wish to extend the approval, you or your representative must request a required concurrent coverage determination at least 24 hours prior to the expiration of the approved period of time or number of treatments. When you or your representative requests such a determination, Cigna will notify you or your representative of the determination within 24 hours after receiving the request.
Postservice Determinations
When you or your representative requests a coverage determination or a claim payment determination after services have been rendered, Cigna will notify you or your representative of the determination within 30 days after
receiving the request. However, if more time is needed to
make a determination due to matters beyond Cigna’s control, Cigna will notify you or your representative within 30 days after receiving the request. This notice will include the date a determination can be expected, which will be no more than 45 days after receipt of the request.
If more time is needed because necessary information is missing from the request, the notice will also specify what information is needed, and you or your representative must provide the specified information to Cigna within 45 days after receiving the notice. The determination period will be suspended on the date Cigna sends such a notice of missing information, and the determination period will resume on the date you or your representative responds to the notice.
Notice of Adverse Determination
Every notice of an adverse benefit determination will be provided in writing or electronically, and will include all of the following that pertain to the determination: the specific reason or reasons for the adverse determination; reference to the specific plan provisions on which the determination is based; a description of any additional material or information necessary to perfect the claim and an explanation of why such material or information is necessary; a description of the plan’s review procedures and the time limits applicable, including a statement of a claimant’s rights to bring a civil action under section 502(a) of ERISA following an adverse benefit determination on appeal, (if applicable); upon request and free of charge, a copy of any internal rule, guideline, protocol or other similar criterion that was relied upon in making the adverse determination regarding your claim; and an explanation of the scientific or clinical judgment for a determination that is based on a Medical Necessity, experimental treatment or other similar exclusion or limit; and in the case of a claim involving urgent care, a description of the expedited review process applicable to such claim.
HC-FED79 | 03-13 | |||
COBRA Continuation Rights Under Federal Law
For You and Your Dependents
What is COBRA Continuation Coverage?
Under federal law, you and/or your Dependents must be given the opportunity to continue health insurance when there is a “qualifying event” that would result in loss of coverage under the Plan. You and/or your Dependents will be permitted to continue the same coverage under which you or your Dependents were covered on the day before the qualifying event occurred, unless you move out of that plan’s coverage
_____________________________________________________________________________________________________________
24 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
area or the plan is no longer available. You and/or your Dependents cannot change coverage options until the next open enrollment period.
When is COBRA Continuation Available?
For you and your Dependents, COBRA continuation is available for up to 18 months from the date of the following qualifying events if the event would result in a loss of coverage under the Plan:
• | your termination of employment for any reason, other than gross misconduct; or |
• | your reduction in work hours. |
For your Dependents, COBRA continuation coverage is available for up to 36 months from the date of the following qualifying events if the event would result in a loss of coverage under the Plan:
• | your death; |
• | your divorce or legal separation; or |
• | for a Dependent child, failure to continue to qualify as a Dependent under the Plan. |
Who is Entitled to COBRA Continuation?
Only a “qualified beneficiary” (as defined by federal law) may elect to continue health insurance coverage. A qualified beneficiary may include the following individuals who were covered by the Plan on the day the qualifying event occurred: you, your spouse, and your Dependent children. Each qualified beneficiary has their own right to elect or decline COBRA continuation coverage even if you decline or are not eligible for COBRA continuation.
The following individuals are not qualified beneficiaries for purposes of COBRA continuation: domestic partners, grandchildren (unless adopted by you), stepchildren (unless adopted by you). Although these individuals do not have an independent right to elect COBRA continuation coverage, if you elect COBRA continuation coverage for yourself, you may also cover your Dependents even if they are not considered qualified beneficiaries under COBRA. However, such individuals’ coverage will terminate when your COBRA continuation coverage terminates. The sections titled “Secondary Qualifying Events” and “Medicare Extension For Your Dependents” are not applicable to these individuals.
Secondary Qualifying Events
If, as a result of your termination of employment or reduction in work hours, your Dependent(s) have elected COBRA continuation coverage and one or more Dependents experience another COBRA qualifying event, the affected Dependent(s) may elect to extend their COBRA continuation coverage for an additional 18 months (7 months if the secondary event occurs within the disability extension period) for a maximum of 36 months from the initial qualifying event. The second
qualifying event must occur before the end of the initial 18 months of COBRA continuation coverage or within the disability extension period discussed below. Under no
circumstances will COBRA continuation coverage be available for more than 36 months from the initial qualifying event. Secondary qualifying events are: your death; your divorce or legal separation; or, for a Dependent child, failure to continue to qualify as a Dependent under the Plan.
Disability Extension
If, after electing COBRA continuation coverage due to your termination of employment or reduction in work hours, you or one of your Dependents is determined by the Social Security Administration (SSA) to be totally disabled under Title II or XVI of the SSA, you and all of your Dependents who have elected COBRA continuation coverage may extend such continuation for an additional 11 months, for a maximum of 29 months from the initial qualifying event.
To qualify for the disability extension, all of the following requirements must be satisfied:
• | SSA must determine that the disability occurred prior to or within 60 days after the disabled individual elected COBRA continuation coverage; and |
• | A copy of the written SSA determination must be provided to the Plan Administrator within 60 calendar days after the date the SSA determination is made AND before the end of the initial 18-month continuation period. |
If the SSA later determines that the individual is no longer disabled, you must notify the Plan Administrator within 30 days after the date the final determination is made by SSA. The 11-month disability extension will terminate for all covered persons on the first day of the month that is more than 30 days after the date the SSA makes a final determination that the disabled individual is no longer disabled.
All causes for “Termination of COBRA Continuation” listed below will also apply to the period of disability extension.
Medicare Extension for Your Dependents
When the qualifying event is your termination of employment or reduction in work hours and you became enrolled in Medicare (Part A, Part B or both) within the 18 months before the qualifying event, COBRA continuation coverage for your Dependents will last for up to 36 months after the date you became enrolled in Medicare. Your COBRA continuation coverage will last for up to 18 months from the date of your termination of employment or reduction in work hours.
Termination of COBRA Continuation
COBRA continuation coverage will be terminated upon the occurrence of any of the following:
• | the end of the COBRA continuation period of 18, 29 or 36 months, as applicable; |
_____________________________________________________________________________________________________________
25 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
• | failure to pay the required premium within 30 calendar days after the due date; |
• | cancellation of the Employer’s policy with Cigna; |
• | after electing COBRA continuation coverage, a qualified beneficiary enrolls in Medicare (Part A, Part B, or both); |
• | after electing COBRA continuation coverage, a qualified beneficiary becomes covered under another group health plan, unless the qualified beneficiary has a condition for which the new plan limits or excludes coverage under a pre- existing condition provision. In such case coverage will continue until the earliest of: the end of the applicable maximum period; the date the pre-existing condition provision is no longer applicable; or the occurrence of an event described in one of the first three bullets above; |
• | any reason the Plan would terminate coverage of a participant or beneficiary who is not receiving continuation coverage (e.g., fraud). |
Employer’s Notification Requirements
Your Employer is required to provide you and/or your Dependents with the following notices:
• | An initial notification of COBRA continuation rights must be provided within 90 days after your (or your spouse’s) coverage under the Plan begins (or the Plan first becomes subject to COBRA continuation requirements, if later). If you and/or your Dependents experience a qualifying event before the end of that 90-day period, the initial notice must be provided within the time frame required for the COBRA continuation coverage election notice as explained below. |
• | A COBRA continuation coverage election notice must be provided to you and/or your Dependents within the following timeframes: |
• | if the Plan provides that COBRA continuation coverage and the period within which an Employer must notify the Plan Administrator of a qualifying event starts upon the loss of coverage, 44 days after loss of coverage under the Plan; |
• | if the Plan provides that COBRA continuation coverage and the period within which an Employer must notify the Plan Administrator of a qualifying event starts upon the occurrence of a qualifying event, 44 days after the qualifying event occurs; or |
• | in the case of a multi-employer plan, no later than 14 days after the end of the period in which Employers must provide notice of a qualifying event to the Plan Administrator. |
How to Elect COBRA Continuation Coverage
The COBRA coverage election notice will list the individuals who are eligible for COBRA continuation coverage and inform you of the applicable premium. The notice will also
include instructions for electing COBRA continuation coverage. You must notify the Plan Administrator of your election no later than the due date stated on the COBRA election notice. If a written election notice is required, it must be post-marked no later than the due date stated on the COBRA election notice. If you do not make proper notification by the due date shown on the notice, you and your Dependents will lose the right to elect COBRA continuation coverage. If you reject COBRA continuation coverage before the due date, you may change your mind as long as you furnish a completed election form before the due date.
Each qualified beneficiary has an independent right to elect COBRA continuation coverage. Continuation coverage may be elected for only one, several, or for all Dependents who are qualified beneficiaries. Parents may elect to continue coverage on behalf of their Dependent children. You or your spouse may elect continuation coverage on behalf of all the qualified beneficiaries. You are not required to elect COBRA continuation coverage in order for your Dependents to elect COBRA continuation.
How Much Does COBRA Continuation Coverage Cost?
Each qualified beneficiary may be required to pay the entire cost of continuation coverage. The amount may not exceed 102% of the cost to the group health plan (including both Employer and Employee contributions) for coverage of a similarly situated active Employee or family member. The premium during the 11-month disability extension may not exceed 150% of the cost to the group health plan (including both employer and employee contributions) for coverage of a similarly situated active Employee or family member.
For example: If the Employee alone elects COBRA continuation coverage, the Employee will be charged 102% (or 150%) of the active Employee premium. If the spouse or one Dependent child alone elects COBRA continuation coverage, they will be charged 102% (or 150%) of the active Employee premium. If more than one qualified beneficiary elects COBRA continuation coverage, they will be charged 102% (or 150%) of the applicable family premium.
When and How to Pay COBRA Premiums
First payment for COBRA continuation
If you elect COBRA continuation coverage, you do not have to send any payment with the election form. However, you must make your first payment no later than 45 calendar days after the date of your election. (This is the date the Election Notice is postmarked, if mailed.) If you do not make your first payment within that 45 days, you will lose all COBRA continuation rights under the Plan.
Subsequent payments
After you make your first payment for COBRA continuation coverage, you will be required to make subsequent payments of the required premium for each additional month of
_____________________________________________________________________________________________________________
26 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
coverage. Payment is due on the first day of each month. If you make a payment on or before its due date, your coverage under the Plan will continue for that coverage period without any break.
Grace periods for subsequent payments
Although subsequent payments are due by the first day of the month, you will be given a grace period of 30 days after the first day of the coverage period to make each monthly payment. Your COBRA continuation coverage will be provided for each coverage period as long as payment for that coverage period is made before the end of the grace period for that payment. However, if your payment is received after the due date, your coverage under the Plan may be suspended during this time. Any providers who contact the Plan to confirm coverage during this time may be informed that coverage has been suspended. If payment is received before the end of the grace period, your coverage will be reinstated back to the beginning of the coverage period. This means that any claim you submit for benefits while your coverage is suspended may be denied and may have to be resubmitted once your coverage is reinstated. If you fail to make a payment before the end of the grace period for that coverage period, you will lose all rights to COBRA continuation coverage under the Plan.
You Must Give Notice of Certain Qualifying Events
If you or your Dependent(s) experience one of the following qualifying events, you must notify the Plan Administrator within 60 calendar days after the later of the date the qualifying event occurs or the date coverage would cease as a result of the qualifying event:
• | Your divorce or legal separation; or |
• | Your child ceases to qualify as a Dependent under the Plan. |
• | The occurrence of a secondary qualifying event as discussed under “Secondary Qualifying Events” above (this notice must be received prior to the end of the initial 18- or 29- month COBRA period). |
(Also refer to the section titled “Disability Extension” for additional notice requirements.)
Notice must be made in writing and must include: the name of the Plan, name and address of the Employee covered under the Plan, name and address(es) of the qualified beneficiaries affected by the qualifying event; the qualifying event; the date the qualifying event occurred; and supporting documentation (e.g., divorce decree, birth certificate, disability determination, etc.).
Newly Acquired Dependents
If you acquire a new Dependent through marriage, birth, adoption or placement for adoption while your coverage is being continued, you may cover such Dependent under your COBRA continuation coverage. However, only your newborn
or adopted Dependent child is a qualified beneficiary and may continue COBRA continuation coverage for the remainder of the coverage period following your early
termination of COBRA coverage or due to a secondary qualifying event.
COBRA coverage for your Dependent spouse and any Dependent children who are not your children (e.g., stepchildren or grandchildren) will cease on the date your COBRA coverage ceases and they are not eligible for a secondary qualifying event.
COBRA Continuation for Retirees Following Employer’s Bankruptcy
If you are covered as a retiree, and a proceeding in bankruptcy is filed with respect to the Employer under Title 11 of the United States Code, you may be entitled to COBRA continuation coverage. If the bankruptcy results in a loss of coverage for you, your Dependents or your surviving spouse within one year before or after such proceeding, you and your covered Dependents will become COBRA qualified beneficiaries with respect to the bankruptcy. You will be entitled to COBRA continuation coverage until your death.
Your surviving spouse and covered Dependent children will be entitled to COBRA continuation coverage for up to 36 months following your death. However, COBRA continuation coverage will cease upon the occurrence of any of the events listed under “Termination of COBRA Continuation” above.
Interaction With Other Continuation Benefits
You may be eligible for other continuation benefits under state law. Refer to the Termination section for any other continuation benefits.
HC-FED66 | 07-14 | |||
ERISA Required Information
The name of the Plan is:
Consolidated Edison Company of New York
The name, address, ZIP code and business telephone number of the sponsor of the Plan is:
Consolidated Edison Company 4 Irving Place, Room 1100 New York, NY 10003
212-780-8211
Employer Identification Number (EIN): | Plan Number: |
135009340 | 501 |
The name, address, ZIP code and business telephone number of the Plan Administrator is:
Employer named above
_____________________________________________________________________________________________________________
27 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
The name, address and ZIP code of the person designated as agent for service of legal process is:
Employer named above
The office designated to consider the appeal of denied claims is:
The Cigna Claim Office responsible for this Plan
The cost of the Plan is shared by Employee and Employer. The Plan’s fiscal year ends on 12/31.
The preceding pages set forth the eligibility requirements and benefits provided for you under this Plan.
Plan Trustees
A list of any Trustees of the Plan, which includes name, title and address, is available upon request to the Plan Administrator.
Plan Type
The plan is a healthcare benefit plan.
Collective Bargaining Agreements
You may contact the Plan Administrator to determine whether the Plan is maintained pursuant to one or more collective bargaining agreements and if a particular Employer is a sponsor. A copy is available for examination from the Plan Administrator upon written request.
Discretionary Authority
The Plan Administrator delegates to Cigna the discretionary authority to interpret and apply plan terms and to make factual determinations in connection with its review of claims under the plan. Such discretionary authority is intended to include, but not limited to, the determination of the eligibility of persons desiring to enroll in or claim benefits under the plan, the determination of whether a person is entitled to benefits under the plan, and the computation of any and all benefit payments. The Plan Administrator also delegates to Cigna the discretionary authority to perform a full and fair review, as required by ERISA, of each claim denial which has been appealed by the claimant or his duly authorized representative.
Plan Modification, Amendment and Termination
The Employer as Plan Sponsor reserves the right to, at any time, change or terminate benefits under the Plan, to change or terminate the eligibility of classes of employees to be covered by the Plan, to amend or eliminate any other plan term or condition, and to terminate the whole plan or any part of it.
Contact the Employer for the procedure by which benefits may be changed or terminated, by which the eligibility of classes of employees may be changed or terminated, or by which part or all of the Plan may be terminated. No consent of any participant is required to terminate, modify, amend or change the Plan.
Termination of the Plan together with termination of the insurance policy(s) which funds the Plan benefits will have no adverse effect on any benefits to be paid under the policy(s) for any covered medical expenses incurred prior to the date that policy(s) terminates. Likewise, any extension of benefits under the policy(s) due to you or your Dependent's total disability which began prior to and has continued beyond the date the policy(s) terminates will not be affected by the Plan termination. Rights to purchase limited amounts of life and medical insurance to replace part of the benefits lost because the policy(s) terminated may arise under the terms of the policy(s). A subsequent Plan termination will not affect the extension of benefits and rights under the policy(s).
Your coverage under the Plan’s insurance policy(s) will end on the earliest of the following dates:
• | the date you leave Active Service (or later as explained in the Termination Section;) |
• | the date you are no longer in an eligible class; |
• | if the Plan is contributory, the date you cease to contribute; |
• | the date the policy(s) terminates. |
See your Plan Administrator to determine if any extension of benefits or rights are available to you or your Dependents under this policy(s). No extension of benefits or rights will be available solely because the Plan terminates.
Statement of Rights
As a participant in the plan you are entitled to certain rights and protections under the Employee Retirement Income Security Act of 1974 (ERISA). ERISA provides that all plan participants shall be entitled to:
Receive Information About Your Plan and Benefits
• | examine, without charge, at the Plan Administrator’s office and at other specified locations, such as worksites and union halls, all documents governing the plan, including insurance contracts and collective bargaining agreements and a copy of the latest annual report (Form 5500 Series) filed by the plan with the U.S. Department of Labor and available at the Public Disclosure room of the Employee Benefits Security Administration. |
• | obtain, upon written request to the Plan Administrator, copies of documents governing the Plan, including insurance contracts and collective bargaining agreements, and a copy of the latest annual report (Form 5500 Series) and updated summary plan description. The administrator may make a reasonable charge for the copies. |
• | receive a summary of the Plan’s annual financial report. The Plan Administrator is required by law to furnish each person under the Plan with a copy of this summary financial report. |
_____________________________________________________________________________________________________________
28 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
Continue Group Health Plan Coverage
• | continue health care coverage for yourself, your spouse or Dependents if there is a loss of coverage under the Plan as a result of a qualifying event. You or your Dependents may have to pay for such coverage. Review the documents governing the Plan on the rules governing your federal continuation coverage rights. |
Prudent Actions by Plan Fiduciaries
In addition to creating rights for plan participants, ERISA imposes duties upon the people responsible for the operation of the employee benefit plan. The people who operate your plan, called “fiduciaries” of the Plan, have a duty to do so prudently and in the interest of you and other plan participants and beneficiaries. No one, including your employer, your union, or any other person may fire you or otherwise discriminate against you in any way to prevent you from obtaining a welfare benefit or exercising your rights under ERISA. If your claim for a welfare benefit is denied or ignored you have a right to know why this was done, to obtain copies of documents relating to the decision without charge, and to appeal any denial, all within certain time schedules.
Enforce Your Rights
Under ERISA, there are steps you can take to enforce the above rights. For instance, if you request a copy of documents governing the plan or the latest annual report from the plan and do not receive them within 30 days, you may file suit in a federal court. In such a case, the court may require the plan administrator to provide the materials and pay you up to $110 a day until you receive the materials, unless the materials were not sent because of reasons beyond the control of the administrator. If you have a claim for benefits which is denied or ignored, in whole or in part, you may file suit in a state or federal court.
In addition, if you disagree with the plan’s decision or lack thereof concerning the qualified status of a domestic relations order or a medical child support order, you may file suit in federal court. If it should happen that plan fiduciaries misuse the plan’s money, or if you are discriminated against for asserting your rights, you may seek assistance from the U.S. Department of Labor, or you may file suit in a federal court. The court will decide who should pay court costs and legal fees. If you are successful the court may order the person you have sued to pay these costs and fees. If you lose, the court may order you to pay these costs and fees, for example if it finds your claim is frivolous.
Assistance with Your Questions
If you have any questions about your plan, you should contact the plan administrator. If you have any questions about this statement or about your rights under ERISA, or if you need assistance in obtaining documents from the plan administrator, you should contact the nearest office of the Employee Benefits
Security Administration, U.S. Department of Labor listed in your telephone directory or the Division of Technical Assistance and Inquiries, Employee Benefits Security Administration, U.S. Department of Labor, 200 Constitution Avenue N.W., Washington, D.C. 20210. You may also obtain certain publications about your rights and responsibilities under ERISA by calling the publications hotline of the Employee Benefits Security Administration.
HC-FED72 | 05-15 | |||
Notice of an Appeal or a Grievance
The appeal or grievance provision in this certificate may be superseded by the law of your state. Please see your explanation of benefits for the applicable appeal or grievance procedure.
HC-SPP4 | 04-10 | |||
VI | ||||
When You Have A Concern Or Complaint
For the purposes of this section, any reference to “you,” “your” or “Member” also refers to a representative or provider designated by you to act on your behalf, unless otherwise noted and a “Physician reviewer” is a licensed Physician who is also a Medical Director or his or her designee who rendered the initial adverse determination.
We want you to be completely satisfied with the care you receive. That is why we have established a process for addressing your concerns and solving your problems.
Complaints and Administrative Appeals Regarding Contractual Benefits, Quality of Care and Services
Start with Member Services
We are here to listen and help. If you have a specific concern or complaint regarding a person, a service, the quality of care, choice of or access to providers, provider network adequacy or contractual benefits, you or your designated representative (including your treating Provider) can call our toll-free number and explain your concern to one of our Customer Service representatives. You can also express that concern in writing. Please call or write to us at the following:
Customer Services Toll-Free Number or address that appears on your Benefit Identification card, explanation of benefits or claim form.
_____________________________________________________________________________________________________________
29 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
We will do our best to resolve the matter on your initial contact. If we need more time to review or investigate your concern, we will get back to you as soon as possible, but in any case within 30 calendar days.
If you are not satisfied with the results of a coverage decision, you can start the appeals procedure.
Administrative Appeals Procedure
Cigna has a two step appeals procedure for coverage decisions. To initiate an Administrative appeal, you must submit a request for an appeal in writing within 180 days of receipt of a denial notice. You should state the reason why you feel your appeal should be approved and include any information supporting your appeal. If you are unable or choose not to write, you may ask to register your appeal by calling the toll-free number on your Benefit Identification card. If you choose to designate a representative to appeal on your behalf, including your provider, all correspondence related to your appeal will be sent to your designated representative and you. If you do not want such representative to pursue the appeal on your behalf, you must notify Cigna that you do not want this representative appealing this issue on your behalf.
Level One Appeal
Your appeal will be reviewed and the decision made by someone not involved in the initial decision. Expedited appeals will be considered by a health care professional.
For level one appeals, we will acknowledge in writing that we have received your request within 10 business days and respond in writing with a decision within 30 calendar days after we receive an appeal for a post-service coverage determination or within 15 calendar days for a pre-service coverage determination. If more time or information is needed to make the determination, we will notify you in writing to request an extension of up to 15 calendar days and to specify any additional information needed to complete the review.
You may request that the appeal process be expedited if the time frames under this process would seriously jeopardize your life, health or ability to regain maximum function or in the opinion of your Physician would cause you severe pain which cannot be managed without the requested services; or your appeal involves non-authorization of an admission or continuing inpatient Hospital stay. Cigna's Physician reviewer, in consultation with the treating Physician, will decide if an expedited appeal is necessary. When an appeal is expedited, we will respond with a decision within 72 hours.
Level Two Appeal
If you are dissatisfied with our level one appeal decision, you may request a second review. To initiate a level two appeal, follow the same process required for a level one appeal, except that such a request must be submitted within 60 days from your receipt of a Level One Appeal decision.
Receipt of requests for a second review will be acknowledged in writing within 10 business days. Post-service requests will be completed within 30 calendar days, while most pre-service requests will be completed within 15 calendar days. If more time or information is needed to make the determination, we will notify you in writing to request an extension of up to 15 calendar days and to specify any additional information needed to complete the review. You will be notified in writing of the decision.
You may request that the appeal process be expedited if the time frames under this process would seriously jeopardize your life, health or ability to regain maximum function or in the opinion of your Physician would cause you severe pain which cannot be managed without the requested services; or your appeal involves nonauthorization of an admission or continuing inpatient Hospital stay. Cigna's Physician reviewer, in consultation with the treating Physician will decide if an expedited appeal is necessary. When an appeal is expedited, we will respond with a decision within 72 hours.
Appeal to the State of New Jersey
For appeals regarding a person, a service, the quality of care, choice of or access to providers, provider network adequacy, or the contractual benefits, if you remain dissatisfied after exhausting Cigna's Complaint and Appeal procedure, you may appeal to the State of New Jersey Department of Banking and Insurance at the following address and telephone number:
Consumer Protection Services
New Jersey Department of Banking and Insurance 20 West State Street, 9th Floor
P.O. Box 329
Trenton, NJ 08625-0329
(609) 292-5316
You may also wish to access an online New Jersey complaint form at: www.state.nj.us/dobi/enfcon.htm.
Appeals Regarding Required Medical Necessity and Utilization Review Determinations
Initial Determination
Cigna is responsible for making decisions about the appropriateness, medical necessity and efficiency of health care services provided to Members under this Certificate. All decisions to deny or limit coverage for an inpatient admission, a service, a procedure or an extension of inpatient stay, are made by a New Jersey-licensed Physician.
The health care determinations made by Cigna are directly communicated to the treating or requesting Provider (including a Provider acting on your behalf with your consent, if such Provider is the requesting Provider) on a timely basis appropriate to the Member's medical needs. Cigna will not reverse its initial determination of medical necessity or appropriateness unless misrepresented or fraudulent
_____________________________________________________________________________________________________________
30 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
information was submitted to Cigna as part of the request for health care services.
You or your designated representative (including a provider acting on your behalf with your consent) may request a written notice of an initial determination made by Cigna, including an explanation of the Medical Necessity Appeal process.
Medical Necessity Appeals Procedure
Cigna has a two step procedure for coverage decisions. To initiate a Medical Necessity appeal, you must submit a request for an appeal in writing to the address that appears on your Benefit Identification card, explanation of benefits or claim form within 180 days of receipt of a denial notice. You should state the reason why you feel your appeal should be approved and include any information supporting your appeal. If you are unable or choose not to write, you may ask to register your appeal by calling the toll-free number on your Benefit Identification card. If you choose to designate a representative to appeal on your behalf, including your provider, all correspondence related to your appeal will be sent to your designated representative and you. If you do not want such representative to pursue the appeal on your behalf, you must notify Cigna that you do not want this representative appealing this issue on your behalf.
Level One Appeal
You have the opportunity to speak with, and may request appeal review by, Cigna's Physician reviewer.
For level one appeals, we will respond in writing with a decision within five business days after we receive an appeal.
You may request that the appeal process be expedited if: the time frames under this process would seriously jeopardize your life, health or ability to regain maximum function or in the opinion of your Physician would cause you severe pain which cannot be managed without the requested services; your appeal involves non-authorization of an admission or continuing inpatient Hospital stay; or your appeal addresses a determination regarding urgent or emergency care. Cigna's Physician reviewer, in consultation with the treating Physician will decide if an expedited appeal is necessary. When an appeal is expedited, we will respond with a decision within 72 hours.
Level Two Appeal
If you are dissatisfied with our level one appeal decision, you may request a second review. To initiate a level two appeal, follow the same process required for a level one appeal, except that such a request must be submitted within 60 days from your receipt of a Level One Appeal decision.
Most requests for a second review will be conducted by the Appeals Committee, which consists of at least one Physician reviewer and two other Physicians/health care professionals. Anyone involved in the prior decision may not participate on
the Appeal Committee. The committee will consult with at least one Physician in the same or similar specialty as the care under consideration, as determined by Cigna's Physician reviewer. You may request that the same or similar specialist be a participant on the committee. You may present your situation to the committee in person or by conference call.
For level two appeals we will acknowledge in writing that we have received your request within 10 business days and schedule a committee review. The committee review will be completed within 15 calendar days for pre-service appeals and 20 business days for post-service appeals. If more time or information is needed to make the determination, we will notify the Department of Banking and Insurance and you in writing to request an extension of up to 15 calendar days for pre-service appeals and 20 business days for post-service appeals and to specify any additional information needed by the Appeals Committee to complete the review. You will be notified in writing of the Appeals Committee's decision.
You may request that the appeal process be expedited if: the time frames under this process would seriously jeopardize your life, health or ability to regain maximum function or in the opinion of your Physician would cause you severe pain which cannot be managed without the requested services; your appeal involves non-authorization of an admission or continuing inpatient Hospital stay; or your appeal addresses a determination regarding urgent or emergency care. When an appeal is expedited, we will respond with a decision within 72 hours.
External Appeals of Utilization Management Determinations
After exhausting Cigna's Medical Necessity Appeal procedure, if you remain dissatisfied with Cigna's health care determination, you may initiate a review by an Independent Utilization Review Organization (IURO) within 60 calendar days from the receipt of Cigna's final written decision. To initiate a review, you or your Provider, on your behalf, should complete the State of New Jersey IURO forms provided by Cigna and mail the completed forms to:
Consumer Protection Services
New Jersey Department of Banking and Insurance 20 West State Street, 9th Floor
P.O. Box 329
Trenton, NJ 08625-0329
(609) 292-5316
along with a check or money order for $25 payable to the “New Jersey Department of Banking and Insurance” (this fee may be reduced to $2 in cases of financial hardship). If a Provider is appealing to the IURO on your behalf, the Provider is responsible for paying your portion of the cost of the IURO appeal (e.g. $25, or $2 if financial hardship). Cigna will bear the remaining costs of the review.
_____________________________________________________________________________________________________________
31 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
You or your Provider, on your behalf, may also request review of your appeal by the IURO if Cigna has missed any timeframes associated with the processing of your medical necessity appeal. If this is the case, you must certify to the IURO that you or your Provider, on your behalf, did not hinder Cigna from making a timely determination by failing to provide the information required for Cigna to make its decision.
Once the IURO communicates its decision, Cigna will respond within 10 business days to you (or the Provider, on your behalf) the IURO and the Department of Banking and Insurance with a written report describing how Cigna will implement the IURO’s decision.
The External Appeals Program is a voluntary program. The decision of the IURO is binding on Cigna.
Appeal to the State of New Jersey
You have the right to contact the New Jersey Department of Banking and Insurance for assistance at any time. The New Jersey Department of Banking and Insurance may be contacted at the following address and telephone number:
Consumer Protection Services
New Jersey Department of Banking and Insurance 20 West State Street, 9th Floor
P.O. Box 329
Trenton, NJ 08625-0329
(609) 292-5316
Notice of Benefit Determination on Appeal
Every notice of a determination on appeal will be provided in writing or electronically and, if an adverse determination, will include:
• | the specific reason or reasons for the adverse determination; |
• | reference to the specific plan provisions on which the determination is based; |
• | a statement that the claimant is entitled to receive, upon request and free of charge, reasonable access to and copies of all documents, records, and other Relevant Information as defined; |
• | a statement describing: |
• | the procedure to initiate the next level of appeal; |
• | any voluntary appeal procedures offered by the plan; and |
• | the claimant's right to bring an action under ERISA section 502(a); |
• | upon request and free of charge, a copy of any internal rule, guideline, protocol or other similar criterion that was relied upon in making the adverse determination regarding your appeal, and an explanation of the scientific or clinical judgment for a determination that is based on a Medical Necessity, experimental treatment or other similar exclusion or limit. |
You also have the right to bring a civil action under Section 502(a) of ERISA if you are not satisfied with the Level Two Appeal decision (or with the Level One Appeal decision if expedited). You or your plan may have other voluntary alternative dispute resolution options such as Mediation. One way to find out what may be available is to contact your local
U.S. Department of Labor office and your State insurance regulatory agency. You may also contact the Plan Administrator.
Relevant Information
Relevant Information is any document, record, or other information which: was relied upon in making the benefit determination; was submitted, considered, or generated in the course of making the benefit determination, without regard to whether such document, record, or other information was relied upon in making the benefit determination; demonstrates compliance with the administrative processes and safeguards required by federal law in making the benefit determination; or constitutes a statement of policy or guidance with respect to the plan concerning the denied treatment option or benefit or the claimant's diagnosis, without regard to whether such advice or statement was relied upon in making the benefit determination.
Legal Action Following Appeals
If your plan is governed by ERISA, you have the right to bring a civil action in federal court under Section 502(a) of ERISA if you are not satisfied with the outcome of the Appeals Procedure. In most instances, you may not initiate a legal action against Cigna until you have completed the Level One and Level Two Appeal processes. If your Appeal is expedited, there is no need to complete the Level Two process prior to bringing legal action in federal court.
If your plan is governed by New Jersey P.L.2001, c.187 (2A:53A-30 et seq), you have the right to bring action in state court accordance with that statute. You must exhaust the Independent Health Care Appeals Program procedures created pursuant to section 11 of P.L.1997, c.192 (C26:2S-11), before filing an action in state court, unless serious or significant harm to the covered person has occurred or will imminently occur, before filing an action in state court for economic and non-economic loss that occurs as a result of Cigna's negligence with respect to the denial of or delay in approving or providing medically necessary covered services, which denial or delay is the proximate cause of a covered person's: death; serious and protracted or permanent impairment of a bodily function or system; loss of a body organ necessary for normal bodily function; loss of a body member; exacerbation of a serious or life-threatening disease or condition that results in serious or significant harm or requires substantial medical treatment; a physical condition resulting in chronic and significant pain; or substantial physical or mental harm which
_____________________________________________________________________________________________________________
32 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
resulted in further substantial medical treatment made medically necessary by the denial or delay of care.
HC-APL26 | 04-10 | |||
VI | ||||
Definitions
Active Service
You will be considered in Active Service:
• | on any of your Employer's scheduled work days if you are performing the regular duties of your work on a full-time basis on that day either at your Employer's place of business or at some location to which you are required to travel for your Employer's business. |
• | on a day which is not one of your Employer's scheduled work days if you were in Active Service on the preceding scheduled work day. |
HC-DFS1 | 04-10 | |||
VI | ||||
Bed and Board
The term Bed and Board includes all charges made by a Hospital on its own behalf for room and meals and for all general services and activities needed for the care of registered bed patients.
HC-DFS2 | 04-10 | |||
V2 | ||||
Biologically-Based Mental Illness
A mental or nervous condition that is caused by a biological disorder of the brain and results in a clinically significant or psychological syndrome or pattern that substantially limits the functioning of the person with the illness, including but not limited to: schizophrenia; schizoaffective disorder; major depressive disorder; bipolar disorder; paranoia and other psychotic disorders; obsessive-compulsive disorder; panic disorder; and pervasive developmental disorder or autism.
HC-DFS110 | 04-10 | |||
V1 | ||||
Custodial Services
Any services that are of a sheltering, protective, or safeguarding nature. Such services may include a stay in an
institutional setting, at-home care, or nursing services to care for someone because of age or mental or physical condition. This service primarily helps the person in daily
living.
Custodial care also can provide medical services, given mainly to maintain the person’s current state of health. These services cannot be intended to greatly improve a medical condition; they are intended to provide care while the patient cannot care for himself or herself. Custodial Services include but are not limited to:
• | Services related to watching or protecting a person; |
• | Services related to performing or assisting a person in performing any activities of daily living, such as: walking, grooming, bathing, dressing, getting in or out of bed, toileting, eating, preparing foods, or taking medications that can be self administered, and |
• | Services not required to be performed by trained or skilled medical or paramedical personnel. |
HC-DFS4 | 04-10 | |||
V1 | ||||
Dependent
Dependents are:
• | your lawful spouse or civil union partner; or |
• | your Domestic Partner; and |
• | any child of yours who is: |
• | less than 26 years old. |
• | 26 or more years old, not married nor in a civil union partnership nor in a Domestic Partnership, and primarily supported by you and incapable of self-sustaining employment by reason of mental or physical disability which arose while the child was covered as a Dependent under this Plan, or while covered as a dependent under a prior plan with no break in coverage. |
Proof of the child's condition and dependence must be submitted to Cigna within 31 days after the date the child ceases to qualify above. From time to time, but not more frequently than once a year, Cigna may require proof of the continuation of such condition and dependence.
The term child means a child born to you or a child legally adopted by you. It also includes a stepchild or a child for whom you are the legal guardian. If your civil union partner has a child, that child will also be included as a Dependent. If your Domestic Partner has a child, that child will also be included as a Dependent.
Benefits for a Dependent child will continue until the last day of the calendar month in which the limiting age is reached.
_____________________________________________________________________________________________________________
33 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
Anyone who is eligible as an Employee will not be considered as a Dependent spouse. A child under age 26 who is eligible as an Employee and a Dependent child may be covered as either an Employee or as a Dependent child.
No one may be considered as a Dependent of more than one Employee.
HC-DFS646 | 01-15 | |||
V1 | ||||
Domestic Partner
A Domestic Partner is party to a domestic partnership, which is established when all of the following requirements are met:
• | Both persons have a common residence and are otherwise jointly responsible for each other’s common welfare as evidenced by joint financial arrangements or joint ownership of real or personal property, demonstrated by at least one of the following: |
• | a joint deed, mortgage agreement or lease; |
• | a joint bank account; |
• | designation of one of the persons as a primary beneficiary in the other person’s will; |
• | designation of one of the persons as a primary beneficiary in the other person’s life insurance policy or retirement plan; or |
• | joint ownership of a motor vehicle. |
• | Both persons agree to be jointly responsible for each other’s basic living expenses during the domestic partnership. |
• | Neither person is in a marriage or civil union partnership recognized by New Jersey law, or a member of another domestic partnership. |
• | Neither person is related to the other by blood or affinity, up to and including the fourth degree of consanguinity. |
• | Both persons have chosen to share each other’s lives in a committed relationship of mutual caring. |
• | Both persons are at least 18 years of age. |
• | Both persons file jointly an Affidavit of Domestic Partnership. |
• | Neither person has been a partner in a domestic partnership that was terminated less than 180 days prior to the filing of the current Affidavit of Domestic Partnership, except that this prohibition will not apply if one of the partners dies. |
The section of this certificate entitled "COBRA Continuation Rights Under Federal Law" will not apply to your Domestic Partner and his or her Dependents.
HC-DFS120 | 04-10 | |||
V1 | ||||
Emergency Services
Emergency services are medical, psychiatric, surgical, Hospital and related health care services and testing, including ambulance service, which are required to treat a sudden, unexpected onset of a bodily Injury or serious Sickness which could reasonably be expected by a prudent layperson to result in serious medical complications, loss of life or permanent impairment to bodily functions in the absence of immediate medical attention. Examples of such Injury or Sickness are conditions that produce loss of consciousness or excessive bleeding, as well as conditions which may otherwise be determined by Cigna, in accordance with generally accepted medical standards, to require immediate medical attention The presenting symptoms, as coded by the provider and recorded by the Hospital on the claim form, or the final diagnosis, will be the basis for the determination of coverage.
HC-DFS111 | 04-10 | |||
V1 | ||||
Employee
The term Employee means a full-time employee of the Employer who is currently in Active Service. The term does not include employees who are part-time or temporary or who normally work less than 20 hours a week for the Employer.
HC-DFS7 | 04-10 | |||
V3 | ||||
Employer
The term Employer means the Policyholder and all Affiliated Employers.
HC-DFS8 | 04-10 | |||
V1 | ||||
Essential Health Benefits
Essential health benefits means, to the extent covered under the plan, expenses incurred with respect to covered services, in at least the following categories: ambulatory patient services, emergency services, hospitalization, maternity and newborn
_____________________________________________________________________________________________________________
34 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
care, mental health and substance use disorder services, including behavioral health treatment, prescription drugs, rehabilitative and habilitative services and devices, laboratory services, preventive and wellness services and chronic disease management and pediatric services, including oral and vision care.
HC-DFS411 | 01-11 | |||
Expense Incurred
An expense is incurred when the service or the supply for which it is incurred is provided.
HC-DFS10 | 04-10 | |||
VI | ||||
Free-Standing Surgical Facility
The term Free-standing Surgical Facility means an institution which meets all of the following requirements:
• | it has a medical staff of Physicians, Nurses and licensed anesthesiologists; |
• | it maintains at least two operating rooms and one recovery room; |
• | it maintains diagnostic laboratory and x-ray facilities; |
• | it has equipment for emergency care; |
• | it has a blood supply; |
• | it maintains medical records; |
• | it has agreements with Hospitals for immediate acceptance of patients who need Hospital Confinement on an inpatient basis; and |
• | it is licensed in accordance with the laws of the appropriate legally authorized agency. |
HC-DFS11 | 04-10 | |||
VI | ||||
Hospice Care Program
The term Hospice Care Program means:
• | a coordinated, interdisciplinary program to meet the physical, psychological, spiritual and social needs of dying persons and their families; |
• | a program that provides palliative and supportive medical, nursing and other health services through home or inpatient care during the illness; |
• | a program for persons who have a Terminal Illness and for the families of those persons. |
HC-DFS51 | 04-10 | |||
VI | ||||
Hospice Care Services
The term Hospice Care Services means any services provided by: a Hospital, a Skilled Nursing Facility or a similar institution, a Home Health Care Agency, a Hospice Facility, or any other licensed facility or agency under a Hospice Care Program.
HC-DFS52 | 04-10 | |||
VI | ||||
Hospice Facility
The term Hospice Facility means an institution or part of it which:
• | primarily provides care for Terminally Ill patients; |
• | is accredited by the National Hospice Organization; |
• | meets standards established by Cigna; and |
• | fulfills any licensing requirements of the state or locality in which it operates. |
HC-DFS53 | 04-10 | |||
VI | ||||
Hospital
The term Hospital means:
• | an institution licensed as a hospital, which: maintains, on the premises, all facilities necessary for medical and surgical treatment; provides such treatment on an inpatient basis, for compensation, under the supervision of Physicians; and provides 24-hour service by Registered Graduate Nurses; |
• | an institution which qualifies as a hospital, a psychiatric hospital or a tuberculosis hospital, and a provider of services under Medicare, if such institution is accredited as a hospital by the Joint Commission on the Accreditation of Healthcare Organizations; |
• | a public or private hospital or detoxification facility licensed by the state to provide treatment for alcoholism or a licensed residential treatment facility which provides an alcoholic treatment program which meets minimum standards of such care prescribed by the Joint Commission on the Accreditation of Healthcare Organizations. |
_____________________________________________________________________________________________________________
35 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
The term Hospital will not include an institution which is primarily a place for rest, a place for the aged, or a nursing home.
HC-DFS115 | 04-10 | |||
VI | ||||
Hospital Confinement or Confined in a Hospital
A person will be considered Confined in a Hospital if he is:
• | a registered bed patient in a Hospital upon the recommendation of a Physician; |
• | receiving emergency care in a Hospital for: an Injury, on his first visit as an outpatient within 72 hours after the Injury is received; or a sudden and unexpected Sickness within 12 hours after the Sickness begins, if lack of such care would cause his condition to worsen seriously; |
• | receiving treatment for Mental Health and Substance Abuse Services in a Partial Hospitalization program; |
• | receiving treatment for Substance Abuse Services in a Substance Abuse Residential Treatment Center. |
HC-DFS116 | 04-10 | |||
VI | ||||
Injury
The term Injury means an accidental bodily injury.
HC-DFS12 | 04-10 | |||
VI | ||||
Medicaid
The term Medicaid means a state program of medical aid for needy persons established under Title XIX of the Social Security Act of 1965 as amended.
HC-DFS16 | 04-10 | |||
VI | ||||
Medically Necessary/Medical Necessity
Medically Necessary Covered Services and Supplies means or describes a health care service that a health care provider, exercising his prudent clinical judgment, would provide to a covered person for the purpose of evaluating, diagnosing or treating an illness, injury, disease or its symptoms and that is: in accordance with the generally accepted standards of medical practice; clinically appropriate, in terms of type,
frequency, extent, site and duration, and considered effective for the covered person's illness, injury or disease; not primarily for the convenience of the covered person or the health care provider; and not more costly than an alternative service or sequence of services at least as likely to produce equivalent therapeutic or diagnostic results as to the diagnosis or treatment of that covered person's illness, injury or disease.
HC-DFS113 | 04-10 | |||
VI | ||||
Medicare
The term Medicare means the program of medical care benefits provided under Title XVIII of the Social Security Act of 1965 as amended.
HC-DFS17 | 04-10 | |||
VI | ||||
Necessary Services and Supplies
The term Necessary Services and Supplies includes any charges, except charges for Bed and Board, made by a Hospital on its own behalf for medical services and supplies actually used during Hospital Confinement, any charges, by whomever made, for licensed ambulance service to or from the nearest Hospital where the needed medical care and treatment can be provided; and any charges, by whomever made, for the administration of anesthetics during Hospital Confinement.
The term Necessary Services and Supplies will not include any charges for special nursing fees, dental fees or medical fees.
HC-DFS21 | 04-10 | |||
VI | ||||
Nurse
The term Nurse means a Registered Graduate Nurse, a Licensed Practical Nurse or a Licensed Vocational Nurse who has the right to use the abbreviation "R.N.," "L.P.N." or "L.V.N."
HC-DFS22 | 04-10 | |||
VI | ||||
_____________________________________________________________________________________________________________
36 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
Other Health Care Facility/Other Health Professional
The term Other Health Care Facility means a facility other than a Hospital or hospice facility. Examples of Other Health Care Facilities include, but are not limited to, licensed skilled nursing facilities, rehabilitation Hospitals and subacute facilities. The term Other Health Professional means an individual other than a Physician who is licensed or otherwise authorized under the applicable state law to deliver medical services and supplies. Other Health Professionals include, but are not limited to physical therapists, registered nurses and licensed practical nurses. Other Health Professionals do not include providers such as Certified First Assistants, Certified Operating Room Technicians, Certified Surgical Assistants/Technicians, Licensed Certified Surgical Assistants/Technicians, Licensed Surgical Assistants, Orthopedic Physician Assistants and Surgical First Assistants.
HC-DFS23 | 04-10 | |||
VI | ||||
Patient Protection and Affordable Care Act of 2010 (“PPACA”)
Patient Protection and Affordable Care Act of 2010 means the Patient Protection and Affordable Care Act of 2010 (Public Law 111-148) as amended by the Health Care and Education Reconciliation Act of 2010 (Public Law 111-152).
HC-DFS412 | 01-11 | |||
Physician
The term Physician means a licensed medical practitioner who is practicing within the scope of his license and who is licensed to prescribe and administer drugs or to perform surgery. It will also include any other licensed medical practitioner whose services are required to be covered by law in the locality where the policy is issued if he is:
• | operating within the scope of his license; and |
• | performing a service for which benefits are provided under this plan when performed by a Physician. |
HC-DFS25 | 04-10 | |||
VI | ||||
Psychologist
The term Psychologist means a person who is licensed or certified as a clinical psychologist. Where no licensure or certification exists, the term Psychologist means a person who is considered qualified as a clinical psychologist by a
recognized psychological association. It will also include any other licensed counseling practitioner whose services are required to be covered by law in the locality where the policy is issued if he is operating within the scope of his license and performing a service for which benefits are provided under this plan when performed by a Psychologist.
HC-DFS26 | 04-10 | |||
VI | ||||
Review Organization
The term Review Organization refers to an affiliate of Cigna or another entity to which Cigna has delegated responsibility for performing utilization review services. The Review Organization is an organization with a staff of clinicians which may include Physicians, Registered Graduate Nurses, licensed mental health and substance abuse professionals, and other trained staff members who perform utilization review services.
HC-DFS30 | 04-10 | |||
VI | ||||
Sickness - For Medical Insurance
The term Sickness means a physical or mental illness. It also includes pregnancy. Expenses incurred for routine Hospital and pediatric care of a newborn child prior to discharge from the Hospital nursery will be considered to be incurred as a result of Sickness.
HC-DFS50 | 04-10 | |||
VI | ||||
Skilled Nursing Facility
The term Skilled Nursing Facility means a licensed institution (other than a Hospital, as defined) which specializes in:
• | physical rehabilitation on an inpatient basis; or |
• | skilled nursing and medical care on an inpatient basis; |
but only if that institution: maintains on the premises all facilities necessary for medical treatment; provides such treatment, for compensation, under the supervision of Physicians; and provides Nurses' services.
HC-DFS31 | 04-10 | |||
VI | ||||
_____________________________________________________________________________________________________________
37 | myCigna.com | |
Exhibit 10.2.1

_____________________________________________________________________________________________
Terminal Illness
A Terminal Illness will be considered to exist if a person becomes terminally ill with a prognosis of six months or less to live, as diagnosed by a Physician.
HC-DFS54 | 04-10 | |||
VI | ||||
Urgent Care
Urgent Care is medical, surgical, Hospital or related health care services and testing which are not Emergency Services, but which are determined by Cigna, in accordance with generally accepted medical standards, to have been necessary to treat an unforeseen condition requiring immediate medical attention. This does not include care that could have been foreseen before leaving the immediate area where you ordinarily receive and/or were scheduled to receive services. Such care includes, but is not limited to, delivery beyond the 35th week of pregnancy, dialysis, scheduled medical treatments or therapy, or care received after a Physician's recommendation that the insured should not travel due to any medical condition.
HC-DFS114 | 04-10 | |||
VI | ||||
_____________________________________________________________________________________________________________
38 | myCigna.com | |
