Attached files
| file | filename |
|---|---|
| EX-99.2 - EX-99.2 - CRISPR Therapeutics AG | crsp-ex992_178.htm |
| EX-99.1 - EX-99.1 - CRISPR Therapeutics AG | crsp-ex991_11.htm |
| 8-K - 8-K - CRISPR Therapeutics AG | crsp-8k_20210611.htm |
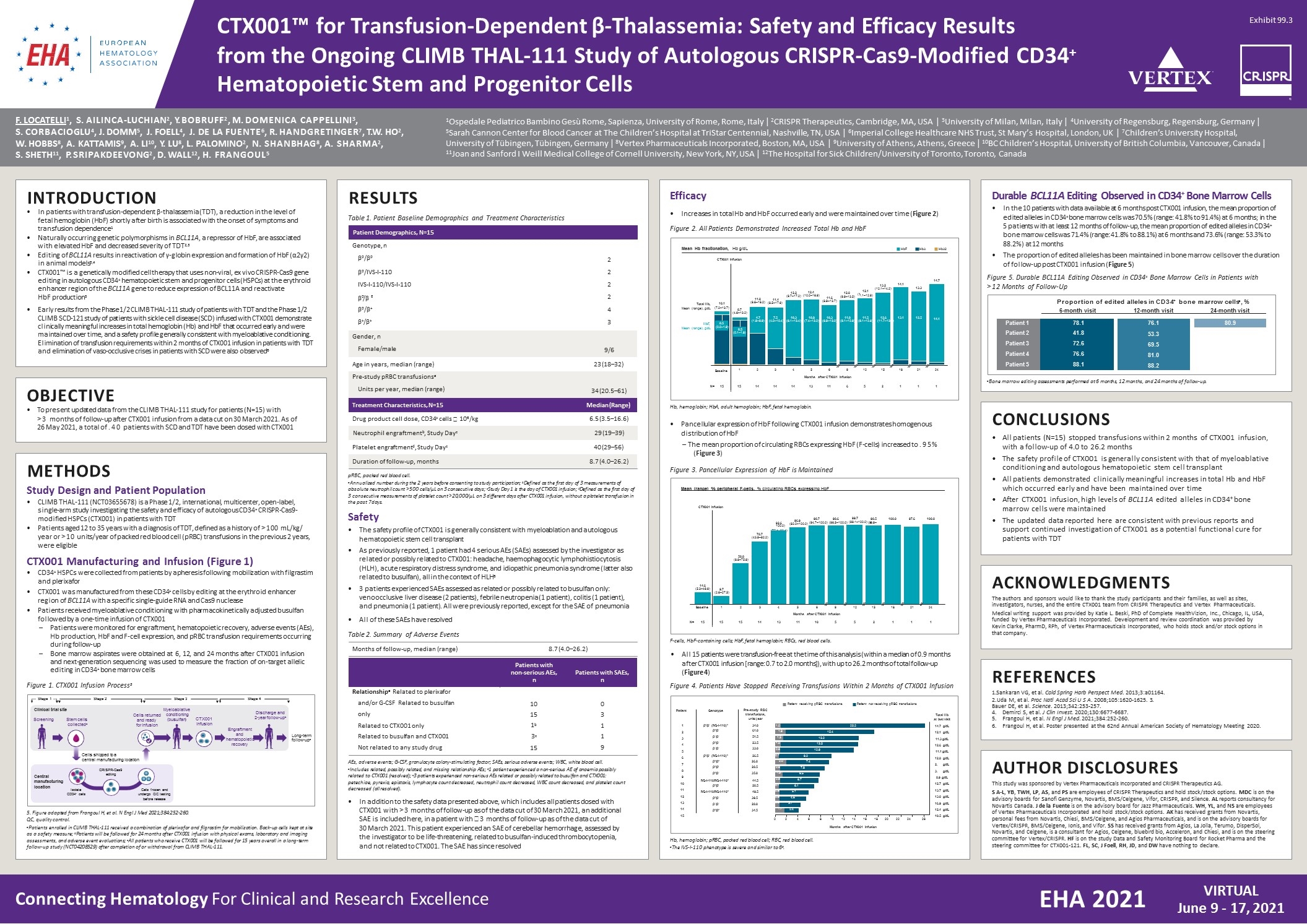
Connecting Hematology For Clinical and Research Excellence VIRTUAL June 9 - 17, 2021 EHA 2021 CTX001™ for Transfusion-Dependent β-Thalassemia: Safety and Efficacy Results from the Ongoing CLIMB THAL-111 Study of Autologous CRISPR-Cas9-Modified CD34+ Hematopoietic Stem and Progenitor Cells F. LOCATELLI1, S. AILINCA-LUCHIAN2, Y. BOBRUFF2, M. DOMENICA CAPPELLINI3, S. CORBACIOGLU4, J. DOMM5, J. FOELL4, J. DE LA FUENTE6, R. HANDGRETINGER7, T.W. HO2, W. HOBBS8, A. KATTAMIS9, A. LI10, Y. LU8, L. PALOMINO2, N. SHANBHAG8, A. SHARMA2, S. SHETH11, P. SRIPAKDEEVONG2, D. WALL12, H. FRANGOUL5 1Ospedale Pediatrico Bambino Gesù Rome, Sapienza, University of Rome, Rome, Italy | 2CRISPR Therapeutics, Cambridge, MA, USA | 3University of Milan, Milan, Italy | 4University of Regensburg, Regensburg, Germany | 5Sarah Cannon Center for Blood Cancer at The Children’s Hospital at TriStar Centennial, Nashville, TN, USA | 6Imperial College Healthcare NHS Trust, St Mary’s Hospital, London, UK | 7Children’s University Hospital, University of Tübingen, Tübingen, Germany | 8Vertex Pharmaceuticals Incorporated, Boston, MA, USA | 9University of Athens, Athens, Greece | 10BC Children’s Hospital, University of British Columbia, Vancouver, Canada | 11Joan and Sanford I Weill Medical College of Cornell University, New York, NY, USA | 12The Hospital for Sick Children/University of Toronto, Toronto, Canada INTRODUCTION In patients with transfusion-dependent β-thalassemia (TDT), a reduction in the level of fetal hemoglobin (HbF) shortly after birth is associated with the onset of symptoms and transfusion dependence1 Naturally occurring genetic polymorphisms in BCL11A, a repressor of HbF, are associated with elevated HbF and decreased severity of TDT2,3 Editing of BCL11A results in reactivation of γ-globin expression and formation of HbF (α2γ2) in animal models3,4 CTX001™ is a genetically modified cell therapy that uses non-viral, ex vivo CRISPR-Cas9 gene editing in autologous CD34+ hematopoietic stem and progenitor cells (HSPCs) at the erythroid enhancer region of the BCL11A gene to reduce expression of BCL11A and reactivate HbF production5 Early results from the Phase 1/2 CLIMB THAL-111 study of patients with TDT and the Phase 1/2 CLIMB SCD-121 study of patients with sickle cell disease (SCD) infused with CTX001 demonstrate clinically meaningful increases in total hemoglobin (Hb) and HbF that occurred early and were maintained over time, and a safety profile generally consistent with myeloablative conditioning. Elimination of transfusion requirements within 2 months of CTX001 infusion in patients with TDT and elimination of vaso-occlusive crises in patients with SCD were also observed6 OBJECTIVE To present updated data from the CLIMB THAL-111 study for patients (N=15) with >3 months of follow-up after CTX001 infusion from a data cut on 30 March 2021. As of 26 May 2021, a total of .40 patients with SCD and TDT have been dosed with CTX001 METHODS Study Design and Patient Population CLIMB THAL-111 (NCT03655678) is a Phase 1/2, international, multicenter, open-label, single-arm study investigating the safety and efficacy of autologous CD34+ CRISPR-Cas9- modified HSPCs (CTX001) in patients with TDT Patients aged 12 to 35 years with a diagnosis of TDT, defined as a history of >100 mL/kg/ year or >10 units/year of packed red blood cell (pRBC) transfusions in the previous 2 years, were eligible CTX001 Manufacturing and Infusion (Figure 1) CD34+ HSPCs were collected from patients by apheresis following mobilization with filgrastim and plerixafor + CTX001 was manufactured from these CD34 cells by editing at the erythroid enhancer region of BCL11A with a specific single-guide RNA and Cas9 nuclease Patients received myeloablative conditioning with pharmacokinetically adjusted busulfan followed by a one-time infusion of CTX001 Patients were monitored for engraftment, hematopoietic recovery, adverse events (AEs), Hb production, HbF and F-cell expression, and pRBC transfusion requirements occurring during follow-up Bone marrow aspirates were obtained at 6, 12, and 24 months after CTX001 infusion and next-generation sequencing was used to measure the fraction of on-target allelic editing in CD34+ bone marrow cells The safety profile of CTX001 is generally consistent with myeloablation and autologous hematopoietic stem cell transplant As previously reported, 1 patient had 4 serious AEs (SAEs) assessed by the investigator as related or possibly related to CTX001: headache, haemophagocytic lymphohistiocytosis (HLH), acute respiratory distress syndrome, and idiopathic pneumonia syndrome (latter also related to busulfan), all in the context of HLH6 3 patients experienced SAEs assessed as related or possibly related to busulfan only: venoocclusive liver disease (2 patients), febrile neutropenia (1 patient), colitis (1 patient), and pneumonia (1 patient). All were previously reported, except for the SAE of pneumonia All of these SAEs have resolved CONCLUSIONS All patients (N=15) stopped transfusions within 2 months of CTX001 infusion, with a follow-up of 4.0 to 26.2 months The safety profile of CTX001 is generally consistent with that of myeloablative conditioning and autologous hematopoietic stem cell transplant All patients demonstrated clinically meaningful increases in total Hb and HbF which occurred early and have been maintained over time After CTX001 infusion, high levels of BCL11A edited alleles in CD34+ bone marrow cells were maintained The updated data reported here are consistent with previous reports and support continued investigation of CTX001 as a potential functional cure for patients with TDT Durable BCL11A Editing Observed in CD34+ Bone Marrow Cells In the 10 patients with data available at 6 months post CTX001 infusion, the mean proportion of edited alleles in CD34+ bone marrow cells was 70.5% (range: 41.8% to 91.4%) at 6 months; in the 5 patients with at least 12 months of follow-up, the mean proportion of edited alleles in CD34+ bone marrow cells was 71.4% (range: 41.8% to 88.1%) at 6 months and 73.6% (range: 53.3% to 88.2%) at 12 months The proportion of edited alleles has been maintained in bone marrow cells over the duration of follow-up post CTX001 infusion (Figure 5) ACKNOWLEDGMENTS The authors and sponsors would like to thank the study participants and their families, as well as sites, investigators, nurses, and the entire CTX001 team from CRISPR Therapeutics and Vertex Pharmaceuticals. Medical writing support was provided by Katie L. Beski, PhD of Complete HealthVizion, Inc., Chicago, IL, USA, funded by Vertex Pharmaceuticals Incorporated. Development and review coordination was provided by Kevin Clarke, PharmD, RPh, of Vertex Pharmaceuticals Incorporated, who holds stock and/or stock options in that company. REFERENCES Sankaran VG, et al. Cold Spring Harb Perspect Med. 2013;3:a01164. Uda M, et al. Proc Natl Acad Sci U S A. 2008;105:1620-1625. 3. Bauer DE, et al. Science. 2013;342:253-257. Demirci S, et al. J Clin Invest. 2020;130:6677-6687. Frangoul H, et al. N Engl J Med. 2021;384:252-260. Frangoul H, et al. Poster presented at the 62nd Annual American Society of Hematology Meeting 2020. AUTHOR DISCLOSURES This study was sponsored by Vertex Pharmaceuticals Incorporated and CRISPR Therapeutics AG. S A-L, YB, TWH, LP, AS, and PS are employees of CRISPR Therapeutics and hold stock/stock options. MDC is on the advisory boards for Sanofi Genzyme, Novartis, BMS/Celgene, Vifor, CRISPR, and Silence. AL reports consultancy for Novartis Canada. J de la Fuente is on the advisory board for Jazz Pharmaceuticals. WH, YL, and NS are employees of Vertex Pharmaceuticals Incorporated and hold stock/stock options. AK has received grants from Novartis, personal fees from Novartis, Chiesi, BMS/Celgene, and Agios Pharmaceuticals, and is on the advisory boards for Vertex/CRISPR, BMS/Celgene, Ionis, and Vifor. SS has received grants from Agios, La Jolla, Terumo, DisperSol, Novartis, and Celgene, is a consultant for Agios, Celgene, bluebird bio, Acceleron, and Chiesi, and is on the steering committee for Vertex/CRISPR. HF is on the study Data and Safety Monitoring Board for Rocket Pharma and the steering committee for CTX001-121. FL, SC, J Foell, RH, JD, and DW have nothing to declare. RESULTS Table 1. Patient Baseline Demographics and Treatment Characteristics Patient Demographics, N=15 Genotype, n β0/β0 β0/IVS-I-110 IVS-I-110/IVS-I-110 β /β 0 E β0/β+ β+/β+ 2 2 2 2 4 3 Gender, n Female/male 9/6 Age in years, median (range) 23 (18–32) Pre-study pRBC transfusionsa Units per year, median (range) 34 (20.5–61) Treatment Characteristics, N=15 Median (Range) Drug product cell dose, CD34+ cells 106/kg6.5 (3.5–16.6) Neutrophil engraftmentb, Study Dayc29 (19–39) Platelet engraftmentd, Study Dayc40 (29–56) Duration of follow-up, months8.7 (4.0–26.2) pRBC, packed red blood cell. aAnnualized number during the 2 years before consenting to study participation; bDefined as the first day of 3 measurements of absolute neutrophil count >500 cells/µL on 3 consecutive days; cStudy Day 1 is the day of CTX001 infusion; dDefined as the first day of 3 consecutive measurements of platelet count >20,000/µL on 3 different days after CTX001 infusion, without a platelet transfusion in the past 7 days. Safety Table 2. Summary of Adverse Events Months of follow-up, median (range) 8.7 (4.0–26.2) Patients with non-serious AEs, n Patients with SAEs, n Relationshipa Related to plerixafor and/or G-CSF Related to busulfan only Related to CTX001 only Related to busulfan and CTX001 Not related to any study drug 10 15 1b 3c 15 0 3 1 1 9 AEs, adverse events; G-CSF, granulocyte colony-stimulating factor; SAEs, serious adverse events; WBC, white blood cell. aIncludes related, possibly related, and missing relationship AEs; b1 patient experienced a non-serious AE of anaemia possibly related to CTX001 (resolved); c3 patients experienced non-serious AEs related or possibly related to busulfan and CTX001: petechiae, pyrexia, epistaxis, lymphocyte count decreased, neutrophil count decreased, WBC count decreased, and platelet count decreased (all resolved). In addition to the safety data presented above, which includes all patients dosed with CTX001 with >3 months of follow-up as of the data cut of 30 March 2021, an additional SAE is included here, in a patient with 3 months of follow-up as of the data cut of 30 March 2021. This patient experienced an SAE of cerebellar hemorrhage, assessed by the investigator to be life-threatening, related to busulfan-induced thrombocytopenia, and not related to CTX001. The SAE has since resolved Stage 3 Stage 4 Clinical trial site ScreeningStem cells collecteda Myeloablative Cells returned conditioning and ready(busulfan) for infusion CTX001 infusion Discharge and 2-year follow-upb Engraftment andLong-term hematopoieticfollow-upc recovery Cells frozen and undergo QC testing before release Central manufacturing location Cells shipped to a central manufacturing location CRISPR-Cas9 editing Isolate CD34+ cells 5. Figure adapted from Frangoul H, et al. N Engl J Med 2021;384:252-260. QC, quality control. aPatients enrolled in CLIMB THAL-111 received a combination of plerixafor and filgrastim for mobilization. Back-up cells kept at site as a safety measure; bPatients will be followed for 24 months after CTX001 infusion with physical exams, laboratory and imaging assessments, and adverse event evaluations; cAll patients who receive CTX001 will be followed for 15 years overall in a long-term follow-up study (NCT04208529) after completion of or withdrawal from CLIMB THAL-111. Figure 1. CTX001 Infusion Process5 Stage 1Stage 2 11.6 (8.9–13.7) 12.0 CTX001 Infusion 11.011.4 (6.6–16.2) (8.5–17.6) 12.212.4 (9.7–17.2) (10.0–16.9) 12.1 (1 (9.9–13.5) 1.1–12.9) 13.2 (12.1–14.2) 14.1 13.3 4.77.510.310.810.311.011.512.613.112.5 (1.9–9.9) (4.0–10.4) (6.1–13.4) (7.4–13.2) (6.9–13.0) (9.1–12.9) (9.1–12.6) (11.7–13.5) 14.7 14.1 2345691215182124 Months after CTX001 Infusion Total Hb, 10.1 Mean (range), g/dL (7.2–13.7) HbF, 0.5 Mean (range), g/dL (0.0–1.9) N= 1515141414131165211 1 1 8.7 (4.6–13.2) 0.5 (0.1–1.8) Baseline Mean Hb fractionation, Hb g/dL HbFHbAHbA2 Hb, hemoglobin; HbA, adult hemoglobin; HbF, fetal hemoglobin. Efficacy Increases in total Hb and HbF occurred early and were maintained over time (Figure 2) Figure 2. All Patients Demonstrated Increased Total Hb and HbF +a Proportion of edited alleles in CD34 bone marrow cells , % 80.9 6-month visit 12-month visit 24-month visit Patient 1 78.1 Patient 2 41.8 Patient 3 72.6 Patient 4 76.6 Patient 5 88.1 76.1 53.3 69.5 81.0 88.2 aBone marrow editing assessments performed at 6 months, 12 months, and 24 months of follow-up. Figure 5. Durable BCL11A Editing Observed in CD34+ Bone Marrow Cells in Patients with >12 Months of Follow-Up 14.6 (5.3–46.6) 9.7 (2.6–27.5) 50.8 (8.8–75.8) 78.7 (43.9–92.2) 96.9 99.7 92.6 (82.0–100.0) (94.7–100.0) (96.5–100.0) (99.1–100.0) (96.9–100.0) (75.4–98.4) 98.798.698.5100.097.6100.0 Mean (range) % peripheral F-cells, % circulating RBCs expressing HbF CTX001 Infusion Baseline123456912151821 24 Months after CTX001 Infusion N= 15151514131110552111 F-cells, HbF-containing cells; HbF, fetal hemoglobin; RBCs, red blood cells. Pancellular expression of HbF following CTX001 infusion demonstrates homogenous distribution of HbF – The mean proportion of circulating RBCs expressing HbF (F-cells) increased to .95% (Figure 3) Figure 3. Pancellular Expression of HbF is Maintained 0246810 12 14 16 18 20 22 24 26 Months after CTX001 Infusion 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Genotype Pre-study RBC transfusions, units/year β0/β+ (IVS-I-110)a34.0 β0/β+ 61.0 β+/β+ 51.5 β0/β+ 23.5 β+/β+ 33.0 β0/β+ (IVS-I-110)a26.5 β0/β0 26.0 β0/βE 28.5 β0/β+ 35.0 IVS-I-110/IVS-I-110a44.5 β0/βE 20.5 IVS-I-110/IVS-I-110a 49.5 β0/β+ 39.5 β+/β+ 28.0 β0/β0 34.5 Total Hb at last visit 14.7 g/dL 12.1 g/dL 11.3 g/dL 12.6 g/dL 11.1 g/dL 12.8 g/dL g/dL g/dL 8.9 g/dL 12.7 g/dL 13.7 g/dL 13.0 g/dL 16.9 g/dL 12.4 g/dL 10.5 g/dL Patient receiving pRBC transfusionsPatient not receiving pRBC transfusions Patient 9.2 7.4 7.8 6.5 6.7 6.1 5.1 4.6 3.7 2.4 13.2 13.5 12.9 15.4 1.0 1.9 1.5 1.0 0.9 0.7 2.0 0.9 1.3 0.9 0.7 0.8 0.8 0.8 1.7 25.2 Hb, hemoglobin; pRBC, packed red blood cell; RBC, red blood cell. aThe IVS-I-110 phenotype is severe and similar to β0. All 15 patients were transfusion-free at the time of this analysis (within a median of 0.9 months after CTX001 infusion [range: 0.7 to 2.0 months]), with up to 26.2 months of total follow-up (Figure 4) Figure 4. Patients Have Stopped Receiving Transfusions Within 2 Months of CTX001 Infusion Exhibit 99.3
