Attached files
| file | filename |
|---|---|
| 8-K - FORM 8-K - TITAN PHARMACEUTICALS INC | d333750d8k.htm |
| EX-1.1 - PLACEMENT AGENT AGREEMENT - TITAN PHARMACEUTICALS INC | d333750dex11.htm |
| EX-4.1 - FORM OF SERIES A WARRANT - TITAN PHARMACEUTICALS INC | d333750dex41.htm |
| EX-4.3 - AMENDMENT NO. 2 TO RIGHTS AGREEMENT - TITAN PHARMACEUTICALS INC | d333750dex43.htm |
| EX-4.2 - FORM OF SERIES B WARRANT - TITAN PHARMACEUTICALS INC | d333750dex42.htm |
| EX-10.1 - FORM OF SUBSCRIPTION AGREEMENT - TITAN PHARMACEUTICALS INC | d333750dex101.htm |
| EX-99.1 - PRESS RELEASE - TITAN PHARMACEUTICALS INC | d333750dex991.htm |
 Corporate Presentation
March 2012
1
Exhibit 10.2 |
 The
presentation
may
contain
“forward-looking
statements”
within
the
meaning
of
Section
27A
of
the
Securities
Act
of
1933
and
Section
21E
of
the Securities Exchange Act of 1934. Reference is made in particular to
the description of our plans and objectives for future operations,
assumptions underlying such plans and objectives and other forward-
looking terminology such as “may,”
“expects,”
“believes,”
“anticipates,”
“intends,”
“expects,”
“projects,”
or similar terms,
variations of such terms or the negative of such terms. Forward-looking
statements are based on management’s current expectations. Actual
results
could
differ
materially
from
those
currently
anticipated
due
to
a
number of factors, including but not limited to, uncertainties relating to
financing and strategic agreements and relationships; difficulties or
delays in the regulatory approval process; uncertainties relating to
sales, marketing and distribution of the Company's drug candidates that
may be successfully developed and approved for commercialization;
adverse side effects or inadequate therapeutic efficacy of the
Company's drug candidates that could slow or prevent product
development or commercialization; dependence on third party
suppliers; the uncertainty of protection for the Company's patents and
other intellectual property or trade secrets; and competition.
Safe Harbor
2 |
 •
Titan Pharmaceuticals Highlights
•
Probuphine Development
•
Probuphine Market Opportunity
•
Financial Summary
•
Summary
Presentation Content
3 |
 •
Specialty pharmaceutical company focused in CNS with an NDA
submission
for
Probuphine™
expected
in
Q3,
2012
•
Probuphine has the potential to be the first long acting therapeutic
on the market for the treatment of opioid dependence
–
Six month controlled release formulation of an approved drug, buprenorphine
–
Clinical development completed
–
Addresses U.S. market of over $1B and growing
–
Significant unmet needs continue to exist in the market place
–
Potential peak sales of $300m –
$500m
–
U.S. patent life to 2024
–
Probuphine has the potential to be developed for treating chronic pain
•
ProNeura™
–
unique long term drug delivery system can provide
around the clock medication and has potential in additional
applications
•
Near term value-creating milestones
•
Lean and capital efficient organization
Titan Pharmaceuticals: Highlights
4 |
 Probuphine Development
5 |
 •
Addiction is a primary, chronic disease of brain reward,
motivation, memory and related neurobiological circuitry*
•
inability to consistently abstain
•
impairment in behavioral control
•
craving
•
diminished recognition of significant problems with one’s behaviors
•
Addiction involves cycles of relapse and remission
•
Without treatment or engagement in recovery activities, addiction
is progressive and can result in disability or premature death
*American Society of Addiction Medicine, Inc., 2011
Disease Overview
6 |
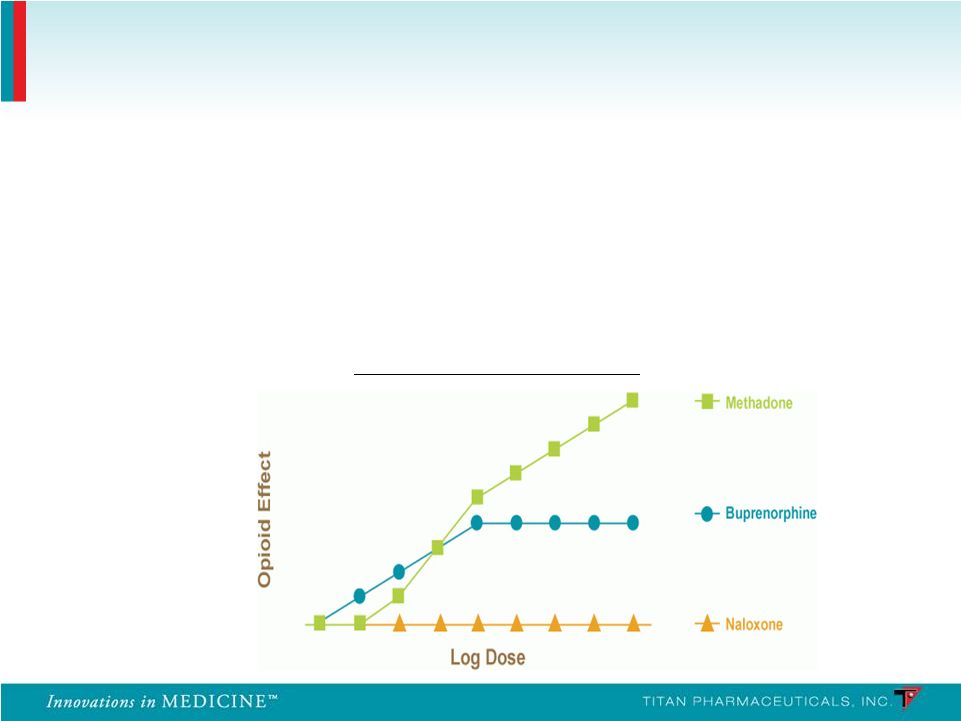 •
In the U.S. buprenorphine has replaced methadone as the gold standard in treating
opioid dependence
•
Buprenorphine is a mixed partial agonist at the mu receptor and an antagonist at
the kappa receptor
•
Ceiling effect
•
Improved safety profile
•
Lack of euphoria
Ceiling
Effect
of
Buprenorphine
Disease Treatment Overview
7 |
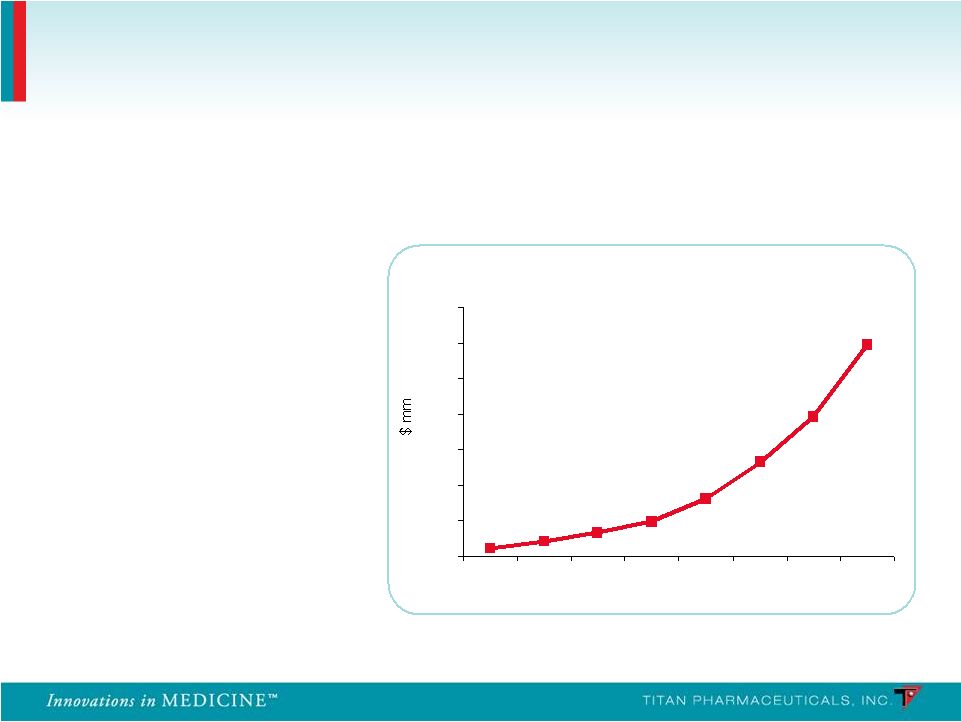 Launched in 2003
Global sales exceed
$1.2B in 2010 (U.S.
sales of $1B)
Source: EvaluatePharma; Reckitt Benckiser 2010 Annual Report
Suboxone
®
Franchise WW Sales
0
200
400
600
800
1000
1200
1400
2003
2004
2005
2006
2007
2008
2009
2010
58% CAGR for
the last 4 years
Suboxone has grown rapidly
Incremental Treatment Improvements Have Driven
Conversion and Growth of the Market
8 |
 •
Efficacy
•
Medication compliance
•
Retention of patients
•
Reduction in the use of opioids and other substances
•
Safety and tolerability
•
Risks of misuse, abuse, diversion
•
Risk of precipitating withdrawal
•
Risk of overdose
Significant Unmet Medical Needs in the Treatment of
Opioid Dependence
9 |
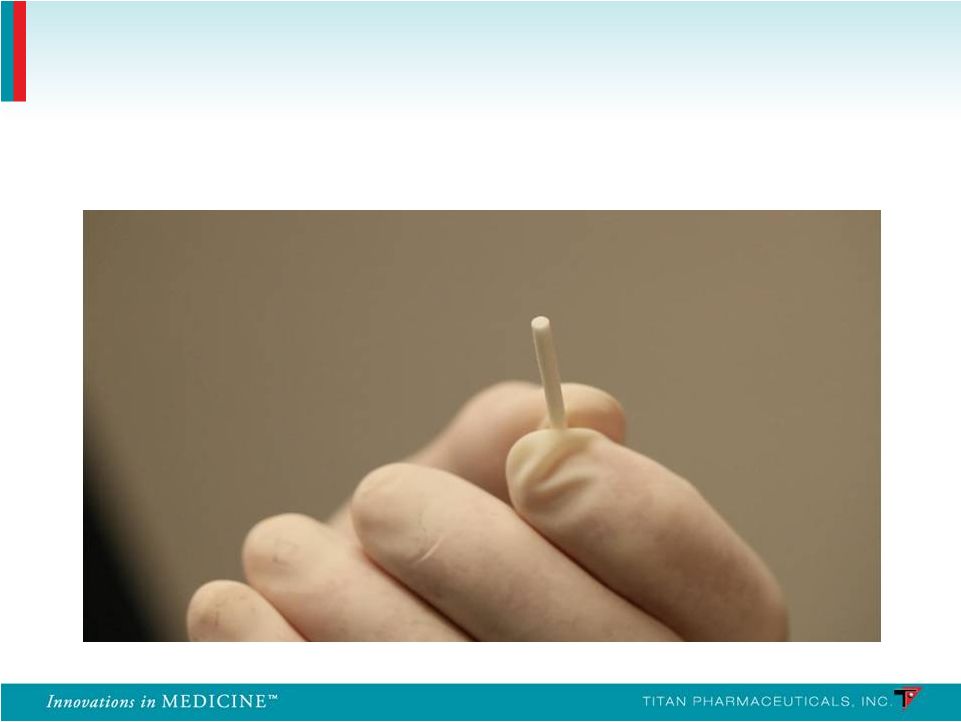
 Solid Matrix Long-Term Delivery
•
Non-biodegradable
•
Inserted subcutaneously
•
Stable non-fluctuating blood levels of drug maintained for over 6 months
Probuphine is a subcutaneous implant capable of delivering continuous and
persistent around the clock blood levels of buprenorphine for 6 months
following a single treatment, enhancing patient compliance and retention
Probuphine
10 |
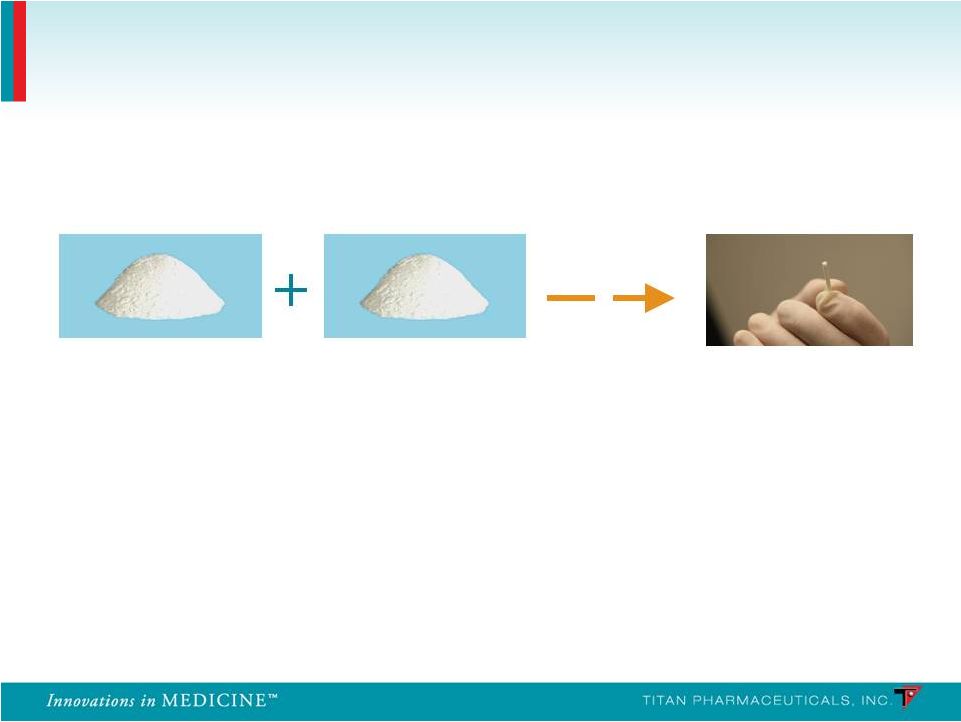 EVA
polymer Buprenorphine
Each implant contains 80 mg of buprenorphine HCl which has been blended and
extruded with ethylene vinyl acetate (EVA) co-polymer
Probuphine
Probuphine
11
26 mm long,
2.5 mm
diameter
Inert component of
several
approved products
Approved for treatment of
opioid addiction, and
acute and chronic pain
Blended
&
Extruded |
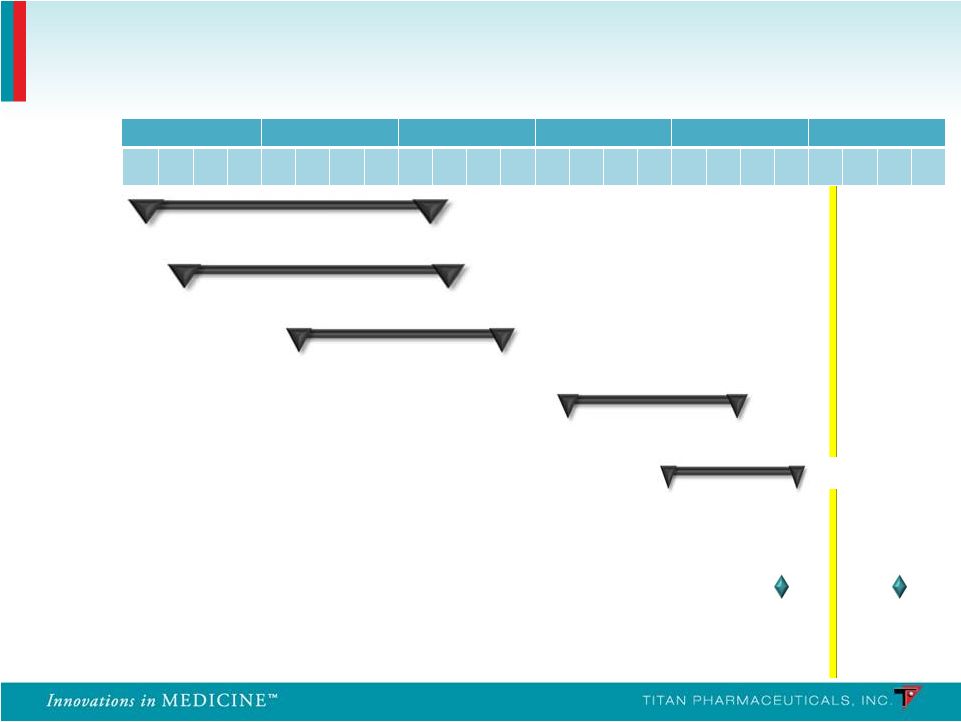 PRO-810
Pharmacokinetics
Pharmacokinetics
PRO-806
U.S. Efficacy 2
U.S. Efficacy 2
Pre-NDA meeting
U.S. Retreatment 2
U.S. Retreatment 2
2007
2008
2009
2010
2011
2012
Q
1
Q
2
Q
3
Q
4
Q
1
Q
2
Q
3
Q
4
Q
1
Q
2
Q
3
Q
4
Q
1
Q
2
Q
3
Q
4
Q
1
Q
2
Q
3
Q
4
Q
1
Q
2
Q
3
Q
4
PRO-805
U.S. Efficacy 1
U.S. Efficacy 1
PRO-807
U.S. Retreatment 1
U.S. Retreatment 1
n = 163
n = 163
n = 62
n = 62
n = 9
n = 9
n = 287
n = 287
n = 85
n = 85
Probuphine: Clinical Development Program
NDA
NDA
submission
submission
12
PRO-811 |
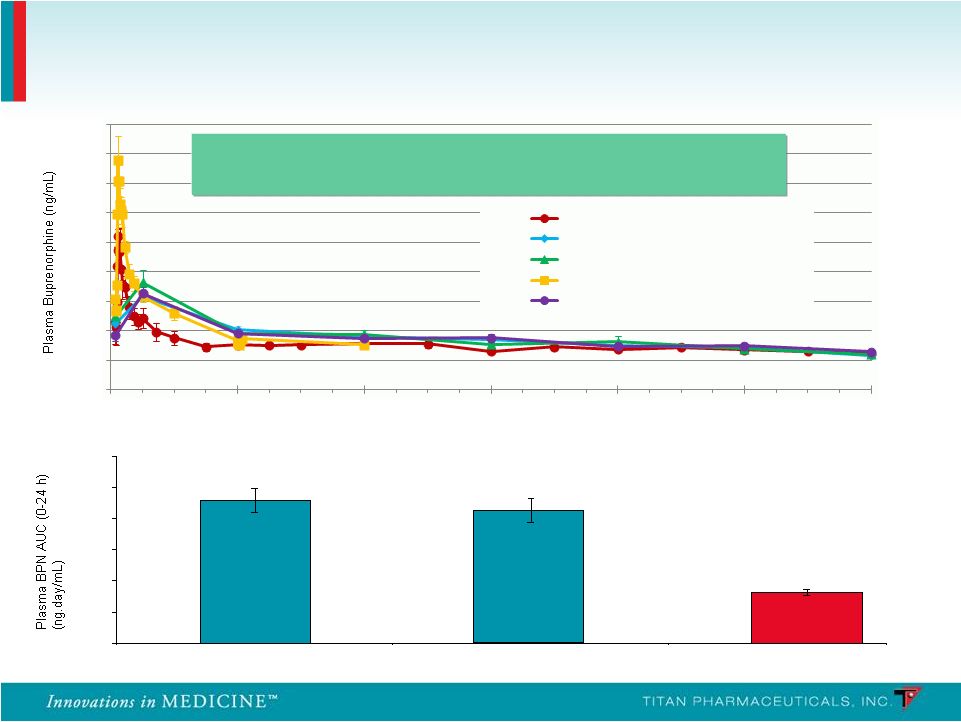 PRO
810 – Mean Plasma Buprenorphine AUC (0-24 h)
2.29
2.13
0.82
0
0.5
1
1.5
2
2.5
3
Suboxone (Day -2)
Suboxone (Day -1)
Probuphine
(Steady State)
Probuphine: Plasma Pharmacokinetics
13
Continuous, around the clock medication maintaining a
Continuous, around the clock medication maintaining a
stable level of buprenorphine in the patient
stable level of buprenorphine in the patient
Weeks on Study
0.00
0.50
1.00
1.50
2.00
2.50
3.00
3.50
4.00
4.50
0
4
8
12
16
20
24
Phase 1/2 (4 implants, n=6)
PRO
805 (4 or 5 Implants, n=104)
PRO
807 (4 or 5 Implants, n=61)
PRO
810 (4 Implants, n=9)
PRO
806 (4 or 5 Implants, n=113)
-
-
-
- |
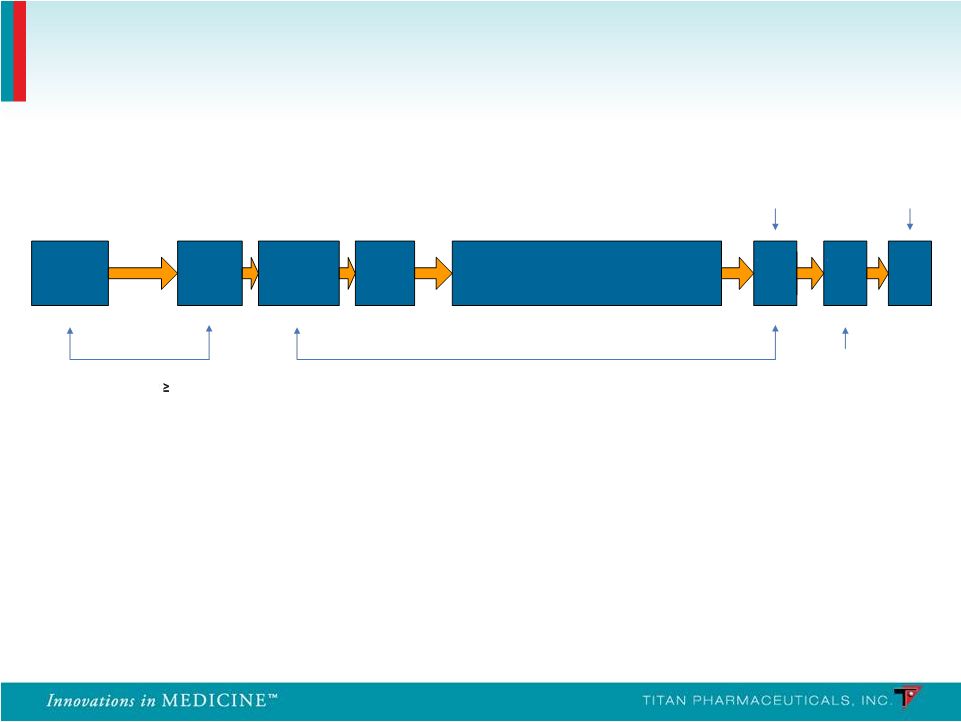 Study 2 (PRO-806):
•
n = 287; 20 sites
•
Three-arm: Double-blind
randomized, placebo-controlled
and open-label active
(Suboxone)
Study 1 (PRO-805):
•
n = 163; 18 sites
•
Two-arm: Double-blind
randomized, placebo-
controlled
(Urine Toxicology Three Times Per Week)
Probuphine: Two Phase 3 Controlled Studies
14
Up to 16 days
SL BPN Dose
12
16 mg/day
3 Days
6-month Treatment Phase
Telephone
Call
Implant Removal
End of Treatment /
Induction
Follow-up
Screening
Baseline
Implant
Visit
Randomize/
-
Post
Implant
Treatment and
x/
week Urine Visits
3
(Weeks 1 –
24)
Week
24
Week
26
Week
25
- |
 •
Urine toxicology (blinded to sites and patients)
•
Tests for presence of opioids (heroin, methadone, prescription pain medications,
etc.)
•
Clinical Global Improvement
•
Clinician-rated
•
Patient-rated
•
Symptoms of opioid withdrawal and craving
•
Clinician-rated (COWS)
•
Patient-rated (SOWS and craving VAS)
•
Patient-reported illicit drug use
•
Mood
•
Beck Depression Inventory II
Study Assessments
15 |
 Outcome Measures
Outcome Measures
Probuphine
Probuphine
> Placebo
> Placebo
CDF of % Negative Urines
(24 weeks)
p = 0.0117 (primary)
Treatment Retention
(24 weeks)
p < 0.0001
Global Severity of Opioid Addiction
(Patient Rated)
(24 Weeks)
p < 0.0021
Global Severity of Opioid Addiction
(Physician Rated)
(24 Weeks)
p < 0.0086
Patient-rated opioid withdrawal
(24 weeks)
p = 0.0005
Clinician-rated opioid withdrawal
(24 weeks)
p = 0.0008
Opioid craving
(24 weeks)
p = 0.0006
Study 1: Efficacy Results –
Probuphine vs Placebo
16 |
 Outcome Measures
Outcome Measures
Probuphine > Placebo
Probuphine > Placebo
p < 0.0001 (primary)
p < 0.0001 (primary)
p = 0.0002
p = 0.005
p = 0.031
p = 0.0003
p = 0.0002
p < 0.0001
p < 0.0001
p < 0.0001
Study 2: Efficacy Results –
Probuphine vs Placebo
17
CDF of % Negative Urines
(24 weeks)
CDF of % Negative Urines Incorporating Patient
Self Report (24 weeks)
Treatment Retention
(24 weeks)
Patient-Rated Global Severity
Global Improvement
(24 Weeks)
Clinician-Rated Global Severity
Global Improvement
(24 Weeks)
Patient-rated opioid withdrawal
(24 weeks)
Clinician-rated opioid withdrawal
(24 weeks)
Opioid craving
(24 weeks) |
 Probuphine vs. Suboxone: Percentage of Urine Samples
Probuphine vs. Suboxone: Percentage of Urine Samples
Negative for Illicit Opioids in Weeks 1-24
Negative for Illicit Opioids in Weeks 1-24
•
Non-Inferiority Comparison (-15% Margin):
•
31% Probuphine vs. 33% Suboxone
•
95% Confidence Interval for Difference:
-10.8, 5.9
•
Least-Squared Means Comparison:
•
36% Probuphine vs. 35% Suboxone
Study 2: Efficacy Results –
Probuphine vs Suboxone
18 |
 PRO-805
End
of
Treatment
/
PRO-807
Baseline
Start
SL
BPN
Induction
Implant
Visit
/
4
Probuphine
Implants
Post-
Implant
Visit
Wk
1
Wk
24
Wk
25
Wk
26
Wk
8
Wk
12
Wk
16
Wk
20
Wk
4
Implants Removed
Stop Sublingual Buprenorphine
12-24 Hours
Prior to
Implantation
End of
Treatment/
Implant
Removal
Follow-Up
Visit
Telephone
Call
24 Hours
Up to 14 Days
Six-Month, Open-Label, Multicenter Retreatment Trials in
Patients Completing the Controlled Studies
PRO -
807
•
14 study sites in the U.S.
•
62 patients who completed PRO-805
received 4 initial Probuphine implants
•
6 patients received a 5
th
implant
PRO -
811
•
20 study sites in the U.S.
•
85 patients who completed PRO-806
received 4 initial Probuphine implants
•
Study completed end of Dec 2011 and initial
results released in Feb 2012
19 |
 •
Probuphine was clinically and statistically superior to placebo in the
treatment of opioid-addicted patients, and demonstrated non-inferiority to
Suboxone.
•
Adverse events were mild to moderate in severity and generally consistent
with the patient population and the known safety profile of buprenorphine in
all studies.
•
Early termination due to adverse events was low in all studies.
•
The number and profile of serious adverse events was low in all studies and
similar to placebo.
•
The implant procedure was generally well tolerated in all studies and there
was no evidence of implant diversion or misuse.
•
Probuphine delivers an efficacious, low level of buprenorphine continuously
for six months.
Clinical Summary
20 |
 •
Pre-NDA meeting completed with the FDA on October 25, 2011
•
Clinical
data
on
safety
and
efficacy
of
Probuphine
considered
to
be
sufficient for NDA submission
•
Manufacturing scale up plans are acceptable to the FDA, however,
additional data on the characterization of the EVA and Probuphine is
required to complete the Chemistry, Manufacturing and Controls
section
•
FDA provided guidance on the requirements for a Priority Review
designation and suggested that appropriate information should be
included with the NDA submission
•
NDA submission is targeted for Q3, 2012
•
CMC section related analytical testing underway at two vendors
•
Electronic NDA document preparation commenced at CRO
•
Manufacturing facility expansion and production scale-up in process
NDA Preparation Status
21 |
 •
Buprenorphine has several advantages over other opioids used for
chronic pain
•
Safer than other opioids
–
ceiling effect for respiratory depression, relatively long half-life, minimal
euphoric effect
•
Buprenorphine transdermal patch (3-7 days) is approved in U.S.,
Europe and Australia for the treatment of moderate to severe chronic
pain
•
Therapeutic window of 0.1 –
0.5 ng/ml plasma level can be delivered with
1 to 2 Probuphine implants
•
Probuphine value proposition for treating chronic pain
•
Around the clock non-fluctuating therapeutic levels, no on/off therapy
cycling, enhances compliance and increases patient convenience
Sources: NEJM 2003;349:1943-53
Sittl, Expert Rev. Neurotherapeutics 2005;5(3): 315-323
Probuphine for the Treatment of Chronic Pain
22 |
 Probuphine Market Opportunity
23 |
 •
Prevalence is large and growing rapidly
•
Worldwide: > 6m persons addicted to opioids
•
U.S. > 2m, range varies between 2-4m depending on source
•
Opioid addiction is a chronic long term illness
•
Patients who stop all medically-assisted therapy (MAT) are highly
susceptible to relapse
•
Opioid addiction market is now >$1.2B globally
•
Opioid prescriptions have grown 400% from 1997-2007
•
Hospitalizations have increased 500% over the last 10 years
•
Treatment for abuse of pain relievers increased at a 13% CAGR
from 2002-2009
Sources: EPIDEMIC: RESPONDING TO AMERICA’S PRESCRIPTION DRUG ABUSE CRISIS,
Executive Office of the President of the United States (2011); 2009 National Survey on
Drug Use and Health (NSDUH); “A Wave of Addiction and Crime, with the Medicine
Cabinet to Blame”, New York Times (Sept 23, 2010); Drug Abuse Warning Network (DAWN),
SAMHSA, HHS; “A General in the Drug War”, New York Times (Jun 14,
2011) Market Overview
24 |
 •
Methadone tablets mainstay for opioid addition in U.S. from late
1960’s to 2002
•
Strong
restrictions
regarding
patient
access
and
administration
access
in
U.S.
•
Can be lethal and has high potential for misuse, abuse and diversion
•
Subutex
®
and Suboxone
®
oral formulations approved in 2002
•
Safer than methadone and other opioids
•
Buprenorphine can occupy opioid receptors but produces ”ceiling
effect” •
Mitigates euphoric effect and respiratory depression
•
Fewer restrictions on patient access
•
Enabled treatment in office-based setting
•
Misuse, abuse and diversion problematic
•
Naltrexone
•
Opioid antagonist
•
Must be completely detoxified before initiating therapy
•
Minority of opioid addicted patients succeed
Competitors: Few and Well Established with no New
Innovations on Immediate Horizon
25 |
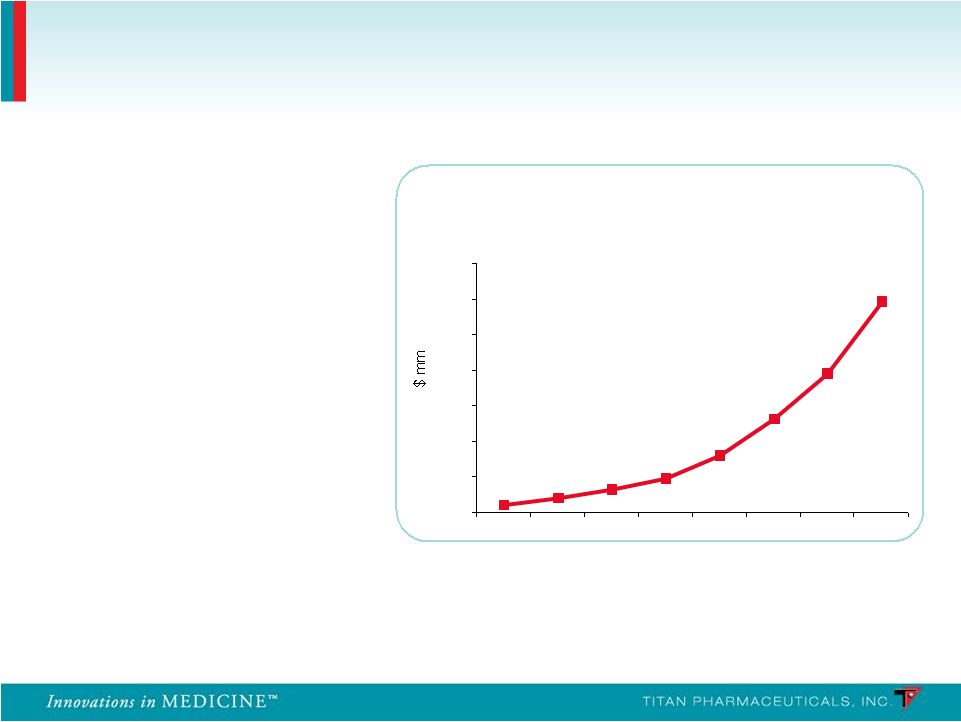 •
Launched in 2003
•
Global sales exceed $1.2B in 2010 (U.S. sales of $1B)
Source: EvaluatePharma; Reckitt Benckiser 2010 Annual Report
Suboxone
®
Franchise WW Sales
0
200
400
600
800
1000
1200
1400
2003
2004
2005
2006
2007
2008
2009
2010
58% CAGR for
the last 4 years
90% of prescriptions
were written by 5,037
physicians
Suboxone
®
Sales
Exceed $1B a Year in
the U.S.
Suboxone
®
sales
have
grown at a 58% CAGR
over the last 4 years
Extremely Concentrated Prescriber Base
26 |
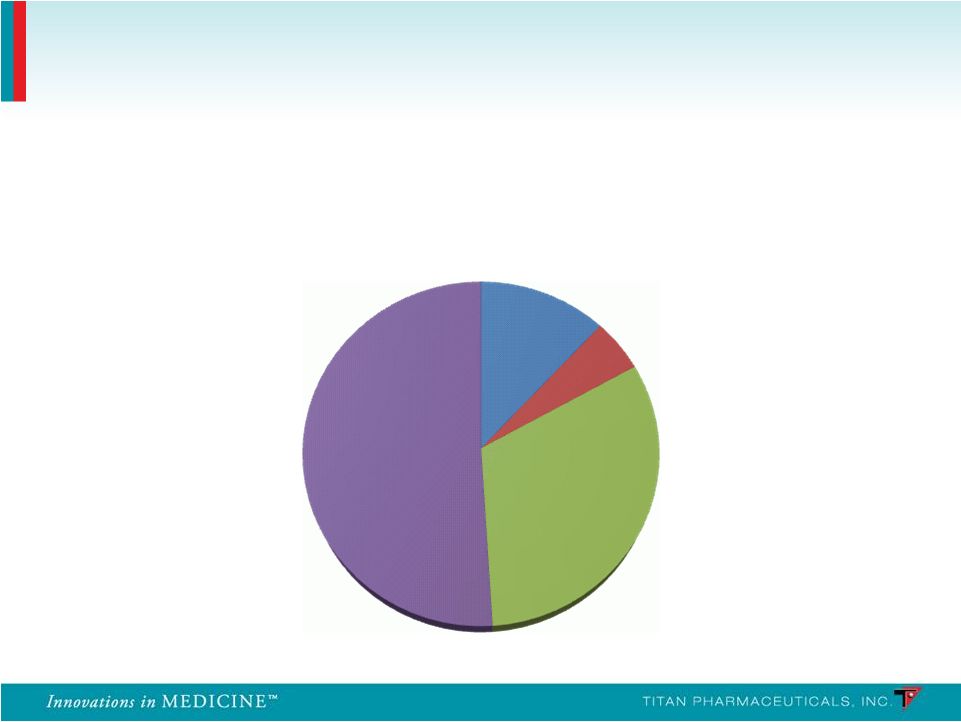 Suboxone Prescribing Physicians
27
Breakdown of Suboxone Prescribing Physicians
Other
12%
Pain/Neuro
5%
Psych
32%
IM/FP/GP
51%
Source: IMS Health |
 •
Efficacy
•
Reduction in the use of opioids
•
Retention of patients and their treatment on therapy
•
Reduction in the use of other substances
•
Safety and tolerability
•
Risk of overdose
•
Risk of misuse, abuse, diversion
•
Risk of precipitating withdrawal
•
Accessibility / cost
•
Delivery
•
Onset of action
•
Restrictions on administration
Source: Decision Resources 2011
Top Unmet Needs Defined by Physicians
28 |
 Efficacy
Effective in reducing illicit opioid use
Enhanced compliance may lead to superior outcomes
Safety
Lower drug exposure may provide superior safety and tolerability
Ease of Use
Unique delivery system dosed once every six months
Continuous buprenorphine delivery
•
Non-fluctuating blood levels, around-the clock medication
•
Potential 100% compliance
Diversion
Limited access to implants
•
Subcutaneous placement
•
Specific distribution (non-retail)
Probuphine Value Proposition
Probuphine is the first and only potential treatment for opioid dependence
that can provide continuous and persistent around the clock blood levels
of buprenorphine for six months, enhancing patient compliance and
retention and preventing diversion
29 |
 •
Billion dollar market large and growing
•
Significant unmet needs continue to exist in the market
place
•
Excellent margins due to small, target prescriber population
•
5,037
physicians
wrote
90%
of
buprenorphine
prescriptions
in
the
U.S.
in
2010
•
Sales Force of 50 reps can cover majority of prescribers
•
Controlled distribution facilitates efficiency and maintenance of accounts
•
Unique value proposition for Probuphine better addresses
unmet needs and has the potential to become the new gold
standard
of
treatment
–
Peak
sales
$300-500m
Market Opportunity Ideal as Specialty Pharma Stand-
alone or as an Addition to Existing CNS Franchise
30 |
 •
Patent applications are for method-of-use claims
•
Method-of-use and similar claims provide strong protection of commercial
product: •
Alternate device or alternate indication would require de novo clinical
trials Country
Opioid Dependence
U.S.
Granted (to 2024)
Pending
Europe
Pending
Pending
Japan
Granted (to 2023)
Granted (to 2023)
Canada
Pending
Pending
Mexico
Granted (to 2023)
Granted (to 2023)
Australia
Granted (to 2023)
Granted (to 2023)
New Zealand
Granted (to 2023)
Granted (to 2023)
Hong Kong
Pending
Pending
India
Pending
Pending
Probuphine Intellectual Property
31
Pain Treatment |
 •
Equity
•
Common Stock Outstanding
59.4m
•
Stock Options/ Restricted Stock
5.6m
–
weighted-average exercise price of $1.56 per share
•
Warrants
13.0m
–
weighted-average exercise price of $1.78 per share
•
December 30, 2011
•
Cash
$ 5.4m
•
Debt
$ 12.3m
–
Principal $10m + Present Value of Interest $2.3m
Financial Summary
32 |
 Probuphine
•
Billion dollar opioid dependence market is large and growing
•
Worldwide: > 6m people addicted to opioids
•
Addresses significant unmet needs that exist in the market place
•
Reduction in the use of opioids
•
Retention of patients on therapy (persistence and compliance)
•
Diversion, abuse
•
Probuphine has the potential to be the first long acting therapeutic on the
market for the treatment of opioid dependence
•
Six month controlled release formulation of buprenorphine has key advantages in
patient compliance to treatment, and avoidance of diversion/abuse
•
$300-500m potential annual peak sales in opioid dependence
•
Potential application in treating chronic pain
•
Goal to establish U.S. commercialization partnership by the time
of NDA filing
ProNeura
•
Possible applications of technology for long term drug delivery in other
chronic illnesses, e.g. Parkinson’s Disease
Titan Pharmaceuticals Summary
33 |
 Marc Rubin, M.D.
July 30, 2008
34 |
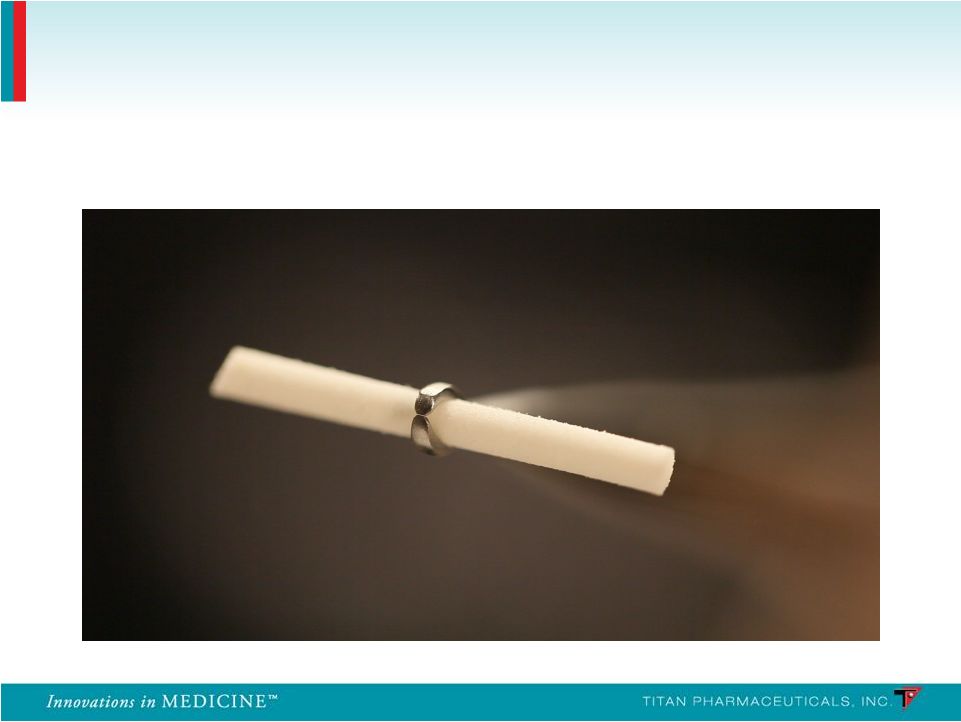
 Buprenorphine Implant
35 |
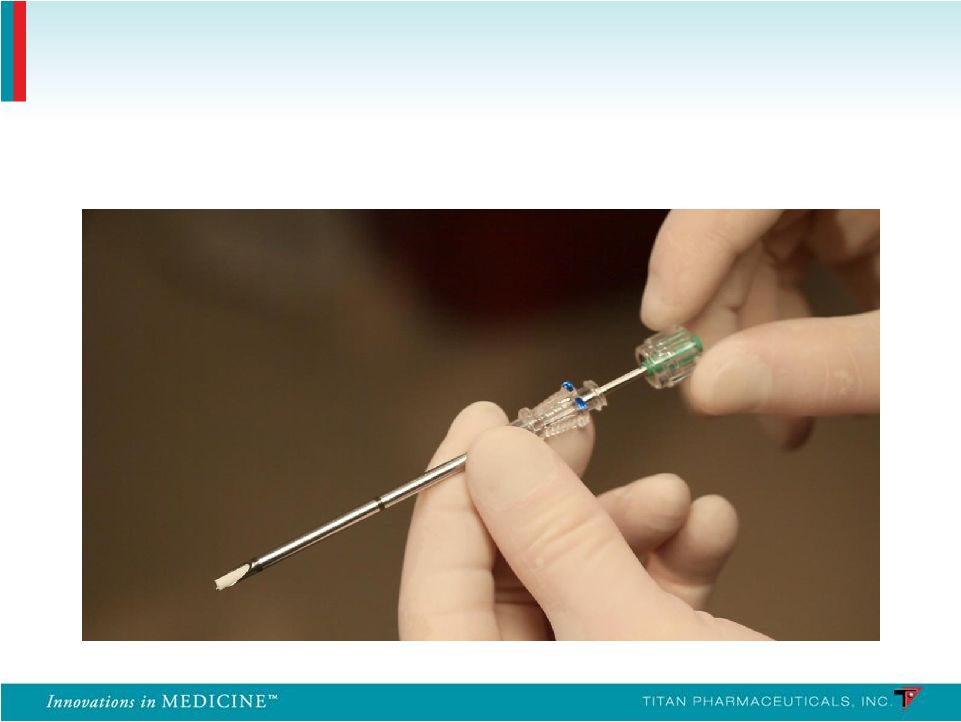 Insertion Applicator
36 |
 Insertion Location
37 |
 Removal Clamp
38 |
 Summary of Non-Implant Site Adverse Events
Frequency (
10% in Any Treatment Group)
PRO-805
PRO-807
Probuphine
(n = 108)
Placebo
(n = 55)
Probuphine
(n = 62)
System Organ Class
n
%
n
%
n
%
Any Adverse Events
85
78.7
41
74.5
43
69.4
Gastrointestinal
Constipation
15
13.9
3
5.5
8
12.9
Diarrhea
6
5.6
7
12.7
2
3.2
Nausea
15
13.9
7
12.7
2
3.2
Toothache
12
11.1
3
5.5
3
4.8
Infections
Nasopharyngitis
15
13.9
3
5.5
2
3.2
Upper Respiratory
14
13.0
6
10.9
3
4.8
Musculoskeletal
Back Pain
13
12.0
3
5.5
5
8.1
Nervous System
Headache
27
25.0
10
18.2
11
17.7
Psychiatric
Anxiety
11
10.2
5
9.1
2
3.2
Insomnia
23
21.3
12
21.8
8
12.9
39 |
 PRO-806
PRO-811
Probuphine
(n = 114)
Placebo
(n = 54)
Suboxone
(n = 119)
Probuphine
(n = 85)
System Organ Class
n
%
n
%
n
%
n
%
Any Adverse Events
77
67.5
33
61.1
85
71.4
57
67.1
Gastrointestinal
Constipation
5
4.4
1
1.9
5
4.2
2
2.4
Diarrhea
2
1.8
3
5.6
2
1.7
2
2.4
Nausea
7
6.1
1
1.9
8
6.7
3
3.5
Toothache
4
3.5
1
1.9
5
4.2
3
3.5
Infections
Nasopharyngitis
6
5.3
3
5.6
12
10.1
2
2.4
Upper Respiratory
10
8.8
4
7.4
11
9.2
7
8.2
Musculoskeletal
Back Pain
6
5.3
3
5.6
7
5.9
5
5.9
Nervous System
Headache
15
13.2
5
9.3
19
16.0
10
11.8
Psychiatric
Anxiety
2
1.8
3
5.6
6
5.0
3
3.5
Insomnia
9
7.9
8
14.8
16
13.4
2
2.4
Summary of Non-Implant Site Adverse Events
Frequency ( 10% in Any Treatment Group)
40 |
 Summary of Implant Site Adverse Events Frequency
(
10%
in
Any
Treatment
Group)
PRO-805
PRO-807
PRO-806
PRO-811
Probuphine
(n = 108)
Placebo
(n = 55)
Probuphine
(n = 62)
Probuphine
(n = 114)
Placebo
(n = 54)
Probuphine
(n = 85)
Erythema
25.0%
21.8%
25.8%
3.5%
0%
1.2%
Edema
13.0%
9.1%
12.9%
1.8%
0%
0.0%
Itching
25.0%
14.5%
19.4%
4.4%
3.7%
1.2%
Pain
22.2%
10.9%
19.4%
8.8%
9.3%
0.0%
Bleeding
12.0%
12.7%
16.1%
1.8%
3.7%
3.5%
Bruising
5.6%
14.5%
9.7%
7.9%
11.1%
3.6%
Scar
9.3%
12.7%
1.6%
0%
0%
1.6%
41 |
