Attached files
| file | filename |
|---|---|
| 8-K - FORM 8-K - TENET HEALTHCARE CORP | d8k.htm |
| EX-99.1 - COMPLAINT - TENET HEALTHCARE CORP | dex991.htm |
 Summary of Allegations in the Complaint
Filed by Tenet Healthcare Corporation
Against Community Health Systems
April 11, 2011
Exhibit 99.2 |
  2
Additional Information
Tenet Healthcare Corporation (“Tenet”) will file with the Securities and
Exchange Commission (“SEC”) a proxy statement, accompanied by a
WHITE proxy card, in connection with its 2011 annual meeting of stockholders. Any definitive proxy
statement will be mailed to stockholders of Tenet. INVESTORS AND
SECURITYHOLDERS OF TENET ARE URGED TO READ THESE AND OTHER DOCUMENTS FILED
WITH THE SEC CAREFULLY IN THEIR ENTIRETY WHEN THEY BECOME AVAILABLE BECAUSE
THEY WILL CONTAIN IMPORTANT INFORMATION. Investors and securityholders will
be able to obtain free copies of these documents (when available) and other
documents filed with the SEC by Tenet through the website maintained by the
SEC at http://www.sec.gov. The information contained in this filing is a
summary of allegations made in a complaint filed by Tenet against Community
Health
Systems,
Inc.,
Wayne
T.
Smith,
and
W.
Larry
Cash
on
April
11,
2011,
in
the
United
States
District
Court
for
the
Northern District of Texas. A copy of the complaint has been filed by Tenet
with the SEC and is available through the website maintained by the SEC at
http://www.sec.gov. Certain Information Regarding Participants
Tenet and certain of its respective directors and executive officers are deemed to
be participants under the rules of the SEC. Information regarding
these participants is contained in a filing under Rule 14a-12 filed by Tenet with the SEC on January 7,
2011. This filing and other documents can be obtained free of charge from the
source indicated above. Additional information
regarding
the
interests
of
these
participants
in
any
proxy
solicitation
and
a
description
of
their
direct
and
indirect
interests, by security holdings or otherwise, will also be included in any proxy
statement and other relevant materials to be filed with the SEC if and when
they become available. Legal disclaimer |
  3
Overview
CHS has for many years systematically billed cases as higher-paying inpatient
admissions that would have been billed as lower-paying outpatient
observations in most U.S. hospitals. CHS’ strategy specifically focuses on converting
emergency room visits to medically unnecessary inpatient admissions.
When patients present themselves to hospitals, they are either 1) seen and
discharged; 2) placed in
outpatient
observation
status;
or
3)
admitted
as
inpatients.
Doctors
make
the
treatment
decision, with input from hospital employees. Most (>75%) U.S. hospitals
use one of two objective systems as the basis for these determinations. CHS
uses its own set of “Admissions Justifications” called the
“Blue Book.” The difference in Medicare payments between an
outpatient observation stay and an inpatient admission is
substantial. Other payers (e.g., Medicaid and Managed Care) generally pay more for
inpatient admissions than for observations, but actual rates depend on contracts.
Only Medicare fee-for-service data is publicly available.
CHS’
use of observation status is less than half the national average rate for
U.S. hospitals. There is no legitimate explanation for the difference.
No other publicly traded hospital company follows a similar practice.
|
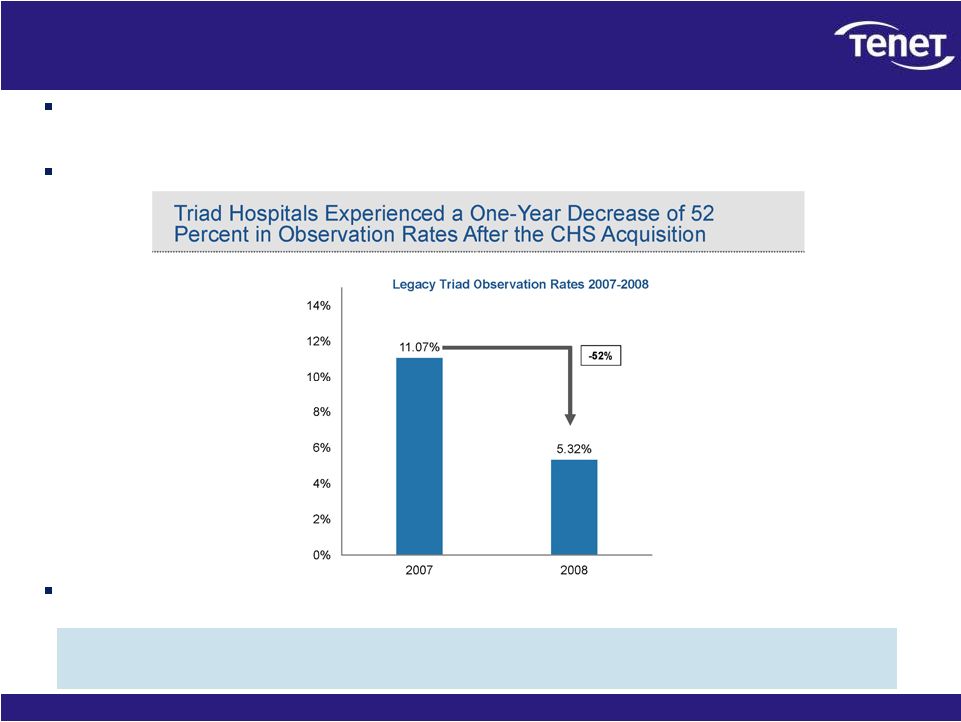
  4
CHS’
strategy
of
driving
up
admissions
and
driving
down
observations
is
unsustainable:
It depends
on
a
continuing
pipeline
of
acquisitions
of
hospitals
with
normal
observation rates that can be driven down. CHS dropped Triad’s observation
rate 52% following the acquisition.
Low observations, one-day stays, and related issues are already a focus area
of government investigators and contractors.
Implications for CHS:
Unwinding the strategy will materially reduce admissions, revenues, profits, and
cash flows going forward.
Potential
liability
is
well
in
excess
of
$1
billion
for
2006
–
2009
for
the
Medicare
fee-
for-service portion of CHS’
business alone.
Serious
questions
are
raised
regarding
the
accuracy
of
CHS’
historical
financial
statements.
Implications for CHS’
$6 proposal to acquire Tenet:
CHS’
stock is worth less than stated.
CHS’
ability to finance the cash portion of the offer may
be impaired. Overview, cont. |
  5
What is the nature of this litigation?
The litigation seeks to compel CHS to disclose fully its unique and
non-industry standard patient admissions criteria and billing practices
and the financial and legal implications arising
from
them.
Under
SEC
rules,
CHS’
statements
are
proxy
solicitation
materials
directed toward Tenet’s stockholders.
CHS’
actions have resulted in materially misleading financial reports and
statements: •
Admissions statistics and trends have been overstated.
•
Revenues, profits, and cash flows have been overstated.
•
CHS’
explanations of business trends have been misleading.
•
CHS’
explanations of synergies from acquired hospitals have been misleading and
incomplete. CHS has followed an unsustainable business practice that is
inconsistent with Federal regulations.
Substantial
undisclosed
liabilities
may
exist
to
Medicare,
state
Medicaid
programs,
private
insurance companies, and patients.
The litigation seeks to compel CHS to fully and accurately disclose the
risks and financial impact of its admissions strategy, and to prevent
further misleading statements. |
  6
Has CHS violated Medicare requirements?
Medicare reimburses hospitals only for treatment that is “reasonable and
necessary.” 42 U.S.C.
§
1395y(a)(1)(A).
Inpatient care rather than outpatient care is required only if the patient’s
medical condition, safety or health would be significantly and directly
threatened if care was provided in a less intensive setting. Medicare Program Integrity Manual, Chapter 6, Section 6.5.2.
Outpatient observation is a well-defined set of specific, clinically
appropriate services, which include ongoing short term treatment, assessment
and reassessment, rendered before a decision can be made regarding whether a
patient will require further treatment as an inpatient or is able to be
discharged. Observation services are commonly ordered for patients who
present to the emergency department and who require a period of
treatment
or
monitoring
before
making
a
decision
on
admission
or
discharge.
Medicare
Benefit
Policy Manual, Chapter 6, Section 20.6. See also Medicare Claims
Processing Manual, Chapter 4, Section 290. CHS causes patients to be
admitted to its hospitals who should be observed under Medicare
requirements. CHS overbills these cases as inpatient admissions when they
should be billed as outpatient observations.
CHS systematically overbills Medicare and likely other payers.
|
  7
How did Tenet learn of these practices?
CHS stated on a December 10, 2010 conference call that a combination with Tenet
would offer opportunities for synergies.
Tenet conducted due diligence to evaluate potential synergies that might be created
through a combination with CHS.
Tenet’s independent consultant, using the American Hospital Directory
database, found significant discrepancies
between admission patterns at CHS and the industry. Tenet
then
engaged
a
second
consulting
firm,
Avalere
Health
LLC,
to
perform
a
second
independent
analysis
using
the
Centers
for
Medicare
&
Medicaid
Services’
Inpatient
Prospective Payment System Standard Analytic Files (which contains source data from
which the MedPAR database is constructed) and Outpatient Standard Analytic
Files. Each analysis found CHS’
observation rate* to be significantly lower than the industry and
its peer companies.
CHS “grew”
admissions by implementing dramatic reductions in observation status at
hospitals it acquired, particularly in the case of Triad.
Two independent consultants have confirmed that
CHS’
observation rate is less than half of the national average.
* A hospital’s “observation rate” is essentially the percentage of patients treated in
a hospital bed that are billed as “observation” rather than “inpatient.”
|
  8
CHS’
strategy inflates admissions, revenues,
profits, and cash flows
CHS admitted approximately 62,000 Medicare fee-for-service patients from
2006-2009 (approximately 20,000 in 2009 alone) who would have been
observed as outpatients if CHS’
observation rate were at the national average.
CHS admitted approximately 82,000 Medicare fee-for-service patients from
2006-2009 (approximately 31,000 in 2009 alone) who would have been
observed as outpatients if CHS’
observation rate were the same as LifePoint.
Taking only CHS’
highest volume and lowest acuity Medicare patients, CHS receives, on
average,
over
$3,300
(or
approximately
257%)
more
per
“admitted”
patient than
“observed”
patient.
Medicare
fee-for-service
patients
generated
27%
of
CHS’
net
operating
revenue
in
2010.
The effect of CHS’
admissions strategy on its performance is much greater if the strategy
has been applied across all patient categories.
This practice results in greater profits to CHS, but additional costs to Medicare,
and likely to Medicaid programs, private insurance companies, and
patients. CHS systematically overbills Medicare, and likely other
payers, overstating profits. |
  9
These practices may subject CHS to substantial
undisclosed liability
Under the Federal False Claims Act, the government may recover damages of up to
three times the originally billed amount, plus penalties of up to $11,000
per false claim. 31 USC §
3729(a).
As a result of CHS’
admissions practices, it may have overbilled payers for Medicare fee-
for-service patients by approximately $280 million to $377 million in
2006-2009 alone. If treated
as
false
claims,
this
conduct
could
result
in
liabilities
well
in
excess
of
$1
billion
for
2006-2009 alone.
As the Blue Book was copyrighted in 2000, it appears the practice of driving down
observation status has existed for at least ten years.
During this same period, CHS likely overbilled other payers as well, such as
Medicare Advantage plans.
CHS’
hospitals may also be subject to exclusion from participating in Medicare.
CHS may have significant financial exposure and could face exclusion
from participating in Medicare.
* |
  10
CHS’
admissions practices are not sustainable
The
Office
of
Inspector
General
of
the
U.S.
Department
of
Health
and
Human
Services (“OIG”) closely scrutinizes medically unnecessary inpatient
admissions.
In late 2010, Medicare Recovery Audit Contractors (RACs) began recovering
overpayments from medically unnecessary inpatient admissions.
Numerous non-CHS hospitals with low observation rates have been
investigated by the U.S. Department of Justice.
In its 10-K, CHS disclosed that the OIG issued a subpoena for documents
related to, among other things, CHS’
admissions criteria, case management,
coding, billing, and compliance in its hospital in Laredo, Texas. CHS also
disclosed that the Attorney General of Texas issued Civil Investigative
Demands for all of CHS’
hospitals in Texas concerning “emergency department
procedures and billing.” |
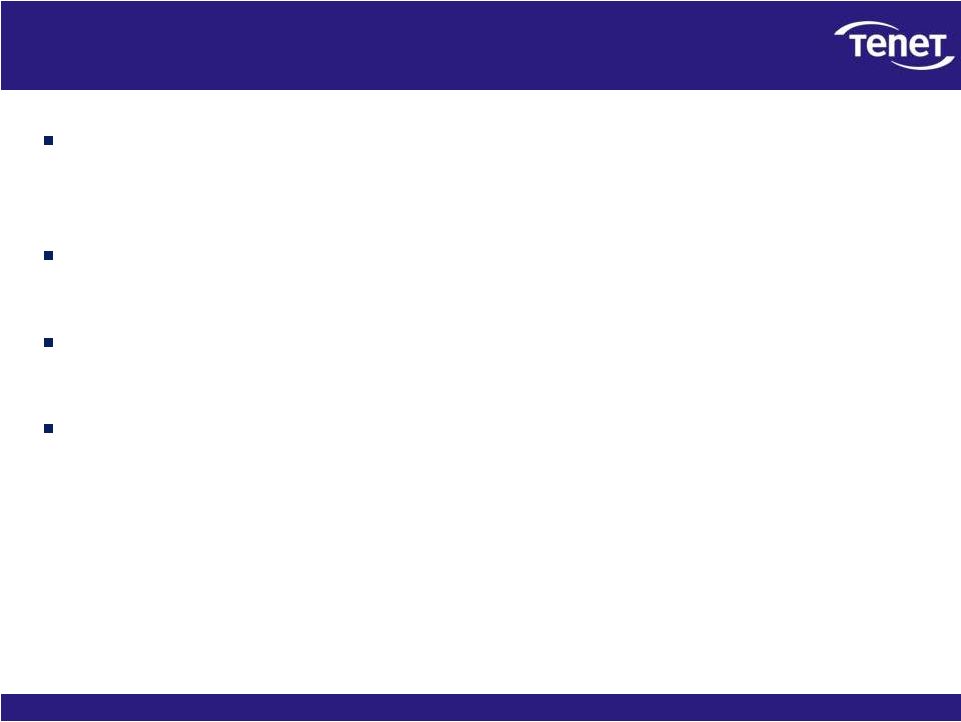
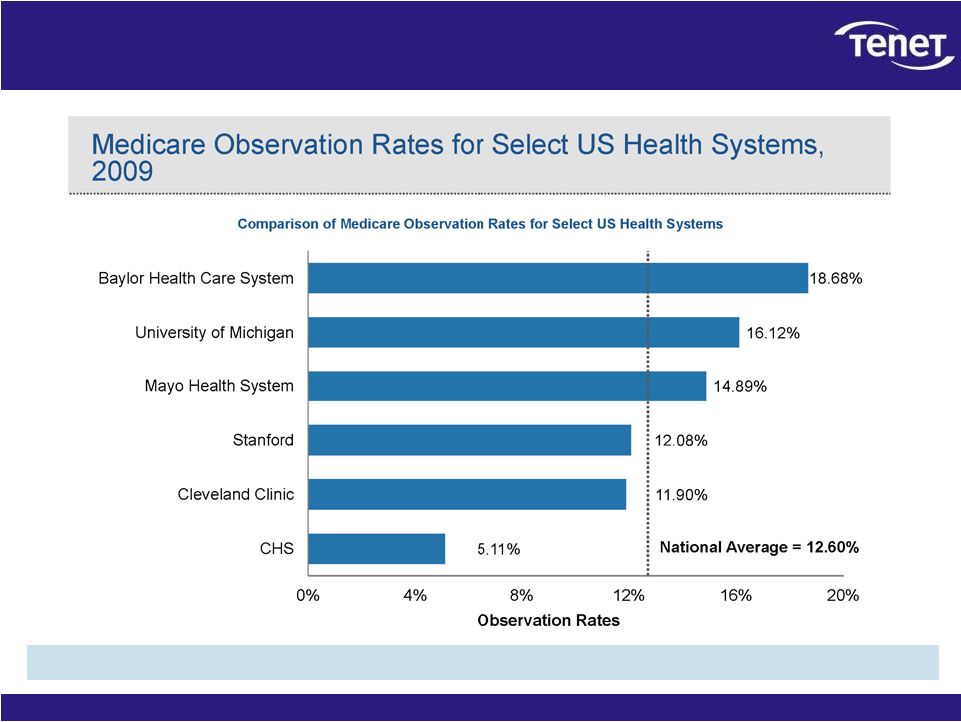
  11
CHS’
observation rate is much lower than other
large hospital groups and the industry as a whole
* Observation rate
is
defined
as
total
unique
observation
claims
divided
by
the
sum
of
total
unique
observation
claims
and
total
inpatient
short-stay
acute
care
hospital
claims.
** National average represents all short-stay acute care hospitals with
emergency departments and observation stays, with the exception of critical access hospital (CAHs); for a total of 3,004 hospitals in 2009.
*** Our analysis
limited
the
130
CHS
hospitals
to
111
hospitals
in
2009,
which
excluded
3
non-inpatient
short-stay
acute
care
hospitals,
4
hospitals
acquired
in
2010,
6
CAHs,
and
6
hospitals
that
did
not
bill
for
ER
visits and/or observation stays.
Source:
Analysis
based
on
the
Centers
for
Medicare
&
Medicaid
Services’
Outpatient
Standard
Analytic
Files
(SAFs)
for
CYs
2006-2009
and
the
Inpatient
Prospective
Payment
System
SAFs
for
CYs
2006-2009;
the
inpatient
SAFs
represent
similar
data
found
in
MedPAR
but
more
granular
since
the
SAFs’
unit
of
analysis
is
the
claim
and
MedPAR
data
is
aggregated
to
the
beneficiary
stay.
Other publicly traded hospital groups have
observation rates near or above the industry average. |
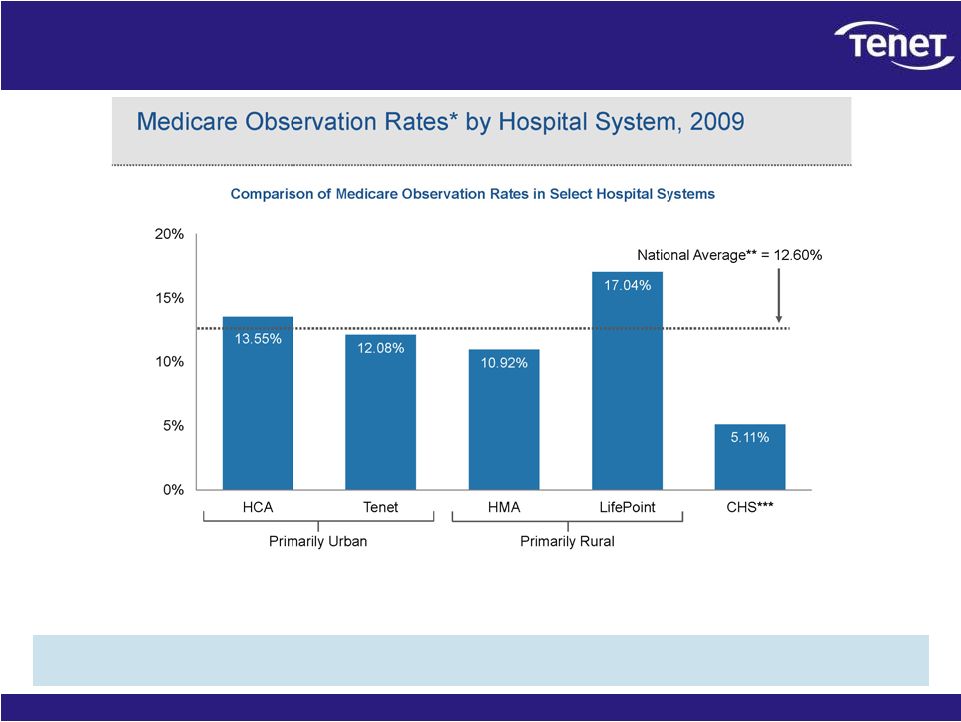
  12
CHS’
hospitals, classified by facility type,
have observation rates well below national averages
CHS’
observation rates by Medicare facility type are well below
the rates for similar facilities across the U.S.
* Non-CHS Average is comprised of all inpatient short-stay acute care
hospitals excluding all CHS hospitals. |
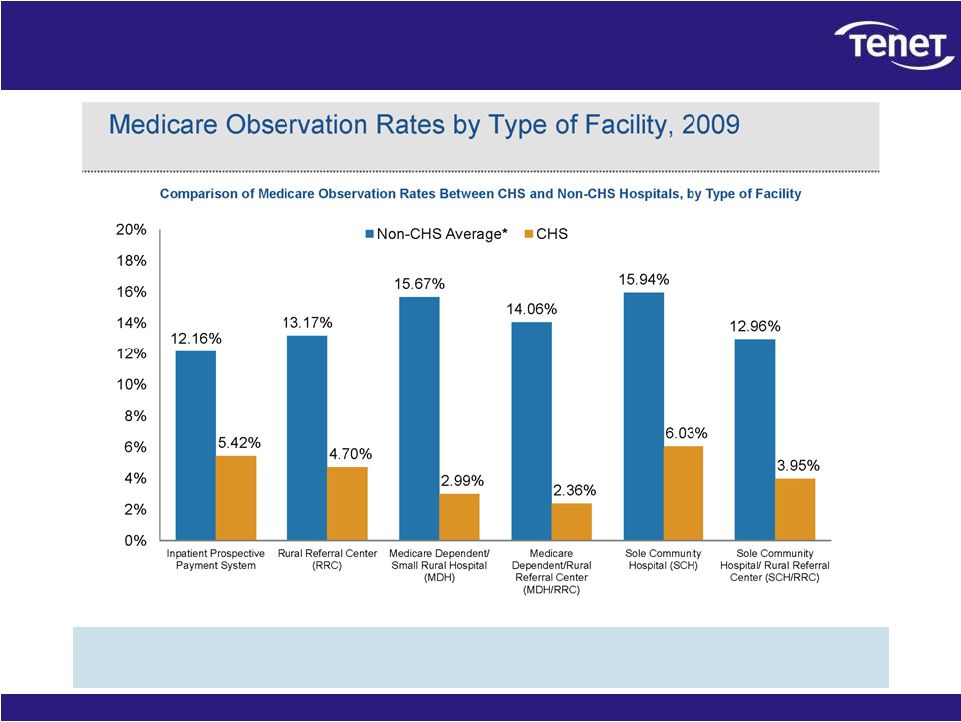
  13
CHS’
hospitals have less than half the observation
rate of hospitals in the same markets
Observation rates for hospitals within the 3-digit zip codes of CHS hospitals
are more than two times that of CHS hospitals.
The location of CHS hospitals does not explain their low observation rate.
|
  14
Prominent hospital groups do not have low
observation rates
Nationally recognized hospital groups have observation rates well in excess of
CHS’. |
  15
The lower acuity mix of CHS’
hospitals does not
explain CHS’
low observation rate
Hospitals with lower acuity –
like CHS –
tend to have higher, not
lower, observation rates.
A hospital’s Medicare “Case Mix Index”
measures the acuity level of its patients.
Hospitals with a higher Case Mix Index see more acutely ill patients that
require more complex or extensive treatments.
Hospitals with a lower Case Mix Index see less acutely ill patients that
require less complex or extensive treatments.
The average CHS hospital has a lower Case Mix Index (1.28) than the average
hospital nationally (1.43).
This makes sense –
CHS’
predominantly rural hospitals tend to see less
acute patients who require less complex or extensive treatments.
Statistical analysis shows that hospitals with a lower Case Mix Index have
higher, not lower, observation rates. |
  16
There is no reasonable explanation for CHS’
high
admission rate and low observation rate
It’s
not
the
facility
type:
CHS’
observation
rate
is
well
below
industry
peers with similar facility types including other rural hospitals.
It’s
not
the
location:
CHS’
hospitals
have
less
than
half
the
observation
rate of other hospitals in the same markets.
It’s
not
the
quality
of
care:
CHS’
observation
rate
is
lower
than
hospital
groups known for high quality.
It’s
not
the
acuity
mix:
CHS’
lower
acuity
hospitals
should
result
in
a
higher
observation
rate
–
not
lower. |
  17
CHS uses the Blue Book to drive admissions higher
and observations lower
Approximately three-quarters of U.S. hospitals, as well as many Medicare
auditors, utilize one of two sets of independent, evidence-based
clinical criteria to determine whether a patient qualifies for inpatient
admission. •
Approximately
3,700
U.S.
hospitals
use
the
InterQual
Criteria,
developed
by
McKesson
Corporation.
•
Approximately
1,000
U.S.
hospitals
use
the
Milliman
Care
Guidelines,
developed
by
Milliman,
Inc.
•
InterQual and Milliman were developed by independent physicians and contain
thousands of medical references.
CHS uses a 40-page “Blue Book.”
•
The
CHS
Blue
Book
was
developed
by
CHS,
copyrighted
in
2000,
and
lacks
a
single
reference
to
a medical journal or other independent source.
•
The
Blue
Book
is
utilized
only
by
CHS’
hospitals.
Unlike the InterQual and Milliman criteria, the Blue Book criteria are called
“Admission Justifications.”
In
numerous
cases,
including
those
under
scrutiny
by
regulators,
the
Blue
Book
justifies
admission when standard clinical practice and InterQual and Milliman do not.
CHS’
Blue Book is inconsistent with industry standard practice, but
drives higher revenues and profits. |
  18
The Triad case study
CHS
has
repeatedly
cited
the
“synergies”
it
achieved
in
the
acquisition
of
Triad
Hospitals,
Inc.
in
2007.
Never has it disclosed that these synergies were based
on driving medically unnecessary admissions and reducing
observations. Prior to its acquisition by CHS, Triad’s hospitals had an
observation rate above the national average. Following CHS’
acquisition, the observation rate of the acquired Triad hospitals dropped by 52%
while observation rates nationally were increasing.
A
potentially
material
portion
of
the
“synergies”
achieved
at
Triad
resulted from driving down observation rates. |
  19
Tenet’s lawsuit seeks to compel CHS to disclose its admissions
practices. CHS has increased its revenues and its profits by inappropriately
billing Medicare, and likely
state
Medicaid
programs
and
other
payers,
for
higher-paying
inpatient
admissions
rather than lower-paying outpatient observation stays.
No other publicly traded hospital company follows a similar practice.
CHS’
strategy is unsustainable; unwinding the practice will materially reduce
admissions revenues, profits, and cash flows; and it has exposed the company
to significant potential liabilities.
Improper billings for Medicare fee-for-service patients are estimated at
$280 million to $377 million between 2006-2009 alone.
Revenue
from
Medicare
fee-for-service
patients
represents
only
27%
of
CHS’
net
operating
revenues.
Revenues from other payers are also likely impacted.
Liabilities for this conduct related to Medicare fee-for-service patients
alone could be well in excess of $1 billion.
The
implications
for
CHS’
proposal
to
acquire
Tenet:
CHS’
stock is worth less than stated.
CHS’
ability to finance the cash portion may be
impaired. Summary |
