Attached files
| file | filename |
|---|---|
| EX-23.2 - EX-23.2 - GoHealth, Inc. | d797183dex232.htm |
| EX-23.1 - EX-23.1 - GoHealth, Inc. | d797183dex231.htm |
| EX-10.9 - EX-10.9 - GoHealth, Inc. | d797183dex109.htm |
| EX-10.5 - EX-10.5 - GoHealth, Inc. | d797183dex105.htm |
| EX-4.1 - EX-4.1 - GoHealth, Inc. | d797183dex41.htm |
| EX-3.3 - EX-3.3 - GoHealth, Inc. | d797183dex33.htm |
| EX-3.1 - EX-3.1 - GoHealth, Inc. | d797183dex31.htm |
Table of Contents
As filed with the Securities and Exchange Commission on June 19, 2020
Registration No. 333-
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
FORM S-1
REGISTRATION STATEMENT
UNDER
THE SECURITIES ACT OF 1933
GoHealth, Inc.
(Exact name of registrant as specified in its charter)
| Delaware | 6411 | 85-0563805 | ||
| (State or other jurisdiction of incorporation or organization) |
(Primary Standard Industrial Classification Code Number) |
(I.R.S. Employer Identification No.) |
214 West Huron St.
Chicago, Illinois 60654
Telephone: (312) 386-8200
(Address, including zip code, and telephone number, including area code, of registrant’s principal executive offices)
Bradley Burd
General Counsel
214 West Huron St.
Chicago, Illinois 60654
Telephone: (312) 386-8200
(Name, address, including zip code, and telephone number, including area code, of agent for service)
Copies to:
| Ian D. Schuman, Esq. Stelios G. Saffos, Esq. Ryan K. deFord, Esq. Latham & Watkins LLP 885 Third Avenue New York, New York 10022 Telephone: (212) 906-1200 Fax: (212) 751-4864 |
Bradley Burd General Counsel GoHealth, Inc. 214 West Huron St. Chicago, Illinois 60654 Telephone: (312) 386-8200 |
Samir A. Gandhi, Esq. David Ni, Esq. Sidley Austin LLP 787 7th Avenue New York, New York 10019 Telephone: (212) 839-5300 Fax: (212) 839-5599 |
APPROXIMATE DATE OF COMMENCEMENT OF PROPOSED SALE TO THE PUBLIC: AS SOON AS PRACTICABLE AFTER THIS REGISTRATION STATEMENT IS DECLARED EFFECTIVE.
If any of the securities being registered on this Form are to be offered on a delayed or continuous basis pursuant to Rule 415 under the Securities Act of 1933 check the following box. ☐
If this Form is filed to register additional securities for an offering pursuant to Rule 462(b) under the Securities Act, check the following box and list the Securities Act registration statement number of the earlier effective registration statement for the same offering. ☐
If this Form is a post-effective amendment filed pursuant to Rule 462(c) under the Securities Act, check the following box and list the Securities Act registration statement number of the earlier effective registration statement for the same offering. ☐
If this Form is a post-effective amendment filed pursuant to Rule 462(d) under the Securities Act, check the following box and list the Securities Act registration statement number of the earlier effective registration statement for the same offering. ☐
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, a smaller reporting company, or an emerging growth company. See the definitions of “large accelerated filer,” “accelerated filer,” “smaller reporting company,” and “emerging growth company” in Rule 12b-2 of the Exchange Act.
| Large accelerated filer | ☐ | Accelerated filer | ☐ | |||
| Non-accelerated filer | ☒ | Smaller reporting company | ☐ | |||
| Emerging growth company | ☒ | |||||
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 7(a)(2)(B) of the Securities Act. ☐
CALCULATION OF REGISTRATION FEE
|
| ||||
| Title of Each Class of Securities to be Registered |
Proposed Maximum Aggregate Offering Price(1)(2) |
Amount of Registration Fee | ||
| Class A common stock, $0.0001 par value per share |
$100,000,000 | $12,980 | ||
|
| ||||
|
| ||||
| (1) | Estimated solely for the purpose of calculating the registration fee pursuant to Rule 457(o) under the Securities Act of 1933, as amended. |
| (2) | Includes the offering price of shares of Class A common stock that may be sold if the option to purchase additional shares of Class A common stock granted by the Registrant to the underwriters is executed. |
The Registrant hereby amends this Registration Statement on such date or dates as may be necessary to delay its effective date until the Registrant shall file a further amendment which specifically states that this Registration Statement shall thereafter become effective in accordance with Section 8(a) of the Securities Act of 1933, as amended or until the Registration Statement shall become effective on such date as the Securities and Exchange Commission, acting pursuant to said Section 8(a), may determine.
Table of Contents
The information in this preliminary prospectus is not complete and may be changed. These securities may not be sold until the registration statement filed with the Securities and Exchange Commission is effective. This preliminary prospectus is not an offer to sell nor does it seek an offer to buy these securities in any jurisdiction where the offer or sale is not permitted.
Subject to completion, dated June 19, 2020.
Shares

GoHealth, Inc.
Class A Common Stock
This is an initial public offering of shares of Class A common stock of GoHealth, Inc. We are selling shares of Class A common stock.
Prior to this offering, there has been no public market for the Class A common stock. It is currently estimated that the initial public offering price per share of Class A common stock will be between $ and $ . We have applied to list our Class A common stock on The Nasdaq Global Market under the symbol “GHTH.”
We will have two classes of common stock outstanding after this offering: Class A common stock and Class B common stock. Each share of our Class A common stock entitles its holder to one vote per share and each share of our Class B common stock entitles its holder to one vote per share on all matters presented to our stockholders generally. Immediately following the consummation of this offering, all of the outstanding shares of our Class B common stock will be held by the Continuing Equity Owners (as defined below), which will represent in the aggregate approximately % of the voting power of our outstanding common stock after this offering (or approximately % if the underwriters exercise in full their option to purchase additional shares).
We will be a holding company, and upon consummation of this offering and the application of proceeds therefrom, our principal asset will consist of LLC Interests (as defined below) we acquire directly from GoHealth Holdings, LLC and indirectly from certain of the Continuing Equity Owners and the Blocker Shareholders with the proceeds from this offering, collectively representing an aggregate % economic interest in GoHealth Holdings, LLC. Of the remaining % economic interest in GoHealth Holdings, LLC, % will be owned by the Continuing Equity Owners (excluding Centerbridge Capital Partners III, L.P.) through their ownership of LLC Interests and % will be owned by Centerbridge Capital Partners III, L.P., our majority owner through their ownership of LLC Interests.
GoHealth, Inc. will be the sole managing member of GoHealth Holdings, LLC. We will operate and control all of the business and affairs of GoHealth Holdings, LLC and its direct and indirect subsidiaries and, through GoHealth Holdings, LLC and its direct and indirect subsidiaries, conduct our business.
Following this offering, we will be a “controlled company” within the meaning of the Nasdaq rules. See “Our Organizational Structure” and “Management—Controlled Company Exception.”
We are an “emerging growth company,” as defined in Section 2(a) of the Securities Act of 1933, as amended, or the Securities Act, and will be subject to reduced disclosure and public reporting requirements. This prospectus complies with the requirements that apply to an issuer that is an emerging growth company.
See “Risk Factors” beginning on page 31 to read about factors you should consider before buying shares of our Class A common stock.
Neither the Securities and Exchange Commission nor any other regulatory body has approved or disapproved of these securities or passed upon the accuracy or adequacy of this prospectus. Any representation to the contrary is a criminal offense.
| Per Share |
Total | |||||||
| Initial public offering price |
$ | $ | ||||||
| Underwriting discount(1) |
$ | $ | ||||||
| Proceeds, before expenses, to GoHealth, Inc. |
$ | $ | ||||||
| (1) | We have agreed to reimburse the underwriters for certain expenses in connection with this offering. See “Underwriting.” |
The underwriters have the option to purchase up to an additional shares of Class A common stock from us at the initial price to public less the underwriting discount within 30 days of the date of this prospectus.
The underwriters expect to deliver the shares of Class A common stock against payment in New York, New York on , 2020.
| Goldman Sachs & Co. LLC | BofA Securities | Morgan Stanley |
| Barclays | Credit Suisse | Evercore ISI | RBC Capital Markets | William Blair |
| Cantor | SunTrust Robinson Humphrey |
Prospectus dated , 2020.
Table of Contents

Table of Contents
Table of Contents
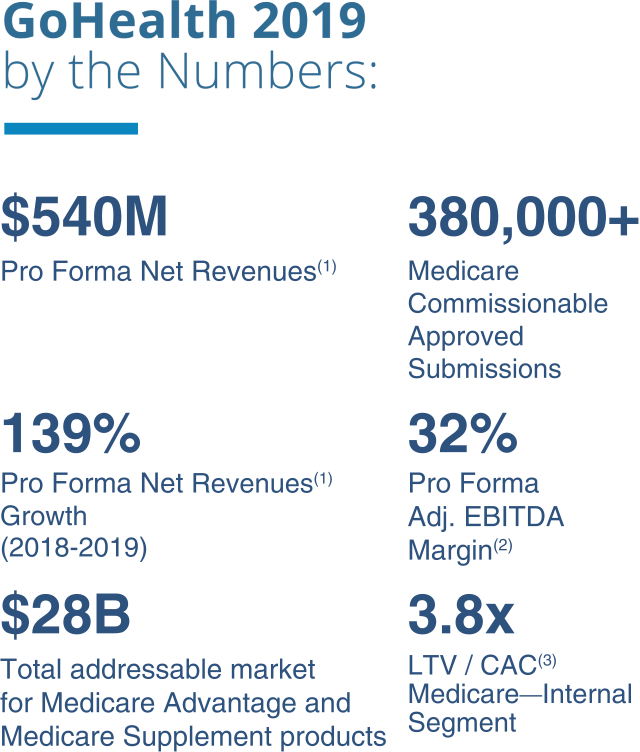
| (1) | See footnote 1 to “Prospectus Summary—Summary Historical and Pro Forma Condensed Consolidated Financial and Other Data” for information regarding our use of pro forma financial information. |
| (2) | See “Prospectus Summary—Summary Historical and Pro Forma Condensed Consolidated Financial and Other Data” for information regarding our use of Adjusted EBITDA, a non-GAAP financial measure, and a reconciliation of Adjusted EBITDA to net income, the most directly comparable financial measure calculated and presented in accordance with GAAP. |
| (3) | See “Basis of Presentation—Key Terms and Performance Indicators Used in this Prospectus; Non-GAAP Financial Measures” for a definition of LTV/CAC. |
Table of Contents
| 1 | ||||
| 31 | ||||
| 77 | ||||
| 78 | ||||
| 82 | ||||
| 83 | ||||
| 85 | ||||
| 86 | ||||
| 88 | ||||
| UNAUDITED PRO FORMA CONDENSED CONSOLIDATED FINANCIAL INFORMATION |
90 | |||
| MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS |
101 | |||
| 133 | ||||
| 152 | ||||
| 159 | ||||
| 172 | ||||
| 184 | ||||
| 186 | ||||
| 192 | ||||
| 195 | ||||
| MATERIAL U.S. FEDERAL INCOME TAX CONSIDERATIONS TO NON-U.S. HOLDERS OF CLASS A COMMON STOCK |
198 | |||
| 202 | ||||
| 209 | ||||
| 209 | ||||
| 209 | ||||
| F-1 |
You should rely only on the information contained in this prospectus and any free writing prospectus prepared by or on behalf of us or to which we have referred you. No dealer, salesperson or other person is authorized to give any information or to represent anything not contained in this prospectus or in any free writing prospectus that we file with the Securities and Exchange Commission. We and the underwriters have not authorized anyone to provide any information or to make any representations other than those contained in this prospectus or in any related free writing prospectuses. We and the underwriters take no responsibility for, and can provide no assurance as to the reliability of, any other information that others may give you. You must not rely on any unauthorized information or representations. This prospectus is an offer to sell only the shares offered by this prospectus, but only under circumstances and in jurisdictions where it is lawful to do so. The information contained in this prospectus is current only as of its date regardless of the time of delivery of this prospectus or of any sale of our Class A common stock. Our business, financial condition, results of operations and prospects may have changed since that date.
Through and including , 2020 (the 25th day after the date of this prospectus), all dealers effecting transactions in these securities, whether or not participating in this offering, may be required to deliver a prospectus. This is in addition to a dealer’s obligation to deliver a prospectus when acting as an underwriter and with respect to an unsold allotment or subscription.
For investors outside the United States: We have not, and the underwriters have not, done anything that would permit this offering or the possession or distribution of this prospectus or any free writing prospectus we may provide to you in connection with this offering in any jurisdiction where action for purpose is required, other than in the United States. Persons outside the United States who come into possession of this prospectus must inform themselves about, and observe any restrictions relating to, the offering of the shares of Class A common stock and the distribution of this prospectus outside the United States. See “Underwriting.”
i
Table of Contents
BASIS OF PRESENTATION
Organizational Structure
In connection with the closing of this offering, we will undertake certain organizational transactions to reorganize our corporate structure. Unless otherwise stated or the context otherwise requires, all information in this prospectus reflects the consummation of the organizational transactions described in the section titled “Our Organizational Structure” and this offering, and the application of the proceeds therefrom, which we refer to collectively as the “Transactions.”
See “Our Organizational Structure” for a diagram depicting our organizational structure after giving effect to the Transactions, including this offering.
Certain Definitions
As used in this prospectus, unless the context otherwise requires:
| • | “we,” “us,” “our,” the “Company,” “GoHealth” and similar references refer: (1) following the consummation of the Transactions, including this offering, to GoHealth, Inc., and, unless otherwise stated, all of its direct and indirect subsidiaries, including GoHealth Holdings, LLC (formerly known as Blizzard Parent, LLC), and (2) prior to the completion of the Transactions, including this offering, to GoHealth Holdings, LLC and, unless otherwise stated, all of its direct and indirect subsidiaries, or, as applicable, the Predecessor. |
| • | “Blocker Company” refers to an entity affiliated with Centerbridge that is an indirect owner of LLC Interests in GoHealth Holdings, LLC prior to the Transactions and is taxable as a corporation for U.S. federal income tax purposes. |
| • | “Blocker Shareholders” refer to entities affiliated with Centerbridge, the owners of the Blocker Company prior to the Transactions, who will exchange their interests in the Blocker Company for shares of our Class A common stock and cash in connection with the consummation of the Transactions. |
| • | “Centerbridge” refers to Centerbridge Capital Partners III, L.P., our majority owner and a Delaware limited partnership, certain funds affiliated with Centerbridge Capital Partners III, L.P. and other entities over which Centerbridge Capital Partners III, L.P. has voting control (including any such fund or entity formed to hold shares of Class A common stock for the Blocker Shareholders). |
| • | “Continuing Equity Owners” refer collectively to holders of LLC Interests and our Class B common stock immediately following consummation of the Transactions, including Centerbridge, Norwest, our Founders and certain executive officers, employees and other minority investors and their respective permitted transferees who may, following the consummation of this offering, exchange at each of their respective options, in whole or in part from time to time, their LLC Interests (along with an equal number of shares of Class B common stock (and such shares shall be immediately cancelled)) for, at our election (determined solely by our independent directors (within the meaning of the Nasdaq rules) who are disinterested), cash or newly-issued shares of our Class A common stock as described in “Certain Relationships and Related Party Transactions—GoHealth Holdings, LLC Agreement—Agreement in Effect Upon Consummation of the Transactions.” |
| • | “Founders” refer to Brandon M. Cruz, our Co-Founder and Chief Strategy Officer and Special Advisor to the Executive Team, and Clinton P. Jones, our Co-Founder and Chief Executive Officer. |
| • | “GoHealth Holdings, LLC Agreement” refers to GoHealth Holdings, LLC’s amended and restated limited liability company agreement, which will become effective substantially concurrently with or prior to the consummation of this offering. |
| • | “LLC Interests” refer to the common units of GoHealth Holdings, LLC, including those that we purchase with a portion of the net proceeds from this offering. |
ii
Table of Contents
| • | “Norwest” refers to Norwest Equity Partners and certain funds affiliated with Norwest Equity Partners. |
| • | “Norvax” or “Predecessor” refers to Norvax, LLC, a Delaware limited liability company and a subsidiary of GoHealth Holdings, LLC. |
| • | “Original Equity Owners” refer to the owners of LLC Interests in GoHealth Holdings, LLC prior to the consummation of the Transactions, collectively, which include Centerbridge, Norwest, our Founders and certain executive officers, employees and other minority investors. |
| • | “Transactions” refer to the organizational transactions and this offering, and the application of the net proceeds therefrom. |
GoHealth, Inc. will be a holding company and the sole managing member of GoHealth Holdings, LLC, and upon consummation of the Transactions, its principal asset will consist of LLC Interests.
Presentation of Financial Information
GoHealth Holdings, LLC is the accounting predecessor of GoHealth, Inc. for financial reporting purposes. GoHealth, Inc. will be the audited financial reporting entity following this offering. Accordingly, this prospectus contains the following historical financial statements:
| • | GoHealth, Inc. Other than the inception balance sheet, dated as of March 27, 2020, the historical financial information of GoHealth, Inc. has not been included in this prospectus as it is a newly incorporated entity, has no business transactions or activities to date and had no assets or liabilities during the periods presented in this prospectus. |
| • | GoHealth Holdings, LLC. Because GoHealth, Inc. will have no interest in any operations other than those of GoHealth Holdings, LLC and its subsidiaries, the historical consolidated financial information included in this prospectus is that of GoHealth Holdings, LLC and its subsidiaries. |
On September 13, 2019, Centerbridge, indirectly through a subsidiary of GoHealth Holdings, LLC (formerly known as Blizzard Parent, LLC), an entity formed in contemplation of the acquisition, acquired a 100% interest in Norvax. We refer to this transaction as the “Centerbridge Acquisition.” As a result of the Centerbridge Acquisition, this prospectus presents certain financial information for two periods, the Predecessor and Successor periods, which relate to the period preceding the Centerbridge Acquisition on September 13, 2019 and the period succeeding the Centerbridge Acquisition, respectively. References to the “Successor 2019 Period” refer to the period from September 13, 2019 through December 31, 2019, and references to the “Predecessor 2019 Period” refer to the period from January 1, 2019 through September 12, 2019. Financial information in the Predecessor 2019 Period principally relates to Norvax and its subsidiaries.
Except as noted in this prospectus, the unaudited pro forma financial information of GoHealth, Inc. presented in this prospectus has been derived from the application of pro forma adjustments to the historical consolidated financial statements of GoHealth Holdings, LLC and its subsidiaries included elsewhere in this prospectus. These pro forma adjustments give effect to the Centerbridge Acquisition and the Transactions as described in “Our Organizational Structure,” including the consummation of this offering, as if all such transactions had occurred on January 1, 2019 in the case of the unaudited pro forma condensed consolidated statements of operations data, and as of March 31, 2020 in the case of the unaudited pro forma condensed consolidated balance sheet data. See “Unaudited Pro Forma Condensed Consolidated Financial Information” for a complete description of the adjustments and assumptions underlying the pro forma financial information included in this prospectus. References to the “Pro Forma Fiscal Year 2019” refer to the pro forma financial information presented in the “Unaudited Pro Forma Condensed Consolidated Financial Information” for the year ended December 31, 2019.
Certain monetary amounts, percentages and other figures included in this prospectus have been subject to rounding adjustments. Percentage amounts included in this prospectus have not in all cases been calculated on
iii
Table of Contents
the basis of such rounded figures, but on the basis of such amounts prior to rounding. For this reason, percentage amounts in this prospectus may vary from those obtained by performing the same calculations using the figures in our consolidated financial statements included elsewhere in this prospectus. Certain other amounts that appear in this prospectus may not sum due to rounding.
Key Terms and Performance Indicators Used in this Prospectus; Non-GAAP Financial Measures
Throughout this prospectus, we use a number of key terms and provide a number of key performance indicators used by management. These key performance indicators are discussed in more detail in the section entitled “Management’s Discussion and Analysis of Financial Condition and Results of Operations—Key Business and Operating Metrics by Segment.” We define these terms and key performance indicators as follows:
| • | “Approved Submissions” refer to Submitted Policies approved by carriers for the identified product during the indicated period. |
| • | “Adjusted EBITDA” represents EBITDA as further adjusted for share-based compensation, change in fair value of earnout liability, Centerbridge Acquisition costs and severance costs. |
| • | “Adjusted EBITDA margin” refers to Adjusted EBITDA divided by net revenues. |
| • | “Consumer interactions” refer to the number of times a consumer calls us or visits us online. |
| • | “Consumer lead” refers to a consumer for which we have collected some personally identifiable information related to health insurance. |
| • | “EBITDA” represents net income (loss) before interest expense, income tax expense (benefit) and depreciation and amortization expense. |
| • | “Impressions” refer to the number of times our advertisement is shown to consumers through any medium, regardless of whether such consumers have viewed, clicked through or otherwise interacted with the advertisement. |
| • | “LTV Per Approved Submission” refers to the Lifetime Value of Commissions per Approved Submission, which we define as (i) aggregate commissions estimated to be collected over the estimated life of all commissionable Approved Submissions for the relevant period based on multiple factors, including but not limited to, contracted commission rates, carrier mix and expected policy persistency with applied constraints, divided by (ii) the number of commissionable Approved Submissions for such period. |
| • | “LTV/CAC” refers to the Lifetime Value of Commissions per Consumer Acquisition Cost, which we define as (i) aggregate commissions estimated to be collected over the estimated life of all commissionable Approved Submissions for the relevant period based on multiple factors, including but not limited to, contracted commission rates, carrier mix and expected policy persistency with applied constraints, or LTV, divided by (ii) the cost to convert a prospect into a customer less other non-commission carrier revenue for such period, or CAC. CAC is comprised of cost of revenue, marketing and advertising expenses and customer care and enrollment expenses less other revenue and is presented on a per commissionable Approved Submission basis. |
| • | “Qualified prospect” refers to a consumer that has confirmed an interest to us in shopping for health insurance over the phone, online or via live transfer to our agents, both through the internal and external channels. |
| • | “Submitted Policies” refer to completed applications that, with respect to each such application, the consumer has authorized us to submit to the carrier. |
We use non-GAAP financial measures, such as EBITDA, Adjusted EBITDA and Adjusted EBITDA margin, to supplement financial information presented in accordance with generally accepted accounting principles in the United States, or GAAP. We believe that excluding certain items from our GAAP results allows management to better understand our consolidated financial performance from period to period and better project our future
iv
Table of Contents
consolidated financial performance as forecasts are developed at a level of detail different from that used to prepare GAAP-based financial measures. Moreover, we believe these non-GAAP financial measures provide our stakeholders with useful information to help them evaluate our operating results by facilitating an enhanced understanding of our operating performance and enabling them to make more meaningful period to period comparisons. There are limitations to the use of the non-GAAP financial measures presented in this prospectus. For example, our non-GAAP financial measures may not be comparable to similarly titled measures of other companies. Other companies, including companies in our industry, may calculate non-GAAP financial measures differently than we do, limiting the usefulness of those measures for comparative purposes. See “Prospectus Summary—Summary Historical and Pro Forma Condensed Consolidated Financial and Other Data” and “Management’s Discussion and Analysis of Financial Condition and Results of Operations.”
TRADEMARKS
This prospectus includes our trademarks and trade names which are protected under applicable intellectual property laws and are our property. This prospectus also contains trademarks, trade names and service marks of other companies, which are the property of their respective owners. Solely for convenience, trademarks, trade names and service marks referred to in this prospectus may appear without the ®, ™ or SM symbols, but such references are not intended to indicate, in any way, that we will not assert, to the fullest extent permitted under applicable law, our rights or the right of the applicable licensor to these trademarks, trade names and service marks. We do not intend our use or display of other parties’ trademarks, trade names or service marks to imply, and such use or display should not be construed to imply, a relationship with, or endorsement or sponsorship of us by, these other parties.
MARKET AND INDUSTRY DATA
Unless otherwise indicated, information contained in this prospectus concerning our industry, competitive position and the markets in which we operate is based on information from independent industry and research organizations, other third-party sources and management estimates. Management estimates are derived from publicly available information released by independent industry analysts and other third-party sources, as well as data from our internal research, and are based on assumptions made by us upon reviewing such data, and our experience in, and knowledge of, such industry and markets, which we believe to be reasonable. In addition, projections, assumptions and estimates of the future performance of the industry in which we operate and our future performance are necessarily subject to uncertainty and risk due to a variety of factors, including those described in “Risk Factors” and “Cautionary Note Regarding Forward-Looking Statements.” These and other factors could cause results to differ materially from those expressed in the estimates made by the independent parties and by us.
v
Table of Contents
This summary highlights selected information included elsewhere in this prospectus. This summary does not contain all of the information that you should consider before deciding to invest in our Class A common stock. You should read the entire prospectus carefully, including the “Risk Factors,” “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and our consolidated financial statements and the related notes included elsewhere in this prospectus, before making an investment decision. Some of the statements in this prospectus constitute forward-looking statements. See “Cautionary Note Regarding Forward-Looking Statements.”
Overview
We are a leading health insurance marketplace whose mission is to improve access to healthcare in America. Our proprietary technology platform leverages modern machine-learning algorithms powered by nearly two decades of insurance behavioral data to reimagine the optimal process for helping individuals find the best health insurance plan for their specific needs. Our differentiated combination of a vertically-integrated consumer acquisition platform and highly skilled and trained licensed agents has enabled us to enroll millions of people in Medicare and individual and family plans since our inception. With over 10,000 Americans turning 65 years old every day and GoHealth’s track record of significant growth in net revenues in the Medicare space in the past five years, we believe we will continue to be one of the top choices for unbiased insurance advice to help navigate one of the most important purchasing decisions individuals make.
Since our inception, we have consistently invested in our technology, data science and business processes to enroll millions of people in health insurance plans while helping carriers scale their product and plan offerings. Our platform utilizes proprietary technology, machine-learning capabilities, data, efficient business processes, and highly skilled and trained licensed agents, or agents, to connect consumers with health insurance carriers, or carriers, through multiple channels. Through our platform, we offer a wide array of health insurance policies, including, but not limited to, Medicare Advantage, Medicare Supplement, prescription drug plans, and individual and family plans, and allow consumers to choose how to purchase these plans, either with the assistance of our agents or directly online.
For many consumers, choosing a health insurance plan is confusing and difficult, and seemingly small differences between health insurance plans can lead to significant out-of-pocket costs or lack of access to critical medicines or providers. We simplify the difficult and confusing process by offering a large selection of health insurance plan choices, unbiased advice informed by consumers’ specific needs, transparency of health insurance plan benefits and fit, assistance accessing available government subsidies and a high-touch TeleCare team. The TeleCare team is focused on increasing consumer engagement with the GoHealth brand, selling new products and services to our consumers that help meet their healthcare needs, and helping consumers maximize their health insurance plan benefits to support long-term health and wellness. Carriers also benefit from our platform, especially those looking to access the large and fast-growing Medicare-eligible population. We believe carriers utilize our large-scale data and technology as well as our efficient marketing and conversion processes to reduce their CAC, compared to carrier-employed agent workforces. In fact, we believe GoHealth is the largest external partner for Medicare Advantage enrollments for many carriers.
We have a 19-year history of consistent revenue growth and entering new market segments of insurance products. We add significant value to consumers and carriers, which is evidenced by our high growth rate and strong customer engagement dynamics. Specifically, net revenues grew by 104.1% to $141.0 million for the three months ended March 31, 2020 compared to $69.1 million for the three months ended March 31, 2019 and by 138.5% to $539.5 million for the Pro Forma Fiscal Year 2019 compared to $226.2 million for the year ended December 31, 2018. Adjusted EBITDA grew by 391.5% to $34.9 million for the three months ended
1
Table of Contents
March 31, 2020 compared to $7.1 million for the three months ended March 31, 2019 and by 386.8% to $170.0 million for the Pro Forma Fiscal Year 2019 from $34.9 million for the year ended December 31, 2018. Net loss was $937 thousand for the three months ended March 31, 2020 compared to net income of $5.0 million for the three months ended March 31, 2019, and net loss was $29.5 million for the Pro Forma Fiscal Year 2019 compared to net income of $28.1 million for the year ended December 31, 2018. See “—Summary Historical and Pro Forma Condensed Consolidated Financial and Other Data” for information regarding our use of (i) pro forma financial information, specifically footnote 1 and (ii) Adjusted EBITDA, a non-GAAP financial measure, and a reconciliation of Adjusted EBITDA to net income, the most directly comparable financial measure calculated and presented in accordance with GAAP.
Over the last four years, we have increasingly shifted our focus towards Medicare products and deemphasized individual and family health insurance products. This shift in focus has enabled us to capitalize on (1) strong demographic trends, with Medicare enrollment expected to grow from approximately 61 million individuals in 2019 to approximately 77 million individuals by 2028, (2) the increasing proportion of the Medicare-eligible population that is choosing commercial insurance solutions, with 38% of Medicare beneficiaries, or approximately 23 million people, enrolled in Medicare Advantage plans in 2019, an increase of approximately 1.5 million people from 2018 to 2019, and (3) an antiquated traditional field agent driven sales process lacking in transparency, choice and convenience and ripe for disruption by digitally-enabled and technology-driven marketplaces like our platform. Today, we estimate a total addressable market of $28 billion for Medicare Advantage and Medicare Supplement products, which is based on third-party estimates of total expected Medicare enrollees for 2020, publicly available industry data for Medicare agents’ first-year compensation and our recent historical policy revenue experience. We believe that these trends will drive a larger market in the coming years that, when taken together with our other product and plan offerings, will result in an even larger addressable market. We also believe that we are poised to benefit from market share gains in what has traditionally been a highly fragmented market.
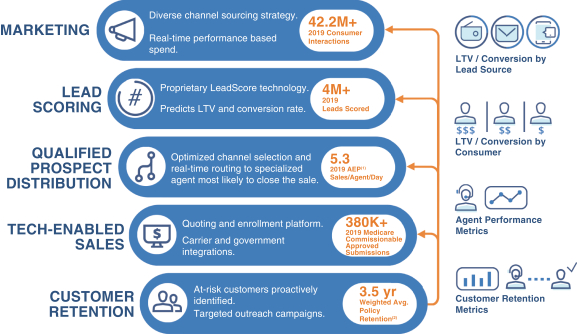
Consumers first engage through our platform either online or telephonically in response to our data-driven, omni-channel marketing efforts. We then use LeadScore, one of our proprietary machine-learning technologies, to evaluate consumer leads in real-time. In 2019, we generated over 42.2 million consumer interactions. The data we generate from each consumer interaction helps inform our marketing, consumer lead scoring, qualified prospect routing, and health insurance plan matching technology in a feedback loop. We also scored over 4 million consumer leads in 2019, which informs us of the potential profitability and conversion probability of the consumer lead and helps us optimize routing of consumer leads to agents. Our proprietary technology and business processes then route qualified prospects online or via live transfer to our agents, both through the internal and external channel. Our technology and workflow allow these agents to work in our Benefits Center, where our sales operations are located, or to work remotely at home. In 2019, we employed an average of 931 agents, reaching a high of 1,453 agents during the three months ended December 31, 2019. Based on consumers’ specific needs and our comprehensive data, our agents use our proprietary technology platform, Marketplace, to identify the optimal health insurance plan options from our vast inventory of insurance products. Marketplace then facilitates seamless quoting and enrollment of the consumer-selected health insurance plan using proprietary and third-party data and direct application program interfaces, or API, connections with carriers. As a result of our Marketplace technology and increasingly robust data and insights, our qualified prospect to Submitted Policy conversion rate increased from 20.7% for the three months ended March 31, 2019 to 24.3% for the three months ended March 31, 2020, and from 20.6% in 2018 to 23.2% in 2019 for the multi-carrier sales outlet of the Medicare—Internal segment. An increase in the conversion rate of qualified prospects to Submitted Policies generally results in greater commissionable Approved Submissions.
Using our proprietary data, we identify consumers who would benefit from proactive engagement and education on their health insurance plan design and guidance on how they can maximize their plan benefits. We believe that using our data-driven targeted consumer outreach and our highly skilled agents and proprietary technology to properly select health insurance plans to meet a consumer’s particular needs results in higher customer
2
Table of Contents
satisfaction. As we enroll more qualified prospects through our Marketplace, the power of our data improves our marketing, technology, and agent performance. Our platform is engineered for rapid scalability, with modern cloud infrastructure that has information security controls that are independently audited by several third-party firms, and technology driven compliance with HIPAA, TCPA and state insurance regulations, and the Centers for Medicare and Medicaid Services, or CMS, regulations.
Consumers do not pay any fees for access to our platform or for our enrollment, education or other services. Generally, we are paid an initial commission by carriers when consumers enroll in their products and become customers, and additional recurring commissions as long as those customers retain their health insurance plans. The commission structure encourages collaboration between us and carriers to increase customer satisfaction by choosing health insurance products that best fit customers’ needs, which drives better outcomes for carriers, customers, our agents, and employees. We use advanced statistical models that are built on observable commissions received rather than solely historic cohorts. Our advanced statistical models consider consumer demographic attributes, health insurance plan characteristics and temporal data to value these future commission streams from which we determine an expected LTV of the commission streams associated with each consumer enrolled in each specific plan product. Total commissions receivable, which represents such expected future commission streams, was $388.8 million as of March 31, 2020, an increase of 223.4% compared to March 31, 2019. In addition to commissions, some of our carriers have historically partnered with us to generate consumer leads and have paid us for marketing services. We do not insure customers and assume no underwriting or medical loss risk associated with placement of customers in our carriers’ products.
The differentiated value of our data science-driven, fully-integrated platform has facilitated our rapid growth. Net revenues grew by 104.1% to $141.0 million for the three months ended March 31, 2020 compared to $69.1 million for the three months ended March 31, 2019 and by 138.5% to $539.5 million for the Pro Forma Fiscal Year 2019 compared to $226.2 million for the year ended December 31, 2018. Adjusted EBITDA grew by 391.5% to $34.9 million for the three months ended March 31, 2020 compared to $7.1 million for the three months ended March 31, 2019 and by 386.8% to $170.0 million for the Pro Forma Fiscal Year 2019 from $34.9 million for the year ended December 31, 2018. Net loss was $937 thousand for the three months ended March 31, 2020 compared to net income of $5.0 million for the three months ended March 31, 2019 and net loss
3
Table of Contents
was $29.5 million for the Pro Forma Fiscal Year 2019 compared to net income of $28.1 million for the year ended December 31, 2018. Our focus on Medicare has also contributed significantly to our growth. Total revenues generated in the Medicare segments grew to $124.2 million for the three months ended March 31, 2020 from $41.2 million for the three months ended March 31, 2019, representing a 201.5% increase, and to $432.7 million for the Pro Forma Fiscal Year 2019 from $112.2 million for the year ended December 31, 2018, representing a 285.7% increase. In the Medicare segments, our total Submitted Policies grew to over 122,400 Medicare policies for the three months ended March 31, 2020, as compared to over 43,200 Medicare policies the three months ended March 31, 2019 and over 427,000 Medicare policies for the year ended December 31, 2019, as compared to over 118,000 Medicare policies for the year ended December 31, 2018. See “—Summary Historical and Pro Forma Condensed Consolidated Financial and Other Data” for information regarding our use of (i) pro forma financial information, specifically footnote 1 and (ii) Adjusted EBITDA, a non-GAAP financial measure, and a reconciliation of Adjusted EBITDA to net income, the most directly comparable financial measure calculated and presented in accordance with GAAP.
Our Business Model
Our Platform
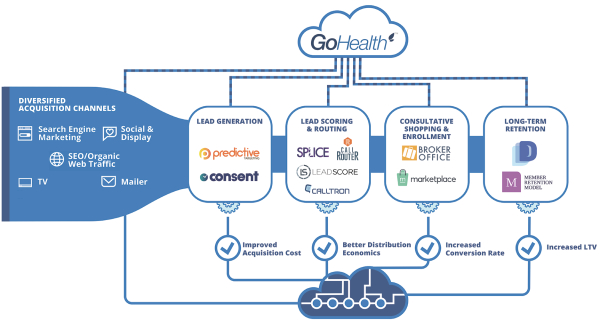
Our platform utilizes proprietary technology, machine-learning capabilities, data, efficient business processes, and highly skilled and trained licensed agents to generate a stable, visible revenue stream that benefits from favorable demographic trends. The key components of our platform are:
| • | Data-Driven, Omni-Channel Marketing. Based on predictive consumer lead targeting and a high cadence of multivariate testing on consumer lead generation properties, our data-driven, omni-channel marketing drives increased impressions and qualified prospects with a target return on marketing spend. |
| • | Proprietary LeadScore Technology. LeadScore, one of our proprietary machine-learning technologies, is built on large-scale, end-to-end sales data, predicts the LTV and conversion probability of consumer leads, and is utilized to optimize routing of the consumer leads in real-time regardless of their source. |
| • | Sophisticated Matching Technology. Our proprietary qualified prospect distribution, routing, and priority queuing technology based on LeadScore and agent performance data models help us to optimally match qualified prospects to those agents most likely to convert the qualified prospect to a customer. |
| • | The Marketplace. Our proprietary Marketplace technology features decision support tools and seamlessly integrates with carrier enterprise systems, empowering our highly skilled and trained agents to quickly and efficiently select the right health insurance plan for each consumer based on their specific needs and enroll them in those plans. |
| • | TeleCare Team. Our high-touch TeleCare team is focused on increasing consumer engagement with the GoHealth brand, selling new products and services to our consumers that help meet their healthcare needs, and helping consumers maximize their health insurance plan benefits to support long-term health and wellness. |
| • | Scalable and Compliant Infrastructure. Our cloud infrastructure and compliance-by-design technology ensures scalability and compliance across our platform. |
Our Value Proposition
We believe the key components of our platform are difficult to replicate for field-based agents, carrier-employed agents, and other digital or telesales competitors, making us increasingly valuable to carriers and consumers. As
4
Table of Contents
we increase the number of Submitted Policies, our data on qualified prospect, agent, and carrier performance becomes richer, feeding into our machine-learning and data science-enabled feedback loops, making our marketing and technology even smarter. This differentiates us from other channels and competitors, allowing us to generate more consumer leads, convert those consumer leads to customers at a higher rate, serve our customers over a longer period of time, and reduce our CAC.
We believe that LTV/CAC provides the best metric on a per commissionable Approved Submission basis into the efficiency and performance of our integrated platform. We focus on strengthening the key drivers of LTV/CAC, including marketing costs, the consumer lead to customer conversion rate and customer satisfaction. While we offer both do-it-yourself and agent-assisted channels to accommodate consumers’ preferences, we believe that for most qualified Medicare prospects, an agent-assisted model maximizes LTV/CAC. As we continue to scale our platform, we improve our key drivers through specialization and optimization using our proprietary data and machine-learning.
Our Products
We operate our business in four segments: (i) Medicare—Internal, (ii) Medicare—External, (iii) Individual and Family Plans, or IFP and Other—Internal and (iv) IFP and Other—External. The Medicare segments focus on sales of Medicare Advantage, Medicare Supplement, Medicare prescription drug plans, and Medicare Special Needs Plans, or SNPs, for multiple carriers. The Medicare segments are organized by distribution channel, as further described below:
| • | Internal. The internal segments primarily consist of sales of products and plans by GoHealth-employed agents offering qualified prospects plans from multiple carriers, GoHealth-employed agents offering qualified prospects plans on a carrier-specific basis, or sales of products and plans through our online platform without the assistance of our agents, which we refer to as DIY. |
| • | External. The external segments represent sales of products and plans under GoHealth’s carrier contracts using an independent, national network of agents, or external agencies, which are not employed by GoHealth. These agents utilize our technology and platform to enroll consumers in health insurance plans and provide a means to earn a return on consumer leads that otherwise may have not been addressed. |
The Medicare—Internal segment is the largest segment by revenue and a primary contributor to our growth and margin expansion. Over the last two years, we grew the Medicare—Internal segment multi-carrier channel agent count and prioritized the placement of qualified prospects into the Medicare—Internal segment. Going forward, we intend to continue our focus on growth and placing qualified prospects within this segment. The Medicare—Internal segment also provides significant benefits to the broader business. For example, carriers that partner with us through one or more of our internal segment businesses will often supplement our marketing and technology investments. Additionally, the external segments can be used when the number of consumer leads in our marketplace is higher than we can address in a timely fashion using our internal channel.
The IFP and Other segments focus on sales of individual and family plans (which include fixed indemnity and major medical products), dental plans, vision plans and other ancillary plans to individuals that are not Medicare-eligible. The IFP and Other segments are also organized by distribution channel, internal and external. The IFP and Other segments represent a valuable source of diversification of products, carriers, consumers and revenue that are not tied solely to Medicare. Many of the products in the IFP and Other segments have a policy life under a single year, and we are paid approximately 90% of our commission streams in these segments in the first year.
For the three months ended March 31, 2020, the Medicare segments represented 88.1% of total revenues compared to 59.7% of total revenues for the three months ended March 31, 2019 and the IFP and Other segments
5
Table of Contents
represented 11.9% of total revenues for the three months ended March 31, 2020 compared to 40.3% of total revenues for the three months ended March 31, 2019. For the Pro Forma Fiscal Year 2019, the Medicare segments represented 80.2% of total revenues compared to 49.6% of total revenues for the year ended December 31, 2018 and the IFP and Other segments represented 19.8% of total revenues for the Pro Forma Fiscal Year 2019 compared to 50.4% of total revenues for the year ended December 31, 2018.
Our Strengths
Fully Integrated End-to-End Insurance Marketplace
Our platform connects insurance consumers with carriers. The strength of our platform is our innovation in enhancing the education of, and transparency and choice for, consumers, which has dramatically changed how consumers purchase health insurance and displaced incumbent market leaders in insurance distribution. The insurance distribution incumbents, such as field-based and carrier-employed agents, offered neither the broad choice of health insurance plans we are able to offer nor the unbiased support in health insurance plan selection based on the years of consumer shopping data we have gathered and the sophisticated models we have developed to match health insurance plans to consumers. We apply our proprietary, machine-learning technology, LeadScore, to target, assess, and prioritize all of our consumer leads (over 4 million in 2019) in real-time. Incumbent insurance distributors do not have access to equivalent technology, and we believe this difference in capabilities allows us to benefit from lower CAC. Our technology is difficult to replicate because acquiring the data underlying our models at our scale (over 10 years of insurance data) and scope, as well as refining those models to the performance we have obtained would be time-consuming, expensive and complicated for newer entrants in this market. Our technology and business processes route qualified consumer leads online or via live transfer to agents across our multiple channels ensuring that few qualified prospects leave our marketplace without an interaction and maximizing each consumer interaction to ensure a higher likelihood of consumer acquisition and higher margin contribution. We use a combination of proprietary and third-party data, direct API connections to many carriers, and our proprietary technology platform, Marketplace, to educate, quote and enroll consumers in real-time to the health insurance plan best suited to meet their specific needs, which enhances long-term customer satisfaction. The resulting increase in the expected LTV of consumers obtained at a lower CAC has made our innovative distribution model more appealing to carriers and has altered their own approach to strategic marketing and consumer acquisition. The data we generate from each consumer interaction helps inform our marketing, consumer lead scoring, qualified prospect routing, and health insurance plan matching technology in a feedback loop. We engineered our marketplace for rapid scalability, with modern cloud infrastructure that has information security controls that are independently audited by several third-party firms and complies with HIPAA, TCPA and DOI and CMS regulations. We had over 122,400 Submitted Policies in the Medicare segments for the three months ended March 31, 2020 and over 427,000 Submitted Policies in the Medicare segments for the year ended December 31, 2019, which we believe makes us one of the largest health insurance marketplaces based on publicly available information about our competitors and our carriers and our general knowledge of the industry acquired over our 19-year operating history. The data generated through the sales process by these consumers helps us increase LTV/CAC through machine-learning enabled feedback loops, and allows us to improve and deepen our relationships with carriers.
6
Table of Contents
| (1) | 2019 AEP Sales/Agent/Day is presented for the multi-carrier sales outlet of the Medicare—Internal segment. |
| (2) | Average policy retention is presented as of January 1, 2019 for selected carriers that we believe are generally representative of our customer base for Medicare Advantage products. |
Data-driven, Omni-channel Marketing
We generate over 42.2 million unique consumer interactions per year across an omni-channel diversified portfolio of sources. These sources include digital methods, such as search engine marketing, impulse-marketing and social-media, and non-digital methods, including television, mailers and radio. We use our real-time consumer lead to customer conversion data from various marketing sources to rapidly and cost-efficiently adjust and scale our marketing sources to maximize LTV/CAC and cost per qualified prospect. We also use our database of over 85 million consumer lead records to build machine-learning models that create complex lookalike audiences to enable us to efficiently target consumer leads that are more likely to convert to customers. Using our rapid test-and-learn approach, in 2019 alone, we tested over 30,000 advertisements and more than 100 site variations, which drove an increase in the website visitor to consumer lead conversion rate to 17.2% in 2020, an increase of over 124% from a rate of 7.7% in 2019. For the multi-carrier sales outlet of the Medicare—Internal segment, we were able to increase qualified prospects from approximately 237,000 in 2018 to approximately 930,000 in 2019, an increase of 292.4%, while also increasing the rate of qualified prospect to Submitted Policy conversions during the three months ended December 31, 2019 for this channel to 27% from 24% during the same period in 2018. We have grown in both number and quality of our consumer interactions while also generating more internal consumer leads, reducing our dependence on acquiring consumer leads from third-party sources. For the three months ended December 31, 2019, the multi-carrier sales outlet of the Medicare—Internal segment had 70% of consumer leads internally generated, compared to 58% for the same period in 2018.
7
Table of Contents
Deep, Tenured and Expanding Relationships with Top Carriers
Our carrier relationships allow us to offer a wide variety of products and plans across our platform and offer solutions tailored to consumers’ healthcare needs. We are a critical partner to our top carriers, for which we use our data and direct API connections to help inform their plan and network design and assist with budgeting. Our carrier relationships are stable, as evidenced by the fact that our relationships with each of our five largest carriers, measured by 2019 submission volume, exceeds five years. Over the past five years, we have expanded those relationships from initially covering individual and family products to covering Medicare Advantage products at all five of these carriers. We are licensed in all 50 states and the District of Columbia, which combined with our data-driven, omni-channel marketing and effective and scalable marketplace, makes us a partner of choice for the leading Medicare Advantage plans nationally and in each state. In 2020, we expect our platform will include Medicare Advantage products from at least one of the top two carriers, as measured by Medicare Advantage enrollees in each county, in 49 states, which collectively represented 95% of 2019 Medicare enrollments. In 2019, our platform included Medicare Advantage products from at least one of the top two carriers, as measured by Medicare Advantage enrollees in each county, in 24 states, which collectively represented 54% of 2019 Medicare enrollments. We believe that consumers increasingly want greater choice and are looking for quality health insurance plans as measured by CMS STAR ratings. We believe that by offering more health insurance plans in each county and more higher-rated health insurance plans, we can increase the rate of consumer lead to customer conversions and customer satisfaction rates.
Best-in-Class Medicare LTV/CAC Ratio Driven by Proprietary Technology, Business Processes, Data and Highly Skilled Agents
Our integrated technology platform, business processes, data and highly skilled and trained agents enable us to rapidly scale while improving our unit economics, as measured by LTV/CAC. As we scale our business, our machine-learning data combined with our omni-channel marketing allows us to become progressively better at acquiring consumer leads with favorable engagement potential and to do so at lower cost. In doing so, we increase the lifetime commissions generated by the consumer leads we convert, which increases LTV per Approved Submission, and we reduce the cost of acquiring consumer leads, lowering CAC per commissionable Approved Submission. With increasing scale, our proprietary LeadScore and CallRouter technologies become better at assessing the profile and predicted value of each incoming consumer lead and routing the consumer lead to the agent most likely to convert the consumer, further lowering CAC per commissionable Approved Submission. The CallRouter platform also utilizes data-driven agent clustering to enable us to train and specialize our agents on specific customer segments to optimize our results. We dynamically route qualified prospects across all of our channels with a focus on converting our highest value qualified prospects in our most profitable channels and enhancing the consumer experience across our platform. Our Marketplace technology quickly compares health insurance plans that most closely match the consumer’s specific needs, which increases the potential conversion and engagement of the consumer to the health insurance plan, increasing the LTV per Approved Submission, while also decreasing agent plan selection time, thus decreasing CAC per commissionable Approved Submission. Finally, our management team has extensive leadership experience managing customer service centers and scaling new sales offices. Our agent recruiting, training, development programs, and technology decision support with our Marketplace technology allow us to improve agent productivity, while also enhancing our consumer experience. We believe our LTV/CAC ratios for the Medicare segments are superior to those achieved by other digital marketplaces, carriers, and field-based agents.
History of Continuous Growth and Innovation and Proven Ability to Add Products
Our Founders and management team have a consistent track record of growth and entry into new market opportunities for our business. Since our founding in 2001, we evolved from a company selling quoting and enrollment technology to independent brokers to the fully integrated end-to-end insurance marketplace we are
8
Table of Contents
today. We have diversified our product mix to add individual and family plans, dental and vision plans, prescription drug plans, and most recently, Medicare plans. This has enabled us to serve more consumers and to prioritize different products depending on regulatory and political environments, carriers’ priorities and consumers’ preferences. Our data assets, technology, and compliance infrastructure have scaled efficiently with each consumer interaction and health insurance plan submission through our platform, and as we have invested in the next generation of our proprietary technology. We believe our management team, entrepreneurial spirit, and data and technology position us well for continuous growth in the future in our current product segments and other insurance products segments we may enter.
Our Growth Strategies
Expand Our Carrier Relationships and Health Insurance Plan Options to Grow the Medicare Segments
We believe we are a partner of choice for the top carriers in the Medicare marketplace because of our scale, efficiency and ability to integrate with carriers using direct API connections to exchange data and insights. Given our growth in Approved Submissions in the Medicare segments and the integrated data and technology of our platform, Medicare carriers have shown increased interest in working with us, including those who have not traditionally used digitally-enabled models. In 2020, we expect our platform will include Medicare Advantage products from at least one of the top two carriers, as measured by Medicare Advantage enrollees in each county, in 49 states, which collectively represented 95% of 2019 Medicare enrollments. In 2019, our platform included Medicare Advantage products from at least one of the top two carriers, as measured by Medicare Advantage enrollees in each county, in 24 states, which collectively represented 54% of 2019 Medicare enrollments. This allows us to benefit from enhanced return of scale, more efficient marketing in these geographies, increased agent conversion rates of qualified prospects to customers, and improved customer satisfaction rates as we meet the needs of our customers. In addition, we are increasingly adding SNPs into our marketplace from both existing and new carrier relationships. Unlike Medicare Advantage products, which can largely be sold only during the Medicare annual enrollment period and open enrollment period, SNPs can generally be sold throughout the special enrollment period. As a result, we are able to maximize the value of our consumer interactions and marketing spend during the special enrollment period and prioritize agent growth year round. As we add more Medicare products and expand SNP offerings, we allocate more of our existing agent seat count to the Medicare—Internal segment from other less profitable channels, reducing the need to open new facilities. Additionally, we have implemented work from home options to increase agent efficiency and capacity without a significant increase in fixed costs.
Continue to Increase Our Profitability By Using our Data to Improve our Technology, Business Processes, and Agent Performance
We are implementing a number of initiatives to help improve our LTV/CAC, which is a key measure of our unit economics and overall business profitability, by using our data to improve our platform and predictive capabilities, business processes, and agent performance.
| • | Upgraded Marketplace Technology. In October 2019, we launched an upgrade to our proprietary Marketplace technology to increase agent productivity by improving the flow of data across our platform, advancing our decision support capabilities, and improving the qualified prospect to Submitted Policy conversion rates of our overall agent population to a level closer to that of our most productive agents. |
| • | Improving LeadScore and Call Routing Technologies. We are improving our LeadScore and call-routing technologies, and expanding our business intelligence and analytics staffing to direct qualified prospects to agents or DIY channels that are most likely to result in such qualified prospects enrolling in the health insurance plan that best meets their needs while remaining economically attractive for us. |
9
Table of Contents
| We are also increasingly using our data to identify the best agent clusters to enroll an individual qualified prospect based on our Marketplace engine’s determination of their likely optimal plan design, carrier, and demographic match based on the information we have about that qualified prospect. Additionally, we are investing in technology that will allow us to use our data to direct our marketing spend into growing our flow of qualified prospects in the highest-value marketing channels and enhancing our proprietary LeadScore technology to assess and iterate, in real-time, the performance of those marketing channels throughout the year. |
| • | Improving Recruiting and Training of Agents. We are improving the recruiting and training of our agents to match the profiles of our highest performing agents. The opportunity to reduce the variability in our agent performance is significant, as our top 25% of agents for the multi-carrier sales outlet of the Medicare—Internal segment on average were 61% more productive than the remaining 75% of our agents for the multi-carrier sales outlet of the Medicare—Internal segment, based on conversion rates of qualified prospects to Submitted Policies for the three months ended March 31, 2020. We have analyzed our most productive agents and revised our recruiting, training and onboarding of the number of licenses and appointments to most closely match the skills and experiences of our most productive agents. |
Build Identification with the GoHealth Brand
We believe we can solidify our position as the largest Medicare marketplace and brand for consumers’ health insurance needs. As the Medicare markets continue to grow and the Medicare Advantage sector continues to gain market share, carriers are and will continue differentiating their health insurance plans by offering additional products and services. This differentiation creates the need for more education, transparency and choice, and the need for a “Trusted Advisor” role that we believe the GoHealth brand can own. By helping customers make this choice, they can more readily identify the GoHealth brand, which we believe differentiates us from our competitors. This allows us to improve customer satisfaction even when their underlying carrier or plan product changes.
We are using technology and data increasingly to build the GoHealth brand and our digital marketing campaigns, which significantly improved impressions in 2019 with over 1.1 billion impressions generated, compared to 225 million impressions generated in 2018. We have launched our new plan comparison tool and are launching a new website that we will consolidate into one consumer website in 2020, which we believe will enhance conversion in our DIY channel.
Provide Additional Products and Services to our Qualified Medicare Prospects, Existing Customers and Carriers
In 2019, we interacted with approximately 930,000 qualified prospects through the multi-carrier sales outlet of the Medicare—Internal segment. While we have focused historically on educating and enrolling those qualified prospects in Medicare products, we have not historically prioritized offering qualified prospects or existing customers additional products, such as life, dental, hearing, or vision plans if their Medicare product does not offer coverage for these services. We have a significant opportunity to sell additional products to our qualified Medicare prospects and existing Medicare customers going forward.
We currently enroll a sizable percentage of Medicare customers for our largest carriers, but there is still significant opportunity to grow our share of enrollments for existing carriers even while we add new carriers to our marketplace. We are using our data to help our largest carriers inform the benefit design of their health insurance plans and product competitiveness in given regions, which is a value added service that traditional field-agents and carrier internal channels cannot offer. We are also focused on increasing offerings of additional
10
Table of Contents
revenue generating services that are valuable to our Medicare carriers and enhance the health of our customers, including by helping new Medicare enrollees sign up for a health-risk assessment, which helps calibrate the Medicare Advantage premium paid by Medicare to the private plan. Additionally, we are exploring opportunities to (1) provide screening of customers for social determinants of health factors, such as loneliness, or food or housing insecurity, that could lead to higher medical costs if not addressed, and (2) promote the benefits of value-based care through referrals of consumers looking to change or add a primary care physician. By offering more services to our Medicare carriers, we can improve the depth of our carrier relationships, open new revenue streams and build customer loyalty.
Provide Additional Products and Services Through Our Marketplace Technology
Our Founders and management team built our Marketplace technology over a 19-year period of continuous investment and growth. We have developed relationships with over 80 carriers and offer a wide variety of products and plans, including individual and family plans, dental, vision, prescription drug and Medicare plans. Our Marketplace technology allows us to efficiently generate meaningful numbers of consumer submissions for health insurance plans, generate commission revenue streams based on Approved Submissions, and maximize the contribution margin of these commissions through efficiencies in CAC. Over the last two years, Medicare had the highest LTV/CAC of the health insurance plan products that we distribute through our Marketplace technology.
We have the technology, carrier, customer relationships and management team to broaden or shift our focus to other products if we think there is a revenue opportunity, and we have demonstrated this capability to add products historically. For example, after the enactment of the Affordable Care Act in 2010, or the ACA, we significantly grew the IFP and Other segments revenue in a relatively short period of time, which we believe made us a leader in the ACA web-broker space.
Our Market and Trends Impacting the Industry
Demographic, consumer preference and regulatory factors are driving growth in the individual health insurance market. We service this market through the Medicare segments and the IFP and Other segments.
Medicare
Medicare enrollment is expected to grow significantly over the next 10 years as 10,000+ individuals turn 65 each day and become Medicare-eligible. The proportion of the population that is age 65 and older increased from 13% in 2010 to 15% in 2016 and is expected to reach 17% by 2020, according to the United States Census Bureau. As a result, Medicare enrollment is growing steadily, with the number of Medicare enrollees expected to grow from 59.9 million in 2018, to approximately 68.4 million in 2023 and 76.7 million by 2028. This growth in Medicare enrollment will increase the numbers of qualified prospects for our marketing efforts. Internet usage by individuals age 65 and older is also increasing, with 73% using the Internet in 2019 compared to 40% in 2009 according to the Pew Research Center. Seniors are also transacting more online, with 55% of people age 65 and older making online purchases monthly according to SheerID, and 63% of people age 65 and older obtained health information from a website, according to the 2018 BMC Health Services Research.
In addition to the growth in Medicare-eligible beneficiaries and higher online usage, the interest in Medicare-eligible individuals in private Medicare plans is expected to continue to increase. In 2019, 38% of all Medicare beneficiaries were enrolled in Medicare Advantage plans and between 2018 and 2019, total Medicare Advantage enrollment grew by about 1.5 million individuals or 7%. LEK Consulting estimated that Medicare Advantage penetration is likely to reach 50% penetration for all Medicare-eligible individuals by 2025 and could reach as high as 60% to 70% between 2030 and 2040. Compared to original Medicare, Medicare Advantage has lower
11
Table of Contents
annual healthcare costs and access to greater benefits, according to a 2019 Milliman report. In addition, we expect the increase in Medicare Advantage penetration to accelerate due to the COVID-19 pandemic because of increasing consumer preference for online and telephonic insurance enrollment as opposed to face-to-face consultations. The number of beneficiaries in SNPs also increased significantly in the last 10 years from 900,000 in 2009 to 2.5 million in 2019 providing additional opportunity for year-round sales outside of the open enrollment period and annual enrollment period. We believe the increased penetration of Medicare Advantage, as well as the growth of the number of Medicare-eligible individuals, will lead to increased submissions for marketplaces, such as ours in the future. Consumers choose Medicare Advantage plans around a specific criteria set which includes premium, total expected costs out of pocket, provider network composition, formulary coverage and supplemental benefits, which we believe are more efficiently addressed through a non-field-based distribution channel.
The growth in Medicare-eligible seniors and growing interest in private Medicare plans has led to an increase in plan choices. Nationwide, 3,148 Medicare Advantage plans will be available in 2020, an increase of 414 plans since 2019. The average beneficiary will be able to choose from among 28 health insurance plans in 2020, up from 18, five years ago. In addition to the increase in plan choices, the differences between health insurance plans has increased significantly. For 2019, CMS eliminated the meaningful difference requirement to improve competition, innovation and available benefit offerings and provide beneficiaries with affordable health insurance plans that are tailored to a consumer’s specific healthcare needs and financial situation. The types of supplemental benefits that health insurance plans cover increased in 2018, 2019 and 2020 and now cover transportation assistance, meal benefits, in-home support, telemonitoring, and caregivers support, among others. This growth in plan choices made education and assistance with plan selection more important for consumers and allows carriers to target specific Medicare Advantage plans with packages of benefits designed to be attractive to different segments of Medicare consumers. Marketplaces such as ours help educate consumers, and assist them in making informed plan choices. In addition, we specifically micro-target our marketing to precise populations to allow carriers to grow increasingly differentiated health insurance plans. This precise marketing is more difficult for traditional radio or television-based marketing channels.
12
Table of Contents
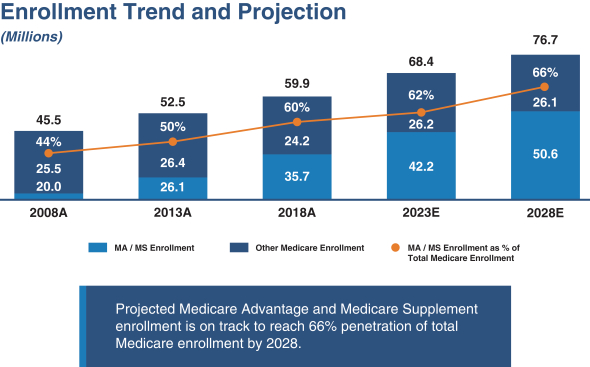
Source: CSG Actuarial (2019) and U.S. Department of Health and Human Services (2019).
Individual and Family Plans
After the passage of the ACA, the individual health insurance market grew from 10.6 million enrollees in 2013 to 17.4 million enrollees in 2015. Such increase was driven by (1) the requirement to purchase health insurance, or the individual mandate, (2) the requirement that carriers not consider pre-existing medical conditions in coverage decisions and (3) premium subsidies for middle and lower income individuals that were also contained in that legislation. With the repeal of the individual mandate in 2017 and broader economic trends, such as gains in employment, which increased the number of people having job-based coverage, the individual market has declined. Despite the decline, the individual market was composed of 13.8 million members in 2018, a meaningful increase from 2011 levels and in 2019, the market size stabilized with 13.7 million members enrolled. This market stabilization was driven by lower premium increases in 2019, as compared to 2018 and 2017 for individual insurance plans; an increase in individuals who do not receive job-based insurance due to the rise of the “gig economy;” and, expanded plan options in the individual market from carriers. According to a Kaiser Family Foundation report published in 2020, in the third quarter of 2019, the average gross margin per member per month for carriers in the individual market was $131.17, as compared to $32.88 in the third quarter of 2016 shortly after the repeal of the individual mandate. This increased profitability for insurers is expected to have a positive impact on the individual market going forward. In addition, the number of individuals eligible for the individual market is growing. Forbes estimated that 57 million U.S. workers, approximately 36% of employees, are in the “gig economy” and many of these individuals will not receive health insurance through their jobs. We believe that growth in the individual market will benefit the Company in the future.
Centerbridge
On September 13, 2019, Centerbridge, indirectly through a subsidiary of GoHealth Holdings, LLC, acquired a 100% interest in Norvax, the predecessor company. Centerbridge is a global private investment firm with over
13
Table of Contents
$25 billion in assets under management and offices in New York and London. The firm manages capital through varied investment funds and special purpose partnerships. For additional information regarding Centerbridge’s ownership in us before and after the Transactions, see “—Summary of the Transactions” and “Principal Stockholders.”
Summary Risk Factors
Participating in this offering involves substantial risk. Our ability to execute our strategy is also subject to certain risks. The risks described under the heading “Risk Factors” included elsewhere in this prospectus may cause us not to realize the full benefits of our strengths or may cause us to be unable to successfully execute all or part of our strategy. Some of the most significant challenges and risks we face include the following:
| • | our ability to comply with the numerous, complex and frequently changing laws regulating the marketing and sale of Medicare plans; |
| • | the potential for an adverse change in our relationships with carriers, including a loss of carrier relationships; |
| • | failure to grow our customer base or retain our existing customers; |
| • | carriers’ ability to reduce commissions paid to us and adversely change their underwriting practices; |
| • | significant consolidation in the healthcare industry that could adversely alter our relationships with carriers; |
| • | information technology system failures or capacity constraints interrupting our operations; |
| • | factors that adversely impact our estimate of LTV; |
| • | our dependence on agents to sell insurance plans; |
| • | changes in the health insurance system and laws and regulation governing health insurance markets; |
| • | inability to effectively advertise our products; and |
| • | the significant influence Centerbridge will have over us after the Transactions, including control over decisions that require the approval of stockholders. |
Before you invest in our Class A common stock, you should carefully consider all the information in this prospectus, including matters set forth under the heading “Risk Factors.”
Summary of the Transactions
GoHealth, Inc., a Delaware corporation, was formed on March 27, 2020 and is the issuer of the Class A common stock offered by this prospectus. Prior to this offering, all of our business operations have been conducted through GoHealth Holdings, LLC and its direct and indirect subsidiaries. Prior to the Transactions, we expect there will initially be one holder of common stock of GoHealth, Inc. We will consummate the following organizational transactions in connection with this offering:
| • | we will amend and restate the existing limited liability company agreement of GoHealth Holdings, LLC, which will become effective substantially concurrently with or prior to the consummation of this offering, to, among other things, (1) recapitalize all existing ownership interests in GoHealth Holdings, LLC (including profits interests awarded under the existing limited liability company agreement of GoHealth Holdings, LLC (and corresponding profits interests issued under the existing limited liability agreement of Blizzard Management Feeder, LLC)) into LLC Interests (and, in the case of corresponding profits interests issued by Blizzard Management Feeder, LLC, into common units of Blizzard Management Feeder, LLC) and (2) appoint GoHealth, Inc. as the sole managing member of GoHealth Holdings, LLC upon its acquisition of LLC Interests in connection with this offering; |
14
Table of Contents
| • | we will amend and restate GoHealth, Inc.’s certificate of incorporation to, among other things, provide (1) for Class A common stock, with each share of our Class A common stock entitling its holder to one vote per share on all matters presented to our stockholders generally and (2) for Class B common stock, with each share of our Class B common stock entitling its holder to one vote per share on all matters presented to our stockholders generally, and that shares of our Class B common stock may only be held by the Continuing Equity Owners and their respective permitted transferees as described in “Description of Capital Stock—Common Stock—Class B Common Stock;” |
| • | we will acquire, by means of one or more mergers, the Blocker Company (the “Blocker Merger”) and will issue to the Blocker Shareholders shares of our Class A common stock and, upon consummation of this offering, $ million (based on the midpoint of the estimated price range set forth on the cover page of this prospectus) in cash to Blocker Shareholders as partial consideration in the Blocker Merger; |
| • | we will issue shares of our Class B common stock to the Continuing Equity Owners, which is equal to the number of LLC Interests held by such Continuing Equity Owners, for nominal consideration; |
| • | we will issue shares of our Class A common stock to the purchasers in this offering (or shares if the underwriters exercise in full their option to purchase additional shares of Class A common stock) in exchange for net proceeds of approximately $ million (or approximately $ million if the underwriters exercise in full their option to purchase additional shares of Class A common stock) based upon an assumed initial public offering price of $ per share (which is the midpoint of the estimated price range set forth on the cover page of this prospectus), less the underwriting discount and estimated offering expenses payable by us; |
| • | we will use the net proceeds from this offering to (i) purchase newly-issued LLC Interests (or LLC Interests if the underwriters exercise in full their option to purchase additional shares of Class A common stock) directly from GoHealth Holdings, LLC at a price per unit equal to the initial public offering price per share of Class A common stock in this offering less the underwriting discount and estimated offering expenses payable by us and (ii) pay $ million in cash to the Blocker Shareholders as partial consideration in the Blocker Merger; |
| • | GoHealth Holdings, LLC intends to use the net proceeds from the sale of LLC Interests to GoHealth, Inc. (i) to partially redeem certain of the LLC Interests held by the Continuing Equity Owners, (ii) to satisfy in full $ million in aggregate principal amount of an obligation relating to an existing equity instrument in connection with the Transactions and (iii) for general corporate purposes to support the growth of the business, in each case, as described under “Use of Proceeds;” and |
| • | GoHealth, Inc. will enter into (1) the Stockholders Agreement with Centerbridge and our Founders, (2) the Registration Rights Agreement with certain of the Continuing Equity Owners and (3) the Tax Receivable Agreement with GoHealth Holdings, LLC, the Continuing Equity Owners and the Blocker Shareholders. For a description of the terms of the Stockholders Agreement, the Registration Rights Agreement and the Tax Receivable Agreement, see “Certain Relationships and Related Party Transactions.” |
Immediately following the consummation of the Transactions (including this offering):
| • | GoHealth, Inc. will be a holding company and its principal asset will consist of LLC Interests it acquires directly from GoHealth Holdings, LLC and indirectly from certain of the Continuing Equity Owners (including the Blocker Shareholders); |
| • | GoHealth, Inc. will be the sole managing member of GoHealth Holdings, LLC and will control the business and affairs of GoHealth Holdings, LLC and its direct and indirect subsidiaries; |
15
Table of Contents
| • | GoHealth, Inc. will own, directly or indirectly, LLC Interests of GoHealth Holdings, LLC, representing approximately % of the economic interest in GoHealth Holdings, LLC (or LLC Interests, representing approximately % of the economic interest in GoHealth Holdings, LLC if the underwriters exercise in full their option to purchase additional shares of Class A common stock); |
| • | the Continuing Equity Owners (excluding Centerbridge) will own (1) LLC Interests of GoHealth Holdings, LLC, representing approximately % of the economic interest in GoHealth Holdings, LLC (or LLC Interests, representing approximately % of the economic interest in GoHealth Holdings, LLC if the underwriters exercise in full their option to purchase additional shares of Class A common stock) and (2) shares of Class B common stock of GoHealth, Inc., representing approximately % of the combined voting power of all of GoHealth, Inc.’s common stock (or shares of Class B common stock of GoHealth, Inc., representing approximately % if the underwriters exercise in full their option to purchase additional shares of Class A common stock); |
| • | Centerbridge (directly or indirectly, including through the Blocker Shareholders) will own (1) shares of Class A common stock of GoHealth, Inc. (or shares of Class A common stock of GoHealth, Inc. if the underwriters exercise in full their option to purchase additional shares of Class A common stock), representing approximately % of the combined voting power of all of GoHealth, Inc.’s common stock and approximately % of the economic interest in GoHealth, Inc. (or approximately % of the combined voting power and approximately % of the economic interest if the underwriters exercise in full their option to purchase additional shares of Class A common stock), (2) directly and indirectly through GoHealth, Inc.’s ownership of LLC Interests, approximately % of the economic interest in GoHealth Holdings, LLC (or approximately % of the economic interest in GoHealth Holdings, LLC if the underwriters exercise in full their option to purchase additional shares of Class A common stock) and (3) shares of Class B common stock of GoHealth, Inc., representing approximately % of the combined voting power of all of GoHealth, Inc.’s common stock (or shares of Class B common stock of GoHealth, Inc., representing approximately % if the underwriters exercise in full their option to purchase additional shares of Class A common stock); and |
| • | the purchasers in this offering will own (1) shares of Class A common stock of GoHealth, Inc. (or shares of Class A common stock of GoHealth, Inc. if the underwriters exercise in full their option to purchase additional shares of Class A common stock), representing approximately % of the combined voting power of all of GoHealth, Inc.’s common stock and approximately % of the economic interest in GoHealth, Inc. (or approximately % of the combined voting power and approximately % of the economic interest if the underwriters exercise in full their option to purchase additional shares of Class A common stock), and (2) through GoHealth, Inc.’s ownership of LLC Interests, indirectly will hold approximately % of the economic interest in GoHealth Holdings, LLC (or approximately % of the economic interest in GoHealth Holdings, LLC if the underwriters exercise in full their option to purchase additional shares of Class A common stock). |
As the sole managing member of GoHealth Holdings, LLC, we will operate and control all of the business and affairs of GoHealth Holdings, LLC and, through GoHealth Holdings, LLC and its direct and indirect subsidiaries, conduct our business. Following the Transactions, including this offering, GoHealth, Inc. will have the majority economic interest in GoHealth Holdings, LLC, and will control the management of GoHealth Holdings, LLC as its sole managing member. As a result, GoHealth, Inc. will consolidate GoHealth Holdings, LLC and record a significant non-controlling interest in a consolidated entity in GoHealth, Inc.’s consolidated financial statements for the economic interest in GoHealth Holdings, LLC held by the Continuing Equity Owners.
Unless otherwise indicated, this prospectus assumes the shares of Class A common stock are offered at $ per share (the midpoint of the estimated price range set forth on the cover page of this prospectus). Pursuant to the terms of the Existing LLC Agreement, the split between the number of LLC Interests will vary depending on
16
Table of Contents
the initial public offering price in this offering. The initial public offering price will also impact the relative allocation of LLC Interests issued in the Transactions among the Original Equity Owners and, in turn, the shares of Class A common stock and Class B common stock issued to the Original Equity Owners in the Transactions. Additionally, while the number of shares of Class A common stock being offered hereby to the public will not change, any increase or decrease in the number of shares of Class A common stock sold by GoHealth, Inc. in this offering due to a change in the initial public offering price will result in a corresponding increase or decrease in the number of LLC Interests purchased by GoHealth, Inc. directly from GoHealth Holdings, LLC at a price per unit equal to the initial public offering price per share of Class A common stock in this offering. Therefore, the indirect economic interest in GoHealth Holdings, LLC represented by the shares of Class A common stock sold in this offering will be largely unaffected by the initial public offering price. For more information regarding the impact of the initial offering price on the share information included throughout this prospectus, see “—The Offering.”
For more information regarding the Transactions and our structure, see “Our Organizational Structure.”
17
Table of Contents
Ownership Structure
The diagram below depicts our organizational structure after giving effect to the Transactions, including this offering, assuming no exercise by the underwriters of their option to purchase additional shares of Class A common stock.
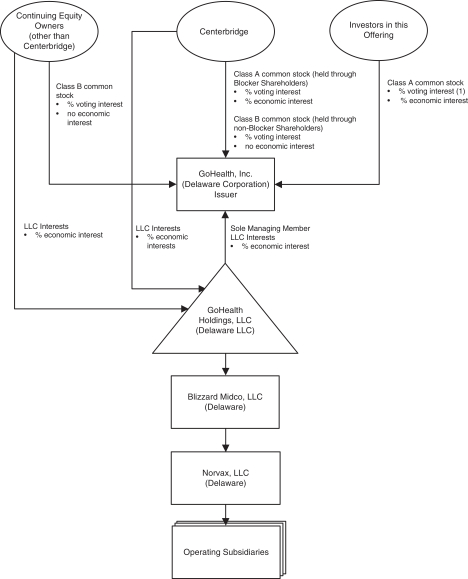
| (1) | Investors in this offering will hold approximately % of the voting interest. |
GoHealth, Inc., the issuer of the Class A common stock in this offering, was incorporated as a Delaware corporation on March 27, 2020. Our corporate headquarters are located at 214 West Huron Street, Chicago, Illinois 60654. Our telephone number is (312) 386-8200. Our principal website address is www.gohealth.com. The information on any of our websites is deemed not to be incorporated in this prospectus or to be part of this prospectus.
18
Table of Contents
After giving effect to the Transactions, including this offering, GoHealth, Inc. will be a holding company whose principal asset will consist of % of the outstanding LLC Interests of GoHealth Holdings, LLC (or % if the underwriters exercise in full their option to purchase additional shares of our Class A common stock).
Implications of Being an Emerging Growth Company
We qualify as an “emerging growth company” as defined in the Jumpstart Our Business Startups Act of 2012, or the JOBS Act. An emerging growth company may take advantage of certain reduced reporting and other requirements that are otherwise generally applicable to public companies. As a result:
| • | we are required to have only two years of audited financial statements and only two years of related selected financial data and management’s discussion and analysis of financial condition and results of operations disclosure; |
| • | we are not required to engage an auditor to report on our internal control over financial reporting pursuant to Section 404(b) of the Sarbanes-Oxley Act of 2002, or the Sarbanes-Oxley Act; |
| • | we are not required to comply with the requirement of the Public Company Accounting Oversight Board, or PCAOB, regarding the communication of critical audit matters in the auditor’s report on the financial statements; |
| • | we are not required to submit certain executive compensation matters to stockholder advisory votes, such as “say-on-pay,” “say-on-frequency” and “say-on-golden parachutes;” and |
| • | we are not required to comply with certain disclosure requirements related to executive compensation, such as the requirement to present a comparison of our Chief Executive Officer’s compensation to our median employee compensation. |
We may take advantage of these reduced reporting and other requirements until the last day of our fiscal year following the fifth anniversary of the completion of this offering, or such earlier time that we are no longer an emerging growth company, including if we have more than $1.07 billion in annual revenue, have more than $700 million in market value of our Class A common stock held by non-affiliates, or issue more than $1.0 billion of non-convertible debt over a three-year period. We may choose to take advantage of some but not all of these reduced burdens. We have elected to adopt the reduced requirements with respect to our financial statements and the related selected financial data and “Management’s Discussion and Analysis of Financial Condition and Results of Operations” disclosure, including in this prospectus.
In addition, the JOBS Act permits an emerging growth company like us to take advantage of an extended transition period to comply with new or revised accounting standards applicable to public companies. We have elected to use this extended transition period. As a result, the information that we provide to stockholders may be different than the information you may receive from other public companies in which you hold equity.
19
Table of Contents
The Offering
| Issuer |
GoHealth, Inc. |
| Shares of Class A common stock offered by us |
shares (or shares if the underwriters exercise in full their option to purchase additional shares). |
| Underwriters’ option to purchase additional shares of Class A common stock from us |
shares. |
| Shares of Class A common stock to be outstanding immediately after this offering |
shares, representing approximately % of the combined voting power of all of GoHealth, Inc.’s common stock (or shares, representing approximately % of the combined voting power of all of GoHealth, Inc.’s common stock if the underwriters exercise in full their option to purchase additional shares of Class A common stock), % of the economic interest in GoHealth, Inc. and % of the indirect economic interest in GoHealth Holdings, LLC. |
| Shares of Class B common stock to be outstanding immediately after this offering |
shares, representing approximately % of the combined voting power of all of GoHealth, Inc.’s common stock (or shares, representing approximately % of the combined voting power of all of GoHealth, Inc.’s common stock if the underwriters exercise in full their option to purchase additional shares of Class A common stock) and no economic interest in GoHealth, Inc. |
| LLC Interests to be held by us immediately after this offering |
LLC Interests, representing approximately % of the economic interest in GoHealth Holdings, LLC (or LLC Interests, representing approximately % of the economic interest in GoHealth Holdings, LLC if the underwriters exercise in full their option to purchase additional shares of Class A common stock). |
| LLC Interests to be held directly by the Continuing Equity Owners (excluding Centerbridge) immediately after this offering |
LLC Interests, representing approximately % of the economic interest in GoHealth Holdings, LLC (or LLC Interests, representing approximately % of the economic interest in GoHealth Holdings, LLC if the underwriters exercise in full their option to purchase additional shares of Class A common stock). |
| LLC Interests to be held by Centerbridge immediately after this offering |
LLC Interests, representing approximately % of the economic interest in GoHealth Holdings, LLC (or LLC Interests, representing approximately % of the economic interest in GoHealth Holdings, LLC if the underwriters exercise in full their option to purchase additional shares of Class A common stock). |
| Ratio of shares of Class A common stock to LLC Interests |
Our amended and restated certificate of incorporation and the GoHealth Holdings, LLC Agreement will require that we and GoHealth Holdings, LLC at all times maintain a one-to-one ratio between the number of shares of Class A common stock issued by us and the number of LLC Interests owned by us, except as otherwise determined by us. |
20
Table of Contents
| Ratio of shares of Class B common stock to LLC Interests |
Our amended and restated certificate of incorporation and the GoHealth Holdings, LLC Agreement will require that we and GoHealth Holdings, LLC at all times maintain a one-to-one ratio between the number of shares of Class B common stock owned by the Continuing Equity Owners and their respective permitted transferees and the number of LLC Interests owned by the Continuing Equity Owners and their respective permitted transferees, except as otherwise determined by us. Immediately after the Transactions, the Continuing Equity Owners will together own 100% of the outstanding shares of our Class B common stock. |
| Permitted holders of shares of Class B common stock |
Only the Continuing Equity Owners and the permitted transferees of Class B common stock as described in this prospectus will be permitted to hold shares of our Class B common stock. Shares of Class B common stock are transferable for shares of Class A common stock only together with an equal number of LLC Interests. See “Certain Relationships and Related Party Transactions—GoHealth Holdings, LLC Agreement—Agreement in Effect Upon Consummation of the Transactions.” |
| Voting rights |
Holders of shares of our Class A common stock and our Class B common stock will vote together as a single class on all matters presented to stockholders for their vote or approval, except as otherwise required by law or our amended and restated certificate of incorporation. Each share of our Class A common stock entitles its holders to one vote per share and each share of our Class B common stock entitles its holders to one vote per share on all matters presented to our stockholders generally. See “Description of Capital Stock.” |
| Redemption rights of holders of LLC Interests |
The Continuing Equity Owners may, subject to certain exceptions, from time to time at each of their options require GoHealth Holdings, LLC to redeem all or a portion of their LLC Interests in exchange for, at our election (determined solely by our independent directors (within the meaning of the Nasdaq rules) who are disinterested), newly-issued shares of our Class A common stock on a one-for-one basis or a cash payment equal to a volume weighted average market price of one share of our Class A common stock for each LLC Interest so redeemed, in each case, in accordance with the terms of the GoHealth Holdings, LLC Agreement; provided that, at our election (determined solely by our independent directors (within the meaning of the Nasdaq rules) who are disinterested), we may effect a direct exchange by GoHealth, Inc. of such Class A common stock or such cash, as applicable, for such LLC Interests. The Continuing Equity Owners may, subject to certain exceptions, exercise such redemption right for as long as their LLC Interests remain outstanding. See “Certain Relationships and Related Party Transactions—GoHealth Holdings, LLC Agreement—Agreement in Effect Upon Consummation of the Transactions.” Simultaneously with the payment of cash or shares of Class A common stock, as applicable, in connection with a redemption or exchange of LLC |
21
Table of Contents
| Interests pursuant to the terms of the GoHealth Holdings, LLC Agreement, a number of shares of our Class B common stock registered in the name of the redeeming or exchanging Continuing Equity Owner will automatically be transferred to the Company and will be cancelled for no consideration on a one-for-one basis with the number of LLC Interests so redeemed or exchanged. |
| Use of proceeds |
We estimate, based upon an assumed initial public offering price of $ per share (which is the midpoint of the estimated price range set forth on the cover page of this prospectus), that we will receive net proceeds from this offering of approximately $ million (or $ million if the underwriters exercise in full their option to purchase additional shares of Class A common stock), after deducting the underwriting discount and estimated offering expenses payable by us. We intend to use the net proceeds from this offering to (i) purchase newly-issued LLC Interests (or LLC Interests if the underwriters exercise in full their option to purchase additional shares of Class A common stock) directly from GoHealth Holdings, LLC at a price per unit equal to the initial public offering price per share of Class A common stock in this offering less the underwriting discount and estimated offering expenses payable by us and (ii) pay $ million in cash to the Blocker Shareholders as partial consideration in the Blocker Merger. GoHealth Holdings, LLC intends to use the net proceeds from the sale of LLC Interests to GoHealth, Inc. (i) to partially redeem certain of the LLC Interests held by the Continuing Equity Owners, (ii) to satisfy in full $ million in aggregate principal amount of an obligation relating to an existing equity instrument in connection with the Transactions and (iii) for general corporate purposes to support the growth of the business. GoHealth Holdings, LLC will bear or reimburse GoHealth, Inc. for all of the expenses of this offering. See “Use of Proceeds.” |
| Dividend policy |
We currently intend to retain all available funds and any future earnings to fund the development and growth of our business and to repay indebtedness, and therefore, we do not anticipate declaring or paying any cash dividends on our Class A common stock in the foreseeable future. Holders of our Class B common stock are not entitled to participate in any dividends declared by our board of directors. Because we are a holding company, our ability to pay cash dividends on our Class A common stock depends on our receipt of cash distributions from GoHealth Holdings, LLC and, through GoHealth Holdings, LLC, cash distributions and dividends from our other direct and indirect subsidiaries. Our ability to pay any cash dividends on our Class A common stock is limited by restrictions on the ability of GoHealth Holdings, LLC and our other direct and indirect subsidiaries to pay dividends or make distributions under the terms of our Credit Facilities. Any future determination as to the declaration and payment of dividends, if any, will be at the discretion of our board of directors, subject to compliance with contractual restrictions and covenants in the agreements governing our current |
22
Table of Contents
| and future indebtedness. Any such determination will also depend upon our business prospects, results of operations, financial condition, cash requirements and availability, industry trends and other factors that our board of directors may deem relevant. See “Dividend Policy.” |
| Controlled company exception |
After the consummation of the Transactions, we will be considered a “controlled company” within the meaning of the listing rules of The Nasdaq Global Market, or the Nasdaq rules, as will have more than 50% of the voting power for the election of directors. See “Principal Stockholders.” As a “controlled company,” we will not be subject to certain corporate governance requirements, including that: (1) a majority of our board of directors consists of “independent directors,” as defined under the Nasdaq rules; (2) we have a nominating and corporate governance committee that is composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities; (3) we have a compensation committee that is composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities; and (4) we perform annual performance evaluations of the nominating and corporate governance and compensation committees. As a result, we may not have a majority of independent directors on our board of directors, an entirely independent nominating and corporate governance committee, an entirely independent compensation committee or perform annual performance evaluations of the nominating and corporate governance and compensation committees unless and until such time as we are required to do so. |
| Tax receivable agreement |
We will enter into a Tax Receivable Agreement with GoHealth Holdings, LLC, the Continuing Equity Owners and the Blocker Shareholders that will provide for the payment by GoHealth, Inc. to the Continuing Equity Owners and the Blocker Shareholders of 85% of the amount of tax benefits, if any, that GoHealth, Inc. actually realizes (or in some circumstances is deemed to realize) as a result of (1) GoHealth, Inc.’s allocable share of existing tax basis acquired in connection with the Transactions (including the Blocker Company’s share of existing tax basis) and increases to such allocable share of existing tax basis; (2) increases in tax basis resulting from (a) GoHealth, Inc.’s purchase of LLC Interests directly from GoHealth Holdings, LLC and the partial redemption of LLC Interests by GoHealth Holdings, LLC, as described under “Use of Proceeds,” (b) future redemptions or exchanges (or deemed exchanges in certain circumstances) of LLC Interests for Class A common stock or cash as described above under “—Redemption rights of holders of LLC Interests” and (c) certain distributions (or deemed distributions) by GoHealth Holdings, LLC; and (3) certain additional tax benefits arising from payments made under the Tax Receivable Agreement. See “Certain Relationships and Related Party Transactions—Tax Receivable Agreement” for a discussion of the Tax Receivable Agreement. |
23
Table of Contents
| Registration rights agreement |
Pursuant to the Registration Rights Agreement, we will, subject to the terms and conditions thereof, agree to register the resale of the shares of our Class A common stock that are issuable to certain of the Continuing Equity Owners in connection with the Transactions. See “Certain Relationships and Related Party Transactions—Registration Rights Agreement” for a discussion of the Registration Rights Agreement. |
| Risk factors |
See “Risk Factors” beginning on page 31 and other information included in this prospectus for a discussion of factors you should carefully consider before deciding to invest in shares of our Class A common stock. |
| Trading symbol |
We have applied to list our Class A common stock on The Nasdaq Global Market under the symbol “GHTH.” |
| Directed share program |
At our request, the underwriters have reserved for sale, at the initial public offering price, up to 5% of the Class A common stock offered by this prospectus for sale to some of our directors, officers and employees through a directed share program, or Directed Share Program. If these persons purchase reserved shares, it will reduce the number of shares of Class A common stock available for sale to the general public. Any reserved shares of Class A common stock that are not so purchased will be offered by the underwriters to the general public on the same terms as the other shares of Class A common stock offered by this prospectus. See “Underwriting—Directed Share Program.” |
Unless we indicate otherwise or the context otherwise requires, all information in this prospectus:
| • | gives effect to the amendment and restatement of the GoHealth Holdings, LLC Agreement that converts all existing ownership interests in GoHealth Holdings, LLC into LLC Interests, as well as the filing of our amended and restated certificate of incorporation; |
| • | gives effect to the other Transactions, including the consummation of this offering; |
| • | excludes shares of Class A common stock reserved for issuance under our 2020 Equity Plan, or 2020 Plan, including approximately shares of Class A common stock issuable pursuant to stock options we intend to grant to certain of our directors, executive officers and other employees in connection with this offering as described under the captions “Executive Compensation— ” and “Executive Compensation— ;” |
| • | assumes an initial public offering price of $ per share of Class A common stock, which is the midpoint of the estimated price range set forth on the cover page of this prospectus; and |
| • | assumes no exercise by the underwriters of their option to purchase additional shares of Class A common stock from us. |
Pursuant to the terms of the Existing LLC Agreement, the split between the number of LLC Interests will vary depending on the initial public offering price in this offering. The initial public offering price will also impact the relative allocation of LLC Interests issued in the Transactions among the Original Equity Owners and, in turn, the shares of Class A common stock and Class B common stock issued to the Original Equity Owners in the
24
Table of Contents
Transactions. Additionally, while the number of shares of Class A common stock being offered hereby to the public will not change, any increase or decrease in the number of shares of Class A common stock sold by GoHealth, Inc. in this offering due to a change in the initial public offering price will result in a corresponding increase or decrease in the number of LLC Interests purchased by GoHealth, Inc. directly from GoHealth Holdings, LLC at a price per unit equal to the initial public offering price per share of Class A common stock in this offering. Therefore, the indirect economic interest in GoHealth Holdings, LLC represented by the shares of Class A common stock sold in this offering will be largely unaffected by the initial public offering price.
For illustrative purposes only, the table below shows the number of shares of Class A common stock we are selling in this offering (assuming no exercise of the underwriters’ option to purchase additional shares of Class A common stock from us), along with the number of LLC Interests that GoHealth, Inc. will purchase directly from GoHealth Holdings, LLC and indirectly from certain of the Continuing Equity Owners (including the Blocker Shareholders) at various initial public offering prices:
| Class A Common Stock offered by GoHealth, Inc. |
LLC Interests purchased by GoHealth, Inc. |
LLC Interests held by Continuing Equity Owners and Indirectly Purchased by GoHealth, Inc. |
||||||||||
| $ |
||||||||||||
| $ |
||||||||||||
| $ |
||||||||||||
| $ |
||||||||||||
For illustrative purposes only, the table below shows the number of LLC Interests, shares of Class A common stock and Class B common stock outstanding after giving effect to the Transactions and this offering (assuming no exercise of the underwriters’ option to purchase additional shares of Class A common stock from us) at various initial public offering prices:
| LLC Interests held by Continuing Equity Owners (excluding Centerbridge) |
LLC Interests held by Centerbridge |
LLC Interests held by GoHealth, Inc. |
Class A Common Stock |
Class B Common |
||||||||||||||||
| $ |
||||||||||||||||||||
| $ |
||||||||||||||||||||
| $ |
||||||||||||||||||||
| $ |
||||||||||||||||||||
For illustrative purposes only, the table below shows the combined voting power in GoHealth, Inc. and the combined direct or indirect (in the case of the Continuing Equity Owners and Centerbridge, through GoHealth, Inc.’s ownership of LLC Interests) economic interest in GoHealth Holdings, LLC of certain holders of shares of Class A common stock and Class B common stock after giving effect to the Transactions and this offering (assuming no exercise of the underwriters’ option to purchase additional shares of Class A common stock from us) at various initial public offering prices:
| Continuing Equity Owners (excluding Centerbridge) |
Centerbridge | Investors in this Offering |
||||||||||||||||||
| Voting Power | Economic Interest | Voting Power | Economic Interest | Voting Power | Economic Interest | |||||||||||||||
| $ |
||||||||||||||||||||
| $ |
||||||||||||||||||||
| $ |
||||||||||||||||||||
| $ |
||||||||||||||||||||
25
Table of Contents
Summary Historical and Pro Forma Condensed Consolidated Financial and Other Data
The following tables present the summary historical consolidated financial and other data for GoHealth Holdings, LLC and its subsidiaries and the summary pro forma condensed consolidated financial and other data for GoHealth, Inc. GoHealth Holdings, LLC is the predecessor of GoHealth, Inc. for financial reporting purposes. The summary consolidated statements of operations data and statements of cash flows data for the period from September 13, 2019 through December 31, 2019 (Successor), the period from January 1, 2019 through September 12, 2019 (Predecessor) and the year ended December 31, 2018 (Predecessor), and the summary consolidated balance sheet data as of December 31, 2019 are derived from the audited consolidated financial statements of GoHealth Holdings, LLC included elsewhere in this prospectus. The summary condensed consolidated statements of operations data and statements of cash flows data for the three months ended March 31, 2020 and 2019, and the summary condensed consolidated balance sheet data as of March 31, 2020, are derived from the unaudited condensed consolidated financial statements of GoHealth Holdings, LLC included elsewhere in this prospectus. The results of operations for the periods presented below are not necessarily indicative of the results to be expected for any future period. The information set forth below should be read together with the “Selected Historical Condensed Consolidated Financial Data,” “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and the consolidated financial statements and the accompanying notes included elsewhere in this prospectus.
The summary unaudited pro forma condensed consolidated financial data of GoHealth, Inc. presented below have been derived from our unaudited pro forma condensed consolidated financial information included elsewhere in this prospectus. The summary unaudited pro forma condensed consolidated financial information as of and for the three months ended March 31, 2020, and for the Successor 2019 Period and Predecessor 2019 Period gives effect to the Centerbridge Acquisition and the Transactions, including the consummation of this offering and the use of proceeds therefrom, as described in “Our Organizational Structure” and “Use of Proceeds,” as if all such transactions had occurred on January 1, 2019 in the case of the unaudited pro forma condensed consolidated statements of operations data, and as of March 31, 2020, in the case of the unaudited pro forma condensed consolidated balance sheet data. The unaudited pro forma condensed consolidated financial information includes various estimates which are subject to material change and may not be indicative of what our operations or financial position would have been had this offering and related transactions taken place on the dates indicated, or that may be expected to occur in the future. See “Unaudited Pro Forma Condensed Consolidated Financial Information” for a complete description of the adjustments and assumptions underlying the summary unaudited pro forma condensed consolidated financial information.
26
Table of Contents
The summary historical consolidated financial and other data of GoHealth, Inc. has not been presented because GoHealth, Inc. is a newly incorporated entity, has had no business transactions or activities to date and had no assets or liabilities during the periods presented in this section.
| Pro Forma GoHealth, Inc. |
Historical GoHealth Holdings, LLC | |||||||||||||||||||||||||||
| Three Months Ended March 31, 2020 |
Year Ended December 31, 2019 |
Three Months Ended March 31, |
Successor 2019 Period |
Predecessor 2019 Period |
Year Ended December 31, 2018 (Predecessor) |
|||||||||||||||||||||||
| (in thousands, except per share data) | 2020 (Successor) |
2019 (Predecessor) |
||||||||||||||||||||||||||
| Consolidated Statement of Operations: |
||||||||||||||||||||||||||||
| Net revenues: |
||||||||||||||||||||||||||||
| Commission |
$ | $ | $ | 112,510 | $ | 51,215 | $ | 243,347 | $ | 175,834 | $ | 144,378 | ||||||||||||||||
| Other |
28,500 | 17,874 | 65,144 | 55,176 | 81,827 | |||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Net revenues |
141,010 | 69,089 | 308,491 | 231,010 | 226,205 | |||||||||||||||||||||||
| Operating expenses: |
||||||||||||||||||||||||||||
| Cost of revenue |
42,134 | 27,552 | 90,384 | 79,169 | 79,582 | |||||||||||||||||||||||
| Marketing and advertising |
26,073 | 11,411 | 24,811 | 37,769 | 28,129 | |||||||||||||||||||||||
| Customer care and enrollment |
23,978 | 13,939 | 44,356 | 49,149 | 46,076 | |||||||||||||||||||||||
| Technology |
4,593 | 4,155 | 6,006 | 40,312 | 16,197 | |||||||||||||||||||||||
| General and administrative |
10,491 | 6,990 | 13,674 | 79,219 | 27,458 | |||||||||||||||||||||||
| Change in fair value of contingent consideration liability |
4,400 | — | 70,700 | — | — | |||||||||||||||||||||||
| Amortization of intangible assets |
23,514 | — | 28,217 | — | — | |||||||||||||||||||||||
| Transaction costs |
— | — | 6,245 | 2,267 | — | |||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Total operating expenses |
135,183 | 64,047 | 284,393 | 287,885 | 197,442 | |||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Income (loss) from operations |
5,827 | 5,042 | 24,098 | (56,875 | ) | 28,763 | ||||||||||||||||||||||
| Interest expense |
6,756 | 28 | 8,076 | 140 | 224 | |||||||||||||||||||||||
| Other income (expense) |
10 | 10 | 17 | (114 | ) | (379 | ) | |||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Income (loss) before income taxes |
(939 | ) | 5,004 | 16,039 | (57,129 | ) | 28,160 | |||||||||||||||||||||
| Income tax expense (benefit) |
(2 | ) | 2 | 44 | (66 | ) | 46 | |||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Net income (loss) |
$ | $ | $ | (937 | ) | $ | 5,002 | $ | 15,995 | $ | (57,063 | ) | $ | 28,114 | ||||||||||||||
| Less: Net loss attributable to non-controlling interests |
— | — | — | — | (3 | ) | ||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Net income (loss) attributable to GoHealth Holdings, LLC and subsidiaries |
$ | $ | $ | (937 | ) | $ | 5,002 | $ | 15,995 | $ | (57,063 | ) | $ | 28,117 | ||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Pro Forma Net Loss per Share Data: |
||||||||||||||||||||||||||||
| Pro forma weighted average shares of Class A common stock outstanding: |
||||||||||||||||||||||||||||
| Basic |
||||||||||||||||||||||||||||
| Diluted |
||||||||||||||||||||||||||||
| Pro forma net loss available to Class A common stock per share: |
||||||||||||||||||||||||||||
| Basic |
$ | $ | ||||||||||||||||||||||||||
| Diluted |
$ | $ | ||||||||||||||||||||||||||
| Consolidated Statement of Cash Flows Data: |
||||||||||||||||||||||||||||
| Net cash (used in) provided by operating activities |
$ | 23,587 | $ | 1,222 | $ | (9,284 | ) | $ | 9,281 | $ | 5,443 | |||||||||||||||||
| Net cash used in investing activities |
(3,522 | ) | (1,944 | ) | (810,010 | ) | (5,597 | ) | (6,170 | ) | ||||||||||||||||||
| Net cash provided by (used in) financing activities |
120,167 | 1,147 | 830,879 | (3,449 | ) | 63 | ||||||||||||||||||||||
27
Table of Contents
| Pro Forma GoHealth, Inc. |
Historical GoHealth Holdings, LLC |
|||||||||||
| (in thousands) | March 31, 2020 |
March 31, 2020 (Successor) |
December 31, 2019 (Predecessor) |
|||||||||
| Consolidated Balance Sheet: |
||||||||||||
| Cash and cash equivalents |
$ | $ | 152,423 | $ | 12,276 | |||||||
| Total assets |
1,709,649 | 1,602,295 | ||||||||||
| Total liabilities |
840,047 | 742,151 | ||||||||||
| Total members’ equity |
869,602 | 860,144 | ||||||||||
| Pro Forma GoHealth, Inc. |
||||||||||||||||||||||||||||
| (in thousands, except percentages) | Three Months Ended March 31, 2020 |
Year Ended December 31, 2019 (1) |
Three Months Ended March 31, |
Successor 2019 Period |
Predecessor 2019 Period |
Year Ended December 31, 2018 (Predecessor) |
||||||||||||||||||||||
| 2020 (Successor) |
2019 (Predecessor) |
|||||||||||||||||||||||||||
| Selected Non-GAAP Financial Data: |
||||||||||||||||||||||||||||
| EBITDA(2) |
$ | $ | 96,474 | $ | 29,965 | $ | 6,569 | $ | 52,853 | $ | (52,742 | ) | $ | 34,544 | ||||||||||||||
| Adjusted EBITDA(2) |
$ | $ | 169,994 | $ | 34,921 | $ | 7,135 | $ | 130,465 | $ | 39,973 | $ | 34,863 | |||||||||||||||
| Adjusted EBITDA margin(2) |
% | 31.5 | % | 24.8 | % | 10.3 | % | 42.3 | % | 17.3 | % | 15.4 | % | |||||||||||||||
| Three Months Ended March 31, |
Year Ended December 31, 2019 |
Successor 2019 Period |
Predecessor 2019 Period |
Year Ended December 31, 2018 (Predecessor) |
||||||||||||||||||||
| 2020 | 2019 | |||||||||||||||||||||||
| Other Operating Data(3): |
||||||||||||||||||||||||
| LTV/CAC (Medicare—Internal segment) |
2.7x | 1.7x | 3.8x | 5.1x | 2.7x | 2.7x | ||||||||||||||||||
| Cost per Qualified Prospect (Medicare—Internal segment) |
$ | 57 | $ | 87 | $ | 63 | $ | 53 | $ | 77 | $ | 48 | ||||||||||||
| Total Medicare Submitted Policies |
132,014 | 43,283 | 427,697 | 268,882 | 158,815 | 118,376 | ||||||||||||||||||
| Medicare—Internal Commissionable Approved Submissions |
86,604 | 22,114 | 265,584 | 170,764 | 94,820 | 57,744 | ||||||||||||||||||
| Medicare—External Commissionable Approved Submissions |
34,326 | 20,319 | 120,676 | 62,673 | 58,003 | 57,947 | ||||||||||||||||||
| LTV Per Approved Submission—Medicare Advantage (Medicare segments) |
$ | 857 | $ | 860 | $ | 978 | $ | 1,024 | $ | 906 | $ | 936 | ||||||||||||
| LTV Per Approved Submission—Medicare Supplement (Medicare segments) |
$ | 920 | $ | 926 | $ | 957 | $ | 944 | $ | 964 | $ | 798 | ||||||||||||
| LTV Per Approved Submission—Prescription Drug Plans (Medicare segments) |
$ | 215 | $ | 191 | $ | 206 | $ | 213 | $ | 194 | $ | 190 | ||||||||||||
| Total Submitted Policies (IFP and Other segments) |
38,002 | 53,886 | 296,772 | 146,228 | 150,544 | 207,695 | ||||||||||||||||||
| (1) | The financial information presented for the Pro Forma Fiscal Year 2019 give effect to the Centerbridge Acquisition, but does not give effect to the adjustments for the Transactions, including adjustments related to this offering and the other adjustments described in the section titled “Unaudited Pro Forma Condensed Consolidated Financial Information.” Such adjustments will be included in a subsequent filing based on the actual initial public offering price, the number of shares sold in this offering, and other terms of this offering determined at pricing. |
| (2) | We use supplemental measures of our performance that are derived from our consolidated financial information, but which are not presented in our consolidated financial statements prepared in accordance with GAAP. These non-GAAP financial measures include net income (loss) before interest expense, income |
28
Table of Contents
| tax expense (benefit) and depreciation and amortization expense, or EBITDA; Adjusted EBITDA and Adjusted EBITDA margin. Adjusted EBITDA is the primary financial performance measure used by management to evaluate its business and monitor its results of operations. |
Adjusted EBITDA represents EBITDA as further adjusted for share-based compensation, change in fair value of earnout liability, Centerbridge Acquisition costs and severance costs.
Adjusted EBITDA margin represents Adjusted EBITDA divided by net revenues.
We use non-GAAP financial measures to supplement financial information presented on a GAAP basis. We believe that excluding certain items from our GAAP results allows management to better understand our consolidated financial performance from period to period and better project our future consolidated financial performance as forecasts are developed at a level of detail different from that used to prepare GAAP-based financial measures. Moreover, we believe these non-GAAP financial measures provide our stakeholders with useful information to help them evaluate our operating results by facilitating an enhanced understanding of our operating performance and enabling them to make more meaningful period to period comparisons. There are limitations to the use of the non-GAAP financial measures presented in this prospectus. For example, our non-GAAP financial measures may not be comparable to similarly titled measures of other companies. Other companies, including companies in our industry, may calculate non-GAAP financial measures differently than we do, limiting the usefulness of those measures for comparative purposes.
The non-GAAP financial measures are not meant to be considered as indicators of performance in isolation from or as a substitute for net income (loss) prepared in accordance with GAAP, and should be read only in conjunction with financial information presented on a GAAP basis. Reconciliations of each of EBITDA and Adjusted EBITDA to its most directly comparable GAAP financial measure, net income (loss), are presented below. We encourage you to review the reconciliations in conjunction with the presentation of the non-GAAP financial measures for each of the periods presented. In future periods, we may exclude such items, may incur income and expenses similar to these excluded items and include other expenses, costs and non-recurring items. The tables below provide reconciliations of EBITDA and Adjusted EBITDA to net income (loss) on a consolidated basis for the periods indicated.
29
Table of Contents
EBITDA and Adjusted EBITDA:
| Pro Forma GoHealth, Inc. | ||||||||||||||||||||||||||||
| Three Months Ended March 31, 2020 |
Year Ended December 31, 2019 |
Three Months Ended March 31, |
Successor 2019 Period |
Predecessor 2019 Period |
Year Ended December 31, 2018 (Predecessor) |
|||||||||||||||||||||||
| (in thousands) | 2020 (Successor) |
2019 (Predecessor) |
||||||||||||||||||||||||||
| Net income (loss) |
$ | $ | (29,501 | ) | $ | (937 | ) | $ | 5,002 | $ | 15,995 | $ | (57,063 | ) | $ | 28,114 | ||||||||||||
| Interest expense |
27,172 | 6,756 | 28 | 8,076 | 140 | 224 | ||||||||||||||||||||||
| Income tax expense (benefit) |
(22 | ) | (2 | ) | 2 | 44 | (66 | ) | 46 | |||||||||||||||||||
| Depreciation and amortization expense |
98,825 | 24,147 | 1,538 | 28,738 | 4,247 | 6,160 | ||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| EBITDA |
96,474 | 29,965 | 6,569 | 52,853 | (52,742 | ) | 34,544 | |||||||||||||||||||||
| Share-based compensation(a) |
1,853 | 479 | — | 448 | 87,060 | — | ||||||||||||||||||||||
| Change in fair value of contingent consideration liability(b) |
70,700 | 4,400 | — | 70,700 | — | — | ||||||||||||||||||||||
| Centerbridge Acquisition costs(c) |
— | — | — | 6,245 | 4,908 | — | ||||||||||||||||||||||
| Severance costs(d) |
966 | 77 | 566 | 219 | 747 | 319 | ||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Adjusted EBITDA |
$ | $ | 169,994 | $ | 34,921 | $ | 7,135 | $ | 130,465 | $ | 39,973 | $ | 34,863 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| (a) | Represents non-cash share-based compensation expense in connection with profits interests and incentive share units. Share-based compensation expense for the Predecessor 2019 Period is fully attributable to the automatic acceleration of legacy profits interests and legacy incentive share units in connection with the Centerbridge Acquisition and is allocated to the marketing and advertising, technology and general and administrative line items in the income statement based on the department of the individual who received the compensation. |
| (b) | Represents the fair value of the earnout liability due to the predecessor owners of the Company arising from the Centerbridge Acquisition. Prior to the consummation of this offering, we intend to update the disclosure as necessary for the resolution of the earnout liability. |
| (c) | Represents legal, accounting, consulting, and other costs related to the Centerbridge Acquisition. |
| (d) | Represents costs associated with the termination of employment. |
| (3) | For definitions and further information about how we calculate other operating data, please see “Management’s Discussion and Analysis of Financial Condition and Results of Operations—Key Business and Operating Metrics by Segment.” |
30
Table of Contents
Investing in our Class A common stock involves a high degree of risk. You should carefully consider the risks and uncertainties described below, together with all of the other information in this prospectus, including our consolidated financial statements and the related notes, before deciding to invest in our Class A common stock. The occurrence of any of the events described below could harm our business, operating results and financial condition. In such an event, the market price of our Class A common stock could decline, and you may lose all or part of your investment. Additional risks and uncertainties not presently known to us or that we currently deem immaterial may also impair our business. See “Cautionary Note Regarding Forward-Looking Statements.”
Risks Related to Our Business
The marketing and sale of Medicare plans are subject to numerous, complex and frequently changing laws, regulations and guidelines, and non-compliance with or changes in laws, regulations and guidelines could harm our business, operating results and financial condition.
Our business and operating results are heavily dependent on marketing and selling Medicare plans. The marketing and sale of Medicare Advantage and Medicare Part D prescription drug plans are principally regulated by CMS, but are also subject to state laws. The marketing and sale of Medicare Supplement plans are principally regulated on a state-by-state basis by state departments of insurance or equivalent state departments. The laws and regulations applicable to the marketing and sale of Medicare plans are numerous, ambiguous and complex, and, particularly with respect to regulations and guidance issued by CMS for Medicare Advantage and Medicare Part D prescription drug plans are frequently changing. We have and will continue to take steps to ensure compliance with laws, regulations and guidelines applicable to the sale and marketing of Medicare plans. For example, we have tailored our websites and sales processes for Medicare plans to comply with several requirements that are solely applicable to the sale and marketing of Medicare-related health insurance plans. Many aspects of our online platforms and our marketing material and processes, as well as changes to these platforms, materials and processes, including call center scripts, must be filed with CMS and reviewed and approved by carriers in light of CMS requirements. In addition, certain aspects of our Medicare plan marketing partner relationships have been in the past, and will be in the future, subjected to CMS review and carrier review. Changes to the laws, regulations and guidelines relating to the sale and marketing of Medicare plans, their interpretation or the manner in which they are enforced could be incompatible with these relationships, the manner in which we conduct our business, our platforms or our sale of Medicare plans, which could harm our business, operating results and financial condition.
CMS scrutinizes Medicare carriers and Medicare carriers may be held responsible for actions that we and our agents take. As a result, carriers may terminate their relationship with us or take other corrective action against us if our Medicare product sales, marketing or operations are not in compliance with Medicare or other requirements or give rise to too many complaints. See “—Our business may be harmed if we lose our relationship with carriers or if our relationships with carriers change, particularly if we or our contracted carriers temporarily or permanently lose the ability to market and sell Medicare plans.”
Due to potential changes in CMS guidance, enforcement, interpretation or, in light of the COVID-19 pandemic, waivers, of existing laws, regulations and guidance applicable to our marketing and sale of Medicare products, or as a result of new laws, regulations and guidelines, CMS, state departments of insurance or carriers may object to or not approve aspects of our online platforms or marketing materials and processes and determine that certain existing aspects of our Medicare-related business are not in compliance with the applicable laws, regulations and guidance. As a result, the progress of our Medicare operations could be slowed or we could be prevented from operating aspects of our Medicare revenue generating activities altogether, which would harm our business, operating results and financial condition, particularly if it occurred during the Medicare annual enrollment period.
31
Table of Contents
Our business may be harmed if we lose our relationship with carriers or if our relationships with carriers change, particularly if we or our contracted carriers temporarily or permanently lose the ability to market and sell Medicare plans.
Our contractual relationships with carriers, including those with whom we have carrier-branded sales arrangements, are typically non-exclusive and terminable on short notice by either party for any reason. Carriers may be unwilling to allow us to sell their insurance products for a variety of reasons, including competitive or regulatory reasons, dissatisfaction with the insureds that we place with them or because they do not want to be associated with our brand. Additionally, in the future, an increasing number of carriers may decide to rely on their own internal distribution channels, including traditional in-house agents and their own websites, to sell their own products, which could limit or prohibit us from distributing their products. Also, because we do not have exclusive relationships with carriers, carriers can and do use our competitors to sell their products.
If a carrier is not satisfied with our services, it could cause us to incur additional costs and impact our profitability. For example, a carrier could terminate our services, decrease our commissions going forward or restrict our ability to market their products. Moreover, if we fail to meet our contractual obligations to any of our carriers, we could be subject to legal liability or lose our carrier relationships. In addition, these claims against us may produce negative publicity that could hurt our reputation and business and adversely affect our ability to retain business, find new consumers to sell products to or secure new business with other carriers.
In addition, with respect to the plans we sell in the IFP and Other segments and Medicare Supplement plans, carriers periodically change the criteria they use for determining whether they are willing to insure individuals. Future changes in carrier underwriting criteria could negatively impact sales of, or the renewal or approval rates of, insurance policies on our platform, which could negatively impact our revenue.
We may decide to terminate our relationship with a carrier for a number of reasons and the termination of our relationship with a carrier could reduce the variety of insurance products we distribute. In connection with such a termination, we would lose a source of commissions for future sales, and, in a limited number of cases, future commissions for past sales. Our business could also be harmed if we fail to develop new carrier relationships or offer customers a wide variety of insurance products.
We may also lose the ability to market and sell Medicare plans for one or more Medicare carriers. The regulations for selling Medicare health insurance are complex and can change frequently and may change in response to the COVID-19 pandemic. If we, our agents, or a carrier violate any of the requirements imposed by CMS, or federal or state laws or regulations, a carrier may terminate our relationship, or CMS may penalize a carrier by suspending, limiting, or terminating that carrier’s ability to market and sell Medicare plans. Moreover, if any of our carriers terminate its relationship with us for cause, we may have to disclose such termination to other carriers, which may result in termination of additional carrier relationships. Because the Medicare products we sell are sourced from a relatively small number of carriers, if we lose the ability to market one of those carrier’s Medicare plans, even temporarily, or if one of those carriers loses its Medicare product membership, our business, operating results and financial condition could be harmed.
Our failure to grow our customer base or retain our existing customers could adversely impact our business, operating results and financial condition.
We receive commissions from carriers for health insurance plans sold through us. When one of these plans is canceled, or if we otherwise do not remain the agent on the plan, we no longer receive the related commission payment and do not receive any commissions from renewals. Our customers may choose to discontinue their health insurance plans for a variety of reasons. Any decrease in the amount of time we retain our customers could adversely impact the estimated LTV we use for purposes of recognizing revenue. See “—Our operating results may be adversely impacted by factors that impact our estimate of LTV.” Moreover, if we are not able to successfully retain existing customers and limit health insurance plan turnover, our cash flows from operations will be adversely impacted and our business, operating results and financial condition would be harmed.
32
Table of Contents
In addition, in certain circumstances, the Medicare-related commission rates that we receive may be higher in the first calendar year of a plan if the plan is the first Medicare Advantage plan issued to the customer. Similarly, the individual and family plans commission rates that we receive are typically higher in the first twelve months of a policy. After the first twelve months, they generally decline significantly. As a result, if we do not add a sufficient number of customers to new plans, our business, operating results and financial condition would be harmed.
Our business primarily generates revenue through the sale of Medicare Advantage plans. In some instances, traditional Medicare may be more attractive than Medicare Advantage because, for example, potential provider network restrictions imposed by Medicare Advantage plans do not exist in traditional Medicare, allowing patients with traditional Medicare to visit any doctor that accepts Medicare. In those instances, consumers may opt not to purchase a Medicare Advantage plan from us.
In general, the growth in our customer base is highly dependent upon our success in attracting new customers during the Medicare annual enrollment period. In 2019, approximately 61% of our Medicare Advantage and Medicare Supplement policies were submitted during the three months ended December 31, 2019. If our ability to market and sell Medicare-related health insurance and individual and family plans is constrained during an enrollment period for any reason, such as technology failures, reduced allocation of resources, any inability to timely employ, license, train, certify and retain our employees and our contractors and their agents to sell plans, interruptions in the operation of our website or systems, disruptions caused by other external factors, such as the COVID-19 pandemic, or issues with government-run health insurance exchanges, we could acquire fewer customers or suffer a reduction in our existing customer base and our business, operating results and financial condition could be harmed.
Carriers may reduce the commissions paid to us and change their underwriting practices in ways that reduce the number of, or impact the renewal or approval rates of, insurance policies sold through our platform, which could harm our business, operating results and financial condition.
Our commission rates from carriers are either set by each carrier or negotiated between us and each carrier. The commission rates we are paid are, for any given plan for a given customer, based on a number factors, including the carriers offering those plans, the state of residence of customers, the laws and regulations in the jurisdictions where the customer is located, and the customer’s previous Medicare enrollment history (if any). Carriers have the right to alter these commission rates with relatively short notice and have altered, and may in the future alter, the contractual relationships we have with them, including, in certain instances by unilateral amendment of our contracts relating to commission rates or otherwise. For example, CMS could reduce the amount paid by CMS to Medicare Advantage plans or change the regulations and/or timelines applicable to the Medicare Advantage program, particularly in response to the COVID-19 pandemic, which could result in decreased commission rates or reduce carrier participation in the Medicare Advantage program. Changes of this nature could result in reduced commissions, or could impact our relationship with such carriers and potentially lead to contract termination. Because revenue in the Medicare segments is concentrated in a relatively small number of carriers, we are particularly vulnerable to changes in commission rates and changes in the competitiveness of our carriers’ Medicare products.
Significant consolidation in the health insurance industry could adversely alter our relationships with carriers and harm our business, operating results and financial condition.
The health insurance industry in the United States has experienced a substantial amount of consolidation, resulting in a decrease in the number of carriers. Consolidation in the health insurance industry, particularly involving one of our key carriers, could cause a loss of, or changes in, our relationship with that carrier and may reduce our commission or other revenue from that carrier. In the future, due to this consolidation, we may be forced to offer health insurance from a reduced number of carriers or to derive a greater portion of our revenue from a more concentrated number of carriers as our business and the health insurance industry evolve. Additionally, mergers among carriers or an acquisition of one carrier by another carrier may trigger changes to
33
Table of Contents
our agreements with such carriers. For example, carriers may unilaterally amend or terminate our agreements on short notice, which could adversely impact or terminate the commission payments that we receive from these carriers. Our revenue could be adversely impacted if we are unable to maintain currently existing levels of business with any of our significant carriers if we are unable to offset any loss of business with alternative carriers. We expect that a small number of carriers will account for a significant portion of our revenue for the foreseeable future and any impairment of our relationship with, or the material financial impairment of, these carriers could adversely affect our business, operating results and financial condition. See “—We currently depend on a small group of carriers for a substantial portion of our revenue.”
Information technology system failures could interrupt our operations and have a material adverse effect on our business, financial condition and results of operations.
Our ability to sell insurance is dependent upon our information technology systems. In connection with sales of Medicare plans, CMS rules require that our health insurance agent employees utilize CMS-approved scripts and that we record and maintain the recording of telephonic interactions. We rely on telephone, call recording, customer relationship management and other systems and technology in our sales operations to sell Medicare plans, and we are dependent upon third parties for some of these systems and technologies, including our telephone services, which are provided by Five9, call recording systems and other communications systems. Carriers often audit these recordings for compliance purposes and listen to them in connection with investigating complaints. We have had in the past, and may in the future, experience failures of certain of our systems, including our telephone and call recording systems. For example, we have experienced failures of our systems due to power outages, which have negatively impacted our ability to sell plans. The effectiveness and stability of our systems and technology are critical to our ability to sell Medicare plans, particularly during the Medicare enrollment periods and the failure or interruption of any of these systems and technologies or any inability to handle increased business volume may have a material adverse effect on our business, operating results and financial condition and subject us to litigation or to actions by regulatory authorities.
Our operating results may be adversely impacted by factors that impact our estimate of LTV.
As a result of the adoption of Accounting Standards Codification, or ASC, 606, Revenue from Contracts with Customers, we recognize revenue at the time a Submitted Policy becomes an Approved Policy by applying the latest estimated LTV for that product. We estimate commission revenue for each product by using a portfolio approach to a group of approved customers that are organized based on a variety of attributes, which we refer to as “cohorts.” We estimate the cash commissions we expect to collect for each approved customer cohort by evaluating various factors, including, but not limited to, commission rates, carriers, estimated average plan duration, the regulatory environment, and historic cancellations of health insurance plans offered by carriers with which we have a relationship. On a quarterly basis, we recompute LTV at a cohort level for all outstanding cohorts, review and monitor changes in the data used to estimate LTV as well as the cash received for each cohort as compared to our original estimates. The fluctuations of cash received for each cohort and LTV may be significant and may or may not be indicative of the need to adjust LTVs for prior period cohorts. Management analyzes these fluctuations and, to the extent we see changes in our estimates of the cash commission collections that we believe are indicative of an increase or decrease to prior period LTVs, we will adjust LTVs for the affected cohorts at the time such determination is made. Changes in LTV may result in an increase or a decrease to revenue and a corresponding increase or decrease to commissions receivable, accordingly. We refer to the net commission revenue from customers approved in prior periods as “adjustment revenue” and our revenue can fluctuate significantly from period to period as a result of adjustment revenue.
As we continue to evaluate our LTV estimation models, we may in the future make further changes based on a number of factors and such changes could result in significant increases or decreases in revenue. LTVs are estimates and are based on a number of assumptions, which include, but are not limited to, estimates of the conversion rates of commissionable Approved Submissions into customers, forecasted average plan duration and forecasted commission rates we expect to receive per approved customer’s plan. These assumptions are based on
34
Table of Contents
historical trends and require significant judgment by our management in interpreting those trends. Changes in our historical trends will result in changes to our LTV estimates in future periods and, therefore, could adversely affect our revenue and financial results in those future periods. As a result, negative changes in the factors upon which we estimate LTVs, such as reduced conversion of commissionable Approved Submissions to customers, increased health insurance plan termination or a reduction in the lifetime commission amounts we expect to receive for selling the plan to a customer or other changes could harm our business, operating results and financial condition. In addition, if we ultimately receive commission payments that are less than the amount we estimated when we recognized commission revenues, we would need to write off the remaining commissions receivable balance, which could materially adversely impact our operating results and financial condition.
The forecasted average plan duration is another important factor in our estimation of LTV. We receive commissions from carriers for policies sold through us that go on to become customers of those carriers. When one of these plans is canceled, or if we otherwise do not remain the agent on the policy, we no longer receive the related commission payment. Our forecasted average plan duration and health insurance plan termination rates are calculated based on our historical data by plan type and for certain products, such as our Medicare Advantage products which constitute the majority of our revenue, and if we are unable to produce an accurate forecasted average plan duration, our business, operating results and financial condition may be adversely impacted.
Additionally, from time to time, carriers may stop offering products in a geographic area. While in many cases, carriers will still support existing customers in those geographic areas, because they are no longer offering new plans, the retention of those customers may be adversely impacted, thereby impacting our expected LTV.
Commission rates are also a factor in estimating our LTVs, which are impacted by a variety of factors, including the particular health insurance plans chosen by our customers, the carriers offering those plans, our customers’ states of residence, the laws and regulations in those jurisdictions, the average premiums of plans purchased through us and healthcare reform. Any reduction in our average commission revenue per customer could harm our business, operating results and financial condition.
System failures or capacity constraints could harm our business, financial condition and operating results.
The performance, reliability and availability of our technology platform and underlying network infrastructures are critical to our financial results, our brand and our relationship with customers, marketing partners and carriers. Although we regularly attempt to enhance our technology platform and system infrastructure, system failures and interruptions may occur if we are unsuccessful in these efforts, if we are unable to accurately project the rate or timing of increases in our website traffic or inbound call volume or for other reasons, some of which are completely outside our control. Additionally, we are also reliant on the systems of our carriers to submit plan enrollment applications from potential customers. We have in the past, and could in the future, experience significant failures and interruptions of our systems and the systems of our carriers, which would harm our business, operating results and financial condition. If these failures or interruptions occurred during the Medicare annual enrollment period or during the open enrollment period under healthcare reform, the negative impact on us would be particularly pronounced.
We rely in part upon third-party vendors, including data center and bandwidth providers, to operate our technology platform. We cannot predict whether additional network capacity will be available from these vendors as we need it, and our network or our suppliers’ networks might be unable to achieve or maintain a sufficiently high capacity of data transmission to allow us to process health insurance applications in a timely manner or effectively download data, especially if our website traffic increases. For example, a rapid expansion of our business could affect the service levels at our data centers or cause such data centers and systems to fail. Any system failure or service level reduction that causes an interruption to, or decreases the responsiveness of, our services would impair our revenue-generating capabilities and damage our reputation. In addition, any loss of data could result in loss of customers and subject us to potential liability. Our databases and systems are vulnerable to damage or interruption from human error, fire, floods, power loss, telecommunications failures,
35
Table of Contents
physical or electronic break-ins, computer viruses, acts of terrorism, other attempts to harm our systems and similar events. In addition, our operations are vulnerable to earthquakes, fires, severe weather, pandemics and other natural disasters in Illinois, North Carolina, Utah, Honduras, Slovakia and other parts of the world where we, our agents and vendors operate.
The owners of our data center facilities and our other third-party vendors have no obligation to renew their agreements with us on commercially reasonable terms, or at all. If we are unable to renew these agreements on commercially reasonable terms, or if one of our data center operators is acquired, we may be required to transfer our servers and other infrastructure to new data center facilities, and we may incur significant costs and possible service interruption in connection with doing so. Problems faced by our third-party data center locations with the telecommunications network providers with whom we or they contract, or with the systems by which our telecommunications providers allocate capacity among their clients, including us, could adversely affect the experience of our clients and consumers. Our third-party data center operators could decide to close their facilities without adequate notice. In addition, any financial difficulties, such as bankruptcy faced by our third-party data centers, operators or any of the service providers with whom we or they contract may have negative effects on our business, the nature and extent of which are difficult to predict.
Our ability to sell Medicare-related health insurance plans is largely dependent on our licensed health insurance agents.
The success of our operations is largely dependent on our licensed health insurance agents, upon whom we rely to sell insurance. In order to sell Medicare-related health insurance plans, agents must be licensed by the states in which they are selling plans and certified and appointed with the carrier that offers the plans in each applicable state. Because a significant number of Medicare plans are sold in the fourth quarter each year during the Medicare annual enrollment period, we retain and train a significant number of additional employees in a limited period of time. We must also ensure that our agents are timely licensed in a significant number of states and certified and appointed with the carriers whose products we sell. We depend upon our employees, state departments of insurance and carriers for the licensing, certification and appointment of our agents. We may not be successful in timely hiring or sourcing a sufficient number of additional agents or other employees needed to operate our business. Even if we are successful in hiring or sourcing a sufficient number of agents, we may experience temporary shortages of agents due to illness, poor weather conditions or other natural disasters, personal emergencies and other events outside our control. See “—The extent to which the COVID-19 outbreak and measures taken in response thereto impact our business, results of operations and financial condition will depend on future developments, which are highly uncertain and cannot be predicted.”
We have recently implemented a work from home program for our agents, partly in response to the effects from the COVID-19 pandemic. It may be more difficult for us to manage and monitor our agents in remote settings and we may have to expend more management time and incur more costs to do so. Agents may also face additional distractions working from home that may prevent them from efficiently selling plans. If our agents are not able to effectively work from home, we may not be able to sell as many plans, which would negatively impact our business, financial condition and results of operations.
Our success in recruiting highly skilled and qualified agents can depend on factors outside of our control, including the strength of the general economy and local employment markets and the availability of alternative forms of employment. During periods when we are unable to recruit high-performing agents, we tend to experience higher turnover rates. The productivity of our agents is influenced by their average tenure. Without qualified individuals to serve in customer facing roles, we may produce less commission revenue, which could have a material adverse effect on our business, operating results and financial condition.
36
Table of Contents
Changes and developments in the health insurance system and laws and regulations governing the health insurance markets in the United States could materially adversely affect our business, operating results, financial condition and qualified prospects.
Our business depends upon the public and private sector of the U.S. insurance system, which is subject to a changing regulatory environment. Accordingly, the future financial performance of our business will depend in part on our ability to adapt to regulatory developments, including changes in laws and regulations or changes to interpretations of such laws or regulations, especially laws and regulations governing Medicare. For example, in March 2010, the ACA became law. The ACA substantially changed the way healthcare is financed by both commercial and government payers and contains a number of provisions that impact our business and operations, including the expansion of Medicaid eligibility to additional categories of individuals. Since its enactment, there have been judicial and Congressional challenges to certain aspects of the ACA, and we expect there will be additional challenges and amendments to the ACA in the future. On December 14, 2018, a Texas U.S. District Court Judge ruled that the ACA is unconstitutional in its entirety because the “individual mandate” was repealed by Congress as part of the Tax Cuts and Jobs Act. On December 18, 2019, the U.S. Court of Appeals for the 5th Circuit ruled that the individual mandate was unconstitutional and remanded the case back to the District Court to determine whether the remaining provisions of the ACA are invalid as well. On March 2, 2020, the U.S. Supreme Court granted the petitions for writs of certiorari to review the case, although it is unclear when a decision will be made or how the Supreme Court will rule.
Additionally, ongoing health reform efforts and measures may expand the role of government-sponsored coverage, including single payer or so called “Medicare-for-All” proposals, which could have far-reaching implications for the insurance industry if enacted. Some proposals would seek to eliminate the private marketplace, whereas others would expand a government-sponsored option to a larger population. We are unable to predict the full impact of healthcare reform initiatives on our operations in light of the uncertainty of whether initiatives will be successful and the uncertainty regarding the terms and timing of any provisions enacted and the impact of any of those provisions on various healthcare and insurance industry participants. In particular, because our platform provides customers with a venue to shop for insurance policies from a curated panel of the nation’s leading carriers, the expansion of government-sponsored coverage through “Medicare-for-All” or the implantation of a single payer system may materially and adversely impact our business, operating results, financial condition and prospects. We expect there will be continuing efforts to challenge, repeal, or replace the ACA, which may have a material impact on our business by eliminating Medicaid eligibility for certain patients and reducing the size of the SNP-eligible population.
Changes in laws, regulations and guidelines governing health insurance may also be incompatible with various aspects of our business and require that we make significant modifications to our existing technology or practices, which may be costly and time-consuming to implement and could also harm our business, operating results and financial condition.
We have received, and may in the future receive, inquiries from regulators regarding our marketing and business practices and compliance with laws and regulations. We may be required to modify our practices in connection with the inquiries. Failure to adequately respond to such inquiries could result in adverse regulatory action that could harm our business, operating results and financial condition. See “—The marketing and sale of Medicare plans are subject to numerous, complex and frequently changing laws, regulations and guidelines, and non-compliance with or changes in laws, regulations and guidelines could harm our business, operating results and financial condition.”
Additionally, some carriers provide us with marketing development funds, consistent with CMS regulations. If regulatory developments limit or remove the ability for carriers to compensate us through these funds, or the government determines that our arrangements do not meet the regulatory requirements, the compensation we receive from carriers would decline, which would materially and adversely impact our business, operating results and financial condition.
37
Table of Contents
Various aspects of healthcare reform could also cause carriers to discontinue certain health insurance products or prohibit us from distributing certain health insurance products in particular jurisdictions. Our business, operating results, financial condition and prospects may be materially and adversely affected if we are unable to adapt to developments in healthcare reform in the United States.
Our business could be harmed if we are unable to effectively advertise our products on a cost-effective basis or market the availability of our products through specific channels.
We use the Internet, television, radio, mail, e-mail and the telephone, among other channels, to market our services and to communicate with qualified prospects or our existing customers. Some of our competitors have greater financial resources, which enable them to purchase significantly more advertising than we are able to purchase. Further, the cost of marketing and advertising may fluctuate significantly based on demand. If the cost of marketing and advertising increases for any reason, we may not be able to purchase as many advertisements as we typically would or would have to incur greater costs to do so. For example, we expect a significant increase in the demand for television and radio advertisements as we approach the U.S. presidential election in November 2020. The election coincides with the Medicare annual enrollment period, which is a period of heightened television and radio advertising for our business. As a result of this increase in demand and costs, we may not be able to purchase all of the television and radio advertising we typically purchase during a Medicare annual enrollment period or we may have to pay more to purchase television and radio advertisements, which could materially and adversely impact our business, financial condition and results of operations.
Additionally, we derive a significant portion of our website traffic from consumers who search for health insurance through Internet search engines and through social media. A critical factor in attracting consumers to our website is whether we are prominently displayed in response to an Internet search relating to health insurance or on a social media platform. Search engines typically provide two types of search results, algorithmic listings and paid advertisements. We rely primarily on paid advertisements to attract consumers to our websites and otherwise generate demand for our services. To the extent the competition for advertising is high, we may experience increases in the cost of paid Internet search advertising and social media advertising. Further, the competition for search engine placement and social media presence increases substantially during the enrollment periods for Medicare-related health insurance and for individual and family health insurance. If paid search advertising costs or social media advertising costs increase or become cost prohibitive, whether as a result of competition, algorithm changes or otherwise, our advertising expenses could rise significantly or we could reduce or discontinue our paid search advertisements or social media advertisements, in either case which would harm our business, operating results and financial condition.
Our ability to advertise is also dependent on the laws and regulations governing the advertising and marketing of health insurance products and our other products or services, which continue to evolve and carry significant penalties for violations of law. Changes in technology, the marketplace or consumer preferences may lead to the adoption of additional laws or regulations or changes in interpretation of existing laws or regulations. If new laws or regulations are adopted, or existing laws and regulations are interpreted or enforced, to impose additional restrictions on our ability to advertise to our customers or qualified prospects, we may not be able to communicate with them in a cost-effective manner.
For example, Internet service providers, e-mail service providers and others attempt to block the transmission of unsolicited e-mail, commonly known as “spam.” Many Internet and e-mail service providers have relationships with organizations whose purpose it is to detect and notify the Internet and e-mail service providers of entities that the organization believes are sending unsolicited e-mail. If an Internet or e-mail service provider identifies e-mail from us as “spam” as a result of reports from these organizations or otherwise, we can be placed on a restricted list that will block our e-mail to customers or qualified prospects. Further, we are subject to the CAN-SPAM Act, which regulates commercial e-mail messages and specifies penalties for the transmission of commercial e-mail messages that do not comply with certain requirements, such as providing an opt-out mechanism for stopping future e-mails from senders.
38
Table of Contents
We also use telephones to communicate with and market to customers and prospective customers and some of these communications may be subject to the Telephone Consumer Protection Act, or TCPA, and other telemarketing laws. The TCPA and other laws, including state laws, relating to telemarketing restrict our ability to market and engage in other communications using the telephone in certain respects. For instance, the TCPA prohibits us from using an automatic telephone dialing system to make certain telephone calls or transmit text messages to wireless telephone numbers without prior express consent or without consulting the FTC’s national “Do Not Call” registry. We have policies and technical controls in place to comply with the TCPA and other telemarketing laws, including processes and procedures to consult the “Do Not Call” registry and to ensure that automated telephone calls are not performed without obtaining prior consent. However, despite our legal compliance, we have in the past and may in the future become subject to claims that we have violated the TCPA and/or other telemarketing laws. See “—From time to time we are subject to various legal proceedings which could adversely affect our business, financial condition or results of operations.” The TCPA provides for private rights of action and potential statutory damages for each violation and additional penalties for each willful violation, and other telemarketing laws may entail additional remedies. In the event that we are found to have violated the TCPA and/or other telemarketing laws, our business, operating results and financial condition could be harmed and liability incurred. In addition, telephone carriers may block or put customer warnings on calls originating from call centers. Customers increasingly screen their incoming e-mails, telephone calls, and text messages, including by using screening tools and warnings, and, therefore, our customers or qualified prospects may not reliably receive our communications. If we are unable to communicate effectively by e-mail or telephone with our customers and qualified prospects as a result of legislation, blockage, screening technologies or otherwise, our business, operating results and financial condition would be harmed.
We currently depend on a small group of carriers for a substantial portion of our revenue.
We derive a large portion of our revenue from a limited number of carriers. Carriers owned by Humana and Anthem accounted for (i) approximately 42% and 32%, respectively, of net revenues for the three months ended March 31, 2020 and 28% and 15%, respectively, of net revenues for the three months ended March 31, 2019, approximately 40% and 20%, respectively, of net revenues for the Pro Forma Fiscal Year 2019 and 25% and 8%, respectively, of net revenues for the year ended December 31, 2018; (ii) approximately 47% and 38%, respectively, of Medicare—Internal segment revenue for the three months ended March 31, 2020, and 60% and 22%, respectively, of Medicare—Internal segment revenue for the three months ended March 31, 2019, approximately 51% and 23%, respectively, of Medicare—Internal segment revenue for the Pro Forma Fiscal Year 2019, and 63% and 15%, respectively, of Medicare—Internal segment revenue for the year ended December 31, 2018; and (iii) approximately 55% and 31%, respectively, of Medicare—External segment revenue for the three months ended March 31, 2020 and 36% and 27%, respectively, of Medicare—External segment revenue for the three months ended March 31, 2019, approximately 46% and 32%, respectively, of Medicare—External segment revenue for the Pro Forma Fiscal Year 2019, and 41% and 18%, respectively, of Medicare—External segment revenue for the year ended December 31, 2018. In addition, carriers owned by UnitedHealth Group represented approximately 37% and 29% of IFP and Other—Internal segment revenue for the three months ended March 31, 2020 and for the three months ended March 31, 2019, respectively, approximately 27% and 11% of IFP and Other—Internal segment revenue for the Pro Forma Fiscal Year 2019 and for the year ended December 31, 2018, respectively, and 55% and 37% of IFP and Other—External segment revenue for the three months ended March 31, 2020 and 2019, respectively, and 41% and 19% of IFP and Other—External segment revenue for the Pro Forma Fiscal Year 2019 and year ended December 31, 2018, respectively.
Our agreements with carriers to sell policies are typically terminable by our carriers without cause. Should we become dependent on fewer carrier relationships (whether as a result of the termination of carrier relationships, carrier consolidation or otherwise), we may become more vulnerable to adverse changes in our relationships with carriers, particularly in states where we distribute insurance from a relatively smaller number of carriers or where a small number of carriers dominate the market, and our business, operating results and financial condition could be harmed.
39
Table of Contents
If investments we make in enrollment periods do not result in a significant number of Approved Submissions, our business, operating results and financial condition would be harmed.
In an attempt to attract and enroll a large number of individuals during the Medicare annual enrollment period and the healthcare reform open enrollment period, we may invest in areas of our business, including technology and content, customer care and enrollment, and marketing and advertising. We have in the past made investments in areas of our business in advance of enrollment periods that have not yielded the results we expected when making those investments. Any investment we make in any enrollment period may not result in a significant number of Approved Submissions to offset the investments we make. To the extent our investment does not yield a significant number of Approved Submissions, our business, operating results and financial condition would be harmed.
We rely on carriers to prepare accurate commission reports and send them to us in a timely manner.
Our carriers typically pay us a specified percentage of the premium amount collected by the carrier or a flat rate per policy during the period that a consumer maintains coverage under a policy. We rely on carriers to report the amount of commissions we earn accurately and on time. We use carriers’ commission reports to calculate our revenue, prepare our financial reports, projections, and budgets and direct our marketing and other operating efforts. It is often difficult for us to independently determine whether carriers are reporting all commissions due to us, primarily because the majority of the purchasers of our insurance products who terminate their policies do so by discontinuing their premium payments to the carrier instead of informing us of the cancellation. For example, there have been instances where we have determined that policy cancellation data reported to us by a carrier has not been accurate. To the extent that carriers inaccurately or belatedly report the amount of commissions due to us, we may not be able to collect and recognize revenue to which we are entitled, which would harm our business, operating results and financial condition. In addition, the technological connections of our systems with the carriers’ systems that provide us up-to-date information about coverage and commissions could fail or carriers could cease providing us with access to this information, which could impede our ability to compile our operating results in a timely manner.
Changes in the health insurance market or in the variety, quality and affordability of the insurance products offered by carriers could harm our business, operating results and financial condition.
The demand for our agency services is impacted by the variety, quality and price of the insurance products we distribute. If insurance carriers do not continue to provide us with a variety of insurance products, or if as a result of consolidation in the insurance industry or for any other reason the choices of carrier products that we are able to offer are limited, our sales may decrease and our business, operating results and financial condition could be harmed.
Our quarterly results of operations may fluctuate significantly due to seasonality.
The Medicare annual enrollment period occurs from October 15th to December 7th each year. As a result, we experience an increase in the number of submitted Medicare-related applications during the fourth quarter and an increase in expense related to the Medicare segments during the third and fourth quarters. Additionally, as a result of the annual Medicare Advantage open enrollment period that occurs from January 1st to March 31st, commission revenue is typically second-highest in our first quarter. The individual and family health insurance open enrollment period runs from November 1st through December 15th of each year for most states, and we expect the number of approved applications for individual and family health insurance to be higher in the fourth quarter compared to other quarters of the year as a result. A significant portion of our marketing and advertising expenses is driven by the number of health insurance applications submitted through us. Marketing and advertising expenses are generally higher in the fourth quarter during the Medicare annual enrollment period, but because commissions from approved customers are paid to us over time, our operating cash flows could be adversely impacted by a substantial increase in marketing and advertising expense as a result of a higher volume of applications submitted during the fourth quarter or positively impacted by a substantial decline in marketing and advertising expenses as a result of lower volume of applications submitted during the fourth quarter.
40
Table of Contents
The seasonality of our business could change in the future due to other factors, including as a result of changes in timing of the Medicare or individual and family health plan enrollment periods and changes in the laws and regulations that govern the sale of health insurance. We may not be able to timely adjust to changes in the seasonality of our business. If the timing of the enrollment periods for Medicare-related health insurance or individual and family health insurance changes, we may not be able to timely adapt to changes in customer demand. If we are not successful in responding to changes in the seasonality of our business, our business, operating results and financial condition could be harmed.
Pressure from existing and new competitors may adversely affect our business, operating results and financial condition.
Our competitors provide services designed to help customers shop for insurance. Some of these competitors include:
| • | companies that operate insurance search websites or websites that provide quote information or the opportunity to purchase insurance products online, including aggregators and lead generators; |
| • | companies that advertise primarily through the television; |
| • | individual insurance carriers, including through the operation of their own websites, physical storefront operations and broker arrangements; |
| • | traditional insurance agents or brokers; and |
| • | field marketing organizations. |
New competitors may enter the market for the distribution of insurance products with competing insurance platforms, which could have an adverse effect on our business, operating results and financial condition. Our competitors could significantly impede our ability to maintain or increase the number of policies sold through our platform and may develop and market new technologies that render our platform less competitive or obsolete. In addition, if our competitors develop platforms with similar or superior functionality to ours and we are not able to produce certain volumes for our carriers, we may see a reduction in our production bonuses or marketing payments and our revenue would likely be reduced and our business, operating results and financial condition would be adversely affected.
If we do not successfully compete with government-run health insurance exchanges, our business may be harmed.
Our business competes with government-run health insurance exchanges with respect to our sale of Medicare-related health insurance and individual and family plans. Consumers can shop for and purchase Medicare Advantage and Medicare Part D Prescription Drug plans through a website operated by the federal government and can also obtain plan selection assistance from the federal government in connection with their purchase of a Medicare Advantage and Medicare Part D Prescription Drug plan. Competition from government-run health insurance exchanges could increase our marketing costs, reduce our revenue and could otherwise harm our business, operating results and financial condition.
If we fail to comply with certain healthcare laws, including fraud and abuse laws, we could face substantial penalties and our business, results of operations and financial condition could be adversely affected.
Our arrangements with carriers, particularly those that contract with federal healthcare care programs, are highly regulated and subject us to broadly applicable federal and state fraud and abuse and other federal and state healthcare laws and regulations. These laws may constrain the business or financial arrangements and relationships through which we conduct our operations, including the following:
| • | the federal Anti-Kickback Statute, which prohibits, among other things, persons or entities from knowingly and willfully soliciting, offering, receiving or providing any remuneration (including any kickback, bribe or |
41
Table of Contents
| certain rebates), directly or indirectly, overtly or covertly, in cash or in kind, in return for, either the referral of an individual or the purchase, lease, or order, or arranging for or recommending the purchase, lease, or order of any good, facility, item or service, for which payment may be made, in whole or in part, under a federal healthcare program such as Medicare and Medicaid. The term remuneration has been interpreted broadly to include anything of value. The federal Anti-Kickback Statute has been interpreted to apply to, among others, financial arrangements between entities that have the ability to refer and generate business that is subject to reimbursement under federal healthcare programs. There are a number of statutory exceptions and regulatory safe harbors protecting some common activities from prosecution. The exceptions and safe harbors are drawn narrowly and practices that involve remuneration that may be alleged to be intended to induce prescribing, purchasing, ordering, or recommending may be subject to scrutiny if they do not qualify for an exception or safe harbor. Failure to meet all of the requirements of an applicable statutory exception or regulatory safe harbor does not make the conduct per se illegal under the federal Anti-Kickback Statute. Instead, the legality of the arrangement will be evaluated on a case-by-case basis based on a cumulative review of all of its facts and circumstances. Our practices may not in all cases meet all of the criteria for protection under a statutory exception or regulatory safe harbor. A person or entity does not need to have actual knowledge of the federal Anti-Kickback Statute or specific intent to violate it in order to have committed a violation, and a claim including items or services resulting from a violation of the federal Anti-Kickback Statute constitutes a false or fraudulent claim for purposes of the False Claims Act (described immediately below); |
| • | the federal false claims, including the civil False Claims Act, which, among other things, impose criminal and civil penalties against individuals or entities for knowingly presenting, or causing to be presented, to the federal government, claims for payment or approval that are false or fraudulent, knowingly making, using or causing to be made or used, a false record or statement material to a false or fraudulent claim, or from knowingly making or causing to be made a false statement to avoid, decrease or conceal an obligation to pay money to the federal government. The False Claims Act can be enforced by private citizens through civil qui tam actions. A claim includes “any request or demand” for money or property presented to the U.S. government; |
| • | the federal beneficiary inducement civil monetary laws, which generally prohibit giving something of value to an individual if the remuneration is likely to influence that beneficiary’s choice of a particular provider, supplier or practitioner for services covered by applicable federal healthcare programs. There are a number of exceptions, such as, remuneration that “promotes access to care and poses a low risk of harm to patients and federal healthcare programs.” A violation of this statute includes fines or exclusion from federal healthcare programs; |
| • | HIPAA, which created additional federal criminal statutes that prohibit, among other things, knowingly and willfully executing, or attempting to execute, a scheme to defraud or to obtain, by means of false or fraudulent pretenses, representations or promises, any money or property owned by, or under the control or custody of, any healthcare benefit program, including private third-party payers, willingly obstructing a criminal investigation of a healthcare offense, and knowingly and willfully falsifying, concealing or covering up by trick, scheme or device, a material fact or making any materially false, fictitious or fraudulent statement in connection with the delivery of or payment for healthcare benefits, items or services. Like the federal Anti-Kickback Statute, a person or entity need not have actual knowledge of the statute or specific intent to violate it in order to have committed a violation; and |
| • | analogous state and foreign laws and regulations, such as state anti-kickback and false claims laws, which may be more restrictive and may apply to healthcare items or services reimbursed by non-governmental third-party payors, including private insurers, or by the patients themselves. |
Ensuring business arrangements with third parties comply with applicable healthcare laws and regulations is a costly endeavor. If our operations are found to be in violation of any of the federal and state healthcare laws described above or any other current or future governmental regulations that apply to us, we may be subject to
42
Table of Contents
penalties, including without limitation, civil, criminal and/or administrative penalties, damages, fines, disgorgement, individual imprisonment, exclusion from participation in government programs, such as Medicare and Medicaid, injunctions, private “qui tam” actions brought by individual whistleblowers in the name of the government, or refusal to allow us to enter into government contracts, contractual damages, reputational harm, administrative burdens, diminished profits and future earnings, additional reporting obligations and oversight if we become subject to a corporate integrity agreement or other agreement to resolve allegations of non-compliance with these laws, and the curtailment or restructuring of our operations, any of which could adversely affect our ability to operate our business and our results of operations.
We operate in a complex state regulatory environment that is constantly changing. If we fail to comply with the numerous state laws and regulations that are applicable to the sale of health insurance, our business, operating results and financial condition could be harmed.
The offer, sale and purchase of health insurance is heavily regulated by various states and the regulatory landscape is constantly changing. States have adopted and will continue to adopt new laws and regulations, including in response to healthcare reform legislation and it is difficult to predict how these new laws and regulations will impact our business. In some cases such laws and regulations could amplify the adverse impacts of healthcare reform to our business, or states may adopt new requirements that adversely impact our business, operating results and financial condition. For example, certain states have adopted or are contemplating rules and regulations that would either ban the sale of individual and family plans that do not qualify as minimum essential coverage under the ACA (such as short-term health insurance), limit the duration and renewability of those plans, or apply certain aspects of the ACA to those plans, such as the essential health benefits or requiring that such plans cover pre-existing conditions. Rules and regulations, such as these could adversely impact our sale of individual and family plans for several reasons, including because carriers may exit the market of selling such plans due to regulatory concerns, determine it is not profitable to sell the plans or increase plan premiums to a degree that reduces customer demand for them.
Additionally, a long-standing provision in almost all states’ laws provides that once health insurance premiums are set by the carrier and approved by state regulators, they are fixed and not generally subject to negotiation or discounting by insurance companies or agents. Additionally, state regulations generally prohibit carriers, agents and brokers from providing financial incentives, such as rebates, to their customers in connection with the sale of health insurance. As a result, we do not currently compete with carriers or other agents and brokers on the price of the health insurance plans offered on our website. If these regulations change, we could be forced to reduce prices or provide rebates or other incentives for the health insurance plans sold through our technology platform, which would harm our business, operating results and financial condition. Although commissions do not currently have to be disclosed to the public, if commissions become more regulated and commissions paid to us have to be disclosed, it is possible that carriers may lower our commission rates, which could reduce our revenue.
We rely heavily on SNPs during the special enrollment periods, which allows us to utilize our agents throughout the year. If states adopt new laws and regulations or modify the existing laws and regulations governing Medicaid, such changes could decrease the number of individuals eligible for D-SNP, which could have a material adverse impact on our business, operating results and financial condition.
State regulators require us to maintain a valid license in each state in which we transact health insurance business and further require that we adhere to sales, documentation and administration practices specific to that state. We must maintain our health insurance licenses to continue selling plans and to continue to receive commissions from carriers. In addition, each employee who transacts health insurance business on our behalf must maintain a valid license in one or more states. Because we do business in all 50 states and the District of Columbia, compliance with health insurance-related laws, rules and regulations is difficult and imposes significant costs on our business. Each jurisdiction’s insurance department typically has the power, among other things, to:
| • | grant and revoke licenses to transact insurance business; |
43
Table of Contents
| • | conduct inquiries into the insurance-related activities and conduct of agents and agencies; |
| • | require and regulate disclosure in connection with the sale and solicitation of health insurance; |
| • | authorize how, by which personnel and under what circumstances insurance premiums can be quoted and published and an insurance policy sold; |
| • | approve which entities can be paid commissions from carriers and the circumstances under which they may be paid; |
| • | regulate the content of insurance-related advertisements, including web pages, and other marketing practices; |
| • | approve policy forms, require specific benefits and benefit levels and regulate premium rates; |
| • | impose fines and other penalties; and |
| • | impose continuing education requirements. |
In addition, we must ensure that our agents have received all licenses, appointments and certifications required by state authorities and our carriers in order to transact business. If the relevant state authorities or our carriers experience shutdowns or continued business disruptions due to the COVID-19 pandemic, we may be unable to secure these required licenses, appointments and certifications for our agents in a timely manner, or at all.
Due to the complexity, periodic modification and differing interpretations of state insurance laws and regulations, we may not have always been, and we may not always be, in compliance with them. New state insurance laws, regulations and guidelines also may not be compatible with the sale of health insurance over the Internet or with various aspects of our platform or manner of marketing or selling health insurance plans. Failure to comply with insurance laws, regulations and guidelines or other laws and regulations applicable to our business could result in significant liability, additional department of insurance licensing requirements, required modification of our advertising and business practices, the revocation of our licenses in a particular jurisdiction, termination of our relationship with carriers, loss of commissions and/or our inability to sell health insurance plans, which could significantly increase our operating expenses, result in the loss of carrier relationships and our commission revenue and otherwise harm our business, operating results and financial condition. Moreover, an adverse regulatory action in one jurisdiction could result in penalties and adversely affect our license status, business or reputation in other jurisdictions due to the requirement that adverse regulatory actions in one jurisdiction be reported to other jurisdictions. Even if the allegations in any regulatory or other action against us are proven false, any surrounding negative publicity could harm consumer, marketing partner or carrier confidence in us, which could significantly damage our brand.
If we are not successful in cost-effectively converting consumer leads into customers for which we receive commissions, our business, operating results and financial condition would be harmed.
Obtaining quality consumer leads is important to our business, but our ability to convert these consumer leads to customers is also a key to our success. Our growth depends in large part upon growth in Approved Submissions in a given period. The rate at which we grow our Approved Submissions directly impacts our revenue. In addition, the rate at which Submitted Policies turn into commissionable Approved Submissions impacts the expected LTV of our customers, which impacts the revenue that we are able to recognize. A number of factors have influenced, and could in the future influence, these conversion rates for any given period, some of which are outside of our control. These factors include:
| • | changes in customer shopping behavior due to circumstances outside of our control, such as economic conditions, customers’ ability or willingness to pay for health insurance, adverse weather conditions or natural disasters, the effects of pandemics, such as COVID-19, availability of unemployment benefits or proposed or enacted legislative or regulatory changes impacting our business, including healthcare reform; |
44
Table of Contents
| • | the quality of, and changes to, the customer experience on our platform; |
| • | regulatory requirements, including those that make the experience on our platform cumbersome or difficult to navigate or reduce the ability of customers to purchase plans outside of enrollment periods; |
| • | the variety, competitiveness and affordability of the health insurance plans that we offer; |
| • | system failures or interruptions in the operation of our technology platform or call center operations; |
| • | changes in the mix of customers who are referred to us through our direct, marketing partner and online advertising customer acquisition channels; |
| • | carriers offering health insurance plans for which customers have expressed interest, and the degree to which our technology is integrated with those carriers; |
| • | carrier guidelines applicable to applications submitted by customers, the amount of time a carrier takes to make a decision on that application and the percentage of submitted applications approved by carriers; |
| • | the effectiveness of agents in assisting customers; and |
| • | our ability to enroll subsidy-eligible individuals in qualified health plans through government-run health insurance exchanges and the efficacy of the process we are required to use to do so. |
Our conversion rates can be impacted by changes in the mix of customers referred to us through our customer acquisition channels. We may make changes to our technology platform in response to regulatory requirements or undertake other initiatives in an attempt to improve the customer experience or for other reasons. These changes have in the past, and may in the future have the unintended consequence of adversely impacting our conversion rates. A decline in the percentage of consumers who submit health insurance applications on our platform and are converted into approved customers could cause an increase in our CAC and impact our revenue in any given period. To the extent our conversion rate suffers, our customer base may decline, which would harm our business, operating results and financial condition.
We receive commission payments from carriers over time, but incur significant upfront expenses to enroll customers.
The enrollment of consumers on our platform requires significant upfront expenses, including marketing and advertising expenses and customer care and enrollment expenses, in order to generate qualified prospects, educate and enroll those consumers in our products and plans, and submit completed applications to carriers. However, the resulting commissions are generally paid to us over time, with the first payments often several weeks or months after we submit completed applications to our carriers. These factors cause us to require significant cash to fund our working capital needs, and our operating cash flows could be adversely impacted by a substantial increase in the volume of applications submitted by us.
If we are unable to maintain effective relationships with our existing third-party marketing companies or if we do not establish successful relationships with new marketing companies our business, operating results and financial condition could be harmed.
We frequently enter into contractual marketing relationships with online and offline businesses that help us acquire consumer leads. These marketing partners include television advertisers, online advertising companies, call referral programs, and other marketing vendors. We compensate some marketing companies on a fee-per-service model and some on a submitted health insurance application basis. The success of our relationship with each marketing company is dependent on a number of factors, including but not limited to: the continued positive market presence, reputation and growth of the marketing company, the effectiveness of the marketing company’s advertisements, the compliance of each marketing company with applicable laws, regulations and guidelines and the contractual terms we negotiate with the marketing company, including the marketing fees we agree to pay.
45
Table of Contents
While we have relationships with a large number of marketing companies, we depend upon services and/or referrals from only a limited number for a significant portion of the submitted applications we receive. Given our reliance on various marketing companies, our business operating results and financial condition would be harmed if (i) we are unable to maintain successful relationships with these companies; (ii) we fail to establish successful relationships with new marketing companies; (iii) we experience competition in our provision of services from key marketing companies; and (iv) if we are required to pay increased amounts to these marketing companies.
Competition for referrals from third-party lead referral companies has increased particularly during the enrollment periods for Medicare-related health insurance and individual and family health insurance. We may lose referrals if our competitors pay these companies more than we do or be forced to pay increased fees, which could harm our business, operating results and financial condition. In addition, the promulgation of laws, regulations or guidelines, or the interpretation of existing laws, regulations and guidelines, by state departments of insurance or by CMS, could cause our relationships with third-party referral companies to be in non-compliance with those laws, regulations and guidelines. If CMS or state departments of insurance were to change existing laws, regulations or guidelines, or interpret existing laws, regulations or guidelines, to prohibit these arrangements, we could experience a significant decline in the number of Medicare-eligible individuals who are referred to our platforms and Benefits Center, which would harm our business, operating results and financial condition.
If we lose key management or fail to meet our need for qualified employees, our business, financial condition and results of operations could be materially adversely affected.
We rely, in part, upon the accumulated knowledge, skills and experience of our executive officers. Our Chief Executive Officer has been with us for more than 19 years and our executive officers have a combined total of 63 years of experience in the health insurance industry. The loss of the services of any of our executive officers could have a material adverse effect on our business, financial condition and results of operations, as we may not be able to find suitable individuals to replace such officers on a timely basis or without incurring increased costs, or at all. We currently do not have any key man insurance covering our Chief Executive Officer. If our executive officers were to leave us or become incapacitated, it might negatively impact our planning and execution of business strategy and operations. We believe that our future success will depend on our continued ability to attract and retain highly skilled and qualified executive personnel for all areas of our organization, for which there is a high level of competition for such personnel in our industry. Our inability to meet our executive staffing requirements in the future could have a material adverse effect on our business, financial condition and results of operations.
Our future success is also dependent upon our ability to attract, retain and effectively deploy qualified employees. We may need to offer higher compensation and other benefits in order to attract and retain key personnel in the future. To attract top talent, we must offer competitive compensation packages before we have the opportunity to validate the productivity and effectiveness of new employees. Additionally, we may not be able to hire new employees quickly enough, we may not have adequate resources to meet our hiring needs, and we may not effectively deploy our workforce in order to efficiently allocate our internal resources. If we fail to meet our hiring needs, successfully integrate our new hires or effectively deploy our existing personnel, our efficiency and ability to meet our forecasts, our ability to successfully execute on our strategic plan to return to revenue growth and our employee morale, productivity and retention could all suffer. Any of these factors could materially adversely affect our business, operating results and financial condition.
We are subject to privacy and data protection laws governing the transmission, security and privacy of personal information, particularly individually identifiable health information, which may impose restrictions on the manner in which we process such information and subject us to enforcement and penalties if we are unable to fully comply with such laws.
Numerous federal, state and international laws and regulations govern the collection, use, disclosure, storage, processing, transmission and destruction of personal information, including individually identifiable health
46
Table of Contents
information. These laws and regulations, including their interpretation by governmental agencies and regulators, are subject to frequent change. These regulations could have a negative impact on our business, for example:
| • | HIPAA and its implementing regulations were enacted to ensure that employees can retain and at times transfer their health insurance when they change jobs, and to simplify healthcare administrative processes. The enactment of HIPAA also expanded protection of the privacy and security of protected health information and required the adoption of standards for the exchange of electronic health information. Among the standards that the Department of Health and Human Services has adopted pursuant to HIPAA are standards for electronic transactions and code sets, unique identifiers for providers, employers, health plans and individuals, security, electronic signatures, privacy and enforcement. Failure to comply with HIPAA could result in enforcement activity, fines, penalties and litigation that could have a material adverse effect on us; |
| • | The HITECH Act sets forth health information security breach notification requirements and increased penalties for violation of HIPAA. The HITECH Act requires individual notification for all breaches, media notification of breaches of over 500 individuals and at least annual reporting of all breaches to the Department of Health and Human Services. The HITECH Act also replaced the prior penalty system of one tier of penalties of $100 per violation and an annual maximum of $25,000 with a four-tier system of sanctions for breaches ranging from the original $100 per violation and an annual maximum of $25,000 for the first tier to a fourth-tier minimum of $50,000 per violation and an annual maximum of $1.5 million per violation category. These penalties are required to be adjusted for inflation. Failure to comply with the HITECH Act could result in enforcement activity, fines, penalties and litigation that could have a material adverse effect on us; |
| • | Other federal and state laws restricting the use and protecting the privacy and security of individually identifiable information may apply, many of which are not preempted by HIPAA; and |
| • | Federal and state consumer protection laws are increasingly being applied by the FTC, and states’ attorneys general to regulate the collection, use, processing, destruction, storage and disclosure of individually identifiable information, through websites or otherwise, and to regulate the presentation of website content. |
We are required to comply with federal and state laws governing the transmission, security and privacy of personal information that we may obtain or have access to in connection with the provision of our services. Despite the security measures that we have in place to ensure compliance with privacy and data protection laws, our facilities and systems, and those of our third-party vendors and subcontractors, are vulnerable to security breaches, acts of vandalism or theft, computer viruses, malware, ransomware, denial-of-service attacks, misplaced or lost data, programming and human errors or other similar events. Due to the enactment of the HITECH Act, we are not able to predict the extent of the impact such incidents may have on our business. Our failure to comply may result in criminal and civil liability especially because the potential for enforcement action against business associates is now greater. Enforcement actions against us could be costly and could interrupt regular operations or the availability of data, which may adversely affect our business. While we have received inquiries relating to our compliance with various privacy acts, including inquiries originating from allegations of a potential breach, to date none have been found or determined to be actual violations by the Company.
Under the HITECH Act, as a business associate we may also be directly or independently liable for privacy and security breaches and failures of our subcontractors. Even though we provide for appropriate protections through our agreements with our subcontractors and exercise appropriate oversight of such subcontractors, we still have limited control over their actions and practices. A breach of privacy or security of individually identifiable health information by a subcontractor or other entity operating on our behalf may result in an enforcement action, including criminal and civil liability, against us or litigation by a covered entity with whom we have a contractual relationship. In addition, numerous other federal and state laws protect the confidentiality of individually identifiable information as well as employee personal information, including state medical privacy laws, state social security number protection laws, and federal and state consumer protection laws. These various laws in
47
Table of Contents
many cases are not preempted by HIPAA and may be subject to varying interpretations by the courts and government agencies, creating complex compliance issues for us and our customers and potentially exposing us to additional expense, adverse publicity and liability, any of which could adversely affect our business, operating results and financial condition.
State and federal laws may apply to our collection, use, handling, processing, destruction, disclosure, and storage as well. For example, the California Consumer Privacy Act of 2018, or the CCPA, effective as of January 1, 2020, affords consumers expanded privacy protections and control over the collection, use and sharing of their personal information. The CCPA was recently amended, and it is possible it will be amended again by other pending legislative initiatives or by popular referendum. The Attorney General of California is promulgating implementing CCPA regulations which are undergoing successive rounds of public comment and revision. The potential effects of this legislation, including whether and how the law will be applied to the consumer health-related data we collect through our service, are far-reaching and may require us to modify our data processing practices and policies and to incur substantial costs and expenses in an effort to comply. The CCPA gives California residents expanded rights to access and require deletion of their personal information, opt out of certain personal information sharing and receive detailed information about how their personal information is used. The CCPA also provides for civil penalties for violations, as well as a private right of action for data breaches that may increase data breach litigation. The CCPA does contain an exemption for medical information governed by the California Confidentiality of Medical Information Act (CMIA), and for protected health information collected by a covered entity or business associate governed by the privacy, security and breach notification rule established pursuant to HIPAA and HITECH, but the precise application and scope of this exemption as well as how it would apply to our business is not yet clear.
With laws and regulations such as HIPAA and the CCPA imposing relatively burdensome obligations, and with substantial uncertainty over the interpretation and application of these and other laws and regulations to our business, we may face challenges in addressing their requirements and making necessary changes to our policies and practices, and may incur significant costs and expenses in an effort to do so. For example, the increased consumer control over the sharing of their personal information under the CCPA may affect our customers’ ability to share such personal information with us or may require us to delete or remove consumer information from our records or data sets, which may create considerable costs or loss of revenue for our organization.
In addition, any failure or perceived failure by us to maintain posted privacy policies which are accurate, comprehensive and fully implemented, and any violation or perceived violation of our privacy-, data protection- or information security-related obligations to customers, users or other third parties or any of our other legal obligations relating to privacy, data protection or information security may result in governmental investigations or enforcement actions, litigation, claims or public statements against us by consumer advocacy groups or others, and could result in significant liability, loss of relationships with key third parties including carriers, social media networks and other data providers, or cause our consumers to lose trust in us, which could have material impacts on our revenue and operations.
We may not be able to maintain compliance with all current and potentially applicable U.S. federal and state or foreign laws and regulations relating to privacy and cybersecurity, and actions by regulatory authorities or changes in legislation and regulation in the jurisdictions in which we operate could have a material adverse effect on our business.
We are subject to a variety of laws and regulations that involve user privacy and the collection, processing, storing, sharing, disclosing, using, transfer and protecting of personal information and other data. These laws and regulations constantly evolve and remain subject to significant change. In addition, the application and interpretation of these laws and regulations are often uncertain. Because we store, process and use data, some of which contain personal information, we are subject to complex and evolving federal, state and local laws and regulations regarding privacy, data protection and other matters. Many of these laws and regulations are subject to change and uncertain interpretation. The U.S. federal and state governments and agencies may in the future
48
Table of Contents
enact new legislation and promulgate new regulations governing collection, use, disclosure, storage, processing, transmission and destruction of personal information and other data. New privacy laws add additional complexity, requirements, restrictions and potential legal risk, require additional investment in resources to compliance programs, and could impact trading strategies and availability of previously useful data.
The New York Department of Financial Services, or NYDFS, Cybersecurity Regulation for financial services companies, including insurance entities under NYDFS jurisdiction, requires entities to establish and maintain a cybersecurity program designed to protect private consumer data, and implement a risk assessment designed to perform core cybersecurity functions. The regulation specifically provides for: (i) controls relating to the governance framework for a cybersecurity program; (ii) risk-based minimum standards for technology systems for data protection; (iii) minimum standards for cyber breach responses, including notice to the NYDFS, of material events; and (iv) identification and documentation of material deficiencies, remediation plans and annual certification of regulatory compliance with the NYDFS. The Cybersecurity Regulation also requires implementation of continuous monitoring of information technology systems or periodic penetration testing and vulnerability assessments. Similarly, the Massachusetts data protection law and the New York Stop Hacks and Improve Data Security Act, or SHIELD Act, both require companies to implement a written information security program that contains appropriate administrative, technical, and physical safeguards as defined in the respective statute.
In October 2017, the National Association of Insurance Commissioners, or NAIC, adopted the Insurance Data Security Model Law, or the Cybersecurity Model Law, which is intended to establish the standards for data security and for the investigation and notification of data breaches applicable to insurance licensees in states adopting such law. To date, the Cybersecurity Model Law has been adopted by Alabama, Connecticut, Delaware, Michigan, Mississippi, New Hampshire, Ohio and South Carolina, with several other states expected to adopt in the near future. The Cybersecurity Model Law could impose significant new regulatory burdens intended to protect the confidentiality, integrity and availability of information systems. The NAIC model law is functionally similar to the NYDFS rule.
In addition, the California legislature enacted the CCPA in September 2018, which entered into effect in January 2020, and has encouraged “copycat” legislative proposals in other states across the country such as Nevada, Virginia, New Hampshire, Illinois and Nebraska. These legislative proposals may add additional complexity, variation in requirements, restrictions and potential legal risk, require additional investment in resources to compliance programs, and could impact strategies and availability of previously useful data.
Compliance with existing and emerging privacy and cybersecurity laws and regulations could result in increased compliance costs and/or lead to changes in business practices and policies, and any failure to protect the confidentiality of client information could adversely affect our reputation, lend to private litigation against us, and require additional investment in resources, impact strategies and availability of previously useful data any of which could materially and adversely affect our business, operating results and financial condition.
Risks from third-party products could adversely affect our businesses.
We offer third-party health insurance products. Insurance involves a transfer of risk and our reputation may be harmed and we may become a target for litigation if risk is not transferred in the way expected by customers and carriers. In addition, if these insurance products do not generate competitive risk-adjusted returns that satisfy our carriers, it may be difficult to maintain existing business with, and attract new business from, them. Significant declines in the performance of these third-party products could subject us to reputational damage and litigation risk.
Our ability to match consumers to insurance products that suit their needs is dependent upon their provision of accurate information during the insurance shopping process.
Our business depends on consumers’ provision of accurate information during the insurance shopping process. To the extent consumers provide us with inaccurate information, the quality of their insurance shopping
49
Table of Contents
experience may suffer and we may be unable to match them with insurance products that suit their needs. Our inability to suggest suitable insurance products to consumers could lead to an increase in the number of policies we submit to carriers that are ultimately rejected or an increase in plans that are cancelled earlier than expected or otherwise terminated, which could materially and adversely affect our business, operating results and financial condition.
Our international operations subject us to additional risks which could have an adverse effect on our business, operating results and financial condition.
We have attempted to control our operating expenses by utilizing lower cost labor in foreign countries such as Slovakia and Honduras and we may in the future expand our reliance on offshore labor to other countries. As of March 31, 2020, 47 of our employees were based in Slovakia. Our employees in Slovakia help develop, test and maintain our Marketplace technology. Additionally, we outsource certain of our call center operations to a company in Honduras. Countries outside of the United States may be subject to relatively higher degrees of political and social instability and may lack the infrastructure to withstand political unrest or natural disasters. The occurrence of natural disasters, pandemics, such as COVID-19, or political or economic instability in these countries could interfere with work performed by these labor sources, or could result in our having to replace or reduce these labor sources. Our vendors in other countries could potentially shut down suddenly for any reason, including financial problems or personnel issues. Such disruptions could decrease efficiency, increase our costs and have an adverse effect on our business or results of operations.
The practice of utilizing labor based in foreign countries has come under increased scrutiny in the United States. Governmental authorities, including CMS, could seek to impose financial costs or restrictions on foreign companies providing services to customers or companies in the United States. Governmental authorities may attempt to prohibit or otherwise discourage us from sourcing services from offshore labor. In addition, carriers may require us to use labor based in the United States for regulatory or other reasons. To the extent that we are required to use labor based in the United States, we may face increased costs as a result of higher-priced United States-based labor.
The FCPA and other applicable anti-corruption laws and regulations prohibit certain types of payments by our employees, vendors and agents. Any violation of the applicable anti-corruption laws or regulations by us, our subsidiaries or our local agents could expose us to significant penalties, fines, settlements, costs and consent orders that may curtail or restrict our business as it is currently conducted and could have an adverse effect on our business, financial condition or results of operations.
Weakness of the United States dollar in relation to the currencies used in these foreign countries may also reduce the savings achievable through this strategy and could have an adverse effect on our business, financial condition and results of operations.
If we are not able to maintain and enhance our brand, our business and operating results will be harmed. Damage to our reputation and negative publicity could have a material adverse effect on our business, financial condition and results of operations.
We believe that maintaining and enhancing our brand identity is critical to our relationships with our existing carriers and to our ability to attract new customers, marketing partners and carriers. We also intend to grow our brand awareness among consumers, marketing partners and carriers in order to further expand our marketplace and attract new consumers, marketing partners and carriers. The promotion of our brand in these and other ways may require us to make substantial investments and we anticipate that, as our market becomes increasingly competitive, these branding initiatives may become increasingly difficult and expensive. Our brand promotion activities may not be successful or yield increased revenue, and to the extent that these activities yield increased revenue, the increased revenue may not offset the expenses we incur and our operating results could be harmed. If we do not successfully maintain and enhance our brand, our business may not grow and we could lose our relationships with carriers, marketing partners or customers, which would harm our business, operating results and financial condition.
50
Table of Contents
We may be adversely affected by negative publicity relating to brand and activities. For instance, if our brand receives negative publicity, the number of customers visiting our platforms or Benefits Center could decrease, and our cost of acquiring customers could increase as a result of a reduction in the number of consumers coming from our direct customer acquisition channel. Additionally, there is at least one other third party business which uses the “GoHealth” name, but is not affiliated with our business. While we agreed with the third party that our “GoHealth” marks can coexist with the third party’s use of “GoHealth” in their business without creating a likelihood of consumer confusion, we entered into a co-existence agreement with the third-party that, among other things, places certain restrictions on both their use of “GoHealth,” as well as ours, in order to further mitigate any risk of confusion. Nevertheless, if despite these measures, our business is mistakenly confused with their business or another business, the value of our brand could be adversely impacted, which could harm our business, operating results and financial condition.
Any legal liability, regulatory penalties, or negative publicity for the information on our website or that we otherwise provide could harm our business, operating results and financial condition.
We provide information on our website, through our Benefits Center, in our marketing materials and in other ways regarding health insurance in general and the health insurance plans we market and sell, including information relating to insurance premiums, coverage, benefits, provider networks, exclusions, limitations, availability, plan comparisons and insurance company ratings. A significant amount of both automated and manual effort is required to maintain the considerable amount of insurance plan information on our website. If the information we provide on our website, through our Benefits Center, in our marketing materials or otherwise is not accurate or is construed as misleading, or if we do not properly assist individuals and businesses in purchasing health insurance, customers, carriers and others could attempt to hold us liable for damages, our relationships with carriers could be terminated or impaired and regulators could attempt to subject us to penalties, revoke our licenses to transact health insurance business in a particular jurisdiction, and/or compromise the status of our licenses to transact health insurance business in other jurisdictions, which could result in our loss of our commission revenue. In the ordinary course of operating our business, we have received complaints that the information we provided was not accurate or was misleading. Although in the past we have resolved these complaints without significant financial cost or impact to our brand or reputation, we cannot guarantee that we will be able to do so in the future. Our sales of individual and family plans that do not qualify as minimum essential coverage, thereby lacking the same benefits as major medical health insurance plans, may increase the risk that we receive complaints regarding our marketing and business practices due to the potential for customer confusion between such plans and major medical health insurance. In addition, these types of claims could be time-consuming and expensive to defend, could divert our management’s attention and other resources, and could cause a loss of confidence in our services. As a result, whether or not we are able to successfully resolve these claims, they could harm our business, operating results and financial condition.
In the ordinary course of our business, we have received and may continue to receive inquiries from state regulators relating to various matters. We also have become, and may in the future become, involved in litigation or claims in the ordinary course of our business, including with respect to employment-related claims such as workplace discrimination or harassment. We have and may in the future, face claims of violations of other local, state, and federal labor or employment laws, laws and regulations relating to marketing and laws and regulations relating to the sale of insurance. If we are found to have violated laws or regulations, we could lose our relationship with carriers and be subject to various fines and penalties, including revocation of our licenses to sell insurance which would cause us to lose our commission revenue, and our business, operating results and financial condition would be materially harmed. In addition, if regulators believe our websites or marketing material are not compliant with applicable laws or regulations, we could be forced to stop using our websites, marketing material or certain aspects of them, which would harm our business, operating results and financial condition.
51
Table of Contents
The extent to which the COVID-19 outbreak and measures taken in response thereto impact our business, results of operations and financial condition will depend on future developments, which are highly uncertain and cannot be predicted.
In late 2019, a novel strain of coronavirus, SARS-CoV-2, surfaced in China, which has now spread to the United States and almost every country in the world. SARS-CoV-2 causes a clinical illness known as COVID-19. Global health concerns relating to the outbreak of COVID-19 have been weighing on the macroeconomic environment, and the outbreak has significantly increased economic uncertainty. The outbreak has resulted in authorities implementing numerous measures to try to contain the virus, such as travel bans and restrictions, quarantines, shelter in place orders, and business shutdowns. These measures have not only negatively impacted consumer spending and business spending habits, they have adversely impacted and may further impact our workforce and operations and the operations of carriers, consumers and our business partners. Although certain of these measures are beginning to ease in some geographic regions, overall measures to contain the COVID-19 outbreak may remain in place for a significant period of time and may adversely affect our business, results of operations and financial condition.
The spread of COVID-19 has caused us to modify our business practices (including employee travel, employee work locations, and cancellation of physical participation in meetings, events and conferences), and we may take further actions as may be required by government authorities or that we determine are in the best interests of our employees, customers and business partners. For example, we have implemented work from home measures, which have required us to provide technical support to our agents to enable them to connect to our technology platform from their homes, including by purchasing laptops for our agents and upgrading their Internet connections. In addition to an investment of financial resources, implementing work from home measures to respond to COVID-19 has diverted management’s time and attention. If our agents are not able to effectively work from home, or if our agents contract COVID-19 or another contagious disease, we may not be able to sell as many plans, which would negatively impact our business, financial condition and results of operations. There is also no certainty that the measures we have taken to mitigate the impact of COVID-19 on our business will be sufficient or otherwise be satisfactory to government authorities.
Further, because most of our employees are working remotely in connection with the COVID-19 pandemic, we may experience an increase the risk of security breaches, loss of data, and other disruptions as a result of accessing sensitive information from remote locations. Correspondingly, it remains unclear how the third-party firms or organizations who have independently audited our information security program against specific standards will assess and evaluate the sufficiency of the security measures we have taken to mitigate work-from-home related information security risks. Failure to meet these standards could impact our ability to service customers in the healthcare industry, which could have a material adverse impact on our business, financial condition and results of operations.
Additionally, our carriers and vendors have similarly adjusted their operations in light of the COVID-19 pandemic. If our carriers or vendors experience shutdowns or continued business disruptions, our ability to conduct our business operations as planned could be materially and negatively affected. For example, our carriers may experience delays in the underwriting process, and those delays could affect our ability to timely bind and sell policies. Furthermore, our business, operating results and financial condition could be adversely affected if, as a result of the macro-economic effects of the COVID-19 pandemic, demand for the products we sell on behalf of carriers declines, our carriers seek to renegotiate their commission arrangements with us or the policyholders to whom we have sold policies stop making their premium payments.
The full extent to which the outbreak of COVID-19 impacts our business, results of operations and financial condition is still unknown and will depend on future developments, which are highly uncertain and cannot be predicted, including, but not limited to, the duration and spread of the outbreak, its severity, the actions to contain the virus or treat its impact, and how quickly and to what extent normal economic and operating conditions can resume. Even after the outbreak of COVID-19 has subsided, we may continue to experience materially adverse
52
Table of Contents
impacts to our business as a result of its global economic impact, including any recession that has occurred or may occur in the future.
While governmental and non-governmental organizations are engaging in efforts to combat the spread and severity of the COVID-19 pandemic and related public health issues, these measures may not be effective. We also cannot predict how legal and regulatory responses to concerns about the COVID-19 pandemic and related public health issues will impact our business. Such events or conditions could result in additional regulation or restrictions affecting the conduct of our business in the future.
There are no comparable recent events which may provide guidance as to the effect of the spread of COVID-19 and a global pandemic, and, as a result, the ultimate impact of the COVID-19 outbreak or a similar health epidemic is highly uncertain and subject to change. We do not yet know the full extent of the impacts on our business, our operations or the global economy as a whole. However, the effects could have a material impact on our results of operations.
To the extent the COVID-19 pandemic adversely affects our business, operating results and financial condition, it may also have the effect of heightening many of the other risks described in this “Risk Factors” section, such as those relating to our level of indebtedness, our need to generate sufficient cash flows to service our indebtedness and our ability to comply with the covenants contained in our Credit Facilities.
We rely upon third parties to operate our Marketplace technology and any disruption of or interference with our use of such third-party providers would adversely affect our business, results of operations and financial condition.
We outsource our hosting infrastructure to Amazon Web Services and Rackspace (together, “Hosting Providers”), which host our Marketplace technology. Consumers and agents must have the ability to access our Marketplace technology at any time, without interruption or degradation of performance. Our Hosting Providers run their own infrastructure upon which our Marketplace technology and products depend, and we are, therefore, vulnerable to service interruptions at each Hosting Provider. Though very rare, we have experienced, and expect that in the future we may experience interruptions, delays and outages in service and availability from time to time due to a variety of factors, including infrastructure changes, human or software errors, application hosting disruptions and capacity constraints. Capacity constraints could be due to a number of potential causes including technical failures, natural disasters, fraud or security attacks. In addition, if our security, or that of one of our Hosting Providers, is compromised, our platform or products are unavailable or our users are unable to use our products within a reasonable amount of time or at all, then our business, results of operations and financial condition could be adversely affected. We note that our ability to conduct security audits on our Hosting Providers is limited, therefore, we rely heavily on third-party security reviews, such as SSAE 16 assessments. Our contracts do not contain strong indemnification terms in our favor. In some instances, we may not be able to identify and/or remedy the cause or causes of these performance problems within a period of time acceptable to our customers. It may become increasingly difficult to maintain and improve our marketplace platform performance, especially during peak usage times, as our marketplace platform becomes more complex and the usage of the platform increases. To the extent we do not effectively address capacity constraints, either through our Hosting Providers or alternative providers of cloud infrastructure, our business, results of operations and financial condition may be adversely affected. In addition, any changes in service levels from our Hosting Providers may adversely affect our ability to meet our customers’ requirements.
The substantial majority of the services we use from our Hosting Providers are for cloud-based server capacity and managed colocation services. We access our Hosting Providers’ infrastructure through standard Internet connectivity. Our Hosting Providers provide us with computing and storage capacity, network capacity, managed colocation space, and leased computing hardware pursuant to agreements that continue until terminated by either party. If any of the data centers become unavailable to us without sufficient advance notice, we would likely
53
Table of Contents
experience delays in delivering our platform and products until we could migrate to an alternate data center provider. Our disaster recovery program contemplates transitioning our platform and products to our backup center in the event of a catastrophe, but we have not yet fully tested the procedure, and our platform and products may be unavailable, in whole or in part, during any transition procedure. Although we expect that we could receive similar services from other third parties, if any of our arrangements with our Hosting Providers are terminated, we could experience interruptions on our platform and in our ability to make our products available to customers, as well as delays and additional expenses (including research and development expenses) in arranging alternative cloud infrastructure services.
Any of the above circumstances or events may cause outages where we are unable to generate revenue, harm our reputation, cause customers to stop using our products, impair our ability to attract new customers and increase revenue from customers, subject us to financial penalties and liabilities under our service level agreements and otherwise harm our revenue, business, results of operations and financial condition.
If individuals or carriers opt for more traditional or alternative channels for the purchase and sale of health insurance, our business could be harmed.
Our success depends, in part, upon continued growth in the use of the Internet as a source of research on health insurance products and pricing, as well as willingness for individuals to use the Internet to request further information or contact the distributors directly or indirectly that sell the products we offer. Individuals and carriers may choose to depend more on traditional sources, such as individual agents, or alternative sources may develop, including as a result of healthcare reform. Our future growth, if any, will depend in part upon:
| • | the growth of the Internet as a market for individual health insurance plans and services; |
| • | individuals’ willingness and ability to conduct their own health insurance research; |
| • | our ability to make the process of purchasing health insurance online an attractive alternative to traditional and new means of purchasing health insurance; |
| • | our ability to successfully and cost-effectively market our services as superior to traditional or alternative sources for health insurance to a sufficiently large number of individuals; and |
| • | carriers’ willingness to use us and the Internet as a distribution channel for health insurance products and plans. |
If individuals and carriers determine that other sources of health insurance and health insurance applications are superior, our business will not grow, and our business, operating results and financial condition could be harmed.
From time to time we are subject to various legal proceedings which could adversely affect our business, financial condition or results of operations.
We are involved in various litigation matters from time to time. Such matters can be time-consuming, divert management’s attention and resources and cause us to incur significant expenses. Our insurance and indemnities may not cover all claims that may be asserted against us, and any claims asserted against us, regardless of merit or eventual outcome, may harm our reputation. If we are unsuccessful in our defense in these litigation matters, or any other legal proceeding, we may be forced to pay damages or fines, enter into consent decrees or change our business practices, any of which could adversely affect our business, financial condition or results of operations.
Our balance sheet includes significant amounts of goodwill and intangible assets. The impairment of a significant portion of these assets would negatively affect our financial condition or results of operations.
A significant portion of our total assets consists of goodwill and intangible assets. Goodwill and intangible assets, net, together accounted for approximately 66.9% of total assets on our balance sheet as of March 31, 2020. We
54
Table of Contents
evaluate goodwill and intangible assets for impairment annually at in the fourth quarter and whenever events or circumstances make it more likely than not that impairment may have occurred. Under current accounting rules, any determination that impairment has occurred would require us to record an impairment charge, which would adversely affect our earnings. An impairment of a significant portion of goodwill or intangible assets could adversely affect our operating results and financial condition.
Changes in lease accounting standards may materially and adversely affect us.
Beginning on January 1, 2022, the Financial Accounting Standards Board, or FASB, rules will require that we account for our office space leases as assets and liabilities on our balance sheet. We previously accounted for such leases on an “off-balance sheet” basis. As a result of these changes to the FASB rules, we will be required to record lease-related assets and liabilities on our balance sheet, and the way in which we record and classify our lease-related expenses may change as well. Though these changes will not have any direct effect on our overall financial condition, they will cause the total amount of assets and liabilities we report to increase.
Operating and growing our business may require additional capital, and if capital is not available to us, our business, operating results and financial condition may suffer.
Operating and growing our business is expected to require further investments in our business. We may be presented with opportunities that we want to pursue, and unforeseen challenges may present themselves, any of which could cause us to require additional capital. Our business model does not require us to hold a significant amount of cash and cash equivalents at any given time and if our cash needs exceed our expectations or we experience rapid growth, we could experience strain in our cash flow, which could adversely affect our operations in the event we were unable to obtain other sources of liquidity. If we seek to raise funds through equity or debt financing, those funds may prove to be unavailable, may only be available on terms that are not acceptable to us or may result in significant dilution to you or higher levels of leverage. If we are unable to obtain adequate financing or financing on terms satisfactory to us, when we require it, our ability to continue to pursue our business objectives and to respond to business opportunities, challenges or unforeseen circumstances could be significantly limited, and our business, operating results and financial condition could be materially and adversely affected.
If we fail to manage future growth effectively, our business, operating results and financial condition would be harmed.
We have expanded our operations significantly and anticipate that further expansion will be required in order for us to grow our business. Our growth has placed and will continue to place increasing and significant demands on our management, our operational and financial systems and infrastructure and our other resources. If we do not effectively manage our growth, the quality of our services could suffer, which could harm our business, operating results and financial condition. In order to manage future growth, we will need to hire, integrate and retain highly skilled and motivated employees. We may not be able to hire new employees quickly enough to meet our needs. If we fail to effectively manage our hiring needs and successfully integrate our new hires, our efficiency and ability to meet our forecasts and our employee morale, productivity and retention could suffer, and our business, operating results and financial condition could be harmed. We will also be required to continue to improve our existing systems for operational and financial management, including our reporting systems, procedures and controls. These improvements may require significant capital expenditures and will place increasing demands on our management. We may not be successful in managing or expanding our operations or in maintaining adequate financial and operating systems and controls. If we do not successfully implement improvements in these areas, our business, operating results and financial condition will be harmed.
If we are unable to maintain a high level of service, our business, operating results and financial condition may be harmed.
One of the key attributes of our business is providing high quality service to our carriers and customers. We may be unable to sustain these levels of service, which would harm our reputation and our business. Alternatively, we
55
Table of Contents
may only be able to sustain high levels of service by significantly increasing our operating costs, which would materially and adversely affect our operating results. The level of service we are able to provide depends on our personnel to a significant extent. Our personnel must be well-trained in our processes and able to handle customer calls effectively and efficiently. Any inability of our personnel to meet our demand, whether due to absenteeism, training, turnover, disruptions at our facilities, including due to the effects of the COVID-19 pandemic, bad weather, power outages or other reasons, could adversely impact our business. If we are unable to maintain high levels of service performance, our reputation could suffer and our business, operating results and financial condition would be harmed.
Economic sanction laws in the United States and other jurisdictions may prohibit us and our affiliates from transacting with certain countries, individuals and companies, which could negatively impact our business, operating results and financial condition.
The Foreign Corrupt Practices Act, or the FCPA, and other anti-corruption laws and regulations, as well as anti-boycott regulations, may apply to and restrict our activities, including our software development operations in Slovakia. If we were to violate any such laws or regulations, we may face significant legal and monetary penalties. The U.S. government has indicated that it is focused on FCPA enforcement, which may increase the risk that we become the subject of such actual or threatened enforcement. As such, a violation of the FCPA or other applicable regulations could have a material adverse effect on our business.
Global economic conditions could materially and adversely affect our revenue and results of operations.
Our business has been and may continue to be affected by a number of factors that are beyond our control, such as general geopolitical, economic and business conditions, and conditions in the financial markets. A severe or prolonged economic downturn could adversely affect consumers’ financial condition and the demand for insurance products.
We are also exposed to risks associated with the potential financial instability of our carriers and customers, many of whom may be adversely affected by volatile conditions in the financial markets or an economic slowdown. As a result of uncertainties with respect to financial institutions and the global credit markets and other macroeconomic challenges currently or potentially affecting the economy of the U.S. and other parts of the world, customers may experience serious cash flow problems and other financial difficulties, decreasing demand for the products of our carriers. In addition, events in the U.S. or foreign markets, such as the U.K.’s exit from the European Union, the worldwide effects from the spread of COVID-19 and political and social unrest in various countries around the world, can impact the global economy and capital markets. Our carriers may modify, delay, or cancel plans to offer new products or may make changes in the mix of products purchased that are unfavorable to us. Additionally, if carriers are not successful in generating sufficient revenue or are precluded from securing financing, their businesses will suffer, which may materially and adversely affect our business, operating results and financial condition.
In addition, we are susceptible to risks associated with the potential financial instability of the vendors on which we rely to provide services or to whom we delegate certain functions. The same conditions that may affect carriers and customers also could adversely affect our vendors, causing them to significantly and quickly increase their prices or reduce their output. Our business depends on our ability to perform, in an efficient and uninterrupted fashion, our necessary business functions, and any interruption in the services provided by third parties could also adversely affect our business, operating results and financial condition. See “—The extent to which the COVID-19 outbreak and measures taken in response thereto impact our business, results of operations and financial condition will depend on future developments, which are highly uncertain and cannot be predicted.”
56
Table of Contents
Acquisitions of other businesses or technologies could disrupt and harm our business, operating results and financial condition.
We have in the past acquired businesses and in the future may decide to acquire other businesses, products and technologies. Our ability as an organization to successfully make and integrate acquisitions is unproven. Acquisitions could require significant capital infusions and could involve many risks, including the following:
| • | an acquisition may negatively impact our results of operations because it will require us to incur transaction expenses, and after the transaction, may require us to incur charges and substantial debt or liabilities, may require the amortization, write down or impairment of amounts related to deferred compensation, goodwill and other intangible assets, or may cause adverse tax consequences, substantial depreciation or deferred compensation charges; |
| • | an acquisition undertaken for strategic business purposes may negatively impact our results of operations; |
| • | we may encounter difficulties in assimilating and integrating the business, technologies, products, personnel or operations of companies that we acquire, particularly if key personnel of the acquired company decide not to work for us; |
| • | an acquisition may disrupt our ongoing business, divert resources, increase our expenses and distract our management; |
| • | we may be required to implement or improve internal controls, procedures and policies appropriate for a public company at a business that prior to the acquisition lacked these controls, procedures and policies; |
| • | the acquired businesses may have unexpected liabilities that we will be forced to assume; |
| • | the acquired businesses, products or technologies may not generate sufficient revenue to offset acquisition costs or to maintain our financial results; and |
| • | acquisitions may involve the entry into geographic or business markets in which we have little or no prior experience, such as our acquisition of Creatix which had operations in Slovakia. |
We cannot assure you that we will be able to identify or consummate any future acquisition on favorable terms, or at all. If we do pursue an acquisition, it is possible that we may not realize the anticipated benefits from the acquisition or that the financial markets or investors will negatively view the acquisition. Even if we successfully complete an acquisition, it could harm our business, operating results and financial condition.
Our business may not grow if consumers are not informed about the availability and accessibility of affordable health insurance.
Numerous health insurance products are available to consumers in any given market. Most of these products vary by price, benefits and other policy features. Health insurance terminology and provisions are often confusing and difficult to understand. As a result, researching, selecting and purchasing health insurance can be a complex process. We believe that this complexity has contributed to a perception held by many consumers that individual health insurance is prohibitively expensive and difficult to obtain. If consumers are not informed about the availability and accessibility of affordable health insurance, our business may not grow and our business, operating results and financial condition would be harmed.
Changes in our provision for income taxes or adverse outcomes resulting from examination of our income or other tax returns or changes in tax legislation could adversely affect our business, operating results and financial condition.
Our provision for income taxes is subject to volatility and could be adversely affected by a number of factors, including earnings differing materially from our projections, changes in the valuation of our deferred tax assets
57
Table of Contents
and liabilities, expected timing and amount of the release of any tax valuation allowances, tax effects of share-based compensation, outcomes as a result of tax examinations or by changes in tax laws, regulations, accounting principles, including accounting for uncertain tax positions, or interpretations thereof.
To the extent that our provision for income taxes is subject to volatility or adverse outcomes as a result of tax examinations, our operating results could be harmed. Significant judgment is required to determine the recognition and measurement attribute prescribed in U.S. GAAP relating to accounting for income taxes. In addition, we are subject to examinations of our income tax returns by the Internal Revenue Service, or IRS, and other tax authorities. We assess the likelihood of adverse outcomes resulting from these examinations to determine the adequacy of our provision for income taxes. There may be exposure that the outcomes from these examinations will have an adverse effect on our business, operating results and financial condition.
On March 27, 2020, in response to the COVID-19 pandemic, the Coronavirus Aid, Relief, and Economic Security Act (the “CARES Act”) was signed into law. The CARES Act, among other things, includes provisions relating to refundable payroll tax credits, deferment of employer side social security payments, net operating loss carryback periods, alternative minimum tax credit refunds, modifications to the net interest deduction limitations and technical corrections to tax depreciation methods for qualified improvement property. We continue to evaluate the applicability of the CARES Act to us; however, we believe that the CARES Act will not have a material impact on our business.
Risks Related to Our Intellectual Property and Technology
We rely on data provided to us by customers, carriers and third-party lead suppliers to improve our technology and service offerings, and if we are unable to maintain or grow such data, we may be unable to provide customers with an insurance shopping experience that is relevant, efficient and effective, which could adversely affect our business.
Our business relies on the data provided to us by customers, carriers and third-party lead suppliers. The large amount of data that we use in operating our marketplace platform, and the accuracy of such data, is critical to our ability to provide a relevant, efficient and effective insurance shopping experience for customers. For example, if the data provided to us by our customers during the insurance shopping process is not accurate, our ability to match our customers with relevant and suitable insurance products would be impaired, which could lead to an increase in rejections of policies that we submit to carriers. Further, if we are unable to maintain or effectively utilize the data provided to us, the value that we provide to customers and carriers may be limited as well. If we do not obtain accurate data from our consumers or if we are unable to maintain or effectively utilize the data provided to us, consumers who use our platform could have a negative shopping experience, which could materially and adversely affect our business, operating results and financial condition.
Although we have made substantial investments into our technology systems, we cannot assure you that we will be able to continually collect and retain sufficient data, or improve our data technologies to satisfy our operating needs. Failure to do so could materially and adversely affect our business, operating results and financial condition.
Our business is subject to security risks and, if we are subject to cyber-attacks, security breaches or otherwise unable to safeguard the security and privacy of confidential data, including personal health information, our business will be harmed.
Our services involve the collection and storage of confidential and personal information of consumers and employees, including protected health information subject to HIPAA and other individually identifiable health information, and the transmission of this information to their chosen carriers and to government. For example, in our online lead generation business, we collect and disclose names, contact information, date of birth, and sensitive information regarding the medical history of consumers. Information security risks have generally
58
Table of Contents
increased in recent years because of the proliferation of new technologies and the increased sophistication and activities of perpetrators of cyber-attacks. Hackers and data thieves are increasingly sophisticated and operating large-scale and complex automated attacks, including on companies within the healthcare industry. As cyber threats continue to evolve, we may be required to expend additional resources to further enhance our information security measures, develop additional protocols and/or to investigate and remediate any information security vulnerabilities.
Because our services involve the collection, processing, use, storage and transmission of confidential and personal information of consumers and employees, including protected health information subject to HIPAA and other individually identifiable health information, we are subject to various laws, regulations, industry standards and contractual requirements regarding the collection, maintenance, protection, use, transmission, disclosure and disposal of personal information. We also hold a significant amount of personal information relating to our current and former employees. We cannot guarantee that our facilities and systems, and those of our third-party service providers, will be free of security breaches, cyber-attacks, acts of vandalism, computer viruses, malware, ransomware, denial-of-service attacks, misplaced or lost data, programming and/or human errors or other similar events. Compliance with privacy and security laws, requirements and regulations may result in cost increases due to new constraints on our business, the development of new processes, the effects of potential non-compliance by us or third-party service providers, and enforcement actions. We may be required to expend significant amounts and other resources to protect against security breaches or to alleviate problems caused by security breaches and other threats to our information technology systems. Despite our implementation of security measures, techniques used to obtain unauthorized access or to sabotage systems change frequently. As a result, we may be unable to anticipate these techniques or to implement adequate preventative measures. Additionally, our third-party service providers who process information on our behalf may cause security breaches for which we are responsible.
Any compromise or perceived compromise of the security of our systems or the systems of one or more of our vendors or service providers could damage our reputation, cause the termination of relationships with government-run health insurance exchanges, carriers, and/or our customers, result in disruption or interruption to our business operations, marketing partners and carriers, reduce demand for our services and subject us to significant liability and expense as well as regulatory action and lawsuits, which would harm our business, operating results and financial condition. The CCPA, in particular, includes a private right of action for California consumers whose CCPA-covered personal information is impacted by a data security incident resulting from a company’s failure to maintain reasonable security procedures, and hence may result in civil litigation in the event of a data breach impacting such information. Although we maintain insurance covering certain security and privacy damages and claim expenses, we may not carry insurance or maintain coverage sufficient to compensate for all liability and in any event, insurance coverage would not address the reputational damage that could result from a security incident or any regulatory actions or litigation that may result. In addition, in the event that additional data security laws are implemented, or our carrier or other partners determine to impose additional requirements on us relating to data security, we may not be able to timely comply with such requirements or such requirements may not be compatible with our current processes. For example, legislators and regulators in the U.S. have enacted and are proposing new and more robust privacy and cybersecurity laws and regulations in response to increasing broad-based cyberattacks, including the CCPA and the New York SHIELD Act. New data security laws add additional complexity, requirements, restrictions and potential legal risk and compliance programs may require additional investment in resources, and could impact strategies and availability of previously useful data. Changing our processes to comply with new laws or new requirements imposed by our carriers could be time consuming and expensive, and failure to timely implement required changes could result in our inability to sell health insurance plans in a particular jurisdiction or for a particular carrier or subject us to liability for non-compliance, any of which would damage our business, operating results and financial condition. For instance, carriers may require us to be compliant with the Payment Card Industry Data Security Standard, or PCI DSS, security standards in order to accept credit card information from customers or require us to comply with privacy and security standards to do business with us at all. PCI DSS compliance and compliance with other privacy and security standards are regularly assessed, and the
59
Table of Contents
possibility exists that we may not always be compliant with the standards. If we are not in compliance, we may not be able to accept credit card information from customers to the extent needed, or conduct health insurance business, and our relationship with carriers could be adversely impacted or terminated, which would harm our business, operating results and financial condition.
We may not be able to adequately protect our intellectual property, which could harm our business and operating results.
We believe that our intellectual property is an essential asset of our business and that our technology currently gives us a competitive advantage in the distribution of Medicare-related, individual and family health insurance. We rely on a combination of copyright, trademark and trade secret laws as well as confidentiality procedures and contractual provisions to establish and protect our intellectual property rights in the United States. The efforts we have taken to protect our intellectual property may not be sufficient or effective. In addition, monitoring unauthorized uses of our intellectual property and unauthorized disclosures of our trade secrets and other confidential or proprietary information can be difficult, and even if we do detect violations, litigation may be necessary to enforce our intellectual property rights. Any enforcement efforts we undertake, including litigation, could be time-consuming and expensive, could divert our management’s attention and may result in a court determining that our intellectual property or other proprietary rights are unenforceable. If we are not successful in cost-effectively protecting our confidential information, trade secrets and other intellectual property rights, our business, operating results and financial condition could be harmed. Further, if a competitor lawfully obtains or independently develops the technology that we maintain as a trade secret, we would have no right to prevent such competitor from using that technology or proprietary information to compete with us, which could harm our competitive position.
In addition, we use open source software in connection with our proprietary software and expect to continue to use open source software in the future. Some open-source licenses, commonly referred to as “copyleft” licenses, require licensors to provide source code to licensees upon request, or prohibit licensors from charging a fee to licensees. We try to insulate our proprietary code from the effects of such “copyleft” provisions. While we have policies in place to avoid usage of software from “copyleft” licenses, and while we conduct audits and have other procedures in place in an effort to ensure these policies are followed, we cannot guarantee that these efforts will be successful. Accordingly, we may face claims from others claiming ownership of, or seeking to enforce the license terms applicable to such open source software, including by demanding release of the open source software, derivative works or our proprietary source code that was developed or distributed with such software. These claims could also result in litigation, require us to purchase a costly license or require us to devote additional research and development resources to change our software, any of which would have a negative effect on our business and results of operations. In addition, if the license terms for the open source software change, we may be forced to re-engineer our software or incur additional costs. We cannot assure you that we have not incorporated open source software into our proprietary software in a manner that may subject our proprietary software to an open source license that requires disclosure, to customers or the public, of the source code to such proprietary software. Any such disclosure would have a negative effect on our business and the value of our proprietary software.
We may become subject to intellectual property disputes, which are costly and may subject us to significant liability and increased costs of doing business.
Third parties may be able to successfully challenge, oppose, invalidate, render unenforceable, dilute, misappropriate or circumvent our trademarks, copyrights and other intellectual property rights. Our success depends, in part, on our ability to develop and commercialize our products and services without infringing, misappropriating or otherwise violating the intellectual property rights of third parties. However, we may not be aware that our products or services are infringing, misappropriating or otherwise violating third-party intellectual property rights and such third parties may bring claims alleging such infringement, misappropriation or violation.
60
Table of Contents
Actions we may take to enforce our intellectual property rights may be expensive and divert management’s attention away from the ordinary operation of our business, and our inability to secure and protect our intellectual property rights could materially and adversely affect our brand and business, operating results and financial condition. Furthermore, such enforcement actions, even if successful, may not result in an adequate remedy. In addition, many companies have the capability to dedicate greater resources to enforce their intellectual property rights and to defend claims that may be brought against them. If a third-party is able to obtain an injunction preventing us from accessing such third-party intellectual property rights, or if we cannot license or develop alternative technology for any infringing aspect of our business, we would be forced to limit or stop sales of our products and platform capabilities or cease business activities related to such intellectual property.
Although we carry general liability insurance, our insurance may not cover potential claims of this type and may not be adequate to indemnify us for all liability that may be imposed. We cannot predict the outcome of lawsuits and cannot ensure that the results of any such actions will not have an adverse effect on our business, financial condition or results of operations. Such claims could subject us to significant liability for damages and could result in our having to stop using technology found to be in violation of a third party’s rights. Further, we might be required to seek a license for third-party intellectual property, which may not be available on reasonable royalty or other terms. Alternatively, we could be required to develop alternative non-infringing technology, which could require significant effort and expense. If we cannot license or develop technology for any infringing aspect of our business, we would be forced to limit our services, which could affect our ability to compete effectively. Any of these results would harm our business, operating results and financial condition.
Risks Related to Our Indebtedness
Our debt obligations contain restrictions that impact our business and expose us to risks that could materially adversely affect our liquidity and financial condition.
The total principal amount of debt outstanding under our Credit Facilities, excluding unamortized debt discount and deferred issuance costs, as of March 31, 2020 was $415.5 million, consisting of $298.5 million and $117.0 million outstanding under our Term Loan Facility and Incremental Term Loan Facility, respectively. Our indebtedness could have significant effects on our business, such as:
| • | limiting our ability to borrow additional amounts to fund capital expenditures, acquisitions, debt service requirements, execution of our growth strategy and other purposes; |
| • | limiting our ability to make investments, including acquisitions, loans and advances, and to sell, transfer or otherwise dispose of assets; |
| • | requiring us to dedicate a substantial portion of our cash flow from operations to pay principal and interest on our borrowings, which would reduce availability of our cash flow to fund working capital, capital expenditures, acquisitions, execution of our growth strategy and other general corporate purposes; |
| • | making us more vulnerable to adverse changes in general economic, industry and competitive conditions, in government regulation and in our business by limiting our ability to plan for and react to changing conditions; |
| • | placing us at a competitive disadvantage compared with our competitors that have less debt; and |
| • | exposing us to risks inherent in interest rate fluctuations because our borrowings are at variable rates of interest, which could result in higher interest expense in the event of increases in interest rates. |
In addition, we may not be able to generate sufficient cash flow from our operations to repay our indebtedness when it becomes due and to meet our other cash needs. If we are not able to pay our borrowings as they become due, we will be required to pursue one or more alternative strategies, such as selling assets, refinancing or restructuring our indebtedness or selling additional debt or equity securities. We may not be able to refinance our debt or sell additional debt or equity securities or our assets on favorable terms, if at all, and if we must sell our assets, it may negatively affect our business, financial condition and results of operations.
61
Table of Contents
Restrictions imposed by our Credit Facilities may materially limit our ability to operate our business and finance our future operations or capital needs.
The terms of our Credit Facilities restrict us and our restricted subsidiaries from engaging in specified types of transactions. These covenants restrict our ability, and that of our restricted subsidiaries, to, among other things:
| • | incur indebtedness; |
| • | incur certain liens; |
| • | consolidate, merge or sell or otherwise dispose of assets; |
| • | make investments, loans, advances, guarantees and acquisitions; |
| • | pay dividends or make other distributions on equity interests, or redeem, repurchase or retire equity interests; |
| • | enter into transactions with affiliates; |
| • | alter the business conducted by us and our subsidiaries; |
| • | change their fiscal year; and |
| • | amend or modify governing documents. |
A breach of any of these covenants, or any other covenant in the documents governing our Credit Facilities, could result in a default or event of default under our Credit Facilities. In the event of any event of default under our Credit Facilities, the applicable lenders or agents could elect to terminate borrowing commitments and declare all borrowings and loans outstanding thereunder, together with accrued and unpaid interest and any fees and other obligations, to be immediately due and payable. In addition, or in the alternative, the applicable lenders or agents could exercise their rights under the security documents entered into in connection with our Credit Facilities. We have pledged substantially all of our assets as collateral securing our Credit Facilities and any such exercise of remedies on any material portion of such collateral would likely materially adversely affect our business, financial condition or results of operations.
If we were unable to repay or otherwise refinance these borrowings and loans when due, and the applicable lenders proceeded against the collateral granted to them to secure that indebtedness, we may be forced into bankruptcy or liquidation. In the event the applicable lenders accelerate the repayment of our borrowings, we may not have sufficient assets to repay that indebtedness. Any acceleration of amounts due under our Credit Facilities or other outstanding indebtedness would also likely have a material adverse effect on us.
Pursuant to our Credit Agreement, we are required to maintain, on a consolidated basis, a maximum ratio of consolidated total net debt to consolidated EBITDA (with certain adjustments as set forth in the Credit Agreement), tested as of the last day of the most recently completed four consecutive fiscal quarters. Our ability to borrow under our Credit Agreement depends on our compliance with this financial covenant. Events beyond our control, including changes in general economic and business conditions, may affect our ability to satisfy the financial covenant. We cannot assure you that we will satisfy the financial covenant in the future, or that our lenders will waive any failure to satisfy the financial covenant.
Developments with respect to LIBOR may affect our borrowings under our Credit Facilities.
Regulators and law enforcement agencies in the U.K. and elsewhere are conducting civil and criminal investigations into whether the banks that contribute to the British Bankers’ Association (“BBA”) in connection with the calculation of daily LIBOR may have been under-reporting or otherwise manipulating or attempting to manipulate LIBOR. A number of BBA member banks have entered into settlements with their regulators and law enforcement agencies with respect to this alleged manipulation of LIBOR. Actions by the BBA, regulators or law enforcement agencies may result in changes to the manner in which LIBOR is determined or the establishment of alternative reference rates. For example, on July 27, 2017, the U.K. Financial Conduct Authority announced that it intends to stop persuading or compelling banks to submit LIBOR quotes after 2021.
62
Table of Contents
Our Credit Agreement provides that interest may be based on LIBOR and for the use of an alternate rate to LIBOR in the event LIBOR is phased-out; however, uncertainty remains as to any such replacement rate and any such replacement rate may be higher or lower than LIBOR may have been. The establishment of alternative reference rates or implementation of any other potential changes may materially and adversely affect our business, operating results and financial condition.
Risks Related to Our Organizational Structure
Our principal asset after the completion of this offering will be our interest in GoHealth Holdings, LLC, and, as a result, we will depend on distributions from GoHealth Holdings, LLC to pay our taxes and expenses, including payments under the Tax Receivable Agreement. GoHealth Holdings, LLC’s ability to make such distributions may be subject to various limitations and restrictions.
Upon the consummation of this offering and the Transactions, we will be a holding company and will have no material assets other than our ownership of LLC Interests. As such, we will have no independent means of generating revenue or cash flow, and our ability to pay our taxes and operating expenses or declare and pay dividends in the future, if any, will be dependent upon the financial results and cash flows of GoHealth Holdings, LLC and its subsidiaries and distributions we receive from GoHealth Holdings, LLC. There can be no assurance that GoHealth Holdings, LLC and its subsidiaries will generate sufficient cash flow to distribute funds to us or that applicable state law and contractual restrictions, including negative covenants in our debt instruments, will permit such distributions. Although GoHealth Holdings, LLC is not currently subject to any debt instruments or other agreements that would restrict its ability to make distributions to us, the terms of our Credit Facilities and other outstanding indebtedness restrict the ability of our subsidiaries to pay dividends to GoHealth Holdings, LLC.
GoHealth Holdings, LLC will continue to be treated as a partnership for U.S. federal income tax purposes and, as such, generally will not be subject to any entity-level U.S. federal income tax. Instead, any taxable income of GoHealth Holdings, LLC will be allocated to holders of LLC Interests, including us. Accordingly, we will incur income taxes on our allocable share of any net taxable income of GoHealth Holdings, LLC. Under the terms of the GoHealth Holdings, LLC Agreement, GoHealth Holdings, LLC will be obligated, subject to various limitations and restrictions, including with respect to our debt agreements, to make tax distributions to holders of LLC Interests, including us. In addition to tax expenses, we will also incur expenses related to our operations, including payments under the Tax Receivable Agreement, which we expect could be significant. See “Certain Relationships and Related Party Transactions—Tax Receivable Agreement.” We intend, as its managing member, to cause GoHealth Holdings, LLC to make cash distributions to the holders of LLC Interests in an amount sufficient to (1) fund all or part of their tax obligations in respect of taxable income allocated to them and (2) cover our operating expenses, including payments under the Tax Receivable Agreement. However, GoHealth Holdings, LLC’s ability to make such distributions may be subject to various limitations and restrictions, such as restrictions on distributions that would either violate any contract or agreement to which GoHealth Holdings, LLC is then a party, including debt agreements, or any applicable law, or that would have the effect of rendering GoHealth Holdings, LLC insolvent. If we do not have sufficient funds to pay tax or other liabilities, or to fund our operations (including, if applicable, as a result of an acceleration of our obligations under the Tax Receivable Agreement), we may have to borrow funds, which could materially and adversely affect our liquidity and financial condition, and subject us to various restrictions imposed by any lenders of such funds. To the extent we are unable to make timely payments under the Tax Receivable Agreement for any reason, such payments generally will be deferred and will accrue interest until paid; provided, however, that nonpayment for a specified period may constitute a material breach of a material obligation under the Tax Receivable Agreement resulting in the acceleration of payments due under the Tax Receivable Agreement. See “Certain Relationships and Related Party Transactions—Tax Receivable Agreement” and “Certain Relationships and Related Party Transactions— GoHealth Holdings, LLC Agreement—Agreement in Effect Upon Consummation of the Transactions—Distributions.” In addition, if GoHealth Holdings, LLC does not have sufficient funds to make distributions, our ability to declare and pay cash dividends will also be restricted or impaired. See “—Risks Related to the Offering and Ownership of our Class A Common Stock” and “Dividend Policy.”
63
Table of Contents
Under the GoHealth Holdings, LLC Agreement, we intend to cause GoHealth Holdings, LLC, from time to time, to make distributions in cash to its equityholders (including us) in amounts sufficient to cover the taxes imposed on their allocable share of taxable income of GoHealth Holdings, LLC. As a result of (1) potential differences in the amount of net taxable income allocable to us and to GoHealth Holdings, LLC’s other equityholders, (2) the lower tax rate applicable to corporations as opposed to individuals, and (3) certain tax benefits that we anticipate from (a) future purchases or redemptions of LLC Interests from the Continuing Equity Owners, (b) payments under the Tax Receivable Agreement and (c) any acquisition of interests in GoHealth Holdings, LLC from other equityholders in connection with the consummation of the Transactions, these tax distributions may be in amounts that exceed our tax liabilities. Our board of directors will determine the appropriate uses for any excess cash so accumulated, which may include, among other uses, the payment of obligations under the Tax Receivable Agreement and the payment of other expenses. We will have no obligation to distribute such cash (or other available cash) to our stockholders. No adjustments to the exchange ratio for LLC Interests and corresponding shares of Class A common stock will be made as a result of any cash distribution by us or any retention of cash by us. To the extent we do not distribute such excess cash as dividends on our Class A common stock we may take other actions with respect to such excess cash, for example, holding such excess cash, or lending it (or a portion thereof) to GoHealth Holdings, LLC, which may result in shares of our Class A common stock increasing in value relative to the value of LLC Interests. The holders of LLC Interests may benefit from any value attributable to such cash balances if they acquire shares of Class A common stock in exchange for their LLC Interests, notwithstanding that such holders may have participated previously as holders of LLC Interests in distributions that resulted in such excess cash balances.
The Tax Receivable Agreement with the Continuing Equity Owners requires us to make cash payments to them in respect of certain tax benefits to which we may become entitled, and we expect that such payments will be substantial.
In connection with the consummation of this offering, we will enter into a Tax Receivable Agreement with GoHealth Holdings, LLC and each of the Continuing Equity Owners and Blocker Shareholders. Under the Tax Receivable Agreement, we will be required to make cash payments to the Continuing Equity Owners and the Blocker Shareholders equal to 85% of the tax benefits, if any, that we actually realize, or in certain circumstances are deemed to realize, as a result of (1) GoHealth, Inc.’s allocable share of existing tax basis acquired in connection with the Transactions (including the Blocker Company’s share of existing tax basis) and increases to such allocable share of existing tax basis; (2) the increases in our share of the tax basis of assets of GoHealth Holdings, LLC resulting from (a) the purchase of LLC Interests directly from GoHealth Holdings, LLC and the partial redemption of LLC Interests by GoHealth Holdings, LLC as described under “Use of Proceeds,” (b) any future redemptions or exchanges of LLC Interests from the Continuing Equity Owners as described under “Certain Relationships and Related Party Transactions—GoHealth Holdings, LLC Agreement—Agreement in Effect Upon Consummation of the Transactions—Common Unit Redemption Right,” and (c) certain distributions (or deemed distributions) by GoHealth Holdings, LLC; and (3) certain other tax benefits arising from payments under the Tax Receivable Agreement. We expect that the amount of the cash payments we will be required to make under the Tax Receivable Agreement will be substantial. Any payments made by us to the Continuing Equity Owners and the Blocker Shareholders under the Tax Receivable Agreement will not be available for reinvestment in our business and will generally reduce the amount of overall cash flow that might have otherwise been available to us. To the extent that we are unable to make timely payments under the Tax Receivable Agreement for any reason, the unpaid amounts will be deferred and will accrue interest until paid by us. Payments under the Tax Receivable Agreement are not conditioned upon one or more of the Continuing Equity Owners maintaining a continued ownership interest in GoHealth Holdings, LLC. Furthermore, our future obligation to make payments under the Tax Receivable Agreement could make us a less attractive target for an acquisition, particularly in the case of an acquirer that cannot use some or all of the tax benefits that are the subject of the Tax Receivable Agreement. For more information, see “Certain Relationships and Related Party Transactions—Tax Receivable Agreement.” The existing tax basis acquired in connection with the Transactions, the actual increase in tax basis, and the actual utilization of any resulting tax benefits, as well as the amount and timing of any payments under the Tax Receivable Agreement, will vary depending upon a number of factors:
64
Table of Contents
including the timing of redemptions by the Continuing Equity Owners; the price of shares of our Class A common stock at the time of the exchange; the extent to which such exchanges are taxable; the amount of gain recognized by such Continuing Equity Owners; the amount and timing of the taxable income allocated to us or otherwise generated by us in the future; the portion of our payments under the Tax Receivable Agreement constituting imputed interest; and the federal and state tax rates then applicable.
Our organizational structure, including the Tax Receivable Agreement, confers certain benefits upon the Continuing Equity Owners that will not benefit holders of our Class A common stock to the same extent that it will benefit the Continuing Equity Owners.
Our organizational structure, including the Tax Receivable Agreement, confers certain benefits upon the Continuing Equity Owners that will not benefit the holders of our Class A common stock to the same extent that it will benefit the Continuing Equity Owners. We will enter into the Tax Receivable Agreement with GoHealth Holdings, LLC and the Continuing Equity Owners and the Blocker Shareholders in connection with the completion of this offering and the Transactions, which will provide for the payment by us to the Continuing Equity Owners and the Blocker Shareholders of 85% of the amount of tax benefits, if any, that we actually realize, or in some circumstances are deemed to realize, as a result of (1) GoHealth, Inc.’s allocable share of existing tax basis acquired in connection with the Transactions (including the Blocker Company’s share of existing tax basis) and increases to such allocable share of existing tax basis; (2) the increases in our share of the tax basis of assets of GoHealth Holdings, LLC resulting from (a) the purchase of LLC Interests directly from GoHealth Holdings, LLC and, the partial redemption of LLC Interests by GoHealth Holdings, LLC as described under “Use of Proceeds,” (b) any future redemptions or exchanges of LLC Interests from the Continuing Equity Owners as described under “Certain Relationships and Related Party Transactions— GoHealth Holdings, LLC Agreement—Agreement in Effect Upon Consummation of the Transactions—Common Unit Redemption Right” and (c) certain distributions (or deemed distributions) by GoHealth Holdings, LLC; and (3) certain other tax benefits arising from payments under the Tax Receivable Agreement. See “Certain Relationships and Related Party Transactions—Tax Receivable Agreement.” Although we will retain 15% of the amount of such tax benefits, this and other aspects of our organizational structure may adversely impact the future trading market for the Class A common stock.
In certain cases, payments under the Tax Receivable Agreement to the Continuing Equity Owners and the Blocker Shareholders may be accelerated or significantly exceed any actual benefits we realize in respect of the tax attributes subject to the Tax Receivable Agreement.
The Tax Receivable Agreement will provide that if (1) we materially breach any of our material obligations under the Tax Receivable Agreement, (2) certain mergers, asset sales, other forms of business combinations or other changes of control were to occur after the consummation of this offering, or (3) we elect an early termination of the Tax Receivable Agreement, then our obligations, or our successor’s obligations, under the Tax Receivable Agreement to make payments would be based on certain assumptions, including an assumption that we would have sufficient taxable income to fully utilize all potential future tax benefits that are subject to the Tax Receivable Agreement.
As a result of the foregoing, we would be required to make an immediate cash payment equal to the present value of the anticipated future tax benefits that are the subject of the Tax Receivable Agreement, based on certain assumptions, which payment may be made significantly in advance of the actual realization, if any, of such future tax benefits. We could also be required to make cash payments to the Continuing Equity Owners and the Blocker Shareholders that are greater than the specified percentage of any actual benefits we ultimately realize in respect of the tax benefits that are subject to the Tax Receivable Agreement. In these situations, our obligations under the Tax Receivable Agreement could have a substantial negative impact on our liquidity and could have the effect of delaying, deferring or preventing certain mergers, asset sales, other forms of business combinations or other changes of control. There can be no assurance that we will be able to fund or finance our obligations under the Tax Receivable Agreement. We may need to incur debt to finance payments under the Tax Receivable
65
Table of Contents
Agreement to the extent our cash resources are insufficient to meet our obligations under the Tax Receivable Agreement as a result of timing discrepancies or otherwise.
We will not be reimbursed for any payments made to the Continuing Equity Owners and the Blocker Shareholders under the Tax Receivable Agreement in the event that any tax benefits are disallowed.
Payments under the Tax Receivable Agreement will be based on the tax reporting positions that we determine, and the U.S. Internal Revenue Service, or the IRS, or another tax authority, may challenge all or part of the tax basis increases or other tax benefits we claim, as well as other related tax positions we take, and a court could sustain such challenge. If the outcome of any such challenge would reasonably be expected to materially and adversely affect a recipient’s payments under the Tax Receivable Agreement, then we will not be permitted to settle or fail to contest such challenge without the consent (not to be unreasonably withheld or delayed) of Centerbridge and the Founders. The interests of Centerbridge or the Founders in any such challenge may differ from or conflict with our interests and your interests, and Centerbridge or the Founders may exercise their consent rights relating to any such challenge in a manner adverse to our interests and your interests. We will not be reimbursed for any cash payments previously made to the Continuing Equity Owners and the Blocker Shareholders under the Tax Receivable Agreement in the event that any tax benefits initially claimed by us and for which payment has been made to a Continuing Equity Owner or a Blocker Shareholder are subsequently challenged by a taxing authority and are ultimately disallowed. Instead, any excess cash payments made by us to a Continuing Equity Owner and/or a Blocker Shareholder, as applicable, will be netted against any future cash payments we might otherwise be required to make to such Continuing Equity Owner and/or such Blocker Shareholder, under the terms of the Tax Receivable Agreement. However, we might not determine that we have effectively made an excess cash payment to a Continuing Equity Owner and/or a Blocker Shareholder, as applicable, for a number of years following the initial time of such payment and, if any of our tax reporting positions are challenged by a taxing authority, we will not be permitted to reduce any future cash payments under the Tax Receivable Agreement until any such challenge is finally settled or determined. Moreover, the excess cash payments we made previously under the Tax Receivable Agreement could be greater than the amount of future cash payments against which we would otherwise be permitted to net such excess. The applicable U.S. federal income tax rules for determining applicable tax benefits we may claim are complex and factual in nature, and there can be no assurance that the IRS or a court will not disagree with our tax reporting positions. As a result, payments could be made under the Tax Receivable Agreement significantly in excess of any actual cash tax savings that we realize in respect of the tax attributes with respect to a Continuing Equity Owner and/or a Blocker Shareholder that are the subject of the Tax Receivable Agreement.
Unanticipated changes in effective tax rates or adverse outcomes resulting from examination of our income or other tax returns could adversely affect our results of operations and financial condition.
We are subject to taxes by the U.S. federal, state, local and foreign tax authorities. Our future effective tax rates could be subject to volatility or adversely affected by a number of factors, including:
| • | allocation of expenses to and among different jurisdictions; |
| • | changes in the valuation of our deferred tax assets and liabilities; |
| • | expected timing and amount of the release of any tax valuation allowances; |
| • | tax effects of stock-based compensation; |
| • | costs related to intercompany restructurings; |
| • | changes in tax laws, tax treaties, regulations or interpretations thereof; or |
| • | lower than anticipated future earnings in jurisdictions where we have lower statutory tax rates and higher than anticipated future earnings in jurisdictions where we have higher statutory tax rates. |
66
Table of Contents
In addition, we may be subject to audits of our income, sales and other taxes by U.S. federal, state, and local and foreign taxing authorities. Outcomes from these audits could have an adverse effect on our operating results and financial condition.
If we were deemed to be an investment company under the Investment Company Act of 1940, as amended, or the 1940 Act, including as a result of our ownership of GoHealth Holdings, LLC, applicable restrictions could make it impractical for us to continue our business as contemplated and could have a material adverse effect on our business.
Under Sections 3(a)(1)(A) and (C) of the 1940 Act, a company generally will be deemed to be an “investment company” for purposes of the 1940 Act if (1) it is, or holds itself out as being, engaged primarily, or proposes to engage primarily, in the business of investing, reinvesting or trading in securities, or (2) it engages, or proposes to engage, in the business of investing, reinvesting, owning, holding or trading in securities and it owns or proposes to acquire investment securities having a value exceeding 40% of the value of its total assets (exclusive of U.S. government securities and cash items) on an unconsolidated basis. We do not believe that we are an “investment company,” as such term is defined in either of those sections of the 1940 Act.
We and GoHealth Holdings, LLC intend to conduct our operations so that we will not be deemed an investment company. As the sole managing member of GoHealth Holdings, LLC, we will control and operate GoHealth Holdings, LLC. On that basis, we believe that our interest in GoHealth Holdings, LLC is not an “investment security” as that term is used in the 1940 Act. However, if we were to cease participation in the management of GoHealth Holdings, LLC, or if GoHealth Holdings, LLC itself becomes an investment company, our interest in GoHealth Holdings, LLC could be deemed an “investment security” for purposes of the 1940 Act.
We and GoHealth Holdings, LLC intend to conduct our operations so that we will not be deemed an investment company. If it were established that we were an unregistered investment company, there would be a risk that we would be subject to monetary penalties and injunctive relief in an action brought by the SEC, that we would be unable to enforce contracts with third parties and that third parties could seek to obtain rescission of transactions undertaken during the period it was established that we were an unregistered investment company. If we were required to register as an investment company, restrictions imposed by the 1940 Act, including limitations on our capital structure and our ability to transact with affiliates, could make it impractical for us to continue our business as contemplated and could have a material adverse effect on our business.
Risks Related to the Offering and Ownership of our Class A Common Stock
The Continuing Equity Owners will continue to have significant influence over us after this offering, including control over decisions that require the approval of stockholders.
Upon consummation of this offering, the Continuing Equity Owners will control, in the aggregate, approximately % of the voting power represented by all our outstanding classes of stock. In addition, certain of our directors, officers and employees have indicated an interest to purchase an aggregate of up to 5% of the Class A common stock in this offering at the initial public offering price in the Directed Share Program. If such directors, officers or employees purchase all shares they have indicated interests in purchasing under the Directed Share Program, our directors, officers, holders of 5% or more of our capital stock and their respective affiliates will control, in the aggregate, approximately % of the voting power represented by all of our outstanding classes of stock upon consummation of this offering (based on the assumed initial public offering price of $ per share, the midpoint of the estimated price range set forth on the cover page of this prospectus and assuming no exercise of the underwriters’ option to purchase additional shares and no exercise of outstanding options). As a result, the Continuing Equity Owners will continue to exercise significant influence over all matters requiring stockholder approval, including the election and removal of directors and the size of our board, any amendment of our amended and restated certificate of incorporation or bylaws and any approval of significant corporate transactions (including a sale of all or substantially all of our assets), and will continue to have significant control over our business, affairs and policies, including the appointment of our management.
67
Table of Contents
The directors the Continuing Equity Owners elect have the authority to incur additional debt, issue or repurchase stock, declare dividends and make other decisions that could be detrimental to stockholders.
We expect that members of our board will continue to be appointed by and/or affiliated with the Continuing Equity Owners who will have the ability to appoint the majority of directors. The Continuing Equity Owners can take actions that have the effect of delaying or preventing a change of control of us or discouraging others from making tender offers for our shares, which could prevent stockholders from receiving a premium for their shares. These actions may be taken even if other stockholders oppose them. The concentration of voting power with the Continuing Equity Owners may have an adverse effect on the price of our Class A common stock. The Continuing Equity Owners may have interests that are different from yours and may vote in a way with which you disagree and that may be adverse to your interests.
Further, our amended and restated certificate of incorporation, which will be in effect upon the consummation of the Transactions, will provide that the doctrine of “corporate opportunity” will not apply with respect to any director or stockholder who is not employed by us or our subsidiaries. See “—Our amended and restated certificate of incorporation provides that the doctrine of “corporate opportunity” will not apply with respect to any director or stockholder who is not employed by us or our subsidiaries.”
Centerbridge and its affiliates, a Continuing Equity Owner, engage in a broad spectrum of activities. In the ordinary course of its business activities, Centerbridge and its affiliates may engage in activities where their interests conflict with our interests or those of our other stockholders. Centerbridge or one of its affiliates may also pursue acquisition opportunities that may be complementary to our business, and, as a result, those acquisition opportunities may not be available to us. In addition, Centerbridge may have an interest in us pursuing acquisitions, divestitures and other transactions that, in its judgment, could enhance its investment, even though such transactions might involve risks to you. See “Description of Capital Stock—Corporate Opportunity Doctrine.”
We cannot predict the effect our dual class structure may have on the market price of our Class A common stock.
We cannot predict whether our dual class structure will result in a lower or more volatile market price of our Class A common stock, in adverse publicity, or other adverse consequences. For example, certain index providers have announced restrictions on including companies with multiple-class share structures in certain of their indices. In July 2017, FTSE Russell announced that it plans to require new constituents of its indices to have greater than 5% of the company’s voting rights in the hands of public stockholders, and S&P Dow Jones announced that it will no longer admit companies with multiple-class share structures to certain of its indices. Affected indices include the Russell 2000 and the S&P 500, S&P MidCap 400, and S&P SmallCap 600, which together make up the S&P Composite 1500. Also in 2017, MSCI, a leading stock index provider, opened public consultations on their treatment of no-vote and multi-class structures and temporarily barred new multi-class listings from certain of its indices and in October 2018, MSCI announced its decision to include equity securities “with unequal voting structures” in its indices and to launch a new index that specifically includes voting rights in its eligibility criteria. Under such announced policies, the dual class structure of our stock would make us ineligible for inclusion in certain indices and, as a result, mutual funds, exchange-traded funds and other investment vehicles that attempt to track those indices would not invest in our Class A common stock. These policies are relatively new and it is unclear what effect, if any, they will have on the valuations of publicly-traded companies excluded from such indices, but it is possible they may depress valuations, compared to similar companies that are included. Given the sustained flow of investment funds into passive strategies that seek to track certain indices, exclusion from certain stock indices would likely preclude investment by many of these funds and could make our Class A common stock less attractive to other investors. As a result, the market price of our Class A common stock could be adversely affected.
68
Table of Contents
We are a “controlled company” within the meaning of the Nasdaq rules and, as a result, will qualify for, and intend to rely on, exemptions from certain corporate governance requirements. You may not have the same protections afforded to stockholders of companies that are subject to such corporate governance requirements.
After the consummation of the Transactions, will have more than 50% of the voting power for the election of directors, and, as a result, we will be considered a “controlled company” within the meaning of the Nasdaq rules. As such, we will qualify for, and intend to rely on, exemptions from certain corporate governance requirements, including the requirements to have a majority of independent directors on our board of directors, an entirely independent nominating and corporate governance committee, an entirely independent compensation committee or to perform annual performance evaluations of the nominating and corporate governance and compensation committees.
The corporate governance requirements and, specifically, the independence standards are intended to ensure directors who are considered independent are free of any conflicting interest that could influence their actions as directors. Following this offering, we intend to utilize certain exemptions afforded to a “controlled company.” As a result, we will not be subject to certain corporate governance requirements, including that a majority of our board of directors consists of “independent directors,” as defined under the Nasdaq rules. In addition, we will not be required to have a nominating and corporate governance committee or compensation committee that is composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities, or to conduct annual performance evaluations of the nominating and corporate governance and compensation committees.
Accordingly, you may not have the same protections afforded to stockholders of companies that are subject to all of the corporate governance requirements of the Nasdaq rules. Our status as a controlled company could make our Class A common stock less attractive to some investors or otherwise harm our stock price.
Certain provisions of Delaware law and antitakeover provisions in our organizational documents could delay or prevent a change of control.
Certain provisions of Delaware law and our amended and restated certificate of incorporation and amended and restated bylaws may have an antitakeover effect and may delay, defer, or prevent a merger, acquisition, tender offer, takeover attempt or other change of control transaction that a stockholder might consider in its best interest, including those attempts that might result in a premium over the market price for the shares held by our stockholders. These provisions provide for, among other things:
| • | a classified board of directors with staggered three-year terms; |
| • | the ability of our board of directors to issue one or more series of preferred stock; |
| • | advance notice for nominations of directors by stockholders and for stockholders to include matters to be considered at our annual meetings; |
| • | certain limitations on convening special stockholder meetings; |
| • | prohibit cumulative voting in the election of directors; |
| • | the removal of directors only for cause and only upon the affirmative vote of the holders of at least 662/3% of the voting power represented by our then-outstanding common stock; and |
| • | that certain provisions of amended and restated certificate of incorporation may be amended only by the affirmative vote of at least 662/3% of the voting power represented by our then-outstanding common stock. |
These antitakeover provisions could make it more difficult for a third party to acquire us, even if the third party’s offer may be considered beneficial by many of our stockholders. As a result, our stockholders may be limited in their ability to obtain a premium for their shares.
69
Table of Contents
In addition, we have opted out of Section 203 of the General Corporation Law of the State of Delaware, which we refer to as the DGCL, but our amended and restated certificate of incorporation will provide that engaging in any of a broad range of business combinations with any “interested” stockholder (any stockholder with % or more of our voting stock) for a period of three years following the date on which the stockholder became an “interested” stockholder is prohibited, subject to certain exceptions. See “Description of Capital Stock.”
The JOBS Act will allow us to postpone the date by which we must comply with certain laws and regulations intended to protect investors and to reduce the amount of information we provide in our reports filed with the SEC. We cannot be certain if this reduced disclosure will make our Class A common stock less attractive to investors.
The JOBS Act is intended to reduce the regulatory burden on “emerging growth companies.” As defined in the JOBS Act, a public company whose initial public offering of common equity securities occurs after December 8, 2011, and whose annual net revenues are less than $1.07 billion will, in general, qualify as an “emerging growth company” until the earliest of:
| • | the last day of its fiscal year following the fifth anniversary of the date of its initial public offering of common equity securities; |
| • | the last day of its fiscal year in which it has annual gross revenue of $1.07 billion or more; |
| • | the date on which it has, during the previous three-year period, issued more than $1.07 billion in nonconvertible debt; and |
| • | the date on which it is deemed to be a “large accelerated filer, ” which will occur at such time as the company (1) has an aggregate worldwide market value of common equity securities held by non-affiliates of $700 million or more as of the last business day of its most recently completed second fiscal quarter, (2) has been required to file annual and quarterly reports under the Securities Exchange Act of 1934, as amended, or the Exchange Act, for a period of at least 12 months, and (3) has filed at least one annual report pursuant to the Exchange Act. |
Under this definition, we will be an “emerging growth company” upon completion of this offering and could remain an “emerging growth company” until as late as the fifth anniversary of the completion of this offering. For so long as we are an “emerging growth company,” we will, among other things:
| • | not be required to comply with the auditor attestation requirements of Section 404(b) of the Sarbanes-Oxley Act; |
| • | not be required to hold a nonbinding advisory stockholder vote on executive compensation pursuant to Section 14A(a) of the Exchange Act; |
| • | not be required to seek stockholder approval of any golden parachute payments not previously approved pursuant to Section 14A(b) of the Exchange Act; |
| • | be exempt from the requirement of the Public Company Accounting Oversight Board, or PCAOB, regarding the communication of critical audit matters in the auditor’s report on the financial statements; and |
| • | be subject to reduced disclosure obligations regarding executive compensation in our periodic reports and proxy statements. |
In addition, Section 107 of the JOBS Act provides that an emerging growth company can use the extended transition period provided in Section 7(a)(2)(B) of the Securities Act for complying with new or revised accounting standards. This permits an emerging growth company to delay the adoption of certain accounting standards until those standards would otherwise apply to private companies. We have elected to use this extended transition period and, as a result, our consolidated financial statements may not be comparable to the financial statements of issuers who are required to comply with the effective dates for new or revised accounting standards that are applicable to public companies.
70
Table of Contents
We cannot predict if investors will find our Class A common stock less attractive as a result of our decision to take advantage of some or all of the reduced disclosure requirements above. If some investors find our Class A common stock less attractive as a result, there may be a less active trading market for our Class A common stock and our stock price may be more volatile.
Our management team will have immediate and broad discretion over the use of the net proceeds from this offering and may not use them effectively.
We currently intend to use a portion of the net proceeds of this offering for general corporate purposes to support the growth of the business. See “Use of Proceeds.” Our management will have broad discretion in the application of the net proceeds. Our shareholders may not agree with how our management chooses to allocate the net proceeds from this offering. The failure by our management to apply these funds effectively could have a material adverse effect on our business, financial condition, and results of operations. Pending their use, we may invest the net proceeds from this offering in a manner that does not produce income. The decisions made by our management may not result in positive returns on your investment and you will not have an opportunity to evaluate the economic, financial, or other information upon which our management bases its decisions.
Because we have no current plans to pay regular cash dividends on our Class A common stock following this offering, you may not receive any return on investment unless you sell your Class A common stock for a price greater than that which you paid for it.
We do not anticipate paying any regular cash dividends on our Class A common stock following this offering. Any decision to declare and pay dividends in the future will be made at the discretion of our board of directors and will depend on, among other things, general and economic conditions, our results of operations and financial condition, our available cash and current and anticipated cash needs, capital requirements, contractual, legal, tax and regulatory restrictions, and such other factors that our board of directors may deem relevant. In addition, our ability to pay dividends is, and may be, limited by covenants of existing and any future outstanding indebtedness we or our subsidiaries incur, including under our Credit Facilities. Therefore, any return on investment in our Class A common stock is solely dependent upon the appreciation of the price of our Class A common stock on the open market, which may not occur. See “Dividend Policy” for more detail.
No market currently exists for our Class A common stock, and an active, liquid trading market for our Class A common stock may not develop, which may cause our Class A common stock to trade at a discount from the initial offering price and make it difficult for you to sell the Class A common stock you purchase.
Prior to this offering, there has not been a public market for our Class A common stock. We cannot predict the extent to which investor interest in us will lead to the development of a trading market or how active and liquid that market may become. If an active and liquid trading market does not develop or continue, you may have difficulty selling any of our Class A common stock that you purchase at a price above the price you purchase it or at all. The initial public offering price for the shares was determined by negotiations between us and the underwriters and may not be indicative of prices that will prevail in the open market following this offering. The failure of an active and liquid trading market to develop and continue would likely have a material adverse effect on the value of our Class A common stock. The market price of our Class A common stock may decline below the initial offering price, and you may not be able to sell your shares of our Class A common stock at or above the price you paid in this offering, or at all. An inactive market may also impair our ability to raise capital to continue to fund operations by selling shares and may impair our ability to acquire other companies or technologies by using our shares as consideration.
71
Table of Contents
Our amended and restated certificate of incorporation will provide that the Court of Chancery of the State of Delaware will be the sole and exclusive forum for certain stockholder litigation matters and the federal district courts of the United States shall be the exclusive forum for the resolution of any complaint asserting a cause of action arising under the Securities Act, which could limit our stockholders’ ability to obtain a favorable judicial forum for disputes with us or our directors, officers, employees or stockholders.
Our amended and restated certificate of incorporation will provide (A) (i) any derivative action or proceeding brought on behalf of the Company, (ii) any action asserting a claim of breach of a fiduciary duty owed by any current or former director, officer, other employee or stockholder of the Company to the Company or the Company’s stockholders, (iii) any action asserting a claim arising pursuant to any provision of the DGCL, our amended and restated certificate of incorporation or our amended and restated bylaws (as either may be amended or restated) or as to which the DGCL confers jurisdiction on the Court of Chancery of the State of Delaware or (iv) any action asserting a claim governed by the internal affairs doctrine of the law of the State of Delaware shall, to the fullest extent permitted by law, be exclusively brought in the Court of Chancery of the State of Delaware or, if such court does not have subject matter jurisdiction thereof, the federal district court of the State of Delaware; and (B) the federal district courts of the United States shall be the exclusive forum for the resolution of any complaint asserting a cause of action arising under the Securities Act. Notwithstanding the foregoing, the exclusive forum provision shall not apply to claims seeking to enforce any liability or duty created by the Exchange Act. The choice of forum provision may limit a stockholder’s ability to bring a claim in a judicial forum that it finds favorable for disputes with us or our directors, officers, or other employees, which may discourage such lawsuits against us and our directors, officers, and other employees, although our stockholders will not be deemed to have waived our compliance with federal securities laws and the rules and regulations thereunder. Alternatively, if a court were to find the choice of forum provision contained in our amended and restated certificate of incorporation to be inapplicable or unenforceable in an action, we may incur additional costs associated with resolving such action in other jurisdictions, which could harm our business, results of operations, and financial condition. Any person or entity purchasing or otherwise acquiring any interest in shares of our capital stock shall be deemed to have notice of and consented to the forum provisions in our amended and restated certificate of incorporation.
Our amended and restated certificate of incorporation provides that the doctrine of “corporate opportunity” will not apply with respect to any director or stockholder who is not employed by us or our subsidiaries.
The doctrine of corporate opportunity generally provides that a corporate fiduciary may not develop an opportunity using corporate resources, acquire an interest adverse to that of the corporation or acquire property that is reasonably incident to the present or prospective business of the corporation or in which the corporation has a present or expectancy interest, unless that opportunity is first presented to the corporation and the corporation chooses not to pursue that opportunity. The doctrine of corporate opportunity is intended to preclude officers or directors or other fiduciaries from personally benefiting from opportunities that belong to the corporation. Our amended and restated certificate of incorporation, which will be in effect upon the consummation of the Transactions, will provide that the doctrine of “corporate opportunity” will not apply with respect to any director or stockholder who is not employed by us or our subsidiaries. Any director or stockholder who is not employed by us or our subsidiaries will, therefore, have no duty to communicate or present corporate opportunities to us, and will have the right to either hold any corporate opportunity for their (and their affiliates’) own account and benefit or to recommend, assign or otherwise transfer such corporate opportunity to persons other than us, including to any director or stockholder who is not employed by us or our subsidiaries.
As a result, certain of our stockholders, directors and their respective affiliates will not be prohibited from operating or investing in competing businesses. We, therefore, may find ourselves in competition with certain of our stockholders, directors or their respective affiliates, and we may not have knowledge of, or be able to pursue, transactions that could potentially be beneficial to us. Accordingly, we may lose a corporate opportunity or suffer competitive harm, which could negatively impact our business, operating results and financial condition.
72
Table of Contents
If securities analysts do not publish research or reports about our business or if they downgrade our stock or our sector, or if there is any fluctuation in our credit rating, our stock price and trading volume could decline.
The trading market for our Class A common stock will rely in part on the research and reports that industry or financial analysts publish about us or our business. We do not control these analysts. Securities and industry analysts do not currently, and may never, publish research on our company. If no securities or industry analysts commence coverage of us, the trading price of our shares would likely be negatively impacted. Furthermore, if one or more of the analysts who do cover us downgrade our stock or our industry, or the stock of any of our competitors, or publish inaccurate or unfavorable research about our business, the price of our stock could decline. If one or more of these analysts stops covering us or fails to publish reports on us regularly, we could lose visibility in the market, which, in turn, could cause our stock price or trading volume to decline.
Additionally, any fluctuation in the credit rating of us or our subsidiaries may impact our ability to access debt markets in the future or increase our cost of future debt, which could have a material adverse effect on our operations and financial condition, which in return may adversely affect the trading price of shares of our Class A common stock.
As a public reporting company, we will be subject to the Nasdaq rules and the rules and regulations established from time to time by the SEC regarding our internal control over financial reporting. If we fail to establish and maintain effective internal control over financial reporting and disclosure controls and procedures, we may not be able to accurately report our financial results, or report them in a timely manner.
Upon completion of this offering, we will become a public reporting company subject to the Nasdaq rules and the rules and regulations established from time to time by the SEC. These rules and regulations will require, among other things, that we establish and periodically evaluate procedures with respect to our internal control over financial reporting. Reporting obligations as a public company are likely to place a considerable strain on our financial and management systems, processes and controls, as well as on our personnel.
In addition, as a public company we will be required to document and test our internal control over financial reporting pursuant to Section 404 of the Sarbanes-Oxley Act so that our management can certify as to the effectiveness of our internal control over financial reporting by the time our second annual report is filed with the SEC and thereafter, which will require us to document and make significant changes to our internal control over financial reporting. Likewise, our independent registered public accounting firm will be required to provide an attestation report on the effectiveness of our internal control over financial reporting at such time as we cease to be an “emerging growth company,” as defined in the JOBS Act, and we become an accelerated or large accelerated filer. As described above, we could potentially qualify as an “emerging growth company” until as late as the fifth anniversary of the completion of this offering.
We expect to incur costs related to implementing an internal audit and compliance function in the upcoming years to further improve our internal control environment. If we identify future deficiencies in our internal control over financial reporting or if we are unable to comply with the demands that will be placed upon us as a public company, including the requirements of Section 404 of the Sarbanes-Oxley Act, in a timely manner, we may be unable to accurately report our financial results, or report them within the timeframes required by the SEC. We also could become subject to sanctions or investigations by the SEC or other regulatory authorities. In addition, if we are unable to assert that our internal control over financial reporting is effective, or if our independent registered public accounting firm is unable to express an opinion as to the effectiveness of our internal control over financial reporting, when required, investors may lose confidence in the accuracy and completeness of our financial reports, we may face restricted access to the capital markets and our stock price may be adversely affected.
We will incur significant costs as a result of operating as a public company.
Prior to this offering, we operated on a private basis. After this offering, we will be subject to the reporting requirements of the Exchange Act, the Sarbanes-Oxley Act, the Dodd-Frank Act, the listing requirements of
73
Table of Contents
the and other applicable securities laws and regulations. The expenses incurred by public companies generally for reporting and corporate governance purposes have been increasing. We expect these rules and regulations to increase our legal and financial compliance costs and to make some activities more difficult, time-consuming and costly, although we are currently unable to estimate these costs with any degree of certainty. We also expect that being a public company and being subject to new rules and regulations will make it more expensive for us to obtain director and officer liability insurance, and we may be required to accept reduced coverage or incur substantially higher costs to obtain coverage. These laws and regulations could also make it more difficult for us to attract and retain qualified persons to serve on our board of directors, our board committees or as our executive officers. Furthermore, if we are unable to satisfy our obligations as a public company, we could be subject to delisting of our Class A common stock, fines, sanctions and other regulatory action and potentially civil litigation. These factors may, therefore, strain our resources, divert management’s attention and affect our ability to attract and retain qualified board members.
Future sales, or the perception of future sales, by us or our existing stockholders in the public market following this offering could cause the market price for our Class A common stock to decline.
After this offering, the sale of shares of our Class A common stock in the public market, or the perception that such sales could occur, could harm the prevailing market price of shares of our Class A common stock. These sales, or the possibility that these sales may occur, also might make it more difficult for us to sell equity securities in the future at a time and at a price that we deem appropriate.
Upon consummation of the Transactions, we will have outstanding a total of shares of Class A common stock. Of the outstanding shares, the shares sold in this offering (or shares if the underwriters exercise in full their option to purchase additional shares) will be freely tradable without restriction or further registration under the Securities Act, other than any shares held by our affiliates. In addition, the shares of Class A common stock issued to the Blocker Shareholders in the Transactions will be eligible for resale pursuant to Rule 144 without restriction or further registration under the Securities Act, other than affiliate restrictions under Rule 144. Any shares of Class A common stock held by our affiliates will be eligible for resale pursuant to Rule 144 under the Securities Act, subject to the volume, manner of sale, holding period and other limitations of Rule 144.
Our directors and executive officers, and substantially all of our stockholders have entered into lock-up agreements with the underwriters prior to the commencement of this offering pursuant to which each of these persons or entities, subject to certain exceptions, for a period of 180 days after the date of this prospectus, may not, without the prior written consent of any two of Goldman Sachs & Co. LLC, BofA Securities, Inc. and Morgan Stanley & Co. LLC, (1) offer, sell, contract to sell, pledge, grant any option to purchase, lend or otherwise dispose of any shares of our Class A common stock, or any options or warrants to purchase any shares of our Class A common stock, or any securities convertible into or exchangeable for or that represent the right to receive shares of our Class A common stock (including, without limitation, common stock or such other securities which may be deemed to be beneficially owned by such directors, executive officers, managers and members in accordance with the rules and regulations of the SEC and securities which may be issued upon exercise of a stock option or warrant); (2) engage in any hedging or other transaction or arrangement (including, without limitation, any short sale or the purchase or sale of, or entry into, any put or call option, or combination thereof, forward, swap or any other derivative transaction or instrument, however described or defined) which is designed to, or which reasonably could be expected to lead to, or result in, a sale, loan, pledge or other disposition of shares of our Class A common stock or such other securities, whether any such transaction described in clause (1) or (2) above is to be settled by delivery of Class A common stock or such other securities, in cash or otherwise; or (3) make any demand for or exercise any right with respect to the registration of any shares of our Class A common stock or any security convertible into or exercisable or exchangeable for our common stock. See “Underwriting.”
In addition, we have reserved shares of Class A common stock equal to % of the total number of outstanding LLC Interests following this offering for issuance under the 2020 Plan. Any Class A common stock that we issue under the 2020 Plan or other equity incentive plans that we may adopt in the future would dilute the percentage ownership held by the investors who purchase Class A common stock in this offering.
74
Table of Contents
As restrictions on resale end or if these stockholders exercise their registration rights, the market price of our shares of Class A common stock could drop significantly if the holders of these shares sell them or are perceived by the market as intending to sell them. These factors could also make it more difficult for us to raise additional funds through future offerings of our shares of Class A common stock or other securities.
In the future, we may also issue securities in connection with investments, acquisitions or capital raising activities. In particular, the number of shares of our Class A common stock issued in connection with an investment or acquisition, or to raise additional equity capital, could constitute a material portion of our then-outstanding shares of our Class A common stock. Any such issuance of additional securities in the future may result in additional dilution to you, or may adversely impact the price of our Class A common stock.
Our stock price may change significantly following the offering, and you may not be able to resell shares of our Class A common stock at or above the price you paid or at all, and you could lose all or part of your investment as a result.
The initial public offering price for the shares was determined by negotiations between us and the underwriters. You may not be able to resell your shares at or above the initial public offering price due to a number of factors included herein, including the following:
| • | results of operations that vary from the expectations of securities analysts and investors; |
| • | results of operations that vary from those of our competitors; |
| • | changes in expectations as to our future financial performance, including financial estimates and investment recommendations by securities analysts and investors; |
| • | technology changes, changes in consumer behavior or changes in merchant relationships in our industry; |
| • | security breaches related to our systems or those of our merchants, affiliates or strategic partners; |
| • | changes in economic conditions for companies in our industry; |
| • | changes in market valuations of, or earnings and other announcements by, companies in our industry; |
| • | declines in the market prices of stocks generally, particularly those of global payment companies; |
| • | strategic actions by us or our competitors; |
| • | announcements by us, our competitors or our strategic partners of significant contracts, new products, acquisitions, joint marketing relationships, joint ventures, other strategic relationships, or capital commitments; |
| • | changes in general economic or market conditions or trends in our industry or the economy as a whole and, in particular, in the consumer spending environment; |
| • | changes in business or regulatory conditions; |
| • | future sales of our Class A common stock or other securities; |
| • | investor perceptions of the investment opportunity associated with our Class A common stock relative to other investment alternatives; |
| • | the public’s response to press releases or other public announcements by us or third parties, including our filings with the SEC; |
| • | announcements relating to litigation or governmental investigations; |
| • | guidance, if any, that we provide to the public, any changes in this guidance, or our failure to meet this guidance; |
75
Table of Contents
| • | the development and sustainability of an active trading market for our stock; |
| • | changes in accounting principles; and |
| • | other events or factors, including those resulting from system failures and disruptions, natural disasters, war, acts of terrorism, an outbreak of highly infectious or contagious diseases, such as COVID-19, or responses to these events. |
Furthermore, the stock market may experience extreme volatility that, in some cases, may be unrelated or disproportionate to the operating performance of particular companies. These broad market and industry fluctuations may adversely affect the market price of our Class A common stock, regardless of our actual operating performance. In addition, price volatility may be greater if the public float and trading volume of our Class A common stock is low.
In the past, following periods of market volatility, stockholders have instituted securities class action litigation. If we were involved in securities litigation, it could have a substantial cost and divert resources and the attention of management from our business regardless of the outcome of such litigation.
If you purchase shares of Class A common stock in this offering, you will suffer immediate and substantial dilution of your investment.
The initial public offering price of our Class A common stock is substantially higher than the pro forma net tangible book value per share of our Class A common stock. Therefore, if you purchase shares of our Class A common stock in this offering, you will pay a price per share that substantially exceeds our pro forma net tangible book value per share after this offering. You will experience immediate dilution of $ per share, representing the difference between our pro forma net tangible book value per share after giving effect to this offering and the initial public offering price. In addition, investors who purchase Class A common stock from us in this offering will have contributed % of the aggregate price paid by all purchasers of our outstanding equity but will own only approximately % of our outstanding equity after this offering. See “Dilution” for more detail, including the calculation of the pro forma net tangible book value per share of our Class A common stock.
76
Table of Contents
CAUTIONARY NOTE REGARDING FORWARD-LOOKING STATEMENTS
This prospectus contains forward-looking statements. All statements other than statements of historical facts contained in this prospectus may be forward-looking statements. Statements regarding our future results of operations and financial position, business strategy and plans and objectives of management for future operations, including, among others, statements regarding the Transactions, including the consummation of this offering, expected growth, future capital expenditures and debt service obligations, are forward-looking statements. In some cases, you can identify forward-looking statements by terms, such as “may,” “will,” “should,” “expects,” “plans,” “anticipates,” “could,” “intends,” “targets,” “projects,” “contemplates,” “believes,” “estimates,” “predicts,” “potential” or “continue” or the negative of these terms or other similar expressions. Accordingly, we caution you that any such forward-looking statements are not guarantees of future performance and are subject to risks, assumptions and uncertainties that are difficult to predict. Although we believe that the expectations reflected in these forward-looking statements are reasonable as of the date made, actual results may prove to be materially different from the results expressed or implied by the forward-looking statements.
There are or will be important factors that could cause our actual results to differ materially from those indicated in these forward-looking statements, including, but are not limited to, the following
| • | our ability to comply with the numerous, complex and frequently changing laws regulating the marketing and sale of Medicare plans; |
| • | the potential for an adverse change in our relationships with carriers, including a loss of carrier relationships; |
| • | failure to grow our customer base or retain our existing customers; |
| • | carriers’ ability to reduce commissions paid to us and adversely change their underwriting practices; |
| • | significant consolidation in the healthcare industry that could adversely alter our relationships with carriers; |
| • | information technology systems failures or capacity constraints interrupting our operations; |
| • | factors that adversely impact our estimate of LTV; |
| • | our dependence on agents to sell insurance plans; |
| • | changes in the health insurance system and laws and regulation governing health insurance markets; |
| • | inability to effectively advertise our products; and |
| • | the significant influence Continuing Equity Owners will have over us after the Transactions, including control over decisions that require the approval of stockholders. |
The foregoing factors should not be construed as exhaustive and should be read together with the other cautionary statements included in this prospectus. If one or more events related to these or other risks or uncertainties materialize, or if our underlying assumptions prove to be incorrect, actual results may differ materially from what we anticipate. Many of the important factors that will determine these results are beyond our ability to control or predict. Accordingly, you should not place undue reliance on any such forward-looking statements. Any forward-looking statement speaks only as of the date on which it is made, and, except as otherwise required by law, we do not undertake any obligation to publicly update or review any forward-looking statement, whether as a result of new information, future developments or otherwise. New factors emerge from time to time, and it is not possible for us to predict which will arise. In addition, we cannot assess the impact of each factor on our business or the extent to which any factor, or combination of factors, may cause actual results to differ materially from those contained in any forward-looking statements.
77
Table of Contents
GoHealth, Inc., a Delaware corporation, was formed on March 27, 2020 and is the issuer of the Class A common stock offered by this prospectus. Prior to this offering and the Transactions (as defined below), all of our business operations have been conducted through GoHealth Holdings, LLC and its direct and indirect subsidiaries and the Original Equity Owners are the only owners of GoHealth Holdings, LLC. We will consummate the Transactions, excluding this offering, substantially concurrently with or prior to the consummation of this offering.
Existing Organization
GoHealth Holdings, LLC is treated as a partnership for U.S. federal income tax purposes and, as such is generally not subject to any U.S. federal entity-level income taxes. Taxable income or loss of GoHealth Holdings, LLC is included in the U.S. federal income tax returns of GoHealth Holdings, LLC’s members. Prior to the consummation of this offering, the Original Equity Owners were the only members of GoHealth Holdings, LLC.
Transactions
Prior to the Transactions, we expect there will initially be one holder of common stock of GoHealth, Inc. We will consummate the following organizational transactions in connection with this offering:
| • | we will amend and restate the existing limited liability company agreement of GoHealth Holdings, LLC, which will become effective substantially concurrently with or prior to the consummation of this offering, to, among other things, (1) recapitalize all existing ownership interests in GoHealth Holdings, LLC (including profits interests awarded under the existing limited liability company agreement of GoHealth Holdings, LLC (and corresponding profits interests issued under the existing limited liability agreement of Blizzard Management Feeder, LLC)) into LLC Interests (and, in the case of corresponding profits interests issued by Blizzard Management Feeder, LLC, into common units of Blizzard Management Feeder, LLC) and (2) appoint GoHealth, Inc. as the sole managing member of GoHealth Holdings, LLC upon its acquisition of LLC Interests in connection with this offering; |
| • | we will amend and restate GoHealth, Inc.’s certificate of incorporation to, among other things, provide (1) for Class A common stock, with each share of our Class A common stock entitling its holder to one vote per share on all matters presented to our stockholders generally and (2) for Class B common stock, with each share of our Class B common stock entitling its holder to one vote per share on all matters presented to our stockholders generally, and that shares of our Class B common stock may only be held by the Continuing Equity Owners and their respective permitted transferees as described in “Description of Capital Stock—Common Stock—Class B Common Stock;” |
| • | we will acquire, by means of one or more mergers, the Blocker Company (the “Blocker Merger”) and will issue to the Blocker Shareholders shares of our Class A common stock and, upon consummation of this offering, $ million (based on the midpoint of the estimated price range set forth on the cover page of this prospectus) in cash to Blocker Shareholders as partial consideration in the Blocker Merger; |
| • | we will issue shares of our Class B common stock to the Continuing Equity Owners, which is equal to the number of LLC Interests held by such Continuing Equity Owners, for nominal consideration; |
| • | we will issue shares of our Class A common stock to the purchasers in this offering (or shares if the underwriters exercise in full their option to purchase additional shares of Class A common stock) in exchange for net proceeds of approximately $ million (or approximately $ million if the underwriters exercise in full their option to purchase additional shares of Class A common stock) based upon an assumed initial public offering price of $ per share (which is the midpoint of the estimated price range set forth on the cover page of this prospectus), less the underwriting discount and estimated offering expenses payable by us; |
78
Table of Contents
| • | we will use the net proceeds from this offering to (i) purchase newly-issued LLC Interests (or LLC Interests if the underwriters exercise in full their option to purchase additional shares of Class A common stock) directly from GoHealth Holdings, LLC at a price per unit equal to the initial public offering price per share of Class A common stock in this offering less the underwriting discount and estimated offering expenses payable by us and (ii) pay $ million in cash to the Blocker Shareholders as partial consideration in the Blocker Merger; |
| • | GoHealth Holdings, LLC intends to use the net proceeds from the sale of LLC Interests to GoHealth, Inc. (i) to partially redeem certain of the LLC Interests held by the Continuing Equity Owners, (ii) to satisfy in full $ million in aggregate principal amount of an obligation relating to an existing equity instrument in connection with the Transactions and (iii) for general corporate purposes to support the growth of the business, in each case, as described under “Use of Proceeds;” and |
| • | GoHealth, Inc. will enter into (1) the Stockholders Agreement with Centerbridge and our Founders, (2) the Registration Rights Agreement with certain of the Continuing Equity Owners and (3) the Tax Receivable Agreement with GoHealth Holdings, LLC, the Continuing Equity Owners and the Blocker Shareholders. For a description of the terms of the Stockholders Agreement, the Registration Rights Agreement and the Tax Receivable Agreement, see “Certain Relationships and Related Party Transactions.” |
Organizational Structure Following the Transactions
| • | GoHealth, Inc. will be a holding company and its principal asset will consist of LLC Interests it acquires directly from GoHealth Holdings, LLC and indirectly from certain of the Continuing Equity Owners (including the Blocker Shareholders); |
| • | GoHealth, Inc. will be the sole managing member of GoHealth Holdings, LLC and will control the business and affairs of GoHealth Holdings, LLC and its direct and indirect subsidiaries; |
| • | GoHealth, Inc. will own, directly or indirectly, LLC Interests of GoHealth Holdings, LLC, representing approximately % of the economic interest in GoHealth Holdings, LLC (or LLC Interests, representing approximately % of the economic interest in GoHealth Holdings, LLC if the underwriters exercise in full their option to purchase additional shares of Class A common stock); |
| • | the Continuing Equity Owners (excluding Centerbridge) will own (1) LLC Interests of GoHealth Holdings, LLC, representing approximately % of the economic interest in GoHealth Holdings, LLC (or LLC Interests, representing approximately % of the economic interest in GoHealth Holdings, LLC if the underwriters exercise in full their option to purchase additional shares of Class A common stock) and (2) shares of Class B common stock of GoHealth, Inc., representing approximately % of the combined voting power of all of GoHealth, Inc.’s common stock (or shares of Class B common stock of GoHealth, Inc., representing approximately % if the underwriters exercise in full their option to purchase additional shares of Class A common stock); |
| • | Centerbridge (directly or indirectly, including through the Blocker Shareholders) will own (1) shares of Class A common stock of GoHealth, Inc. (or shares of Class A common stock of GoHealth, Inc. if the underwriters exercise in full their option to purchase additional shares of Class A common stock), representing approximately % of the combined voting power of all of GoHealth, Inc.’s common stock and approximately % of the economic interest in GoHealth, Inc. (or approximately % of the combined voting power and approximately % of the economic interest if the underwriters exercise in full their option to purchase additional shares of Class A common stock), (2) directly and indirectly through GoHealth, Inc.’s ownership of LLC Interests, approximately % of the economic interest in GoHealth Holdings, LLC (or approximately % of the economic interest in GoHealth Holdings, LLC if the underwriters exercise in full their option to purchase additional shares of Class A common stock) and (3) shares of Class B common stock of GoHealth, Inc., representing approximately % of the combined voting power of all of GoHealth, Inc.’s common stock (or shares of Class B common stock of GoHealth, Inc., representing approximately % if the underwriters exercise in full their option to purchase additional shares of Class A common stock); and |
79
Table of Contents
| • | the purchasers in this offering will own (1) shares of Class A common stock of GoHealth, Inc. (or shares of Class A common stock of GoHealth, Inc. if the underwriters exercise in full their option to purchase additional shares of Class A common stock), representing approximately % of the combined voting power of all of GoHealth, Inc.’s common stock and approximately % of the economic interest in GoHealth, Inc. (or approximately % of the combined voting power and approximately % of the economic interest if the underwriters exercise in full their option to purchase additional shares of Class A common stock), and (2) through GoHealth, Inc.’s ownership of LLC Interests, indirectly will hold approximately % of the economic interest in GoHealth Holdings, LLC (or approximately % of the economic interest in GoHealth Holdings, LLC if the underwriters exercise in full their option to purchase additional shares of Class A common stock). |
The diagram below depicts our organizational structure after giving effect to the Transactions, including this offering, assuming no exercise by the underwriters of their option to purchase additional shares of Class A common stock.
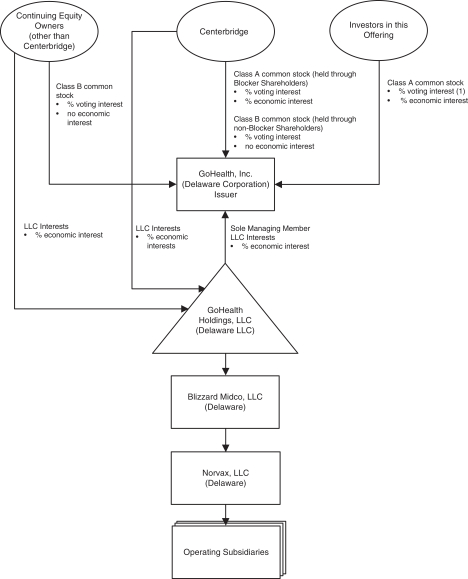
| (1) | Investors in this offering will hold approximately % of the voting interest. |
80
Table of Contents
As the sole managing member of GoHealth Holdings, LLC, we will operate and control all of the business and affairs of GoHealth Holdings, LLC and, through GoHealth Holdings, LLC and its direct and indirect subsidiaries, conduct our business. Following the Transactions, including this offering, GoHealth, Inc. will have the majority economic interest in GoHealth Holdings, LLC, and will control the management of GoHealth Holdings, LLC as its sole managing member. As a result, GoHealth, Inc. will consolidate GoHealth Holdings, LLC and record a significant non-controlling interest in a consolidated entity in GoHealth, Inc.’s consolidated financial statements for the economic interest in GoHealth Holdings, LLC held by the Continuing Equity Owners.
Unless otherwise indicated, this prospectus assumes the shares of Class A common stock are offered at $ per share (the midpoint of the estimated price range set forth on the cover page of this prospectus). Pursuant to the terms of the Existing LLC Agreement, the split between the number of LLC Interests among the Original Equity Owners will vary depending on the initial public offering price in this offering. The initial public offering price will also impact the relative allocation of LLC Interests issued in the Transactions among the Original Equity Owners and, in turn, the shares of Class A common stock and Class B common stock issued to the Original Equity Owners in the Transactions. Additionally, while the number of shares of Class A common stock being offered hereby to the public will not change, any increase or decrease in the number of shares of Class A common stock sold by GoHealth, Inc. in this offering due to a change in the initial public offering price will result in a corresponding increase or decrease in the number of LLC Interests purchased by GoHealth, Inc. directly from GoHealth Holdings, LLC at a price per unit equal to the initial public offering price per share of Class A common stock in this offering. Therefore, the indirect economic interest in GoHealth Holdings, LLC represented by the shares of Class A common stock sold in this offering will be largely unaffected by the initial public offering price.
Incorporation of GoHealth, Inc.
GoHealth, Inc., the issuer of the Class A common stock offered by this prospectus, was incorporated as a Delaware corporation on March 27, 2020. GoHealth, Inc. has not engaged in any material business or other activities except in connection with its formation and the Transactions. The amended and restated certificate of incorporation of GoHealth, Inc. that will become effective immediately prior to the consummation of this offering will, among other things, authorize two classes of common stock, Class A common stock and Class B common stock, each having the terms described in “Description of Capital Stock.”
Reclassification and Amendment and Restatement of the GoHealth Holdings, LLC Agreement
Prior to or substantially concurrently with the consummation of this offering, the existing limited liability company agreement of GoHealth Holdings, LLC will be amended and restated to, among other things, recapitalize its capital structure by creating a single new class of units that we refer to as “common units” and provide for a right of redemption of common units in exchange for, at our election (determined solely by our independent directors (within the meaning of the Nasdaq rules), who are disinterested), shares of our Class A common stock or cash. See “Certain Relationships and Related Party Transactions—GoHealth Holdings, LLC Agreement.”
81
Table of Contents
We estimate, based upon an assumed initial public offering price of $ per share (which is the midpoint of the estimated price range set forth on the cover page of this prospectus), that we will receive net proceeds from this offering of approximately $ million (or $ million if the underwriters exercise in full their option to purchase additional shares of Class A common stock), after deducting the underwriting discount and estimated offering expenses payable by us.
We intend to use the net proceeds from this offering to (i) purchase newly-issued LLC Interests (or LLC Interests if the underwriters exercise in full their option to purchase additional shares of Class A common stock) directly from GoHealth Holdings, LLC at a price per unit equal to the initial public offering price per share of Class A common stock in this offering less the underwriting discount and estimated offering expenses payable by us and (ii) pay $ million in cash to the Blocker Shareholders as partial consideration in the Blocker Merger.
GoHealth Holdings, LLC intends to use the net proceeds from the sale of LLC Interests to GoHealth, Inc. (i) to partially redeem certain of the LLC Interests held by the Continuing Equity Owners, (ii) to satisfy in full $ million in aggregate principal amount of an obligation relating to an existing equity instrument in connection with the Transactions and (iii) for general corporate purposes to support the growth of the business.
Assuming no exercise of the underwriters’ option to purchase additional shares of Class A common stock, each $1.00 increase (decrease) in the assumed initial public offering price of $ per share (which is the midpoint of the estimated price range set forth on the cover page of this prospectus) would increase (decrease) the net proceeds to us from this offering by approximately $ million and, in turn, the net proceeds received by GoHealth Holdings, LLC from the sale of LLC Interests to GoHealth, Inc. by $ million, assuming the number of shares offered, as set forth on the cover page of this prospectus, remains the same, and after deducting the underwriting discount and estimated offering expenses payable by us.
Each 1,000,000 share increase (decrease) in the number of shares offered by us in this offering would increase (decrease) the net proceeds to us from this offering by approximately $ million and, in turn, the net proceeds received by GoHealth Holdings, LLC from the sale of LLC Interests to GoHealth, Inc. by $ million, assuming that the price per share for the offering remains at $ (which is the midpoint of the estimated price range set forth on the cover page of this prospectus), and after deducting the underwriting discount and estimated offering expenses payable by us.
GoHealth Holdings, LLC will bear or reimburse GoHealth, Inc. for all of the expenses incurred in connection with the Transactions, including this offering.
82
Table of Contents
The following table sets forth the cash and capitalization as of March 31, 2020, as follows:
| • | of GoHealth Holdings, LLC and its subsidiaries on a historical basis; |
| • | of GoHealth, Inc. and its subsidiaries on a pro forma basis to give effect to the Transactions, excluding this offering; and |
| • | of GoHealth, Inc. and its subsidiaries on a pro forma as adjusted basis to give effect to the Transactions, including the sale of the shares of Class A common stock in this offering at an assumed initial public offering price of $ per share (which is the midpoint of the estimated price range set forth on the cover page of this prospectus), after deducting the underwriting discount and estimated offering expenses payable by us, and the application of the net proceeds therefrom as described under “Use of Proceeds.” |
For more information, please see “Our Organizational Structure,” “Use of Proceeds” and “Unaudited Pro Forma Condensed Consolidated Financial Information” included elsewhere in this prospectus. You should read this information in conjunction with our consolidated financial statements and the related notes included elsewhere in this prospectus and the “Management’s Discussion and Analysis of Financial Condition and Results of Operations” section and other financial information contained in this prospectus.
| As of March 31, 2020 | ||||||||||||
| (in thousands, except per share and share amounts) | GoHealth Holdings, LLC Historical |
GoHealth, Inc. Pro Forma |
GoHealth, Inc. Pro Forma As Adjusted |
|||||||||
| Cash and cash equivalents |
$ | 152,423 | $ | $ | ||||||||
|
|
|
|
|
|
|
|||||||
| Long-term debt (including current portion)(1): |
||||||||||||
| Term Loan Facility(2) |
$ | 290,834 | $ | $ | ||||||||
| Incremental Term Loan Facility(2) |
110,988 | |||||||||||
|
|
|
|
|
|
|
|||||||
| Total long-term debt |
$ | 401,822 | $ | $ | ||||||||
| Members’/stockholders’ equity (deficit): |
||||||||||||
| Member’s equity: |
||||||||||||
| Preferred units |
546,972 | |||||||||||
| Class A common units |
219,139 | |||||||||||
| Class B common units |
103,593 | |||||||||||
| Accumulated other comprehensive (loss) income |
(102 | ) | ||||||||||
| Retained earnings (deficit) |
— | |||||||||||
| Stockholders’ equity: |
||||||||||||
| Class A common stock, par value $ per share; shares authorized, shares issued and outstanding, pro forma; and shares authorized, shares issued and outstanding, pro forma as adjusted |
— | |||||||||||
| Class B common stock, par value $ per share; shares authorized, shares issued and outstanding, pro forma; and shares authorized, shares issued and outstanding, pro forma as adjusted |
— | |||||||||||
|
|
|
|
|
|
|
|||||||
| Total members’/stockholders’ equity (deficit) |
869,602 | |||||||||||
|
|
|
|
|
|
|
|||||||
| Total capitalization |
$ | 1,271,424 | $ | $ | ||||||||
|
|
|
|
|
|
|
|||||||
| (1) | See “Description of Indebtedness” for a description of our currently outstanding indebtedness. |
| (2) | Net of $8 million and $6 million of original issue discount and debt issuance costs related to the Term Loan Facility and Incremental Term Loan Facility, respectively. |
83
Table of Contents
Each $1.00 increase (decrease) in the assumed public offering price of $ per share, the midpoint of the estimated price range set forth on the cover page of this prospectus, would increase (decrease) each of total indebtedness, additional paid-in capital and total members’ / stockholders’ equity on a pro forma as adjusted basis by approximately $ million, assuming that the price per share for the offering remains at $ (which is the midpoint of the estimated price range set forth on the cover page of this prospectus), and after deducting the underwriting discount and estimated offering expenses payable by us.
Each 1,000,000 share increase or decrease in the number of shares offered in this offering by us would increase or decrease each of total indebtedness, additional paid-in capital and total members’ / stockholders’ equity on a pro forma as adjusted basis by approximately $ million, assuming that the price per share for the offering remains at $ (which is the midpoint of the estimated price range set forth on the cover page of this prospectus), and after deducting the underwriting discount and estimated offering expenses payable by us.
84
Table of Contents
We currently intend to retain all available funds and any future earnings to fund the development and growth of our business and to repay indebtedness, and therefore we do not anticipate declaring or paying any cash dividends on our Class A common stock in the foreseeable future. Holders of our Class B common stock are not entitled to participate in any dividends declared by our board of directors. Furthermore, because we are a holding company, our ability to pay cash dividends on our Class A common stock depends on our receipt of cash distributions from GoHealth Holdings, LLC and, through GoHealth Holdings, LLC, cash distributions and dividends from our other direct and indirect subsidiaries. Our ability to pay dividends may be restricted by the terms of any future credit agreement or any future debt or preferred equity securities of us or our subsidiaries. See “Description of Capital Stock,” “Description of Indebtedness” and “Management’s Discussion and Analysis of Financial Condition and Results of Operation—Liquidity and Capital Resources.” Any future determination as to the declaration and payment of dividends, if any, will be at the discretion of our board of directors, subject to compliance with contractual restrictions and covenants in the agreements governing our current and future indebtedness. Any such determination will also depend upon our business prospects, results of operations, financial condition, cash requirements and availability and other factors that our board of directors may deem relevant.
Accordingly, you may need to sell your shares of our Class A common stock to realize a return on your investment, and you may not be able to sell your shares at or above the price you paid for them. See “Risk Factors—Risks Related to the Offering and Ownership of our Class A Common Stock—Because we have no current plans to pay regular cash dividends on our Class A common stock following this offering, you may not receive any return on investment unless you sell your Class A common stock for a price greater than that which you paid for it.”
Immediately following this offering, we will be a holding company, and our principal asset will be the LLC Interests we purchase from GoHealth Holdings, LLC. If we decide to pay a dividend in the future, we would need to cause GoHealth Holdings, LLC to make distributions to us in an amount sufficient to cover such dividend. If GoHealth Holdings, LLC makes such distributions to us, the other holders of LLC Interests will be entitled to receive pro rata distributions. See “Risk Factors—Risks Related to Our Organizational Structure—Our principal asset after the completion of this offering will be our interest in GoHealth Holdings, LLC, and, as a result, we will depend on distributions from GoHealth Holdings, LLC to pay our taxes and expenses, including payments under the Tax Receivable Agreement. GoHealth Holdings, LLC’s ability to make such distributions may be subject to various limitations and restrictions.”
85
Table of Contents
The Continuing Equity Owners will own LLC Interests after the Transactions. Because the Continuing Equity Owners do not own any Class A common stock or have any right to receive distributions from GoHealth, Inc., we have presented dilution in pro forma net tangible book value per share both before and after this offering assuming that all of the holders of LLC Interests (other than GoHealth, Inc.) had their LLC Interests redeemed or exchanged for newly-issued shares of Class A common stock on a one-for-one basis (rather than for cash) and the automatic transfer to the Company and cancellation for no consideration of all of their shares of Class B common stock (which are not entitled to receive distributions or dividends, whether cash or stock from GoHealth, Inc.) in order to more meaningfully present the dilutive impact on the investors in this offering. We refer to the assumed redemption or exchange of all LLC Interests for shares of Class A common stock as described in the previous sentence as the Assumed Redemption.
Dilution is the amount by which the offering price paid by the purchasers of the Class A common stock in this offering exceeds the pro forma net tangible book value per share of Class A common stock after the offering. GoHealth Holdings, LLC’s pro forma net tangible book value as of March 31, 2020 prior to this offering and after giving effect to the other Transactions and the Assumed Redemption was a deficit of $ million. Pro forma net tangible book value per share prior to this offering is determined by subtracting our total liabilities from the total book value of our tangible assets and dividing the difference by the number of shares of Class A common stock deemed to be outstanding after giving effect to the Assumed Redemption.
If you invest in our Class A common stock in this offering, your ownership interest will be immediately diluted to the extent of the difference between the initial public offering price per share and the pro forma net tangible book value per share of our Class A common stock after this offering.
Pro forma net tangible book value per share after this offering is determined by subtracting our total liabilities from the total book value of our tangible assets and dividing the difference by the number of shares of Class A common stock deemed to be outstanding, after giving effect to the Transactions, including this offering and the application of the proceeds from this offering as described in “Use of Proceeds,” and the Assumed Redemption. Our pro forma net tangible book value as of March 31, 2020, after giving effect to this offering would have been approximately a deficit of $ million, or $ per share of Class A common stock. This amount represents an immediate increase in pro forma net tangible book value of $ per share to our existing stockholders and an immediate dilution in pro forma net tangible book value of approximately $ per share to new investors purchasing shares of Class A common stock in this offering. We determine dilution by subtracting the pro forma net tangible book value per share after this offering from the amount of cash that a new investor paid for a share of Class A common stock. The following table illustrates this dilution:
| Assumed initial public offering price per share |
$ | |||||||
| Pro forma net tangible book value (deficit) per share as of March 31, 2020 before this offering |
$ | |||||||
| Increase per share attributable to new investors in this offering |
$ | |||||||
|
|
|
|||||||
| Pro forma net tangible book value (deficit) per share after this offering |
||||||||
| Dilution per share to new Class A common stock investors in this offering |
$ | |||||||
|
|
|
A $1.00 increase (decrease) in the assumed initial public offering price of $ per share, which is the midpoint of the estimated price range set forth on the cover page of this prospectus, would increase the pro forma net tangible book value (deficit) per share after this offering by approximately $ , and dilution in pro forma net tangible book value (deficit) per share to new investors by approximately $ assuming that the number of shares offered by us, as set forth on the cover page of this prospectus, remains the same and after deducting the underwriting discount and estimated offering expenses payable by us.
86
Table of Contents
If the underwriters exercise in full their option to purchase additional shares of Class A common stock, the pro forma net tangible book value (deficit) after the offering would be $ per share, the increase in pro forma net tangible book value per share to existing stockholders would be $ per share and the dilution in pro forma net tangible book value to new investors would be $ per share, in each case assuming an initial public offering price of $ per share, which is the midpoint of the estimated price range set forth on the cover page of this prospectus.
The following table summarizes, as of March 31, 2020, after giving effect to the Transactions (including this offering) and the Assumed Redemption, the number of shares of Class A common stock purchased from us, the total consideration paid, or to be paid, to us and the average price per share paid, or to be paid, by existing owners and by the new investors. The calculation below is based on an assumed initial public offering price of $ per share, which is the midpoint of the estimated price range set forth on the cover page of this prospectus, before deducting the underwriting discount and estimated offering expenses payable by us.
| Shares Purchased |
Total Consideration | Average Price Per Share |
||||||||||||||||||
| Number | Percent | Amount | Percent | |||||||||||||||||
| Original Equity Owners |
% | $ | % | $ | ||||||||||||||||
| New investors |
||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total |
100 | % | $ | 100 | % | $ | ||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
Each $1.00 increase (decrease) in the assumed initial public offering price of $ per share would increase (decrease) the total consideration paid by new investors and the total consideration paid by all stockholders by $ million, assuming the number of shares offered by us remains the same and after deducting the underwriting discount but before estimated offering expenses.
Except as otherwise indicated, the discussion and the tables above assume no exercise of the underwriters’ option to purchase additional shares of Class A common stock. In addition, the discussion and tables above exclude shares of Class B common stock, because holders of the Class B common stock are not entitled to distributions or dividends, whether cash or stock, from GoHealth, Inc. The number of shares of our Class A common stock outstanding after this offering as shown in the tables above is based on the number of shares outstanding as of March 31, 2020, after giving effect to the Transactions and the Assumed Redemption, and excludes shares of Class A common stock reserved for issuance under our 2020 Plan (as described in “Executive Compensation— ”), including approximately shares of Class A common stock issuable pursuant to stock options we intend to grant to certain of our directors, executive officers and other employees, including certain of our named executive officers, in connection with this offering as described in “Executive Compensation— ” and “Executive Compensation— .”
To the extent any of these outstanding options are exercised, there will be further dilution to new investors. To the extent all of such outstanding options had been exercised as of March 31, 2020 the pro forma net tangible book value (deficit) per share after this offering would be $ , and total dilution per share to new investors would be $ .
If the underwriters exercise in full their option to purchase additional shares of Class A common stock:
| • | the percentage of shares of Class A common stock held by the Original Equity Owners will decrease to approximately % of the total number of shares of our Class A common stock outstanding after this offering; and |
| • | the number of shares held by new investors will increase to , or approximately % of the total number of shares of our Class A common stock outstanding after this offering. |
87
Table of Contents
SELECTED HISTORICAL CONDENSED CONSOLIDATED FINANCIAL DATA
The following table presents the selected historical condensed consolidated financial data for GoHealth Holdings, LLC and its subsidiaries. GoHealth Holdings, LLC is the predecessor of the issuer, GoHealth, Inc., for financial reporting purposes. The selected consolidated statements of operations data and statements of cash flows data for the period from September 13, 2019 through December 31, 2019 (Successor), the period from January 1, 2019 through September 12, 2019 (Predecessor) and the year ended December 31, 2018 (Predecessor), and the selected consolidated balance sheet data as of December 31, 2019 and 2018 are derived from the audited consolidated financial statements of GoHealth Holdings, LLC included elsewhere in this prospectus. The selected condensed consolidated statements of operations and statements of cash flows data for the three months ended March 31, 2020 and 2019, and the summary condensed consolidated balance sheet data as of March 31, 2020, are derived from the unaudited condensed consolidated financial statements of GoHealth Holdings, LLC included elsewhere in this prospectus. The results of operations for the periods presented below are not necessarily indicative of the results to be expected for any future period. The information set forth below should be read together with the “Management’s Discussion and Analysis of Financial Condition and Results of Operations” section and the consolidated financial statements and the accompanying notes included elsewhere in this prospectus.
88
Table of Contents
The selected historical financial data of GoHealth, Inc. has not been presented because GoHealth, Inc. is a newly incorporated entity, has had no business transactions or activities to date and had no assets or liabilities during the periods presented in this section.
| (in thousands, except per share data) | Three Months Ended March 31, |
Successor 2019 Period |
Predecessor 2019 Period |
Year Ended December 31, 2018 (Predecessor) |
||||||||||||||||
| 2020 (Successor) |
2019 (Predecessor) |
|||||||||||||||||||
| Consolidated Statement of Operations: |
||||||||||||||||||||
| Net revenues: |
||||||||||||||||||||
| Commission |
$ | 112,510 | $ | 51,215 | $ | 243,347 | $ | 175,834 | $ | 144,378 | ||||||||||
| Other |
28,500 | 17,874 | 65,144 | 55,176 | 81,827 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Net revenues |
141,010 | 69,089 | 308,491 | 231,010 | 226,205 | |||||||||||||||
| Operating expenses: |
||||||||||||||||||||
| Cost of revenue |
42,134 | 27,552 | 90,384 | 79,169 | 79,582 | |||||||||||||||
| Marketing and advertising |
26,073 | 11,411 | 24,811 | 37,769 | 28,129 | |||||||||||||||
| Customer care and enrollment |
23,978 | 13,939 | 44,356 | 49,149 | 46,076 | |||||||||||||||
| Technology |
4,593 | 4,155 | 6,006 | 40,312 | 16,197 | |||||||||||||||
| General and administrative |
10,491 | 6,990 | 13,674 | 79,219 | 27,458 | |||||||||||||||
| Change in fair value of contingent consideration liability |
4,400 | — | 70,700 | — | — | |||||||||||||||
| Amortization of intangible assets |
23,514 | — | 28,217 | — | — | |||||||||||||||
| Transaction costs |
— | — | 6,245 | 2,267 | — | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total operating expenses |
135,183 | 64,047 | 284,393 | 287,885 | 197,442 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Income (loss) from operations |
5,827 | 5,042 | 24,098 | (56,875 | ) | 28,763 | ||||||||||||||
| Interest expense |
6,756 | 28 | 8,076 | 140 | 224 | |||||||||||||||
| Other income (expense) |
10 | 10 | 17 | (114 | ) | (379 | ) | |||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Income (loss) before income taxes |
(939 | ) | 5,004 | 16,039 | (57,129 | ) | 28,160 | |||||||||||||
| Income tax expense (benefit) |
(2 | ) | 2 | 44 | (66 | ) | 46 | |||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Net income (loss) |
$ | (937 | ) | $ | 5,002 | $ | 15,995 | $ | (57,063 | ) | $ | 28,114 | ||||||||
| Less: Net loss attributable to non-controlling interests |
— | — | — | — | (3 | ) | ||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Net income (loss) attributable to GoHealth Holdings, LLC and subsidiaries |
$ | (937 | ) | $ | 5,002 | $ | 15,995 | $ | (57,063 | ) | $ | 28,117 | ||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Consolidated Statement of Cash Flows: |
||||||||||||||||||||
| Net cash (used in) provided by operating activities |
$ | 23,587 | $ | 1,222 | $ | (9,284 | ) | $ | 9,281 | $ | 5,443 | |||||||||
| Net cash used in investing activities |
(3,522 | ) | (1,944 | ) | (810,010 | ) | (5,597 | ) | (6,170 | ) | ||||||||||
| Net cash provided by (used in) financing activities |
120,167 | 1,147 | 830,879 | (3,449 | ) | 63 | ||||||||||||||
| As of March 31, 2020 (Successor) |
As of December 31, 2019 (Successor) |
As of December 31, 2018 (Predecessor) |
||||||||||
| (in thousands) | ||||||||||||
| Consolidated Balance Sheet: |
||||||||||||
| Cash and cash equivalents |
$ | 152,423 | $ | 12,276 | $ | 505 | ||||||
| Total assets |
1,709,649 | 1,602,295 | 142,837 | |||||||||
| Total liabilities |
840,047 | 742,151 | 83,490 | |||||||||
| Total members’ equity (deficit) |
869,602 | 860,144 | (186,653 | ) | ||||||||
89
Table of Contents
UNAUDITED PRO FORMA CONDENSED CONSOLIDATED FINANCIAL INFORMATION
The following unaudited pro forma condensed consolidated financial information reflects (i) the Centerbridge Acquisition and (ii) the impact of this offering, after giving effect to the Transactions discussed in “Our Organizational Structure.” Following the completion of the Transactions, GoHealth, Inc. will be a holding company whose principal asset will consist of % of the outstanding LLC Interests (or % of LLC Interests if the underwriters exercise in full their option to purchase additional shares of Class A common stock) that it acquires directly from GoHealth Holdings, LLC and indirectly from certain of the Continuing Equity Owners and the Blocker Shareholders in connection with this offering. The remaining LLC Interests will be held by the Continuing Equity Owners. GoHealth, Inc. will act as the sole managing member of GoHealth Holdings, LLC, will operate and control the business and affairs of GoHealth Holdings, LLC and its direct and indirect subsidiaries and, through GoHealth Holdings, LLC and its direct and indirect subsidiaries, conduct its business.
The following unaudited pro forma condensed consolidated statements of operations for the year ended December 31, 2019 and the three months ended March 31, 2020 give effect to the Centerbridge Acquisition and the Transactions, including this offering, as if the same had occurred on January 1, 2019. The unaudited pro forma condensed consolidated balance sheet as of March 31, 2020 presents our unaudited pro forma balance sheet giving effect to the Transactions, including this offering, as if they had occurred as of March 31, 2020.
We have derived the unaudited pro forma condensed consolidated statement of operations and unaudited pro forma condensed consolidated balance sheet from the consolidated financial statements of GoHealth Holdings, LLC and its subsidiaries as of March 31, 2020 and for the Successor 2019 Period and Predecessor 2019 Period included elsewhere in this prospectus. The historical consolidated financial information of GoHealth Holdings, LLC has been adjusted in this unaudited pro forma condensed consolidated financial information to give effect to events that are directly attributable to the Centerbridge Acquisition and the Transactions, are factually supportable and, with respect to the condensed consolidated statement of operations, are expected to have a continuing impact on GoHealth, Inc. The unaudited pro forma condensed consolidated financial information reflects adjustments that are described in the accompanying notes and are based on available information and certain assumptions we believe are reasonable, but are subject to change.
We refer to the adjustments related to the Centerbridge Acquisition, excluding the adjustments related to the Offering, as the “Pro Forma Centerbridge Acquisition Adjustments.” We refer to the adjustments related to the Transactions, including the impact of the Transactions described in “Our Organizational Structure,” but excluding the adjustments related to the Offering, as the Pro Forma Transaction Adjustments.
The adjustments related to this offering, which we refer to as the Pro Forma Offering Adjustments, are described in the notes to the unaudited pro forma condensed consolidated financial information, and principally include the following:
| • | the amendment and restatement of the limited liability company agreement of GoHealth Holdings, LLC to, among other things, appoint GoHealth, Inc. as the sole managing member of GoHealth Holdings, LLC and provide certain redemption rights to the Continuing Equity Owners; |
| • | the issuance of shares of our Class A common stock to the investors in this offering in exchange for net proceeds of approximately $ (based on an assumed initial public offering price of $ per share, the midpoint of the estimated price range set forth on the cover page of this prospectus), after deducting the underwriting discount but before estimated offering expenses payable by us; |
| • | the payment of fees and expenses related to this offering and the application of the net proceeds from the sale of Class A common stock in this offering to purchase LLC Interests directly from GoHealth Holdings, LLC, at a purchase price per LLC Interest equal to the initial public offering price per share of Class A common stock less the underwriting discount and estimated offering expenses payable by us, with such LLC Interests representing % of the outstanding LLC Interests; and |
90
Table of Contents
| • | the application by GoHealth Holdings, LLC of the proceeds from the sale of LLC Interests to us as described under “Use of Proceeds.” |
Except as otherwise indicated, the unaudited pro forma condensed consolidated financial information presented assumes no exercise by the underwriters of their option to purchase additional shares of Class A common stock in the offering.
As a public company, we will be implementing additional procedures and processes for the purpose of addressing the standards and requirements applicable to public companies. We expect to incur additional annual expenses related to these additional procedures and processes and, among other things, additional directors’ and officers’ liability insurance, director fees, additional expenses associated with complying with the reporting requirements of the SEC, transfer agent fees, costs relating to additional accounting, legal and administrative personnel, increased auditing, tax and legal fees, stock exchange listing fees and other public company expenses. We have not included any pro forma adjustments relating to these costs in the information below.
The unaudited pro forma condensed consolidated financial information is included for informational purposes only. The unaudited pro forma condensed consolidated financial information should not be relied upon as being indicative of our results of operations or financial condition had the Centerbridge Acquisition and the Transactions, including this offering, occurred on the dates assumed. The unaudited pro forma condensed consolidated financial information also does not project our results of operations or financial position for any future period or date. The unaudited pro forma condensed consolidated statement of operations and balance sheet should be read in conjunction with the “Risk Factors,” “Prospectus Summary—Summary Historical and Pro Forma Condensed Consolidated Financial and Other Data,” “Selected Historical Condensed Consolidated Financial Data,” “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and our consolidated financial statements and related notes included elsewhere in this prospectus.
GoHealth, Inc. and subsidiaries
Unaudited pro forma condensed consolidated balance sheet as of March 31, 2020
| (in thousands, except share amounts) |
Successor GoHealth Holdings, LLC Historical |
Pro Forma Transactions Adjustments |
As Further Adjusted for Pro Forma Transactions |
Pro Forma Offering Adjustments |
GoHealth, Inc. Pro Forma |
|||||||||||||||
| Assets |
||||||||||||||||||||
| Current assets: |
||||||||||||||||||||
| Cash and cash equivalents |
$ | 152,423 | (1 | ) | ||||||||||||||||
| Accounts receivable, net of allowance for doubtful accounts of $651 in 2020 |
6,422 | |||||||||||||||||||
| Commissions receivable—current |
58,173 | |||||||||||||||||||
| Prepaid expenses and other current assets |
6,010 | |||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total current assets |
223,028 | |||||||||||||||||||
| Commissions receivable—non-current |
330,617 | |||||||||||||||||||
| Property, equipment, and capitalized software, net |
9,228 | |||||||||||||||||||
| Intangible assets, net |
759,269 | |||||||||||||||||||
| Goodwill |
386,553 | |||||||||||||||||||
| Other long-term assets |
954 | |||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total assets |
$ | 1,709,649 | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
91
Table of Contents
| (in thousands, except share amounts) |
Successor GoHealth Holdings, LLC Historical |
Pro Forma Transactions Adjustments |
As Further Adjusted for Pro Forma Transactions |
Pro Forma Offering Adjustments |
GoHealth, Inc. Pro Forma |
|||||||||||||||
| Liabilities and members’ equity |
||||||||||||||||||||
| Current liabilities: |
||||||||||||||||||||
| Accounts payable |
12,718 | |||||||||||||||||||
| Accrued liabilities |
11,740 | |||||||||||||||||||
| Commissions payable—current |
34,536 | |||||||||||||||||||
| Deferred revenue |
14,867 | |||||||||||||||||||
| Current portion of debt |
4,170 | |||||||||||||||||||
| Other current liabilities |
3,178 | |||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total current liabilities |
81,209 | |||||||||||||||||||
| Non-current liabilities: |
||||||||||||||||||||
| Commissions payable—non-current |
113,516 | |||||||||||||||||||
| Long-term debt, net of current portion |
397,652 | |||||||||||||||||||
| Contingent consideration |
247,100 | |||||||||||||||||||
| Capital lease obligations, less current portion |
345 | |||||||||||||||||||
| Incentive share liability |
— | |||||||||||||||||||
| Deferred tax liability |
225 | (2 | ) | |||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total non-current liabilities |
$ | 758,838 | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Members’ equity |
||||||||||||||||||||
| Preferred Units – $1.00 par value; 541,263,042 units authorized, issued and outstanding at March 31, 2020 |
546,972 | |||||||||||||||||||
| Class A Common units – $1.00 par value; 237,938,682 units authorized, issued and outstanding at March 31, 2020 |
219,139 | (3 | ) | |||||||||||||||||
| Class B Common units – $1.00 par value; 108,727,667 units authorized, issued and outstanding at March 31, 2020 |
103,593 | (3 | ) | |||||||||||||||||
| Senior Preferred Earnout Units – no par value; none authorized, issued, and outstanding at March 31, 2020 |
— | |||||||||||||||||||
| Profits Units – no par value; 97,918,116 units authorized at March 31, 2020; 84,399,921 units issued at March 31, 2020; and none outstanding as of March 31, 2020 |
— | |||||||||||||||||||
| Class A common stock – $ par value per share, shares authorized on a pro forma basis, shares issued and outstanding on a pro forma basis |
(4 | ) | ||||||||||||||||||
92
Table of Contents
| (in thousands, except share amounts) |
Successor GoHealth Holdings, LLC Historical |
Pro Forma Transactions Adjustments |
As Further Adjusted for Pro Forma Transactions |
Pro Forma Offering Adjustments |
GoHealth, Inc. Pro Forma |
|||||||||||||||
| Class B common stock – $ par value per share, shares authorized on a pro forma basis, shares issued and outstanding on a pro forma basis |
(4 | ) | ||||||||||||||||||
| Accumulated other comprehensive (loss) income |
(102 | ) | ||||||||||||||||||
| Retained earnings |
— | (3 | ) | |||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total members’/stockholders’ equity attributable to GoHealth Holdings, LLC/GoHealth, Inc. (a) |
869,602 | (3 | ) | |||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Non-controlling interest |
— | (3 | ) | (3 | ) | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total members’/stockholders’ equity |
869,602 | |||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total liabilities and equity |
$ | 1,709,649 | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
(a) For historical amounts, represents total members’ deficit attributable to GoHealth Holdings, LLC. For Pro Forma amounts, represents total members’/stockholders’ equity attributable to GoHealth, Inc.
GoHealth, Inc. and subsidiaries
Notes to unaudited pro forma condensed consolidated balance sheet
| (1) | Reflects the net effect on cash of the receipt of offering proceeds to us of $ million, based on the assumed sale of shares of Class A common stock at an assumed initial public offering of $ per share, the midpoint of the estimated price range set forth on the cover page of this prospectus, after deducting the underwriting discount and estimated offering expenses payable by us. These amounts, as described in “Use of Proceeds,” relate to: |
| (a) | payment of $ million to purchase newly-issued LLC Interests (or LLC Interests if the underwriters exercise in full their option to purchase additional shares of Class A common stock) directly from GoHealth Holdings, LLC at an assumed initial public offering of $ per share, the midpoint of the estimated price range set forth on the cover page of this prospectus after deducting the underwriting discount and estimated offering expenses payable by us; |
| (b) | payment of approximately $ million in cash to the Blocker Shareholders as partial consideration in the Blocker Merger; and |
| (c) | payment of approximately $ million of underwriting discount and estimated offering expenses. |
| (2) | As described in greater detail under “Our Organizational Structure” and “Certain Relationships and Related Party Transactions—Tax Receivable Agreement,” in connection with the completion of this offering, we will enter into a Tax Receivable Agreement with GoHealth Holdings, LLC and the Continuing Equity Owners and the Blocker Shareholders that will provide for the payment by GoHealth, Inc. to the Continuing Equity Owners and the Blocker Shareholders of 85% of the amount of certain tax benefits, if any, that GoHealth, Inc. actually realizes, or in some circumstances is deemed to realize, as a result of (1) GoHealth, Inc.’s allocable share of existing tax basis acquired in connection with the Transactions (including the Blocker Company’s share of existing tax basis) and increases to such allocable share of existing tax basis; (2) increases in tax basis resulting from (a) the purchase of LLC Interests directly from GoHealth Holdings, LLC and |
93
Table of Contents
| the partial redemption of LLC Interests by GoHealth Holdings, LLC, as described under “Use of Proceeds,” (b) any future redemptions or exchanges or exchanges of LLC Interests from the Continuing Equity Owners as described under “Certain Relationships and Related Party Transactions— GoHealth Holdings, LLC Agreement—Agreement in Effect Upon Consummation of this Offering—Common Unit Redemption Right,” and (c) certain distributions (or deemed distributions) by GoHealth Holdings, LLC; and (3) certain additional tax benefits arising from payments made under the Tax Receivable Agreement. |
Due to the uncertainty in the amount and timing of future redemptions or exchanges of LLC Interests by the Continuing Equity Owners, the unaudited pro forma consolidated financial information assumes that no redemptions or exchanges of LLC Interests have occurred and, therefore, no increases in tax basis in GoHealth Holdings, LLC’s assets or other tax benefits that may be realized thereunder have been assumed in the unaudited pro forma consolidated financial information. However, if all of the Continuing Equity Owners were to exchange or redeem their LLC Interests, we would recognize a deferred tax asset of approximately $ million and a related liability for payments under the Tax Receivable Agreement of approximately $ million, assuming, among other factors, (i) all exchanges occurred on the same day; (ii) a price of $ per share of Class A common stock (the midpoint of the estimated offering price set forth on the cover of this prospectus); (iii) a constant corporate tax rate of %; (iv) we will have sufficient taxable income to fully utilize the tax benefits; (v) GoHealth Holdings, LLC is able to fully depreciate or amortize its assets; and (vi) no material changes in applicable tax law. For each 5% increase (decrease) in the amount of LLC Interests exchanged by the Continuing Equity Owners, our deferred tax asset would increase (decrease) by approximately $ million and the related liability for payments under the Tax Receivable Agreement would increase (decrease) by approximately $ million, assuming that the price per share of the Class A Common Stock at the time of the exchange and corporate tax rate remain the same. These amounts are estimates and have been prepared for informational purposes only. The actual amount of deferred tax assets and related liabilities that we will recognize will differ based on, among other things, the timing of the redemptions or exchanges, the price of our shares of Class A common stock at the time of the redemptions or exchanges and the tax rates then in effect.
Under the Tax Receivable Agreement, we may elect to terminate the Tax Receivable Agreement early by making an immediate cash payment equal to the present value of the anticipated future tax benefits that would be required to be paid by us to the Continuing Equity Owners and the Blocker Shareholders under the Tax Receivable Agreement. The calculation of such cash payment would be based on certain assumptions, including, among others (i) that any Continuing Equity Owners’ LLC Interests that have not been exchanged are deemed exchanged, in general, for the market value of our Class A common stock that would be received by such Continuing Equity Owner if such LLC Interests had been exchanged at the time of termination; (ii) we will have sufficient taxable income in each future taxable year to fully realize all potential tax savings; (iii) the federal tax rates for future years will be those specified in the law as in effect at the time of termination and the combined state and local tax rates will be an assumed tax rate; and (iv) certain non-amortizable assets are deemed disposed of within specified time periods. In addition, the present value of such tax benefit payments are discounted at a rate equal to the lessor of (x) % per annum, compounded annually and (y) basis points. Assuming that the market value of our Class A common stock were to be equal to $ , the midpoint of the estimated offering price set forth on the cover of this prospectus and that LIBO Rate were to be %, we estimate that the aggregate amount of these termination payments would be approximately $ million if we were to exercise our termination right immediately following this offering.
| (3) | Upon completion of the Transactions, we will become the sole managing member of GoHealth Holdings, LLC. Although we will have a minority economic interest in GoHealth Holdings, LLC, we will have the sole voting interest in, and control of the management of, GoHealth Holdings, |
94
Table of Contents
| LLC. As a result, we will consolidate the financial results of GoHealth Holdings, LLC and will report a noncontrolling interest related to the interests in GoHealth Holdings, LLC held by the Continuing Equity Owners on our consolidated balance sheet. Immediately following the Transactions, the economic interests held by the noncontrolling interest will be approximately %. If the underwriters were to exercise their option to purchase additional shares of our Class A common stock in full, the economic interests held by the noncontrolling interest would be approximately %. |
| (4) | Reflects the exchange of GoHealth Holdings, LLC common units held by the Continuing Equity Owners for shares of our Class A common stock, and the issuance of a number of shares of our Class B common stock to the Continuing Equity Owners, equal to the number of GoHealth Holdings, LLC common units retained by each, for nominal consideration. |
95
Table of Contents
GoHealth, Inc. and subsidiaries
Unaudited pro forma condensed consolidated statement of operations for the three months ended March 31, 2020
| (in thousands, except share amounts) | GoHealth Holdings, LLC Historical |
Pro Forma Transactions Adjustments |
As Further Adjusted for Pro Forma Transactions |
Pro Forma Offering Adjustments |
GoHealth, Inc. Pro Forma |
|||||||||||||||
| Net revenues: |
||||||||||||||||||||
| Commission |
112,510 | |||||||||||||||||||
| Other |
28,500 | |||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Net revenues |
$ | 141,010 | $ | $ | $ | $ | ||||||||||||||
| Operating expenses: |
||||||||||||||||||||
| Cost of revenue |
42,134 | |||||||||||||||||||
| Marketing and advertising |
26,073 | |||||||||||||||||||
| Customer care and enrollment |
23,978 | |||||||||||||||||||
| Technology |
4,593 | |||||||||||||||||||
| General and administrative |
10,491 | |||||||||||||||||||
| Change in fair value of contingent consideration liability |
4,400 | |||||||||||||||||||
| Amortization of intangible assets |
23,514 | |||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total operating expenses |
$ | 135,183 | $ | $ | $ | $ | ||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Income (loss) from operations |
5,827 | |||||||||||||||||||
| Interest expense |
6,756 | |||||||||||||||||||
| Other income (expense) |
10 | |||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Income (loss) before income taxes |
(939 | ) | ||||||||||||||||||
| Income tax expense (benefit) |
(2 | ) | (6 | ) | ||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Net income (loss) |
(937 | ) | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Net income attributable to noncontrolling interests |
— | (7 | ) | (7 | ) | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Net income attributable to GoHealth, Inc. |
$ | (937 | ) | $ | $ | $ | $ | |||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Pro Forma Per Share Data: |
||||||||||||||||||||
| Net income per share |
||||||||||||||||||||
| Basic |
||||||||||||||||||||
| Diluted |
||||||||||||||||||||
| Weighted-average shares used to compute net income per share |
||||||||||||||||||||
| Basic |
||||||||||||||||||||
| Diluted |
||||||||||||||||||||
96
Table of Contents
Unaudited pro forma condensed consolidated statement of operations for the Successor 2019 Period and Predecessor 2019 Period
| Predecessor 2019 Period |
Successor 2019 Period |
|||||||||||||||||||||||||||||||
| (in thousands, except share amounts) |
GoHealth Holdings, LLC Historical |
Successor GoHealth Holdings, LLC Historical |
Pro Forma Centerbridge Acquisition Adjustments |
As Adjusted for Pro Forma Centerbridge Acquisition Adjustments |
Pro Forma Transactions Adjustments |
As Further Adjusted for Pro Forma Transactions |
Pro Forma Offering Adjustments |
GoHealth, Inc. Pro Forma |
||||||||||||||||||||||||
| Net revenues: |
||||||||||||||||||||||||||||||||
| Commission |
$ | 175,834 | $ | 243,347 | $ | — | $ | 419,181 | ||||||||||||||||||||||||
| Other |
55,176 | 65,144 | — | 120,320 | ||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Net revenues |
231,010 | 308,491 | — | 539,501 | ||||||||||||||||||||||||||||
| Operating expenses: |
||||||||||||||||||||||||||||||||
| Cost of revenue |
79,169 | 90,384 | — | 169,553 | ||||||||||||||||||||||||||||
| Marketing and advertising |
37,769 | 24,811 | (1,509 | )(5) | 61,071 | |||||||||||||||||||||||||||
| Customer care and enrollment |
49,149 | 44,356 | 62 | (5) | 93,567 | |||||||||||||||||||||||||||
| Technology |
40,312 | 6,006 | (26,848 | )(5) | 19,470 | |||||||||||||||||||||||||||
| General and administrative |
79,219 | 13,674 | (59,557 | )(1)(5) | 33,336 | |||||||||||||||||||||||||||
| Change in fair value of contingent consideration liability |
— | 70,700 | — | 70,700 | ||||||||||||||||||||||||||||
| Amortization of intangible assets |
— | 28,217 | 65,840 | (2) | 94,057 | |||||||||||||||||||||||||||
| Transaction costs |
2,267 | 6,245 | (8,512 | )(3) | — | |||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Total operating expenses |
287,885 | 284,393 | (30,523 | ) | 541,755 | |||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Income (loss) from operations |
$ | (56,875 | ) | $ | 24,098 | $ | 30,523 | $ | (2,254 | ) | ||||||||||||||||||||||
| Interest expense |
140 | 8,076 | 18,956 | (4) | 27,172 | |||||||||||||||||||||||||||
| Other income (expense) |
(114 | ) | 17 | — | (97 | ) | ||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Income (loss) before income taxes |
(57,129 | ) | 16,039 | 11,567 | (29,523 | ) | ||||||||||||||||||||||||||
| Income tax expense (benefit) |
(66 | ) | 44 | — | (22 | ) | (6 | ) | ||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Net income (loss) |
(57,063 | ) | 15,995 | 11,567 | $ | (29,501 | ) | |||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Net income attributable to noncontrolling interests |
— | — | — | — | (7 | ) | (7 | ) | ||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Net income attributable to GoHealth, Inc. |
$ | (57,063 | ) | $ | 15,995 | $ | 11,567 | $ | (29,501 | ) | $ | $ | $ | $ | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Pro Forma Per Share Data: |
||||||||||||||||||||||||||||||||
| Net income per share |
||||||||||||||||||||||||||||||||
| Basic |
||||||||||||||||||||||||||||||||
| Diluted |
||||||||||||||||||||||||||||||||
| Weighted-average shares used to compute net income per share |
||||||||||||||||||||||||||||||||
| Basic |
||||||||||||||||||||||||||||||||
| Diluted |
||||||||||||||||||||||||||||||||
97
Table of Contents
GoHealth, Inc. and subsidiaries
Notes to unaudited pro forma condensed consolidated statement of operations
| (1) | Represents (i) the elimination of transaction-related bonuses paid to certain executive officers and employees incurred in connection with the Centerbridge Acquisition, which are not expected to have a continuing impact on the results of operations and (ii) a non-cash adjustment to rent expense associated with the resetting of deferred rent and the removal of leasehold improvement obligations through purchase accounting in connection with the Centerbridge Acquisition. The following table represents the pro forma adjustment to general and administrative expense for the year ended December 31, 2019: |
| (in thousands) | Year Ended December 31, 2019 |
|||
| Non-recurring transaction bonuses |
$ | (2,641 | ) | |
| Non-cash adjustments to rent expense made through purchase accounting |
444 | |||
|
|
|
|||
| Pro forma adjustment for general and administrative expense attributable to bonuses and rent expense |
$ | (2,197 | ) | |
|
|
|
|||
| (2) | Represents the incremental amortization expense related to certain definite-lived intangible assets, reflected in the purchase price allocation at the date of the Centerbridge Acquisition, as if those certain definite-lived intangible assets were put into place on January 1, 2019. The following table represents the pro forma adjustment to estimated amortization expense for the year ended December 31, 2019: |
| (in thousands) | Estimated Fair Value at Acquisition |
Estimated Useful Life |
Year Ended December 31, 2019 |
|||||||||
| Developed Technology |
$ | 496,000 | 7 years | $ | 70,857 | |||||||
| Customer Relationships |
232,000 | 10 years | 23,200 | |||||||||
|
|
|
|||||||||||
| Annual pro forma amortization expense |
$ | 94,057 | ||||||||||
| Less amount recorded |
28,217 | |||||||||||
|
|
|
|||||||||||
| Pro forma adjustment for estimated amortization expense |
$ | 65,840 | ||||||||||
|
|
|
|||||||||||
| (3) | Represents the elimination of direct and incremental transaction costs incurred in connection with the Centerbridge Acquisition, which are not expected to have a continuing impact on the results of operations. |
98
Table of Contents
| (4) | Represents (i) the elimination of interest expense related to our financing in place during the Predecessor 2019 Period, which was repaid in conjunction with the Centerbridge Acquisition and (ii) the incremental interest expense, accretion of debt discount, and amortization of debt issuance costs associated with our Credit Facilities incurred as part of the Centerbridge Acquisition. The following table represents the pro forma adjustment to interest expense for the year ended December 31, 2019: |
| (in thousands) | Year Ended December 31, 2019 |
|||
| Interest on credit agreement |
$ | 25,598 | ||
| Accretion of debt discount |
1,259 | |||
| Amortization of debt issuance costs |
317 | |||
|
|
|
|||
| Annual pro forma interest expense |
27,173 | |||
| Less expense recorded |
8,216 | |||
|
|
|
|||
| Pro forma adjustment for interest expense |
$ | 18,956 | ||
|
|
|
|||
| See “Description of Indebtedness” for a description of the Credit Facilities. |
| (5) | Represents a non-cash adjustment to removal of equity incentive compensation expense triggered as part of the Centerbridge Acquisition due to change in control provision which accelerated vesting, and includes the incremental share-based compensation expense related to the equity incentive compensation plan put in place in connection with the Centerbridge Acquisition, as if that plan had been in place since January 1, 2019. This adjustment was allocated to line items on the income statement based on the department the individual is in who received the compensation. The following tables represent the pro forma adjustments to each of the marketing and advertising, technology, general and administrative and customer care and enrollment expenses. |
| Marketing and Advertising |
| (in thousands) | Year Ended December 31, 2019 |
|||
| Equity incentive compensation triggered by Centerbridge Acquisition |
$ | (1,674 | ) | |
| Incremental share-based compensation expense |
166 | |||
|
|
|
|||
| Pro forma adjustment for marketing and advertising expense |
$ | (1,509 | ) | |
|
|
|
|||
| Technology |
| (in thousands) | Year Ended December 31, 2019 |
|||
| Equity incentive compensation triggered by Centerbridge Acquisition |
$ | (27,058 | ) | |
| Incremental share-based compensation expense |
211 | |||
|
|
|
|||
| Pro forma adjustment for technology expense |
$ | (26,848 | ) | |
|
|
|
|||
99
Table of Contents
| General and Administrative |
| (in thousands) | Year Ended December 31, 2019 |
|||
| Equity incentive compensation triggered by Centerbridge Acquisition |
$ | (58,327 | ) | |
| Incremental share-based compensation expense |
967 | |||
|
|
|
|||
| Pro forma adjustment for general and administrative expense attributable to share-based compensation |
$ | (57,360 | ) | |
|
|
|
|||
| Customer Care and Enrollment |
| (in thousands) | Year Ended December 31, 2019 |
|||
| Equity incentive compensation triggered by Centerbridge Acquisition |
$ | — | ||
| Incremental share-based compensation expense |
62 | |||
|
|
|
|||
| Pro forma adjustment for customer care and enrollment |
$ | 62 | ||
|
|
|
|||
| (6) | Following the Transactions, we will be subject to United States federal income taxes, in addition to applicable state and local taxes, with respect to our allocable share of any net taxable income of GoHealth Holdings, LLC. As a result, the unaudited pro forma consolidated statement of operations includes an adjustment to our income tax expense to reflect an effective income tax rate of %, which includes a provision for United States federal income taxes and assumes the highest statutory rates apportioned to each state and local jurisdiction. |
| (7) | After the Transactions we will become the managing member of GoHealth Holdings, LLC. We will own % of the economic interest in GoHealth Holdings, LLC, but will have % of the voting power and control the management of GoHealth Holdings, LLC. The Continuing Equity Owners will own the remaining % of the economic interest in GoHealth Holdings, LLC, which will be accounted for as a noncontrolling interest in our future consolidated financial results. |
100
Table of Contents
MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS
This section presents management’s perspective on our financial condition and results of operations. The following discussion and analysis is intended to highlight and supplement data and information presented elsewhere in this prospectus, including the consolidated financial statements and related notes, and should be read in conjunction with the accompanying tables and our annual audited financial statements. To the extent that this discussion describes prior performance, the descriptions relate only to the periods listed, which may not be indicative of our future financial outcomes. In addition to historical information, this discussion contains forward-looking statements that involve risks, uncertainties and assumptions that could cause results to differ materially from management’s expectations. Factors that could cause such differences are discussed in the sections titled “Cautionary Note Regarding Forward-Looking Statements,” “Risk Factors” and “Unaudited Pro Forma Condensed Consolidated Financial Information.” We assume no obligation to update any of these forward-looking statements.
Overview
We are a leading health insurance marketplace whose mission is to improve access to healthcare in America. Our proprietary technology platform leverages modern machine-learning algorithms powered by nearly two decades of insurance behavioral data to reimagine the optimal process for helping individuals find the best health insurance plan for their specific needs. Our differentiated combination of a vertically-integrated consumer acquisition platform and highly skilled and trained licensed agents, or agents, has enabled us to enroll millions of people in Medicare and individual and family plans since our inception. With over 10,000 Americans turning 65 years old every day and GoHealth’s track record of significant growth in net revenues in the Medicare space in the past five years, we believe we will continue to be one of the top choices for unbiased insurance advice to help navigate one of the most important purchasing decisions individuals make.
We have a 19-year history of consistent revenue growth and entering new market segments of insurance products. We add significant value to consumers and carriers, which is evidenced by our high growth rate and strong customer engagement dynamics. Specifically, net revenues grew by 104.1% to $141.0 million for the three months ended March 31, 2020 compared to $69.1 million for the three months ended March 31, 2019 and by 138.5% to $539.5 million for the Pro Forma Fiscal Year 2019 compared to $226.2 million for the year ended December 31, 2018. Adjusted EBITDA grew by 391.5% to $34.9 million for the three months ended March 31, 2020 compared to $7.1 million for the three months ended March 31, 2019 and by 386.8% to $170.0 million for the Pro Forma Fiscal Year 2019 from $34.9 million for the year ended December 31, 2018. Net loss was $937 thousand for the three months ended March 31, 2020 compared to net income of $5.0 million for the three months ended March 31, 2019, and net loss was $29.5 million for the Pro Forma Fiscal Year 2019 compared to net income of $28.1 million for the year ended December 31, 2018. See “Prospectus Summary—Summary Historical and Pro Forma Condensed Consolidated Financial and Other Data” for information regarding our use of (i) pro forma financial information, specifically footnote 1 and (ii) Adjusted EBITDA, a non-GAAP financial measure, and a reconciliation of Adjusted EBITDA to net income, the most directly comparable financial measure calculated and presented in accordance with GAAP.
Business Segments
We have four reportable segments: (i) Medicare—Internal, (ii) Medicare—External, (iii) Individual and Family Plans, or IFP and Other—Internal and (iv) IFP and Other—External. We organize the segments by product type, Medicare and IFP and Other, as well as by distribution channel, internal and external, as further described below. In addition, we separately report other expenses (classified as “Corporate” in our financial statements), the primary components of which are corporate overhead expenses and shared service expenses that have not been allocated to the reportable segments. The segment results provided herein may not be comparable to other companies. We refer to the Medicare—Internal and Medicare—External segments collectively as the “Medicare
101
Table of Contents
segments” and the IFP and Other—Internal and IFP and Other—External segments as the “IFP and Other segments.”
| • | Medicare—Internal. The Medicare—Internal segment relates to sales of products and plans by GoHealth-employed agents offering qualified prospects plans from multiple carriers, GoHealth-employed agents offering qualified prospects plans on a carrier-specific basis, or sales of products and plans through our online platform without the assistance of our agents, which we refer to as DIY. In this segment, we sell Medicare Advantage, Medicare Supplement, Medicare prescription drug plans, and Medicare Special Needs Plans, or SNPs. We earn revenue in this segment through commissions paid by carriers based on sales we generate, as well as enrollment fees, hourly fees and other fees for services performed for specific carriers and other partners. For the three months ended March 31, 2020 and 2019, the Pro Forma Fiscal Year 2019 and for the year ended December 31, 2018, this segment generated 67.6%, 30.3%, 58.9% and 23.6%, respectively, of total revenue and 98.4%, 46.8%, 88.5% and 52.8%, respectively, of total profit. |
| • | Medicare—External. The Medicare—External segment relates to sales of products and plans under GoHealth’s carrier contracts using an independent, national network of agents, or external agencies, agents of which are not employed by GoHealth. These agents utilize our technology and platform to enroll consumers in health insurance plans and provide a means to earn a return on leads that otherwise may have not been addressed. In this segment, we sell Medicare Advantage, Medicare Supplement, Medicare prescription drug plans, and SNPs. We earn revenue in this segment through commissions paid by carriers as a result of policy sales, as well as sales of consumer leads to external agencies. For the three months ended March 31, 2020 and 2019, the Pro Forma Fiscal Year 2019 and for the year ended December 31, 2018, this segment generated 20.5%, 29.4%, 21.3% and 26.0%, respectively, of total revenue and (0.8)%, 32.5%, 8.2% and 19.7%, respectively, of total profit. |
| • | IFP and Other—Internal. The IFP and Other—Internal segment relates to sales of products and plans by GoHealth-employed agents offering qualified prospects plans from multiple carriers, GoHealth-employed agents offering qualified prospects plans on a carrier-specific basis, or DIY. In this segment, we sell individual and family plans, dental plans, vision plans and other ancillary plans to individuals that are not Medicare-eligible. We earn revenue in this segment through commissions paid by carriers based on sales we generate, as well as enrollment fees, and hourly fees and other fees for services performed for specific carriers and other partners. For the three months ended March 31, 2020 and 2019, the Pro Forma Fiscal Year 2019 and for the year ended December 31, 2018, this segment generated 6.1%, 20.9%, 10.9% and 27.9%, respectively, of total revenue and 1.1%, 8.5%, 2.0% and 21.2% respectively, of total profit. |
| • | IFP and Other—External. The IFP and Other—External segment relates to sales of products and plans under GoHealth’s carrier contracts using external agencies, who use agents that are not employed by GoHealth. These agents utilize our technology and platform to enroll consumers in health insurance plans. We also sell consumer leads generated by us to external agencies. In this segment, we sell individual and family plans, dental plans, vision plans and other ancillary plans to individuals that are not Medicare-eligible. We earn revenue in this segment through commissions paid by carriers as a result of policy sales, as well as sales of consumer leads to external agencies. For the three months ended March 31, 2020 and 2019, the Pro Forma Fiscal Year 2019 and for the year ended December 31, 2018, this segment generated 5.8%, 19.4%, 8.9% and 22.5%, respectively, of total revenue and 1.2%, 12.2%, 1.2% and 6.2%, respectively, of total profit. |
Industry Trends
The Medicare segments benefit from strong demographic trends. Medicare enrollment is expected to grow from approximately 61 million individuals in 2019 to approximately 77 million individuals by 2028. An increasing proportion of the Medicare-eligible population is choosing commercial insurance solutions, with 38% of Medicare beneficiaries, or approximately 23 million people, enrolled in Medicare Advantage plans in 2019, an
102
Table of Contents
increase of approximately 1.5 million people from 2018 to 2019. As a result of these trends, today, we estimate a total addressable market of $28 billion for Medicare Advantage and Medicare Supplement products, which is based on third-party estimates of total expected Medicare enrollees for 2020, publicly available industry data for Medicare agents’ first-year compensation and our recent historical policy revenue experience. We believe that these trends will help us continue to grow revenue.
In the IFP and Other segments, the individual health insurance market grew from 10.6 million enrollees in 2013 to 17.4 million enrollees in 2015. Such increase was driven by the passage of the ACA, namely (1) the requirement to purchase health insurance, or the individual mandate, (2) the requirement that carriers not consider pre-existing medical conditions in coverage decisions and (3) premium subsidies for middle and lower income individuals that were also contained in that legislation. With the repeal of the individual mandate in 2017 and broader economic trends, such as gains in employment, which increased the number of people having job-based coverage, the individual market has declined. Despite the decline, the individual market was composed of 13.8 million members in 2018, a meaningful increase from 2011 levels and in 2019, the market size stabilized with 13.7 million members enrolled. This market stabilization was driven by lower premium increases in 2019, as compared to 2018 and 2017 for individual insurance plans; an increase in individuals who do not receive job-based insurance due to the rise of the “gig economy;” and, expanded plan options in the individual market from carriers. According to a Kaiser Family Foundation report published in 2020, in the third quarter of 2019, the average gross margin per member per month for carriers in the individual market was $131.17, as compared to $32.88 in the third quarter of 2016 shortly after the repeal of the individual mandate. This increased profitability for insurers is expected to have a positive impact on the individual market going forward. In addition, the number of individuals eligible for the individual market is growing. Forbes estimated that 57 million U.S. workers, approximately 36% of employees, are in the “gig economy” and many of these individuals will not receive health insurance through their jobs. We believe that growth in the individual market will benefit the Company’s revenue growth in the future.
Reorganization Transactions
The historical results of operations discussed in this section are those of GoHealth Holdings, LLC prior to the completion of the Transactions, including this offering, and do not reflect certain items that we expect will affect our results of operations and financial condition after giving effect to the Transactions and the use of proceeds from this offering.
Following the completion of the Transactions, GoHealth, Inc. will become the sole managing member of GoHealth Holdings, LLC. Although we will have a minority economic interest in GoHealth Holdings, LLC, we will have the sole voting interest in, and control of the business and affairs of, GoHealth Holdings, LLC and its direct and indirect subsidiaries. As a result, GoHealth, Inc. will consolidate GoHealth Holdings, LLC and record a significant non-controlling interest in a consolidated entity in GoHealth, Inc.’s consolidated financial statements for the economic interest in GoHealth Holdings, LLC held by the Continuing Equity Owners. Immediately after the Transactions, investors in this offering will collectively own % of our outstanding Class A common stock, consisting of shares (or shares if the underwriters exercise in full their option to purchase additional shares of Class A common stock), GoHealth, Inc. will own LLC Interests (or LLC Interests if the underwriters exercise in full their option to purchase additional shares of Class A common stock), representing % of the LLC Interests (or % if the underwriters exercise in full their option to purchase additional shares of Class A common stock) and the Continuing Equity Owners will collectively own LLC Interests, representing % of the LLC Interests (or % if the underwriters exercise in full their option to purchase additional shares of Class A common stock). Accordingly, net income (loss) attributable to non-controlling interests will represent % of the income (loss) before income tax benefit (expense) of GoHealth, Inc. (or % if the underwriters exercise in full their option to purchase additional shares of Class A common stock). GoHealth, Inc. is a holding company that conducts no operations and, as of the consummation of this offering, its principal asset will be LLC Interests we purchase from GoHealth Holdings, LLC.
After consummation of this offering, GoHealth, Inc. will become subject to U.S. federal, state and local income taxes with respect to our allocable share of any taxable income of GoHealth Holdings, LLC and will be taxed at
103
Table of Contents
the prevailing corporate tax rates. In addition to tax expenses, we also will incur expenses related to our status as a public company, plus payment obligations under the Tax Receivable Agreement, which we expect to be significant. We intend to cause GoHealth Holdings, LLC to make distributions to us in an amount sufficient to allow us to pay these expenses and fund any payments due under the Tax Receivable Agreement. See “Certain Relationships and Related Party Transactions—GoHealth LLC Agreement—Agreement in Effect Upon Consummation of the Transactions—Distributions.”
Factors Affecting Our Results of Operations
Our financial condition and results of operations have been, and will continue to be affected by, a number of important factors, including:
| • | Ability to Attract New Carriers and Expand Relationships with Existing Carriers. We generate revenue primarily from commissions earned through policy sales utilizing our platform. Carriers and other partners also pay us enrollment fees, hourly fees and other fees for services performed for specific carriers. Attracting new carriers and expanding relationships with our existing carriers to offer more products and plans is critical to the growth of our business, particularly in the Medicare segments, which drive the highest LTV/CAC of the products and plans we offer. We are strategically adding carriers in the Medicare segments in order to offer top-rated plans and multiple plan choices in each of the U.S. counties in which we operate. This also allows us to market more efficiently in these geographies, increase conversion rates on consumer leads, and improve customer satisfaction rates as we are better able to meet consumers’ specific needs, which drives revenue growth. In order to strengthen the relationships with existing and prospective Medicare carriers, we are offering more services to them, such as (i) helping new Medicare enrollees sign up for a health-risk assessment, which helps calibrate the Medicare Advantage premium paid by Medicare to the private plan, and (ii) using our data to help our largest carriers inform the benefit design of their health insurance plans and competitiveness of their products in given regions. If we are unsuccessful in adding new carriers and expanding existing relationships with carriers to offer more products and plans, it may become more difficult to compete against competitors with more diverse product and plan offerings. |
| • | Data and Technology. Our ability to harness our data and proprietary technology is a significant contributor to improving LTV/CAC and driving profitability. In 2019, we upgraded our Marketplace technology to improve the flow of data across our platform and advance decision support capabilities. We are also improving our LeadScore and call-routing technologies, as well as expanding our business intelligence and analytics staffing, to direct qualified prospects to agents or DIY channels that are most likely to result in such qualified prospects enrolling in the plan that best meets their needs while remaining economically attractive for us, as described further below. Additionally, we are investing in technology that will allow us to use our data to direct our marketing spend into growing the number of qualified prospects in the highest-value marketing channels and enhancing our proprietary LeadScore technology to assess and improve, in real time, the performance of those marketing channels throughout the year. If we are not able to harness our data to improve our technology, our LTV/CAC may remain stagnant or decline. |
| • | Agent Productivity, Training, Recruiting and Retention. Our success largely depends on the productivity of our agents, as well as our ability to recruit and retain quality agents to sell products and plans. The productivity of our agents is primarily supported by our technology, which helps increase agent efficiency. For example, the improvements to our LeadScore and call-routing technologies allow us to assess the profile and predicted value of each incoming consumer lead and to route the consumer lead to the agent most likely to enroll them. Our technology considers the incoming consumer lead’s potential needs and the agent’s ability to deliver a suitable policy and, in doing so, increases our LTV per Approved Submission and decreases the amount of time it takes for an agent to select plans for the consumer, thus decreasing CAC per commissionable Approved Submission. Our call-routing technology also utilizes data-driven agent clustering to enable us to train and specialize our agents on specific customer segments to optimize our results. Additionally, we are retooling our recruiting and |
104
Table of Contents
| training programs to better attract agent candidates whose profiles align with those of current, high performing agents we employ. The opportunity to reduce the variability in our agent performance is significant, as our top 25% of agents for the multi-carrier sales outlet of the Medicare—Internal segment on average were 61% more productive than the remaining 75% of our agents for the multi-carrier sales outlet of the Medicare—Internal segment, based on conversion rates of qualified prospects to Submitted Policies for the three months ended March 31, 2020. These top 25% of agents for the multi-carrier sales outlet of the Medicare—Internal segment achieved a 34% conversion rate of qualified prospects to Submitted Policies over the same three month period as compared to 21% conversion rate for the remaining 75% of our agents for the multi-carrier sales outlet of the Medicare—Internal segment over the same period. Our ability to sell more products and plans is dependent on the number of qualified, licensed agents we have that are able to sell those products and plans. Therefore, recruiting and retaining quality agents is also a key driver of our business. If we are unable to recruit and retain agents, we may be limited in the number of products and plans we can sell for a carrier or in a particular geography and we may have difficulty in quickly and efficiently managing the volume of qualified prospects that we generate. |
| • | Customer Engagement. Increasing customer engagement is a key driver of our business and results of operations. Our ability to improve long-term customer satisfaction is dependent on the level of engagement we have with our customers. We are able to improve our long-term customer satisfaction by ensuring that we are successfully matching products and plans to consumers at the point of enrollment and having continued customer interactions throughout the life of the policy, both digitally and telephonically. We have a TeleCare team that is tasked with improving outreach efforts to our customers after their enrollment, which has allowed us to (1) educate customers on how to utilize these supplemental benefits, (2) educate customers on how to ensure that their physicians and medications are within their plan benefits, and (3) through more frequent interactions, identify if there are changes in a customer’s health, financial or other circumstances that make another plan a better choice for their specific needs. As a marketplace that represents a multitude of both plans and carriers, we can educate customers even as their underlying plan or carrier changes if we proactively engage with them. |
| • | Seasonality of Our Revenue. We derive a substantial portion of our commission revenue in the fourth quarter because the annual Medicare annual enrollment period occurs from October 15th to December 7th. Additionally, as a result of the annual Medicare Advantage open enrollment period that occurs from January 1st to March 31st, commission revenue is typically second-highest in our first quarter. Although we are able to generate revenue throughout the year, including through selling products and plans to individuals who turn 65 or qualify for a Medicare special enrollment period, as well as offering additional services and ancillary products and plans throughout the year, our success is substantially dependent on selling products and plans during the Medicare annual enrollment period and the Medicare Advantage open enrollment period. |
Response to COVID-19
With social distancing measures having been implemented to curtail the spread of COVID-19, we successfully transitioned our agents and other employees to a work from home working environment. We believe the investments we have made in our technology infrastructure have allowed for a seamless transition to a remote working environment without any material impacts to our business, highlighting the resilience of our business. We believe that a business like ours is well-suited to navigate the current environment in which consumers are particularly focused on healthcare issues and mortality and social distancing requirements push consumers to conduct business remotely, while the underlying demand dynamics for our core products remain unchanged. Additionally, because of our remote agent platform, we believe agents will continue to be attracted to our commission-based agent compensation model and the stable and attractive source of income it can provide, thereby allowing us to continue to retain and recruit agents. Further, as consumers become more comfortable with conducting business remotely, we believe consumer adoption of distribution models such as ours may continue to accelerate long after the COVID-19 pandemic ends.
105
Table of Contents
As a result of the COVID-19 pandemic, we transitioned over 99% of our agents to work from home over an approximately 72-hour period in March 2020. Our agents have remained efficient during this work from home period, with daily sales per agent seat in the multi-carrier sales outlet of the Medicare—Internal segment of 2.3, 2.6 and 2.2 for February, March and April 2020, respectively, compared to 2.0, 2.1 and 1.5 daily sales per agent seat for the same three months in 2019. In addition, we had 23,609, 25,777 and 20,851 Approved Submissions in the multi-carrier sales outlet of the Medicare—Internal segment for February, March and April 2020, respectively, compared to 5,047, 6,384 and 6,699 Approved Submissions for the same three months in 2019.
There are no comparable recent events which may provide guidance as to the effect of the spread of COVID-19 and a global pandemic, and, as a result, the ultimate impact of the COVID-19 outbreak or a similar health epidemic is highly uncertain and subject to change. We do not yet know the full extent of the impacts on our business, our operations or the global economy as a whole. However, the effects could have a material impact on our results of operations. See “Risk Factors—Risks Related to Our Business—The extent to which the COVID-19 outbreak and measures taken in response thereto impact our business, results of operations and financial condition will depend on future developments, which are highly uncertain and cannot be predicted.”
Key Business and Operating Metrics by Segment
In addition to traditional financial metrics, we rely upon certain business and operating metrics to evaluate our business performance and facilitate our operations. Below are the most relevant business and operating metrics for each segment, except for EBITDA and Adjusted EBITDA, which are not presented on a segment basis.
Medicare Segments
Lifetime Value of Commissions per Consumer Acquisition Cost
Lifetime value of commissions per consumer acquisition cost, or LTV/CAC, represents (i) aggregate commissions estimated to be collected over the estimated life of all commissionable Approved Submissions for the relevant period based on multiple factors, including but not limited to, contracted commission rates, carrier mix and expected policy persistency with applied constraints, or LTV, divided by (ii) the cost to convert a qualified prospect into a Submitted Policy (comprised of cost of revenue, marketing and advertising expenses and customer care and enrollment expenses) less other non-commission carrier revenue for such period, or CAC. CAC is comprised of cost of revenue, marketing and advertising expenses and customer care and enrollment expenses less other revenue and is presented on a per commissionable Approved Submission basis. The estimate of the future renewal commissions is determined by using the contracted renewal commission rates constrained by a persistency-adjusted renewal period. The persistency-adjusted renewal period is determined based on our historical experience and available industry and insurance carrier historical data. Persistency-adjustments allow us to estimate renewal revenue only to the extent probable that a material reversal in revenue would not be expected to occur. These factors may result in varying values from period to period. See “Risk Factors—Risks Related to Our Business—Our operating results may be adversely impacted by factors that impact our estimate of LTV.”
The LTV/CAC for the Medicare—Internal segment increased to 2.7x (with a CAC of $26.7 million) for the three months ended March 31, 2020 compared to 1.7x (with a CAC of $10.5 million) for the three months ended March 31, 2019. The increase in LTV/CAC from March 31, 2019 to March 31, 2020 is attributable to the same factors as contributed to the increase from 2018 to 2019, as described below. The LTV/CAC for the Medicare—Internal segment decreased to 6.0x (with a CAC of 26.4 million) for the three months ended December 31, 2019 compared to 6.8x (with a CAC of 4.3 million) for the three months ended December 31, 2018. The decrease in LTV/CAC from December 31, 2018 to December 31, 2019 is the direct result of the Company scaling up its production to drive roughly 5.4x revenue growth period over the same period.
The LTV/CAC for the Medicare—Internal segment was 3.8x (with a CAC of $63.2 million) for the year ended December 31, 2019, 5.1x (with a CAC of $32.5 million) for the Successor 2019 Period and 2.7x (with a CAC of
106
Table of Contents
$30.7 million) for the Predecessor 2019 Period compared to 2.7x (with a CAC of $17.3 million) for the year ended December 31, 2018. The increase in LTV/CAC from 2018 to 2019 was primarily attributable to a decrease in CAC due to improvements in our LeadScore and call-routing technologies allowing our agents to successfully convert more qualified prospects into Submitted Policies. Additionally, improved marketing efficiencies driven by our rapid test-and-learn approach across our marketing channels, as well as an expansion of the diversity and breadth of our omni-channel marketing efforts also contributed to an increase in LTV/CAC by enabling the acquisition of higher quality prospects at a lower effective cost per submission.
Cost Per Qualified Prospect
Cost per qualified prospect represents all variable marketing costs to generate qualified prospects, including direct media expenses, merchant service fees and Advocate expenses, divided by the number of qualified prospects.
The following table shows cost per qualified prospect for the Medicare—Internal segment:
| Three Months Ended March 31, |
Year Ended December 31, 2019 |
Successor 2019 Period |
Predecessor 2019 Period |
Year Ended December 31, 2018 (Predecessor) |
||||||||||||||||||||
| 2020 (Successor) |
2019 (Predecessor) |
|||||||||||||||||||||||
| Cost per Qualified Prospect (Medicare—Internal segment) |
$ | 57 | $ | 87 | $ | 63 | $ | 53 | $ | 77 | $ | 48 | ||||||||||||
Cost per qualified prospect decreased by 34.5% for the three months ended March 31, 2020 compared to the three months ended March 31, 2019. The decrease is primarily attributable to a shift of lead production to rely more on internally generated leads rather than externally generated leads. Costs for new consumer lead sources in 2019 were reduced through a robust test-and-learn approach to marketing efforts throughout 2019 and early 2020.
Cost per qualified prospect was $63 for the year ended December 31, 2019, $53 for the Successor 2019 Period and $77 for the Predecessor 2019 Period compared to $48 for the year ended December 31, 2018. The increase of 31.3% from 2018 to 2019 was primarily attributable to increased volume of consumer lead sources over the same period. New consumer lead sources initially resulted in increased costs compared to more mature consumer lead sources in early 2019. However, costs associated with new consumer lead sources decreased over the course of 2019 as we optimized new and existing sources through our rapid test-and-learn approach.
Submitted Policies
Submitted Policies represent completed applications that, with respect to each such application, the consumer has authorized us to submit to the carrier. The applicant may need to take additional actions, including providing subsequent information before the application is reviewed by the carrier.
107
Table of Contents
The following table shows the number of Submitted Policies by product for the Medicare segments for the periods presented, split between those submissions that are commissionable (compensated through commissions received from carriers), compared to those that are non-commissionable (compensated via hourly fees and enrollment fees):
| Three Months Ended March 31, |
Year Ended December 31, 2019 |
Successor 2019 Period |
Predecessor 2019 Period |
Year Ended December 31, 2018 (Predecessor) |
||||||||||||||||||||
| 2020 (Successor) |
2019 (Predecessor) |
|||||||||||||||||||||||
| Medicare Advantage |
117,312 | 36,056 | 356,772 | 213,821 | 134,885 | 91,314 | ||||||||||||||||||
| Medicare Supplement |
2,671 | 3,854 | 18,649 | 5,778 | 10,263 | 11,606 | ||||||||||||||||||
| Prescription Drug Plans |
2,494 | 2,692 | 21,513 | 13,838 | 7,675 | 12,617 | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Total Medicare—Commissionable |
122,477 | 42,602 | 396,934 | 233,437 | 152,823 | 115,537 | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Medicare Advantage |
6,927 | 498 | 22,015 | 26,553 | 3,528 | 1,172 | ||||||||||||||||||
| Medicare Supplement |
1,812 | 156 | 5,236 | 5,851 | 1,993 | 1,340 | ||||||||||||||||||
| Prescription Drug Plans |
798 | 27 | 3,512 | 3,041 | 471 | 327 | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Total Medicare—Non Commissionable |
9,537 | 681 | 30,763 | 35,445 | 5,992 | 2,839 | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Total Medicare Submitted Policies |
132,014 | 43,283 | 427,697 | 268,882 | 158,815 | 118,376 | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
Total Medicare Submitted Policies increased by 205.3% for the three months ended March 31, 2020 compared to the three months ended March 31, 2019. The increase is attributable to the same factors that contributed to the increase from 2018 to 2019, as described below.
Total Medicare Submitted Policies was 427,697 for the year ended December 31, 2019, 146,228 for the Successor 2019 Period and 150,544 for the Predecessor 2019 Period compared to 118,376 for the year ended December 31, 2018. The increase of 261.3% from 2018 to 2019 in Total Medicare Submitted Policies was primarily attributable to improved multichannel marketing strategies that allowed us to generate a greater number of high quality prospects, along with increased efficiency of our agents. Agent efficiency increased due to the implementation of more efficient marketing strategies and improvements in our LeadScore and call-routing technologies, which allowed our agents to increase the number of qualified prospects they are able to talk to and improve the rate at which a qualified prospect converts to a Submitted Policy. Additionally, the expansion of our facilities to accommodate additional agents and the hiring of additional agents also contributed to the increase in Submitted Policies in the Medicare—Internal segment. During the 2019 Medicare annual enrollment period, the Medicare—Internal segment had at its peak roughly 1,040 full time equivalent agents, compared to roughly 230 in the comparable period of 2018. For the Medicare—External segment, the increase in total Submitted Policies was due to our ability to recruit and onboard additional external agencies to enroll consumers in Medicare plans using our technology and platform.
Approved Submissions
Approved Submissions represent Submitted Policies approved by carriers for the identified product during the indicated period. Not all Approved Submissions will go in force, as some individuals we enroll may not ultimately pay their insurance premiums or may switch out of a policy within the disenrollment period during the first 90 days of the policy. In general, the relationship between Submitted Policies and Approved Submissions has been steady over time. Therefore, factors impacting the number of Submitted Policies also impact the number of Approved Submissions.
The following table shows the number of Approved Submissions relating to commissionable policies for each of the Medicare segments for the periods presented. Only commissionable policies are used to calculate our LTV.
108
Table of Contents
Medicare—Internal
| Three Months Ended March 31, |
Year Ended December 31, 2019 |
Successor 2019 Period |
Predecessor 2019 Period |
Year Ended December 31, 2018 (Predecessor) |
||||||||||||||||||||
| 2020 | 2019 | |||||||||||||||||||||||
| Medicare Advantage |
83,608 | 19,460 | 246,513 | 159,969 | 86,544 | 45,876 | ||||||||||||||||||
| Medicare Supplement |
822 | 1,069 | 5,050 | 1,852 | 3,198 | 3,753 | ||||||||||||||||||
| Prescription Drug Plans |
2,174 | 1,585 | 14,021 | 8,943 | 5,078 | 8,115 | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Medicare—Internal Commissionable Approved Submissions |
86,604 | 22,114 | 265,584 | 170,764 | 94,820 | 57,744 | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
Medicare—Internal commissionable Approved Submissions increased by 291.6% for the three months ended March 31, 2020 compared to the three months ended March 31, 2019. The growth in Medicare—Internal commissionable Approved Submissions was attributable to the same drivers that increased Medicare—Internal commissionable Approved Submissions for the year ended December 31, 2019, as described below.
Medicare—Internal commissionable Approved Submissions were 265,584 for the year ended December 31, 2019, 170,764 for the Successor 2019 Period and 94,820 for the Predecessor 2019 Period compared to 57,744 for the year ended December 31, 2018. The growth of 359.9% from 2018 to 2019 in Medicare—Internal commissionable Approved Submissions was primarily attributable to the hiring of additional agents (including the expansion of our facilities to accommodate additional agents), the increased efficiency of our agents due to technology improvements and improved multichannel marketing strategies that allowed us to generate a greater number of high quality prospects.
Medicare—External
| Three Months Ended March 31, |
Year Ended December 31, 2019 |
Successor 2019 Period |
Predecessor 2019 Period |
Year Ended December 31, 2018 (Predecessor) |
||||||||||||||||||||
| 2020 | 2019 | |||||||||||||||||||||||
| Medicare Advantage |
32,287 | 16,614 | 102,193 | 53,852 | 48,341 | 45,397 | ||||||||||||||||||
| Medicare Supplement |
1,558 | 2,598 | 10,991 | 3,926 | 7,065 | 8,048 | ||||||||||||||||||
| Prescription Drug Plans |
481 | 1,107 | 7,492 | 4,895 | 2,597 | 4,502 | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Medicare—External Commissionable Approved Submissions |
34,326 | 20,319 | 120,676 | 62,673 | 58,003 | 57,947 | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
Medicare—External commissionable Approved Submissions increased by 68.9% for the three months ended March 31, 2020 compared to the three months ended March 31, 2019. The growth in Medicare—External commissionable Approved Submissions was attributable to the same drivers that increased Medicare—External commissionable Approved Submissions for the year ended December 31, 2019, as described below.
Medicare—External commissionable Approved Submissions were 120,676 for the year ended December 31, 2019, 62,673 for the Successor 2019 Period and 58,003 for the Predecessor 2019 Period compared to 57,947 for the year ended December 31, 2018. The growth of 108.3% from 2018 to 2019 in Medicare—External commissionable Approved Submissions was primarily attributable to our ability to recruit and onboard additional external agencies to enroll consumers in Medicare plans.
Lifetime Value of Commissions per Approved Submission
Lifetime value of commissions per commissionable Approved Submission, or LTV per Approved Submission, represents (i) aggregate commissions estimated to be collected over the estimated life of all commissionable
109
Table of Contents
Approved Submissions for the relevant period based on multiple factors, including but not limited to, contracted commission rates, carrier mix and expected policy persistency with applied constraints, divided by (ii) the number of commissionable Approved Submissions for such period. LTV per Approved Submission is equal to the sum of the commission revenue due upon the initial sale of a policy, and when applicable, an estimate of future renewal commissions per commissionable Approved Submissions. The estimate of the future renewal commissions is determined by using the contracted renewal commission rates constrained by a persistency-adjusted renewal period. The persistency-adjusted renewal period is determined based on our historical experience and available industry and carrier historical data. Persistency-adjustments allow us to estimate renewal revenue only to the extent probable that a material reversal in revenue would not be expected to occur. These factors may result in varying values from period to period. LTV per Approved Submission represents commissions only from policies sold during the period, but excludes policies originally submitted in prior periods.
The following table shows the LTV per Approved Submission for the Medicare segments for the periods presented:
| Three Months Ended March 31, |
Year Ended December 31, 2019 |
Successor 2019 Period |
Predecessor 2019 Period |
Year Ended December 31, 2018 (Predecessor) |
||||||||||||||||||||||||
| 2020 (Successor) |
2019 (Predecessor) |
|||||||||||||||||||||||||||
| Medicare Advantage |
$ | 857 | $ | 860 | $ | 978 | $ | 1,024 | $ | 906 | $ | 936 | ||||||||||||||||
| Medicare Supplement |
$ | 920 | $ | 926 | $ | 957 | $ | 944 | $ | 964 | $ | 798 | ||||||||||||||||
| Prescription Drug Plans |
$ | 215 | $ | 191 | $ | 206 | $ | 213 | $ | 194 | $ | 190 | ||||||||||||||||
LTV per Approved Submission for Medicare Advantage remained approximately flat for the three months ended March 31, 2020 compared to the three months ended March 31, 2019 as commission rates slightly increased but were offset by a variance in carrier mix and slight changes in policy effectuation and churn during this time period. LTV per Approved Submission for Medicare Supplement remained approximately flat for the three months ended March 31, 2020 compared to the three months ended March 31, 2019 as changes in carrier mix were offset by decreases in the estimates of plan persistency. LTV per Approved Submission for prescription drug plans increased by 12.4% for the three months ended March 31, 2020 compared to the three months ended March 31, 2019 primarily due to improved persistency rates and carrier mix shifts.
LTV per Approved Submission for Medicare Advantage was $978 for the year ended December 31, 2019, $1,024 for the Successor 2019 Period and $906 for the Predecessor 2019 Period compared to $936 for the year ended December 31, 2018. The increase of 4.5% from 2018 to 2019 was primarily due to an increase in CMS-approved commission rates and a more diverse carrier base allowing us to offer more products and plans that could satisfy a diverse range of needs contributing to more long-term customer satisfaction with their policy, partially offset by the effect of our seasonality, given the greater mix of our volumes in 2019 was generated outside of the Medicare annual enrollment period when LTV per Approved Submission is generally lower. LTV per Approved Submission for Medicare Supplement was $957 for the year ended December 31, 2019, $944 for the Successor 2019 Period and $964 for the Predecessor 2019 Period compared to $798 for the year ended December 31, 2018. The increase of 19.9% from 2018 to 2019 was primarily due to improved persistency rates and carrier mix shifts. LTV per Approved Submission for prescription drug plans was $206 for the year ended December 31, 2019, $213 for the Successor 2019 Period and $194 for the Predecessor 2019 Period compared to $190 for the year ended December 31, 2018. The increase of 8.4% from 2018 to 2019 was primarily due to improved persistency rates and carrier mix shifts.
110
Table of Contents
IFP and Other Segments
Submitted Policies
Submitted Policies represent the number of completed applications that, with respect to each such application, the consumer has authorized us to submit to the carrier. The applicant may need to take additional actions, including providing subsequent information before the application is reviewed by the carrier.
Total Submitted Policies for the IFP and Other segments decreased by 29.5% to 38,002 for the three months ended March 31, 2020 compared to 53,886 for the three months ended March 31, 2019 due to a change in strategy to prioritize agents and marketing and advertising spend in the Medicare segments instead of IFP and Other.
Total Submitted Policies for the IFP and Other segments was 296,772 for the year ended December 31, 2019, 146,228 for the Successor 2019 Period and 150,544 for the Predecessor 2019 Period compared to 207,695 for the year ended December 31, 2018. The increase of 42.9% from 2018 to 2019 was driven by the growth of our single carrier partnerships.
EBITDA, Adjusted EBITDA and Adjusted EBITDA Margin
| Pro Forma GoHealth, Inc. | ||||||||||||||||||||||||||||||||
| (in thousands) |
Three Months Ended March 31, 2020 |
Year Ended December 31, 2019 |
Three Months Ended March 31, |
Successor 2019 Period |
Predecessor 2019 Period |
Year Ended December 31, 2018 (Predecessor) |
||||||||||||||||||||||||||
| 2020 (Successor) |
2019 (Predecessor) |
|||||||||||||||||||||||||||||||
| Net income (loss) |
$ | $ | (29,501 | ) | $ | (937 | ) | $ | 5,002 | $ | 15,995 | $ | (57,063 | ) | $ | 28,114 | ||||||||||||||||
| Interest expense |
27,172 | 6,756 | 28 | 8,076 | 140 | 224 | ||||||||||||||||||||||||||
| Income tax expense (benefit) |
(22 | ) | (2 | ) | 2 | 44 | (66 | ) | 46 | |||||||||||||||||||||||
| Depreciation and amortization expense |
98,825 | 24,147 | 1,538 | 28,738 | 4,247 | 6,160 | ||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
| EBITDA |
96,474 | 29,965 | 6,569 | 52,853 | (52,742 | ) | 34,544 | |||||||||||||||||||||||||
| Share-based compensation(1) |
1,853 | 479 | — | 448 | 87,060 | — | ||||||||||||||||||||||||||
| Change in fair value of contingent consideration liability(2) |
70,700 | 4,400 | — | 70,700 | — | — | ||||||||||||||||||||||||||
| Centerbridge Acquisition costs(3) |
— | — | — | 6,245 | 4,908 | — | ||||||||||||||||||||||||||
| Severance costs(4) |
966 | 77 | 566 | 219 | 747 | 319 | ||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
| Adjusted EBITDA |
$ | $ | 169,994 | $ | 34,921 | $ | 7,135 | $ | 130,465 | $ | 39,973 | $ | 34,863 | |||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
| Adjusted EBITDA margin |
31.5 | % | 24.8 | % | 10.3 | % | 42.3 | % | 17.3 | % | 15.4 | % | ||||||||||||||||||||
| (1) | Represents non-cash share-based compensation expense in connection with profits interests and incentive share units. Share-based compensation expense for the Predecessor 2019 Period is fully attributable to the automatic acceleration of legacy profits interests and legacy incentive share units in connection with the Centerbridge Acquisition and is allocated to the marketing and advertising, technology and general and administrative line items in the income statement based on the department of the individual who received the compensation. |
111
Table of Contents
| (2) | Represents the fair value of the earnout liability due to the predecessor owners of the Company arising from the Centerbridge Acquisition. Prior to the consummation of this offering, we intend to update the disclosure as necessary for the resolution of the earnout liability. |
| (3) | Represents legal, accounting, consulting, and other costs related to the Centerbridge Acquisition. |
| (4) | Represents costs associated with the termination of employment. |
See “Prospectus Summary—Summary Historical and Pro Forma Condensed Consolidated Financial and Other Data” for information regarding our use of EBITDA, Adjusted EBITDA and Adjusted EBITDA margin, each a non-GAAP financial measure.
Key Components of Results of Operations
Net Revenues
We primarily generate revenues from commissions received from carriers for the multiple types of insurance products and plans sold by us on behalf of carriers. Commission revenues represent the consideration paid to us by carriers in the form of commissions, which primarily are calculated as a percentage of the premium amount collected by the carrier during the period the customer is enrolled in the insurance plan or product. The maximum allowable commission rates carriers are allowed to pay to independent agents and brokers, such as ourselves, for Medicare products are determined on an annual basis by CMS and CMS generally increases the commission rates allowed to be paid each year. The value we bring to carriers in the Medicare space typically enables us to negotiate for the maximum allowable commission rates, and we expect to continue to be able to do so. However, the commission rates that ultimately are paid to us are based on a variety of factors and the commission rates we receive could change. See “Risk Factors—Risks Related to Our Business—Carriers may reduce the commissions paid to us and change their underwriting practices in ways that reduce the number of, or impact the renewal or approval rates of, insurance policies sold through our platform, which could harm our business, operating results and financial condition.” We generally continue to receive commission payments from the relevant carrier until the plan or product is canceled. Our contracts with carriers contain a single-performance obligation satisfied by carrier acceptance of a submission, at which point we recognize the full transaction price of the policy sold as revenue in that period.
We also generate revenues from providing marketing, enrollment and other services to third parties, primarily carriers. Typically, we are paid enrollment fees and hourly fees to staff for services performed for specific carriers and other partners, which we recognize as the services are performed under a contractual arrangement. In addition, these agreements generally include performance-based fees based on specified performance criteria, such as volume, efficiency and certain other service-level agreements. We also generate revenue from referring customers to carriers and other third-party partners. Additionally, we provide technology services through our Marketplace technology to carriers.
Operating Expenses
Cost of Revenue
Cost of revenue represents payments related to policies sold to customers who were enrolled by partners with whom we have commissions revenue-sharing arrangements. In order to enter into a revenue-sharing arrangement, partners must be licensed to sell health insurance plans in the state where the policy is sold. Costs related to revenue-sharing arrangements are expensed as the related revenue is recognized.
Marketing and Advertising
Marketing expense consists primarily of expenses associated with our direct, online advertising, and marketing partner channels, in addition to compensation (including share-based compensation expense) and other expenses related to marketing personnel who manage campaigns and optimize consumer activity. Marketing costs are
112
Table of Contents
expensed as incurred. Our direct channel expenses primarily consist of costs for e-mail marketing and direct mail marketing. Online advertising expenses primarily consist of paid keyword search advertising on search engines. Marketing partner channel expenses primarily consist of fees paid to marketing partners and affiliates. Advertising expenses consist of costs incurred to acquire consumers through online, television, and direct mail advertisements. We also have arrangements with certain carriers that allow us to increase marketing efforts, including through direct mail, television, and online advertising for various insurance products that are being offered by these carriers. We record the amounts received as a reduction of the marketing costs incurred. Generally, our marketing and advertising expenses increase during annual enrollment period and open enrollment so that we may generate more leads during these high-volume periods.
Customer Care and Enrollment
Customer care and enrollment expense consists primarily of expenses associated with compensation (including share-based compensation expense) and benefits costs for agents and other personnel who assist consumers during the policy application process, along with management and support personnel.
Technology
Technology expense consists primarily of compensation (including share-based compensation expense) and benefits costs for personnel associated with developing and enhancing our technology platform, data analytics and business intelligence, as well as maintaining our online presence and integrations with carrier and federal marketplaces. Technology expense also includes costs for contracted services and supplies, and amortization expense to capitalized software. We plan to increase our investment in this area as we continue to enhance our platform.
General and Administrative
General and administrative expense consists of compensation (including share-based compensation expense) and benefits costs for staff working with our executive, finance, legal, human resources, facilities and internal operations departments. These expenses also include facilities costs and fees paid for outside professional services, including audit, tax, legal and governmental affairs.
Change in Fair Value of Contingent Consideration Liability
Change in fair value of contingent consideration liability relates to the earnout liability incurred in connection with the Centerbridge Acquisition, in which we agreed to pay additional consideration in additional common and senior preferred units if Adjusted EBITDA (as defined in the agreement entered into in connection with the Centerbridge Acquisition) exceeds certain thresholds for the year ended December 31, 2019 and 2020. See Note 4 of each of the audited consolidated financial statements and interim condensed consolidated financial statements included elsewhere in this prospectus for fair value estimates recorded at March 31, 2020 and December 31, 2019.
Amortization of Intangible Assets
Amortization of intangible assets represents amortization of developed technology and customer relationships over the estimated useful lives of such assets which was reflected in the purchase price allocation attributable to the Centerbridge Acquisition.
Transaction Costs
Transaction costs consist of legal, accounting, consulting and other costs incurred in connection with the Centerbridge Acquisition.
113
Table of Contents
Interest Expense
Interest expense consists primarily of interest expense on our outstanding debt.
Basis of Presentation
The Centerbridge Acquisition took place on September 13, 2019. Accordingly, the accompanying consolidated financial statements presented elsewhere in this prospectus for the year ended December 31, 2018 reflect the period prior to the Centerbridge Acquisition. The consolidated financial statements for December 31, 2019 are presented separately for the Predecessor period from January 1, 2019 through September 12, 2019 (the “Predecessor 2019 Period”) and the Successor period from September 13, 2019 through December 31, 2019 (the “Successor 2019 Period”). The financial position and results of the Successor reflect the application of purchase accounting in accordance with ASC 805.
The financial information presented for the unaudited pro forma condensed consolidated financial information included elsewhere in this prospectus for the year ended December 31, 2019 (the “Pro Forma Fiscal Year 2019”) gives effect to the Centerbridge Acquisition, but does not give effect to the adjustments for the Transactions, including adjustments related to this offering and the other adjustments described in the section titled “Unaudited Pro Forma Condensed Consolidated Financial Information.” Such adjustments will be included in a subsequent filing based on the actual initial public offering price, the number of shares sold in this offering, and other terms of this offering determined at pricing. The unaudited pro forma consolidated statement of operations for the Pro Forma Fiscal Year 2019 presented elsewhere in this prospectus and the pro forma adjustments are not audited and have been derived from our audited consolidated financial statements included elsewhere in this prospectus.
We believe that the discussion of the results of operations comparing the Predecessor 2019 Period, the Successor 2019 Period and the consolidated financial statements of the Predecessor for the year ended December 31, 2018 is not meaningful on a standalone basis as the Centerbridge Acquisition was accounted for as a business combination in accordance with ASC 805, and the resulting new basis of accounting is reflected in our consolidated financial statements for all periods beginning on or after September 13, 2019, and therefore, the two periods are not comparable. In particular, pro forma adjustments for general and administrative expense, amortization of intangible assets, transaction costs and interest expense significantly impacted the comparability of our results, among other adjustments. We believe that the comparison of the Pro Forma Fiscal Year 2019 to the year ended December 31, 2018 provides a more meaningful discussion of our 2019 and 2018 results of operations for potential investors.
114
Table of Contents
Results of Operations
Three Months Ended March 31, 2020 Compared to Three Months Ended March 31, 2019
The following table sets forth the components of our results of operations for the periods indicated:
| Three Months Ended March 31, 2020 (Successor) |
Three Months Ended March 31, 2019 (Predecessor) |
|||||||||||||||||||||||
| (in thousands) | Dollars | % of Net Revenues |
Dollars | % of Net Revenues |
$ Change | % Change | ||||||||||||||||||
| Net revenues: |
||||||||||||||||||||||||
| Commission |
$ | 112,510 | 79.8 | % | $ | 51,215 | 74.1 | % | $ | 61,295 | 119.7 | % | ||||||||||||
| Other |
28,500 | 20.2 | % | 17,874 | 25.9 | % | 10,625 | 59.4 | % | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Net revenues |
141,010 | 100.0 | % | 69,089 | 100.0 | % | 71,921 | 104.1 | % | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Operating expenses: |
||||||||||||||||||||||||
| Cost of revenue |
42,134 | 29.9 | % | 27,552 | 39.9 | % | 14,582 | 52.9 | % | |||||||||||||||
| Marketing and advertising |
26,073 | 18.5 | % | 11,411 | 16.5 | % | 14,662 | 128.5 | % | |||||||||||||||
| Customer care and enrollment |
23,978 | 17.0 | % | 13,939 | 20.2 | % | 10,039 | 72.0 | % | |||||||||||||||
| Technology |
4,593 | 3.3 | % | 4,155 | 6.0 | % | 437 | 10.5 | % | |||||||||||||||
| General and administrative |
10,491 | 7.4 | % | 6,990 | 10.1 | % | 3,501 | 50.0 | % | |||||||||||||||
| Change in fair value of contingent consideration liability |
4,400 | 3.1 | % | — | — | 4,400 | NM | |||||||||||||||||
| Amortization of intangible assets |
23,514 | 16.7 | % | — | — | 23,514 | NM | |||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Total operating expenses |
135,183 | 95.9 | % | 64,047 | 92.7 | % | 71,315 | 111.1 | % | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Income from operations |
5,827 | 4.1 | % | 5,042 | 7.3 | % | 785 | 15.6 | % | |||||||||||||||
| Interest expense |
6,756 | 4.8 | % | 28 | 0.0 | % | 6,729 | NM | ||||||||||||||||
| Other expense |
10 | 0.0 | % | 10 | 0.0 | % | 0 | (4.4 | )% | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Income (loss) before income tax expense (benefit) |
(939 | ) | (0.7 | )% | 5,004 | 7.2 | % | (5,943 | ) | (118.8 | )% | |||||||||||||
| Income tax expense (benefit) |
(2 | ) | 0.0 | % | 2 | 0.0 | % | (4 | ) | (173.0 | )% | |||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Net income (loss) |
$ | (937 | ) | (0.7 | )% | $ | 5,002 | 7.2 | % | $ | (5,939 | ) | (118.7 | )% | ||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| * | NM indicates that the percentage is not meaningful. |
Net Revenues
Commission Revenues
Commission revenues were $112.5 million for the three months ended March 31, 2020 compared to $51.2 million for the three months ended March 31, 2019, an increase of 119.7%, which was primarily attributable to increases in commission revenues from (i) the Medicare—Internal segment of $74.4 million driven by a 291.6% increase in Medicare commissionable Approved Submissions due to the implementation of new marketing strategies to generate a greater number of prospects, an improvement in the efficiency of our agents driven by improvements in our technology, and the hiring of additional agents and (ii) the Medicare—External segment of $8.6 million driven by a 68.9% increase in Medicare commissionable Approved Submissions due to our ability to recruit and onboard additional external agencies to enroll consumers in Medicare plans using our technology and platform.
Other Revenues
Other revenues were $28.5 million for the three months ended March 31, 2020 compared to $17.9 million for the three months ended March 31, 2019, an increase of 59.4%. The increase was primarily attributable to an increase in Medicare—Internal other revenues of $20.0 million due to the expansion of carrier-specific sponsorships and
115
Table of Contents
programs. The increase was partially offset by declines in the IFP and Other segments and the Medicare—External segment other revenues of $6.6 million in aggregate due to a decrease in consumer lead sales to external third parties as we strategically shifted to generating consumer leads in the internal channel.
See further analysis in “—Segment Information” below.
Operating Expenses
Cost of Revenue
Cost of revenue was $42.1 million for the three months ended March 31, 2020 compared to $27.5 million for the three months ended March 31, 2019, an increase of 52.9%. The increase was primarily due to a 68.9% increase in commissionable Approved Submissions in the Medicare—External segment, which increased the amount of expense we recognized pursuant to our revenue-sharing agreements with external agencies and other partners.
Marketing and Advertising
Marketing and advertising expense was $26.0 million for the three months ended March 31, 2020 compared to $11.4 million for the three months ended March 31, 2019, an increase of 128.5%. The increase was primarily due to an increase in our advertising costs for the Medicare—Internal segment to generate more qualified prospects, which contributed to a 291.6% increase in commissionable Approved Submissions in the Medicare—Internal segment.
Customer Care and Enrollment
Customer care and enrollment expense was $24.0 million for the three months ended March 31, 2020 compared to $13.9 million for the three months ended March 31, 2019, an increase of 72.0%. The increase was primarily attributable to the hiring of additional agents in the Medicare—Internal segment in order to drive the conversion of a greater number of qualified prospects into commissionable Approved Submissions. As of March 31, 2020, we had 781 full time equivalent agents compared to 529 full time equivalent agents as of March 31, 2019.
Technology
Technology expense was $4.6 million for the three months ended March 31, 2020 compared to $4.2 million for the three months ended March 31, 2019, an increase of 10.5%. The increase was primarily due to the hiring of additional employees in our technology and data science teams, which drove improvements to our LeadScore and call-routing technologies and expansion of our business intelligence and analytics staffing in order to support the growth of the Medicare-Internal segment.
General and Administrative
General and administrative expense was $10.5 million for the three months ended March 31, 2020 compared to $7.0 million for the three months ended March 31, 2019, an increase of 50.0%. The increase was primarily due to investments in corporate infrastructure, such as legal, human resources, and finance, to support the growth of the business.
Amortization of Intangible Assets
Amortization of intangible assets expense was $23.5 million for the three months ended March 31, 2020 compared to none for the three months ended March 31, 2019. Amortization expense for the three months ended March 31, 2020 relates to the amortization of definite-lived intangible assets that was reflected in the purchase price allocation at the date of the Centerbridge Acquisition.
116
Table of Contents
Interest Expense
Interest expense was $6.8 million for the three months ended March 31, 2020 compared to $28 thousand for the three months ended March 31, 2019. The increase was due to the incurrence of additional debt under the Credit Facilities in connection with the Centerbridge Acquisition.
Period from Successor 2019 Period and Predecessor 2019 Period Compared to Fiscal Year Ended December 31, 2018 (Predecessor)
The results of operations discussion below compares the Successor 2019 Period, the Predecessor 2019 Period and the year ended December 31, 2018. Due to the application of purchasing accounting at September 12, 2019, we believe that the comparison of the Pro Forma Fiscal Year 2019 to the year ended December 31, 2018, presented below, provides the most meaningful supplemental discussion of our 2019 and 2018 results of operations for potential investors. Due to, in part, the seasonality of our business, the results of operations for the Successor 2019 Period compared to the Predecessor 2019 Period are not comparable. See “—Seasonality.”
The following table sets forth the components of our results of operations for the periods indicated:
| Successor 2019 Period | Predecessor 2019 Period | Year Ended December 31, 2018 (Predecessor) |
||||||||||||||||||||||||||||||
| (in thousands) | Dollars | % of Net Revenues |
Dollars | % of Net Revenues |
Dollars | % of Net Revenues | ||||||||||||||||||||||||||
| Net revenues: |
||||||||||||||||||||||||||||||||
| Commission |
$ | 243,347 | 78.9 | % | $ | 175,834 | 76.1 | % | $ | 144,378 | 63.8 | % | ||||||||||||||||||||
| Other |
65,144 | 21.1 | % | 55,176 | 23.9 | % | 81,827 | 36.2 | % | |||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| ||||||||||||||||||
| Net revenues |
308,491 | 100.0 | % | 231,010 | 100.0 | % | 226,205 | 100.0 | % | |||||||||||||||||||||||
| Operating expenses: |
||||||||||||||||||||||||||||||||
| Cost of revenue |
90,384 | 29.3 | % | 79,169 | 34.3 | % | 79,582 | 35.2 | % | |||||||||||||||||||||||
| Marketing and advertising |
24,811 | 8.0 | % | 37,769 | 16.3 | % | 28,129 | 12.4 | % | |||||||||||||||||||||||
| Customer care and enrollment |
44,356 | 14.4 | % | 49,149 | 21.3 | % | 46,076 | 20.4 | % | |||||||||||||||||||||||
| Technology |
6,006 | 1.9 | % | 40,312 | 17.5 | % | 16,197 | 7.2 | % | |||||||||||||||||||||||
| General and administrative |
13,674 | 4.4 | % | 79,219 | 34.3 | % | 27,458 | 12.1 | % | |||||||||||||||||||||||
| Change in fair value of contingent consideration liability |
70,700 | 22.9 | % | — | — | — | — | |||||||||||||||||||||||||
| Amortization of intangible assets |
28,217 | 9.1 | % | — | — | — | — | |||||||||||||||||||||||||
| Transaction costs |
6,245 | 2.0 | % | 2,267 | 0.9 | % | — | — | ||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| ||||||||||||||||||
| Total operating expenses |
284,393 | 92.2 | % | 287,885 | 124.6 | % | 197,442 | 87.3 | % | |||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| ||||||||||||||||||
| Income (loss) from operations |
24,098 | 7.8 | % | (56,875 | ) | (24.6 | )% | 28,763 | 12.7 | % | ||||||||||||||||||||||
| Interest expense |
8,076 | 2.6 | % | 140 | 0.1 | % | 224 | 0.1 | % | |||||||||||||||||||||||
| Other income (expense) |
17 | — | (114 | ) | — | (379 | ) | (0.2 | )% | |||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| ||||||||||||||||||
| Income (loss) before income taxes |
16,039 | 5.2 | % | (57,129 | ) | (24.7 | )% | 28,160 | 12.4 | % | ||||||||||||||||||||||
| Income tax expense (benefit) |
44 | — | (66 | ) | — | 46 | — | |||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| ||||||||||||||||||
| Net income (loss) |
$ | 15,995 | 5.2 | % | $ | (57,063 | ) | (24.7 | )% | $ | 28,114 | 12.4 | % | |||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| ||||||||||||||||||
Net Revenues
Commission Revenues
Commission revenues were $243.3 million for the Successor 2019 Period and $175.8 million for the Predecessor 2019 Period compared to $144.4 million for the year ended December 31, 2018 which was primarily attributable to increases in commission revenue from (i) the Medicare—Internal segment driven by a 359.9% increase in
117
Table of Contents
Medicare commissionable Approved Submissions due the hiring of additional agents (in 2019, at our peak, we had approximately 1,700 full time equivalent agents during the annual enrollment period, compared to approximately 1,200 full time equivalent agents at our peak in 2018 during the annual enrollment period), the increased utilization and efficiency of our agents and the implementation of new marketing strategies to generate a greater number of qualified prospects. and (ii) the Medicare—External segment driven by a 108.3% increase in commissionable Approved Submissions due to our ability to recruit and onboard additional external agencies to enroll consumers in Medicare plans using our technology and platform.
Other Revenues
Other revenues were $65.1 million for the Successor 2019 Period and $55.2 million for the Predecessor 2019 Period compared to $81.8 million for the year ended December 31, 2018. The increase was primarily attributable to an increase in Medicare—Internal other revenues of $62.3 million due to the expansion of carrier-specific sponsorships and programs. The increase was partially offset by declines in the IFP and Other segments and the Medicare—External segment of $23.4 million in aggregate due to a decrease in consumer lead sales to external third parties as we strategically shifted to generating consumer leads in the internal channel.
See further analysis in “—Segment Information” below.
Operating Expenses
Cost of Revenue
Cost of revenue was $90.4 million for the Successor 2019 Period and $79.2 million for the Predecessor 2019 Period compared to $79.6 million for the year ended December 31, 2018. The increase was primarily due to a 108.3% increase in commissionable Approved Submissions in the Medicare—External segment, which increased the amount of expense we recognized pursuant to our revenue-sharing agreements with external agencies and other partners.
Marketing and Advertising
Marketing and advertising expense was $24.8 million for the Successor 2019 Period and $37.8 million for the Predecessor 2019 Period compared to $28.1 million for the year ended December 31, 2018. The increase was primarily due to an increase in our advertising costs, particularly in the Predecessor 2019 Period, for the Medicare—Internal segment to generate more qualified prospects, which contributed to a 359.9% increase in Medicare—Internal Approved Submissions from 2019 compared to 2018. Additionally, marketing and advertising expense also increased as compared to 2018 due to share-based compensation expense of $1.6 million in the Predecessor 2019 Period in connection with the accelerated vesting of certain legacy profits interests and legacy incentive share units granted prior to the Centerbridge Acquisition.
Customer Care and Enrollment
Customer care and enrollment expense was $44.4 million for the Successor 2019 Period and $49.1 million for the Predecessor 2019 Period compared to $46.1 million for the year ended December 31, 2018. The increase was primarily attributable to the hiring of additional agents in the Medicare—Internal channel in order to drive the conversion of a greater number of qualified prospects into Approved Submissions. In 2019, at our peak, we had roughly 1,700 full time equivalent agents during the Medicare annual enrollment period, compared to roughly 1,200 full time equivalent agents at our peak in 2018 during the Medicare annual enrollment period
Technology
Technology expense was $6.0 million for the Successor 2019 Period and $40.3 million for the Predecessor 2019 Period compared to $16.2 million for the year ended December 31, 2018. The increase was primarily due to share-based compensation expense of $27.1 million in the Predecessor 2019 Period in connection with the
118
Table of Contents
accelerated vesting of certain legacy profits interests and legacy incentive share units granted prior to the Centerbridge Acquisition. Additionally, the increase was also attributable to the hiring of additional employees in our technology and data science teams totaling $3.1 million which drove improvements to our LeadScore and call-routing technologies and expansion of our business intelligence and analytics staffing in order to support the growth of the Internal Medicare segments.
General and Administrative
General and administrative expense was $13.7 million for the Successor 2019 Period and $79.2 million for the Predecessor 2019 Period compared to $27.5 million for the year ended December 31, 2018. The increase was primarily due to share-based compensation expense of $58.3 million in the Predecessor 2019 Period in connection with the accelerated vesting of certain legacy profits interests and legacy incentive share units granted prior to the Centerbridge Acquisition. Additionally, the increase was also attributable to investments of $6.1 million in corporate infrastructure, such as legal, human resources, and finance, to support the growth of the business.
Change in Fair Value of Contingent Consideration Liability
Change in fair value of contingent consideration liability was $70.7 million for the Successor 2019 Period, which we incurred in connection with the Centerbridge Acquisition. We had no earnout liability in the prior periods.
Amortization of Intangible Assets
Amortization of intangible assets expense was $28.2 million for the Successor 2019 Period. We had no amortization of intangible assets in the prior periods. Amortization expense for the Successor 2019 Period relates to the amortization of definite-lived intangible assets which was reflected in the purchase price allocation at the date of the Centerbridge Acquisition.
Transaction Costs
Transaction costs were $6.2 million for the Successor 2019 Period and $2.3 million for the Predecessor 2019 Period compared to none for the year ended December 31, 2018. Transaction costs in 2019 were due to the Centerbridge Acquisition, for which we incurred legal, accounting, consulting and other costs.
Interest Expense
Interest expense was $8.1 million for the Successor 2019 Period and $140.0 thousand for the Predecessor 2019 Period compared to $224.0 thousand for the year ended December 31, 2018. The increase from 2018 to 2019 was due to the incurrence of additional debt under the Credit Facilities in connection with the Centerbridge Acquisition.
119
Table of Contents
Unaudited Pro Forma Fiscal Year 2019 Compared to Fiscal Year Ended December 31, 2018 (Predecessor)
The following table sets forth the operating results and the related percentage of net revenues for the periods indicated:
| Pro Forma Fiscal Year 2019(1) |
Year Ended December 31, 2018 (Predecessor) |
|||||||||||||||||||||||
| (in thousands) | Dollars | % of Net Revenues |
Dollars | % of Net Revenues |
$ Change | % Change | ||||||||||||||||||
| Net revenues: |
||||||||||||||||||||||||
| Commission |
$ | 419,181 | 77.7 | % | $ | 144,378 | 63.8 | % | $ | 274,803 | 190.3 | % | ||||||||||||
| Other |
120,320 | 22.3 | % | 81,827 | 36.2 | % | 38,493 | 47.0 | % | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| ||||||||||
| Net revenues |
539,501 | 100.0 | % | 226,205 | 100.0 | % | 313,296 | 138.5 | % | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| ||||||||||
| Operating expenses: |
||||||||||||||||||||||||
| Cost of revenue |
169,553 | 31.4 | % | 79,582 | 35.2 | % | 89,971 | 113.1 | % | |||||||||||||||
| Marketing and advertising |
61,071 | 11.3 | % | 28,129 | 12.4 | % | 32,942 | 117.1 | % | |||||||||||||||
| Customer care and enrollment |
93,567 | 17.3 | % | 46,076 | 20.4 | % | 47,491 | 103.1 | % | |||||||||||||||
| Technology |
19,470 | 3.6 | % | 16,197 | 7.2 | % | 3,273 | 20.2 | % | |||||||||||||||
| General and administrative |
33,336 | 6.2 | % | 27,458 | 12.1 | % | 5,878 | 21.4 | % | |||||||||||||||
| Change in fair value of contingent consideration liability |
70,700 | 13.1 | % | — | — | 70,700 | — | |||||||||||||||||
| Amortization of intangible assets |
94,057 | 17.4 | % | — | — | 94,057 | — | |||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| ||||||||||
| Total operating expenses |
541,755 | 100.4 | % | 197,442 | 87.3 | % | 344,313 | 174.4 | % | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| ||||||||||
| Income (loss) from operations |
(2,254 | ) | (0.4 | %) | 28,763 | 12.7 | % | (31,017 | ) | (107.8 | )% | |||||||||||||
| Interest expense |
27,172 | 5.0 | % | 224 | 0.1 | % | 26,948 | 12,030.5 | % | |||||||||||||||
| Other income (loss) |
(97 | ) | — | (379 | ) | (0.2 | )% | 282 | (74.7 | )% | ||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| ||||||||||
| Income (loss) before income tax expense (benefit) |
(29,523 | ) | (5.5 | )% | 28,160 | 12.4 | % | (57,683 | ) | (204.8 | )% | |||||||||||||
| Income tax expense (benefit) |
(22 | ) | — | 46 | — | (68 | ) | (147.8 | )% | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| ||||||||||
| Net income (loss) |
$ | (29,501 | ) | (5.5 | )% | $ | 28,114 | 12.4 | % | $ | (57,615 | ) | (204.9 | )% | ||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| ||||||||||
| (1) | For a discussion of the Successor 2019 Period and the Predecessor 2019 Period compared to the year ended December 31, 2019, see “—Period from Successor 2019 Period and Predecessor 2019 Period Compared to Fiscal Year Ended December 31, 2018 (Predecessor).” |
Net Revenues
Commission Revenues
Commission revenues were $419.2 million for the Pro Forma Fiscal Year 2019 compared to $144.4 million for the year ended December 31, 2018, an increase of 190.3%, which was primarily attributable to increases in commission revenue from (i) the Medicare—Internal segment of $201.5 million driven by a 359.9% increase in Medicare commissionable Approved Submissions due the hiring of additional agents (in 2019, at our peak, we had approximately 1,700 full time equivalent agents during the annual enrollment period, compared to approximately 1,200 full time equivalent agents at our peak in 2018 during the annual enrollment period), the increased utilization and efficiency of our agents and the implementation of new marketing strategies to generate a greater number of qualified prospects and (ii) the Medicare—External segment of $57.5 million driven by a 108.3% increase in commissionable Approved Submissions in the Medicare—External segment due to our ability to recruit and onboard additional external agencies to enroll consumers in Medicare plans using our technology and platform.
120
Table of Contents
Other Revenues
Other revenues were $120.3 million for the Pro Forma Fiscal Year 2019 compared to $81.8 million for the year ended December 31, 2018, an increase of 47.0%. The increase was primarily attributable to an increase in Medicare—Internal other revenues of $62.3 million due to the expansion of carrier-specific sponsorships and programs. The increase was partially offset by declines in the IFP and Other segments and the Medicare—External segment of $23.4 million in aggregate due to a decrease in consumer lead sales to external third parties as we strategically shifted to generating consumer leads in our internal channels.
See further analysis in “—Segment Information” below.
Operating Expenses
Cost of Revenue
Cost of revenue was $169.6 million for the Pro Forma Fiscal Year 2019 compared to $79.6 million for the year ended December 31, 2018, an increase of 113.1%. The increase was primarily due to a 108.3% increase in commissionable Approved Submissions in the Medicare—External segment, which increased the amount of expense we recognized pursuant to our revenue-sharing agreements with external agencies and other partners.
Marketing and Advertising
Marketing and advertising expense was $61.1 million for the Pro Forma Fiscal Year 2019 compared to $28.1 million for the year ended December 31, 2018, an increase of 117.1%. The increase was primarily due to an increase in our advertising costs for the Medicare—Internal segment to generate more qualified prospects, which contributed to a 359.9% increase in Medicare—Internal Approved Submissions from 2019 compared to 2018.
Customer Care and Enrollment
Customer care and enrollment expense was $93.6 million for the Pro Forma Fiscal Year 2019 compared to $46.1 million for the year ended December 31, 2018, an increase of 103.1%. The increase was primarily attributable to the hiring of additional agents in the Medicare—Internal channel in order to drive the conversion of a greater number of qualified prospects into Approved Submissions. In 2019, at our peak, we had roughly 1,700 full time equivalent agents during the Medicare annual enrollment period, compared to roughly 1,200 full time equivalent agents at our peak in 2018 during the Medicare annual enrollment period.
Technology
Technology expense was $19.5 million for the Pro Forma Fiscal Year 2019 compared to $16.2 million for the year ended December 31, 2018, an increase of 20.2%. The increase was primarily due to our hiring of additional employees in our technology and data science teams totaling $3.1 million which drove improvements to our LeadScore and call-routing technologies and expansion of our business intelligence and analytics staffing in order to support the growth of the Internal Medicare segments.
General and Administrative
General and administrative expense was $33.3 million for the Pro Forma Fiscal Year 2019 compared to $27.5 million for the year ended December 31, 2018, an increase of 21.4%. The increase was primarily due to investments in corporate infrastructure, such as legal, human resources, and finance, to support the growth of the business.
121
Table of Contents
Change in Fair Value of Contingent Consideration Liability
Change in fair value of contingent consideration liability was $70.7 million for the Pro Forma Fiscal Year 2019, which we incurred in connection with the Centerbridge Acquisition. We had no earnout liability in the prior period.
Amortization of Intangible Assets
Amortization of intangible assets expense was $94.1 million for the Pro Forma Fiscal Year 2019 compared to none for the year ended December 31, 2018. Amortization expense for Pro Forma Fiscal Year 2019 relates to the amortization of certain definite-lived intangible assets that was reflected in the purchase price allocation at the date of the Centerbridge Acquisition.
Interest Expense
Interest expense was $27.2 million for the Pro Forma Fiscal Year 2019 compared to $0.2 million for the year ended December 31, 2018. The increase from 2018 to 2019 was due to the incurrence of additional debt under the Credit Facilities in connection with the Centerbridge Acquisition.
Segment Information
Our reportable segments have been determined in accordance with Accounting Standards Codification, or ASC, 280, Segment Reporting. Currently, we have four reportable segments: Medicare—Internal, Medicare—External, IFP and Other—Internal, and IFP and Other—External. In addition, we separately report other expenses (classified as “Corporate“ in the following table), the primary components of which are corporate overhead expenses and shared service expenses that have not been allocated to the reportable segments, as they are not the responsibility of segment operating management.
The segment measurements provided to and evaluated by the chief operating decision maker are described in the notes to the audited consolidated financial statements and the interim condensed consolidated financial statements included elsewhere in this prospectus. These results should be considered in addition to, not as a substitute for, results reported in accordance with GAAP.
122
Table of Contents
Three Months Ended March 31, 2020 Compared to Three Months Ended March 31, 2019
| Three Months Ended March 31, 2020 (Successor) |
Three Months Ended March 31, 2019 (Predecessor) |
|||||||||||||||||||||||
| (in thousands) | Dollars | % of Total Revenues |
Dollars | % of Total Revenues |
$ Change | % Change | ||||||||||||||||||
| Net revenues: |
||||||||||||||||||||||||
| Medicare—Internal |
$ | 95,287 | 67.6 | % | $ | 20,911 | 30.3 | % | $ | 74,376 | 355.7 | % | ||||||||||||
| Medicare—External |
28,945 | 20.5 | % | 20,335 | 29.4 | % | 8,610 | 42.3 | % | |||||||||||||||
| IFP and Other—Internal |
8,632 | 6.1 | % | 14,440 | 20.9 | % | (5,808 | ) | (40.2 | )% | ||||||||||||||
| IFP and Other—External |
8,146 | 5.8 | % | 13,403 | 19.4 | % | (5,257 | ) | (39.2 | )% | ||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Total revenues |
141,010 | 100.0 | % | 69,089 | 100.0 | % | 71,921 | 104.1 | % | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Segment profit: |
||||||||||||||||||||||||
| Medicare—Internal segment profit |
41,735 | 29.6 | % | 4,864 | 7.0 | % | 36,871 | 758.0 | % | |||||||||||||||
| Medicare—External segment profit |
(322 | ) | (0.2 | )% | 3,380 | 4.9 | % | (3,702 | ) | (109.5 | )% | |||||||||||||
| IFP and Other—Internal segment profit |
481 | 0.3 | % | 881 | 1.3 | % | (400 | ) | (45.4 | )% | ||||||||||||||
| IFP and Other—External segment profit |
512 | 0.4 | % | 1,263 | 1.8 | % | (751 | ) | (59.5 | )% | ||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Total segment profit |
42,406 | 30.1 | % | 10,388 | 15.0 | % | 32,018 | 308.2 | % | |||||||||||||||
| Corporate |
8,665 | 6.1 | % | 5,346 | 7.7 | % | 3,319 | 62.1 | % | |||||||||||||||
| Change in fair value of contingent consideration liability |
4,400 | 3.1 | % | — | — | 4,400 | NM | |||||||||||||||||
| Amortization of intangible assets |
23,514 | 16.7 | % | — | — | 23,514 | NM | |||||||||||||||||
| Interest expense |
6,756 | 4.8 | % | 28 | 0.0 | % | 6,729 | NM | ||||||||||||||||
| Other expense |
10 | 0.0 | % | 10 | 0.0 | % | 1 | 0.0 | % | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Income (loss) before income taxes |
$ | (939 | ) | (0.7 | )% | $ | 5,004 | 7.2 | % | $ | (5,943 | ) | (118.8 | )% | ||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| * | NM indicates that the percentage is not meaningful. |
Net Revenues
Net revenues for the Medicare—Internal segment were $95.3 million for the three months ended March 31, 2020 compared to $20.9 million for the three months ended March 31, 2019, which was primarily driven by the hiring of additional agents and the increased utilization and efficiency of our agents, which contributed to a 291.6% increase in commissionable Approved Submissions. As of March 31, 2020, we had 781 full time equivalent agents compared to 529 full time equivalent agents as of March 31, 2019. In addition to increasing our agent count, we were able to increase the efficiency of our agents due to improvements in our technology. We were also able to utilize more agents on a year-round basis instead of during enrollment periods due to the addition of SNPs into our marketplace which are able to be sold at any time of year. Net revenues also increased in this segment due to the implementation of new marketing strategies to generate a greater number of qualified prospects and due to an increase in non-commission revenues. Net revenues for the Medicare—External segment were $28.9 million for the three months ended March 31, 2020 compared to $20.3 million for the three months ended March 31, 2019, which was primarily driven by a 68.9% increase in Medicare commissionable Approved Submissions due to our ability to recruit and onboard additional external agencies to enroll consumers in Medicare plans using our technology and platform.
Net revenues for the IFP and Other—Internal segment were $8.6 million for the three months ended March 31, 2020 compared to $14.4 million for the three months ended March 31, 2019. Net revenues for the IFP and Other—External segment were $8.1 million for the three months ended March 31, 2020 compared to $13.4
123
Table of Contents
million for the three months ended March 31, 2019. For each of the IFP and Other segments, the decreases were primarily driven by a change in product mix sold within the IFP and Other segments.
Segment Profit
Segment profit is calculated as total revenue for the applicable segment less direct and allocated cost of revenue, marketing and advertising, customer care and enrollment, technology and general and administrative operating expenses, excluding change in fair value of contingent consideration liability, amortization of intangibles assets, share-based compensation, transaction costs, interest expense, and other income (loss).
Segment profit for the Medicare—Internal segment was $41.7 million for the three months ended March 31, 2020 compared to $4.9 million for the three months ended March 31, 2019. The increase was driven by the increase of Medicare commissionable Approved Submissions and an increase in our LTV/CAC ratio to 2.7x for the three months ended March 31, 2020 compared to 1.7x for the three months ended March 31, 2019. The increase of Medicare commissionable Approved Submissions was primarily attributable to (i) improvements in our LeadScore and call-routing technologies allowing our agents to successfully convert more consumer leads into customers and (ii) an expansion of the diversity and breadth of our omni-channel marketing efforts, which enabled the acquisition of higher quality prospects. The increase in LTV/CAC was primarily attributable to improved marketing efficiencies driven by our rapid test-and-learn approach across our marketing channels.
Segment loss for the Medicare—External segment was $0.3 million for the three months ended March 31, 2020 compared to segment profit of $3.4 million for the three months ended March 31, 2019. The decrease was primarily driven by a 68.9% increase in commissionable Approved Submissions in the Medicare—External segment, which increased the amount of expense we recognized pursuant to our revenue-sharing agreements with external agencies and other partners.
Segment profit for the IFP and Other—Internal segment was $0.5 million for the three months ended March 31, 2020 compared to $0.8 million for the three months ended March 31, 2019. The decrease was primarily driven by a change in product mix sold by agents for IFP and Other plans.
Segment profit for the IFP and Other—External segment was $0.5 million for the three months ended March 31, 2020 compared to $1.3 million for the three months ended March 31, 2019. The decrease was driven by a change in product mix sold by external agencies.
124
Table of Contents
Unaudited Pro Forma Fiscal Year 2019 Compared to Fiscal Year Ended December 31, 2018 (Predecessor)
| Successor 2019 Period | Predecessor 2019 Period |
Pro Forma Fiscal Year 2019 |
Year Ended December 31, 2018 (Predecessor) |
|||||||||||||||||||||||||||||||||||||
| (in thousands) | Dollars | % of Total Revenues |
Dollars | % of Total Revenues |
Dollars | % of Total Revenues |
Dollars | % of Total Revenues | ||||||||||||||||||||||||||||||||
| Net revenues: |
||||||||||||||||||||||||||||||||||||||||
| Medicare—Internal |
$ | 215,322 | 69.8 | % | $ | 102,196 | 44.2 | % | $ | 317,518 | 58.9 | % | $ | 53,365 | 23.6 | % | ||||||||||||||||||||||||
| Medicare—External |
59,152 | 19.2 | % | 55,981 | 24.2 | % | 115,132 | 21.3 | % | 58,834 | 26.0 | % | ||||||||||||||||||||||||||||
| IFP and Other—Internal |
20,850 | 6.8 | % | 37,909 | 16.4 | % | 58,759 | 10.9 | % | 63,009 | 27.9 | % | ||||||||||||||||||||||||||||
| IFP and Other—External |
13,167 | 4.3 | % | 34,924 | 15.1 | % | 48,093 | 8.9 | % | 50,997 | 22.5 | % | ||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||||||||||||||||||||
| Total revenues |
308,491 | 100.0 | % | 231,010 | 100.0 | % | 539,502 | 100.0 | % | 226,205 | 100.0 | % | ||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||||||||||||||||||||
| Segment profit: |
||||||||||||||||||||||||||||||||||||||||
| Medicare—Internal segment profit |
126,210 | 40.9 | % | 40,024 | 17.3 | % | 166,234 | 30.8 | % | 24,183 | 10.7 | % | ||||||||||||||||||||||||||||
| Medicare—External segment profit |
10,584 | 3.4 | % | 4,893 | 2.1 | % | 15,476 | 2.9 | % | 9,034 | 4.0 | % | ||||||||||||||||||||||||||||
| IFP and Other—Internal segment profit |
1,650 | 0.5 | % | 2,195 | 1.0 | % | 3,845 | 0.7 | % | 9,707 | 4.3 | % | ||||||||||||||||||||||||||||
| IFP and Other—External segment profit |
584 | 0.2 | % | 1,748 | 0.8 | % | 2,332 | 0.4 | % | 2,848 | 1.3 | % | ||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||||||||||||||||||||
| Total segment profit |
139,027 | 45.1 | % | 48,860 | 21.2 | % | 187,887 | 34.8 | % | 45,773 | 20.2 | % | ||||||||||||||||||||||||||||
| Corporate |
9,767 | 3.2 | % | 103,469 | 44.8 | % | 25,385 | 4.7 | % | 17,009 | 7.5 | % | ||||||||||||||||||||||||||||
| Change in fair value of contingent consideration liability |
70,700 | 22.9 | % | — | — | 70,700 | 13.1 | % | — | — | ||||||||||||||||||||||||||||||
| Amortization of intangible assets |
28,217 | 9.1 | % | — | — | 94,057 | 17.4 | % | — | — | ||||||||||||||||||||||||||||||
| Transaction costs |
6,245 | 2.0 | % | 2,267 | 0.9 | % | — | — | % | — | — | |||||||||||||||||||||||||||||
| Interest expense |
8,076 | 2.6 | % | 140 | 0.1 | % | 27,172 | 5.0 | % | 224 | 0.1 | % | ||||||||||||||||||||||||||||
| Other income (expense) |
17 | — | (114 | ) | — | (97 | ) | — | (379 | ) | (0.2 | )% | ||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||||||||||||||||||||
| Income (loss) before income taxes |
$ | 16,039 | 5.2 | % | $ | (57,129 | ) | (24.7 | )% | $ | (29,523 | ) | (5.5 | )% | $ | 28,160 | 12.4 | % | ||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||||||||||||||||||||
Net Revenues
Net revenues for the Medicare—Internal segment were $317.5 million for Pro Forma Fiscal Year 2019 compared to $53.4 million for the year ended December 31, 2018, which was primarily driven by the hiring of additional agents and the increased utilization and efficiency of our agents, which contributed to a 359.9% increase in commissionable Approved Submissions. In 2019, at our peak, we had approximately 1,700 full time equivalent agents during the Medicare annual enrollment period, compared to approximately 1,200 full time equivalent agents at our peak in 2018 during the Medicare annual enrollment period. In addition to increasing our agent count, we were able to increase the efficiency of our agents due to improvements in our technology. We were also able to utilize more agents on a year-round basis instead of during enrollment periods due to the addition of SNPs into our marketplace which are able to be sold at any time of year. Net revenues also increased in this segment due to the implementation of new marketing strategies to generate a greater number of qualified prospects and due to an increase in non-commission revenues. Revenues for the Medicare—External segment
125
Table of Contents
were $115.1 million for the Pro Forma Fiscal Year 2019 compared to $58.8 million for the year ended December 31, 2018, which was primarily driven by a 108.3% increase in commissionable Approved Submissions in the Medicare—External segment due to our ability to recruit and onboard additional external agencies to enroll consumers in Medicare plans using our technology and platform.
Net revenues for the IFP and Other—Internal segment were $58.8 million for Pro Forma Fiscal Year 2019 compared to $63.0 million for the year ended December 31, 2018. Net revenues for the IFP and Other—External segment were $48.1 million for Pro Forma Fiscal Year 2019 compared to $51.0 million for the year ended December 31, 2018. For each of the IFP and Other segments, the decreases were primarily driven by a change in product mix sold within the IFP and Other segments.
Segment Profit
Segment profit for the Medicare—Internal segment was $166.2 million for Pro Forma Fiscal Year 2019 compared to $24.2 million for the year ended December 31, 2018. The increase was driven by the increase of Medicare commissionable Approved Submissions and an increase in our LTV/CAC ratio to 3.8x for the year ended December 31, 2019 compared to 2.7x for the year ended December 31, 2018. The increase in LTV/CAC was primarily attributable to a decrease in CAC due to (i) improvements in our LeadScore and call-routing technologies allowing our agents to successfully convert more qualified prospects into Submitted Policies and (ii) improved marketing efficiencies driven by our rapid test-and-learn approach across our marketing channels, as well as an expansion of the diversity and breadth of our omni-channel marketing efforts, which together enabled the acquisition of higher quality prospects at a lower effective cost per submission.
Segment profit for the Medicare—External segment was $15.5 million for Pro Forma Fiscal Year 2019 compared to $9.0 million for the year ended December 31, 2018. The increase was primarily driven by the increase in commissionable Approved Submissions.
Segment profit for the IFP and Other—Internal segment was $3.8 million for Pro Forma Fiscal Year 2019 compared to $9.7 million for the year ended December 31, 2018. The decrease was primarily driven by a change in product mix sold for IFP and Other plans, combined with higher marketing and advertising costs to acquire customers in 2019.
Segment profit for the IFP and Other—External segment was $2.3 million for Pro Forma Fiscal Year 2019 compared to $2.8 million for the year ended December 31, 2018. The decrease was driven by a change in product mix sold by external agencies.
Liquidity and Capital Resources
Overview
Our liquidity needs primarily include working capital and debt service requirements. As of March 31, 2020 and December 31, 2019, cash and cash equivalents totaled $152.4 million and $12.3 million, respectively. We believe that our current sources of liquidity, which include cash and funds available under the Credit Facilities, along with the proceeds of this offering, will be sufficient to meet our projected operating and debt service requirements for at least the next 12 months. Short-term liquidity needs will primarily be funded through the Revolving Credit Facility portion of the Credit Facilities. As of March 31, 2020, our capacity under the Revolving Credit Facility was $30.0 million, with $30.0 million available for additional borrowings. Additionally, on May 7, 2020, we entered into an amendment to the Credit Agreement, which provides $20.0 million of additional revolving commitment under the Credit Facilities. To the extent that our current liquidity is insufficient to fund future activities, we may need to raise additional funds. In the future, we may attempt to raise additional capital through the sale of equity securities or through debt financing arrangements. If we raise additional funds by issuing equity securities, the ownership of our existing stockholders will be diluted. The incurrence of additional debt financing would result in debt service obligations, and any future instruments governing such debt could provide for operating and financing covenants that could restrict our operations.
126
Table of Contents
The following table presents a summary of cash flows for the periods presented:
| Three Months Ended March 31, |
Successor 2019 Period |
Successor 2018 Period |
Year Ended December 31, 2018 |
|||||||||||||||||
| (in thousands) | 2020 (Successor) |
2019 (Predecessor) |
||||||||||||||||||
| Net cash (used in) provided by operating activities |
$ | 23,587 | $ | 1,222 | $ | (9,284 | ) | $ | 9,281 | $ | 5,443 | |||||||||
| Net cash used in investing activities |
(3,522 | ) | (1,944 | ) | (810,010 | ) | (5,597 | ) | (6,170 | ) | ||||||||||
| Net cash provided by (used in) financing activities |
120,167 | 1,147 | 830,879 | (3,449 | ) | 63 | ||||||||||||||
Operating Activities
Cash provided by operating activities primarily consists of net income (loss) adjusted for certain non-cash items including share-based compensation; depreciation and amortization; amortization of intangible assets and internally developed software and the effect of changes in working capital and other activities.
Collection of commissions receivable depends upon the timing of the receipt of commission payments and associated commission statements from carriers. If there were to be a delay in receiving a commission payment from a carrier within a quarter, the operating cash flows for that quarter could be adversely impacted.
A significant portion of marketing and advertising expense is driven by the number of qualified prospects required to generate the insurance applications submitted to carriers. Marketing and advertising costs are expensed and generally paid as incurred and since commission revenue is recognized upon approval of a submission but commission payments are paid to us over time, there are working capital requirements to fund the upfront cost of acquiring new policies.
Net cash provided by operating activities was $23.6 million for the three months ended March 31, 2020, which consisted of $937 thousand in net loss and adjustments for non-cash items of $29.1 million, offset by the effect of changes in operating assets and liabilities representing a $4.6 million use of cash. The change in operating assets and liabilities was primarily driven by a decrease in accounts receivable of $18.4 million partially offset by an increase in commissions receivable of $5.9 million and decreases in accrued liabilities and commissions payable of $10.8 million and $5.4 million, respectively.
Net cash provided by operating activities was $1.2 million for the three months ended March 31, 2019, which consisted of $5.0 million in net income and adjustments for non-cash items of $2.2 million, offset by the effect of changes in operating assets and liabilities representing a $6.0 million use of cash. The change in operating assets and liabilities was primarily driven by increases in commissions receivable and commissions payable of $4.7 million and $1.1 million, respectively, and a decrease in accrued liabilities of $2.1 million.
Net cash used in operating activities was $9.3 million for the Successor 2019 Period, which consisted of $16.0 million in net income and adjustments for non-cash items of $100.8 million, offset by the effect of changes in operating assets and liabilities representing a $126.1 million use of cash. The change in operating assets and liabilities was primarily driven by an increase in commissions receivable of $204.0 million partially offset by an increase in commissions payables of $80.8 million, which were each driven by an increase in Medicare commissionable Approved Submissions.
Net cash provided by operating activities was $9.3 million for the Predecessor 2019 Period and primarily consisted of $57.1 million in net loss and adjustments for non-cash items of $91.5 million, offset by the effect of
127
Table of Contents
changes in operating assets and liabilities representing a $25.1 million use of cash. The change in operating assets and liabilities was primarily driven by commissions receivable of $63.4 million, offset by increases in commissions payables of $19.2 million, which were each driven by increases in Medicare commissionable Approved Submissions.
Net cash provided by operating activities was $5.4 million for the year ended December 31, 2018, which consisted of $28.1 million of net income and adjustments for non-cash items of $7.0 million, offset by the effect of changes in operating assets and liabilities representing a $29.6 million. The change in operating assets and liabilities was primarily driven by increases in commissions receivable of $65.4 million partially offset by increases in commissions payable of $30.9 million.
Investing Activities
Investing activities primarily consist of the Centerbridge Acquisition and purchases of property, equipment and software.
Net cash used in investing activities of $3.5 million for the three months ended March 31, 2020 was primarily attributable to both capitalized internal-use software related to new technology, software, and systems and purchases of property and equipment.
Net cash used in investing activities of $1.9 million for the three months ended March 31, 2019 was primarily attributable to capitalized internal-use software related to new technology, software, and systems.
Net cash used in investing activities of $810.0 million for the Successor 2019 Period was primarily attributable to the Centerbridge Acquisition, which comprised $807.6 million of net cash used in investing activities.
Net cash used in investing activities of $5.6 million for the Predecessor 2019 Period was primarily attributable to capitalized internal-use software related to new technology, software, and systems.
Net cash used in investing activities of $6.2 million in 2018 was primarily attributable to capitalized internal-use software related to new technology, software, and systems.
Financing Activities
Financing activities primarily consist of borrowings under the Term Loan Facility and the issuance of preferred and common units.
Net cash provided by financing activities of $120.2 million for the three months ended March 31, 2020 was due to borrowings under the Incremental Term Loan Facility, which comprised $117.0 million of net cash provided by financing activities and the issuance of common units, which comprised $10.0 million of net cash provided by financing activities, and was partially offset by payments of existing debt and debt issuance costs associated with the Incremental Term Loan Facility.
Net cash provided by financing activities of $1.1 million for the three months ended March 31, 2019 was due to net borrowings under our predecessor revolving credit facility of $1.2 million, partially offset by capital lease obligations payments of $16.0 thousand associated with computer equipment and furniture acquired under capital leases.
Net cash provided by financing activities of $830.9 million for the Successor 2019 Period was primarily attributable to the issuance of preferred units in connection with the Centerbridge Acquisition, which comprised $541.3 million of net cash provided by financing activities and borrowings under the Term Loan Facility, which compromised $300.0 million of net cash provided by financing activities, and was partially offset by payments of existing debt, capital lease obligations and debt issuance costs.
128
Table of Contents
Net cash used in financing activities of $3.4 million for the Predecessor 2019 Period was due to borrowings under our predecessor revolving credit facility of $56.5 million, which was offset by the repayment of such borrowings (and related expenses in relation thereto) in the amount of $59.9 million, as well as payments of our capital lease obligations.
Net cash provided by financing activities of $63.0 thousand in 2018 was due to borrowings under our predecessor revolving credit facility of $82.6 million, which was offset by the repayment of such borrowings in the amount of $82.3 million, as well as principal payments under our capital lease obligations and member distributions to non-controlling interests.
Credit Facilities
On September 13, 2019, in connection with the Centerbridge Acquisition, Norvax entered into a first lien credit agreement, or the Credit Agreement, which provides for a (i) $300.0 million aggregate principal amount senior secured term loan facility, or the Term Loan Facility and (ii) $30.0 million aggregate principal amount senior secured revolving credit facility, or the Revolving Credit Facility.
On March 20, 2020, the Borrower entered into an amendment to the Credit Agreement, which provides $117.0 million of incremental term loans, or the Incremental Term Loan Facility. On May 7, 2020, the Borrower entered into an additional amendment to the Credit Agreement, which provides $20.0 million of additional revolving commitments.
As of March 31, 2020, we had $415.5 million outstanding on the Term Loan Facility (including the Incremental Term Loan Facility). The Revolving Credit Facility had remaining capacity of $30.0 million as of March 31, 2020.
See “Description of Indebtedness” for further information about the terms of the Credit Facilities.
Contractual Obligations
The following tables summarize our contractual obligations as of December 31, 2019. The principal commitments consisted of obligations under outstanding operating leases for office facilities, capital leases related to copy machines and our long-term debt. The amount of the obligations presented in the table summarizes the commitments to settle contractual obligations in cash as of the dates presented (in thousands).
| Payments Due by Period(2)(3) | ||||||||||||||||||||
| (in thousands) | Total | Less than 1 Year |
1-3 Years | 4-5 Years | More Than 5 Years |
|||||||||||||||
| Operating lease obligations |
$ | 37,261 | $ | 5,921 | $ | 12,272 | $ | 11,489 | $ | 7,220 | ||||||||||
| Capital lease obligations |
768 | 328 | 440 | — | — | |||||||||||||||
| Long-term debt obligations(1) |
441,872 | 28,420 | 56,072 | 55,049 | 302,330 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total contractual obligations |
$ | 479,902 | $ | 34,669 | $ | 68,784 | $ | 66,538 | $ | 309,550 | ||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| (1) | Includes borrowings under the Term Loan Facility and assumes interest payments of $142.6 million through stated maturity of the Credit Facilities by applying the interest rate of 8.4% in effect as of December 31, 2019 under our Term Loan Facility. Payments herein are subject to change, as payments for variable rate debt have been estimated. As of December 31, 2019, the total principal amount of debt outstanding under our Credit Facilities, excluding unamortized debt discount and deferred issuance costs, was $299.3 million. See “Description of Indebtedness.” |
| (2) | We have not included amounts related to our earnout liabilities for the Centerbridge Acquisition as these amounts are not currently known. See Note 4 of the audited consolidated financial statements included elsewhere in this prospectus for fair value estimates recorded at December 31, 2019. |
129
Table of Contents
| (3) | The payments that we may be required to make under the Tax Receivable Agreement to the Continuing Equity Owners and the Blocker Shareholders may be significant and are not reflected in the contractual obligations tables set forth above as they are dependent upon future taxable income. See “Certain Relationships and Related Party Transactions—Tax Receivable Agreement.” |
Subsequent to December 31, 2019, on March 20, 2020, the Borrower entered into an amendment to the Credit Agreement, which, among other things, provides $117.0 million of incremental term loans. Additionally, on May 7, 2020, the Borrower entered into an amendment to the Credit Agreement, which provides $20.0 million of additional revolving commitment under the Credit Facilities, or the Incremental Revolving Loan Facility.
Off-Balance Sheet Arrangements
We have not entered into any off-balance sheet arrangements, as defined in Regulation S-K.
Recent Accounting Pronouncements
For a discussion of new accounting pronouncements recently adopted and not yet adopted, see the notes to the audited consolidated financial statements included elsewhere in this prospectus.
Quantitative and Qualitative Disclosures about Market Risk
In the normal course of business, we are subject to market risks. Market risk represents the risk of loss that may impact our financial position due to adverse changes in financial market prices and rates. Financial instruments that are exposed to concentrations of credit risk primarily consist of accounts and commissions receivable. We do not require collateral or other security for receivables, but believe the potential for collection issues with any customers was minimal as of March 31, 2020, based on the lack of collection issues in the past and the high financial standards we require of customers. As of March 31, 2020, four carriers accounted for 27%, 17%, 14% and 14% of total accounts receivable. As of December 31, 2019, five carriers accounted for 17%, 16%, 16%, 16% and 15% of total accounts receivable and as of December 31, 2018, three carriers accounted for 24%, 14% and 11% of total accounts receivable.
Interest Rate Risk
As of March 31, 2020, we had cash of $152.4 million deposited in non-interest bearing accounts at a major bank with limited to no-interest rate risk. We do not enter into investments for trading or speculative purposes and have not used any derivative financial instruments to manage interest rate risk exposure.
See “Risk Factors—Risks Related to Our Indebtedness—Developments with respect to LIBOR may affect our borrowings under our Credit Facilities” for additional information.
Seasonality
The Medicare annual enrollment period occurs from October 15th to December 7th. As a result, we experience an increase in the number of submitted Medicare-related applications during the fourth quarter and an increase in expense related to the Medicare segments during the third and fourth quarters. Additionally, as a result of the annual Medicare Advantage open enrollment period that occurs from January 1st to March 31st, commission revenue is typically second-highest in our first quarter. The individual and family health insurance open enrollment period runs from November 1st through December 15th of each year for most states, and we expect the number of approved applications for individual and family health insurance to be higher in the fourth quarter compared to other quarters of the year as a result. A significant portion of our marketing and advertising expenses is driven by the number of health insurance applications submitted through us. Marketing and advertising expenses are generally higher in the
130
Table of Contents
fourth quarter during the Medicare annual enrollment period, but because commissions from approved customers are paid to us over time, our operating cash flows could be adversely impacted by a substantial increase in marketing and advertising expenses as a result of a higher volume of applications submitted during the fourth quarter or positively impacted by a substantial decline in marketing and advertising expenses as a result of lower volume of applications submitted during the fourth quarter.
Critical Accounting Policies and Estimates
The preparation of consolidated financial statements in conformity with GAAP requires management to make estimates and assumptions that affect the reported amounts of revenues, expenses, assets, and liabilities and disclosure of contingent assets and liabilities in our financial statements. We regularly assess these estimates; however, actual amounts could differ from those estimates. The most significant items involving management’s estimates include estimates of revenue recognition, commissions receivable, and commissions payable. The impact of changes in estimates is recorded in the period in which they become known.
An accounting policy is considered to be critical if the nature of the estimates or assumptions is material due to the levels of subjectivity and judgment necessary to account for highly uncertain matters or the susceptibility of such matters to change, and the effect of the estimates and assumptions on financial condition or operating performance. The accounting policies we believe to reflect our more significant estimates, judgments and assumptions that are most critical to understanding and evaluating our reported financial results are: revenue recognition, commissions receivable, and commissions payable.
Revenue Recognition and Commissions Receivable
In accordance with ASC 606, revenue is recognized when a customer obtains control of promised goods or services and is recognized in an amount that reflects the consideration that an entity expects to receive in exchange for those goods or services. We apply the following five-step model in order to determine this amount: (i) identification of the promised goods in the contract; (ii) determination of whether the promised goods are performance obligations, including whether they are distinct in the context of the contract; (iii) measurement of the transaction price, including the constraint on variable consideration; (iv) allocation of the transaction price to the performance obligations; and (v) recognition of revenue when (or as) we satisfy each performance obligation.
Significant management judgments and estimates must be made in connection with determination of the revenue to be recognized in any accounting period. If we made different judgments or utilized different estimates for any period, material differences in the amount and timing of revenue recognized could result. The accounting estimates and judgments related to the recognition of revenue require us to make assumptions about numerous factors, such as the determination of performance obligations and determination of the transaction price. The estimates of renewal commissions and production bonuses are considered variable consideration in the transaction price and require significant judgment including determining the number of periods in which a renewal will occur and the value of those renewal commissions to be received if renewed. We utilize the expected value approach to do this, incorporating a combination of historical lapse and premium increase data, available industry and carrier experience data, historical payment data by segment and carrier, as well as current forecast data to estimate forecasted renewal consideration and production bonuses and then to constrain revenue recognized to the extent that it is probable that a significant reversal in the amount of cumulative revenue recognized will not occur. Before the adoption of ASC 606, we were already using a similar method to calculate the lifetime revenue value of a contract for internal forecasting purposes so we believe we have the ability to make reasonable estimates for these items and have the appropriate accounting policies and controls in place to do so. The uncertainty associated with the variable consideration is subsequently resolved when the policy renews, and any adjustments in variable consideration are recognized in the period incurred.
Commissions receivable represents the variable consideration for policies that have not renewed yet, and therefore, are subject to the same assumptions, judgments and estimates used when recognizing revenue as noted above.
131
Table of Contents
Income Taxes
We account for income taxes using an asset and liability approach. Deferred income tax assets and liabilities result from temporary differences between the tax basis of assets and liabilities and their reported amounts in the consolidated financial statements that will result in taxable or deductible amounts in future years. Valuation allowances are provided when necessary to reduce deferred tax assets to the amount expected to be realized.
The determination of our provision for income taxes requires management’s judgment in the use of estimates and the interpretation and application of complex tax laws. Judgment is also required in assessing the timing and amounts of deductible and taxable items. We establish liabilities for material, known tax exposures relating to deductions, transactions and other matters involving some uncertainty as to the proper tax treatment of the item. Our liabilities reflect our judgment as to the resolution of the issues involved if subject to judicial review. When facts and circumstances change (including a resolution of an issue or statute of limitations expiration), these liabilities are adjusted through the provision for income taxes in the period of change.
JOBS Act
We qualify as an “emerging growth company” pursuant to the provisions of the JOBS Act, enacted on April 5, 2012. Section 102 of the JOBS Act provides that an “emerging growth company” can take advantage of the extended transition period provided in Section 7(a)(2)(B) of the Securities Act for complying with new or revised accounting standards. We are electing to delay the adoption of new or revised accounting standards, and as a result, we may not comply with new or revised accounting standards on the relevant dates on which adoption of such standards is required for non-emerging growth companies. As a result, our consolidated financial statements may not be comparable to companies that comply with new or revised accounting pronouncements as of public company effective dates.
We are in the process of evaluating the benefits of relying on other exemptions and reduced reporting requirements provided by the JOBS Act. Subject to certain conditions set forth in the JOBS Act, if as an emerging growth company we choose to rely on such exemptions, we may not be required to, among other things, (1) provide an auditor’s attestation report on our systems of internal controls over financial reporting pursuant to Section 404, (2) provide all of the compensation disclosure that may be required of non-emerging growth public companies under the Dodd-Frank Act, (3) comply with the requirement of the PCAOB regarding the communication of critical audit matters in the auditor’s report on the financial statements, and (4) disclose certain executive compensation-related items, such as the correlation between executive compensation and performance and comparisons of the Chief Executive Officer’s compensation to median employee compensation. These exemptions will apply until we no longer meet the requirements of being an emerging growth company. We will remain an emerging growth company until the earlier of (a) the last day of the fiscal year (i) following the fifth anniversary of the completion of our initial public offering, (ii) in which we have total annual gross revenue of at least $1.07 billion or (iii) in which we are deemed to be a large accelerated filer, which means the market value of our common stock that is held by non-affiliates exceeds $700.0 million as of the last business day of our prior second fiscal quarter, and (b) the date on which we have issued more than $1.07 billion in non-convertible debt during the prior three-year period.
132
Table of Contents
Overview
We are a leading health insurance marketplace whose mission is to improve access to healthcare in America. Our proprietary technology platform leverages modern machine-learning algorithms powered by nearly two decades of insurance behavioral data to reimagine the optimal process for helping individuals find the best health insurance plan for their specific needs. Our differentiated combination of a vertically-integrated consumer acquisition platform and highly skilled and trained licensed agents has enabled us to enroll millions of people in Medicare and individual and family plans since our inception. With over 10,000 Americans turning 65 years old every day and GoHealth’s track record of significant growth in net revenues in the Medicare space in the past five years, we believe we will continue to be one of the top choices for unbiased insurance advice to help navigate one of the most important purchasing decisions individuals make.
Since our inception, we have consistently invested in our technology, data science and business processes to enroll millions of people in health insurance plans while helping carriers scale their product and plan offerings. Our platform utilizes proprietary technology, machine-learning capabilities, data, efficient business processes, and highly skilled and trained licensed agents to connect consumers with carriers through multiple channels. Through our platform, we offer a wide array of health insurance policies, including, but not limited to, Medicare Advantage, Medicare Supplement, prescription drug plans, and individual and family plans, and allow consumers to choose how to purchase these plans, either with the assistance of our agents or directly online.
For many consumers, choosing a health insurance plan is confusing and difficult, and seemingly small differences between health insurance plans can lead to significant out-of-pocket costs or lack of access to critical medicines or providers. We simplify the difficult and confusing process by offering a large selection of health insurance plan choices, unbiased advice informed by consumers’ specific needs, transparency of health insurance plan benefits and fit, assistance accessing available government subsidies and a high-touch TeleCare team. The TeleCare team is focused on increasing consumer engagement with the GoHealth brand, selling new products and services to our consumers that help meet their healthcare needs, and helping consumers maximize their health insurance plan benefits to support long-term health and wellness. Carriers also benefit from our platform, especially those looking to access the large and fast-growing Medicare-eligible population. We believe carriers utilize our large-scale data and technology as well as our efficient marketing and conversion processes to reduce their CAC, compared to carrier-employed agent workforces. In fact, we believe GoHealth is the largest external partner for Medicare Advantage enrollments for many carriers.
We have a 19-year history of consistent revenue growth and entering new market segments of insurance products. We add significant value to consumers and carriers, which is evidenced by our high growth rate and strong customer engagement dynamics. Specifically, net revenues grew by 104.1% to $141.0 million for the three months ended March 31, 2020 compared to $69.1 million for the three months ended March 31, 2019 and by 138.5% to $539.5 million for the Pro Forma Fiscal Year 2019 compared to $226.2 million for the year ended December 31, 2018. Adjusted EBITDA grew by 391.5% to $34.9 million for the three months ended March 31, 2020 compared to $7.1 million for the three months ended March 31, 2019 and by 386.8% to $170.0 million for the Pro Forma Fiscal Year 2019 from $34.9 million for the year ended December 31, 2018. Net loss was $937 thousand for the three months ended March 31, 2020 compared to net income of $5.0 million for the three months ended March 31, 2019, and net loss was $29.5 million for the Pro Forma Fiscal Year 2019 compared to net income of $28.1 million for the year ended December 31, 2018. See “Prospectus Summary—Summary Historical and Pro Forma Condensed Consolidated Financial and Other Data” for information regarding our use of (i) pro forma financial information, specifically footnote 1 and (ii) Adjusted EBITDA, a non-GAAP financial measure, and a reconciliation of Adjusted EBITDA to net income, the most directly comparable financial measure calculated and presented in accordance with GAAP.
Over the last four years, we have increasingly shifted our focus towards Medicare products and deemphasized individual and family health insurance products. This shift in focus has enabled us to capitalize on (1) strong
133
Table of Contents
demographic trends, with Medicare enrollment expected to grow from approximately 61 million individuals in 2019 to approximately 77 million individuals by 2028, (2) the increasing proportion of the Medicare-eligible population that is choosing commercial insurance solutions, with 38% of Medicare beneficiaries, or approximately 23 million people, enrolled in Medicare Advantage plans in 2019, an increase of approximately 1.5 million people from 2018 to 2019, and (3) an antiquated traditional field agent driven sales process lacking in transparency, choice and convenience and ripe for disruption by digitally-enabled and technology-driven marketplaces like our platform. Today, we estimate a total addressable market of $28 billion for Medicare Advantage and Medicare Supplement products, which is based on third-party estimates of total expected Medicare enrollees for 2020, publicly available industry data for Medicare agents’ first-year compensation and our recent historical policy revenue experience. We believe that these trends will drive a larger market in the coming years that, when taken together with our other product and plan offerings, will result in an even larger addressable market. We also believe that we are poised to benefit from market share gains in what has traditionally been a highly fragmented market.
Consumers first engage through our platform either online or telephonically in response to our data-driven, omni-channel marketing efforts. We then use LeadScore, one of our proprietary machine-learning technologies, to evaluate consumer leads in real-time. In 2019, we generated over 42.2 million consumer interactions. The data we generate from each consumer interaction helps inform our marketing, consumer lead scoring, qualified prospect routing, and health insurance plan matching technology in a feedback loop. We also scored over 4 million consumer leads in 2019, which informs us of the potential profitability and conversion probability of the consumer lead and helps us optimize routing of consumer leads to agents. Our proprietary technology and business processes then route qualified prospects online or via live transfer to our agents, both through the internal and external channel. Our technology and workflow allow these agents to work in our Benefits Center, where our sales operations are located, or to work remotely at home. In 2019, we employed an average of 931 agents, reaching a high of 1,453 agents during the three months ended December 31, 2019. Based on consumers’ specific needs and our comprehensive data, our agents use our proprietary technology platform, Marketplace, to identify the optimal health insurance plan options from our vast inventory of insurance products. Marketplace then facilitates seamless quoting and enrollment of the consumer-selected health insurance plan using proprietary and third-party data and direct API connections with carriers. As a result of our Marketplace technology and increasingly robust data and insights, our qualified prospect to Submitted Policy conversion rate increased from 20.7% for the three months ended March 31, 2019 to 24.3% for the three months ended March 31, 2020, and from 20.6% in 2018 to 23.2% in 2019 for the multi-carrier sales outlet of the Medicare—Internal segment. An increase in the conversion rate of qualified prospects to Submitted Policies generally results in greater commissionable Approved Submissions.
Using our proprietary data, we identify consumers who would benefit from proactive engagement and education on their health insurance plan design and guidance on how they can maximize their plan benefits. We believe that using our data-driven targeted consumer outreach and our highly skilled agents and proprietary technology to properly select health insurance plans to meet a consumer’s particular needs results in higher customer satisfaction. As we enroll more qualified prospects through our Marketplace, the power of our data improves our marketing, technology, and agent performance. Our platform is engineered for rapid scalability, with modern cloud infrastructure that has information security controls that are independently audited by several third-party firms, and technology driven compliance with HIPAA, TCPA and state insurance regulations, and the CMS regulations.
134
Table of Contents
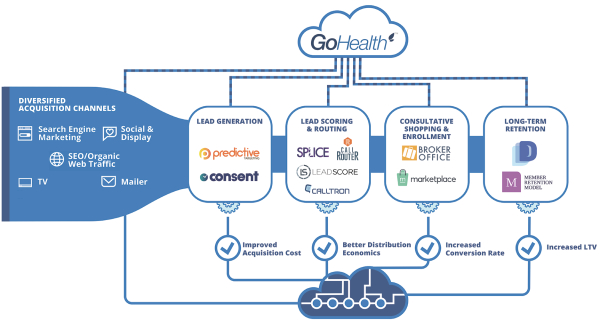
Consumers do not pay any fees for access to our platform or for our enrollment, education or other services. Generally, we are paid an initial commission by carriers when consumers enroll in their products and become customers, and additional recurring commissions as long as those customers retain their health insurance plans. The commission structure encourages collaboration between us and carriers to increase customer satisfaction by choosing health insurance products that best fit customers’ needs, which drives better outcomes for carriers, customers, our agents, and employees. We use advanced statistical models that are built on observable commissions received rather than solely historic cohorts. Our advanced statistical models consider consumer demographic attributes, health insurance plan characteristics and temporal data to value these future commission streams from which we determine an expected LTV of the commission streams associated with each consumer enrolled in each specific plan product. Total commissions receivable, which represents such expected future commission streams, was $388.8 million as of March 31, 2020, an increase of 223.4% compared to March 31, 2019. In addition to commissions, some of our carriers have historically partnered with us to generate consumer leads and have paid us for marketing services. We do not insure customers and assume no underwriting or medical loss risk associated with placement of customers in our carriers’ products.
The differentiated value of our data science-driven, fully-integrated platform has facilitated our rapid growth. Net revenues grew by 104.1% to $141.0 million for the three months ended March 31, 2020 compared to $69.1 million for the three months ended March 31, 2019 and by 138.5% to $539.5 million for the Pro Forma Fiscal Year 2019 compared to $226.2 million for the year ended December 31, 2018. Adjusted EBITDA grew by 391.5% to $34.9 million for the three months ended March 31, 2020 compared to $7.1 million for the three months ended March 31, 2019 and by 386.8% to $170.0 million for the Pro Forma Fiscal Year 2019 from $34.9 million for the year ended December 31, 2018. Net loss was $937 thousand for the three months ended March 31, 2020 compared to net income of $5.0 million for the three months ended March 31, 2019 and net loss was $29.5 million for the Pro Forma Fiscal Year 2019 compared to net income of $28.1 million for the year ended December 31, 2018. Our focus on Medicare has also contributed significantly to our growth. Total revenues generated in the Medicare segments grew to $124.2 million for the three months ended March 31, 2020 from $41.2 million for the three months ended March 31, 2019, representing a 201.5% increase, and to $432.7 million for the Pro Forma Fiscal Year 2019 from $112.2 million for the year ended December 31, 2018, representing a 285.7% increase. In the Medicare segments, our total Submitted Policies grew to over 122,400 Medicare policies for the three months ended March 31, 2020, as compared to over 43,200 Medicare policies the three months ended March 31, 2019 and over 427,000 Medicare policies for the year ended December 31, 2019,
135
Table of Contents
as compared to over 118,000 Medicare policies for the year ended December 31, 2018. See “Prospectus Summary—Summary Historical and Pro Forma Condensed Consolidated Financial and Other Data” for information regarding our use of (i) pro forma financial information, specifically footnote 1 and (ii) Adjusted EBITDA, a non-GAAP financial measure, and a reconciliation of Adjusted EBITDA to net income, the most directly comparable financial measure calculated and presented in accordance with GAAP.
Our Business Model
Our Platform
Our platform utilizes proprietary technology, machine-learning capabilities, data, efficient business processes, and highly skilled and trained licensed agents to generate a stable, visible revenue stream that benefits from favorable demographic trends. The key components of our platform are:
| • | Data-Driven, Omni-Channel Marketing. Based on predictive consumer lead targeting and a high cadence of multivariate testing on consumer lead generation properties, our data-driven, omni-channel marketing drives increased impressions and qualified prospects with a target return on marketing spend. |
| • | Proprietary LeadScore Technology. LeadScore, one of our proprietary machine-learning technologies, is built on large-scale, end-to-end sales data, predicts the LTV and conversion probability of consumer leads, and is utilized to optimize routing of the consumer leads in real-time regardless of their source. |
| • | Sophisticated Matching Technology. Our proprietary qualified prospect distribution, routing, and priority queuing technology based on LeadScore and agent performance data models help us to optimally match qualified prospects to those agents most likely to convert the qualified prospect to a customer. |
| • | The Marketplace. Our proprietary Marketplace technology features decision support tools and seamlessly integrates with carrier enterprise systems, empowering our highly skilled and trained agents to quickly and efficiently select the right health insurance plan for each consumer based on their specific needs and enroll them in those plans. |
| • | TeleCare Team. Our high-touch TeleCare team is focused on increasing consumer engagement with the GoHealth brand, selling new products and services to our consumers that help meet their healthcare needs, and helping consumers maximize their health insurance plan benefits to support long-term health and wellness. |
| • | Scalable and Compliant Infrastructure. Our cloud infrastructure and compliance-by-design technology ensures scalability and compliance across our platform. |
Our Value Proposition
We believe the key components of our platform are difficult to replicate for field-based agents, carrier-employed agents, and other digital or telesales competitors, making us increasingly valuable to carriers and consumers. As we increase the number of Submitted Policies, our data on qualified prospect, agent, and carrier performance becomes richer, feeding into our machine-learning and data science-enabled feedback loops, making our marketing and technology even smarter. This differentiates us from other channels and competitors, allowing us to generate more consumer leads, convert those consumer leads to customers at a higher rate, serve our customers over a longer period of time, and reduce our CAC.
We believe that LTV/CAC provides the best metric on a per commissionable Approved Submission basis into the efficiency and performance of our integrated platform. We focus on strengthening the key drivers of LTV/CAC, including marketing costs, the consumer lead to customer conversion rate and customer satisfaction. While we offer both do-it-yourself and agent-assisted channels to accommodate consumers’ preferences, we believe
136
Table of Contents
that for most qualified Medicare prospects, an agent-assisted model maximizes LTV/CAC. As we continue to scale our platform, we improve our key drivers through specialization and optimization using our proprietary data and machine-learning.
Our Products
We operate our business in four segments: (i) Medicare—Internal, (ii) Medicare—External, (iii) IFP and Other—Internal and (iv) IFP and Other—External. The Medicare segments focus on sales of Medicare Advantage, Medicare Supplement, Medicare prescription drug plans, and Medicare SNPs for multiple carriers. The Medicare segments are organized by distribution channel, as further described below:
| • | Internal. The internal segments primarily consist of sales of products and plans by GoHealth-employed agents offering qualified prospects plans from multiple carriers, GoHealth-employed agents offering qualified prospects plans on a carrier-specific basis, or sales of products and plans through our online platform without the assistance of our agents, which we refer to as DIY. |
| • | External. The external segments represent sales of products and plans under GoHealth’s carrier contracts using external agencies, who use agents that are not employed by GoHealth. These agents utilize our technology and platform to enroll consumers in health insurance plans and provide a means to earn a return on consumer leads that otherwise may have not been addressed. |
The Medicare—Internal segment is the largest segment by revenue and a primary contributor to our growth and margin expansion. Medicare Advantage products generate the majority of net revenues in the Medicare—Internal segment. Medicare Advantage plans accounted for (i) approximately 70.4% and 44.9%, respectively, of net revenues for the three months ended March 31, 2020 and 2019 and approximately 62.6% and 37.2%, respectively, of net revenues for the Pro Forma Fiscal Year 2019 and for the year ended December 31, 2018; (ii) approximately 75.4% and 81.0%, respectively, of Medicare—Internal segment revenue for the three months ended March 31, 2020 and 2019 and approximately 75.8% and 80.2%, respectively, of Medicare—Internal segment revenue for the Pro Forma Fiscal Year 2019 and for the year ended December 31, 2018; and (iii) approximately 94.8% and 69.3%, respectively, of Medicare—External segment revenue for the three months ended March 31, 2020 and 2019 and approximately 84.1% and 70.4%, respectively, of Medicare—External segment revenue for the Pro Forma Fiscal Year 2019 and for the year ended December 31, 2018. No other products in the Medicare segments contribute more than 10% of net revenues for either of the Medicare segments or total net revenues for the financial statement periods presented in this prospectus. Over the last two years, we grew the Medicare—Internal segment multi-carrier channel agent count and prioritized the placement of qualified prospects into the Medicare—Internal segment. Going forward, we intend to continue our focus on growth and placing qualified prospects within this segment. The Medicare—Internal segment also provides significant benefits to the broader business. For example, carriers that partner with us through one or more of our internal segment businesses will often supplement our marketing and technology investments. Additionally, the external segments can be used when the number of consumer leads in our marketplace is higher than we can address in a timely fashion using our internal channel.
The IFP and Other segments focus on sales of individual and family plans (which includes fixed indemnity and major medical plans), dental plans, vision plans and other ancillary plans to individuals that are not Medicare-eligible. The IFP and Other segments are also organized by distribution channel, internal and external. The IFP and Other segments represent a valuable source of diversification of products, carriers, consumers and revenue that are not tied solely to Medicare. Many of the products in the IFP and Other segments have a policy life under a single year, and we are paid approximately 90% of our commission streams in these segments in the first year. Fixed Indemnity plans accounted for (i) approximately 22.0% of net revenues for the three months ended March 31, 2019 and 15.0% of net revenues for the year ended December 31, 2018; (ii) approximately 12.5% and 50.4%, respectively, of IFP-Internal segment revenue for the three months ended March 31, 2020 and 2019 and approximately 36.7% and 22.1%, respectively, of IFP—Internal segment revenue for the Pro Forma Fiscal Year 2019 and for the year ended December 31, 2018; and (iii) approximately 38.2% and 59.2%, respectively, of
137
Table of Contents
IFP—External segment revenue for the three months ended March 31, 2020 and 2019 and approximately 53.7% and 39.1%, respectively, of IFP—External segment revenue for the Pro Forma Fiscal Year 2019 and for the year ended December 31, 2018. No other products in the IFP and Other segments contribute more than 10% of net revenues for either of the IFP segments or to total net revenues for the financial statement periods presented in this prospectus.
For the three months ended March 31, 2020, the Medicare segments represented 88.1% of total revenues compared to 59.7% of total revenues for the three months ended March 31, 2019 and the IFP and Other segments represented 11.9% of total revenues for the three months ended March 31, 2020 compared to 40.3% of total revenues for the three months ended March 31, 2019. For the Pro Forma Fiscal Year 2019, the Medicare segments represented 80.2% of total revenues compared to 49.6% of total revenues for the year ended December 31, 2018 and the IFP and Other segments represented 19.8% of total revenues for the Pro Forma Fiscal Year 2019 compared to 50.4% of total revenues for the year ended December 31, 2018.
Our Strengths
Fully Integrated End-to-End Insurance Marketplace
Our platform connects insurance consumers with carriers. The strength of our platform is our innovation in enhancing the education of, and transparency and choice for, consumers, which has dramatically changed how consumers purchase health insurance and displaced incumbent market leaders in insurance distribution. The insurance distribution incumbents, such as field-based and carrier-employed agents, offered neither the broad choice of health insurance plans we are able to offer nor the unbiased support in health insurance plan selection based on the years of consumer shopping data we have gathered and the sophisticated models we have developed to match health insurance plans to consumers. We apply our proprietary, machine-learning technology, LeadScore, to target, assess, and prioritize all of our consumer leads (over 4 million in 2019) in real-time.
Incumbent insurance distributors do not have access to equivalent technology, and we believe this difference in capabilities allows us to benefit from lower CAC. Our technology is difficult to replicate because acquiring the data underlying our models at our scale (over 10 years of insurance data) and scope, as well as refining those models to the performance we have obtained would be time-consuming, expensive and complicated for newer entrants in this market. Our technology and business processes route qualified consumer leads online or via live transfer to agents across our multiple channels ensuring that few qualified prospects leave our marketplace without an interaction and maximizing each consumer interaction to ensure a higher likelihood of consumer acquisition and higher margin contribution. We use a combination of proprietary and third-party data, direct API connections to many carriers, and our proprietary technology platform, Marketplace, to educate, quote and enroll consumers in real-time to the health insurance plan best suited to meet their specific needs, which enhances long-term customer satisfaction. The resulting increase in the expected LTV of consumers obtained at a lower CAC has made our innovative distribution model more appealing to carriers and has altered their own approach to strategic marketing and consumer acquisition. The data we generate from each consumer interaction helps inform our marketing, consumer lead scoring, qualified prospect routing, and health insurance plan matching technology in a feedback loop. We engineered our marketplace for rapid scalability, with modern cloud infrastructure that has information security controls that are independently audited by several third-party firms and complies with HIPAA, TCPA and DOI and CMS regulations. We had over 122,400 Submitted Policies in the Medicare segments for the three months ended March 31, 2020 and over 427,000 Submitted Policies in the Medicare segments for the year ended December 31, 2019, which we believe makes us one of the largest health insurance marketplaces based on publicly available information about our competitors and our carriers and our general knowledge of the industry acquired over our 19-year operating history. The data generated through the sales process by these consumers helps us increase LTV/CAC through machine-learning enabled feedback loops, and allows us to improve and deepen our relationships with carriers.
138
Table of Contents
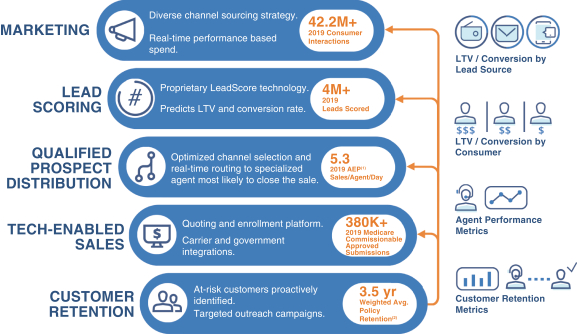
| (1) | 2019 AEP Sales/Agent/Day is presented for the multi-carrier sales outlet of the Medicare—Internal segment. |
| (2) | Average policy retention is presented as of January 1, 2019 for selected carriers that we believe are generally representative of our customer base for Medicare Advantage products. |
Data-driven, Omni-channel Marketing
We generate over 42.2 million unique consumer interactions per year across an omni-channel diversified portfolio of sources. These sources include digital methods, such as search engine marketing, impulse-marketing and social-media, and non-digital methods, including television, mailers and radio. We use our real-time consumer lead to customer conversion data from various marketing sources to rapidly and cost-efficiently adjust and scale our marketing sources to maximize LTV/CAC and cost per qualified prospect. We also use our database of over 85 million consumer lead records to build machine-learning models that create complex lookalike audiences to enable us to efficiently target consumer leads that are more likely to convert to customers. Using our rapid test-and-learn approach, in 2019 alone, we tested over 30,000 advertisements and more than 100 site variations, which drove an increase in the website visitor to consumer lead conversion rate to 17.2% in 2020, an increase of over 124% from a rate of 7.7% in 2019. For the multi-carrier sales outlet of the Medicare—Internal segment, we were able to increase qualified prospects from approximately 237,000 in 2018 to approximately 930,000 in 2019, an increase of 292.4%, while also increasing the rate of qualified prospect to Submitted Policy conversions during the three months ended December 31, 2019 for this channel to 27% from 24% during the same period in 2018. We have grown in both number and quality of our consumer interactions while also generating more internal consumer leads, reducing our dependence on acquiring consumer leads from third-party sources. For the three months ended December 31, 2019, the multi-carrier sales outlet of the Medicare—Internal segment had 70% of consumer leads internally generated, compared to 58% for the same period in 2018.
Deep, Tenured and Expanding Relationships with Top Carriers
Our carrier relationships allow us to offer a wide variety of products and plans across our platform and offer solutions tailored to consumers’ healthcare needs. We are a critical partner to our top carriers, for which we use
139
Table of Contents
our data and direct API connections to help inform their plan and network design and assist with budgeting. Our carrier relationships are stable, as evidenced by the fact that our relationships with each of our five largest carriers, measured by 2019 submission volume, exceeds five years. Over the past five years, we have expanded those relationships from initially covering individual and family products to covering Medicare Advantage products at all five of these carriers. We are licensed in all 50 states and the District of Columbia, which combined with our data-driven, omni-channel marketing and effective and scalable marketplace, makes us a partner of choice for the leading Medicare Advantage plans nationally and in each state. In 2020, we expect our platform will include Medicare Advantage products from at least one of the top two carriers, as measured by Medicare Advantage enrollees in each county, in 49 states, which collectively represented 95% of 2019 Medicare enrollments. In 2019, our platform included Medicare Advantage products from at least one of the top two carriers, as measured by Medicare Advantage enrollees in each county, in 24 states, which collectively represented 54% of 2019 Medicare enrollments. We believe that consumers increasingly want greater choice and are looking for quality health insurance plans as measured by CMS STAR ratings. We believe that by offering more health insurance plans in each county and more higher-rated health insurance plans, we can increase the rate of consumer lead to customer conversions and customer satisfaction rates.
Best-in-Class Medicare LTV/CAC Ratio Driven by Proprietary Technology, Business Processes, Data and Highly Skilled Agents
Our integrated technology platform, business processes, data and highly skilled and trained agents enable us to rapidly scale while improving our unit economics, as measured by LTV/CAC. As we scale our business, our machine-learning data combined with our omni-channel marketing allows us to become progressively better at acquiring consumer leads with favorable engagement potential and to do so at lower cost. In doing so, we increase the lifetime commissions generated by the consumer leads we convert, which increases LTV per Approved Submission, and we reduce the cost of acquiring consumer leads, lowering CAC per commissionable Approved Submission. With increasing scale, our proprietary LeadScore and CallRouter technologies become better at assessing the profile and predicted value of each incoming consumer lead and routing the consumer lead to the agent most likely to convert the consumer, further lowering CAC per commissionable Approved Submission. The CallRouter platform also utilizes data-driven agent clustering to enable us to train and specialize our agents on specific customer segments to optimize our results. We dynamically route qualified prospects across all of our channels with a focus on converting our highest value qualified prospects in our most profitable channels and enhancing the consumer experience across our platform. Our Marketplace technology quickly compares health insurance plans that most closely match the consumer’s specific needs, which increases the potential conversion and engagement of the consumer to the health insurance plan, increasing the LTV per Approved Submission, while also decreasing agent plan selection time, thus decreasing CAC per commissionable Approved Submission. Finally, our management team has extensive leadership experience managing customer service centers and scaling new sales offices. Our agent recruiting, training, development programs, and technology decision support with our Marketplace technology allow us to improve agent productivity, while also enhancing our consumer experience. We believe our LTV/CAC ratios for the Medicare segments are superior to those achieved by other digital marketplaces, carriers, and field-based agents.
History of Continuous Growth and Innovation and Proven Ability to Add Products
Our Founders and management team have a consistent track record of growth and entry into new market opportunities for our business. Since our founding in 2001, we evolved from a company selling quoting and enrollment technology to independent brokers to the fully integrated end-to-end insurance marketplace we are today. We have diversified our product mix to add individual and family plans, dental and vision plans, prescription drug plans, and most recently, Medicare plans. This has enabled us to serve more consumers and to prioritize different products depending on regulatory and political environments, carriers’ priorities and consumers’ preferences. Our data assets, technology, and compliance infrastructure have scaled efficiently with each consumer interaction and health insurance plan submission through our platform, and as we have invested in the next generation of our proprietary technology. We believe our management team, entrepreneurial spirit, and
140
Table of Contents
data and technology position us well for continuous growth in the future in our current product segments and other insurance products segments we may enter.
Our Growth Strategies
Expand Our Carrier Relationships and Health Insurance Plan Options to Grow the Medicare Segments
We believe we are a partner of choice for the top carriers in the Medicare marketplace because of our scale, efficiency and ability to integrate with carriers using direct API connections to exchange data and insights. Given our growth in Approved Submissions in the Medicare segments and the integrated data and technology of our platform, Medicare carriers have shown increased interest in working with us, including those who have not traditionally used digitally-enabled models. In 2020, we expect our platform will include Medicare Advantage products from at least one of the top two carriers, as measured by Medicare Advantage enrollees in each county, in 49 states, which collectively represented 95% of 2019 Medicare enrollments. In 2019, our platform included Medicare Advantage products from at least one of the top two carriers, as measured by Medicare Advantage enrollees in each county, in 24 states, which collectively represented 54% of 2019 Medicare enrollments. This allows us to benefit from enhanced return of scale, more efficient marketing in these geographies, increased agent conversion rates of qualified prospects to customers, and improved customer satisfaction rates as we meet the needs of our customers. In addition, we are increasingly adding SNPs into our marketplace from both existing and new carrier relationships. Unlike Medicare Advantage products, which can largely be sold only during the Medicare annual enrollment period and open enrollment period, SNPs can generally be sold throughout the special enrollment period. As a result, we are able to maximize the value of our consumer interactions and marketing spend during the special enrollment period and prioritize agent growth year round. As we add more Medicare products and expand SNP offerings, we allocate more of our existing agent seat count to the Medicare—Internal segment from other less profitable channels, reducing the need to open new facilities. Additionally, we have implemented work from home options to increase agent efficiency and capacity without a significant increase in fixed costs.
Continue to Increase Our Profitability By Using our Data to Improve our Technology, Business Processes, and Agent Performance
We are implementing a number of initiatives to help improve our LTV/CAC, which is a key measure of our unit economics and overall business profitability, by using our data to improve our platform and predictive capabilities, business processes, and agent performance.
| • | Upgraded Marketplace Technology. In October 2019, we launched an upgrade to our proprietary Marketplace technology to increase agent productivity by improving the flow of data across our platform, advancing our decision support capabilities, and improving the qualified prospect to Submitted Policy conversion rates of our overall agent population to a level closer to that of our most productive agents. |
| • | Improving LeadScore and Call Routing Technologies. We are improving our LeadScore and call-routing technologies, and expanding our business intelligence and analytics staffing to direct qualified prospects to agents or DIY channels that are most likely to result in such qualified prospects enrolling in the health insurance plan that best meets their needs while remaining economically attractive for us. We are also increasingly using our data to identify the best agent clusters to enroll an individual qualified prospect based on our Marketplace engine’s determination of their likely optimal plan design, carrier, and demographic match based on the information we have about that qualified prospect. Additionally, we are investing in technology that will allow us to use our data to direct our marketing spend into growing our flow of qualified prospects in the highest-value marketing channels and enhancing our proprietary LeadScore technology to assess and iterate, in real-time, the performance of those marketing channels throughout the year. |
| • | Improving Recruiting and Training of Agents. We are improving the recruiting and training of our agents to match the profiles of our highest performing agents. The opportunity to reduce the variability |
141
Table of Contents
| in our agent performance is significant, as our top 25% of agents for the multi-carrier sales outlet of the Medicare—Internal segment on average were 61% more productive than the remaining 75% of our agents for the multi-carrier sales outlet of the Medicare—Internal segment, based on conversion rates of qualified prospects to Submitted Policies for the three months ended March 31, 2020. We have analyzed our most productive agents and revised our recruiting, training and onboarding of the number of licenses and appointments to most closely match the skills and experiences of our most productive agents. |
Build Identification with the GoHealth Brand
We believe we can solidify our position as the largest Medicare marketplace and brand for consumers’ health insurance needs. As the Medicare markets continue to grow and the Medicare Advantage sector continues to gain market share, carriers are and will continue differentiating their health insurance plans by offering additional products and services. This differentiation creates the need for more education, transparency and choice, and the need for a “Trusted Advisor” role that we believe the GoHealth brand can own. By helping customers make this choice, they can more readily identify the GoHealth brand, which we believe differentiates us from our competitors. This allows us to improve customer satisfaction even when their underlying carrier or plan product changes.
We are using technology and data increasingly to build the GoHealth brand and our digital marketing campaigns, which significantly improved impressions in 2019 with over 1.1 billion impressions generated, compared to 225 million impressions generated in 2018. We have launched our new plan comparison tool and are launching a new website that we will consolidate into one consumer website in 2020, which we believe will enhance conversion in our DIY channel.
Provide Additional Products and Services to our Qualified Medicare Prospects, Existing Customers and Carriers
In 2019, we interacted with approximately 930,000 qualified prospects through the multi-carrier sales outlet of the Medicare—Internal segment. While we have focused historically on educating and enrolling those qualified prospects in Medicare products, we have not historically prioritized offering qualified prospects or existing customers additional products, such as life, dental, hearing, or vision plans if their Medicare product does not offer coverage for these services. We have a significant opportunity to sell additional products to our qualified Medicare prospects and existing Medicare customers going forward.
We currently enroll a sizable percentage of Medicare customers for our largest carriers, but there is still significant opportunity to grow our share of enrollments for existing carriers even while we add new carriers to our marketplace. We are using our data to help our largest carriers inform the benefit design of their health insurance plans and product competitiveness in given regions, which is a value added service that traditional field-agents and carrier internal channels cannot offer. We are also focused on increasing offerings of additional revenue generating services that are valuable to our Medicare carriers and enhance the health of our customers, including by helping new Medicare enrollees sign up for a health-risk assessment, which helps calibrate the Medicare Advantage premium paid by Medicare to the private plan. Additionally, we are exploring opportunities to (1) provide screening of customers for social determinants of health factors, such as loneliness, or food or housing insecurity, that could lead to higher medical costs if not addressed; and (2) promote the benefits of value-based care through referrals of consumers looking to change or add a primary care physician. By offering more services to our Medicare carriers, we can improve the depth of our carrier relationships, open new revenue streams and build customer loyalty.
Provide Additional Products and Services Through Our Marketplace Technology
Our Founders and management team built our Marketplace technology over a 19-year period of continuous investment and growth. We have developed relationships with over 80 carriers and offer a wide variety of
142
Table of Contents
products and plans, including individual and family plans (which includes fixed indemnity and major medical plans), dental, vision, prescription drug and Medicare plans. Our Marketplace technology allows us to efficiently generate meaningful numbers of consumer submissions for health insurance plans, generate commission revenue streams based on Approved Submissions, and maximize the contribution margin of these commissions through efficiencies in CAC. Over the last two years, Medicare had the highest LTV/CAC of the health insurance plan products that we distribute through our Marketplace technology.
We have the technology, carrier, customer relationships and management team to broaden or shift our focus to other products if we think there is a revenue opportunity, and we have demonstrated this capability to add products historically. For example, after the enactment of the ACA, we significantly grew the IFP and Other segments revenue in a relatively short period of time, which we believe made us a leader in the ACA web-broker space.
Our Market and Trends Impacting the Industry
Demographic, consumer preference and regulatory factors are driving growth in the individual health insurance market. We service this market through the Medicare segments and the IFP and Other segments.
Medicare
Medicare enrollment is expected to grow significantly over the next 10 years as 10,000+ individuals turn 65 each day and become Medicare-eligible. The proportion of the population that is age 65 and older increased from 13% in 2010 to 15% in 2016 and is expected to reach 17% by 2020, according to the United States Census Bureau. As a result, Medicare enrollment is growing steadily, with the number of Medicare enrollees expected to grow from 59.9 million in 2018, to approximately 68.4 million in 2023 and 76.7 million by 2028. This growth in Medicare enrollment will increase the numbers of qualified prospects for our marketing efforts. Internet usage by individuals age 65 and older is also increasing, with 73% using the Internet in 2019 compared to 40% in 2009 according to the Pew Research Center. Seniors are also transacting more online, with 55% of people age 65 and older making online purchases monthly according to SheerID, and 63% of people age 65 and older obtained health information from a website, according to the 2018 BMC Health Services Research.
In addition to the growth in Medicare-eligible beneficiaries and higher online usage, the interest in Medicare-eligible individuals in private Medicare plans is expected to continue to increase. In 2019, 38% of all Medicare beneficiaries were enrolled in Medicare Advantage plans and between 2018 and 2019, total Medicare Advantage enrollment grew by about 1.5 million individuals or 7%. LEK Consulting estimated that Medicare Advantage penetration is likely to reach 50% penetration for all Medicare-eligible individuals by 2025 and could reach as high as 60% to 70% between 2030 and 2040. Compared to original Medicare, Medicare Advantage has lower annual healthcare costs and access to greater benefits, according to a 2019 Milliman report. In addition, we expect the increase in Medicare Advantage penetration to accelerate due to the COVID-19 pandemic because of increasing consumer preference for online and telephonic insurance enrollment as opposed to face-to-face consultations. The number of beneficiaries in SNPs also increased significantly in the last 10 years from 900,000 in 2009 to 2.5 million in 2019 providing additional opportunity for year-round sales outside of the open enrollment period and annual enrollment period. We believe the increased penetration of Medicare Advantage, as well as the growth of the number of Medicare-eligible individuals, will lead to increased submissions for marketplaces, such as ours in the future. Consumers choose Medicare Advantage plans around a specific criteria set which includes premium, total expected costs out of pocket, provider network composition, formulary coverage and supplemental benefits, which we believe are more efficiently addressed through a non-field-based distribution channel.
The growth in Medicare-eligible seniors and growing interest in private Medicare plans has led to an increase in plan choices. Nationwide, 3,148 Medicare Advantage plans will be available in 2020, an increase of 414 plans since 2019. The average beneficiary will be able to choose from among 28 health insurance plans in 2020, up
143
Table of Contents
from 18, five years ago. In addition to the increase in plan choices, the differences between health insurance plans has increased significantly. For 2019, CMS eliminated the meaningful difference requirement to improve competition, innovation and available benefit offerings and provide beneficiaries with affordable health insurance plans that are tailored to a consumer’s specific healthcare needs and financial situation. The types of supplemental benefits that health insurance plans cover increased in 2018, 2019 and 2020 and now cover transportation assistance, meal benefits, in-home support, telemonitoring, and caregivers support, among others. This growth in plan choices made education and assistance with plan selection more important for consumers and allows carriers to target specific Medicare Advantage plans with packages of benefits designed to be attractive to different segments of Medicare consumers. Marketplaces such as ours help educate consumers, and assist them in making informed plan choices. In addition, we specifically micro-target our marketing to precise populations to allow carriers to grow increasingly differentiated health insurance plans. This precise marketing is more difficult for traditional radio or television-based marketing channels.
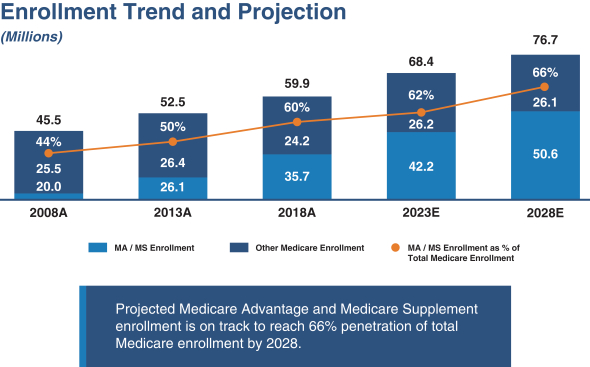
Source: CSG Actuarial (2019) and U.S. Department of Health and Human Services (2019).
Individual and Family Plans
After the passage of the ACA, the individual health insurance market grew from 10.6 million enrollees in 2013 to 17.4 million enrollees in 2015. Such increase was driven by (1) the requirement to purchase health insurance, or the individual mandate, (2) the requirement that carriers not consider pre-existing medical conditions in coverage decisions and (3) premium subsidies for middle and lower income individuals that were also contained in that legislation. With the repeal of the individual mandate in 2017 and broader economic trends, such as gains in employment, which increased the number of people having job-based coverage, the individual market has declined. Despite the decline, the individual market was composed of 13.8 million members in 2018, a meaningful increase from 2011 levels and in 2019, the market size stabilized with 13.7 million members enrolled. This market stabilization was driven by lower premium increases in 2019, as compared to 2018 and 2017 for individual insurance plans; an increase in individuals who do not receive job-based insurance due to the rise of “gig economy;” and, expanded plan options in the individual market from carriers. According to a Kaiser
144
Table of Contents
Family Foundation report published in 2020, in the third quarter of 2019, the average gross margin per member per month for carriers in the individual market was $131.17, as compared to $32.88 in the third quarter of 2016 shortly after the repeal of the individual mandate. This increased profitability for insurers is expected to have a positive impact on the individual market going forward. In addition, the number of individuals eligible for the individual market is growing. Forbes estimated that 57 million U.S. workers, approximately 36% of employees, are in the “gig economy” and many of these individuals will not receive health insurance through their jobs. We believe that growth in the individual market will benefit the Company in the future.
Carriers
We maintain longstanding, deeply integrated relationships with leading carriers in the United States, who have some of the industry’s most widely recognizable brands. For the year ended December 31, 2019 and the three month period ended March 31, 2020, the primary carriers that we served in the Medicare segments were carriers owned by Humana and Anthem, the primary carriers that we served in the IFP and Other segments were carriers owned by UnitedHealth Group. These high-quality relationships have resulted in strong carrier retention rates; since our inception, we have never had a carrier terminate for performance. We typically enter into contractual agency relationships with carriers that are non-exclusive and terminable on short notice by either party for any reason. Carriers often have the ability to terminate or amend our agreements unilaterally on short notice, including provisions in our agreements relating to our commission rates.
We believe carriers see our method of acquiring consumers as scalable and efficient and, ultimately, as cost-advantageous compared to their own models, and provide us, in some cases, with marketing development. The carriers are responsible for paying our commissions and, for these purposes, act as our customers. We do not currently generate revenues directly from the consumers to whom we sell insurance policies on behalf of carriers.
A core element of our value proposition to carriers relates to our ability to reliably place policies in compliance with applicable regulations and carrier-specific requirements. As such, we work closely with carriers to develop approved scripts and to undertake regular audits of our compliance with carrier requirements. In addition, our agents operate under compensation structures established to fully align their incentives with our compliance objectives.
Carriers owned by Humana and Anthem accounted for (i) approximately 40% and 20%, respectively, of net revenues for the Pro Forma Fiscal Year 2019 and 25% and 8%, respectively, of net revenues for the year ended December 31, 2018; (ii) approximately 51% and 23%, respectively, of Medicare—Internal segment revenue for the Pro Forma Fiscal Year 2019, and 63% and 15%, respectively, of Medicare—Internal segment revenue for the year ended December 31, 2018; and (iii) approximately 46% and 32%, respectively, of Medicare—External segment revenue for the Pro Forma Fiscal Year 2019, and 41% and 18%, respectively, of Medicare—External segment revenue for the year ended December 31, 2018. In addition, carriers owned by UnitedHealth Group represented approximately 27% and 11% of IFP and Other—Internal segment revenue for the Pro Forma Fiscal Year 2019 and for the year ended December 31, 2018, respectively, and 41% and 19% of IFP and Other—External segment revenue for the Pro Forma Fiscal Year 2019 and year ended December 31, 2018, respectively. See “Risk Factors—Risks Related to Our Business—We currently depend on a small group of carriers for a substantial portion of our revenue.”
We continue to focus on building out our carrier footprint in order to provide our consumers with a greater choice of health insurance plans. In 2020, we expect our platform will include Medicare Advantage products from at least one of the top two carriers, as measured by Medicare Advantage enrollees in each county, in 49 states, which collectively represented 95% of 2019 Medicare enrollments. In 2019, our platform included Medicare Advantage products from at least one of the top two carriers, as measured by Medicare Advantage enrollees in each county, in 24 states, which collectively represented 54% of 2019 Medicare enrollments.
145
Table of Contents
Technology
We have a technology culture that incentivizes the relentless improvement of every measurable point of the consumer experience. We harness our data, in unison with a deep investment in data expertise, to power key decision engines that scrutinize every step of the consumer journey and identify areas where technology and process-improvement investment will most impact our unit economics, including driving improvements in LTV/CAC. We operate dozens of proprietary technology systems, which support a data-driven consumer acquisition, service, and retention lifecycle within the health insurance market.
| • | Consumer Lead Acquisition. We acquire consumer leads through many channels, including paid Internet searches, television advertising, direct mail, affiliate sources, organic traffic from GoHealth.com and other channels. We use our streaming data systems to monitor CAC, the attributes and volume of consumer leads, the efficiency of the sales process, and historical performance benchmarks on a real-time basis. These systems allow our marketing team and automated marketing systems to make informed consumer lead acquisition decisions, resulting in lower CAC. Further, we have engineered our online lead generation forms that capture consumer leads to conduct high-volume testing of our consumer lead systems. Finally, our Consent Manager system ensures the capture of verifiable consent to call or text each consumer lead in compliance with the TCPA. |
| • | Lead Scoring. When consumers engage with us through the telephone or our website, our data systems capture attributes about the consumer, including the specific advertisement and channel that precipitated the consumer’s engagement. Our proprietary LeadScore technology applies a machine-learning model to years of historical consumer lead data we have gathered and their measured long-term outcomes to predict the expected LTV of all incoming consumer leads from the moment they connect with us. We use LeadScore to make several decisions throughout the sales process about how to optimize the routing of the consumer lead and what agents or agencies are best suited to serve each consumer. |
| • | Contact Queuing. We utilize our SPLICE system, a proprietary contact queue prioritized by LTV and throttled by an integrated monitor of agent capacity, to optimize outreach to our most valuable online consumer leads at a point in time when they can be connected to our agents with minimal wait time. |
| • | Outbound Contact and Qualification. Following SPLICE’s automated decision for consumer outreach, our automatic telephony system contacts the consumer and immediately places them on the phone with an agent, who gathers information to personalize the consumer’s sales experience, who we refer to as an Advocate. We also use the data gathered by our Advocates to improve the sales process by experimenting with the questions our Advocates ask and building data models of how consumers’ answers affect agent-consumer fit, consumer-product fit, CAC, LTV, and long-term customer satisfaction. |
| • | Lead Distribution. At the conclusion of the information-gathering process, and while the consumer is still on the phone, we use our proprietary lead auction system to make a health insurance market for the lead. External agencies participate in the auction along with our internal agency and programs, and present a pricing bid based on the consumer lead’s profile. We compete in the auction, winning the lead in the vast majority of cases, as our unit economics make typical consumer leads far more profitable for us to service than to distribute to external agencies. Our Assisted Live Transfer technology connects the call to the winner, via either warm (attended) transfer or cold (blind) transfer, dynamically chosen based on the availability of Advocates. |
| • | Optimized Call Routing. If the consumer lead is distributed from an Advocate further into our internal sales process, our CallRouter technology partitions the consumer leads into clusters based on lead and agent attributes. Each cluster is serviced by insurance agents with specialized licensing, training, experience, and performance characteristics tailored to that cluster. An agent can be assigned to one or more clusters, and each agent has a rank within each cluster to express the agent’s relative proficiency for servicing consumer leads in the cluster. Agent, consumer lead, and cluster performance data are |
146
Table of Contents
| continuously gathered and regularly analyzed by machine-learning experts and sales managers alike to ensure optimal call-routing. |
| • | Consumer Lead Management. As consumer leads are assigned and connected to agents, our BrokerOffice technology provides guidance to the agents on the most appealing value proposition to the consumer based on the information previously collected about the consumer. |
| • | Marketplace. After reviewing the consumer’s profile in BrokerOffice, the agent launches our Marketplace technology. Our Marketplace technology provides comparative shopping capabilities for all products available to the consumer in their geography and across carriers. It also ensures that while the agent has access to, and is able to compare, all products in the market, they only sell products for which they are appointed and licensed. The Marketplace has a growing set of decision support capabilities to guide the agent to the consumer’s ideal plan. For example, agents have the ability to look up each consumer’s providers and prescription drugs to compare their coverage inclusion and cost across plans. When the agent is ready to apply for a specific plan with the consumer, they may do so directly through the Marketplace. If the consumer requires time to consider the plan, the agent can send a personalized plan proposal either by email or SMS text message. Consumers can review proposals and enroll on their own directly from their phone, tablet, or computer. |
| • | Electronic Applications. We utilize proprietary domain-specific language for the rapid development and deployment of compliant electronic insurance applications. We ensure that insurance applications can be built and validated using standard, reusable modules wherever appropriate, while still being able to seamlessly integrate custom components as necessary. Completed applications are delivered directly to the corresponding carrier through custom integration partnerships. |
| • | Consumer Lifecycle Management. We receive application submission, commission, and book of business data regularly from each integrated carrier. We integrate this data with the other consumer data gathered throughout the consumer lifecycle to build a Retention Model using our machine-learning technology, which identifies consumers in need of engagement. Similar to many of our other systems, the Retention Model is continuously tested to increase performance and capability. We also use post-sale data from carriers to model how retention outcomes relate to consumer, marketing, and customer journey attributes so that every piece of our technology can be further optimized to maximize customer satisfaction and improve the sales process. |
| • | Monitoring. We have also developed several enabling and monitoring technologies to detect and automatically address anomalies and inefficiencies in our operations based on deviations from baseline norms, and to ensure that our operations are fully compliant. Agent calls are continuously monitored so that we automatically redact PCI from compliant call recordings in real time. Various network and agent performance metrics are tracked so that we can exert control over our advertising and sales operations. |
Agents
Since our inception, our highly skilled and trained licensed agents have enabled us to enroll millions of people in Medicare and individual and family plans. In 2019, we employed on average over 931 agents, reaching a high of 1,453 agents employed during the three months ended December 31, 2019. Our technology, lead distribution, and workflow allow agents to work in our Benefits Center or to work remotely at home, providing us with a sustainable avenue for growth.
Our agents benefit from a rigorous training program consisting of 6-8 weeks of classroom and interactive instruction prior to engaging with consumers. Our training courses cover insurance licensing, compliance requirements, customer service interactions, live role playing, and systems use. Most importantly, our trainings emphasize the GoHealth Way by prioritizing the trust and wellbeing of our customers above all else. We provide additional training on a regular basis to ensure our agents have the most up-to-date information regarding plan
147
Table of Contents
benefits, changing regulations, and best practices. We are continuously updating and improving agent training to drive increased agent efficiency. We have analyzed our most productive agents and revised our recruiting, training and onboarding processes to most closely match the skills and experiences of our most successful agents. The opportunity to reduce the variability in our agent performance is significant, as our top 25% of agents for the multi-carrier sales outlet of the Medicare—Internal segment on average are 61% more productive than the remaining 75% of our agents for the multi-carrier sales outlet of the Medicare—Internal segment, based on conversion rates of qualified prospects to Submitted Policies for the three months ended March 31, 2020. These top 25% of agents for the multi-carrier sales outlet of the Medicare—Internal segment achieved a 34% conversion rate of qualified prospects to Submitted Policies over the same three month period as compared to 21% conversion rate for the remaining 75% of our agents for the multi-carrier sales outlet of the Medicare—Internal segment over the same period.
We competitively compensate agents to incentivize their productivity, increase member retention, and improve customer satisfaction. In addition to paying each agent an hourly wage, we also compensate our agents through a structured bonus program. Our bonus program is designed to compensate agents based on the customer experience and plan lifetime. Customer experience is measured through a customer satisfaction survey. Plan lifetime is measured through policy issuance and retention.
Marketing
We employ data-driven, omni-channel marketing efforts to increase consumer phone calls and visits to our website and convert those calls and visits into customers. Our marketing initiatives include:
| • | Offline Media Marketing. Our offline media channel consists of branded advertisements run on television (both linear and over-the-top) and radio, as well as targeted direct mail campaigns. |
| • | Digital (Online) Media. Our digital media channel consists of branded advertisements run on paid search, display, native and social media platforms. These paid media efforts are supported by unpaid email and organic search campaigns. Our online advertising programs are delivered across all Internet-enabled devices, including desktop computers, tablet computers and smart phones. |
| • | Marketing Partners. Our marketing partner consumer acquisition channel consists of a network comprised of hundreds of partners that drive consumers to our e-commerce platform and Benefits Center. These partners include healthcare industry participants, such as insurance carriers, financial and online services partners in industries, such as banking and insurance, as well as affiliate organizations. |
Government Regulation and Compliance
The marketing and sale of insurance products and plans is a heavily regulated industry. Various aspects of our business are, may become, or may be viewed by regulators from time to time as subject, directly or indirectly, to U.S. federal, state and foreign laws and regulations. We are affected by laws and regulations that apply to businesses in general, the healthcare industry, and the insurance industry, as well as to businesses operating on the internet. This includes a continually expanding and evolving range of laws, regulations and standards that address financial services, information security, data protection, privacy and data collection and destruction, marketing of Medicare Advantage and other Medicare plans, healthcare compliance and fraud and abuse, among other things. We are also subject to laws governing marketing and advertising activities conducted by telephone, email, mobile devices and the internet. In addition, we are a licensed insurance producer in all 50 U.S. states and the District of Columbia. Insurance is highly regulated by the states in which we do business, and we are required to comply with and maintain various licenses and approvals. Regulatory authorities often have the discretion to grant, renew and revoke the various licenses and approvals we need to conduct our activities and, should we fail to retain our licenses, our business and results of operations could be adversely affected.
The Medicare segments are subject to regulations and guidelines issued by CMS that place a number of requirements on carriers, agents and brokers in connection with the marketing and sale of Medicare Advantage
148
Table of Contents
and Medicare Part D prescription drug plans. State insurance departments also regulate the marketing and sale of Medicare Supplement plans. CMS and state insurance department regulations and guidelines include a number of prohibitions regarding the ability to contact Medicare-eligible individuals and place many restrictions on the marketing of Medicare-related plans. For example, our carriers are required to file with CMS and state departments of insurance certain of our platforms, our call center scripts and other marketing materials we use to market Medicare-related plans. In some instances, CMS or state departments of insurance must approve the material before we use it. In addition, the laws and regulations applicable to the marketing and sale of Medicare-related plans are ambiguous, complex and, with respect to regulations and guidance issued by CMS for Medicare Advantage and Medicare Part D prescription drug plans, change frequently, and may do so as a result of the effects of the COVID-19 pandemic.
There are also numerous state and federal laws and regulations related to the privacy and security of health information. Laws in all 50 states require businesses to provide notices to affected individuals whose personal information has been disclosed as a result of a data breach, and certain states require notifications for data breaches involving individually identifiable health information. Most states require holders of personal information to maintain safeguards and take certain actions in response to a data breach, such as maintaining reasonable security measures and providing prompt notification of the breach to affected individuals and the state’s attorney general. In particular, regulations promulgated pursuant to the Health Insurance Portability and Accountability Act, or HIPAA, require us to maintain the privacy of individually-identifiable health information that we collect on behalf of carriers, implement measures to safeguard such information and provide notification in the event of a breach in the privacy or confidentiality of such information. If we were to be found to have breached our obligations under HIPAA, we could be subject to enforcement actions by the U.S. Department of Health and Human Services Office for Civil Rights (“OCR”) and state health regulators and lawsuits, including class action law suits, by private plaintiffs. In addition, OCR performs compliance audits in order to proactively enforce the HIPAA privacy and security standards. OCR has become an increasingly active regulator and has signaled its intention to continue this trend. OCR has the discretion to impose penalties without being required to attempt to resolve violations through informal means; further OCR may require companies to enter into resolution agreements and corrective action plans which impose ongoing compliance requirements. OCR enforcement activity can result in financial liability and reputational harm, and responses to such enforcement activity can consume significant internal resources. In addition to enforcement by OCR, state attorneys general are authorized to bring civil actions under either HIPAA or relevant state laws seeking either injunctions or damages in response to violations that threaten the privacy of state residents. Although we have implemented and maintained policies, processes and a compliance program infrastructure to assist us in complying with these laws and regulations and our contractual obligations, we cannot provide assurance regarding how these laws and regulations will be interpreted, enforced or applied to our operations. In addition to the risks associated with enforcement activities and potential contractual liabilities, our ongoing efforts to comply with evolving laws and regulations at the federal and state levels also might require us to make costly system purchases and/or modifications or otherwise divert significant resources to HIPAA compliance initiatives from time to time.
In addition, we have entered into contracts with carriers and others regarding the collection, maintenance, protection, use, transmission, disclosure or disposal of sensitive personal information. The use and disclosure of certain data that we collect from consumers are also regulated in some instances by other federal laws, including the Gramm-Leach-Bliley Act, or GLBA, and state statutes implementing GLBA, which generally require brokers to provide customers with notice regarding how their non-public personal health and financial information is used and the opportunity to “opt out” of certain disclosures before sharing such information with a third party, and which generally require safeguards for the protection of personal information. We regularly assess our compliance with privacy and security requirements.
These requirements are evolving, and states are beginning to adopt additional requirements, including California, where the CCPA took effect beginning January 1, 2020. The CCPA gives California residents expanded rights to access and delete their personal information, opt out of certain personal information sharing, and receive detailed information about how their personal information is used. The CCPA provides for civil penalties for violations,
149
Table of Contents
as well as a private right of action for data breaches that is expected to increase data breach litigation. In addition to government action, health insurance carrier expectations relating to privacy and security protections are increasing and evolving. We have incurred significant costs to develop new processes and procedures and to adopt new technology in an effort to comply with privacy and security laws and regulations and carrier expectations and to protect against cybersecurity risks and security breaches. We expect to continue to do so in the future. Violations of federal and state privacy and security laws and other contractual requirements may result in significant liability and expense, damage to our reputation or termination of relationship with government-run health insurance exchanges and our members, marketing partners and carriers.
Federal and state consumer protection laws are being applied increasingly by the Federal Trade Commission, or FTC, Federal Communications Commission, or FCC, and states’ attorneys general to regulate the collection, use, storage and disclosure of personal or health information, through websites or otherwise, and to regulate the presentation of website content. Courts may also adopt the standards for fair information practices promulgated by the FTC, which concern consumer notice, choice, security and access. Consumer protection laws require us to publish statements to our members that describe how we handle personal information and choices members may have about the way we handle personal information. If such information that we publish is considered untrue, we may be subject to government claims of unfair or deceptive trade practices, which could lead to significant liabilities and consequences.
New York’s cybersecurity regulation for financial services companies requires entities under the jurisdiction of NYDFS, including insurance entities, to establish and maintain a cybersecurity program designed to protect private consumer data. The Cybersecurity Model Law adopted by the NAIC is functionally similar to the NYDFS rule and is intended to establish the standards for data security and for the investigation and notification of data breaches applicable to insurance licensees in states adopting the law.
In addition, the United States regulates marketing and certain other communications by telephone and email, and individual states also impose restrictions on telephone marketing. The laws and regulations governing the use of emails and telephone calls for such purposes continue to evolve, and changes in technology, the marketplace or consumer preferences may lead to the adoption of additional laws or regulations or changes in interpretation of existing laws or regulations. The Telephone Consumer Protection Act and other federal and state laws prohibit companies from making telemarketing calls to numbers listed in the Federal Do-Not-Call Registry and impose other obligations and limitations on making phone calls and sending text messages to consumers. The CAN-SPAM Act regulates commercial email messages and specifies penalties for the transmission of commercial email messages that do not comply with certain requirements, such as providing an opt-out mechanism for stopping future emails from senders. We are required to comply with these and similar laws, rules and regulations.
Competition
The market for the distribution of health insurance products and plans is highly competitive, fragmented and evolving as purchasing behavior shifts from traditional field-based agent models towards digital and telephonic platforms. Our competition leverages a variety of channels including government-run health insurance exchanges, carrier-employed agents, field based independent agents and brokers, or platforms that distribute directly to the consumer digitally or telephonically. We aim to differentiate our products and services on the basis of our ability to match consumers with the insurance products that best match their needs by leveraging our carrier relationships, proprietary technology, machine-learning capabilities and extensive data, efficient business processes, and highly skilled and trained agents.
Government. We compete with the federal government’s original Medicare program in marketing Medicare insurance plans. CMS also offers Medicare-plan online enrollment, information and comparison tools, and has established call centers for the sale of Medicare Advantage and Medicare Part D prescription drug plans (collectively Medicare Plans). CMS has regulatory authority over Medicare Plans and can influence the
150
Table of Contents
competitiveness of Medicare Plans compared to the original Medicare program, as well as the compensation that health insurance carriers are allowed to pay to us.
Carrier-employed agents. Some health insurance carriers directly market and sell their plans to consumers through their own agents, call centers and websites. Although we offer health insurance plans for many of these carriers, they also compete with us by offering their plans directly to consumers. Most of these carriers have brand recognition, significant financial resources, and have become experienced in marketing their products to consumers through traditional and emerging channels.
Independent agents and brokers. We compete with thousands of local insurance agents and brokers across the United States who sell insurance products in their communities. While many of these agents offer health insurance products without significant utilization of advanced technology or the Internet, a number have embraced telesales or established websites providing an online shopping experience for consumers.
Internet marketers and telesales distribution platforms. There are many marketing companies and distribution platforms that use the Internet or telesales models to find consumers interested in purchasing health insurance and are compensated for referring those consumers to agents and carriers. We compete with these companies using similar business models to ours, such as eHealth, Inc. and SelectQuote Inc., for qualified prospects, sales, and carrier relationships.
Patents, Trademarks and Other Intellectual Property
We rely on a combination of copyright, trademark and trade secret laws as well as confidentiality procedures and contractual provisions to protect our proprietary software, including Marketplace, and our brands. We have registered or applied to register certain of our trademarks in the United States and several other countries. We also license intellectual property from third parties, including software that is incorporated in or bundled with our proprietary software applications. We generally control access to and use of our proprietary software and other confidential information through the use of internal and external controls, including entering into non-disclosure and confidentiality agreements with both our employees and third parties.
Employees
As of March 31, 2020, we employed 1,857 full-time employees, including 781 full time equivalent agents, and no part-time employees. We employed 1,810 people in the United States and 47 in Slovakia. During the Medicare annual enrollment period, we typically hire additional full time employees. None of our employees are represented by a labor union or are party to a collective bargaining agreement, and we have had no labor-related work stoppages. We believe that we have good relationships with our employees.
Facilities
Our principal executive offices are located in Chicago, Illinois. In addition to our principal executive offices, we operate from one additional office located in Chicago, Illinois and from offices located in Charlotte, North Carolina; Lindon, Utah; and Slovakia. We lease each of our offices.
For leases that are scheduled to expire during the next 12 months, we may negotiate new lease agreements, renew existing lease agreements or use alternate facilities. We believe that our facilities are adequate for our needs and believe that we should be able to renew any of our leases or secure similar property without an adverse impact on our operations.
Legal Proceedings
We are, from time to time, party to various claims and legal proceedings arising out of our ordinary course of business, but we do not believe that any of these claims or proceedings will have a material effect on our business, consolidated financial condition or results of operations.
151
Table of Contents
The following table provides information regarding our executive officers and members of our board of directors as of the date of this prospectus:
| Name |
Age | Position(s) | ||
| Clinton P. Jones |
42 | Co-Founder, Chief Executive Officer and Director | ||
| Brandon M. Cruz |
42 | Co-Founder, Chief Strategy Officer, Special Advisor to the Executive Team and Director | ||
| Shane E. Cruz |
40 | Chief Operating Officer | ||
| Travis J. Matthiesen |
36 | Chief Financial Officer | ||
| James A. Sharman |
61 | President | ||
| Rahm Emanuel |
60 | Director | ||
| Joseph G. Flanagan |
49 | Director | ||
| Jeremy W. Gelber |
44 | Director | ||
| Miriam A. Tawil |
35 | Director | ||
| Alexander E. Timm |
32 | Director |
Executive Officers
Clinton P. Jones is the co-founder of GoHealth and has served as GoHealth’s Chief Executive Officer since GoHealth’s founding in 2001. He has also been a member of GoHealth, Inc.’s board of directors since 2020 and a member of GoHealth Holdings, LLC’s board of managers since 2019, as well as serving on the board of managers of GoHealth’s predecessor since its founding in 2001. He also serves as member of the board of directors of Bridge Legal. From June 2000 to January 2001, Mr. Jones served as Intranet Market Manager for Holt Value, a former division of Credit Suisse. Mr. Jones speaks regularly at industry events and conferences. He is also active in insurance regulatory forums. In 2013, Mr. Jones was recognized by Ernst & Young as the Midwest Entrepreneur of the Year and was also named to the annual Chicago leadership list, Crain’s 40 under 40. Mr. Jones holds Bachelor of Science degrees in both Marketing and Management Information Systems from Miami University.
We believe Mr. Jones is qualified to serve on GoHealth, Inc.’s board of directors due to his extensive experience in the insurance industry and his knowledge of our business in particular, gained through his services as our co-founder and Chief Executive Officer.
Brandon M. Cruz is the co-founder of GoHealth and has served as GoHealth’s Chief Strategy Officer and Special Advisor to the Executive Team since 2020. Prior to this role, he served as President of GoHealth since its founding in 2001. He has also been a member of GoHealth, Inc.’s board of directors since 2020 and a member of GoHealth Holdings, LLC’s board of managers since 2019, as well as serving on the board of managers of GoHealth’s predecessor since its founding. From 1999 to 2000, Mr. Cruz worked at Lante Corp. as a systems developer. Mr. Cruz is recognized throughout the technology industry as an influential thought leader, and speaks regularly on topics related to technology, health insurance and business operations. He is a board member of the Young Presidents’ Organization and serves on the board of Homecare Holdings, HealthJoy, and Imerman Angels. Mr. Cruz has also served as a member of the board of directors of Creatix, Inc., our subsidiary, from 2016 to 2019. In 2013, Mr. Cruz was recognized by Ernst & Young as the Midwest Entrepreneur of the Year and was also named to the annual Chicago leadership list, Crain’s 40 under 40. Mr. Cruz holds a Bachelor of Science degree in Management Information Systems from Miami University, and is a member of the Miami University Business Advisory Council.
We believe Mr. Cruz is qualified to serve on GoHealth, Inc.’s board of directors due to his extensive experience in the insurance industry and his knowledge of our business in particular, gained through his services as our co-founder and Chief Strategy Officer and Special Advisor to the Executive Team.
152
Table of Contents
Shane E. Cruz has served as GoHealth’s Chief Operating Officer since 2020 and prior to that, was the Chief Technology Officer of GoHealth since 2014. Previously, Mr. Cruz served as GoHealth’s Senior Vice President of Technology from 2012 to 2014 and as Vice President of Technology from 2006 to 2012. Mr. Cruz also served as a member of the board of directors of HealthJoy, our affiliate, from 2014 to 2019 and as a member of the board of directors of Creatix, Inc., our subsidiary, from 2015 to 2019. Mr. Cruz holds Bachelor of Science degrees in Computer Science and Engineering and a Master of Engineering in Electrical Engineering and Computer Science from the Massachusetts Institute of Technology.
Travis J. Matthiesen has served as GoHealth’s Chief Financial Officer since 2018. Prior to serving as Chief Financial Officer, he served as GoHealth’s Vice President of Finance and Marketplace Operations from 2017 to 2018 and as GoHealth’s Corporate Controller from 2010 to 2017. He also served as a member of the board of directors of Creatix, Inc., our subsidiary, from 2018 to 2019. From 2006 to 2010, Mr. Matthiesen worked at the Assurance and Advisory Services Department of Ernst & Young LLP. Mr. Matthiesen holds a Master of Business Administration from the University of Notre Dame and a Bachelor of Science degree in Accounting from Cedarville University.
James A. Sharman has served as GoHealth’s President since 2020 and prior to that, was the Chief Operating Officer of GoHealth since 2018. Mr. Sharman was also appointed as a director of Spartan Motors Inc., which specializes in vehicle manufacturing and assembly for the commercial and retail vehicle industries, in February 2016 and has served as its Chairman since 2018. From 2015 through 2018, Mr. Sharman served as Chief Operating Officer of Coyote Logistics, a freight broker and logistics services provider and a wholly-owned subsidiary of United Parcel Service, Inc. From 2006 through 2014, Mr. Sharman served as Managing Partner of Truecast Capital, LLC, an investment firm. His work history includes President and Chief Executive Officer of World Kitchen, Inc. and Rubicon Technology, Inc. He was Senior Vice President of Global Supply Chain for CNH as well as Vice President and General Manager, Latin America, for the Case Corporation. He served as the Commanding Officer of an Engineering Company in the United States Army and was an Assistant Professor at the United States Military Academy at West Point. Mr. Sharman holds a Master of Business Administration from Duke University and Bachelor of Science degree in Engineering from the United States Military Academy at West Point.
Directors
Rahm Emanuel has served as a member of GoHealth, Inc.’s board of directors since 2020 and as a member of GoHealth Holdings, LLC’s board of managers since 2020. Mr. Emanuel has been Senior Counselor at Centerview Partners since 2019, served as Mayor of Chicago from 2011 to 2019, as White House Chief of Staff from 2009 to 2010, as Chairman of the House Democratic Caucus from 2007 to 2009 and as a member of the United States House of Representatives from Illinois’s 5th District from 2003 to 2009. From 2005 to 2007, Mr. Emanuel was the Chairman of the Democratic Congressional Campaign Committee. Mr. Emanuel worked at the investment bank Wasserstein Parella & Co. from 1998 to 2000 and served as a member of the board of directors of Freddie Mac from 2000 to 2001 and a member of the board of directors of the Chicago Mercantile Exchange from 1999 to 2001. Under President Clinton’s administration, Mr. Emanuel served as Senior Advisor to the President from 1992 to 1998. Mr. Emanuel holds a Bachelor of Arts degree from Sarah Lawrence College and a Master of Arts degree from Northwestern University.
We believe Mr. Emanuel is qualified to serve on GoHealth, Inc.’s board of directors due to his financial expertise and many years of leadership experience.
Joseph G. Flanagan has served as a member of GoHealth, Inc.’s board of directors since 2020 and as a member of GoHealth Holdings, LLC’s board of managers since 2020. Mr. Flanagan has also served as our President and Chief Executive Officer and as a member of the board of directors of R1 RCM Inc. (“R1”), a healthcare revenue cycle management company, since May 2016, after having served as R1’s President and Chief Operating Officer since April 2016. Mr. Flanagan joined R1 as Chief Operating Officer in April 2013 after serving as Senior Vice
153
Table of Contents
President of worldwide operations and supply chain at Applied Materials, Inc., a supplier of equipment, services and software for the manufacture of semiconductor chips for electronics, from 2010 to 2013, and as President of Nortel Business Services for Nortel Networks from 2009 to 2010. From 1993 to 2006, Mr. Flanagan worked for General Electric, holding leadership positions in many divisions. Mr. Flanagan holds a Bachelor of Science degree in Engineering from the United States Merchant Marine Academy.
We believe Mr. Flanagan is qualified to serve on GoHealth, Inc.’s board of directors due to his knowledge of the healthcare industry and extensive board experience.
Jeremy W. Gelber has served as a member of GoHealth, Inc.’s board of directors since 2020 and as a member of GoHealth Holdings, LLC’s board of managers since 2019. Mr. Gelber has been a Senior Managing Director of Centerbridge since 2018, where he focuses on investments in the healthcare sector, and has also served as a member of the board of directors of American Renal Associates Holdings, Inc. since 2020, Civitas Solutions, Inc. since 2019 and Remedi SeniorCare Holding Corporation since 2019. Prior to joining Centerbridge, Mr. Gelber was a Partner at Pamplona Capital, a private equity firm, and also served as Executive Director in the Healthcare Investment Banking Division at Morgan Stanley. Mr. Gelber holds a Bachelor of Science degree from Dartmouth College and a Doctor of Medicine degree from Jefferson Medical College.
We believe Mr. Gelber is qualified to serve on GoHealth, Inc.’s board of directors due to his knowledge of the healthcare industry, broad financial expertise and many years of leadership experience.
Miriam A. Tawil has served as a member of GoHealth, Inc.’s board of directors since 2020. Ms. Tawil has been a Managing Director of Centerbridge since 2012, where she focuses on investments in the healthcare and financial services sectors. Ms. Tawil also serves as a member of the board of directors of Civitas Solutions, Inc., Duo Bank of Canada and Remedi SeniorCare Holding Corporation. Prior to joining Centerbridge, Ms. Tawil was an associate at TPG Capital from 2008 to 2010 and an analyst in the Mergers and Acquisitions Group of The Blackstone Group L.P. from 2006 to 2008. Ms. Tawil holds a Bachelor of Arts from Harvard College and a Master in Business Administration degree from Harvard Business School.
We believe Ms. Tawil is qualified to serve on GoHealth, Inc.’s board of directors due to her extensive knowledge of the healthcare industry, broad financial expertise and years of leadership experience.
Alexander E. Timm has served as a member of GoHealth, Inc.’s board of directors since 2020 and as a member of GoHealth Holdings, LLC’s board of managers since 2020. Mr. Timm is also the Chief Executive Officer of Root Insurance Company, which he co-founded in 2015. Additionally, from 2011 to 2015, Mr. Timm worked at Nationwide Insurance as a senior consultant in corporate strategy. Mr. Timm holds a Bachelor of Science degree in Business Administration and a Bachelor of Arts degree in Actuarial Studies, Accounting and Mathematics from Drake University.
We believe Mr. Timm is qualified to serve on GoHealth, Inc.’s board of directors due to his extensive insurance industry experience, as well as his success in the entrepreneurial, tech, and data science industries.
Family Relationships
Brandon M. Cruz, our Co-Founder, Chief Strategy Officer and Special Advisor to the Executive Team and Director is the brother of Shane E. Cruz, our Chief Operating Officer. Otherwise, there are no family relationships among any of our executive officers or directors.
Composition of our Board of Directors
Our business and affairs are managed under the direction of our board of directors, which will consist of members upon consummation of the Transactions. Our amended and restated certificate of incorporation will
154
Table of Contents
provide that, subject to the rights of the holders of preferred stock, the number of directors on our board of directors shall be fixed exclusively by resolution adopted by our board of directors (provided that such number shall not be less than the aggregate number of directors that the parties to the Stockholders Agreement are entitled to designate from time to time). Our amended and restated certificate of incorporation and our amended and restated bylaws will provide that our board of directors will be divided into three classes, as nearly equal in number as possible, with the directors in each class serving for a three-year term, and one class being elected each year by our stockholders.
When considering whether directors have the experience, qualifications, attributes or skills, taken as a whole, to enable our board of directors to satisfy its oversight responsibilities effectively in light of our business and structure, the board of directors focuses primarily on each person’s background and experience as reflected in the information discussed in each of the directors’ individual biographies set forth above. We believe that our directors provide an appropriate mix of experience and skills relevant to the size and nature of our business.
Prior to the consummation of the Transactions, we will enter into the Stockholders Agreement with Centerbridge and our Founders, pursuant to which each party thereto will agree to vote, or cause to be voted, all of their outstanding shares of our Class A common stock and Class B common stock at any annual or special meeting of stockholders in which directors are elected, so as to cause the election of the Centerbridge Directors. Immediately following the consummation of the Transactions, Centerbridge will own shares of Class B common stock of GoHealth, Inc., which represents approximately % of the combined voting power of all of GoHealth, Inc.’s common stock. Our Founders will own shares of Class B common stock of GoHealth, Inc., which represents approximately % of the combined voting power of all of GoHealth, Inc.’s common stock. For a description of the terms of the Stockholders Agreement, see “Certain Relationships and Related Party Transactions—Stockholders Agreement.”
In accordance with our amended and restated certificate of incorporation and amended and restated bylaws, each of which will be in effect immediately prior to the consummation of the Transactions, our board of directors will be divided into three classes with staggered three year terms. At each annual meeting of stockholders after the initial classification, the successors to the directors whose terms will then expire will be elected to serve from the time of election and qualification until the third annual meeting following their election. Our directors will be divided among the three classes as follows:
| • | the Class I directors will be , and , and their terms will expire at the annual meeting of stockholders to be held in ; |
| • | the Class II directors will be , and , and their terms will expire at the annual meeting of stockholders to be held in ; and |
| • | the Class III directors will be , and , and their terms will expire at the annual meeting of stockholders to be held in . |
Any increase or decrease in the number of directors will be distributed among the three classes so that, as nearly as possible, each class will consist of one-third of the directors. This classification of our board of directors may have the effect of delaying or preventing changes in control of the Company. See “Description of Capital Stock—Anti-Takeover Provisions.”
Director Independence
Prior to the consummation of the Transactions, our board of directors undertook a review of the independence of our directors and considered whether any director has a relationship with us that could compromise that director’s ability to exercise independent judgment in carrying out that director’s responsibilities. Our board of directors has affirmatively determined that , and are each an “independent director,” as defined under the Nasdaq rules. In making these determinations, our board of directors considered the current
155
Table of Contents
and prior relationships that each director has with the Company and all other facts and circumstances our board of directors deemed relevant in determining his or her independence, including the beneficial ownership of our capital stock by each director, and the transactions involving them described in the section titled “Certain Relationships and Related Party Transactions.”
Controlled Company Exception
After the consummation of the Transactions, will have more than 50% of the combined voting power of our common stock. As a result, we will be a “controlled company” within the meaning of the corporate governance standards of the Nasdaq rules and intend to elect not to comply with certain corporate governance standards, including that: (1) a majority of our board of directors consists of “independent directors,” as defined under the Nasdaq rules; (2) we have a nominating and corporate governance committee that is composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities; (3) we have a compensation committee that is composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities; and (4) we perform annual performance evaluations of the nominating and corporate governance and compensation committees. We intend to rely on the foregoing exemptions provided to controlled companies under the Nasdaq rules. Therefore, immediately following the consummation of the Transactions, we may not have a majority of independent directors on our board of directors, an entirely independent nominating and corporate governance committee, an entirely independent compensation committee or perform annual performance evaluations of the nominating and corporate governance and compensation committees unless and until such time as we are required to do so. Accordingly, you may not have the same protections afforded to stockholders of companies that are subject to all of these corporate governance requirements. In the event that we cease to be a “controlled company” and our shares continue to be listed on the Nasdaq, we will be required to comply with these provisions within the applicable transition periods. See “Risk Factors—Risks Related to the Offering and Ownership of our Class A Common Stock—We are a “controlled company” within the meaning of the Nasdaq rules and, as a result, will qualify for, and intend to rely on, exemptions from certain corporate governance requirements. You may not have the same protections afforded to stockholders of companies that are subject to such corporate governance requirements.”
Committees of Our Board of Directors
Our board of directors directs the management of our business and affairs, as provided by Delaware law, and conducts its business through meetings of the board of directors and its standing committees. We will have a standing audit committee, nominating and corporate governance committee and compensation committee. In addition, from time to time, special committees may be established under the direction of the board of directors when necessary to address specific issues.
Audit Committee
Our audit committee will be responsible for, among other things:
| • | appointing, approving the fees of, retaining and overseeing our independent registered public accounting firm; |
| • | discussing with our independent registered public accounting firm their independence from management; |
| • | discussing with our independent registered public accounting firm any audit problems or difficulties and management’s response; |
| • | approving all audit and permissible non-audit services to be performed by our independent registered public accounting firm; |
| • | overseeing the financial reporting process and discussing with management and our independent registered public accounting firm the interim and annual financial statements that we file with the SEC; |
156
Table of Contents
| • | reviewing our policies on risk assessment and risk management; |
| • | reviewing related person transactions; and |
| • | establishing procedures for the confidential anonymous submission of complaints regarding questionable accounting, internal controls or auditing matters. |
Upon the consummation of the Transactions, our audit committee will consist of , and , with serving as chair. Rule 10A-3 of the Exchange Act and the Nasdaq rules require that our audit committee have at least one independent member upon the listing of our Class A common stock, have a majority of independent members within 90 days of the date of this prospectus and be composed entirely of independent members within one year of the date of this prospectus. Our board of directors has affirmatively determined that , and each meet the definition of “independent director” for purposes of serving on the audit committee under the Nasdaq rules and the independence standards under Rule 10A-3 of the Exchange Act and the Nasdaq rules. Each member of our audit committee meets the financial literacy requirements of the Nasdaq rules. In addition, our board of directors has determined that will qualify as an “audit committee financial expert,” as such term is defined in Item 407(d)(5) of Regulation S-K. Our board of directors will adopt a written charter for the audit committee, which will be available on our principal corporate website at www.gohealth.com substantially concurrently with the consummation of the Transactions. The information on any of our websites is deemed not to be incorporated in this prospectus or to be part of this prospectus.
Nominating and Corporate Governance Committee
Our nominating and corporate governance committee will be responsible for, among other things:
| • | identifying individuals qualified to become members of our board of directors, consistent with criteria approved by our board of directors as set forth in our corporate governance guidelines and in accordance with the terms of the Stockholders Agreement; |
| • | annually reviewing the committee structure of the board of directors and recommending to the board of the directors the directors to serve as members of each committee; and |
| • | developing and recommending to our board of directors a set of corporate governance guidelines. |
Upon the consummation of the Transactions, our nominating and corporate governance committee will consist of , and , with serving as chair. We intend to avail ourselves of the “controlled company” exception under the Nasdaq rules, which exempts us from the requirement that we have a nominating and corporate governance committee composed entirely of independent directors. , and do not qualify as “independent directors” under the Nasdaq rules. Our board of directors will adopt a written charter for the nominating and corporate governance committee, which will be available on our principal corporate website at www.gohealth.com substantially concurrently with the consummation of the Transactions. The information on any of our websites is deemed not to be incorporated in this prospectus or to be part of this prospectus.
Compensation Committee
Our compensation committee will be responsible for, among other things:
| • | reviewing and approving, or recommending that the board of directors approve, the compensation of our Chief Executive Officer and other executive officers; |
| • | making recommendations to the board of directors regarding director compensation; and |
| • | reviewing and approving incentive compensation and equity-based plans and arrangements and making grants of cash-based and equity-based awards under such plans. |
157
Table of Contents
Upon the consummation of the Transactions, our compensation committee will consist of , and , with serving as chair. We intend to avail ourselves of the “controlled company” exception under the Nasdaq rules, which exempts us from the requirement that we have a compensation committee composed entirely of independent directors. , and do not qualify as “independent directors” under the Nasdaq rules. Our board of directors will adopt a written charter for the compensation committee, which will be available on our principal corporate website at www.gohealth.com substantially concurrently with the consummation of the Transactions. The information on any of our websites is deemed not to be incorporated in this prospectus or to be part of this prospectus.
Risk Oversight
Our board of directors is responsible for overseeing our risk management process. Our board of directors focuses on our general risk management policies and strategy, the most significant risks facing us, and oversees the implementation of risk mitigation strategies by management. Our board of directors is also apprised of particular risk management matters in connection with its general oversight and approval of corporate matters and significant transactions.
Compensation Committee Interlocks and Insider Participation
None of the members of our compensation committee is or has been an officer or employee of the Company. None of our executive officers serves as a member of the board of directors or compensation committee (or other committee performing equivalent functions) of any entity that has one or more executive officers serving on our board of directors or compensation committee.
Code of Business Conduct and Ethics
Prior to the completion of the Transactions, we will adopt a written code of business conduct and ethics that applies to our directors, officers and employees, including our principal executive officer, principal financial officer, principal accounting officer or controller, or persons performing similar functions. A copy of the code will be posted on our website, www.gohealth.com. In addition, we intend to post on our website all disclosures that are required by law or the Nasdaq rules concerning any amendments to, or waivers from, any provision of the code. The information on any of our websites is deemed not to be incorporated in this prospectus or to be part of this prospectus.
158
Table of Contents
This section discusses the material components of the executive compensation program for our executive officers who are named in the “2019 Summary Compensation Table” below. For the year ended December 31, 2019, our “named executive officers” and their positions were as follows:
| • | Brandon M. Cruz, President (together with Clinton P. Jones, the co-principal executive officer); |
| • | Clinton P. Jones, Chief Executive Officer (together with Brandon M. Cruz, the co-principal executive officer); |
| • | Shane E. Cruz, Chief Technology Officer; and |
| • | James A. Sharman, Chief Operating Officer. |
This discussion may contain forward-looking statements that are based on our current plans, considerations, expectations and determinations regarding future compensation programs. Actual compensation programs that we adopt following the completion of the IPO may differ materially from the currently planned programs summarized in this discussion. As an “emerging growth company” as defined in the JOBS Act, we are not required to include a Compensation Discussion and Analysis section and have elected to comply with the scaled disclosure requirements applicable to emerging growth companies.
2019 Summary Compensation Table
The following table sets forth information concerning the compensation of our named executive officers for the year ended December 31, 2019.
| Name and Principal |
Year | Salary ($) | Stock Awards ($) (1) |
Non-Equity Incentive Plan Compensation ($) (2) |
All Other Compensation ($) |
Total ($) | ||||||||||||||||||
| Brandon M. Cruz |
2019 | 325,000 | 4,343,304 | 350,000 | 5,893 | (3) | 5,024,197 | |||||||||||||||||
| President |
||||||||||||||||||||||||
| Clinton P. Jones |
2019 | 325,000 | 4,343,304 | 350,000 | 5,893 | (3) | 5,024,197 | |||||||||||||||||
| Chief Executive Officer |
||||||||||||||||||||||||
| Shane E. Cruz |
2019 | 300,000 | 1,737,322 | 350,000 | 8,657,748 | (4) | 11,045,070 | |||||||||||||||||
| Chief Technology Officer |
||||||||||||||||||||||||
| James A. Sharman |
2019 | 400,000 | 1,737,322 | 700,000 | 15,136,805 | (5) | 17,974,127 | |||||||||||||||||
| Chief Operating Officer |
||||||||||||||||||||||||
| (1) | Amounts reflect the aggregate grant date fair value of profits interests granted during the year ended December 31, 2019 computed in accordance with FASB ASC Topic 718, Compensation—Stock Compensation. See Note 8 of the audited consolidated financial statements included elsewhere in this prospectus for a discussion of the relevant assumptions used in calculating these amounts. The amounts reported in this column reflect the aggregate grant date fair value for the profits interests as determined for financial accounting purposes and do not correspond to the actual economic value that may be received by the named executive officers from these awards. With respect to all performance-vesting awards granted in the year ended December 31, 2019, the value was calculated using a Monte-Carlo simulation model. Under ASC 718, the vesting condition related to the profits interests is considered a market condition and not a performance condition. Accordingly, there is no grant date fair value below or in excess of the amount reflected in the table above for the profits interests that could be calculated and disclosed based on achievement of the underlying market condition. |
159
Table of Contents
| (2) | Amounts reflect annual cash performance-based bonuses earned during the year ended December 31, 2019. For additional information about the annual cash performance-based bonuses, please see the section titled “2019 Bonuses” below. |
| (3) | Amount reflects (i) $293 in life and accidental death and dismemberment, or AD&D, insurance premiums; and (ii) $5,600 in matching contributions under the Company’s 401(k) plan. |
| (4) | Amount reflects (i) $270 in life and AD&D insurance premiums; (ii) $5,600 in matching contributions under the Company’s 401(k) plan; (iii) a $716,725 distribution payment made to Mr. Cruz in connection with the Centerbridge Acquisition in respect of NVX Holdings, Inc. phantom stock held by Mr. Cruz at the time of the distribution payment, and which Mr. Cruz continued to hold thereafter, and (iv) a $7,935,153 change in control payment made to Mr. Cruz in exchange for (and as the result of a modification of) his Norvax, LLC Class C Units in connection with the Centerbridge Acquisition. |
| (5) | Amount reflects (i) $293 in life and AD&D insurance premiums and (ii) a $15,136,512 change in control payment made to Mr. Sharman in exchange for (and as the result of a modification of) his Norvax, LLC Class C Units in connection with the Centerbridge Acquisition. |
2019 Salaries
The named executive officers receive a base salary to compensate them for services rendered to the Company. The base salary payable to each named executive officer is intended to provide a fixed component of compensation reflecting the executive’s skill set, experience, role and responsibilities. Base salaries were not changed for the year ended December 31, 2019.
In connection with this offering, we expect that our executive compensation program will evolve to reflect our status as a newly publicly-traded company, while still supporting our overall business and compensation objectives. In connection with this offering, management has retained Pearl Meyer, an independent executive compensation consultant, to help advise on our post-offering executive compensation program.
2019 Bonuses
The Company provides annual incentive cash bonuses, which we refer to as “Annual Bonuses,” to its named executive officers under its 2019 Executive Compensation and Bonus Plan, which we refer to as the “Annual Bonus Plan.” Under the Annual Bonus Plan, Annual Bonuses are determined based on achievement of Company revenue and EBITDA targets. Company targets are generally established by the Board in its discretion during the first quarter of the fiscal year.
Annual Bonuses are generally paid after the end of the fiscal year in which they were earned, with any payments occurring prior to the completion of our annual audit reconciled after the completion of the annual audit. In the event Company revenue or EBITDA falls below 80% of the pre-established target in any given year, no Annual Bonus is paid in respect of that target. For the fiscal year ended December 31, 2019, 60% of each named executive officer’s Annual Bonus was based on the Company’s EBITDA performance and 40% of each named executive officer’s Annual Bonus was based on the Company’s revenue performance.
Annual Bonus amounts are based on individualized target amounts for the applicable year, with ultimate payouts ranging from 20% to 200% of these individualized targets. For the fiscal year ended December 31, 2019, the target Annual Bonus amounts for Brandon M. Cruz, Clinton P. Jones, and Shane E. Cruz were $175,000 and the target Annual Bonus amount for James A. Sharman was $350,000. For the fiscal year ended December 31, 2019, Annual Bonuses were paid out at 200% of target, resulting in Annual Bonuses of $350,000 each for Brandon M. Cruz, Clinton P. Jones, and Shane E. Cruz and $700,000 for James A. Sharman.
Share-Based Compensation
Our named executive officers currently hold profits interests in Blizzard Management Feeder, LLC. We refer to these profits interests as “Incentive Units.” Specifically, in the fiscal year ended December 31, 2019, Brandon M.
160
Table of Contents
Cruz and Clinton P. Jones were each granted 12,239,764 Incentive Units and Shane E. Cruz and James A. Sharman were each granted 4,895,906 Incentive Units, as set forth below. The Incentive Units are divided approximately one-third and two-thirds between Service Units, which generally vest in equal annual installments over five years, and Performance Units, which generally vest subject to satisfaction of performance-vesting targets, respectively.
In connection with this offering, we intend to adjust the vesting of Performance Units. Under such modification, satisfaction of the Performance Units’ performance-vesting targets will be measured against the initial public offering price of this offering, after which one-third (1/3) of those Performance Units that have satisfied their performance-vesting targets based on such measurement will vest six (6) months after the effective date of this prospectus and the remaining two-thirds (2/3) of the Performance Units that have satisfied their performance-vesting targets based on such measurement will vest eighteen (18) months after the effective date of this prospectus.
Further, in connection with this offering, we intend to exchange each Incentive Unit for common units of Blizzard Management Feeder, LLC, which we refer to as “Management Common Units,” on a “value-for-value” basis based on the fair market value of the Incentive Units at the time of the offering and the common stock price in the offering. Following this conversion, the Management Common Units which are Service Units will be subject to the same vesting conditions as well as all other terms and conditions applicable to the Incentive Units which are Service Units under the existing Incentive Unit award agreements. Following this conversion, the Management Common Units which are Performance Units will be subject to the modified vesting conditions described above. For additional information about the profits units to which the Incentive Units correspond, please see the section titled “Profits Unit Plan” below.
Under the documentation of the Incentive Units in effect as of December 31, 2019, the vesting of all Service Units is generally subject to acceleration upon the occurrence of certain corporate transactions or the holder’s death or disability, and a pro-rata portion of the Service Units are generally subject to acceleration upon the holder’s termination of employment by the Company without Cause (as such term is defined in the Incentive Unit plan document) or by the holder with Good Reason (to the extent such term is defined in the named executive officer’s services agreement with the Company, which agreements are described under the section titled “Executive Compensation Arrangements” below), and the vesting of the Performance Units is based on achieving specified multiples of invested capital by Centerbridge, subject to the named executive officer’s continuous employment through the applicable vesting date. Additionally, in the event a named executive officer is terminated without Cause or as a result of death or disability or resigns for Good Reason, and any event occurs during the six-month period following the date of such termination that would have otherwise caused any unvested Incentive Units to become vested if the named executive officer had remained employed through the date of such event, then such unvested Incentive Units that would have become vested in connection with such event shall vest as though the named executive officer had remained employed during such period. The Compensation Committee of GoHealth Holdings, LLC, as the administrator of the Incentive Unit plan, has the discretion to accelerate the vesting of any Incentive Units, all Incentive Units, or any class of Incentive Units at any time and from time to time.
The Incentive Unit plan document assigns to “Cause” the definition in the applicable participant’s employment or services agreement with the Company, or, in the absence of such an employment or services agreement, the meaning set forth in the Company’s operating agreement, which defines “Cause” as (i)(A) the willful failure or refusal to perform material responsibilities that have been reasonably requested by the Board; (B) dishonesty to the Board with respect to any material matter; or (C) misappropriation of funds or property of the Company or any of its subsidiaries or affiliates other than the occasional, customary and de minimis use of Company property for personal purposes; provided, in the case of each of clause (i)(A)-(C), that, where the Company has determined reasonably and in good faith that such act can reasonably be cured, the Company has provided 30 days’ prior written notice of such conduct and such conduct is not cured within such 30 day period; (ii) the arrest or charging for (A) any felony or (B) a misdemeanor involving moral turpitude, deceit, dishonesty or fraud; (iii) the engagement in on-the-job conduct that consists either of gross misconduct or a material violation of the
161
Table of Contents
Company or any of its subsidiaries’ written code of ethics or company policies, and which is materially detrimental to the Company and its subsidiaries (including material reputational harm); or (iv) a breach of a non-competition covenant set forth in an employment agreement or restrictive covenants agreement.
The following table sets forth the Incentive Units granted to our named executive officers in the fiscal year ended December 31, 2019.
| Named Executive Officer |
2019 Incentive Units Granted |
|||
| Brandon M. Cruz |
12,239,764 | |||
| Clinton P. Jones |
12,239,764 | |||
| Shane E. Cruz |
4,895,906 | |||
| James A. Sharman |
4,895,906 | |||
We intend to adopt a 2020 Incentive Award Plan in order to facilitate the grant of cash and equity incentives to directors, employees (including our named executive officers) and consultants of our company and certain of its affiliates and to enable our company and certain of its affiliates to obtain and retain services of these individuals, which we believe is essential to our long-term success. We expect that the 2020 Incentive Award Plan will be effective prior to the effectiveness of this offering. For additional information about the 2020 Incentive Award Plan, please see the section titled “New Incentive Plans” below.
Other Elements of Compensation
Retirement Plans
We maintain a 401(k) retirement savings plan for our employees, including our named executive officers, who satisfy certain eligibility requirements. The Internal Revenue Code allows eligible employees to defer a portion of their compensation, within prescribed limits, on a pre-tax basis through contributions to the 401(k) plan. Currently, we match 50% of contributions made by participants in the 401(k) plan up to 4% of participant compensation (for a maximum match of 2% of participant compensation), and these matching contributions vest in equal annual installments over four years. We also may make non-elective contributions to the 401(k) plan, which, if made, vest 20% after two years and 20% annually thereafter. We believe that providing a vehicle for tax-deferred retirement savings though our 401(k) plan, and making matching and non-elective contributions, adds to the overall desirability of our executive compensation package and further incentivizes our employees, including our named executive officers, in accordance with our compensation policies.
Employee Benefits and Perquisites
Health/Welfare Plans. All of our full-time employees, including our named executive officers, are eligible to participate in our health and welfare plans, including:
| • | medical, dental and vision benefits; |
| • | medical and dependent care flexible spending accounts; |
| • | short-term and long-term disability insurance; |
| • | life insurance; |
| • | commuter benefits; and |
| • | an employee assistance program. |
We believe the benefits described above are necessary and appropriate to provide a competitive compensation package to our employees, including our named executive officers. During the year ended December 31, 2019, we did not provide any perquisites to our employees.
162
Table of Contents
No Tax Gross-Ups
We do not make gross-up payments to cover our named executive officers’ personal income taxes that may pertain to any of the compensation or benefits paid or provided by our Company.
Outstanding Equity Awards at 2019 Fiscal Year-End
The following table summarizes the number of Incentive Units underlying outstanding equity incentive plan awards for each named executive officer as of December 31, 2019.
| Incentive Unit Awards | ||||||||||||||||||||
| Name |
Grant Date | Number of Service Incentive Units That Have Not Vested (#) (1) |
Market Value of Service Incentive Units That Have Not Vested ($) (2) |
Number of Unearned Performance Incentive Units That Have Not Vested (#) (3) |
Market Value of Unearned Performance Incentive Units That Have Not Vested ($) (2) |
|||||||||||||||
| Brandon M. Cruz |
October 3, 2019 | 4,039,122 | 1,986,440 | 8,200,642 | 2,356,864 | |||||||||||||||
| Clinton P. Jones |
October 3, 2019 | 4,039,122 | 1,986,440 | 8,200,642 | 2,356,864 | |||||||||||||||
| Shane E. Cruz |
October 3, 2019 | 1,615,649 | 794,576 | 3,280,257 | 942,746 | |||||||||||||||
| James A. Sharman |
October 3, 2019 | 1,615,649 | 794,576 | 3,280,257 | 942,746 | |||||||||||||||
| (1) | Represents Service Units that vest in five equal annual installments on each of the first through fifth anniversaries of September 13, 2019, subject to the named executive officer’s continuous employment through the applicable vesting date. The vesting of all Service Units is generally subject to acceleration upon the occurrence of certain corporate transactions or the holder’s death or disability, and a pro-rata portion of the Service Units are generally subject to acceleration upon the holder’s termination of employment by the Company without Cause (as such term is defined in the Incentive Unit plan document) or by the holder with Good Reason (as such term is defined in the applicable participant’s services agreement with the Company). |
| (2) | The profits interests are not publicly traded and, therefore, there was no ascertainable public market value for the profits interests as of December 31, 2019. Therefore, the profits interests have been valued on the basis set forth in Footnote 1 of the 2019 Summary Compensation Table, above. |
| (3) | Represents Performance Units that vest subject to satisfaction of performance-vesting targets. |
Executive Compensation Arrangements
Our named executive officers’ employment and non-compete agreements are described below. Additionally, in connection with this offering, we intend to enter into new employment agreements with each of our named executive officers. The material terms of the new employment agreements have not yet been determined; once determined, the material terms of the new employment agreements will be disclosed in a future filing.
Brandon M. Cruz Non-Compete Agreement
Mr. Cruz entered into a Non-Disclosure, Invention Assignment, Non-Competition and Non-Solicitation Agreement with the Company, which we refer to as a “Non-Competition Agreement,” prior to commencing employment, under which he is subject to a covenant not to compete with the Company and a covenant not to solicit employees or customers of the Company, in each case for two years after the termination of Mr. Cruz’s employment with the Company. The Non-Competition Agreement also includes an invention assignment covenant and a covenant not to disclose any confidential information of the Company or any of its affiliates at all times following a termination of Mr. Cruz’s employment for any reason.
Mr. Cruz’s Incentive Units are subject to accelerated vesting as described in the section titled “Equity Compensation,” above. Mr. Cruz is not subject to any compensation arrangement entitling him to severance benefits upon a termination of employment or change in control occurring as of December 31, 2019.
163
Table of Contents
Clinton P. Jones Non-Compete Agreement
Mr. Jones entered into a Non-Competition Agreement with the Company prior to commencing employment, under which he is subject to a covenant not to compete with the Company and a covenant not to solicit employees or customers of the Company, in each case for two years after the termination of Mr. Jones’ employment with the Company. The Non-Competition Agreement also includes an invention assignment covenant and a covenant not to disclose any confidential information of the Company or any of its affiliates at all times following a termination of Mr. Jones’ employment for any reason.
Mr. Jones’ Incentive Units are subject to accelerated vesting as described in the section titled “Equity Compensation,” above. Mr. Jones is not subject to any compensation arrangement entitling him to severance benefits upon a termination of employment or change in control occurring as of December 31, 2019.
Shane E. Cruz Offer Letter
On June 7, 2012, Mr. Cruz commenced employment with the Company under an employment offer letter entered into in connection with his hiring as the Company’s Vice President of Technology, as amended on April 3, 2018 and which continued to govern his employment as the Company’s Chief Technology Officer for the year ended December 31, 2019. Mr. Cruz’s offer letter provides for a base salary, eligibility to participate in the Annual Bonus Plan, and participation in the Company’s standard benefit plans. Mr. Cruz’s offer letter has no fixed term.
If Mr. Cruz’s employment is terminated by the Company without cause, Mr. Cruz will receive from the Company four months’ severance pay based on his base salary on the date of such termination.
Pursuant to the terms of his offer letter, Mr. Cruz also entered into a Non-Competition Agreement with the Company prior to commencing employment, under which he is subject to a covenant not to compete with the Company and a covenant not to solicit employees or customers of the Company, in each case for two years after the termination of Mr. Cruz’s employment with the Company. The Non-Competition Agreement also includes an invention assignment covenant and a covenant not to disclose any confidential information of the Company or any of its affiliates at all times following a termination of Mr. Cruz’s employment for any reason.
Mr. Cruz’s Incentive Units are subject to accelerated vesting as described in the section titled “Equity Compensation,” above.
James A. Sharman Offer Letter
On February 5, 2018, Mr. Sharman commenced employment with the Company under an employment offer letter dated December 21, 2017 entered into in connection with his hiring as the Company’s Chief Operating Officer, which continued to govern his employment for the year ended December 31, 2019. Mr. Sharman’s offer letter provides for a base salary, eligibility to participate in the Annual Bonus Plan, eligibility to receive a profits interest grant, and participation in the Company’s standard benefit plans. Mr. Sharman’s offer letter has no fixed term.
If Mr. Sharman’s employment is terminated by the Company without Cause or by Mr. Sharman for Good Reason, Mr. Sharman will receive from the Company (i) six months’ severance pay based on his base salary rate on the date of such termination, to be paid in accordance with normal payroll practices beginning on the first payroll date after the 60th day following such termination and (ii) a pro-rata Annual Bonus based on the number of days during the calendar year in which Mr. Sharman is employed with the Company, in each case subject to Mr. Sharman’s execution of a release of claims in favor of the Company and his compliance with the covenants and restrictions in his Non-Compete Agreement, described below. Additionally, upon Mr. Sharman’s death or disability, Mr. Sharman will receive from the Company the pro-rated Annual Bonus described above.
164
Table of Contents
Pursuant to the terms of his offer letter, Mr. Sharman also entered into a Non-Competition Agreement with the Company prior to commencing employment, under which he is subject to a covenant not to compete with the Company and a covenant not to solicit employees or customers of the Company, each for two years after the termination of Mr. Sharman’s employment with the Company. The Non-Competition Agreement also includes an invention assignment covenant and a covenant to not disclose any confidential information of the Company or any of its affiliates at all times following a termination of Mr. Sharman’s employment for any reason.
Mr. Sharman’s offer letter defines “Cause” as (i) Mr. Sharman’s gross negligence in the performance of his duties and responsibilities to the Company or any of its affiliates, or refusal or failure to follow or carry out any reasonable, written direction of the board of directors of the Company; (ii) a material breach by Mr. Sharman of any provision of his offer letter or Non-Competition Agreement that, if capable of cure, is not cured within 30 days of written notice of such breach by the Company to Mr. Sharman, provided, that the Company will not have to provide more than one notice and opportunity to cure with respect to any multiple, repeated, related or substantially similar events or circumstances; (iii) the commission of fraud, embezzlement, theft or other material dishonesty by Mr. Sharman; (iv) the commission by Mr. Sharman of, or plea by the executive of nolo contendere to, any felony or any other crime involving dishonesty or moral turpitude; or (v) any other conduct by Mr. Sharman that involves a material breach of fiduciary obligations on his part or otherwise could reasonably be expected to have a significant adverse effect upon the business, interests or reputation of the Company or any of its affiliates.
Mr. Sharman’s offer letter defines, “Good Reason” as, without Mr. Sharman’s written consent, (i) a material reduction in Mr. Sharman’s salary which is not cured within 90 days following the Company’s receipt of written notice thereof from Mr. Sharman; (ii) a change in Mr. Sharman’s principal place of employment to outside of a 50 mile radius of Chicago, Illinois; (iii) a material adverse change in Mr. Sharman’s title, authority, duties, or responsibilities which is not cured within 90 days following the Company’s receipt of written notice thereof from Mr. Sharman; or (iv) any breach by the Company of any other material provision of Mr. Sharman’s offer letter, which breach is not cured within 30 days following Company’s receipt of written notice thereof from Mr. Sharman.
Mr. Sharman’s Incentive Units are subject to accelerated vesting as described in the section titled “Equity Compensation,” above.
2019 Director Compensation
None of our non-employee directors received any compensation for his or her service as a non-employee director during the year ended December 31, 2019 and none of our non-employee directors held Incentive Units (vested or unvested) as of December 31, 2019. In connection with this offering, we intend to adopt a new compensation program for our non-employee directors.
Parent Unit Plan
The Incentive Units held by our named executive officers correspond to profits units issued under the GoHealth Holdings, LLC Profits Unit Plan, which we refer to as the “Parent Unit Plan,” to Blizzard Management Feeder, LLC. We refer to such units issued under the Parent Unit Plan as “Parent Units.” Parent Units and corresponding Incentive Units are issued under the same grant agreements, are subject to the same vesting conditions, and any changes to Parent Units flow through to the corresponding Incentive Units. Under the Parent Unit Plan, any acceleration of Parent Units upon a termination of employment is governed by the applicable award agreement. Additionally, GoHealth Holdings, LLC may make modifications to the Parent Unit Plan and any outstanding Parent Units as it determines to be necessary or appropriate in connection with an initial public offering. In connection with this offering, GoHealth Holdings, LLC intends to use its discretion to convert each outstanding Parent Unit into a common unit of GoHealth Holdings, LLC, which will cause a corresponding conversion of all outstanding Incentive Units into common units of Blizzard Management Feeder, LLC, as described in the section titled “Equity Compensation” above.
165
Table of Contents
New Incentive Plans
2020 Incentive Award Plan
We intend to adopt the 2020 Incentive Award Plan, or the 2020 Plan, subject to approval by our stockholders, under which we may grant cash and equity incentive awards to eligible employees and other service providers in order to attract, motivate and retain the talent for which we compete. The material terms of the 2020 Plan, as it is currently contemplated, are summarized below. Our board of directors is still in the process of developing, approving and implementing the 2020 Plan and, accordingly, this summary is subject to change.
Eligibility and Administration. Our employees, consultants and directors, and the employees, consultants and directors of our parents and affiliates, will be eligible to receive awards under the 2020 Plan. Following our initial public offering, the 2020 Plan will be administered by our board of directors with respect to awards to non-employee directors and by our compensation committee with respect to other participants, each of which may delegate its duties and responsibilities to committees of our directors and/or officers (referred to collectively as the “plan administrator” below), subject to certain limitations that may be imposed under the 2020 Plan, Section 16 of the Exchange Act, and/or stock exchange rules, as applicable. The plan administrator will have the authority to make all determinations and interpretations under, prescribe all forms for use with, and adopt rules for the administration of, the 2020 Plan, subject to its express terms and conditions. The plan administrator will also set the terms and conditions of all awards under the 2020 Plan, including any vesting and vesting acceleration conditions.
Limitation on Awards and Shares Available.. An aggregate of shares of our common stock will initially be available for issuance under the 2020 Plan. The number of shares initially available for issuance will be increased by an annual increase on January 1 of each calendar year beginning in 2021 and ending in and including 2030, equal to the lesser of (A) % of the shares of our common stock outstanding on the final day of the immediately preceding calendar year and (B) a smaller number of shares as determined by our board of directors. No more than shares of common stock may be issued under the 2020 Plan upon the exercise of incentive stock options. Shares available under the 2020 Plan may be authorized but unissued shares, shares purchased on the open market or treasury shares.
If an award under the 2020 Plan is forfeited, expires or is settled for cash, any shares subject to such award may, to the extent of such forfeiture, expiration or cash settlement, be used again for new grants under the 2020 Plan. However, the following shares may not be used again for grant under the 2020 Plan: (i) shares tendered or withheld to satisfy grant or exercise price or tax withholding obligations associated with an award; (ii) shares tendered or withheld to satisfy any tax withholding obligation with respect to an award; (iii) shares subject to a stock appreciation right, or SAR, or other stock-settled award that are not issued in connection with the stock settlement of the stock appreciation right or other stock-settled award on its exercise; and (iv) shares purchased on the open market with the cash proceeds from the exercise of options.
Awards granted under the 2020 Plan upon the assumption of, or in substitution for, outstanding equity awards previously granted by an entity in connection with a corporate transaction, such as a merger, combination, consolidation or acquisition of property or stock, will not reduce the shares available for grant under the 2020 Plan.
The 2020 Plan provides that the sum of any cash compensation and the aggregate grant date fair value (determined as of the date of the grant under Financial Accounting Standards Board Accounting Standards Codification Topic 718, or any successor thereto) of all awards granted to a non-employee director pursuant to the 2020 Plan as compensation for services as a non-employee director during any calendar year shall not exceed the amount equal to $ (with such amount increased to $ for the calendar year of a non-employee director’s initial service). The plan administrator may make exceptions to this limit for individual non-employee directors in extraordinary circumstances, as the plan administrator may determine in its discretion, provided that the non-employee director receiving such additional compensation may not participate in the
166
Table of Contents
decision to award such compensation or in other contemporaneous compensation decisions involving non-employee directors.
Awards. The 2020 Plan provides for the grant of stock options, including incentive stock options, or ISOs, and nonqualified stock options, or NSOs, restricted stock, dividend equivalents, stock payments, restricted stock units, or RSUs, other incentive awards, stock appreciation rights, or SARs, and cash awards. No determination has been made as to the types or amounts of awards that will be granted to specific individuals pursuant to the 2020 Plan. Certain awards under the 2020 Plan may constitute or provide for a deferral of compensation, subject to Section 409A of the Internal Revenue Code, which may impose additional requirements on the terms and conditions of such awards. All awards under the 2020 Plan will be set forth in award agreements, which will detail all terms and conditions of the awards, including any applicable vesting and payment terms and post-termination exercise limitations. Awards other than cash awards generally will be settled in shares of our common stock, but the plan administrator may provide for cash settlement of any award. A brief description of each award type follows.
| • | Stock Options. Stock options provide for the purchase of shares of our common stock in the future at an exercise price set on the grant date. ISOs, by contrast to NSOs, may provide tax deferral beyond exercise and favorable capital gains tax treatment to their holders if certain holding period and other requirements of the Internal Revenue Code are satisfied. The exercise price of a stock option may not be less than 100% of the fair market value of the underlying share on the date of grant (or 110% in the case of ISOs granted to certain significant stockholders), except with respect to certain substitute options granted in connection with a corporate transaction. The term of a stock option may not be longer than ten years (or five years in the case of ISOs granted to certain significant stockholders). Vesting conditions determined by the plan administrator may apply to stock options and may include continued service, performance and/or other conditions. |
| • | SARs. SARs entitle their holder, upon exercise, to receive from us an amount equal to the appreciation of the shares subject to the award between the grant date and the exercise date. The exercise price of a SAR may not be less than 100% of the fair market value of the underlying share on the date of grant (except with respect to certain substitute SARs granted in connection with a corporate transaction) and the term of a SAR may not be longer than ten years. Vesting conditions determined by the plan administrator may apply to SARs and may include continued service, performance and/or other conditions. |
| • | Restricted Stock and RSUs. Restricted stock is an award of nontransferable shares of our common stock that remain forfeitable unless and until specified conditions are met, and which may be subject to a purchase price. RSUs are contractual promises to deliver shares of our common stock in the future, which may also remain forfeitable unless and until specified conditions are met. Delivery of the shares underlying RSUs may be deferred under the terms of the award or at the election of the participant, if the plan administrator permits such a deferral. Conditions applicable to restricted stock and RSUs may be based on continuing service, the attainment of performance goals and/or such other conditions as the plan administrator may determine. |
| • | Other Stock or Cash Based Awards. Other stock or cash based awards are awards of cash, fully vested shares of our common stock and other awards denominated in, linked to, or derived from shares of our common stock or value metrics related to our shares. Other stock or cash based awards may be granted to participants and may also be available as a payment form in the settlement of other awards, as standalone payments and as payment in lieu of base salary, bonus, fees or other cash compensation otherwise payable to any individual who is eligible to receive awards. Conditions applicable to other stock or cash based awards may be based on continuing service, the attainment of performance goals and/or such other conditions as the plan administrator may determine. |
| • | Dividend Equivalents. Dividend equivalents represent the right to receive the equivalent value of dividends paid on shares of our common stock and may be granted alone or in tandem with awards |
167
Table of Contents
| other than stock options or SARs. Dividend equivalents are credited as of dividend record dates during the period between the date an award is granted and the date such award terminates or expires, as determined by the plan administrator. |
Performance Awards. Performance awards include any of the foregoing awards that are granted subject to vesting and/or payment based on the attainment of specified performance goals or other criteria the plan administrator may determine, which may or may not be objectively determinable. Performance criteria upon which performance goals are established by the plan administrator may include but are not limited to: (i) net earnings or losses (either before or after one or more of the following: (A) interest, (B) taxes, (C) depreciation, (D) amortization and (E) non-cash equity-based compensation expense); (ii) gross or net sales or revenue or sales or revenue growth; (iii) net income (either before or after taxes); (iv) adjusted net income; (v) operating earnings or profit (either before or after taxes); (vi) cash flow (including, but not limited to, operating cash flow and free cash flow); (vii) return on assets; (viii) return on capital (or invested capital) and cost of capital; (ix) return on stockholders’ equity; (x) total stockholder return; (xi) return on sales; (xii) gross or net profit or operating margin; (xiii) costs, reductions in costs and cost control measures; (xiv) expenses; (xv) working capital; (xvi) earnings or loss per share; (xvii) adjusted earnings or loss per share; (xviii) price per share or dividends per share (or appreciation in and/or maintenance of such price or dividends); (xix) regulatory achievements or compliance (including, without limitation, regulatory body approval for commercialization of a product); (xx) implementation or completion of critical projects; (xxi) market share; (xxii) economic value; (xxiii) individual employee performance; or (xxiv) any combination of the foregoing, any of which may be measured either in absolute terms for us or any operating unit of our company or as compared to any incremental increase or decrease or as compared to results of a peer group or to market performance indicators or indices.
Certain Transactions and Adjustments. The plan administrator has broad discretion to take action under the 2020 Plan, as well as make adjustments to the terms and conditions of existing and future awards, to prevent the dilution or enlargement of intended benefits and facilitate necessary or desirable changes in the event of certain transactions and events affecting our common stock, such as stock dividends, stock splits, mergers, acquisitions, consolidations and other corporate transactions. In addition, in the event of certain non-reciprocal transactions with our stockholders known as “equity restructurings,” the plan administrator will make equitable adjustments to the 2020 Plan and outstanding awards. In the event of a change in control of our company (as defined in the 2020 Plan), to the extent that the surviving entity declines to continue, convert, assume or replace outstanding awards, the administrator may terminate any or all such awards in exchange for cash, rights or other property or may cause any or all such awards to become fully exercisable immediately prior to the transaction and all applicable forfeiture restrictions to lapse. In the case of any award so exercisable in lieu of assumption or substitution, the plan administrator shall provide notice that such awards will remain fully exercisable for fifteen (15) days after the date the plan administrator provides such notice (contingent upon the occurrence of the change in control) and that such awards shall terminate at the end of such period. In the event an outstanding award is assumed or substituted for an equivalent award in connection with a change in control and the holder of such award terminates employment without “cause” (as such term is defined in the sole discretion of the plan administrator or as set forth in the award agreement relating to such award) within the 12 months following the change in control, then such award will become fully vested and exercisable in connection with the termination of employment. Individual award agreements may provide for additional accelerated vesting and payment provisions. In addition, the plan administrator has discretion to institute and determine the terms and conditions of an exchange program, which is a program under which outstanding awards may be surrendered or cancelled in exchange for awards of the same type (which may have higher or lower exercise prices and different terms), awards of a different type, and/or cash, under which participants have the opportunity to transfer outstanding awards to a financial institution or other person or entity selected by the plan administrator, or under which the exercise price of an outstanding award may be reduced or increased.
Foreign Participants, Claw-Back Provisions, Transferability, and Participant Payments. The plan administrator may modify award terms, establish subplans and/or adjust other terms and conditions of awards, subject to the share limits described above, in order to facilitate grants of awards subject to the laws and/or stock exchange
168
Table of Contents
rules of countries outside of the United States. All awards will be subject to the provisions of any claw-back policy implemented by our company to the extent set forth in such claw-back policy and/or in the applicable award agreement. With limited exceptions for estate planning, domestic relations orders, certain beneficiary designations and the laws of descent and distribution, awards under the 2020 Plan are generally non-transferable, and are exercisable only by the participant. With regard to tax withholding, exercise price and purchase price obligations arising in connection with awards under the 2020 Plan, the plan administrator may, in its discretion, accept cash or check, provide for net withholding of shares, allow shares of our common stock that meet specified conditions to be repurchased, allow a “market sell order” or such other consideration as it deems suitable.
Plan Amendment and Termination. Our board of directors may amend or terminate the 2020 Plan at any time; however, except in connection with certain changes in our capital structure, stockholder approval will be required for any amendment that increases the number of shares available under the 2020 Plan. No award may be granted pursuant to the 2020 Plan after the tenth anniversary of the date on which our board of directors adopts the 2020 Plan.
2020 Employee Stock Purchase Plan
In connection with the offering, we intend to adopt the 2020 Employee Stock Purchase Plan, or ESPP, which will become effective on the day the ESPP is adopted by our board of directors. The material terms of the ESPP, as it is currently contemplated, are summarized below. Our board of directors is still in the process of developing, approving and implementing the ESPP and, accordingly, this summary is subject to change.
We expect that the ESPP will be comprised of two distinct components in order to provide increased flexibility to grant options to purchase shares under the 2020 ESPP. Specifically, we expect that the ESPP will authorize (1) the grant of options to employees that are intended to qualify for favorable U.S. federal tax treatment under Section 423 of the Code (the “Section 423 Component”), and (2) the grant of options that are not intended to be tax qualified under Section 423 of the Code to facilitate participation for employees who are not eligible to benefit from favorable U.S. federal tax treatment and, to the extent applicable, to provide flexibility to comply with non U.S. law and other considerations (the “Non Section 423 Component”). We expect that the Non Section 423 Component will generally be operated and administered on terms and conditions similar to the Section 423 Component, except as otherwise required by applicable law, rule or regulation.
Shares Available; Administration. We expect a total of shares of our common stock to be initially reserved for issuance under our ESPP. In addition, we expect that the number of shares available for issuance under the ESPP will be annually increased on January 1 of each calendar year beginning in 2021 and ending in 2030, by an amount equal to the lesser of: (i) % of the aggregate number of shares of common stock outstanding on the final day of the immediately preceding calendar year and (ii) such smaller number of shares as is determined by our board of directors. In no event will more than shares of our common stock be available for issuance under the Section 423 Component.
The compensation committee of our board of directors will be the plan administrator of the ESPP and will have authority to interpret the terms of the ESPP and determine eligibility of participants.
Eligibility. The plan administrator may designate certain of our subsidiaries as participating “designated subsidiaries” in the ESPP and may change these designations from time to time. Employees of our company and our designated subsidiaries are eligible to participate in the ESPP if they meet the eligibility requirements under the ESPP established from time to time by the plan administrator. However, an employee may not be granted rights to purchase stock under the ESPP if such employee, immediately after the grant, would own (directly or through attribution) stock possessing 5% or more of the total combined voting power or value of all classes of our common or other class of stock.
169
Table of Contents
If the grant of a purchase right under the ESPP to any eligible employee who is a citizen or resident of a foreign jurisdiction would be prohibited under the laws of such foreign jurisdiction or the grant of a purchase right to such employee in compliance with the laws of such foreign jurisdiction would cause the ESPP to violate the requirements of Section 423 of the Code, as determined by the plan administrator in its sole discretion, such employee will not be permitted to participate in the Section 423 Component.
Eligible employees become participants in the ESPP by enrolling and authorizing payroll deductions by the deadline established by the plan administrator prior to the relevant offering date. Directors who are not employees, as well as consultants, are not eligible to participate. Employees who choose not to participate, or are not eligible to participate at the start of an offering period but who become eligible thereafter, may enroll in any subsequent offering period.
Participation in an Offering. Stock will be offered under the ESPP during offering periods. The length of offering periods under the ESPP will be determined by the plan administrator and may be up to 27 months long. Employee payroll deductions will be used to purchase shares on each payday during an offering period. Offering periods under the ESPP will commence when determined by the plan administrator. The plan administrator may, in its discretion, modify the terms of future offering periods. . To the extent applicable, in non U.S. jurisdictions where participation in the ESPP through payroll deductions is prohibited, the plan administrator may provide that an eligible employee may elect to participate through contributions to the participant’s account under the ESPP in a form acceptable to the ESPP administrator in lieu of or in addition to payroll deductions.
We expect that the ESPP will permit participants to purchase our common stock through payroll deductions of up to % of their eligible compensation, which will include a participant’s gross base compensation for services to us. The plan administrator will establish a maximum number of shares that may be purchased by a participant during any offering period or purchase period, which, in the absence of a contrary designation, will be shares. In addition, no employee will be permitted to accrue the right to purchase stock under the Section 423 Component at a rate in excess of $25,000 worth of shares during any calendar year during which such a purchase right is outstanding (based on the fair market value per share of our common stock as of the first day of the offering period).
On the first trading day of each offering period, each participant automatically will be granted an option to purchase shares of our common stock. The option will be exercised on the applicable purchase date(s) during the offering period, to the extent of the payroll deductions accumulated during the applicable purchase period. We expect that the purchase price of the shares, in the absence of a contrary determination by the plan administrator, will be 85% of the lower of the fair market value of our common stock on the first trading day of the offering period or on the applicable purchase date, which will be the final trading day of the applicable purchase period.
Participants may voluntarily end their participation in the ESPP at any time at least one week prior to the end of the applicable offering period (or such longer or shorter period specified by the plan administrator), and will be paid their accrued payroll deductions that have not yet been used to purchase shares of common stock. Participation ends automatically upon a participant’s termination of employment.
Transferability. A participant may not transfer rights granted under the ESPP other than by will, the laws of descent and distribution or as otherwise provided in the ESPP.
Certain Transactions. In the event of certain transactions or events affecting our common stock, such as any stock dividend or other distribution, change in control, reorganization, merger, consolidation or other corporate transaction, the plan administrator will make equitable adjustments to the ESPP and outstanding rights. In addition, in the event of the foregoing transactions or events or certain significant transactions, including a change in control, the plan administrator may provide for (i) either the replacement of outstanding rights with other rights or property or termination of outstanding rights in exchange for cash, (ii) the assumption or substitution of outstanding rights by the successor or survivor corporation or parent or subsidiary thereof, (iii) the
170
Table of Contents
adjustment in the number and type of shares of stock subject to outstanding rights, (iv) the use of participants’ accumulated payroll deductions to purchase stock on a new purchase date prior to the next scheduled purchase date and termination of any rights under ongoing offering periods or (v) the termination of all outstanding rights.
Plan Amendment; Termination. The plan administrator may amend, suspend or terminate the ESPP at any time. However, stockholder approval of any amendment to the ESPP must be obtained for any amendment which increases the aggregate number or changes the type of shares that may be sold pursuant to rights under the ESPP or changes the corporations or classes of corporations whose employees are eligible to participate in the ESPP.
171
Table of Contents
CERTAIN RELATIONSHIPS AND RELATED PARTY TRANSACTIONS
The following are summaries of certain transactions and relationships with our directors, executive officers and stockholders and certain provisions of our related party agreements and are qualified in their entirety by reference to all of the provisions of such agreements. Because these descriptions are only summaries of the applicable agreements, they do not necessarily contain all of the information that you may find useful. We, therefore, urge you to review the agreements in their entirety. Copies of the forms of the agreements have been filed as exhibits to the registration statement of which this prospectus is a part, and are available electronically on the website of the SEC at www.sec.gov.
Related Party Agreements in Effect Prior to the Transactions
Expense Reimbursement Agreement
On September 13, 2019, in connection with the Centerbridge Acquisition, GoHealth Holdings, LLC, Norvax, LLC and an affiliate of the Sponsor entered into an expense reimbursement and indemnification agreement pursuant to which, GoHealth Holdings, LLC and Norvax, LLC agreed to indemnify and reimburse the Sponsor for up to $500,000 of certain out-of-pocket costs, fees and expenses incurred by or on behalf of the Sponsors in connection with the Centerbridge Acquisition and certain services provided to us by the Sponsor. To date, we have made payments totaling less than $60,000 pursuant to this agreement.
Agreements Involving our Founders
We have entered into various lease agreements (as amended and restated, the “RPT Leases”) with Wilson Tech 5, LLC, 214 W Huron LLC, 220 W Huron Street Holdings LLC and 215 W Superior LLC, each of which are controlled by our Founders, to lease our corporate offices at 214 West Huron Street, Chicago, Illinois, 220 West Huron Street, Chicago, Illinois, 215 West Superior Street, Chicago, Illinois, and a proposed site in Linden, Utah, beginning in 2022. Our lease agreement with Wilson Tech 5, LLC expires on May 11, 2030; our lease agreement with 214 W Huron LLC expires on July 31, 2024; our lease agreements with 220 W Huron Street Holdings LLC expire on May 31, 2024 and July 31, 2024; and our lease agreement with 215 W Superior LLC expires on December 31, 2030. In addition to the lease payments, we are also required to pay operating expenses, maintenance and utilities under the terms of the RPT Leases. For the three months ended March 31, 2020, the Successor 2019 Period, Predecessor 2019 Period and for the year ended December 31, 2018, we made aggregate lease payments of $321,000, $298,000, $758,000 and $1,025,000, respectively under the RPT Leases. Assuming none of the RPT Leases are terminated early, the remaining amounts due under the RPT Leases in aggregate is expected to be $6.9 million.
On January 1, 2020, we entered into a non-exclusive aircraft dry lease agreement with N157BC, LLC, an entity wholly-owned and controlled by our Founders. The agreement allowed us to use an aircraft owned by N157BC, LLC for our business and on an as-needed basis. The agreement has no set term and is terminable without cause by either party upon 30 days’ prior written notice. Under the agreement, we are required to pay $6,036.94 per flight hour for use of the aircraft. We expect to terminate this agreement upon consummation of the Transactions.
On March 2, 2018, we entered into an agreement with Rank Me Media, LLC, an entity wholly-owned and controlled by Patrick Cruz, brother to each of Brandon M. Cruz, our Chief Strategy Officer and Special Advisor to the Executive Team and a member of our board directors, and Shane E. Cruz, our Chief Operating Officer, to provide search engine optimization consulting services. This agreement had an initial term of 6 months and after the expiration of such period, automatically renews 1 month each month unless terminated by either party with a 30-day prior written notice. Under the agreement, we are required to pay a monthly flat fee retainer of $6,000 per month. For the three months ended March 31, 2020, the Successor 2019 Period, Predecessor 2019 Period and for the year ended December 31, 2018, we made aggregate payments of $18,000, $18,000, $57,000 and $42,000, respectively under this agreement.
172
Table of Contents
The Transactions
In connection with the Transactions, we will engage in certain transactions with certain of our directors, executive officers and other persons and entities which are or will become holders of 5% or more of our voting securities upon the consummation of the Transactions. These transactions are described in “Our Organizational Structure.”
We intend to use the net proceeds from this offering (including any net proceeds from any exercise of the underwriters’ option to purchase additional shares of Class A common stock) to purchase LLC
Interests (or LLC Interests if the underwriters exercise in full their option to purchase additional shares of Class A common stock) directly from GoHealth Holdings, LLC at a price per unit equal to the initial public offering price per share of Class A common stock in this offering less the underwriting discount and estimated offering expenses payable by us and to pay cash to the Blocker Shareholders as partial consideration in the Blocker Merger.
Tax Receivable Agreement
As described in “Our Organizational Structure,” we intend to use the net proceeds from this offering to purchase newly-issued LLC Interests directly from GoHealth Holdings, LLC and to pay cash to the Blocker Shareholders as partial consideration in the Blocker Merger. In addition, GoHealth Holdings, LLC intends to use the net proceeds it receives from the sale of LLC Interests to us to partially redeem certain of the LLC Interests held by the Continuing Equity Owners, which is intended to be treated as a taxable sale of LLC Interests for U.S. federal income tax purposes. We expect to obtain an increase in our share of the tax basis of the assets of GoHealth Holdings, LLC in connection with the purchase of LLC Interests directly from GoHealth Holdings, LLC, the partial redemption of LLC Interests by GoHealth Holdings and the Blocker Merger. We will also acquire an allocable share of the existing tax basis in GoHealth Holdings, LLC’s assets in connection with the Transactions, including the Blocker Company’s share of existing tax basis, and we may obtain an increase to such allocable share of existing tax basis in connection with the consummation of the Transactions and in the future. In addition, we may obtain an increase in our share of the tax basis of the assets of GoHealth Holdings, LLC in the future, when (as described below under “—GoHealth Holdings, LLC Agreement—Agreement in Effect Upon Consummation of the Transactions—Common Unit Redemption Right”) a Continuing Equity Owner receives Class A common stock or, at our election (determined solely by our independent directors (within the meaning of the Nasdaq rules) who are disinterested), cash, as applicable, from us in connection with an exercise of such Continuing Equity Owner’s right to have LLC Interests held by such Continuing Equity Owner redeemed by GoHealth Holdings, LLC or, at our election, exchanged or when GoHealth Holdings, LLC makes, or is deemed to make, certain distributions to the Continuing Equity Owners. We intend to treat such redemptions or exchanges as our direct purchase of LLC Interests from such Continuing Equity Owner for U.S. federal income and other applicable tax purposes, regardless of whether such LLC Interests are surrendered by a Continuing Equity Owner to GoHealth Holdings, LLC for redemption or sold to us upon the exercise of our election to acquire such LLC Interests directly (any resulting basis increases, together with the basis increases arising from (a) the purchase of newly-issued LLC Interests directly from GoHealth Holdings, LLC and the partial redemption of LLC Interests by GoHealth Holdings, LLC, as described under “Use of Proceeds,” and (b) certain distributions (or deemed distributions) from GoHealth Holdings, LLC, the “Basis Adjustments”). Any Basis Adjustment and our allocable share of the existing tax basis in GoHealth Holdings, LLC’s assets, including the Blocker Company’s share of existing tax basis (and increases to such allocable share of existing tax basis), may have the effect of reducing the amounts that we would otherwise pay in the future to various tax authorities. The Basis Adjustments and such existing tax basis (and increases to such allocable share of existing tax basis) may also decrease gains (or increase losses) on future dispositions of certain assets to the extent tax basis is allocated to those assets.
In connection with the transactions described above, we will enter into a Tax Receivable Agreement with GoHealth Holdings, LLC, Continuing Equity Owners and the Blocker Shareholders that will provide for the
173
Table of Contents
payment by GoHealth, Inc. to the Continuing Equity Owners and the Blocker Shareholders of 85% of the amount of certain tax benefits, if any, that GoHealth, Inc. actually realizes, or in some circumstances is deemed to realize as a result of the transactions described above, including the acquisition of GoHealth, Inc.’s allocable share of the existing tax basis in GoHealth Holdings, LLC’s assets in connection with the Transactions (including the Blocker Company’s share of existing tax basis), increases to such allocable share of existing tax basis, the Basis Adjustments and certain other tax benefits arising from payments made under the Tax Receivable Agreement. GoHealth Holdings, LLC will have in effect an election under Section 754 of the Code effective for each taxable year in which a redemption or exchange (including deemed exchange, and including for this purpose the purchase of LLC Interests directly from certain Continuing Equity Owners described above) of LLC Interests for Class A common stock or cash occurs or when GoHealth Holdings, LLC makes (or is deemed to make) certain distributions. These Tax Receivable Agreement payments are not conditioned upon one or more of the Continuing Equity Owners maintaining a continued ownership interest in GoHealth Holdings, LLC. If a Continuing Equity Owner transfers LLC Interests but does not assign to the transferee of such units its rights under the Tax Receivable Agreement, such Continuing Equity Owner generally will continue to be entitled to receive payments under the Tax Receivable Agreement arising in respect of a subsequent exchange of such LLC Interests. In general, the Continuing Equity Owners’ and Blocker Shareholders’ rights under the Tax Receivable Agreement may not be assigned, sold, pledged or otherwise alienated to any person, other than certain permitted transferees, without such person becoming a party to the Tax Receivable Agreement and agreeing to succeed to the applicable Continuing Equity Owner’s or Blocker Shareholders’ interest therein.
The actual Basis Adjustments, as well as any amounts paid to the Continuing Equity Owners and the Blocker Shareholders under the Tax Receivable Agreement will vary depending on a number of factors, including:
| • | the timing of any future redemptions or exchanges—for instance, the increase in any tax deductions will vary depending on the fair value, which may fluctuate over time, of the depreciable or amortizable assets of GoHealth Holdings, LLC at the time of each redemption, exchange or distribution (or deemed distribution) as well as the amount of remaining existing tax basis at the time of such redemption, exchange or distribution (or deemed distribution); |
| • | the price of shares of our Class A common stock at the time of the purchases from the Continuing Equity Owners in connection with this offering and any applicable redemptions or exchanges—the Basis Adjustments, as well as any related increase in any tax deductions, are directly related to the price of shares of our Class A common stock at the time of such purchases or future redemptions or exchanges; |
| • | the extent to which such redemptions or exchanges are taxable—if a redemption or exchange is not taxable for any reason, increased tax deductions will not be available; and |
| • | the amount and timing of our income—the Tax Receivable Agreement generally will require us to pay 85% of the tax benefits as and when those benefits are treated as realized under the terms of the Tax Receivable Agreement. If we do not have sufficient taxable income to realize any of the applicable tax benefits, we generally will not be required (absent a material breach of a material obligation under the Tax Receivable Agreement, change of control or other circumstances requiring an early termination payment and treating any outstanding LLC Interests held by Continuing Equity Owners as having been exchanged for Class A common stock for purposes of determining such early termination payment) to make payments under the Tax Receivable Agreement for that taxable year because no tax benefits will have been actually realized. However, any tax benefits that do not result in realized tax benefits in a given taxable year may generate tax attributes that may be utilized to generate tax benefits in previous or future taxable years. The utilization of any such tax attributes will result in payments under the Tax Receivable Agreement. |
Although the amount of our allocable share of existing tax basis in GoHealth Holdings, LLC’s assets acquired in connection with the Transactions with respect to which the Continuing Equity Owners and the Blocker Shareholders will be entitled to receive payments under the Tax Receivable Agreement has been determined to
174
Table of Contents
be approximately $ million, the timing and amount of any related payments under the Tax Receivable Agreement is uncertain since both are dependent on our taxable income and our ability to utilize other tax attributes.
For purposes of the Tax Receivable Agreement, cash savings in income tax will be computed by comparing our actual income tax liability to the amount of such taxes that we would have been required to pay had there been no existing basis in GoHealth Holdings, LLC’s assets, had there been no increases to such allocable share of existing tax basis, had there been no Basis Adjustments, had the Tax Receivable Agreement not been entered into and had there been no tax benefits to us as a result of any payments made under the Tax Receivable Agreement; provided that, for purposes of determining cash savings with respect to state and local income taxes we will use an assumed tax rate. The Tax Receivable Agreement will generally apply to each of our taxable years, beginning with the first taxable year ending after the consummation of the Transactions. There is no maximum term for the Tax Receivable Agreement; however, the Tax Receivable Agreement may be terminated by us pursuant to an early termination procedure that requires us to pay the Continuing Equity Owners an agreed-upon amount equal to the estimated present value of the remaining payments to be made under the agreement (calculated with certain assumptions, including regarding tax rates and utilization of the Basis Adjustments).
The payment obligations under the Tax Receivable Agreement are obligations of GoHealth, Inc. and not of GoHealth Holdings, LLC. Although the actual timing and amount of any payments that may be made under the Tax Receivable Agreement will vary, we expect that the payments that we may be required to make to the Continuing Equity Owners and the Blocker Shareholders could be substantial. Any payments made by us to the Continuing Equity Owners and the Blocker Shareholders under the Tax Receivable Agreement will generally reduce the amount of overall cash flow that might have otherwise been available to us or to GoHealth Holdings, LLC and, to the extent that we are unable to make payments under the Tax Receivable Agreement for any reason, the unpaid amounts will be deferred and will accrue interest until paid by us; provided, however, that nonpayment for a specified period may constitute a material breach of a material obligation under the Tax Receivable Agreement and, therefore, may accelerate payments due under the Tax Receivable Agreement. We anticipate funding ordinary course payments under the Tax Receivable Agreement from cash flow from operations of our subsidiaries, available cash or available borrowings under our Credit Facilities or any future debt agreements. See “Unaudited Pro Forma Condensed Consolidated Financial Information.” Decisions made by us in the course of running our business, such as with respect to mergers, asset sales, other forms of business combinations or other changes in control, may influence the timing and amount of payments that are received by a redeeming Continuing Equity Owner or a Blocker Shareholder under the Tax Receivable Agreement. For example, the earlier disposition of assets following an exchange or acquisition transaction will generally accelerate payments under the Tax Receivable Agreement and increase the present value of such payments.
The Tax Receivable Agreement provides that if certain mergers, asset sales, other forms of business combination, or other changes of control were to occur, if we materially breach any of our material obligations under the Tax Receivable Agreement or if, at any time, we elect an early termination of the Tax Receivable Agreement, then the Tax Receivable Agreement will terminate and our obligations, or our successor’s obligations, under the Tax Receivable Agreement would accelerate and become due and payable, based on certain assumptions, including an assumption that we would have sufficient taxable income to fully utilize all potential future tax benefits that are subject to the Tax Receivable Agreement. In those circumstances, Continuing Equity Owners would be deemed to exchange any remaining outstanding LLC Interests for Class A common stock and would generally be entitled to payments under the Tax Receivable Agreement resulting from such deemed exchanges.
We may elect to completely terminate the Tax Receivable Agreement early only with the written approval of each of a majority of GoHealth, Inc.’s “independent directors” (within the meaning of Rule 10A-3 promulgated under the Exchange Act and the Nasdaq rules).
As a result of the foregoing, we could be required to make an immediate cash payment equal to the present value of the anticipated future tax benefits that are the subject of the Tax Receivable Agreement, which payment may
175
Table of Contents
be made significantly in advance of the actual realization, if any, of such future tax benefits. We also could be required to make cash payments to the Continuing Equity Owners and the Blocker Shareholders that are greater than the specified percentage of the actual benefits we ultimately realize in respect of the tax benefits that are subject to the Tax Receivable Agreement. In these situations, our obligations under the Tax Receivable Agreement could have a substantial negative impact on our liquidity and could have the effect of delaying, deferring or preventing certain mergers, asset sales, other forms of business combination, or other changes of control. There can be no assurance that we will be able to finance our obligations under the Tax Receivable Agreement.
Payments under the Tax Receivable Agreement will generally be based on the tax reporting positions that we determine. We will not be reimbursed for any cash payments previously made to the Continuing Equity Owners and the Blocker Shareholders pursuant to the Tax Receivable Agreement if any tax benefits initially claimed by us are subsequently challenged by a taxing authority and ultimately disallowed. Instead, any excess cash payments made by us to a Continuing Equity Owner or a Blocker Shareholder will be netted against any future cash payments we might otherwise be required to make under the terms of the Tax Receivable Agreement to such Continuing Equity Owner or such Blocker Shareholder, as applicable. However, a challenge to any tax benefits initially claimed by us may not arise for a number of years following the initial time of such payment or, even if challenged early, such excess cash payment may be greater than the amount of future cash payments we might otherwise be required to make under the terms of the Tax Receivable Agreement and, as a result, there might not be future cash payments from which to net against. The applicable U.S. federal income tax rules are complex and factual in nature, and there can be no assurance that the IRS or a court will not disagree with our tax reporting positions. As a result, it is possible that we could make cash payments under the Tax Receivable Agreement that are substantially greater than our actual cash tax savings. If we determine that a tax reserve or contingent liability must be established by us for generally accepted accounting principles in respect of an issue that would affect payments under the Tax Receivable Agreement, we may withhold payments to the Continuing Equity Owners and/or the Blocker Shareholders, as applicable, under the Tax Receivable Agreement and place them in an interest-bearing escrow account until the reserve or contingent liability is resolved.
We will have full responsibility for, and sole discretion over, all GoHealth, Inc. tax matters, including the filing and amendment of all tax returns and claims for refund and defense of all tax contests, subject to certain participation and approval rights held by Centerbridge and the Founders. If the outcome of any challenge to all or part of the Basis Adjustments or other tax benefits we claim, including as a result of acquiring our allocable share of the existing tax basis in GoHealth Holdings, LLC’s assets and increases to such allocable share of existing tax basis, would reasonably be expected to materially and adversely affect the payments to Continuing Equity Owners’ from us under the Tax Receivable Agreement, then we will not be permitted to settle or fail to contest such challenge without the consent (not to be unreasonably withheld or delayed) of Centerbridge and the Founders. The interests of Centerbridge or the Founders in any such challenge may differ from or conflict with our interests and your interests, and Centerbridge or the Founders may exercise their consent rights relating to any such challenge in a manner adverse to our interests.
Under the Tax Receivable Agreement, we are required to provide the Continuing Equity Owners and Blocker Shareholders that hold an interest in the Tax Receivable Agreement with a schedule showing the calculation of payments that are due under the Tax Receivable Agreement with respect to each taxable year with respect to which a payment obligation arises within 90 days after filing our U.S. federal income tax return for such taxable year. This calculation will be based upon the advice of our tax advisors. Payments under the Tax Receivable Agreement will generally be made to the Continuing Equity Owners and the Blocker Shareholders within three business days after this schedule becomes final pursuant to the procedures set forth in the Tax Receivable Agreement, although interest on such payments will begin to accrue at a rate of LIBOR plus 100 basis points from the due date (without extensions) of such tax return. Any late payments that may be made under the Tax Receivable Agreement will continue to accrue interest at a rate equal to LIBOR plus 500 basis points, until such payments are made, generally including any late payments that we may subsequently make because we did not have enough available cash to satisfy our payment obligations at the time at which they originally arose.
176
Table of Contents
GoHealth Holdings, LLC Agreement
Agreement in Effect Before Consummation of the Transactions
GoHealth Holdings, LLC and the Original Equity Owners are parties to the Amended and Restated Limited Liability Company Agreement of GoHealth Holdings, LLC (formerly known as Blizzard Parent, LLC), dated as of September 13, 2019, which governs the business operations of GoHealth Holdings, LLC and defines the relative rights and privileges associated with the existing units of GoHealth Holdings, LLC. We refer to this agreement as the Existing LLC Agreement. Under the Existing LLC Agreement, the board of managers of GoHealth Holdings, LLC has the full, exclusive and complete right, authority and discretion to manage and control the business and affairs of GoHealth Holdings, LLC, to interpret the provisions of the Existing LLC Agreement, to make all decisions affecting the business and affairs of GoHealth Holdings, LLC, to take all such actions as it deems necessary or appropriate to accomplish the purpose of the Company, and the day-to-day business operations of GoHealth Holdings, LLC are overseen and implemented by officers of GoHealth Holdings, LLC. Each Original Equity Owner’s rights under the Existing LLC Agreement continue until the effective time of the new GoHealth Holdings, LLC operating agreement to be adopted in connection with the Transactions, as described below, at which time the Continuing Equity Owners will continue as members that hold LLC Interests with the respective rights thereunder.
Agreement in Effect Upon Consummation of the Transactions
In connection with the consummation of the Transactions, we and the Continuing Equity Owners will enter into GoHealth Holdings, LLC’s Second Amended and Restated Limited Liability Company Agreement, which we refer to as the GoHealth Holdings, LLC Agreement.
| • | Appointment as Managing Member. Under the GoHealth Holdings, LLC Agreement, we will become a member and the sole manager of GoHealth Holdings, LLC. As the sole manager, we will be able to control all of the day-to-day business affairs and decision-making of GoHealth Holdings, LLC without the approval of any other member. As such, we, through our officers and directors, will be responsible for all operational and administrative decisions of GoHealth Holdings, LLC and daily management of GoHealth Holdings, LLC’s business. Pursuant to the terms of the GoHealth Holdings, LLC Agreement, we cannot be removed or replaced as the sole manager of GoHealth Holdings, LLC except by our resignation, which may be given at any time by written notice to the members. |
| • | Compensation, Fees and Expenses. We will not be entitled to compensation for our services as the manager of GoHealth Holdings, LLC. We will be entitled to reimbursement by GoHealth Holdings, LLC for reasonable fees and expenses incurred on behalf of GoHealth Holdings, LLC, including all expenses associated with the Transactions, any subsequent offering of our Class A common stock, being a public company and maintaining our corporate existence. |
| • | Distributions. The GoHealth Holdings, LLC Agreement will require “tax distributions,” as that term is used in the agreement to be made by GoHealth Holdings, LLC to its members on a pro rata basis, except to the extent such distributions would render GoHealth Holdings, LLC insolvent or are otherwise prohibited by law, our Credit Facilities or any of our future debt agreements. Tax distributions will be made on a quarterly basis, to each member of GoHealth Holdings, LLC, including us, based on such member’s allocable share of the taxable income of GoHealth Holdings, LLC and an assumed tax rate that will be determined by us, as described below. For this purpose, GoHealth, Inc.’s allocable share of GoHealth Holdings, LLC’s taxable income shall be net of its share of taxable losses of GoHealth Holdings, LLC and shall be determined without regard to any Basis Adjustments (as described above under “—Tax Receivable Agreement”). The assumed tax rate for purposes of determining tax distributions from GoHealth Holdings, LLC to its members will be the highest combined federal, state, and local tax rate that may potentially apply to any one of GoHealth Holdings, LLC’s members, regardless of the actual final tax liability of any such member. The GoHealth |
177
Table of Contents
| Holdings, LLC Agreement will also allow for cash distributions to be made by GoHealth Holdings, LLC (subject to our sole discretion as the sole manager of GoHealth Holdings, LLC) to its members on a pro rata basis out of “distributable cash,” as that term is defined in the agreement. We expect GoHealth Holdings, LLC may make distributions out of distributable cash periodically and as necessary to enable us to cover our operating expenses and other obligations, including our tax liability and obligations under the Tax Receivable Agreement, except to the extent such distributions would render GoHealth Holdings, LLC insolvent or are otherwise prohibited by law, our Credit Facilities or any of our future debt agreements. |
| • | Transfer Restrictions. The GoHealth Holdings, LLC Agreement generally does not permit transfers of LLC Interests by members, except for transfers to permitted transferees, transfers pursuant to the participation right described below and other limited exceptions. The GoHealth Holdings, LLC Agreement may impose additional restrictions on transfers (including redemptions described below with respect to each common unit) that are necessary or advisable so that GoHealth Holdings, LLC is not treated as a “publicly traded partnership” for U.S. federal income tax purposes. In the event of a permitted transfer under the GoHealth Holdings, LLC Agreement, such member will be required to simultaneously transfer shares of Class B common stock to such transferee equal to the number of LLC Interests that were transferred to such transferee in such permitted transfer. |
The GoHealth Holdings, LLC Agreement provides that, in the event that a tender offer, share exchange offer, issuer bid, take-over bid, recapitalization or similar transaction with respect to our Class A common stock, each of which we refer to as a Pubco Offer, is approved by our board of directors or otherwise effected or to be effected with the consent or approval of our board of directors, each holder of LLC Interests shall be permitted to participate in such Pubco Offer by delivering a redemption notice, which shall be effective immediately prior to, and contingent upon, the consummation of such Pubco Offer. If a Pubco Offer is proposed by GoHealth, Inc., then GoHealth, Inc. is required to use its reasonable best efforts expeditiously and in good faith to take all such actions and do all such things as are necessary or desirable to enable and permit the holders of such LLC Interests to participate in such Pubco Offer to the same extent as or on an economically equivalent basis with the holders of shares of Class A common stock, provided that in no event shall any holder of LLC Interests be entitled to receive aggregate consideration for each common unit that is greater than the consideration payable in respect of each share of Class A common stock pursuant to the Pubco Offer.
Except for certain exceptions, any transferee of LLC Interests must assume, by operation of law or executing a joinder to the GoHealth Holdings, LLC Agreement, all of the obligations of a transferring member with respect to the transferred units, and such transferee shall be bound by any limitations and obligations under the GoHealth Holdings, LLC Agreement even if the transferee is not admitted as a member of GoHealth Holdings, LLC. A member shall remain as a member with all rights and obligations until the transferee is accepted as substitute member in accordance with GoHealth Holdings, LLC Agreement.
| • | Recapitalization. The GoHealth Holdings, LLC Agreement will recapitalize the units currently held by the existing members of GoHealth Holdings, LLC into a new single class of LLC Interests. The GoHealth Holdings, LLC Agreement will also reflect a split of LLC Interests such that one common unit can be acquired with the net proceeds received in the initial offering from the sale of one share of our Class A common stock, after the deduction of the underwriting discount and estimated offering expenses payable by us. Each common unit generally will entitle the holder to a pro-rata share of the net profits and net losses and distributions of GoHealth Holdings, LLC. |
| • | Maintenance of One-to-one Ratio between Shares of Class A Common Stock and LLC Interests Owned by the Company, and One-to-one Ratio between Shares of Class B Common Stock and LLC Interests Owned by Centerbridge and our Founders. Except as otherwise determined by us, the |
178
Table of Contents
| GoHealth Holdings, LLC Agreement requires GoHealth Holdings, LLC to take all actions with respect to its LLC Interests, including issuances, reclassifications, distributions, divisions or recapitalizations, such that (1) we at all times maintain a ratio of one common unit owned by us, directly or indirectly, for each share of Class A common stock issued and outstanding, and (2) GoHealth Holdings, LLC at all times maintains (a) a one-to-one ratio between the number of shares of Class A common stock issued and outstanding and the number of LLC Interests owned by us and (b) a one-to-one ratio between the number of shares of Class B common stock issued and outstanding and the number of LLC Interests owned by Centerbridge, our Founders and their permitted transferees, collectively. This ratio requirement disregards (1) shares of our Class A common stock under unvested options issued by us, (2) treasury stock, and (3) preferred stock or other debt or equity securities (including warrants, options or rights) issued by us that are convertible into or exercisable or exchangeable for shares of Class A common stock, except to the extent we have contributed the net proceeds from such other securities, including any exercise or purchase price payable upon conversion, exercise or exchange thereof, to the equity capital of GoHealth Holdings, LLC. In addition, the Class A common stock ratio requirement disregards all LLC Interests at any time held by any other person, including the Continuing Equity Owners and the holders of options over LLC Interests. If we issue, transfer or deliver from treasury stock or repurchase shares of Class A common stock in a transaction not contemplated by the GoHealth Holdings, LLC Agreement, we as manager of GoHealth Holdings, LLC have the authority to take all actions such that, after giving effect to all such issuances, transfers, deliveries or repurchases, the number of outstanding LLC Interests we own equals, on a one-for-one basis, the number of outstanding shares of Class A common stock. If we issue, transfer or deliver from treasury stock or repurchase or redeem any of our preferred stock in a transaction not contemplated by the GoHealth Holdings, LLC Agreement, we as manager have the authority to take all actions such that, after giving effect to all such issuances, transfers, deliveries repurchases or redemptions, we hold (in the case of any issuance, transfer or delivery) or cease to hold (in the case of any repurchase or redemption) equity interests in GoHealth Holdings, LLC which (in our good faith determination) are in the aggregate substantially equivalent to our preferred stock so issued, transferred, delivered, repurchased or redeemed. GoHealth Holdings, LLC is prohibited from undertaking any subdivision (by any split of units, distribution of units, reclassification, recapitalization or similar event) or combination (by reverse split of units, reclassification, recapitalization or similar event) of the LLC Interests that is not accompanied by an identical subdivision or combination of (1) our Class A common stock to maintain at all times a one-to-one ratio between the number of LLC Interests owned by us and the number of outstanding shares of our Class A common stock and (2) our Class B common stock to maintain at all times a one-to-one ratio between the number of LLC Interests owned by Centerbridge and our Founders and their permitted transferees, collectively, and the number of outstanding shares of our Class B common stock, as applicable, in each case, subject to exceptions. |
| • | Issuance of LLC Interests upon Exercise of Options or Issuance of Other Equity Compensation. Upon the exercise of options issued by us (as opposed to options issued by GoHealth Holdings, LLC), or the issuance of other types of equity compensation by us (such as the issuance of restricted or non-restricted stock, payment of bonuses in stock or settlement of stock appreciation rights in stock), we will have the right to acquire from GoHealth Holdings, LLC a number of LLC Interests equal to the number of our shares of Class A common stock being issued in connection with the exercise of such options or issuance of other types of equity compensation. When we issue shares of Class A common stock in settlement of stock options granted to persons that are not officers or employees of GoHealth Holdings, LLC or its subsidiaries, we will make, or be deemed to make, a capital contribution in GoHealth Holdings, LLC equal to the aggregate value of such shares of Class A common stock and GoHealth Holdings, LLC will issue to us a number of LLC Interests equal to the number of shares we issued. When we issue shares of Class A common stock in settlement of stock options granted to persons that are officers or employees of GoHealth Holdings, LLC or its subsidiaries, then we will be deemed to have sold directly to the person exercising such award a portion of the value of each share of Class A common stock equal to the exercise price per share, and we will be deemed to have sold |
179
Table of Contents
| directly to GoHealth Holdings, LLC (or the applicable subsidiary of GoHealth Holdings, LLC) the difference between the exercise price and market price per share for each such share of Class A common stock. In cases where we grant other types of equity compensation to employees of GoHealth Holdings, LLC or its subsidiaries, on each applicable vesting date we will be deemed to have sold to GoHealth Holdings, LLC (or such subsidiary) the number of vested shares at a price equal to the market price per share, GoHealth Holdings, LLC (or such subsidiary) will deliver the shares to the applicable person, and we will be deemed to have made a capital contribution in GoHealth Holdings, LLC equal to the purchase price for such shares in exchange for an equal number of LLC Interests. |
| • | Dissolution. The GoHealth Holdings, LLC Agreement will provide that the consent of GoHealth, Inc. as the managing member of GoHealth Holdings, LLC and members holding a majority of the voting units will be required to voluntarily dissolve GoHealth Holdings, LLC. In addition to a voluntary dissolution, GoHealth Holdings, LLC will be dissolved upon the entry of a decree of judicial dissolution or other circumstances in accordance with Delaware law. Upon a dissolution event, the proceeds of a liquidation will be distributed in the following order: (1) first, to pay the expenses of winding up GoHealth Holdings, LLC; (2) second, to pay debts and liabilities owed to creditors of GoHealth Holdings, LLC, other than members; and (3) third, to the members pro-rata in accordance with their respective percentage ownership interests in GoHealth Holdings, LLC (as determined based on the number of LLC Interests held by a member relative to the aggregate number of all outstanding LLC Interests). |
| • | Confidentiality. We, as manager, and each member agree to maintain the confidentiality of GoHealth Holdings, LLC’s confidential information. This obligation excludes information independently obtained or developed by the members, information that is in the public domain or otherwise disclosed to a member, in either such case not in violation of a confidentiality obligation of the GoHealth Holdings, LLC Agreement or approved for release by written authorization of the Chief Executive Officer, the Chief Financial Officer or the General Counsel of either GoHealth, Inc. or GoHealth Holdings, LLC. |
| • | Indemnification. The GoHealth Holdings, LLC Agreement will provide for indemnification of the manager, members and officers of GoHealth Holdings, LLC and their respective subsidiaries or affiliates. |
| • | Common Unit Redemption Right. The GoHealth Holdings, LLC Agreement will provide a redemption right to the Continuing Equity Owners which will entitle them to have their LLC Interests redeemed for, at our election (determined solely by our independent directors (within the meaning of the Nasdaq rules) who are disinterested), newly-issued shares of our Class A common stock on a one-for-one basis or a cash payment equal to a volume weighted average market price of one share of Class A common stock for each LLC interest so redeemed, in each case in accordance with the terms of the GoHealth Holdings, LLC Agreement; provided that, at our election (determined solely by our independent directors (within the meaning of the Nasdaq rules) who are disinterested), we may effect a direct exchange by GoHealth, Inc. of such Class A common stock or such cash, as applicable, for such LLC Interests. The Continuing Equity Owners may exercise such redemption right, subject to certain exceptions, for as long as their LLC Interests remain outstanding. In connection with the exercise of the redemption or exchange of LLC Interests (1) the Continuing Equity Owners will be required to surrender a number of shares of our Class B common stock registered in the name of such redeeming or exchanging Continuing Equity Owner, and therefore, will automatically be transferred to the Company and will be canceled for no consideration on a one-for-one basis with the number of LLC Interests so redeemed or exchanged and (2) all redeeming members will surrender LLC Interests to GoHealth Holdings, LLC for cancellation. |
Each Continuing Equity Owner’s redemption rights will be subject to certain customary limitations, including the expiration of any contractual lock-up period relating to the shares of our Class A common
180
Table of Contents
stock that may be applicable to such Continuing Equity Owner and the absence of any liens or encumbrances on such LLC Interests redeemed. Additionally, in the case we elect a cash settlement, such Continuing Equity Owner may rescind its redemption request within a specified period of time. Moreover, in the case of a settlement in Class A common stock, such redemption may be conditioned on the closing of an underwritten distribution of the shares of Class A common stock that may be issued in connection with such proposed redemption. In the case of a settlement in Class A common stock, such Continuing Equity Owner may also revoke or delay its redemption request if the following conditions exist: (1) any registration statement pursuant to which the resale of the Class A common stock to be registered for such Continuing Equity Owner at or immediately following the consummation of the redemption shall have ceased to be effective pursuant to any action or inaction by the SEC or no such resale registration statement has yet become effective; (2) we failed to cause any related prospectus to be supplemented by any required prospectus supplement necessary to effect such redemption; (3) we exercised our right to defer, delay or suspend the filing or effectiveness of a registration statement and such deferral, delay or suspension shall affect the ability of such Continuing Equity Owner to have its Class A common stock registered at or immediately following the consummation of the redemption; (4) such Continuing Equity Owner is in possession of any material non-public information concerning us, the receipt of which results in such Continuing Equity Owner being prohibited or restricted from selling Class A common stock at or immediately following the redemption without disclosure of such information (and we do not permit disclosure); (5) any stop order relating to the registration statement pursuant to which the Class A common stock was to be registered by such Continuing Equity Owner at or immediately following the redemption shall have been issued by the SEC; (6) there shall have occurred a material disruption in the securities markets generally or in the market or markets in which the Class A common stock is then traded; (7) there shall be in effect an injunction, a restraining order or a decree of any nature of any governmental entity that restrains or prohibits the redemption; (8) we shall have failed to comply in all material respects with our obligations under the Registration Rights Agreement, and such failure shall have affected the ability of such Continuing Equity Owner to consummate the resale of the Class A common stock to be received upon such redemption pursuant to an effective registration statement; or (9) the redemption date would occur three business days or less prior to, or during, a black-out period.
The GoHealth Holdings, LLC Agreement will require that in the case of a redemption by a Continuing Equity Owner we contribute cash or shares of our Class A common stock, as applicable, to GoHealth Holdings, LLC in exchange for an amount of newly-issued LLC Interests that will be issued to us equal to the number of LLC Interests redeemed from the Continuing Equity Owner. GoHealth Holdings, LLC will then distribute the cash or shares of our Class A common stock, as applicable, to such Continuing Equity Owner to complete the redemption. In the event of an election by a Continuing Equity Owner, we may, at our option, effect a direct exchange by GoHealth, Inc. of cash or our Class A common stock, as applicable, for such LLC Interests in lieu of such a redemption. Whether by redemption or exchange, we are obligated to ensure that at all times the number of LLC Interests that we own equals the number of our outstanding shares of Class A common stock (subject to certain exceptions for treasury shares and shares underlying certain convertible or exchangeable securities).
| • | Amendments. In addition to certain other requirements, our consent, as manager, and the consent of members holding a majority of the LLC Interests then outstanding and entitled to vote (excluding LLC Interests held directly or indirectly by us) will generally be required to amend or modify the GoHealth Holdings, LLC Agreement. |
Stockholders Agreement
Pursuant to the Stockholders Agreement, Centerbridge will have the right to designate of our directors, or the Centerbridge Directors, which will be Centerbridge Directors for as long as Centerbridge directly or indirectly, beneficially owns, in the aggregate, % or more of our Class A common stock (assuming that all
181
Table of Contents
outstanding LLC Interests in GoHealth Holdings, LLC are redeemed for newly-issued shares of our Class A common stock on a one-for-one basis), and our Founders shall have the right to designate of our directors, or the Founders Directors, which will be the Founders Directors for as long as our Founders directly or indirectly, beneficially own, in the aggregate, % or more of our Class A common stock (assuming that all outstanding LLC Interests are redeemed for newly-issued shares of our class A common stock on a one-for-one basis). Each of Centerbridge and our Founders will also agree to vote, or cause to vote, all of their outstanding shares of our Class A common stock and Class B common stock at any annual or special meeting of stockholders in which directors are elected, so as to cause the election of the Centerbridge Directors, Founders Directors and one of our Founders for as long as such individual is our Chief Executive Officer. Additionally, pursuant to the Stockholders Agreement, we shall take all commercially reasonable actions to cause (1) the board of directors to be comprised of at least directors or such other number of directors as our board of directors may determine; (2) the individuals designated in accordance with the terms of the Stockholders Agreement to be included in the slate of nominees to be elected to the board of directors at the next annual or special meeting of our stockholders at which directors are to be elected and at each annual meeting of our stockholders thereafter at which a director’s term expires; and (3) the individuals designated in accordance with the terms of the Stockholders Agreement to fill the applicable vacancies on the board of directors. The Stockholders Agreement allows for the board of directors to reject the nomination, appointment or election of a particular director if such nomination, appointment or election would constitute a breach of the board of directors’ fiduciary duties to our stockholders or does not otherwise comply with any requirements of our amended and restated certificate of incorporation or our amended and restated bylaws or the charter for, or related guidelines of, the board of directors’ nominating and corporate governance committee. See “Management—Composition of our Board of Directors.”
In addition, the Stockholders Agreement provides that for as long as beneficially own, directly or indirectly, in the aggregate, % or more of all issued and outstanding shares of our Class A common stock (assuming that all outstanding LLC Interests are redeemed for newly-issued shares of our Class A common stock on a one-for-one basis), we will not take, and will cause our subsidiaries not to take, certain actions (whether by merger, consolidation or otherwise) without the prior written approval of , including:
| • | ; and |
| • | . |
The Stockholders Agreement will terminate upon the earlier to occur of .
Registration Rights Agreement
We intend to enter into a Registration Rights Agreement with certain of the Continuing Equity Owners in connection with this offering. The Registration Rights Agreement will provide certain of the Continuing Equity Owners with “demand” registration rights whereby, at any time after 180 days following our initial public offering and the expiration of any related lock-up period, such Continuing Equity Owners can require us to register under the Securities Act the offer and sale of shares of Class A common stock issuable to them, at our election (determined solely by our independent directors (within the meaning of the Nasdaq rules) who are disinterested), upon redemption or exchange of their LLC Interests. The Registration Rights Agreement will also provide for customary “piggyback” registration rights for all parties to the agreement.
Employment Agreements
We intend to enter into an employment agreement with certain of our named executive officers in connection with this offering. See “Executive Compensation.”
182
Table of Contents
Directed Share Program
At our request, the underwriters have reserved for sale, at the initial public offering price, up to 5% of the Class A common stock offered by this prospectus for sale to certain of our directors, officers and employees through a directed share program. See “Underwriting—Directed Share Program” for more information.
Director and Officer Indemnification and Insurance
Prior to the consummation of this offering, we intend to enter into separate indemnification agreements with each of our directors and executive officers. We have also purchased directors’ and officers’ liability insurance. See “Description of Capital Stock—Limitations on Liability and Indemnification of Officers and Directors.”
Our Policy Regarding Related Party Transactions
Our board of directors will adopt a written related person transaction policy, to be effective upon the closing of this offering, setting forth the policies and procedures for the review and approval or ratification by our audit committee of related person transactions. This policy will cover, with certain exceptions set forth in Item 404 of Regulation S-K under the Securities Act, any transaction, arrangement or relationship, or any series of similar transactions, arrangements or relationships, in which we were or are to be a participant, where the amount involved exceeds $120,000 in any fiscal year and a related person had, has or will have a direct or indirect material interest, including without limitation, purchases of goods or services by or from the related person or entities in which the related person has a material interest, indebtedness, guarantees of indebtedness and employment by us of a related person. In reviewing and approving any such transactions, our audit committee is tasked to consider all relevant facts and circumstances, including, but not limited to, whether the transaction is on terms comparable to those that could be obtained in an arm’s length transaction and the extent of the related person’s interest in the transaction. All of the transactions described in this section occurred prior to the adoption of this policy.
183
Table of Contents
The following table sets forth information with respect to the beneficial ownership of our Class A common stock and Class B common stock (1) immediately following the consummation of the Transactions (excluding this offering), as described in “Our Organizational Structure” and (2) as adjusted to give effect to this offering, for:
| • | each person known by us to beneficially own more than 5% of our Class A common stock or our Class B common stock; |
| • | each of our directors; |
| • | each of our named executive officers; and |
| • | all of our executive officers and directors as a group. |
As described in “Our Organizational Structure” and “Certain Relationships and Related Party Transactions,” each common unit (other than LLC Interests held by us) is redeemable from time to time at each holder’s option for, at our election (determined solely by our independent directors (within the meaning of the Nasdaq rules) who are disinterested), newly-issued shares of our Class A common stock on a one-for-one basis or a cash payment equal to a volume weighted average market price of one share of Class A common stock for each LLC Interest so redeemed, in each case, in accordance with the terms of the GoHealth Holdings, LLC Agreement; provided that, at our election (determined solely by our independent directors (within the meaning of the Nasdaq rules) who are disinterested), we may effect a direct exchange by GoHealth, Inc. of such Class A common stock or such cash, as applicable, for such LLC Interests. The Continuing Equity Owners may, subject to certain exceptions, exercise such redemption right for as long as their LLC Interests remain outstanding. See “Certain Relationships and Related Party Transactions—GoHealth Holdings, LLC Agreement.” In connection with this offering, we will issue to each Continuing Equity Owner, for nominal consideration, one share of Class B common stock for each common unit of GoHealth Holdings, LLC such Continuing Equity Owner will own, respectively. As a result, the number of shares of Class B common stock listed in the table below correlates to the number of LLC Interests Centerbridge and our Founders will own immediately after the Transactions. Although the number of shares of Class A common stock being offered hereby to the public and the total number of LLC Interests outstanding after the offering will remain fixed regardless of the initial public offering price in this offering, the shares of Class B common stock held by the beneficial owners set forth in the table below after the consummation of the Transactions will vary, depending on the initial public offering price in this offering. The table below assumes the shares of Class A common stock are offered at $ per share (the midpoint of the estimated price range set forth on the cover page of this prospectus). See “Our Organizational Structure.”
The number of shares beneficially owned by each stockholder as described in this prospectus is determined under rules issued by the SEC. Under these rules, beneficial ownership includes any shares as to which the individual or entity has sole or shared voting power or investment power. In computing the number of shares beneficially owned by an individual or entity and the percentage ownership of that person, shares of common stock subject to options, or other rights, including the redemption right described above with respect to each common unit, held by such person that are currently exercisable or will become exercisable within 60 days of the date of this prospectus, are considered outstanding, although these shares are not considered outstanding for purposes of computing the percentage ownership of any other person. The percentage ownership of each individual or entity after giving effect to the Transactions and before this offering is computed on the basis of shares of our Class A common stock outstanding and shares of our Class B common stock outstanding. The percentage ownership of each individual or entity after the Transactions is computed on the basis of shares of our Class A common stock outstanding and shares of our Class B common stock outstanding. Unless otherwise indicated, the address of all listed stockholders is 214 West Huron Street, Chicago, Illinois 60654.
184
Table of Contents
Each of the stockholders listed has sole voting and investment power with respect to the shares beneficially owned by the stockholder unless noted otherwise, subject to community property laws where applicable.
| Class A Common Stock Beneficially Owned(1) |
Class B Common Stock Beneficially Owned |
Combined Voting Power(2) |
||||||||||||||||||||||||||||||||||||||||||||||||||||||
| After Giving Effect to the Transactions and Before this Offering |
After Giving Effect to the Transactions and this Offering (No Exercise Option) |
After Giving Effect to the Transactions and this Offering (With Full Exercise Option) |
After Giving Effect to the Transactions and Before this Offering |
After Giving Effect to the Transactions and this Offering (No Exercise Option) |
After Giving Effect to the Transactions and this Offering (With Full Exercise Option) |
After Giving Effect to the Transactions and this Offering (No Exercise Option) |
After Giving Effect to the Transactions and this Offering (With Full Exercise Option) |
|||||||||||||||||||||||||||||||||||||||||||||||||
| Name of beneficial owner |
Number | % | Number | % | Number | % | Number | % | Number | % | Number | % | % | % | ||||||||||||||||||||||||||||||||||||||||||
| 5% Stockholders |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Centerbridge Capital Partners III, L.P. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Named Executive Officers and Directors |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Clinton P. Jones |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Brandon M. Cruz |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Shane E. Cruz James A. Sharman |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Rahm Emanuel Joseph G. Flanagan |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Jeremy W. Gelber |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Miriam A. Tawil |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Alexander E. Timm |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| All directors, director designees and executive officers as a group ( persons) |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| * | Represents beneficial ownership of less than 1%. |
| (1) | Each common unit is redeemable from time to time at each holder’s option for, at our election (determined solely by our independent directors (within the meaning of the rules of the ) who are disinterested), newly-issued shares of our Class A common stock on a one-for-one basis or a cash payment equal to a volume weighted average market price of one share of Class A common stock for each LLC Interest so redeemed, in each case, in accordance with the terms of the GoHealth Holdings, LLC Agreement; provided that, at our election (determined solely by our independent directors (within the meaning of the rules of the ) who are disinterested), we may effect a direct exchange by GoHealth, Inc. of such Class A common stock or such cash, as applicable, for such LLC Interests. The Continuing Equity Owners may, subject to certain exceptions, exercise such redemption right for as long as their LLC Interests remain outstanding. See “Certain Relationships and Related Party Transactions—GoHealth Holdings, LLC Agreement.” In these tables, beneficial ownership of LLC Interests has been reflected as beneficial ownership of shares of our Class A common stock for which such LLC Interests may be exchanged. When a common unit is exchanged by Centerbridge, who holds shares of our Class B common stock, a corresponding share of Class B common stock will be cancelled. |
| (2) | Represents the percentage of voting power of our Class A common stock and Class B common stock voting as a single class. Each share of Class A common stock entitles the registered holder to one vote per share and each share of Class B common stock entitles the registered holder thereof to votes per share on all matters presented to stockholders for a vote generally, including the election of directors. The Class A common stock and Class B common stock will vote as a single class on all matters except as required by law or our amended and restated certificate of incorporation. |
185
Table of Contents
General
Prior to the consummation of this offering, we will file an amended and restated certificate of incorporation and we will adopt our amended and restated bylaws. Our amended and restated certificate of incorporation will authorize capital stock consisting of:
| • | shares of Class A common stock, par value $ per share; |
| • | shares of Class B common stock, par value $ per share; and |
| • | shares of preferred stock, par value $ per share. |
We are selling shares of Class A common stock in this offering ( shares if the underwriters exercise in full their option to purchase additional shares of our Class A common stock). All shares of our Class A common stock outstanding upon consummation of this offering will be fully paid and non-assessable. We are issuing shares of Class B common stock to the Continuing Equity Owners in connection with the Transactions for nominal consideration.
The following summary describes the material provisions of our capital stock. We urge you to read our amended and restated certificate of incorporation and our amended and restated bylaws, which are included as exhibits to the registration statement of which this prospectus forms a part.
Certain provisions of our amended and restated certificate of incorporation and our amended and restated bylaws summarized below may be deemed to have an anti-takeover effect and may delay or prevent a tender offer or takeover attempt that a stockholder might consider in its best interest, including those attempts that might result in a premium over the market price for the shares of common stock.
Common Stock
Class A Common Stock
Holders of shares of our Class A common stock are entitled to one vote for each share held of record on all matters submitted to a vote of stockholders.
Holders of shares of our Class A common stock are entitled to receive dividends when and if declared by our board of directors out of funds legally available therefor, subject to any statutory or contractual restrictions on the payment of dividends and to any restrictions on the payment of dividends imposed by the terms of any outstanding preferred stock.
Upon our dissolution or liquidation, after payment in full of all amounts required to be paid to creditors and to the holders of preferred stock having liquidation preferences, if any, the holders of shares of our Class A common stock will be entitled to receive pro rata our remaining assets available for distribution.
Holders of shares of our Class A common stock do not have preemptive, subscription, redemption or conversion rights. There will be no redemption or sinking fund provisions applicable to the Class A common stock.
Class B Common Stock
Each share of our Class B common stock entitles its holders to one vote per share on all matters presented to our stockholders generally.
Shares of Class B common stock will be issued in the future only to the extent necessary to maintain a one-to-one ratio between the number of LLC Interests held by the Continuing Equity Owners and the number of shares of
186
Table of Contents
Class B common stock issued to the Continuing Equity Owners. Shares of Class B common stock are transferable only together with an equal number of LLC Interests. Only permitted transferees of LLC Interests held by the Continuing Equity Owners will be permitted transferees of Class B common stock. See “Certain Relationships and Related Party Transactions—GoHealth Holdings, LLC Agreement.”
Holders of shares of our Class B common stock will vote together with holders of our Class A common stock as a single class on all matters presented to our stockholders for their vote or approval, except for certain amendments to our amended and restated certificate of incorporation described below or as otherwise required by applicable law or the amended and restated certificate of incorporation.
Holders of our Class B common stock do not have any right to receive dividends or to receive a distribution upon dissolution or liquidation. Additionally, holders of shares of our Class B common stock do not have preemptive, subscription, redemption or conversion rights. There will be no redemption or sinking fund provisions applicable to the Class B common stock. Any amendment of our amended and restated certificate of incorporation that gives holders of our Class B common stock (1) any rights to receive dividends or any other kind of distribution, (2) any right to convert into or be exchanged for Class A common stock or (3) any other economic rights will require, in addition to stockholder approval, the affirmative vote of holders of our Class A common stock voting separately as a class.
Upon the consummation of the Transactions, the Continuing Equity Owners will own, in the aggregate, shares of our Class B common stock.
Preferred Stock
Upon the consummation of the Transactions and the effectiveness of our amended and restated certificate of incorporation that will become effective immediately prior to the consummation of the Transactions, the total of our authorized shares of preferred stock will be shares. Upon the consummation of the Transactions, we will have no shares of preferred stock outstanding.
Under the terms of our amended and restated certificate of incorporation that will become effective immediately prior to the consummation of the Transactions, our board of directors is authorized to direct us to issue shares of preferred stock in one or more series without stockholder approval. Our board of directors has the discretion to determine the rights, preferences, privileges and restrictions, including voting rights, dividend rights, conversion rights, redemption privileges and liquidation preferences, of each series of preferred stock.
The purpose of authorizing our board of directors to issue preferred stock and determine its rights and preferences is to eliminate delays associated with a stockholder vote on specific issuances. The issuance of preferred stock, while providing flexibility in connection with possible acquisitions, future financings and other corporate purposes, could have the effect of making it more difficult for a third party to acquire, or could discourage a third party from seeking to acquire, a majority of our outstanding voting stock. Additionally, the issuance of preferred stock may adversely affect the holders of our Class A common stock by restricting dividends on the Class A common stock, diluting the voting power of the Class A common stock or subordinating the liquidation rights of the Class A common stock. As a result of these or other factors, the issuance of preferred stock could have an adverse impact on the market price of our Class A common stock.
Registration Rights
We intend to enter into a Registration Rights Agreement with certain of the Continuing Equity Owners in connection with this offering pursuant to which such parties will have specified rights to require us to register all or a portion of their shares under the Securities Act. See “Certain Relationships and Related Party Transactions—Registration Rights Agreement.”
187
Table of Contents
Forum Selection
Our amended and restated certificate of incorporation will provide (A) (i) any derivative action or proceeding brought on behalf of the Company, (ii) any action asserting a claim of breach of a fiduciary duty owed by any current or former director, officer, other employee or stockholder of the Company to the Company or the Company’s stockholders, (iii) any action asserting a claim arising pursuant to any provision of the DGCL, our amended and restated certificate of incorporation or our amended and restated bylaws (as either may be amended or restated) or as to which the DGCL confers jurisdiction on the Court of Chancery of the State of Delaware or (iv) any action asserting a claim governed by the internal affairs doctrine of the law of the State of Delaware shall, to the fullest extent permitted by law, be exclusively brought in the Court of Chancery of the State of Delaware or, if such court does not have subject matter jurisdiction thereof, the federal district court of the State of Delaware; and (B) the federal district courts of the United States shall be the exclusive forum for the resolution of any complaint asserting a cause of action arising under the Securities Act. Notwithstanding the foregoing, the exclusive forum provision shall not apply to claims seeking to enforce any liability or duty created by the Exchange Act. Our amended and restated certificate of incorporation will also provide that, to the fullest extent permitted by law, any person or entity purchasing or otherwise acquiring or holding any interest in shares of our capital stock shall be deemed to have notice of and consented to the foregoing. By agreeing to this provision, however, stockholders will not be deemed to have waived our compliance with the federal securities laws and the rules and regulations thereunder.
Dividends
Declaration and payment of any dividend will be subject to the discretion of our board of directors. The time and amount of dividends will be dependent upon our business prospects, results of operations, financial condition, cash requirements and availability, debt repayment obligations, capital expenditure needs, contractual restrictions, covenants in the agreements governing our current and future indebtedness, industry trends, the provisions of Delaware law affecting the payment of distributions to stockholders and any other factors our board of directors may consider relevant. We currently intend to retain all available funds and any future earnings to fund the development and growth of our business and to repay indebtedness, and therefore, do not anticipate declaring or paying any cash dividends on our Class A common stock in the foreseeable future. See “Dividend Policy” and “Risk Factors—Risks Related to the Offering and Ownership of our Class A Common Stock—Because we have no current plans to pay regular cash dividends on our Class A common stock following this offering, you may not receive any return on investment unless you sell your Class A common stock for a price greater than that which you paid for it.”
Anti-Takeover Provisions
Our amended and restated certificate of incorporation and amended and restated bylaws, as they will be in effect immediately prior to the consummation of the Transactions, will contain provisions that may delay, defer or discourage another party from acquiring control of us. We expect that these provisions, which are summarized below, will discourage coercive takeover practices or inadequate takeover bids. These provisions are also designed to encourage persons seeking to acquire control of us to first negotiate with our board of directors, which we believe may result in an improvement of the terms of any such acquisition in favor of our stockholders. However, they also give our board of directors the power to discourage acquisitions that some stockholders may favor.
Authorized but Unissued Shares
The authorized but unissued shares of our common stock and our preferred stock are available for future issuance without stockholder approval, subject to any limitations imposed by the Nasdaq rules. These additional shares may be used for a variety of corporate finance transactions, acquisitions and employee benefit plans and, as described under “Certain Relationships and Related Party Transactions—GoHealth Holdings, LLC Agreement—
188
Table of Contents
Agreement in Effect Upon Consummation of the Transactions—Common Unit Redemption Right,” funding of redemptions of LLC Interests. The existence of authorized but unissued and unreserved common stock and preferred stock could make more difficult or discourage an attempt to obtain control of us by means of a proxy contest, tender offer, merger or otherwise.
Classified Board of Directors
Our amended and restated certificate of incorporation will provide that our board of directors will be divided into three classes, with the classes as nearly equal in number as possible and each class serving three-year staggered terms. Pursuant to the terms of the Stockholders Agreement, directors designated by Centerbridge may only be removed with or without cause by the request of the party entitled to designate such director. In all other cases and at any other time, directors may only be removed from our board of directors for cause by the affirmative vote of a majority of the shares entitled to vote. See “Management—Composition of our Board of Directors.” These provisions may have the effect of deferring, delaying or discouraging hostile takeovers, or changes in control of us or our management.
Stockholder Action by Written Consent
Our amended and restated certificate of incorporation will provide that at any time when Centerbridge beneficially owns, in the aggregate, at least forty percent (40%) in voting power of the corporation entitled to vote generally in the election of directors, any action required or permitted to be taken by our stockholders at an annual meeting or special meeting of stockholders may be taken without a meeting, without prior notice and without a vote, if a written consent, setting forth the action so taken, is signed by the holders of our outstanding shares of common stock representing not less than the minimum number of votes that would be necessary to authorize such action at a meeting at which all outstanding shares of common stock entitled to vote thereon were present and voted and such consent is delivered to us in accordance with applicable law.
Special Meetings of Stockholders
Our amended and restated bylaws will provide that only the chairperson of our board of directors or a majority of our board of directors may call special meetings of our stockholders.
Advance Notice Requirements for Stockholder Proposals and Director Nominations
In addition, our amended and restated bylaws will establish an advance notice procedure for stockholder proposals to be brought before an annual meeting of stockholders, including proposed nominations of candidates for election to our board of directors; provided, however, that so long as Centerbridge is entitled to nominate a director pursuant to the Stockholders Agreement, such advance notice provisions will not apply to Centerbridge in connection with the nomination of directors. In order for any matter to be “properly brought” before a meeting, a stockholder will have to comply with advance notice and duration of ownership requirements and provide us with certain information. Stockholders at an annual meeting may only consider proposals or nominations specified in the notice of meeting or brought before the meeting by or at the direction of our board of directors or by a qualified stockholder of record on the record date for the meeting, who is entitled to vote at the meeting and who has delivered timely written notice in proper form to our secretary of the stockholder’s intention to bring such business before the meeting. These provisions could have the effect of delaying stockholder actions that are favored by the holders of a majority of our outstanding voting securities until the next stockholder meeting.
Amendment of Certificate of Incorporation or Bylaws
The Delaware General Corporation Law provides generally that the affirmative vote of a majority of the shares entitled to vote on any matter is required to amend a corporation’s certificate of incorporation or bylaws, unless a corporation’s certificate of incorporation or bylaws, as the case may be, requires a greater percentage. Upon
189
Table of Contents
consummation of the Transactions, our bylaws may be amended or repealed by (i) a majority vote of our board of directors or (ii) at any time when Centerbridge beneficially owns, in the aggregate, less than forty percent (40%) in voting power of the corporation entitled to vote generally in the election of directors, by the affirmative vote of at least sixty-six and two-thirds percent (66 2/3%) of the voting power of all outstanding voting stock of the corporation entitled to vote, voting together as a single class.
Section 203 of the DGCL
We will opt out of Section 203 of the DGCL. However, our amended and restated certificate of incorporation will contain provisions that are similar to Section 203. Specifically, our amended and restated certificate of incorporation will provide that, subject to certain exceptions, we will not be able to engage in a “business combination” with any “interested stockholder” for three years following the date that the person became an interested stockholder, unless the interested stockholder attained such status with the approval of our board of directors or unless the business combination is approved in a prescribed manner. A “business combination” includes, among other things, a merger or consolidation involving us and the “interested stockholder” and the sale of more than 10% of our assets. In general, an “interested stockholder” is any entity or person beneficially owning 15% or more of our outstanding voting stock and any entity or person affiliated with or controlling or controlled by such entity or person.
However, under our amended and restated certificate of incorporation, Centerbridge and NVX Holdings, Inc. and any of their respective affiliates will not be deemed to be interested stockholders regardless of the percentage of our outstanding voting stock owned by them, and accordingly will not be subject to such restrictions.
Limitations on Liability and Indemnification of Officers and Directors
Our amended and restated certificate of incorporation and amended and restated bylaws provide indemnification for our directors and officers to the fullest extent permitted by the Delaware General Corporation Law. Prior to the consummation of the Transactions, we intend to enter into indemnification agreements with each of our directors and executive officers that may, in some cases, be broader than the specific indemnification provisions contained under Delaware law. In addition, as permitted by Delaware law, our amended and restated certificate of incorporation includes provisions that eliminate the personal liability of our directors for monetary damages resulting from breaches of certain fiduciary duties as a director. The effect of this provision is to restrict our rights and the rights of our stockholders in derivative suits to recover monetary damages against a director for breach of fiduciary duties as a director.
These provisions may be held not to be enforceable for violations of the federal securities laws of the United States.
Corporate Opportunity Doctrine
Delaware law permits corporations to adopt provisions renouncing any interest or expectancy in certain opportunities that are presented to the corporation or its officers, directors or stockholders. Our amended and restated certificate of incorporation will, to the maximum extent permitted from time to time by Delaware law, renounce any interest or expectancy that we have in, or right to be offered an opportunity to participate in, specified business opportunities that are from time to time presented to Centerbridge, any of our directors who are employees of or affiliated with Centerbridge, or any director or stockholder who is not employed by us or our subsidiaries. Our amended and restated certificate of incorporation will provide that, to the fullest extent permitted by law, Centerbridge, any of our directors who are employees of or affiliated with Centerbridge, or any director or stockholder who is not employed by us or our affiliates will not have any duty to refrain from (1) engaging in a corporate opportunity in the same or similar lines of business in which we or our affiliates now engage or propose to engage or (2) otherwise competing with us or our affiliates. In addition, to the fullest extent permitted by law, if Centerbridge, any of our directors who are employees of or affiliated with Centerbridge, or any director or stockholder who is not employed by us or our subsidiaries acquires knowledge of a potential
190
Table of Contents
transaction or other business opportunity which may be a corporate opportunity for itself or himself or its or his affiliates or for us or our affiliates, such person will have no duty to communicate or offer such transaction or business opportunity to us or any of our affiliates and they may take any such opportunity for themselves or offer it to another person or entity, unless such opportunity was expressly offered to them solely in their capacity as a director, executive officer or employee of us or our affiliates. To the fullest extent permitted by Delaware law, no potential transaction or business opportunity may be deemed to be a corporate opportunity of the corporation or its subsidiaries unless (1) we or our subsidiaries would be permitted to undertake such transaction or opportunity in accordance with the amended and restated certificate of incorporation, (2) we or our subsidiaries, at such time have sufficient financial resources to undertake such transaction or opportunity, (3) we have an interest or expectancy in such transaction or opportunity, and (4) such transaction or opportunity would be in the same or similar line of our or our subsidiaries’ business in which we or our subsidiaries are engaged or a line of business that is reasonably related to, or a reasonable extension of, such line of business. Our amended and restated certificate of incorporation will not renounce our interest in any business opportunity that is expressly offered to an employee director or employee in his or her capacity as a director or employee of GoHealth, Inc.
Dissenters’ Rights of Appraisal and Payment
Under the DGCL, with certain exceptions, our stockholders will have appraisal rights in connection with a merger or consolidation of GoHealth, Inc. Pursuant to the DGCL, stockholders who properly request and perfect appraisal rights in connection with such merger or consolidation will have the right to receive payment of the fair value of their shares as determined by the Delaware Court of Chancery.
Stockholders’ Derivative Actions
Under the DGCL, any of our stockholders may bring an action in our name to procure a judgment in our favor, also known as a derivative action, provided that the stockholder bringing the action is a holder of our shares at the time of the transaction to which the action relates or such stockholder’s stock thereafter devolved by operation of law.
Transfer Agent and Registrar
The transfer agent and registrar for our Class A common stock is American Stock Transfer & Trust Company, LLC.
Trading Symbol and Market
We have applied to list our Class A common stock on The Nasdaq Global Market under the symbol “GHTH.”
191
Table of Contents
Credit Facilities
General
On September 13, 2019, in connection with the Centerbridge Acquisition, Norvax, LLC, or the Borrower, entered into a first lien credit agreement, or the Credit Agreement, which provides for the following:
| • | a $300.0 million aggregate principal amount senior secured term loan facility, or the Term Loan Facility; and |
| • | a $30.0 million aggregate principal amount senior secured revolving credit facility, or the Revolving Credit Facility. |
On March 20, 2020, the Borrower entered into an amendment to the Credit Agreement, which provides $117.0 million of incremental term loans, or the Incremental Term Loan Facility.
As of March 31, 2020, we had $298.5 million and $117.0 million outstanding under the Term Loan Facility and the Incremental Term Loan Facility, respectively. As of March 31, 2020, our capacity under the Revolving Credit Facility was $30.0 million, with $30.0 million available for additional borrowings.
Additionally, on May 7, 2020, the Borrower entered into an amendment to the Credit Agreement, which provides $20.0 million of additional revolving commitment under the Credit Facilities, or the Incremental Revolving Loan Facility.
We collectively refer to the Term Loan Facility, the Revolving Credit Facility, the Incremental Term Loan Facility and the Incremental Revolving Loan Facility as the Credit Facilities.
Interest Rates and Fees
Borrowings under the Credit Facilities are, at the option of the Borrower, either alternate base rate, or ABR, loans or LIBO Rate loans. Term loans, incremental term loans and revolving loans comprising each ABR borrowing under the Credit Facilities accrue interest at the ABR plus an applicable rate equal to 5.50% per annum. Term loans, incremental term loans and revolving loans comprising each LIBO Rate borrowing bear interest at the LIBO Rate plus an applicable rate equal to 6.50% per annum.
In addition to paying interest on the principal amounts outstanding under the Credit Facilities, the Borrower is required to pay a commitment fee of 0.50% per annum under the Revolving Credit Facility in respect of the unutilized commitments thereunder. The Borrower is also subject to customary letter of credit and agency fees.
Mandatory Prepayments
The Credit Agreement requires that the Borrower, following the end of each fiscal year, commencing with the fiscal year ending December 31, 2020, repay the outstanding principal amount of all term loans under the Credit Facilities in an aggregate amount equal to (A) 50% of the excess cash flow of the Borrower and its restricted subsidiaries for such fiscal year if the Total Net Cash Leverage Ratio (as defined in the Credit Agreement) is greater than 4.50:1.00, which percentage is reduced to 25% if the Total Net Cash Leverage Ratio is less than or equal to 4.50:1.00 and greater than 4.00:1.00, which percentage is further reduced to 0% if the Total Net Cash Leverage Ratio is less than or equal to 4.00:1.00, minus (B) at the option of the Borrower, (x) the aggregate amount of certain voluntary prepayments of term loans under the Credit Agreement during such fiscal year or after year-end and prior to the time such Excess Cash Flow prepayment is due, (y) the aggregate principal amount of any voluntary prepayments of indebtedness under pari passu incremental facilities, incremental equivalent debt and/or certain refinancing indebtedness, made during such fiscal year or after such fiscal year and prior to the time such prepayment is due.
192
Table of Contents
The Credit Agreement requires the Borrower to repay amounts equal to 100% of the net cash proceeds of certain asset sales or other dispositions of property (including insurance and condemnation proceeds ); provided, that, in the case of any prepayment events required in connection with certain dispositions and casualty events, if the net proceeds therefrom are invested (or committed to be invested) within 12 months after the receipt of such net proceeds, then no prepayment shall be required except to the extent such net proceeds have not been so invested (or committed to be invested) by the end of such 12-month period.
The Credit Agreement requires 100% of the net proceeds from the issuance or incurrence of certain indebtedness to be applied to prepay the term loans under the Term Loan Facility and the Incremental Term Loan Facility, except to the extent the indebtedness constitutes refinancing indebtedness.
Voluntary Prepayment
The Borrower may voluntarily prepay outstanding borrowings under the Credit Facilities at any time in whole or in part without premium or penalty; provided, that, with respect to voluntary prepayments of the Term Loan Facility and the Incremental Term Loan Facility and in certain other circumstances, the Borrower may have to pay a prepayment premium.
Amortization and Final Maturity
The Term Loan Facility is payable in quarterly installments (commencing on December 31, 2019) in the principal amount of 0.25% of the original principal amount of the Term Loan Facility. The remaining unpaid balance on the Term Loan Facility, together with all accrued and unpaid interest thereon, is due and payable on or prior to September 13, 2025. The Incremental Term Loan Facility is payable in quarterly installments (commencing on June 30, 2020) in the principal amount of 0.25% of the original principal amount of the Incremental Term Loan Facility. The remaining unpaid balance on the Term Loan Facility and the Incremental Term Loan Facility, together with all accrued and unpaid interest thereon, is due and payable on or prior to September 13, 2025. Outstanding borrowings under the Revolving Credit Facility do not amortize and are due and payable on September 13, 2024.
Guarantees and Security
The Borrower’s obligations under the Credit Facilities are guaranteed by Blizzard Midco, LLC and certain of the Borrower’s subsidiaries. All obligations under the Credit Agreement are secured by a first priority lien on substantially all of the assets of the Borrower, including a pledge of all of the equity interests of its subsidiaries.
Covenants and Other Matters
The Credit Agreement contains a number of covenants that, among other things and subject to certain exceptions, restrict the Borrower’s and its restricted subsidiaries’ ability to:
| • | incur indebtedness; |
| • | incur certain liens; |
| • | consolidate, merge or sell or otherwise dispose of assets; |
| • | make investments, loans, advances, guarantees and acquisitions; |
| • | pay dividends or make other distributions on equity interests, or redeem, repurchase or retire equity interests; |
| • | enter into transactions with affiliates; |
| • | alter the business conducted by us and our subsidiaries; |
| • | change their fiscal year; and |
| • | amend or modify governing documents. |
193
Table of Contents
In addition, the Credit Agreement contains financial covenants with respect to each of the Total Net Leverage Ratio, LTV Ratio and Liquidity, as detailed below.
| • | If the Borrower’s Total Net Cash Leverage Ratio requires the Borrower to maintain a Total Net Leverage Ratio no greater than (i) for the fiscal quarter ending on March 31, 2020 to and including the fiscal quarter ending on June 30, 2020, 4.50:1.00, (ii) for the fiscal quarter ending on September 30, 2020 to and including the fiscal quarter ending on December 31, 2020, 4.00:1.00, (iii) for the fiscal quarter ending on March 31, 2021 to and including the fiscal quarter ending on December 31, 2021, 3.50:1.00 and (iv) for the fiscal quarter ending on March 31, 2022 and each fiscal quarter ending thereafter, 3.00:1.00, tested as of the last day of each fiscal quarter and determined on the basis of the four consecutive most recently ended fiscal quarters of the Borrower for which financial statements have been delivered pursuant to the Credit Agreement. |
| • | If the Borrower’s Total Net Cash Leverage Ratio is greater than 5.50:1.00, the LTV Covenant requires the Borrower to maintain a LTV Ratio no greater than (i) for the fiscal quarter ending on March 31, 2020 to and including the fiscal quarter ending on June 30, 2020, 2.50:1.00, (ii) for the fiscal quarter ending on September 30, 2020 to and including the fiscal quarter ending on December 31, 2020, 2.00:1.00, (iii) for the fiscal quarter ending on March 31, 2021, 1.50:1.00, (iv) for the fiscal quarter ending on June 30, 2021 to and including the fiscal quarter ending on December 31, 2021, 1.25:1.00 and (v) for the fiscal quarter ending on March 31, 2022 and each fiscal quarter ending thereafter, 1.00:1.00, tested as of the last day of each fiscal quarter and determined on the basis of the four consecutive most recently ended fiscal quarters of the Borrower for which financial statements have been delivered pursuant to the Credit Agreement. |
| • | At all times, the Minimum Liquidity Covenant requires the Borrower to maintain Liquidity of no less than $10 million. |
The Company is in compliance with all covenants as of March 31, 2020.
The Credit Agreement also contains certain customary representations and warranties and affirmative covenants, and certain reporting obligations. In addition, the lenders under the Credit Facilities will be permitted to accelerate all outstanding borrowings and other obligations, terminate outstanding commitments and exercise other specified remedies upon the occurrence of certain events of default (subject to certain grace periods and exceptions), which include, among other things, payment defaults, breaches of representations and warranties, covenant defaults, certain cross-defaults and cross-accelerations to other indebtedness, certain events of bankruptcy and insolvency, certain judgments and changes of control.
The foregoing summary describes the material provisions of the Credit Agreement, but may not contain all information that is important to you. We urge you to read the provisions of the Credit Agreement, which has been filed as an exhibit to the registration statement of which this prospectus forms a part.
194
Table of Contents
SHARES ELIGIBLE FOR FUTURE SALE
Immediately prior to this offering, there was no public market for our Class A common stock. Future sales of substantial amounts of Class A common stock in the public market (including shares of Class A common stock issuable upon redemption or exchange of LLC Interests of our Continuing Equity Owners), or the perception that such sales may occur, could adversely affect the market price of our Class A common stock. Although we intend to apply to have our Class A common stock listed on the , we cannot assure you that there will be an active public market for our Class A common stock.
Upon the closing of this offering, we will have outstanding an aggregate of shares of Class A common stock, assuming the issuance of shares of Class A common stock offered by us in this offering and the issuance of shares of Class A common stock to the Blocker Shareholders in the Transactions. Of these shares, all shares sold in this offering will be freely tradable without restriction or further registration under the Securities Act, except for any shares purchased by our “affiliates,” as that term is defined in Rule 144 under the Securities Act, whose sales would be subject to the Rule 144 resale restrictions described below, other than the holding period requirement, and any Class A common stock purchased by our directors, officers and employees pursuant to our Directed Share Program shall be subject to the lock-up agreements as described below under “—Lock-Up Agreements.”
The remaining shares of Class A common stock will be “restricted securities,” as that term is defined in Rule 144 under the Securities Act. These restricted securities are eligible for public sale only if they are registered under the Securities Act or if they qualify for an exemption from registration under the Securities Act, including Rules 144 or 701 under the Securities Act, which are summarized below.
In addition, each common unit held by our Continuing Equity Owners will be redeemable, at the election of each Continuing Equity Owner, for, at our election (determined solely by our independent directors (within the meaning of the rules of the ) who are disinterested), newly-issued shares of our Class A common stock on a one-for-one basis or a cash payment equal to a volume weighted average market price of one share of Class A common stock for LLC Interest so redeemed, in each case, in accordance with the terms of the GoHealth Holdings, LLC Agreement; provided that, at our election (determined solely by our independent directors (within the meaning of the rules of the ) who are disinterested), we may effect a direct exchange by GoHealth, Inc. of such Class A common stock or such cash, as applicable, for such LLC Interests. The Continuing Equity Owners may, subject to certain exceptions, exercise such redemption right for as long as their LLC Interests remain outstanding. See “Certain Relationships and Related Party Transactions—GoHealth Holdings, LLC Agreement.” Upon consummation of the Transactions, our Continuing Equity Owners will hold LLC Interests, all of which will be exchangeable for shares of our Class A common stock. The shares of Class A common stock we issue upon such exchanges would be “restricted securities” as defined in Rule 144 unless we register such issuances. However, we will enter into a Registration Rights Agreement with certain of the Original Equity Owners that will require us, subject to customary conditions, to register under the Securities Act these shares of Class A common stock. See “Certain Relationships and Related Party Transactions—Registration Rights Agreement.”
Lock-Up Agreements
We, our officers and directors and the Original Equity Owners will agree that, without the prior written consent of any two of Goldman Sachs & Co. LLC, BofA Securities, Inc. and Morgan Stanley & Co. LLC, we and they will not, subject to certain exceptions, during the period ending 180 days after the date of this prospectus:
| • | offer, sell, contract to sell, pledge, grant any option to purchase, lend or otherwise dispose of any shares of our Class A common stock, or any options or warrants to purchase any shares of our Class A common stock, or any securities convertible into, or exchangeable for, or that represent the right to receive, shares of our Class A common stock; or |
195
Table of Contents
| • | engage in any hedging or other transaction or arrangement (including, without limitation, any short sale or the purchase or sale of, or entry into, any put or call option, or combination thereof, forward, swap or any other derivative transaction or instrument, however described or defined) which is designed to, or which reasonably could be expected to lead to, or result in, a sale, loan, pledge or other disposition of shares of our Class A common stock or any securities convertible into or exercisable or exchangeable for shares of our Class A common stock, |
whether any transaction described above is to be settled by delivery of our Class A common stock or such other securities, in cash or otherwise.
Upon the expiration of the applicable lock-up periods, substantially all of the shares subject to such lock-up restrictions will become eligible for sale, subject to the limitations discussed above.
Rule 144
In general, a person who has beneficially owned our Class A common stock that are restricted shares for at least six months would be entitled to sell such securities, provided that (1) such person is not deemed to have been one of our affiliates at the time of, or at any time during the 90 days preceding, a sale and (2) we are subject to the Exchange Act periodic reporting requirements for at least 90 days before the sale. Persons who have beneficially owned our Class A common stock that are restricted shares for at least six months but who are our affiliates at the time of, or any time during the 90 days preceding, a sale, would be subject to additional restrictions, by which such person would be entitled to sell within any three month period only a number of securities that does not exceed the greater of either of the following:
| • | 1% of the number of our Class A common stock then outstanding; or |
| • | the average weekly trading volume of our Class A common stock on the Nasdaq during the four calendar weeks preceding the filing of a notice on Form 144 with respect to the sale; provided, in each case, that we are subject to the Exchange Act periodic reporting requirements for at least 90 days before the sale. Such sales both by affiliates and by non-affiliates must also comply with the manner of sale, current public information and notice provisions of Rule 144 to the extent applicable. |
Rule 701
In general, under Rule 701, any of our employees, directors, officers, consultants or advisors who purchases shares from us in connection with a compensatory stock or option plan or other written agreement before the effective date of the registration statement of which this prospectus forms a part is entitled to sell such shares 90 days after such effective date in reliance on Rule 144. Our affiliates can resell shares in reliance on Rule 144 without having to comply with the holding period requirement, and non-affiliates of the issuer can resell shares in reliance on Rule 144 without having to comply with the current public information and holding period requirements.
The SEC has indicated that Rule 701 will apply to typical stock options granted by an issuer before it becomes subject to the reporting requirements of the Exchange Act, along with the shares acquired upon exercise of such options, including exercises after an issuer becomes subject to the reporting requirements of the Exchange Act.
Equity Plans
We intend to file one or more registration statements on Form S-8 under the Securities Act to register the offer and sale of all shares of Class A common stock subject to outstanding stock options and Class A common stock issued or issuable under our 2020 Plan. As of the date of this prospectus, options to purchase LLC Interests were outstanding and stock options covering a total of approximately shares of our Class A common stock are intended to be granted to certain of our directors, executive officers and other employees in connection with this offering.
196
Table of Contents
We expect to file the registration statement covering shares offered pursuant to our 2020 Plan shortly after the date of this prospectus, permitting the resale of such shares by nonaffiliates in the public market without restriction under the Securities Act and the sale by affiliates in the public market subject to compliance with the resale provisions of Rule 144.
Registration Rights
See “Certain Relationships and Related Party Transactions—Registration Rights Agreement.”
197
Table of Contents
MATERIAL U.S. FEDERAL INCOME TAX CONSIDERATIONS
TO NON-U.S. HOLDERS OF CLASS A COMMON STOCK
The following discussion is a summary of the material U.S. federal income tax consequences to Non-U.S. Holders (as defined below) of the purchase, ownership and disposition of our Class A common stock issued pursuant to this offering, but does not purport to be a complete analysis of all potential tax effects. The effects of other U.S. federal tax laws, such as estate and gift tax laws, and any applicable state, local or non-U.S. tax laws are not discussed. This discussion is based on the U.S. Internal Revenue Code of 1986, as amended (the “Code”), Treasury Regulations promulgated thereunder, judicial decisions, and published rulings and administrative pronouncements of the U.S. Internal Revenue Service (the “IRS”), in each case in effect as of the date hereof. These authorities may change or be subject to differing interpretations. Any such change or differing interpretation may be applied retroactively in a manner that could adversely affect a Non-U.S. Holder of our Class A common stock. We have not sought and will not seek any rulings from the IRS regarding the matters discussed below. There can be no assurance the IRS or a court will not take a contrary position to that discussed below regarding the tax consequences of the purchase, ownership and disposition of our Class A common stock.
This discussion is limited to Non-U.S. Holders that hold our Class A common stock as a “capital asset” within the meaning of Section 1221 of the Code (generally, property held for investment). This discussion does not address all U.S. federal income tax consequences relevant to a Non-U.S. Holder’s particular circumstances, including the impact of the Medicare contribution tax on net investment income. In addition, it does not address consequences relevant to Non-U.S. Holders subject to special rules, including, without limitation:
| • | U.S. expatriates and former citizens or long-term residents of the United States; |
| • | persons subject to the alternative minimum tax; |
| • | persons holding our Class A common stock as part of a hedge, straddle or other risk reduction strategy or as part of a conversion transaction or other integrated investment; |
| • | banks, insurance companies, and other financial institutions; |
| • | brokers, dealers or traders in securities; |
| • | “controlled foreign corporations,” “passive foreign investment companies,” and corporations that accumulate earnings to avoid U.S. federal income tax; |
| • | partnerships or other entities or arrangements treated as partnerships for U.S. federal income tax purposes (and investors therein); |
| • | tax-exempt organizations or governmental organizations; |
| • | persons deemed to sell our Class A common stock under the constructive sale provisions of the Code; |
| • | persons who hold or receive our Class A common stock pursuant to the exercise of any employee stock option or otherwise as compensation; |
| • | tax-qualified retirement plans; |
| • | “qualified foreign pension funds” as defined in Section 897(l)(2) of the Code and entities all of the interests of which are held by qualified foreign pension funds; and |
| • | persons subject to special tax accounting rules as a result of any item of gross income with respect to the stock being taken into account in an applicable financial statement. |
If an entity treated as a partnership for U.S. federal income tax purposes holds our Class A common stock, the tax treatment of an owner in such an entity will depend on the status of the owner, the activities of such entity and certain determinations made at the owner level. Accordingly, entities treated as partnerships for U.S. federal income tax purposes holding our Class A common stock and the owners in such entities should consult their tax advisors regarding the U.S. federal income tax consequences to them.
198
Table of Contents
THIS DISCUSSION IS FOR INFORMATIONAL PURPOSES ONLY AND IS NOT TAX ADVICE. INVESTORS SHOULD CONSULT THEIR TAX ADVISORS WITH RESPECT TO THE APPLICATION OF THE U.S. FEDERAL INCOME TAX LAWS TO THEIR PARTICULAR SITUATIONS AS WELL AS ANY TAX CONSEQUENCES OF THE PURCHASE, OWNERSHIP AND DISPOSITION OF OUR CLASS A COMMON STOCK ARISING UNDER THE U.S. FEDERAL ESTATE OR GIFT TAX LAWS OR UNDER THE LAWS OF ANY STATE, LOCAL OR NON-U.S. TAXING JURISDICTION OR UNDER ANY APPLICABLE INCOME TAX TREATY.
Definition of a Non-U.S. Holder
For purposes of this discussion, a “Non-U.S. Holder” is any beneficial owner of our Class A common stock that is neither a “U.S. person” nor an entity treated as a partnership for U.S. federal income tax purposes. A U.S. person is any person that, for U.S. federal income tax purposes, is or is treated as any of the following:
| • | an individual who is a citizen or resident of the United States; |
| • | a corporation created or organized under the laws of the United States, any state thereof, or the District of Columbia; |
| • | an estate, the income of which is subject to U.S. federal income tax regardless of its source; or |
| • | a trust that (1) is subject to the primary supervision of a U.S. court and the control of one or more “United States persons” (within the meaning of Section 7701(a)(30) of the Code), or (2) has a valid election in effect to be treated as a United States person for U.S. federal income tax purposes. |
Distributions
As described in the section entitled “Dividend Policy,” we do not anticipate declaring or paying dividends to holders of our Class A common stock in the foreseeable future. However, if we do make distributions of cash or property on our Class A common stock, such distributions will constitute dividends for U.S. federal income tax purposes to the extent paid from our current or accumulated earnings and profits, as determined under U.S. federal income tax principles. Amounts not treated as dividends for U.S. federal income tax purposes will constitute a return of capital and first be applied against and reduce a Non-U.S. Holder’s adjusted tax basis in its Class A common stock, but not below zero. Any excess will be treated as capital gain and will be treated as described below under “—Sale or Other Taxable Disposition.”
Subject to the discussion below on effectively connected income, dividends paid to a Non-U.S. Holder of our Class A common stock will be subject to U.S. federal withholding tax at a rate of 30% of the gross amount of the dividends (or such lower rate specified by an applicable income tax treaty, provided the Non-U.S. Holder furnishes a valid IRS Form W-8BEN or W-8BEN-E (or other applicable documentation) certifying qualification for the lower treaty rate). A Non-U.S. Holder that does not timely furnish the required documentation, but that qualifies for a reduced treaty rate, may obtain a refund of any excess amounts withheld by timely filing an appropriate claim for refund with the IRS. Non-U.S. Holders should consult their tax advisors regarding their entitlement to benefits under any applicable income tax treaty.
If dividends paid to a Non-U.S. Holder are effectively connected with the Non-U.S. Holder’s conduct of a trade or business within the United States (and, if required by an applicable income tax treaty, the Non-U.S. Holder maintains a permanent establishment in the United States to which such dividends are attributable), the Non-U.S. Holder will be exempt from the U.S. federal withholding tax described above. To claim the exemption, the Non-U.S. Holder must furnish to the applicable withholding agent a valid IRS Form W-8ECI, certifying that the dividends are effectively connected with the Non-U.S. Holder’s conduct of a trade or business within the United States.
Any such effectively connected dividends will be subject to U.S. federal income tax on a net income basis at the regular graduated rates. A Non-U.S. Holder that is a corporation also may be subject to a branch profits tax at a
199
Table of Contents
rate of 30% (or such lower rate specified by an applicable income tax treaty) on such effectively connected dividends, as adjusted for certain items. Non-U.S. Holders should consult their tax advisors regarding any applicable tax treaties that may provide for different rules.
Sale or Other Taxable Disposition
A Non-U.S. Holder will not be subject to U.S. federal income tax on any gain realized upon the sale or other taxable disposition of our Class A common stock unless:
| • | the gain is effectively connected with the Non-U.S. Holder’s conduct of a trade or business within the United States (and, if required by an applicable income tax treaty, the Non-U.S. Holder maintains a permanent establishment in the United States to which such gain is attributable); |
| • | the Non-U.S. Holder is a nonresident alien individual present in the United States for 183 days or more during the taxable year of the disposition and certain other requirements are met; or |
| • | our common stock constitutes a U.S. real property interest (“USRPI”) by reason of our status as a U.S. real property holding corporation (“USRPHC”) for U.S. federal income tax purposes. |
Gain described in the first bullet point above generally will be subject to U.S. federal income tax on a net income basis at the regular graduated rates. A Non-U.S. Holder that is a corporation also may be subject to a branch profits tax at a rate of 30% (or such lower rate specified by an applicable income tax treaty) on such effectively connected gain, as adjusted for certain items.
Gain described in the second bullet point above will be subject to U.S. federal income tax at a rate of 30% (or such lower rate specified by an applicable income tax treaty), which may be offset by U.S. source capital losses of the Non-U.S. Holder (even though the individual is not considered a resident of the United States), provided the Non-U.S. Holder has timely filed U.S. federal income tax returns with respect to such losses.
With respect to the third bullet point above, we believe we currently are not, and do not anticipate becoming, a USRPHC. Because the determination of whether we are a USRPHC depends, however, on the fair market value of our USRPIs relative to the fair market value of our non-U.S. real property interests and our other business assets, there can be no assurance we currently are not a USRPHC or will not become one in the future. Even if we are or were to become a USRPHC, gain arising from the sale or other taxable disposition by a Non-U.S. Holder of our common stock will not be subject to U.S. federal income tax if our common stock is “regularly traded,” as defined by applicable Treasury Regulations, on an established securities market, and such Non-U.S. Holder owned, actually and constructively, 5% or less of our Class A common stock throughout the shorter of the five-year period ending on the date of the sale or other taxable disposition or the Non-U.S. Holder’s holding period.
Non-U.S. Holders should consult their tax advisors regarding potentially applicable income tax treaties that may provide for different rules.
Information Reporting and Backup Withholding
Payments of dividends on our Class A common stock will not be subject to backup withholding, provided the applicable withholding agent does not have actual knowledge or reason to know the holder is a United States person and the holder either certifies its non-U.S. status, such as by furnishing a valid IRS Form W-8BEN, W-8BEN-E or W-8ECI, or otherwise establishes an exemption. However, information returns are required to be filed with the IRS in connection with any distributions on our Class A common stock paid to the Non-U.S. Holder, regardless of whether such distributions constitute dividends or whether any tax was actually withheld. In addition, proceeds of the sale or other taxable disposition of our Class A common stock within the United States or conducted through certain U.S.-related brokers generally will not be subject to backup withholding or
200
Table of Contents
information reporting, if the applicable withholding agent receives the certification described above and does not have actual knowledge or reason to know that such holder is a United States person, or the holder otherwise establishes an exemption. Proceeds of a disposition of our Class A common stock conducted through a non-U.S. office of a non-U.S. broker generally will not be subject to backup withholding or information reporting.
Copies of information returns that are filed with the IRS may also be made available under the provisions of an applicable treaty or agreement to the tax authorities of the country in which the Non-U.S. Holder resides or is established.
Backup withholding is not an additional tax. Any amounts withheld under the backup withholding rules may be allowed as a refund or a credit against a Non-U.S. Holder’s U.S. federal income tax liability, provided the required information is timely furnished to the IRS.
Additional Withholding Tax on Payments Made to Foreign Accounts
Withholding taxes may be imposed under Sections 1471 to 1474 of the Code (such Sections commonly referred to as the Foreign Account Tax Compliance Act, or “FATCA”) on certain types of payments made to non-U.S. financial institutions and certain other non-U.S. entities. Specifically, a 30% withholding tax may be imposed on dividends on, or (subject to the proposed Treasury Regulations discussed below) gross proceeds from the sale or other disposition of, our Class A common stock paid to a “foreign financial institution” or a “non-financial foreign entity” (each as defined in the Code), unless (1) the foreign financial institution undertakes certain diligence and reporting obligations, (2) the non-financial foreign entity either certifies it does not have any “substantial United States owners” (as defined in the Code) or furnishes identifying information regarding each substantial United States owner, or (3) the foreign financial institution or non-financial foreign entity otherwise qualifies for an exemption from these rules. If the payee is a foreign financial institution and is subject to the diligence and reporting requirements in (1) above, it must enter into an agreement with the U.S. Department of the Treasury requiring, among other things, that it undertake to identify accounts held by certain “specified United States persons” or “United States owned foreign entities” (each as defined in the Code), annually report certain information about such accounts, and withhold 30% on certain payments to non-compliant foreign financial institutions and certain other account holders. Foreign financial institutions located in jurisdictions that have an intergovernmental agreement with the United States governing FATCA may be subject to different rules.
Under the applicable Treasury Regulations and administrative guidance, withholding under FATCA generally applies to payments of dividends on our Class A common stock. While withholding under FATCA would have applied also to payments of gross proceeds from the sale or other disposition of stock on or after January 1, 2019, proposed Treasury Regulations eliminate FATCA withholding on payments of gross proceeds entirely. Taxpayers generally may rely on these proposed Treasury Regulations until final Treasury Regulations are issued.
Prospective investors should consult their tax advisors regarding the potential application of withholding under FATCA to their investment in our common stock.
201
Table of Contents
We, GoHealth Holdings, LLC and Goldman Sachs & Co. LLC, BofA Securities, Inc., and Morgan Stanley & Co. LLC, acting as representatives of the underwriters named below, have entered into an underwriting agreement with respect to the shares of Class A common stock being offered. Subject to certain conditions, each underwriter has severally agreed to purchase the number of shares of Class A common stock indicated in the following table.
| Underwriters |
Number of Shares | |||
| Goldman Sachs & Co. LLC |
||||
| BofA Securities, Inc. |
||||
| Morgan Stanley & Co. LLC |
||||
| Barclays Capital Inc. |
||||
| Credit Suisse Securities (USA) LLC |
||||
| Evercore Group L.L.C |
||||
| RBC Capital Markets, LLC |
||||
| William Blair & Company, L.L.C |
||||
| Cantor Fitzgerald & Co. |
||||
| SunTrust Robinson Humphrey, Inc. |
||||
|
|
|
|||
| Total |
||||
|
|
|
|||
The underwriters are committed to take and pay for all of the shares of Class A common stock being offered, if any are taken, other than the shares of Class A common stock covered by the option described below unless and until this option is exercised.
The underwriters have an option to buy up to an additional shares of Class A common stock from us to cover sales by the underwriters of a greater number of shares of Class A common stock than the total number set forth in the table above. They may exercise that option for 30 days. If any shares of Class A common stock are purchased pursuant to this option, the underwriters will severally purchase shares of Class A common stock in approximately the same proportion as set forth in the table above.
The following tables show the per share and total underwriting discount to be paid to the underwriters by us. Such amounts are shown assuming both no exercise and full exercise of the underwriters’ option to purchase additional shares of Class A common stock.
| No Exercise |
Full Exercise |
|||||||
| Per Share |
$ | $ | ||||||
| Total |
$ | $ | ||||||
Shares of Class A common stock sold by the underwriters to the public will initially be offered at the initial public offering price set forth on the cover of this prospectus. Any shares of Class A common stock sold by the underwriters to securities dealers may be sold at a discount of up to $ per share of Class A common stock from the initial public offering price. After the initial offering of the shares of Class A common stock, the representatives may change the offering price and the other selling terms. The offering of the shares of Class A common stock by the underwriters is subject to receipt and acceptance and subject to the underwriters’ right to reject any order in whole or in part.
We and our officers, directors, and holders of substantially all of the Company’s common stock have agreed with the underwriters, subject to certain exceptions, not to dispose of or hedge any of their common stock or securities convertible into or exchangeable for shares of common stock during the period from the date of this prospectus continuing through the date 180 days after the date of this prospectus, except with the prior written consent of any two of Goldman Sachs & Co. LLC, BofA Securities, Inc. and Morgan Stanley & Co. LLC. This agreement does not apply to any existing employee benefit plans. See “Shares Eligible for Future Sale” for a discussion of certain transfer restrictions.
202
Table of Contents
Prior to the offering, there has been no public market for the shares of Class A common stock. The initial public offering price has been negotiated among us and the representatives. Among the factors to be considered in determining the initial public offering price of the shares of Class A common stock, in addition to prevailing market conditions, will be our historical performance, estimates our business potential and earnings prospects, an assessment of our management and the consideration of the above factors in relation to market valuation of companies in related businesses.
We have applied to list our Class A common stock on The Nasdaq Global Market under the symbol “GHTH.”
In connection with the offering, the underwriters may purchase and sell shares of Class A common stock in the open market. These transactions may include short sales, stabilizing transactions and purchases to cover positions created by short sales. Short sales involve the sale by the underwriters of a greater number of shares of Class A common stock than they are required to purchase in the offering, and a short position represents the amount of such sales that have not been covered by subsequent purchases. A “covered short position” is a short position that is not greater than the amount of additional shares of Class A common stock for which the underwriters’ option described above may be exercised. The underwriters may cover any covered short position by either exercising their option to purchase additional shares of Class A common stock or purchasing shares of Class A common stock in the open market. In determining the source of shares of Class A common stock to cover the covered short position, the underwriters will consider, among other things, the price of shares of Class A common stock available for purchase in the open market as compared to the price at which they may purchase additional shares of Class A common stock pursuant to the option described above. “Naked” short sales are any short sales that create a short position greater than the amount of additional shares of Class A common stock for which the option described above may be exercised. The underwriters must cover any such naked short position by purchasing shares of Class A common stock in the open market. A naked short position is more likely to be created if the underwriters are concerned that there may be downward pressure on the price of the common stock in the open market after pricing that could adversely affect investors who purchase in the offering. Stabilizing transactions consist of various bids for or purchases of common stock made by the underwriters in the open market prior to the completion of the offering.
The underwriters may also impose a penalty bid. This occurs when a particular underwriter repays to the underwriters a portion of the underwriting discount received by it because the representatives have repurchased shares of Class A common stock sold by or for the account of such underwriter in stabilizing or short covering transactions.
Purchases to cover a short position and stabilizing transactions, as well as other purchases by the underwriters for their own accounts, may have the effect of preventing or retarding a decline in the market price of the Class A common stock, and together with the imposition of the penalty bid, may stabilize, maintain or otherwise affect the market price of the Class A common stock. As a result, the price of the Class A common stock may be higher than the price that otherwise might exist in the open market. The underwriters are not required to engage in these activities and may end any of these activities at any time. These transactions may be effected on , in the over-the-counter market or otherwise.
Directed Share Program
At our request, the underwriters have reserved for sale, at the initial public offering price, up to 5% of the Class A common stock offered by this prospectus for sale to certain of our directors, officers and employees through a directed share program, or Directed Share Program. If these persons purchase reserved shares of Class A common stock, it will reduce the number of shares of Class A common stock available for sale to the general public. Any reserved shares of Class A common stock that are not so purchased will be offered by the underwriters to the general public on the same terms as the other shares of Class A common stock offered by this prospectus. Any shares sold in the Directed Share Program to a party who has entered into a lock-up agreement shall be subject to the provisions of such lock-up agreement.
European Economic Area and the United Kingdom
This prospectus is not a prospectus for the purposes of the Prospectus Regulation (as defined below). This prospectus and any offer if made subsequently is directed only at persons in Member States of the European Economic Area (the “EEA”)
203
Table of Contents
or in the United Kingdom (each, a “Relevant State”) who are “qualified investors” within the meaning of Article 2(e) of the Prospectus Regulation. This prospectus has been prepared on the basis that any offer of shares of Class A common stock in any Relevant State will be made pursuant to an exemption under the Prospectus Regulation from the requirement to publish a prospectus for offers of shares of Class A common stock. Accordingly any person making or intending to make an offer in that Relevant State of shares of Class A common stock which are the subject of the offering contemplated in this prospectus may only do so in circumstances in which no obligation arises for us or the underwriters to publish a prospectus pursuant to Article 3 of the Prospectus Regulation in relation to such offer. Neither us nor the underwriters have authorized, nor do they authorize, the making of any offer of shares of Class A common stock in circumstances in which an obligation arises for us or the underwriters to publish a prospectus for such offer.
In relation to each Relevant State, no offer of shares of Class A common stock which are the subject of the offering contemplated by this prospectus to the public may be made in that Relevant State other than:
| (a) | to any legal entity which is a qualified investor as defined in the Prospectus Regulation; |
| (b) | to fewer than 150 natural or legal persons (other than qualified investors as defined in the Prospectus Regulation), subject to obtaining the prior consent of the representatives for any such offer; or |
| (c) | in any other circumstances falling within Article 1(4) of the Prospectus Regulation, |
provided that no such offer of shares of Class A common stock shall require us or any representative to publish a prospectus pursuant to Article 3 of the Prospectus Regulation or supplement a prospectus pursuant to Article 23 of the Prospectus Regulation.
For the purposes of this provision, the expression an “offer to the public” in relation to any shares of Class A common stock in any Relevant State means the communication in any form and by any means of sufficient information on the terms of the offer and any shares of Class A common stock to be offered so as to enable an investor to decide to purchase or subscribe for any shares of Class A common stock, and the expression “Prospectus Regulation” means Regulation (EU) 2017/1129.
United Kingdom
This prospectus may not be distributed or circulated to any person in the United Kingdom other than to (i) persons who have professional experience in matters relating to investments falling within Article 19(5) of the Financial Services and Markets Act 2000 (Financial Promotion) Order 2005, as amended (the “Order”); and (ii) high net worth entities falling within Article 49(2)(a) to (d) of the Order (all such persons together being referred to as “relevant persons”). This prospectus is directed only at relevant persons. Other persons should not act on this prospectus or any of its contents. This prospectus is confidential and is being supplied to you solely for your information and may not be reproduced, redistributed or passed on to any other person or published, in whole or in part, for any other purpose.
Any invitation or inducement to engage in investment activity (within the meaning of Section 21 of the Financial Services and Markets Act 2000 (the “FSMA”)) in connection with the issue or sale of the shares of Class A common stock may only be communicated or caused to be communicated in circumstances in which Section 21(1) of the FSMA does not apply to us.
All applicable provisions of the FSMA must be complied with in respect to anything done by any person in relation to the shares of Class A common stock in, from or otherwise involving the United Kingdom.
Canada
The securities may be sold in Canada only to purchasers purchasing, or deemed to be purchasing, as principal that are accredited investors, as defined in National Instrument 45-106 Prospectus Exemptions or subsection 73.3(1) of the Securities Act (Ontario), and are permitted clients, as defined in National Instrument 31-103
204
Table of Contents
Registration Requirements, Exemptions, and Ongoing Registrant Obligations. Any resale of the securities must be made in accordance with an exemption form, or in a transaction not subject to, the prospectus requirements of applicable securities laws.
Securities legislation in certain provinces or territories of Canada may provide a purchaser with remedies for rescission or damages if this prospectus (including any amendment thereto) contains a misrepresentation, provided that the remedies for rescission or damages are exercised by the purchaser within the time limit prescribed by the securities legislation of the purchaser’s province or territory. The purchaser should refer to any applicable provisions of the securities legislation of the purchaser’s province or territory of these rights or consult with a legal advisor.
Pursuant to section 3A.3 of National Instrument 33-105 Underwriting Conflicts (NI 33-105), the underwriters are not required to comply with the disclosure requirements of NI 33-105 regarding underwriter conflicts of interest in connection with this offering.
Hong Kong
The shares of Class A common stock have not been and will not be offered or sold in Hong Kong by means of any document other than (i) to “professional investors” within the meaning of the Securities and Futures Ordinance of Hong Kong (Cap. 571, Laws of Hong Kong) (the “SFO”) and any rules made thereunder, or (ii) in other circumstances which do not result in the document being a “prospectus” within the meaning of the Companies (Winding Up and Miscellaneous Provisions) Ordinance of Hong Kong (Cap. 32, Laws of Hong Kong) (the “C(WUMP)O”) or which do not constitute an offer to the public within the meaning of the C(WUMP)O; and no advertisement, invitation or document relating to the shares of Class A common stock have been or will be issued or have been or will be in the possession of any person for the purpose of issue (in each case whether in Hong Kong or elsewhere), which is directed at, or the contents of which are likely to be accessed or read by, the public in Hong Kong (except if permitted to do so under the securities laws of Hong Kong) other than with respect to the shares of Class A common stock which are or are intended to be disposed of only to persons outside Hong Kong or only to “professional investors” within the meaning of the SFO and any rules made thereunder.
Singapore
This prospectus has not been registered as a prospectus with the Monetary Authority of Singapore. Accordingly, this prospectus and any other document or material in connection with the offer or sale, or invitation for subscription or purchase, of the shares of Class A common stock may not be circulated or distributed, nor may the shares of Class A common stock be offered or sold, or be made the subject of an invitation for subscription or purchase, whether directly or indirectly, to persons in Singapore other than (i) to an institutional investor (as defined under Section 4A of the Securities and Futures Act, Chapter 289 of Singapore (the “SFA”)) under Section 274 of the SFA, (ii) to a relevant person (as defined in Section 275(2) of the SFA) pursuant to Section 275(1) of the SFA, or any person pursuant to Section 275(1A) of the SFA, and in accordance with the conditions specified in Section 275 of the SFA and (where applicable) Regulation 3 of the Securities and Futures (Classes of Investors) Regulations 2018 or (iii) otherwise pursuant to, and in accordance with the conditions of, any other applicable provision of the SFA, in each case subject to conditions set forth in the SFA.
Where the shares of Class A common stock are subscribed or purchased under Section 275 of the SFA by a relevant person which is a corporation (which is not an accredited investor (as defined in Section 4A of the SFA)) the sole business of which is to hold investments and the entire share capital of which is owned by one or more individuals, each of whom is an accredited investor, the securities or securities-based derivatives (each as defined in Section 2(1) of the SFA) of that corporation shall not be transferable for 6 months after that corporation has acquired the shares of Class A common stock under Section 275 of the SFA except: (1) to an institutional investor under Section 274 of the SFA or to a relevant person (as defined in Section 275(2) of the SFA), (2)
205
Table of Contents
where such transfer arises from an offer in that corporation’s securities or securities-based derivatives pursuant to Section 275(1A) of the SFA, (3) where no consideration is or will be given for the transfer, (4) where the transfer is by operation of law, (5) as specified in Section 276(7) of the SFA, or (6) as specified in Regulation 37A of the Securities and Futures (Offers of Investments) (Shares and Securities-based Derivatives Contracts) Regulations 2018 of Singapore (“Regulation 37A”).
Where the shares of Class A common stock are subscribed or purchased under Section 275 of the SFA by a relevant person which is a trust (where the trustee is not an accredited investor (as defined in Section 4A of the SFA)) whose sole purpose is to hold investments and each beneficiary of the trust is an accredited investor, the beneficiaries‘ rights and interest (howsoever described) in that trust shall not be transferable for 6 months after that trust has acquired the shares of Class A common stock under Section 275 of the SFA except: (1) to an institutional investor under Section 274 of the SFA or to a relevant person (as defined in Section 275(2) of the SFA), (2) where such transfer arises from an offer that is made on terms that such rights or interest are acquired at a consideration of not less than S$200,000 (or its equivalent in a foreign currency) for each transaction (whether such amount is to be paid for in cash or by exchange of securities or securities-based derivatives or other assets), (3) where no consideration is or will be given for the transfer, (4) where the transfer is by operation of law, (5) as specified in Section 276(7) of the SFA, or (6) as specified in Regulation 37A.
Japan
The shares of Class A common stock have not been and will not be registered under the Financial Instruments and Exchange Act of Japan (Act No. 25 of 1948, as amended), or the FIEA. The shares of Class A common stock have not been and will not be offered or sold, directly or indirectly, in Japan or to or for the account or benefit of any resident of Japan (including any person resident in Japan or any corporation or other entity organized under the laws of Japan) or to, or for the account or benefit of, others for reoffering or resale, directly or indirectly, in Japan or to or for the account or benefit of any resident of Japan, except pursuant to an exemption from the registration requirements of the FIEA and otherwise in compliance with any relevant laws and regulations of Japan.
Switzerland
The shares of Class A common stock may not be publicly offered in Switzerland and will not be listed on the SIX Swiss Exchange (“SIX”) or on any other stock exchange or regulated trading facility in Switzerland. This document has been prepared without regard to the disclosure standards for issuance prospectuses under art. 652a or art. 1156 of the Swiss Code of Obligations or the disclosure standards for listing prospectuses under art. 27 ff. of the SIX Listing Rules or the listing rules of any other stock exchange or regulated trading facility in Switzerland. Neither this document nor any other offering or marketing material relating to the shares of Class A common stock or the offering may be publicly distributed or otherwise made publicly available in Switzerland.
Neither this document nor any other offering or marketing material relating to the offering, the Company, or the shares of Class A common stock have been or will be filed with or approved by any Swiss regulatory authority. In particular, this document will not be filed with, and the offer of shares of Class A common stock will not be supervised by, the Swiss Financial Market Supervisory Authority FINMA (FINMA), and the offer of shares of Class A common stock has not been and will not be authorized under the Swiss Federal Act on Collective Investment Schemes (“CISA”). The investor protection afforded to acquirers of interests in collective investment schemes under the CISA does not extend to acquirers of shares.
Dubai International Financial Centre
This prospectus relates to an Exempt Offer in accordance with the Offered Securities Rules of the Dubai Financial Services Authority (“DFSA”). This prospectus is intended for distribution only to persons of a type specified in the Offered Securities Rules of the DFSA. It must not be delivered to, or relied on by, any other
206
Table of Contents
person. The DFSA has no responsibility for reviewing or verifying any documents in connection with Exempt Offers. The DFSA has not approved this prospectus nor taken steps to verify the information set forth herein and has no responsibility for the prospectus. The shares to which this prospectus relates may be illiquid and/or subject to restrictions on their resale. Prospective purchasers of the shares offered should conduct their own due diligence on the shares. If you do not understand the contents of this prospectus you should consult an authorized financial advisor.
Australia
No placement document, prospectus, product disclosure statement or other disclosure document has been lodged with the Australian Securities and Investments Commission (“ASIC”), in relation to the offering. This prospectus does not constitute a prospectus, product disclosure statement or other disclosure document under the Corporations Act 2001 (the “Corporations Act”), and does not purport to include the information required for a prospectus, product disclosure statement or other disclosure document under the Corporations Act.
Any offer in Australia of the shares of Class A common stock may only be made to persons (the “Exempt Investors”) who are “sophisticated investors” (within the meaning of section 708(8) of the Corporations Act), “professional investors” (within the meaning of section 708(11) of the Corporations Act) or otherwise pursuant to one or more exemptions contained in section 708 of the Corporations Act so that it is lawful to offer the shares without disclosure to investors under Chapter 6D of the Corporations Act.
The shares applied for by Exempt Investors in Australia must not be offered for sale in Australia in the period of 12 months after the date of allotment under the offering, except in circumstances where disclosure to investors under Chapter 6D of the Corporations Act would not be required pursuant to an exemption under section 708 of the Corporations Act or otherwise or where the offer is pursuant to a disclosure document which complies with Chapter 6D of the Corporations Act. Any person acquiring shares must observe such Australian on-sale restrictions.
This prospectus contains general information only and does not take account of the investment objectives, financial situation or particular needs of any particular person. It does not contain any securities recommendations or financial product advice. Before making an investment decision, investors need to consider whether the information in this prospectus is appropriate to their needs, objectives and circumstances, and, if necessary, seek expert advice on those matters.
We estimate that our share of the total expenses of the offering, excluding the underwriting discount, will be approximately $ .
We and GoHealth Holdings, LLC have agreed to indemnify the several underwriters against certain liabilities, including liabilities under the Securities Act.
The underwriters and their respective affiliates are full service financial institutions engaged in various activities, which may include sales and trading, commercial and investment banking, advisory, investment management, investment research, principal investment, hedging, market making, brokerage and other financial and non-financial activities and services. Certain of the underwriters and their respective affiliates have provided, and may in the future provide, a variety of these services to the issuer and to persons and entities with relationships with the issuer, for which they received or will receive customary fees and expenses.
In the ordinary course of their various business activities, the underwriters and their respective affiliates, officers, directors and employees may purchase, sell or hold a broad array of investments and actively traded securities, derivatives, loans, commodities, currencies, credit default swaps and other financial instruments for their own account and for the accounts of their customers, and such investment and trading activities may involve or relate to assets, securities and/or instruments of the issuer (directly, as collateral securing other obligations or
207
Table of Contents
otherwise) and/or persons and entities with relationships with the issuer. The underwriters and their respective affiliates may also communicate independent investment recommendations, market color or trading ideas and/or publish or express independent research views in respect of such assets, securities or instruments and may at any time hold, or recommend to clients that they should acquire, long and/or short positions in such assets, securities and instruments.
208
Table of Contents
The validity of the shares of Class A common stock offered hereby will be passed upon for us by Latham & Watkins LLP, New York, New York. Sidley Austin LLP, New York, New York, has acted as counsel for the underwriters in connection with certain legal matters related to this offering.
The consolidated financial statements of GoHealth Holdings, LLC and its subsidiaries at December 31, 2019 (Successor period) and 2018 (Predecessor period), and for the period from September 13, 2019 to December 31, 2019 (Successor period), the period from January 1, 2019 to September 12, 2019 and the year ended December 31, 2018 (Predecessor period), appearing in this prospectus and registration statement have been audited by Ernst & Young LLP, independent registered public accounting firm, as set forth in their report thereon appearing elsewhere herein, and are included in reliance upon such report given on the authority of such firm as experts in accounting and auditing.
The financial statement of GoHealth, Inc. as of March 27, 2020, appearing in this prospectus and registration statement has been audited by Ernst & Young LLP, independent registered public accounting firm, as set forth in their report thereon appearing elsewhere herein, and are included in reliance upon such report given on the authority of such firm as experts in accounting and auditing.
WHERE YOU CAN FIND MORE INFORMATION
We have filed with the Securities and Exchange Commission a registration statement on Form S-1 under the Securities Act with respect to the shares of Class A common stock offered hereby. This prospectus, which constitutes a part of the registration statement, does not contain all of the information set forth in the registration statement or the exhibits and schedules filed with the registration statement. For further information about us and the Class A common stock offered hereby, we refer you to the registration statement and the exhibits filed with the registration statement. Statements contained in this prospectus regarding the contents of any contract or any other document that is filed as an exhibit to the registration statement are not necessarily complete, and each such statement is qualified in all respects by reference to the full text of such contract or other document filed as an exhibit to the registration statement.
Upon the closing of this offering, we will be required to file periodic reports, proxy statements, and other information with the SEC pursuant to the Exchange Act. The SEC also maintains an internet website that contains reports, proxy statements and other information about registrants, like us, that file electronically with the SEC. The address of that site is www.sec.gov. We also maintain a website at www.gohealth.com, through which you may access these materials free of charge as soon as reasonably practicable after they are electronically filed with, or furnished to, the SEC. Information contained on our website is not a part of this prospectus and the inclusion of our website address in this prospectus is an inactive textual reference only.
209
Table of Contents
INDEX TO CONSOLIDATED FINANCIAL STATEMENTS
| Audited Consolidated Financial Statements |
Page | |||
| GoHealth, Inc. |
||||
| F-1 | ||||
| F-2 | ||||
| F-3 | ||||
| GoHealth Holdings, LLC and subsidiaries |
||||
| F-4 | ||||
| F-5 | ||||
| F-6 | ||||
| Consolidated balance sheets as of December 31, 2019 and 2018 |
F-7 | |||
| F-8 | ||||
| F-9 | ||||
| F-10 | ||||
| Unaudited Condensed Consolidated Financial Statements |
||||
| GoHealth Holdings, LLC and subsidiaries |
||||
| F-42 | ||||
| F-43 | ||||
| Condensed consolidated balance sheets as of March 31, 2020 and December 31, 2019 |
F-44 | |||
| Condensed consolidated statements of changes in members’ equity as of March 31, 2020 and 2019 |
F-45 | |||
| Condensed consolidated statements of cash flows for the three months ended March 31, 2020 and 2019 |
F-46 | |||
| F-47 | ||||
Table of Contents
Report of Independent Registered Public Accounting Firm
To the Shareholder and Board of Directors of GoHealth, Inc.
Opinion on the Financial Statement
We have audited the accompanying balance sheet of GoHealth, Inc. (the “Company”) as of March 27, 2020, and the related notes (collectively referred to as the “financial statement”). In our opinion, the financial statement presents fairly, in all material respects, the financial position of GoHealth, Inc. at March 27, 2020, in conformity with U.S. generally accepted accounting principles.
Basis for Opinion
The financial statement is the responsibility of the Company’s management. Our responsibility is to express an opinion on the Company’s financial statement based on our audit. We are a public accounting firm registered with the Public Company Accounting Oversight Board (United States) (PCAOB) and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audit in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statement is free of material misstatement, whether due to error or fraud. The Company is not required to have, nor were we engaged to perform, an audit of its internal control over financial reporting. As part of our audit we are required to obtain an understanding of internal control over financial reporting but not for the purpose of expressing an opinion on the effectiveness of the Company’s internal control over financial reporting. Accordingly, we express no such opinion.
Our audit included performing procedures to assess the risks of material misstatement of the financial statement, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the financial statement. Our audit also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the financial statement. We believe that our audit provides a reasonable basis for our opinion.
/s/ Ernst & Young LLP
We have served as the Company’s auditor since 2013.
Chicago, Illinois
May 8, 2020
Table of Contents
Balance Sheet
(dollars in actuals)
| As of March 27, 2020 |
||||
| Assets |
||||
| Current assets: |
||||
| Cash |
$ | 1 | ||
|
|
|
|||
| Total assets |
$ | 1 | ||
|
|
|
|||
| Commitments and contingencies |
||||
| Stockholder’s equity: |
||||
| Common stock, $0.001 par value, 1,000 shares authorized, issued and outstanding |
1 | |||
|
|
|
|||
| Total stockholder’s equity |
$ | 1 | ||
|
|
|
|||
See accompanying notes to balance sheet.
F-2
Table of Contents
GoHealth, Inc.
Note 1: Nature of Business and Basis of Presentation
Nature of Business
GoHealth, Inc. (the “Company”) was incorporated in Delaware on March 27, 2020. Pursuant to a reorganization into a holding company structure, the Company will be a holding company and its principal asset will be a controlling equity interest in GoHealth Holdings, LLC (“GHH, LLC”), formerly known as Blizzard Parent, LLC. As the sole managing member of GHH, LLC, the Company will operate and control all of the business and affairs of GHH, LLC, and through GHH, LLC and its subsidiaries, conduct its business.
Basis of Presentation
The balance sheet is presented in accordance with accounting principles generally accepted in the United States. Separate statements of income, comprehensive income, changes in stockholder’s equity, and cash flows have not been presented because the Company has not engaged in any activities except in connection with its formation.
Note 2: Summary of Significant Accounting Policies
Cash
All cash as of the balance sheet date was cash on hand held in deposit, and is carried at fair value, which approximates carrying value.
Income Taxes
The Company is treated as a subchapter C corporation, and therefore, is subject to both federal and state income taxes. GHH, LLC continues to be recognized as a limited liability company, a pass-through entity for income tax purposes.
Note 3: Stockholder’s Equity
On March 27, 2020, the Company was authorized to issue 1,000 shares of common stock, $0.001 par value. On March 27, 2020, the Company issued 1,000 shares of common stock for $1, all of which were owned by GHH, LLC.
Note 4: Subsequent Events
The Company has evaluated subsequent events through May 8, 2020, the date on which the balance sheet was available for issuance, and is not aware of any subsequent events that would require recognition or disclosure in the financial statement.
F-3
Table of Contents
Report of Independent Registered Public Accounting Firm
To the Members and Board of Directors of GoHealth Holdings, LLC and Subsidiaries
Opinion on the Financial Statements
We have audited the accompanying consolidated balance sheets of GoHealth Holdings, LLC and subsidiaries (Successor) (the “Company”) as of December 31, 2019 (Successor period) and 2018 (Predecessor period), the related consolidated statements of income (loss), comprehensive income (loss), changes in members’ equity and cash flows for the period from September 13, 2019 to December 31, 2019 (Successor period), the period from January 1, 2019 to September 12, 2019 and the year ended December 31, 2018 (Predecessor period), and the related notes (collectively referred to as the “consolidated financial statements”). In our opinion, the consolidated financial statements present fairly, in all material respects, the financial position of the Company at December 31, 2019 (Successor period) and 2018 (Predecessor period), and the results of its operations and its cash flows for the period from September 13, 2019 to December 31, 2019 (Successor period), the period from January 1, 2019 to September 12, 2019 and the year ended December 31, 2018 (Predecessor period), in conformity with U.S. generally accepted accounting principles.
Adoption of New Accounting Standard
As discussed in Note 1 to the consolidated financial statements, the Company changed its method of accounting for revenue as a result of the full retrospective adoption of Accounting Standards Update (“ASU”) No. 2014-09 “Revenue from Contracts with Customers (Topic 606),” as amended.
Basis for Opinion
These financial statements are the responsibility of the Company’s management. Our responsibility is to express an opinion on the Company’s financial statements based on our audits. We are a public accounting firm registered with the Public Company Accounting Oversight Board (United States) (PCAOB) and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audits in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement, whether due to error or fraud. The Company is not required to have, nor were we engaged to perform, an audit of its internal control over financial reporting. As part of our audits we are required to obtain an understanding of internal control over financial reporting but not for the purpose of expressing an opinion on the effectiveness of the Company’s internal control over financial reporting. Accordingly, we express no such opinion.
Our audits included performing procedures to assess the risks of material misstatement of the financial statements, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the financial statements. Our audits also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the financial statements. We believe that our audits provide a reasonable basis for our opinion.
/s/ Ernst & Young LLP
We have served as the Company’s auditor since 2013.
Chicago, Illinois
May 8, 2020
F-4
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Consolidated Statements of Income (Loss)
(dollars in thousands)
| Successor | Predecessor | |||||||||||||||||||
| Period from September 13, 2019 through December 31, 2019 |
Period from January 1, 2019 through September 12, 2019 |
Year Ended December 31, 2018 |
||||||||||||||||||
| Net revenues: |
||||||||||||||||||||
| Commission |
$ | 243,347 | $ | 175,834 | $ | 144,378 | ||||||||||||||
| Other |
65,144 | 55,176 | 81,827 | |||||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Net revenues |
308,491 | 231,010 | 226,205 | |||||||||||||||||
| Operating expenses: |
||||||||||||||||||||
| Cost of revenue |
90,384 | 79,169 | 79,582 | |||||||||||||||||
| Marketing and advertising |
24,811 | 37,769 | 28,129 | |||||||||||||||||
| Customer care and enrollment |
44,356 | 49,149 | 46,076 | |||||||||||||||||
| Technology |
6,006 | 40,312 | 16,197 | |||||||||||||||||
| General and administrative |
13,674 | 79,219 | 27,458 | |||||||||||||||||
| Change in fair value of contingent consideration liability |
70,700 | — | — | |||||||||||||||||
| Amortization of intangible assets |
28,217 | — | — | |||||||||||||||||
| Transaction costs |
6,245 | 2,267 | — | |||||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Total operating expenses |
284,393 | 287,885 | 197,442 | |||||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Income (loss) from operations |
24,098 | (56,875 | ) | 28,763 | ||||||||||||||||
| Interest expense |
8,076 | 140 | 224 | |||||||||||||||||
| Other income (expense) |
17 | (114 | ) | (379 | ) | |||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Income (loss) before income taxes |
16,039 | (57,129 | ) | 28,160 | ||||||||||||||||
| Income tax expense (benefit) |
44 | (66 | ) | 46 | ||||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Net income (loss) |
15,995 | (57,063 | ) | 28,114 | ||||||||||||||||
| Less: Net loss attributable to non-controlling interests |
— | — | (3 | ) | ||||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Net income (loss) attributable to GoHealth Holdings, LLC and Subsidiaries |
$ | 15,995 | $ | (57,063 | ) | $ | 28,117 | |||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
The accompanying notes are an integral part of these consolidated financial statements.
F-5
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Consolidated Statements of Comprehensive Income (Loss)
(dollars in thousands)
| Successor | Predecessor | |||||||||||||||
| Period from September 13, 2019 through December 31, 2019 |
Period from January 1, 2019 through September 12, 2019 |
Year Ended December 31, 2018 |
||||||||||||||
| Net income (loss) |
$ | 15,995 | $ | (57,063 | ) | $ | 28,114 | |||||||||
| Other comprehensive loss: |
||||||||||||||||
| Foreign currency translation adjustments |
(17 | ) | (32 | ) | (8 | ) | ||||||||||
|
|
|
|
|
|
|
|||||||||||
| Other comprehensive loss |
(17 | ) | (32 | ) | (8 | ) | ||||||||||
|
|
|
|
|
|
|
|||||||||||
| Total comprehensive income (loss) |
$ | 15,978 | $ | (57,095 | ) | $ | 28,106 | |||||||||
|
|
|
|
|
|
|
|||||||||||
| Less: Net comprehensive loss attributable to non-controlling interests |
— | — | (3 | ) | ||||||||||||
|
|
|
|
|
|
|
|||||||||||
| Net comprehensive income (loss) attributable to GoHealth Holdings, LLC and Subsidiaries |
$ | 15,978 | $ | (57,095 | ) | $ | 28,109 | |||||||||
|
|
|
|
|
|
|
|||||||||||
The accompanying notes are an integral part of these consolidated financial statements.
F-6
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Consolidated Balance Sheets
(dollars in thousands, except share and per share data)
| Successor | Predecessor | |||||||||||
| December 31, 2019 |
December 31, 2018 |
|||||||||||
| Assets |
||||||||||||
| Current assets: |
||||||||||||
| Cash and cash equivalents |
$ | 12,276 | $ | 505 | ||||||||
| Accounts receivable, net of allowance for doubtful accounts of $904 in 2019 and $835 in 2018 |
24,461 | 9,855 | ||||||||||
| Commissions receivable – current |
101,078 | 38,685 | ||||||||||
| Prepaid expenses and other current assets |
5,954 | 4,983 | ||||||||||
|
|
|
|
|
|||||||||
| Total current assets |
143,769 | 54,028 | ||||||||||
| Commissions receivable – non-current |
281,853 | 76,842 | ||||||||||
| Property, equipment, and capitalized software, net |
6,339 | 11,782 | ||||||||||
| Intangible assets, net |
782,783 | — | ||||||||||
| Goodwill |
386,553 | — | ||||||||||
| Other long-term assets |
998 | 185 | ||||||||||
|
|
|
|
|
|||||||||
| Total assets |
$ | 1,602,295 | $ | 142,837 | ||||||||
|
|
|
|
|
|||||||||
| Liabilities and members’ equity |
||||||||||||
| Current liabilities: |
||||||||||||
| Accounts payable |
$ | 13,582 | $ | 10,534 | ||||||||
| Accrued liabilities |
22,568 | 9,720 | ||||||||||
| Commissions payable – current |
56,003 | 18,336 | ||||||||||
| Deferred revenue |
15,218 | 1,357 | ||||||||||
| Current portion of debt |
3,000 | 4,856 | ||||||||||
| Other current liabilities |
2,694 | 3,181 | ||||||||||
|
|
|
|
|
|||||||||
| Total current liabilities |
113,065 | 47,984 | ||||||||||
| Non-current liabilities: |
||||||||||||
| Commissions payable – non-current |
97,489 | 35,100 | ||||||||||
| Long-term debt, net of current portion |
288,233 | — | ||||||||||
| Contingent consideration |
242,700 | — | ||||||||||
| Capital lease obligations, less current portion |
421 | 152 | ||||||||||
| Incentive share liability |
— | 28 | ||||||||||
| Deferred tax liability |
243 | 226 | ||||||||||
|
|
|
|
|
|||||||||
| Total non-current liabilities |
629,086 | 35,506 | ||||||||||
|
|
|
|
|
|||||||||
| Commitments and contingencies (Note 10) |
||||||||||||
| Redeemable Class B units – $10.00 par value; 4,930,000 issued and outstanding as of December 31, 2018 |
246,000 | |||||||||||
| Members’ Equity: |
||||||||||||
| Preferred units – $1.00 par value; 541,263,042 units authorized, issued and outstanding at December 31, 2019 |
547,542 | |||||||||||
| Class A Common units – $1.00 par value; 237,938,682 units authorized, issued and outstanding at December 31, 2019 |
218,911 | |||||||||||
| Class B Common units – $1.00 par value; 102,061,318 units authorized, issued and outstanding at December 31, 2019 |
93,708 | |||||||||||
| Senior Preferred Earnout Units – no par value; none authorized, issued, and outstanding at December 31, 2019 |
— | — | ||||||||||
| Profits Units – no par value; 97,918,116 units authorized; 78,398,133 units issued; and none outstanding as of December 31, 2019 |
— | — | ||||||||||
| Class A units – $10.00 par value; 8,365,000 units issued and outstanding as of December 31, 2018 |
— | 235 | ||||||||||
| Class B units – $10.00 par value; 220,000 units issued and outstanding as of December 31, 2018 |
— | 2,200 | ||||||||||
| Accumulated other comprehensive (loss) income |
(17 | ) | 14 | |||||||||
| Retained earnings (deficit) |
— | (189,102 | ) | |||||||||
|
|
|
|
|
|||||||||
| Total members’ equity (deficit) |
860,144 | (186,653 | ) | |||||||||
|
|
|
|
|
|||||||||
| Total liabilities, Redeemable Class B units and members’ equity |
$ | 1,602,295 | $ | 142,837 | ||||||||
|
|
|
|
|
|||||||||
The accompanying notes are an integral part of these consolidated financial statements.
F-7
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Consolidated Statements of Changes in Members’ Equity
(dollars and units in thousands)
| Preferred Units | Class A Common Units |
Class B Common Units |
Class A Units | Class B Units | Retained Earnings (Deficit) |
Non-Controlling Interests |
Accumulated Other Comprehensive (Loss) Income |
Members’ Equity (Deficit) |
||||||||||||||||||||||||||||||||||||||||||||||||
| Units | Amount | Units | Amount | Units | Amount | Units | Amount | Units | Amount | |||||||||||||||||||||||||||||||||||||||||||||||
| Predecessor: |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Balance at January 1,2018, before the cumulative effect of adoption of ASC 606 |
8,365 | $ | 235 | $ | (49,238 | ) | $ | 194 | 22 | $ | (48,787 | ) | ||||||||||||||||||||||||||||||||||||||||||||
| Cumulative effect of adoption of ASC 606 |
28,607 | 28,607 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Balance at January 1, 2018, after the cumulative effect of adoption of ASC 606 |
8,365 | $ | 235 | $ | (20,631 | ) | $ | 194 | 22 | $ | (20,180 | ) | ||||||||||||||||||||||||||||||||||||||||||||
| Redeemable Class B unit accretion |
(196,700 | ) | (196,700 | ) | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Reclassification of Redeemable Class B to Class B Units |
220 | $ | 2,200 | 2,200 | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Member distributions non-controlling interests |
(79 | ) | (79 | ) | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Foreign currency translation adjustment |
(8 | ) | (8 | ) | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Acquisition of non-controlling interests |
112 | (112 | ) | — | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Net income (loss) |
28,117 | (3 | ) | 28,114 | ||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||
| Balance at December 31, 2018 |
8,365 | $ | 235 | 220 | $ | 2,200 | $ | (189,102 | ) | $ | — | $ | 14 | $ | (186,653 | ) | ||||||||||||||||||||||||||||||||||||||||
| Redeemable Class B unit accretion |
(138,404 | ) | (138,404 | ) | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Conversion of Redeemable Class B Units and Class B Units to Class A Units |
5,150 | $ | 386,604 | (220 | ) | $ | (2,200 | ) | 384,404 | |||||||||||||||||||||||||||||||||||||||||||||||
| Foreign currency translation adjustment |
(32 | ) | (32 | ) | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Net loss |
(57,063 | ) | (57,063 | ) | ||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||
| Balance at September 12, 2019 |
13,515 | $ | 386,839 | — | $ | — | $ | (384,569 | ) | $ | — | $ | (18 | ) | $ | 2,252 | ||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||
| Successor: |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Balance at September 13, 2019 |
541,263 | $ | 541,263 | 237,939 | $ | 214,145 | 102,061 | $ | 91,855 | $ | 847,263 | |||||||||||||||||||||||||||||||||||||||||||||
| Other |
(3,545 | ) | (3,545 | ) | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Share-based compensation expense |
448 | 448 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Foreign currency translation adjustment |
(17 | ) | (17 | ) | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Net income |
9,824 | 4,318 | 1,853 | 15,995 | ||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||
| Balance at December 31, 2019 |
541,263 | $ | 547,542 | 237,939 | $ | 218,911 | 102,061 | $ | 93,708 | $ | — | $ | — | $ | (17 | ) | $ | 860,144 | ||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||
The accompanying notes are an integral part of these consolidated financial statements.
F-8
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Consolidated Statements of Cash Flows
(dollars in thousands)
| Successor | Predecessor | |||||||||||||||
| Period from September 13, 2019 through December 31, 2019 |
Period from January 1, 2019 through September 12, 2019 |
Year Ended December 31, 2018 |
||||||||||||||
| Operating activities |
||||||||||||||||
| Net income (loss) |
$ | 15,995 | $ | (57,063 | ) | $ | 28,114 | |||||||||
| Adjustments to reconcile net income (loss) to net cash (used in) provided by operating activities: |
||||||||||||||||
| Share-based compensation |
448 | 87,060 | — | |||||||||||||
| Depreciation and amortization |
521 | 4,247 | 6,160 | |||||||||||||
| Amortization of intangible assets |
28,217 | — | — | |||||||||||||
| Accretion of discount on long-term debt |
428 | — | — | |||||||||||||
| Amortization of debt issuance costs |
44 | — | — | |||||||||||||
| Change in fair value of contingent consideration |
70,700 | — | — | |||||||||||||
| Other non-cash items |
417 | 150 | 791 | |||||||||||||
| Changes in assets and liabilities: |
||||||||||||||||
| Accounts receivable |
(15,113 | ) | (108 | ) | 736 | |||||||||||
| Commissions receivable |
(203,956 | ) | (63,448 | ) | (65,445 | ) | ||||||||||
| Prepaid expenses and other assets |
(2,316 | ) | 1,325 | (1,712 | ) | |||||||||||
| Accounts payable |
5,031 | (1,981 | ) | 3,108 | ||||||||||||
| Accrued liabilities |
31 | 17,860 | 2,891 | |||||||||||||
| Deferred revenue |
11,935 | 1,926 | 126 | |||||||||||||
| Commissions payable |
80,828 | 19,228 | 30,896 | |||||||||||||
| Other liabilities |
(2,494 | ) | 85 | (222 | ) | |||||||||||
|
|
|
|
|
|
|
|||||||||||
| Net cash (used in) provided by operating activities |
(9,284 | ) | 9,281 | 5,443 | ||||||||||||
| Investing activities |
||||||||||||||||
| Acquisition of business |
(807,591 | ) | — | — | ||||||||||||
| Purchases of property, equipment and software |
(2,419 | ) | (5,597 | ) | (6,170 | ) | ||||||||||
|
|
|
|
|
|
|
|||||||||||
| Net cash used in investing activities |
(810,010 | ) | (5,597 | ) | (6,170 | ) | ||||||||||
| Financing activities |
||||||||||||||||
| Borrowings under term loans |
300,000 | — | — | |||||||||||||
| Principal payments under term loans |
(750 | ) | — | — | ||||||||||||
| Principal payments under capital lease obligations |
(351 | ) | (68 | ) | (93 | ) | ||||||||||
| Borrowings under revolving credit facilities |
— | 56,534 | 82,555 | |||||||||||||
| Payments under revolving credit facilities |
— | (59,915 | ) | (82,320 | ) | |||||||||||
| Debt issuance cost payments |
(9,283 | ) | — | — | ||||||||||||
| Proceeds received upon issuance of preferred units |
541,263 | — | — | |||||||||||||
| Member distributions to non-controlling interests |
— | — | (79 | ) | ||||||||||||
|
|
|
|
|
|
|
|||||||||||
| Net cash provided by (used in) financing activities |
830,879 | (3,449 | ) | 63 | ||||||||||||
| Effect of exchange rate changes on cash |
(17 | ) | (32 | ) | (3 | ) | ||||||||||
| Increase (decrease) in cash and cash equivalents |
11,568 | 203 | (667 | ) | ||||||||||||
| Cash and cash equivalents at beginning of period |
708 | 505 | 1,172 | |||||||||||||
|
|
|
|
|
|
|
|||||||||||
| Cash and cash equivalents at end of period |
$ | 12,276 | $ | 708 | $ | 505 | ||||||||||
|
|
|
|
|
|
|
|||||||||||
| Interest paid |
$ | 5,437 | $ | 140 | $ | 219 | ||||||||||
|
|
|
|
|
|
|
|||||||||||
| Taxes paid |
$ | 55 | $ | 122 | $ | 32 | ||||||||||
|
|
|
|
|
|
|
|||||||||||
The accompanying notes are an integral part of the consolidated financial statements.
F-9
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements
Period from September 13, 2019 through December 31, 2019 (Successor),
Period from January 1, 2019 through September 12, 2019 (Predecessor)
and Year Ended December 31, 2018 (Predecessor)
(dollars in thousands)
1. SUMMARY OF BUSINESS AND SIGNIFICANT ACCOUNTING POLICIES
Description of Business
GoHealth Holdings, LLC (formerly known as Blizzard Parent, LLC), a Delaware limited liability company, and its wholly owned subsidiaries (collectively, the “Company”) is a leading health insurance marketplace whose mission is to improve healthcare in America. The Company works with insurance carriers to provide solutions to efficiently enroll individuals in health insurance plans. The Company’s proprietary technology platform leverages modern machine-learning algorithms powered by nearly two decades of insurance purchasing behavior to reimagine the optimal process for helping individuals find the best health insurance plan for their specific needs. The Company’s insurance agents leverage the power of its vertically integrated customer acquisition platform to enroll members in Medicare and individual and family plans. Certain of the Company’s operations do business as GoHealth, LLC (“GoHealth”), a wholly owned subsidiary of the Company that was founded in 2001.
Basis of Presentation and Principles of Consolidation
GoHealth Holdings, LLC is a holding company with no operating assets or operations and was formed to acquire a 100% equity interest in Norvax, LLC (“Norvax”). On May 6, 2020, Blizzard Parent, LLC changed its name to GoHealth Holdings, LLC. GoHealth Holdings, LLC owns 100% of Blizzard Midco, LLC, which owns 100% of Norvax. For all of the periods reported in these consolidated financial statements, GoHealth Holdings, LLC has not and does not have any material operations on a standalone basis, and all of the operations of the Company are carried out by Norvax. On August 15, 2019, GoHealth Holdings, LLC entered a series of arrangements to acquire 100% of the equity interest in Norvax. On September 13, 2019, Blizzard Merger Sub LLC, a transitory merger company of Blizzard Midco, LLC, merged into Norvax, with Norvax continuing as the surviving limited liability company and the Company’s operating entity (the “Acquisition”).
As a result of the Acquisition, which is discussed further in Note 2 – Acquisition, Norvax was determined to be the accounting acquirer and Norvax’s historical assets and liabilities are reflected at fair value as of the acquisition date. The financial information for the period after September 13, 2019, represents the consolidated financial information of the “Successor” company. Prior to September 13, 2019, the consolidated financial statements include the accounts of the “Predecessor” company. References to the “Successor 2019 Period” refer to the period from September 13, 2019 through December 31, 2019. References to the “Predecessor 2019 Period” refer to the period from January 1, 2019 through September 12, 2019, prior to the Acquisition. Due to the change in the basis of accounting, resulting from the application of the acquisition method of accounting, the Predecessor’s consolidated financial statements and the Successor’s consolidated financial statements are not necessarily comparable.
The accompanying consolidated financial statements include the accounts of the Company and its wholly-owned subsidiaries. The consolidated financial statements have been prepared in conformity with accounting principles generally accepted in the United States of America (“U.S. GAAP”). All intercompany balances and transactions are eliminated in consolidation.
Adoption of New Accounting Standard
Effective January 1, 2019, the Company adopted the requirements of Accounting Standards Update (“ASU”) No. 2014-09, Revenue from Contracts with Customers (“ASC 606”), using the full retrospective method, which
F-10
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
requires adjusting prior periods as if ASC 606 had been in effect as of the beginning of the earliest period presented. Thus, the accompanying consolidated predecessor balance sheet of Norvax as of December 31, 2018, as well as the accompanying consolidated statements of income (loss), comprehensive income (loss), changes in members’ equity, and cash flows for the year then ended, have been adjusted to reflect the adoption of ASC 606, as have all related disclosures. The adoption had a material impact on the Company’s consolidated financial statements. See “Revenue Recognition” below for additional information on ASC 606 and Note 13 – Adoption Impact of New Revenue Standard for further discussion of the adoption and the impact on the Company’s previously reported historical results.
Use of Estimates
The preparation of the consolidated financial statements in conformity with U.S. GAAP requires management to make estimates, judgments, and assumptions that affect the reported amounts of assets and liabilities at the date of the consolidated financial statements, and the reported amounts of revenues and expenses during the reporting periods. The Company bases its estimates on historical experience and on various other assumptions that management believes are reasonable under the circumstances, the results of which form the basis for making judgments about carrying values of assets and liabilities that are not readily apparent from other sources. Actual results could differ from those estimates.
Cash and Cash Equivalents
We consider all investments with an original maturity of 90 days or less from the date of purchase to be cash equivalents. Cash includes all deposits in banks. The Company maintains its cash balances at financial institutions in the United States and Europe.
Cash accounts in the United States are insured by the Federal Deposit Insurance Corporation (“FDIC”) up to $250,000. As of December 31, 2019, and 2018, the Company’s cash balances in the United States exceeded the FDIC-insured limits by $12,026 and $255, respectively. The Company also has an immaterial amount of cash held in Europe to fund its Slovakian operations. The Company does not believe it is exposed to any significant risk with respect to cash balances.
Concentration of Credit Risk
Financial instruments that potentially subject the Company to concentrations of credit risk consist principally of cash, accounts receivable, and commissions receivable. The maximum exposure risk of these accounts is equal to the amounts stated on the Company’s Consolidated Balance Sheets. The Company places its cash with high-credit-quality financial institutions and, at times, such deposits may be in excess of federally insured limits. To date, the Company has not experienced any losses on its cash balances and periodic evaluations of the relative credit standing of the financial institutions are performed.
Accounts receivable and commissions receivable are primarily derived from customers located in North America. The Company performs ongoing credit evaluations of customers’ financial condition and requires no collateral from customers. The Company maintains an allowance for doubtful accounts receivable based upon the expected collectability of accounts receivable balances.
The Company does not require collateral or other security in granting credit. As of December 31, 2019, five customers each represented 10% or more of the Company’s total accounts receivable and, in aggregate, represented 87%, or $21,220, of the Company’s total accounts receivable. As of December 31, 2018, three customers each represented 10% or more of the Company’s total accounts receivable and, in aggregate, represented 58%, or $5,681, of the Company’s total accounts receivable. No other customers represented 10% or more of the Company’s total accounts receivable at December 31, 2019 and 2018.
F-11
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
Foreign Currency
The Company is exposed to currency fluctuations from certain vendors and customers that transact business in Euros. Assets and liabilities of the Company’s foreign affiliate in Slovakia, which uses the local currency as its functional currency, are translated at period-end exchange rates, and income and expense items are translated at a rate that approximates the weighted-average exchange rate for the period. Translation adjustments are included as a component of accumulated other comprehensive (loss) income. Gains and losses from foreign currency transactions are included in other income (expense) and are immaterial for all periods presented.
Accounts Receivable and Allowance for Doubtful Accounts
Accounts receivable are recorded at the invoiced amount and typically do not bear interest. The Company provides allowances for doubtful accounts related to accounts receivable for estimated losses resulting from the inability of its customers to make required payments. The Company takes into consideration the overall quality of the receivables portfolio, along with specifically identified customer risks in establishing allowances. Accounts receivable are charged off against the allowance for doubtful accounts when it is determined the receivable is uncollectible.
Commissions Receivable
Commissions receivable are contract assets that represent estimated variable consideration for renewal commissions to be received from insurance carriers for performance obligations that have been satisfied. The current portion of commissions receivable are future renewal commissions expected to be received within one year, while the non-current portion of commissions receivable are expected to be received beyond one year. The Company assesses impairment for uncollectible consideration when information available indicates it is probable that an asset has been impaired. There were no impairments recorded during the years ended December 31, 2019 or 2018.
Commissions Payable
Commissions payable represent the estimated share of policy renewal commissions earned by the Company’s external channel agents. The current portion of commissions payable are future renewal commissions expected to be paid within one year, while the non-current portion of commissions payable are expected to be paid beyond one year.
Property, Equipment, and Capitalized Software, net
Property and equipment are stated at cost, less accumulated depreciation. Depreciation is computed using the straight-line method over the estimated useful lives as follows:
| Asset Description |
Estimated Useful Life | |
| Computer equipment and software |
3 years | |
| Office equipment and furniture |
7 years | |
| Leasehold improvements |
Lesser of useful life (typically 5 years) or remaining lease term |
Expenditures for major renewals and improvements that extend the useful life of property and equipment are capitalized. Expenditure of maintenance and repairs are charged to expense as incurred.
F-12
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
The Company accounts for costs incurred to develop and maintain source code software and other internally developed software applications, primarily consisting of employee-related and third-party contractor costs, pursuant to ASC Topic 350-40, Internal Use Software. Costs incurred during the planning and post-implementation phases of software development are expensed. During the application development phase, costs incurred are capitalized. Capitalized software development costs are amortized over the estimated useful life, which is generally three years. These capitalized costs are recorded within property, equipment, and capitalized software, net, on the Company’s Consolidated Balance Sheets and the amortization is charged to technology expense in the Consolidated Statements of Income (Loss).
Business Combinations
The Company allocates the fair value of the purchase consideration of its acquired businesses to the tangible assets, liabilities assumed, and intangible assets acquired based on the estimated fair values at the acquisition date. The excess of the fair value of purchase consideration over the fair values of these identifiable assets and liabilities is recorded as goodwill. Transaction costs are recognized separately from the business combination and are expensed as incurred.
Goodwill and Intangible Assets
The Company tests goodwill for impairment on an annual basis in the fourth quarter of each year or whenever events or changes in circumstances indicate that the goodwill may be impaired.
An intangible asset determined to have an indefinite useful life is not amortized until its useful life is determined to no longer be indefinite. Indefinite-lived intangible assets are evaluated each reporting period to determine whether events and circumstances continue to support an indefinite useful life. Indefinite-lived intangible assets are tested for impairment annually, or more frequently if events or changes in circumstances indicate that the asset might be impaired, such as a significant decline in the observable market value of an asset, a significant change in the extent or manner in which an asset is used, or any other significant, adverse change that would indicate that the carrying amount of an asset or group of assets may not be recoverable. If the carrying amount of an indefinite-lived intangible asset exceeds its fair value, an impairment loss is recognized in an amount equal to that excess.
Significant judgment is applied when goodwill and indefinite-lived intangible assets are assessed for impairment. This judgment may include an assessment of qualitative or quantitative factors, such as developing cash flow projections and selecting appropriate royalty and discount rates.
The Company amortizes the cost of definite-lived intangible assets over the respective estimated useful lives on a straight-line basis. Significant judgment is applied when evaluating if an intangible asset has a definite useful life. Intangible assets subject to amortization are also evaluated for impairment when indicators of impairment are determined to exist. Definite-lived intangible assets could become impaired in the future as a result of declines in profitability due to changes in volume, market pricing, cost, manner in which an asset is used, laws and regulations, or the business environment.
Fair Value of Financial Instruments
The Company applies the accounting guidance related to fair value measurements and discloses information on all financial instruments reported at fair value that enables an assessment of the inputs used in determining the reported fair values. See Note 4 – Fair Value Measurements for further discussion around fair value determinations.
F-13
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
Revenue Recognition
In May 2014, the Financial Accounting Standards Board (“FASB”) issued ASC 606, requiring an entity to recognize revenue when it transfers promised goods or services to customers in an amount that reflects the consideration to which the entity expects to be entitled to in exchange for those goods or services. The Company adopted ASC 606 using the full retrospective method and, accordingly, its historical financial statements and related disclosures have been recasted herein to reflect the adoption of ASC 606 for all periods presented.
The Company is compensated by the receipt of commission payments from health insurance carriers whose health insurance policies are purchased through the Company’s ecommerce platforms or customer care centers. The Company also generates revenue from non-commission revenue sources, which include providing dedicated insurance agent resources for carrier-specific programs, sales of insurance leads to other marketing agencies and carriers, and the implementation and use of the Company’s platform. The Company accounts for payments made under certain carrier-specific arrangements as deductions to revenue.
The core principle of ASC 606 is to recognize revenue upon the transfer of promised goods or services to customers in an amount that reflects the consideration the entity expects to be entitled to in exchange for those goods or services. Accordingly, the Company recognizes revenue for its services in accordance with the following five steps outlined in ASC 606:
| • | Identification of the contract, or contracts, with a customer. A contract with a customer exists when (i) the Company enters into an enforceable contract with a customer that defines each party’s rights regarding the goods or services to be transferred and identifies the payment terms related to these goods or services, (ii) the contract has commercial substance and, (iii) the Company determines that collection of substantially all consideration for goods or services that are transferred is probable based on the customer’s intent and ability to pay the promised consideration. Payment of commissions typically commences within 60 days from the effective date. Payment terms from non-commission revenue are typically 30 days from the invoice date. |
| • | Identification of the performance obligations in the contract. Performance obligations promised in a contract are identified based on the goods or services that will be transferred to the customer that are both capable of being distinct, whereby the customer can benefit from the goods or services either on their own or together with other resources that are readily available from third parties or from the Company, and are distinct in the context of the contract, whereby the transfer of the goods or services is separately identifiable from other promises in the contract. |
| • | Determination of the transaction price. The transaction price is determined based on the consideration to which the Company will be entitled in exchange for transferring goods or services to the customer. |
| • | Allocation of the transaction price to the performance obligations in the contract. If the contract contains a single performance obligation, the entire transaction price is allocated to the single performance obligation. Contracts that contain multiple performance obligations require an allocation of the transaction price to each performance obligation based on a relative standalone selling price (“SSP”) basis. |
| • | Recognition of revenue when, or as, the Company satisfies a performance obligation. The Company satisfies performance obligations either over time or at a point in time, as discussed in further detail below. Revenue is recognized at the time the related performance obligation is satisfied by transferring the promised good or service to the customer. |
F-14
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
Commission Revenue
The Company recognizes commission revenue from the sale of insurance products at the point when carriers approve an insurance application produced by the Company. As a result of the implementation of ASC 606, the Company records as commission revenue the expected amount of commissions received from the insurance carriers and any renewal commissions to be paid on such placement as long as the policyholder remains with the same insurance product. The Company defines its customer to be the health insurance carrier.
The Company typically enters contractual agency relationships with health insurance carriers that are non-exclusive and terminable on short notice by either party for any reason. In addition, health insurance carriers often can terminate or amend agreements unilaterally on short notice, including provisions in agreements relating to the commission rates paid to the Company by the health insurance carriers. The amendment or termination of an agreement the Company has with a health insurance carrier may adversely impact the commissions it is paid on health insurance plans purchased from the carrier.
Compensation in the form of commissions is received from insurance carriers for the multiple types of insurance products sold by the Company on behalf of the carriers. For Medicare and non-Medicare eligible products, commission revenue generally represents a percentage of the premium amount expected to be collected by the carrier while the policyholder is enrolled in the insurance product, including renewal periods. The Company’s performance obligation is complete when a carrier has received and approved an insurance application. As such, the Company recognizes revenue at this point in time, which represents the total estimated lifetime commissions it expects to receive for selling the product after the carrier approves an application, net of an estimated constraint. The Company’s consideration is variable based on the amount of time it estimates a policy will remain in force. The Company estimates the amount of variable consideration that it expects to receive based on historical experience or carrier experience to the extent available, industry data, and expectations as to future retention rates. Additionally, the Company considers application of the constraint and only recognizes the amount of variable consideration that it believes is probable that it will be entitled to receive and will not be subject to a significant revenue reversal in the future. The Company monitors and updates this estimate at each reporting date. The Company does not have any remaining performance obligations in its contracts with customers.
The Company utilizes a practical expedient to estimate commission revenue for each insurance product by applying the use of a portfolio approach to group approved members by the effective month of the relevant policy (referred to as a “cohort”). This allows the Company to estimate the commissions it expects to collect for each cohort by evaluating various factors, including but not limited to, contracted commission rates, carrier mix, and expected member churn.
The Company’s variable consideration includes estimated and constrained lifetime values as the “constrained LTV” for the plans. The Company’s estimate of commission revenue for each product line is based on a number of assumptions, which include, but are not limited to, estimating conversion of an approved applicant to a paying policyholder, forecasting persistency and forecasting the commission amounts likely to be received per policyholder. These assumptions are based on historical trends and incorporate management’s judgment in interpreting those trends and in applying constraints. To the extent the Company makes changes to the assumptions, it will recognize any impact of the changes to commission revenue in the reporting period in which the change is made, including revisions of estimated lifetime commissions either below or in excess of previously estimated constrained LTV recognized as revenue.
F-15
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
Other Revenue
Within the Company’s Medicare and IFP and Other segments, the Company provides trained licensed agents dedicated to carrier programs that assist in producing health insurance policies, typically prior to and during the annual enrollment period. The Company is compensated for the hours incurred on the carrier program at the time hours are incurred as well as performance-based enrollment fees relating to the Company enrolling individuals into health insurance plans. The Company recognizes revenue as control transfers over the term of the contract.
The Company recognizes revenue at a point in time resulting from the sale of leads to third parties and independent agents. The Company generates this revenue through the sale of leads sourced through its marketing efforts.
The Company provides certain customers access to its technology platform, where it charges for the implementation and monthly access to the software. This application allows carriers the use of the Company’s e-commerce platform to offer their own health insurance policies on their websites and agents to utilize the Company’s technology to power their online quoting, content and application submission processes. Typically, the Company is paid a one-time implementation fee, which it recognizes as control is transferred on a straight-line basis over the estimated term of the customer relationship (generally the initial term of the agreement), commencing once the technology is available for use by the third party.
Additionally, the Company earns development funds, based on delivering call volumes to certain insurance carriers. The Company recognizes revenue as control transfers over the term of the contract.
Deferred Revenue
Deferred revenue includes deferred technology licensing implementation fees and amounts collected from development funds or technology licensing customers in advance of the Company satisfying its performance obligations for such customers. The Company expects to recognize revenue associated with these remaining performance obligations in the next 12 months.
F-16
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
Disaggregation of Revenue
The table below depicts the disaggregation of revenue by product, and is consistent with how the Company evaluates its financial performance:
| Successor | Predecessor | |||||||||||||||
| Period from September 13, 2019 through December 31, 2019 |
Period from January 1, 2019 through September 12, 2019 |
Year Ended December 31, 2018 |
||||||||||||||
| Commission revenue: |
||||||||||||||||
| Medicare |
||||||||||||||||
| Medicare Advantage |
$ | 217,763 | $ | 119,828 | $ | 84,218 | ||||||||||
| Medicare Supplement |
5,407 | 9,354 | 9,610 | |||||||||||||
| Medicare Part D |
2,942 | 1,486 | 2,396 | |||||||||||||
|
|
|
|
|
|
|
|||||||||||
| Total Medicare |
226,112 | 130,668 | 96,224 | |||||||||||||
| Individual and Family Plan: |
||||||||||||||||
| Fixed Indemnity |
12,080 | 35,320 | 33,861 | |||||||||||||
| Short Term |
2,272 | 2,906 | 2,895 | |||||||||||||
| Major Medical |
1,057 | 412 | 2,763 | |||||||||||||
|
|
|
|
|
|
|
|||||||||||
| Total Individual and Family Plan |
15,409 | 38,638 | 39,519 | |||||||||||||
| Ancillary |
1,428 | 5,483 | 7,511 | |||||||||||||
| Small Group |
398 | 1,045 | 1,124 | |||||||||||||
|
|
|
|
|
|
|
|||||||||||
| Total Commission Revenue |
243,347 | 175,834 | 144,378 | |||||||||||||
| Other Revenue |
65,144 | 55,176 | 81,827 | |||||||||||||
|
|
|
|
|
|
|
|||||||||||
| Net Revenues |
$ | 308,491 |
|
|
|
$ | 231,010 | $ | 226,205 | |||||||
|
|
|
|
|
|
|
|||||||||||
Incremental Costs to Obtain a Contract
The Company reviewed its sales compensation plans, which are directed at converting leads into carrier approved submissions, and concluded that they are fulfillment costs and not costs to obtain a contract with a health insurance carrier, which the Company defines as its customer. Additionally, the Company reviewed compensation plans related to personnel responsible for identifying new health insurance carriers as well as entering into contracts with new health insurance carriers and concluded that no incremental costs are incurred to obtain such contracts.
Cost of Revenue
Cost of revenue represents payments related to health insurance policies sold to members who were enrolled by partners with whom the Company has commissions revenue-sharing arrangements. In order to enter into a revenue-sharing arrangement, partners must be licensed to sell health insurance in the state where the policy is sold. Costs related to revenue-sharing arrangements are expensed as the related revenue is recognized.
Marketing and Advertising
Marketing expense consists primarily of expenses associated with the Company’s direct, online advertising, and marketing partner channels, in addition to compensation (including share-based compensation expense) and other expenses related to marketing personnel who manage campaigns and optimize consumer activity. The Company’s direct channel expenses primarily consist of costs for e-mail marketing and direct mail marketing. Online advertising expenses primarily consist of paid. keyword search advertising on search engines. Marketing partner channel expenses primarily consist of fees paid to marketing partners and affiliates. Marketing costs are expensed as incurred.
F-17
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
Advertising expenses consist of costs incurred to acquire consumers through online, television, and direct mail advertisements. Advertising costs incurred in the Successor 2019 Period, Predecessor 2019 Period, and in the year ended December 31, 2018, totaled $18,844, $29,308, and $25,613, respectively.
The Company also has arrangements with certain carriers that allow the Company to increase marketing efforts, including through direct mail, television advertisements, and online advertising for various insurance products that are being offered by these carriers. The Company records the amounts received as a reduction of the marketing costs incurred.
Customer Care and Enrollment
Customer care and enrollment expenses primarily consist of compensation (including share-based compensation expense) and benefits costs for enrollment personnel who assist consumers during the insurance policy application process, along with management and support personnel.
Technology
Technology expense consists primarily of compensation (including share-based compensation expense) and benefits costs for personnel associated with developing and enhancing the Company’s technology platform, data analytics and business intelligence, as well as maintaining the Company’s online presence and integrations with carrier and federal marketplaces. Technology expense also includes costs for contracted services and supplies, and amortization expense to capitalized software.
General and Administrative Expenses
General and administrative expenses include compensation and benefits costs for staff working in the Company’s executive, finance, legal, human resources, and facilities departments. These expenses also include facilities costs and fees paid for outside professional services, including audit, tax, legal, and governmental affairs.
Share-Based Compensation Expense
The Company grants time-vesting units and performance-vesting profit units. Compensation expense for time-vesting units is recognized on a straight-line basis over the requisite service period. Performance-vesting profit units contain market conditions and an implied performance condition, which results in compensation cost being recognized when the performance condition is considered probable of being satisfied. Performance-vesting profit units vest upon the achievement of a contingent exit event that is defined as a transaction in which the ultimate parent disposes of all or substantially all its investment in the Company. Such an exit event is not considered probable until it consummates. The estimated grant date fair value of the Company’s profit interests is determined using a Monte Carlo simulation and Level 3 inputs.
Assumptions utilized in the model for valuing the awards include expected volatility, dividend yield and risk-free interest rate. Additionally, forfeitures are accounted for as they occur.
401(k) Plan
The Company maintains a tax-qualified 401(k) retirement plan (the Plan) that provides eligible employees with an opportunity to save for retirement on a tax-advantaged basis. Eligible employees may defer compensation
F-18
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
subject to applicable annual Internal Revenue Code (Code) limits. The Plan permits participants to make both pretax and after-tax deferral contributions. These contributions are allocated to each participant’s individual account and are then invested in selected investment alternatives according to the participants’ directions. Employees are fully vested immediately in their contributions. The Plan is qualified under Section 401(a) of the Code and the related trust is tax-exempt under Section 501(a) of the Code.
The Company contributes 50% of the first 4% of compensation a participant contributes to the Plan. These matching contributions are expensed as incurred. The Company recognized expense of $150, $346 and $392 for the Successor 2019 Period, the Predecessor 2019 Period, and the year ended December 31, 2018, respectively, related to these matching contributions. The Company also may make non-elective contributions to the 401(k) plan, which, if made, vest 20% after two years and 20% annually thereafter.
Contingencies
The Company analyzes whether it is probable that an asset has been impaired, or a liability has been incurred, and whether the amount of loss can be reasonably estimated. If the loss contingency is both probable and reasonably estimable, the Company records the loss at management’s best estimate of the loss, or when a best estimate cannot be made, a minimum loss contingency amount is recorded. Legal fees are expensed as incurred. If no accrual is made but the loss contingency is reasonably possible, the nature of the contingency and the corresponding estimated loss, if such an estimate can be made, is disclosed. Loss contingencies include, but are not limited to, possible losses related to legal proceedings and regulatory compliance matters.
Income Taxes
The Company accounts for income taxes under the liability method in accordance with ASC Topic 740, Income Taxes. Accordingly, deferred income taxes are provided for the future tax consequences attributable to differences between the carrying amounts of assets and liabilities for financial reporting and income tax purposes. Deferred tax assets and liabilities are measured using tax rates in effect for the year in which those temporary differences are expected to be recovered or settled.
The Company is a limited liability company and has elected to be treated as a partnership for income tax purposes. The Company is not directly liable for income taxes for federal purposes.
On a consolidated basis, income from the Company’s Slovakian subsidiary is taxed at a blended U.S. Federal and state statutory rate as it is a C-Corporation for tax purposes. The Slovakian subsidiary records taxes on its income at the Slovakian statutory rate and records tax on its worldwide income at the applicable blended U.S. Federal and state statutory rate, net of the foreign tax credit associated with foreign taxes.
At December 31, 2019 and 2018, there is no liability for uncertain tax positions recorded on the accompanying Consolidated Balance Sheets.
Seasonality
A greater number of the Company’s Medicare-related health insurance plans are sold in its fourth quarter during the Medicare annual enrollment period when Medicare-eligible individuals are permitted to change their Medicare Advantage and Medicare Part D prescription drug coverage for the following year. As a result, the Company’s Medicare plan-related commission revenue is highest in the Company’s fourth quarter.
The majority of the Company’s individual and family health insurance plans are sold in the fourth quarter during the annual open enrollment period as defined under the federal Patient Protection and Affordable Care Act and
F-19
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
related amendments in the Health Care and Education Reconciliation Act. Individuals and families generally are not able to purchase individual and family health insurance outside of these open enrollment periods, unless they qualify for a special enrollment period as a result of certain qualifying events, such as losing employer-sponsored health insurance or moving to another state.
Recent Accounting Pronouncements
In January 2017, the FASB issued ASU No. 2017-04, Simplifying the Test for Goodwill Impairment (Topic 350). Under the new standard, goodwill impairment is measured as the amount by which a reporting unit’s carrying value exceeds its fair value, not to exceed the carrying value of goodwill. This ASU eliminates existing guidance that requires an entity to determine goodwill impairment by calculating the implied fair value of goodwill by hypothetically assigning the fair value of a reporting unit to all of its assets and liabilities as if that reporting unit had been acquired in a business combination. This ASU is applied on a prospective basis and is effective for the Company on January 1, 2021, however, early adoption is permitted. The Company adopted this standard in 2019 and the adoption did not significantly impact the consolidated financial statements.
In February 2016, the FASB issued ASU 2016-02, Leases (Topic 842). The guidance specifies that lessees will need to recognize a right-of-use asset and a lease liability for virtually all their leases except those which meet the definition of a short-term lease. For income statement purposes, the FASB retained a dual model, requiring leases to be classified as either operating or financing. Classification will be based on criteria that are similar to those applied in current lease accounting, but without explicit bright lines. Per ASU 2019-10, Financial Instruments—Credit Losses (Topic 326), Derivatives and Hedging (Topic 815), and Leases (Topic 842): Effective Dates, issued November 2019, the guidance in ASU 2016-02, as amended, is effective for fiscal years beginning after December 15, 2020, and interim periods within fiscal years beginning after December 15, 2021. Early adoption is permitted. The Company is currently evaluating the new guidance to determine the impact it will have on its consolidated financial statements.
In June 2018, the FASB issued ASU 2018-07, Stock Compensation – Improvements to Nonemployee Share-Based Payment Accounting (Topic 718). This guidance expands the scope of Topic 718 to include share-based payment transactions for acquiring goods and services from nonemployees. Per ASU 2019-08, issued November 2019, the guidance is effective for fiscal years beginning after December 15, 2019, and interim periods within fiscal years beginning after December 15, 2019. Early adoption is permitted, but no earlier than an entity’s adoption date of Topic 606. The Company is currently evaluating the new guidance to determine the impact it will have on its consolidated financial statements.
In November 2019, the FASB issued ASU 2019-11, Financial Instruments — Credit Losses (Topic 326), which amends the guidance for accounting for assets that are potentially subject to credit risk. The amendments affect contract assets, loans, debt securities, trade receivables, net investments in leases, off-balance-sheet credit exposures, reinsurance receivables, and any other financial assets not excluded from the scope that have the contractual right to receive cash. Per ASU 2019-10, issued November 2019, the guidance is effective for annual and interim periods beginning after December 15, 2022. Early adoption is permitted. The Company is currently evaluating the new guidance to determine the impact it will have on its consolidated financial statements.
In August 2018, the FASB issued ASU 2018-13, Fair Value Measurement Disclosure Framework—Changes to the Disclosure Requirements for Fair Value Measurement (Topic 820), which amended the disclosure requirements under ASC 820. This update clarifies and unifies the disclosure of Level 3 fair value instruments. This guidance is effective for fiscal years beginning after December 15, 2019 and for interim periods within those fiscal years, although early adoption is permitted for either the entire standard or only the provisions that eliminate or modify the requirements. The Company plans to adopt this standard on January 1, 2020, and does not expect the adoption to have a material effect on our consolidated financial statements.
F-20
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
2. ACQUISITION
Acquisition of Norvax, LLC
On September 13, 2019, the Company acquired a 100% interest in Norvax, for $807,591 in cash and $306,000 in equity. In connection with the Acquisition, the Company also agreed to pay additional consideration of up to $275,000 in additional Common and Senior Preferred Earnout Units, if Adjusted EBITDA, as defined in the terms of the acquisition agreement, exceeds certain thresholds for the period September 13, 2019 to December 31, 2019 and the year ended December 31, 2020 (“Earnout” or “contingent consideration”).
Transaction costs incurred by the Company were $6,245 and $2,267 for the Successor 2019 Period and the Predecessor 2019 Period, respectively, and are recorded within transaction costs in the Consolidated Statements of Income (Loss). The elements of the purchase consideration are as follows:
| Cash paid |
$ | 807,591 | ||
| Fair value of Class A and B common units issued |
306,000 | |||
| Fair value of Earnout |
172,000 | |||
|
|
|
|||
| Total consideration |
$ | 1,285,591 | ||
|
|
|
Contingent Consideration
The contingent consideration represents the fair value of the Earnout payments to Norvax’s selling shareholders and will be adjusted to fair value at each reporting date until settled. The contingent consideration will be settled in Common and Senior Preferred Earnout Units within 60 days of the issuance of the 2019 and 2020 audited financial statements. The Senior Preferred Earnout Units earn an annual coupon of 10.3% that provides for the accrual of additional units. Changes in fair value of the contingent consideration are recognized in income (loss) from operations. The full amount available relative to the 2019 target was earned as of December 31, 2019, and, as a result, the Company recorded a $75,000 fair value adjustment to the contingent consideration liability for achieving the 2019 target. The Company recorded a fair value adjustment of $4,300 to reduce the contingent consideration liability related to the 2020 target due to changes in forecasts.
Allocation of Preliminary Purchase Price
The preliminary allocation of the purchase price is based on the fair value of assets acquired and liabilities assumed as of the acquisition date. The components of the preliminary purchase price allocation are as follows:
| Net working capital |
$ |
18,787 |
| |
| Commission receivable – non-current |
113,565 | |||
| Property and equipment |
4,442 | |||
| Other noncurrent assets |
218 | |||
| Other noncurrent liabilities |
(963 | ) | ||
| Trade names |
83,000 | |||
| Developed technology |
496,000 | |||
| Customer relationships |
232,000 | |||
| Goodwill |
386,553 | |||
| Deferred revenue |
(3,283 | ) | ||
| Commissions payable – non-current |
|
(44,728 |
) | |
|
|
|
|||
| Total consideration transferred |
$ | 1,285,591 | ||
|
|
|
F-21
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
Goodwill represents the excess of the consideration paid over the estimated fair value of assets acquired and liabilities assumed in a business combination and is primarily attributable to future growth and the assembled workforce.
The Acquisition was accounted for using the acquisition method of accounting. The Company’s consolidated financial statements reflect the preliminary allocation of the purchase price to the assets and liabilities assumed based on fair value as of the date of the acquisition.
Had the Acquisition been completed on January 1, 2018, net revenues would be unchanged and the net loss would be approximately $29,500 and $95,380 for the years ended December 31, 2019 and December 31, 2018, respectively. This unaudited pro forma financial information is presented for illustrative purposes only and is not necessarily indicative of what the operating results actually would have been if the Acquisition had taken place on January 1, 2018, nor is it indicative of future operating results. The pro forma amounts include the historical operating results of the Company prior to the acquisition, with adjustments factually supportable and directly attributable to the Acquisition, primarily related to transaction costs, the amortization of intangible assets, and interest expense. Share-based compensation and transaction bonuses and costs totaling $98,213 for the year ended December 31, 2019 are non-recurring pro forma adjustments.
3. BALANCE SHEET ACCOUNTS
Commissions Receivable
Commissions receivable activity is summarized as follows:
| Successor | Predecessor | |||||||||||||||||||
| Period from September 13, 2019 through December 31, 2019 |
Period from January 1, 2019 through September 12, 2019 |
Year Ended December 31, 2018 | ||||||||||||||||||
| Beginning balance |
$ | 178,975 | $ | 115,527 | $ | 50,082 | ||||||||||||||
| Commission revenue |
243,347 | 175,834 | 144,378 | |||||||||||||||||
| Cash receipts |
(39,391 | ) | (112,386 | ) | (78,933 | ) | ||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Ending balance |
382,931 | 178,975 | 115,527 | |||||||||||||||||
| Less: Commissions receivable – current |
101,078 | 65,410 | 38,685 | |||||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Commissions receivable – non-current |
$ | 281,853 |
|
|
|
$ | 113,565 | $ | 76,842 | |||||||||||
|
|
|
|
|
|
|
|||||||||||||||
The commissions receivable balance as of December 31, 2019 and 2018, primarily relates to Medicare Advantage Plans sold during the fourth quarters of 2019 and 2018 with effective dates in 2020 and 2019, respectively.
F-22
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
Property, Equipment, and Capitalized Software, net
Property, equipment, and capitalized software, net, consist of the following:
| Successor December 31, 2019 |
|
Predecessor December 31, 2018 |
||||||||||
| Computer equipment |
$ | 3,163 | $ | 7,055 | ||||||||
| Leasehold improvements |
1,046 | 4,110 | ||||||||||
| Office equipment and furniture |
689 | 1,658 | ||||||||||
|
|
|
|
|
|||||||||
| Property and equipment |
4,898 | 12,823 | ||||||||||
| Capitalized software |
1,962 | 18,981 | ||||||||||
|
|
|
|
|
|||||||||
| Less: accumulated depreciation and amortization |
(521 | ) | (20,022 | ) | ||||||||
|
|
|
|
|
|||||||||
| Property, equipment, and capitalized software, net |
$ | 6,339 |
|
|
|
$ | 11,782 | |||||
|
|
|
|
|
|||||||||
Depreciation expense for the Successor 2019 Period, the Predecessor 2019 Period, and the year ended December 31, 2018, was $421, $1,262 and $1,547, respectively. These amounts include $91 in the Successor 2019 Period, $73 in the Predecessor 2019 Period and $96 in 2018 of depreciation of assets recorded under capital leases.
Amortization expense related to capitalized software was $100, $2,985 and $4,613 for the period from September 13, 2019 through December 31, 2019, the period from January 1, 2019 through September 12, 2019 and the year ended December 31, 2018, respectively.
Accrued Liabilities
Accrued liabilities consist of the following:
| Successor December 31, 2019 |
|
Predecessor December 31, 2018 |
||||||||||
| Bonuses and commissions |
$ | 12,292 | $ | 5,372 | ||||||||
| Marketing costs |
2,384 | 1,975 | ||||||||||
| Interest expense |
2,167 | — | ||||||||||
| Other accrued expenses |
5,725 | 2,373 | ||||||||||
|
|
|
|
|
|||||||||
| Accrued liabilities |
$ | 22,568 | $ | 9,720 | ||||||||
|
|
|
|
|
|||||||||
F-23
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
4. FAIR VALUE MEASUREMENTS
The Company defines fair value as the price that would be received for an asset or paid to transfer a liability (an exit price) in the principal or most advantageous market for the asset or liability in an orderly transaction between market participants on the measurement date. Valuation techniques the Company uses to measure fair value maximize the use of observable inputs and minimize the use of unobservable inputs. The Company classifies the inputs used to measure fair value into the following hierarchy:
| Level 1 | Unadjusted quoted prices in active markets for identical assets or liabilities. |
| Level 2 | Unadjusted quoted prices in active markets for similar assets or liabilities; unadjusted quoted prices for identical or similar assets or liabilities in markets that are not active; inputs other than quoted prices that are observable for the asset or liability. |
| Level 3 | Unobservable inputs for the asset or liability. |
Fair Value Measurements
The fair value of the acquired developed technology has been estimated using the multi-period excess earnings model. This method discounts the amount of excess cash flows generated by the asset. The fair value of the acquired trade names was estimated using the relief from-royalty method which required that the Company estimate hypothetical royalty payments that would be required over the economic life of the asset as if it were to be licensed instead of purchased. These payments were then discounted to their present value. Both developed technology and trade names represent a Level 3 measurement within the fair value hierarchy.
The fair value of the acquired customer relationships was estimated using the distributor method under the income approach, which included Level 3 inputs such as revenue, attrition, margin and contributory asset charges.
The fair value of the contingent consideration was measured using a Monte Carlo simulation and is discounted using a rate that appropriately captures the risk associated with the obligation. The contingent consideration was part of the acquisition consideration and will be adjusted to fair value at each reporting date until settled. The following table sets forth the fair value and a summary of the changes to fair value of the contingent consideration:
| Balance at September 13, 2019 |
$ | 172,000 | ||
| Successor 2019 Period earnout fair value adjustment |
75,000 | |||
| 2020 earnout fair value adjustment |
(4,300 | ) | ||
|
|
|
|||
| Balance at December 31, 2019 |
$ | 242,700 | ||
|
|
|
The carrying amount of certain financial instruments, including cash, accounts receivable, commissions receivable, accounts payable, accrued expenses, and commissions payable approximate fair value due to the short maturity of these instruments. Commissions receivable are recorded at constrained lifetime values.
F-24
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
5. GOODWILL AND INTANGIBLE ASSETS, NET
The carrying amounts, accumulated amortization, net carrying value and weighted average remaining life of the Company’s definite-lived amortizable intangible assets, as well as its definite-lived intangible trademarks, are presented in the table below (weighted-average useful life is as of December 31, 2019):
| December 31, 2019 (Successor) | ||||||||||||||||
| Gross Carrying Amount |
Accumulated Amortization |
Net carrying amount |
Weighted average useful life |
|||||||||||||
| Developed technology |
$ | 496,000 | $ | 21,257 | $ | 474,743 | 7 | |||||||||
| Customer relationships |
232,000 | 6,960 | 225,040 | 10 | ||||||||||||
|
|
|
|
|
|
|
|||||||||||
| Total intangible assets subject to amortization |
$ | 728,000 | $ | 28,217 | $ | 699,783 | ||||||||||
|
|
|
|
|
|
|
|||||||||||
| Indefinite-lived trademarks |
83,000 | |||||||||||||||
|
|
|
|||||||||||||||
| Intangible Assets |
$ | 782,783 | ||||||||||||||
|
|
|
|||||||||||||||
There were no intangible assets or goodwill in the Predecessor 2019 Period or at December 31, 2018.
As of December 31, 2019, expected amortization expense related to intangible assets in future periods is as follows:
| Years Ending December 31, |
Developed Technology |
Customer Relationships |
Total | |||||||||
| 2020 |
$ | 70,857 | $ | 23,200 | $ | 94,057 | ||||||
| 2021 |
70,857 | 23,200 | 94,057 | |||||||||
| 2022 |
70,857 | 23,200 | 94,057 | |||||||||
| 2023 |
70,857 | 23,200 | 94,057 | |||||||||
| 2024 |
70,857 | 23,200 | 94,057 | |||||||||
| Thereafter |
120,458 | 109,040 | 229,498 | |||||||||
|
|
|
|
|
|
|
|||||||
| Total |
$ | 474,743 | $ | 225,040 | $ | 699,783 | ||||||
|
|
|
|
|
|
|
|||||||
The Company allocated $380,327 and $6,226 of the goodwill recognized in connection with the Acquisition to its Medicare—Internal segment and Medicare—External segment, respectively, based on an estimate of the relative fair value of each segment. There was no impairment of goodwill or intangible assets for the Successor 2019 Period.
F-25
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
6. LONG TERM DEBT
The Company’s long-term debt consisted of the following:
| Interest rate | Successor December 31, 2019 |
Predecessor December 31, 2018 | ||||||||||||||||||
| Predecessor Credit Facility |
$ | — | $ | 4,856 | ||||||||||||||||
|
|
|
|
|
|||||||||||||||||
| Total debt |
$ | — | $ | 4,856 | ||||||||||||||||
|
|
|
|
|
|||||||||||||||||
| Credit Facility |
8.29% - 8.55% | $ | 299,250 | $ | — | |||||||||||||||
| Less: unamortized debt discount and capitalized issuance costs |
(8,017 | ) | — | |||||||||||||||||
|
|
|
|
|
|||||||||||||||||
| Total debt |
291,233 | $ | 4,856 | |||||||||||||||||
| Less: current portion |
(3,000 | ) | 4,856 | |||||||||||||||||
|
|
|
|
|
|||||||||||||||||
| Total long-term debt |
$ | 288,233 | $ | — | ||||||||||||||||
|
|
|
|
|
|||||||||||||||||
Maturities of long-term debt for each of the next five years and thereafter are as follows:
| 2020 |
3,000 | |||
| 2021 |
3,000 | |||
| 2022 |
3,000 | |||
| 2023 |
3,000 | |||
| 2024 |
3,000 | |||
| Thereafter |
284,250 | |||
|
|
|
|||
| Total |
299,250 | |||
|
|
|
Successor
General
On September 13, 2019, in connection with the Acquisition, Norvax, or the Borrower, entered into a first lien credit agreement (the “Credit Agreement”) which provides for the following:
| • | $300,000 aggregate principal amount senior secured term loan facility, or the Term Loan Facility; and |
| • | $30,000 aggregate principal amount senior secured revolving credit facility, or the Revolving Credit Facility. |
On March 20, 2020, the Company entered into an amendment to the Credit Agreement, which provided $117 million of incremental term loans, or the “Incremental Term Loan Facility”. The Company collectively refers to the Term Loan Facility, the Revolving Credit Facility, and the Incremental Term Loan Facility as the “Credit Facilities”.
The Company incurred $9,283 of debt issuance costs associated with the Credit Facility, which is being amortized over the life of the debt under the effective interest rate method to interest expense.
As of December 31, 2019, the Company had a principal amount of $299,250 outstanding on the Term Loan Facility and no amounts outstanding on the Revolving Credit Facility. The Revolving Credit Facility had remaining capacity of $30,000 as of December 31, 2019.
F-26
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
Interest Rates and Fees
Borrowings under the Credit Facilities are, at the option of the Borrower, either alternate base rate (“ABR”) loans or LIBOR loans. Term loans and revolving loans comprising each ABR borrowing under the Term Loan Facility accrue interest at the ABR plus an applicable rate. The current applicable rate for ABR term loans and revolving loans is 5.50% per annum and ranges from 4.75% to 5.50% per annum, in each case, based upon specified leverage ratios. Term loans and revolving loans comprising each LIBOR borrowing bear interest at the LIBOR plus an applicable rate. The current applicable rate for LIBOR term loans and revolving loans is 6.50% per annum and ranges from 5.75% to 6.50% per annum, in each case, based upon specified leverage ratios.
In addition to paying interest on the principal amounts outstanding under the Credit Facilities, the Borrower is required to pay a commitment fee of 0.50% per annum under the Revolving Credit Facility in respect of the unutilized commitments thereunder. The Borrower is also subject to customary letter of credit and agency fees.
Mandatory Prepayments
The Credit Agreement requires that the Borrower, following the end of each fiscal year, commencing with the fiscal year ending December 31, 2020, repay the outstanding principal amount of all term loans under the Credit Facilities in an aggregate amount equal to (A) 50.0% of the excess cash flow of the Borrower and its restricted subsidiaries for such fiscal year if the Total Net Leverage Ratio (as defined in the Credit Agreement) is greater than 4.50:1.00, which percentage is reduced to 25% if the Total Net Leverage Ratio is less than or equal to 4.50:1.00 and greater than 4.00:1.00, which percentage is further reduced to 0% if the Total Net Leverage Ratio is less than or equal to 4.00:1.00, minus (B) at the option of the Borrower, (x) the aggregate amount of certain voluntary prepayments of term loans under the Credit Agreement during such fiscal year or after year-end and prior to the time such Excess Cash Flow prepayment is due, (y) the aggregate principal amount of any voluntary prepayments of indebtedness under pari passu incremental facilities, incremental equivalent debt and/or certain refinancing indebtedness, made during such fiscal year or after such fiscal year and prior to the time such prepayment is due.
The Credit Agreement requires the Borrower to repay amounts equal to 100% of the net cash proceeds of certain asset sales or other dispositions of property (including insurance and condemnation proceeds); provided, that, in the case of any prepayment events required in connection with certain dispositions and casualty events, if the net proceeds therefrom are invested (or committed to be invested) within 12 months after the receipt of such net proceeds, then no prepayment shall be required except to the extent such net proceeds have not been so invested (or committed to be invested) by the end of such 12-month period.
The Credit Agreement requires 100% of the net proceeds from the issuance or incurrence of certain indebtedness to be applied to prepay the term loans under the Term Loan Facility, except to the extent the indebtedness constitutes refinancing indebtedness.
Voluntary Prepayment
The Borrower may voluntarily prepay outstanding borrowings under the Credit Facilities at any time in whole or in part without premium or penalty; provided, that, with respect to voluntary prepayments of the Term Loan Facility and in certain other circumstances, the Borrower may have to pay a prepayment premium.
F-27
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
Amortization and Final Maturity
The Term Loan Facility is payable in quarterly installments (commencing on December 31, 2019) in the principal amount of 0.25% of the original principal amount. The remaining unpaid balance on the Term Loan Facility, together with all accrued and unpaid interest thereon, is due and payable on or prior to September 13, 2025. Outstanding borrowings under the Revolving Credit Facility do not amortize and are due and payable on September 13, 2024.
Guarantees and Security
The Borrower’s obligations under the Credit Facilities are guaranteed by Blizzard Midco, LLC and certain of the Borrower’s subsidiaries. All obligations under the Credit Agreement are secured by a first priority lien on substantially all of the assets of the Borrower, including a pledge of all of the equity interests of its subsidiaries.
Covenants and Other Matters
The Credit Agreement contains a number of covenants that, among other things and subject to certain exceptions, restrict the Borrower’s and its restricted subsidiaries’ ability to:
| • | incur indebtedness; |
| • | incur certain liens; |
| • | consolidate, merge or sell or otherwise dispose of assets; |
| • | make investments, loans, advances, guarantees and acquisitions; |
| • | pay dividends or make other distributions on equity interests, or redeem, repurchase or retire equity interests; |
| • | enter into transactions with affiliates; |
| • | alter the business conducted by the Company and subsidiaries; |
| • | change their fiscal year; and |
| • | amend or modify governing documents. |
In addition, the Credit Agreement contains financial and non-financial covenants. The Company is in compliance with all covenants as of December 31, 2019.
The Credit Agreement also contains certain customary representations and warranties and affirmative covenants, and certain reporting obligations. In addition, the lenders under the Credit Facilities will be permitted to accelerate all outstanding borrowings and other obligations, terminate outstanding commitments and exercise other specified remedies upon the occurrence of certain events of default (subject to certain grace periods and exceptions), which include, among other things, payment defaults, breaches of representations and warranties, covenant defaults, certain cross-defaults and cross-accelerations to other indebtedness, certain events of bankruptcy and insolvency, certain judgments and changes of control. Subject to certain limited exceptions, substantially all of the Company’s assets are restricted from distribution.
Predecessor
During 2019, Norvax had a senior secured revolving credit facility (the “Predecessor Credit Facility”) with The Huntington National Bank (formerly FirstMerit Bank N.A.). In connection with the Acquisition, this facility was paid off and retired.
F-28
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
During 2018, Norvax amended its credit facility to increase the Predecessor Credit Facility from a maximum borrowing of $10,000 to $12,000 and again from $12,000 to $16,000. The Predecessor Credit Facility provided for borrowings up to a maximum of $16,000 based upon 80% of eligible trade accounts receivable, plus 40% of certain earned enrollment/commission fees. Norvax paid a variable interest rate on borrowings equal to, at Norvax’s discretion, Prime minus 50 basis points or LIBOR plus 250 basis points. Proceeds from borrowings were used to finance working capital and other general corporate purposes. The Predecessor Credit Facility was collateralized by substantially all the assets of Norvax and was subject to certain financial covenants. These covenants included maintaining a minimum fixed charge coverage ratio and not exceeding a maximum funded debt to earnings before interest, taxes, depreciation and amortization ratio (as defined in the credit agreement). The Predecessor Credit Facility originally matured in August 2019 and Norvax and The Huntington National Bank agreed to extend the maturity to November 2019.
7. MEMBERS’ EQUITY
Successor
The GoHealth Holdings, LLC operating agreement (“Operating Agreement”) provides for the classes of units, allocation of profits and losses, and other member rights. The Operating Agreement allows for equity Preferred units (the “Preferred”) and Common units (the “Common”). Preferred units are divided into two classes: Senior Preferred Earnout Units, which are non-voting, and Preferred Units (“Preferred Unit”), which have voting rights. Common units are divided into two classes: Class A Common units (“Class A”), which have voting rights and Class B Common units (“Class B”), which are non-voting. Members of management will be issued profits interests (the “Profit Units”, and together with the Preferred units and the Common units, the “Units”) from an equity pool with an aggregate value equal to 10% of the Company’s fully diluted equity.
Voting Rights
Each Preferred Unit and Class A unit has equal voting rights. The Preferred Unit and Class A unit holders also elect the members of the board of managers of the Company based on the percentage of units held by such investor.
Liquidation Preference
Upon a liquidity event defined as: (a) sale or disposition of all or substantially all of the assets of the Company; or (b) the liquidation, dissolution or winding up of the Company; first, in connection with refinancing or repayment of debt, Senior Preferred Earnout Units, the ceiling of which is the face amount of the Senior Preferred Earnout Units; second, Preferred Unit holders up to 150% of their invested capital; third, to Common holders, up to 150% of their invested capital; fourth, to the Profit Unit holders, pro rata, with the residual to the Common holders, pro rata, up to 150% of their invested capital, inclusive of prior distributions; fifth, to the Profit Unit holders, pro rata, with the residual to all members until each has received an aggregate amount of additional capital contributions, less amounts previously distributed; sixth, to Preferred Unit, Common and Profit Unit holders until Preferred Unit holders have received a cumulative amount equal to 250% of their invested capital; seventh, to Common holders equal to $75,000; eighth, pro rata, 100% Common, 100% Profit units, and 90% Preferred Unit/10% Common until Preferred Unit holders have received 300% of their invested capital; ninth, Common holders equal to $75,000; tenth, pro rata, 100% Common, 100% Profit units, 85% Preferred Unit/15% Common until Preferred Unit holders receive 400% of their invested capital; and, eleventh, pro rata, 100% Common, 100% Profit units and 80% Preferred Unit/20% Common.
F-29
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
Right of First Offer
Following the fifth anniversary of the Closing, Common units will be freely transferable, subject to customary “prohibited transfer” restrictions and a right of first offer for the benefit of the Company, first, and any non-transferring Investors, second.
Predecessor
The Norvax operating agreement (“Norvax Operating Agreement”) provided for classes of units, allocation of profits and losses, distribution rights, and other member rights. The Norvax Operating Agreement allowed for equity units (Class A units and Class B units) and profits interests units (Class C units). Class A and Class B units had voting rights. Except for board of manager composition, any action taken by the Class A and Class B members required a majority of members holding the outstanding Class A and Class B units, voting together as a single class. Class C units were nonvoting and represented profit interests’ units and entailed no initial capital contribution. Members were limited in their liability to their capital contributions. Immediately prior to the Acquisition described in Note 2 – Acquisition, all Class B units converted to Class A units.
Distribution Rights
Class A and Class B unit holders were entitled to distributions on a pro-rata basis, as approved by the board of managers. To the extent that Norvax had available cash, it distributed to each Class A and Class B unit holder a tax distribution in an amount equal to the product of the aggregate total of all taxable income allocable to the members multiplied by the tax rate. The tax rate is 45% as set forth in the Norvax Operating Agreement.
Voting Rights
Each Class A and Class B unit had equal voting rights and preferences, except Norwest Equity partners (“NEP”) was granted authority to approve certain actions. The Class A and Class B unit holders also elected the members of the board of managers of Norvax.
Antidilution Rights
Class B units contained an antidilution feature that required an adjustment to the conversion ratio in the event of subsequent issuances of securities by Norvax at a price below the conversion price in effect immediately prior to each such issuance. The Class B conversion ratio could be adjusted in the event that grants of options or changes in option prices or conversion rates on convertible securities resulted in prices below the conversion price in effect immediately prior to each such grant or change.
Liquidation Preference
Upon a liquidity event defined as: (a) sale or disposition of all or substantially all of the assets of Norvax; (b) the liquidation, dissolution or winding up of Norvax; or (c) any consolidation or merger of Norvax in which the Class A and Class B unit holders owned less than 50% of the voting power of the outstanding securities immediately after the consolidation or merger, the Class B units are first to be paid proceeds at a liquidation amount of $10.00 per unit, and from time to time, was decreased by subtracting distributions (other than tax distributions) made in respect to Class B units.
Upon the occurrence of a Dissolution Event, Norvax continued solely for the purposes of winding up its affairs in an orderly manner, liquidating its assets, and satisfying the claims of its creditors and members. A Dissolution
F-30
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
Event is an event by the order of a court pursuant to Section 18-802 of the Delaware Code or by action of the members with NEP’s approval. Net income, net losses, and other items of Norvax’s income, gain, loss, or deduction was to continue to be allocated in the manner provided in the Norvax Operating Agreement. In a Dissolution Event, Class B units received the liquidation preference specified above.
Involuntary Transfer Rights
Upon any involuntary transfer, Norvax had the first option, and the purchase option unit holders had the subsequent options, to purchase all or any portion of the units subject to the involuntary transfer.
Right of First Refusal
A unit holder could transfer, sell, or assign any Class A or Class B units in a permitted transfer, given that Norvax first had the option to purchase the units being transferred.
Class B Put Option
Class B units are classified as temporary equity as they were redeemable upon exercise of the Class B put option, which was outside of Norvax’s control, for cash at a put price equal to the greater of the Class B unit fair value or their original cost. Because the Class B units were redeemable, the Company was accreting the change up to the maximum redemption amount. The Company recorded accretion of $196,700 in the year ended December 31, 2018. These amounts appear as Class B unit accretion on the Consolidated Statements of Changes in Members’ Equity.
Immediately prior to the Acquisition described in Note 2 – Acquisition, Norvax recorded accretion of $138,404 to adjust NEP’s Redeemable Class B units to their full redemption amounts and were then converted to Class A units.
8. SHARE-BASED COMPENSATION PLANS
The following table summarizes the share-based compensation expense by operating function for the following periods:
| Successor | Predecessor | |||||||||||||||
| Period from September 13, 2019 through December 31, 2019 |
Period from January 1, 2019 through September 12, 20191 |
Year Ended December 31, 2018 |
||||||||||||||
| Marking and advertising |
$ | 53 | $ | 1,674 | $ | — | ||||||||||
| Customer care and enrollment |
20 | — | — | |||||||||||||
| Technology |
66 | 27,059 | — | |||||||||||||
| General and administrative |
309 | 58,327 | — | |||||||||||||
|
|
|
|
|
|
|
|||||||||||
| Total share-based compensation expense |
$ | 448 | $ | 87,060 | $ | — | ||||||||||
|
|
|
|
|
|
|
|||||||||||
| 1 | Includes Class C incentive plan and incentive share plan |
Successor
Effective September 13, 2019 and in conjunction with the Acquisition, the Company authorized the grants of non-voting Profit Units. The Profits Units are issued by Blizzard Management Feeder, LLC, to employees on
F-31
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
behalf of the Company. One-third of the Profit Units granted to each employee (“Time-Vesting Units”) will vest in five (5) equal installments on the first through fifth anniversaries of the date of grant, so long as the employee remains employed by the Company through the applicable vesting date. Two-thirds of the Profit Units granted to each individual will vest upon a liquidity event based on the extent to which the distributions received by the Preferred and the Common exceed their investment in the Company (“Performance-Vesting Units”).
Compensation expense for the Time-Vesting Units is recognized on a straight-line basis over the five-year requisite service period. Performance-Vesting Units contain market conditions and an implied performance condition, which results in compensation cost being recognized when the performance condition is considered probable of being satisfied. Performance-Vesting Units vest upon the achievement of a contingent exit event that is defined as a transaction in which the ultimate parent disposes of all or substantially all its investment in the Company. Such an exit event is not considered probable until it consummates.
The number of Profit Units eligible for issuance will equal, in the aggregate, approximately 10% of the fully diluted equity of the Company at the closing of the Acquisition. All Profit Units (i.e., issued at closing of the Acquisition or issued thereafter) will have the economic rights and entitlements in relation to other equity interests in the Company under the waterfall described in the Operating Agreement.
A summary of the share-based compensation awards issued to employees of the Company by Blizzard Management Feeder, LLC, is as follows:
| Time Vesting Units |
Weighted Average Fair Value at Date of Grant per Unit |
Performance Vesting Units |
Weighted Average Fair Value at Date of Grant per Unit |
|||||||||||||
| Unvested units at September 13, 2019 |
— | — | ||||||||||||||
| Granted |
25,871,374 | $ | 0.36 | 52,526,759 | $ | 0.31 | ||||||||||
| Vested |
— | — | ||||||||||||||
|
|
|
|
|
|||||||||||||
| Unvested units at December 31, 2019 |
25,871,374 | 52,526,759 | ||||||||||||||
|
|
|
|
|
|||||||||||||
The fair value of the Profit Units is determined using a Monte Carlo simulation and the following assumptions:
| Period from September 13, 2019 through December 31, 2019 | ||
| Risk free interest rate |
1.73% | |
| Expected volatility |
50% | |
| Expected life (years) |
5.0 | |
| Expected dividend yield |
0.0% |
The expected life is based on estimates of the likely timing of a liquidity event. Volatility was determined based on an analysis of publicly traded peers.
As of December 31, 2019, there was $8,819 of unamortized share-based compensation expense related to the Time-Vesting Units and these costs are expected to be recognized over a remaining weighted average period of 4.8 years. There was $16,284 of unrecognized share-based compensation expense related to the Performance-Vesting Units. The Company will recognize these costs upon the achievement of a contingent exit event.
The Company granted an additional 6,001,788 of Profits Units in 2020, of which 1,980,580 and 4,021,208 were Time-Vesting Units and Performance-Vesting Units, respectively.
F-32
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
Predecessor
Class C Incentive Plan
Norvax had a Class C Incentive Plan (the “Class C Plan”), which Norvax accounted for as a liability award. Class C units granted under the plan represented profit interests’ units and entailed no initial capital contribution. Class C units had no voting rights.
On September 13, 2019, GoHealth Holdings, LLC acquired a 100% interest in Norvax. Per the Class C Plan, all eligible unvested units became vested and the Company recorded $73,938 of compensation expense in the Predecessor 2019 Period.
Incentive Share Plan
Norvax had an Incentive Share Plan, which Norvax accounted for as a liability award. The plan consisted of incentive share grants made to employees that provided for cash payments to participants upon the occurrence of a triggering event. Triggering events included a change in control or an employee’s involuntary termination without cause. In the event of a change in control, the triggering event value per share was the average per share purchase price of the common stock giving rise to such change in control. Cash payments were based on the difference between the triggering event value per share and the value per share on the grant date. In the event of an involuntary termination without cause, cash payments were calculated as the positive difference between the book value per share of Norvax’s stock on the date of the triggering event and the value per share on the grant date for each incentive share then triggered, as defined in the Incentive Share Plan.
On September 13, 2019, GoHealth Holdings, LLC acquired a 100% interest in Norvax. Per the Incentive Share Plan, a change in control triggering event occurred and employees granted incentive shares under this plan became eligible for cash payments and as a result, the Company recorded $13,122 in incentive share expense in the Predecessor 2019 Period.
F-33
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
9. INCOME TAXES
The Company’s provision for income taxes consists of the following for the Predecessor 2019 Period, the Successor 2019 Period, and the year ended December 31, 2018:
| Successor | Predecessor | |||||||||||||||||||
| Period from September 13, 2019 through December 31, 2019 |
Period from January 1, 2019 through September 12, 2019 |
Year Ended December 31, 2018 |
||||||||||||||||||
| Income (loss) before provision for income taxes: |
||||||||||||||||||||
| U.S. |
$ | 15,514 | $ | (57,227 | ) | 28,166 | ||||||||||||||
| Foreign |
525 | 98 | (6 | ) | ||||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Total |
16,039 | (57,129 | ) | 28,160 | ||||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Provision (benefit) from income taxes: |
||||||||||||||||||||
| Current: |
||||||||||||||||||||
| U.S. Federal |
(3 | ) | — | 38 | ||||||||||||||||
| State and Local |
(1 | ) | 57 | 12 | ||||||||||||||||
| Foreign |
110 | 21 | — | |||||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Total current |
106 | 78 | 50 | |||||||||||||||||
| Deferred: |
||||||||||||||||||||
| U.S. Federal |
(75 | ) | (114 | ) | (3 | ) | ||||||||||||||
| State and Local |
13 | (30 | ) | (1 | ) | |||||||||||||||
| Foreign |
— | — | — | |||||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Total deferred |
(62 | ) | (144 | ) | (4 | ) | ||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Total provision (benefit) for income taxes |
$ | 44 | $ | (66 | ) | 46 | ||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
As of both December 31, 2019 and 2018, the Company had no state tax net operating loss carryforwards or state tax credit carryforwards.
10. COMMITMENTS AND CONTINGENCIES
Leases
As of December 31, 2019, the Company had $821 of assets acquired under capital leases, for which the net book value was $725. The Company has capital lease arrangements to obtain computer equipment and furniture for the Company’s operations.
The Company entered into various non-cancelable operating lease agreements for certain of the Company’s offices and data centers with lease periods expiring in 2030. Certain of these arrangements have free rent periods or escalating rent payment provisions, and the Company recognizes rent expense under such arrangements on a straight-line basis. The Company recognized rent expense of $1,979, $3,102 and $2,795 for the Successor 2019 Period, the Predecessor 2019 Period, and year ended December 31, 2018, respectively.
F-34
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
Future minimum lease payments required under non-cancelable capital and operating leases as of December 31, 2019 were as follows:
| Capital Leases |
Operating Leases |
|||||||
| 2020 |
$ | 328 | $ | 5,921 | ||||
| 2021 |
335 | 6,063 | ||||||
| 2022 |
105 | 6,209 | ||||||
| 2023 |
— | 6,360 | ||||||
| 2024 and thereafter |
— | 12,708 | ||||||
|
|
|
|
|
|||||
| Total minimum lease payments |
$ | 768 | $ | 37,261 | ||||
|
|
|
|||||||
| Less: amounts representing interest and taxes |
(55 | ) | ||||||
| Less: current portion of the present value of minimum lease payments |
(292 | ) | ||||||
|
|
|
|||||||
| Non-current liabilities, net of current portion |
$ | 421 | ||||||
|
|
|
|||||||
Legal Proceedings
From time to time, the Company is party to various litigation matters incidental to the conduct of its business. The Company is not presently party to any legal proceedings the resolution of which it believes would have a material adverse effect on its business, prospects, financial condition, liquidity, results of operation, cash flows or capital levels.
11. RELATED-PARTY TRANSACTIONS
The Company has entered into various lease agreements with 214 W Huron LLC, 220 W Huron Street Holdings LLC, and 215 W Superior LLC, each of which are controlled by significant shareholders, to lease its corporate offices in Chicago, Illinois. The Company pays rent, operating expenses, maintenance, and utilities under the terms of the leases. For the period from September 13, 2019 through December 31, 2019, the period from January 1, 2019 through September 12, 2019 and the year ended December 31, 2018, the Company made aggregate lease payments of $298, $758, and $1,025, respectively, under these leases. In November 2019, the Company entered into an agreement with 215 W Superior LLC, to lease additional office space beginning in January 2020 and expiring on December 31, 2030. The lease’s first year annual rent is $145, with annual increases of $0.50 per square foot thereafter.
On January 1, 2020, the Company entered into a non-exclusive aircraft dry lease agreement with an entity wholly-owned and controlled by significant shareholders. The agreement allows the Company to use an aircraft owned by this entity for business and on an as-needed basis. The agreement has no set term and is terminable without cause by either party upon 30 days’ prior written notice. Under the agreement, the Company is required to pay $7,855.94 per flight hour for use of the aircraft.
12. OPERATING SEGMENTS AND SIGNIFICANT CUSTOMERS
Operating Segments
The Company reports segment information based on how the Company’s chief operating decision maker (“CODM”), regularly reviews operating results, allocates resources and makes decisions regarding business operations. The performance measures of the segments include total revenue and profit (loss). For segment
F-35
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
reporting purposes in accordance with ASC 280-10, Segment Reporting, the Company’s business structure is comprised of four operating and reportable segments:
| • | Medicare Internal and External: The Medicare internal and external segments consist primarily of revenues earned from sales of Medicare Advantage, Medicare Supplement, Prescription Drug Plans, and Medicare Special Needs Plans (or “SNPs”), for multiple carriers. |
| • | Individual and Family Plan and Other (“IFP and Other”) Internal and External: The IFP and Other internal and external segments consist primarily of revenues earned from sales of individual and family plans, dental plans, vision plans and other ancillary plans to individuals that are not Medicare-eligible. |
The Internal and External segments relative to both Medicare and IFP are defined as follows:
| • | Internal: The two internal segments primarily consist of sales of products and plans by Company-employed agents offering qualified prospects plans from multiple carriers, Company-employed agents offering qualified prospects plans on a carrier-specific basis, or sales of products and plans through our online platform without the assistance of our agents (do-it-yourself or “DIY”). The Company earns revenue in this channel through commissions paid by carriers based on sales the Company generates, as well as enrollment fees, hourly fees and other fees for services performed for specific carriers and other partners |
| • | External: The two external segments represent sales of products and plans under the Company’s carrier contracts using an independent, national network of agents who are not employed by Company. These agents utilize the Company’s technology and platform to enroll consumers in health insurance plans and provide a means to earn a return on leads that otherwise may have not been addressed. The Company also sells insurance prospects (or “leads”) to agencies within this channel. The Company earns revenue in this channel through commissions paid by carriers as a result of policy sales, as well as sales of leads to external agencies. |
F-36
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
The following table presents summary results of the Company’s operating segments for the following periods:
| Successor | Predecessor | |||||||||||||||||||
| Period from September 13, 2019 through December 31, 2019 |
Period from January 1, 2019 through September 12, 2019 |
Year Ended December 31, 2018 |
||||||||||||||||||
| Revenues: |
||||||||||||||||||||
| Medicare: |
||||||||||||||||||||
| Internal channel |
$ | 215,322 | $ | 102,196 | $ | 53,365 | ||||||||||||||
| External channel |
59,152 | 55,981 | 58,834 | |||||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Total Medicare |
274,474 | 158,177 | 112,199 | |||||||||||||||||
| Individual and Family Plan and Other: |
||||||||||||||||||||
| Internal channel |
20,850 | 37,909 | 63,009 | |||||||||||||||||
| External channel |
13,167 | 34,924 | 50,997 | |||||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Total Individual and Family Plan and Other |
34,017 | 72,833 | 114,006 | |||||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Total revenues |
308,491 | 231,010 | 226,205 | |||||||||||||||||
| Segment profit: |
||||||||||||||||||||
| Medicare: |
||||||||||||||||||||
| Internal channel |
126,210 | 40,024 | 24,183 | |||||||||||||||||
| External channel |
10,584 | 4,893 | 9,034 | |||||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Total Medicare segment profit |
136,794 | 44,917 | 33,217 | |||||||||||||||||
| Individual and Family Plan and Other: |
||||||||||||||||||||
| Internal channel |
1,650 | 2,195 | 9,707 | |||||||||||||||||
| External channel |
584 | 1,748 | 2,848 | |||||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Total Individual and Family Plan and Other segment profit |
2,234 | 3,943 | 12,555 | |||||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Total segment profit |
139,027 | 48,860 | 45,773 | |||||||||||||||||
| Corporate |
9,767 | 103,469 | 1 | 17,009 | ||||||||||||||||
| Change in fair value of contingent consideration liability |
70,700 | — | — | |||||||||||||||||
| Amortization of intangible assets |
28,217 | — | — | |||||||||||||||||
| Transaction costs |
6,245 | 2,267 | — | |||||||||||||||||
| Interest expense |
8,076 | 140 | 224 | |||||||||||||||||
| Other income (expense) |
17 | (114 | ) | (379 | ) | |||||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
| Income (loss) before income taxes |
$ | 16,039 | $ | (57,129 | ) | $ | 28,160 | |||||||||||||
|
|
|
|
|
|
|
|||||||||||||||
Operating expenses that are directly attributable to a segment are reported within the applicable segment. Indirect marketing and advertising, customer care and enrollment and technology operating expenses are allocated to each segment based on various measures, including headcount and policy submissions. Other indirect general and administrative operating expenses are managed in a corporate shared services environment and, since these expenses are not the responsibility of segment operating management, are not allocated to the operating segments and are presented as a reconciling item to the Company’s consolidated financial results within a line item designated as “Corporate”.
| 1 | Includes the Class C share-based compensation and incentive share plan expense recorded in connection with the Acquisition |
F-37
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
Segment profit is calculated as total revenue for the applicable segment less direct and allocated cost of revenue, marketing and advertising, customer care and enrollment, technology and general and administrative operating expenses, excluding change in fair value of contingent consideration liability, amortization of intangibles assets, share-based compensation, transaction costs, interest expense, and other income (loss).
There are no internal revenue transactions between the Company’s operating segments. The Company’s CODM does not separately evaluate assets by segment, and therefore assets by segment are not presented. The Company’s assets are primarily located in the United States.
Significant Customers
Substantially all revenue for the years ended December 31, 2019 and 2018 was generated from customers located in the United States. Carriers representing 10% or more of the Company’s total revenue for the following periods are presented in the table below:
| Successor | Predecessor | |||||||||||||||
| Period from September 13, 2019 through December 31, 2019 |
Period from January 1, 2019 through September 12, 2019 |
Year Ended December 31, 2018 |
||||||||||||||
| Humana |
46 | % | 31 | % | 25 | % | ||||||||||
| Anthem |
22 | % | 18 | % | 8 | % | ||||||||||
13. ADOPTION IMPACT OF NEW REVENUE STANDARD
As discussed in Note 1 - Summary of Business and Significant Accounting Policies, the FASB issued ASU 2014-09 in 2014, which, as amended, created ASC 606. The core principle of ASC 606 is that an entity shall recognize revenue to depict the transfer of promised goods or services to customers in an amount that reflects the consideration to which the entity expects to be entitled in exchange for those goods or services. The standard also contains significant new disclosure requirements regarding the nature, amount, timing and uncertainty of revenue and cash flows arising from contracts with customers. The Company adopted ASC 606 effective January 1, 2019, on a full retrospective basis, and recorded a cumulative effect adjustment of $28,607 to increase retained earnings (deficit) as of January 1, 2018. The Company has applied the standard to all contracts.
F-38
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
The following tables present the impact of the adoption of ASC 606 on the Company’s previously reported historical results for the periods presented:
2018 Balance Sheet Impact
| Predecessor December 31, 2018 | ||||||||||||
| As Reported | ASC 606 Adoption Adjustment |
As Adjusted |
||||||||||
| Assets |
||||||||||||
| Current assets: |
||||||||||||
| Cash |
$ | 505 | $ | — | $ | 505 | ||||||
| Accounts receivable, net |
19,331 | (9,477 | ) | 9,855 | ||||||||
| Commissions receivable – current |
— | 38,685 | 38,685 | |||||||||
| Prepaid expenses and other current assets |
8,653 | (3,669 | ) | 4,983 | ||||||||
|
|
|
|
|
|
|
|||||||
| Total current assets |
28,489 | 25,539 | 54,028 | |||||||||
| Commissions receivable – non-current |
— | 76,842 | 76,842 | |||||||||
| Property, equipment, and capitalized software, net |
11,782 | — | 11,782 | |||||||||
| Other long-term assets |
185 | — | 185 | |||||||||
|
|
|
|
|
|
|
|||||||
| Total assets |
$ | 40,456 | $ | 102,381 | $ | 142,837 | ||||||
|
|
|
|
|
|
|
|||||||
| Liabilities and members’ equity |
||||||||||||
| Current liabilities: |
||||||||||||
| Accounts payable |
$ | 10,534 | $ | — | $ | 10,534 | ||||||
| Accrued liabilities |
13,223 | (3,503 | ) | 9,720 | ||||||||
| Commission payable – current |
— | 18,336 | 18,336 | |||||||||
| Deferred revenue |
6,619 | (5,262 | ) | 1,357 | ||||||||
| Current portion of debt |
4,856 | — | 4,856 | |||||||||
| Other current liabilities |
3,181 | — | 3,181 | |||||||||
|
|
|
|
|
|
|
|||||||
| Total current liabilities |
38,413 | 9,571 | 47,984 | |||||||||
| Non-current liabilities: |
||||||||||||
| Commission payable – non-current |
— | 35,100 | 35,100 | |||||||||
| Capital lease obligations, less current portion |
152 | — | 152 | |||||||||
| Incentive share liability |
28 | — | 28 | |||||||||
| Deferred tax liability |
226 | — | 226 | |||||||||
|
|
|
|
|
|
|
|||||||
| Total non-current liabilities |
406 | 35,100 | 35,506 | |||||||||
|
|
|
|
|
|
|
|||||||
| Redeemable Class B units – $10.00 par value; 4,930,000 issued and outstanding as of December 31, 2018 |
246,000 | — | 246,000 | |||||||||
| Members’ Equity: |
||||||||||||
| Class A units – $10.00 par value; 8,365,000 issued and outstanding as of December 31, 2018 |
235 | — | 235 | |||||||||
| Class B units – $10.00 par value; 220,000 issued and outstanding as of December 31, 2018 |
2,200 | — | 2,200 | |||||||||
| Accumulated other comprehensive income |
14 | — | 14 | |||||||||
| Retained earnings (deficit) |
(246,812 | ) | 57,710 | (189,102 | ) | |||||||
|
|
|
|
|
|
|
|||||||
| Total members’ equity (deficit) |
(244,363 | ) | 57,710 | (186,653 | ) | |||||||
|
|
|
|
|
|
|
|||||||
| Total liabilities, Redeemable Class B units and members’ equity |
$ | 40,456 | $ | 102,381 | $ | 142,837 | ||||||
|
|
|
|
|
|
|
|||||||
F-39
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
2018 Income Statement Impact
| Predecessor December 31, 2018 | ||||||||||||
| As Reported |
ASC 606 Adoption Adjustment |
As Adjusted |
||||||||||
| Net revenues |
$ | 167,260 | $ | 58,945 | $ | 226,205 | ||||||
| Operating expenses: |
||||||||||||
| Cost of revenue |
51,308 | 28,274 | 79,582 | |||||||||
| Marketing and advertising |
28,129 | — | 28,129 | |||||||||
| Customer care and enrollment |
44,509 | 1,567 | 46,076 | |||||||||
| Technology |
16,197 | — | 16,197 | |||||||||
| General and administrative |
27,458 | — | 27,458 | |||||||||
|
|
|
|
|
|
|
|||||||
| Total operating expenses |
167,601 | 29,841 | 197,442 | |||||||||
|
|
|
|
|
|
|
|||||||
| Income (loss) from operations |
(341 | ) | 29,103 | 28,763 | ||||||||
| Interest expense |
224 | — | 224 | |||||||||
| Other income (expense) |
(379 | ) | — | (379 | ) | |||||||
|
|
|
|
|
|
|
|||||||
| Income (loss) before income taxes |
(944 | ) | 29,103 | 28,160 | ||||||||
| Income tax expense (benefit) |
46 | — | 46 | |||||||||
|
|
|
|
|
|
|
|||||||
| Net income (loss) |
(989 | ) | 29,103 | 28,114 | ||||||||
| Less: Net loss attributable to non-controlling interests |
(3 | ) | — | (3 | ) | |||||||
|
|
|
|
|
|
|
|||||||
| Net income (loss) attributable to GoHealth Holdings, LLC |
$ | (986 | ) | $ | 29,103 | $ | 28,117 | |||||
|
|
|
|
|
|
|
|||||||
2018 Cash Flow Impact – Operating Activities
| Predecessor December 31, 2018 | ||||||||||||
| As Reported |
ASC 606 Adoption Adjustment |
As Adjusted |
||||||||||
| Operating activities |
||||||||||||
| Net income (loss) |
$ | (989 | ) | $ | 29,103 | $ | 28,114 | |||||
| Adjustments to reconcile net income (loss) to net cash (used in) provided by operating activities: |
||||||||||||
| Depreciation and amortization |
6,160 | — | 6,160 | |||||||||
| Other non-cash items |
791 | — | 791 | |||||||||
| Changes in assets and liabilities: |
||||||||||||
| Accounts receivable |
(8,023 | ) | 8,759 | 736 | ||||||||
| Commissions receivable |
— | (65,445 | ) | (65,445 | ) | |||||||
| Prepaid expenses and other assets |
(2,172 | ) | 460 | (1,712 | ) | |||||||
| Accounts payable |
3,108 | — | 3,108 | |||||||||
| Accrued expenses |
5,291 | (2,400 | ) | 2,891 | ||||||||
| Deferred revenue |
1,499 | (1,373 | ) | 126 | ||||||||
| Commissions payable |
— | 30,896 | 30,896 | |||||||||
| Other liabilities |
(222 | ) | — | (222 | ) | |||||||
|
|
|
|
|
|
|
|||||||
| Net cash provided by operating activities |
$ | 5,443 | $ | — | $ | 5,443 | ||||||
F-40
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Consolidated Financial Statements (continued)
14. SUBSEQUENT EVENTS
Management has reviewed its December 31, 2019, consolidated financial statements for subsequent events through May 8, 2020, the date the financial statements were available to be issued. Other than the subsequent events described in Note 6 – Long Term Debt, Note 8 – Share-Based Compensation Plans, and Note 11 – Related-Party Transactions, the Company is not aware of any subsequent events that would require recognition or disclosure in the consolidated financial statements.
F-41
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Condensed Consolidated Statements of Income (Loss)
(dollars in thousands, unaudited)
| Successor | Predecessor | |||||||||||||||
| Three Months Ended March 31, 2020 |
Three Months Ended March 31, 2019 |
|||||||||||||||
| Net revenues: |
||||||||||||||||
| Commission |
$ | 112,510 | $ | 51,215 | ||||||||||||
| Other |
28,500 | 17,874 | ||||||||||||||
|
|
|
|
|
|||||||||||||
| Net revenues |
141,010 | 69,089 | ||||||||||||||
| Operating expenses: |
||||||||||||||||
| Cost of revenue |
42,134 | 27,552 | ||||||||||||||
| Marketing and advertising |
26,073 | 11,411 | ||||||||||||||
| Customer care and enrollment |
23,978 | 13,939 | ||||||||||||||
| Technology |
4,593 | 4,155 | ||||||||||||||
| General and administrative |
10,491 | 6,990 | ||||||||||||||
| Change in fair value of contingent consideration liability |
4,400 | — | ||||||||||||||
| Amortization of intangible assets |
23,514 | — | ||||||||||||||
|
|
|
|
|
|||||||||||||
| Total operating expenses |
135,183 | 64,047 | ||||||||||||||
|
|
|
|
|
|||||||||||||
| Income from operations |
5,827 | 5,042 | ||||||||||||||
| Interest expense |
6,756 | 28 | ||||||||||||||
| Other expense |
10 | 10 | ||||||||||||||
|
|
|
|
|
|||||||||||||
| Income (loss) before income taxes |
(939 | ) | 5,004 | |||||||||||||
| Income tax expense (benefit) |
(2 | ) | 2 | |||||||||||||
|
|
|
|
|
|||||||||||||
| Net income (loss) |
$ | (937 | ) | $ | 5,002 | |||||||||||
|
|
|
|
|
|||||||||||||
The accompanying notes are an integral part of these condensed consolidated financial statements.
F-42
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Condensed Consolidated Statements of Comprehensive Income (Loss)
(dollars in thousands, unaudited)
| Successor | Predecessor | |||||||||||||||
| Three Months Ended March 31, 2020 |
Three Months Ended March 31, 2019 |
|||||||||||||||
| Net income (loss) |
$ | (937 | ) | $ | 5,002 | |||||||||||
| Other comprehensive loss: |
||||||||||||||||
| Foreign currency translation adjustments |
(85 | ) | (46 | ) | ||||||||||||
|
|
|
|
|
|||||||||||||
| Other comprehensive loss |
(85 | ) | (46 | ) | ||||||||||||
|
|
|
|
|
|||||||||||||
| Total comprehensive income (loss) |
$ | (1,022 | ) | $ | 4,956 | |||||||||||
|
|
|
|
|
|||||||||||||
The accompanying notes are an integral part of these condensed consolidated financial statements.
F-43
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Condensed Consolidated Balance Sheets
(dollars in thousands, except share and per share data)
| Successor | Successor | |||||||||||
| March 31, 2020 |
December 31, 2019 |
|||||||||||
| (Unaudited) | ||||||||||||
| Assets |
||||||||||||
| Current assets: |
||||||||||||
| Cash and cash equivalents |
$ | 152,423 | $ | 12,276 | ||||||||
| Accounts receivable, net of allowance for doubtful accounts of $651 in 2020 and $904 in 2019 |
6,422 | 24,461 | ||||||||||
| Commissions receivable – current |
58,173 | 101,078 | ||||||||||
| Prepaid expenses and other current assets |
6,010 | 5,954 | ||||||||||
|
|
|
|
|
|||||||||
| Total current assets |
223,028 | 143,769 | ||||||||||
| Commissions receivable – non-current |
330,617 | 281,853 | ||||||||||
| Property, equipment, and capitalized software, net |
9,228 | 6,339 | ||||||||||
| Intangible assets, net |
759,269 | 782,783 | ||||||||||
| Goodwill |
386,553 | 386,553 | ||||||||||
| Other long-term assets |
954 | 998 | ||||||||||
|
|
|
|
|
|||||||||
| Total assets |
$ | 1,709,649 | $ | 1,602,295 | ||||||||
|
|
|
|
|
|||||||||
| Liabilities and members’ equity |
||||||||||||
| Current liabilities: |
||||||||||||
| Accounts payable |
$ | 12,718 | $ | 13,582 | ||||||||
| Accrued liabilities |
11,740 | 22,568 | ||||||||||
| Commissions payable – current |
34,536 | 56,003 | ||||||||||
| Deferred revenue |
14,867 | 15,218 | ||||||||||
| Current portion of debt |
4,170 | 3,000 | ||||||||||
| Other current liabilities |
3,178 | 2,694 | ||||||||||
|
|
|
|
|
|||||||||
| Total current liabilities |
81,209 | 113,065 | ||||||||||
| Non-current liabilities: |
||||||||||||
| Commissions payable – non-current |
113,516 | 97,489 | ||||||||||
| Long-term debt, net of current portion |
397,652 | 288,233 | ||||||||||
| Contingent consideration |
247,100 | 242,700 | ||||||||||
| Capital lease obligations, less current portion |
345 | 421 | ||||||||||
| Incentive share liability |
— | — | ||||||||||
| Deferred tax liability |
225 | 243 | ||||||||||
|
|
|
|
|
|||||||||
| Total non-current liabilities |
758,838 | 629,086 | ||||||||||
|
|
|
|
|
|||||||||
| Commitments and contingencies (Note 10) |
||||||||||||
| Members’ Equity: |
||||||||||||
| Preferred units – $1.00 par value; 541,263,042 units authorized, issued and outstanding at March 31, 2020 and December 31, 2019 |
546,972 | 547,542 | ||||||||||
| Class A Common units – $1.00 par value; 237,938,682 units authorized, issued and outstanding at March 31, 2020 and December 31, 2019 |
219,139 | 218,911 | ||||||||||
| Class B Common units – $1.00 par value; 108,727,667 and 102,061,318 units authorized, issued and outstanding at March 31, 2020 and December 31, 2019, respectively |
103,593 | 93,708 | ||||||||||
| Senior Preferred Earnout Units – no par value; none authorized, issued, and outstanding at March 31, 2020 or December 31, 2019 |
— | — | ||||||||||
| Profits Units – no par value; 97,918,116 units authorized at March 31, 2020 and December 31, 2019; 84,399,921 and 78,398,133 units issued at March 31, 2020 and December 31, 2019, respectively; and none outstanding at March 31, 2020 and December 31, 2019 |
— | — | ||||||||||
| Accumulated other comprehensive (loss) income |
(102 | ) | (17 | ) | ||||||||
|
|
|
|
|
|||||||||
| Total members’ equity |
869,602 | 860,144 | ||||||||||
|
|
|
|
|
|||||||||
| Total liabilities, Redeemable Class B units and members’ equity |
$ | 1,709,649 | $ | 1,602,295 | ||||||||
|
|
|
|
|
|||||||||
The accompanying notes are an integral part of these condensed consolidated financial statements.
F-44
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Condensed Consolidated Statements of Changes in Members’ Equity
(dollars and units in thousands, unaudited)
| Three Months Ended March 31, 2020 |
||||||||||||||||||||||||||||||||||||||||||||||||||||
| Preferred Units | Class A Common Units |
Class B Common Units |
Class A Units | Class B Units | Retained Earnings (Deficit) |
Accumulated Other Comprehensive (Loss) Income |
Members’ Equity (Deficit) |
|||||||||||||||||||||||||||||||||||||||||||||
| Units | Amount | Units | Amount | Units | Amount | Units | Amount | Units | Amount | |||||||||||||||||||||||||||||||||||||||||||
| Successor: |
||||||||||||||||||||||||||||||||||||||||||||||||||||
| Balance at January 1, 2020 |
541,263 | $ | 547,542 | 237,939 | $ | 218,911 | 102,061 | $ | 93,708 | $ | — | (17 | ) | $ | 860,144 | |||||||||||||||||||||||||||||||||||||
| Foreign currency translation adjustment |
(85 | ) | (85 | ) | ||||||||||||||||||||||||||||||||||||||||||||||||
| Issuance of common units |
6,667 | 10,000 | 10,000 | |||||||||||||||||||||||||||||||||||||||||||||||||
| Share-based compensation expense |
479 | 479 | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Net loss |
(570 | ) | (251 | ) | (115 | ) | (937 | ) | ||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||
| Balance at March 31, 2020 |
541,263 | $ | 546,972 | 237,939 | $ | 219,139 | 108,728 | $ | 103,593 | $ | — | $ | (102 | ) | $ | 869,602 | ||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||
| Three Months Ended March 31, 2019 |
||||||||||||||||||||||||||||||||||||||||||||||||||||
| Predecessor: |
||||||||||||||||||||||||||||||||||||||||||||||||||||
| Balance at January 1, 2019 |
8,365 | $ | 235 | 220 | $ | 2,200 | $ | (189,102 | ) | $ | 14 | $ | (186,653 | ) | ||||||||||||||||||||||||||||||||||||||
| Redeemable Class B unit accretion |
(115,000 | ) | (115,000 | ) | ||||||||||||||||||||||||||||||||||||||||||||||||
| Foreign currency translation adjustment |
(46 | ) | (46 | ) | ||||||||||||||||||||||||||||||||||||||||||||||||
| Net income |
5,002 | 5,002 | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||
| Balance at March 31, 2019 |
8,365 | $ | 235 | 220 | $ | 2,200 | $ | (299,100 | ) | $ | (32 | ) | $ | (296,697 | ) | |||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||
The accompanying notes are an integral part of these condensed consolidated financial statements.
F-45
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Condensed Consolidated Statements of Cash Flows
(dollars in thousands, unaudited)
| Successor | Predecessor | |||||||||||
| Three Months Ended March 31, 2020 |
Three Months Ended March 31, 2019 |
|||||||||||
| Operating activities |
||||||||||||
| Net income (loss) |
$ | (937 | ) | $ | 5,002 | |||||||
| Adjustments to reconcile net income (loss) to net cash provided by operating activities: |
||||||||||||
| Share-based compensation |
479 | — | ||||||||||
| Depreciation and amortization |
633 | 1,538 | ||||||||||
| Amortization of intangible assets |
23,514 | — | ||||||||||
| Accretion of discount on long-term debt |
315 | — | ||||||||||
| Amortization of debt issuance costs |
79 | — | ||||||||||
| Change in fair value of contingent consideration |
4,400 | — | ||||||||||
| Other non-cash items |
(341 | ) | 614 | |||||||||
| Changes in assets and liabilities: |
||||||||||||
| Accounts receivable |
18,365 | (640 | ) | |||||||||
| Commissions receivable |
(5,859 | ) | (4,685 | ) | ||||||||
| Prepaid expenses and other assets |
(56 | ) | 63 | |||||||||
| Accounts payable |
(864 | ) | (567 | ) | ||||||||
| Accrued liabilities |
(10,828 | ) | (2,137 | ) | ||||||||
| Deferred revenue |
(351 | ) | 24 | |||||||||
| Commissions payable |
(5,441 | ) | 1,099 | |||||||||
| Other liabilities |
479 | 911 | ||||||||||
|
|
|
|
|
|||||||||
| Net cash provided by operating activities |
23,587 | 1,222 | ||||||||||
| Investing activities |
||||||||||||
| Purchases of property, equipment and software |
(3,522 | ) | (1,944 | ) | ||||||||
|
|
|
|
|
|||||||||
| Net cash used in investing activities |
(3,522 | ) | (1,944 | ) | ||||||||
| Financing activities |
||||||||||||
| Borrowings under term loans |
117,000 | — | ||||||||||
| Principal payments under term loans |
(750 | ) | — | |||||||||
| Principal payments under capital lease obligations |
(72 | ) | (16 | ) | ||||||||
| Borrowings under revolving credit facilities, net of payments |
— | 1,163 | ||||||||||
| Debt issuance cost payments |
(6,011 | ) | — | |||||||||
| Proceeds received upon issuance of common units |
10,000 | — | ||||||||||
|
|
|
|
|
|||||||||
| Net cash provided by financing activities |
120,167 | 1,147 | ||||||||||
| Effect of exchange rate changes on cash |
(85 | ) | (46 | ) | ||||||||
| Increase in cash and cash equivalents |
140,147 | 379 | ||||||||||
| Cash and cash equivalents at beginning of period |
12,276 | 505 | ||||||||||
|
|
|
|
|
|||||||||
| Cash and cash equivalents at end of period |
$ | 152,423 | $ | 884 | ||||||||
|
|
|
|
|
|||||||||
| Interest paid |
$ | 6,362 | $ | 28 | ||||||||
|
|
|
|
|
|||||||||
| Taxes paid |
$ | 15 | $ | 25 | ||||||||
|
|
|
|
|
|||||||||
The accompanying notes are an integral part of these condensed consolidated financial statements.
F-46
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Condensed Consolidated Financial Statements
Three Month Period Ended March 31, 2020 (Successor)
and Three Month Period Ended March 31, 2019 (Predecessor)
(dollars in thousands, unaudited)
1. SUMMARY OF BUSINESS AND SIGNIFICANT ACCOUNTING POLICIES
Description of Business
GoHealth Holdings, LLC (formerly known as Blizzard Parent, LLC), a Delaware limited liability company, and its wholly owned subsidiaries (collectively, the “Company”) is a leading health insurance marketplace whose mission is to improve healthcare in America. The Company works with insurance carriers to provide solutions to efficiently enroll individuals in health insurance plans. The Company’s proprietary technology platform leverages modern machine-learning algorithms powered by nearly two decades of insurance purchasing behavior to reimagine the optimal process for helping individuals find the best health insurance plan for their specific needs. The Company’s insurance agents leverage the power of its vertically integrated customer acquisition platform to enroll members in Medicare and individual and family plans. Certain of the Company’s operations do business as GoHealth, LLC (“GoHealth”), a wholly owned subsidiary of the Company that was founded in 2001.
Basis of Presentation and Principles of Consolidation
GoHealth Holdings, LLC is a holding company with no operating assets or operations and was formed to acquire a 100% equity interest in Norvax, LLC (“Norvax”). On May 6, 2020, Blizzard Parent, LLC changed its name to GoHealth Holdings, LLC. GoHealth Holdings, LLC owns 100% of Blizzard Midco, LLC, which owns 100% of Norvax. For all of the periods reported in these condensed consolidated financial statements, GoHealth Holdings, LLC has not and does not have any material operations on a standalone basis, and all of the operations of the Company are carried out by Norvax. On August 15, 2019, GoHealth Holdings, LLC entered a series of arrangements to acquire 100% of the equity interest in Norvax. On September 13, 2019, Blizzard Merger Sub LLC, a transitory merger company of Blizzard Midco, LLC, merged into Norvax, with Norvax continuing as the surviving limited liability company and the Company’s operating entity (the “Acquisition”).
As a result of the Acquisition, which is discussed further in Note 2 – Acquisition, Norvax was determined to be the accounting acquirer and Norvax’s historical assets and liabilities are reflected at fair value as of the acquisition date. The financial information for the period after September 13, 2019, represents the condensed consolidated financial information of the “Successor” company. Prior to September 13, 2019, the condensed consolidated financial statements include the accounts of the “Predecessor” company. Due to the change in the basis of accounting resulting from the application of the acquisition method of accounting, the Predecessor’s condensed consolidated financial statements and the Successor’s condensed consolidated financial statements are not necessarily comparable.
The accompanying condensed consolidated financial statements have been prepared in accordance with U.S. generally accepted accounting principles (“U.S. GAAP”) for interim financial information, but do not include all information and footnote disclosures required under U.S. GAAP for annual financial statements. In the opinion of management, the interim condensed consolidated financial statements include all adjustments, consisting only of normal recurring adjustments, necessary for the fair presentation of the Company’s financial position, results of operations and cash flows as of the dates and for the periods presented. All intercompany transactions and balances are eliminated in consolidation.
These interim financial statements should be read in conjunction with the Company’s audited consolidated financial statements and notes thereto as of and for the year ended December 31, 2019, which are included elsewhere in this Registration Statement on Form S-1. Interim results are not necessarily indicative of results for the full fiscal year due to seasonality and other factors.
F-47
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Condensed Consolidated Financial Statements (continued)
Use of Estimates
The preparation of the condensed consolidated financial statements in conformity with U.S. GAAP requires management to make estimates, judgments, and assumptions that affect the reported amounts of assets and liabilities at the date of the condensed consolidated financial statements, and the reported amounts of revenues and expenses during the reporting periods. The Company bases its estimates on historical experience and on various other assumptions that management believes are reasonable under the circumstances, the results of which form the basis for making judgments about carrying values of assets and liabilities that are not readily apparent from other sources. Actual results could differ from those estimates. There have been no material changes to the Company’s significant accounting policies as discussed in the notes to the Company’s audited consolidated financial statements as of and for the year ended December 31, 2019.
Cash and Cash Equivalents
We consider all investments with an original maturity of 90 days or less from the date of purchase to be cash equivalents. Cash includes all deposits in banks. The Company maintains its cash balances at financial institutions in the United States and Europe.
Cash accounts in the United States are insured by the Federal Deposit Insurance Corporation (“FDIC”) up to $250,000. As of March 31, 2020 and December 31, 2019, the Company’s cash balances in the United States exceeded the FDIC-insured limits by $151,904 and $11,936, respectively. The Company also has an immaterial amount of cash held in Europe to fund its Slovakian operations. The Company does not believe it is exposed to any significant risk with respect to cash balances.
Concentration of Credit Risk
The Company does not require collateral or other security in granting credit. As of March 31, 2020, three customers each represented 10% or more of the Company’s total accounts receivable and, in aggregate, represented 66%, or $4,268, of the Company’s total accounts receivable. As of December 31, 2019, five customers each represented 10% or more of the Company’s total accounts receivable and, in aggregate, represented 87%, or $21,220, of the Company’s total accounts receivable. No other customers represented 10% or more of the Company’s total accounts receivable at March 31, 2020 and December 31, 2019.
Revenue Recognition
In May 2014, the Financial Accounting Standards Board (“FASB”) issued ASC 606, requiring an entity to recognize revenue when it transfers promised goods or services to customers in an amount that reflects the consideration to which the entity expects to be entitled to in exchange for those goods or services.
The Company is compensated by the receipt of commission payments from health insurance carriers whose health insurance policies are purchased through the Company’s ecommerce platforms or customer care centers. The Company also generates revenue from non-commission revenue sources, which include providing dedicated insurance agent resources for carrier-specific programs, sales of insurance leads to other marketing agencies and carriers, and the implementation and use of the Company’s platform. The Company accounts for payments made under certain carrier-specific arrangements as deductions to revenue.
The core principle of ASC 606 is to recognize revenue upon the transfer of promised goods or services to customers in an amount that reflects the consideration the entity expects to be entitled to in exchange for those
F-48
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Condensed Consolidated Financial Statements (continued)
goods or services. Accordingly, the Company recognizes revenue for its services in accordance with the following five steps outlined in ASC 606:
| • | Identification of the contract, or contracts, with a customer. A contract with a customer exists when (i) the Company enters into an enforceable contract with a customer that defines each party’s rights regarding the goods or services to be transferred and identifies the payment terms related to these goods or services, (ii) the contract has commercial substance and, (iii) the Company determines that collection of substantially all consideration for goods or services that are transferred is probable based on the customer’s intent and ability to pay the promised consideration. Payment of commissions typically commences within 60 days from the effective date. Payment terms from non-commission revenue are typically 30 days from the invoice date. |
| • | Identification of the performance obligations in the contract. Performance obligations promised in a contract are identified based on the goods or services that will be transferred to the customer that are both capable of being distinct, whereby the customer can benefit from the goods or services either on their own or together with other resources that are readily available from third parties or from the Company, and are distinct in the context of the contract, whereby the transfer of the goods or services is separately identifiable from other promises in the contract. |
| • | Determination of the transaction price. The transaction price is determined based on the consideration to which the Company will be entitled in exchange for transferring goods or services to the customer. |
| • | Allocation of the transaction price to the performance obligations in the contract. If the contract contains a single performance obligation, the entire transaction price is allocated to the single performance obligation. Contracts that contain multiple performance obligations require an allocation of the transaction price to each performance obligation based on a relative standalone selling price (“SSP”) basis. |
| • | Recognition of revenue when, or as, the Company satisfies a performance obligation. The Company satisfies performance obligations either over time or at a point in time, as discussed in further detail below. Revenue is recognized at the time the related performance obligation is satisfied by transferring the promised good or service to the customer. |
Commission Revenue
The Company recognizes commission revenue from the sale of insurance products at the point when carriers approve an insurance application produced by the Company. The Company records as commission revenue the expected amount of commissions received from the insurance carriers and any renewal commissions to be paid on such placement as long as the policyholder remains with the same insurance product. The Company defines its customer to be the health insurance carrier.
The Company typically enters contractual agency relationships with health insurance carriers that are non-exclusive and terminable on short notice by either party for any reason. In addition, health insurance carriers often can terminate or amend agreements unilaterally on short notice, including provisions in agreements relating to the commission rates paid to the Company by the health insurance carriers. The amendment or termination of an agreement the Company has with a health insurance carrier may adversely impact the commissions it is paid on health insurance plans purchased from the carrier.
Compensation in the form of commissions is received from insurance carriers for the multiple types of insurance products sold by the Company on behalf of the carriers. For Medicare and non-Medicare eligible products, commission revenue generally represents a percentage of the premium amount expected to be collected by the
F-49
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Condensed Consolidated Financial Statements (continued)
carrier while the policyholder is enrolled in the insurance product, including renewal periods. The Company’s performance obligation is complete when a carrier has received and approved an insurance application. As such, the Company recognizes revenue at this point in time, which represents the total estimated lifetime commissions it expects to receive for selling the product after the carrier approves an application, net of an estimated constraint. The Company’s consideration is variable based on the amount of time it estimates a policy will remain in force. The Company estimates the amount of variable consideration that it expects to receive based on historical experience or carrier experience to the extent available, industry data, and expectations as to future retention rates. Additionally, the Company considers application of the constraint and only recognizes the amount of variable consideration that it believes is probable that it will be entitled to receive and will not be subject to a significant revenue reversal in the future. The Company monitors and updates this estimate at each reporting date. The Company does not have any remaining performance obligations in its contracts with customers.
The Company utilizes a practical expedient to estimate commission revenue for each insurance product by applying the use of a portfolio approach to group approved members by the effective month of the relevant policy (referred to as a “cohort”). This allows the Company to estimate the commissions it expects to collect for each cohort by evaluating various factors, including but not limited to, contracted commission rates, carrier mix, and expected member churn.
The Company’s variable consideration includes estimated and constrained lifetime values as the “constrained LTV” for the plans. The Company’s estimate of commission revenue for each product line is based on a number of assumptions, which include, but are not limited to, estimating conversion of an approved applicant to a paying policyholder, forecasting persistency and forecasting the commission amounts likely to be received per policyholder. These assumptions are based on historical trends and incorporate management’s judgment in interpreting those trends and in applying constraints. To the extent the Company makes changes to the assumptions, it will recognize any impact of the changes to commission revenue in the reporting period in which the change is made, including revisions of estimated lifetime commissions either below or in excess of previously estimated constrained LTV recognized as revenue.
Other Revenue
Within the Company’s Medicare and IFP and Other segments, the Company provides trained licensed agents dedicated to carrier programs that assist in producing health insurance policies, typically prior to and during the annual enrollment period. The Company is compensated for the hours incurred on the carrier program at the time hours are incurred as well as performance-based enrollment fees relating to the Company enrolling individuals into health insurance plans. The Company recognizes revenue as control transfers over the term of the contract.
The Company recognizes revenue at a point in time resulting from the sale of leads to third parties and independent agents. The Company generates this revenue through the sale of leads sourced through its marketing efforts.
The Company provides certain customers access to its technology platform, where it charges for the implementation and monthly access to the software. This application allows carriers the use of the Company’s e-commerce platform to offer their own health insurance policies on their websites and agents to utilize the Company’s technology to power their online quoting, content and application submission processes. Typically, the Company is paid a one-time implementation fee, which it recognizes as control is transferred on a straight-line basis over the estimated term of the customer relationship (generally the initial term of the agreement), commencing once the technology is available for use by the third party.
F-50
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Condensed Consolidated Financial Statements (continued)
Additionally, the Company earns development funds, based on delivering call volumes to certain insurance carriers. The Company recognizes revenue as control transfers over the term of the contract.
Disaggregation of Revenue
The table below depicts the disaggregation of revenue by product, and is consistent with how the Company evaluates its financial performance:
| Successor | Predecessor | |||||||||||
| Three Months Ended March 31, 2020 |
Three Months Ended March 31, 2019 |
|||||||||||
| Commission revenue: |
||||||||||||
| Medicare |
||||||||||||
| Medicare Advantage |
$ | 99,291 | $ | 31,029 | ||||||||
| Medicare Supplement |
2,189 | 3,394 | ||||||||||
| Medicare Part D |
571 | 515 | ||||||||||
|
|
|
|
|
|||||||||
| Total Medicare |
102,051 | 34,938 | ||||||||||
| Individual and Family Plan: |
||||||||||||
| Fixed Indemnity |
6,779 | 12,638 | ||||||||||
| Short Term |
1,778 | 1,054 | ||||||||||
| Major Medical |
186 | 160 | ||||||||||
|
|
|
|
|
|||||||||
| Total Individual and Family Plan |
8,743 | 13,852 | ||||||||||
| Ancillary |
1,266 | 2,020 | ||||||||||
| Small Group |
450 | 405 | ||||||||||
|
|
|
|
|
|||||||||
| Total Commission Revenue |
112,510 | 51,215 | ||||||||||
| Other Revenue |
28,500 | 17,874 | ||||||||||
|
|
|
|
|
|||||||||
| Net Revenues |
$ | 141,010 |
|
|
|
$ | 69,089 | |||||
|
|
|
|
|
|||||||||
Seasonality
A greater number of the Company’s Medicare-related health insurance plans are sold in its fourth quarter during the Medicare annual enrollment period when Medicare-eligible individuals are permitted to change their Medicare Advantage and Medicare Part D prescription drug coverage for the following year. As a result, the Company’s Medicare plan-related commission revenue is highest in the Company’s fourth quarter.
The majority of the Company’s individual and family health insurance plans are sold in the fourth quarter during the annual open enrollment period as defined under the federal Patient Protection and Affordable Care Act and related amendments in the Health Care and Education Reconciliation Act. Individuals and families generally are not able to purchase individual and family health insurance outside of these open enrollment periods, unless they qualify for a special enrollment period as a result of certain qualifying events, such as losing employer-sponsored health insurance or moving to another state.
Recent Accounting Pronouncements
In August 2018, the FASB issued ASU 2018-13, Fair Value Measurement Disclosure Framework – Changes to the Disclosure Requirements for Fair Value Measurement (Topic 820), which amended the disclosure requirements under ASC 820. This update clarifies and unifies the disclosure of Level 3 fair value instruments.
F-51
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Condensed Consolidated Financial Statements (continued)
This guidance is effective for fiscal years beginning after December 15, 2019 and for interim periods within those fiscal years, although early adoption is permitted for either the entire standard or only the provisions that eliminate or modify the requirements. The Company adopted this standard on January 1, 2020, and the adoption did not have a material effect on our condensed consolidated financial statements.
In June 2018, the FASB issued ASU 2018-07, Stock Compensation – Improvements to Nonemployee Share-Based Payment Accounting (Topic 718). This guidance expands the scope of Topic 718 to include share-based payment transactions for acquiring goods and services from nonemployees. Per ASU 2019-08, issued November 2019, the guidance is effective for fiscal years beginning after December 15, 2019, and interim periods within fiscal years beginning after December 15, 2019. Early adoption is permitted, but no earlier than an entity’s adoption date of Topic 606. The Company adopted this standard on January 1, 2020, and the adoption did not have a material effect on our condensed consolidated financial statements.
In February 2016, the FASB issued ASU 2016-02, Leases (Topic 842). The guidance specifies that lessees will need to recognize a right-of-use asset and a lease liability for virtually all their leases except those which meet the definition of a short-term lease. For income statement purposes, the FASB retained a dual model, requiring leases to be classified as either operating or financing. Classification will be based on criteria that are similar to those applied in current lease accounting, but without explicit bright lines. Per ASU 2020-05, Revenue from Contracts with Customers (Topic 606) and Leases (Topic 842): Effective Dates for Certain Entities, issued June 2020, the guidance in ASU 2016-02, as amended, is effective for fiscal years beginning after December 15, 2021, and interim periods within fiscal years beginning after December 15, 2022. Early adoption is permitted. The Company is currently evaluating the new guidance to determine the impact it will have on its condensed consolidated financial statements.
In November 2019, the FASB issued ASU 2019-11, Financial Instruments – Credit Losses (Topic 326), which amends the guidance for accounting for assets that are potentially subject to credit risk. The amendments affect contract assets, loans, debt securities, trade receivables, net investments in leases, off-balance-sheet credit exposures, reinsurance receivables, and any other financial assets not excluded from the scope that have the contractual right to receive cash. Per ASU 2019-10, issued November 2019, the guidance is effective for annual and interim periods beginning after December 15, 2022. Early adoption is permitted. The Company is currently evaluating the new guidance to determine the impact it will have on its condensed consolidated financial statements.
2. ACQUISITION
Acquisition of Norvax, LLC
On September 13, 2019, the Company acquired a 100% interest in Norvax, for $807,591 in cash and $306,000 in equity. In connection with the Acquisition, the Company also agreed to pay additional consideration of up to $275,000 in additional Common and Senior Preferred Earnout Units, if Adjusted EBITDA, as defined in the terms of the acquisition agreement, exceeds certain thresholds for the period September 13, 2019 to December 31, 2019 and the year ended December 31, 2020 (“Earnout” or “contingent consideration”).
The elements of the purchase consideration are as follows:
| Cash paid |
$ | 807,591 | ||
| Fair value of Class A and B Common units issued |
306,000 | |||
| Fair value of Earnout |
172,000 | |||
|
|
|
|||
| Total consideration |
$ | 1,285,591 | ||
|
|
|
F-52
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Condensed Consolidated Financial Statements (continued)
Contingent Consideration
The contingent consideration represents the fair value of the Earnout payments to Norvax’s selling shareholders and will be adjusted to fair value at each reporting date until settled. The contingent consideration will be settled in Common and Senior Preferred Earnout Units within 60 days of the issuance of the 2019 and 2020 audited financial statements. The Senior Preferred Earnout Units earn an annual coupon of 10.3% that provides for the accrual of additional units. Changes in fair value of the contingent consideration are recognized in income from operations.
The full amount available relative to the 2019 target was earned as of December 31, 2019. On May 15, 2020, the contingent consideration related to the 2019 target of $200,000 was settled with the issuance of 113,407,000 Class A Common units, 48,644,750 Class B Common units, and 100,000,000 Senior Preferred Earnout Units.
Allocation of Preliminary Purchase Price
The preliminary allocation of the purchase price is based on the fair value of assets acquired and liabilities assumed as of the acquisition date. The components of the preliminary purchase price allocation are as follows:
| Net working capital |
$ | 18,787 | ||
| Commission receivable – non-current |
113,565 | |||
| Property and equipment |
4,442 | |||
| Other noncurrent assets |
218 | |||
| Other noncurrent liabilities |
(963 | ) | ||
| Trade names |
83,000 | |||
| Developed technology |
496,000 | |||
| Customer relationships |
232,000 | |||
| Goodwill |
386,553 | |||
| Deferred revenue |
(3,283 | ) | ||
| Commissions payable – non-current |
(44,728 | ) | ||
|
|
|
|||
| Total consideration transferred |
$ | 1,285,591 | ||
|
|
|
Goodwill represents the excess of the consideration paid over the estimated fair value of assets acquired and liabilities assumed in a business combination and is primarily attributable to future growth and the assembled workforce.
3. BALANCE SHEET ACCOUNTS
Commissions Receivable
Commissions receivable activity is summarized as follows:
| Successor | ||||
| Three Months Ended March 31, 2020 |
||||
| Beginning balance |
$ | 382,931 | ||
| Commission revenue |
112,510 | |||
| Cash receipts |
(106,651 | ) | ||
|
|
|
|||
| Ending balance |
388,790 | |||
| Less: Commissions receivable – current |
58,173 | |||
|
|
|
|||
| Commissions receivable – non-current |
$ | 330,617 | ||
|
|
|
|||
F-53
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Condensed Consolidated Financial Statements (continued)
For the three months ended March 31, 2020, the Company recognized $14,577 of revenue that was deferred as of December 31, 2019.
4. FAIR VALUE MEASUREMENTS
The Company defines fair value as the price that would be received for an asset or paid to transfer a liability (an exit price) in the principal or most advantageous market for the asset or liability in an orderly transaction between market participants on the measurement date. Valuation techniques the Company uses to measure fair value maximize the use of observable inputs and minimize the use of unobservable inputs. The Company classifies the inputs used to measure fair value into the following hierarchy:
| Level 1 | Unadjusted quoted prices in active markets for identical assets or liabilities. |
| Level 2 | Unadjusted quoted prices in active markets for similar assets or liabilities; unadjusted quoted prices for identical or similar assets or liabilities in markets that are not active; inputs other than quoted prices that are observable for the asset or liability. |
| Level 3 | Unobservable inputs for the asset or liability. |
Fair Value Measurements
The fair value of the acquired developed technology has been estimated using the multi-period excess earnings model. This method discounts the amount of excess cash flows generated by the asset. The fair value of the acquired trade names was estimated using the relief from-royalty method which required that the Company estimate hypothetical royalty payments that would be required over the economic life of the asset as if it were to be licensed instead of purchased. These payments were then discounted to their present value. Both developed technology and trade names represent a Level 3 measurement within the fair value hierarchy.
The fair value of the acquired customer relationships was estimated using the distributor method under the income approach, which included Level 3 inputs such as revenue, attrition, margin and contributory asset charges.
The fair value of the contingent consideration was measured using a Monte Carlo simulation and is discounted using a rate that appropriately captures the risk associated with the obligation. The weighted average discount rate used to value the contingent consideration as of March 31, 2020, was approximately 13% and was based on an analysis of publicly traded peers. Expected volatility was estimated to be 45%, based on an analysis of publicly traded peers that ranged from approximately 40% to 117%. The contingent consideration was part of the acquisition consideration and will be adjusted to fair value at each reporting date until settled. The following table sets forth the fair value and a summary of the changes to fair value of the contingent consideration:
| Balance at December 31, 2019 |
$ | 242,700 | ||
| 2020 earnout fair value adjustment |
4,400 | |||
|
|
|
|||
| Balance at March 31, 2020 |
$ | 247,100 | ||
|
|
|
The carrying amount of certain financial instruments, including cash and cash equivalents, accounts receivable, commissions receivable, accounts payable, accrued expenses, and commissions payable approximate fair value due to the short maturity of these instruments. Commissions receivable are recorded at constrained lifetime values. The carrying value of debt approximates fair value due to the variable nature of interest rates.
F-54
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Condensed Consolidated Financial Statements (continued)
5. GOODWILL AND INTANGIBLE ASSETS, NET
The carrying amounts, accumulated amortization, and net carrying value of the Company’s definite-lived amortizable intangible assets, as well as its definite-lived intangible trademarks, are presented in the tables below:
| March 31, 2020 (Successor) | ||||||||||||
| Gross Carrying Amount |
Accumulated Amortization |
Net carrying amount |
||||||||||
| Developed technology |
$ | 496,000 | $ | 38,971 | $ | 457,029 | ||||||
| Customer relationships |
232,000 | 12,760 | 219,240 | |||||||||
|
|
|
|
|
|
|
|||||||
| Total intangible assets subject to amortization |
$ | 728,000 | $ | 51,731 | $ | 676,269 | ||||||
|
|
|
|
|
|
|
|||||||
| Indefinite-lived trademarks |
83,000 | |||||||||||
|
|
|
|||||||||||
| Intangible Assets |
$ | 759,269 | ||||||||||
|
|
|
|||||||||||
| December 31, 2019 (Successor) | ||||||||||||
| Gross Carrying Amount |
Accumulated Amortization |
Net carrying amount |
||||||||||
| Developed technology |
$ | 496,000 | $ | 21,257 | $ | 474,743 | ||||||
| Customer relationships |
232,000 | 6,960 | 225,040 | |||||||||
|
|
|
|
|
|
|
|||||||
| Total intangible assets subject to amortization |
$ | 728,000 | $ | 28,217 | $ | 699,783 | ||||||
|
|
|
|
|
|
|
|||||||
| Indefinite-lived trademarks |
83,000 | |||||||||||
|
|
|
|||||||||||
| Intangible Assets |
$ | 782,783 | ||||||||||
|
|
|
|||||||||||
There was no impairment of goodwill or intangible assets for the three months ended March 31, 2020.
6. LONG TERM DEBT
The Company’s long-term debt consisted of the following:
| Interest rate | Successor March 31, 2020 |
Successor December 31, 2019 |
||||||||||
| Credit Facility |
8.11% - 8.41% | $ | 415,500 | $ | 299,250 | |||||||
| Less: unamortized debt discount and issuance costs |
(13,678 | ) | (8,017 | ) | ||||||||
|
|
|
|
|
|||||||||
| Total debt |
401,822 | $ | 291,233 | |||||||||
| Less: current portion |
(4,170 | ) | (3,000 | ) | ||||||||
|
|
|
|
|
|||||||||
| Total long-term debt |
$ | 397,652 | $ | 288,233 | ||||||||
|
|
|
|
|
|||||||||
Successor
General
On September 13, 2019, in connection with the Acquisition, Norvax, or the Borrower, entered into a first lien credit agreement (the “Credit Agreement”) which provides for the following:
| • | $300,000 aggregate principal amount senior secured term loan facility, or the Term Loan Facility; and |
| • | $30,000 aggregate principal amount senior secured revolving credit facility, or the Revolving Credit Facility. |
F-55
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Condensed Consolidated Financial Statements (continued)
On March 20, 2020, the Company entered into an amendment to the Credit Agreement, which provided $117,000 of incremental term loans, or the “Incremental Term Loan Facility”. On March 23, 2020, the Company issued 6,666,667 Class B Common units to a lender that is party to the Company’s Credit Agreement for $10,000 in proceeds.
On May 7, 2020, the Company entered into a second amendment to the Credit Agreement, which provided $20,000 of incremental revolving credit, or the “Incremental Revolving Credit Facility”. The Company collectively refers to the Term Loan Facility, the Revolving Credit Facility, the Incremental Term Loan Facility, and the Incremental Revolving Credit Facility as the “Credit Facilities”.
The Company incurred $9,283 and $6,011 of debt issuance costs associated with the Term Loan Facility and the Incremental Term Loan Facility, respectively, which are being amortized over the life of the debt under the effective interest rate method to interest expense.
As of March 31, 2020, the Company had a principal amount of $298,500 and $117,000 outstanding on the Term Loan Facility and Incremental Term Loan Facility, respectively. The Company had no amounts outstanding on the Revolving Credit Facility, which had remaining capacity of $30,000 as of March 31, 2020.
Interest Rates and Fees
Borrowings under the Credit Facilities are, at the option of the Borrower, either alternate base rate (“ABR”) loans or LIBOR loans. Term loans and revolving loans comprising each ABR borrowing under the Term Loan Facility accrue interest at the ABR plus an applicable rate of 5.50% per annum. Term loans and revolving loans comprising each LIBOR borrowing bear interest at the LIBOR plus an applicable rate of 6.50% per annum.
In addition to paying interest on the principal amounts outstanding under the Credit Facilities, the Borrower is required to pay a commitment fee of 0.50% per annum under the Revolving Credit Facility and the Incremental Revolving Credit Facility in respect of the unutilized commitments thereunder. The Borrower is also subject to customary letter of credit and agency fees.
Mandatory Prepayments
The Credit Agreement requires that the Borrower, following the end of each fiscal year, commencing with the fiscal year ending December 31, 2020, repay the outstanding principal amount of all term loans under the Credit Facilities in an aggregate amount equal to (A) 50.0% of the excess cash flow of the Borrower and its restricted subsidiaries for such fiscal year if the Total Net Leverage Ratio (as defined in the Credit Agreement) is greater than 4.50:1.00, which percentage is reduced to 25% if the Total Net Leverage Ratio is less than or equal to 4.50:1.00 and greater than 4.00:1.00, which percentage is further reduced to 0% if the Total Net Leverage Ratio is less than or equal to 4.00:1.00, minus (B) at the option of the Borrower, (x) the aggregate amount of certain voluntary prepayments of term loans under the Credit Agreement during such fiscal year or after year-end and prior to the time such Excess Cash Flow prepayment is due, (y) the aggregate principal amount of any voluntary prepayments of indebtedness under pari passu incremental facilities, incremental equivalent debt and/or certain refinancing indebtedness, made during such fiscal year or after such fiscal year and prior to the time such prepayment is due.
The Credit Agreement requires the Borrower to repay amounts equal to 100% of the net cash proceeds of certain asset sales or other dispositions of property (including insurance and condemnation proceeds); provided, that, in the case of any prepayment events required in connection with certain dispositions and casualty events, if the net proceeds therefrom are invested (or committed to be invested) within 12 months after the receipt of such net proceeds, then no prepayment shall be required except to the extent such net proceeds have not been so invested (or committed to be invested) by the end of such 12-month period.
The Credit Agreement requires 100% of the net proceeds from the issuance or incurrence of certain indebtedness to be applied to prepay the term loans under the Term Loan Facility and the Incremental Term Loan Facility, except to the extent the indebtedness constitutes refinancing indebtedness.
F-56
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Condensed Consolidated Financial Statements (continued)
Voluntary Prepayment
The Borrower may voluntarily prepay outstanding borrowings under the Credit Facilities at any time in whole or in part without premium or penalty; provided, that, with respect to voluntary prepayments of the Term Loan Facility and the Incremental Term Loan Facility and in certain other circumstances, the Borrower may have to pay a prepayment premium.
Amortization and Final Maturity
The Term Loan Facility and Incremental Term Loan Facility are payable in quarterly installments in the principal amount of 0.25% of the original principal amount. The remaining unpaid balance on the Term Loan Facility and Incremental Term Loan Facility, together with all accrued and unpaid interest thereon, is due and payable on or prior to September 13, 2025. Outstanding borrowings under the Revolving Credit Facility and the Incremental Revolving Credit Facility do not amortize and are due and payable on September 13, 2024.
Guarantees and Security
The Borrower’s obligations under the Credit Facilities are guaranteed by Blizzard Midco, LLC and certain of the Borrower’s subsidiaries. All obligations under the Credit Agreement are secured by a first priority lien on substantially all of the assets of the Borrower, including a pledge of all of the equity interests of its subsidiaries.
Covenants and Other Matters
The Credit Agreement contains a number of covenants that, among other things and subject to certain exceptions, restrict the Borrower’s and its restricted subsidiaries’ ability to:
| • | incur indebtedness; |
| • | incur certain liens; |
| • | consolidate, merge or sell or otherwise dispose of assets; |
| • | make investments, loans, advances, guarantees and acquisitions; |
| • | pay dividends or make other distributions on equity interests, or redeem, repurchase or retire equity interests; |
| • | enter into transactions with affiliates; |
| • | alter the business conducted by the Company and subsidiaries; |
| • | change their fiscal year; and |
| • | amend or modify governing documents. |
In addition, the Credit Agreement contains financial and non-financial covenants. The Company is in compliance with all covenants as of March 31, 2020.
The Credit Agreement also contains certain customary representations and warranties and affirmative covenants, and certain reporting obligations. In addition, the lenders under the Credit Facilities will be permitted to accelerate all outstanding borrowings and other obligations, terminate outstanding commitments and exercise other specified remedies upon the occurrence of certain events of default (subject to certain grace periods and exceptions), which include, among other things, payment defaults, breaches of representations and warranties, covenant defaults, certain cross-defaults and cross-accelerations to other indebtedness, certain events of bankruptcy and insolvency, certain judgments and changes of control. Subject to certain limited exceptions, substantially all of the Company’s assets are restricted from distribution.
F-57
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Condensed Consolidated Financial Statements (continued)
Predecessor
During 2019, Norvax had a senior secured revolving credit facility (the “Predecessor Credit Facility”) with The Huntington National Bank (formerly FirstMerit Bank N.A.). In connection with the Acquisition, this facility was paid off and retired.
During 2018, Norvax amended its credit facility to increase the Predecessor Credit Facility from a maximum borrowing of $10,000 to $12,000 and again from $12,000 to $16,000. The Predecessor Credit Facility provided for borrowings up to a maximum of $16,000 based upon 80% of eligible trade accounts receivable, plus 40% of certain earned enrollment/commission fees. Norvax paid a variable interest rate on borrowings equal to, at Norvax’s discretion, Prime minus 50 basis points or LIBOR plus 250 basis points. Proceeds from borrowings were used to finance working capital and other general corporate purposes. The Predecessor Credit Facility was collateralized by substantially all the assets of Norvax and was subject to certain financial covenants. These covenants included maintaining a minimum fixed charge coverage ratio and not exceeding a maximum funded debt to earnings before interest, taxes, depreciation and amortization ratio (as defined in the credit agreement). The Predecessor Credit Facility originally matured in August 2019 and Norvax and The Huntington National Bank agreed to extend the maturity to November 2019.
7. MEMBERS’ EQUITY
Successor
The GoHealth Holdings, LLC operating agreement (“Operating Agreement”) provides for the classes of units, allocation of profits and losses, and other member rights. The Operating Agreement allows for equity Preferred units (the “Preferred”) and Common units (the “Common”). Preferred units are divided into two classes: Senior Preferred Earnout Units, which are non-voting, and Preferred Units (“Preferred Unit”), which have voting rights. Common units are divided into two classes: Class A Common units (“Class A”), which have voting rights and Class B Common units (“Class B”), which are non-voting. Members of management will be issued profits interests (the “Profit Units”, and together with the Preferred units and the Common units, the “Units”) from an equity pool with an aggregate value equal to 10% of the Company’s fully diluted equity.
Voting Rights
Each Preferred Unit and Class A unit has equal voting rights. The Preferred Unit and Class A unit holders also elect the members of the board of managers of the Company based on the percentage of units held by such investor.
Liquidation Preference
Upon a liquidity event defined as: (a) sale or disposition of all or substantially all of the assets of the Company; or (b) the liquidation, dissolution or winding up of the Company; first, in connection with refinancing or repayment of debt, Senior Preferred Earnout Units, the ceiling of which is the face amount of the Senior Preferred Earnout Units; second, Preferred Unit holders up to 150% of their invested capital; third, to Common holders, up to 150% of their invested capital; fourth, to the Profit Unit holders, pro rata, with the residual to the Common holders, pro rata, up to 150% of their invested capital, inclusive of prior distributions; fifth, to the Profit Unit holders, pro rata, with the residual to all members until each has received an aggregate amount of additional capital contributions, less amounts previously distributed; sixth, to Preferred Unit, Common and Profit Unit holders until Preferred Unit holders have received a cumulative amount equal to 250% of their invested capital; seventh, to Common holders equal to $75,000; eighth, pro rata, 100% Common, 100% Profit units, and 90% Preferred Unit/10% Common until Preferred Unit holders have received 300% of their invested capital; ninth,
F-58
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Condensed Consolidated Financial Statements (continued)
Common holders equal to $75,000; tenth, pro rata, 100% Common, 100% Profit units, 85% Preferred Unit/15% Common until Preferred Unit holders receive 400% of their invested capital; and, eleventh, pro rata, 100% Common, 100% Profit units and 80% Preferred Unit/20% Common.
Right of First Offer
Following the fifth anniversary of the Closing, Common units will be freely transferable, subject to customary “prohibited transfer” restrictions and a right of first offer for the benefit of the Company, first, and any non-transferring Investors, second.
Predecessor
The Norvax operating agreement (“Norvax Operating Agreement”) provided for classes of units, allocation of profits and losses, distribution rights, and other member rights. The Norvax Operating Agreement allowed for equity units (Class A units and Class B units) and profits interests units (Class C units). Class A and Class B units had voting rights. Except for board of manager composition, any action taken by the Class A and Class B members required a majority of members holding the outstanding Class A and Class B units, voting together as a single class. Class C units were nonvoting and represented profit interests’ units and entailed no initial capital contribution. Members were limited in their liability to their capital contributions. Immediately prior to the Acquisition described in Note 2 – Acquisition, all Class B units converted to Class A units.
Distribution Rights
Class A and Class B unit holders were entitled to distributions on a pro-rata basis, as approved by the board of managers. To the extent that Norvax had available cash, it distributed to each Class A and Class B unit holder a tax distribution in an amount equal to the product of the aggregate total of all taxable income allocable to the members multiplied by the tax rate. The tax rate is 45% as set forth in the Norvax Operating Agreement.
Voting Rights
Each Class A and Class B unit had equal voting rights and preferences, except Norwest Equity partners (“NEP”) was granted authority to approve certain actions. The Class A and Class B unit holders also elected the members of the board of managers of Norvax.
Antidilution Rights
Class B units contained an antidilution feature that required an adjustment to the conversion ratio in the event of subsequent issuances of securities by Norvax at a price below the conversion price in effect immediately prior to each such issuance. The Class B conversion ratio could be adjusted in the event that grants of options or changes in option prices or conversion rates on convertible securities resulted in prices below the conversion price in effect immediately prior to each such grant or change.
Liquidation Preference
Upon a liquidity event defined as: (a) sale or disposition of all or substantially all of the assets of Norvax; (b) the liquidation, dissolution or winding up of Norvax; or (c) any consolidation or merger of Norvax in which the Class A and Class B unit holders owned less than 50% of the voting power of the outstanding securities immediately after the consolidation or merger, the Class B units are first to be paid proceeds at a liquidation amount of $10.00 per unit, and from time to time, was decreased by subtracting distributions (other than tax distributions) made in respect to Class B units.
F-59
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Condensed Consolidated Financial Statements (continued)
Upon the occurrence of a Dissolution Event, Norvax continued solely for the purposes of winding up its affairs in an orderly manner, liquidating its assets, and satisfying the claims of its creditors and members. A Dissolution Event is an event by the order of a court pursuant to Section 18-802 of the Delaware Code or by action of the members with NEP’s approval. Net income, net losses, and other items of Norvax’s income, gain, loss, or deduction was to continue to be allocated in the manner provided in the Norvax Operating Agreement. In a Dissolution Event, Class B units received the liquidation preference specified above.
Involuntary Transfer Rights
Upon any involuntary transfer, Norvax had the first option, and the purchase option unit holders had the subsequent options, to purchase all or any portion of the units subject to the involuntary transfer.
Right of First Refusal
A unit holder could transfer, sell, or assign any Class A or Class B units in a permitted transfer, given that Norvax first had the option to purchase the units being transferred.
Class B Put Option
Class B units are classified as temporary equity as they were redeemable upon exercise of the Class B put option, which was outside of Norvax’s control, for cash at a put price equal to the greater of the Class B unit fair value or their original cost. Because the Class B units were redeemable, the Company was accreting the change up to the maximum redemption amount. The Company recorded accretion of $115,000 in the three months ended March 31, 2019. These amounts appear as Redeemable Class B unit accretion on the condensed consolidated statements of changes in members’ equity.
Immediately prior to the Acquisition described in Note 2 – Acquisition, Norvax adjusted NEP’s Redeemable Class B units to their full redemption amounts and were then converted to Class A units.
8. SHARE-BASED COMPENSATION PLANS
The following table summarizes the share-based compensation expense by operating function for the three months ended March 31, 2020:
| Successor | ||||
| Three Months Ended March 31, 2020 |
||||
| Marking and advertising |
$ | 57 | ||
| Customer care and enrollment |
24 | |||
| Technology |
73 | |||
| General and administrative |
325 | |||
|
|
|
|||
| Total share-based compensation expense |
$ | 479 | ||
|
|
|
|||
Successor
Effective September 13, 2019 and in conjunction with the Acquisition, the Company authorized the grants of non-voting Profit Units. The Profits Units are issued by Blizzard Management Feeder, LLC, to employees on behalf of the Company. One-third of the Profit Units granted to each employee (“Time-Vesting Units”) will vest in five (5) equal installments on the first through fifth anniversaries of the date of grant, so long as the employee remains employed by the Company through the applicable vesting date. Two-thirds of the Profit Units granted to
F-60
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Condensed Consolidated Financial Statements (continued)
each individual will vest upon a liquidity event based on the extent to which the distributions received by the Preferred and the Common exceed their investment in the Company (“Performance-Vesting Units”).
Compensation expense for the Time-Vesting Units is recognized on a straight-line basis over the five-year requisite service period. Performance-Vesting Units contain market conditions and an implied performance condition, which results in compensation cost being recognized when the performance condition is considered probable of being satisfied. Performance-Vesting Units vest upon the achievement of a contingent exit event that is defined as a transaction in which the ultimate parent disposes of all or substantially all its investment in the Company. Such an exit event is not considered probable until it consummates.
The number of Profit Units eligible for issuance will equal, in the aggregate, approximately 10% of the fully diluted equity of the Company at the closing of the Acquisition. All Profit Units (i.e., issued at closing of the Acquisition or issued thereafter) will have the economic rights and entitlements in relation to other equity interests in the Company under the waterfall described in the Operating Agreement.
The Company granted 6,001,788 of Profits Units in the three months ended March 31, 2020, of which 1,980,580 and 4,021,208 were Time-Vesting Units and Performance-Vesting Units, respectively.
Predecessor
Class C Incentive Plan
Norvax had a Class C Incentive Plan (the “Class C Plan”), which Norvax accounted for as a liability award. Class C units granted under the plan represented profit interests’ units and entailed no initial capital contribution. Class C units had no voting rights.
Incentive Share Plan
Norvax had an Incentive Share Plan, which Norvax accounted for as a liability award. The plan consisted of incentive share grants made to employees that provided for cash payments to participants upon the occurrence of a triggering event. Triggering events included a change in control or an employee’s involuntary termination without cause. In the event of a change in control, the triggering event value per share was the average per share purchase price of the common stock giving rise to such change in control. Cash payments were based on the difference between the triggering event value per share and the value per share on the grant date. In the event of an involuntary termination without cause, cash payments were calculated as the positive difference between the book value per share of Norvax’s stock on the date of the triggering event and the value per share on the grant date for each incentive share then triggered, as defined in the Incentive Share Plan.
9. INCOME TAXES
The Company’s effective tax rate for the first quarter of 2020 and 2019 was 0.14% and 0.05%, respectively. The effective tax rate for each period is lower than the statutory tax rate primarily due to the effect of tax-exempt entity status.
10. COMMITMENTS AND CONTINGENCIES
Leases
The Company entered into various non-cancelable operating lease agreements for certain of the Company’s offices and data centers with lease periods expiring in 2030. Certain of these arrangements have free rent periods or escalating rent payment provisions, and the Company recognizes rent expense under such arrangements on a straight-line basis.
F-61
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Condensed Consolidated Financial Statements (continued)
Legal Proceedings
From time to time, the Company is party to various litigation matters incidental to the conduct of its business. The Company is not presently party to any legal proceedings the resolution of which it believes would have a material adverse effect on its business, prospects, financial condition, liquidity, results of operation, cash flows or capital levels.
11. RELATED-PARTY TRANSACTIONS
The Company has entered into various lease agreements with 214 W Huron LLC, 220 W Huron Street Holdings LLC, and 215 W Superior LLC, each of which are controlled by significant shareholders, to lease its corporate offices in Chicago, Illinois. The Company pays rent, operating expenses, maintenance, and utilities under the terms of the leases. For the three months ended March 31, 2020 and 2019, the Company made aggregate lease payments of $321 and $245, respectively, under these leases.
On January 1, 2020, the Company entered into a non-exclusive aircraft dry lease agreement with an entity wholly-owned and controlled by significant shareholders. The agreement allows the Company to use an aircraft owned by this entity for business and on an as-needed basis. The agreement has no set term and is terminable without cause by either party upon 30 days’ prior written notice. Under the agreement, the Company is required to pay $6,036.94 per flight hour for use of the aircraft. For the three months ended March 31, 2020, the Company recorded expense of $747 under this lease, all of which was unpaid and recorded as accounts payable in the condensed consolidated balance sheet as of March 31, 2020.
On May 12, 2020, the Company entered into a lease agreement with Wilson Tech 5, which is controlled by significant shareholders, for a proposed site in Linden, Utah, beginning in 2022. This lease agreement expires on May 11, 2030.
12. OPERATING SEGMENTS AND SIGNIFICANT CUSTOMERS
Operating Segments
The Company reports segment information based on how the Company’s chief operating decision maker (“CODM”), regularly reviews operating results, allocates resources and makes decisions regarding business operations. The performance measures of the segments include total revenue and profit (loss). The Company’s business structure is comprised of four operating and reportable segments: Medicare Internal, Medicare External, Individual and Family Plan and Other (“IFP and Other”) Internal, and IFP External.
F-62
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Condensed Consolidated Financial Statements (continued)
The following table presents summary results of the Company’s operating segments for the following periods:
| Successor | Predecessor | |||||||||||||||
| Three Months Ended March 31, 2020 |
Three Months Ended March 31, 2019 |
|||||||||||||||
| Revenues: |
||||||||||||||||
| Medicare: |
||||||||||||||||
| Internal channel |
$ | 95,287 | $ | 20,911 | ||||||||||||
| External channel |
28,945 | 20,335 | ||||||||||||||
|
|
|
|
|
|||||||||||||
| Total Medicare |
124,232 | 41,246 | ||||||||||||||
| Individual and Family Plan and Other: |
||||||||||||||||
| Internal channel |
8,632 | 14,440 | ||||||||||||||
| External channel |
8,146 | 13,403 | ||||||||||||||
|
|
|
|
|
|||||||||||||
| Total Individual and Family Plan and Other |
16,778 | 27,843 | ||||||||||||||
|
|
|
|
|
|||||||||||||
| Total revenues |
141,010 | 69,089 | ||||||||||||||
| Segment profit (loss): |
||||||||||||||||
| Medicare: |
||||||||||||||||
| Internal channel |
41,735 | 4,864 | ||||||||||||||
| External channel |
(322 | ) | 3,380 | |||||||||||||
|
|
|
|
|
|||||||||||||
| Total Medicare segment profit |
41,413 | 8,244 | ||||||||||||||
| Individual and Family Plan and Other: |
||||||||||||||||
| Internal channel |
481 | 881 | ||||||||||||||
| External channel |
512 | 1,263 | ||||||||||||||
|
|
|
|
|
|||||||||||||
| Total Individual and Family Plan and Other segment profit |
993 | 2,144 | ||||||||||||||
|
|
|
|
|
|||||||||||||
| Total segment profit |
42,406 | 10,388 | ||||||||||||||
| Corporate |
8,665 | 5,346 | ||||||||||||||
| Change in fair value of contingent consideration liability |
4,400 | — | ||||||||||||||
| Amortization of intangible assets |
23,514 | — | ||||||||||||||
| Interest expense |
6,756 | 28 | ||||||||||||||
| Other expense |
10 | 10 | ||||||||||||||
|
|
|
|
|
|||||||||||||
| Income (loss) before income taxes |
$ | (939 | ) | $ | 5,004 | |||||||||||
|
|
|
|
|
|||||||||||||
There are no internal revenue transactions between the Company’s operating segments. The Company’s CODM does not separately evaluate assets by segment, and therefore assets by segment are not presented. The Company’s assets are primarily located in the United States.
Significant Customers
Substantially all revenue for the three months ended March 31, 2020 and 2019 was generated from customers located in the United States. Carriers representing 10% or more of the Company’s total revenue for the following periods are presented in the table below:
| Successor | Predecessor | |||||||||||
| March 31, 2020 | March 31, 2019 | |||||||||||
| Humana |
42 | % | 28 | % | ||||||||
| Anthem |
32 | % | 15 | % | ||||||||
F-63
Table of Contents
GoHealth Holdings, LLC and Subsidiaries
Notes to Condensed Consolidated Financial Statements (continued)
13. SUBSEQUENT EVENTS
Management has reviewed its March 31, 2020, condensed consolidated financial statements for subsequent events through June 15, 2020, the date the financial statements were available to be issued. Other than the subsequent events described in Note 1 – Summary of Business and Significant Accounting Policies, Note 2 – Acquisition, Note 6 – Long Term Debt, and Note 11 – Related-Party Transactions, the Company is not aware of any subsequent events that would require recognition or disclosure in the consolidated financial statements.
F-64
Table of Contents
Shares

GoHealth, Inc.
Class A Common Stock
PROSPECTUS
Goldman Sachs & Co. LLC
BofA Securities
Morgan Stanley
Barclays
Credit Suisse
Evercore ISI
RBC Capital Markets
William Blair
Cantor
SunTrust Robinson Humphrey
, 2020
Table of Contents
PART II
INFORMATION NOT REQUIRED IN THE PROSPECTUS
Item 13. Other expenses of issuance and distribution.
The following table sets forth all fees and expenses, other than the underwriting discount payable solely by GoHealth, Inc. in connection with the offer and sale of the securities being registered. All amounts shown are estimated except for the SEC registration fee, the Financial Industry Regulatory Authority, Inc., or FINRA, filing fee and the Nasdaq listing fee.
| SEC registration fee |
$ | * | ||
| FINRA filing fee |
* | |||
| Nasdaq listing fee |
* | |||
| Printing and engraving expenses |
* | |||
| Legal fees and expenses |
* | |||
| Accounting fees and expenses |
* | |||
| Blue sky qualification fees and expenses |
* | |||
| Transfer agent fees and expenses |
* | |||
| Miscellaneous fees and expenses |
* | |||
|
|
|
|||
| Total |
$ | * | ||
|
|
|
| * | To be filed by amendment |
Item 14. Indemnification of directors and officers.
Section 102 of the General Corporation Law of the State of Delaware permits a corporation to eliminate the personal liability of directors of a corporation to the corporation or its stockholders for monetary damages for a breach of fiduciary duty as a director, except where the director breached his duty of loyalty, failed to act in good faith, engaged in intentional misconduct or knowingly violated a law, authorized the payment of a dividend or approved a stock repurchase or redemption in violation of Delaware corporate law or obtained an improper personal benefit. Our amended and restated certificate of incorporation provides that no director of GoHealth, Inc. shall be personally liable to it or its stockholders for monetary damages for any breach of fiduciary duty as a director, notwithstanding any provision of law imposing such liability, except to the extent that the General Corporation Law of the State of Delaware prohibits the elimination or limitation of liability of directors for breaches of fiduciary duty.
Section 145 of the General Corporation Law of the State of Delaware provides that a corporation has the power to indemnify a director, officer, employee, or agent of the corporation, or a person serving at the request of the corporation for another corporation, partnership, joint venture, trust or other enterprise in related capacities against expenses (including attorneys’ fees), judgments, fines and amounts paid in settlement actually and reasonably incurred by the person in connection with an action, suit or proceeding to which he was or is a party or is threatened to be made a party to any threatened, ending or completed action, suit or proceeding by reason of such position, if such person acted in good faith and in a manner he reasonably believed to be in or not opposed to the best interests of the corporation, and, in any criminal action or proceeding, had no reasonable cause to believe his conduct was unlawful, except that, in the case of actions brought by or in the right of the corporation, no indemnification shall be made with respect to any claim, issue or matter as to which such person shall have been adjudged to be liable to the corporation unless and only to the extent that the Court of Chancery or other adjudicating court determines that, despite the adjudication of liability but in view of all of the circumstances of the case, such person is fairly and reasonably entitled to indemnity for such expenses which the Court of Chancery or such other court shall deem proper.
II-1
Table of Contents
Upon consummation of the Transactions, our amended and restated certificate of incorporation and amended and restated bylaws will provide indemnification for our directors and officers to the fullest extent permitted by the General Corporation Law of the State of Delaware. We will indemnify each person who was or is a party or threatened to be made a party to any threatened, pending or completed action, suit or proceeding (other than an action by or in the right of us) by reason of the fact that he or she is or was, or has agreed to become, a director or officer, or is or was serving, or has agreed to serve, at our request as a director, officer, partner, employee or trustee of, or in a similar capacity with, another corporation, partnership, joint venture, trust or other enterprise (all such persons being referred to as an “Indemnitee”), or by reason of any action alleged to have been taken or omitted in such capacity, against all expenses (including attorneys’ fees), judgments, fines and amounts paid in settlement actually and reasonably incurred in connection with such action, suit or proceeding and any appeal therefrom, if such Indemnitee acted in good faith and in a manner he or she reasonably believed to be in, or not opposed to, our best interests, and, with respect to any criminal action or proceeding, he or she had no reasonable cause to believe his or her conduct was unlawful. Our amended and restated certificate of incorporation and amended and restated bylaws will provide that we will indemnify any Indemnitee who was or is a party to an action or suit by or in the right of us to procure a judgment in our favor by reason of the fact that the Indemnitee is or was, or has agreed to become, a director or officer, or is or was serving, or has agreed to serve, at our request as a director, officer, partner, employee or trustee of, or in a similar capacity with, another corporation, partnership, joint venture, trust or other enterprise, or by reason of any action alleged to have been taken or omitted in such capacity, against all expenses (including attorneys’ fees) and, to the extent permitted by law, amounts paid in settlement actually and reasonably incurred in connection with such action, suit or proceeding, and any appeal therefrom, if the Indemnitee acted in good faith and in a manner he or she reasonably believed to be in, or not opposed to, our best interests, except that no indemnification shall be made with respect to any claim, issue or matter as to which such person shall have been adjudged to be liable to us, unless a court determines that, despite such adjudication but in view of all of the circumstances, he or she is entitled to indemnification of such expenses. Notwithstanding the foregoing, to the extent that any Indemnitee has been successful, on the merits or otherwise, he or she will be indemnified by us against all expenses (including attorneys’ fees) actually and reasonably incurred in connection therewith. Expenses must be advanced to an Indemnitee under certain circumstances.
Prior to the consummation of this offering, we intend to enter into separate indemnification agreements with each of our directors and executive officers. Each indemnification agreement will provide, among other things, for indemnification to the fullest extent permitted by law against any and all expenses, judgments, fines, penalties and amounts paid in settlement of any claim. The indemnification agreements will provide for the advancement or payment of all expenses to the indemnitee and for the reimbursement to us if it is found that such indemnitee is not entitled to such indemnification under applicable law and our amended and restated certificate of incorporation and amended and restated bylaws.
We maintain a general liability insurance policy that covers certain liabilities of directors and officers of our corporation arising out of claims based on acts or omissions in their capacities as directors or officers.
In any underwriting agreement we enter into in connection with the sale of Class A common stock being registered hereby, the underwriters will agree to indemnify, under certain conditions, us, our directors, our officers and persons who control us within the meaning of the Securities Act, against certain liabilities.
Item 15. Recent sales of unregistered securities.
On March 27, 2020, GoHealth, Inc. agreed to issue 1,000 shares of common stock, par value $0.001 per share, which will be redeemed upon the consummation of the Transactions, to GoHealth Holdings, LLC in exchange for $1.00. The issuance was exempt from registration under Section 4(a)(2) of the Securities Act, as a transaction by an issuer not involving any public offering.
II-2
Table of Contents
Item 16. Exhibits and financial statements.
| (a) | Exhibits |
The following documents are filed as exhibits to this registration statement.
| Exhibit |
||
| 1.1* | Form of Underwriting Agreement. | |
| 3.1 | Certificate of Incorporation of GoHealth, Inc., as in effect prior to the consummation of the Transactions. | |
| 3.2* | Form of Amended and Restated Certificate of Incorporation of GoHealth, Inc., to be in effect upon the consummation of the Transactions. | |
| 3.3 | Bylaws of GoHealth, Inc., as in effect prior to the consummation of the Transactions. | |
| 3.4* | Form of Amended and Restated Bylaws of GoHealth, Inc., to be in effect upon the consummation of the Transactions. | |
| 4.1 | Specimen Stock Certificate evidencing the shares of Class A common stock. | |
| 5.1* | Opinion of Latham & Watkins LLP. | |
| 10.1* | Form of Tax Receivable Agreement, to be effective upon the consummation of the Transactions. | |
| 10.2* | Form of Second Amended and Restated LLC Agreement of GoHealth Holdings, LLC, to be effective upon the consummation of the Transactions. | |
| 10.3* | Form of Stockholders Agreement, to be effective upon the consummation of the Transactions. | |
| 10.4* | Form of Registration Rights Agreement, to be effective upon the consummation of the Transactions. | |
| 10.5+† | Incremental Facility Agreement and Technical Amendment No. 2 to Credit Agreement, dated as of May 7, 2020, among Norvax, LLC, as borrower, Blizzard Midco, LLC, as a guarantor, the other guarantors party thereto, Owl Rock Capital Corporation, as administrative agent, collateral agent and swingline lender and the other lenders from time to time party thereto. | |
| 10.7*# | 2020 Incentive Award Plan. | |
| 10.8*# | 2020 Employee Stock Purchase Plan. | |
| 10.9† | Form of Indemnification Agreement between GoHealth, Inc. and its directors and officers. | |
| 21.1* | List of Subsidiaries of GoHealth, Inc. | |
| 23.1 | Consent of Ernst & Young LLP, as to GoHealth, Inc. | |
| 23.2 | Consent of Ernst & Young LLP, as to GoHealth Holdings, LLC. | |
| 23.3* | Consent of Latham & Watkins LLP (contained in its opinion filed as Exhibit 5.1 hereto). | |
| 24.1 | Power of Attorney (included on signature page). | |
| * | To be filed by amendment |
| # | Indicates management contract or compensatory plan |
| + | Certain of the schedules and attachments to this exhibit have been omitted pursuant to Regulation S-K, Item 601(a)(5). The registrant hereby undertakes to provide further information regarding such omitted materials to the Commission upon request. |
| † | Certain portions of this exhibit (indicated by “####”) have been omitted pursuant to Regulation S-K, Item 601(a)(6). |
Item 17. Undertakings.
| (a) | The undersigned registrant hereby undertakes to provide to the underwriters at the closing specified in the underwriting agreement certificates in such denominations and registered in such names as required by the underwriters to permit prompt delivery to each purchaser. |
| (b) | Insofar as indemnification for liabilities arising under the Securities Act may be permitted to directors, officers and controlling persons of GoHealth, Inc. pursuant to the foregoing provisions, or otherwise, |
II-3
Table of Contents
| GoHealth, Inc. has been advised that in the opinion of the SEC such indemnification is against public policy as expressed in the Securities Act and is, therefore, unenforceable. In the event that a claim for indemnification against such liabilities (other than the payment by GoHealth, Inc. of expenses incurred or paid by a director, officer or controlling person of GoHealth, Inc. in the successful defense of any action, suit or proceeding) is asserted by such director, officer or controlling person in connection with the securities being registered, GoHealth, Inc. will, unless in the opinion of its counsel the matter has been settled by controlling precedent, submit to a court of appropriate jurisdiction, the question whether such indemnification by it is against public policy as expressed in the Securities Act and will be governed by the final adjudication of such issue. |
| (c) | The undersigned hereby further undertakes that: |
| (1) | For purposes of determining any liability under the Securities Act the information omitted from the form of prospectus filed as part of this registration statement in reliance upon Rule 430A and contained in a form of prospectus filed by GoHealth, Inc. pursuant to Rule 424(b)(1) or (4) or 497(h) under the Securities Act shall be deemed to be part of this registration statement as of the time it was declared effective. |
| (2) | For the purpose of determining any liability under the Securities Act each post-effective amendment that contains a form of prospectus shall be deemed to be a new registration statement relating to the securities offered therein, and the offering of such securities at that time shall be deemed to be the initial bona fide offering thereof. |
II-4
Table of Contents
Pursuant to the requirements of the Securities Act of 1933, as amended, GoHealth, Inc. has duly caused this registration statement to be signed on its behalf by the undersigned, thereunto duly authorized, in the city of Chicago, state of Illinois, on this 19th day of June, 2020.
| GoHealth, Inc. | ||
| By: |
/s/ Clinton P. Jones | |
| Clinton P. Jones Chief Executive Officer | ||
POWER OF ATTORNEY
Each of the undersigned officers and directors of GoHealth, Inc. hereby constitutes and appoints Clinton P. Jones and Travis J. Matthiesen, and each of them any of whom may act without joinder of the other, the individual’s true and lawful attorneys-in-fact and agents, each with full power of substitution and resubstitution, for the person and in his or her name, place and stead, in any and all capacities, to sign this registration statement of GoHealth, Inc. on Form S-1, and any other registration statement relating to the same offering (including any registration statement, or amendment thereto, that is to become effective upon filing pursuant to Rule 462(b) under the Securities Act of 1933, as amended), and any and all amendments thereto (including post-effective amendments to the registration statement), and to file the same, with all exhibits thereto, and all other documents in connection therewith, with the Securities and Exchange Commission, granting unto said attorneys-in-fact and agents, and each of them, full power and authority to do and perform each and every act and thing requisite and necessary to be done in connection therewith, as fully to all intents and purposes as he or she might or could do in person, hereby ratifying and confirming all that said attorneys-in-fact and agents or any of them, or their substitute or substitutes, may lawfully do or cause to be done by virtue hereof.
Pursuant to the requirements of the Securities Act of 1933, as amended, this registration statement on Form S-1 has been signed by the following persons in the capacities set forth opposite their names and on the date indicated above.
| Signature | Title | Date | ||
| /s/ Clinton P. Jones |
Chief Executive Officer and Director (Principal Executive Officer) | June 19, 2020 | ||
| Clinton P. Jones | ||||
| /s/ Travis J. Matthiesen |
Chief Financial Officer (Principal Financial Officer and Principal Accounting Officer) | June 19, 2020 | ||
| Travis J. Matthiesen | ||||
| /s/ Brandon M. Cruz |
Director | June 19, 2020 | ||
| Brandon M. Cruz | ||||
| /s/ Rahm Emanuel |
Director | June 19, 2020 | ||
| Rahm Emanuel | ||||
| /s/ Joseph G. Flanagan |
Director | June 19, 2020 | ||
| Joseph G. Flanagan | ||||
| /s/ Jeremy W. Gelber |
Director | June 19, 2020 | ||
| Jeremy W. Gelber | ||||
| /s/ Miriam A. Tawil |
Director | June 19, 2020 | ||
| Miriam A. Tawil | ||||
| /s/ Alexander E. Timm |
Director | June 19, 2020 | ||
| Alexander E. Timm | ||||
II-5
