Attached files
| file | filename |
|---|---|
| EX-32 - EXHIBIT 32 - Diversicare Healthcare Services, Inc. | dvcrex32certificationofthe.htm |
| EX-31.2 - EXHIBIT 31.2 - Diversicare Healthcare Services, Inc. | dvcrex312cfocertification1.htm |
| EX-31.1 - EXHIBIT 31.1 - Diversicare Healthcare Services, Inc. | dvcrex311ceocertification1.htm |
| EX-23.1 - EXHIBIT 23.1 - Diversicare Healthcare Services, Inc. | dvcrex231-123117.htm |
| EX-21 - EXHIBIT 21 - Diversicare Healthcare Services, Inc. | dvcrex21-subsidiarieslisti.htm |
| EX-10.62 - EXHIBIT 10.62 - Diversicare Healthcare Services, Inc. | dvcrex1062-thirdamendmentt.htm |
| EX-10.61 - EXHIBIT 10.61 - Diversicare Healthcare Services, Inc. | dvcrex1061-fifthamendmentt.htm |
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
________________________________
FORM 10-K
________________________________
CHECK ONE:
ý | ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the fiscal year ended December 31, 2017
OR
¨ | TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the transition period from to .
Commission file No.: 1-12996
________________________________
Diversicare Healthcare Services, Inc.
(exact name of registrant as specified in its charter)
________________________________
Delaware | 62-1559667 | |
(State or other jurisdiction of incorporation or organization) | (IRS Employer Identification No.) | |
1621 Galleria Boulevard, Brentwood, TN | 37027 |
(Address of principal executive offices) | (Zip Code) |
Registrant's telephone number, including area code: (615) 771-7575
Securities registered pursuant to Section 12(b) of the Act:
Title of each class | Name of each Exchange on which registered |
Common Stock, $0.01 par value per share | The NASDAQ Capital Market |
Securities registered pursuant to Section 12(g) of the Act:
None.
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act.
Yes ¨ No þ
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act.
Yes ¨ No þ
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes þ No ¨
Indicate by check mark whether the registrant has submitted electronically and posted on its corporate Web site, if any, every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S-T (§232.405 of this chapter) during the preceding 12 months (or for such shorter period that the registrant was required to submit and post such files). Yes þ No ¨
Indicate by check mark if disclosure of delinquent filers pursuant to Item 405 of Regulation S-K is not contained herein, and will not be contained, to the best of registrant's knowledge, in definitive proxy or information statements incorporated by reference in Part III of this Form 10-K or any amendment to this Form 10-K. ¨
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, a smaller reporting company, or an emerging growth company. See the definitions of “large accelerated filer,” “accelerated filer”, “smaller reporting company,” and "emerging growth company" in Rule 12b-2 of the Exchange Act.
Large accelerated filer ¨ Accelerated filer ¨ Non-accelerated filer ¨ Smaller reporting company þ
Emerging growth company ¨
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Act). Yes ¨ No þ
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. | ¨ |
The aggregate market value of Common Stock held by non-affiliates on June 30, 2017 (based on the closing price of such shares on the NASDAQ Capital Market) was approximately $38,398,000. For purposes of the foregoing calculation only, all directors, named executive officers and persons known to the registrant to be holders of 5% or more of the registrant's Common Stock have been deemed affiliates of the registrant.
On February 15, 2018, 6,455,487 shares of the registrant's $0.01 par value Common Stock were outstanding.
Documents Incorporated by Reference
Registrant's definitive proxy materials for its 2018 annual meeting of shareholders are incorporated by reference into Part III, Items 10, 11, 12, 13 and 14 of this Form 10-K.
Table of Contents | |||
Page | |||
Part I | |||
Item 1. | Business | ||
Item 1A. | Risk Factors | ||
Item 1B. | Unresolved Staff Comments | ||
Item 2. | Properties | ||
Item 3. | Legal Proceedings | ||
Item 4. | Mine Safety Disclosures | ||
Part II | |||
Item 5. | Market for Registrant's Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities | 24 | |
Item 6. | Selected Consolidated Financial Data | ||
Item 7. | Management's Discussion and Analysis of Financial Condition and Results of Operations | 27 | |
Item 7A. | Quantitative and Qualitative Disclosures about Market Risk | ||
Item 8. | Financial Statements and Supplementary Data | ||
Item 9. | Changes in and Disagreements with Accountants on Accounting and Financial Disclosure | ||
Item 9A. | Controls and Procedures | ||
Item 9B. | Other Information | ||
Part III | |||
Item 10. | Directors, Executive Officers and Corporate Governance | ||
Item 11. | Executive Compensation | ||
Item 12. | Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters | ||
Item 13. | Certain Relationships and Related Transactions, and Director Independence | ||
Item 14. | Principal Accountant Fees and Services | ||
Part IV | |||
Item 15. | Exhibits and Financial Statement Schedules | ||
Item 16. | Form 10-K Summary | ||
PART 1
ITEM 1. BUSINESS
Introductory Summary.
Diversicare Healthcare Services, Inc. provides post-acute care services to skilled nursing facilities, referred to as"skilled nursing centers," "nursing centers," or "centers," patients and residents in ten states, primarily in the Southeast, Midwest, and Southwest United States. Unless the context indicates otherwise, references herein to “Diversicare,” “the Company,” “we,” “us” and “our” include Diversicare Healthcare Services, Inc. and all of our consolidated subsidiaries. Diversicare Healthcare Services, Inc. was incorporated as a Delaware corporation in 1994.
The post-acute care profession encompasses a broad range of non-institutional and institutional services. For those among the aging, infirmed, or disabled requiring temporary or limited special services, a variety of home care options exist. As the need for assistance in activities of daily living develop, assisted living centers become the most viable and cost effective option. For those amongst the aging, disabled, or infirmed requiring more extensive assistance and intensive care, skilled nursing center care may become the only viable option. We have chosen to focus our business primarily on the skilled nursing centers sector and to specialize in this aspect of the post-acute care continuum.
Principal Address and Website.
Our principal executive offices are located at 1621 Galleria Boulevard, Brentwood, Tennessee 37027. Our telephone number at that address is 615.771.7575, and our facsimile number is 615.771.7409. Our website is located at www.dvcr.com. The information on our website does not constitute part of this Annual Report on Form 10-K.
Operating and Growth Strategy.
Our operating objective is to optimize market position in the delivery of health care and related services to the patients and residents in need of post-acute care in the communities in which we operate. Our strategic operations development plan focuses on (i) providing a broad range of high quality, cost-effective post-acute care services; (ii) improving skilled mix in our nursing centers via enhanced capabilities for rehabilitation and transitional care; (iii) building clinical competencies and programs consistent with marketplace needs; and (iv) clustering our operations on a regional basis. Interwoven into our objectives and operating strategy is our mission:
• Improve Every Life We Touch
• Provide Exceptional Healthcare
• Exceed Expectations
• Increase Shareholder Value
Strategic operating initiatives. Our key strategic operating initiatives include improving skilled mix in our nursing centers by enhancing our staffing complement to address the increased medical complexity of certain patients, increasing clinical competencies, and adding clinical programs. The investments in nursing and clinical care have been implemented in concert with additional investments in nursing center-based sales representatives to cultivate referral and Managed Care relationships. These investments have positioned us and are expected to continue to position us to be a destination for patients covered by Medicare and Managed Care as well as certain private pay individuals. These enhancements and investments have positioned us to admit higher acuity patients.
Another strategic operating initiative was to implement an Electronic Medical Records (“EMR”) platform. See description of our EMR implementation below. We completed the implementation of Electronic Medical Records in all our nursing centers in December 2011, and implement EMR at all new centers near the time we commence operations.
To achieve our objectives, we:
Provide a broad range of quality cost-effective services. Our objective is to provide a variety of services to meet the needs of the increasing post-acute care population requiring skilled nursing and rehabilitation care. Our service offerings currently include skilled nursing, comprehensive rehabilitation services, programming for Life Steps and Memory Care units (described below) and other specialty programming. By addressing varying levels of acuity, we work to meet the needs of the population we serve. We seek to establish a reputation as the provider of choice in each of our markets. Furthermore, we believe we are able to deliver quality services cost-effectively, compared to other healthcare providers along the spectrum of care, thereby expanding the population base that can benefit from our services.
1
Improve skilled mix in our nursing centers. By enhancing our registered nurse coverage and adding specialized clinical care, we believe we can admit patients with more medically complex conditions, thereby improving skilled mix and reimbursement. The investments in nursing and clinical care are being conducted in concert with additional investments in nursing center-based sales representatives to develop referral and Managed Care relationships. These investments will better attract quality payor sources for patients covered by Medicare, Managed Care and Medicare replacement payors as well as certain private pay individuals. We will also continue our program for the renovation and improvement of our nursing centers to attract and retain patients and residents.
Cluster operations on a regional basis. We have developed regional concentrations of operations in order to achieve operating efficiencies, generate economies of scale and capitalize on marketing opportunities created by having multiple operations in a regional market area.
Key elements of our growth strategy are to:
Increase revenues and profitability at existing nursing centers. Our strategy includes increasing center revenues and profitability through improving payor mix, providing an increasing level of higher acuity care, obtaining appropriate reimbursement for the care we provide, and providing high quality patient care. Ongoing investments are being made in expanded nursing and clinical care. We continue to enhance center-based marketing initiatives to promote higher occupancy levels and improved skilled mix at our nursing centers.
Development of additional specialty services. Our strategy includes the development of additional specialty units and programming in nursing centers that could benefit from these services. The specialty programming will vary depending on the needs of the specific market, and may include complex medical and rehabilitation services, as well as memory care units and other specialty programming. These services allow our centers to meet market needs while improving census and payor mix. A center specific assessment of the market and the current programming being offered is conducted related to specialty programming to determine if unmet needs exist as a predictor of the success of particular niche offerings and services.
Acquisition, leasing and development of new centers. We continue to pursue and investigate opportunities to acquire, lease or develop new centers, focusing primarily on opportunities that can leverage our existing infrastructure.
Nursing Centers and Services.
Diversicare provides a broad range of post-acute care services to patients and residents including skilled nursing, ancillary health care services and assisted living. In addition to the nursing and social services usually provided in long-term care centers, we offer a variety of rehabilitative, nutritional, respiratory, and other specialized ancillary services. As of December 31, 2017, our continuing operations consist of 76 nursing centers with 8,456 licensed skilled nursing beds. Our nursing centers range in size from 48 to 320 licensed nursing beds. The licensed nursing bed count does not include 489 licensed assisted living beds. Our continuing operations include centers in Alabama, Florida, Indiana, Kansas, Kentucky, Mississippi, Missouri, Ohio, Tennessee, and Texas.
2
The following table summarizes certain information with respect to the nursing centers we own or lease as of December 31, 2017:
Number of Centers | Licensed Nursing Beds (1) | Available Nursing Beds (1) | ||||||
Operating Locations: | ||||||||
Alabama | 20 | 2,385 | 2,318 | |||||
Florida | 1 | 79 | 79 | |||||
Indiana | 1 | 158 | 158 | |||||
Kansas | 6 | 464 | 464 | |||||
Kentucky | 13 | 1,127 | 1,123 | |||||
Mississippi | 9 | 1,039 | 1,004 | |||||
Missouri | 3 | 339 | 339 | |||||
Ohio | 5 | 403 | 393 | |||||
Tennessee | 5 | 617 | 551 | |||||
Texas | 13 | 1,845 | 1,662 | |||||
76 | 8,456 | 8,091 | ||||||
Classification: | ||||||||
Owned | 18 | 1,607 | 1,404 | |||||
Leased | 58 | 6,849 | 6,687 | |||||
Total | 76 | 8,456 | 8,091 | |||||
____________
(1) | The number of Licensed Nursing Beds is based on the regulatory licenses for the nursing center. The Company reports its occupancy based on licensed nursing beds. The number of Available Nursing Beds represents Licensed Nursing Beds reduced by beds removed from service. Available Nursing Beds is subject to change based upon the needs of the centers, including configuration of patient rooms, common usage areas and offices, status of beds (private, semi-private, ward, etc.) and renovations. The number of Licensed and Available Nursing Beds does not include 489 Licensed Assisted Living/Residential Beds, all of which are also available, and the number of centers excludes one stand-alone Assisted Living Facility in Ohio. These beds are excluded from the bed counts as our operating statistics such as occupancy are calculated using Nursing Beds only. |
Our nursing centers provide skilled nursing health care services, including nutrition services, recreational therapy, social services, housekeeping and laundry services. Skilled nursing care is provided for post-acute patients and residents with comorbidities. This care includes assessment using evidence based tools; individualized care plan development based on identified areas of risk and care needs; and skilled interventions such as IV services. We also provide for the delivery of ancillary medical services at the nursing centers we operate. These specialty services include rehabilitation therapy services, such as audiology, speech, occupational and physical therapies, which are provided through licensed therapists and registered nurses, and the provision of medical supplies, nutritional support, infusion therapies and related clinical services. The majority of these services are provided using our internal resources and clinicians.
Within the framework of a nursing center, we may provide other specialty care, including:
Transitional Care Unit. Many of our nursing centers have units designated as transitional care units, our designation for patients requiring transitional care following an acute stay in the hospital. These units specialize in short-term nursing and rehabilitation with the goal of returning the patient to their highest potential level of functionality. These units provide enhanced services with emphasis on upgraded amenities. The design and programming of the units generally appeal to the clinical and hospitality needs of individuals as they progress to the next appropriate level of care. Specialized therapeutic treatment regimens include orthopedic rehabilitation, neurological rehabilitation and complex medical rehabilitation. While these patients generally have a shorter length of stay, the intensive level of nursing and rehabilitation required by these patients typically results in higher levels of reimbursement.
Memory Care Unit. Like our transitional care units, many of our nursing centers have memory care units, our designation for advanced care for dementia-related disorders including Alzheimer's disease. The goal of the units is to provide a safe, homelike and supportive environment for cognitively impaired patients, utilizing an interdisciplinary team approach. Family and community involvement complement structured programming in the secure environment instrumental in fostering as much resident independence and purposeful quality of life as long as possible despite diminished capacity.
3
Enhanced Therapy Services. We have complemented our traditional therapy services with programs that provide electrotherapy, vital stimulation, ultrasound and shortwave diathermy therapy treatments that promote pain management, wound healing, muscle strengthening, and/or contractures management, improving outcomes for our patients and residents receiving therapy treatments.
Other Specialty Programming. We implement other specialty programming based on a center's specific needs. We have developed two adult day care centers on nursing center campuses. We have developed specialty programming for bariatric patients (generally, patients weighing more than 350 pounds) at one of these centers as these individuals have unique psychosocial and equipment needs.
Quality Assurance and Performance Improvement. We have in place a Quality Assurance and Performance Improvement (“QAPI”) program, which is focused on monitoring and improving all aspects of the care provided in a center by identifying outcomes and acting on areas of improvement. The QAPI program in our centers addresses all systems of care and management practices. Key quality indicators are determined and performance goals and benchmarks are established based on industry research standards via a Balanced Scorecard. Gaps and opportunities in performance versus benchmarks are addressed with analysis and performance improvement plans. Outcomes from each center in the areas of quality, employee workplace, customer satisfaction, and stewardship are collected monthly and overseen by regional and company quality committees.
Utilization of Electronic Medical Records. We successfully completed the full implementation of EMR in our nursing centers. EMR improves our ability to accurately record the care provided to our patients and quickly respond to areas of need. We now implement the use of EMR near the time of acquisition for new centers. EMR improves customer and employee satisfaction, nursing center regulatory compliance and provides real-time monitoring and scheduling of care delivery. We believe our EMR system supports our quality initiatives and positions us for higher acuity service offerings. Our EMR system is comprehensive in its functionality, providing key components, such as:
• | Tracking Activities of Daily Living (“ADLs”). ADLs are the functions that each person must perform on a daily basis including, but not limited to, getting dressed, bathing, and eating. ADL tracking allows us to capture the provision of care provided by our nursing, dietary and housekeeping staff in assisting with ADLs quickly, efficiently and electronically. |
• | Progress Notes. Progress notes are an important component of our medical records. Licensed nursing professionals provide documentation reflecting assessment of each patient's condition and intervention of skilled care provided. The EMR system provides means for a comprehensive chronological record resulting in improved capture, monitoring and review of documentation of condition and care provided. |
• | Medications. Our patients receive a number of daily medications. This module assists with electronic tracking and documenting of required medications and treatments. This provides a more accurate and efficient care system for our nurses and patients. |
• | Wound Module. This allows for an evidence-based risk assessment to drive patient specific interventions to prevent skin breakdown. When skin abnormalities are present, it provides for accurate depiction of anatomical location and description which drives individualized care treatments. |
• | Incident Module. Allows for capturing any event, such as a fall, and provides quality assurance steps for root cause and patient-specific care plans. |
For all modules, the EMR system provides a dashboard that can be reviewed at a number of kiosks throughout the nursing center, allowing our staff to securely access a list of upcoming patient care tasks and providing supervisors a tool to help manage and monitor staff performance. We believe the EMR system provides better support, efficiency, and improves the quality of care for our patients. We originally invested approximately $112,000 per nursing center to deploy EMR in all our centers at the time of implementation. We currently implement EMR at each of the centers we acquire or at which time we assume operations during the transition process.
Organization. Our nursing centers are currently organized into ten regions, each of which is supervised by a regional vice president. The regional vice president is generally supported by specialists in several functions, including clinical, human resources, marketing, revenue cycle management and administration, all of whom are employed by us. The day-to-day operations of each of our nursing centers are led by an on-site, licensed administrator. The administrator of each nursing center is supported by other professional personnel, including a medical director, who assists in the medical management of the nursing center, and a director of nursing, who supervises a team of registered nurses, licensed practical nurses and nurse aides. Other personnel include those providing therapy, dietary, activities and social service, housekeeping, laundry, maintenance and office services. The majority of personnel at our nursing centers, including the administrators, are our employees.
4
Marketing.
We believe that skilled nursing care is fundamentally a local business in which both patients and their referral sources are typically based in the immediate geographic area in which the nursing center is located. Our marketing plan and related support activities emphasize the role and contributions of the administrators, admissions coordinators and clinical liaisons of each nursing center, all of whom are responsible for developing relationships with various referral sources such as doctors, hospitals, hospital case managers and discharge planners, and various healthcare and community organizations. Training, sales tools and job aids are provided for the sales and marketing teams for the product knowledge, market knowledge, and selling skills necessary to support their efforts in the field. As part of our business strategy, we have dedicated sales and marketing personnel who develop strong partnerships with physicians and hospital executives as well as Accountable Care Organizations ("ACO"), Bundled Payments for Care Improvement ("BPCI"), and Managed Care organizations. We believe these relationships will be mutually beneficial, providing the community with high quality healthcare while helping customers to navigate choices, manage transitions, and control costs.
At the local level, our sales and marketing efforts are designed to:
•Identify and develop strong healthcare partnerships
•Help facilitate smooth transitions between care settings
•Promote collaboration with ACOs, BPCIs, and healthcare organizations
•Educate referral sources and community on our key differentiators and capabilities
•Position ourselves as a valuable resource and healthcare partner
•Enhance the customer experience
•Contribute to a strong community presence
•Promote higher occupancy levels
•Foster optimal payor mix
In addition to soliciting admissions from current and potential referral sources, we emphasize involvement in community and healthcare events and opportunities to promote a public awareness of our nursing centers and services. Activities include ongoing family councils and community based “family night” functions, providing the opportunity to educate the public on various topics such as Medicare benefits, powers of attorney, and other topics of interest. We also promote a positive customer experience, best practices, strong surveys, and a high Star Rating; we seek feedback through third-party resident and family surveys. We host tour and “open house” opportunities, where members of the local community are invited to visit the center to see any improvements or to better understand our environment and services. We look for ways to offer increased clinical capabilities and services to better meet the needs of the community and referral sources. In addition, we have regional oversight to support the overall marketing strategies in each local center, in order to promote higher occupancy levels and improved payor and case mixes at our nursing centers. We offer the resources and metrics for strong healthcare partnerships with our referral sources, including ACOs and other Managed Care partners. Our support center marketing personnel support regional and local marketing personnel and efforts.
We have monthly marketing programs and ongoing marketing initiatives, developed internally, that focus on educating and meeting the needs of our customers while growing our business. Resources are also available to assist each nursing center administrator in analysis of local demographics and competition with a view toward complementary service development. We consider the primary referral area in long-term care to generally lie within a five-to-fifteen-mile radius of each nursing center depending on population density; consequently, we focus on local marketing efforts rather than broad-based advertising.
Acquisitions, Significant Transactions and Divestitures.
Acquisitions
Effective July 1, 2017, the Company acquired a 103-bed skilled nursing center in Selma, Alabama, for an aggregate purchase price of $8,750,000, pursuant to an Asset Purchase Agreement with Park Place Nursing and Rehabilitation Center, LLC, Dunn Nursing Home, Inc., Wood Properties of Selma LLC, and Homewood of Selma, LLC.
On February 26, 2016, the Company exercised its purchase options to acquire the real estate assets for Diversicare of Hutchinson in Hutchinson, Kansas and Clinton Place in Clinton, Kentucky for $4,250,000 and $3,300,000, respectively. The Company has operated these centers since February 2015 and April 2012, respectively. Hutchinson is an 85-bed skilled nursing center and Clinton is an 88-bed skilled nursing center.
Golden Living Transaction
On August 15, 2016, the Company entered into an Operation Transfer Agreement with Golden Living (the "Lessor") to assume the operations of 22 centers in Alabama and Mississippi. On October 1, 2016, the Company entered into a Master Lease Agreement (the "Lease") with Golden Living to directly lease 8 centers located in Mississippi from the Lessor. The Company also assumed
5
individual leases of two centers in Mississippi from third parties. On November, 1 2016, the Company amended and restated the Lease ("Amended Lease") with the Lessor to directly lease an additional twelve centers located in Alabama. Refer to the chart below for a complete listing of these centers' locations and number of licensed beds.
Lease Agreements and Assumption of Operations
During 2016, the Company assumed operations at 22 centers comprising a total increase of 2,574 licensed beds. The Company did not enter into any lease agreements to assume operations during 2017. See table below for details of the 2016 operations acquired by the Company:
Center | Location | Effective Date | Licensed Bed Count | |
Diversicare of Amory | Amory, Mississippi | October 1, 2016 | 152 | |
Diversicare of Batesville | Batesville, Mississippi | October 1, 2016 | 130 | |
Diversicare of Brookhaven | Brookhaven, Mississippi | October 1, 2016 | 58 | |
Diversicare of Carthage | Carthage, Mississippi | October 1, 2016 | 99 | |
Diversicare of Eupora | Eupora, Mississippi | October 1, 2016 | 119 | |
Diversicare of Meridian | Meridian, Mississippi | October 1, 2016 | 120 | |
Diversicare of Ripley | Ripley, Mississippi | October 1, 2016 | 140 | |
Diversicare of Southaven | Southaven, Mississippi | October 1, 2016 | 140 | |
Diversicare of Tupelo | Tupelo, Mississippi | October 1, 2016 | 120 | |
Diversicare of Tylertown | Tylertown, Mississippi | October 1, 2016 | 60 | |
Diversicare of Arab | Arab, Alabama | November 1, 2016 | 87 | |
Diversicare of Bessemer | Bessemer, Alabama | November 1, 2016 | 180 | |
Diversicare of Riverchase | Birmingham, Alabama | November 1, 2016 | 132 | |
Diversicare of Boaz | Boaz, Alabama | November 1, 2016 | 100 | |
Diversicare of Foley | Foley, Alabama | November 1, 2016 | 154 | |
Baron House of Hueytown | Hueytown, Alabama | November 1, 2016 | 50 | |
Diversicare of Lanett | Lanett, Alabama | November 1, 2016 | 85 | |
Diversicare of Montgomery | Montgomery, Alabama | November 1, 2016 | 138 | |
Diversicare of Oneonta | Oneonta, Alabama | November 1, 2016 | 120 | |
Diversicare of Oxford | Oxford, Alabama | November 1, 2016 | 173 | |
Diversicare of Pell City | Pell City, Alabama | November 1, 2016 | 94 | |
Diversicare of Winfield | Winfield, Alabama | November 1, 2016 | 123 | |
Lease Terminations
Effective September 30, 2017, the Company entered into an Agreement with Trend Health and Rehab of Carthage, LLC ("Trend Health") to terminate the lease and the Company's right of possession of the center in Carthage, Mississippi. In consideration of the early termination of the lease, Trend Health provided the Company with a $250,000 cash termination payment.
Effective May 31, 2016, the Company entered into an Agreement with Avon Ohio, LLC to amend the original lease agreement, thus terminating the Company's right of possession of the center. As a result, the Company incurred lease termination costs of $2,008,000 in the second quarter of 2016. Under the amended agreement, the Company is required to pay $300,000 per year through the term of the original lease agreement, July 31, 2024.
Under current accounting guidance, these transactions were not reported as discontinued operations, as the disposals did not represent a strategic shift that has (or will have) a major effect on the Company's operations and financial results.
Pharmacy Partnership
Effective October 28, 2016, the Company and its partners entered into an asset purchase agreement to sell the pharmacy joint venture. The sale resulted in a $1,366,000 gain in the fourth quarter of 2016. Subsequently, we recognized an additional gain of $733,000 in the first quarter of 2017, related to the continuing liquidation of remaining net assets affiliated with the partnership.
6
Nursing Center Industry.
We believe there are a number of significant trends within the post-acute care industry that will support the continued growth of the nursing center profession. These trends are also likely to impact our business. These factors include:
Demographic trends. The primary market for our post-acute health care services is comprised of persons aged 75 and older. This age group is one of the fastest growing segments of the United States population. As the number of persons aged 75 and over continues to grow, we believe that there will be corresponding increases in the number of persons who need skilled nursing care.
Cost containment pressures. In response to rapidly rising health care costs, governmental and other third-party payors have adopted cost-containment measures to reduce admissions and encourage reduced lengths of stays in hospitals and other acute care settings. As a result, hospitals are discharging patients earlier and referring elderly patients, who may be too sick or frail to manage their lives without assistance, to nursing centers where the cost of providing care is typically lower than hospital care.
Limited supply of centers. As the nation's population of seniors continues to grow, life expectancy continues to expand, and there continues to be limitations on granting Certificates of Need (“CON”) in most states for new skilled nursing centers, so we believe that there will be continued demand for skilled nursing beds in the markets in which we operate. CON laws generally require a state agency to determine public need for any construction or expansion of healthcare facilities. We believe that the CON process tends to restrict the supply and availability of licensed skilled nursing center beds. High construction costs, limitations on state and federal government reimbursement for the full costs of construction, and start-up expenses also act to restrict growth in the supply for such centers.
Reduced reliance on family care. Historically, the family has been the primary provider of care for seniors. We believe that the increase in the percentage of dual income families, the reduction of average family size and the increased mobility in society will reduce the role of the family as the traditional care-giver for aging parents. We believe that this trend will make it necessary for many seniors to look outside the family for assistance as they age.
Competition.
The post-acute care business is highly competitive. We face direct competition for additional centers, and our centers face competition for employees and patients. Some of our present and potential competitors for acquisitions are significantly larger and have or may obtain greater financial and marketing resources. Competing companies may offer new or more modern centers or new or different services that may be more attractive to patients than some of the services we offer.
The nursing centers operated by us compete with other centers in their respective markets, including rehabilitation hospitals and other skilled and personal care residential centers. In the few urban markets in which we operate, some of the long-term care providers with which our centers compete are significantly larger and have or may obtain greater financial and marketing resources than our centers. Some of these providers are not-for-profit organizations with access to sources of funds not available to our centers. Construction of new long-term care centers near our existing centers could adversely affect our business. We believe that the most important competitive factors in the long-term care business are: a nursing center's local reputation with referral sources, such as acute care hospitals, physicians, religious groups, other community organizations, Managed Care organizations, and a patient's family and friends; physical plant condition; the ability to identify and meet particular care needs in the community; the availability of qualified personnel to provide the requisite care; and the rates charged for services. There is limited, if any, price competition with respect to Medicaid and Medicare patients, since revenues for services to such patients are strictly controlled and are based on fixed rates and cost reimbursement principles. Although the degree of success with which our centers compete varies from location to location, we believe that our centers generally compete effectively with respect to these factors.
7
Revenue Sources
We classify our revenues earned from patients and residents into four major categories: Medicaid, Medicare, managed care, and private pay and other. Medicaid revenues are those received under the traditional Medicaid program, which provides benefits to those in need of financial assistance in the securing of medical services. Medicare revenues include revenues received under both Part A and Part B. Managed Care revenues are received from insurance entities, including third-party plans that administer Medicare benefits, known as Medicare Advantage plans. The private pay and other revenues are composed primarily of individuals or parties who directly pay for their services. Included in the private pay and other category are patients who are hospice beneficiaries as well as the recipients of Veterans Administration benefits. Veterans Administration payments are made pursuant to renewable contracts negotiated with these payors.
The following table sets forth net patient revenues related to our continuing operations by payor source for the periods presented (dollar amounts in thousands):
Year Ended December 31, | ||||||||||||||||||||
2017 | 2016 | 2015 | ||||||||||||||||||
Medicaid | $ | 300,926 | 52.4 | % | $ | 215,381 | 50.6 | % | $ | 188,323 | 48.6 | % | ||||||||
Medicare | 149,020 | 25.9 | % | 117,143 | 27.5 | % | 112,305 | 29.0 | % | |||||||||||
Managed Care | 42,673 | 7.4 | % | 29,066 | 6.8 | % | 27,856 | 7.2 | % | |||||||||||
Private Pay and other | 82,175 | 14.3 | % | 64,473 | 15.1 | % | 59,111 | 15.2 | % | |||||||||||
Total | $ | 574,794 | 100.0 | % | $ | 426,063 | 100.0 | % | $ | 387,595 | 100.0 | % | ||||||||
The following table sets forth average daily skilled nursing census, or average number of patients per day, by payor source for our continuing operations for the periods presented:
Year Ended December 31, | |||||||||||||||||
2017 | 2016 | 2015 | |||||||||||||||
Medicaid | 4,681 | 69.1 | % | 3,448 | 68.1 | % | 3,104 | 67.1 | % | ||||||||
Medicare | 760 | 11.2 | % | 591 | 11.7 | % | 577 | 12.5 | % | ||||||||
Managed Care | 265 | 3.9 | % | 178 | 3.5 | % | 173 | 3.7 | % | ||||||||
Private Pay and other | 1,072 | 15.8 | % | 844 | 16.7 | % | 772 | 16.7 | % | ||||||||
Total | 6,778 | 100.0 | % | 5,061 | 100.0 | % | 4,626 | 100.0 | % | ||||||||
Consistent with the nursing center industry in general, changes in the mix of a center's patient population among Medicaid, Medicare, Managed Care, and private pay and other can significantly affect the profitability of the center's operations. We will attempt to increase revenues from non-governmental sources to the extent capital is available to do so. However, private payors, including managed care payors, are increasingly demanding that providers accept discounted fees or assume all or a portion of the financial risk for the delivery of health care services. Such measures may include capitated payments, which can result in significant losses to health care providers if patients require expensive treatment not adequately covered by the capitated rate.
Medicare and Medicaid Reimbursement
A significant portion of our revenues are derived from government-sponsored health insurance programs, primarily Medicare and Medicaid. We employ third-party specialists in reimbursement and also use these services to monitor regulatory developments to comply with reporting requirements and to ensure that proper payments are made to our operated nursing centers.
Medicare
Medicare is a federally-funded and administered health insurance program for the aged and for certain chronically disabled individuals. Part A of the Medicare program covers certain services furnished by skilled nursing centers and other institutional providers and inpatient hospital services. Part B covers physician services, durable medical equipment, various outpatient services and certain ancillary services. Medicare generally covers skilled nursing center services for beneficiaries who require nursing care or rehabilitation services after a qualifying hospital stay. Medicare pays a per diem rate for each beneficiary, adjusted for patient acuity and additional factors such as geographic differences in wage rates. The payment rates are set forth under a prospective payment system that uses nursing and therapy indexes to assign a payment rate to each beneficiary. The Centers for Medicare &
8
Medicaid Services (“CMS”) updates the rates annually. The payment rates cover all services to be provided to a beneficiary, including room and board, skilled nursing care, therapy, and medications.
In August 2017, CMS issued its final rule outlining Medicare payment rates and policies for skilled nursing centers for federal fiscal year 2018, which began October 1, 2017. CMS projects that aggregate payments to skilled nursing centers will increase by a net 1.0% for federal fiscal year 2018. This reflects a 1.0% market basket increase, as required by the Medicare Access and CHIP Reauthorization Act of 2015 (“MACRA”). The payment rates for federal fiscal year 2017, which were projected to increase aggregate payments to skilled nursing centers by 2.4%, reflected a 2.7% market basket increase with a 0.3 percentage point productivity reduction required by the Patient Protection and Affordable Care Act, as amended by the Health Care and Education Reconciliation Act of 2010 (collectively, “Affordable Care Act”).
In addition to the adjustments described above, payment rates are reduced pursuant to ongoing sequestration. The Budget Control Act of 2011 (“BCA”) requires automatic spending reductions to reduce the federal deficit, including Medicare spending reductions of up to 2% per fiscal year, with a uniform percentage reduction across all Medicare programs. CMS began imposing a 2% reduction on Medicare claims in April of 2013. These reductions have been extended through 2027.
CMS has increasingly introduced policies intended to shift Medicare to value-based payment methodologies, tying reimbursement to quality of care rather than quantity. For example, CMS has implemented the Quality Reporting Program, under which skilled nursing centers are required to report quality data. Beginning in federal fiscal year 2018, skilled nursing centers that fail to submit required data will be subject to a 2% reduction to the annual market basket update. Beginning in federal fiscal year 2019, the Skilled Nursing Facility Value-Based Purchasing (“SNF VBP”) Program will make incentive payments available to skilled nursing centers based on their past performance on a specified quality measure related to hospital readmissions. CMS will fund the SNF VPB Program incentive payment pool by withholding 2% of skilled nursing center payments and then redistributing the withheld payments. Data from the calendar year 2017 performance period will be used to calculate incentive payments for federal fiscal year 2019; data from the federal fiscal year 2018 performance period will be used to calculate incentive payments for federal fiscal year 2020. CMS will publish rankings based on performance scores on the Nursing Home Compare website beginning in 2018.
The Nursing Home Compare website is intended to assist the public in finding and comparing skilled care providers. Under the Five-Star Quality Rating System, each nursing home is given a rating between 1 and 5 stars, which is published on the Nursing Home Compare website. An overall star rating is determined based on three components (information from the last three years of health inspections, staffing information, and quality measures), each of which also has its own five-star rating. The ratings are based, in part, on the quality data nursing centers are required to report. For example, nursing centers must report the percentage of short-stay residents who are successfully discharged into the community and the percentage who had an outpatient emergency department visit. We remain diligent in continuing to provide outstanding patient care to achieve high rankings for our centers, as well as assuring that our rankings are correct and appropriately reflect our quality results.
MACRA required the establishment of the Quality Payment Program (“QPP”), a payment methodology intended to reward high-quality patient care. Beginning in 2017, physicians and certain other clinicians are required to participate in one of two QPP tracks. Under both tracks, performance data collected in 2017 will affect Medicare payments in 2019, and performance data collected in 2018 will affect Medicare payments in 2020. The Advanced Alternative Payment Model (“Advanced APM”) track makes incentive payments available for participation in specific innovative payment models approved by CMS. A provider with sufficient participation in an Advanced APM is exempt from the reporting requirements and payment adjustments imposed under the second track, the Merit-Based Incentive Payment System (“MIPS”). Providers electing to participate in MIPS will receive either payment incentives or be subject to payment reductions based on their performance with respect to clinical quality, resource use, clinical improvement activities, and meaningful use of electronic health records. MIPS consolidates components of previously established incentive programs, including the Value-Based Payment Modifier program and the Physician Quality Reporting System.
Therapy Services. Reimbursement for physical therapy, occupational therapy, and speech-language pathology services covered under Medicare Part B is determined according to the Medicare Physician Fee Schedule ("MPFS"), which is updated annually. Under MACRA, the MPFS reimbursement rate increases 0.5% in calendar year 2018. If a beneficiary receives multiple therapy treatments in one day, Medicare Part B pays the full rate for the therapy unit of service that has the highest Practice Expense ("PE") component. A multiple procedure payment reduction is applied to the second and subsequent therapy units, reducing reimbursement to 50% of the applicable PE component.
The Bipartisan Budget Act of 2018 repealed the annual per-beneficiary payment limits on therapy services covered under Medicare Part B for services provided after December 31, 2017. Instead, targeted medical reviews will be performed when expenses for a beneficiary exceed a threshold of $3,000 for physical and speech therapy services combined or $3,000 for occupational therapy services alone. Deductible and coinsurance amounts paid by the beneficiary for therapy services count toward the amount applied to the limit. Claims above the threshold may be subject to post-payment review of medical necessity documentation by Supplemental Medical Review Contractors.
9
10
Medicaid
Medicaid is a medical assistance program for the indigent that is funded jointly by the federal and state governments and administered by the states. Federal law requires states to cover certain nursing center services for Medicaid-eligible individuals when other payment options are unavailable. However, Medicaid eligibility requirements and benefits vary by state, and states may impose limitations on nursing services. States may also establish levels of service or payment methodologies by acuity or specialization of a nursing center.
The Affordable Care Act, as currently structured, requires states to expand Medicaid coverage by adjusting eligibility requirements such as income thresholds. However, the Presidential administration and certain members of Congress continue to attempt to repeal or significantly modify the Affordable Care Act, which may result in changes to Medicaid. Further, states may opt out of the Medicaid expansion. Some states use or have applied to use waivers granted by CMS to implement expansion, impose different eligibility or enrollment restrictions, or otherwise implement programs that vary from federal standards.
For example, effective February 1, 2015, the Company began participating in Indiana's Upper Payment Limit ("UPL") supplemental payment program, which provides supplemental Medicaid payments for skilled nursing centers that are licensed to non-state government entities such as county hospital districts. One skilled nursing center previously operated by the Company entered into a transaction with one such hospital district participating in the UPL program, providing for the transfer of the license from the Company to the hospital district. The Company's operating subsidiary retained the management of the center on behalf of the hospital district. The agreement between the hospital district and the Company is terminable by either party.
We receive the majority of our annual Medicaid rate increases during the third quarter of each year. The rate changes received in 2017 and 2016, along with increased Medicaid acuity in our acuity based states, were the primary contributor to our 3.3% increase in average rate per day for Medicaid patients in 2017 compared to 2016. Based on the rate changes received during the third quarter of 2017, we expect a favorable impact to our rate per day for Medicaid patients as we move into 2018 due to modest rate increases in many of the states within which we operate.
Several states in which we operate face budget shortfalls, which could result in reductions in Medicaid funding for nursing centers. Pressures on state budgets are expected to continue in the future. Certain of the states in which we operate are actively seeking ways to reduce Medicaid spending for nursing center care by such methods as capitated payments and substantial reductions in reimbursement rates. Some states are promoting alternatives such as community and home-based services. CMS administrators have indicated that they intend to increase state flexibility in the administration of Medicaid programs. We are unable to predict what, if any, reform proposals or reimbursement limitations will be implemented in the future, or the effect such changes would have on our operations. For the year ended December 31, 2017, we derived 25.9% and 52.4% of our total patient revenues related to continuing operations from the Medicare and Medicaid programs, respectively. Any health care reforms that significantly limit rates of reimbursement under these programs could, therefore, have a material adverse effect on our financial position and profitability.
Employees.
As of February 2, 2018, we employed approximately 8,800 employees, referred to as "team members," in connection with our continuing operations, approximately 6,300 of which are considered full-time team members. We believe that our team member relations are good. Approximately 842 of our team members are represented by a labor union.
Although we believe we are able to employ sufficient nurses and therapists to provide our services, a shortage of health care professional personnel in any of the geographic areas in which we operate could affect our ability to recruit and retain qualified team members and could increase our operating costs. We compete with other health care providers for both professional and non-professional team members and with non-health care providers for non-professional team members. This competition contributed to a significant increase in the salaries that we had to pay to hire and retain these team members. As is common in the health care industry, we expect the salary and wage increases for our skilled healthcare providers will continue to be higher than average salary and wage increases nationally.
Supplies and Equipment.
We purchase drugs, solutions and other materials and lease certain equipment required in connection with our business from many suppliers. We have not experienced, and do not anticipate that we will experience, any significant difficulty in purchasing supplies or leasing equipment from current suppliers. In the event that such suppliers are unable or fail to sell us supplies or lease equipment, we believe that other suppliers are available to adequately meet our needs at comparable prices. National purchasing contracts are in place for all major supplies, such as food, linens and medical supplies. These contracts assist in maintaining quality, consistency and efficient pricing. Based on contract pricing for food and other supplies, we expect cost increases in 2018 to be relatively the same or slightly lower than the increases we experienced in 2017.
11
Government Regulation.
The health care industry is subject to numerous laws and regulations of federal, state and local governments. These laws and regulations include, but are not necessarily limited to, matters such as licensure, accreditation, government health care program participation requirements, reimbursement for patient services, quality of patient care and Medicare and Medicaid fraud and abuse. Over the last several years, government activity has increased with respect to investigations and allegations concerning possible violations by health care providers of a number of statutes and regulations, including those regulating fraud and abuse, false claims , patient privacy and quality of care issues. Violations of these laws and regulations could result in exclusion from government health care programs together with the imposition of significant fines and penalties, as well as significant repayments for patient services previously billed. Compliance with such laws and regulations is subject to ongoing government review and interpretation, as well as regulatory actions in which government agencies seek to impose fines and penalties. The Company is involved in regulatory actions of this type from time to time.
Licensure and Certification.
All our nursing centers must be licensed by the state in which they are located in order to accept patients, regardless of payor source. In most states, nursing centers are subject to Certificate of Need ("CON") laws, which require us to obtain government approval for the construction of new nursing centers or the addition of new licensed beds to existing centers. Our nursing centers must comply with detailed statutory and regulatory requirements on an ongoing basis in order to qualify for licensure, as well as for certification as a provider eligible to receive payments from the Medicare and Medicaid programs. Generally, the requirements for licensure and Medicare/Medicaid certification are similar and relate to quality and adequacy of personnel, quality of medical care, record keeping, dietary services, patient rights, and the physical condition of the nursing center and the adequacy of the equipment used therein. Failure to comply with applicable laws and regulations could result in exclusion from the Medicare and Medicaid programs, which could have an adverse impact on our business, financial condition, or results of operations.
In 2016, CMS published a comprehensive update to the health and safety standards applicable to long-term care facilities participating in the Medicare or Medicaid programs. These revisions are aimed at improving quality of life, care and services in long-term care facilities, optimizing resident safety, and reflecting current professional standards. For example, CMS added requirements related to infection prevention and control, compliance and ethics programs, staff training. and QAPI programs. To allow facilities time to achieve compliance, CMS is implementing the requirements in three phases, over a three year period. We are in substantial compliance with the Phase 1 and Phase 2 requirements, and expect to be in substantial compliance with the Phase 3 requirements by the deadline of November 28, 2019. The total costs associated with implementing the requirements is not known at this time.
Each center is subject to periodic inspections, known as “surveys” by health care regulators, to determine compliance with all applicable licensure and certification standards. Such requirements are both subjective and subject to change. If the survey concludes that there are deficiencies in compliance, the center is subject to various sanctions, including but not limited to monetary fines and penalties, suspension of new admissions, non-payment for new admissions and loss of licensure or certification. Generally, however, once a center receives written notice of any compliance deficiencies, it may submit a written plan of correction and is given a reasonable opportunity to correct the deficiencies. There can be no assurance that, in the future, we will be able to maintain such licenses and certifications for our centers or that we will not be required to expend significant sums in order to comply with regulatory requirements.
Health care and health insurance reform.
In recent years, the U.S. Congress and some state legislatures have considered and enacted significant legislation concerning health care and health insurance. The most prominent of these efforts, The Affordable Care Act affects how health care services are covered, delivered and reimbursed. As currently structured, the Affordable Care Act expands coverage through a combination of public program expansion and private sector reforms, provides for reduced growth in Medicare program spending, and promotes initiatives that tie reimbursement to quality and care coordination. Some of the provisions, such as the requirement that large employers provide health insurance benefits to full-time employees, have increased our operating expenses. The Affordable Care Act expands the role of home-based and community services, which may place downward pressure on our sustaining population of Medicaid patients. Reforms that we believe may have a material impact on the long-term care industry and on our business include, among others, possible modifications to the conditions of qualification for payment, bundling of payments to cover both acute and post-acute care and the imposition of enrollment limitations on new providers. However, there is considerable uncertainty regarding the future of the Affordable Care Act. The Presidential administration and certain members of Congress have expressed
their intent to repeal or make significant changes to the law, its implementation or its interpretation. For example, in 2017, Congress eliminated the financial penalty associated with the individual mandate, effective January 1, 2019.
Skilled nursing centers are required to bill Medicare on a consolidated basis for certain items and services that they furnish to patients, regardless of the cost to deliver these services. This consolidated billing requirement essentially makes the skilled nursing center responsible for billing Medicare for all care services delivered to the patient during the length of stay. CMS has instituted a number of test programs designed to extend the reimbursement and financial responsibilities under consolidated billing beyond the traditional discharge date to include a broader set of bundled services. Such examples may include, but are not exclusive to, home health, durable medical equipment, home and community based services, and the cost of re-hospitalizations during a specified bundled period. Currently, these test programs for bundled reimbursement are confined to a small set of clinical conditions, but CMS has indicated that it is developing additional bundled payment models. This bundled form of reimbursement could be extended to a broader range of diagnosis related conditions in the future. The potential impact on skilled nursing center utilization and reimbursement is currently unknown. The process for defining bundled services has not been fully determined by CMS and therefore is subject to change during the rule making process.
Health Insurance Portability and Accountability Act of 1996 Compliance.
The Health Insurance Portability and Accountability Act of 1996 (“HIPAA”) has mandated an extensive set of regulations to standardize electronic patient health, administrative and financial data transactions and to protect the privacy of individually identifiable health information. We have a HIPAA compliance committee and designated privacy and security officers.
The HIPAA transaction standards are intended to simplify the electronic claims process and other healthcare transactions by encouraging electronic transmission rather than paper submission. These regulations provide for uniform standards for data reporting, formatting and coding that we must use in certain transactions with health plans. The HIPAA security regulations establish requirements for safeguarding protected health information that is electronically transmitted or electronically stored. Some of the security regulations are technical in nature, while others are addressed through policies and procedures.
The HIPAA regulations related to privacy establish comprehensive federal standards relating to the use and disclosure of individually identifiable health information (“protected health information”). The privacy regulations establish limits on the use and disclosure of protected health information, provide for patients' rights, including rights to access, to request amendment of, and to receive an accounting of certain disclosures of protected health information, and require certain safeguards for protected health information. In addition, each covered entity must contractually bind individuals and entities that furnish services to the covered entity or perform a function on its behalf, and to which the covered entity discloses protected health information, to restrictions on the use and disclosure of that protected health information. In general, the HIPAA regulations do not supersede state laws that are more stringent or grant greater privacy rights to individuals. Thus, we must reconcile the HIPAA regulations and other state privacy laws.
Although we believe that we are in material compliance with these HIPAA regulations, inadvertent violations of these regulations may occur in the course of our business. For this and other reasons, the HIPAA regulations are expected to continue to impact us operationally and financially and may pose increased regulatory risk.
Self-Referral and Anti-Kickback Legislation.
The health care industry is subject to state and federal laws that regulate the relationships of providers of health care services, physicians and other clinicians. These self-referral laws impose restrictions on physician referrals to any entity with which they have a financial relationship, which is a broadly defined term. We believe our relationships with physicians are in compliance with the self-referral laws. Failure to comply with self-referral laws could subject us to a range of sanctions, including civil monetary penalties and possible exclusion from government reimbursement programs. There are also federal and state laws making it illegal to offer anyone anything of value in return for referral of patients. These laws, generally known as “anti-kickback” laws, are broad and subject to interpretations that are highly fact dependent. Given the lack of clarity of these laws, there can be no absolute assurance that any health care provider, including us, will not be found in violation of the anti-kickback laws in any given factual situation. Strict sanctions, including fines and penalties, exclusion from the Medicare and Medicaid programs and criminal penalties, may be imposed for violation of the anti-kickback laws.
Reporting Obligations under Section 111 of the Medicare, Medicaid and SCHIP Extension Act of 2007 (“MMSEA”).
The MMSEA expanded the Medicare Secondary Reporting Act. Since January 1, 2010, we have reported specific information regarding all claimants and claim settlements involving Medicare participants so CMS can recover Medicare funds expended to provide healthcare treatment to the claimant. The requirements are to ensure that CMS is notified so that it may recoup the amounts paid for services from the settlement proceeds. This does not result in us making additional payments to CMS for these services
12
provided and does not result in an incremental cost to us. Strict sanctions, including fines and penalties, exclusion from the Medicare and Medicaid programs and criminal penalties, may be imposed for non-compliance with these reporting obligations.
Available Information.
We file reports with the Securities and Exchange Commission (“SEC”), including annual reports on Form 10-K, quarterly reports on Form 10-Q, and current reports on Form 8-K. Copies of our reports filed with the SEC may be obtained by the public at the SEC's Public Reference Room located at 100 F Street, NE, Washington, DC 20549 on official business days during the hours of 10 a.m. to 3 p.m. The public may obtain information on the operation of the Public Reference Room by calling the SEC at 1-800-SEC-0330. The SEC also maintains electronic versions of the Company's reports on its website at www.sec.gov. We also make available, free of charge through our website, our annual reports on Form 10-K, quarterly reports on Form 10-Q, current reports on Form 8-K, and other materials filed with the SEC as soon as reasonably practical after such material is electronically filed with or furnished to the SEC via a link to the SEC's EDGAR system. Our website address is www.dvcr.com. The information provided on our website is not part of this report, and is therefore not incorporated by reference unless such information is otherwise specifically referenced elsewhere in this report.
In addition, copies of the Company's annual report will be made available, free of charge, upon written request.
Corporate Governance Principles.
The Company has adopted Corporate Governance Principles relating to the conduct and operations of the Board of Directors. The Corporate Governance Principles are posted on the Company's website (www.dvcr.com) and are available in print to any stockholder who requests a copy.
Committee Charters.
The Board of Directors has an Audit Committee, Compensation Committee, Corporate Governance Committee, Risk Management Committee, and Executive Committee. The Board of Directors has adopted written charters for each committee, except for the Executive Committee, which are posted on the Company's website (www.dvcr.com) and are available in print to any stockholder who requests a copy.
ITEM 1A. RISK FACTORS
There have been a number of material developments both within the Company and the long-term care industry. These developments have had and are likely to continue to have a material impact on us. This section summarizes these developments, as well as other risks that should be considered by our shareholders and prospective investors.
Risks Related to our Operations
We are substantially self-insured and have significant potential professional liability exposure.
The provision of health care services entails an inherent risk of liability. Participants in the health care industry are subject to an increasing number of lawsuits alleging malpractice, negligence, product liability or related legal theories, many of which involve large claims and significant defense costs. Like many other companies engaged in the long-term care profession in the United States, we have numerous pending liability claims, disputes and legal actions for professional liability and other related issues. We expect to continue to be subject to such suits as a result of the nature of our business. We have professional liability insurance coverage for our nursing centers that, based on historical claims experience, is likely to be substantially less than the amount required to satisfy claims that are expected to be incurred. See “Item 3. Legal Proceedings” for further descriptions of pending claims and see “Item 7. Management's Discussion and Analysis of Financial Condition - Accounting Policies and Judgments - Professional Liability and Other Self-Insurance Reserves” for discussion of our reserve for self-insured claims and of our ability to meet our anticipated cash needs.
We may have substantial adjustments to our accrual for professional liability claims which could cause significant changes in our net earnings.
Each year, we record adjustments to our accrual for self-insured risks associated with professional liability claims. While these adjustments to the accrual result in changes to reported expenses and income, they are not directly related to changes in cash because the accrual is not funded. These self-insurance reserves are assessed on a quarterly basis, with changes in estimated losses being recorded in the consolidated statements of operations in the period identified. Any increase in the accrual decreases income in the period, and any reduction in the accrual increases income during the period. Our actual professional liabilities may vary significantly from the accrual due to an increase in the number of claims asserted or claim costs in excess of estimates, and the amount of the accrual has and may continue to fluctuate by a material
13
amount in any given quarter. For the years ended December 31, 2017, 2016 and 2015, we recorded professional liability expense of $10.8 million, $8.5 million and $8.1 million, respectively.
Our outstanding indebtedness is subject to various financial covenants and floating rates of interest which could be subject to fluctuations based on changing interest rates.
We have long-term indebtedness of $88.1 million at December 31, 2017. Certain of our debt agreements contain various financial covenants, the most restrictive of which relate to minimum cash deposits, cash flow and debt service coverage ratios. As of December 31, 2017, we were in compliance with these financial covenants. Our failure to comply with those covenants could result in an event of default, which, if not cured or waived, could result in the acceleration of some or all of our debts. Such non-compliance could result in a material adverse impact to our financial position, results of operations and cash flows. See “Item 7. Management's Discussion and Analysis of Financial Condition and Results of Operations - Liquidity and Capital Resources” for additional discussion of our covenants.
In connection with the refinancing transaction in February 2016 discussed in “Item 7. Management's Discussion and Analysis of Financial Condition and Results of Operations - Liquidity and Capital Resources,” we entered into an interest rate swap with respect to a portion of the mortgage loan to mitigate the floating interest rate risk of such borrowing. The interest rate swap converted the variable rate on our mortgage indebtedness to a fixed interest rate for the five year term of this indebtedness, decreasing our exposure to risks of variable rates of interest. While limiting our risk to increases in interest rates by utilizing the interest rate swap, we forgo benefits that might result from downward fluctuations in interest rates. We also are exposed to the risk that our counterpart to the swap agreement will default on its obligations.
Our accrual for professional liability claims is not funded, and if a material judgment is entered against us in any lawsuit, we may lack adequate cash to pay the judgment.
As of December 31, 2017, we are engaged in 72 professional liability lawsuits. Although we work diligently to limit the cash required to settle and defend professional liability claims, a significant judgment entered against us in one or more legal actions could have a material adverse impact on our cash flows and could result in our being unable to meet all of our cash needs as they become due.
The U.S. Department of Justice has commenced an investigation of our practices related to the provision of therapy and the completion of certain resident admission forms, which could adversely affect our operations and financial condition.
Our business is currently under investigation for potential civil and criminal violations of the federal False Claims Act ("FCA") and other laws governmental health care benefit programs. See Legal Proceedings for further information regarding this investigation. Any finding that we are not in compliance with these laws could require us to change our operations or could subject us to treble damages, penalties and/or make us ineligible to participate in certain government funded healthcare programs, any of which could in turn significantly harm our business and financial condition.
Our operational and strategic flexibility is limited due to the number of our centers that are leased from third parties.
A substantial majority of our centers are leased from third parties. The loss or deterioration of our relationship with any of our landlords may adversely affect our business. The terms of such leases generally require us to operate such centers as skilled nursing centers, and generally do not allow us to assign the lease to a third party without the applicable landlord’s consent. Therefore, our ability to divest such leased properties is limited, and we may be forced to continue operating such centers as skilled nursing centers even if doing so becomes unprofitable.
While we expect to renew or extend our leases in the normal course of business, there can be no assurance that these rights will be exercised in the future or that we will be able to satisfy the conditions precedent to exercising any such renewal or extension, to the extent that such provisions exist in our leases. In addition, if we are unable to renew or extend any of our master leases, we may lose all of the facilities subject to that master lease agreement. If we are not able to renew or extend our leases at or prior to the end of the existing lease terms, or if the terms of such options are unfavorable or unacceptable to us, our business, financial condition and results of operation could be adversely affected.
14
Our failure to pay rent or otherwise comply with the provisions of any of our Master Lease Agreements could materially adversely affect our business, financial position, results of operations, and liquidity.
Many of our facilities are under a Master Lease Agreement. Our failure to pay the rent or otherwise comply with the provisions of any of our lease agreements could result in an “event of default” under such lease agreement and also could result in a cross default under other master lease agreements and the agreements for our indebtedness. Upon an event of default, remedies available to our landlords generally include, without limitation, terminating such lease agreement, repossessing and reletting the leased properties and requiring us to remain liable for all obligations under such lease agreement, including the difference between the rent under such lease agreement and the rent payable as a result of reletting the leased properties, or requiring us to pay the net present value of the rent due for the balance of the term of such lease agreement. The exercise of such remedies would have a material adverse effect on our business, financial position, results of operations and liquidity. An event of default under any of our Master Lease Agreements could result in a default under the Credit Facilities and, if repayment of the borrowings under the Credit Facilities were accelerated, the payments under the indentures governing our outstanding notes could also be accelerated. The exercise of remedies by any of our landlords could have a material adverse effect on our business, financial position, results of operations, and liquidity.
We are highly dependent on reimbursement by third-party payors and delays in reimbursement for any reason may cause liquidity problems.
Substantially all of our nursing center revenues are directly or indirectly dependent upon reimbursement from third-party payors, including the Medicare and Medicaid programs and private insurers. For the year ended December 31, 2017, our patient revenues from continuing operations derived from Medicaid, Medicare, Managed Care and private pay (including private insurers) sources were approximately 52.4%, 25.9%, 7.4%, and 14.3%, respectively. Changes in the mix of our patients among Medicare, Medicaid, Managed Care and private pay categories and among different types of private pay sources may affect our net revenues and profitability. Our net revenues and profitability are also affected by the continuing efforts of all payors to contain or reduce the costs of health care. Efforts to impose reduced payments, greater discounts and more stringent cost controls by government and other payors are expected to continue.
The federal government makes frequent changes to the reimbursement provided under the Medicare program. Future changes to payment rates or methodology could significantly reduce the reimbursement we receive. Also, a number of state governments, including several of the states in which we operate, face projected budget shortfalls and/or deficit spending situations. Because Medicaid is typically a substantial part of a state’s budget, many states are considering or have implemented strategies to reduce Medicaid spending or decrease spending growth. Some states are exploring or implementing alternatives to traditional long-term care, including community and home-based nursing services.
Any changes in reimbursement levels or in the timing of payments under Medicare, Medicaid or private pay programs and any changes in applicable government regulations could have a material adverse effect on our net revenues, net income (loss) and cash flows. We are limited in our ability to reduce the direct costs of providing care. We are unable to predict the nature and success of future financial or delivery system reforms or the effect such changes will have on our operations. No assurance can be given that such reforms will not have a material adverse effect on us. See “Item 1. Business - Government Regulation and Reimbursement.”
If we have problems with our information systems that affect payment or if other issues arise with Medicare, Medicaid or other payors that affect the amount or timeliness of reimbursements, we may encounter delays in our payment cycle. Any significant payment timing delay could cause us to experience working capital shortages. Working capital management, including prompt and diligent billing and collection, is an important factor in our consolidated results of operations and liquidity. Our working capital management procedures may not successfully mitigate the effects of any delays in our receipt of payments or reimbursements. Accordingly, such delays could have an adverse effect on our liquidity and financial condition.
We operate in an industry that is highly competitive.
The long-term care industry generally, and the nursing home business particularly, is highly competitive. We face direct competition for the acquisition of centers. In turn, our centers face competition for patients. Our ability to compete is based on several factors including, but not limited to, building age and appearance, reputation, relationships with referral sources, availability of patients, survey history and CMS rankings. Some of our present and potential competitors are significantly larger and have or may obtain greater financial and marketing resources than we can. In addition, some competitors are implementing vertical alignment strategies. For example, some hospitals provide long-term care services and some providers are aligned or are pursuing alignment strategies with payors. Certain of our competitors are operated by not-for-profit, non-taxpaying or governmental agencies that can finance capital expenditures on a tax exempt basis
15
and receive funds and charitable contributions unavailable to us. In addition, we may encounter substantial competition from new market entrants. Consequently, there can be no assurance that we will not encounter increased competition in the future, which could limit our ability to attract patients or expand our business, and could materially and adversely affect our business or decrease our market share.
We may have difficulty attracting and retaining qualified nurses, therapists, healthcare professionals and other key personnel, which, along with a growing number of minimum wage and compensation related regulations, may increase our costs related to these employees.
Our team members are essential to our business. We rely on our ability to attract and retain qualified nurses, therapists and other healthcare professionals. The market for these key personnel is highly competitive, and we could experience significant increases in our operating costs due to shortages in their availability. Like other healthcare providers, we have at times experienced difficulties in attracting and retaining qualified personnel. We may continue to experience increases in our labor costs, primarily due to higher wages and greater benefits required to attract and retain qualified healthcare personnel, and such increases may adversely affect our profitability. Furthermore, while we attempt to manage overall labor costs in the most efficient way, our efforts to manage them through wage freezes and similar means may have limited effectiveness and may lead to increased turnover and other challenges.
Tight labor markets and high demand for such team members can contribute to high turnover among clinical professional staff. A shortage of qualified personnel at a facility could result in significant increases in labor costs and increased reliance on overtime and expensive temporary staffing agencies, and could otherwise adversely affect operations at the affected centers. If we are unable to attract and retain qualified professionals, our ability to adequately provide services to our residents and patients may decline and our ability to grow may be constrained.
Our cost of labor may be influenced by unanticipated factors in certain markets or, with respect to collective bargaining agreements that we are a party to, we may experience above-market increases. A substantial number of our team members are hourly team members whose wage rates are affected by increases in the federal or state minimum wage rate. As collective bargaining agreements are renegotiated or minimum wage rates increase we may need to increase the wages paid to team members. This may be applicable to not only minimum wage team members but also to team members at wage rates which are currently above the minimum wage.
The Department of Labor issued rule changes to the Fair Labor Standards Act that increased the minimum salary threshold for team members exempt from overtime along with an automatic annual increase to this salary threshold. The future of these rule changes, as well as other potential changes, remains uncertain given the recent change in Presidential administrations. However, these rule changes could increase our cost of services provided.
Because we are largely funded by government programs according to predetermined, nonnegotiable rates, we do not have an ability to pass such wage increases through to revenue sources. Any such mandated wage increases could have a material adverse effect on our results of operations, liquidity and financial condition.
Possible changes in the acuity of residents and patients, as well as payor mix and payment methodologies, may significantly affect our profitability.
The sources and amount of our revenues are determined by a number of factors, including the occupancy rates of our facilities, the length of stay, the payor mix of residents and patients, rates of reimbursement, and patient acuity. Changes in patient acuity as well as payor mix among private pay, Medicare, and Medicaid may significantly affect our profitability. In particular, any significant decrease in our population of high-acuity patients or any significant increase in our Medicaid population could have a material adverse effect on our business, financial position, results of operations, and liquidity, especially if state Medicaid programs continue to limit, or more aggressively seek limits on, reimbursement rates or service levels.
Our systems are subject to security breaches and other cybersecurity incidents.
While we maintain information technology security and safeguards, complex medical systems have been and may continue to be targeted for cyber attacks, which may result in unauthorized parties obtaining access to our computer systems and networks. Cyber attacks could result in the misappropriation of our patient information that is protected by law, private employee information, proprietary business information and technology or result in interruptions to our business. The reliability and security of our information technology infrastructure is critical to our business. To the extent that any disruptions or security breaches result in significant loss or damage to our data, or inappropriate use or disclosure of patient, employee or proprietary information, we could be required to notify affected individuals, state and federal agencies and the media of the breach, could experience damage to our reputation and patient relationships and be subject to civil
16
and/or criminal fines and penalties or related class action litigation, any of which could have a material adverse effect on our business, results of operations and financial condition.
The success of previous and future acquisitions cannot be guaranteed and such acquisitions may consume substantial capital and other resources and could expose us to unforeseen liabilities and integration risks.
We have in the past and plan to in the future make investments in additional centers, whether by opening new centers or acquiring existing centers. Such acquisitions may involve significant cash expenditures, debt incurrence, operating losses and additional expenses that could have a material adverse effect on our financial position, results of operations and liquidity. Acquisitions involve numerous risks, including:
• | difficulties integrating acquired operations, personnel and accounting and information systems, or in realizing projected efficiencies and cost savings; |
• | diversion of management's attention from other business concerns; |
• | potential loss of key team members or customers of acquired companies; |
• | entry into markets in which we may have limited or no experience; |
• | increased indebtedness and reduced ability to access additional capital when needed; |
• | assumption of unknown liabilities or regulatory issues of acquired companies, including failure to comply with healthcare regulations or to establish internal financial controls; and |
• | straining of our resources, including internal controls relating to information and accounting systems, regulatory compliance, logistics and others. |
Furthermore, certain of the foregoing risks could be exacerbated when combined with other growth measures that we may pursue.
Investing in our business initiatives and development could adversely impact our results of operations and financial condition.
We plan to invest in business initiatives and development that will increase our operating expenses. These initiatives may or may not be successful in growing our census or revenues. There is typically a time delay between incurring such expenses and the attaining of revenues and cash flows expected from these initiatives and development. As a result, our revenue and operating cash flow may not increase enough during a reporting period to cover these increased expenses. Such additional revenues may not materialize to the level we anticipate, if at all.
Disasters and similar events may seriously harm our business.
Natural and man-made disasters and similar events, including terrorist attacks and acts of nature such as hurricanes, tornados, earthquakes and wildfires, may cause damage or disruption to us, our employees and our centers, which could have an adverse impact on our patients and our business. In order to provide care for our patients, we are dependent on consistent and reliable delivery of food, pharmaceuticals, utilities and other goods to our centers, and the availability of employees to provide services at our centers. If the delivery of goods or the ability of employees to reach our centers were interrupted in any material respect due to a natural disaster or other reasons, it would have a significant impact on our centers and our business. Furthermore, the impact, or impending threat, of a natural disaster has in the past and may in the future require that we evacuate one or more centers, which would be costly and would involve risks, including potentially fatal risks, for the patients. The impact of disasters and similar events is inherently uncertain. Such events could harm our patients and employees, severely damage or destroy one or more of our centers, harm our business, reputation and financial performance, or otherwise cause our business to suffer in ways that we currently cannot predict.
Failure to maintain effective internal control over our financial reporting could have an adverse effect on our ability to report our financial results on a timely and accurate basis.
Our management is responsible for establishing and maintaining adequate internal control over financial reporting, as defined in Rule 13a-15(f) under the Securities Exchange Act of 1934 (the “Exchange Act”), and is required to evaluate the effectiveness of these controls and procedures on a periodic basis and publicly disclose the results of these evaluations and related matters in accordance with the requirements of Section 404 of the Sarbanes-Oxley Act of 2002. Effective internal control over financial reporting is necessary for us to provide reliable financial reports, to help mitigate the risk of fraud and to operate successfully. However, testing and maintaining our internal control over financial reporting can be expensive and divert our management's attention from other business matters. Any failure to implement and maintain effective internal controls could result in material weaknesses or material misstatements in our consolidated financial statements.
17
If we fail to maintain effective internal control over financial reporting, we may be required to take corrective measures or restate the affected historical financial statements. In addition, we may be subjected to investigations and/or sanctions by federal and state securities regulators, and/or civil lawsuits by security holders. Any of the foregoing could also cause investors to lose confidence in our reported financial information and in our company and would likely result in a decline in the market price of our stock and in our ability to raise additional financing if needed in the future.
New accounting pronouncements or new interpretations of existing standards could require us to make adjustments in our accounting policies that could affect our financial statements.
We prepare our consolidated financial statements in accordance with accounting principles generally accepted in the United States of America (“GAAP”). The Financial Accounting Standards Board, the SEC, or other accounting organizations or governmental entities frequently issue new pronouncements or new interpretations of existing accounting standards. Changes in accounting standards, how the accounting standards are interpreted, or the adoption of new accounting standards can have a significant effect on our reported results, and could even retroactively affect previously reported transactions, and may require that we make significant changes to our systems, processes and controls.
Changes resulting from these new standards may result in materially different financial results and may require that we change how we process, analyze and report financial information and that we change financial reporting controls. Such changes in accounting standards may have an adverse effect on our business, financial position, and income, which may negatively impact our financial results.
Risks Related to Government Regulations
We are subject to significant government regulation.
The health care industry is subject to numerous laws and regulations of federal, state and local governments. These laws and regulations include, but are not necessarily limited to, matters such as licensure, accreditation, government health care program participation requirements, protection of patient health information, reimbursement for patient services, quality of patient care, Medicare and Medicaid fraud and abuse, debt collection and communications with consumers. Various federal and state laws regulate relationships among providers of services, including employment or service contracts and investment relationships. The operation of long-term care centers and the provision of services are also subject to extensive federal, state, and local laws relating to, among other things, the adequacy of medical care, distribution of pharmaceuticals, equipment, personnel, operating policies, environmental compliance, compliance with the Americans with Disabilities Act, fire prevention and compliance with building codes.
Long-term care facilities are subject to periodic inspection to assure continued compliance with various standards and licensing requirements under state law, as well as with Medicare and Medicaid conditions of participation. The failure to obtain or renew any required regulatory approvals or licenses could prevent us from offering our existing or additional services, subject us to penalties, and adversely affect our growth. In addition, health care is an area of extensive and frequent regulatory change. Changes in the laws or new interpretations of existing laws can have a significant effect on methods and costs of doing business and amounts of payments received from governmental and other payors. Our operations could be adversely affected by, among other things, regulatory developments such as mandatory increases in the scope and quality of care to be afforded patients and revisions in licensing and certification standards. We attempt at all times to comply with all applicable laws; however, there can be no assurance that we will remain in compliance at all times with all applicable laws and regulations or that new legislation or administrative or judicial interpretation of existing laws or regulations will not have a material adverse effect on our operations or financial condition. Federal or state proceedings seeking to impose fines and penalties for violations of applicable laws and regulations, as well as federal and state changes in these laws and regulations, may negatively impact us. See “Item 1. Business - Government Regulation.” See also “Item 3. Legal Proceedings.”
We are the subject of governmental audits, investigations, claims and litigation, which could have an adverse effect on our business or financial position.
Healthcare companies are subject to high levels of regulatory scrutiny. Various government agencies and their agents may conduct audits of our operations, including the Department of Health and Human Services (“HHS”) Office of Inspector General (“OIG”), which is tasked with combating fraud, waste and abuse within the Medicare and Medicaid programs. The OIG’s enforcement priorities are outlined in a work plan that is updated monthly. Recent additions to the work plan include life safety reviews and compliant billing practices. The OIG has also focused on quality of care, assessment and monitoring, poorly performing nursing facilities, hospitalizations, criminal background checks, Medicare part B services, accuracy of nursing facilities Minimum Data, transparency of ownership, and civil monetary penalty funds. We cannot predict the likelihood, scope or outcome of any OIG investigations of our centers.
18
The costs associated with potential litigation or the public announcement that we are being investigated, even if a dispute is resolved in our favor, or any determination that we have violated laws or regulations could have an adverse effect on our business, financial position or results of operations. In particular, government investigations, as well as qui tam lawsuits, may lead to significant penalties, including fines, damages payments or exclusion from government healthcare programs. Settlements of lawsuits involving Medicare and Medicaid issues routinely involve both financial penalties and corporate integrity agreements, either of which could have an adverse effect on our business, financial position or results of operations.
Payments we receive from Medicare and Medicaid are subject to audits. Such audits could result in an obligation to refund amounts previously paid to us.
Payments we receive from Medicare and Medicaid can be retroactively adjusted after examination during the claims settlement process or as a result of post-payment audits. Private pay sources also reserve the right to conduct audits. Payors may disallow our requests for reimbursement, or recoup amounts previously reimbursed, based on determinations by the payors or their third-party audit contractors that certain costs are not reimbursable because either adequate or additional documentation was not provided or because certain services were not covered or deemed to not be medically necessary. We believe that billing and reimbursement errors and disagreements are common in our industry. Significant adjustments, recoupments or repayments of our Medicare or Medicaid revenue could adversely affect our business, financial condition or results of operations.
We are subject to claims under the false claims, self-referral and anti-kickback legislation.
We are subject to numerous federal and state laws intended to prevent fraud, waste and abuse within the healthcare industry. Violations of these laws may result in substantial damage awards, civil or criminal penalties for individuals or entities, including large civil monetary penalties and exclusion from participation in the Medicare or Medicaid programs. Such awards, exclusion or penalties, if applied to us, could have a material adverse effect on our financial position and profitability.
In the United States, various state and federal laws regulate the relationships between providers of health care services, physicians, and other clinicians. These laws impose restrictions on physician referrals for designated health services to entities with which they have financial relationships. These laws also prohibit the offering, payment, solicitation or receipt of any form of remuneration in return for the referral of Medicare or state health care program patients or patient care opportunities for the purchase, lease or order of any item or service that is covered by the Medicare and Medicaid programs. To the extent that we, any of our centers through which we do business, or any of the owners or directors have a financial relationship with each other or with other health care entities providing services to long-term care patients, such relationships could be subject to increased scrutiny.
Federal and state laws prohibit the submission of false claims for reimbursement and prohibit the making of false claims or statements. Under the FCA, actions against a provider can be initiated by the federal government or by a private party on behalf of the federal government. These private parties, who are often referred to as “qui tam relators” or “relators,” are entitled to share in any amounts recovered by the government. Both direct enforcement activity by the government and qui tam relator actions have increased significantly in recent years.
A FCA violation occurs when a provider knowingly submits a claim for items or services not provided. Liability also arises for the knowing failure to report and refund an overpayment received from the government. The submission of false claims or the failure to timely repay overpayments may lead to the imposition of significant civil monetary penalties, significant criminal fines and imprisonment, and/or exclusion from participation in state and federally-funded healthcare programs, including the Medicare and Medicaid programs. Some courts have held that providers who allegedly have violated other statutes, such as self-referral or kickback laws, have thereby submitted false claims under the FCA. Allegations of poor quality of care can also lead to FCA actions under a theory of worthless services, which contends that care provided was so deficient that it was tantamount to no service at all.
The implied certification theory expands of the scope of the FCA. Under the implied certification theory, a violation of the FCA occurs when a provider’s request for payment implies a certification of compliance with the applicable statutes, regulations or contract provisions that are preconditions to payment. The recognition of this theory has increased the risk that a healthcare company will have to defend a false claims action, pay fines and treble damages or settlement amounts or be excluded from the federal and state healthcare programs as a result of an investigation arising out of the FCA. Many states have enacted similar laws providing for imposition of civil and criminal penalties for the filing of fraudulent claims.
Because we submit thousands of claims to Medicare each year and there is a relatively long statute of limitations under the FCA, there is a risk that intentional, or even negligent or recklessly submitted claims that prove to be incorrect, or
19
even billing errors, cost reporting errors or lapses in statutory or regulatory compliance with regard to the provision of healthcare services (including, without limitation the Anti-Kickback Statue and the self-referral laws discussed above), could result in significant civil or criminal penalties against us. At least one false claims act case is pending against us, and there can be no assurance that our operations will not be subject to review, scrutiny, penalties or enforcement actions under these laws, or that these laws will not change in the future. Any penalties or allegations involving false claims, whether valid or not, could have a significant impact on our business.
We are subject to laws governing the confidentiality of patient health information.
Both federal and state laws impose certain requirements regarding maintaining the confidentiality of patient health information. In particular, HIPAA rules and regulations require us to protect the medical records and other personal health information of our patients, limit our use of and ability to disclose such information, and give patients a right to access and amend their personal health information. A violation of HIPAA or any other federal or state laws regarding the confidentiality or use of such information could subject us to civil or criminal penalties, and could in turn damage our reputation, affect our ability to attract or retain patients, and thereby have a material adverse effect on our revenues, financial position, results of operations and cash flows.
We cannot predict the effects that healthcare reform initiatives, including possible repeal of or changes to the Affordable Care Act, and other changes in government programs may have on our business, financial condition or results of operations.
In recent years, there have been initiatives on the federal and state levels for comprehensive reforms affecting the availability, payment and reimbursement of healthcare services in the United States. The most prominent of these efforts is the Affordable Care Act, which affects how healthcare services are covered, delivered and reimbursed. However, there is significant uncertainty regarding the future of the Affordable Care Act. The Presidential administration and certain members of Congress have expressed their intent to repeal or make significant changes to the law, its implementation or interpretation. It is difficult to predict the impact of the Affordable Care Act and related regulations or the impact of its modification on our operations in light of the uncertainty regarding whether, when or how the law will be changed and what alternative reforms, if any, may be enacted. Significant changes to, or repeal of, the Affordable Care Act or other healthcare legislation or regulations could materially and adversely our business.
State efforts to regulate or deregulate the healthcare services industry or the construction or expansion of healthcare facilities could impair our ability to expand our operations, or could result in increased competition.
Some states require healthcare providers to obtain prior approval, known as a certificate of need, for:
• the purchase, construction or expansion of healthcare facilities;
• capital expenditures exceeding a prescribed amount; or
• changes in services or bed capacity.
In addition, other states that do not require certificates of need have effectively barred the expansion of existing facilities and the development of new ones by placing partial or complete moratoria on the number of new Medicaid beds they will certify in certain areas or in the entire state. Other states have established such stringent development standards and approval procedures for constructing new healthcare facilities that the construction of new facilities, or the expansion or renovation of existing facilities, may become cost prohibitive or extremely time-consuming. In addition, some states the acquisition of a facility being operated by a non-profit organization requires the approval of the state Attorney General.
Our ability to acquire or construct new facilities or expand or provide new services at existing facilities would be adversely affected if we are unable to obtain the necessary approvals, if there are changes in the standards applicable to those approvals, or if we experience delays and increased expenses associated with obtaining those approvals. We may not be able to obtain licensure, certificate of need approval, Medicaid certification, Attorney General approval or other necessary approvals for future expansion projects. Conversely, the elimination or reduction of state regulations that limit the construction, expansion or renovation of new or existing facilities could result in increased competition to us or result in overbuilding of facilities in some of our markets. If overbuilding in the healthcare industry in the markets in which we operate were to occur, it could reduce the occupancy rates of existing facilities and, in some cases, might reduce the private rates that we charge for our services.
20
Changes to federal and state income tax laws and regulations could adversely affect our position on income taxes and estimated income liabilities.
We are subject to both state and federal income taxes in the U.S. and our operations, plans and results are affected by tax and other initiatives. On December 22, 2017, a law commonly known as the Tax Cuts and Jobs Act (“Tax Act") was enacted in the United States. As a result, our 2017 results include a non-cash increase in the provisions for income taxes of $5.5 million related to the estimated impact of the Tax Act on our deferred tax assets and liabilities.
The Company considers the accounting for the deferred tax re-measurements and other items to be complete, but ongoing accounting guidance and interpretation could result in adjustments to the consolidated financial statements. Among other things, the Tax Act reduces the U.S. corporate income tax rate to 21 percent, which could result in changes in the valuation of our deferred tax asset and liabilities. Any such change in valuation could have a material impact on our income tax expense and deferred tax balances.
We are also subject to regular reviews, examinations, and audits by the Internal Revenue Service and other taxing authorities with respect to our taxes. There are uncertainties and ambiguities in the application of the Tax Act and it is possible that the IRS could issue subsequent guidance or take positions on audit that differ from our interpretations and assumptions. Although we believe our tax estimates are reasonable, if a taxing authority disagrees with the positions we have taken, we could face additional tax liability, including interest and penalties. Our effective tax rate could be adversely affected by changes in the mix of earnings in states with different statutory tax rates, changes in the valuation of deferred tax assets and liabilities, changes in tax laws and regulations, changes in our interpretations of tax laws, including the Tax Act. Unanticipated changes in our tax rates or exposure to additional income tax liabilities could affect our profitability. There can be no assurance that payment of such additional amounts upon final adjudication of any disputes will not have a material impact on our results of operations and financial position.
Risks Related to our Common Stock
Our ability and intent to pay cash dividends in the future may be limited.
We currently pay a $0.055 quarterly dividend on our common shares, and while the Board of Directors intends to pay quarterly dividends, the Board will make the determination of the amount of future cash dividends, if any, to be declared and paid based on, among other things, our financial condition, funds from operations, the level of our capital expenditures and future business prospects. The Company is restricted by its debt agreements in its ability to pay dividends.
Our securities are now and have historically been thinly traded. An active trading market in our equity securities may cease to exist, which would adversely affect the market price and liquidity of our common stock, in addition our stock price has been subject to fluctuating prices.
Shares of our common stock are now and have been thinly traded, meaning that the number of persons interested in purchasing our common stock at or near ask prices at any given time may be relatively small or non-existent. As a consequence, our stock price may not reflect an actual or perceived value of the business. Also, there may be periods of several days or more when trading activity in our shares is minimal or non-existent, as compared to an issuer that has a large and steady volume of trading activity that will generally support continuous sales without an adverse effect on share price. We cannot predict the actions of market makers, investors or other market participants, and can offer no assurances that the market for our securities will be stable. If there is no active trading market in our equity securities, the market price and liquidity of the securities will be adversely affected. The market price of our common stock could decline as a result of sales of a large number of shares of our common stock in the market or the perception that these sales could occur. Due to these conditions, you may not be able to sell your shares at or near ask prices or at all if you need money or otherwise desire to liquidate your shares. These conditions also might make it more difficult for us to sell equity securities in the future at a time and at a price that we deem appropriate.
We have a number of policies in place that could be considered anti-takeover protections.
Our Certificate of Incorporation (the “Certificate”) requires the approval of the holders of two-thirds of the outstanding shares to amend certain provisions of the Certificate. Section 203 of the Delaware General Corporate Law restricts the ability of a Delaware corporation to engage in any business combination with an interested shareholder. We are also authorized to issue up to 795,000 shares of preferred stock, the rights of which may be fixed by our Board without shareholder approval. Provisions in certain of our executive officers' employment agreements provide for post-termination compensation, including payment of amounts up to two times their annual salary, following certain changes in control (as defined in such agreements). Our stock incentive plans provide for the acceleration of the vesting of options in the event of certain changes in control (as defined in such plans). Certain changes in control also constitute an event of default
21
under our bank credit facility. The foregoing matters may, together or separately, have the effect of discouraging or making more difficult an acquisition or change of control of the company.
ITEM 1B. UNRESOLVED STAFF COMMENTS
None.
22
ITEM 2. PROPERTIES
We own 18 and lease 58 long-term care centers as discussed in “Item 1 Business - Nursing Centers and Services.” See further details below.
Our current operations include 58 nursing centers subject to operating leases, including 35 owned by Omega Health Investors ("Omega"), 20 owned by Golden Living and three owned by other parties. In our role as lessee, we are responsible for the day-to-day operations of all operated centers. These responsibilities include recruiting, hiring and training all nursing and other personnel, and providing patient care, nutrition services, marketing, quality improvement, accounting, and data processing services for each center. The lease agreements pertaining to our 58 leased centers are “triple net” leases, requiring us to maintain the premises, provide insurance, pay taxes and pay for all utilities. The average remaining term of our lease agreements, including renewal options, is approximately 16 years. See the table below for a summary of owned and leased beds operated by the Company.
State | Centers | Leased Beds | Owned Beds | Total Operational Beds (1) | ||||||||
Alabama | 20 | 2,079 | 306 | 2,385 | ||||||||
Florida | 1 | 79 | — | 79 | ||||||||
Indiana | 1 | 172 | — | 172 | ||||||||
Kansas | 6 | — | 483 | 483 | ||||||||
Kentucky | 13 | 917 | 252 | 1,169 | ||||||||
Mississippi | 9 | 1,039 | — | 1,039 | ||||||||
Missouri | 3 | 455 | — | 455 | ||||||||
Ohio | 5 | 701 | — | 701 | ||||||||
Tennessee | 5 | 497 | 120 | 617 | ||||||||
Texas | 13 | 1,370 | 475 | 1,845 | ||||||||
Total | 76 | 7,309 | 1,636 | 8,945 | ||||||||
____________
(1) | The number of Operational Beds includes 489 Licensed Assisted Living/Residential Beds. |
Brentwood Support Center and Regional Offices
We lease approximately 29,000 square feet of office space in Brentwood, Tennessee that houses our executive offices, and centralized management support functions. Lease periods on these centers range up to three years. Regional executives for Kansas work from an office of approximately 922 square feet. We believe that our leased properties are adequate for our present needs and that suitable additional or replacement space will be available as required.
ITEM 3. LEGAL PROCEEDINGS
The provision of health care services entails an inherent risk of liability. Participants in the health care industry are subject to lawsuits alleging malpractice, negligence, violations of false claims acts, product liability, or related legal theories, many of which involve large claims and significant defense costs. Like many other companies engaged in the long-term care profession in the United States, we have numerous pending liability claims, disputes and legal actions for professional liability and other related issues. It is expected that we will continue to be subject to such suits as a result of the nature of our business. Further, as with all health care providers, we are periodically subject to regulatory actions seeking fines and penalties for alleged violations of health care laws and are potentially subject to the increased scrutiny of regulators for issues related to compliance with health care fraud and abuse laws and with respect to the quality of care provided to residents of our center. Like other health care providers, in the ordinary course of our business, we are also subject to claims made by employees and other disputes and litigation arising from the conduct of our business.
As of December 31, 2017, we are engaged in 72 professional liability lawsuits. Five lawsuits are currently scheduled for trial or arbitration during the next twelve months, and it is expected that additional cases will be set for trial or hearing. The ultimate results of any of our professional liability claims and disputes cannot be predicted. We have limited, and sometimes no, professional liability insurance with regard to most of these claims. A significant judgment entered against us in one or more of these legal actions could have a material adverse impact on our financial position and cash flows.
In July 2013, the Company learned that the United States Attorney for the Middle District of Tennessee ("DOJ") had commenced a civil investigation of potential violations of the False Claims Act ("FCA").
23
In October 2014, the Company learned that the investigation was started by the filing under seal of a false claims action against the two centers that were the subject of the original civil investigative demand ("CID"). In connection with this matter, between July 2013 and early February 2016, the Company has received three civil investigative demands (a form of subpoena) for documents and information relating to our practices and policies for rehabilitation, and other services, our preadmission evaluation forms ("PAEs") required by TennCare and our Pre-Admission Screening and Resident Reviews ("PASRRs"). We have responded to those requests. The DOJ has also issued CID’s for testimony from current and former employees of the Company. The DOJ’s civil investigation of the Company’s practices and policies for rehabilitation now covers all of the Company’s centers, but thus far only documents from six of our centers have been requested.
In June 2016, the Company received an authorized investigative demand (a form of subpoena) for documents in connection with a criminal investigation by the DOJ related to our practices with respect to PAEs and PASRRs, and the Company has provided documents responsive to this subpoena and continues to provide additional information as requested. The Company cannot predict the outcome of these investigations or the related lawsuits, and the outcome could have a materially adverse effect on the Company, including the imposition of treble damages, criminal charges, fines, penalties and/or a corporate integrity agreement. Additionally, the uncertainty regarding the outcome of this investigation makes it more difficult for the Company to pursue strategic possibilities, longer term initiatives or to make significant financial commitments outside of the normal course of its business. The Company is committed to provide caring and professional services to its patients and residents in compliance with applicable laws and regulations.
In January 2009, a purported class action complaint was filed in the Circuit Court of Garland County, Arkansas against the Company and certain of its subsidiaries and Garland Nursing & Rehabilitation Center (the “Center”). The complaint alleges that the defendants breached their statutory and contractual obligations to the patients of the Center over the five-year period prior to the filing of the complaints. The Court has not yet ruled on the motion to dismiss, so lawsuit remains in its early stages and has not yet been certified by the court as a class action. The Company intends to defend the lawsuit vigorously.
We cannot currently predict with certainty the ultimate impact of any of the above cases on our financial condition, cash flows or results of operations. Our reserve for professional liability expenses does not include any amounts for the pending DOJ investigation or the purported class action against the Arkansas centers. An unfavorable outcome in any of these lawsuits or any of our professional liability actions, any regulatory action, any investigation or lawsuit alleging violations of fraud and abuse laws or of elderly abuse laws or any state or Federal False Claims Act case could subject us to fines, penalties and damages, including exclusion from the Medicare or Medicaid programs, and could have a material adverse impact on our financial condition, cash flows or results of operations.
ITEM 4. MINE SAFETY DISCLOSURES
Not applicable.
24
PART II
ITEM 5. MARKET FOR REGISTRANT'S COMMON EQUITY, RELATED STOCKHOLDER MATTERS AND ISSUER PURCHASES OF EQUITY SECURITIES
Market Information. Our common stock is traded on the NASDAQ Capital Market and began trading there on September 12, 2006 under the symbol “AVCA.” Effective March 15, 2013, the Company changed its name from Advocat Inc. to Diversicare Healthcare Services, Inc. as a result of a merger of the Company and a wholly-owned subsidiary. In connection with the name change, the Company changed its NASDAQ ticker symbol from “AVCA” to “DVCR” effective with the market open on
Monday, March 18, 2013. The following table sets forth the high and low bid prices of our common stock, as reported by NASDAQ.com, for each quarter in 2017 and 2016:
Period | High | Low | Dividends | |||||||||
2016 | — | 1st | Quarter | $ | 9.95 | $ | 6.75 | $ | 0.055 | |||
2016 | — | 2nd | Quarter | $ | 8.90 | $ | 7.00 | $ | 0.055 | |||
2016 | — | 3rd | Quarter | $ | 10.07 | $ | 6.41 | $ | 0.055 | |||
2016 | — | 4th | Quarter | $ | 12.82 | $ | 9.98 | $ | 0.055 | |||
2017 | — | 1st | Quarter | $ | 11.91 | $ | 8.40 | $ | 0.055 | |||
2017 | — | 2nd | Quarter | $ | 11.20 | $ | 8.70 | $ | 0.055 | |||
2017 | — | 3rd | Quarter | $ | 11.60 | $ | 8.50 | $ | 0.055 | |||
2017 | — | 4th | Quarter | $ | 12.25 | $ | 9.40 | $ | 0.055 | |||
Our common stock has been traded since May 10, 1994. On February 15, 2018, the closing price for our common stock was $7.76, as reported by NASDAQ.com.
Holders. On February 15, 2018, there were approximately 261 holders of record. Most of our shareholders have their holdings in the street name of their broker/dealer.
Dividends. For each of the two most recent fiscal years, we have paid a quarterly dividend of $0.055 per common share. While the Board of Directors intends to continue to pay quarterly dividends, the Board will make the determination of the amount of future cash dividends, if any, to be declared and paid based on, among other things, the Company's financial condition, funds from operations, the level of its capital expenditures and its future business prospects. The Company is restricted by its debt agreements in its ability to pay dividends.
ITEM 6. SELECTED CONSOLIDATED FINANCIAL DATA
The selected financial data of Diversicare presented in the following table has been derived from our consolidated financial statements, and should be read in conjunction with the annual consolidated financial statements and related notes and Management's Discussion and Analysis of Financial Condition and Results of Operations. This selected financial data for all periods shown has been reclassified to present the effects of certain divestitures as discontinued operations.
25
Year Ended December 31, | ||||||||||||||||||||
2017 | 2016 | 2015 | 2014 | 2013 | ||||||||||||||||
Statement of Operations Data | (in thousands, except per share amounts) | |||||||||||||||||||
REVENUES: | ||||||||||||||||||||
Patient revenues, net | $ | 574,794 | $ | 426,063 | $ | 387,595 | $ | 344,192 | $ | 260,221 | ||||||||||
EXPENSES: | ||||||||||||||||||||
Operating | 458,122 | 342,932 | 311,035 | 275,605 | 213,064 | |||||||||||||||
Lease and rent expense | 54,988 | 33,364 | 28,690 | 26,151 | 20,396 | |||||||||||||||
Professional liability | 10,764 | 8,456 | 8,122 | 7,216 | 5,666 | |||||||||||||||
General and administrative | 33,311 | 30,271 | 24,793 | 22,133 | 20,940 | |||||||||||||||
Depreciation and amortization | 10,902 | 8,292 | 7,524 | 7,078 | 6,363 | |||||||||||||||
Lease termination costs (receipts) | (180 | ) | 2,008 | — | — | — | ||||||||||||||
Restructuring | — | — | — | — | 1,446 | |||||||||||||||
567,907 | 425,323 | 380,164 | 338,183 | 267,875 | ||||||||||||||||
OPERATING INCOME (LOSS) | 6,887 | 740 | 7,431 | 6,009 | (7,654 | ) | ||||||||||||||
OTHER INCOME (EXPENSE): | ||||||||||||||||||||
Equity in net income (losses) of investment in unconsolidated affiliate | — | 273 | 339 | (5 | ) | (183 | ) | |||||||||||||
Gain on bargain purchase | 925 | — | — | — | — | |||||||||||||||
Gain on sale of investment in unconsolidated affiliate | 733 | 1,366 | — | |||||||||||||||||
Hurricane costs | (232 | ) | — | — | — | — | ||||||||||||||
Interest expense, net | (6,369 | ) | (4,802 | ) | (4,102 | ) | (3,697 | ) | (3,032 | ) | ||||||||||
Debt retirement costs | — | (351 | ) | — | — | (320 | ) | |||||||||||||
(4,943 | ) | (3,514 | ) | (3,763 | ) | (3,702 | ) | (3,535 | ) | |||||||||||
INCOME (LOSS) FROM CONTINUING OPERATIONS BEFORE INCOME TAXES | 1,944 | (2,774 | ) | 3,668 | 2,307 | (11,189 | ) | |||||||||||||
BENEFIT (PROVISION) FOR INCOME TAXES | (6,743 | ) | 1,030 | (916 | ) | (857 | ) | 4,196 | ||||||||||||
INCOME (LOSS) FROM CONTINUING OPERATIONS | (4,799 | ) | (1,744 | ) | 2,752 | 1,450 | (6,993 | ) | ||||||||||||
DISCONTINUED OPERATIONS, net of taxes | (28 | ) | (67 | ) | (1,128 | ) | 3,258 | (1,469 | ) | |||||||||||
NET INCOME (LOSS) | $ | (4,827 | ) | $ | (1,811 | ) | $ | 1,624 | $ | 4,708 | $ | (8,462 | ) | |||||||
INCOME (LOSS) PER COMMON SHARE: | ||||||||||||||||||||
Basic | ||||||||||||||||||||
Continuing operations | $ | (0.76 | ) | $ | (0.28 | ) | $ | 0.45 | $ | 0.21 | $ | (1.26 | ) | |||||||
Discontinued operations | (0.01 | ) | (0.01 | ) | (0.18 | ) | 0.54 | (0.25 | ) | |||||||||||
Net income (loss) per common share | $ | (0.77 | ) | $ | (0.29 | ) | $ | 0.27 | $ | 0.75 | $ | (1.51 | ) | |||||||
Diluted | ||||||||||||||||||||
Continuing operations | $ | (0.76 | ) | $ | (0.28 | ) | $ | 0.44 | 0.20 | (1.26 | ) | |||||||||
Discontinued operations | (0.01 | ) | (0.01 | ) | (0.18 | ) | 0.52 | (0.25 | ) | |||||||||||
Net income (loss) per common share | $ | (0.77 | ) | $ | (0.29 | ) | $ | 0.26 | $ | 0.72 | $ | (1.51 | ) | |||||||
CASH DIVIDENDS DECLARED PER COMMON SHARE | $ | 0.22 | $ | 0.22 | $ | 0.22 | $ | 0.22 | $ | 0.22 | ||||||||||
WEIGHTED AVERAGE COMMON SHARES OUTSTANDING: | ||||||||||||||||||||
Basic | 6,279 | 6,199 | 6,100 | 6,011 | 5,899 | |||||||||||||||
Diluted | 6,279 | 6,199 | 6,315 | 6,197 | 5,899 | |||||||||||||||
26
December 31, | ||||||||||||||||||||
2017 | 2016 | 2015 | 2014 | 2013 | ||||||||||||||||
Balance Sheet Data | (in thousands) | |||||||||||||||||||
Working capital | $ | 8,391 | $ | 13,521 | $ | 13,052 | $ | 8,797 | $ | 8,044 | ||||||||||
Total assets | $ | 167,569 | $ | 163,051 | $ | 137,084 | $ | 129,089 | $ | 137,744 | ||||||||||
Long-term debt and capitalized lease obligations, less current portion and deferred financing costs, net | $ | 89,552 | $ | 82,133 | $ | 60,867 | $ | 48,265 | $ | 53,577 | ||||||||||
Preferred Stock - Series C | $ | — | $ | — | $ | — | $ | — | $ | 4,918 | ||||||||||
Total Shareholders' Equity of Diversicare Healthcare Services, Inc. | $ | 6,462 | $ | 11,420 | $ | 13,267 | $ | 11,754 | $ | 8,129 | ||||||||||
Total Equity | $ | 6,462 | $ | 11,420 | $ | 13,267 | $ | 11,754 | $ | 9,566 | ||||||||||
27
ITEM 7. MANAGEMENT'S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS
Overview
Diversicare Healthcare Services, Inc. provides long-term care services to nursing center patients in ten states, primarily in the Southeast, Midwest and Southwest. Our centers provide a range of health care services to their patients and residents. In addition to the nursing, personal care and social services usually provided in long-term care centers, we offer a variety of comprehensive rehabilitation services as well as nutritional support services. As of December 31, 2017, our continuing operations consist of 76 nursing centers with 8,456 licensed skilled nursing beds and 489 assisted-living and other residential beds. We own 18 and lease 58 of our nursing centers included in continuing operations. The Company's continuing operations include centers in Alabama, Florida, Indiana, Kansas, Kentucky, Mississippi, Missouri, Ohio, Tennessee, and Texas.
Key Performance Metrics
Skilled mix. Skilled mix represents the number of days our Medicare and Managed Care patients are receiving services at the skilled nursing facilities divided by the total number of days patients (less days from assisted living services) from all payor sources are receiving services at the skilled nursing facilities for any given period.
Average rate per day. Average rate per day is the revenue by payor source for a period at the skilled nursing facility divided by actual patient days for the revenue source for a given period.
Average daily skilled nursing census. Average daily skilled nursing census is the average number of patients who are receiving skilled nursing care as a percentage of total number of patient days.
Strategic Operating Initiatives
We identified several key strategic objectives to increase shareholder value through improved operations and business development. These strategic operating initiatives include: improving our facilities’ quality metrics, improving skilled mix in our nursing centers, improving our average Medicare rate, implementing and maintaining Electronic Medical Records (“EMR”) to improve Medicaid capture, and completing strategic acquisitions and divestitures. We have experienced success in these initiatives and expect to continue to build on these improvements. In light of challenges facing the industry and the Company specifically, including the unresolved governmental investigation. we believe that now is not the time to attempt to engage in a company-wide strategic transaction.
Improving skilled mix and average Medicare rate:
One of our key performance indicators is skilled mix. Our strategic operating initiatives of improving our skilled mix and our average Medicare rate required investing in nursing and clinical care to treat more acute patients along with nursing center-based marketing representatives to attract these patients. These initiatives developed referral and Managed Care relationships that have attracted and are expected to continue to attract payor sources for patients covered by Medicare and Managed Care. The Company's skilled mix for the years ended December 31, 2017, 2016 and 2015 was 15.1%, 15.2% and 16.2%, respectively. The graph below illustrates our average Medicare rate per day:
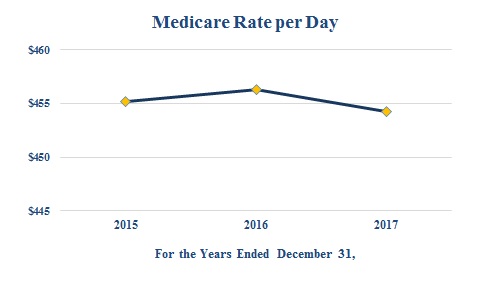
28
Utilizing Electronic Medical Records to improve Medicaid acuity capture:
As another part of our strategic operating initiatives, we successfully completed a full implemented of EMR in our nursing centers to improve Medicaid acuity capture, primarily in our states where the Medicaid payments are acuity based. We completed the implementation on time and under budget, and since implementation, have increased our average Medicaid rate despite rate cuts in certain acuity based states by accurate and timely capture of care delivery. The graph below illustrates our success with increasing our average Medicaid rate per day since implementation:
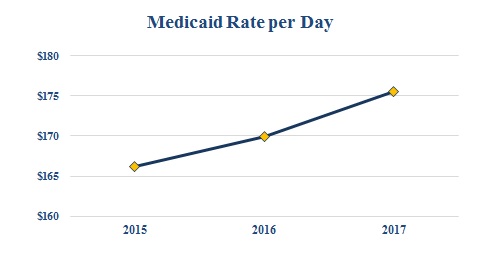
Completing strategic transactions:
Our strategic operating initiatives include a renewed focus on completing strategic acquisitions. We continue to pursue and investigate opportunities to acquire, lease or develop new centers, focusing primarily on opportunities within our existing geographic areas of operation. We expect to announce additional development projects in the near future.
Effective July 1, 2017, the Company acquired a 103-bed skilled nursing center in Selma, Alabama, for an aggregate purchase price of $8,750,000, pursuant to an Asset Purchase Agreement with Park Place Nursing and Rehabilitation Center, LLC, Dunn Nursing Home, Inc., Wood Properties of Selma LLC, and Homewood of Selma, LLC. Additionally, on October 1, 2016 and November 1, 2016, we assumed the operations of ten centers in Mississippi and 12 centers in Alabama, respectively. These transactions are further discussed in Note 2 "Business Development and Other Significant Transactions" to the consolidated financial statements.
Divestitures
As part of our strategic efforts, we have also performed thorough analysis on our existing centers in order to determine whether continuing operations within certain markets or regions was in line with the short-term and long-term strategy of the business. As a result, in September 2017, we ceased operations at our Carthage, Mississippi, facility, thus terminating our lease with Trend Health and Rehab of Carthage, LLC. Additionally, in May 2016, we ceased operations at our Avon, Ohio, facility, thus terminating our lease with Avon Ohio, LLC. These transactions were not reported as discontinued operations as described in Note 2 "Business Development and Other Significant Transactions" to the consolidated financial statements.
Basis of Financial Statements.
Our patient revenues consist of the fees charged for the care of patients in the nursing centers we own and lease. Our operating expenses include the costs, other than lease, depreciation and amortization expenses, incurred in the operation of the nursing centers we own and lease. Our general and administrative expenses consist of the costs of the corporate office and regional support functions. Our interest, depreciation and amortization expenses include all such expenses across the range of our operations.
29
Selected Financial and Operating Data
The following table summarizes the Diversicare statements of continuing operations for the years ended December 31, 2017, 2016 and 2015, and sets forth this data as a percentage of revenues for the same year:
Year Ended December 31, | |||||||||||||||||||||
(Dollars in thousands) | |||||||||||||||||||||
2017 | 2016 | 2015 | |||||||||||||||||||
Revenues: | |||||||||||||||||||||
Patient revenues, net | $ | 574,794 | 100.0 | % | $ | 426,063 | 100.0 | % | $ | 387,595 | 100.0 | % | |||||||||
Expenses: | |||||||||||||||||||||
Operating | 458,122 | 79.7 | % | 342,932 | 80.5 | % | 311,035 | 80.2 | % | ||||||||||||
Lease and rent expense | 54,988 | 9.6 | % | 33,364 | 7.8 | % | 28,690 | 7.4 | % | ||||||||||||
Professional liability | 10,764 | 1.9 | % | 8,456 | 2.0 | % | 8,122 | 2.1 | % | ||||||||||||
General & administrative | 33,311 | 5.8 | % | 30,271 | 7.1 | % | 24,793 | 6.4 | % | ||||||||||||
Depreciation and amortization | 10,902 | 1.9 | % | 8,292 | 1.9 | % | 7,524 | 1.9 | % | ||||||||||||
Lease termination costs (receipts) | (180 | ) | — | % | 2,008 | 0.5 | % | — | — | % | |||||||||||
567,907 | 98.9 | % | 425,323 | 99.8 | % | 380,164 | 98.0 | % | |||||||||||||
Operating income | 6,887 | 1.1 | % | 740 | 0.2 | % | 7,431 | 2.0 | % | ||||||||||||
Other income (expense): | |||||||||||||||||||||
Equity in net income of unconsolidated affiliate | — | — | % | 273 | 0.1 | % | 339 | 0.1 | % | ||||||||||||
Gain on bargain purchase | 925 | 0.2 | % | — | — | % | — | — | % | ||||||||||||
Gain on sale of investment in unconsolidated affiliate | 733 | 0.1 | % | 1,366 | 0.3 | % | — | — | % | ||||||||||||
Hurricane costs | (232 | ) | — | % | — | — | % | — | — | % | |||||||||||
Interest expense, net | (6,369 | ) | (1.1 | )% | (4,802 | ) | (1.1 | )% | (4,102 | ) | (1.1 | )% | |||||||||
Debt retirement costs | — | — | % | (351 | ) | (0.1 | )% | — | — | % | |||||||||||
(4,943 | ) | (0.8 | )% | (3,514 | ) | (0.8 | )% | (3,763 | ) | (1.0 | )% | ||||||||||
Income (loss) from continuing operations before income taxes | 1,944 | 0.3 | % | (2,774 | ) | (0.6 | )% | 3,668 | 1.0 | % | |||||||||||
Benefit (provision) for income taxes | (6,743 | ) | (1.2 | )% | 1,030 | 0.2 | % | (916 | ) | (0.2 | )% | ||||||||||
Income (loss) from continuing operations | $ | (4,799 | ) | (0.9 | )% | $ | (1,744 | ) | (0.4 | )% | $ | 2,752 | 0.8 | % | |||||||
The following table presents data about the centers we operated as part of our continuing operations as of the dates:
December 31, | |||||||||
2017 | 2016 | 2015 | |||||||
Licensed Nursing Center Beds: | |||||||||
Owned | 1,607 | 1,504 | 1,370 | ||||||
Leased | 6,849 | 6,949 | 4,690 | ||||||
Total | 8,456 | 8,453 | 6,060 | ||||||
Facilities: | |||||||||
Owned | 18 | 17 | 15 | ||||||
Leased | 58 | 59 | 40 | ||||||
Total | 76 | 76 | 55 | ||||||
30
Critical Accounting Policies and Judgments
A “critical accounting policy” is one which is both important to the understanding of our financial condition and results of operations and requires management's most difficult, subjective or complex judgments, often of the need to make estimates about the effect of matters that are inherently uncertain. Actual results could differ from those estimates and cause our reported net income (loss) to vary significantly from period to period. Our accounting policies that fit this definition include the following:
Revenues
Patient Revenues, Net
The fees we charge patients in our nursing centers are recorded on an accrual basis. These rates are contractually adjusted with respect to individuals receiving benefits under federal and state-funded programs and other third-party payors. Our net revenues are derived substantially from Medicare, Medicaid and other government programs (approximately 78.3%, 78.1% and 77.6% for 2017, 2016, and 2015, respectively). Medicare intermediaries make retroactive adjustments based on changes in allowed claims. In addition, certain of the states in which we operate require complicated detailed cost reports which are subject to review and adjustments. In the opinion of management, adequate provision has been made for adjustments that may result from such reviews. Retroactive adjustments, if any, are recorded when objectively determinable, generally within three years of the close of a reimbursement year depending upon the timing of appeals and third-party settlement reviews or audits.
Allowance for Doubtful Accounts
We evaluate the collectability of our accounts receivable by reviewing current aging summaries of accounts receivable, historical collections data and other factors. As a percentage of revenue, our provision for doubtful accounts was approximately 1.6%, 1.7%, and 1.9% for 2017, 2016, and 2015, respectively. Historical bad debts have generally resulted from uncollectible private pay balances, some uncollectible coinsurance and deductibles and other factors. Receivables that are deemed to be uncollectible are written off.
Professional Liability and Other Self-Insurance Reserves
Accrual for Professional and General Liability Claims
The Company has professional liability insurance coverage for its nursing centers that, based on historical claims experience, is likely to be substantially less than the claims that are expected to be incurred. Effective July 1, 2013, the Company established a wholly-owned, consolidated offshore limited purpose insurance subsidiary, SHC Risk Carriers, Inc. (“SHC”), which has issued a policy insuring claims made against all of the Company's nursing centers in Florida and Tennessee, the Company’s formerly operated Arkansas and West Virginia centers, and several of the Company’s nursing centers in Alabama, Kentucky, Ohio, and Texas. The insurance coverage provided for these centers under the SHC policy include coverage limits of $500,000 or $1,000,000 per medical incident with a sublimit per center of $1,000,000 and total annual aggregate policy limits of $5,000,000. All other centers within the Company’s portfolio are covered through various commercial insurance policies which provide coverage limits of $1,000,000 per claim and have sublimits of $3,000,000 per center, with varying aggregate policy limits and deductibles. The deductibles for these policies are covered through the insurance subsidiary.
Because our actual liability for existing and anticipated professional liability and general liability claims will exceed our limited insurance coverage, we have recorded total liabilities for reported professional liability claims and estimates for incurred but unreported claims of $20.1 million as of December 31, 2017, including $1.4 million for settlements that are expected to be paid in 2018, estimates of liability for incurred but not reported claims, estimates of liability for reported but unresolved claims, and estimates of related legal costs incurred and expected to be incurred. All losses are projected on an undiscounted basis.
The Company evaluates the adequacy of this liability on a quarterly basis. Semi-annually, the Company retains a third-party actuarial firm to assist in the evaluation of this reserve. Since May 2012, Merlinos & Associates, Inc. (“Merlinos”) has assisted management in the preparation of the appropriate accrual for incurred but not reported general and professional liability claims based on data furnished as of May 31 and November 30 of each year. Merlinos primarily utilizes historical data regarding the frequency and cost of the Company's past claims over a multi-year period, industry data and information regarding the number of occupied beds to develop its estimates of the Company's ultimate professional liability cost for current periods.
On a quarterly basis, we obtain reports of asserted claims and lawsuits from our insurers and a third party claims administrator. These reports contain information relevant to the liability actually incurred to date with that claim as well as the third-party administrator's estimate of the anticipated total cost of the claim. This information is reviewed by us quarterly and provided to the actuary semi-annually. We use this information to determine the timing of claims reporting and the development of reserves and compare the information obtained to our previously recorded estimates of liability. Based on the actual claim information obtained, on the semi-annual estimates received from the actuary and on estimates regarding the number and cost of additional claims
31
anticipated in the future, the reserve estimate for a particular period may be revised upward or downward on a quarterly basis. Final determination of our actual liability for claims incurred in any given period is a process that takes years.
The Company's cash expenditures for self-insured professional liability costs from continuing operations were $6.6 million, $4.5 million and $3.3 million for the years ended December 31, 2017, 2016 and 2015, respectively.
Although we retain a third-party actuarial firm to assist us, professional and general liability claims are inherently uncertain, and the liability associated with anticipated claims is very difficult to estimate. Professional liability cases have a long cycle from the date of an incident to the date a case is resolved, and final determination of our actual liability for claims incurred in any given period is a process that takes years. As a result, our actual liabilities may vary significantly from the accrual, and the amount of the accrual has and may continue to fluctuate by a material amount in any given quarter due to the significance of judgments and estimates.
Professional liability costs are material to our financial position, and changes in estimates, as well as differences between estimates and the ultimate amount of loss, may cause a material fluctuation in our reported results of operations. Our professional liability expense was $10.8 million, $8.5 million and $8.1 million for the years ended December 31, 2017, 2016 and 2015, respectively. These amounts are material in relation to our reported income (loss) from continuing operations for the related periods of $(4.8) million, $(1.7) million and $2.8 million, respectively. The total liability recorded at December 31, 2017 was $20.1 million, compared to current assets of $72.7 million and total assets of $167.6 million.
Accrual for Other Self-Insured Claims
With respect to workers' compensation insurance, substantially all of our employees became covered under either a prefunded deductible policy or state-sponsored programs. We have been and remain a non-subscriber to the Texas workers' compensation system and are, therefore, completely self-insured for employee injuries with respect to our Texas operations. From June 30, 2003 until June 30, 2007, our workers' compensation insurance programs provided coverage for claims incurred with premium adjustments depending on incurred losses. For the period from July 1, 2007 until June 30, 2008, the Company is completely insured for workers' compensation exposure. For the period from July 1, 2008 through December 31, 2017, we are covered by a prefunded deductible policy. Under this policy, we are self-insured for the first $500,000 per claim, subject to an aggregate maximum of $3,000,000. We fund a loss fund account with the insurer to pay for claims below the deductible. We account for premium expense under this policy based on its estimate of the level of claims subject to the policy deductibles expected to be incurred.
We are self-insured for health insurance benefits for certain employees and dependents for amounts up to $200,000 per individual annually. We provide reserves for the settlement of outstanding self-insured health claims at amounts believed to be adequate, based on known claims and estimates of unknown claims based on historical information. The differences between actual settlements and reserves are included in expense in the period finalized. Our reserves for health insurance benefits can fluctuate materially from one year to the next depending on the number of significant health issues of our covered employees and their dependents.
Asset Impairment
We evaluate our property, equipment and other long-lived assets on a quarterly basis to determine if facts and circumstances suggest that the assets may be impaired or that the estimated depreciable life of the asset may need to be changed for significant physical changes in the property, or significant adverse changes in general economic conditions, and significant deteriorations of the underlying cash flows or fair values of the property if impairment indicators exist. The need to recognize impairment is based on estimated undiscounted future cash flows from a property compared to the carrying value of that property. If recognition of impairment is necessary, it is measured as the amount by which the carrying amount of the property exceeds the fair value of the property.
No impairment of long lived assets was recognized during 2017, 2016, or 2015. If our estimates or assumptions with respect to a property change in the future, we may be required to record additional impairment charges for our assets.
Business Combinations
For business combination transactions, we recognize and measure the identifiable assets acquired, the liabilities assumed, any noncontrolling interest in the acquiree, as well as the goodwill acquired or gain recognized in a bargain purchase, and we make certain valuations to determine the acquisition date fair value of assets acquired and the liabilities assumed. These valuations are subject to adjustments during the measurement period, generally not to exceed twelve-months from the acquisition date. Such valuations require us to make significant estimates, judgments and assumptions, including projections of future events and operating performance.
Stock-Based Compensation
We recognize compensation cost for all share-based payments granted on a straight-line basis over the vesting period. We calculated the recognized and unrecognized stock-based compensation for options and stock-only stock appreciation rights ("SOSARs")
32
using the Black-Scholes-Merton option valuation method, which requires us to use certain key assumptions to develop the fair value estimates. These key assumptions include expected volatility, risk-free interest rate, expected dividends and expected term. For restricted shares, we utilize the market price at the grant date in order to calculate the stock-based compensation expense to be recognized during the vesting period. During the years ended December 31, 2017, 2016, and 2015, we recorded charges of approximately $1.0 million, $1.0 million and $1.2 million in stock-based compensation, respectively. Stock-based compensation expense is a non-cash expense and such amounts are included as a component of general and administrative expense or operating expense based upon the classification of cash compensation paid to the related employees.
Income Taxes
Deferred tax assets and liabilities are established for temporary differences between the financial reporting basis and the tax basis of our assets and liabilities at tax rates in effect when such temporary differences are expected to reverse. We generally expect to fully utilize our deferred tax assets; however, when necessary, we record a valuation allowance to reduce our net deferred tax assets to the amount that is more likely than not to be realized.
In determining the need for a valuation allowance or the need for and magnitude of liabilities for uncertain tax positions, we make certain estimates and assumptions. These estimates and assumptions are based on, among other things, knowledge of operations, markets, historical trends and likely future changes and, when appropriate, the opinions of advisors with knowledge and expertise in certain fields. Due to certain risks associated with our estimates and assumptions, actual results could differ.
As a result of the Tax Act, we revaluated our net deferred tax assets, which led to an increase in our income tax expense by $5.5 million for the year ended December 31, 2017. The Company considers the accounting for the deferred tax re-measurements and other items to be complete, but ongoing accounting guidance and interpretation could result in adjustments to the consolidated financial statements. The Tax Act will decrease the corporate income tax rate from 35.0% to 21.0% beginning on January 1, 2018.
Contractual Obligations and Commercial Commitments
We have certain contractual obligations of continuing operations as of December 31, 2017, summarized by the period in which payment is due, as follows (dollar amounts in thousands):
Contractual Obligations | Total | Less than 1 year | 1 to 3 Years | 3 to 5 Years | After 5 Years | |||||||||||||||
Long-term debt obligations (1) | $ | 103,464 | $ | 17,906 | $ | 25,982 | $ | 59,576 | $ | — | ||||||||||
Settlement obligations (2) | 1,369 | 1,369 | — | — | — | |||||||||||||||
Elimination of Preferred Stock Conversion feature (3) | 515 | 515 | — | — | — | |||||||||||||||
Operating leases (4) | 1,065,640 | 58,046 | 119,988 | 123,475 | 764,131 | |||||||||||||||
Required capital expenditures under operating leases (5) | 11,911 | 1,216 | 2,433 | 2,433 | 5,829 | |||||||||||||||
Total | $ | 1,182,899 | $ | 79,052 | $ | 148,403 | $ | 185,484 | $ | 769,960 | ||||||||||
(1) | Long-term debt obligations include scheduled future payments of principal and interest of long-term debt and amounts outstanding on our capital lease obligations. Our long-term debt obligations increased $8.2 million between December 31, 2016 and December 31, 2017, which is related to assumption of operations for the Golden Living centers and purchase of the center in Selma, Alabama. See Note 5, "Long-Term Debt and Interest Rate Swap," to the consolidated financial statements included in this report for additional information. |
(2) | Settlement obligations relate to professional liability cases that are expected to be paid within the next twelve months. The professional liabilities are included in our current portion of self-insurance reserves. |
(3) | Payments to Omega, from whom we lease 35 nursing centers, for the elimination of the preferred stock conversion feature in connection with restructuring the preferred stock and master lease agreements. Monthly payments of approximately $0.1 million will be made through the end of the initial lease period that ends in September 2018. |
(4) | Represents lease payments under our operating lease agreements. Assumes all renewals periods are enacted. Our operating lease obligations decreased $66.2 million between December 31, 2016 and December 31, 2017. |
(5) | Includes annual expenditure requirements under operating leases. Our required capital expenditures decreased $1.3 million between December 31, 2016 and December 31, 2017. |
We have employment agreements with certain members of management that provide for the payment to these members of amounts up to two times their annual salary in the event of a termination without cause, a constructive discharge (as defined), or upon a change of control of the Company (as defined). The maximum contingent liability under these agreements is approximately $1.8 million as of December 31, 2017. The terms of such agreements are for one year and automatically renew for one year if not
33
terminated by us or the employee. In addition, upon the occurrence of any triggering event, those certain members of management may elect to require that we purchase equity awards granted to them for a purchase price equal to the difference in the fair market value of our common stock at the date of termination versus the stated equity award exercise price. Based on the closing price of our common stock on December 31, 2017, there is $0.4 million in contingent liabilities for the repurchase of the equity grants. No amounts have been accrued for these contingent liabilities.
Results of Operations
As discussed in the overview at the beginning of Management's Discussion and Analysis of Financial Condition and Results of Operations, we have completed certain divestitures, acquisitions and entered several new lease agreements. We have reclassified our Consolidated Financial Statements to present certain divestitures as discontinued operations for all periods presented. The following discussion only relates to our continuing operations.
(in thousands) | Year Ended December 31, | ||||||||||||||
2017 | 2016 | Change | % | ||||||||||||
PATIENT REVENUES, net | $ | 574,794 | $ | 426,063 | $ | 148,731 | 34.9 | % | |||||||
EXPENSES: | |||||||||||||||
Operating | 458,122 | 342,932 | 115,190 | 33.6 | % | ||||||||||
Lease and rent expense | 54,988 | 33,364 | 21,624 | 64.8 | % | ||||||||||
Professional liability | 10,764 | 8,456 | 2,308 | 27.3 | % | ||||||||||
General and administrative | 33,311 | 30,271 | 3,040 | 10.0 | % | ||||||||||
Depreciation and amortization | 10,902 | 8,292 | 2,610 | 31.5 | % | ||||||||||
Lease termination costs (receipts) | (180 | ) | 2,008 | (2,188 | ) | (109.0 | )% | ||||||||
Total expenses | 567,907 | 425,323 | 142,584 | 33.5 | % | ||||||||||
OPERATING INCOME | 6,887 | 740 | 6,147 | 830.7 | % | ||||||||||
OTHER INCOME (EXPENSE): | |||||||||||||||
Equity in net income of investment in unconsolidated affiliate | — | 273 | (273 | ) | (100.0 | )% | |||||||||
Gain on bargain purchase | 925 | — | 925 | 100.0 | % | ||||||||||
Gain on sale of investment in unconsolidated affiliate | 733 | 1,366 | (633 | ) | (46.3 | )% | |||||||||
Hurricane costs | (232 | ) | — | (232 | ) | (100.0 | )% | ||||||||
Interest expense, net | (6,369 | ) | (4,802 | ) | (1,567 | ) | (32.6 | )% | |||||||
Debt retirement costs | — | (351 | ) | 351 | 100.0 | % | |||||||||
(4,943 | ) | (3,514 | ) | (1,429 | ) | (40.7 | )% | ||||||||
INCOME (LOSS) FROM CONTINUING OPERATIONS BEFORE INCOME TAXES | 1,944 | (2,774 | ) | 4,718 | 170.1 | % | |||||||||
BENEFIT (PROVISION) FOR INCOME TAXES | (6,743 | ) | 1,030 | (7,773 | ) | (754.7 | )% | ||||||||
LOSS FROM CONTINUING OPERATIONS | $ | (4,799 | ) | $ | (1,744 | ) | $ | (3,055 | ) | (175.2 | )% | ||||
34
(in thousands) | Year Ended December 31, | ||||||||||||||
2016 | 2015 | Change | % | ||||||||||||
PATIENT REVENUES, net | $ | 426,063 | $ | 387,595 | $ | 38,468 | 9.9 | % | |||||||
EXPENSES: | |||||||||||||||
Operating | 342,932 | 311,035 | 31,897 | 10.3 | % | ||||||||||
Lease and rent expense | 33,364 | 28,690 | 4,674 | 16.3 | % | ||||||||||
Professional liability | 8,456 | 8,122 | 334 | 4.1 | % | ||||||||||
General and administrative | 30,271 | 24,793 | 5,478 | 22.1 | % | ||||||||||
Depreciation and amortization | 8,292 | 7,524 | 768 | 10.2 | % | ||||||||||
Lease termination costs | 2,008 | — | 2,008 | 100.0 | % | ||||||||||
Total expenses | 425,323 | 380,164 | 45,159 | 11.9 | % | ||||||||||
OPERATING INCOME | 740 | 7,431 | (6,691 | ) | (90.0 | )% | |||||||||
OTHER INCOME (EXPENSE): | |||||||||||||||
Equity in net income of investment in unconsolidated affiliate | 273 | 339 | (66 | ) | (19.5 | )% | |||||||||
Gain on sale of investment in unconsolidated affiliate | 1,366 | — | 1,366 | 100.0 | % | ||||||||||
Interest expense, net | (4,802 | ) | (4,102 | ) | (700 | ) | (17.1 | )% | |||||||
Debt retirement costs | (351 | ) | — | (351 | ) | (100.0 | )% | ||||||||
(3,514 | ) | (3,763 | ) | 249 | 6.6 | % | |||||||||
INCOME (LOSS) FROM CONTINUING OPERATIONS BEFORE INCOME TAXES | (2,774 | ) | 3,668 | (6,442 | ) | (175.6 | )% | ||||||||
PROVISION FOR INCOME TAXES | 1,030 | (916 | ) | 1,946 | 212.4 | % | |||||||||
INCOME (LOSS) FROM CONTINUING OPERATIONS | $ | (1,744 | ) | $ | 2,752 | $ | (4,496 | ) | (163.4 | )% | |||||
Year Ended December 31, 2017 Compared With Year Ended December 31, 2016
Patient Revenues
Patient revenues were $574.8 million in 2017 and $426.1 million in 2016, an increase of $148.7 million or 34.9%. This increase is primarily attributable to the acquisition of Golden Living operations in Alabama and Mississippi during the fourth quarter of 2016. The following table summarizes the revenue increases attributable to our portfolio growth (in thousands):
Year Ended December 31, | |||||||||||
2017 | 2016 | Change | |||||||||
Same-store revenue | $ | 386,576 | $ | 388,890 | $ | (2,314 | ) | ||||
2016 acquisition revenue | 183,665 | 37,173 | 146,492 | ||||||||
2017 acquisition revenue | 4,553 | — | 4,553 | ||||||||
Total revenue | $ | 574,794 | $ | 426,063 | 148,731 | ||||||
The overall increase in revenue of $148.7 million is primarily attributable to revenue contributions from the acquisition of Golden Living operations in Alabama and Mississippi during the fourth quarter of 2016 of $146.5 million and Park Place during the third quarter of 2017 of $4.6 million. The increase from the acquisition activity was partially offset by a decrease in same-store revenue of $2.3 million which is explained in more detail below.
35
The following table summarizes key revenue and census statistics for continuing operations for each period:
Year Ended December 31, | |||||||||
2017 | 2016 | ||||||||
Skilled nursing occupancy | 79.7 | % | 78.1 | % | |||||
As a percent of total census: | |||||||||
Medicaid census | 69.1 | % | 68.1 | % | |||||
Medicare census | 11.2 | % | 11.7 | % | |||||
Managed Care census | 3.9 | % | 3.5 | % | |||||
As a percent of total revenues: | |||||||||
Medicaid revenues | 52.4 | % | 50.6 | % | |||||
Medicare revenues | 25.9 | % | 27.5 | % | |||||
Managed Care revenues | 7.4 | % | 6.8 | % | |||||
Average rate per day: | |||||||||
Medicare | $ | 454.22 | $ | 456.30 | |||||
Medicaid | $ | 175.58 | $ | 169.91 | |||||
Managed Care | $ | 381.46 | $ | 385.71 | |||||
The average Medicaid rate per patient day for same-store nursing centers in 2017 increased 1.7% compared to 2016, resulting in an increase in revenue of $3.3 million. This average rate per day for Medicaid patients is the result of rate increases in certain states and increasing patient acuity levels. The average Medicare rate per patient day for same-store nursing centers in 2017 increased 1.6% compared to 2016, resulting in an increase in revenue of $1.5 million also related to our ability to attract and provide care for patients with increased acuity levels.
Our total average daily census increased by approximately 33.9% for the full portfolio compared to 2016 on a consolidated basis, but was primarily attributable to the aforementioned acquisition activity. On a same-store basis, our Medicare, Medicaid and Private average daily census for 2017 decreased compared to 2016, resulting in decreases in revenue of $5.0 million, $1.4 million and $2.2 million, respectively. Conversely, our Managed Care average daily census increased in 2017 compared to 2016 by $2.0 million.
Our same-store centers for 2017 experienced one less day of operations compared to 2016, resulting in a decrease in revenue of $1.0 million or 2.7%.
Operating Expense
Operating expense increased to $458.1 million in 2017 from $342.9 million in 2016, driven primarily by the $115.9 million in operating costs from the Golden Living nursing centers added in 2016, and $3.6 million from the center acquired in 2017. Operating expense decreased to 79.7% of revenue in 2017, compared to 80.5% of revenue in 2016.
Year Ended December 31, | |||||||||||
2017 | 2016 | Change | |||||||||
Same-store operating expenses | $ | 310,571 | $ | 314,944 | $ | (4,373 | ) | ||||
2016 acquisition operating expenses | 143,911 | 27,988 | 115,923 | ||||||||
2017 acquisition operating expenses | 3,640 | — | 3,640 | ||||||||
Total operating expenses | $ | 458,122 | $ | 342,932 | 115,190 | ||||||
The largest component of operating expenses is wages, which increased to $268.4 million in 2017 from $199.6 million in 2016, an increase of $68.8 million, or 34.4%.
On a same-store center basis, operating expenses decreased $4.4 million, which is primarily attributable to a decrease in our bad debt expense by $1.1 million and a provider tax refund of $2.8 million from the state of Kentucky. Our same-store nursing and ancillary and dietary expenses decreased by $0.1 million and $0.3 million, respectively. Conversely, these positive variances were
36
slightly offset by an increase in salaries and related taxes of $1.0 million in 2017. However, due to one less day of operations in 2017, we experienced $0.5 million less in salaries and related taxes.
Lease Expense
Lease expense increased to $55.0 million in 2017 from $33.4 million in 2016, an increase of $21.6 million, or 64.8%. The increase in lease expense was driven by $22.1 million from the assumption of the Golden Living centers in the fourth quarter of 2016. This was slightly offset from the termination of the Carthage, Mississippi lease in September 2017.
Professional Liability
Professional liability expense was $10.8 million in 2017 compared to $8.5 million in 2016, an increase of $2.3 million, or 27.3%. As centers have been acquired in 2016 and 2017, the Company has accessed commercial insurance markets, which accounts for a significant portion of the growth in professional liability expense in the current year. We were engaged in 72 professional liability lawsuits as of December 31, 2017, compared to 67 as of December 31, 2016. Our cash expenditures for professional liability costs of continuing operations were $6.6 million and $4.5 million for 2017 and 2016, respectively. Professional liability expense and cash expenditures fluctuate from year to year based respectively on the results of our third-party professional liability actuarial studies, the premium costs of purchased insurance, and on the costs incurred in defending and settling existing claims. See “Liquidity and Capital Resources” for further discussion of the accrual for professional liability.
General and Administrative Expense
General and administrative expenses were approximately $33.3 million in 2017 compared to $30.3 million in 2016, an increase of $3.0 million, or 10.0%. The overall increase in general and administrative expenses were attributable to a $3.7 million increase in salaries and related expenses associated with continued growth at the regional level, as well as additional corporate infrastructure to support the on-going growth of the portfolio. Legal expenses decreased by $0.7 million in 2017 compared to 2016, which is attributable to the 2016 acquisitions.
Depreciation and Amortization
Depreciation and amortization expense was approximately $10.9 million in 2017 and $8.3 million in 2016. The Company incurred an increase of $2.1 million in depreciation and amortization expenses related to capital expenditures for the assumed Golden Living operations in the fourth quarter of 2016.
Lease termination costs (receipts)
The Company ceased operations at our Carthage, Mississippi, center in September 2017, which resulted in a $0.2 million cash termination receipt, net of legal costs. Lease termination costs were $2.0 million in 2016 due to the termination of the Avon, Ohio operating lease in May 2016.
Gain on bargain purchase
The Company acquired the operations and assets of a center in Selma, Alabama in July 2017. In connection with the business combination, we recognized a $0.9 million gain on bargain purchase.
Gain on sale of investment in unconsolidated affiliate
The sale of the pharmacy joint venture resulted in a $1.4 million gain in the fourth quarter of 2016. Subsequently, we recognized an additional gain of $0.7 million in the first quarter of 2017, related to the continuing liquidation of remaining net assets affiliated with the partnership.
Interest Expense, Net
Interest expense has increased to $6.4 million in 2017 compared to $4.8 million in 2016, an increase of $1.6 million. The increase was primarily attributable to higher debt balances in 2017 as a result of additional borrowings made during the change in ownership processes for the newly acquired centers in Alabama and Mississippi, and the amendment of the term loan facility that occurred in June 2017.
Debt retirement costs
Debt retirement costs were $0.4 million in 2016, which relates to the write off of our term loan deferred financing costs, as a result of our debt refinance that took place in February 2016.
Income (loss) from Continuing Operations before Income Taxes; Income (loss) from Continuing Operations per Common Share
37
As a result of the above, continuing operations reported income before taxes of $1.9 million in 2017, as compared to loss before taxes of $2.8 million in 2016. The provision for income taxes was $6.7 million in 2017, an effective rate of 346.9% and the provision for income taxes was $1.0 million in 2016, an effective rate of 37.1%. The higher effective tax rate reflects the impact of our revaluation of our net deferred tax assets of $5.5 million as a result of the Tax Act. The basic and diluted loss per common share from continuing operations were $0.76 and $0.76 in 2017, respectively, compared to a basic and diluted loss per common share from continuing operations of $0.28 and $0.28 in 2016, respectively.
38
Year Ended December 31, 2016 Compared With Year Ended December 31, 2015
Patient Revenues
Patient revenues were $426.1 million in 2016 and $387.6 million in 2015, an increase of $38.5 million or 9.9%. This increase is primarily attributable to the acquisition of Golden Living operations in Alabama and Mississippi during the fourth quarter of 2016. The following table summarizes the revenue increases attributable to our portfolio growth (in thousands):
Year Ended December 31, | |||||||||||
2016 | 2015 | Change | |||||||||
Same-store revenue | $ | 372,452 | $ | 376,497 | $ | (4,045 | ) | ||||
2015 acquisition revenue | 16,438 | 11,098 | 5,340 | ||||||||
2016 acquisition revenue | 37,173 | — | 37,173 | ||||||||
Total revenue | $ | 426,063 | $ | 387,595 | 38,468 | ||||||
The overall increase in revenue of $38.5 million is primarily attributable to revenue contributions from the acquisition of Golden Living operations in Alabama and Mississippi during the fourth quarter of 2016 of $37.2 million. Additionally, the 2015 acquisitions experienced an incremental increase in revenues of $5.3 million as a result of having a full year in operations during 2016. The increase from the acquisition activity was partially offset by a decrease in same-store revenue of $4.0 million which is explained in more detail below.
The following table summarizes key revenue and census statistics for continuing operations for each period:
Year Ended December 31, | |||||||||
2016 | 2015 | ||||||||
Skilled nursing occupancy | 78.1 | % | 77.1 | % | |||||
As a percent of total census: | |||||||||
Medicaid census | 68.1 | % | 67.1 | % | |||||
Medicare census | 11.7 | % | 12.5 | % | |||||
Managed Care census | 3.5 | % | 3.7 | % | |||||
As a percent of total revenues: | |||||||||
Medicaid revenues | 50.6 | % | 48.6 | % | |||||
Medicare revenues | 27.5 | % | 29.0 | % | |||||
Managed Care revenues | 6.8 | % | 7.2 | % | |||||
Average rate per day: | |||||||||
Medicare | $ | 456.30 | $ | 455.24 | |||||
Medicaid | $ | 169.91 | $ | 166.16 | |||||
Managed Care | $ | 385.71 | $ | 389.73 | |||||
The average Medicaid rate per patient day for same-store nursing centers in 2016 increased 1.2% compared to 2015, resulting in an increase in revenue of $2.2 million. This average rate per day for Medicaid patients is the result of rate increases in certain states and increasing patient acuity levels. The average Medicare rate per patient day for same-store nursing centers in 2016 increased 1.0% compared to 2015, resulting in an increase in revenue of $0.9 million also related to our ability to attract and provide care for patients with increased acuity levels. Same-store Private payors rate per patient day for 2016 also experienced favorable results compared to 2015 resulting in a $1.0 million increase in revenue.
Our total average daily census increased by approximately 9.4% for the full portfolio compared to 2015 on a consolidated basis, but was primarily attributable to the aforementioned acquisition activity. On a same-store basis, our Medicare and Medicaid average daily census for 2016 decreased compared to 2015, resulting in decreases in revenue of $7.5 million and $0.8 million, respectively.
39
Operating Expense
Operating expense increased to $342.9 million in 2016 from $311.0 million in 2015, driven primarily by the $28.0 million in operating costs at the Golden Living nursing centers added in 2016, and $3.6 million incremental increase from the centers acquired in 2015 due to a full year of operations. Operating expense increased to 80.5% of revenue in 2016, compared to 80.2% of revenue in 2015.
Year Ended December 31, | |||||||||||
2016 | 2015 | Change | |||||||||
Same-store operating expenses | $ | 301,991 | $ | 301,720 | $ | 271 | |||||
2015 acquisition operating expenses | 12,953 | 9,315 | 3,638 | ||||||||
2016 acquisition operating expenses | 27,988 | — | 27,988 | ||||||||
Total operating expenses | $ | 342,932 | $ | 311,035 | 31,897 | ||||||
The largest component of operating expenses is wages, which increased to $199.6 million in 2016 from $180.8 million in 2015, an increase of $18.8 million, or 10.4%. On a same-store basis, wages were controlled and increased by $0.4 million to $175.8 million in 2016 from $175.4 million in 2015, which is a direct result from our decrease in same-store revenues during 2016.
Other factors driving the fluctuation in operating expenses at the same-store nursing centers include an increase in health insurance premiums by $1.2 million, which was offset by a $1.2 million decrease in nursing and ancillary related expenses. Bad debt expenses decreased by $0.3 million. This fluctuation was driven significantly by the growth in Medicare and Medicaid patients undergoing the initial qualification process.
Lease Expense
Lease expense increased to $33.4 million in 2016 from $28.7 million in 2015, an increase of $4.7 million, or 16.3%. The increase in lease expense was driven by $5.7 million from the assumption of the Golden Living centers in the fourth quarter of 2016. This was slightly offset from the purchase of Clinton and Hutchinson in February 2016, and the termination of the Avon, Ohio lease in May 2016.
Professional Liability
Professional liability expense was $8.5 million in 2016 compared to $8.1 million in 2015, an increase of $0.4 million, or 4.1%. As centers have been acquired in 2015 and 2016, the Company has accessed commercial insurance markets, which accounts for a significant portion of the growth in professional liability expense in the current year. We were engaged in 67 professional liability lawsuits as of December 31, 2016, compared to 55 as of December 31, 2015. Our cash expenditures for professional liability costs of continuing operations were $4.5 million and $3.3 million for 2016 and 2015, respectively. Professional liability expense and cash expenditures fluctuate from year to year based respectively on the results of our third-party professional liability actuarial studies, the premium costs of purchased insurance, and on the costs incurred in defending and settling existing claims. See “Liquidity and Capital Resources” for further discussion of the accrual for professional liability.
General and Administrative Expense
General and administrative expenses were approximately $30.3 million in 2016 compared to $24.8 million in 2015, an increase of $5.5 million, or 22.1%. The overall increase in general and administrative expenses were attributable to a $1.6 million increase in salaries and related expenses associated with continued growth at the regional level, as well as additional corporate infrastructure to support the on-going growth of the portfolio. Legal and consulting fees experienced an increase of $1.2 million and $1.3 million, respectively, related to regulatory and acquisition expenses.
Depreciation and Amortization
Depreciation and amortization expense was approximately $8.3 million in 2016 and $7.5 million in 2015. The increase in 2016 is primarily due to $0.4 million of depreciation associated with the purchases of Hutchinson and Clinton in February 2016. Additionally, the Company incurred an increase of $0.3 million in depreciation and amortization expenses related to the assumed Golden Living operations in the fourth quarter of 2016.
Lease termination costs
Lease termination costs were $2.0 million in 2016 due to the termination of the Avon, Ohio operating lease in May 2016.
40
Gain on sale of investment in unconsolidated affiliate
Gain on the sale of the pharmacy joint venture was $1.4 million, which occurred in the fourth quarter of 2016. This transaction also resulted in an immaterial gain contingency, which has not been recorded and income has not been recognized.
Interest Expense, Net
Interest expense has increased to $4.8 million in 2016 compared to $4.1 million in 2015, an increase of $0.7 million. The increase was primarily attributable to higher debt balances in 2016 as a result of higher outstanding borrowings on the revolving credit facility from the purchase of Hutchinson and Clinton during the first quarter of 2016, as well as a result of the change in ownership processes for the newly acquired Golden Living centers.
Debt retirement costs
Debt retirement costs were $0.4 million in 2016, which relates to the write off of our term loan deferred financing costs, as a result of our debt refinance that took place in February 2016.
Income (loss) from Continuing Operations before Income Taxes; Income (loss) from Continuing Operations per Common Share
As a result of the above, continuing operations reported a loss before taxes of $2.8 million in 2016, as compared to income of $3.7 million in 2015. The benefit for income taxes was $1.0 million in 2016, an effective rate of 37.1% and the provision for income taxes was $0.9 million in 2015, an effective rate of 25.0%. The increase in our effective tax rate is due to an increase in our Work Opportunity Tax Credit ("WOTC") and the valuation allowance. The basic and diluted loss per common share from continuing operations were $0.28 and $0.28 in 2016, respectively, compared to a basic and diluted income per common share from continuing operations of $0.45 and $0.44 in 2015, respectively.
Liquidity and Capital Resources
Liquidity
Our primary source of liquidity is the net cash flows provided by the operating activities of our centers. These internally generated cash flows are used to service existing debt obligations, fund required capital expenditures as well as provide cash flows for investing opportunities. In determining priorities for our cash flow, we evaluate alternatives available to us and select the ones that we believe will most benefit us over the long term. Options for our cash include, but are not limited to, capital improvements, dividends, repurchase of additional shares of our common stock, acquisitions, and payment of existing debt obligations, as well as initiatives to improve nursing center performance. We review these potential uses and align them to our cash flows with a goal of achieving long-term success.
Net cash provided by operating activities of continuing operations totaled $13.4 million in 2017, compared to net cash used in operating activities of continuing operations of $2.1 million in 2016 and net cash provided by operating activities of continuing operations of $10.3 million in 2015. One primary driver of the increase in cash provided by operating activities from continuing operations is related to the Company completing the Change in Ownership ("CHOW") process for the nursing centers acquired in the fourth quarter of 2016, which increased the cash inflows from these centers. Operating activities of centers we no longer operate used cash of $1.3 million, $3.5 million and $7.0 million in 2017, 2016 and 2015, respectively.
Our cash expenditures related to professional liability claims of continuing operations were $6.6 million, $4.5 million and $3.3 million for 2017, 2016 and 2015, respectively. We also continue to experience cash expenditures related to professional liability claims of discontinued operations. Our cash expenditures related to professional liability claims of centers we no longer operate were $1.3 million, $3.6 million, and $8.2 million for 2017, 2016 and 2015, respectively. The Company will continue to defend, and make cash payments when required related to, professional liability claims asserted against centers we no longer operate. Although we work diligently to limit the cash required to settle and defend professional liability claims, a significant judgment entered against us in one or more legal actions could have a material adverse impact on our cash flows and could result in our being unable to meet all of our cash needs as they become due.
Investing activities of continuing operations used cash of $17.4 million, $9.8 million and $13.1 million in 2017, 2016 and 2015, respectively. The cash used in 2017 is primarily attributable to the asset purchase of Park Place in Selma, Alabama in July 2017 for $8.8 million, and capital expenditures related to our 2016 acquisitions. The cash used in 2016 was the result of the purchase of Hutchinson and Clinton for $4.3 million and $3.3 million, respectively, and cash used to assume the operations of the twenty-two Golden Living centers in the fourth quarter of 2016. The cash used in 2015 is primarily attributable to the $7.0 million and $3.9 million of assets purchased in the Glasgow and Fulton transactions, respectively. We have used $9.7 million, $6.0 million, and $4.6 million in 2017, 2016 and 2015, respectively, for capital expenditures of continuing operations.
Financing activities of continuing operations provided cash of $4.6 million, $15.1 million and $10.6 million in 2017, 2016 and 2015. Cash provided by financing activities in 2017 is primarily due to draws on the Company's revolving credit facility of $21.0
41
million, acquisition revolver of $8.5 million and amending our credit facility resulting in proceeds of $7.5 million. The proceeds received were offset by repayments of $30.2 million. Cash provided by financing activiteis in 2016 is primarily attributable to the proceeds received from refinancing our credit facility resulting in proceeds of $92.8 million, offset by the repayment of the existing mortgage loan and other debt payments during the year of $73.4 million. Financing activities in 2015 reflect the proceeds received from refinancing our credit facility resulting in proceeds of $27.9 million, offset by the repayment of the existing mortgage loan and other debt payments during the year of $15.3 million. Financing activities reflect common stock of $1.4 million 2017, $1.4 million in 2016, and $1.3 million in 2015.
Dividends
On February 22, 2018, the Board of Directors declared a quarterly dividend on common shares of $0.055 per share. While the Board of Directors intends to pay quarterly dividends, the Board will make the determination of the amount of future cash dividends, if any, to be declared and paid based on, among other things, the Company’s financial condition, funds from operations, the level of its capital expenditures and its future business prospects and opportunities. The Company is restricted by its debt agreements in its ability to pay dividends.
Professional Liability
The Company has professional liability insurance coverage for its nursing centers that, based on historical claims experience, is likely to be substantially less than the claims that are expected to be incurred. Effective July 1, 2013, the Company established a wholly-owned, consolidated offshore limited purpose insurance subsidiary, SHC, which has issued a policy insuring claims made against all of the Company's nursing centers in Florida and Tennessee, the Company’s formerly operated Arkansas and West Virginia centers, and several of the Company’s nursing centers in Alabama, Kentucky, Ohio, and Texas. The insurance coverage provided for these centers under the SHC policy include coverage limits of $500,000 or $1,000,000 per medical incident with a sublimit per center of $1,000,000 and total annual aggregate policy limits of $5,000,000. All other centers within the Company’s portfolio are covered through various commercial insurance policies which provide coverage limits of $1,000,000 per claim and have sublimits of $3,000,000 per center, with varying aggregate policy limits and deductibles. The deductibles for these policies are covered through the insurance subsidiary.
As of December 31, 2017, we have recorded total liabilities for reported professional liability claims and estimates for incurred, but unreported claims of $20.1 million. Our calculation of this estimated liability is based on the Company's best estimates of the likelihood of adverse judgments with respect to any asserted claim; however, a significant judgment could be entered against us in one or more of these legal actions, and such a judgment could have a material adverse impact on our financial position and cash flows.
Capital Resources
As of December 31, 2017, we had $89.6 million of outstanding long-term debt and capital lease obligations. The $89.6 million total includes $1.4 million in capital lease obligations. The balance of the long-term debt is comprised of $64.6 million owed on our collateralized mortgage debt, $16.0 million currently outstanding on the revolving credit facility, and $7.5 million on the acquisition loan facility.
Under the terms of the agreements, the syndicate of banks provided the Amended Mortgage Loan with an original balance of $72.5 million with a five year maturity through February 26, 2021, consisting of $60.0 million term and $12.5 million acquisition loan facilities, and a $52.3 million Amended Revolver through February 26, 2021. The Amended Mortgage Loan has a term of five years, with principal and interest payable monthly based on a 25 year amortization. Interest on the term and acquisition loan facilities are based on LIBOR plus 4.0% and 4.75%, respectively. A portion of the Amended Mortgage Loan is effectively fixed at 5.79% pursuant to an interest rate swap with an initial notional amount of $30.0 million. The Amended Mortgage Loan balance was $72.1 million as of December 31, 2017, consisting of $64.6 million on the term loan facility with an interest rate of 5.5% and $7.5 million on the acquisition loan facility with an interest rate of 6.25%. The Amended Mortgage Loan is secured by 18 owned nursing centers, related equipment and a lien on the accounts receivable of these centers. The Amended Mortgage Loan and the Amended Revolver are cross-collateralized and cross-defaulted. The Company's Amended Revolver has an interest rate of LIBOR plus 4.0% and is secured by accounts receivable and is subject to limits on the maximum amount of loans that can be outstanding under the revolver based on borrowing base restrictions. Eligible accounts receivable are calculated as defined and consider 80% of certain net receivables while excluding receivables from private pay patients, those pending approval by Medicaid and receivables greater than 120 days.
As of December 31, 2017, the Company had $16.0 million borrowings outstanding under the Amended Revolver compared to $15.0 million outstanding as of December 31, 2016. The outstanding borrowings on the revolver primarily reflect the Company's approach to accumulated Medicaid and Medicare receivables at recently acquired centers as these centers proceed through the
42
change in ownership process with CMS. Annual fees for letters of credit issued under the Amended Revolver are 3.0% of the amount outstanding. The Company has letters of credit of $4.8 million and $6.2 million to serve as a security deposit for our Omega and Golden Living leases, respectively. Finally, we have nine other letters of credit, totaling $2.4 million, to serve as security deposits at certain centers. Considering the balance of eligible accounts receivable at December 31, 2017, the letters of credit, the amounts outstanding under the revolving credit facility and the maximum loan amount of $39.3 million, the balance available for borrowing under the Amended Revolver is $9.9 million at December 31, 2017.
Our lending agreements contain various financial covenants, the most restrictive of which relate to debt service coverage ratios. We are in compliance with all such covenants at December 31, 2017.
Our calculated compliance with financial covenants is presented below:
Requirement | Level at December 31, 2017 | ||
Minimum fixed charge coverage ratio | 1.05:1.00 | 1.07:1.05 | |
Minimum adjusted EBITDA | $13.0 million | $18.3 million | |
EBITDAR (mortgaged centers) | $10.0 million | $16.3 million | |
Current ratio (as defined in agreement) | 1.00:1.00 | 1.22:1.00 | |
As part of the debt agreements entered into in February 2016, the Company entered into an interest rate swap agreement with a member of the bank syndicate as the counterparty. The interest rate swap agreement has the same effective date and maturity date as the Amended Mortgage Loan, and carries an initial notional amount of $30.0 million. The interest rate swap agreement requires the Company to make fixed rate payments to the bank calculated on the applicable notional amount at an annual fixed rate of 5.79% while the bank is obligated to make payments to us based on LIBOR on the same notional amounts. We entered into the interest rate swap agreement to mitigate the variable interest rate risk on our outstanding mortgage borrowings.
Capitalized Lease Obligations
Upon acquisition of certain centers, we assume certain leases, primarily related to equipment, that constitute capital leases. Additionally, the Company leases certain technology equipment that supports the clinical systems, including electronic medical records, at our nursing centers that constitute capital leases.
As a result of the lease agreements above, we have recorded the underlying lease assets and capitalized lease obligations of $1.4 million, $2.1 million, and $0.6 million as of December 31, 2017, 2016, and 2015, respectively. These lease agreements provide terms of three to five years.
Receivables
Our operations could be adversely affected if we experience significant delays in reimbursement from Medicare, Medicaid and other third-party revenue sources. Our future liquidity will continue to be dependent upon the relative amounts of current assets (principally cash, accounts receivable and inventories) and current liabilities (principally accounts payable and accrued expenses). In that regard, accounts receivable can have a significant impact on our liquidity. Continued efforts by governmental and third-party payors to contain or reduce the acceleration of costs by monitoring reimbursement rates, by increasing medical review of bills for services, or by negotiating reduced contract rates, as well as any delay by us in the processing of our invoices, could adversely affect our liquidity and financial position.
Gross accounts receivable attributable to patient services of continuing operations totaled $79.2 million at December 31, 2017 compared to $72.5 million at December 31, 2016, representing approximately 49 days and 47 days revenue in accounts receivable, respectively. The balance as of December 31, 2017 reflects a full year of ownership of the twenty-two newly leased Golden Living centers in Alabama and Mississippi. The Company has completed the change in ownership process and is utilizing our billing credentials to perform the billing of the Medicare and Medicaid receivables.
43
The allowance for bad debt was $14.2 million and $10.3 million at December 31, 2017 and 2016, respectively, which is commensurate with our overall revenue and receivables growth. We continually evaluate the adequacy of our bad debt reserves based on patient mix trends, aging of older balances, payment terms and delays with regard to third-party payors, collateral and deposit resources, as well as other factors. We continue to evaluate and implement additional procedures to strengthen our collection efforts and reduce the incidence of uncollectible accounts.
Inflation
Based on contract pricing for food and other supplies and recent market conditions, we expect cost increases in 2018 to be relatively the same or slightly lower than the increases in 2017. We expect salary and wage increases for our skilled health care providers to continue to be higher than average salary and wage increases, as is common in the healthcare industry.
Off-Balance Sheet Arrangements
We have eleven letters of credit outstanding totaling approximately $13.4 million as of December 31, 2017. Eleven of these letters of credit serve as a security deposits for certain center leases, while one was issued in conjunction with the initial funding of our wholly-owned captive insurance company. The letters of credit were issued under our revolving credit facility. Our accounts receivable serve as the collateral for this revolving credit facility.
Forward-Looking Statements
The foregoing discussion and analysis provides information deemed by management to be relevant to an assessment and understanding of our consolidated results of operations and financial condition. This discussion and analysis should be read in conjunction with our consolidated financial statements included herein. Certain statements made by or on behalf of us, including those contained in this “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and elsewhere, are forward-looking statements as defined in the Private Securities Litigation Reform Act of 1995. Actual results could differ materially from those contemplated by the forward-looking statements made herein. Forward-looking statements are predictive in nature and are frequently identified by the use of terms such as "may," "will," "should," "expect," "believe," "estimate," "intend," and similar words indicating possible future expectations, events or actions. In addition to any assumptions and other factors referred to specifically in connection with such statements, other factors, many of which are beyond our ability to control or predict, could cause our actual results to differ materially from the results expressed or implied in any forward-looking statements including, but not limited to:
• | our ability to successfully integrate the operations of our new nursing centers in Alabama and Mississippi, as well as successfully operate all of our centers, |
• | our ability to increase census and occupancy rates at our centers, |
• | changes in governmental reimbursement, |
• | government regulation, |
• | the impact of the Affordable Care Act, efforts to repeal or significantly modify the Affordable Care Act, and other health care reform initiatives, |
• | any increases in the cost of borrowing under our credit agreements, |
• | our ability to comply with covenants contained in those credit agreements, |
• | our ability to comply with the terms of our master lease agreements, |
• | our ability to renew or extend our leases at or prior to the end of the existing lease terms, |
• | the outcome of professional liability lawsuits and claims, |
• | our ability to control ultimate professional liability costs, |
• | the accuracy of our estimate of our anticipated professional liability expense, |
• | the impact of future licensing surveys, |
• | the outcome of proceedings alleging violations of state or federal False Claims Acts, |
• | laws and regulations governing quality of care or other laws and regulations applicable to our business including HIPAA and laws governing reimbursement from government payors, |
• | the costs of investing in our business initiatives and development, |
• | our ability to control costs, |
• | our ability to attract and retain qualified healthcare professionals, |
• | changes to our valuation of deferred tax assets, |
44
• | changing economic and competitive conditions, |
• | changes in anticipated revenue and cost growth, |
• | changes in the anticipated results of operations, |
• | the effect of changes in accounting policies as well as others. |
Investors also should refer to the risks identified in this “Management's Discussion and Analysis of Financial Condition and Results of Operations” as well as risks identified in “Part I. Item 1A. Risk Factors” for a discussion of various risk factors of the Company and that are inherent in the health care industry. Given these risks and uncertainties, we can give no assurances that these forward-looking statements will, in fact, transpire and, therefore, caution investors not to place undue reliance on them. These assumptions may not materialize to the extent assumed, and risks and uncertainties may cause actual results to be different from anticipated results. These risks and uncertainties also may result in changes to the Company’s business plans and prospects. Such cautionary statements identify important factors that could cause our actual results to materially differ from those projected in forward-looking statements. In addition, we disclaim any intent or obligation to update these forward-looking statements.
ITEM 7A. QUANTITATIVE AND QUALITATIVE DISCLOSURES ABOUT MARKET RISK
The chief market risk factor affecting our financial condition and operating results is interest rate risk. As of December 31, 2017, we had outstanding borrowings of approximately $88.1 million, $52.1 million of which were subject to variable interest rates. In connection with February 2016 financing agreement, we entered into an interest rate swap with respect to one half of the Amended Mortgage Loan to mitigate the floating interest rate risk of such borrowing. In the event that interest rates were to change 1%, the impact on future pre-tax cash flows would be approximately $0.6 million annually, representing the impact of increased or decreased interest expense on variable rate debt.
ITEM 8. FINANCIAL STATEMENTS AND SUPPLEMENTARY DATA
Audited financial statements are contained on pages F-1 through F-31 of this Annual Report on Form 10-K and are incorporated herein by reference. Audited supplemental schedule data is contained on pages S-1 through S-2 of this Annual Report on Form 10-K and is incorporated herein by reference.
ITEM 9. CHANGES IN AND DISAGREEMENTS WITH ACCOUNTANTS ON ACCOUNTING AND FINANCIAL DISCLOSURE
Not applicable.
ITEM 9A. CONTROLS AND PROCEDURES
Diversicare, with the participation of our principal executive and financial officers, has evaluated the effectiveness of our disclosure controls and procedures, as such term is defined under Rules 13a-15(e) and 15d-15(e) promulgated under the Securities Exchange Act of 1934, as amended, as of December 31, 2017. Based on this evaluation, the principal executive and financial officers have determined that such disclosure controls and procedures are effective to ensure that information required to be disclosed in our filings under the Securities Exchange Act of 1934 is recorded, processed, summarized and reported within the time periods specified in the Securities Exchange Commission's rules and forms.
Management's Report on Internal Control over Financial Reporting
Our management is responsible for establishing and maintaining adequate internal control over financial reporting (as defined in Rule 13a-15(f) under the Securities Exchange Act of 1934, as amended). Our management conducted an evaluation of the effectiveness of our internal control over financial reporting based on the framework in Internal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (2013 framework). Based on this evaluation, management concluded that our internal control over financial reporting was effective as of December 31, 2017. Management reviewed the results of its assessment with our Audit Committee.
Changes in Internal Control over Financial Reporting
There has been no change (including corrective actions with regard to significant deficiencies or material weaknesses) in our internal control over financial reporting that has occurred during our fiscal quarter ended December 31, 2017 that has materially affected, or is reasonably likely to materially affect, our internal control over financial reporting.
Our management does not expect that our disclosure controls and procedures or our internal controls will prevent all errors and all fraud. A control system, no matter how well conceived and operated, can provide only reasonable, not absolute, assurance that the objectives of the control system are met. Further, the design of a control system must reflect the fact that there are resource
45
constraints, and the benefit of controls must be considered relative to their costs. Because of the inherent limitations in all control systems, no evaluation of controls can provide absolute assurance that misstatements due to error or fraud will not occur or that all control issues and instances of fraud, if any, have been detected. These inherent limitations include the realities that judgments in decision making can be faulty and that breakdowns can occur because of simple error or mistake. Controls can also be circumvented by the individual acts of some persons, by collusion of two or more people, or by management override of the controls. The design of any system of controls is based in part on certain assumptions about the likelihood of future events and there can be no assurance that any design will succeed in achieving its stated goals under all potential future conditions.
ITEM 9B. OTHER INFORMATION
Effective February 27, 2018, the Company executed a Fifth Amendment to the Amended Revolver and a Third Amendment to the Amended Mortgage Loan with a syndicate of financial institutions and banks, including CIBC BANK USA (formerly known as The PrivateBank and Trust Company), the administrative agent. Under the terms of the Amendments, the minimum fixed charge coverage ratio shall not be less than 1.01 to 1.00 for the quarter ending March 31, 2018 and for each quarter thereafter.
46
PART III
ITEM 10. DIRECTORS, EXECUTIVE OFFICERS AND CORPORATE GOVERNANCE
Information concerning our Directors, Executive Officers and Corporate Governance is incorporated herein by reference to our definitive proxy statement for our 2018 Annual Meeting of Shareholders, which we will file within 120 days of the end of the fiscal year to which this Report relates.
ITEM 11. EXECUTIVE COMPENSATION
Information concerning Executive Compensation is incorporated herein by reference to our definitive proxy statement for our 2018 Annual Meeting of Shareholders, which we will file within 120 days of the end of the fiscal year to which this Report relates.
ITEM 12. SECURITY OWNERSHIP OF CERTAIN BENEFICIAL OWNERS AND MANAGEMENT AND RELATED SHAREHOLDER MATTERS
Information concerning Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters is incorporated herein by reference to our definitive proxy statement for our 2018 Annual Meeting of Shareholders, which we will file within 120 days of the end of the fiscal year to which this Report relates.
ITEM 13. CERTAIN RELATIONSHIPS AND RELATED TRANSACTIONS, AND DIRECTOR INDEPENDENCE
Information concerning Certain Relationships and Related Transactions, and Director Independence is incorporated herein by reference to our definitive proxy statement for our 2018 Annual Meeting of Shareholders, which we will file within 120 days of the end of the fiscal year to which this Report relates.
ITEM 14. PRINCIPAL ACCOUNTANT FEES AND SERVICES
Information concerning the fees and services provided by our principal accountant is incorporated herein by reference to our definitive proxy statement for our 2018 Annual Meeting of Shareholders, which we will file within 120 days of the end of the fiscal year to which this Report relates.
47
PART IV
ITEM 15. EXHIBITS, FINANCIAL STATEMENT SCHEDULES
The Financial statements and schedule for us and our subsidiaries required to be included in Part II, Item 8 are listed below.
Form 10-K Pages | |
Financial Statements | |
Report of Independent Registered Public Accounting Firm | F-1 |
Consolidated Balance Sheets as of December 31, 2017 and 2016 | F-2 |
Consolidated Statements of Operations for the Years Ended December 31, 2017, 2016 and 2015 | F-3 |
Consolidated Statements of Comprehensive Income (Loss) for the Years Ended December 31, 2017, 2016 and 2015 | F-4 |
Consolidated Statements of Shareholders' Equity for the Years Ended December 31, 2017, 2016 and 2015 | F-5 |
Consolidated Statements of Cash Flows for the Years Ended December 31, 2017, 2016 and 2015 | F-6 |
Notes to Consolidated Financial Statements as of December 31, 2017, 2016 and 2015 | F-8 to F-31 |
Financial Statement Schedule | |
Schedule II - Valuation and Qualifying Accounts | S-1 to S-2 |
Exhibits
The exhibits filed as part of this Report on Form 10-K are listed in the Exhibit Index immediately following the financial statement pages.
ITEM 16. FORM 10-K SUMMARY
None.
48
SIGNATURES
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized.
DIVERSICARE HEALTHCARE SERVICES, INC.
/s/ Chad A. McCurdy
Chad A. McCurdy
Chairman of the Board
March 1, 2018
/s/ Kelly J. Gill
Kelly J. Gill
President and Chief Executive Officer
(Principal Executive Officer)
March 1, 2018
/s/ James R. McKnight, Jr.
James R. McKnight, Jr.
Executive Vice President and Chief Financial Officer
(Principal Financial and Accounting Officer)
March 1, 2018
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed below by the following persons on behalf of the registrant and in the capacities and on the dates indicated.
/s/ Chad A. McCurdy | /s/ Robert Z. Hensley |
Chad A. McCurdy | Robert Z. Hensley |
Chairman of the Board and Director | Director |
March 1, 2018 | March 1, 2018 |
/s/ Kelly J. Gill | /s/ William C. O'Neil, Jr. |
Kelly J. Gill | William C. O'Neil, Jr. |
President and Chief Executive Officer | Director |
Director | March 1, 2018 |
March 1, 2018 | |
/s/ Robert A. McCabe, Jr. | /s/ Richard M. Brame |
Robert A. McCabe, Jr. | Richard M. Brame |
Director | Director |
March 1, 2018 | March 1, 2018 |
49
DIVERSICARE HEALTHCARE SERVICES, INC. AND SUBSIDIARIES
Consolidated Financial Statements
For the Years Ended December 31, 2017, 2016 and 2015
Together with Report of Independent Registered Public Accounting Firm
50
INDEX TO CONSOLIDATED FINANCIAL STATEMENTS
F-8 to F-31 | |
Schedule II - Valuation and Qualifying Accounts | S-1 to S-2 |
51
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
Shareholders and Board of Directors
Diversicare Healthcare Services, Inc.
Brentwood, Tennessee
Opinion on the Consolidated Financial Statements
We have audited the accompanying consolidated balance sheets of Diversicare Healthcare Services, Inc. (the "Company") and subsidiaries as of December 31, 2017 and 2016, the related consolidated statements of operations, comprehensive income (loss), shareholders’ equity, and cash flows for each of the three years in the period ended December 31, 2017, and the related notes and financial statement schedule listed in the accompanying index (collectively referred to as the “consolidated financial statements”). In our opinion, the consolidated financial statements present fairly, in all material respects, the financial position of the Company and subsidiaries at December 31, 2017 and 2016, and the results of their operations and their cash flows for each of the three years in the period ended December 31, 2017, in conformity with accounting principles generally accepted in the United States of America.
Basis for Opinion
These consolidated financial statements are the responsibility of the Company’s management. Our responsibility is to express an opinion on the Company’s consolidated financial statements based on our audits. We are a public accounting firm registered with the Public Company Accounting Oversight Board (United States) (“PCAOB”) and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audits in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the consolidated financial statements are free of material misstatement, whether due to error or fraud. The Company is not required to have, nor were we engaged to perform, an audit of its internal control over financial reporting. As part of our audits we are required to obtain an understanding of internal control over financial reporting but not for the purpose of expressing an opinion on the effectiveness of the Company’s internal control over financial reporting. Accordingly, we express no such opinion.
Our audits included performing procedures to assess the risks of material misstatement of the consolidated financial statements, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the consolidated financial statements. Our audits also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the consolidated financial statements. We believe that our audits provide a reasonable basis for our opinion.
/s/ BDO USA, LLP
We have served as the Company's auditor since 2002.
Nashville, Tennessee
March 1, 2018
F-1
DIVERSICARE HEALTHCARE SERVICES, INC. AND SUBSIDIARIES
CONSOLIDATED BALANCE SHEETS
DECEMBER 31, 2017 AND 2016
(in thousands, except per share amounts)
ASSETS | 2017 | 2016 | LIABILITIES AND SHAREHOLDERS' EQUITY | 2017 | 2016 | |||||||||||||
CURRENT ASSETS: | CURRENT LIABILITIES: | |||||||||||||||||
Cash and cash equivalents | $ | 3,524 | $ | 4,263 | Current portion of long-term debt and capitalized lease obligations, less deferred financing costs, net | $ | 13,065 | $ | 7,715 | |||||||||
Receivables, less allowance for doubtful accounts of $14,235 and $10,326, respectively | 64,929 | 62,152 | Trade accounts payable | 14,080 | 12,972 | |||||||||||||
Other receivables | 375 | 1,193 | Current liabilities of discontinued operations | 461 | 427 | |||||||||||||
Prepaid expenses and other current assets | 3,248 | 3,623 | Accrued expenses: | |||||||||||||||
Income tax refundable | 537 | 431 | Payroll and employee benefits | 20,013 | 20,108 | |||||||||||||
Current assets of discontinued operations | 45 | 28 | Self-insurance reserves, current portion | 8,792 | 9,401 | |||||||||||||
Total current assets | 72,658 | 71,690 | Provider taxes | 3,090 | 3,114 | |||||||||||||
Other current liabilities | 4,766 | 4,432 | ||||||||||||||||
Total current liabilities | 64,267 | 58,169 | ||||||||||||||||
PROPERTY AND EQUIPMENT, at cost | 147,549 | 128,822 | NONCURRENT LIABILITIES: | |||||||||||||||
Less accumulated depreciation and amortization | (78,345 | ) | (69,022 | ) | Long-term debt and capitalized lease obligations, less current portion and deferred financing costs, net | 74,603 | 72,145 | |||||||||||
69,204 | 59,800 | Self-insurance reserves, noncurrent portion | 13,458 | 11,766 | ||||||||||||||
Other noncurrent liabilities | 8,779 | 9,551 | ||||||||||||||||
Total noncurrent liabilities | 96,840 | 93,462 | ||||||||||||||||
COMMITMENTS AND CONTINGENCIES | ||||||||||||||||||
SHAREHOLDERS’ EQUITY: | ||||||||||||||||||
OTHER ASSETS: | Common stock, authorized 20,000 shares, $.01 par value, 6,687 and 6,592 shares issued, and 6,455 and 6,361 shares outstanding, respectively | 67 | 66 | |||||||||||||||
Deferred income taxes, net | 15,154 | 21,185 | Treasury stock at cost, 232 shares of common stock | (2,500 | ) | (2,500 | ) | |||||||||||
Deferred leasehold costs | 137 | 193 | Paid-in capital | 22,720 | 21,935 | |||||||||||||
Other noncurrent assets | 3,725 | 3,108 | Accumulated deficit | (14,534 | ) | (8,276 | ) | |||||||||||
Acquired leasehold interest, net | 6,691 | 7,075 | Accumulated other comprehensive income | 709 | 195 | |||||||||||||
Total other assets | 25,707 | 31,561 | Total shareholders’ equity | 6,462 | 11,420 | |||||||||||||
$ | 167,569 | $ | 163,051 | $ | 167,569 | $ | 163,051 | |||||||||||
The accompanying notes are an integral part of these consolidated financial statements.
F-2
DIVERSICARE HEALTHCARE SERVICES, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF OPERATIONS
(in thousands, except per share amounts)
Years Ended December 31, | |||||||||||
2017 | 2016 | 2015 | |||||||||
PATIENT REVENUES, net | $ | 574,794 | $ | 426,063 | $ | 387,595 | |||||
EXPENSES: | |||||||||||
Operating | 458,122 | 342,932 | 311,035 | ||||||||
Lease and rent expense | 54,988 | 33,364 | 28,690 | ||||||||
Professional liability | 10,764 | 8,456 | 8,122 | ||||||||
General and administrative | 33,311 | 30,271 | 24,793 | ||||||||
Depreciation and amortization | 10,902 | 8,292 | 7,524 | ||||||||
Lease termination costs (receipts) | (180 | ) | 2,008 | — | |||||||
Total expenses | 567,907 | 425,323 | 380,164 | ||||||||
OPERATING INCOME | 6,887 | 740 | 7,431 | ||||||||
OTHER INCOME (EXPENSE): | |||||||||||
Equity in net income of investment in unconsolidated affiliate | — | 273 | 339 | ||||||||
Gain on bargain purchase | 925 | — | — | ||||||||
Gain on sale of investment in unconsolidated affiliate | 733 | 1,366 | — | ||||||||
Hurricane costs | (232 | ) | — | — | |||||||
Interest expense, net | (6,369 | ) | (4,802 | ) | (4,102 | ) | |||||
Debt retirement costs | — | (351 | ) | — | |||||||
(4,943 | ) | (3,514 | ) | (3,763 | ) | ||||||
INCOME (LOSS) FROM CONTINUING OPERATIONS BEFORE INCOME TAXES | 1,944 | (2,774 | ) | 3,668 | |||||||
BENEFIT (PROVISION) FOR INCOME TAXES | (6,743 | ) | 1,030 | (916 | ) | ||||||
INCOME (LOSS) FROM CONTINUING OPERATIONS | (4,799 | ) | (1,744 | ) | 2,752 | ||||||
LOSS FROM DISCONTINUED OPERATIONS: | |||||||||||
Operating loss, net of income tax benefit of $43, $41 and $375, respectively | (28 | ) | (67 | ) | (1,128 | ) | |||||
LOSS FROM DISCONTINUED OPERATIONS | (28 | ) | (67 | ) | (1,128 | ) | |||||
NET INCOME (LOSS) | $ | (4,827 | ) | $ | (1,811 | ) | $ | 1,624 | |||
NET INCOME (LOSS) PER COMMON SHARE: | |||||||||||
Per common share – basic | |||||||||||
Continuing operations | $ | (0.76 | ) | $ | (0.28 | ) | $ | 0.45 | |||
Discontinued operations | (0.01 | ) | (0.01 | ) | (0.18 | ) | |||||
$ | (0.77 | ) | $ | (0.29 | ) | $ | 0.27 | ||||
Per common share – diluted | |||||||||||
Continuing operations | $ | (0.76 | ) | $ | (0.28 | ) | $ | 0.44 | |||
Discontinued operations | (0.01 | ) | (0.01 | ) | (0.18 | ) | |||||
$ | (0.77 | ) | $ | (0.29 | ) | $ | 0.26 | ||||
DIVIDENDS DECLARED PER SHARE OF COMMON STOCK | $ | 0.22 | $ | 0.22 | $ | 0.22 | |||||
WEIGHTED AVERAGE COMMON SHARES OUTSTANDING: | |||||||||||
Basic | 6,279 | 6,199 | 6,100 | ||||||||
Diluted | 6,279 | 6,199 | 6,315 | ||||||||
The accompanying notes are an integral part of these consolidated financial statements.
F-3
DIVERSICARE HEALTHCARE SERVICES, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF COMPREHENSIVE INCOME (LOSS)
(in thousands)
Years Ended December 31, | |||||||||||
2017 | 2016 | 2015 | |||||||||
NET INCOME (LOSS) | $ | (4,827 | ) | $ | (1,811 | ) | $ | 1,624 | |||
OTHER COMPREHENSIVE INCOME (LOSS): | |||||||||||
Change in fair value of cash flow hedge, net of tax | 976 | 1,082 | 556 | ||||||||
Less: reclassification adjustment for amounts recognized in net income (loss) | (462 | ) | (500 | ) | (448 | ) | |||||
Total other comprehensive income | 514 | 582 | 108 | ||||||||
COMPREHENSIVE INCOME (LOSS) | $ | (4,313 | ) | $ | (1,229 | ) | $ | 1,732 | |||
The accompanying notes are an integral part of these consolidated financial statements.
F-4
DIVERSICARE HEALTHCARE SERVICES, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF SHAREHOLDERS' EQUITY
(in thousands)
Common Stock | Treasury Stock | Paid-in Capital | Accumulated Deficit | Accumulated Other Comprehensive Income (Loss) | Total Shareholders' Equity | ||||||||||||||||||||||||
Shares Issued | Amount | Shares | Amount | ||||||||||||||||||||||||||
BALANCE, DECEMBER 31, 2014 | 6,388 | $ | 64 | 232 | $ | (2,500 | ) | $ | 19,970 | $ | (5,285 | ) | $ | (495 | ) | $ | 11,754 | ||||||||||||
Net income | — | — | — | — | — | 1,624 | — | 1,624 | |||||||||||||||||||||
Common stock dividends declared | — | — | — | — | 45 | (1,392 | ) | — | (1,347 | ) | |||||||||||||||||||
Issuance/redemption of equity grants, net | 125 | 1 | — | — | 78 | — | — | 79 | |||||||||||||||||||||
Interest rate cash flow hedge | — | — | — | — | — | — | 108 | 108 | |||||||||||||||||||||
Tax impact of equity grant exercises | — | — | — | — | 62 | — | — | 62 | |||||||||||||||||||||
Stock based compensation | — | — | — | — | 987 | — | — | 987 | |||||||||||||||||||||
BALANCE, DECEMBER 31, 2015 | 6,513 | 65 | 232 | (2,500 | ) | 21,142 | (5,053 | ) | (387 | ) | 13,267 | ||||||||||||||||||
Net loss | — | — | — | — | — | (1,811 | ) | — | (1,811 | ) | |||||||||||||||||||
Common stock dividends declared | — | — | — | — | 46 | (1,412 | ) | — | (1,366 | ) | |||||||||||||||||||
Issuance/redemption of equity grants, net | 79 | 1 | — | — | (106 | ) | — | — | (105 | ) | |||||||||||||||||||
Interest rate cash flow hedge | — | — | — | — | — | — | 582 | 582 | |||||||||||||||||||||
Tax impact of equity grant exercises | — | — | — | — | 65 | — | — | 65 | |||||||||||||||||||||
Stock based compensation | — | — | — | — | 788 | — | — | 788 | |||||||||||||||||||||
BALANCE, DECEMBER 31, 2016 | 6,592 | 66 | 232 | (2,500 | ) | 21,935 | (8,276 | ) | 195 | 11,420 | |||||||||||||||||||
Net loss | — | — | — | — | — | (4,827 | ) | — | (4,827 | ) | |||||||||||||||||||
Common stock dividends declared | — | — | — | — | 47 | (1,431 | ) | — | (1,384 | ) | |||||||||||||||||||
Issuance/redemption of equity grants, net | 95 | 1 | — | — | (95 | ) | — | — | (94 | ) | |||||||||||||||||||
Interest rate cash flow hedge | — | — | — | — | — | — | 514 | 514 | |||||||||||||||||||||
Stock based compensation | — | — | — | — | 833 | — | — | 833 | |||||||||||||||||||||
BALANCE, DECEMBER 31, 2017 | 6,687 | $ | 67 | 232 | $ | (2,500 | ) | $ | 22,720 | $ | (14,534 | ) | $ | 709 | $ | 6,462 | |||||||||||||
The accompanying notes are an integral part of these consolidated financial statements.
F-5
DIVERSICARE HEALTHCARE SERVICES, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF CASH FLOWS
(in thousands)
Years Ended December 31, | |||||||||||
2017 | 2016 | 2015 | |||||||||
CASH FLOWS FROM OPERATING ACTIVITIES: | |||||||||||
Net income (loss) | $ | (4,827 | ) | $ | (1,811 | ) | $ | 1,624 | |||
Loss from discontinued operations | (28 | ) | (67 | ) | (1,128 | ) | |||||
Income (loss) from continuing operations | (4,799 | ) | (1,744 | ) | 2,752 | ||||||
Adjustments to reconcile income (loss) from continuing operations to net cash provided by (used in) operating activities: | |||||||||||
Depreciation and amortization | 10,902 | 8,292 | 7,524 | ||||||||
Provision for doubtful accounts | 8,958 | 7,163 | 7,507 | ||||||||
Deferred income tax provision (benefit) | 5,997 | (1,569 | ) | (1,222 | ) | ||||||
Provision for self-insured professional liability, net of cash payments | 1,342 | 1,968 | 3,200 | ||||||||
Stock based compensation | 1,027 | 1,012 | 1,152 | ||||||||
Debt retirement costs | — | 351 | — | ||||||||
Provision for leases, net of cash payments | (936 | ) | (1,773 | ) | (1,749 | ) | |||||
Lease termination costs, net of cash payments | — | 1,863 | — | ||||||||
Equity in net income of investment in unconsolidated affiliate | — | (271 | ) | (335 | ) | ||||||
Gain on sale of investment in unconsolidated affiliate | (733 | ) | (1,366 | ) | — | ||||||
Gain on bargain purchase | (925 | ) | — | — | |||||||
Deferred bonus | 761 | 350 | — | ||||||||
Other | 523 | 576 | 396 | ||||||||
Changes in other assets and liabilities affecting operating activities: | |||||||||||
Receivables, net | (10,721 | ) | (25,551 | ) | (9,883 | ) | |||||
Prepaid expenses and other assets | 385 | (1,620 | ) | (60 | ) | ||||||
Trade accounts payable and accrued expenses | 1,589 | 10,224 | 1,009 | ||||||||
Net cash provided by (used in) continuing operations | 13,370 | (2,095 | ) | 10,291 | |||||||
Net cash used in discontinued operations | (1,310 | ) | (3,523 | ) | (7,014 | ) | |||||
Net cash provided by (used in) operating activities | 12,060 | (5,618 | ) | 3,277 | |||||||
CASH FLOWS FROM INVESTING ACTIVITIES: | |||||||||||
Purchases of property and equipment | (9,730 | ) | (6,022 | ) | (4,646 | ) | |||||
Nursing center acquisitions | — | (7,550 | ) | — | |||||||
Acquisition of property and equipment through business combination | (8,750 | ) | — | (10,900 | ) | ||||||
Proceeds from sale of unconsolidated affiliate | 1,100 | 2,068 | — | ||||||||
Change in restricted cash | — | 1,658 | 2,489 | ||||||||
Deposits and other deferred balances | — | — | (9 | ) | |||||||
Net cash used in continuing operations | (17,380 | ) | (9,846 | ) | (13,066 | ) | |||||
Net cash used in discontinued operations | — | — | — | ||||||||
Net cash used in investing activities | (17,380 | ) | (9,846 | ) | (13,066 | ) | |||||
CASH FLOWS FROM FINANCING ACTIVITIES: | |||||||||||
Repayment of debt obligations | (30,154 | ) | (73,374 | ) | (15,342 | ) | |||||
Proceeds from issuance of debt | 37,067 | 92,789 | 27,945 | ||||||||
Financing costs | (195 | ) | (2,162 | ) | (160 | ) | |||||
Issuance and redemption of employee equity awards | (94 | ) | (105 | ) | 79 | ||||||
Payment of common stock dividends | (1,384 | ) | (1,366 | ) | (1,347 | ) | |||||
Payment for preferred stock restructuring | (659 | ) | (640 | ) | (619 | ) | |||||
Net cash provided by continuing operations | 4,581 | 15,142 | 10,556 | ||||||||
Net cash used in discontinued operations | — | — | — | ||||||||
Net cash provided by financing activities | 4,581 | 15,142 | 10,556 | ||||||||
(Continued)
F-6
DIVERSICARE HEALTHCARE SERVICES, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF CASH FLOWS
(in thousands)
(continued)
Years Ended December 31, | |||||||||||
2017 | 2016 | 2015 | |||||||||
NET INCREASE (DECREASE) IN CASH AND CASH EQUIVALENTS | $ | (739 | ) | $ | (322 | ) | $ | 767 | |||
CASH AND CASH EQUIVALENTS, beginning of period | 4,263 | 4,585 | 3,818 | ||||||||
CASH AND CASH EQUIVALENTS, end of period | $ | 3,524 | $ | 4,263 | $ | 4,585 | |||||
SUPPLEMENTAL DISCLOSURE OF CASH FLOW INFORMATION: | |||||||||||
Cash payments of interest, net of amounts capitalized | $ | 5,404 | $ | 3,965 | $ | 3,629 | |||||
Cash payments of income taxes | $ | 847 | $ | 549 | $ | 205 | |||||
SUPPLEMENTAL INFORMATION ON NON-CASH INVESTING AND FINANCING TRANSACTIONS: | |||||||||||
Acquisition of equipment through capital lease | $ | 507 | $ | 1,851 | $ | — | |||||
The accompanying notes are an integral part of these consolidated financial statements.
F-7
DIVERSICARE HEALTHCARE SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS
DECEMBER 31, 2017, 2016, and 2015
1. BUSINESS AND SUMMARY OF SIGNIFICANT ACCOUNTING POLICIES
Description of Business
Diversicare Healthcare Services, Inc. ("Diversicare" or the "Company") provides a broad range of post-acute care services to patients and residents including skilled nursing, ancillary health care services and assisted living. In addition to the nursing and social services usually provided in long-term care centers, we offer a variety of rehabilitative, nutritional, respiratory, and other specialized ancillary services.
As of December 31, 2017, our continuing operations consist of 76 nursing centers with 8,456 licensed skilled nursing beds. Our nursing centers range in size from 48 to 320 licensed nursing beds. The licensed nursing bed count does not include 489 licensed assisted living and other residential beds. Our continuing operations include centers in Alabama, Florida, Indiana, Kansas, Kentucky, Mississippi, Missouri, Ohio, Tennessee, and Texas. The number of centers and beds denoted in these consolidated financial statements are unaudited.
Summary of Significant Accounting Policies
Principles of Consolidation
The consolidated financial statements include the financial position, operations and accounts of Diversicare and its subsidiaries, all wholly-owned. All significant intercompany accounts and transactions have been eliminated in consolidation.
Any joint ventures are accounted for using the equity method, which is an investment in an entity over which the Company lacks control, but otherwise has the ability to exercise significant influence over operating and financial policies. The Company had one equity method investee through the fourth quarter of 2016. The Company’s share of the profits and losses from this investment are reported in equity in earnings of investment in unconsolidated affiliate and the proceeds received from the sale are reported in gain on sale of investment in unconsolidated affiliate in the accompanying consolidated statement of operations.
Use of Estimates
The preparation of consolidated financial statements in conformity with accounting principles generally accepted in the United States of America requires management to make estimates and assumptions that affect the reported amounts of assets and liabilities and disclosure of contingent assets and liabilities at the date of the consolidated financial statements and the reported amounts of revenues and expenses during the reporting period. Actual results could differ from those estimates.
Revenue Recognition
The fees charged by the Company to patients in its nursing centers are recorded on an accrual basis. These rates are contractually adjusted with respect to individuals receiving benefits under federal and state-funded programs and other third-party payors. Rates under federal and state-funded programs are determined prospectively for each center and may be based on the acuity of the care and services provided. These rates may be based on a center's actual costs subject to program ceilings and other limitations or on established rates based on acuity and services provided as determined by the federal and state-funded programs. Amounts earned under federal and state programs with respect to nursing home patients are subject to review by the third-party payors which may result in retroactive adjustments. In the opinion of management, adequate provision has been made for any adjustments that may result from such reviews. Retroactive adjustments, if any, are recorded when objectively determinable, generally within three years of the close of a reimbursement year depending upon the timing of appeals and third-party settlement reviews or audits. During the years ended December 31, 2017, 2016 and 2015, the Company recorded $99,000, $38,000 and $141,000 of net unfavorable estimated settlements from federal and state programs for periods prior to the beginning of fiscal 2017, 2016 and 2015, respectively.
Allowance for Doubtful Accounts
The Company's allowance for doubtful accounts is estimated utilizing current agings of accounts receivable, historical collections data and other factors. Management monitors these factors and determines the estimated provision for doubtful accounts. Historical bad debts have generally resulted from uncollectible private balances, some uncollectible coinsurance and deductibles and other factors. Receivables that are deemed to be uncollectible are written off. The allowance for doubtful accounts balance is assessed on a quarterly basis, with changes in estimated losses being recorded in the Consolidated Statements of Operations in the period identified.
F-8
The Company includes the provision for doubtful accounts in operating expenses in its Consolidated Statements of Operations. The provisions for doubtful accounts of continuing operations were $8,958,000, $7,163,000, and $7,507,000 for 2017, 2016 and 2015, respectively. The provision for doubtful accounts of continuing operations was 1.6%, 1.7%, and 1.9% of net revenue during 2017, 2016, and 2015, respectively.
Lease Expense
As of December 31, 2017, the Company operates 58 nursing centers under operating leases, including 35 owned by Omega, 20 owned by Golden Living and three owned by other parties. The Company's operating leases generally require the Company to pay stated rent, subject to increases based on changes in the Consumer Price Index, a minimum percentage increase, or increases in the net revenues of the leased properties. The Company's Omega and Golden Living leases require the Company to pay certain scheduled rent increases. Such scheduled rent increases are recorded as additional lease expense on a straight-line basis recognized over the term of the related leases and the difference between the amounts recorded for rent expense as compared to rent payments as an accrued liability.
See Note 2, "Business Development and Other Significant Transactions" and Note 9, "Commitments and Contingencies" for a discussion regarding the Company's Master Leases with Omega and Golden Living and the addition of certain leased centers.
Classification of Expenses
The Company classifies all expenses (except lease, interest, depreciation and amortization expenses) that are associated with its corporate and regional management support functions as general and administrative expenses. All other expenses (except lease, professional liability, interest, depreciation and amortization expenses) incurred by the Company at the center level are classified as operating expenses. Operating expenses for the year ended December 31, 2017 are net of approximately $2.2 million received during 2017 related to a settlement of provider taxes appealed by the Company.
Property and Equipment
Property and equipment are recorded at cost or at fair value determined on the respective dates of acquisition for assets obtained in a business combination, with depreciation and amortization being provided over the shorter of the remaining lease term (where applicable) or the assets' estimated useful lives on the straight-line basis as follows:
Buildings and improvements | - | 5 to 40 years |
Leasehold improvements | - | 2 to 10 years |
Furniture, fixtures and equipment | - | 2 to 15 years |
Interest incurred during construction periods for qualifying expenditures is capitalized as part of the building cost. Maintenance and repairs are expensed as incurred, and major betterments and improvements are capitalized.
The Company routinely evaluates the recoverability of the carrying value of its long-lived assets, including when significant adverse changes in the general economic conditions and significant deteriorations of the underlying undiscounted cash flows or fair values of the property indicate that the carrying amount of the property may not be recoverable. If circumstances suggest that the recorded amounts are not recoverable based upon estimated future undiscounted cash flows, the carrying values of such assets are reduced to fair value.
Cash and Cash Equivalents
Cash and cash equivalents include cash on deposit with banks and all highly liquid investments with original maturities of three months or less when purchased. Our cash on deposit with banks was subject to the Federal Deposit Insurance Corporation ("FDIC") minimum insurance levels. Effective January 1, 2013, the coverage provided by the FDIC that had been unlimited under the Dodd-Frank Deposit Insurance Provision is limited to the legal maximum, which is generally $250,000 per ownership category.
Deferred Financing and Other Costs
The Company records deferred financing and lease costs for direct and incremental expenditures related to entering into or amending debt and lease agreements. These expenditures include lenders and attorneys fees. Financing costs are amortized using the effective interest method over the term of the related debt. The amortization is reflected as interest expense in the accompanying consolidated statements of operations. Deferred lease costs are amortized on a straight-line basis over the term of the related leases. See Note 5, "Long-term Debt, Interest Rate Swap and Capitalized Lease Obligations" for further discussion. As a result of our January 2016 adoption of Accounting Standards Update ("ASU") No. 2015-03 issued by the Financial Accounting Standards Board ("FASB"), the Company nets long-term debt and deferred financing costs in the consolidated balance sheets.
F-9
Acquired Leasehold Interest
The Company has recorded an acquired leasehold interest intangible asset related to an acquisition completed during 2007. The intangible asset is accounted for in accordance with the FASB's guidance on goodwill and other intangible assets, and is amortized on a straight-line basis over the remaining life of the acquired lease, including renewal periods, the original period of which is approximately 28 years from the date of acquisition. The lease terms for the seven centers this intangible relates to provide for an initial term and renewal periods at the Company's option through May 31, 2035. As the renewal periods of the acquired leased centers are solely based on the Company's option, it is expected that costs (if any) to renew the lease through its current amortization period would be nominal and the decision to continue to lease the acquired centers lies solely within the Company's intent to continue to operate the seven centers. Any renewal costs would be included in deferred lease costs and amortized over the renewal period. Amortization expense of approximately $384,000 related to this intangible asset was recorded during each of the years ended December 31, 2017, 2016 and 2015, respectively.
The carrying value of the acquired leasehold interest intangible and the accumulated amortization are as follows:
December 31, | |||||||
2017 | 2016 | ||||||
Intangible assets | $ | 10,652,000 | $ | 10,652,000 | |||
Accumulated amortization | (3,961,000 | ) | (3,577,000 | ) | |||
Net intangible assets | $ | 6,691,000 | $ | 7,075,000 | |||
The Company evaluates the recoverability of the carrying value of the acquired leasehold intangible in accordance with the FASB's guidance on accounting for the impairment or disposal of long-lived assets. Included in this evaluation is whether significant adverse changes in general economic conditions, and significant deteriorations of the underlying cash flows or fair values of the intangible asset, indicate that the carrying amount of the intangible asset may not be recoverable. The need to recognize an impairment charge is based on estimated future undiscounted cash flows from the asset compared to the carrying value of that asset. If recognition of an impairment charge is necessary, it is measured as the amount by which the carrying amount of the intangible asset exceeds the fair value of the intangible asset.
The expected amortization expense for the acquired leasehold interest intangible asset is as follows:
2018 | $ | 384,000 | ||
2019 | 384,000 | |||
2020 | 384,000 | |||
2021 | 384,000 | |||
2022 | 384,000 | |||
Thereafter | 4,771,000 | |||
$ | 6,691,000 | |||
Self-Insurance
Self-insurance liabilities primarily represent the unfunded accrual for self insured risks associated with general and professional liability claims, employee health insurance and workers' compensation. The Company's health insurance liability is based on known claims incurred and an estimate of incurred but unreported claims determined by an analysis of historical claims paid. The Company's workers' compensation liability relates primarily to periods of self insurance and consists of an estimate of the future costs to be incurred for the known claims.
Final determination of the Company's actual liability for incurred general and professional liability claims is a process that takes years. The Company evaluates the adequacy of this liability on a quarterly basis. Semi-annually, the Company retains a third-party actuarial firm to assist in the evaluation of this unfunded accrual. Since May 2012, Merlinos & Associates, Inc. (“Merlinos”) has assisted management in the preparation of the appropriate accrual for incurred but not reported general and professional liability claims based on data furnished by the Company. Merlinos primarily utilizes historical data regarding the frequency and cost of the Company's past claims over a multi-year period, industry data and information regarding the number of occupied beds to develop its estimates of the Company's ultimate professional liability cost for current periods.
F-10
On a quarterly basis, the Company obtains reports of asserted claims and lawsuits incurred. These reports, which are provided by the Company's insurers and a third party claims administrator, contain information relevant to the actual expense already incurred with each claim as well as the third-party administrator's estimate of the anticipated total cost of the claim. This information is reviewed by the Company quarterly and provided to the actuary semi-annually. Based on the Company's evaluation of the actual claim information obtained, the semi-annual estimates received from the third-party actuary, the amounts paid and committed for settlements of claims and on estimates regarding the number and cost of additional claims anticipated in the future, the reserve estimate for a particular period may be revised upward or downward on a quarterly basis. Any increase in the accrual has an unfavorable impact on results of operations in the period and any reduction in the accrual increases results of operations during the period.
All losses are projected on an undiscounted basis. The self-insurance liabilities include estimates of liability for incurred but not reported claims, estimates of liability for reported but unresolved claims, actual liabilities related to settlements, including settlements to be paid over time, and estimates of related legal costs incurred and expected to be incurred.
One of the key assumptions in the actuarial analysis is that historical losses provide an accurate forecast of future losses. Changes in legislation such as tort reform, changes in our financial condition, changes in our risk management practices and other factors may affect the severity and frequency of claims incurred in future periods as compared to historical claims.
The facts and circumstances of each claim vary significantly, and the amount of ultimate liability for an individual claim may vary due to many factors, including whether the case can be settled by agreement, the quality of legal representation, the individual jurisdiction in which the claim is pending, and the views of the particular judge or jury deciding the case.
Although the Company adjusts its unfunded accrual for professional and general liability claims on a quarterly basis and retains a third-party actuarial firm semi-annually to assist management in estimating the appropriate accrual, professional and general liability claims are inherently uncertain, and the liability associated with anticipated claims is very difficult to estimate. Professional liability cases have a long cycle from the date of an incident to the date a case is resolved, and final determination of the Company's actual liability for claims incurred in any given period is a process that takes years. As a result, the Company's actual liabilities may vary significantly from the unfunded accrual, and the amount of the accrual has and may continue to fluctuate by a material amount in any given period. Each change in the amount of this accrual will directly affect the Company's results of operations and financial position for the period in which the change in accrual is made.
Income Taxes
The Tax Cuts and Job Act (the Tax Act), which was enacted in December 2017, increased the Company's income tax expense by $5,476,000 for the year ended December 31, 2017, which was a result of our revaluation of our net deferred tax assets. The Company considers the accounting for the deferred tax re-measurements and other items to be complete, but ongoing accounting guidance and interpretation could result in adjustments to the consolidated financial statements. The Tax Act will decrease the corporate income tax rate from 35.0% to 21.0% beginning on January 1, 2018. See Note 8, "Income Taxes" for further detail.
The Company follows the FASB's guidance on Accounting for Income Taxes, which requires the asset and liability method of accounting for income taxes whereby deferred income taxes are recorded for the future tax consequences attributable to differences between the financial statement and tax bases of assets and liabilities. Deferred tax assets and liabilities are measured using enacted tax rates expected to apply to taxable income in the years in which those temporary differences are expected to be recovered or settled. Valuation allowances are provided against any estimated non-realizable deferred tax assets where necessary.
Where the Company believes that a tax position is supportable for income tax purposes, the item is included in its income tax returns. Where treatment of a position is uncertain, liabilities are recorded based upon the Company’s evaluation of the “more likely than not” outcome considering the technical merits of the position. While the judgments and estimates made by the Company are based on management’s evaluation of the technical merits of a matter, historical experience and other assumptions that management believes are appropriate and reasonable under current circumstances, actual resolution of these matters may differ from recorded estimated amounts, resulting in charges or credits that could materially affect future financial statements. See Note 8, "Income Taxes" for additional information related to the provision for income taxes.
Disclosure of Fair Value of Financial Instruments
Fair value is defined as the price that would be received to sell an asset, or paid to transfer a liability, in an orderly transaction between market participants. In calculating fair value, a company must maximize the use of observable market inputs, minimize the use of unobservable market inputs and disclose in the form of an outlined hierarchy the details of such fair value measurements. The carrying amounts of cash and cash equivalents, receivables, trade accounts payable and accrued expenses approximate fair value because of the short-term nature of these accounts. The Company's self-insurance liabilities are reported on an undiscounted basis as the timing of estimated settlements cannot be determined.
F-11
The Company follows the FASB's guidance on Fair Value Measurements and Disclosures which provides rules for using fair value to measure assets and liabilities as well as a fair value hierarchy that prioritizes the information used to develop the measurements. It applies whenever other guidance requires (or permits) assets or liabilities to be measured at fair value and gives the highest priority to unadjusted quoted prices in active markets for identical assets or liabilities (Level 1 measurements) and the lowest priority to unobservable inputs (Level 3 measurements).
A summary of the fair value hierarchy that prioritizes observable and unobservable inputs used to measure fair value into three broad levels is described below:
Level 1: Quoted prices (unadjusted) in active markets that are accessible at the measurement date for identical assets or liabilities. The fair value hierarchy gives the highest priority to Level 1 inputs.
Level 2: Observable prices that are based on inputs not quoted on active markets, but corroborated by market data.
Level 3: Unobservable inputs are used when little or no market data is available. The fair value hierarchy gives the lowest priority to Level 3 inputs.
As further discussed in Note 5, "Long-term Debt, Interest Rate Swap and Capitalized Lease Obligations", in conjunction with the debt agreements entered into in February 2016, the Company entered into an interest rate swap agreement with a member of the bank syndicate as the counterparty. The applicable guidance requires companies to recognize all derivative instruments as either assets or liabilities at fair value in a company's balance sheets.
As the Company's interest rate swap, a cash flow hedge, is not traded on a market exchange, the fair value is determined using a valuation model based on a discounted cash flow analysis. This analysis reflects the contractual terms of the interest rate swap agreement and uses observable market-based inputs, including estimated future LIBOR interest rates. The fair value of the Company's interest rate swap is the net difference in the discounted future fixed cash payments and the discounted expected variable cash receipts. The variable cash receipts are based on the expectation of future interest rates and are observable inputs available to a market participant. The interest rate swap valuation is classified in Level 2 of the fair value hierarchy. The debt balances as presented in the consolidated balance sheets approximate the fair value of the respective instruments as the debt is at a variable rate, the estimates of which are considered Level 2 fair value calculations within the fair value hierarchy.
The following table presents by level, within the fair value hierarchy, assets and liabilities measured at fair value on a recurring basis as of December 31, 2017 and 2016:
December 31, 2017 | Fair Value Measurements - Assets (Liabilities) | |||||||||||||||
Total | Level 1 | Level 2 | Level 3 | |||||||||||||
Interest rate swap | $ | 211,000 | $ | — | $ | 211,000 | $ | — | ||||||||
December 31, 2016 | Fair Value Measurements - Assets (Liabilities) | |||||||||||||||
Total | Level 1 | Level 2 | Level 3 | |||||||||||||
Interest rate swap | $ | (129,000 | ) | $ | — | $ | (129,000 | ) | $ | — | ||||||
The change in fair value of the Company's cash flow hedge is detailed in the Company's Consolidated Statements of Comprehensive Income (Loss).
Net Income (Loss) per Common Share
The Company follows the FASB's guidance on Earnings Per Share for the financial reporting of net income (loss) per common share. Basic earnings per common share excludes dilution and restricted shares and is computed by dividing income available to common shareholders by the weighted-average number of common shares, excluding restricted shares, outstanding for the period. Diluted earnings per common share reflects the potential dilution that could occur if securities or other contracts to issue common stock were exercised or converted into common stock or otherwise resulted in the issuance of common stock that then shared in the earnings of the Company. See Note 7, "Net Income (Loss) per Common Share" for additional disclosures about the Company's Net Income (Loss) per Common Share.
Stock Based Compensation
The Company follows the FASB's guidance on Stock Compensation to account for share-based payments granted to team members and recorded non-cash stock based compensation expense of $1,027,000, $1,012,000 and $1,152,000 during the years ended December 31, 2017, 2016 and 2015, respectively. Such amounts are included as components of general and administrative expense
F-12
or operating expense based upon the classification of cash compensation paid to the related employees. See Note 6, "Shareholders' Equity, Stock Plans and Preferred Stock" for additional disclosures about the Company's stock based compensation plans.
Accumulated Other Comprehensive Income
Accumulated other comprehensive income consists of other comprehensive income (loss). Comprehensive income (loss) is a more inclusive financial reporting method that includes disclosure of financial information that historically has not been recognized in the calculation of net income (loss). The Company has chosen to present the components of other comprehensive income (loss) in a separate statement of comprehensive income (loss). Currently, the Company's other comprehensive income (loss) consists of the change in fair value of the Company's interest rate swap transaction accounted for as a cash flow hedge.
Recent Accounting Guidance
In May 2014, the Financial Accounting Standards Board ("FASB") issued Accounting Standards Update ("ASU") No. 2014-09, Revenue from Contracts with Customers (Topic 606), which outlines a single comprehensive model for recognizing revenue and supersedes most existing revenue recognition guidance, including guidance specific to the healthcare industry. For public companies, Topic 606 is effective for annual and interim reporting periods beginning after December 15, 2017. The Company adopted the requirements of this standard effective January 1, 2018. The Company elected to apply the modified retrospective approach with the cumulative transition effect recognized in beginning retained earnings as of the date of adoption. The Company performed analysis into the application of the portfolio approach as a practical expedient to group patient contracts with similar characteristics, such that revenue for a given portfolio would not be materially different than if it were evaluated on a contract-by-contract basis. As part of the impact assessment, the Company evaluated any variable consideration and potential constraints on the estimate of variable consideration. The Company is required to update its estimate of the transaction price at the end of each reporting period, and any amounts allocated to a satisfied performance obligation are recognized as revenue or a reduction of revenue in the period in which the transaction price changes. Changes in the Company’s expectation of the amount it will receive from the patient or third-party payors will be recorded in revenue unless there is a specific event that suggests the patient or third-party payor no longer has the ability and intent to pay the amount due and, therefore, the changes in its estimate of variable consideration better represent an impairment, or bad debt. Additionally, the new guidance requires enhanced disclosures about the nature, amount, timing, and uncertainty of revenue and cash flows arising from patient contracts, including revenue recognition policies to identify performance obligations, assets recognized from costs incurred to obtain and fulfill a contract, and significant judgments in measurement and recognition. The implementation has been completed and the impact to the consolidated financial statements for periods subsequent to adoption is not material.
In November 2015, the FASB issued ASU No. 2015-17, Balance Sheet Classification of Deferred Taxes, which changes how deferred taxes are classified on the Company's balance sheets. The Company adopted ASU No. 2015-17 as of January 1, 2017, and the new standard was applied on a retrospective basis. The adoption of this guidance resulted in a $7,644,000 reclassification between current deferred income taxes and non-current deferred income taxes as of December 31, 2016.
In February 2016, the FASB issued ASU No. 2016-02, Leases. The new standard establishes a right-of-use (ROU) model that requires a lessee to record a ROU asset and a lease liability on the balance sheet for all leases with terms longer than 12 months. Leases will be classified as either finance or operating, with classification affecting the pattern of expense recognition in the income statement. The new standard is effective for fiscal years beginning after December 15, 2018, including interim periods within those fiscal years. A modified retrospective transition approach is required for lessees for capital and operating leases existing at, or entered into after, the beginning of the earliest comparative period presented in the financial statements, with certain practical expedients available. Disclosures will be required to meet the objective of enabling users of financial statements to assess the amount, timing, and uncertainty of cash flows arising from leases. We anticipate this standard will have a material impact on our consolidated financial statements. While we are continuing to assess all potential impacts of the standard, we currently believe the most significant impact relates to our accounting for building and equipment operating leases and will result in a significant increase in the assets and liabilities on the consolidated balance sheet.
In March 2016, the FASB issued ASU No. 2016-09, Compensation - Stock Compensation (Topic 718): Improvements to Employee Share-Based Payment Accounting. The ASU was issued as part of the FASB Simplification Initiative and involves several aspects of accounting for share-based payment transactions, including the income tax consequences and classification on the statement of cash flows. We adopted this standard as of January 1, 2017. The adoption did not have a material impact on our financial position, results of operations or cash flows.
In June 2016, the FASB issued ASU No. 2016-13, Measurement of Credit Losses on Financial Instruments. This update is intended to improve financial reporting by requiring more timely recognition of credit losses on loans and other financial instruments that are not accounted for at fair value through net income, including loans held for investment, held-to-maturity debt securities, trade and other receivables, net investment in leases and other such commitments. This update requires that financial statement assets measured at an amortized cost be presented at the net amount expected to be collected, through an allowance for credit losses that is deducted from the amortized cost basis. This standard is effective for the fiscal year beginning after December 15, 2019 with
F-13
early adoption permitted. The Company is in the initial stages of evaluating the impact from the adoption of this new standard on the consolidated financial statements and related notes.
In August 2016, the FASB issued ASU No. 2016-15, Statement of Cash Flows (Topic 230). The ASU provides clarification regarding how certain cash receipts and cash payments are presented and classified in the statement of cash flows. The guidance addresses eight specific cash flow issues with the objective of reducing the existing diversity in practice. The ASU is effective for annual and interim periods beginning after December 15, 2017, which required the Company to adopt these provisions in the first quarter of fiscal 2018 using a retrospective approach. The Company is currently evaluating the impact this standard will have on our consolidated financial statements.
In November 2016, the FASB issued ASU No. 2016-18, Statement of Cash Flows (Topic 230): Restricted Cash, which requires that the Statement of Cash Flows explain the changes during the period of cash and cash equivalents inclusive of amounts categorized as Restricted Cash. As a result, amounts generally described as restricted cash and restricted cash equivalents should be included with cash and cash equivalents when reconciling the beginning-of-period and end-of-period total amounts shown on the statement of cash flows. The standard is effective for periods beginning after December 15, 2017, which will be the Company's fiscal year 2018. The adoption of ASU 2016-18 is not expected to have a material impact on the Company’s consolidated statements of cash flows.
In January 2017, the FASB issued ASU No. 2017-01, Business Combinations (Topic 805) - Clarifying the Definition of a Business, which provides guidance to assist entities with evaluating whether transactions should be accounted for as acquisitions (or disposals) of assets or businesses. The adoption is effective for annual and interim periods beginning after December 15, 2017, with early adoption permitted in certain circumstances. The Company is still evaluating the effect, if any, the standard will have on the Company's consolidated financial condition and results of operations. The Company will evaluate future acquisitions under this guidance, which may result in future acquisitions being asset acquisitions.
In May 2017, the FASB issued ASU No. 2017-09, Compensation - Stock Compensation (Topic 718): Scope of Modification Accounting. The amended standard specifies the modification accounting applicable to any entity which changes the terms or conditions of a share-based payment award. The new guidance is effective for all entities after December 15, 2017. Early adoption is permitted. The Company does not presently believe adoption of this new standard will be material to its consolidated financial statements.
In August 2017, the FASB issued ASU No. 2017-12, Derivatives and Hedging - Targeted Improvements to Accounting for Hedging Activities, which is intended to simplify and amend the application of hedge accounting to more clearly portray the economics of an entity’s risk management strategies in its financial statements. The new guidance will make more financial and nonfinancial hedging strategies eligible for hedge accounting and reduce complexity in fair value hedges of interest rate risk. The new guidance also changes how companies assess effectiveness and amends the presentation and disclosure requirements. The new guidance eliminates the requirement to separately measure and report hedge ineffectiveness and generally the entire change in the fair value of a hedging instrument will be required to be presented in the same income statement line as the hedged item. The new guidance also eases certain documentation and assessment requirements and modifies the accounting for components excluded from the assessment of hedge effectiveness. The new guidance is effective for public entities for fiscal years beginning after December 15, 2018, including interim periods within those years. Early adoption is permitted in any interim period or fiscal year before the effective date. The Company is evaluating the effect this guidance will have on our consolidated financial statements and related disclosures.
2. BUSINESS DEVELOPMENT AND OTHER SIGNIFICANT TRANSACTIONS
2017 Acquisition
During the year ended December 31, 2017, the Company expanded its operations to acquire a center that complements its current portfolio. On June 8, 2017, the Company entered into an Asset Purchase Agreement (the "Purchase Agreement") with Park Place Nursing and Rehabilitation Center, LLC, Dunn Nursing Home, Inc., Wood Properties of Selma LLC, and Homewood of Selma, LLC to acquire a 103-bed skilled nursing center in Selma, Alabama, for an aggregate purchase price of $8,750,000. In connection with the funding of the acquisition, on June 30, 2017, the Company amended the terms of its Second Amended and Restated Term Loan Agreement to increase the facility by $7,500,000, which is described in Note 5 "Long-Term Debt, Interest Rate Swap and Capitalized Lease Obligations." The acquisition of the business closed on July 1, 2017. In accordance with ASC 805, this transaction was accounted for as a business combination, which resulted in the expensing of $140,000 of acquisition costs and a $925,000 recorded gain on bargain purchase for the Company for the year ended December 31, 2017. The operating results of the acquired center have been included in the Company's consolidated statement of operations since the acquisition date. Supplemental pro forma information regarding the acquisition is not material to the consolidated financial statements. The allocation of the purchase price to the net assets acquired is as follows:
F-14
Park Place | ||||
Purchase Price | $ | 8,750,000 | ||
Gain on bargain purchase | 925,000 | |||
$ | 9,675,000 | |||
Allocation: | ||||
Building | $ | 8,435,000 | ||
Land | 760,000 | |||
Land Improvements | 145,000 | |||
Furniture, Fixtures and Equipment | 335,000 | |||
$ | 9,675,000 | |||
Golden Living Transaction
On August 15, 2016, the Company entered into an Operation Transfer Agreement with Golden Living (the "Lessor") to assume the operations of 22 centers in Alabama and Mississippi.
On October 1, 2016, the Company entered into a Master Lease Agreement (the "Lease") with Golden Living to directly lease eight centers located in Mississippi from the Lessor, which include: (i) a 152-bed skilled nursing center known as Golden Living Center - Amory; (ii) a 130-bed skilled nursing center known as Golden Living Center - Batesville; (iii) a 58-bed skilled nursing center known as Golden Living Center - Brook Manor; (iv) a 119-bed skilled nursing center known as Golden Living Center - Eupora; (v) a 140-bed skilled nursing center known as Golden Living Center - Ripley; (vi) a 140-bed skilled nursing center known as Golden Living Center - Southaven; (vii) a 120-bed skilled nursing center known as Golden Living Center - Eason Blvd; (viii) a 60-bed skilled nursing center known as Golden Living Center - Tylertown. See Note 9 "Commitments and Contingencies."
On November, 1 2016, the Company amended and restated the Lease ("Amended Lease") with the Lessor to directly lease an additional twelve centers located in Alabama from the Lessor, which include: (i) a 87-bed skilled nursing center known as Golden Living Center - Arab; (ii) a 180-bed skilled nursing center known as Golden Living Center - Meadowood; (iii) a 132-bed skilled nursing center known as Golden Living Center - Riverchase; (iv) a 100-bed skilled nursing center known as Golden Living Center - Boaz; (v) a 154-bed skilled nursing center known as Golden Living Center - Foley; (vi) a 50-bed skilled nursing center known as Golden Living Center - Hueytown; (vii) a 85-bed skilled nursing center known as Golden Living Center - Lanett; (viii) a 138-bed skilled nursing center known as Golden Living Center - Montgomery; (ix) a 120-bed skilled nursing center known as Golden Living Center - Oneonta; (x) a 173-bed skilled nursing center known as Golden Living Center - Oxford; (xi) a 94-bed skilled nursing center known as Golden Living Center - Pell City; (xii) a 123-bed skilled nursing center known as Golden Living Center - Winfield. See Note 9 "Commitments and Contingencies."
2016 Acquisitions
On February 26, 2016, the Company exercised its purchase options to acquire the real estate assets for Diversicare of Hutchinson in Hutchinson, Kansas and Clinton Place in Clinton, Kentucky for $4,250,000 and $3,300,000, respectively. The Company has operated these centers since February 2015 and April 2012, respectively. Hutchinson is an 85-bed skilled nursing center and Clinton is an 88-bed skilled nursing center. The Company accounted for these transactions as asset acquisitions and, as a result, allocated the purchase price, including acquisition costs, to the net assets acquired based on relative fair value at the acquisition date. The allocation of the purchase price was determined with the assistance of HealthTrust LLC, a third-party real estate valuation firm. The allocation for the assets acquired is as follows:
F-15
Hutchinson | Clinton Place | |||||||
Purchase Price | $ | 4,250,000 | $ | 3,300,000 | ||||
Acquisition Costs | 43,000 | 34,000 | ||||||
$ | 4,293,000 | $ | 3,334,000 | |||||
Allocation: | ||||||||
Buildings | $ | 3,443,000 | $ | 2,898,000 | ||||
Land | 365,000 | 267,000 | ||||||
Furniture, Fixtures and Equipment | 485,000 | 169,000 | ||||||
$ | 4,293,000 | $ | 3,334,000 | |||||
2017 Lease Termination
On September 30, 2017, the Company entered into an Agreement with Trend Health and Rehab of Carthage, LLC ("Trend Health") to terminate the lease and the Company's right of possession of the center in Carthage, Mississippi. In consideration of the early termination of the lease, Trend Health provided the Company with a $250,000 cash termination payment which is included in lease termination receipts in the accompanying consolidated statements of operations for the year ended December 31, 2017, net of costs to terminate. For accounting purposes, this transaction was not reported as a discontinued operation as this disposal did not represent a strategic shift that has (or will have) a major effect on the Company's operations and financial results.
2016 Lease Termination
On May 31, 2016, the Company entered into an Agreement with Avon Ohio, LLC to amend the original lease agreement, thus terminating the Company's right of possession of the center. As a result, the Company incurred lease termination costs of $2,008,000 in the second quarter of 2016. Under the amended agreement, the Company is required to pay $300,000 per year through the term of the original lease agreement, July 31, 2024. For accounting purposes, this transaction was not reported as a discontinued operation as this disposal did not represent a strategic shift that has (or will have) a major effect on the Company's operations and financial results.
2016 Sale of Investment in Unconsolidated Affiliate
On October 28, 2016, the Company and its partners entered into an asset purchase agreement to sell the pharmacy joint venture. The sale resulted in a $1,366,000 gain in the fourth quarter of 2016. Subsequently, we recognized an additional gain of $733,000 in the first quarter of 2017, related to the continuing liquidation of remaining net assets affiliated with the partnership.
3. RECEIVABLES
Receivables, before the allowance for doubtful accounts, consist of the following components:
December 31, | |||||||
2017 | 2016 | ||||||
Medicare | $ | 20,007,000 | $ | 20,402,000 | |||
Medicaid and other non-federal government programs | 29,453,000 | 31,208,000 | |||||
Other patient and resident receivables | 29,704,000 | 20,868,000 | |||||
79,164,000 | 72,478,000 | ||||||
Less: allowance for doubtful accounts | (14,235,000 | ) | (10,326,000 | ) | |||
Accounts receivable, net | 64,929,000 | 62,152,000 | |||||
Other receivables and advances | $ | 375,000 | $ | 1,193,000 | |||
The other receivables and advances balance includes $474,000 related to renovation projects to be funded by Omega at December 31, 2016. None of the other receivables and advances balance at December 31, 2017 included funds related to Omega renovation projects. See Note 9, "Commitments and Contingencies" for additional discussion of these receivables and leased center construction projects.
F-16
Our accounts receivable at December 31, 2017, reflects a full year of ownership of the twenty-two newly leased Golden Living centers in Alabama and Mississippi. The Company has completed the change in ownership process and is utilizing our billing credentials to perform the billing of the Medicare and Medicaid receivables.
The Company provides credit for a substantial portion of its revenues and continually monitors the credit worthiness and collectability from its patients, including proper documentation of third-party coverage. The Company is subject to accounting losses from uncollectible receivables in excess of its reserves.
Substantially all receivables are pledged as collateral on the Company's debt obligations.
4. PROPERTY AND EQUIPMENT
Property and equipment, at cost, consists of the following:
December 31, | |||||||
2017 | 2016 | ||||||
Land | $ | 6,521,000 | $ | 5,761,000 | |||
Buildings and leasehold improvements | 98,140,000 | 85,660,000 | |||||
Furniture, fixtures and equipment | 42,888,000 | 37,401,000 | |||||
147,549,000 | 128,822,000 | ||||||
Less: accumulated depreciation | (78,345,000 | ) | (69,022,000 | ) | |||
Net property and equipment | $ | 69,204,000 | $ | 59,800,000 | |||
As discussed further in Note 5, "Long-term Debt, Interest Rate Swap and Capitalized Lease Obligations", the property and equipment of certain skilled nursing centers are pledged as collateral for mortgage debt obligations. In addition, the Company has assets recorded as capital leased assets purchased through capitalized lease obligations. The Company capitalizes leasehold improvements which will revert back to the lessor of the property at the expiration or termination of the lease, and depreciates these improvements over the shorter of the remaining lease term or the assets' estimated useful lives.
5. LONG-TERM DEBT, INTEREST RATE SWAP AND CAPITALIZED LEASE OBLIGATIONS
Long-term debt consists of the following:
December 31, | ||||||||
2017 | 2016 | |||||||
Mortgage loan with a syndicate of banks; payable monthly, interest at 4.0% above LIBOR, a portion of which is fixed at 5.79% based on the interest rate swap described below. | $ | 64,567,000 | $ | 58,792,000 | ||||
Acquisition loan with Canadian Imperial Bank of Commerce, interest at 4.75% above LIBOR. | 7,500,000 | 6,289,000 | ||||||
Revolving credit facility borrowings payable to a bank; secured by receivables of the Company; interest at 4.0% above LIBOR. | 16,000,000 | 15,000,000 | ||||||
Loan to finance equipment | 40,000 | — | — | |||||
88,107,000 | 80,081,000 | |||||||
Less current portion | (13,065,000 | ) | (7,715,000 | ) | ||||
75,042,000 | 72,366,000 | |||||||
Less deferred financing costs, net | (1,884,000 | ) | (2,273,000 | ) | ||||
Plus capitalized lease obligations | 1,445,000 | 2,052,000 | ||||||
Long-term debt | $ | 74,603,000 | $ | 72,145,000 | ||||
As of December 31, 2017, the Company's weighted average interest rate on long-term debt, including the impact of the interest rate swap, was approximately 5.66%.
F-17
The Company has agreements with a syndicate of banks for a mortgage term loan ("Original Mortgage Loan") and the Company’s revolving credit agreement ("Original Revolver"). On February 26, 2016, the Company executed an Amended and Restated Credit Agreement (the "Credit Agreement") which modified the terms of the Original Mortgage Loan and the Original Revolver Agreements dated April 30, 2013. The Credit Agreement increases the Company's borrowing capacity to $100,000,000 allocated between a $72,500,000 Mortgage Loan ("Amended Mortgage Loan") and a $27,500,000 Revolver ("Amended Revolver"). The Amended Mortgage Loan consists of $60,000,000 term and $12,500,000 acquisition loan facilities. Loan acquisition costs associated with the Amended Mortgage Loan and the Amended Revolver were capitalized in the amount of $195,000 and are being amortized over the five-year term of the agreements, which are included in debt.
Under the terms of the amended agreements, the syndicate of banks provided the Amended Mortgage Loan with an original balance of $72,500,000 with a five-year maturity through February 26, 2021, and a $27,500,000 Amended Revolver through February 26, 2021. The Amended Mortgage Loan has a term of five years, with principal and interest payable monthly based on a 25-year amortization. Interest on the term and acquisition loan facilities are based on LIBOR plus 4.0% and 4.75%, respectively. A portion of the Amended Mortgage Loan is effectively fixed at 5.79% pursuant to an interest rate swap with an initial notional amount of $30,000,000. The Amended Mortgage Loan balance was $72,067,000 as of December 31, 2017, consisting of $64,567,000 on the term loan facility with an interest rate of 5.5% and $7,500,000 on the acquisition loan facility with an interest rate of 6.25%. The Amended Mortgage Loan is secured by 18 owned nursing centers, related equipment and a lien on the accounts receivable of these centers. The Amended Mortgage Loan and the Amended Revolver are cross-collateralized and cross-defaulted. The Company’s Amended Revolver has an interest rate of LIBOR plus 4.0% and is secured by accounts receivable and is subject to limits on the maximum amount of loans that can be outstanding under the revolver based on borrowing base restrictions.
Effective October 3, 2016, the Company entered into the Second Amendment ("Second Revolver Amendment") to amend the Amended Revolver. The Second Amendment increased the Amended Revolver capacity from the $27,500,000 in the Amended Revolver to $52,250,000; provided that the maximum revolving facility be reduced to $42,250,000 on August 1, 2017. Subsequently, on June 30, 2017, the Company executed a Fourth Amendment (the "Fourth Revolver Amendment") to amend the Amended Revolver, which modifies the capacity of the revolver to remain at $52,250,000.
On December 29, 2016, the Company executed a Third Amendment ("Third Revolver Amendment") to amend the Amended Revolver. The Third Amendment modifies the terms of the Amended Mortgage Loan Agreement by increasing the Company’s letter of credit sublimit from $10,000,000 to $15,000,000.
Effective June 30, 2017, the Company entered into a Second Amendment (the "Second Term Amendment") to amend the Amended Mortgage Loan. The Second Term Amendment amends the terms of the Amended Mortgage Loan Agreement by increasing the Company's term loan facility by $7,500,000.
As of December 31, 2017, the Company had $16,000,000 in borrowings outstanding under the Amended Revolver compared to $15,000,000 outstanding as of December 31, 2016. The outstanding borrowings on the revolver were used primarily to compensate for accumulated Medicaid and Medicare receivables at recently acquired centers as these centers proceed through the change in ownership process with CMS. Annual fees for letters of credit issued under the Amended Revolver are 3.0% of the amount outstanding. The Company has 11 letters of credit with a total value of $13,408,000 outstanding as of December 31, 2017. Considering the balance of eligible accounts receivable, the letter of credit, the amounts outstanding under the Amended Revolver and the maximum loan amount of $39,348,000, the balance available for borrowing under the Amended Revolver is $9,940,000 at December 31, 2017.
The Company’s debt agreements contain various financial covenants, the most restrictive of which relates to debt service coverage ratios. The Company is in compliance with all such covenants at December 31, 2017.
In connection with the Company's 2017 and 2016 financing agreements, the Company recorded the following deferred loan costs related to the new financing agreements as a reduction of the debt balances discussed above:
2017 | 2016 | ||||||
Write-off of deferred financing costs | $ | — | $ | 351,000 | |||
Deferred financing costs capitalized | $ | 195,000 | $ | 2,162,000 | |||
The deferred financing costs included in the current and long-term debt balances were $1,884,000 at December 31, 2017 and $2,273,000 at December 31, 2016.
F-18
Scheduled principal payments of long-term debt are as follows:
2018 | $ | 11,902,000 | |
2019 | 9,463,000 | ||
2020 | 8,052,000 | ||
2021 | 58,690,000 | ||
Total | $ | 88,107,000 | |
Interest Rate Swap Cash Flow Hedge
As part of the debt agreements entered into in April 2013, the Company entered into an interest rate swap agreement with a member of the bank syndicate as the counterparty. The Company entered into the interest rate swap agreement to mitigate the variable interest rate risk on its outstanding mortgage borrowings. The Company designated its interest rate swap as a cash flow hedge and the effective portion of the hedge, net of taxes, is reflected as a component of other comprehensive income (loss). In conjunction with the aforementioned amendment to the Credit Agreement that occurred in February 2016, the Company retained the previously agreed upon interest rate swap modifying the terms of the swap to reflect the amended Credit Agreement. The Company redesignated the interest rate swap as a cash flow hedge. The interest rate swap agreement has the same effective date and maturity date as the Amended Mortgage Loan, and has an amortizing notional amount that was $28,565,000 as of December 31, 2017. The interest rate swap agreement requires the Company to make fixed rate payments to the bank calculated on the applicable notional amount at an annual fixed rate of 5.79% while the bank is obligated to make payments to the Company based on LIBOR on the same notional amounts. The applicable guidance requires companies to recognize all derivative instruments as either assets or liabilities at fair value in a company's balance sheets.
The Company assesses the effectiveness of its interest rate swap on a quarterly basis and at December 31, 2017, the Company determined that the interest rate swap was effective. The interest rate swap valuation model indicated a net asset of $211,000 at December 31, 2017. The fair value of the interest rate swap is included in “other noncurrent liabilities” on the Company's consolidated balance sheets. The asset related to the change in the interest rate swap included in accumulated other comprehensive income at December 31, 2017 is $131,000, net of income tax benefit of $80,000. As the Company's interest rate swap is not traded on a market exchange, the fair value is determined using a valuation model based on a discounted cash flow analysis. This analysis reflects the contractual terms of the interest rate swap agreement and uses observable market-based inputs, including estimated future LIBOR interest rates. The fair value of the Company's interest rate swap is the net difference in the discounted future fixed cash payments and the discounted expected variable cash receipts. The variable cash receipts are based on the expectation of future interest rates and are observable inputs available to a market participant. The interest rate swap valuation is classified in Level 2 of the fair value hierarchy, in accordance with the FASB's guidance on Fair Value Measurements and Disclosures.
Capitalized Lease Obligations
Upon acquisition of some centers, we assumed certain leases, primarily related to equipment, that constitute capital leases. As a result, we have recorded the underlying lease assets and capitalized lease obligations of $1,445,000 and $2,052,000 as of December 31, 2017 and 2016, respectively. These lease agreements provide three to five year terms.
Scheduled payments of the capitalized lease obligations are as follows:
2018 | $ | 1,211,000 | |
2019 | 289,000 | ||
Total | 1,500,000 | ||
Amounts related to interest | (55,000 | ) | |
Principal payments on capitalized lease obligation | $ | 1,445,000 | |
6. SHAREHOLDERS' EQUITY, STOCK PLANS AND PREFERRED STOCK
Stock Based Compensation Plans
The Company follows the FASB's guidance on Stock Compensation to account for stock-based payments granted to employees and non-employee directors.
Overview of Plans
In December 2005, the Compensation Committee of the Board of Directors adopted the 2005 Long-Term Incentive Plan (“2005 Plan”). The 2005 Plan allows the Company to issue stock options and other share and cash based awards. Under the 2005 Plan,
F-19
700,000 shares of the Company's common stock have been reserved for issuance upon exercise of equity awards granted thereunder. All grants under this plan expire 10 years from the date the grants were authorized by the Board of Directors.
In June 2008, the Company adopted the Advocat Inc. 2008 Stock Purchase Plan for Key Personnel (“Stock Purchase Plan”). The Stock Purchase Plan provides for the granting of rights to purchase shares of the Company's common stock to directors and officers and 150,000 shares of the Company's common stock has been reserved for issuance under the Stock Purchase Plan. The Stock Purchase Plan allows participants to elect to utilize a specified portion of base salary, annual cash bonus, or director compensation to purchase restricted shares or restricted share units (“RSU's”) at 85% of the quoted market price of a share of the Company's common stock on the date of purchase. The restriction period under the Stock Purchase Plan is generally two years from the date of purchase and during which the shares will have the rights to receive dividends, however, the restricted share certificates will not be delivered to the shareholder and the shares cannot be sold, assigned or disposed of during the restriction period and are subject to forfeiture. In June 2016, our shareholders approved an amendment to the Stock Purchase Plan to increase the number of shares of our common stock authorized under the Plan from 150,000 shares to 350,000 shares. No grants can be made under the Stock Purchase Plan after April 25, 2028.
In April 2010, the Compensation Committee of the Board of Directors adopted the 2010 Long-Term Incentive Plan (“2010 Plan”), followed by approval by the Company's shareholders in June 2010. The 2010 Plan allows the Company to issue stock appreciation rights, stock options and other share and cash based awards. In June 2017, our shareholders approved an amendment to the Long-Term Incentive Plan to increase the number of shares of our common stock authorized under the Plan from 380,000 shares to 680,000 shares. No grants can be made under the 2010 Plan after May 31, 2027.
Equity Grants and Valuations
During 2017 and 2016, the Compensation Committee of the Board of Directors approved grants totaling approximately 88,000 and 83,000, respectively, shares of restricted common stock to certain employees and members of the Board of Directors. These restricted shares vest one-third on the first, second and third anniversaries of the grant date. Unvested shares may not be sold or transferred. During the vesting period, dividends accrue on the restricted shares, but are paid in additional shares of common stock upon vesting, subject to the vesting provisions of the underlying restricted shares. The restricted shares are entitled to the same voting rights as other common shares. Upon vesting, all restrictions are removed.
The Company recorded non-cash stock-based compensation expense from continuing operations for equity grants and RSU's issued under the Plans of $1,027,000, $1,012,000, and $1,152,000 during the years ended December 31, 2017, 2016, and 2015, respectively. Such amounts are included as components of general and administrative expense or operating expense based upon the classification of cash compensation paid to the related employees. As of December 31, 2017, there was $593,000 in unrecognized compensation costs related to stock-based compensation to be recognized over the applicable remaining vesting periods. The Company estimated the total recognized and unrecognized compensation for all options and SOSARs using the Black-Scholes-Merton equity grant valuation model. Restricted stock awards are valued using the market price on the grant date.
The table below shows the weighted average assumptions the Company used to develop the fair value estimates under its option valuation model:
Year Ended December 31, | |||||
2017 | 2016 | 2015 | |||
Expected volatility (range) | N/A(1) | N/A(1) | 44%-49% | ||
Risk free interest rate (range) | N/A(1) | N/A(1) | 1.52%-1.87% | ||
Expected dividends | N/A(1) | N/A(1) | 2.15% | ||
Weighted average expected term (years) | N/A(1) | N/A(1) | 6 | ||
___________
(1) | The Company did not issue any options or other equity grants that would require application of the Black-Scholes-Merton equity grant valuation model during the years ended December 31, 2017 and 2016. All equity grants during these periods were restricted common shares which are valued using an intrinsic valuation method based on market price. |
In computing the fair value estimates using the Black-Scholes-Merton valuation model, the Company took into consideration the exercise price of the equity grants and the market price of the Company's stock on the date of grant. The Company used an expected volatility that equals the historical volatility over the most recent period equal to the expected life of the equity grants. The risk free interest rate is based on the U.S. treasury yield curve in effect at the time of grant. The Company used the expected dividend yield at the date of grant, reflecting the level of annual cash dividends currently being paid on its common stock.
In computing the fair value of these equity grants, the Company estimated the equity grants' expected term based on the average of the vesting term and the original contractual terms of the grants.
F-20
The table below describes the resulting weighted average grant date fair values calculated as well as the intrinsic value of options exercised under the Company's equity awards during each of the following years:
Year Ended December 31, | ||||||||||||
2017(1) | 2016(1) | 2015 | ||||||||||
Weighted average grant date fair value | $ | — | $ | — | $ | 3.78 | ||||||
Total intrinsic value of exercises | $ | 2,000 | $ | 3,000 | $ | 249,000 | ||||||
___________
(1) | The Company did not issue any options or other equity grants that would require application of the Black-Scholes-Merton equity grant valuation model during the years ended December 31, 2017 and 2016. All equity grants during this period were restricted common shares which are valued using an intrinsic valuation method based on market price. |
The following table summarizes information regarding stock options and SOSAR grants outstanding as of December 31, 2017:
Weighted | ||||||||||||||||||
Average | Intrinsic | Intrinsic | ||||||||||||||||
Range of | Exercise | Grants | Value-Grants | Grants | Value-Grants | |||||||||||||
Exercise Prices | Prices | Outstanding | Outstanding | Exercisable | Exercisable | |||||||||||||
$10.21 to $10.88 | $ | 10.63 | 44,000 | $ | — | 44,000 | $ | — | ||||||||||
$2.37 to $6.21 | $ | 5.56 | 167,000 | $ | 741,000 | 167,000 | $ | 741,000 | ||||||||||
211,000 | 211,000 | |||||||||||||||||
As of December 31, 2017, the outstanding equity grants have a weighted average remaining life of 3.25 and those outstanding equity grants that are exercisable have a weighted average remaining life of 3.25 years. During the year ended December 31, 2017, approximately 1,000 stock option and SOSAR grants were exercised under these plans. All of the equity grants exercised were net settled. The net proceeds from equity grants exercised in 2017 was $(94,000).
Summarized activity of the equity compensation plans is presented below:
Weighted | ||||||
SOSARs/ | Average | |||||
Options | Exercise Price | |||||
Outstanding, December 31, 2016 | 231,000 | $ | 6.97 | |||
Granted | — | — | ||||
Exercised | (1,000 | ) | 3.91 | |||
Expired or cancelled | (19,000 | ) | 10.73 | |||
Outstanding, December 31, 2017 | 211,000 | $ | 6.64 | |||
Exercisable, December 31, 2017 | 211,000 | $ | 6.64 | |||
Weighted | ||||||
Average | ||||||
Restricted | Grant Date | |||||
Shares | Fair Value | |||||
Outstanding, December 31, 2016 | 153,000 | $ | 9.47 | |||
Granted | 88,000 | 9.98 | ||||
Dividend Equivalents | 4,000 | 10.26 | ||||
Vested | (77,000 | ) | 9.06 | |||
Cancelled | (4,000 | ) | 10.10 | |||
Outstanding December 31, 2017 | 164,000 | $ | 9.95 | |||
F-21
Summarized activity of the Restricted Share Units for the Stock Purchase Plan is as follows:
Weighted | ||||||
Average | ||||||
Restricted | Grant Date | |||||
Share Units | Fair Value | |||||
Outstanding, December 31, 2016 | 54,000 | $ | 11.1 | |||
Granted | 26,000 | 9.98 | ||||
Dividend Equivalents | 1,000 | 10.26 | ||||
Vested | (37,000 | ) | 12.11 | |||
Cancelled | — | — | ||||
Outstanding December 31, 2017 | 44,000 | $ | 9.59 | |||
Series A Preferred Stock
The Company is authorized to issue up to 200,000 shares of Series A Preferred Stock. The Company's Board of Directors is authorized to establish the terms and rights of each series, including the voting powers, designations, preferences, and other special rights, qualifications, limitations, or restrictions thereof.
F-22
7. | NET INCOME (LOSS) PER COMMON SHARE |
Information with respect to the calculation of basic and diluted net income (loss) per common share is presented below:
Years Ended December 31, | ||||||||||||
2017 | 2016 | 2015 | ||||||||||
Numerator: Income (loss): | ||||||||||||
Income (loss) from continuing operations | $ | (4,799,000 | ) | $ | (1,744,000 | ) | $ | 2,752,000 | ||||
Loss from discontinued operations, net of income taxes | (28,000 | ) | (67,000 | ) | (1,128,000 | ) | ||||||
Net income (loss) | $ | (4,827,000 | ) | $ | (1,811,000 | ) | $ | 1,624,000 | ||||
Denominator: Basic Weighted Average Common Shares Outstanding: | 6,279,000 | 6,199,000 | 6,100,000 | |||||||||
Basic net income per common share | ||||||||||||
Income (loss) from continuing operations | $ | (0.76 | ) | $ | (0.28 | ) | $ | 0.45 | ||||
Income (loss) from discontinued operations | ||||||||||||
Operating loss, net of taxes | (0.01 | ) | (0.01 | ) | (0.18 | ) | ||||||
Discontinued operations, net of taxes | (0.01 | ) | (0.01 | ) | (0.18 | ) | ||||||
Basic net income (loss) per common share | $ | (0.77 | ) | $ | (0.29 | ) | $ | 0.27 | ||||
2017 | 2016 | 2015 | ||||||||||
Numerator: Income (loss) from continuing operations | $ | (4,799,000 | ) | $ | (1,744,000 | ) | $ | 2,752,000 | ||||
Loss from discontinued operations, net of income taxes | (28,000 | ) | (67,000 | ) | (1,128,000 | ) | ||||||
Net income (loss) | $ | (4,827,000 | ) | $ | (1,811,000 | ) | $ | 1,624,000 | ||||
Basic weighted average common shares outstanding | 6,279,000 | 6,199,000 | 6,100,000 | |||||||||
Incremental shares from assumed exercise of options, SOSARS and Restricted Stock Units | — | — | 215,000 | |||||||||
Denominator: Diluted Weighted Average Common Shares Outstanding: | 6,279,000 | 6,199,000 | 6,315,000 | |||||||||
Diluted net income per common share | ||||||||||||
Income (loss) from continuing operations | $ | (0.76 | ) | $ | (0.28 | ) | $ | 0.44 | ||||
Income (loss) from discontinued operations | ||||||||||||
Operating loss, net of taxes | (0.01 | ) | (0.01 | ) | (0.18 | ) | ||||||
Discontinued operations, net of taxes | (0.01 | ) | (0.01 | ) | (0.18 | ) | ||||||
Diluted net income (loss) per common share | $ | (0.77 | ) | $ | (0.29 | ) | $ | 0.26 | ||||
The dilutive effects of the Company's stock options, SOSARs, Restricted Shares and Restricted Share Units are included in the computation of diluted income per common share during the periods they are considered dilutive.
The following table reflects the weighted average outstanding SOSARs and Options that were excluded from the computation of diluted earnings per share, as they would have been anti-dilutive:
2017 | 2016 | 2015 | |||
SOSARs/Options Excluded | 45,000 | 31,000 | 62,000 | ||
The weighted average common shares for basic and diluted earnings for common shares was the same due to the losses in 2017 and 2016.
F-23
8. INCOME TAXES
Overview
On December 22, 2017, the President of the United States signed into law the Tax Cuts and Jobs Act tax reform legislation. This legislation creates significant change in U.S. tax law, including a reduction in the corporate tax rates, changes to net operating loss carryforwards and carrybacks, and a repeal of the corporate alternative minimum tax. The legislation did reduce the U.S. corporate tax rate from the current rate of 34% to 21% for tax periods beginning after December 31, 2017. As a result of the enacted law, the Company was required to revalue deferred tax assets and liabilities at the enacted federal and state rate in effect during their scheduled reversals, the federal of which is 21%. This revaluation of deferred tax assets resulted in an expense of $5,476,000 to income tax expense in continuing operations and a corresponding reduction in the deferred tax assets. Net operating losses generated prior to tax periods beginning after December 31, 2017 will not be limited in usage. However, net operating losses generated during tax periods beginning after December 31, 2017 will have limitations, but will carry-forward indefinitely. The other provisions of the Tax Cuts and Jobs Act do not have an expected material impact on the fiscal 2018 consolidated financial statements.
The Company considers the accounting for the deferred tax re-measurements and other items to be complete, but ongoing accounting guidance and interpretation could result in adjustments to the consolidated financial statements. The impact of the enactment of the Tax Act for fiscal year 2017 is reflected in the table below.
The provision (benefit) for income taxes on continuing operations for the years ended December 31, 2017, 2016 and 2015 is summarized as follows:
Year Ended December 31, | ||||||||||||
2017 | 2016 | 2015 | ||||||||||
Current provision (benefit) : | ||||||||||||
Federal | $ | 274,000 | $ | 17,000 | $ | 1,191,000 | ||||||
State | 472,000 | 522,000 | 947,000 | |||||||||
746,000 | 539,000 | 2,138,000 | ||||||||||
Deferred provision (benefit): | ||||||||||||
Federal | 6,585,000 | (1,284,000 | ) | (783,000 | ) | |||||||
State | (588,000 | ) | (285,000 | ) | (439,000 | ) | ||||||
5,997,000 | (1,569,000 | ) | (1,222,000 | ) | ||||||||
Provision (benefit) for income taxes of continuing operations | $ | 6,743,000 | $ | (1,030,000 | ) | $ | 916,000 | |||||
A reconciliation of taxes computed at statutory income tax rates on income (loss) from continuing operations is as follows:
Year Ended December 31, | ||||||||||||
2017 | 2016 | 2015 | ||||||||||
Provision (benefit) for federal income taxes at statutory rates | $ | 711,000 | $ | (889,000 | ) | $ | 1,247,000 | |||||
Provision for state income taxes, net of federal benefit | 421,000 | 120,000 | 688,000 | |||||||||
Valuation allowance changes affecting the provision for income taxes | (372,000 | ) | (45,000 | ) | (534,000 | ) | ||||||
Employment tax credits | (217,000 | ) | (529,000 | ) | (1,249,000 | ) | ||||||
Nondeductible expenses | 496,000 | 453,000 | 862,000 | |||||||||
Stock based compensation expense | (35,000 | ) | (62,000 | ) | (105,000 | ) | ||||||
Effect of Tax Cuts and Jobs Creation Act | 5,476,000 | — | — | |||||||||
Other | 263,000 | (78,000 | ) | 7,000 | ||||||||
Provision (benefit) for income taxes of continuing operations | $ | 6,743,000 | $ | (1,030,000 | ) | $ | 916,000 | |||||
F-24
Deferred Taxes
Deferred income taxes reflect the net tax effects of temporary differences between the carrying amounts of assets and liabilities for financial reporting purposes and the amounts used for income tax purposes. Deferred tax assets are reduced by a valuation allowance if, based upon the weight of available evidence, it is more likely than not that we will realize only some portion of the deferred tax assets. The net deferred tax assets and liabilities, at the respective income tax rates, are as follows:
December 31, | ||||||||
2017 | 2016 | |||||||
Deferred tax assets (liabilities): | ||||||||
Net operating loss and other carryforwards | $ | 495,000 | $ | 1,260,000 | ||||
Credit carryforwards | 3,237,000 | 3,162,000 | ||||||
Allowance for doubtful accounts | 3,626,000 | 3,772,000 | ||||||
Prepaid expenses | (731,000 | ) | (867,000 | ) | ||||
Deferred lease costs | 32,000 | 107,000 | ||||||
Depreciation | 1,190,000 | 2,122,000 | ||||||
Tax goodwill and intangibles | (972,000 | ) | (1,296,000 | ) | ||||
Stock-based compensation | 476,000 | 629,000 | ||||||
Accrued liabilities | 773,000 | 5,011,000 | ||||||
Accrued rent | 1,892,000 | 3,118,000 | ||||||
Kentucky and Kansas acquisition costs | 4,000 | 6,000 | ||||||
Impairment of long-lived assets | 186,000 | 269,000 | ||||||
Interest rate swap | (14,000 | ) | 49,000 | |||||
Hedge Ineffectiveness | (106,000 | ) | (69,000 | ) | ||||
Noncurrent self-insurance liabilities | 5,443,000 | 4,633,000 | ||||||
Other | — | 11,000 | ||||||
15,531,000 | 21,917,000 | |||||||
Less valuation allowance | (377,000 | ) | (732,000 | ) | ||||
$ | 15,154,000 | $ | 21,185,000 | |||||
Deferred Tax Valuation Allowance
The assessment of the amount of value assigned to our deferred tax assets under the applicable accounting standards is highly judgmental. We are required to consider all available positive and negative evidence in evaluating the likelihood that we will be able to realize the benefit of our deferred tax assets in the future. Such evidence includes scheduled reversals of deferred tax assets and liabilities, projected future taxable income, tax-planning strategies, and the results of recent operations. Since this evaluation requires consideration of historical and future events, there is significant judgment involved, and our conclusion could be materially different should certain of our expectations not transpire.
When assessing all available evidence, we consider the weight of the evidence, both positive and negative, based on the objectivity of the underlying evidence and the extent to which it can be verified. For the three-year period ended December 31, 2017, the Company has a cumulative pre-tax income from continuing operations of $2,838,000, which includes $1,944,000 of income attributable to the year ended December 31, 2017. Additionally, the Company recognized governmental and regulatory changes have put downward revenue pressure on the long-term care industry as a piece of negative evidence in our analysis. As a result of this negative evidence, the Company performed a thorough assessment of the available positive and negative evidence in order to ascertain whether it is more-likely-than-not that in future periods the Company will generate sufficient pre-tax income to utilize all of our federal deferred tax assets and our net operating loss and other carryforwards and credits. State deferred tax assets are considered for valuation separately and on a state-by-state basis.
The Company also identified several pieces of objective positive evidence which were considered and weighed in the analysis performed regarding the valuation of deferred tax assets, including, but not limited to the expected accretive strategic acquisitions completed by us during the three-year period, corporate and regional restructuring expected to reduce costs while maintaining revenue levels, the long-term expiration dates of a majority of the net operating losses and credits, our history of not having carryforwards or credits expire unutilized, and the completed divestiture of the centers in Mississippi in 2017 and Ohio in 2016.
F-25
In performing the analysis, the Company contemplated utilization of the deferred tax assets under multiple scenarios. After consideration of these factors, the Company determined that it was more likely than not that future taxable income would be sufficient to realize substantially all of the recorded value of the Company's deferred tax assets for federal income tax purposes.
Realization of the deferred tax assets is not assured and future events could result in a change in judgment. If future events result in a conclusion that realization is no longer more likely than not to occur, the Company would be required to establish a valuation allowance on the deferred tax assets at that time, which would result in a charge to income tax expense and a potentially material decrease in net income in the period in which the factors change our judgment.
At December 31, 2017, the Company had $6,480,000 of net operating losses, which expire at various dates beginning in 2019 and continue through 2021. The use of a portion of these loss carryforwards is limited by change in ownership provisions of the Federal tax code to a maximum of approximately $1,614,000. The Company has reduced the deferred tax asset and the corresponding valuation allowances for net operating loss deductions permanently lost as a result of the change in ownership provisions.
With respect to state deferred tax assets, the Company reduced the valuation allowance by approximately $357,000 in 2017, primarily related to the expectation that deferred tax assets for which valuation allowances had previously been applied would more-likely-than-not be utilized as a result of the increase in taxable income during the year ended December 31, 2017. In 2016 and 2015, the Company recorded a deferred tax provision to adjust approximately $47,000 and $315,000, respectively, of the valuation allowance on state deferred tax assets. The changes in valuation allowance were based on the Company's assessment of the realization of certain individual tax assets. The Company did not record a valuation allowance as of December 31, 2017.
Under the Work Opportunity Tax Credit ("WOTC") program, the Company recorded $210,000, $550,000 and $737,000 in Work Opportunity Tax Credits during 2017, 2016 and 2015, respectively.
The Company received a notice of an audit by the Internal Revenue Service related to the 2012 tax year, which was closed in 2016. As of December 31, 2017, the Company’s tax years for 2013 forward are subject to examination by tax authorities.
9. COMMITMENTS AND CONTINGENCIES
Lease Commitments
The Company is committed under long-term operating leases with various expiration dates and varying renewal options. Minimum annual rentals, including renewal option periods (exclusive of taxes, insurance, and maintenance costs) under these leases beginning January 1, 2018, are as follows:
2018 | $ | 58,046,000 | |
2019 | 59,511,000 | ||
2020 | 60,476,000 | ||
2021 | 61,336,000 | ||
2022 | 62,140,000 | ||
Thereafter | 764,178,000 | ||
$ | 1,065,687,000 | ||
Under these lease agreements, the Company's lease payments are subject to periodic annual escalations as described below and in Note 1, "Business and Summary of Significant Accounting Policies". Total lease expense for continuing operations was $54,988,000, $33,364,000 and $28,690,000 for 2017, 2016 and 2015, respectively. The accrued liability related to straight line rent was $6,983,000 and $7,920,000 at December 31, 2017 and 2016, respectively, and is included in “Other noncurrent liabilities” on the accompanying consolidated balance sheets.
Omega Master Lease
The Company leases 35 nursing centers from Omega, 15 of which are subject to a Master Lease, and another 8 centers are incorporated by amendment to the Master Lease, bringing the total to 23 centers. On October 20, 2006, the Company and Omega entered into a Third Amendment to Consolidated Amended and Restated Master Lease (“Lease Amendment”) to extend the term of its centers leased from Omega under the Master Lease. The Lease amendment extended the term to September 30, 2018 and provided a renewal option of an additional twelve years, and the Company had to notify Omega by September 30, 2017 about exercising the renewal option, which is further discussed below. Consistent with prior terms, the Master Lease provides for annual increases in lease payments equal to the lesser of two times the increase in the consumer price index or 3%. Under generally
F-26
accepted accounting principles, the Company is required to report these scheduled rent increases on a straight line basis over the term of the lease including the 12 year term of the renewal period. These scheduled increases had no effect on cash rent payments at the start of the lease term and only result in additional cash outlay as the annual increases take effect each year.
The Master Lease requires the Company to fund annual capital expenditures related to the leased centers at an amount currently equal to $450 per licensed bed. These amounts are subject to adjustment for increases in the Consumer Price Index. The Company is in compliance with the capital expenditure requirements. Total required capital expenditures during the remaining lease term and renewal options are $2,545,000. These capital expenditures are being depreciated on a straight-line basis over the shorter of the asset life or the appropriate lease term.
Upon expiration of the Master Lease or in the event of a default under the Master Lease, the Company is required to transfer all of the leasehold improvements, equipment, furniture and fixtures of the leased centers to Omega. The assets to be transferred to Omega are being amortized on a straight-line basis over the shorter of the remaining lease term or estimated useful life, and will be fully depreciated upon the expiration of the lease. All of the equipment, inventory and other related assets of the centers leased pursuant to the Master Lease have been pledged as security under the Master Lease. In addition, the Company has a letter of credit of $4,792,000 as a security deposit for the Company's leases with Omega, as described in Note 5, "Long-term Debt, Interest Rate Swap and Capitalized Lease Obligations".
On September 25, 2017, the Company entered into an agreement (the "Agreement") with Omega on certain terms of a new master lease to lease the 35 centers currently owned by Omega and operated by the Company. When finalized, the new master lease contemplated by the Agreement will consolidate the leases for all 35 centers under one new master lease upon the expiration of its current Master Lease on September 30, 2018.The lease will have an initial term of 12 years with two 10 year options to renew, provide a carryforward of monthly lease payment in place on October 1, 2018 and a fixed annual base rent escalator of 2.15%. The common date of annual lease escalators will be consolidated to October 1st of each year beginning on October 1, 2019. The Lease will provide for up to $35 million of landlord funded capital expenditure fund, which is subject to the impact on annual rent, and it will have a mechanism for agreed upon divestitures of centers. The lease will provide a security deposit of three months, as consistent with the existing Master Lease and will require minimum lease coverage ratio of 1.10x and annual minimum capital expenditure requirements with aggregate and per facility minimums.
Renovation Funding
In January 2013, we entered into an amendment to the Master lease with Omega under which Omega agreed to provide an additional $5,000,000 to fund renovations to two nursing centers located in Texas that are leased from Omega. The annual base rent related to these centers will be increased to reflect the amount of capital improvements to the respective centers as the related expenditures are made. The increase is based on a rate of 10.25% per year of the amount financed under this amendment.
The Company completed an expansion to one of its centers by making use of fifteen licensed beds it acquired in 2005. This expansion project was funded by Omega with the renovation funding previously described. Accordingly, the costs incurred to expand the center are recorded as a leasehold improvement asset with the amounts reimbursed by Omega for this project included as a long-term liability and amortized to rent expense over the remaining term of the lease. The capitalized leasehold improvements and lessor reimbursed costs are being amortized over the initial lease term ending in September 2018. The leasehold improvement asset and accumulated amortization are as follows:
December 31 | |||||||
2017 | 2016 | ||||||
Leasehold improvement | $ | 921,000 | $ | 921,000 | |||
Accumulated Amortization | (842,000 | ) | (737,000 | ) | |||
Net | $ | 79,000 | $ | 184,000 | |||
Golden Living Master Lease
The Company leases 20 nursing centers from Golden Living under a Master Lease. On October 1, 2016, the Company and Golden Living entered into a Master Lease agreement to lease eight centers located in Mississippi. On November 1, 2016, the Company and Golden Living entered into an Amended and Restated Master Lease ("Golden Living Lease Amendment") to extend the term of its centers leased from Golden Living and lease an additional twelve centers located in Alabama. The Amended Lease is triple net and has an initial term of ten years with two separate five year options to extend the term. Base rent for the amended lease is $24,675,000 for the first year and escalates 2% annually thereafter. Under generally accepted accounting principles, the Company is required to report these scheduled rent increases on a straight line basis over the term of the lease including the 10 year term of the renewal period. These scheduled increases had no effect on cash rent payments at the start of the lease term and only result in additional cash outlay as the annual increases take effect each year.
F-27
The Master Lease requires the Company to fund annual capital expenditures related to the leased centers at an amount currently equal to $510 per licensed bed. These amounts are subject to adjustment for increases in the Consumer Price Index. The Company is in compliance with the capital expenditure requirements. Total required capital expenditures during the remaining lease term and renewal options are $9,366,000. These capital expenditures are being depreciated on a straight-line basis over the shorter of the asset life or the appropriate lease term.
Upon expiration of the Master Lease or in the event of a default under the Master Lease, the Company is required to transfer all of the leasehold improvements, equipment, furniture and fixtures of the leased centers to Golden Living. The assets to be transferred to Golden Living are being amortized on a straight-line basis over the shorter of the remaining lease term or estimated useful life, and will be fully depreciated upon the expiration of the lease. All of the equipment, inventory and other related assets of the center leased pursuant to the Master Lease have been pledged as security under the Master Lease. In addition, the Company has a letter of credit of $6,169,000 as a security deposit for the Company's leases with Golden Living, as described in Note 5, "Long-term Debt, Interest Rate Swap and Capitalized Lease Obligations".
Other Operating Leases
In addition to the Omega and Golden Living Master Leases, the Company currently leases 15 other nursing centers which primarily operate under individual leases with Omega and other third parties. The lease terms for these centers range from seven years to nineteen years including renewal options. While the individual lease terms vary from center to center, the majority of the leases include annual lease increases which are capped and, in most cases, are subject to adjustment for increases in the Consumer Price Index. All operating leases are accounted for using a straight-line rent methodology.
Insurance Matters
Professional Liability and Other Liability Insurance
The Company has professional liability insurance coverage for its nursing centers that, based on historical claims experience, is likely to be substantially less than the claims that are expected to be incurred. Effective July 1, 2013, the Company established a wholly-owned, offshore limited purpose insurance subsidiary, SHC Risk Carriers, Inc. (“SHC”), to replace some of the expiring commercial policies. SHC covers losses up to specified limits per occurrence. All of the Company's nursing centers in Florida, Tennessee, and West Virginia are now covered under the captive insurance policies along with most of the nursing centers in Alabama, Kentucky, and Texas. The insurance coverage provided for these centers under the SHC policy includes coverage limits of at least $500,000 per medical incident with a sublimit per center of $1,000,000 and total annual aggregate policy limits of $5,000,000. All other centers within the Company’s portfolio are covered through various commercial insurance policies which provide similar coverage limits per medical incident, per location, and on an aggregate basis for covered centers. The deductibles for these policies are covered through the insurance subsidiary.
Reserve for Estimated Self-Insured Professional Liability Claims
Because the Company’s actual liability for existing and anticipated professional liability and general liability claims will exceed the Company’s limited insurance coverage, the Company has recorded total liabilities for reported and incurred, but not reported claims of $20,057,000 as of December 31, 2017. This accrual includes estimates of liability for incurred but not reported claims, estimates of liability for reported but unresolved claims, actual liabilities related to settlements, including settlements to be paid over time, and estimates of legal costs related to these claims. All losses are projected on an undiscounted basis and are presented without regard to any potential insurance recoveries. Amounts are added to the accrual for estimates of anticipated liability for claims incurred during each period, and amounts are deducted from the accrual for settlements paid on existing claims during each period.
The Company evaluates the adequacy of this liability on a quarterly basis. Semi-annually, the Company retains a third-party actuarial firm to assist in the evaluation of this reserve. Since May 2012, Merlinos & Associates, Inc. (“Merlinos”) has assisted management in the preparation of the appropriate accrual for incurred but not reported general and professional liability claims based on data furnished as of May 31 and November 30 of each year. Merlinos primarily utilizes historical data regarding the frequency and cost of the Company’s past claims over a multi-year period, industry data and information regarding the number of occupied beds to develop its estimates of the Company’s ultimate professional liability cost for current periods.
On a quarterly basis, the Company obtains reports of asserted claims and lawsuits incurred. These reports, which are provided by the Company’s insurers and a third party claims administrator, contain information relevant to the actual expense already incurred with each claim as well as the third-party administrator’s estimate of the anticipated total cost of the claim. This information is reviewed by the Company quarterly and provided to the actuary semi-annually. Based on the Company’s evaluation of the actual claim information obtained, the semi-annual estimates received from the third-party actuary, the amounts paid and committed for settlements of claims and on estimates regarding the number and cost of additional claims anticipated in the future, the reserve
F-28
estimate for a particular period may be revised upward or downward on a quarterly basis. Any increase in the accrual decreases results of operations in the period and any reduction in the accrual increases results of operations during the period.
The Company’s cash expenditures for self-insured professional liability costs from continuing operations were $6,593,000, $4,456,000, and $3,328,000 for the years ended December 31, 2017, 2016 and 2015, respectively.
The Company follows the FASB Accounting Standards Update, “Presentation of Insurance Claims and Related Insurance Recoveries,” that clarifies that a health care entity should not net insurance recoveries against a related professional liability claim and that the amount of the claim liability should be determined without consideration of insurance recoveries. Accordingly, the estimated insurance recovery receivables are included within "Other Current Assets" on the Consolidated Balance Sheet. As of December 31, 2017 and 2016, there are no estimated insurance recovery receivables.
Although the Company adjusts its accrual for professional and general liability claims on a quarterly basis and retains a third-party actuarial firm semi-annually to assist management in estimating the appropriate accrual, professional and general liability claims are inherently uncertain, and the liability associated with anticipated claims is very difficult to estimate. Professional liability cases have a long cycle from the date of an incident to the date a case is resolved, and final determination of the Company’s actual liability for claims incurred in any given period is a process that takes years. As a result, the Company’s actual liabilities may vary significantly from the accrual, and the amount of the accrual has and may continue to fluctuate by a material amount in any given period. Each change in the amount of this accrual will directly affect the Company’s reported earnings and financial position for the period in which the change in accrual is made.
Other Insurance
With respect to workers' compensation insurance, substantially all of our employees became covered under either a prefunded deductible policy or state-sponsored programs. The Company has been and remains a non-subscriber to the Texas workers’ compensation system and is, therefore, completely self-insured for employee injuries with respect to its Texas operations. From June 30, 2003 until June 30, 2007, the Company’s workers’ compensation insurance programs provided coverage for claims incurred with premium adjustments depending on incurred losses. For the period from July 1, 2007 until June 30, 2008, the Company is completely insured for workers' compensation exposure. For the period from July 1, 2008 through December 31, 2017, the Company is covered by a prefunded deductible policy. Under this policy, the Company is self-insured for the first $500,000 per claim, subject to an aggregate maximum of $3,000,000. The Company funds a loss fund account with the insurer to pay for claims below the deductible. The Company accounts for premium expense under this policy based on its estimate of the level of claims subject to the policy deductibles expected to be incurred. The liability for workers’ compensation claims is $867,000 at December 31, 2017. The Company has a non-current receivable for workers’ compensation policies covering previous years of $1,113,000 as of December 31, 2017. The non-current receivable is a function of payments paid to the Company’s insurance carrier in excess of the estimated level of claims expected to be incurred.
As of December 31, 2017, the Company is self-insured for health insurance benefits for certain employees and dependents for amounts up to $200,000 per individual annually. The Company provides reserves for the settlement of outstanding self-insured health claims at amounts believed to be adequate. The liability for reported claims and estimates for incurred but unreported claims is $1,326,000 at December 31, 2017. The differences between actual settlements and reserves are included in expense in the period finalized.
Employment Agreements
The Company has employment agreements with certain members of management that provide for the payment to these members of amounts up to 2.0 times their annual salary in the event of a termination without cause, a constructive discharge (as defined in each employee agreement), or upon a change in control of the Company (as defined in each employee agreement). The maximum contingent liability under these agreements is $1,842,000 as of December 31, 2017. The terms of such agreements are from 1 to 3 years and automatically renew for 1 year if not terminated by the employee or the Company. In addition, upon the occurrence of any triggering event, these certain members of management may elect to require the Company to purchase equity awards granted to them for a purchase price equal to the difference in the fair market value of the Company's common stock at the date of termination versus the stated equity award exercise price. Based on the closing price of our common stock on December 31, 2017, there is $422,000 of contingent liabilities for the repurchase of the equity grants.
No amounts have been accrued for these contingent liabilities for members of management the Company currently employs.
Health Care Industry and Legal Proceedings
The provision of health care services entails an inherent risk of liability. Participants in the health care industry are subject to lawsuits alleging malpractice, violations of false claims acts, product liability, or related legal theories, many of which involve large claims and significant defense costs. Like many other companies engaged in the long-term care profession in the United
F-29
States, we have numerous pending liability claims, disputes and legal actions for professional liability and other related issues. It is expected that we will continue to be subject to such suits as a result of the nature of our business. Further, as with all health care providers, we are periodically subject to regulatory actions seeking fines and penalties for alleged violations of health care laws and are potentially subject to the increased scrutiny of regulators for issues related to compliance with health care fraud and abuse laws and with respect to the quality of care provided to residents of our center. Like other health care providers, in the ordinary course of our business, we are also subject to claims made by employees and other disputes and litigation arising from the conduct of our business.
As of December 31, 2017, we are engaged in 72 professional liability lawsuits, which are reserved for as discussed above. Five lawsuits are currently scheduled for trial or arbitration during the next twelve months, and it is expected that additional cases will be set for trial or hearing. The ultimate results of any of our professional liability claims and disputes cannot be predicted. We have limited, and sometimes no, professional liability insurance with regard to most of these claims. A significant judgment entered against us in one or more of these legal actions could have a material adverse impact on our financial position and cash flows.
In July 2013, the Company learned that the United States Attorney for the Middle District of Tennessee ("DOJ") had commenced a civil investigation of potential violations of the False Claims Act ("FCA").
In October 2014, the Company learned that the investigation was started by the filing under seal of a false claims action against the two centers that were the subject of the original CID. In connection with this matter, between July 2013 and early February 2016, the Company has received three civil investigative demands (a form of subpoena) for documents and information relating to our practices and policies for rehabilitation, and other services, our preadmission evaluation forms ("PAEs") required by TennCare and our Pre-Admission Screening and Resident Reviews ("PASRRs"). We have responded to those requests. The DOJ has also issued CID’s for testimony from current and former employees of the Company. The DOJ’s civil investigation of the Company’s practices and policies for rehabilitation now covers all of the Company’s centers, but thus far only documents from six of our centers have been requested.
In June 2016, the Company received an authorized investigative demand (a form of subpoena) for documents in connection with a criminal investigation by the DOJ related to our practices with respect to PAEs and PASRRs, and the Company has provided documents responsive to this subpoena and continues to provide additional information as requested. The Company cannot predict the outcome of these investigations or the related lawsuits, and the outcome could have a materially adverse effect on the Company, including the imposition of treble damages, criminal charges, fines, penalties and/or a corporate integrity agreement. The Company is committed to provide caring and professional services to its patients and residents in compliance with applicable laws and regulations.
In January 2009, a purported class action complaint was filed in the Circuit Court of Garland County, Arkansas against the Company and certain of its subsidiaries and Garland Nursing & Rehabilitation Center (the “Center”). The complaint alleges that the defendants breached their statutory and contractual obligations to the patients of the Center over the five-year period prior to the filing of the complaints. The lawsuit remains in its early stages and has not yet been certified by the court as a class action. The Company intends to defend the lawsuit vigorously.
We cannot currently predict with certainty the ultimate impact of any of the above cases on our financial condition, cash flows or results of operations. Our reserve for professional liability expenses does not include any amounts for the pending DOJ investigation or the purported class action against the Arkansas centers. An unfavorable outcome in any of these lawsuits or any of our professional liability actions, any regulatory action, any investigation or lawsuit alleging violations of fraud and abuse laws or of elderly abuse laws or any state or Federal False Claims Act case could subject us to fines, penalties and damages, including exclusion from the Medicare or Medicaid programs, and could have a material adverse impact on our financial condition, cash flows or results of operations.
11. SUBSEQUENT EVENT
Effective February 27, 2018, the Company executed a Fifth Amendment to the Amended Revolver and a Third Amendment to the Amended Mortgage Loan. Under the terms of the Amendments, the minimum fixed charge coverage ratio shall not be less than 1.01 to 1.00 for the quarter ending March 31, 2018 and for each quarter thereafter. There were no other changes to the terms of these loan agreements.
F-30
10. QUARTERLY FINANCIAL INFORMATION (UNAUDITED)
Selected quarterly financial information for each of the quarters in the years ended December 31, 2017 and 2016 is as follows:
Quarter | ||||||||||||||||
2017 | First | Second | Third | Fourth | ||||||||||||
Patient revenues, net | $ | 141,500,000 | $ | 142,550,000 | $ | 146,377,000 | $ | 144,367,000 | ||||||||
Professional liability expense (1) | 2,670,000 | 2,724,000 | 2,617,000 | 2,753,000 | ||||||||||||
Income (loss) from continuing operations | 1,348,000 | 381,000 | (581,000 | ) | (5,947,000 | ) | ||||||||||
Income (loss) from discontinued operations | (15,000 | ) | (28,000 | ) | 1,000 | 14,000 | ||||||||||
Net income (loss) | $ | 1,333,000 | $ | 353,000 | $ | (580,000 | ) | $ | (5,933,000 | ) | ||||||
Basic net income (loss) per common share: | ||||||||||||||||
Income (loss) from continuing operations | $ | 0.22 | $ | 0.06 | $ | (0.09 | ) | $ | (0.94 | ) | ||||||
Loss from discontinued operations | — | — | — | — | ||||||||||||
Net income (loss) per common share | $ | 0.22 | $ | 0.06 | $ | (0.09 | ) | $ | (0.94 | ) | ||||||
Diluted net income (loss) per common share: | ||||||||||||||||
Income (loss) from continuing operations | $ | 0.21 | $ | 0.06 | $ | (0.09 | ) | $ | (0.94 | ) | ||||||
Loss from discontinued operations | — | — | — | — | ||||||||||||
Net income (loss) per common share | $ | 0.21 | $ | 0.06 | $ | (0.09 | ) | $ | (0.94 | ) | ||||||
(1) | The Company's quarterly results are significantly affected by the amounts recorded for professional liability expense, as discussed further in Note 9, "Commitments and Contingencies". The amount of expense recorded for professional liability in each quarter of 2017 is set forth in the table above. |
F-31
Quarter | ||||||||||||||||
2016 | First | Second | Third | Fourth | ||||||||||||
Patient revenues, net | $ | 97,945,000 | $ | 95,805,000 | $ | 97,313,000 | $ | 135,000,000 | ||||||||
Professional liability expense (1) | 2,066,000 | 1,934,000 | 1,977,000 | 2,479,000 | ||||||||||||
Income (loss) from continuing operations | (74,000 | ) | (2,150,000 | ) | (958,000 | ) | 1,438,000 | |||||||||
Loss from discontinued operations | (37,000 | ) | — | (17,000 | ) | (13,000 | ) | |||||||||
Net income (loss) | $ | (111,000 | ) | $ | (2,150,000 | ) | $ | (975,000 | ) | $ | 1,425,000 | |||||
Basic net income (loss) per common share: | ||||||||||||||||
Income (loss) from continuing operations | $ | (0.01 | ) | $ | (0.35 | ) | $ | (0.16 | ) | $ | 0.24 | |||||
Loss from discontinued operations | (0.01 | ) | — | — | — | |||||||||||
Net income (loss) per common share | $ | (0.02 | ) | $ | (0.35 | ) | $ | (0.16 | ) | $ | 0.24 | |||||
Diluted net income (loss) per common share: | ||||||||||||||||
Income from continuing operations | $ | (0.01 | ) | $ | (0.35 | ) | $ | (0.16 | ) | $ | 0.24 | |||||
Loss from discontinued operations | (0.01 | ) | — | — | — | |||||||||||
Net income (loss) per common share | $ | (0.02 | ) | $ | (0.35 | ) | $ | (0.16 | ) | $ | 0.24 | |||||
(1) | The Company's quarterly results are significantly affected by the amounts recorded for professional liability expense, as discussed further in Note 9, "Commitments and Contingencies". The amount of expense recorded for professional liability in each quarter of 2016 is set forth in the table above. |
F-32
DIVERSICARE HEALTHCARE SERVICES, INC. AND SUBSIDIARIES
SCHEDULE II - VALUATION AND QUALIFYING ACCOUNTS
OF CONTINUING OPERATIONS
(in thousands)
Column A | Column B | Column C | Column D | Column E | ||||||||
Additions | Deductions | |||||||||||
Description | Balance at Beginning of Period | Charged to Costs and Expenses | Charged to Other Accounts | Other | (Write-offs) net of Recoveries | Balance at End of Period | ||||||
Year ended December 31, 2017: Allowance for doubtful accounts | $10,326 | $8,958 | $— | $— | $(5,049) | $14,235 | ||||||
Year ended December 31, 2016: Allowance for doubtful accounts | $8,180 | $7,163 | $— | $— | $(5,017) | $10,326 | ||||||
Year ended December 31, 2015: Allowance for doubtful accounts | $6,044 | $7,507 | $— | $— | $(5,371) | $8,180 | ||||||
S-1
DIVERSICARE HEALTHCARE SERVICES, INC. AND SUBSIDIARIES
SCHEDULE II - VALUATION AND QUALIFYING ACCOUNTS
(in thousands)
Column A | Column B | Column C | Column D | Column E | ||||||||
Additions | Deductions | |||||||||||
Description | Balance at Beginning of Period | Charged to Costs and Expenses | Charged to Other Accounts (2) | Other | Payments (1) | Balance at End of Period | ||||||
Year ended December 31, 2017: | ||||||||||||
Professional Liability Reserve | $19,977 | $7,935 | $— | $— | $(7,855) | $20,057 | ||||||
Workers Compensation Reserve | $171 | $995 | $— | $— | $(299) | $867 | ||||||
Health Insurance Reserve | $1,019 | $13,769 | $— | $— | $(13,462) | $1,326 | ||||||
Year ended December 31, 2016: | ||||||||||||
Professional Liability Reserve | $21,618 | $6,423 | $— | $114 | $(8,178) | $19,977 | ||||||
Workers Compensation Reserve | $227 | $372 | $— | $— | $(428) | $171 | ||||||
Health Insurance Reserve | $686 | $8,896 | $— | $(137) | $(8,426) | $1,019 | ||||||
Year ended December 31, 2015: | ||||||||||||
Professional Liability Reserve | $25,163 | $5,213 | $1,010 | $— | $(9,768) | $21,618 | ||||||
Workers Compensation Reserve | $250 | $364 | $— | $— | $(387) | $227 | ||||||
Health Insurance Reserve | $687 | $6,294 | $— | $— | $(6,295) | $686 | ||||||
(1) | Payments for the Professional Liability Reserve include amounts paid for claims settled during the period as well as payments made under structured arrangements for claims settled in earlier periods. |
(2) | The Company has presented the results of certain divestiture and lease termination transactions as discontinued operations. The amounts charged to Other Accounts represent the amounts charged to discontinued operations. |
S-2
Exhibit | ||
Number | Description of Exhibits | |
3.1 | Certificate of Incorporation of the Registrant (incorporated by reference to Exhibit 3.1 to the Company's Registration Statement No. 33-76150 on Form S-1, filed in paper - hyperlink is not required pursuant to Rule 105 of Regulation S-T). | ||
Certificate of Designation of Registrant (incorporated by reference to Exhibit 3.5 to the Company's quarterly report on Form 10-Q for the quarter ended September 30, 2006). | |||
3.3 | Bylaws of the Company (incorporated by reference to Exhibit 3.2 to the Company's Registration Statement No. 33-76150 on Form S-1, filed in paper - hyperlink is not required pursuant to Rule 105 of Regulation S-T). | ||
Bylaw Amendment adopted November 5, 2007 (incorporated by reference to Exhibit 3.4 to the Company's annual report on Form 10-K for the year ended December 31, 2007). | |||
3.5 | Amendment to Certificate of Incorporation dated March 23, 1995 (incorporated by reference to Exhibit A of Exhibit 1 to the Company's Form 8-A filed March 30, 1995, filed in paper - hyperlink is not required pursuant to Rule 105 of Regulation S-T). | ||
Certificate of Designation of Registrant (incorporated by reference to Exhibit 3.4 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2001). | |||
Certificate of Ownership and Merger of Diversicare Healthcare Services, Inc. with and into Advocat Inc. (incorporated by reference to Exhibit 3.1 to the Company's current report on Form 8-K filed March 14, 2013). | |||
Amendment to Certificate of Incorporation dated June 9, 2016 (incorporated by reference to Exhibit 3.8 to the Company's quarterly report on Form 10-Q for the quarter ended June 30, 2016). | |||
3.9 | Bylaw Second Amendment adopted April 14, 2016 (incorporated by reference to Exhibit 3.9 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2017. | ||
4.1 | Form of Common Stock Certificate (incorporated by reference to Exhibit 4 to the Company's Registration Statement No. 33-76150 on Form S-1, filed in paper - hyperlink is not required pursuant to Rule 105 of Regulation S-T). | ||
Master Agreement and Supplemental Executive Retirement Plan (incorporated by reference to Exhibit 10.6 to the Company's Registration Statement No. 33-76150 on Form S-1). | |||
10.2 | Form of Director Indemnification Agreement (incorporated by reference to Exhibit 10.8 to the Company's Registration Statement No. 33-76150 on Form S-1, filed in paper - hyperlink is not required pursuant to Rule 105 of Regulation S-T). | ||
10.3 | Advocat Inc. Guaranty in favor of Omega Healthcare Investors, Inc. dated May 10, 1994 (incorporated by reference to Exhibit 10.11 to the Company's Annual Report on Form 10-K for the fiscal year ended December 31, 1994, filed in paper - hyperlink is not required pursuant to Rule 105 of Regulation S-T). | ||
Settlement and Restructuring Agreement dated as of October 1, 2000 among Registrant, Diversicare Leasing Corp., Sterling Health Care Management, Inc., Diversicare Management Services Co., Advocat Finance, Inc., Omega Healthcare Investors, Inc. and Sterling Acquisition Corp. (incorporated by reference to Exhibit 10.83 to the Company's Annual Report on Form 10-K for the fiscal year ended December 31, 2000). | |||
Consolidated Amended and Restated Master Lease dated November 8, 2000, effective October 1, 2000, between Sterling Acquisition Corp. (as Lessor) and Diversicare Leasing Corp. (as Lessee) (incorporated by reference to Exhibit 10.84 to the Company's Annual Report on Form 10-K for the fiscal year ended December 31, 2000). | |||
Management Agreement effective October 1, 2000, between Diversicare Leasing Corp. and Diversicare Management Services Co. (incorporated by reference to Exhibit 10.85 to the Company's Annual Report on Form 10-K for the fiscal year ended December 31, 2000). | |||
Amended and Restated Security Agreement dated as of November 8, 2000 between Diversicare Leasing Corp. and Sterling Acquisition Corp. (incorporated by reference to Exhibit 10.86 to the Company's Annual Report on Form 10-K for the fiscal year ended December 31, 2000). | |||
Security Agreement dated as of November 8, 2000 between Sterling Health Care Management, Inc. and Sterling Acquisition Corp. (incorporated by reference to Exhibit 10.87 to the Company's Annual Report on Form 10-K for the fiscal year ended December 31, 2000). | |||
Guaranty given as of November 8, 2000 by Registrant, Advocat Finance, Inc., and Diversicare Management Services Co., in favor of Sterling Acquisition Corp. (incorporated by reference to Exhibit 10.88 to the Company's Annual Report on Form 10-K for the fiscal year ended December 31, 2000). | |||
First Amendment to Consolidated Amended and Restated Master Lease dated September 30, 2001 by and between Sterling Acquisition Corp. and Diversicare Leasing Corporation (incorporated by reference to Exhibit 10.126 to the Company's Annual Report on Form 10-K for the year ended December 31, 2001). | |||
Second Amendment to Consolidated Amended and Restated Master Lease dated as of June 15, 2005 by and between Sterling Acquisition Corp. and Diversicare Leasing Corporation (incorporated by reference to Exhibit 10.1 to the Company's Quarterly Report on Form 10-Q for the quarter ended June 30, 2005). | |||
Restructuring Stock Issuance and Subscription Agreement dated as of October 20, 2006 between Advocat Inc. and Omega Healthcare Investors, Inc. (incorporated by reference to Exhibit 10.1 to the Company's current report on Form 8-K filed October 24, 2006). | |||
Third Amendment to Consolidated Amended and Restated Master Lease executed as of October 20, 2006, to be effective as of October 1, 2006 by and between Sterling Acquisition Corp. and Diversicare Leasing Corporation (incorporated by reference to Exhibit 10.2 to the Company's current report on Form 8-K filed October 24, 2006). | |||
Subordinated Promissory Note in the amount of $2,533,614.53 issued to Omega HealthCare Investors Inc. dated as of October 1, 2006 (incorporated by reference to Exhibit 10.3 to the Company's current report on Form 8-K filed October 24, 2006). | |||
Fourth Amendment to Consolidated Amended and Restated Master Lease executed and delivered as of April 1, 2007 by and between Sterling Acquisition Corp., a Kentucky corporation, and Diversicare Leasing Corp., a Tennessee corporation (incorporated by reference to Exhibit 10.1 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2007). | |||
Fifth Amendment to Consolidated Amended and Restated Master Lease dated as of August 10, 2007 by and between Sterling Acquisition Corp., a Kentucky corporation, and Diversicare Leasing Corp., a Tennessee corporation (incorporated by reference to Exhibit 10.7 to the Company's quarterly report on Form 10-Q for the quarter ended September 30, 2007). | |||
Sixth Amendment to Consolidated Amended and Restated Master Lease dated as of March 14, 2008 by and between Sterling Acquisition Corp., a Kentucky corporation, and Diversicare Leasing Corp., a Tennessee corporation (incorporated by reference to Exhibit 10.1 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2008). | |||
Seventh Amendment to Consolidated Amended and Restated Master Lease dated as of October 24, 2008 by and between Sterling Acquisition Corp., a Kentucky corporation, and Diversicare Leasing Corp., a Tennessee corporation (incorporated by reference to Exhibit 10.1 to the Company's quarterly report on Form 10-Q for the quarter ended September 30, 2008). | |||
Advocat Inc. 2005 Long-Term Incentive Plan (incorporated by reference to Appendix A to the Company's Definitive Proxy Statement on Schedule 14A filed on April 20, 2006). | |||
First Amendment to the Advocat Inc. 2005 Long-Term Incentive Plan (incorporated by reference to Exhibit 10.63 to the Company's annual report on Form 10-K for the year ended December 31, 2008). | |||
Advocat Inc. 2010 Long-Term Incentive Plan (incorporated by reference to Appendix A to the Company's Definitive Proxy Statement on Schedule 14A filed on April 28, 2010). | |||
Advocat Inc. 2008 Stock Purchase Plan for Key Personnel (incorporated by reference to Appendix A to the Company's Definitive Proxy Statement on Schedule 14A filed May 2, 2008). | |||
Ninth Amendment to Consolidated Amended and Restated Master Lease dated as of May 5, 2009 by and between Sterling Acquisition Corp., a Kentucky corporation, and Diversicare Leasing Corp., a Tennessee corporation (incorporated by reference to Exhibit 10.1 to the Company's quarterly report on Form 10-Q for the quarter ended June 30, 2009). | |||
Tenth Amendment to Consolidated Amended and Restated Master Lease dated as of September 8, 2009 by and between Sterling Acquisition Corp., a Kentucky corporation, and Diversicare Leasing Corp., a Tennessee corporation (incorporated by reference to Exhibit 10.1 to the Company's quarterly report on Form 10-Q for the quarter ended September 30, 2009). | |||
Lease Agreement dated as of July 14, 2010 by and between Diversicare Rose Terrace, LLC, a subsidiary of the registrant, and A.B.E., LLC (incorporated by reference to Exhibit 10.4 to the Company's quarterly report on Form 10-Q for the quarter ended June 30, 2010). | |||
Eleventh Amendment to the Amended and Restated Master Lease between the Company and Sterling Acquisition Corp., an affiliate of Omega Healthcare Investors, Inc. (incorporated by reference to Exhibit 10.1 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2011). | |||
Swap Agreement between the Company and The PrivateBank and Trust Company dated as of March 1, 2011 (incorporated by reference to Exhibit 10.6 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2011). | |||
Amended and Restated Employment Agreement effective as of April 1, 2012, by and between Advocat Inc., a Delaware corporation, and Kelly Gill (incorporated by reference to Exhibit 10.2 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2012). | |||
Employment Agreement effective August 20, 2012, between James R. McKnight, Jr. and Advocat Inc. (incorporated by reference to Exhibit 10.1 to the Company's quarterly report on Form 10-Q for the quarter ended September 30, 2012). | |||
Employment Agreement effective January 1, 2013, between Leslie Campbell and Advocat Inc. (incorporated by reference to Exhibit 10.49 to the Company’s annual report on Form 10-K for the year ended December 31, 2012). | |||
Amendment No. 1 to Amended and Restated Employment Agreement effective as of March 1, 2013 by and between Advocat Inc., a Delaware corporation, and Kelly Gill (incorporated by reference to Exhibit 10.50 to the Company's annual report on Form 10-K for the year ended December 31, 2012). | |||
Asset Purchase Agreement effective March 6, 2013 between the Company and Cumberland & Ohio Co. of Texas, as receiver of the assets of SeniorTrust of Florida, Inc. (incorporated by reference to Exhibit 10.3 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2013). | |||
Operations Transfer Agreement effective March 6, 2013 by and between certain subsidiaries of the Company and the Cumberland & Ohio Co. of Texas, as receiver of the assets of SeniorTrust of Florida, Inc. (incorporated by reference to Exhibit 10.4 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2013). | |||
Amended and Restated Revolving Loan and Security Agreement dated April 30, 2013 among the Company and a syndicate of financial institutions and banks, including The PrivateBank as the Administering Agent (incorporated by reference to Exhibit 10.1 to the Company's quarterly report on Form 10-Q for the quarter ended June 30, 2013). | |||
Amended and Restated Term Loan and Security Agreement dated April 30, 2013 among the Company and a syndicate of financial institutions and banks, including The PrivateBank as the Administering Agent (incorporated by reference to Exhibit 10.6 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2013). | |||
Amended and Restated Guaranty (Revolver) dated as of April 30, 2013, by the Company to and for the benefit of The PrivateBank in its capacity as administrative agent (incorporated by reference to Exhibit 10.7 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2013). | |||
Amended and Restated Guaranty (Term Loan) dated as of April 30, 2013, by the Company to and for the benefit of The PrivateBank in its capacity as administrative agent (incorporated by reference to Exhibit 10.8 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2013). | |||
Thirteenth Amendment to Consolidated Amended and Restated Master Lease effective September 1, 2013 by and between Sterling Acquisition Corp. and Diversicare Leasing Corp. (incorporated by reference to Exhibit 10.1 to the Company's quarterly report on Form 10-Q for the quarter ended September 30, 2013). | |||
First Amendment and Consent to Amended and Restated Revolving Loan and Security Agreement dated as of November 1, 2013 among the Company and a syndicate of financial institutions and banks, including The PrivateBank as the Administering Agent (incorporated by reference to Exhibit 10.1 to the Company's annual report on Form 10-K for the year ended Decemeber 31, 2014). | |||
Asset Purchase Agreement dated April 3, 2014, by and between Diversicare Rose Terrace, LLC, and Rose Terrace Acq., LLC (incorporated by reference to exhibit 10.1 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2014). | |||
Second Amendment and Consent to Amended and Restated Revolving Loan and Security Agreement dated as of March 31, 2014, among the Company and a syndicate of financial institutions and banks, including The PrivateBank as the Administering Agent (incorporated by reference to exhibit 10.2 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2014). | |||
Term Loan and Security Agreement effective as of March 27, 2014, by and between Diversicare Rose Terrace, LLC and The PrivateBank And Trust Company (incorporated by reference to exhibit 10.3 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2014). | |||
Third Amendment and Consent to Amended And Restated Revolving Loan and Security Agreement dated as of July 1, 2014 by and among the Company and a syndicate of financial institutions and banks, including The PrivateBank as the Administering Agent (incorporated by reference to exhibit 10.2 to the Company's quarterly report on Form 10-Q for the quarter ended June 30, 2014). | |||
Third Amendment to Amended and Restated Term Loan And Security Agreement dated as of July 1, 2014, by and among the Company and a syndicate of financial institutions and banks, including The PrivateBank as the Administering Agent (incorporated by reference to exhibit 10.1 to the Company's quarterly report on Form 10-Q for the quarter ended June 30, 2014). | |||
Fifteenth Amendment to Consolidated Amended and Restated Master Lease dated as of June 30, 2014 by and between the Company and Sterling Acquisition Corp. (incorporated by reference to exhibit 10.3 to the Company's quarterly report on Form 10-Q for the quarter ended June 30, 2014). | |||
Asset Purchase Agreement dated February 1, 2015 by and between Diversicare Healthcare Services, Inc. and Barren County Health Care Center, Inc. (incorporated by reference to exhibit 10.1 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2015). | |||
Term Loan and Security Agreement dated as of February 2, 2015 by and between Diversicare Glasgow Property, LLC and The PrivateBank And Trust Company (incorporated by reference to exhibit 10.2 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2015). | |||
Asset Purchase Agreement dated November 1, 2015 by and between Diversicare Healthcare Services, Inc. and Haws Fulton Investors, LLC. | |||
Second Amended and Restated Term Loan and Security Agreement dated February 26, 2016 (incorporated by reference to exhibit 10.1 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2016). | |||
Third Amended and Restated Revolving Loan and Security Agreement dated February 26, 2016 (incorporated by reference to exhibit 10.2 to the Company's quarterly report on Form 10-Q for the quarter ended March 31, 2016). | |||
Amendment to Diversicare Healthcare Services, Inc. 2008 Employee Stock Purchase Plan for Key Personnel (incorporated by reference to exhibit 10.1 to the Company's quarterly report on Form 10-Q for the quarter ended June 30, 2016). | |||
First Amendment to Third Amended and Restated Revolving Loan and Security Agreement dated August 3, 2016 (incorporated by reference to exhibit 10.12 to the Company's quarterly report on Form 10-Q for the quarter ended June 30, 2016). | |||
First Amendment to Second Amended and Restated Term Loan and Security Agreement dated August 3, 2016 (incorporated by reference to exhibit 10.3 to the Company's quarterly report on Form 10-Q for the quarter ended June 30, 2016). | |||
Second Amendment to Third Amended and Restated Revolving Loan and Security Agreement dated October 3, 2016 (incorporated by reference to exhibit 10.3 to the Company's quarterly report on Form 10-Q for the quarter ended September 30, 2016). | |||
Third Amendment to the Third Amended and Restated Revolving Loan and Security Agreement dated December 29, 2016. | |||
Golden Living Master Lease Agreement dated October 1, 2016. | |||
Amended and Restated Golden Living Master Lease Agreement dated November 1, 2016. | |||
Fourth Amendment to the Third Amended and Restated Revolving Loan And Security Agreement dated June 30, 2017 (incorporated by reference to exhibit 10.1 to the Company's quarterly report on Form 10-Q for the quarter ended June 30, 2017). | |||
Second Amendment to the Second Amended and Restated Term Loan and Security Agreement dated June 30, 2017 (incorporated by reference to exhibit 10.2 to the Company's quarterly report on Form 10-Q for the quarter ended June 30, 2017). | |||
Binding Term Sheet for Master Lease Agreement dated September 25, 2017 (incorporated by refernce to exhibit 10.1 to the Company's quarterly report on Form 10-Q for the quarter ended September 30, 2017). | |||
Fifth Amendment to Third Amended and Restated Revolving Loan and Security Agreement dated February 27, 2018. | |||
Third Amendment to Second Amended and Restated Term Loan and Security Agreement dated February 27, 2018. | |||
Subsidiaries of the Registrant. | |||
Consent of BDO USA, LLP. | |||
Certification of Chief Executive Officer pursuant to Rule 13a-14(a) or Rule 15d-14(a). | |||
Certification of Chief Financial Officer pursuant to Rule 13a-14(a) or Rule 15d-14(a). | |||
Certification of Chief Executive Officer and Chief Financial Officer pursuant to Rule 13a-14(b) or Rule 15d-14(b). | |||
101.INS | XBRL Instance Document | ||
101.SCH | XBRL Taxonomy Extension Schema Document | ||
101.CAL | XBRL Taxonomy Extension Calculation Linkbase Document | ||
101.LAB | XBRL Taxonomy Extension Labels Linkbase Document | ||
101.PRE | XBRL Taxonomy Extension Presentation Linkbase Document | ||
* | Indicates management contract or compensatory plan or arrangement. | ||
** | Confidential treatment has been requested for portions of this exhibit | ||
