Attached files
| file | filename |
|---|---|
| EX-99.1 - EX-99.1 - AGILE THERAPEUTICS INC | a17-8386_1ex99d1.htm |
| 8-K - 8-K - AGILE THERAPEUTICS INC | a17-8386_18k.htm |
Exhibit 99.2
The SECURE Study, a Real-World Trial of a Low-Dose Contraceptive Patch: Addressing the Changing U.S. Population
AUTHORS:
Anita Nelson, Andrew Kaunitz, Robin Kroll, James Simon, Alfred Poindexter, Joseph Chiodo, Lisa Flood, Elizabeth Garner
OBJECTIVES:
To evaluate the efficacy, safety, and tolerability of AG200-15 in a representative U.S. population of women who wish to use a transdermal contraceptive delivery system (TCDS).
BACKGROUND:
AG200-15 a weekly transdermal contraceptive delivery system (TCDS) with the potential for improved compliance versus daily pills. Historical data regarding of the Ortho Evra® contraceptive patch showed that women and providers were enthusiastic regarding the product. AG200-15 has been shown to deliver similar drug exposure to daily oral doses of 30μg of ethinyl estradiol (EE). The progestin component of the AG200-15 patch, levonorgestrel (LNG), is considered as one of the safest progestins, with the lowest risk for venous thromboembolism (VTE) when combined with EE. AG200-15 delivers similar exposure to daily oral doses of 120ug of LNG.
The generic of Ortho Evra, Xulane®, the only contraceptive patch currently marketed in the U.S. delivers a dose of EE that has been shown, in area-under-the curve (AUC) analyses, to be 60% greater than an oral pill containing 35μg of EE.(1) The possibility that use of Xulane may be associated with an excess risk for cardiovascular events including VTE has resulted in a specific warning in the product label.
SECURE (Study to Evaluate Contraception Use, Reliability, and Effectiveness) a 1-year, single-arm, open-label, multicenter study was conducted to yield reliable data in a more real-world study population. Enrollment criteria and procedures were established to optimize clinical trial conduct and demonstrate efficacy as measured by Pearl Index (PI). The trial included a number of stringent trial design elements, including exclusion of treatment cycles not only for use of back-up contraception but also for lack of sexual activity. SECURE had broad entry criteria, placed no limitations on BMI or other demographic factors during enrollment, and enrolled a large and diverse population from the U.S. to assess efficacy across different groups but excluded women with conditions generally recognized to be contraindications to estrogen use. These entry criteria resulted in the inclusion of a substantial number of women with high BMI, who have frequently been under-represented in contraceptive studies.
METHODS:
The SECURE study enrolled sexually active female subjects at risk for pregnancy. Medical history, physical and gynecological exams, and laboratory testing were performed at screening to determine eligibility. Subjects successfully completing screening were offered enrollment. There were 8 scheduled in-person visits and 6 telephone contact visits over the 12-month treatment period. Scheduled office visits included review of vital signs, urine pregnancy testing, patch application site inspection, review of medication and eDiary compliance, adverse events (AE) and concomitant medications (CMED). Documented phone contacts were completed to review study medication and eDiary compliance, as well as AEs and CMEDs. Subjects recorded the following information in daily electronic diaries: dates of patch application and patch change/removal, anatomic site of patch placement (lower abdomen, buttock, or upper torso), and reasons for any unscheduled patch changes. Subjects also recorded sexual activity and use of back-up contraception. In subjects with documented positive qualitative urine (β-hCG) test serum quantitative β-hCG, pelvic examination and a transvaginal ultrasound were performed to assess the estimated date of contraception. An independent expert Pregnancy Review Committee (PRC) reviewed data for each reported pregnancy. The primary efficacy analysis for the study was based on the calculation of pregnancy rates using the Pearl Index (calculated as the number of on-treatment pregnancies times divided by the number of 28-day on-therapy cycles, multiplied by 1300) in subjects aged 18 to 35 years old at study entry irrespective of BMI, excluding all cycles in which no intercourse occurred or other birth control methods (i.e., back-up contraception) were used. Supportive life table efficacy analyses were also performed. Patch wearability and tolerability were also assessed. Safety was assessed via collection of treatment emergent adverse events in all enrolled subjects who wore at least one patch for any period of time.
RESULTS:
Consistent with its broad entry criteria, the SECURE study population was representative of the population of women in the United States with respect to key demographic criteria. 2,032 women, 18-40 years old, were enrolled and 988 (48.6%) completed the study and used AG200-15 for up to thirteen 28-day cycles (Figure 1).
Figure 1: SECURE Subject Disposition

Of enrolled subjects, 66.9% were Caucasian, 24.3% were African-American, 3.2% were Asian, and 4.7% were other (including 0.5% American Indian or Alaska Native and 0.4% Native Hawaiian or other Pacific Islander). Regarding ethnicity, 19.7% were Hispanic and 80.3% were non-Hispanic. The BMI range of enrolled subjects was 15.1 — 60 kg/m2 with 39.4% of the women being normal (BMI <25 kg/m2), 25.3% overweight (BMI > 25 to < 30), 35.3% obese (BMI > 30 kg/m2).
The PI for the overall intent to treat population of subjects < 35 years of age was 4.80 with an upper-bound of the 95% confidence interval of 6.06. The PI for Caucasian subjects was 4.63 (3.03, 6.23), for African-American subjects 4.05 (1.41, 6.69), and for Hispanic subjects 2.70 (0.34, 5.06). A positive correlation was observed between BMI/weight and % of subjects reporting pregnancies (Table 1) and (Figure 2 and 3).
Table 1: BMI and Pearl Index
|
|
|
|
|
% of Trial |
|
|
|
Upper Bound of |
|
|
BMI Category |
|
BMI (kg/m(2)) |
|
Population |
|
Pearl Index |
|
95% CI |
|
|
Normal |
|
<25 |
|
39 |
% |
3.03 |
|
4.62 |
|
|
Overweight |
|
25 - <30 |
|
25 |
% |
5.36 |
|
7.98 |
|
|
Obese |
|
> 30 |
|
35 |
% |
6.42 |
|
8.88 |
|
|
Non-Obese |
|
< 30 |
|
65 |
% |
3.94 |
|
5.35 |
|
|
Obese |
|
> 30 |
|
35 |
% |
6.42 |
|
8.88 |
|
Figure 2: % Pregnancy vs. Weight categories

Figure 3: % Pregnancy vs. BMI categories

Supportive life table analyses were performed. Results for subjects < 35 years of age are presented in Table 2.
Table 2: Pregnancy Rates Based on Life Table Analysis in Subjects < 35 Years of Age
|
Cycle |
|
Number |
|
Number of on- |
|
Probability |
|
95% CI |
|
|
1 |
|
1816 |
|
3 |
|
0.17 |
|
0.05, 0.51 |
|
|
2 |
|
1681 |
|
11 |
|
0.64 |
|
0.35, 1.15 |
|
|
3 |
|
1556 |
|
17 |
|
1.02 |
|
0.64, 1.64 |
|
|
4 |
|
1448 |
|
26 |
|
1.64 |
|
1.12, 2.40 |
|
|
5 |
|
1349 |
|
31 |
|
2.00 |
|
1.41, 2.84 |
|
|
6 |
|
1263 |
|
39 |
|
2.62 |
|
1.92, 3.58 |
|
|
7 |
|
1192 |
|
41 |
|
2.79 |
|
2.06, 3.77 |
|
|
8 |
|
1130 |
|
46 |
|
3.22 |
|
2.41, 4.28 |
|
|
9 |
|
1068 |
|
48 |
|
3.40 |
|
2.56, 4.50 |
|
|
10 |
|
1004 |
|
49 |
|
3.49 |
|
2.64, 4.61 |
|
|
11 |
|
968 |
|
51 |
|
3.69 |
|
2.81, 4.85 |
|
|
12 |
|
930 |
|
53 |
|
3.90 |
|
2.98, 5.10 |
|
|
13 |
|
893 |
|
56 |
|
4.22 |
|
3.25, 5.48 |
|
Prior to the start of the study, 34.7% were current hormonal contraceptive users, 43.1% were prior users (who had used hormonal contraceptives in the past), and 9.4% had never used hormonal methods. The overall completion rate for study subjects was 49.5%; 11.3% of subjects were lost to follow-up, 10.9% discontinued due to an adverse event, and 15.3% discontinued by withdrawing their consent. The most frequent hormone-related adverse events are shown in Table 3.
Table 3: Adverse Events
|
Adverse Event |
|
SECURE (n=2032) |
|
|
Headache |
|
4.3 |
% |
|
Nausea |
|
4.1 |
% |
|
Breast tenderness/pain/discomfort |
|
2.0 |
% |
|
Mood swings/changes/depression |
|
2.7 |
% |
|
Heavy irregular vaginal bleeding |
|
1.8 |
% |
The most common (>1%) adverse reactions leading to discontinuation were bleeding irregularities (1.8%) and any application site reaction (1.1%); all others were less than 1%. Subjects reported the presence and absences of bleeding as a study outcome in an electronic diary, these analyses are ongoing. Thus, bleeding patterns were rarely reported as an AE. Only 1.4% of women discontinued for bleeding issues. Serious adverse events were observed in 2% of subjects. The most common serious adverse events (occurring in > 2 women) included cholelithiasis (n=4), deep vein thrombosis (n=3), pulmonary embolism (n=3), depression (n=3), gastroenteritis (n=2), cholecystitis (n=2), and ectopic pregnancy (n=2). Overall, patch-related irritation and itching rates of reported patches worn, 83% had no patch site irritation and 65% had no itching. Generally, reported irritation and itching was mild. Severe itching or irritation were observed in 2.3% and 1.5% of patches worn, respectively. Of reported patches worn, the range of detachments was 10% in cycle 1 and reduced to 2% by cycle 13.
DISCUSSION:
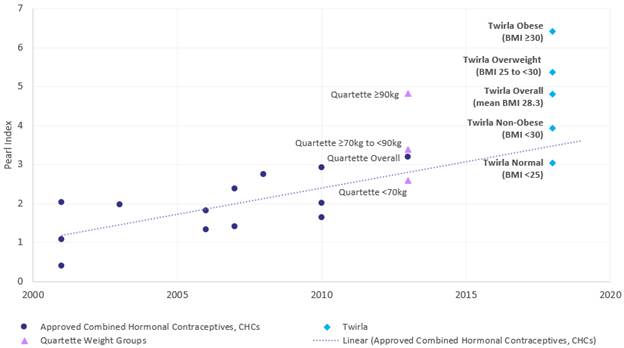
Pearl Indices for approved hormonal contraceptives have steadily risen over time as study design, pregnancy test sensitivity, and characteristics of study participants have changed.(2)
(Figure 4) As described by Trussell, the growing enrollment of more diverse, real-world populations appear to be increasingly representative of the likely actual users once the product is marketed. Therefore, “the rates of contraceptive failure in methods requiring adherence will be much higher than those previously observed”. (2) Considering the historical evolution in contraceptive trial outcomes, and with the emerging role of obesity has a key factor in CHC failure, the SECURE trial results appear to be consistent with expected outcomes for modern contraceptive trials, and within a range consistent with efficacy reported for more recently approved Tier 2 contraceptive methods.
Figure 4: Historical Pearl Indices for CHCs Approved Since 2000 and the Pearl Indices Observed in the SECURE Trial
A drawback of the PI, an efficacy parameter whose use in clinical trials of new contraceptives is mandated by the FDA, is that it assumes a constant failure rate over time. In fact, risk of pregnancy changes as clinical trials continue. Extensive data characterizing the efficacy of contraceptives utilizes the PI, as presented in Figure 5. In contrast with the PI, life table analysis has the advantage of eliminating time-related biases. As a result, the life table analysis is a better representation of a contraceptives effect over time, especially with the use of a patch which requires some learning. In Phase 3 clinical trials in the United States, first year failure rates for products approved before 2011 ranged from 2.1-3.5%.(3) Estimates of typical use failure for OC use in the general population were closer to 8%.(4) Therefore, the rate of 4.22% after 1 year in SECURE may be expected when compared to clinical trial results in trials run in less generalizable, more restrictive trial designs.
The demographics of the U.S. population are changing. Between 1999 and 2014, the prevalence of obesity increased significantly (Figure 5).(5)
Figure 5. Trends in obesity prevalence among adults aged 20 and over and youth aged 2-19 years: United States, 1999-2000 through 2013-2014
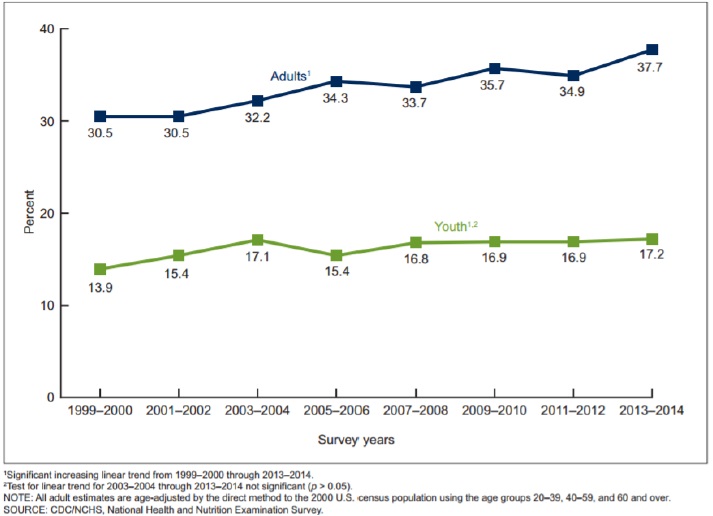
According to the American College of Obstetricians and Gynecologists, obesity represents “the most common health care problem in women of reproductive age,”(6) However, the role of weight and/or BMI as potential risk factors for hormonal contraception failure has remains inadequately studied in prospective clinical trials. In initial 2001 product labeling for Ortho Evra, the first combined HC patch approved in the U.S., a Limitation of Use states: “Ortho Evra may be less effective in preventing pregnancy in women who weigh 198 lbs. (90 kg) or more.”(1) In 2015, the FDA published a seminal paper which brought attention to the increasingly important issue of obesity and effectiveness of hormonal contraception and reported that obesity may increase the risk of unintended pregnancy in women using hormonal contraception.(6) Historically, obese women have often been excluded from and/or under-represented in contraceptive trials. As a result, there has been a paucity of clinical trial data on hormonal contraceptive safety and effectiveness in obese women.
Based on a review of publicly available FDA NDA review documents and relevant published literature, it is likely that the SECURE trial population is the most overweight on record for a pivotal Phase 3 contraceptive trial. In the SECURE trial, AG200-15 failure rate was lowest in
normal weight subjects (BMI < 25 kg/m2), with a Pearl Index (PI) of 3.03 (95% CI 1.44, 4.62). When women with a BMI between 25 and < 30 kg/m2 were combined with normal weight women, the combined PI was marginally higher at 3.94 (95% CI 2.53, 5.35), but still within the range of approved combined hormonal contraceptive products. The PIs for overweight and obese subjects were 5.36 (95% 2.74, 7.98) and 6.42 (95% CI 3.96, 8.88), respectively. Although higher, the PI values in overweight and obese subjects in the SECURE trial are not substantially different from PI values that have been observed in sub-population analyses in a number of more recent NDA reviews of approved products consistent with heavier/higher BMI subjects experiencing lower contraceptive efficacy. A PI for those not using contraception is approximately 190 (James Trussell, personal communication, 5 August 2016). Pearl Indices, reported here, are somewhat lower in non-obese and normal-weight women compared to obese women, but both populations are substantially better than non-hormonal barrier methods. Other factors such as race and ethnicity, did not appear to impact the Pearl Index results.
In summary, AG200-15 has demonstrated contraceptive efficacy that is comparable to products that are currently in use in the U.S. population, particularly for non-obese women. AG200-15 was generally well tolerated and had an overall favorable safety profile, consistent with publicly available information for other low-dose combined hormonal products. Overall, patch-related irritation and itching rates were low and the patch adhesion profile was favorable with a low rate of detachment. Consistent with the emerging literature on the role of obesity in hormonal contraceptive efficacy, a weight effect was observed for AG200-15.
CONCLUSIONS:
· The SECURE trial was conducted in a diverse, real-world population of women that reflects current U.S. obesity trends.
· Pearl Index and life table results from the SECURE trial suggest that AG200-15 is an important contraceptive option for women who prefer a non-daily hormonal method.
· AG200-15 was well tolerated and rates of hormone related adverse events were comparable to approved combined hormonal contraceptives.
· Patch-related irritation and itching rates were low and the patch adhesion profile was favorable.
· The SECURE trial has provided substantial new data on HC effectiveness in obese and very obese women and supports the hypothesis that for short-acting combined hormonal contraceptives, obesity is associated with higher failure rates.
· Additional analyses of clinical trial data are needed to understand not only the magnitude of the impact of obesity, but also to better understand why obese women experience higher contraception failure rates.
REFERENCES:
(1) Ortho Evra label. Accessed Feb. 2017; http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/021180s035lbl.pdf
(2) Trussell J, Portman D. The creeping pearl: why has the rate of contraceptive failure increased in clinical trials of combined hormonal contraceptive pills? Contraception 2013; 88; 604-10.
(3) Dinger J, et al. Effectiveness of oral contraceptive pills in a large U.S. cohort comparing progestogen and regimen. Obstet Gynecol 2011;117:33-40.
(4) Kost K. et al. Estimaters of contraceptive failure from the 2002 National Survery of Family Growth. Contraception 2008; 77(1): 10-21.
(5) Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011—2014. NCHS data brief, no 219. Hyattsville, MD: National Center for Health Statistics. 2015ACOG Practice Bulletin No. 156, Dec 2015.
(6) Yamazaki M, et al. Effect on obesity on the effectiveness of hormonal contraceptives: an individual participant data meta-analysis. Contraception 2015;92,445-452.
