Attached files
| file | filename |
|---|---|
| 8-K - 8-K - Inspyr Therapeutics, Inc. | v399026_8k.htm |
| EX-99.01 - EXHIBIT 99.01 - Inspyr Therapeutics, Inc. | v399026_ex99-01.htm |
| EX-99.02 - EXHIBIT 99.02 - Inspyr Therapeutics, Inc. | v399026_ex99-02.htm |
Exhibit 99.03
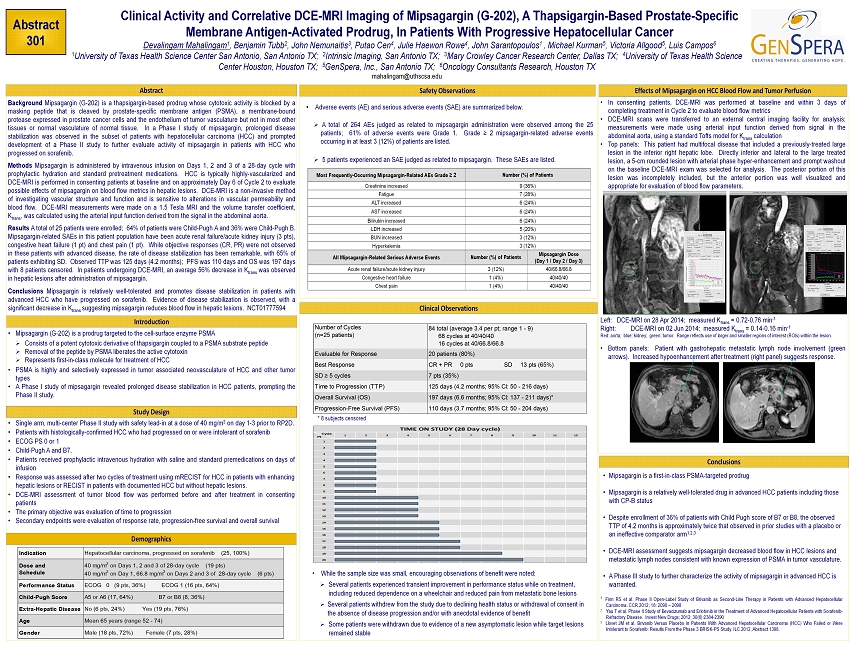
Introduction Clinical Activity and Correlative DCE - MRI Imaging of Mipsagargin (G - 202), A Thapsigargin - Based Prostate - Specific Membrane Antigen - Activated Prodrug, In Patients With Progressive Hepatocellular Cancer Devalingam Mahalingam 1 , Benjamin Tubb 2 , John Nemunaitis 3 , Putao Cen 4 , Julie Haewon Rowe 4 , John Sarantopoulos 1 , Michael Kurman 5 , Victoria Allgood 5 , Luis Campos 6 1 University of Texas Health Science Center San Antonio, San Antonio TX; 2 Intrinsic Imaging, San Antonio TX; 3 Mary Crowley Cancer Research Center, Dallas TX; 4 University of Texas Health Science Center Houston, Houston TX; 5 GenSpera, Inc., San Antonio TX; 6 Oncology Consultants Research, Houston TX mahalingam@uthscsa.edu Background Mipsagargin (G - 202 ) is a thapsigargin - based prodrug whose cytotoxic activity is blocked by a masking peptide that is cleaved by prostate - specific membrane antigen (PSMA), a membrane - bound protease expressed in prostate cancer cells and the endothelium of tumor vasculature but not in most other tissues or normal vasculature of normal tissue . In a Phase I study of mipsagargin, prolonged disease stabilization was observed in the subset of patients with hepatocellular carcinoma (HCC) and prompted development of a Phase II study to further evaluate activity of mipsagargin in patients with HCC who progressed on sorafenib . Methods Mipsagargin is administered by intravenous infusion on Days 1 , 2 and 3 of a 28 - day cycle with prophylactic hydration and standard pretreatment medications . HCC is typically highly - vascularized and DCE - MRI is performed in consenting patients at baseline and on approximately Day 6 of Cycle 2 to evaluate possible effects of mipsagargin on blood flow metrics in hepatic lesions . DCE - MRI is a non - invasive method of investigating vascular structure and function and is sensitive to alterations in vascular permeability and blood flow . DCE - MRI measurements were made on a 1 . 5 Tesla MRI and the volume transfer coefficient, K trans , was calculated using the arterial input function derived from the signal in the abdominal aorta . Results A total of 25 patients were enrolled ; 64 % of patients were Child - Pugh A and 36 % were Child - Pugh B . Mipsagargin - related SAEs in this patient population have been acute renal failure/acute kidney injury ( 3 pts ), congestive heart failure ( 1 pt ) and chest pain ( 1 pt ) . While objective responses (CR, PR) were not observed in these patients with advanced disease, the rate of disease stabilization has been remarkable, with 65 % of patients exhibiting SD . Observed TTP was 125 days ( 4 . 2 months) ; PFS was 110 days and OS was 197 days with 8 patients censored . In patients undergoing DCE - MRI, an average 56 % decrease in K trans was observed in hepatic lesions after administration of mipsagargin . Conclusions Mipsagargin is relatively well - tolerated and promotes disease stabilization in patients with advanced HCC who have progressed on sorafenib . Evidence of disease stabilization is observed, with a significant decrease in K trans suggesting mipsagargin reduces blood flow in hepatic lesions . NCT 01777594 Clinical Observations • Mipsagargin is a first - in - class PSMA - targeted prodrug • Mipsagargin is a relatively well - tolerated drug in advanced HCC patients including those with CP - B status • Despite enrollment of 36% of patients with Child Pugh score of B7 or B8, the observed TTP of 4.2 months is approximately twice that observed in prior studies with a placebo or an ineffective comparator arm 1,2,3 • DCE - MRI assessment suggests mipsagargin decreased blood flow in HCC lesions and metastatic lymph nodes consistent with known expression of PSMA in tumor vasculature . • A Phase III study to further characterize the activity of mipsagargin in advanced HCC is warranted. Abstract 301 Safety Observations • Mipsagargin (G - 202 ) is a prodrug targeted to the cell - surface enzyme PSMA » Consists of a potent cytotoxic derivative of thapsigargin coupled to a PSMA substrate peptide » Removal of the peptide by PSMA liberates the active cytotoxin » Represents first - in - class molecule for treatment of HCC • PSMA is highly and selectively expressed in tumor associated neovasculature of HCC and other tumor types • A Phase I study of mipsagargin revealed prolonged disease stabilization in HCC patients, prompting the Phase II study . Effects of Mipsagargin on HCC Blood Flow and Tumor Perfusion Conclusions Abstract Most Frequently - Occurring Mipsagargin - Related AEs Grade ≥ 2 Number (%) of Patients Creatinine increased 9 (36%) Fatigue 7 (28%) ALT increased 6 (24%) AST increased 6 (24%) Bilirubin increased 6 (24%) LDH increased 5 (20%) BUN increased 3 (12%) Hyperkalemia 3 (12%) All Mipsagargin - Related Serious Adverse Events Number (%) of Patients Mipsagargin Dose (Day 1 / Day 2 / Day 3) Acute renal failure/acute kidney injury 3 (12%) 40/66.8/66.8 Congestive heart failure 1 (4%) 40/40/40 Chest pain 1 (4%) 40/40/40 • In consenting patients, DCE - MRI was performed at baseline and within 3 days of completing treatment in Cycle 2 to evaluate blood flow metrics • DCE - MRI scans were transferred to an external central imaging facility for analysis ; measurements were made using arterial input function derived from signal in the abdominal aorta, using a standard Tofts model for K trans calculation • Top panels : This patient had multifocal disease that included a previously - treated large lesion in the inferior right hepatic lobe . Directly inferior and lateral to the large treated lesion, a 5 - cm rounded lesion with arterial phase hyper - enhancement and prompt washout on the baseline DCE - MRI exam was selected for analysis . The posterior portion of this lesion was incompletely included, but the anterior portion was well visualized and appropriate for evaluation of blood flow parameters . Left : DCE - MRI on 28 Apr 2014 ; measured K trans = 0 . 72 - 0 . 76 min - 1 Right : DCE - MRI on 02 Jun 2014 ; measured K trans = 0 . 14 - 0 . 16 min - 1 Red : aorta ; blue : kidney ; green : tumor . Range reflects use of larger and smaller regions of interest (ROIs) within the lesion . • Bottom panels : Patient with gastrohepatic metastatic lymph node involvement (green arrows) . Increased hypoenhancement after treatment (right panel) suggests response . Study Design • Single arm, multi - center Phase II study with safety lead - in at a dose of 40 mg/m 2 on day 1 - 3 prior to RP 2 D . • Patients with histologically - confirmed HCC who had progressed on or were intolerant of sorafenib • ECOG PS 0 or 1 • Child - Pugh A and B 7 . • Patients received prophylactic intravenous hydration with saline and standard premedications on days of infusion • Response was assessed after two cycles of treatment using mRECIST for HCC in patients with enhancing hepatic lesions or RECIST in patients with documented HCC but without hepatic lesions . • DCE - MRI assessment of tumor blood flow was performed before and after treatment in consenting patients • The primary objective was evaluation of time to progression • Secondary endpoints were evaluation of response rate, progression - free survival and overall survival Demographics • Adverse events (AE) and serious adverse events (SAE) are summarized below . » A total of 264 AEs judged as related to mipsagargin administration were observed among the 25 patients ; 61 % of adverse events were Grade 1 . Grade ≥ 2 mipsagargin - related adverse events occurring in at least 3 ( 12 % ) of patients are listed . » 5 patients experienced an SAE judged as related to mipsagargin . These SAEs are listed . 1 Finn RS et al . Phase II Open - Label Study of Brivanib as Second - Line Therapy in Patients with Advanced Hepatocellular Carcinoma . CCR 2012 ; 18 : 2090 – 2098 2 Yau T et al . Phase II Study of Bevacizumab and Erlotonib in the Treatment of Advanced Hepatocellular Patients with Sorafenib - Refractory Disease . Invest New Drugs ; 2012 ; 30 ( 6 ) : 2384 - 2390 3 Llovet JM et al . Brivanib Versus Placebo in Patients With Advanced Hepatocellular Carcinoma (HCC) Who Failed or Were Intolerant to Sorafenib : Results From the Phase 3 BRISK - PS Study . ILC 2012 , Abstract 1398 . • While the sample size was small, encouraging observations of benefit were noted: » Several patients experienced transient improvement in performance status while on treatment, including reduced dependence on a wheelchair and reduced pain from metastatic bone lesions » Several patients withdrew from the study due to declining health status or withdrawal of consent in the absence of disease progression and/or with anecdotal evidence of benefit » Some patients were withdrawn due to evidence of a new asymptomatic lesion while target lesions remained stable * 8 subjects censored Number of Cycles (n=25 patients) 84 total (average 3.4 per pt; range 1 - 9) 68 cycles at 40/40/40 16 cycles at 40/66.8/66.8 Evaluable for Response 20 patients (80%) Best Response CR + PR 0 pts SD 13 pts (65%) SD ≥ 5 cycles 7 pts (35%) Time to Progression (TTP) 125 days (4.2 months; 95% Cl: 50 - 216 days) Overall Survival (OS) 197 days (6.6 months; 95% Cl: 137 - 211 days)* Progression-Free Survival (PFS) 110 days (3.7 months; 95% Cl: 50 - 204 days) Indication Hepatocellular carcinoma, progressed on sorafenib (25, 100%) Dose and Schedule 40 mg/m 2 on Days 1, 2 and 3 of 28-day cycle (19 pts) 40 mg/m 2 on Day 1, 66.8 mg/m 2 on Days 2 and 3 of 28-day cycle (6 pts) Performance Status ECOG 0 (9 pts, 36%) ECOG 1 (16 pts, 64%) Child-Pugh Score A5 or A6 (17, 64%) B7 or B8 (8, 36%) Extra-Hepatic Disease No (6 pts, 24%) Yes (19 pts, 76%) Age Mean 65 years (range 52 - 74) Gender Male (18 pts, 72%) Female (7 pts, 28%) Cycle Pt 1 2 3 4 5 6 7 8 9 10 11 12 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 TIME ON STUDY (28 Day cycle)
