Attached files
| file | filename |
|---|---|
| EX-23.1 - CONSENT - Benefytt Technologies, Inc. | d439448dex231.htm |
Table of Contents
As filed with the Securities and Exchange Commission on February 4, 2013.
Registration No. 333-185596
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
Amendment No. 3
to
FORM S-1
REGISTRATION STATEMENT
UNDER
THE SECURITIES ACT OF 1933
Health Insurance Innovations, Inc.
(Exact Name of Registrant as Specified in Its Charter)
| Delaware | 6411 | 46-1282634 | ||
| (State or Other Jurisdiction of Incorporation or Organization) |
(Primary Standard Industrial Classification Code Number) |
(I.R.S. Employer Identification Number) |
15438 N. Florida Avenue, Suite 201
Tampa, Florida, 33613
(877) 376-5831
(Address, Including Zip Code, and Telephone Number, Including Area Code, of Registrant’s Principal Executive Offices)
Michael W. Kosloske
Chairman, President and Chief Executive Officer
Health Insurance Innovations, Inc.
15438 N. Florida Avenue, Suite 201
Tampa, Florida, 33613
(877) 376-5831
(Name, Address, Including Zip Code, and Telephone Number, Including Area Code, of Agent For Service)
Copies to:
| Deanna Kirkpatrick, Esq. Davis Polk & Wardwell LLP 450 Lexington Avenue New York, New York 10017 (212) 450-4000 |
William J. Whelan, III, Esq. Cravath, Swaine & Moore LLP 825 Eighth Avenue New York, New York 10019 (212) 474-1000 |
Approximate date of commencement of proposed sale to the public: As soon as practicable after the effective date of this Registration Statement.
If any of the securities being registered on this form are to be offered on a delayed or continuous basis pursuant to Rule 415 under the Securities Act of 1933, check the following box. ¨
If this form is filed to register additional securities for an offering pursuant to Rule 462(b) under the Securities Act, check the following box and list the Securities Act registration statement number of the earlier effective registration statement for the same offering. ¨
If this form is a post-effective amendment filed pursuant to Rule 462(c) under the Securities Act, check the following box and list the Securities Act registration statement number of the earlier effective registration statement for the same offering. ¨
If this form is a post-effective amendment filed pursuant to Rule 462(d) under the Securities Act, check the following box and list the Securities Act registration statement number of the earlier effective registration statement for the same offering. ¨
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, or a smaller reporting company. See the definitions of “large accelerated filer,” “accelerated filer” and “smaller reporting company” in Rule 12b-2 of the Exchange Act.
| Large accelerated filer | ¨ | Accelerated filer | ¨ | |||||
| Non-accelerated filer | ¨ | (Do not check if a smaller reporting company) | Smaller reporting company | x | ||||
CALCULATION OF REGISTRATION FEE
| Title Of Each Class Of Securities To Be Registered |
Amount To Be |
Proposed Maximum Offering Price Per Share |
Proposed Maximum Aggregate Offering Price(2) |
Amount Of Registration Fee(3) |
||||||||||||
| Class A Common Stock, par value $0.001 per share |
5,366,667 | $ | 16.00 | $ | 85,866,672 | $ | 11,712.21 | |||||||||
| (1) | Includes 700,000 shares that the underwriters have the option to purchase to cover over-allotments, if any. |
| (2) | Estimated solely for the purpose of computing the amount of the registration fee pursuant to Rule 457(a) under the Securities Act. |
| (3) | Previously paid. |
The registrant hereby amends this registration statement on such date or dates as may be necessary to delay its effective date until the registrant shall file a further amendment which specifically states that this registration statement shall thereafter become effective in accordance with Section 8(a) of the Securities Act of 1933 or until the registration statement shall become effective on such date as the Commission, acting pursuant to said Section 8(a), may determine.
Table of Contents
The information in this prospectus is not complete and may be changed. We may not sell these securities until the registration statement filed with the Securities and Exchange Commission is effective. This prospectus is not an offer to sell these securities and we are not soliciting offers to buy these securities in any jurisdiction where the offer or sale is not permitted.
SUBJECT TO COMPLETION, DATED FEBRUARY 4, 2013
4,666,667 Shares

Health Insurance Innovations, Inc.
Class A Common Stock
We are selling 4,666,667 shares of our Class A common stock. This is our initial public offering and no public market exists for our Class A common stock. We anticipate that the initial public offering price of our Class A common stock will be between $14 and $16 per share. We have applied to list our Class A common stock on the NASDAQ Global Market under the symbol “HIIQ.”
We will be a holding company and our sole asset will be approximately 35% of the aggregate membership interests of Health Plan Intermediaries Holdings, LLC. Immediately following this offering, the holders of our Class A common stock will collectively own 100% of the economic interests in Health Insurance Innovations, Inc. and have 35% of the voting power of Health Insurance Innovations, Inc. The holders of our Class B common stock, which are entities beneficially owned by our Chairman, President and Chief Executive Officer, will have the remaining 65% of the voting power of Health Insurance Innovations, Inc.
We have granted the underwriters the right to purchase an additional 700,000 shares of Class A common stock to cover over-allotments.
We are an “emerging growth company” as defined in the Jumpstart Our Business Startups Act of 2012 (the “JOBS Act”) and will therefore be subject to reduced reporting requirements.
Investing in our Class A common stock involves risks. See “Risk Factors” beginning on page 16.
| Price to Public |
Underwriting Discounts and |
Proceeds to Company | ||||
| Per Share |
$ | $ | $ | |||
| Total |
$ | $ | $ |
Delivery of the shares of Class A common stock will be made on or about , 2013.
Neither the Securities and Exchange Commission nor any state securities commission has approved or disapproved of these securities or determined if this prospectus is truthful or complete. Any representation to the contrary is a criminal offense.
Joint Book-Running Managers
| Credit Suisse | Citigroup |
BofA Merrill Lynch
Co-Manager
Raymond James
The date of this prospectus is , 2013
Table of Contents
You should rely only on the information contained in this prospectus. Neither we nor the underwriters have authorized anyone to provide you with information different from that contained in this prospectus. We do not, and the underwriters do not, take any responsibility for, and can provide no assurances as to, the reliability of any information that others provide to you. We are offering to sell, and seeking offers to buy, shares of Class A common stock only in jurisdictions where offers and sales are permitted. The information contained in this prospectus is accurate only as of the date of this prospectus, regardless of the time of delivery of this prospectus or of any sale of the Class A common stock.
Until , 2013, all dealers that buy, sell or trade our Class A common stock, whether or not participating in this offering, may be required to deliver a prospectus. This is in addition to the dealers’ obligation to deliver a prospectus when acting as underwriters and with respect to their unsold allotments or subscriptions.
In this prospectus, unless the context otherwise requires, “HII,” the “company,” “we,” “us” and “our” refer to (1) prior to the consummation of the reorganization described under “The Reorganization of Our Corporate Structure,” Health Plan Intermediaries, LLC, and (2) after giving pro forma effect to the reorganization described under “The Reorganization of Our Corporate Structure,” Health Insurance Innovations, Inc. and its consolidated subsidiaries, including Health Plan Intermediaries Holdings, LLC. References to Series B Membership Interests in this prospectus are to Health Plan Intermediaries Holdings, LLC Series B Membership Interests. The term “Predecessor” refers to our company prior to the acquisition described under “Management’s Discussion and Analysis of Financial Condition and Results of Operations—Basis of Presentation,” and the term “Successor” refers to our company following such acquisition. Unless otherwise indicated, all references to the nine months ended September 30, 2012 relate to the nine-month period ended September 30, 2012 of the Successor. All references to the nine months ended September 30, 2011 relate to the nine-month period ended September 30, 2011 of the Predecessor. All references to the year ended December 31, 2011 relate to the combined three-month period ended December 31, 2011 of the Successor and the nine-month period ended September 30, 2011 of the Predecessor. All references to the year ended December 31, 2010 relate to the 12-month period ended December 31, 2010 of the Predecessor. The presentation of combined Predecessor and Successor operating results (which is simply the arithmetic sum of the Predecessor and Successor amounts) is a Non-GAAP presentation, which is provided as a convenience solely for the purpose of facilitating comparisons of current results with combined results over the same period in the prior year.
Unless otherwise indicated, the financial information in the prospectus represents the historical financial information of Health Plan Intermediaries, LLC. The financial results of Health Plan Intermediaries Holdings, LLC and its consolidated subsidiaries will be consolidated in our financial statements after this offering.
i
Table of Contents
This summary highlights information contained elsewhere in this prospectus. This summary may not contain all of the information that you should consider before deciding to invest in our Class A common stock. You should read this entire prospectus carefully, including the “Risk Factors” section and the financial statements and the notes to those statements.
Health Insurance Innovations, Inc.
Overview
Our Company
We are a leading developer and administrator of affordable, web-based individual health insurance plans and ancillary products. Our highly scalable, proprietary, web-based technology platform allows for mass distribution of and online enrollment in our large and diverse portfolio of affordable health insurance offerings.
Our technology platform provides customers, who we refer to as members, immediate access to our products through our distribution partners anytime, anyplace. The health insurance products we develop are underwritten by insurance carrier companies, and we assume no underwriting, insurance or reimbursement risk. Members can price and tailor product selections to meet their needs, buy policies and print policy documents and identification cards in real-time. Our sales are executed online and offer instant electronic fulfillment. Our technology platform uses abbreviated online applications, some with health questionnaires, to provide an immediate accept or reject decision on applications for all products that we offer. Once an application is accepted, individuals can use our automated payment system to complete the enrollment process and obtain instant electronic access to their policy fulfillment documents, including the insurance policy, benefits schedule and identification cards. We receive credit card and Automated Clearing House (ACH) payments directly from members at the time of sale. Our technology platform provides significant operating leverage as we add members and reduces the costs associated with marketing, selling, underwriting and administering policies.
We are an industry leader in the sale of 12-month short-term medical, or STM, insurance plans, an alternative to traditional Individual Major Medical, or IMM, plans. STM plans generally offer qualifying individuals comparable benefits for fixed short-term durations of six or 12 months at approximately half the cost of IMM plans, which provide lifetime renewable coverage. While applications for IMM insurance may take up to 60 days to process, STM plans feature a streamlined underwriting process offering immediate coverage options. We also offer guaranteed-issue hospital indemnity plans for individuals under the age of 65, which pay fixed cash benefits for covered procedures and services, and a variety of ancillary products such as pharmacy benefit cards, dental plans, vision plans and cancer/critical illness plans that are frequently purchased as supplements to STM and hospital indemnity plans. We design and structure insurance products on behalf of insurance carrier companies, market them to individuals through our large network of distributors and manage member relations via our online member portal, which is available 24 hours a day, seven days a week. Our online enrollment process allows us to aggregate and analyze consumer data and purchasing habits to track market trends and drive product innovation. We have established relationships with several highly rated insurance carriers, including Starr Indemnity & Liability Company, Companion Life, United States Fire (a member of the Crum & Forster group), ING, Markel and CIGNA, among others. In addition, as of September 30, 2012, the large independent distribution network we access consists of 32 licensed agent call centers and 248 wholesalers, including Marsh, eHealthInsurance and MasterCard, among others, that work with over 7,300 licensed brokers. Our data-driven product design, technology platform and extensive distribution network have enabled us to grow our revenues from $11,790,000 in 2010 to $29,878,000 in 2011, and from $21,788,000 in the nine-month period ended September 30, 2011 to $30,102,000 in the nine-month period ended September 30, 2012.
1
Table of Contents
We focus on the large and under-penetrated segment of the U.S. population who are uninsured or underinsured, which includes individuals who are unable to afford traditional IMM premiums, individuals not covered by employer-sponsored insurance plans, such as those who are self-employed as well as small business owners and their employees, and underserved “gap populations” that require insurance due to changes caused by life events, such as new graduates, divorcees, early retirees, military discharges, the unemployed, part-time and seasonal employees and temporary workers. Our target market consists of approximately 64 million Americans, including approximately 50 million Americans who were uninsured in 2010, according to the U.S. Census Bureau, and approximately 14 million non-elderly Americans who purchased individual health insurance plans in 2010, according to a 2010 Kaiser Family Foundation survey. As of September 30, 2012, we had approximately 24,416 STM members. We expect the number of uninsured and underinsured to significantly increase due to the rising costs and burdensome underwriting requirements of traditional IMM plans and a decline in employer-sponsored health insurance programs.
As of September 30, 2012, we had 24,416 STM plans in force, compared with 16,838 on September 30, 2011, with an average monthly retention rate of 80% from September 30, 2011 to September 30, 2012. We earn our revenues from commissions and fees related to the sale of products to our members. Our ancillary products have created several additional revenue streams and resulted in a significant portion of our business being generated by monthly member renewals. For the nine months ended September 30, 2012, our premium equivalents, revenue and EBITDA were $54,549,000, $30,102,000 and $3,551,000, respectively, representing a 42.6%, 38.2% and 89.8% increase compared to premium equivalents, revenues and EBITDA of $38,257,000, $21,788,000 and $1,871,000, respectively, for the nine months ended September 30, 2011. See “Selected Historical Financial and Operational Data” for a discussion regarding the use of premium equivalents and EBITDA as financial measures and for reconciliations to the most directly comparable GAAP financial measures.
Health Insurance Industry and Market Opportunity
We believe ongoing changes in the health insurance industry will expand and reshape our target market. For example, the Patient Protection and Affordable Care Act, or PPACA, and the Health Care and Education Reconciliation Act of 2010, or HCERA, which we refer to, collectively, as Healthcare Reform, were signed into law on March 23, 2010. After facing a number of legal challenges, Healthcare Reform was upheld by the U.S. Supreme Court on June 28, 2012. Healthcare Reform includes a mandate requiring individuals to carry health insurance or face tax penalties; a mandate that certain employers with over 50 employees offer their employees group health insurance coverage or face tax penalties; prohibitions against insurance companies that offer traditional IMM insurance plans using pre-existing health conditions as a reason to deny an application for health insurance; and medical loss ratio, or MLR, requirements that require each health insurance carrier to spend a certain percentage of its IMM premium revenue on reimbursement for clinical services and activities that improve healthcare quality.
According to a 2011 McKinsey survey, the implementation of Healthcare Reform will likely increase the number of Americans in the individual health insurance market from 14 million to more than 100 million starting in 2014. We believe this increase will be primarily driven by two key factors: employers dropping group coverage and an additional 45 million uninsured Americans entering the individual insurance market. The McKinsey survey estimates that approximately 30% of employers would “definitely” or “probably” drop employer-sponsored insurance starting in 2014. The estimated penalty employers will face for not providing their employees coverage is $2,000 per employee for employers with over 50 employees (there is no penalty for employers with less than 50 employees), which is significantly less than the estimated price currently paid for employee coverage ($9,000 to $14,000 per employee). Assuming a 30% drop in employer-sponsored insurance, approximately 50 million Americans would join the individual health insurance market starting in 2014. In addition, because Americans will face penalties if they are uninsured, we expect that a large number of the
2
Table of Contents
current uninsured population of 50 million will enter the individual health insurance market. Accordingly, after 2014, we expect that the individual health insurance market will grow more than 600% to over 100 million policyholders, representing annual individual aggregate health insurance premiums in the United States of approximately $361 billion, compared with approximately $50 billion in 2010.
We believe certain dynamics in the health insurance industry present an opportunity to increase our market share in the individual health insurance market. For example, the minimum MLR thresholds require that IMM carriers use 80% of all premiums collected to pay claims. This has significantly reduced distributor commission rates on traditional IMM policies, forcing many distributors to abandon the traditional face-to-face IMM sales model. Starting in 2014, IMM carriers will also be subject to a pre-existing condition mandate, requiring them to accept all customers regardless of their pre-existing conditions. This “must-carry” pre-existing conditions requirement will further increase the costs of IMM coverage. Unlike traditional IMM plans, our STM products are exempt from the minimum MLR thresholds and “must-carry” pre-existing conditions requirements under Healthcare Reform, allowing us to offer attractive distributor commission rates while providing affordable products for individuals. In addition, Healthcare Reform also requires that states establish health insurance exchanges where uninsured individuals can select and purchase health insurance plans. We believe that these exchanges will further the transition from group-based insurance coverage to individual health insurance coverage, and that our STM products will be an attractive option in the non-subsidized exchange environment. Moreover, consumers are increasingly accessing the Internet to find affordable health insurance solutions. The current number of Internet users in the United States continues to grow and, according to a report published by Pew Research Center, represented 74% of the population in 2010. In addition, according to the same report, 33% of Internet users in 2010 looked online for information related to health insurance. This represents approximately 75 million Americans who used the Internet to access information related to health insurance in 2010.
We intend to aggressively pursue opportunities to help consumers identify our STM products as the right choice for healthcare coverage, and we believe our technology platform, product focus and industry expertise will allow us to gain an increasing share of this growing market.
Our Solutions
We believe that our products address a significant portion of the issues facing the healthcare system in the United States and improve access to coverage for certain underserved segments of the population.
| • | Lack of Access to Health Insurance. Due to the streamlined underwriting process for our STM plans, we are able to provide an instant decision regarding acceptance. Individuals applying for STM coverage only have to answer an abbreviated, online questionnaire regarding the status of their health to screen for risks that cannot be supported by the rate structure and design of the plan before a decision is generated. We also offer hospital indemnity plans under which members are paid fixed dollar amounts by procedure or service according to a defined schedule which includes doctor visits, lab tests, surgeries and hospitalizations. As these plans are not based on an individual’s health status, they guarantee issuance to individuals under the age of 65 and provide a viable coverage alternative for otherwise uninsurable individuals. |
| • | Growing Number of Uninsured and Underinsured Americans. We focus on the large and under-penetrated segment of the U.S. population that is uninsured or underinsured. According to the U.S. Census Bureau, 16% of Americans were uninsured in 2011, representing approximately 50 million individuals. In addition, the percentage of non-elderly Americans with employer-sponsored insurance decreased from 68% in 2000 to 59% in 2009, driving more Americans into the individual health insurance market. The number of uninsured and underinsured Americans continues to grow in part due to reductions in employer-provided health benefits. |
3
Table of Contents
| • | High Cost of Health Insurance. We offer affordable alternatives to IMM. According to the U.S. Census Bureau, approximately 34 million of the 50 million uninsured Americans in 2011 were members of families with annual incomes of less than $50,000. Based on these figures, we estimate that a sizable portion of the uninsured population chooses not to purchase insurance primarily due to its high cost. According to a 2010 Kaiser Family Foundation survey, traditional IMM premiums increased an average of approximately 20% over a12-month period, while the cost of our STM plans remained stable. In addition, as a result of Healthcare Reform, IMM premiums are expected to increase significantly in price as a result of guaranteed issue requirements for individuals with pre-existing health conditions. For individuals with pre-existing conditions, we currently offer guaranteed-issue hospital indemnity plans and, only where required by state mandate, STM plans. The implementation of Healthcare Reform will not expand our coverage of such individuals, allowing us to continue to offer attractive distributor commission rates while providing affordable products for members. |
Our Competitive Strengths
We have the following key competitive strengths that we believe collectively provide significant barriers to entry:
| • | Value Generated for All Key Constituents. By combining extensive management experience with our technology platform, we have developed a business model that we believe enables us to create a “win-win” proposition for our key constituents. |
| • | Our Carriers. We offer carriers access to a large member base, substantially all of which has no covered pre-existing conditions. Our technology platform connects our carriers directly to a large independent distribution network. Our platform also provides our carriers access to real-time sales and membership data. We use this information to assist our carriers in designing products that cater to their target populations. We currently utilize several carrier companies, including Starr Indemnity & Liability Company, Companion Life, United States Fire (a member of the Crum & Forster group), ING, Markel and CIGNA among others. Our management team has long-standing relationships with most of the major carrier companies we utilize and has not lost a carrier relationship in over 10 years. |
| • | Our Distributors. At a time when commission rates on many health insurance products, including traditional IMM plans, are declining, we provide our distributors with specialized, highly sought-after product offerings and a compensation structure characterized by attractive commission rates and advance payments. We believe our long-standing relationships with most of the major carriers we utilize, as well as our technology platform, which enables real-time underwriting decisions, immediate sales conversions and access to commission data and selling tools, drive demand for distributors to partner with us. We also offer a turnkey solution that allows us to design products that best meet our distributors’ needs. This solution enables us to assist our distributors in choosing between insurance carriers on a single website and allows them to create customized products for their customers by bundling our STM and hospital indemnity products with our various ancillary products into one package. As of September 30, 2012, we utilized a network of 32 licensed agent call centers and 248 wholesalers that work with over 7,300 licensed brokers nationally. |
| • | Our Members. We provide our members with easy access to health insurance coverage at an affordable price. For qualifying individuals, our STM plans offer benefits comparable to traditional IMM plans at approximately half the cost. For example, according to a 2010 Kaiser Family Foundation survey, the average cost for an IMM plan is $3,606 for an individual and $7,102 for a family. However, the average cost for one of our 12-month STM plans is $1,800 for an individual and $3,600 for a family. Our technology platform allows our members to compare and quote prices for a broad spectrum of STM and hospital indemnity products and, after they have made informed purchase decisions, to buy and print policies online. In addition to STM and hospital indemnity plans, we allow our members the |
4
Table of Contents
| opportunity to purchase high quality ancillary products with automatic, monthly renewals at rates that fit our members’ budgets, all at the click of a button. For example, in September 2012, in addition to the 5,489 STM plans that we sold, we successfully cross-sold 3,008 new ancillary products that month. |
| • | Proprietary, Web-Based Technology Platform. We believe our technology platform represents a distinct competitive advantage as it reduces the need for customer care agents and provides significant operating leverage as we add members and product offerings. Our primary technology platform is named A.R.I.E.S. (Automated Real-Time Integrated E System). We believe our business benefits from the increasing trend of Internet use by individuals to research and purchase health insurance. The Internet offers a means of providing individuals access to health insurance products 24 hours a day, seven days a week and, for the carriers and distributors, reduces the cost and time associated with marketing, selling, underwriting and administering these products. We believe our target market is increasingly researching and applying for health insurance products online and shifting away from more traditional buying patterns. We believe our technology platform positions us for strong continued growth due to the following factors: |
| • | Plan and Product Design. Our technology platform provides real-time data that enables us, our carriers and our distributors to receive immediate information on our members, and allows us to design products that meet the changing demands of the market. Our platform also allows individuals to supplement our STM and hospital indemnity offerings with ancillary products such as pharmacy benefit cards, dental plans, vision plans and cancer/critical illness plans and makes it possible for us to instantly offer these products, which can be bundled to fit member needs. |
| • | Sales. Our technology platform combined with our customer service model drives faster sale conversions. The entire underwriting procedure is processed through our technology platform, which uses abbreviated, online health questionnaires and provides an immediate accept or reject decision, allowing for instant electronic fulfillment. Individuals can obtain full access to our technology platform through our distribution partners and can price products, buy policies and print their policy documents and identification cards anytime, anyplace. Our call centers use our technology platform to, among other functions, perform online, real-time electronic quoting, to process electronic applications and to provide instant electronic approval and fulfillment, back-office administrative support and commission reporting. |
| • | Distribution. Our technology platform allows for low cost mass distribution of our products and provides significant operating leverage. Our automated payment system allows us to collect credit card and ACH payments electronically and directly from members and to disburse commission payments to our distributors in advance, weekly or monthly. In addition, the system provides distributors with direct access to commission statements, selling tools, reporting tools (for example, information as to cancelations, failed credit card and ACH payments and persistency, renewal and cross-sell rates) and custom links to support their business. |
| • | Compliance. In addition to our A.R.I.E.S. platform, we have obtained a license to use a technology platform called HiiVe, which we use to implement a highly automated compliance program that has enhanced quality while minimizing overhead and allowed us to offer higher commissions to our distributors. The compliance program enables us to record each enrollment phone call, retrieve archived calls within seconds and score calls based on script adherence. |
| • | Established Long-Standing Insurance Carrier Relationships. Our access to carriers is essential to our business. Our management team has developed close relationships with the senior management teams of many of our insurance carriers, some lasting over 15 years. Our management team has not lost a carrier relationship in over 10 years. We believe that the nature of our relationships with our insurance carriers, combined with our product knowledge and technology platform, allow us to provide value-added products to our members. |
5
Table of Contents
| • | Extensive Long-Term Relationships with Licensed Insurance Distributors. We believe our product expertise, our relationships with multiple insurance carriers, our focus on compliance and our technology platform make us a partner of choice for our distributors. We offer an appealing, incentive-based compensation structure that we believe drives demand for distributors to partner with us. We have extensive knowledge of the individual health insurance products that we design and administer, which allows us to assist our distribution partners in placing business. Our management team has built a broad distribution network and continuously adds new distributors. As of September 30, 2012, we utilized a network of 32 licensed agent call centers and 248 wholesalers that work with over 7,300 licensed brokers. Over the last 12 months, we added over 3,700 licensed brokers, 10 independent licensed broker call centers and 59 wholesalers to our national distributor network. |
| • | Seasoned Management Team. Our management team has substantial experience and long-standing relationships developed over an average of 25 years in the insurance industry. Our management team draws on its industry experience to identify opportunities to expand our business and collaborate with insurance carriers and distributors to help develop products and respond to market trends. In addition, the majority of our management team has worked together under the leadership of Michael W. Kosloske, our Chairman, President, and Chief Executive Officer, for more than a decade. |
Our Strategy
Our objective is to continue to expand our business and increase our presence in the affordable, web-based health insurance solutions market. Our principal strategies to meet this objective are:
| • | Expand and Enhance Distributor Relationships, Distribution Channels and Lead Generation Methods. We believe we will continue to attract new distributors as the insurance marketplace continues to evolve, and we intend to continue to identify large distributor and lead relationships through the following strategies: |
| • | Advance Commission Structure. We will continue to focus on attracting additional distributors through expansion of our advance commission structure. We believe distributors increasingly demand alternative methods to fund the large and growing costs of lead generation. We estimate that these costs usually range from $2 to $20 per lead and represent a significant startup cost for our distributors. We are in the process of growing our advance commission structure, whereby we pay distributors commissions on policies sold in advance of when they would ordinarily be due to the distributor. Commissions are advanced for up to six months and are made to distributors with an established track record of selling our products. In return, we reduce subsequent commission fees payable to the distributor by up to 2% of premiums for each month that we advance commissions. We believe this structure will assist our distributors in funding their lead generation costs and will provide us with a competitive advantage in attracting and retaining distributors and will increase sales. |
| • | Call Centers. We believe we can grow our distribution network organically by developing call center managers and incentivizing them via attractive commissions. As part of this strategy, we assist in enhancing the sales model of many of our current call centers in order to increase efficiencies and maximize returns, and we established our Insurance Academy in June 2012 to expand the number of call centers selling our products. We anticipate that our Insurance Academy operations will closely resemble a “franchise model,” in that we will provide the tools (sales scripts, key metrics, lead programs, compensation programs, technology systems, etc.) for building a profitable and successful call center that focuses on selling our products and leverages our technology. Our goal is to assist in the training of owners and managers, who in return agree to enter into long-term agreements with us, under which they are required to market our products. We anticipate establishing relationships with 10 to 20 new call centers per year through our Insurance Academy initiative. We believe that this will enhance our ability to convert leads from our current distribution channels into sales. |
6
Table of Contents
| • | Lead Generation and Innovative Distributor Relationships. We will continue to identify large and innovative distributor and lead relationships that we believe will increase revenue and diversify distribution. For example, in September 2012, we entered into an agreement whereby MasterCard, through its approved pre-paid card member networks, will assist us in targeting and acquiring new relationships or “leads” for marketing our products. Upon notification from MasterCard of a prospective lead, we will negotiate a separate referral fee arrangement with MasterCard at which point such prospective lead will be identified to us. We will then attempt to enter into an agreement with the prospective lead under which it will provide us with a list of its customers who hold MasterCard prepaid cards or it will directly market our products to those customers on our behalf. Our first agreement under this arrangement is with KEEPS America LLC, or KEEPS, for our prescription benefits cards. When sending their own pre-paid cards to customers, KEEPS includes our prescription benefits cards in the mailing. If the KEEPS customer uses our card, we pay KEEPS and MasterCard referral fees in connection with the distribution. To further expand our lead generation efforts, we will also continue to explore methods of screening member data for key demographic factors to identify populations for whom our products are well suited. |
| • | Increase Sales of Hospital Indemnity and Ancillary Products. We believe we have a significant opportunity to expand our market share in the hospital indemnity market. Our hospital indemnity plans in force have remained relatively stable with approximately 7,000 plans in force at December 31, 2010 and 5,841 plans in force at September 30, 2012. After the implementation of Healthcare Reform in 2014, we expect hospital indemnity plans to be increasingly used to supplement high deductible plans. In addition, our technology platform enables us to sell ancillary products that carry higher profit margins than our core STM products and that can be issued to a broader population than STM plans. Our members demand a wide range of ancillary products, including pharmacy benefit cards and dental, cancer and critical illness plans. Ancillary product policies in force grew from zero at December 31, 2010 to 23,040 at September 30, 2012. We believe we are well-positioned to take advantage of these additional opportunities at the time of sale. |
| • | Enhance Product and Name Recognition. We are focused on increasing our marketing efforts to consumers. We intend to aggressively pursue opportunities to help consumers identify our products as the right choice for health insurance coverage. We are pursuing multiple avenues to increase our name awareness among distributors, carriers and our target market, such as through our arrangement with MasterCard that introduces our products and name to MasterCard’s large pre-paid card member networks. |
| • | Develop and Establish New and Specialized Products to Meet Consumer Needs. We plan to continue to develop and add new products to our existing portfolio of offerings. By leveraging our technology platform member data, feedback gathered by customer service agents and distributors and expertise in plan design, we believe we are well-positioned to design and bundle products that meet customer needs and add a viable source of revenue for us, our distributors and our carriers. For example, in June 2012, we introduced our cancer plan. We sold 517 of these policies in the first month, and we are currently developing new products, including fully-insured prescription cards. |
Class A Common Stock and Class B Common Stock
After completion of this offering, our outstanding capital stock will consist of Class A common stock and Class B common stock. Investors in this offering will hold shares of Class A common stock. See “Description of Capital Stock.”
7
Table of Contents
Our History and the Reorganization of Our Corporate Structure
We began operations in 2008, and historically, our business was operated through Health Plan Intermediaries, LLC. On September 28, 2011, we entered into an agreement to purchase the units of Health Plan Intermediaries, LLC owned by Naylor Group Partners, LLC for $5,330,000 plus closing costs of $135,000 . Prior to the purchase, which we refer to as the Acquisition, Health Plan Intermediaries, LLC was 50% owned by Naylor Group Partners, LLC and 50% owned by our Chairman, President and Chief Executive Officer, Mr. Kosloske. Following the purchase, Mr. Kosloske became the sole member of Health Plan Intermediaries, LLC.
In anticipation of this offering, on November 7, 2012, Health Plan Intermediaries, LLC assigned the operating assets of our business through a series of transactions to Health Plan Intermediaries Holdings, LLC, and Health Plan Intermediaries Holdings, LLC assumed the operating liabilities of Health Plan Intermediaries, LLC.
Health Insurance Innovations, Inc. was incorporated in the State of Delaware on October 26, 2012 for the purpose of this offering and has engaged to date only in activities in contemplation of this offering. Upon completion of the offering, Health Insurance Innovations, Inc. will be a holding company the principal asset of which will be its interest in Health Plan Intermediaries Holdings, LLC. That interest will represent approximately 35% of the economic interests in Health Plan Intermediaries Holdings, LLC, assuming the underwriters do not exercise their over-allotment option. All of our business will be conducted through Health Plan Intermediaries Holdings, LLC, and the financial results of Health Plan Intermediaries Holdings, LLC and its consolidated subsidiaries will be consolidated in our financial statements. Health Insurance Innovations, Inc. will be the sole managing member of Health Plan Intermediaries Holdings, LLC and will therefore have 100% of the voting rights and control Health Plan Intermediaries Holdings, LLC, Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC (a subsidiary of Health Plan Intermediaries, LLC that was formed on October 31, 2012 in connection with this offering), entities beneficially owned by Mr. Kosloske, will collectively own all of the balance of the economic interests but will generally have no voting rights in Health Plan Intermediaries Holdings, LLC. See “The Reorganization of Our Corporate Structure—Amended and Restated Limited Liability Company Agreement of Health Plan Intermediaries Holdings, LLC—Voting and Economic Rights of Members.” As a holding company, our only source of cash flow from operations will be distributions from Health Plan Intermediaries Holdings, LLC. See “The Reorganization of Our Corporate Structure.” After completion of this offering, Health Insurance Innovations, Inc. will be a “controlled company” under the listing rules of the NASDAQ Global Market.
8
Table of Contents
The diagram below shows our organizational structure immediately after completion of this offering and the reorganization described under “The Reorganization of Our Corporate Structure.”
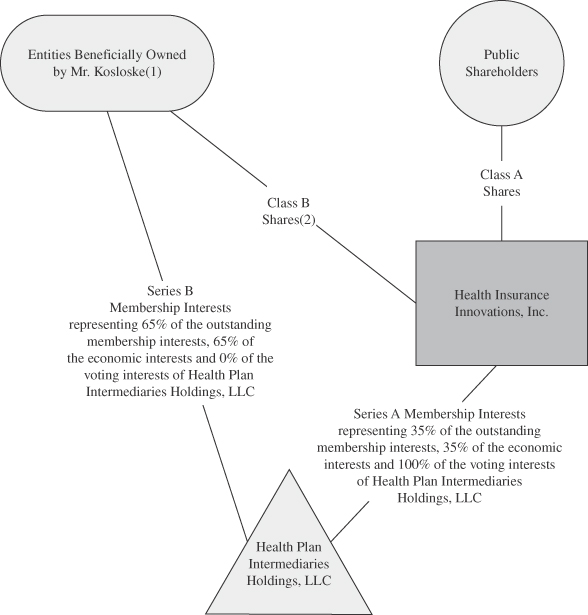
| (1) | The members of Health Plan Intermediaries Holdings, LLC, other than us, will include Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske. |
| (2) | Class B shares do not entitle their holders to any dividends paid by, or rights upon liquidation of, Health Insurance Innovations, Inc. Each share of our Class A common stock and our Class B common stock will entitle its holder to one vote. |
9
Table of Contents
Risk Factors
Before you invest in our stock, you should carefully consider all the information in this prospectus, including matters set forth under the heading “Risk Factors.” We believe the primary risks to our business are:
| • | the decrease in demand for our products; |
| • | the inability to retain our members; |
| • | loss of our relationships with insurance carriers, failure to maintain good relationships with insurance carriers, becoming dependent upon a limited number of insurance carriers or failure to develop new relationships with insurance carriers; |
| • | loss of our relationships with distributors, failure to maintain good relationships with distributors, becoming dependent upon a limited number of distributors or failure to develop new relationships with distributors; |
| • | the reduction of the commissions paid to us or changes in plan pricing practices in ways that reduce the commissions paid to us; |
| • | changes and developments in the health insurance system in the United States, particularly relating to the implementation of Healthcare Reform, that could harm our business; |
| • | the ability to maintain and enhance our name recognition ; and |
| • | our ability to build the necessary infrastructure and processes to maintain effective controls over financial reporting. |
Corporate Information
We lease our principal executive offices located at 15438 N. Florida Avenue, Suite 201, Tampa, Florida, 33613 and our telephone number is (877) 376-5831. We also maintain an Internet site at www.hiiquote.com. Our website and the information contained therein or connected thereto is not incorporated into this prospectus or the registration statement of which it forms a part.
10
Table of Contents
THE OFFERING
| Class A common stock offered |
4,666,667 shares |
| Class A common stock to be outstanding after this offering |
4,666,667 shares (or 13,333,334 shares if each outstanding Series B Membership Interest was exchanged for one share of Class A common stock, as described under “The Reorganization of Our Corporate Structure—Amended and Restated Limited Liability Company Agreement of Health Plan Intermediaries Holdings, LLC”). |
| Over-allotment option |
700,000 shares |
| Class B common stock to be outstanding after this offering |
8,666,667 shares. Following this offering, shares of our Class B common stock will be issued in connection with, and in equal proportion to, issuances of Series B Membership Interests of Health Plan Intermediaries Holdings, LLC. Each Series B Membership Interest of Health Plan Intermediaries Holdings, LLC, together with a share of our Class B common stock, will be exchangeable for one share of Class A common stock, as described under “The Reorganization of Our Corporate Structure—Amended and Restated Limited Liability Company Agreement of Health Plan Intermediaries Holdings, LLC.” |
| Voting rights |
Each share of our Class A common stock and Class B common stock will entitle its holder to one vote on all matters to be voted on by stockholders. Holders of Class A common stock and holders of Class B common stock will vote together as a single class on all matters presented to stockholders for their vote or approval, except as otherwise required by law. After completion of this offering, Mr. Kosloske will beneficially own none of our outstanding Class A common stock and 100% of the total number of shares of our outstanding Class B common stock, and will have effective control over the outcome of votes on all matters requiring approval by our stockholders. |
| Use of proceeds |
We estimate that the net proceeds to us from this offering will be approximately $63,100,000, or approximately $72,865,000 if the underwriters exercise their over-allotment option in full, assuming an initial public offering price of $15 per share (the midpoint of the range set forth on the cover page of this prospectus), after deducting estimated underwriting discounts and commissions and estimated offering expenses. Each $1 increase (decrease) in the public offering price per share would increase (decrease) our net proceeds, after deducting estimated underwriting discounts and commissions, by $326,667 (assuming no exercise of the underwriters’ over-allotment option). We intend to use a portion of the net proceeds of this offering to repay all of the outstanding debt under our term loan. |
11
Table of Contents
| We anticipate that we will use the remaining net proceeds of this offering to provide the funds necessary to expand our advance commission structure and for general corporate purposes, including potential acquisitions that are complementary to our business or that enable us to enter new markets or provide new products or services. If the underwriters exercise their over-allotment option, we intend to use the net proceeds from the sale of such shares to acquire Series B Membership Interests, together with an equal number of shares of our Class B common stock, from Health Plan Intermediaries, LLC, which is controlled by Mr. Kosloske (which Series B Membership Interests will immediately be recapitalized into Series A Membership Interests). See “Use of Proceeds.” |
| Dividend policy |
We do not anticipate paying dividends. “See Dividend Policy.” |
| Risk Factors |
For a discussion of certain factors you should consider before making an investment, see “Risk Factors.” |
| NASDAQ Global Market stock symbol |
HIIQ |
Unless the context requires otherwise, the number of shares to be outstanding after completion of this offering is based on 4,666,667 shares of Class A common stock and 8,666,667 shares of Class B common stock outstanding as of September 30, 2012 after giving pro forma effect to the reorganization transactions described under “The Reorganization of Our Corporate Structure” and the application of the net proceeds of this offering described under “Use of Proceeds,” but excludes:
| • | 8,666,667 shares of Class A common stock that are issuable upon exchanges of Series B Membership Interests (and an equal number of our Class B common shares) that will be outstanding immediately after the completion of this offering; |
| • | 400,000 unvested restricted stock awards to Michael D. Hershberger, our Chief Financial Officer, representing an amount equal to 3% of our enterprise value as determined immediately after the completion of this offering. See “Executive Compensation—Restricted Stock Agreements;” |
| • | the exercise by the underwriters of their over-allotment option to purchase 700,000 additional shares of our Class A common stock, which, if exercised, would decrease the number of Class B shares outstanding by an equal number. |
12
Table of Contents
SUMMARY FINANCIAL AND OPERATIONAL DATA
The following summary financial and operational data of Health Plan Intermediaries, LLC should be read in conjunction with, and are qualified by reference to, “Unaudited Pro Forma Financial Information,” “Selected Historical Financial and Operational Data,” “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and the financial statements and notes thereto included elsewhere in this prospectus. The statements of operations for the nine-month period ended September 30, 2012 (Successor), the three-month period ended December 31, 2011 (Successor), the nine-month period ended September 30, 2011 (Predecessor) and the year ended December 31, 2010 (Predecessor) and the balance sheet data as of September 30, 2012 (Successor) and December 31, 2011 (Successor) are derived from, and qualified by reference to, the audited consolidated financial statements of Health Plan Intermediaries, LLC included elsewhere in this prospectus and should be read in conjunction with those financial statements and notes thereto. Results for the nine-month period ended September 30, 2012 are not necessarily indicative of results that may be expected for the entire year.
The summary unaudited pro forma financial data for the year ended December 31, 2011 and for the nine months ended September 30, 2012 have been prepared to give pro forma effect to all of the reorganization transactions described under “The Reorganization of Our Corporate Structure” and this offering and the application of the net proceeds from this offering as if they had been completed as of January 1, 2011 with respect to the unaudited pro forma statements of operations and as of September 30, 2012 with respect to the unaudited pro forma balance sheet data . These data are subject and give effect to the assumptions and adjustments described in the notes accompanying the unaudited pro forma financial statements included elsewhere in this prospectus. The summary unaudited pro forma financial data are presented for informational purposes only and should not be considered indicative of actual results of operations that would have been achieved had the reorganization transactions and this offering been consummated on the dates indicated, and do not purport to be indicative of statements of financial condition data or results of operations as of any future date or for any future period.
| Pro Forma As Adjusted | Historical | |||||||||||||||||||||||||||||
| Nine Months Ended September 30, 2012 |
Year Ended December 31, 2011 |
Nine Months Ended September 30, 2012 |
Three Months Ended December 31, 2011 |
Nine Months Ended September 30, 2011 |
Year Ended December 31, 2011 |
Year Ended December 31, 2010 |
||||||||||||||||||||||||
| (Combined) (Non- GAAP) |
(Successor) | (Successor) | (Predecessor) | (Combined) (Non-GAAP) |
(Predecessor) | |||||||||||||||||||||||||
| Statements of Operations: |
||||||||||||||||||||||||||||||
| (in thousands, except plans in force) | ||||||||||||||||||||||||||||||
| Revenues |
$ | 30,102 | $ | 29,878 | $ | 30,102 | $ | 8,090 | $ | 21,788 | $ | 29,878 | $ | 11,790 | ||||||||||||||||
| Third-party commissions |
20,093 | 21,704 | 20,093 | 5,601 | 16,103 | 21,704 | 9,010 | |||||||||||||||||||||||
| Credit cards and ACH fees |
693 | 670 | 693 | 197 | 473 | 670 | 275 | |||||||||||||||||||||||
| General and administrative expenses |
6,793 | 8,498 | 5,786 | 1,421 | 3,341 | 4,762 | 2,514 | |||||||||||||||||||||||
| Depreciation and amortization |
771 | 289 | 771 | 269 | 29 | 298 | 7 | |||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Total operating costs and expenses |
28,350 | 31,170 | 27,343 | 7,488 | 19,946 | 27,434 | 11,806 | |||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Income (loss) from operations |
1,752 | (1,292 | ) | 2,759 | 602 | 1,842 | 2,444 | (16 | ) | |||||||||||||||||||||
| Other expenses (income): |
||||||||||||||||||||||||||||||
| Interest expense |
— | — | 194 | 71 | — | 71 | — | |||||||||||||||||||||||
| Interest income |
— | — | — | — | — | — | (3 | ) | ||||||||||||||||||||||
| Other income |
(21 | ) | — | (21 | ) | — | — | — | — | |||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| Pre tax net income (loss) |
$ | 1,773 | $ | (1,292 | ) | $ | 2,586 | $ | 531 | $ | 1,842 | $ | 2,373 | $ | (13 | ) | ||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
| Income Tax |
$ | 673 | (434 | ) | ||||||||||||||||||||||||||
|
|
|
|
|
|||||||||||||||||||||||||||
| Net Income |
$ | 1,100 | (858 | ) | ||||||||||||||||||||||||||
|
|
|
|
|
|||||||||||||||||||||||||||
| Net loss attributable to noncontrolling interest in subsidiary |
$ | 756 | $ | (558 | ) | $ | (63 | ) | $ | — | $ | — | $ | — | $ | — | ||||||||||||||
| Net income (loss) attributable to Health Plan Intermediaries, LLC |
$ | 344 | $ | (300 | ) | $ | 2,649 | $ | 531 | $ | 1,842 | $ | 2,373 | $ | (13 | ) | ||||||||||||||
| Other Financial and Operational Data: |
||||||||||||||||||||||||||||||
| Premium equivalents(1) |
$ | 54,549 | $ | 53,206 | $ | 54,549 | $ | 14,949 | $ | 38,257 | $ | 53,206 | $ | 20,024 | ||||||||||||||||
| Plans in force (end of period)(2) |
53,297 | 29,951 | 53,297 | 29,951 | 22,847 | 29,951 | 13,121 | |||||||||||||||||||||||
| EBITDA(3) |
$ | 2,544 | $ | (994 | ) | $ | 3,551 | $ | 871 | $ | 1,871 | $ | 2,742 | $ | (9 | ) | ||||||||||||||
13
Table of Contents
| (1) | “Premium equivalents” is defined as the combination of premiums, fees for discount benefit plans, fees for distributors and our enrollment fees. Premium equivalents does not represent, and should not be considered as, an alternative to revenues, as determined in accordance with U.S. generally accepted accounting principles, or U.S. GAAP. We have included premium equivalents in this prospectus because it is a key measure used by our management to understand and evaluate our core operating performance and trends, to prepare and approve our annual budget and to develop short- and long-term operational plans. In particular, the inclusion of premium equivalents can provide a useful measure for period-to-period comparisons of our business. Premium equivalents has limitations as an analytical tool, and you should not consider it in isolation or as a substitute for analysis of our results as reported under U.S. GAAP. See “Management Discussion and Analysis of Financial Condition and Results of Operations—Key Business Metrics.” |
The following is a reconciliation of premium equivalents to revenues:
| Nine
Months Ended September 30, 2012 |
Three
Months Ended December 31, 2011 |
Nine
Months Ended September 30, 2011 |
Year
Ended December 31, 2011 |
Year
Ended December 31, 2010 |
||||||||||||||||||
| (Successor) | (Successor) | (Predecessor) | (Combined) (Non-GAAP) |
(Predecessor) | ||||||||||||||||||
| (in thousands) | ||||||||||||||||||||||
| Premium equivalents |
$ | 54,549 | $ | 14,949 | $ | 38,257 | $ | 53,206 | $ | 20,024 | ||||||||||||
| Less risk premium |
(23,296 | ) | (6,380 | ) | (15,180 | ) | (21,560 | ) | (7,616 | ) | ||||||||||||
| Less amounts earned by third-party obligors |
(1,151 | ) | (479 | ) | (1,289 | ) | (1,768 | ) | (618 | ) | ||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Revenues |
$ | 30,102 | $ | 8,090 | $ | 21,788 | $ | 29,878 | $ | 11,790 | ||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| (2) | “Plans in force” is defined as policies or discount benefit plans issued to a member for which we have collected the applicable premium payments and/or discount benefit fees. A member may be enrolled in more than one policy or discount benefit plan simultaneously. See “Management Discussion and Analysis of Financial Condition and Results of Operations—Key Business Metrics.” |
| (3) | “EBITDA” is defined as net income before interest expense, interest income and depreciation and amortization. EBITDA does not represent, and should not be considered as, an alternative to net income or cash flows from operations, each as determined in accordance with U.S. GAAP. We have presented EBITDA because we consider it an important supplemental measure of our performance and believe that it is frequently used by analysts, investors and other interested parties in the evaluation of companies. Other companies may calculate EBITDA differently than we do. EBITDA has limitations as an analytical tool, and you should not consider it in isolation or as a substitute for analysis of our results as reported under U.S. GAAP. See “Management Discussion and Analysis of Financial Condition and Results of Operations—Key Business Metrics.” |
14
Table of Contents
The following is a reconciliation of net income (loss) to EBITDA:
| Pro Forma As Adjusted | Historical | |||||||||||||||||||||||||||||
| Year Ended December 31, 2011 |
Nine Months Ended September 30, 2012 |
Three Months Ended December 31, 2011 |
Nine Months Ended September 30, 2011 |
Year Ended December 31, 2011 |
Year Ended December 31, 2010 |
|||||||||||||||||||||||||
| Nine Months Ended September 30, 2012 |
(Combined) (Non-GAAP) |
(Successor) | (Successor) | (Predecessor) | (Combined) (Non-GAAP) |
(Predecessor) | ||||||||||||||||||||||||
| (in thousands) | ||||||||||||||||||||||||||||||
| Net Income (loss) |
$ | 1,100 | $ | (858 | ) | $ | 2,586 | $ | 531 | $ | 1,842 | $ | 2,373 | $ | (13 | ) | ||||||||||||||
| Income tax |
673 | (434 | ) | — | — | — | — | — | ||||||||||||||||||||||
| Interest expense |
— | — | 194 | 71 | — | 71 | — | |||||||||||||||||||||||
| Interest income |
— | — | — | — | — | — | (3 | ) | ||||||||||||||||||||||
| Depreciation and amortization |
771 | 298 | 771 | 269 | 29 | 298 | 7 | |||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
| EBITDA |
$ | 2,544 | $ | (994 | ) | $ | 3,551 | $ | 871 | $ | 1,871 | $ | 2,742 | $ | (9 | ) | ||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
| As of September 30, |
||||||||||||
| 2012 Pro Forma |
2012 | As
of December 31, 2011 |
||||||||||
| (in thousands) | ||||||||||||
| Balance Sheet Data: |
||||||||||||
| Cash |
$ | 61,455 | $ | 982 | $ | 618 | ||||||
| Total assets |
77,065 | 17,542 | 15,068 | |||||||||
| Debt, noncompete obligation and capital leases |
849 | 4,340 | 4,078 | |||||||||
| Total member’s stockholders’ equity |
69,882 | 6,869 | 6,996 | |||||||||
15
Table of Contents
Investing in our Class A common stock involves a high degree of risk. You should carefully consider the following risks and all of the other information set forth in this prospectus before deciding to invest in shares of our Class A common stock. If any of the following risks actually occur, our business, financial condition or results of operations would likely suffer. In such case, the trading price of our Class A common stock could decline due to any of these risks, and you may lose all or part of your investment.
Risks Relating to Our Business and Industry
The market for health insurance in the United States is rapidly evolving, which makes it difficult to forecast demand for our products.
The market for health insurance in the United States is rapidly evolving. Accordingly, our future financial performance will depend in part on growth in this market and on our ability to adapt to emerging demands in this market. We believe demand for our products has been driven in large part by recent regulatory changes, broader use of the Internet and advances in technology. It is difficult to predict with any precision the future growth rate and size of our target market. The rapidly evolving nature of the market in which we operate, as well as other factors that are beyond our control, reduce our ability to evaluate accurately our long-term outlook and forecast annual performance. A reduction in demand for our products caused by lack of acceptance, technological challenges, competing offerings or other factors would result in a lower revenue growth rate or decreased revenue, either of which could negatively impact our business and results of operations. In addition, our business, financial condition and results of operations may be adversely affected if Healthcare Reform is not implemented in accordance with our expectations and we cannot successfully execute our growth strategies. For example, our STM plans are currently classified as “short-term limited duration” plans under Healthcare Reform. Accordingly, “short-term limited duration” plans are exempt under Healthcare Reform from the minimum MLR thresholds and “must-carry” pre-existing conditions requirements, the requirements for the extension of dependent coverage, certain documentation, reporting and appeals process requirements and the prohibitions against excessive waiting periods, lifetime or annual limits, rescissions and more generally, discrimination against individuals and discrimination on the provision of health care. If our STM plans were no longer classified as short-term limited duration plans, or we were not able to take advantage of certain current exemptions for any other reason, our business could be negatively affected.
If we are unable to retain our members, our business and results of operations would be harmed.
Our revenue is primarily derived from commissions that insurance carriers pay to us for the health insurance plans and products that we market and that remain in effect. When one of these plans or products is cancelled, or if we otherwise do not remain the administrator of record on the policy, we no longer receive the related commission revenue. Members may choose to discontinue their insurance policies for a number of reasons. For example, members may determine that they cannot afford our products or may decide not to renew their policies due to future increases in premiums. In addition, our members may choose to purchase new plans or products using a different administrator if, for example, they are not satisfied with our customer service or the plans or products that we offer. Further, members may discontinue their policies because they no longer need STM insurance because, for example, they have received coverage through an employer or spouse. Insurance carriers may also terminate health insurance plans or products purchased by our members for a variety of reasons. Our cost in acquiring a new member is substantially greater than the cost involved in maintaining our relationship with an existing member. If we are not able to successfully retain existing members and limit member turnover, our revenue and operating margins could be adversely affected.
16
Table of Contents
Our business would be harmed if we lose our relationships with insurance carriers, fail to maintain good relationships with insurance carriers, become dependent upon a limited number of insurance carriers or fail to develop new relationships with insurance carriers.
We typically enter into contractual agency relationships with insurance carriers that are non-exclusive and terminable on short notice by either party for any reason. In many cases, insurance carriers also have the ability to amend the terms of our agreements unilaterally on short notice. Insurance carriers may be unwilling to underwrite our health insurance plans or products or may amend our agreements with them for a variety of reasons, including for competitive or regulatory reasons. Insurance carriers may decide to rely on their own internal distribution channels, including traditional in-house agents, carrier websites or other sales channels, or to market their own plans or products, and, in turn, could limit or prohibit us from marketing their plans or products. Insurance carriers may decide not to underwrite insurance plans or products in the individual health insurance market in certain geographies or altogether. The termination or amendment of our relationship with an insurance carrier could reduce the variety of health insurance plans or products we offer. We also could lose a source of, or be paid reduced commissions for, future sales and could lose renewal commissions for past sales. Our business could also be harmed if we fail to develop new carrier relationships or are unable to offer members a wide variety of health insurance plans and products.
The private health insurance industry in the United States has experienced substantial consolidation over the past several years, resulting in a decrease in the number of insurance carriers. For example, for the nine months ended September 30, 2012, Starr Indemnity & Liability Company accounted for 50% of our premium equivalents and United States Fire (a member of the Crum & Forster group) accounted for 25% of our premium equivalents. In the future, it may become necessary for us to offer insurance plans and products from a reduced number of insurance carriers or to derive a greater portion of our revenue from a more concentrated number of carriers as our business and the health insurance industry evolve. Each of these insurance carriers may terminate our agreements with them, and, in some cases, as a result of the termination we may lose our right to receive future commissions for policies we have sold. In addition, one or more of our carrier companies could experience a failure of its business due to a decline in sales volumes, unavailability of reinsurance, failure of business strategy or otherwise. Should our dependence on a smaller number of insurance carriers increase, whether as a result of the termination of carrier relationships, further insurance carrier consolidation, business failure, bankruptcy or any other reason, we may become more vulnerable to adverse changes in our relationships with our carriers, particularly in states where we offer health insurance plans and products from a relatively small number of carriers or where a small number of insurance carriers dominate the market. The termination, amendment or consolidation of our relationships with our insurance carriers could harm our business, results of operations and financial condition.
Our business would be harmed if we lose our relationships with distributors, fail to maintain good relationships with distributors, become dependent upon a limited number of distributors or fail to develop new relationships with distributors.
We depend on distributors to sell our products. We typically enter into contractual agency relationships with distributors that are non-exclusive and terminable on short notice by either party for any reason. In many cases, distributors also have the ability to amend the terms of our agreements unilaterally on short notice. Distributors may be unwilling to sell our health insurance plans or products or may amend our agreements with them for a variety of reasons, including for competitive or regulatory reasons. For example, distributors may decide to sell plans and products that bring them a higher commission than our plans and products or may decide not to sell STM plans at all. Because we rely on a diverse distributor network to sell our products, any loss of relationships with distributors or failure to maintain good relationships with distributors could harm our business, results of operations and financial condition. Further, we believe that we must grow our distributor network in order to achieve our growth plans. If we are unable to grow our distributor network and develop new relationships with distributors, our revenue could be adversely impacted.
17
Table of Contents
We depend on relationships with third-parties for certain services that are important to our business. An interruption or cessation of such services by any third party could have a material adverse effect on our business.
We depend on a number of third-party relationships to enhance our business. For instance, state regulations may require that individuals enroll in group programs or associations in order to access certain insurance products, benefits and services. We have entered into relationships with such associations in order to provide individuals access to our products. For example, we have an agreement with Med-Sense Guaranteed Association, or Med-Sense, a non-profit association that provides membership benefits to individuals and gives members access to certain of our products. Under the agreement, we primarily market membership in the association and collect certain fees and dues on its behalf. In return, we have sole access to its membership list, and Med-Sense exclusively endorses the insurance products that we offer. Members of the association are given access to a wide variety of our products that are otherwise unavailable to non-members. For the month of September 2012, approximately 81.7% of our business was derived from individuals who became members of Med-Sense. We intend to establish an affiliation with Savers Choice of America, an association offering similar benefits, as an alternative to Med-Sense. We intend to have several of our carriers issue policies to Savers Choice of America members beginning in January 2013. While we believe we could replace Med-Sense with other group programs or associations, there can be no assurance we could find such a replacement on a timely basis or at all. If we were to lose our relationship with Med-Sense and were unable to find another group program or association on a timely basis or at all, this would have a material adverse effect on our business.
In addition, we develop and maintain strategic relationships with our partners in order for them to market our products to their end users. While we have entered into agreements with certain partners pursuant to which our products may be made available to their end-users, such agreements are not exclusive and generally do not obligate the partner to market or distribute our service. For example, we have entered into an agreement with MasterCard whereby MasterCard, through its approved pre-paid card member networks, will assist us in targeting and acquiring new leads for marketing our products. Under such agreement, MasterCard will use good-faith efforts to identify prospective leads.
Our ability to offer our services and operate our business is therefore dependent on maintaining our relationships with third-party partners, particularly Med-Sense, and entering into new relationships to meet the changing needs of our business. Any deterioration in our relationships with such partners, or our failure to enter into agreements with partners in the future would harm our business, results of operations and financial condition. If our partners are unable or unwilling to provide the services necessary to support our business, or if our agreements with such partners are terminated, our operations could be significantly disrupted. We may also incur substantial costs, delays and disruptions to our business in transitioning such services to ourselves or other third-party partners. In addition, third-party partners may not be able to provide the services required in order to meet the changing needs of our business.
Insurance carriers could reduce the commissions paid to us or change their plan pricing practices in ways that reduce the commissions paid to us, which could harm our revenue and results of operations.
Our commission rates are negotiated between us and each carrier. Insurance carriers have altered, and may in the future alter, the contractual relationships we have with them, either by renegotiation or unilateral action. Also, insurance carriers may adjust their commission rates to comply with regulatory guidelines. If these contractual changes result in reduced commissions, our revenue may decline. For example, on June 1, 2011, we entered into a new contract with Starr Indemnity & Liability Company which replaced a previous contract with Starr Global Accident and Health Insurance Agency, LLC to provide similar services for slightly lower commission rates. The reduced commissions had no material impact on our revenue or results of operations, however, as the contract also provided for additional administrative fees paid to us to offset the lower commission rates.
18
Table of Contents
In addition, insurance carriers periodically adjust the premiums they charge to individuals for their insurance policies. These premium changes may cause members to cancel their existing policies and purchase a replacement policy from a different insurance carrier, either through our platform or through another administrator. We may receive a reduced commission or no commission at all when a member purchases a replacement policy. Also, because insurance rates may vary between insurance carriers, plans and enrollment dates, changes in our enrollment mix may impact our commission revenue. Future changes in carrier pricing practices could harm our business, results of operations and financial condition.
We face intense competition and compete with a broad range of market participants within the health insurance industry. If competition increases, our growth and profits may decline.
The market for selling individual health insurance and ancillary products is highly competitive and, except for regulatory considerations, there are limited barriers to entry. Currently, we believe the cost-effective, high-quality STM solutions that we distribute to the individual health insurance market are somewhat rare among our competitors. However, if we achieve our goal of becoming a leader in the distribution of individual health insurance products, we believe that competition for our business model will substantially increase. Because the barriers to entry in our markets are not substantial and members have the flexibility to select new health insurance providers, we believe that the addition of new competitors, or the adoption of our business model by existing competitors, may occur relatively quickly.
We compete with entities and individuals that offer and sell products similar to ours utilizing traditional distribution channels, including insurance agents and brokers across the United States who sell health insurance products in their communities. Some local agents use “lead aggregator” services that use the Internet to find individuals interested in purchasing health insurance and are compensated for referring those individuals to a traditional insurance agent. In addition to health insurance brokers and agents, many insurance carriers directly market and sell their plans and products to individuals through call centers and their own websites. Although we offer health insurance plans and products for many of these insurance carriers, they also compete with us by offering their plans and products directly to individuals or may elect to compete with us by offering their plans and products directly to individuals in the future. We may not be able to compete successfully against our current or future competitors. Some of our current and potential competitors have longer operating histories in the health insurance industry, access to larger customer bases, greater name recognition and significantly greater financial, technical, marketing and other resources than we do. As compared to us, our current and future competitors may be able to:
| • | undertake more extensive marketing campaigns for their brands and services; |
| • | devote more resources to website and systems development; |
| • | negotiate more favorable commission rates; and |
| • | attract potential employees, marketing partners and third-party service providers. |
Further, there are many alternatives to the individual health insurance products that we currently provide. We can make no assurances that we will be able to compete effectively with the various individual health insurance products that are currently available or may become available in the future. Competitive pressures may result in our experiencing increased marketing costs and loss of market share, or may otherwise harm our business, results of operations and financial condition.
Changes and developments in the health insurance system in the United States, in particular the implementation of Healthcare Reform, could harm our business.
Our business depends upon the private sector of the U.S. insurance system, its role in financing healthcare delivery, and insurance carriers’ use of, and payment of commissions to, agents, brokers and other organizations to market and sell health insurance plans and products.
19
Table of Contents
Healthcare Reform contains provisions that have changed and will continue to change the industry in which we operate in substantial ways. Many aspects of Healthcare Reform do not take effect until 2014, although certain provisions currently are effective, such as medical loss ratio requirements for individual, family and small business health insurance and a prohibition against using pre-existing health conditions as a reason to deny health coverage for children. In addition, state governments have adopted, and will continue to adopt, changes to their existing laws and regulations in light of Healthcare Reform and related regulations. Future changes may not be beneficial to us.
Notwithstanding the recent U.S. Supreme Court decision largely upholding the constitutionality of Healthcare Reform, certain key members of Congress have expressed a desire to withhold the funding necessary to implement Healthcare Reform as well as the desire to repeal or amend all or a portion of Healthcare Reform. Any partial or complete repeal or amendment or implementation difficulties, or uncertainty regarding such events, could increase our costs of compliance and adversely affect our results of operations and financial condition. The implementation of Healthcare Reform could have negative effects on us, including:
| • | increasing our competition; |
| • | reducing or eliminating the need for health insurance agents and brokers and/or demand for the health insurance that we sell through the manner in which the federal government and the states implement health insurance exchanges and the process for receiving subsidies and cost-sharing credits; |
| • | decreasing the number of types of health insurance plans and products that we sell, as well as the number of insurance carriers offering such plans and products; |
| • | causing insurance carriers to change the benefits and/or premiums for the plans and products they sell; |
| • | causing insurance carriers to reduce the amount they pay for our services or change their relationships with us in other ways; |
| • | causing STM to not qualify as adequate healthcare coverage, resulting in STM policyholders having to pay the government a penalty or tax; |
| • | causing STM policies to be subject to MLR threshold requirements; or |
| • | causing STM policies to be subject to “must carry” pre-existing condition requirements. |
Any of these effects could materially harm our business, results of operations and financial condition. For example, the manner in which the federal government and the states implement Healthcare Reform could substantially increase our competition and member turnover and substantially reduce the number of individuals who purchase insurance through us. Various aspects of Healthcare Reform could cause insurance carriers to limit the type of health insurance plans and products we are able to sell and the geographies in which we are able to sell them. Changes in the law could also cause insurance carriers to exit the business of selling insurance plans and products in a particular jurisdiction, to eliminate certain categories of products or to attempt to move members into new plans and products for which we receive lower commissions. If insurance carriers decide to limit our ability to sell their plans and products or determine not to sell individual health insurance plans and products altogether, our business, results of operations and financial condition would be materially harmed.
Compliance with the strict regulatory environment applicable to the health insurance industry and the specific products we sell is difficult and costly. If we fail to comply with the numerous laws and regulations that are applicable to our business, our business and results of operations would be harmed.
The health insurance industry is heavily regulated by each state in the United States. For instance, state regulators require us to maintain a valid license in each state in which we transact health insurance business and further require that we adhere to sales, documentation and administration practices specific to each state. In addition, each distributor who transacts health insurance business on our behalf must maintain a valid license in one or more states. Because we do business in the majority of states and the District of Columbia, compliance
20
Table of Contents
with health insurance-related laws, rules and regulations is difficult and imposes significant costs on our business. Each jurisdiction’s insurance department typically has the power, among other things, to:
| • | grant and revoke licenses to transact insurance business; |
| • | conduct inquiries into the insurance-related activities and conduct of agents and agencies; |
| • | require and regulate disclosure in connection with the sale and solicitation of health insurance; |
| • | authorize how, by which personnel and under what circumstances insurance premiums can be quoted and published and an insurance policy sold; |
| • | determine which entities can be paid commissions from carriers; |
| • | regulate the content of insurance-related advertisements, including web pages; |
| • | approve policy forms, require specific benefits and benefit levels and regulate premium rates; |
| • | impose fines and other penalties; and |
| • | impose continuing education requirements on agents and employees. |
Although we believe we are currently in compliance with applicable insurance laws and regulations, due to the complexity, periodic modification and differing interpretations of insurance laws and regulations, we may not have always been, and we may not always be, in compliance with such laws and regulations. Failure to comply could result in significant liability, additional department of insurance licensing requirements or the revocation of licenses in a particular jurisdiction, which could significantly reduce our revenue, increase our operating expenses, prevent us from transacting health insurance business in a particular jurisdiction and otherwise harm our business, results of operations and financial condition. Moreover, an adverse regulatory action in one jurisdiction could result in penalties and adversely affect our license status or reputation in other jurisdictions due to the requirement that adverse regulatory actions in one jurisdiction be reported to other jurisdictions. Even if the allegations in any regulatory or other action against us are proven false, any surrounding negative publicity could harm member, distributor or health insurance carrier confidence in us, which could significantly damage our reputation . Because some members, distributors and health insurance carriers may not be comfortable with the concept of purchasing health insurance using the Internet, any negative publicity may affect us more than it would others in the health insurance industry and would harm our business, results of operations and financial condition.
In addition, we may in the future receive inquiries from state insurance regulators regarding our marketing and business practices. We may modify our practices in connection with any such inquiry. Any modification of our marketing or business practices in response to future regulatory inquiries could harm our business, results of operations or financial condition.
Regulation of the sale of health insurance is subject to change, and future regulations could harm our business and results of operations.
The laws and regulations governing the offer, sale and purchase of health insurance are subject to change, and future changes may be adverse to our business. For example, once health insurance pricing is set by the carrier and approved by state regulators, it is fixed and not generally subject to negotiation or discounting by insurance companies or agents. Additionally, state regulations generally prohibit carriers, agents and brokers from providing financial incentives, such as rebates, to their members in connection with the sale of health insurance. As a result, we do not currently compete with carriers or other agents and brokers on the price of the health insurance products offered on our website. We are also currently allowed to base our revenue structure on various commissions and fees, including commissions from insurance premiums and enrollment, monthly administrative fees and discount benefit fees. However, future laws and regulations could negatively adjust the commissions and fees we receive. If current laws or regulations change, we could be forced to reduce prices, commissions and fees or provide rebates or other incentives for the health insurance products sold through our online platform, which would harm our business, results of operations and financial condition.
21
Table of Contents
Because we use the Internet as our distribution platform, we are subject to additional insurance regulatory risks. In many cases, it is not clear how existing insurance laws and regulations apply to Internet-related health insurance advertisements and transactions. To the extent that new laws or regulations are adopted that conflict with the way we conduct our business, or to the extent that existing laws and regulations are interpreted adversely to us, our business, results of operations and financial condition would be harmed.
Our business may not grow if individuals are not informed about the availability and accessibility of affordable health insurance.
Numerous health insurance plans and products are available to individuals in any given market. Most of these plans and products vary by price, benefits and other policy features. Health insurance terminology and provisions are often confusing and difficult to understand. As a result, researching, selecting and purchasing health insurance can be a complex process. We believe that this complexity has contributed to a perception held by many individuals that individual health insurance is prohibitively expensive and difficult to obtain. If individuals are not informed about the availability and accessibility of affordable health insurance, our business may not grow and our results of operations and financial condition would be harmed.
Changes in the quality and affordability of the health insurance plans and products that carriers offer to us for sale through our technology platform could harm our business and results of operations.
The demand for health insurance marketed through our technology platform is affected by, among other things, the variety, quality and price of the health insurance plans and products we offer. If health insurance carriers do not continue to allow us to sell a variety of high-quality, affordable health insurance plans and products in our markets, or if their offerings are limited or terminated as a result of consolidation in the health insurance industry, the implementation of Healthcare Reform or otherwise, our sales may decrease and our business, results of operations and financial condition would be harmed.
If we are not able to maintain and enhance our name recognition, our business and results of operations will be harmed.
We believe that maintaining and enhancing our name recognition is critical to our relationships with existing members, distributors and carriers and to our ability to attract new members, distributors and carriers. The promotion of our name may require us to make substantial investments and we anticipate that, as our market becomes increasingly competitive, these marketing initiatives may become increasingly difficult and expensive. Our marketing activities may not be successful or yield increased revenue, and to the extent that these activities yield increased revenue, the increased revenue may not offset the expenses we incur and our results of operations could be harmed. If we do not successfully maintain and enhance our name recognition, our business may not grow and we could lose our relationships with carriers, distributors and/or members, which would harm our business, results of operations and financial condition.
In addition, we cannot be certain of the impact of media coverage on our business. If it were to be reduced, the number of distributors selling our products could decrease, and our cost of acquiring members could increase, both of which could harm our business, results of operations and financial condition.
If individuals or carriers opt for more traditional or alternative channels for the purchase and sale of health insurance, our business will be harmed.
Our success depends in part upon widespread individual and carrier acceptance of the Internet as a marketplace for the purchase and sale of health insurance. Individuals and carriers may choose to depend more on traditional sources, such as individual agents, or alternative sources may develop, including as a result of Healthcare Reform. Our future growth, if any, will depend in part upon:
| • | the growth of the Internet as a commerce medium generally, and as a market for individual health insurance plans and services specifically; |
22
Table of Contents
| • | individuals’ willingness to conduct their own health insurance research; |
| • | our ability to make the process of purchasing health insurance online an attractive alternative to traditional and new means of purchasing health insurance; |
| • | our ability to successfully and cost-effectively market our services as superior to traditional or alternative sources for health insurance to a sufficiently large number of individuals; and |
| • | carriers’ willingness to use us and the Internet as a distribution channel for health insurance plans and products. |
If individuals and carriers determine that other sources of health insurance and health insurance applications are superior, our business will not grow and our results of operations and financial condition would be harmed.
Any legal liability, regulatory penalties, or negative publicity for the information on our platform or that we otherwise distribute or provide will likely harm our business and results of operations.
We provide information on our platform, through our call center partners and in other ways regarding health insurance in general and the health insurance plans and products we market and sell, including information relating to insurance premiums, coverage, benefits, provider networks, exclusions, limitations, availability, plan comparisons and insurance company ratings. A significant amount of both automated and manual effort is required to maintain the considerable amount of insurance plan information on our platform. We also regularly provide health insurance plan information in the scripts used by our customer call center partners. If the information we provide on our platform, through our customer call center partners or otherwise is not accurate or is construed as misleading, or if we do not properly assist individuals and businesses in purchasing health insurance, members, carriers and others could attempt to hold us liable for damages, our relationships with carriers could be terminated and regulators could attempt to subject us to penalties, revoke our licenses to transact health insurance business in a particular jurisdiction, and/or compromise the status of our licenses to transact health insurance business in other jurisdictions, which could result in our loss of our commission revenue. In the ordinary course of operating our business, we have received complaints that the information we provided was not accurate or was misleading. Although in the past we have resolved these complaints without significant financial cost, we cannot guarantee that we will be able to do so in the future. In addition, these types of claims could be time-consuming and expensive to defend, could divert our management’s attention and other resources and could cause a loss of confidence in our services. As a result, these claims could harm our business, results of operations and financial condition.
In the ordinary course of our business, we may receive inquiries from state regulators relating to various matters. We may in the future become involved in litigation in the ordinary course of our business. If we are found to have violated laws or regulations, we could lose our relationship with carriers and be subject to various fines and penalties, including revocation of our licenses to sell insurance, and our business, results of operations and financial condition would be materially harmed. We would also be harmed to the extent that related publicity damages our reputation as a trusted source of information relating to health insurance and its affordability. It could also be costly to defend ourselves regardless of the outcome. As a result, inquiries from regulators or our becoming involved in litigation could adversely affect our business, results of operations and financial condition.
If we do not continue to attract new individual customers, we may not achieve our revenue projections, and our results of operations would be harmed.
In order to grow our business, we must continually attract new distributors and individual customers. Our ability to do so depends in large part on the success of our sales and marketing efforts. Potential individual customers may seek out other options for purchasing insurance. Therefore, we must demonstrate that our products provide a viable solution for individual customers to obtain high quality coverage at an attractive price and provide a valuable business opportunity to our distributors. If we fail to provide high quality solutions and convince individual customers and distributors of our value proposition, we may not be able to retain existing
23
Table of Contents
customers or attract new individual customers. Additionally, there is no guarantee that the market for our services will grow as we expect. If the market for our services declines or develops more slowly than we expect, or if the number of individual customers or distributors that use our solutions declines or fails to increase as we expect, our revenue, results of operations, financial condition, business and prospects could be harmed.
Advance commission arrangements between us and some of our distributors expose us to the credit risks of such distributors and may increase our costs and expenses, which could in turn have an adverse effect on our business, financial condition, and results of operations.
We make advance commission payments to some of our licensed distributors in order to assist them with the cost of lead acquisition. As of September 30, 2012, we had prepayment balances for advance commissions in a total amount of approximately $300,000 under such contracts. Part of our strategy is to expand the practice of paying advance commissions, so we expect such balance to increase significantly in the future. In all such cases where we make advance commission payments, we receive collateral and personal guarantees. At a minimum, our collateral includes a claim against all future compensation owed to the distributor for all products sold. As a result, our claims for such payments would rank as secured claims. Depending on the amount of future compensation owed to the distributor, we could be exposed to the credit risks of our distributors in the event of their insolvency or bankruptcy. Where the amount owed to us exceeds the value of the collateral, our claims against the defaulting distributors would rank below those of other secured creditors, which would undermine our chances of obtaining the return of our advance commission payments. We may not be able to recover such advance payments and we may suffer losses should the distributors fail to fulfill their sales obligations under the contracts. Accordingly, any of the above scenarios could harm our business, results of operations and financial condition.
Seasonality may cause fluctuations in our financial results.
The number of member enrollments through our technology platform has generally increased in our third fiscal quarter. Conversely, we have generally experienced a decline in member enrollments in our fourth fiscal quarter. Although we believe that these trends may be influenced by an increase in new enrollments of college graduates in the third quarter and a decrease in new enrollments due to call center closures and reduced operating hours in the fourth quarter, we believe that the sale of health insurance plans and products through the Internet is still in its early stages, and, therefore, the reasons for these seasonal patterns are not entirely apparent. As the use of the Internet for the purchase and sale of health insurance becomes more widely accepted, other seasonality trends may develop and the existing seasonality and member behavior that we experience may change. Any seasonality that we experience may cause fluctuations in our financial results.
If we are unable to successfully introduce new technology solutions or services or fail to keep pace with advances in technology, our business, financial condition and results of operations will be adversely affected.
Our business depends on our ability to adapt to evolving technologies and industry standards and introduce new technology solutions and services accordingly. If we cannot adapt to changing technologies, our technology solutions and services may become obsolete, and our business would suffer. Because the healthcare insurance market is constantly evolving, our existing technology may become obsolete and fail to meet the requirements of current and potential members. Our success will depend, in part, on our ability to continue to enhance our existing technology solutions and services, develop new technology that addresses the increasingly sophisticated and varied needs of our members and respond to technological advances and emerging industry standards and practices on a timely and cost-effective basis. The development of our online platform entails significant technical and business risks. We may not be successful in developing, using, marketing, or maintaining new technologies effectively or adapting our technology to evolving customer requirements or emerging industry standards, and, as a result, our business and reputation could suffer. We may not be able to introduce new technology solutions on schedule, or at all, or such solutions may not achieve market acceptance. We also engage third-party vendors to develop, maintain and enhance our technology solutions, and our ability to develop and
24
Table of Contents
implement new technologies is therefore dependent on our ability to engage suitable vendors. We may also need to license software or technology from third parties in order to maintain, expand or modify our technology platform. However, there is no guarantee we will be able to enter into such agreements on acceptable terms or at all. Moreover, competitors may develop competitive products that could adversely affect our results of operations. A failure by us to introduce new solutions or to introduce these solutions on schedule could have an adverse effect on our business, financial condition and results of operations.
Our failure to obtain, maintain and enforce the intellectual property rights on which our business depends could have a material adverse effect on our business, financial condition and results of operations.
We rely upon intellectual property laws in the United States, and non-disclosure, confidentiality and other types of agreements with our employees, members and other parties, to establish, maintain and enforce our intellectual property and proprietary rights. However, any of our owned or licensed intellectual property rights could be challenged, invalidated, circumvented, infringed or misappropriated, our trade secrets and other confidential information could be disclosed in an unauthorized manner to third-parties, or our intellectual property rights may not be sufficient to permit us to take advantage of current market trends or otherwise to provide us with competitive advantages, which could result in costly redesign efforts, discontinuance of certain offerings or other competitive harm. Efforts to enforce our intellectual property rights may be time consuming and costly, distract management’s attention and resources and ultimately be unsuccessful. In addition, such efforts may result in our intellectual property rights being challenged, limited in scope, or declared invalid or unenforceable. Moreover, our failure to develop and properly manage new intellectual property could adversely affect our market positions and business opportunities.
We may not be able to obtain, maintain and enforce the intellectual property rights that may be necessary to protect and grow our business and to provide us with a meaningful competitive advantage. Also, some of our business and services may rely on technologies and software developed by or licensed from third-parties, and we may not be able to maintain our relationships with such third-parties or enter into similar relationships in the future on reasonable terms or at all. Our failure to obtain, maintain and enforce our intellectual property rights could therefore have a material adverse effect on our business, financial condition and results of operations.
Assertions by third-parties that we violate their intellectual property rights could have a material adverse effect on our business, financial condition and results of operations.
Third-parties may claim that we, our members, our licensees or parties indemnified by us are infringing upon or otherwise violating their intellectual property rights. Such claims may be made by competitors seeking to obtain a competitive advantage or by other parties. Additionally, in recent years, individuals and groups have begun purchasing intellectual property assets for the purpose of making claims of infringement and attempting to extract settlements from companies like ours. Any claims that we violate a third-party’s intellectual property rights can be time consuming and costly to defend and distract management’s attention and resources, even if the claims are without merit. Such claims may also require us to redesign affected products and services, enter into costly settlement or license agreements or pay costly damage awards, or face a temporary or permanent injunction prohibiting us from marketing or providing the affected products and services. Even if we have an agreement to indemnify us against such costs, the indemnifying party may be unable to uphold its contractual obligations. If we cannot or do not license the infringed technology at all, license the technology on reasonable terms or substitute similar technology from another source, our revenue and earnings could be adversely impacted.
In addition, we may use open source software in connection with our products and services. Companies that incorporate open source software into their products have, from time to time, faced claims challenging the ownership of open source software and/or compliance with open source license terms. As a result, we could be subject to suits by parties claiming ownership of what we believe to be open source software or noncompliance with open source licensing terms. Some open source software licenses require users who distribute open source software as part of their software to publicly disclose all or part of the source code to such software and/or make
25
Table of Contents
available any derivative works of the open source code on unfavorable terms or at no cost. Any requirement to disclose our proprietary source code or pay damages for breach of contract could have a material adverse effect on our business, financial condition and results of operations.
Assertions by third-parties that we violate their intellectual property rights could therefore have a material adverse effect on our business, financial condition and results of operations.
If we fail to effectively manage our growth, our business and results of operations could be harmed.
We have expanded our operations significantly since 2008. This has increased the significant demands on our management, our operational and financial systems and infrastructure and other resources. If we do not effectively manage our growth, the quality of our services could suffer. In order to successfully expand our business, we must effectively integrate, develop and motivate new employees, and we must maintain the beneficial aspects of our corporate culture. We may not be able to hire new employees quickly enough to meet our needs. If we fail to effectively manage our hiring needs and successfully integrate our new hires, our efficiency and ability to meet our forecasts and our employee morale, productivity and retention could suffer, and our business and results of operations could be harmed. We also need to continue to improve our existing systems for operational and financial management, including our reporting systems, procedures and controls. These improvements could require significant capital expenditures and place increasing demands on our management. We may not be successful in managing or expanding our operations or in maintaining adequate financial and operating systems and controls. If we do not successfully manage these processes, our business and results of operations will be harmed.
If we are unable to maintain a high level of service, our business and prospects may be harmed.
One of the key attributes of our business is providing high quality service to our carriers, distributors and members. We may be unable to sustain these levels of service, which would harm our reputation and our business. Alternatively, we may only be able to sustain high levels of service by significantly increasing our operating costs, which would materially adversely affect our results of operations. The level of service we are able to provide depends on our personnel to a significant extent. Our personnel must be well-trained in our processes and able to handle customer calls effectively and efficiently. Any inability of our personnel to meet our demand, whether due to absenteeism, training, turnover, disruptions at our facilities, bad weather, power outages or other reasons, could adversely impact our business. If we are unable to maintain high levels of service performance, our reputation could suffer and our results of operations and prospects would be harmed.
We are subject to privacy and data protection laws governing the transmission, security and privacy of health information, which may impose restrictions on the manner in which we access personal data and subject us to penalties if we are unable to fully comply with such laws.
Numerous federal, state and international laws and regulations govern the collection, use, disclosure, storage and transmission of individually identifiable health information. These laws and regulations, including their interpretation by governmental agencies, are subject to frequent change. These regulations could have a negative impact on our business, for example:
| • | The Health Insurance Portability and Accountability Act, or HIPAA, and its implementing regulations were enacted to ensure that employees can retain and at times transfer their health insurance when they change jobs, and to simplify healthcare administrative processes. The enactment of HIPAA also expanded protection of the privacy and security of personal health information and required the adoption of standards for the exchange of electronic health information. Among the standards that the Department of Health and Human Services has adopted pursuant to HIPAA are standards for electronic transactions and code sets, unique identifiers for providers, employers, health plans and individuals, security, electronic signatures, privacy and enforcement. Failure to comply with HIPAA could result in fines and penalties that could have a material adverse effect on us. |
26
Table of Contents
| • | The federal Health Information Technology for Economic and Clinical Health Act, or the HITECH Act, enacted as part of the American Recovery and Reinvestment Act of 2009, also known as the “Stimulus Bill,” effective February 22, 2010, sets forth health information security breach notification requirements and increased penalties for violation of HIPAA. The HITECH Act requires individual notification for all breaches, media notification of breaches of over 500 individuals and at least annual reporting of all breaches to the Department of Health and Human Services. The HITECH Act also replaced the prior penalty system of one tier of penalties of $100 per violation and an annual maximum of $25,000 with a four-tier system of sanctions for breaches. Penalties now range from the original $100 per violation and an annual maximum of $25,000 for the first tier to a fourth-tier minimum of $50,000 per violation and an annual maximum of $1.5 million. Failure to comply with the HITECH Act could result in fines and penalties that could have a material adverse effect on us. |
| • | Other federal and state laws restricting the use and protecting the privacy and security of individually identifiable information may apply, many of which are not preempted by HIPAA. |
| • | Federal and state consumer protection laws are increasingly being applied by the United States Federal Trade Commission, or FTC, and states’ attorneys general to regulate the collection, use, storage and disclosure of personal or individually identifiable information, through websites or otherwise, and to regulate the presentation of website content. |
We are required to comply with federal and state laws governing the transmission, security and privacy of individually identifiable health information that we may obtain or have access to in connection with the provision of our services. Despite the security measures that we have in place to ensure compliance with privacy and data protection laws, our facilities and systems, and those of our third-party vendors and subcontractors, are vulnerable to security breaches, acts of vandalism or theft, computer viruses, misplaced or lost data, programming and human errors or other similar events. Due to the recent enactment of the HITECH Act, we are not able to predict the extent of the impact such incidents may have on our business. Our failure to comply may result in criminal and civil liability because the potential for enforcement action against business associates is now greater. Enforcement actions against us could be costly and could interrupt regular operations, which may adversely affect our business. While we have not received any notices of violation of the applicable privacy and data protection laws and believe we are in compliance with such laws, there can be no assurance that we will not receive such notices in the future.
Under the HITECH Act, as a business associate we may also be liable for privacy and security breaches and failures of our subcontractors. Even though we provide for appropriate protections through our agreements with our subcontractors, we still have limited control over their actions and practices. A breach of privacy or security of individually identifiable health information by a subcontractor may result in an enforcement action, including criminal and civil liability, against us.
In addition, numerous other federal and state laws protect the confidentiality of individually identifiable information as well as employee personal information, including state medical privacy laws, state social security number protection laws, and federal and state consumer protection laws. These various laws in many cases are not preempted by HIPAA and may be subject to varying interpretations by the courts and government agencies, creating complex compliance issues for us and our members and potentially exposing us to additional expense, adverse publicity and liability, any of which could adversely affect our business.
Our business is subject to online security risks, and if we are unable to safeguard the security and privacy of confidential data, our reputation and business will be harmed.
Our services involve the collection and storage of confidential information of members and the transmission of this information to carriers. For example, we collect names, addresses, social security, bank account and credit card numbers, and information regarding the medical history of members in connection with their applications for insurance. In certain cases such information is provided to third-parties, for example to the service providers who provide hosting services for our technology platform, and we may therefore be unable to control the use of
27
Table of Contents
such information or the security protections employed by such third-parties. We may be required to expend significant capital and other resources to protect against security breaches or to alleviate problems caused by security breaches. Despite our implementation of security measures, techniques used to obtain unauthorized access or to sabotage systems change frequently. As a result, we may be unable to anticipate these techniques or to implement adequate preventative measures. Any compromise or perceived compromise of our security (or the security of our third-party service providers who have access to our members’ confidential information) could damage our reputation and our relationship with our members, distributors and carriers, could reduce demand for our services and could subject us to significant liability as well as regulatory action. In addition, in the event that new data security laws are implemented, or our carrier or other partners determine to impose new requirements on us relating to data security, we may not be able to timely comply with such requirements, or such requirements may not be compatible with our current processes. Changing our processes could be time consuming and expensive, and failure to timely implement required changes could result in our inability to sell health insurance plans and products in a particular jurisdiction or for a particular carrier, or subject us to liability for non-compliance.
Our services present the potential for embezzlement, identity theft or other similar illegal behavior by our employees or subcontractors with respect to third-parties.
Among other things, our services involve handling information from members, including credit card information and bank account information. Our services also involve the use and disclosure of personal information that could be used to impersonate third-parties or otherwise gain access to their data or funds. If any of our employees or subcontractors takes, converts or misuses such funds, documents or data, we could be liable for damages, and our business reputation could be damaged. In addition, we could be perceived to have facilitated or participated in illegal misappropriation of funds, documents or data and therefore be subject to civil or criminal liability. Any such illegal activity by our employees or subcontractors could have an adverse effect on our business, financial condition and results of operations.
System failures or capacity constraints could harm our business and results of operations.
The performance, reliability and availability of our technology platform, customer service call center and underlying network infrastructures are critical to our financial results and our relationship with members, distributors and insurance carriers. Although we regularly attempt to enhance and maintain our technology platform, customer service call center and system infrastructure, system failures and interruptions may occur if we are unsuccessful in these efforts or experience difficulties with transitioning existing systems to upgraded systems, if we are unable to accurately project the rate or timing of increases in our platform traffic or customer service call center call volume or for other reasons, some of which are completely outside our control. Significant failures and interruptions, particularly during peak enrollment periods, could harm our business, results of operations and financial condition.
We rely in part upon third-party vendors, including data center and bandwidth providers, to operate and maintain our technology platform. We cannot predict whether additional network capacity will be available from these vendors as we need it, and our network or our suppliers’ networks might be unable to achieve or maintain a sufficiently high capacity of data transmission to allow us to process health insurance applications in a timely manner or effectively download data, especially if our platform traffic increases. Any system failure that causes an interruption in, or decreases the responsiveness of, our services could impair our revenue-generating capabilities, harm our image and subject us to potential liability. Our database and systems are vulnerable to damage or interruption from human error, earthquakes, fire, floods, power loss, telecommunications failures, physical or electronic break-ins, computer viruses, acts of terrorism, other attempts to harm our systems and similar events.
We depend upon third-parties, including telephone service providers and third-party software providers, to operate our customer service call center. Any failure of the systems upon which we rely in the operation of our
28
Table of Contents
customer service call center could negatively impact sales as well as our relationship with members, which could harm our business, results of operations and financial condition.
We rely on third-party vendors to develop, host, maintain, service and enhance our technology platform.
We rely on third-party vendors to develop, host, maintain, support and enhance our technology platform. In particular, we are party to an agreement with BimSym eBusiness Solutions, Inc., or BimSym, pursuant to which BimSym provides various professional services relating to our A.R.I.E.S. technology platform, including hosting, support, maintenance and development services. Our ability to offer our services and operate our business is therefore dependent on maintaining our relationships with third-party vendors, particularly BimSym, and entering into new relationships to meet the changing needs of our business. Any deterioration in our relationships with such vendors, or our failure to enter into agreements with vendors in the future would harm our business, results of operations and financial condition. If our vendors are unable or unwilling to provide the services necessary to support our business, or if our agreements with such vendors are terminated, our operations could be significantly disrupted. We may also incur substantial costs, delays and disruptions to our business in transitioning such services to ourselves or other third-party vendors. In addition, third-party vendors may not be able to provide the services required in order to meet the changing needs of our business.
Carriers and distributors depend upon third-party service providers to access our online platform, and our business and results of operations could be harmed as a result of technical difficulties experienced by these service providers.
Carriers and distributors using our online platform depend upon Internet and other service providers for access to our platform. Many of these service providers have experienced significant outages, delays and other difficulties in the past and could experience them in the future. Any significant interruption in access to our technology platform or increase in our platform’s response time as a result of these difficulties could damage our relationship with carriers, distributors and existing and potential members and could harm our business, results of operations and financial condition.
Economic conditions and other factors beyond our control may negatively impact our business, results of operations and financial condition.
Our revenue depends upon demand for our insurance products, which can be influenced by a variety of factors beyond our control. We have no control over the economic and other factors that influence such demand. We cannot be certain of the future impact that the recent recession will have on our business. A further softening of demand for our products and the services offered by us, whether caused by changes in individual preferences or the regulated environment in which we operate, or by a weak economy, including as a result of recent disruptions in the global financial markets or a decrease in general consumer confidence, will result in decreased revenue and growth. Members may attempt to reduce expenses by canceling existing plans and products purchased through us, not purchasing new plans and products through us or purchasing plans with lower premiums for which we receive lower commissions. A continuing negative economic environment could also adversely impact the carriers whose plans and products are offered on our platform, and they may, among other things, determine to reduce their commission rates, increase premiums or reduce benefits, any of which could negatively impact our business, results of operations and financial condition.
To the extent the economy or other factors adversely impact our member retention, the number or type of insurance applications submitted through us and that are approved by carriers, or the commissions that we receive from carriers, our rate of growth will decline and our business and results of operations will be harmed.
29
Table of Contents
The loss of any member of our management team and our inability to make up for such loss with a qualified replacement could harm our business.
Competition for qualified management in our industry is intense. Many of the companies with which we compete for management personnel have greater financial and other resources than we do or are located in geographic areas which may be considered by some to be more desirable places to live. If we are not able to retain any of our key management personnel, our business could be harmed.
We may make future acquisitions which may be difficult to integrate, divert management resources, result in unanticipated costs or dilute our stockholders.
Part of our continuing business strategy is to acquire or invest in, companies, products or technologies that complement our current products, enhance our market coverage, technical capabilities or production capacity, or offer growth opportunities. Future acquisitions could pose numerous risks to our operations, including:
| • | difficulty integrating the purchased operations, technologies or products; |
| • | incurring substantial unanticipated integration costs; |
| • | assimilating the acquired businesses may divert significant management attention and financial resources from our other operations and could disrupt our ongoing business; |
| • | acquisitions could result in the loss of key employees, particularly those of the acquired operations; |
| • | difficulty retaining or developing the acquired businesses’ customers; |
| • | acquisitions could adversely affect our existing business relationships with suppliers and members; |
| • | failing to realize the potential cost savings or other financial benefits and/or the strategic benefits of the acquisitions; and |
| • | incurring liabilities from the acquired businesses for infringement of intellectual property rights or other claims, and we may not be successful in seeking indemnification for such liabilities or claims. |
In connection with these acquisitions or investments, we could incur debt, amortization expenses related to intangible assets, large and immediate write-offs, assume liabilities or issue stock that would dilute our current stockholders’ percentage of ownership. We may not be able to complete acquisitions or integrate the operations, products or personnel gained through any such acquisition without a material adverse effect on our business, financial condition and results of operations.
The requirements of being a public company may strain our resources and distract our management, which could make it difficult to manage our business, particularly after we are no longer an “emerging growth company.”
Following the completion of this offering, we will be required to comply with various regulatory and reporting requirements, including those required by the Securities and Exchange Commission (the “SEC”). Complying with these reporting and other regulatory requirements will be time-consuming and will result in increased costs to us and could have a negative effect on our business, financial condition and results of operations.
As a public company, we will be subject to the reporting requirements of the Securities Exchange Act of 1934 (as amended, the “Exchange Act”) and the requirements of the Sarbanes-Oxley Act of 2002 (as amended, the “Sarbanes-Oxley Act”). These requirements may place a strain on our systems and resources. The Exchange Act requires that we file annual, quarterly and current reports with respect to our business and financial condition. The Sarbanes-Oxley Act requires that we maintain effective disclosure controls and procedures and internal controls over financial reporting. To maintain and improve the effectiveness of our disclosure controls
30
Table of Contents
and procedures, we will need to commit significant resources, hire additional staff and provide additional management oversight. We will be implementing additional procedures and processes for the purpose of addressing the standards and requirements applicable to public companies. Sustaining our growth also will require us to commit additional management, operational and financial resources to identify new professionals to join our company and to maintain appropriate operational and financial systems to adequately support expansion. These activities may divert management’s attention from other business concerns, which could have a material adverse effect on our business, financial condition and results of operations.
As an “emerging growth company” as defined in the Jumpstart Our Business Startups Act of 2012 (the “JOBS Act”), we intend to take advantage of certain temporary exemptions from various reporting requirements, including, but not limited to, not being required to comply with the auditor attestation requirements of Section 404 of the Sarbanes-Oxley Act and reduced disclosure obligations regarding executive compensation in our periodic reports and proxy statements. In addition, we have elected under the JOBS Act to delay adoption of new or revised accounting pronouncements applicable to public companies until such pronouncements are made applicable to private companies.
When these exemptions cease to apply, we expect to incur additional expenses and devote increased management effort toward ensuring compliance with them. We cannot predict or estimate the amount of additional costs we may incur as a result of becoming a public company or the timing of such costs.
Risks Related to Our Structure
We are a holding company and our only material asset after completion of the reorganization and this offering will be our interest in Health Plan Intermediaries Holdings, LLC and, accordingly, we are dependent upon distributions from Health Plan Intermediaries Holdings, LLC to pay taxes and other expenses.
We will be a holding company and will have no material assets other than our ownership of Series A Membership Interests of Health Plan Intermediaries Holdings, LLC. We will have no independent means of generating revenue. Health Plan Intermediaries Holdings, LLC will be treated as a partnership for U.S. federal income tax purposes and, as such, will not itself be subject to U.S. federal income tax. Instead, its net taxable income will generally be allocated to its members, including us, pro rata according to the number of membership interests each member owns. Accordingly, we will incur income taxes on our proportionate share of any net taxable income of Health Plan Intermediaries Holdings, LLC and also will incur expenses related to our operations. We intend to cause Health Plan Intermediaries Holdings, LLC to distribute cash to its members, including us, in an amount at least equal to the amount necessary to cover their respective tax liabilities, if any, with respect to their allocable share of the net income of Health Plan Intermediaries Holdings, LLC and to cover dividends, if any, declared by us, as well as any payments due under the tax receivable agreement, as described below. To the extent that we need funds to pay our tax or other liabilities or to fund our operations, and Health Plan Intermediaries Holdings, LLC is restricted from making distributions to us under applicable agreements, laws or regulations or does not have sufficient cash to make these distributions, we may have to borrow funds to meet these obligations and operate our business, and our liquidity and financial condition could be materially adversely affected. To the extent that we are unable to make payments under the income tax receivable agreement for any reason, such payments will be deferred and will accrue interest until paid.
We will be required to pay the existing and certain future holders of Series B Membership Interests most of the tax benefits that we may receive as a result of the purchase of Series B Membership Interests with the net proceeds of the sale of any over-allotment shares, future exchanges of Series B Membership Interests for our Class A common stock and payments made under the tax receivable agreement itself, and the amounts we pay could be substantial.
We expect that the purchase of Series B Membership Interests (together with an equal number of shares of our Class B common stock) with the net proceeds of the sale of any over-allotment shares, as well as any future
31
Table of Contents
exchanges of Series B Membership Interests (together with an equal number of shares of our Class B common stock) for shares of our Class A common stock, will result in increases in the tax basis in our share of the tangible and intangible assets of Health Plan Intermediaries Holdings, LLC. Any such increases in tax basis could reduce the amount of tax that we would otherwise be required to pay in the future.
We will enter into a tax receivable agreement with the other current members of Health Plan Intermediaries Holdings, LLC (Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske) and certain future members of Health Plan Intermediaries Holdings, LLC, pursuant to which we will pay them 85% of the amount of the cash savings, if any, in U.S. federal, state and local income tax that we realize (or are deemed to realize in the case of an early termination payment by us, a change in control or a material breach by us of our obligations under the tax receivable agreement, as discussed below) as a result of these possible increases in tax basis resulting from our purchases or exchanges of Series B Membership Interests as well as certain other benefits attributable to payments under the tax receivable agreement itself. Any actual increases in tax basis, as well as the amount and timing of any payments under the tax receivable agreement, cannot be predicted reliably at this time. The amount of any such increases and payments will vary depending upon a number of factors, including the timing of exchanges, the price of our Class A common stock at the time of the exchanges, the amount, character and timing of our income and the tax rates then applicable. The payments that we may be required to make pursuant to the tax receivable agreement could be substantial for periods in which we generate taxable income. Assuming no material changes in the relevant tax law and based on our current operating plan and other assumptions, including our estimate of the tax basis of our assets as of September 30, 2012, if we acquired all of the Series B Membership Interests in taxable transactions at the time of the closing of this offering for a price of $15 (the midpoint of the range on the cover of this prospectus) per share, we estimate that the maximum amount that we would be required to pay under the tax receivable agreement could be approximately $57,126,000. The actual amount may materially differ from this hypothetical amount, as potential future payments will be calculated using the market value of our Class A common stock at the time of relevant exchange and prevailing tax rates in future years and will be dependent on us generating sufficient future taxable income to realize the benefit. See “The Reorganization of Our Corporate Structure—Tax Receivable Agreement.”
In addition, the tax receivable agreement will provide that in the case that we exercise our right to early termination of the tax receivable agreement or in the case of a change in control or a material breach by us of our obligations under the tax receivable agreement, the tax receivable agreement will terminate, and we will be required to make a payment equal to the present value of future payments under the tax receivable agreement, which payment would be based on certain assumptions, including those relating to our future taxable income. In these situations, our obligations under the tax receivable agreement could have a substantial negative impact on our liquidity and could have the effect of delaying, deferring or preventing certain mergers, asset sales, other forms of business combinations or other changes of control. These provisions of the tax receivable agreement may result in situations where Mr. Kosloske may have interests that differ from or are in addition to those of other shareholders. Because we are controlled by Mr. Kosloske, Mr. Kosloske will have effective control over the outcome of votes on all matters requiring approval by our stockholders and accordingly actions that affect such obligations under the tax receivable agreement may be taken even if other stockholders oppose them.
If the Internal Revenue Service successfully challenges the tax basis increases, we will not be reimbursed for any payments made under the tax receivable agreement (although future payments under the tax receivable agreement, if any, would be adjusted to reflect the result of any such successful challenge by the Internal Revenue Service). As a result, in certain circumstances, we could be required to make payments under the tax receivable agreement in excess of our cash tax savings.
32
Table of Contents
We may not be able to realize all or a portion of the tax benefits that are expected to result from the purchase of Series B Membership Interests with the net proceeds of the sale of any over-allotment shares, future exchanges of Series B Membership Interests for our Class A common stock and payments made under the tax receivable agreement itself.
Our ability to benefit from any depreciation or amortization deductions or to realize other tax benefits that we currently expect to be available as a result of the increases in tax basis created by the purchase of Series B Membership Interests (together with an equal number of shares of our Class B common stock) with the net proceeds of the sale of any over-allotment shares, as well as any future exchanges of Series B Membership Interests (together with an equal number of shares of our Class B common stock) for our Class A common stock, and our ability to realize certain other tax benefits attributable to payments under the tax receivable agreement itself depend on a number of assumptions, including that we earn sufficient taxable income each year during the period over which such deductions are available and that there are no adverse changes in applicable law or regulations. If our actual taxable income were insufficient and/or there were adverse changes in applicable law or regulations, we may be unable to realize all or a portion of these expected benefits and our cash flows and stockholders’ equity could be negatively affected. See “The Reorganization of Our Corporate Structure—Tax Receivable Agreement.”
Risks Related to This Offering and Ownership of Our Class A Common Stock
There may not be an active, liquid trading market for our Class A common stock.
Prior to this offering, there has been no public market for shares of our Class A common stock. We cannot predict the extent to which investor interest in our company will lead to the development of a trading market on the NASDAQ Global Market or how liquid that market may become. If an active trading market does not develop, you may have difficulty selling any shares of our Class A common stock that you purchase. The initial public offering price of shares of our Class A common stock is, or will be, determined by negotiation between us and the underwriters and may not be indicative of prices that will prevail following the completion of this offering. The market price of shares of our Class A common stock may decline below the initial public offering price, and you may not be able to resell your shares of our Class A common stock at or above the initial public offering price.
We expect that our stock price will fluctuate significantly, and you may not be able to resell your shares at or above the initial public offering price.
The trading price of our Class A common stock is likely to be volatile and subject to wide price fluctuations in response to various factors, including:
| • | market conditions in the broader stock market in general, or in our industry in particular; |
| • | actual or anticipated fluctuations in our quarterly financial and results of operations; |
| • | our ability to satisfy our ongoing capital needs and unanticipated cash requirements, particularly with respect to our advance commissions structure; |
| • | additional indebtedness incurred in the future; |
| • | introduction of new products and services by us or our competitors; |
| • | issuance of new or changed securities analysts’ reports or recommendations; |
| • | sales of large blocks of our stock; |
| • | additions or departures of key personnel; |
| • | regulatory developments; |
33
Table of Contents
| • | litigation and governmental investigations; and |
| • | economic and political conditions or events. |
These and other factors may cause the market price and demand for our Class A common stock to fluctuate substantially, which may limit or prevent investors from readily selling their shares of Class A common stock and may otherwise negatively affect the liquidity of our Class A common stock. In addition, in the past, when the market price of a stock has been volatile, holders of that stock have instituted securities class action litigation against the company that issued the stock. If any of our stockholders brought a lawsuit against us, we could incur substantial costs defending the lawsuit. Such a lawsuit could also divert the time and attention of our management from our business.
The trading market for our Class A common stock will also be influenced by the research and reports that industry or securities analysts publish about us or our business. As a new public company, we do not currently have and may never obtain research coverage by securities and industry analysts. If no securities or industry analysts commence coverage of our company, the trading price for our stock would be negatively impacted. If we obtain securities or industry analyst coverage and if one or more of these analysts cease coverage of our company or fail to publish reports on us regularly, we could lose visibility in the financial markets, which in turn could cause our stock price or trading volume to decline. Moreover, if one or more of the analysts who cover us downgrades our stock, or if our results of operations do not meet their expectations, our stock price could decline.
If a substantial number of shares become available for sale and are sold in a short period of time, the market price of our Class A common stock could decline.
If our existing stockholders sell substantial amounts of our Class A common stock in the public market following this offering, the market price of our Class A common stock could decrease significantly. The perception in the public market that our existing stockholders might sell shares of Class A common stock could also depress our market price. Upon completion of this offering, we will have 4,666,667 shares of Class A common stock outstanding. In addition, we do not expect that any options that are held by our employees under stock plans that we intend to adopt will be exercisable in 2013. Our executive officers and directors will be subject to the lock-up agreements described under “Underwriting,” the Rule 144 holding period requirements described under “Shares Eligible for Future Sale” and the lock-up periods described under “Underwriting.” The market price of shares of our Class A common stock may drop significantly when the restrictions on resale by our existing stockholders lapse. A decline in the price of shares of our Class A common stock might impede our ability to raise capital through the issuance of additional shares of our Class A common stock or other equity securities.
We are a “controlled company” within the meaning of the rules of the NASDAQ Global Market and, as a result, expect to qualify for, and intend to rely on, exemptions from certain corporate governance requirements. You will not have the same protections afforded to stockholders of companies that are subject to such requirements.
Following the consummation of this offering, entities controlled by Michael W. Kosloske, our Chairman, President and Chief Executive Officer, will control a majority of the combined voting power of all classes of our voting stock. As a result, we expect to be a “controlled company” within the meaning of the corporate governance standards of the NASDAQ Global Market. Under NASDAQ Global Market rules, a company of which more than 50% of the voting power is held by an individual, group or another company is a “controlled company” and may elect not to comply with certain corporate governance requirements, including:
| • | the requirement that a majority of the board of directors consist of independent directors; |
| • | the requirement that we have a nominating and corporate governance committee that is composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities; |
34
Table of Contents
| • | the requirement that we have a compensation committee that is composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities; and |
| • | the requirement for an annual performance evaluation of the nominating and corporate governance and compensation committees. |
Following this offering, we intend to utilize these exemptions if we continue to qualify as a “controlled company.” If we utilize these exemptions we will not have a majority of independent directors and our nominating and corporate governance and compensation committees will not consist entirely of independent directors and such committees will not be subject to annual performance evaluations. Accordingly, you will not have the same protections afforded to stockholders of companies that are subject to all of the corporate governance requirements of the NASDAQ Global Market. See “Management—Controlled Company.”
We are controlled by our existing owner, whose interests may differ from those of our public stockholders.
We are controlled by Mr. Kosloske, and after this offering will continue to be controlled by entities associated with Mr. Kosloske. After the completion of this offering, Mr. Kosloske will beneficially own in the aggregate approximately 65% of the combined voting power of our common stock (or 62% if the underwriters exercise their option to purchase additional shares in full). As a result of this ownership, Mr. Kosloske will have effective control over the outcome of votes on all matters requiring approval by our stockholders, including the election of directors, the adoption of amendments to our certificate of incorporation and bylaws and approval of a sale of the company and other significant corporate transactions , including such corporate transactions that may affect our obligations under the tax receivable agreement. See “We will be required to pay the existing and certain future holders of Series B Membership Interests most of the tax benefits that we may receive as a result of the purchase of Series B Membership Interests with the net proceeds of the sale of any over-allotment shares, future exchanges of Series B Membership Interests for our Class A common stock and payments made under the tax receivable agreement itself, and the amounts we pay could be substantial.” Mr. Kosloske can also take actions that have the effect of delaying or preventing a change in control of us or discouraging others from making tender offers for our shares, which could prevent stockholders from receiving a premium for their shares. These actions may be taken even if other stockholders oppose them.
The market price of our Class A common stock could decline due to the large number of shares of Class A common stock eligible for future sale upon the exchange of Series B Membership Interests.
The market price of our Class A common stock could decline as a result of sales of a large number of shares of our Class A common stock eligible for future sale upon the exchange of Series B Membership Interests (together with an equal number of shares of our Class B common stock), or the perception that such sales could occur. These sales, or the possibility that these sales may occur, may also make it more difficult for us to raise additional capital by selling equity securities in the future, at a time and price that we deem appropriate.
After completion of this offering, approximately 4,666,667 Series A Membership Interests and 8,666,667 Series B Membership Interests of Health Plan Intermediaries Holdings, LLC will be outstanding. Each Series B Membership Interest, together with one share of our Class B common stock, will be exchangeable for one share of Class A common stock, as described under “The Reorganization of Our Corporate Structure—Amended and Restated Limited Liability Company Agreement of Health Plan Intermediaries, LLC.” We will enter into a registration rights agreement with Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC pursuant to which we will grant them registration rights with respect to their shares of Class A common stock delivered in exchange for their Series B Membership Interests. See “The Reorganization of Our Corporate Structure—Registration Rights Agreement.”
35
Table of Contents
Some provisions of Delaware law and our amended and restated certificate of incorporation and amended and restated bylaws may deter third-parties from acquiring us.
Our amended and restated certificate of incorporation and amended and restated bylaws provide for, among other things:
| • | restrictions on the ability of our stockholders to fill a vacancy on the board of directors; |
| • | prohibit stockholder action by written consent after the date on which Mr. Kosloske ceases to beneficially own at least a majority of all of the outstanding shares of our capital stock entitled to vote; |
| • | prohibit cumulative voting in the election of directors, which would otherwise allow holders of less than a majority of stock to elect some directors; |
| • | provide that special meetings of stockholders may be called only by the board of directors, the chairman of the board of directors or the chief executive officer; provided, however, if Mr. Kosloske beneficially owns at least a majority of all of the outstanding shares of our capital stock entitled to vote, special meetings of stockholders may be called by the holders of a majority of the total voting power of our then outstanding capital stock; |
| • | establish advance notice procedures for the nomination of candidates for election as directors or for proposing matters that can be acted upon at stockholder meetings; |
| • | provide that on and after the date Mr. Kosloske collectively ceases to beneficially own a majority of all of the outstanding shares of our capital stock entitled to vote, (a) directors may be removed only for cause and only upon the affirmative vote of holders of at least 75% of all of the outstanding shares of our capital stock entitled to vote, and (b) certain provisions of our amended and restated certificate of incorporation may only be amended upon the affirmative vote of holders of at least 75% of all of the outstanding shares of our capital stock entitled to vote; and |
| • | the authorization of undesignated preferred stock, the terms of which may be established and shares of which may be issued without stockholder approval. |
After the completion of this offering, Mr. Kosloske will beneficially own in the aggregate approximately 65% of the combined voting power of our common stock (or 62% if the underwriters exercise their option to purchase additional shares in full).
These anti-takeover defenses could discourage, delay or prevent a transaction involving a change in control of our company. These provisions could also discourage proxy contests and make it more difficult for you and other stockholders to elect directors of your choosing and cause us to take other corporate actions that you desire.
We do not anticipate paying any cash dividends in the foreseeable future.
We currently intend to retain our future earnings, if any, for the foreseeable future, to repay indebtedness and to fund the development and growth of our business. We do not intend to pay any dividends to holders of our Class A common stock. As a result, capital appreciation in the price of our Class A common stock, if any, will be your only source of gain on an investment in our Class A common stock.
New investors in our Class A common stock will experience immediate and substantial book value dilution after this offering.
The initial public offering price of our Class A common stock will be substantially higher than the pro forma net tangible book value per share of the outstanding Class A common stock immediately after this offering. Based on an assumed initial public offering price of $15 per share (the midpoint of the price range set forth on the cover of this prospectus) and our net tangible book value as of September 30, 2012, if you purchase our Class A common stock in this offering you will pay more for your shares than the amounts paid by our existing stockholders for their shares and you will suffer immediate dilution of approximately $10.51 per share in pro forma net tangible book value. As a result of this dilution, investors purchasing stock in this offering may receive significantly less than the full purchase price that they paid for the shares purchased in this offering in the event of a liquidation.
36
Table of Contents
We have identified a material weakness in our internal control over financial reporting that, if not corrected, could result in material misstatements in our financial statements.
In connection with the preparation of our financial statements for the periods ended December 31, 2011 and 2010 and for the nine-months ended September 30, 2012, we identified a certain matter involving our internal control over financial reporting that constitutes a material weakness under standards established by the Public Company Accounting Oversight Board, which we refer to as PCAOB. The PCAOB defines a material weakness as a deficiency, or combination of deficiencies, in internal control over financial reporting, such that there is a reasonable possibility that a material misstatement of a company’s annual or interim financial statements will not be prevented or detected on a timely basis.
We identified a material weakness where we did not have effective controls over the design and operation of the financial statement close process, which process impacts most of our significant accounts included in the financial statements. The deficiencies in the design and operation of the financial statement close process that resulted in the material weakness included the following:
| • | lack of a formal process for reviewing period-end cutoff of revenues and expenses to ensure amounts are captured in the period earned or incurred under the accrual basis of accounting; |
| • | no process in place to ensure all expenses incurred during the period are accrued as of the month-end date, including expenses for which estimates are required; |
| • | absence of a mechanism through which the accounting implications of significant or unusual events and transactions are formally evaluated; and |
| • | no process to ensure formally executed agreements regarding all significant arrangements with third parties and others are obtained. |
The material weakness affected the financial statements as of and for the year ended December 31, 2010, and we accordingly restated our previously issued financial statements as of and for the year ended December 31, 2010 to correct the identified errors resulting from the material weakness. For example, we identified errors in the presentation of revenues where certain amounts collected on behalf of contracted insurance carriers and discount benefit vendors should have been reported on a net basis, rather than as gross revenues and related costs. This change had no impact on net income (loss) from operations or net income. In addition, we identified errors in revenues and operating costs and expenses where revenues were recorded when cash was received, rather than when amounts were earned, and operating costs and expenses were recorded at the time of cash disbursement rather than when amounts were incurred. The cumulative effect of these errors was a decrease in income (loss) from operations and net income (loss) of approximately $691,000 for the year ended December 31, 2010. We also identified an error in accounting for the sale of units of Health Plan Intermediaries, LLC to the Naylor Group Partners, LLC in 2009. In connection with such sale, we had previously recognized an increase in basis of the assets, but the transaction should have been accounted for as an equity transaction with no increase in basis. This error accounted for substantially all of the change in member’s equity (deficit), beginning of period, December 31, 2010. The effect was a decrease in member’s equity (deficit), beginning of period, December 31, 2010, of approximately $1,153,000. The cumulative impact of the adjustments described above on our previously issued financial statements as of and for the year ended December 31, 2010 was a reduction of revenues of $3,186,000, a reduction of operating costs and expenses of $2,495,000, a reduction of net income of $691,000, a decrease in cash flows of $598,000 and a reduction in member’s equity of $1,823,000.
We are taking steps to address this material weakness by hiring additional personnel with technical accounting expertise and by implementing enhanced training for our finance and accounting personnel to familiarize them with our accounting policies. However, the material weakness will be ongoing until these controls are fully implemented and we will not be able to confirm that we have remediated this material weakness until our newly implemented procedures have been working for a sufficient period of time. As a result
37
Table of Contents
of this and similar activities, management’s attention may be diverted from other business concerns, which could have a material adverse effect on our business, financial condition and results of operations.
If the remedial policies and procedures we implement and resources we hire are insufficient to address the identified material weakness, or if additional material weaknesses or significant deficiencies in our internal controls are discovered in the future, we may fail to meet our future reporting obligations, our financial statements may contain material misstatements and our operating results may be adversely affected.
Our internal controls over financial reporting may not be effective and our independent registered public accounting firm may not be able to certify as to their effectiveness, which could have a significant and adverse effect on our business and reputation.
We are not currently required to comply with SEC rules that implement Section 404 of the Sarbanes-Oxley Act and are therefore not required to make a formal assessment of the effectiveness of our internal controls over financial reporting for that purpose. We will be required, pursuant to the Exchange Act, to furnish a report by management on, among other things, the effectiveness of our internal control over financial reporting for the first fiscal year beginning after the effective date of this offering.
When evaluating our internal controls over financial reporting, we may identify material weaknesses that we may not be able to remediate in time to meet the applicable deadline imposed upon us for compliance with the requirements of Section 404 of the Sarbanes-Oxley Act. In addition, if we fail to achieve and maintain the adequacy of our internal controls, as such standards are modified, supplemented or amended from time to time, we may not be able to ensure that we can conclude, on an ongoing basis, that we have effective internal controls over financial reporting in accordance with Section 404 of the Sarbanes-Oxley Act. We cannot be certain as to the timing of completion of our evaluation, testing and any remediation actions or the impact of the same on our operations. If we are not able to implement the requirements of Section 404 of the Sarbanes-Oxley Act in a timely manner or with adequate compliance, we may be subject to sanctions or investigation by regulatory authorities, such as the SEC. As a result, there could be a negative reaction in the financial markets due to a loss of confidence in the reliability of our financial statements. In addition, we may be required to incur costs in improving our internal control system and the hiring of additional personnel. Any such action could negatively affect our results of operations and cash flows.
We are an “emerging growth company” and we cannot be certain if the reduced disclosure requirements applicable to emerging growth companies will make our Class A common stock less attractive to investors.
We are an “emerging growth company,” as defined in the JOBS Act, and we intend to take advantage of certain exemptions from various reporting requirements that are applicable to other public companies that are not “emerging growth companies” including, but not limited to, not being required to comply with the auditor attestation requirements of Section 404 of the Sarbanes-Oxley Act, which may increase the risk that weaknesses or deficiencies in our internal control over financial reporting go undetected, and reduced disclosure obligations regarding executive compensation in our periodic reports and proxy statements, which may make it more difficult for investors and securities analysts to evaluate our company. In addition, we have elected under the JOBS Act to delay adoption of new or revised accounting pronouncements applicable to public companies until such pronouncements are made applicable to private companies. As a result of this election, our financial statements may not be comparable to companies that comply with public company effective dates. We cannot predict if investors will find our Class A common stock less attractive if we rely on these exemptions. If some investors find our Class A common stock less attractive as a result, there may be a less active trading market for our Class A common stock and our stock price may be more volatile. We may take advantage of these reporting exemptions until we are no longer an emerging growth company, which in certain circumstances could be up to five years.
38
Table of Contents
We will have broad discretion in using the net proceeds of this offering, and we may not effectively expend the proceeds.
We intend to use the net proceeds of this offering to repay all of the outstanding debt under our existing credit facilities, to provide the funds necessary to expand our advance commission structure and for general corporate purposes, including acquisitions. We will have significant flexibility and broad discretion in applying the net proceeds of this offering and we may not apply the net proceeds of this offering effectively. Our management might not be able to yield a significant return, if any, on any investment of these net proceeds. You will not have the opportunity to influence our decisions on how to use our net proceeds from this offering.
Our business and stock price may suffer as a result of our lack of public company operating experience.
We have been a privately-held company since we began operations in 2008. Our lack of public company operating experience may make it difficult to forecast and evaluate our future prospects. If we are unable to execute our business strategy, either as a result of our inability to effectively manage our business in a public company environment or for any other reason, our prospects, financial condition and results of operations may be harmed.
39
Table of Contents
SPECIAL NOTE REGARDING FORWARD-LOOKING STATEMENTS
We have made statements under the captions “Prospectus Summary,” “Risk Factors,” “Management’s Discussion and Analysis of Financial Condition and Results of Operations,” “Business” and in other sections of this prospectus that are forward-looking statements. All statements other than statements of historical fact included in this prospectus are forward-looking statements. You can identify forward-looking statements by the fact that they do not relate strictly to historical or current facts. These statements may include words such as “may,” “might,” “will,” “should,” “expects,” “plans,” “anticipates,” “believes,” “estimates,” “predicts,” “potential” or “continue,” the negative of these terms and other comparable terminology. These forward-looking statements, which are subject to risks, uncertainties and assumptions about us, may include projections of our future financial performance, our anticipated growth strategies and anticipated trends in our business. These statements are only predictions based on our current expectations and projections about future events. There are important factors that could cause our actual results, level of activity, performance or achievements to differ materially from the results, level of activity, performance or achievements expressed or implied by the forward-looking statements, including those factors discussed under the caption entitled “Risk Factors.” You should specifically consider the numerous risks outlined under “Risk Factors.”
Although we believe the expectations reflected in the forward-looking statements are reasonable, we cannot guarantee future results, level of activity, performance or achievements. We are under no duty to update any of these forward-looking statements after the date of this prospectus to conform our prior statements to actual results or revised expectations.
40
Table of Contents
THE REORGANIZATION OF OUR CORPORATE STRUCTURE
Overview
Health Insurance Innovations, Inc. was incorporated as a Delaware corporation on October 26, 2012. Immediately prior to the completion of this offering, we intend to amend and restate our certificate of incorporation to, among other things, authorize two classes of common stock, Class A common stock and Class B common stock, each having the terms described under “Description of Capital Stock.” Our Class A common stock will be issued to investors in this offering and will also be held by certain of our employees. Our Class B common stock will be held by Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC (a subsidiary of Health Plan Intermediaries, LLC that was formed on October 31, 2012 in connection with this offering), which are beneficially owned by our Chairman, President, and Chief Executive Officer, Mr. Kosloske. Shares of our Class B common stock vote together with shares of our Class A common stock as a single class, except as otherwise required by law. See “Description of Capital Stock—Class B Common Stock.” After completion of this offering, Mr. Kosloske will beneficially own 65% of our outstanding Class A and Class B common stock on a combined basis, which equals his combined economic interest in our company, and will have effective control over the outcome of votes on all matters requiring approval by our stockholders. As described in more detail below, each Series B Membership Interest can be exchanged (together with one share of Class B common stock) for one share of Class A common stock.
Health Insurance Innovations, Inc. was formed for purposes of this offering and has, to date, engaged only in activities in contemplation of this offering. Following this offering, Health Insurance Innovations, Inc. will be a holding company the principal asset of which will be Series A Membership Interests in Health Plan Intermediaries Holdings, LLC. Our business began operations in 2008, and historically, we operated through Health Plan Intermediaries, LLC. In anticipation of this offering, on November 7, 2012, Health Plan Intermediaries, LLC assigned the operating assets of our business through a series of transactions to Health Plan Intermediaries Holdings, LLC, and Health Plan Intermediaries Holdings, LLC assumed the operating liabilities of Health Plan Intermediaries, LLC.
There will be 4,666,667 shares of our Class A common stock outstanding after this offering. These shares will represent 100% of the economic rights of the holders of all classes of our common stock to share in our distributions.
41
Table of Contents
The diagram below shows our organizational structure immediately after completion of this offering and the reorganization described herein.
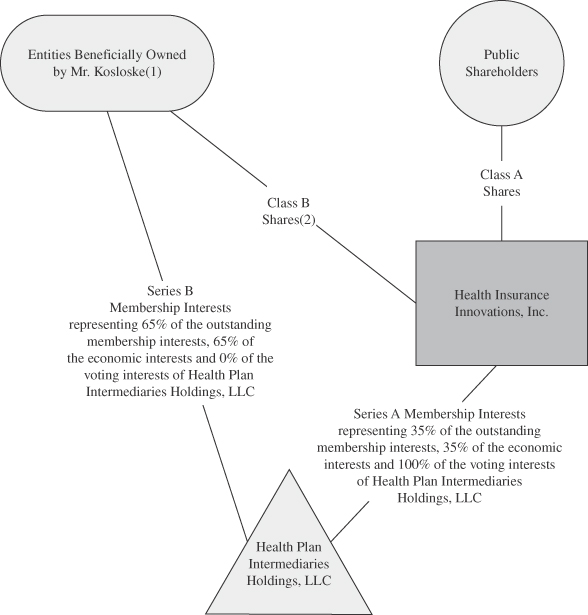
| (1) | The members of Health Plan Intermediaries Holdings, LLC, other than us, will include Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske. |
| (2) | Class B shares do not entitle their holders to any dividends paid by, or rights upon liquidation of, Health Insurance Innovations, Inc. Each share of our Class A common stock and our Class B common stock will entitle its holder to one vote. |
Pursuant to a registration rights agreement that we will enter into with Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, upon request we will use our best efforts to file a registration statement in order to register the resales of the shares of our Class A common stock that are issuable from time to time upon
42
Table of Contents
exchange of Series B Membership Interests (together with an equal number of shares of our Class B common stock) for shares of our Class A common stock. See “—Registration Rights Agreement.”
Holding Company Structure
Our only business after this offering will be to act as sole managing member of Health Plan Intermediaries Holdings, LLC. We will operate and control all of our businesses and affairs through Health Plan Intermediaries Holdings, LLC. Immediately prior to this offering, Health Plan Intermediaries Holdings, LLC’s limited liability company agreement will be amended and restated to, among other things, establish two classes of equity: Series A Membership Interests held by us and Series B Membership Interests held only by persons or entities we permit. The financial results of Health Plan Intermediaries Holdings, LLC and its consolidated subsidiaries will be consolidated in our financial statements.
Amended and Restated Limited Liability Company Agreement of Health Plan Intermediaries Holdings, LLC
Following our reorganization and this offering, we will operate our business through Health Plan Intermediaries Holdings, LLC and its consolidated subsidiaries. The operations of Health Plan Intermediaries Holdings, LLC, and the rights and obligations of its members, will be governed by the amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC, the form of which is filed as an exhibit to the registration statement of which this prospectus forms a part. The following is a description of the material terms of that amended and restated limited liability company agreement.
Governance
We will serve as sole managing member of Health Plan Intermediaries Holdings, LLC. As such, we will control its business and affairs and will be responsible for the management of its business. No other members of Health Plan Intermediaries Holdings, LLC, in their capacity as such, will have any authority or right to control the management of Health Plan Intermediaries Holdings, LLC or to bind it in connection with any matter.
Voting and Economic Rights of Members
Health Plan Intermediaries Holdings, LLC will have two series of outstanding equity: Series A Membership Interests, which may only be issued to Health Insurance Innovations, Inc., as sole managing member, and Series B Membership Interests. The Series B Membership Interests will be held by Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC (a subsidiary of Health Plan Intermediaries, LLC that was formed on October 31, 2012 in connection with this offering), entities beneficially owned by Mr. Kosloske. The Series A Membership Interests and Series B Membership Interests will entitle their holders to equivalent economic rights meaning an equal share in the profits and losses of, and distributions from, Health Plan Intermediaries Holdings, LLC. Holders of Series B Membership Interests will have no voting rights, except for the right to approve certain amendments to the amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC.
Net profits and losses of Health Plan Intermediaries Holdings, LLC generally will be allocated, and distributions made, to its members pro rata in accordance with the number of Membership Interests (Series A or Series B, as the case may be) they hold. Accordingly, net profits and net losses of Health Plan Intermediaries Holdings, LLC will initially be allocated, and distributions will be made, approximately 35% to us and approximately 65% to the holders of Series B Membership Interests (or 38% and 62%, respectively, if the underwriters exercise their over-allotment option in full).
Subject to the availability of net cash flow at the Health Plan Intermediaries Holdings, LLC level and to applicable legal and contractual restrictions, we intend to cause Health Plan Intermediaries Holdings, LLC to distribute to us, and to the other holders of Membership Interests, cash payments for the purposes of funding tax
43
Table of Contents
obligations in respect of any net taxable income that is allocated to us and the other holders of Membership Interests as members of Health Plan Intermediaries Holdings, LLC, to fund dividends, if any, declared by us and to make any payments due under the tax receivable agreement, as described below. See “—Tax Consequences.” If Health Plan Intermediaries Holdings, LLC makes distributions to its members in any given year, the determination to pay dividends, if any, to our Class A common stockholders will be made by our board of directors. We do not, however, expect to declare or pay any cash or other dividends in the foreseeable future on our Class A common stock, as we intend to reinvest any cash flow generated by operations in our business. Class B common stock will not be entitled to any dividend payments. We may enter into credit agreements or other borrowing arrangements in the future that prohibit or restrict our ability to declare or pay dividends on our Class A common stock.
Coordination of Health Insurance Innovations, Inc. and Health Plan Intermediaries Holdings, LLC
Except with respect to shares of Class A Common Stock issued pursuant to the exercise of the over-allotment option, whenever we issue one share of Class A common stock for cash, the net proceeds will be transferred promptly to Health Plan Intermediaries Holdings, LLC, and Health Plan Intermediaries Holdings, LLC will issue to us one Series A Membership Interest. If we issue other classes or series of equity securities, we will contribute to Health Plan Intermediaries Holdings, LLC the net proceeds we receive in connection with such issuance, and Health Plan Intermediaries Holdings, LLC will issue to us an equal number of equity securities with designations, preferences and other rights and terms that are substantially the same as our newly issued equity securities. Conversely, if we repurchase any shares of Class A common stock (or equity securities of other classes or series) for cash, Health Plan Intermediaries Holdings, LLC will, immediately prior to our repurchase, redeem an equal number of Series A Membership Interests (or its equity securities of the corresponding classes or series), upon the same terms and for the same price, as the shares of our Class A common stock (or our equity securities of such other classes or series) are repurchased. Membership Interests and shares of our common stock will be subject to equivalent stock splits, dividends and reclassifications.
We will not conduct any business other than the management and ownership of Health Plan Intermediaries Holdings, LLC and its subsidiaries, or own any other assets (other than on a temporary basis), although we may take such actions and own such assets as are necessary to comply with applicable law, including compliance with our responsibilities as a public company under the U.S. federal securities laws, and may incur indebtedness and may take other actions if we determine that doing so is in the best interest of Health Plan Intermediaries Holdings, LLC.
Issuances of Membership Interests
Series A Membership Interests may be issued only to us as the sole managing member of Health Plan Intermediaries Holdings, LLC. Series B Membership Interests may be issued only to persons or entities we permit, which initially will be Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske. Such issuances shall be in exchange for cash or other consideration. Series B Membership Interests may not be transferred as Series B Membership Interests except to certain permitted transferees and in accordance with the restrictions on transfer set forth in the amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC, and any such transfer must be accompanied by the transfer of an equal number of shares of our Class B common stock.
Exchange Agreement
We will enter into an exchange agreement with the existing and certain future holders of Series B Membership Interests. Pursuant to and subject to the terms of the exchange agreement and the amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC, holders of Series B Membership Interests, at any time and from time to time, may exchange one or more Series B Membership Interests, together with an equal number of shares of our Class B common stock, for shares of our Class A common stock on a one-for-one basis, subject to equitable adjustments for stock splits, stock dividends and reclassifications.
44
Table of Contents
Holders will not have the right to exchange Series B Membership Interests if we determine that such exchange would be prohibited by law or regulation or would violate other agreements to which we may be subject. We may impose additional restrictions on exchange that we determine necessary or advisable so that Health Plan Intermediaries Holdings, LLC is not treated as a “publicly traded partnership” for U.S. federal income tax purposes. If the Internal Revenue Service were to contend successfully that Health Plan Intermediaries Holdings, LLC should be treated as a “publicly traded partnership” for U.S. federal income tax purposes, Health Plan Intermediaries Holdings, LLC would be treated as a corporation for U.S. federal income tax purposes and thus would be subject to entity-level tax on its taxable income.
A holder that exchanges Series B Membership Interests will also be required to deliver an equal number of shares of our Class B common stock. In connection with each exchange, Health Plan Intermediaries Holdings, LLC will cancel the delivered Series B Membership Interests and issue to us Series A Membership Interests on a one-for-one basis. Thus, as holders exchange their Series B Membership Interests for Class A common stock, our interest in Health Plan Intermediaries Holdings, LLC will increase.
We and the exchanging holder will each generally bear our own expenses in connection with an exchange, except that, subject to a limited exception, we are required to pay any transfer taxes, stamp taxes or duties or other similar taxes in connection with such an exchange.
We have reserved for issuance 8,666,667 shares of our Class A common stock for potential exchange in the future for Series B Members Interests, which is the aggregate number of Series B Membership Interests to be outstanding after completion of the reorganization and this offering (assuming no exercise of the underwriters’ over-allotment option).
Exculpation and Indemnification
The amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC contains provisions limiting the liability of its managing member, members, officers and their respective affiliates to Health Plan Intermediaries Holdings, LLC or any of its members. Moreover, the amended and restated limited liability company agreement contains broad indemnification provisions for Health Plan Intermediaries Holdings, LLC’s managing member, members, officers and their respective affiliates. Because Health Plan Intermediaries Holdings, LLC is a limited liability company, these provisions are not subject to the limitations on exculpation and indemnification contained in the Delaware General Corporation Law with respect to the indemnification that may be provided by a Delaware corporation to its directors and officers.
Voting Rights of Class A Stockholders and Class B Stockholders
Each share of our Class A common stock and our Class B common stock will entitle its holder to one vote. Immediately after this offering, our Class B stockholders will collectively hold approximately 65% of the total voting power (and, through the equal number of Series B Membership Interests, economic interests in Health Plan Intermediaries Holdings, LLC) of our common stock (or 62% if the underwriters exercise their over-allotment option in full).
Tax Consequences
Holders of Membership Interests, including Health Insurance Innovations, Inc., generally will incur U.S. federal, state and local income taxes on their proportionate shares of any net taxable income of Health Plan Intermediaries Holdings, LLC. Net profits and net losses of Health Plan Intermediaries Holdings, LLC generally will be allocated to its members pro rata in proportion to the number of Membership Interests they hold. The amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC provides for cash distributions to its members in an amount at least equal to the members’ assumed tax liability attributable to Health Plan Intermediaries Holdings, LLC. Generally, distributions in respect of the members’
45
Table of Contents
assumed tax liability will be computed based on our estimate of the net taxable income of Health Plan Intermediaries Holdings, LLC allocable per Membership Interest multiplied by an assumed tax rate. In accordance with this agreement, Health Plan Intermediaries Holdings, LLC intends to make distributions to its members in respect of such assumed tax liability and to fund dividends, if any, declared by us, as well as any payments we are obligated to make under the tax receivable agreement, described below.
Health Plan Intermediaries Holdings, LLC intends to make an election under Section 754 of the Internal Revenue Code of 1986, as amended, which is effective for 2013 and for each taxable year in which occurs an exchange of Series B Membership Interests, together with an equal number of shares of our Class B common stock, for shares of our Class A common stock. We expect that, as a result of this election, the acquisition of Series B Membership Interests from Health Plan Intermediaries, LLC with the net proceeds of the sale of any over-allotment shares, as well as any future exchanges of Series B Membership Interests, together with an equal number of shares of our Class B common stock, for shares of our Class A common stock, will result in increases in the tax basis in our share of the tangible and intangible assets of Health Plan Intermediaries Holdings, LLC at the time of such acquisition or exchange, which will increase the tax depreciation and amortization deductions available to us and which could create other tax benefits. Any such increases in tax basis and tax depreciation and amortization deductions or other tax benefits could reduce the amount of tax that we would otherwise be required to pay in the future. We will be required to pay a portion of the cash savings we actually realize from such increase (or are deemed to realize in the case of an early termination payment by us, a change in control or a material breach by us of our obligations under the tax receivable agreement, as described below) to certain holders of Series B Membership Interests pursuant to the tax receivable agreement. Furthermore, payments under the tax receivable agreement, as described below, will give rise to additional tax benefits and therefore to additional payments under the tax receivable agreement itself. To the extent that we are unable to make payments under the income tax receivable agreement for any reason, such payments will be deferred and will accrue interest until paid. See “—Tax Receivable Agreement” below.
Tax Receivable Agreement
Assuming the underwriters do not exercise their over-allotment option, this offering is not anticipated to result in an increase in the tax basis in our share of the tangible and intangible assets of Health Plan Intermediaries Holdings, LLC. However, the purchase of Series B Membership Interests (together with an equal number of shares of our Class B common stock) with the net proceeds of the sale of any over-allotment shares, as well as subsequent exchanges of Series B Membership Interests, together with an equal number of shares of our Class B common stock, for shares of our Class A common stock, are expected to increase our tax basis in our share of Health Plan Intermediaries Holdings, LLC’s tangible and intangible assets. These increases in tax basis are expected to increase our depreciation and amortization deductions and create other tax benefits and therefore may reduce the amount of tax that we would otherwise be required to pay in the future.
After giving effect to the reorganization, we will enter into a tax receivable agreement with the existing and certain future holders of Series B Membership Interests (currently Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske). The agreement will require us to pay to such holders 85% of the cash savings, if any, in U.S. federal, state and local income tax we realize (or are deemed to realize in the case of an early termination payment, a change in control or a material breach by us of our obligations under the tax receivable agreement, as discussed below) as a result of any possible future increases in tax basis described above and of certain other tax benefits related to entering into the tax receivable agreement, including tax benefits attributable to payments under the tax receivable agreement itself. This will be our obligation and not an obligation of Health Plan Intermediaries Holdings, LLC. We will benefit from the remaining 15% of any realized cash savings. For purposes of the tax receivable agreement, cash savings in income tax will be computed by comparing our actual income tax liability with our hypothetical liability had we not been able to utilize the tax benefits subject to the tax receivable agreement itself. The tax receivable agreement will become effective upon completion of this offering and will remain in effect until all such tax benefits have been used or expired, unless the agreement is terminated early, as described below. Estimating the
46
Table of Contents
amount of payments to be made under the tax receivable agreement cannot be done reliably at this time because any increase in tax basis, as well as the amount and timing of any payments under the tax receivable agreement, will vary depending on a number of factors, including:
| • | the timing of exchanges of Series B Membership Interests (together with an equal number of shares of our Class B common stock) for shares of our Class A common stock—for instance, the increase in any tax deductions will vary depending on the fair market value of the depreciable and amortizable assets of Health Plan Intermediaries Holdings, LLC at the time of the exchanges, and this value may fluctuate over time; |
| • | the price of our Class A common stock at the time of exchanges of Series B Membership Interests (together with an equal number of shares of our Class B common stock) for shares of our Class A common stock—the increase in our share of the basis in the assets of Health Plan Intermediaries Holdings, LLC, as well as the increase in any tax deductions, will be related to the price of our Class A common stock at the time of these exchanges; |
| • | the tax rates in effect at the time we use the increased amortization and depreciation deductions or realize other tax benefits; and |
| • | the amount, character and timing of our taxable income. We will be required to pay 85% of the tax savings, as and if realized. Except in certain circumstances, if we do not have taxable income in a given taxable year, we will not be required to make payments under the tax receivable agreement for that taxable year because no tax savings will have been realized. |
The payments that we make under the tax receivable agreement could be substantial. Assuming no material changes in relevant tax law and based on our current operating plan and other assumptions, including our estimate of the tax basis of our assets as of September 30, 2012, if all of the Series B Membership Interests were acquired by us in taxable transactions at the time of the closing of this offering for a price of $15 (the midpoint of the range on the cover of this prospectus) per Series B Membership Interest, we estimate that the maximum amount that we would be required to pay under the tax receivable agreement could be approximately $57,126,000. The actual amount may differ materially from this hypothetical amount as potential future payments will vary depending on a number of factors, including those listed above.
We will have the right to terminate the tax receivable agreement at any time. In addition, the tax receivable agreement will terminate early if we (or our successors) breach our obligations under the tax receivable agreement or upon certain mergers, asset sales, other forms of business combinations or other changes of control. If we exercise our right to terminate the tax receivable agreement, or if the tax receivable agreement is terminated early in accordance with its terms, our (or our successors’) payment obligations under the tax receivable agreement with respect to certain exchanged or acquired Membership Interests would be accelerated and would become due and payable based on certain assumptions, including that we would have sufficient taxable income to use in full the deductions arising from the increased tax basis and certain other benefits. As a result, we could make payments under the tax receivable agreement that are substantial and in excess of our actual cash savings in income tax.
Decisions made in the course of running our business, such as with respect to mergers, asset sales, other forms of business combinations or other changes in control, may influence the timing and amount of payments we make under the tax receivable agreement. For example, the earlier disposition of assets following an exchange or acquisition transaction will generally accelerate payments under the tax receivable agreement and increase the present value of such payments. In these situations, our obligations under the tax receivable agreement could have a substantial negative impact on our liquidity and could have the effect of delaying, deferring or preventing certain mergers, asset sales, other forms of business combinations or other changes of control.
Payments are generally due under the tax receivable agreement within a specified period of time following the filing of our tax return for the taxable year with respect to which the payment obligation arises, although interest on such payments will begin to accrue at a rate of LIBOR from the due date (without extensions) of such tax return. Late payments generally accrue interest at a rate of LIBOR plus 300 basis points. However, to the extent, based on certain specified reasons, that we do not have available cash to satisfy our payment obligations under the tax receivable agreement, such deferred payments would accrue interest at a rate of LIBOR.
47
Table of Contents
Were the Internal Revenue Service to challenge successfully the tax basis increases described above, we would not be reimbursed for any payments previously made under the tax receivable agreement although future payments under the tax receivable agreement, if any, would be adjusted to reflect the result of any such successful challenge by the Internal Revenue Service. As a result, we could make payments under the tax receivable agreement in excess of our actual cash savings in income tax.
Registration Rights Agreement
We will enter into a registration rights agreement with Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske, to register for sale under the Securities Act shares of our Class A common stock delivered in exchange for Series B Membership Interests in the circumstances described below. This agreement will provide these two entities (and their affiliates) with the right to require us, at our expense, to register shares of our Class A common stock that are issuable upon exchange of Series B Membership Interests (and an equal number of shares of our Class B common stock) for shares of our Class A common stock. The agreement will also provide that we will pay certain expenses of Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC (and their affiliates) relating to such registrations and indemnify them against certain liabilities, which may arise under the Securities Act. The following description summarizes such rights and circumstances following our reorganization as a corporation.
Demand Rights
Subject to certain limitations, at any time after completion of this offering, Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC (and their affiliates) will have the right, by delivering written notice to us, to require us to register the number of our shares of Class A common stock requested to be so registered in accordance with the registration rights agreement. Within 10 days of receipt of notice of a demand registration, we will be required to give written notice to all other holders of registrable shares of Class A common stock. Subject to certain limitations as described below, we will include in the registration all securities with respect to which we receive a written request for inclusion in the registration within 10 days after we give our notice.
Piggyback Rights
Any holder of registrable shares of Class A common stock will be entitled to request to participate in, or “piggyback” on, registrations of any of our securities for sale by us at any time after this offering. This piggyback right will apply to any registration following this offering other than a demand registration described above, a registration on Form S-4 or S-8 or a registration solely in connection with an exchange offer or any employee benefit or dividend reinvestment plan.
Conditions and Limitations
The registration rights outlined above will be subject to conditions and limitations, including the right of the underwriters to limit the number of shares to be included in a registration statement and our right to delay, suspend or withdraw a registration statement under specified circumstances. For example, our board may, in its good faith judgment, defer any filing for up to 75 days (which deferral may not be used more than once in any 12-month period). Furthermore, our board may, in its good faith judgment, suspend a registration on Form S-3 (which suspension may not be more than an aggregate of 90 days in any 12-month period), for such period of time as is reasonably necessary not in excess of 75 days. Additionally, in certain circumstances we may withdraw a registration upon request by the holder of registrable securities.
If requested by the managing underwriter or underwriters, holders of securities with registration rights will not be able to make any sale of our equity securities (including sales under Rule 144) or give any demand notice during a period commencing on the date of the request and continuing for a period not to exceed 90 days (with respect to any underwritten public offering, other than this offering, made prior to the second anniversary of this offering, and thereafter 60 days rather than 90 days) or such shorter period as may be requested by the underwriters. The managing underwriters for the relevant offering may agree to shorten this period.
48
Table of Contents
We estimate that the net proceeds to us from this offering will be approximately $63,100,000, or approximately $72,865,000 if the underwriters exercise their over-allotment option in full, assuming an initial public offering price of $15 per share (the midpoint of the range set forth on the cover page of this prospectus), after deducting estimated underwriting discounts and commissions and estimated offering expenses payable by us. Each $1 increase (decrease) in the public offering price per share would increase (decrease) our net proceeds, after deducting estimated underwriting discounts and commissions and estimated offering expenses payable by us, by $326,667 (assuming no exercise of the underwriters’ over-allotment option).
We intend to use $3,490,000 of the net proceeds of this offering to repay all of the outstanding debt under our term loan and up to $25,000,000 to provide the funds necessary to expand our advance commission structure. Any remaining net proceeds will be used for general corporate purposes, including potential acquisitions that are complementary to our business or that enable us to enter new markets or provide new products or services. If the underwriters exercise their over-allotment option, we intend to use the net proceeds from the sale of such shares to acquire Series B Membership Interests, together with an equal number of shares of our Class B common stock, from Health Plan Intermediaries, LLC, which is controlled by Mr. Kosloske (which Series B Membership Interests will immediately be recapitalized into Series A Membership Interests). We are not currently a party to any agreements or commitments for any such acquisitions, and we have no current understandings with respect to any such transactions.
The term loan bears fixed interest at 5.25% and will mature after a term of five years on September 27, 2016. The purpose of the term loan was to finance the acquisition of the 50% interest in Health Plan Intermediaries, LLC owned by Naylor Group Partners, LLC. See “Management’s Discussion and Analysis of Financial Condition and Results of Operations—Liquidity and Capital Resources.”
We currently anticipate that we will retain all available funds for use in the operation and expansion of our business, and do not anticipate paying any cash dividends in the foreseeable future. Class B common stock will not be entitled to any dividend payments.
49
Table of Contents
The following table sets forth the cash and capitalization as of September 30, 2012 of:
| • | Health Plan Intermediaries, LLC on an actual basis; |
| • | Health Insurance Innovations, Inc. on a pro forma basis to give effect to the reorganization transactions described under “The Reorganization of Our Corporate Structure;” and |
| • | Health Insurance Innovations, Inc. on a pro forma as adjusted basis to give further effect to the issuance and sale of 4,666,667 shares of Class A common stock by us in the offering at an assumed initial public offering price of $15 per share, the midpoint of the range set forth on the cover page of this prospectus, and the application of the net proceeds of the offering, after deducting estimated underwriting discounts and commissions and offering expenses payable by us, as set forth under “Use of Proceeds.” Each $1 increase (decrease) in the public offering price per share would increase (decrease) our total stockholders’ equity and total capitalization by $326,667 (assuming no exercise of the underwriters’ over-allotment option), after deducting estimated underwriting discounts and commissions and estimated offering expenses payable by us. |
This table should be read in conjunction with “The Reorganization of Our Corporate Structure,” “Unaudited Pro Forma Financial Information,” “Selected Historical Financial and Operational Data,” “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and the financial statements and notes thereto appearing elsewhere in this prospectus.
| As of September 30, 2012 | ||||||||||||
| Health Plan Intermediaries, LLC Actual |
Pro Forma |
Pro Forma As Adjusted |
||||||||||
| (unaudited) (in thousands) |
||||||||||||
| Cash |
$ | 982 | $ | 982 | $ | 61,455 | ||||||
|
|
|
|
|
|
|
|||||||
| Total debt |
$ | 3,490 | $ | 3,490 | $ | — | ||||||
|
|
|
|
|
|
|
|||||||
| Member’s/stockholders’ equity: |
||||||||||||
| Member’s equity |
6,882 | — | — | |||||||||
| Class A common stock, $0.001 par value per share, 100,000,000 shares authorized, no shares outstanding actual, 4,666,667 shares outstanding pro forma and 4,666,667 shares outstanding pro forma as adjusted; |
— | — | 5 | |||||||||
| Class B common stock, $0.001 par value per share, 20,000,000 shares authorized, no shares outstanding actual, 8,666,667 shares outstanding pro forma and 8,666,667 shares outstanding pro forma as adjusted; |
— | 9 | 9 | |||||||||
| Preferred stock, $0.001 par value per share, 5,000,000 shares authorized, no shares outstanding actual, no shares outstanding pro forma and no shares outstanding pro forma as adjusted |
— | — | — | |||||||||
| Additional paid in capital |
— | 1,282 | 23,419 | |||||||||
| Accumulated earnings (loss) |
— | 1,113 | 1,026 | |||||||||
| Non-controlling interest |
(13 | ) | 4,465 | 45,423 | ||||||||
|
|
|
|
|
|
|
|||||||
| Total member’s/stockholders’ equity |
6,869 | 6,869 | 69,882 | |||||||||
|
|
|
|
|
|
|
|||||||
| Total capitalization |
$ | 10,359 | $ | 10,359 | $ | 69,882 | ||||||
|
|
|
|
|
|
|
|||||||
50
Table of Contents
After giving pro forma effect to our corporate reorganization described under “The Reorganization of Our Corporate Structure,” our pro forma net tangible book value as of September 30, 2012 was $(3,221,000) or $(0.37) per share of our Class A and Class B common stock. Pro forma net tangible book value per share represents the amount of our total tangible assets, less the amount of our total liabilities, divided by the aggregate number of shares of Class A and Class B common stock outstanding. After giving pro forma effect to the reorganization, the sale by us of the shares of Class A common stock in this offering, at an assumed initial public offering price of $15 per share, the midpoint of the range set forth on the cover page of this prospectus after deducting estimated underwriting discounts and commissions and estimated offering expenses payable by us, the receipt and application of the net proceeds and assuming all Series B Membership Interests, together with an equal number of shares of our Class B common stock, are exchanged for an equal number of shares of Class A common stock, our pro forma net tangible book value as of September 30, 2012 would have been $59,792,000 or $4.49 per share. This represents an immediate increase in pro forma net tangible book value to existing stockholders of $4.86 per share and an immediate dilution to new investors of $10.51 per share. Dilution per share represents the difference between the price per share to be paid by new investors for the shares of Class A common stock sold in this offering and the pro forma net tangible book value per share immediately after this offering. The following table illustrates this per share dilution:
| Assumed initial public offering price per share |
$ | 15 | ||||||
| Pro forma net tangible book value per share as of September 30, 2012 |
$ | (0.37 | ) | |||||
| Increase in pro forma net tangible book value per share attributable to new investors |
4.86 | |||||||
|
|
|
|||||||
| Adjusted pro forma net tangible book value per share after offering |
4.49 | |||||||
|
|
|
|||||||
| Dilution per share to new investors |
$ | 10.51 | ||||||
|
|
|
The following table sets forth, on a pro forma basis after giving pro forma effect to the reorganization, as of September 30, 2012, the number of shares of Class A common stock purchased from us, the total consideration paid, or to be paid, and the average price per share paid, or to be paid, by existing stockholders and by the new investors, assuming all Series B Membership Interests, together with an equal number of our Class B common shares, are exchanged for an equal number of shares of Class A common stock, at an assumed initial public offering price of $15 per share, the midpoint of the range set forth on the cover page of this prospectus, before deducting estimated underwriting discounts and commissions and offering expenses payable by us:
| Shares Purchased | Total Consideration | Average Price Per Share |
||||||||||||||||||
| Number | Percent | Amount | Percent | |||||||||||||||||
| Existing stockholders |
8,666,667 | 65 | % | $ | 3,689,000 | 5.0 | % | $ | 0.43 | |||||||||||
| New investors |
4,666,667 | 35 | 70,000,000 | 95.0 | % | 15.00 | ||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total |
13,333,334 | 100 | % | $ | 73,689,000 | 100 | % | $ | 5.53 | |||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
The foregoing tables assume no exercise of the underwriters’ over-allotment option.
51
Table of Contents
UNAUDITED PRO FORMA FINANCIAL INFORMATION
The following unaudited pro forma consolidated statements of operations for the year ended December 31, 2011 and the nine months ended September 30, 2012 and the unaudited pro forma consolidated balance sheet as of September 30, 2012 present our consolidated results of operations and financial position to give pro forma effect to the reorganization transactions described in “The Reorganization of Our Corporate Structure” and the sale of shares in this offering (excluding shares issuable upon any exercise of the underwriters’ over-allotment option) and the application of the net proceeds from this offering as if all such transactions had been completed as of January 1, 2011 with respect to the unaudited consolidated pro forma statement of operations data and as of September 30, 2012 with respect to the unaudited pro forma consolidated balance sheet data. The unaudited pro forma consolidated financial statements reflect pro forma adjustments that are described in the accompanying notes and are based on available information and certain assumptions we believe are reasonable, but are subject to change. We have made, in our opinion, all adjustments that are necessary to present fairly the pro forma financial data.
The unaudited pro forma financial information should be read together with “The Reorganization of Our Corporate Structure,” “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and the historical financial statements and related notes included elsewhere in this prospectus.
The pro forma adjustments principally give effect to:
| • | the reorganization transactions described in “The Reorganization of Our Corporate Structure,” including (i) the issuance by Health Plan Intermediaries Holdings, LLC of Series A membership interests to Health Insurance Innovations, Inc. pursuant to the Third Amended and Restated Limited Liability Company Agreement of Health Plan Intermediaries Holdings, LLC, (ii) the consolidation of Health Plan Intermediaries Holdings, LLC and its consolidated subsidiaries into Health Insurance Innovations, Inc.’s financial statements pursuant to ASC 810 and the resulting increase of additional paid-in-capital to allocate a portion of Health Plan Intermediaries Holdings, LLC’s equity to the non-controlling interest, (iii) the conversion of each share of Health Insurance Innovations, Inc.’s outstanding common stock into 86,667.67 shares of Class B common stock pursuant to Health Insurance Innovations, Inc.’s Amended and Restated Certificate of Incorporation and (iv) the issuance of shares of Class A common stock of Health Insurance Innovations, Inc. in connection with this offering; |
| • | with regard to the unaudited pro forma consolidated statements of operations, a provision for corporate income taxes on the income attributable to Health Insurance Innovations, Inc. at an effective rate of 38.0%, which includes a provision for U.S. Federal income taxes and assumes the highest statutory rates apportioned to each state, local and /or foreign jurisdiction; |
| • | the grant to Michael D. Hershberger, our Chief Financial Officer, of restricted stock in connection with this offering; and |
| • | the application of a portion of the proceeds from this offering to repay outstanding indebtedness, as described in “Use of Proceeds.” |
This offering and the reorganization transactions will not result in an immediate step-up in the tax basis in our share of the tangible and intangible assets of Health Plan Intermediaries Holdings, LLC. However, future purchases or exchanges of Series B Membership Interests, together with an equal number of shares of our Class B common stock, for shares of our Class A common stock are expected to increase the tax basis in our share of the tangible and intangible assets of Health Plan Intermediaries Holdings, LLC. The step-up in tax basis would be initially depreciable and amortizable for tax purposes over a period of approximately 15 years. We will enter into a tax receivable agreement with the holders of Series B Membership Interests after giving effect to the reorganization and certain future holders of Series B Membership Interests that will require us to pay such
52
Table of Contents
holders 85% of the amount of cash savings, if any, in U.S. federal, state and local income tax that we actually realize (or are deemed to realize in the case of an early termination payment, a change in control or a material breach by us of our obligations under the tax receivable agreement) as a result of the increases in tax basis and of certain other tax benefits related to entering into the tax receivable agreement, including tax benefits attributable to payments under the tax receivable agreement. Assuming all Series B Membership Interests of Health Plan Intermediaries Holdings, LLC beneficially owned by Mr. Kosloske were acquired by us in a taxable transaction as of the date of this offering, the step-up in the tax basis in our share of the tangible and intangible assets and the resulting estimated maximum payment due under the tax receivable agreement would be $174,947,000 and $57,126,000, respectively, based on our estimate of the tax basis in Health Plan Intermediaries Holdings, LLC’s assets as of September 30, 2012. We are not currently a party to any other agreements or commitments for any such acquisitions, and we have no current understandings with respect to any other such transactions. The actual amount of the tax receivable payment may materially differ from this hypothetical amount, as potential future payments will be calculated using the market value of our Class A common stock at the time of relevant exchange and prevailing tax rates in future years and will be dependent on us generating sufficient future taxable income to realize the benefit. Payments are generally due under the tax receivable agreement within a specified period of time following the filing of our tax return for the taxable year with respect to which the payment obligation arises, although interest on such payments will begin to accrue at a rate of LIBOR from the due date (without extensions) of such tax return. Late payments generally accrue interest at a rate of LIBOR plus 300 basis points. However, to the extent, based on certain specified reasons, that we do not have available cash to satisfy our payment obligations under the tax receivable agreement, such deferred payments would accrue interest at a rate of LIBOR.
The unaudited pro forma financial data are presented for informational purposes only and should not be considered indicative of actual results of operations that would have been achieved had the reorganization transactions and this offering been consummated on the dates indicated, and do not purport to be indicative of statements of financial condition or results of operations as of any future date or any future period.
53
Table of Contents
HEALTH INSURANCE INNOVATIONS, INC.
Unaudited Pro Forma Consolidated Balance Sheet
As of September 30, 2012
(in thousands)
| Health Plan Intermediaries, LLC Historical(1) |
Reorganization Adjustments |
Health Insurance Innovations, Inc. (2) Pro Forma |
Offering Adjustments |
Health Insurance Innovations, Inc. (2) Pro Forma as Adjusted |
||||||||||||||||
| Assets |
||||||||||||||||||||
| Current assets: |
||||||||||||||||||||
| Cash |
$ | 982 | — | $ | 982 | $ | 60,473 | (4) | $ | 61,455 | ||||||||||
| Cash held on behalf of others |
3,571 | — | 3,571 | — | 3,571 | |||||||||||||||
| Credit card transactions receivable |
138 | — | 138 | — | 138 | |||||||||||||||
| Credit card transactions receivable for others |
846 | — | 846 | — | 846 | |||||||||||||||
| Accounts receivable |
315 | — | 315 | — | 315 | |||||||||||||||
| Notes receivable |
95 | — | 95 | — | 95 | |||||||||||||||
| Advanced commissions |
300 | — | 300 | — | 300 | |||||||||||||||
| Prepaid expenses |
27 | — | 27 | — | 27 | |||||||||||||||
| Gateway processor deposit |
— | — | — | — | — | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total current assets |
6,274 | — | 6,274 | 60,473 | 66,747 | |||||||||||||||
| Property and equipment, net of accumulated depreciation |
207 | — | 207 | — | 207 | |||||||||||||||
| Accounts receivable |
— | — | — | — | — | |||||||||||||||
| Deferred financing costs, net |
87 | — | 87 | (87 | )(4) | — | ||||||||||||||
| Capitalized offering costs |
863 | — | 863 | (863 | )(4) | — | ||||||||||||||
| Deposits |
21 | — | 21 | — | 21 | |||||||||||||||
| Goodwill |
5,906 | — | 5,906 | — | 5,906 | |||||||||||||||
| Intangible assets, net of accumulated amortization |
4,184 | — | 4,184 | — | 4,184 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total assets |
$ | 17,542 | $ | — | $ | 17,542 | $ | 59,523 | $ | 77,065 | ||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Liabilities and member’s equity |
||||||||||||||||||||
| Current liabilities: |
||||||||||||||||||||
| Accounts payable and accrued expenses |
$ | 1,540 | — | $ | 1,540 | $ | — | $ | 1,540 | |||||||||||
| Carriers and vendors payable |
2,976 | — | 2,976 | — | 2,976 | |||||||||||||||
| Commissions payable |
1,441 | — | 1,441 | — | 1,441 | |||||||||||||||
| Unearned commissions |
197 | — | 197 | — | 197 | |||||||||||||||
| Notes payable |
110 | — | 110 | — | 110 | |||||||||||||||
| Deferred rent |
14 | — | 14 | — | 14 | |||||||||||||||
| Deferred other income |
8 | — | 8 | — | 8 | |||||||||||||||
| Current portion of long-term debt |
802 | — | 802 | (802 | )(4) | — | ||||||||||||||
| Current portion of noncompete obligation |
177 | — | 177 | — | 177 | |||||||||||||||
| Current portion of capital leases |
2 | — | 2 | — | 2 | |||||||||||||||
| Due to member |
— | — | — | — | — | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total current liabilities |
7,267 | — | 7,267 | (802 | ) | 6,465 | ||||||||||||||
| Capital lease obligations, less current portion |
5 | — | 5 | — | 5 | |||||||||||||||
| Long-term debt, less current portion |
2,688 | — | 2,688 | (2,688 | )(4) | — | ||||||||||||||
| Noncompete obligation |
665 | — | 665 | — | 665 | |||||||||||||||
| Deferred rent |
48 | — | 48 | — | 48 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total liabilities |
10,673 | — | 10,673 | (3,490 | ) | 7,183 | ||||||||||||||
| Member’s equity |
6,882 | (6,882 | )(3) | — | — | — | ||||||||||||||
| Class A par value |
— | — | — | 5 | (5) | 5 | ||||||||||||||
| Class B par value |
— | 9 | (3) | 9 | — | 9 | ||||||||||||||
| Additional Paid in Capital |
— | 1,282 | (3) | 1,282 | 22,137 | (5) | 23,419 | |||||||||||||
| Accumulated Earnings |
— | 1,113 | (3) | 1,113 | (87 | )(5) | 1,026 | |||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total equity attributable to Health Insurance Innovations, Inc. |
6,882 | (4,478 | ) | 2,404 | 22,055 | 24,459 | ||||||||||||||
| Non-controlling interest |
(13 | ) | 4,478 | 4,465 | 40,958 | (5) | 45,423 | |||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total liabilities and equity |
$ | 17,542 | $ | — | $ | 17,542 | $ | 59,523 | $ | 77,065 | ||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| (1) | We have historically operated our business through Health Plan Intermediaries, LLC. As of September 30, 2012, Health Plan Intermediaries, LLC held all of our assets and liabilities and Health Plan Intermediaries Holdings, LLC did not have |
54
Table of Contents
| assets or liabilities and did not conduct operations. Accordingly, the unaudited pro forma consolidated statements of operations for the year ended December 31, 2011 and the nine months ended September 30, 2012 and the unaudited pro forma consolidated balance sheet as of September 30, 2012 present the historical results of Health Plan Intermediaries, LLC as a starting point for the pro forma amounts. On November 7, 2012, Health Plan Intermediaries, LLC assigned all of the operating assets of its business through a series of transactions to Health Plan Intermediaries Holdings, LLC, and Health Plan Intermediaries Holdings, LLC assumed the operating liabilities of Health Plan Intermediaries, LLC and began conducting operations. As a result, Health Plan Intermediaries Holdings, LLC currently operates all of our business. Pursuant to ASC 805-50-45, we assessed whether any pro forma adjustments in connection with the assignment were necessary. First, we concluded that Health Plan Intermediaries, LLC and Health Plan Intermediaries Holdings, LLC were under common control at the time of the assignment. In addition, after eliminating the effects of intra-entity transactions, the results of operations of the entities before and after the assignment were substantially the same. Accordingly, we determined that the transactions did not result in any pro forma effect. |
| (2) | As a newly formed entity, Health Insurance Innovations, Inc. will have no assets or results of operations until the completion of this offering. |
| (3) | Represents adjustments to reflect (i) the portion of Health Plan Intermediaries Holdings, LLC’s accumulated earnings that Health Insurance Innovations, Inc. received in connection with the conversion of the existing shares of common stock of Health Insurance Innovations, Inc. into shares of Class B common stock and (ii) the related additional amount paid in capital resulting from the transaction. |
| As described in “The Reorganization of Our Corporate Structure,” after this offering, assuming the underwriters do not exercise their over-allotment option, and the reorganization transactions that we are undertaking in connection therewith, our only material asset will be the ownership of approximately 35% of the Membership Interests in Health Plan Intermediaries Holdings, LLC and our only business will be to act as the sole managing member of Health Plan Intermediaries Holdings, LLC. Accordingly, pursuant to ASC 810, we will consolidate the financial results of Health Plan Intermediaries Holdings, LLC into our financial statements. |
| Under ASC 810, Health Plan Intermediaries Holdings, LLC meets the definition of a variable interest entity. Further, Health Insurance Innovations, Inc. is the primary beneficiary of Health Plan Intermediaries Holdings, LLC as a result of its 100% voting power and control over Health Plan Intermediaries Holdings, LLC and as a result of its obligation to absorb losses and its right to receive benefits of Health Plan Intermediaries Holdings, LLC that could potentially be significant to Health Plan Intermediaries Holdings, LLC. As a result, Health Insurance Innovations, Inc. will consolidate the financial results of Health Plan Intermediaries Holdings, LLC and record a non-controlling interest for the economic interest in Health Plan Intermediaries Holdings, LLC held by the existing members to the extent that the book value of their interest in Health Plan Intermediaries Holdings, LLC is greater than zero. Health Insurance Innovations, Inc.’s and the non-controlling membership pro forma economic interest in Health Plan Intermediaries Holdings, LLC are 35% and 65%, respectively, as of September 30, 2012. Pro forma net income attributable to the non-controlling interest on the statements of operations represents the portion of earnings or loss attributable to the economic interest in Health Plan Intermediaries Holdings, LLC held by the non-controlling members. Non-controlling interest on the balance sheet represents the portion of net assets of Health Plan Intermediaries Holdings, LLC attributable to the non-controlling members based on total membership interest of Health Plan Intermediaries Holdings, LLC owned by such member. |
| (4) | We expect to receive net proceeds from this offering of $60,473,000 based on an aggregate underwriting discount of $4,900,000 and estimated offering expenses of $2,000,000. We intend to use $3,490,000 of the net proceeds of this offering to repay all of the outstanding debt under our term loan and our revolving credit facility, which we intend to terminate immediately following the completion of this offering. The following table reconciles the gross proceeds from this offering to the net cash provided to Health Insurance Innovations, Inc. ($ in thousands): |
| Assumed share price |
$ | 15 | ||
| Class A shares offered hereby |
4,666,667 | |||
|
|
|
|||
| Gross proceeds from offering |
70,000 | |||
| Offering costs |
(6,900 | ) | ||
| Offering costs already incurred |
863 | |||
| Debt repayment |
(3,490 | ) | ||
|
|
|
|||
| Net cash provided |
$ | 60,473 |
55
Table of Contents
| (5) | Represents adjustments to reflect the allocation of offering proceeds between controlling and non-controlling membership interests. |
| A $1.00 increase (decrease) in the assumed initial public offering price of $15 per share, the mid-point of the range on the front cover of this prospectus, would increase (decrease) each of the pro forma as adjusted cash and cash equivalents and stockholders’ equity by $326,667, after deducting estimated underwriting discounts and commissions and estimated offering expenses. The pro forma as adjusted information discussed above is illustrative only and following completion of this offering will be adjusted based on the actual offering price and other terms of this offering determined at pricing. |
56
Table of Contents
HEALTH INSURANCE INNOVATIONS, INC.
Unaudited Pro Forma Statements of Operations
Year Ended December 31, 2011
(in thousands)
| Historical(1) | ||||||||||||||||||||||||||
| Three Months Ended December 31, 2011 (Successor) |
Nine Months Ended September 30, 2011 (Predecessor) |
Reorganization Adjustments |
Health Insurance Innovations, Inc.(2) Pro Forma |
Offering Adjustments |
Health Insurance Innovations, Inc.(2) Pro Forma as Adjusted |
|||||||||||||||||||||
| Revenue |
$ | 8,090 | $ | 21,788 | — | $ | 29,878 | — | $ | 29,878 | ||||||||||||||||
| Third-party commissions |
5,601 | 16,103 | — | 21,704 | — | 21,704 | ||||||||||||||||||||
| Credit cards and ACH fees |
197 | 473 | — | 670 | — | 670 | ||||||||||||||||||||
| General and administrative expenses |
1,421 | 3,341 | — | 4,762 | 3,736 | (3) | 8,498 | |||||||||||||||||||
| Depreciation and amortization |
269 | 29 | — | 298 | — | 298 | ||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Total operating costs and expenses |
7,488 | 19,946 | — | 27,434 | 3,736 | 31,170 | ||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Income (loss) from operations |
602 | 1,842 | — | 2,444 | (3,736 | ) | (1,292 | ) | ||||||||||||||||||
| Other expenses (income): |
||||||||||||||||||||||||||
| Interest expense |
71 | — | — | 71 | (71 | )(4) | — | |||||||||||||||||||
| Interest income |
— | — | — | — | — | — | ||||||||||||||||||||
| Other |
— | — | — | — | — | — | ||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Pre tax income (loss) |
531 | 1,842 | — | 2,373 | (3,665 | ) | (1,292 | ) | ||||||||||||||||||
| Income tax |
— | — | 897 | (5) | 897 | (1,331 | )(6) | (434 | ) | |||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Net income (loss) |
531 | 1,842 | (897 | ) | 1,476 | (2,334 | ) | (858 | ) | |||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Net income (loss) attributable to non-controlling interest |
— | — | 959 | 959 | (1,517 | )(7) | (558 | ) | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Net income (loss) attributable to Health Insurance Innovations, Inc. |
$ | 531 | $ | 1,842 | $ | (1,856 | ) | $ | 517 | $ | (817 | ) | $ | (300 | ) | |||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
| Weighted average shares Class A common stock outstanding |
||||||||||||||||||||||||||
| Basic |
— | — | — | — | — | 4,826,667 | ||||||||||||||||||||
| Diluted |
— | — | — | — | — | 4,826,667 | ||||||||||||||||||||
| Net income available to Class A common stock per share(8) |
||||||||||||||||||||||||||
| Basic |
— | — | — | — | — | $ | (0.06 | ) | ||||||||||||||||||
| Diluted |
— | — | — | — | — | $ | (0.06 | ) | ||||||||||||||||||
57
Table of Contents
HEALTH INSURANCE INNOVATIONS, INC.
Unaudited Pro Forma Consolidated Statement of Operations
Nine Months Ended September 30, 2012
(in thousands, except share and per share amounts)
| Health Plan Intermediaries, LLC Historical(1) |
Reorganization Adjustments |
Health Insurance Innovations, Inc.(2) Pro Forma |
Offering Adjustments |
Health Insurance Innovations, Inc.(2) Pro Forma as Adjusted |
||||||||||||||||
| Revenue |
$ | 30,102 | — | $ | 30,102 | — | $ | 30,102 | ||||||||||||
| Third-party commissions |
20,093 | — | 20,093 | — | 20,093 | |||||||||||||||
| Credit cards and ACH fees |
693 | — | 693 | — | 693 | |||||||||||||||
| General and administrative expenses |
5,786 | — | 5,786 | 1,007 | (3) | 6,793 | ||||||||||||||
| Depreciation and amortization |
771 | — | 771 | — | 771 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total operating costs and expenses |
27,343 | — | 27,343 | 1,007 | 28,350 | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Income (loss) from operations |
2,759 | — | 2,759 | (1,007 | ) | 1,752 | ||||||||||||||
| Other expenses (income): |
||||||||||||||||||||
| Interest expense |
194 | — | 194 | (194 | )(4) | — | ||||||||||||||
| Interest income |
— | — | — | — | — | |||||||||||||||
| Other income |
(21 | ) | — | (21 | ) | — | (21 | ) | ||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Pre tax income (loss) |
2,586 | — | 2,586 | (813 | ) | 1,773 | ||||||||||||||
| Income tax |
— | 969 | (5) | 969 | (296 | )(6) | 673 | |||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Net income |
2,586 | (969 | ) | 1,617 | (517 | ) | 1,100 | |||||||||||||
| Net loss attributable to |
(63 | ) | 1,092 | 1,029 | (273 | )(7) | 756 | |||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Net income attributable to Health Insurance Innovations, Inc. |
$ | 2,649 | $ | (2,061 | ) | $ | 588 | $ | (244 | ) | $ | 344 | ||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Weighted average shares Class A common stock outstanding |
||||||||||||||||||||
| Basic |
— | — | — | — | 4,906,667 | |||||||||||||||
| Diluted |
— | — | — | — | 4,982,822 | |||||||||||||||
| Net income available to Class A common stock per share(8) |
||||||||||||||||||||
| Basic |
— | — | — | — | $ | 0.07 | ||||||||||||||
| Diluted |
— | — | — | — | $ | 0.07 | ||||||||||||||
| (1) | We have historically operated our business through Health Plan Intermediaries, LLC. As of September 30, 2012, Health Plan Intermediaries, LLC held all of our assets and liabilities and Health Plan Intermediaries Holdings, LLC did not have assets or liabilities and did not conduct operations. Accordingly, the unaudited pro forma consolidated statements of operations for the year ended December 31, 2011 and the nine months ended September 30, 2012 and the unaudited pro forma consolidated balance sheet as of September 30, 2012 present the historical results of Health Plan Intermediaries, LLC as a starting point for the pro forma amounts. On November 7, 2012, Health Plan Intermediaries, LLC assigned all of the operating assets of its business through a series of transactions to Health Plan Intermediaries Holdings, LLC, and Health Plan Intermediaries Holdings, LLC assumed the operating liabilities of Health Plan Intermediaries, LLC and began conducting operations. As a result, Health Plan Intermediaries Holdings, LLC currently operates all of our business. Pursuant to ASC 805-50-45, we assessed whether any pro forma adjustments in connection with the assignment were necessary. First, we concluded that Health Plan Intermediaries, LLC and Health Plan Intermediaries Holdings, LLC were under common control at the time of the assignment. In addition, after eliminating the effects of intra-entity transactions, the results of operations of the entities before and |
58
Table of Contents
| after the assignment were substantially the same. Accordingly, we determined that the transactions did not result in any pro forma effect. |
| (2) | As a newly formed entity, Health Insurance Innovations, Inc. will have no assets or results of operations until the completion of this offering. |
| (3) | Represents expected total stock compensation expense related to Mr. Hershberger’s restricted stock grant calculated in accordance with ASC 718, Compensation—Stock Compensation. Upon the consummation of this offering, Mr. Hershberger will be entitled to an amount equal to 3% of Health Insurance Innovations, Inc.’s enterprise value as determined immediately following the this offering. We calculated total stock compensation expense over the term of the grant by accounting for an estimated 400,000 shares granted and an estimated grant date price of $15, which represents the mid-point of the price range of $14 - $16 set forth on the cover page of the prospectus, to arrive at a total stock compensation amount of $6,000,000. Taking into consideration the accelerated graded vesting schedule of the grant whereby 40% of the total shares granted vest in 2013 and then the remaining shares vest 20% every October 1 from 2014 through 2016, we calculated $3,736,000 of estimated stock compensation expense for the pro forma twelve months ended December 31, 2011 and $1,007,000 of stock compensation expense for the pro forma nine months ended September 30, 2012. |
| (4) | Represents amounts to be eliminated in connection with this offering following application of a portion of the net proceeds of this offering to pay off all of our outstanding debt, which represent a five-year term loan bearing fixed interest at 5.25%. |
| (5) | Health Plan Intermediaries Holdings, LLC is not currently subject to entity-level federal income taxation and taxes with respect to income of Health Plan Intermediaries Holdings, LLC are payable by Health Plan Intermediaries Holdings, LLC’s equity holders at rates applicable to them. Following this offering, and the reorganization that we are undertaking in connection therewith, earnings recorded by us will be subject to federal income taxation. |
| (6) | Following this offering, Health Insurance Innovations, Inc. will be subject to U.S. federal income taxes, in addition to state and local taxes, with respect to its allocable share of any taxable income of Health Plan Intermediaries Holdings, LLC. As a result, the pro forma consolidated statement of operations reflects an adjustment to our provision for corporate income taxes to reflect an effective rate of 38%, which includes provision for U.S. federal income taxes. |
| (7) | As described in “The Reorganization of Our Corporate Structure,” after this offering, assuming the underwriters do not exercise their over-allotment option, and the reorganization transactions that we are undertaking in connection therewith, our only material asset will be the ownership of approximately 35% of the Membership Interests in Health Plan Intermediaries Holdings, LLC and our only business will be to act as the sole managing member of Health Plan Intermediaries Holdings, LLC. Accordingly, pursuant to ASC 810, we will consolidate the financial results of Health Plan Intermediaries Holdings, LLC into our financial statements. The ownership interests of the other members of Health Plan Intermediaries Holdings, LLC (Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC) will be accounted for as a non-controlling interest in our consolidated financial statements after this offering. Represents adjustments to reflect non-controlling interest resulting from the existing members’ ownership interest of 100% of the Series B Membership Interests of Health Plan Intermediaries Holdings, LLC. Immediately following this offering, the non-controlling interest will be approximately 65%. Net income (loss) attributable to the non-controlling interest represents 65%, or $756,000 of net income of $1,100,000 for the nine months ended September 30, 2012 and 65%, or $(558,000) of net loss of $858,000 for the year ended December 31, 2011. These amounts have been determined based on an offering price of $15.00 and the assumption that the underwriter’s option to purchase additional shares is not exercised. |
| (8) | Pro forma basic and diluted net income (loss) per share was computed by dividing the pro forma net income attributable to our Class A stockholders by the 4,666,667 shares of Class A common stock that we will issue and sell in this offering and the vested shares of Mr. Hershberger’s Class A restricted stock grant (assuming that the underwriters do not exercise their option to purchase an additional 700,000 shares of Class A common stock to cover over-allotments). The shares of Class B common stock do not share in our earnings and are therefore not included in the weighted average shares outstanding or net income available per share. |
59
Table of Contents
SELECTED HISTORICAL FINANCIAL AND OPERATIONAL DATA
The following selected historical financial and operational data of Health Plan Intermediaries, LLC should be read in conjunction with, and are qualified by reference to, “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and the financial statements and notes thereto included elsewhere in this prospectus. The statements of operations for the nine-month period ended September 30, 2012 (Successor), the three-month period ended December 31, 2011 (Successor), the nine-month period ended September 30, 2011 (Predecessor) and the year ended December 31, 2010 (Predecessor) and the balance sheet data as of September 30, 2012 (Successor) and December 31, 2011 (Successor) are derived from, and qualified by reference to, the audited consolidated financial statements of Health Plan Intermediaries, LLC included elsewhere in this prospectus and should be read in conjunction with those financial statements and notes thereto. Results for the nine-month period ended September 30, 2012 are not necessarily indicative of results that may be expected for the entire year.
| Nine Months Ended September 30, 2012 |
Three Months Ended December 31, 2011 |
Nine Months Ended September 30, 2011 |
Year Ended December 31, 2011 |
Year Ended December 31, 2010 |
||||||||||||||||||
| (Successor) | (Successor) | (Predecessor) | (Combined) (Non-GAAP) |
(Predecessor) | ||||||||||||||||||
| (in thousands, except plans in force) | ||||||||||||||||||||||
| Statements of Operations: |
||||||||||||||||||||||
| Revenues |
$ | 30,102 | $ | 8,090 | $ | 21,788 | $ | 29,878 | $ | 11,790 | ||||||||||||
| Third-party commissions |
20,093 | 5,601 | 16,103 | 21,704 | 9,010 | |||||||||||||||||
| Credit cards and ACH fees |
693 | 197 | 473 | 670 | 275 | |||||||||||||||||
| General and administrative expenses |
5,786 | 1,421 | 3,341 | 4,762 | 2,514 | |||||||||||||||||
| Depreciation and amortization |
771 | 269 | 29 | 298 | 7 | |||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Total operating costs and expenses |
27,343 | 7,488 | 19,946 | 27,434 | 11,806 | |||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Income (loss) from operations |
2,759 | 602 | 1,842 | 2,444 | (16 | ) | ||||||||||||||||
| Other expenses (income): |
||||||||||||||||||||||
| Interest expense |
194 | 71 | — | 71 | — | |||||||||||||||||
| Interest income |
— | — | — | (3 | ) | |||||||||||||||||
| Other income |
(21 | ) | — | — | ||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Net income (loss) |
$ | 2,586 | $ | 531 | $ | 1,842 | $ | 2,373 | $ | (13 | ) | |||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Net loss attributable to noncontrolling interest in subsidiary |
(63 | ) | — | — | — | — | ||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Net income (loss) attributable to Health Plan Intermediaries, LLC |
$ | 2,649 | $ | 531 | $ | 1,842 | $ | 2,373 | $ | (13 | ) | |||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Other Financial and Operational Data: |
||||||||||||||||||||||
| Premium equivalents(1) |
$ | 54,549 | $ | 14,949 | $ | 38,257 | $ | 53,206 | $ | 20,024 | ||||||||||||
| Plans in force (end of period)(2) |
53,297 | 29,951 | 22,847 | 29,951 | 13,121 | |||||||||||||||||
| EBITDA(3) |
$ | 3,551 | $ | 871 | $ | 1,871 | $ | 2,742 | $ | (9 | ) | |||||||||||
| (1) | “Premium equivalents” is defined as the combination of premiums, fees for discount benefit plans, fees for distributors and our enrollment fees. Premium equivalents does not represent, and should not be considered as, an alternative to revenues, as determined in accordance with U.S. generally accepted accounting principles, or U.S. GAAP. We have included premium equivalents in this prospectus because it is a key measure used by our management to understand and evaluate our core operating performance and trends, to prepare and approve our annual budget and to develop short- and long-term operational plans. In particular, the inclusion of premium equivalents can provide a useful measure for period-to-period comparisons of our business. Premium equivalents has limitations as an analytical tool, and you should not consider it in isolation or as a substitute for analysis of our results as reported under U.S. GAAP. See “Management Discussion and Analysis of Financial Condition and Results of Operations—Key Business Metrics.” |
60
Table of Contents
The following is a reconciliation of premium equivalents to revenues:
| Nine Months Ended September 30, 2012 |
Three Months Ended December 31, 2011 |
Nine Months Ended September 30, 2011 |
Year Ended December 31, 2011 |
Year Ended December 31, 2010 |
||||||||||||||||||
| (Successor) | (Successor) | (Predecessor) | (Combined) (Non-GAAP) |
(Predecessor) | ||||||||||||||||||
| (in thousands) | ||||||||||||||||||||||
| Premium equivalents |
$ | 54,549 | $ | 14,949 | $ | 38,257 | $ | 53,206 | $ | 20,024 | ||||||||||||
| Less risk premium |
(23,296 | ) | (6,380 | ) | (15,180 | ) | (21,560 | ) | (7,616 | ) | ||||||||||||
| Less amounts earned by third-party obligors |
(1,151 | ) | (479 | ) | (1,289 | ) | (1,768 | ) | (618 | ) | ||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| Revenues |
$ | 30,102 | $ | 8,090 | $ | 21,788 | $ | 29,878 | $ | 11,790 | ||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| (2) | “Plans in force” is defined as policies or discount benefit plans issued to a member for which we have collected the applicable premium payments and/or discount benefit fees. See “Management Discussion and Analysis of Financial Condition and Results of Operations—Key Business Metrics.” A member may be enrolled in more than one policy or discount benefit plan simultaneously. |
| (3) | “EBITDA” is defined as net income before interest expense, interest income and depreciation and amortization. EBITDA does not represent, and should not be considered as, an alternative to net income or cash flows from operations, each as determined in accordance with U.S. GAAP. We have presented EBITDA because we consider it an important supplemental measure of our performance and believe that it is frequently used by analysts, investors and other interested parties in the evaluation of companies. Other companies may calculate EBITDA differently than we do. EBITDA has limitations as an analytical tool, and you should not consider it in isolation or as a substitute for analysis of our results as reported under U.S. GAAP. |
The following is a reconciliation of net income (loss) to EBITDA:
| Nine Months Ended September 30, 2012 |
Three Months Ended December 31, 2011 |
Nine Months Ended September 30, 2011 |
Year Ended December 31, 2011 |
Year Ended December 31, 2010 |
||||||||||||||||||
| (Successor) | (Successor) | (Predecessor) | (Combined) (Non-GAAP) |
(Predecessor) | ||||||||||||||||||
| (in thousands) | ||||||||||||||||||||||
| Net Income (loss) |
$ | 2,586 | $ | 531 | $ | 1,842 | $ | 2,373 | $ | (13 | ) | |||||||||||
| Interest expense |
194 | 71 | — | 71 | — | |||||||||||||||||
| Interest income |
— | — | — | — | (3 | ) | ||||||||||||||||
| Depreciation and amortization |
771 | 269 | 29 | 298 | 7 | |||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| EBITDA |
$ | 3,551 | $ | 871 | $ | 1,871 | $ | 2,742 | $ | (9 | ) | |||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
| As of September 30, 2012 |
As of December 31, 2011 |
|||||||
| (in thousands) | ||||||||
| Balance Sheet Data: |
||||||||
| Cash |
$ | 982 | $ | 618 | ||||
| Total assets |
17,542 | 15,068 | ||||||
| Debt, noncompete obligation and capital leases |
4,340 | 4,078 | ||||||
| Total member’s equity |
6,869 | 6,996 | ||||||
61
Table of Contents
MANAGEMENT’S DISCUSSION AND ANALYSIS
OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS
You should read the following discussion together in conjunction with our financial statements and the notes thereto included in this prospectus. The following discussion contains forward-looking statements. Actual results could differ materially from the results discussed in the forward-looking statements. See “Risk Factors” and “Special Note Regarding Forward-Looking Statements” above.
We are a leading developer and administrator of affordable, web-based individual health insurance plans and ancillary products. Our highly scalable, proprietary, web-based technology platform allows for mass distribution of and online enrollment in our large and diverse portfolio of affordable health insurance offerings.
Our technology platform provides customers, who we refer to as members, immediate access to our products through our distribution partners anytime, anyplace. The health insurance products we develop are underwritten by insurance carrier companies, and we assume no underwriting, insurance or reimbursement risk. Members can price and tailor product selections to meet their needs, buy policies and print policy documents and identification cards in real-time. Our sales are executed online and offer instant electronic fulfillment. Our technology platform uses abbreviated online applications, some with health questionnaires, to provide an immediate accept or reject decision on applications for all products that we offer. Once an application is accepted, individuals can use our automated payment system to complete the enrollment process and obtain instant electronic access to their policy fulfillment documents, including the insurance policy, benefits schedule and identification cards. We receive credit card and Automated Clearing House (ACH) payments directly from members at the time of sale. Our technology platform provides significant operating leverage as we add members and reduces the costs associated with marketing, selling, underwriting and administering policies.
We are an industry leader in the sale of 12-month short-term medical, or STM, insurance plans, an alternative to traditional Individual Major Medical, or IMM, plans, which provide lifetime renewable coverage. STM plans generally offer qualifying individuals comparable benefits for fixed short-term durations of six or 12 months at approximately half the cost of IMM plans. While applications for IMM insurance may take up to 60 days to process, STM plans feature a streamlined underwriting process offering immediate coverage options. We also offer guaranteed-issue hospital indemnity plans for individuals under the age of 65, which pay fixed cash benefits for covered procedures and services, and a variety of ancillary products such as pharmacy benefit cards, dental plans, vision plans and cancer/critical illness plans that are frequently purchased as supplements to STM and hospital indemnity plans. We design and structure insurance products on behalf of insurance carrier companies, market them to individuals through our large network of distributors and manage member relations via our online member portal, which is available 24 hours a day, seven days a week. Our online enrollment process allows us to aggregate and analyze consumer data and purchasing habits to track market trends and drive product innovation. We have established relationships with several highly rated insurance carriers, including Starr Indemnity & Liability Company, Companion Life, United States Fire (a member of the Crum & Forster group), ING, Markel and CIGNA among others. In addition, as of September 30, 2012, the large independent distribution network we access consists of 32 licensed agent call centers and 248 wholesalers, including Marsh, eHealthInsurance and MasterCard, among others, that work with over 7,300 licensed brokers. Our data-driven product design, technology platform and extensive distribution network have enabled us to grow our revenues from $11,790,000 in 2010 to $29,878,000 in 2011, and from $21,788,000 in the nine-month period ended September 30, 2011 to $30,102,000 in the nine-month period ended September 30, 2012.
We focus on the large and under-penetrated segment of the U.S. population who are uninsured or underinsured, which includes individuals who are unable to afford traditional IMM premiums, individuals not covered by employer-sponsored insurance plans, such as those who are self-employed as well as small business owners and their employees, and underserved “gap populations” that require insurance due to changes caused by life events, such as new graduates, divorcees, early retirees, military discharges, the unemployed, part-time and seasonal employees and temporary workers. Our target market consists of approximately 64 million Americans, including approximately 50 million Americans who were uninsured in 2010, according to the U.S. Census
62
Table of Contents
Bureau, and approximately 14 million non-elderly Americans who purchased individual health insurance plans in 2010, according to a 2010 Kaiser Family Foundation survey. As of September 30, 2012, we had approximately 24,416 STM members. We expect the number of uninsured and underinsured to significantly increase due to the rising costs and burdensome underwriting requirements of traditional IMM plans and a decline in employer-sponsored health insurance programs.
As of September 30, 2012, we had 24,416 STM plans in force, compared with 16,838 on September 30, 2011, with an average monthly retention rate of 80% from September 30, 2011 to September 30, 2012. We earn our revenues from commissions and fees related to the sale of products to our members. Our ancillary products have created several additional revenue streams and resulted in a significant portion of our business being generated by monthly member renewals. For the nine months ended September 30, 2012, our premium equivalents, revenue and EBITDA were $54,549,000, $30,102,000 and $3,551,000, respectively, representing a 42.6%, 38.2% and 89.8% increase compared to premium equivalents, revenues and EBITDA of $38,257,000, $21,788,000 and $1,871,000, respectively, for the nine months ended September 30, 2011. See “Selected Historical Financial and Operational Data” for a discussion regarding the use of premium equivalents and EBITDA as financial measures and for reconciliations to the most directly comparable GAAP financial measures.
Basis of Presentation
On September 28, 2011, we entered into an agreement to purchase of the units of Health Plan Intermediaries, LLC owned by Naylor Group Partners, LLC. Prior to the purchase, which we refer to as the Acquisition, Health Plan Intermediaries, LLC was 50% owned by Naylor Group Partners, LLC and 50% owned by Mr. Kosloske. Following the purchase, Mr. Kosloske became the sole member of Health Plan Intermediaries, LLC. The Acquisition was accounted for as a purchase and the purchase price was reflected on our financial statements using push-down accounting. Accordingly, purchase accounting adjustments have been reflected in our financial statements for the period commencing on October 1, 2011. The new basis of accounting reflects the estimated fair value of the our assets and liabilities as of the date of the Acquisition. We used October 1, 2011, as the effective date of the transaction, since the operating activity between that date and the September 28, 2011 transaction date was not material.
The following discussion and analysis of our financial condition and results of operations covers periods before and after the Acquisition. The discussion and analysis of periods prior to September 30, 2011 do not reflect the purchase accounting adjustments discussed above and in the financial statements and notes thereto included elsewhere in this prospectus. However, the general nature of our operations was not impacted by the Acquisition. As such, for comparative purposes we will discuss changes between the periods without reference to the effects of the Predecessor and Successor periods, which is consistent with the manner in which we evaluate the results of operations. All references to the nine months ended September 30, 2012 relate to the nine-month period ended September 30, 2012 of the Successor. All references to the nine months ended September 30, 2011 relate to the nine-month period ended September 30, 2011 of the Predecessor. All references to the year ended December 31, 2011 relate to the combined three-month period ended December 31, 2011 of the Successor and the nine-month period ended September 30, 2011 of the Predecessor. All references to the year ended December 31, 2010 relate to the year ended December 31, 2010 of the Predecessor. The presentation of combined Predecessor and Successor operating results (which is simply the arithmetic sum of the Predecessor and Successor amounts) is a Non-GAAP presentation, which is provided as a convenience solely for the purpose of facilitating comparisons of current results with combined results over the same period in the prior year. Effects of the Acquisition will be discussed where applicable.
Effects of the Reorganization
Health Insurance Innovations, Inc. was formed for the purpose of this offering and has engaged to date only in activities in contemplation of this offering. Upon completion of the offering, all of our business will be conducted through Health Plan Intermediaries Holdings, LLC, and the financial results of Health Plan Intermediaries Holdings, LLC and its consolidated subsidiaries will be consolidated in our financial statements.
63
Table of Contents
Historically, our business was operated through Health Plan Intermediaries, LLC. In anticipation of this offering, on November 7, 2012, Health Plan Intermediaries, LLC assigned the operating assets of our business through a series of transactions to Health Plan Intermediaries Holdings, LLC, and Health Plan Intermediaries Holdings, LLC assumed the operating liabilities of Health Plan Intermediaries, LLC.
Health Insurance Innovations, Inc. will be a holding company whose principal asset will be its interest in Health Plan Intermediaries Holdings, LLC. All of the equity of Health Plan Intermediaries Holdings, LLC outstanding prior to the reorganization will be exchanged for Series B Membership Interests of Health Plan Intermediaries Holdings, LLC and an equal number of shares of our Class B common stock. For more information regarding our reorganization and holding company structure, see “The Reorganization of Our Corporate Structure.”
We expect that future exchanges of Series B Membership Interests (together with an equal number of our Class B common shares) for shares of our Class A common stock, as well as the acquisition, with the net proceeds of the sale of any over-allotment shares, of Series B Membership Interests (together with an equal number of shares of our Class B common stock) from Health Plan Intermediaries, LLC (which Series B Membership Interests will immediately be recapitalized into Series A Membership Interests), see “Use of Proceeds,” will result in increases in the tax basis in our share of the tangible and intangible assets of Health Plan Intermediaries Holdings, LLC. We expect that these increases in tax basis, which would not have been available but for our new holding company structure, will reduce the amount of tax that we would otherwise be required to pay in the future. We will be required to pay a portion of the cash savings we actually realize from such increase (or are deemed to realize in the case of an early termination payment by us, a change in control or a material breach by us of our obligations under the tax receivable agreement, as discussed above) to the existing and certain future holders of Series B Membership Interests (currently Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske), pursuant to a tax receivable agreement. Furthermore, payments under the tax receivable agreement will give rise to additional tax benefits and therefore additional payments under the tax receivable agreement itself. See “The Reorganization and Our Corporate Structure—Tax Receivable Agreement.”
Our former operating entity, Health Plan Intermediaries, LLC, is taxed as an S corporation for income tax purposes. Therefore, we have not been subject to entity-level federal or state income taxation. Health Plan Intermediaries Holdings, LLC is currently taxed as a partnership for federal income tax purposes; and as a result, the members of Health Plan Intermediaries Holdings, LLC pay taxes with respect to their allocable shares of its net taxable income. Following the reorganization and this offering, all of the earnings of Health Insurance Innovations, Inc. will be subject to federal income taxation.
Factors Affecting Our Results of Operations
As the managing general underwriter of our individual health insurance plans and ancillary products, we receive all amounts due in connection with our plans on behalf of the providers of the services. We refer to these total collections as premium equivalents, which typically represent a combination of premiums, fees for discount benefit plans (a non-insurance benefit product that supplements or enhances an insurance product), fees for distributors and our enrollment fees. From premium equivalents, we remit risk premium to carriers and amounts earned by discount benefit plan providers, who we refer to as third-party obligors, such carriers and third-party obligors being the ultimate parties responsible for providing the insurance coverage or discount benefits to the member. Our revenues consist of the balance of the premium equivalents.
We collect premium equivalents upon the initial sale of the plan and then monthly upon each subsequent periodic payment under such plan. We receive most premium equivalents through online credit card or ACH processing. As a result, we have limited accounts receivable. We remit the risk premium to the applicable carriers and the amounts earned by third-party obligors on a monthly basis based on the respective compensation arrangements.
64
Table of Contents
Commission revenue and fees attributable to revenues from STM plans and hospital indemnity policies represented substantially all of our revenues for the periods presented. Our commissions represent premiums and fees for discount benefit plans, net of risk premium and amounts earned by third-party obligors, respectively. We recognize commissions as we collect the premiums and fees for discount benefit plans.
Commission rates for all insurance plans are approved in advance by the relevant carrier. Our commission rates and the length of the commission period typically vary by carrier and plan type. Under our carrier compensation arrangements, the commission rate schedule that is in effect on the policy effective date will govern the commissions over the life of the plan.
We continue to receive a commission payment until the plan expires or is terminated. Accordingly, a portion of our monthly revenues is predictable on a month-to-month basis and revenues increase in direct proportion to the growth we experience in the number of plans in force.
We pay fees to distributors for their services in selling our plans, which are included in our operating costs and expenses.
Key Business Metrics
In addition to traditional financial metrics, we rely upon the following key business metrics to evaluate our business performance and facilitate long-term strategic planning:
Premium equivalents. We define this metric as the combination of premiums, fees for discount benefit plans, fees for distributors and our enrollment fees. All amounts not paid out as risk premium to carriers or paid out to other third-party obligors are considered to be revenues for financial reporting purposes. We have included premium equivalents in this prospectus because it is a key measure used by our management to understand and evaluate our core operating performance and trends, to prepare and approve our annual budget and to develop short- and long-term operational plans. In particular, the inclusion of premium equivalents can provide a useful measure for period-to-period comparisons of our business.
Plans in force. We consider a plan to be in force when we have issued a member his or her insurance policy or discount benefit plan and have collected the applicable premium payments and/or discount benefit fees. Our plans in force are an important indicator of our expected revenues, as we receive a monthly commission for up to six months for our six-month STM plan, up to 12 months for our 12-month STM plan and often more than 12 months for our hospital indemnity and discount benefit plans, provided that the policy or discount benefit plan is not cancelled. A member may be enrolled in more than one policy or discount benefit plan simultaneously. A plan becomes inactive upon notification to us of termination of its policy or discount benefit plan, when the member’s policy or discount benefit plan expires or following non-payment of premiums or discount benefit fees when due.
EBITDA. We define this metric as net income before interest expense, income taxes, interest income and depreciation and amortization. We have included EBITDA in this prospectus because it is a key measure used by our management and board of directors to understand and evaluate our core operating performance and trends, to prepare and approve our annual budget and to develop short- and long-term operational plans. In particular, the exclusion of certain expenses in calculating EBITDA can provide a useful measure for period-to-period comparisons of our business.
Key Components of Our Statements of Operations
Revenues
Our revenues consist primarily of commissions earned for our insurance policies and discount benefit plans issued to members, enrollment fees paid by members and administration fees paid by members as a direct result of our enrollment services. We recognize revenues upon the member’s acceptance of a policy. We expect our revenues to increase as we add new members.
65
Table of Contents
Operating Costs and Expenses
Operating costs and expenses consist of fees and commissions paid to distributors for selling our products to members, credit card or ACH processing fees and general and administrative expenses. We expect our operating costs and expenses to represent a decreasing percentage of our revenues due to the scalable nature of our technology platform that allows for mass distribution and online enrollment of our products, requiring minimal maintenance and incremental costs.
Third-party Commissions
Our third-party commissions consist of fees and commissions paid to distributors for selling our products to members, which we pay monthly for existing members and on a weekly basis for new members. We expect third-party commissions as a percentage of revenue to remain generally consistent with prior periods.
Credit Cards and ACH Fees
Our credit card and ACH fees are fees paid to our banks and processors for the collection of credit card and ACH payments. We expect credit card and ACH fees as a percentage of revenue to remain generally consistent with prior periods.
General and Administrative Expenses
Our general and administrative expenses primarily consist of personnel costs, which represent salaries, bonuses, commissions, payroll taxes and benefits. General and administrative expenses also include marketing campaign expenditures and travel costs associated with obtaining new distributor relationships. In addition, these expenses also include technology expenses and personnel costs and expenses for outside professional services, including legal, audit and financial services. Following the completion of this offering, we expect general and administrative expenses to increase due to the anticipated growth of our business and infrastructure and the costs associated with becoming a public company, such as costs associated with SEC reporting and compliance, developing and maintaining internal controls over financial reporting, insurance, investor relations and other related costs. In addition, as a result of the grant to Mr. Hershberger of restricted stock in connection with the offering, we will recognize compensation expense in accordance with the vesting schedule of the restricted stock. See “Executive Compensation—Restricted Stock Agreements.” While such expense will depend on the stock price at the time each tranche of units vest, assuming an initial public offering price of $15, we would expect such expense with respect to units vesting in the 12-month period following the offering to equal 3,904,000 for such 12-month period.
Depreciation and Amortization
Depreciation and amortization expense is primarily a function of amortization of intangible assets as well as depreciation of property and equipment used in our business. As a result of the Acquisition described above, we expect our depreciation and amortization expenses to increase, reflecting growth of intangible assets.
Major classes of amortizable intangible assets at September 30, 2012 consist of the following:
| Weighted-Average Amortization Period (In Years) |
Gross Carrying Amount |
Accumulated Amortization |
Intangible Asset, net |
|||||||||||||
| Distributor relationships |
7 | $ | 3,610,000 | $ | 516,000 | $ | 3,094,000 | |||||||||
| Carrier network |
5 | 40,000 | 8,000 | 32,000 | ||||||||||||
| Brand |
2 | 400,000 | 200,000 | 200,000 | ||||||||||||
| Capitalized software |
5 | 45,000 | 2,000 | 43,000 | ||||||||||||
| Noncompete agreement |
5 | 843,000 | 28,000 | 815,000 | ||||||||||||
|
|
|
|
|
|
|
|||||||||||
| Total intangible assets |
$ | 4,938,000 | $ | 754,000 | $ | 4,184,000 | ||||||||||
|
|
|
|
|
|
|
|||||||||||
66
Table of Contents
Interest Expense
Interest expense consists of interest incurred on our outstanding debt. We expect interest to be eliminated in connection with this offering following application of a portion of the net proceeds of this offering to pay off debt.
Interest Income
Interest income consists of interest income earned on our cash balances.
Other Income
Other income includes fees charged to distributors for advance commissions, whereby we pay distributors commissions on policies sold in advance of when they would ordinarily be due to the distributor. These advance commissions are made to distributors with an established track record of selling our products. Advance commission fees range from 0% up to 2% of the premiums for each month that we advance commissions. Advanced commissions to a distributor are based upon the number of future months of expected premium equivalent multiplied by a distributor’s commission rate. We expect other income to increase as we expand our advance commission structure with the application of the net proceeds of this offering.
Income Tax Expenses
Our former operating entity, Health Plan Intermediaries, LLC, is taxed as an S corporation for income tax purposes. Therefore, we have not been subject to entity-level federal or state income taxation. Health Plan Intermediaries Holdings, LLC is currently taxed as a partnership for federal income tax purposes; and as a result, the members of Health Plan Intermediaries Holdings, LLC pay taxes with respect to their allocable shares of its net taxable income. Following the reorganization and this offering, all of the earnings of Health Insurance Innovations, Inc. will be subject to federal income taxation. Health Insurance Innovations, Inc. will account for income taxes in accordance with the provisions of ASC 740. Based on this guidance, our historical statements of operations would have reflected total income tax expense in the amount of approximately $896,000 and $1,000 for the years ended December 31, 2011 and 2010, respectively, and $964,000 for the nine months ended September 30, 2012.
Noncontrolling Interest
On June 1, 2012, we and TSG Agency, or TSG, formed Insurance Center for Excellence, LLC doing business as Insurance Academy, or ICE. ICE is a call center training facility for our distributors. Pursuant to the terms of the transaction, we contributed $80,000 in cash, and TSG contributed $20,000 in cash to the newly created limited liability company. In connection with the transaction, we received an 80% controlling interest in ICE and TSG received a 20% noncontrolling interest in ICE. The intent of this transaction was to attract potential call centers and educate them on our model and best practices with the ultimate goal of these call centers joining our distribution network. We do not expect that ICE will have a material impact on our results from operations in the next fiscal year.
67
Table of Contents
Results of Operations
The following table is a summary of our statements of operations as a percentage of our total revenues.
| Percentage of Total Revenue | ||||||||||||||||
| Nine Months Ended September 30, | Year Ended December 31, | |||||||||||||||
| 2012 | 2011 | 2011 | 2010 | |||||||||||||
| Revenues |
100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | ||||||||
| Third-party commissions |
66.7 | % | 73.9 | % | 72.6 | % | 76.4 | % | ||||||||
| Credit cards and ACH fees |
2.3 | % | 2.2 | % | 2.2 | % | 2.3 | % | ||||||||
| General and administrative expenses |
19.2 | % | 15.3 | % | 15.9 | % | 21.3 | % | ||||||||
| Depreciation and amortization |
2.6 | % | 0.1 | % | 1.0 | % | 0.1 | % | ||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Total operating costs and expenses |
90.8 | % | 91.5 | % | 91.8 | % | 100.1 | % | ||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Income (loss) from operations |
9.2 | % | 8.5 | % | 8.2 | % | (0.1 | )% | ||||||||
| Other expenses (income): |
||||||||||||||||
| Interest expense |
0.6 | % | — | 0.2 | % | — | ||||||||||
| Interest income |
— | — | — | 0.0 | % | |||||||||||
| Other income |
(0.1 | )% | — | — | — | |||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Net income (loss) |
8.6 | % | 8.5 | % | 7.9 | % | (0.1 | )% | ||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Net loss attributable to noncontrolling interest in subsidiary |
(0.2 | )% | — | — | — | |||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Net income (loss) attributable to Health Plan Intermediaries, LLC |
8.8 | % | 8.5 | % | 7.9 | % | (0.1 | )% | ||||||||
|
|
|
|
|
|
|
|
|
|||||||||
Comparison of Nine Months Ended September 30, 2012 and 2011
The following table presents our historical results of operations and the changes in these results in dollars and as a percentage for the periods presented:
| Nine Months Ended September 30, | ||||||||||||||||
| 2012 | 2011 | Change ($) | Change (%) | |||||||||||||
| (in thousands, except percentages) | ||||||||||||||||
| Revenues |
$ | 30,102 | $ | 21,788 | $ | 8,314 | 38.2 | % | ||||||||
| Third-party commissions |
20,093 | 16,103 | 3,990 | 24.8 | % | |||||||||||
| Credit cards and ACH fees |
693 | 473 | 220 | 46.5 | % | |||||||||||
| General and administrative expenses |
5,786 | 3,341 | 2,445 | 73.2 | % | |||||||||||
| Depreciation and amortization |
771 | 29 | 742 | >100 | % | |||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Total operating costs and expenses |
27,343 | 19,946 | 7,397 | 37.1 | % | |||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Income from operations |
2,759 | 1,842 | 917 | 49.8 | % | |||||||||||
| Other expenses (income): |
||||||||||||||||
| Interest expense |
194 | — | 194 | 100.0 | % | |||||||||||
| Interest income |
— | — | — | — | ||||||||||||
| Other income |
(21 | ) | — | (21 | ) | (100.0 | )% | |||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Net income |
$ | 2,586 | $ | 1,842 | $ | 744 | 40.4 | % | ||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Net loss attributable to noncontrolling interest in subsidiary |
(63 | ) | — | (63 | ) | 100.0 | % | |||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Net income attributable to Health Plan Intermediaries, LLC |
$ | 2,649 | $ | 1,842 | $ | 807 | 43.8 | % | ||||||||
|
|
|
|
|
|
|
|
|
|||||||||
68
Table of Contents
Revenues
Revenues for the nine months ended September 30, 2012 were approximately $30,102,000, an increase of approximately $8,314,000, or 38.2%, compared to the nine months ended September 30, 2011. Revenue growth was primarily due to a 133.3% increase in the number of plans in force from 22,847 at September 30, 2011 to 53,297 at September 30, 2012. STM policies in force grew from 16,838 at September 30, 2011 to 24,416 at September 30, 2012, hospital indemnity policies in force grew from 5,645 at September 30, 2011 to 5,841 at September 30, 2012 as we concentrated on the sales of our other products and ancillary product policies in force grew from 364 at September 30, 2011 to 23,040 at September 30, 2012.
Third-party Commissions
Third-party commissions for the nine months ended September 30, 2012 were approximately $20,093,000, an increase of approximately $3,990,000, or 24.8%, compared to the nine months ended September 30, 2011. The growth in third-party commissions was primarily due to the increase in the number of plans in force. Third-party commissions represented 66.7% of revenues for the nine months ended September 30, 2012 and 73.9% of revenues for the nine months ended September 30, 2011.
Credit Card and ACH Fees
Credit card and ACH fees for the nine months ended September 30, 2012 were approximately $693,000, an increase of approximately $220,000, or 46.5%, compared to the nine months ended September 30, 2011. This growth in credit card and ACH fees was primarily due to the increase in the number of policies in force. Credit card and ACH fees represented approximately 2.3% of revenues for the nine months ended September 30, 2012 and 2.2% of revenues for the nine months ended September 30, 2011.
General and Administrative Expenses
General and administrative expenses for the nine months ended September 30, 2012 were approximately $5,786,000, an increase of approximately $2,445,000, or 73.2%, compared to the nine months ended September 30, 2011. The increase in general and administrative expenses was driven by an increase in personnel costs of $1,845,000, professional fees of $649,000 and selling, marketing and other expenses of $729,000. Personnel costs increased primarily due to additional sales and financial reporting personnel added to accommodate our growth. Professional fees increased as a result of legal fees and accounting costs associated with establishing a financial reporting department subsequent to the Acquisition. We also incurred professional fees to maintain our administrative technology platform. The increase in selling and marketing was primarily due to our adoption of a revised sales strategy and adding additional employees to implement this strategy. These increases were offset by a decrease of $615,000 of guaranteed payment expense for payments to Mr. Kosloske that were recorded to general and administrative expenses during Predecessor periods. General and administrative expenses represented 19.2% of revenues for the nine months ended September 30, 2012 and 15.3% of revenues for the nine months ended September 30, 2011.
Depreciation and Amortization
Depreciation and amortization expenses for the nine months ended September 30, 2012 were $771,000, an increase of $742,000, compared to the nine months ended September 30, 2011. This increase was primarily driven by amortization of intangible assets that were recognized from the Acquisition.
Interest Expense
Interest expense for the nine months ended September 30, 2012 was $194,000, an increase of $194,000 compared to the nine months ended September 30, 2011. This increase was the result of our entering into a bank loan agreement in September 2011 to finance the Acquisition. The original principal balance of the loan was
69
Table of Contents
$4,250,000, and the loan is a five-year loan bearing fixed interest at 5.25% with equal monthly payments of approximately $81,000, which consist of principal and interest. A balance of $3,490,000 remains outstanding as of September 30, 2012, including a current portion of $802,000.
Other Income
Other income for the nine months ended September 30, 2012 was $21,000, an increase of $21,000 as compared to the nine months ended September 30, 2011. The increase in other income was primarily driven by fees charged to distributors for advance commissions. We began to distribute advance commissions in November 2011.
Comparison of 2011 and 2010
The following table presents our historical results of operations and the changes in these results in dollars and as a percentage for the periods presented:
| Year Ended December 31, | ||||||||||||||||
| 2011 | 2010 | Change ($) | Change (%) | |||||||||||||
| (in thousands, except percentages) | ||||||||||||||||
| Revenues |
$ | 29,878 | $ | 11,790 | $ | 18,088 | 153.4 | % | ||||||||
| Third-party commissions |
21,704 | 9,010 | 12,694 | 140.9 | % | |||||||||||
| Credit cards and ACH fees |
670 | 275 | 395 | 143.6 | % | |||||||||||
| General and administrative expenses |
4,762 | 2,514 | 2,248 | 89.4 | % | |||||||||||
| Depreciation and amortization |
298 | 7 | 291 | >100.0 | % | |||||||||||
|
|
|
|
|
|
|
|||||||||||
| Total operating costs and expenses |
27,434 | 11,806 | 15,628 | 132.4 | % | |||||||||||
|
|
|
|
|
|
|
|||||||||||
| Income (loss) from operations |
2,444 | (16 | ) | 2,460 | >(100.0) | % | ||||||||||
| Other expenses (income): |
||||||||||||||||
| Interest expense |
71 | — | 71 | 100 | % | |||||||||||
| Interest income |
— | (3 | ) | 3 | (100 | %) | ||||||||||
|
|
|
|
|
|
|
|||||||||||
| Net income (loss) |
$ | 2,373 | $ | (13 | ) | $ | 2,386 | >(100.0) | % | |||||||
|
|
|
|
|
|
|
|||||||||||
Revenues
Revenues for 2011 were $29,878,000, an increase of $18,088,000, or 153.4%, compared to 2010. Revenue growth was primarily due to a 128.3% increase in the number of policies in force from 13,121 at December 31, 2010 to 29,951 at December 31, 2011. STM policies in force grew from 5,627 at December 31, 2010 to 18,059 at December 31, 2011, hospital indemnity policies in force declined from 7,494 at December 31, 2010 to 5,243 at December 31, 2011 as we concentrated on the sales of our other products and ancillary product policies in force grew from zero at December 31, 2010 to 6,649 at December 31, 2011.
Third-party Commissions
Third-party commissions for 2011 were approximately $21,704,000, an increase of approximately $12,694,000, or 140.9%, compared to 2010. The growth in third-party commissions was primarily due to the increase in the number of plans in force. Third-party commissions represented 72.6% of revenues for 2011 and 76.4% of revenues for 2010.
Credit Card and ACH Fees
Credit card and ACH fees for 2011 were approximately $670,000, an increase of approximately $395,000, or 143.6%, compared to 2010. The growth in credit card and ACH fees was primarily due to the increase in the number of plans in force. Credit card and ACH fees represented 2.2% of revenues for 2011 and 2.3% of revenues for 2010.
70
Table of Contents
General and Administrative Expenses
General and administrative expenses for 2011 were $4,762,000, an increase of $2,248,000, or 89.4%, compared to 2010. This increase in general and administrative expenses was driven by an increase in personnel costs of $1,456,000, professional fees of $157,000, selling and marketing expenses of $456,000 and other office related expenses of $178,000. Personnel costs increased primarily due to an increase in senior managerial staff. Professional fees increased as a result of legal fees and accounting costs associated with establishing a financial reporting department subsequent to the Acquisition. The increase in selling and marketing and other office related expenses was primarily due to our adoption of a revised sales strategy and adding additional employees to implement the strategy subsequent to the Acquisition. General and administrative expenses represented 15.9% of revenues for 2011 and 21.3% of revenues for 2010.
Depreciation and Amortization
Depreciation and amortization expenses for 2011 were $298,000, an increase of $291,000, compared to 2010. This increase was primarily driven by amortization of intangible assets that were recognized from the Acquisition.
Interest Expense
Interest expense for 2011 was $71,000, an increase of $71,000, compared to 2010. This increase was due to the bank loan agreement entered into September 2011 to finance the Acquisition.
Interest Income
Interest income for 2011 was $0, a decrease of $3,000, compared to 2010. This decrease was primarily driven by our decision to forgo interest in exchange for having our commercial accounts fully insured by the Federal Deposit Insurance Corporation (FDIC).
Quarterly Results of Operations
The following table sets forth our unaudited (with the exception of the three months ended December 31, 2011) quarterly statements of operations data for each of the four quarters presented below (certain items may not foot due to rounding). We have prepared the unaudited quarterly data on a consistent basis with the audited financial statements included in this prospectus. In the opinion of management, the financial information reflects all necessary adjustments, consisting only of normal recurring adjustments, necessary for a fair presentation of this data. This information should be read in conjunction with our audited financial statements and the related notes included elsewhere in this prospectus. The results of historical periods are not necessarily indicative of the results of operations for a full year or any future period.
| Three Months Ended | ||||||||||||||||
| September
30, 2012 (Successor) |
June
30, 2012 (Successor) |
March
31, 2012 (Successor) |
December
31, 2011 (Successor) |
|||||||||||||
| (unaudited) | (unaudited) | (unaudited) | ||||||||||||||
| (in thousands) | ||||||||||||||||
| Statements of Operations: |
||||||||||||||||
| Revenues |
$ | 11,613 | $ | 9,945 | $ | 8,544 | $ | 8,090 | ||||||||
| Income from operations |
963 | 940 | 856 | 602 | ||||||||||||
| Net income |
907 | 883 | 796 | 531 | ||||||||||||
| EBITDA(1) |
1,203 | 1,216 | 1,132 | 871 | ||||||||||||
| (1) | “EBITDA” is defined as net income before interest expense, interest income and depreciation and amortization. EBITDA does not represent, and should not be considered as, an alternative to net income or cash flows from operations, each as determined in accordance with U.S. GAAP. We have presented |
71
Table of Contents
| EBITDA because we consider it an important supplemental measure of our performance and believe that it is frequently used by analysts, investors and other interested parties in the evaluation of companies. Other companies may calculate EBITDA differently than we do. EBITDA has limitations as an analytical tool, and you should not consider it in isolation or as a substitute for analysis of our results as reported under U.S. GAAP. See “—Key Business Metrics.” |
The following is a reconciliation of net income to EBITDA:
| Three Months Ended | ||||||||||||||||
| September
30, 2012 (Successor) |
June
30, 2012 (Successor) |
March
31, 2012 (Successor) |
December
31, 2011 (Successor) |
|||||||||||||
| (unaudited) | (unaudited) | (unaudited) | ||||||||||||||
| (in thousands) | ||||||||||||||||
| Net income |
$ | 907 | $ | 883 | $ | 796 | $ | 531 | ||||||||
| Interest expense |
68 | 62 | 64 | 71 | ||||||||||||
| Interest income |
— | — | — | — | ||||||||||||
| Depreciation and amortization |
228 | 271 | 272 | 269 | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| EBITDA |
$ | 1,203 | $ | 1,216 | $ | 1,132 | $ | 871 | ||||||||
|
|
|
|
|
|
|
|
|
|||||||||
Revenue increased sequentially in all quarters presented primarily due to an increasing number of members, as we continued to enroll new members and retain a large percentage of existing members.
There are seasonal factors that affect our revenue. A large number of undergraduate and post-graduate students complete their studies during the second fiscal quarter of each year and are no longer eligible for health insurance coverage through the insurance plans of their parents or educational institutions. As a result, we experience a higher volume of new member enrollment from these demographics during the third fiscal quarter when such students purchase our products, producing a seasonal increase in revenue. During the fourth quarter of each fiscal year, many of our call centers and licensed agents are closed or maintain shorter business hours for varying periods of time due to the holiday season. We experience a lower volume of new member enrollment during the fourth quarter compared with other quarters, resulting in a seasonal decrease in revenue. We are not expecting a decrease in revenue for the fourth quarter 2012 as compared to the third quarter because of increasing member renewals associated with our increasing member base. However, at the end of the fourth quarter 2012, we expect the number of STM plans in force to decline slightly as compared to the number of STM plans in force at the end of the third quarter 2012 primarily due to a larger than normal decrease in new policies written. We believe the seasonality trends generally resulting in lower volume of new member enrollment in the fourth quarter were mildly exacerbated in 2012 by uncertainty related to the future of Healthcare Reform in the lead-up to the November presidential election as well as the expansion of advance commission structures by our competitors. However, while there can be no assurances, we believe the market confusion related to the election has since dissipated and that with the proceeds of this offering we will be able to effectively compete with other providers that offer advance commission incentives.
Liquidity and Capital Resources
General
As of September 30, 2012, we had $982,000 of cash. Since the fourth quarter of fiscal 2009, we have funded our operations primarily with cash flows from operations and, to a lesser extent, working capital and borrowings, as described below.
During the nine months ended September 30, 2012, Health Plan Intermediaries, LLC paid cash distributions of $2,763,000 to Mr. Kosloske in accordance with the terms of its Operating Agreement. Such payments made to members in 2011 totaled $1,301,000 ($681,000 was paid to Naylor Group Partners, LLC and $620,000 was paid to Mr. Kosloske).
72
Table of Contents
We experienced positive cash flows from operations during 2011. We expect that we will continue to generate positive cash flows from operations on an annual basis, although this may fluctuate significantly on a quarterly basis. We believe that our available cash, cash flows expected to be generated from operations and net proceeds from this offering will be adequate to satisfy our current and planned operations for at least the next 12 months . We believe that the net proceeds of this offering will be sufficient to implement our advance commission strategy. Our future capital requirements will depend on many factors, including our rate of revenue growth, the expansion of our sales and marketing activities, our expansion into other markets and our results of operations. To the extent that existing cash, cash from operations and credit facilities are insufficient to fund our future activities, we may need to raise additional funds through public equity or debt financing. The sale of additional equity could result in additional dilution to our stockholders. If we raise additional funds by obtaining loans from third-parties, the terms of those financing arrangements may include additional covenants or other loan restrictions on our business that could impair our operating flexibility, and would also require us to incur interest expense. We can provide no assurance that additional financing will be available at all or, if available, that we would be able to obtain financing on terms acceptable to us.
Our Indebtedness
Term Loan Agreement. In September 2011, we entered into a bank loan agreement with SunTrust Bank with a principal amount of $4,250,000. The purpose of this bank loan was to finance the Acquisition of the remaining 50% interest in Health Plan Intermediaries, LLC as discussed in “Relationships and Related Party Transactions—Purchase of Membership Interest in Health Plan Intermediaries, LLC.” Seventy-five percent of the loan is guaranteed by the U.S. Small Business Administration. Borrowings under the loan are secured by all of our assets, including, but not limited to, cash accounts, accounts receivable and property and equipment. The loan is further secured with a personal unlimited guarantee by Mr. Kosloske and Lori Kosloske, our Chief Broker Compliance Officer and Mr. Kosloske’s wife, and certain real properties owned by Mr. Kosloske and Mrs. Kosloske in Tampa, Florida and Keystone, Colorado. The loan is a five-year loan bearing fixed interest at 5.25% with equal monthly payments of $81,000. A balance of $3,490,000 remains outstanding as of September 30, 2012, including a current portion of $802,000.
The loan is subject to customary covenants and restrictions which, among other things, limit our ability to incur additional indebtedness. In addition, the loan agreement also includes certain financial covenants that would require immediate payment if we, among other things, reorganize, merge, consolidate, or otherwise change ownership or business structure without the bank’s prior written consent. We have obtained the bank’s written consent in order to effectuate this offering.
The loan agreement also contains customary representations and warranties and events of default. The payment of outstanding principal under the loan and accrued interest thereon may be accelerated and become immediately due and payable upon our default of payment or other performance obligations or our failure to comply with financial or other covenants in the loan agreement, subject to applicable notice requirements and cure periods as provided in the loan agreement.
On January 24, 2013, we signed a commitment letter with SunTrust Bank to supplement the existing bank loan agreement with SunTrust Bank with a new $2,000,000 revolving credit facility. If we enter into and draw on the revolving credit facility, the proceeds will be used to finance costs associated with this offering and to fund advance commission payments to distributors. The new revolving credit facility will have a total commitment for loans up to $2,000,000. The maturity of the new revolving credit facility will be 364 days from the date of closing and the loans will bear interest at a rate of LIBOR plus 3.50%. Borrowings under the revolving credit facility will be collateralized by substantially all of our assets (as well as the pledge of equity interests in Health Plan Intermediaries, LLC owned by Mr. Kosloske and a further assignment of a $4,500,000 life insurance policy on Mr. Kosloske), and SunTrust Bank will have a second lien position behind SunTrust Bank’s existing first lien on substantially all of our assets pursuant to the existing bank loan agreement. The new revolving credit facility will have customary affirmative and negative covenants including, without limitation, a minimum net worth
73
Table of Contents
covenant and limitations on dividends during any event of default. The commitment is conditional upon, among other things, no material adverse change in our business and final negotiation of the credit agreement. The commitment letter expires on March 31, 2013.
We intend to use a portion of the net proceeds of this offering to repay all of the outstanding debt under our term loan. See “Use of Proceeds.”
Cash Flows
The following summary of cash flows for the periods indicated has been derived from our financial statements included elsewhere in this prospectus:
| Nine Months Ended September 30, | Year Ended December 31, | |||||||||||||||
| 2012 | 2011 | 2011 | 2010 | |||||||||||||
| (in thousands) | ||||||||||||||||
| Statements of Cash Flows Data: |
||||||||||||||||
| Net cash provided by (used in) operating activities |
$ | 4,643 | $ | 1,637 | $ | 2,247 | $ | (31 | ) | |||||||
| Net cash used in investing activities |
$ | (213 | ) | $ | (38 | ) | $ | (5,392 | ) | $ | (80 | ) | ||||
| Net cash (used in) provided by financing activities |
$ | (4,066 | ) | $ | (1,305 | ) | $ | 3,757 | $ | 99 | ||||||
Cash Flows from Operating Activities
We experienced positive cash flows from operating activities during 2011 and 2010 primarily as a result of our increased revenues and the resulting net income during these periods. Our primary source of cash from operating activities is retention of commissions from premium equivalents. Our primary uses of cash for operating activities are for compensation-related expenditures, settlement of accounts payable to vendors and to fund our advance commission structure.
During the nine months ended September 30, 2012, cash provided by operating activities was $4,643,000 as compared to $1,637,000 for the nine months ended September 30, 2011. This increase of $3,006,000 was primarily due to an increase in net income as a result of revenue growth, an increase in vendor and carrier payable driven by sales growth and an increase in accounts payable, accrued and deferred expenses. The increase of $1,207,000 in accounts payable, accrued and deferred expenses compared to the prior period was primarily due to increased professional fees in connection with this offering, increased processing fees associated with sales growth and accrued wages driven by an increase in employee headcount in order to accommodate our growth. In addition, the increase in depreciation and amortization of $742,000 is a result of amortization of assets acquired in September 2011.
During the year ended December 31, 2011, cash provided by operating activities was $2,247,000 as compared to net cash used in operations of $(31,000) for the year ended December 31, 2010. This increase of $2,278,000 was primarily due to revenue growth and our scalable technology platform.
Cash Flows from Investing Activities
Our primary investing activities have consisted of purchases of equipment and the Acquisition. Our capital expenditures primarily consist of purchases of computer equipment, furniture and fixtures and computer software. In the future, we expect that we will continue to incur capital expenditures to support our expanding operations.
During the nine months ended September 30, 2012, cash used for investing activities was $213,000 as compared to $38,000 for the nine months ended September 30, 2011. The increase of $175,000 was primarily due to purchases of fixed assets required to support our growth.
During the year ended December 30, 2011, cash used in investing activities was $5,392,000 as compared to $80,000 for the year ended December 30, 2010. The increase of $5,312,000 was primarily due to payments made for the Acquisition.
74
Table of Contents
Cash Flows from Financing Activities
Our financing activities have consisted primarily of issuance of long-term debt, periodic repayments of debt, capital contributions from members and distributions of earnings to our members.
During the nine months ended September 30, 2012, cash used in financing activities of $4,066,000 was primarily attributable to $2,763,000 of distributions made to Mr. Kosloske as sole member of Health Plan Intermediaries, LLC, $863,000 of payments to third-parties in connection with preparation of this offering, $573,000 of principal payments on our term loan, $100,000 of proceeds from a note payable, $50,000 of proceeds from our non-controlling interest in subsidiary and $8,000 of payments on capital leases.
During the year ended December 31, 2011, cash provided by financing activities was $3,757,000 as compared to $99,000 for the year ended December 31, 2010. This increase of $3,658,000 was primarily due to our entering into a bank loan agreement in September 2011 to finance the Acquisition.
Contractual Obligations
The following summarizes our contractual obligations as of September 30, 2012:
| Payments Due by Period | ||||||||||||||||||||
| Total | Less Than 1 Year | 1 to 3 Years | 3 to 5 Years | More Than 5 Years | ||||||||||||||||
| (in thousands) | ||||||||||||||||||||
| Contractual Obligations: |
||||||||||||||||||||
| Operating leases |
$ | 598 | $ | 219 | $ | 378 | $ | 1 | $ | — | ||||||||||
| Software maintenance |
1,508 | 312 | 624 | 572 | — | |||||||||||||||
| Exclusivity agreement |
928 | 192 | 384 | 352 | — | |||||||||||||||
| Payments on debt obligations, including interest |
3,884 | 968 | 1,937 | 979 | — | |||||||||||||||
| Capital lease obligations |
7 | 3 | 4 | — | — | |||||||||||||||
| Other |
100 | 100 | — | — | — | |||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| Total contractual obligations(1) |
$ | 7,025 | $ | 1,794 | $ | 3,327 | $ | 1,904 | $ | — | ||||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
| (1) | Payments to holders of Series B Membership Interests pursuant to our tax receivable agreement are excluded from our contractual obligations. For additional information, see “The Reorganization of Our Structure—Tax Receivable Agreement.” |
Off-Balance Sheet Arrangements
Through September 30, 2012, we had not entered into any off-balance sheet arrangements, other than the operating leases noted above, and do not have any holdings in variable interest entities.
JOBS Act
The JOBS Act contains provisions that, among other things, reduce certain reporting requirements for qualifying public companies. As an “emerging growth company” we have elected under the JOBS Act to delay adoption of new or revised accounting pronouncements applicable to public companies until such pronouncements are made applicable to private companies. Additionally, we are in the process of evaluating the benefits of relying on the other reduced reporting requirements provided by the JOBS Act.
Subject to certain conditions set forth in the JOBS Act, if, as an “emerging growth company”, we choose to rely on such exemptions we may not be required to, among other things, (1) provide an auditor’s attestation report on our system of internal controls over financial reporting pursuant to Section 404, (2) provide all of the compensation disclosure that may be required of non-emerging growth public companies under the Dodd-Frank
75
Table of Contents
Wall Street Reform and Consumer Protection Act, (3) comply with any requirement that may be adopted by the PCAOB regarding mandatory audit firm rotation or a supplement to the auditor’s report providing additional information about the audit and the financial statements (auditor discussion and analysis), and (4) disclose certain executive compensation related items such as the correlation between executive compensation and performance and comparisons of the CEO’s compensation to median employee compensation. These exemptions will apply until the earliest of:
| • | the last day of the fiscal year following the fifth anniversary of the date of our initial public offering of common equity securities; |
| • | the last day of the fiscal year in which we have annual gross revenue of $1.0 billion or more; |
| • | the date on which we have, during the previous three-year period, issued more than $1.0 billion in non-convertible debt; and |
| • | the date on which we are deemed to be a “large accelerated filer,” which will occur at such time as the company (a) has an aggregate worldwide market value of common equity securities held by non-affiliates of $700 million or more as of the last business day of its most recently completed second fiscal quarter, (b) has been required to file annual and quarterly reports under the Securities Exchange Act of 1934 for a period of at least 12 months, and (c) has filed at least one annual report pursuant to the Securities Act of 1934. |
Accordingly, we could remain an “emerging growth company” until as late as December 31, 2018.
Quantitative and Qualitative Disclosures about Market Risk
We are exposed to market risks in the ordinary course of our business. Market risk represents the risk of loss that may impact our financial position due to adverse changes in financial market prices and rates. Our market risk exposure is primarily a result of fluctuations in interest rates.
Interest Rate Risk
We had cash of $982,000 as of September 30, 2012, which consist of bank deposits with FDIC participating banks. The cash on deposit with banks is not susceptible to interest rate risk.
We had outstanding indebtedness of $3,490,000 as of September 30, 2012. Our outstanding indebtedness consists of a fixed rate term loan. Our obligations under the term loan carry interest rates that are fixed and are not subject to fluctuation.
We do not enter into investments for trading or speculative purposes and have not used any derivative financial instruments to manage our interest rate risk exposure.
Inflation Risk
We do not believe that inflation has had a material effect on our business, financial condition or results of operations. If our costs were to become subject to significant inflationary pressures, we may not be able to fully offset such higher costs through price increases. Our inability or failure to do so could harm our business, financial condition and results of operations.
Critical Accounting Policies
Our financial statements are prepared in accordance with United States Generally Accepted Accounting Principles (GAAP). The preparation of these financial statements requires our management to make estimates, assumptions and judgments that affect the reported amounts of assets and liabilities and disclosure of contingent assets and liabilities at the date of the financial statements, and the reported amounts of revenues and expenses during the applicable periods. We base our estimates, assumptions and judgments on historical experience and on
76
Table of Contents
various other factors that we believe to be reasonable under the circumstances. Different assumptions and judgments could change the estimates used in the preparation of our financial statements, which, in turn, could change the results from those reported. We evaluate our estimates, assumptions and judgments on an ongoing basis. The critical accounting estimates, assumptions and judgments that we believe have the most significant impact on our financial statements are described below. We have elected under the JOBS Act to delay adoption of new or revised accounting pronouncements applicable to public companies until such pronouncements are made applicable to private companies. As a result of this election, our financial statements may not be comparable to companies that comply with public company effective dates.
Revenue Recognition
Our revenues consist primarily of commissions earned for our insurance policies and discount benefit plans issued to members, enrollment fees paid by members and administration fees paid by members as a direct result of our enrollment services. The member’s payment includes a combination of premiums, fees for discount benefit plans, fees for distributors and enrollment fees, which are collectively referred to as “premium equivalents.” Reported revenues are net of risk premium remitted to insurance carriers and amounts earned by third-party obligors. Commissions and fees attributable to the sale of STM plans and hospital indemnity policies represent substantially all our revenues for the periods presented. Revenues are net of an allowance for policies expected to be cancelled by members during a limited cancellation period. We establish the allowance for estimated policy cancellations through a charge to revenue. The allowance is estimated using historical data to project future experience. Such estimates and assumptions could change in the future as more information becomes known, which could impact the amounts reported. We periodically review the adequacy of the allowance and record adjustments as necessary. The net allowance for estimated policy cancellations was $43,000 and $12,000 at September 30, 2012 and December 31, 2011, respectively.
Revenue is earned at the time of sale . Commission rates for all of our products are agreed to in advance with the relevant insurance carrier and vary by carrier and policy type. Under our carrier compensation arrangements, the commission rate schedule that is in effect on the policy effective date governs the commissions over the life of the policy. In addition, we earn enrollment and administration fees on policies issued.
We report our revenues net of amounts paid to our contracted insurance carrier companies and third-party obligors as we are not the ultimate party responsible for providing the insurance coverage or discount benefits to the member. As a result, we recognize the net amount of revenues earned as the agent in these transactions.
Goodwill and Intangible Assets
Our intangible assets arose from the Acquisition and consist of goodwill, in-force members, our brand, the carrier network and distributor relationships. Finite-lived intangible assets are amortized over their useful lives from eight months to seven years.
Goodwill and other intangible assets determined to have indefinite useful lives are not amortized, but are tested for impairment, at least annually or more frequently if indicators of impairment arise. Impairment, if any, is based on the excess of the carrying amount over the fair value of those assets. We perform our annual review for goodwill impairment as of October 1 of each year.
The evaluation is performed by comparing the carrying amount of these assets to their estimated fair value. If the estimated fair value is less than the carrying amount of the intangible assets, an impairment charge is recorded to reduce the asset to its estimated fair value. Our valuation methodologies include, but are not limited to, a discounted cash flow model, which estimates the net present value of our projected cash flows and a market approach, which evaluates comparative market multiples applied to our business to yield a second assumed value.
In estimating fair value, our methodology requires us to make assumptions, the most material of which are sales projections attributable to products sold with these trade names and a weighted-average discount rate. These assumptions are subject to change based on changes in the markets in which these products are sold, which
77
Table of Contents
reflect our projections of future revenues. Factors affecting the weighted-average discount rate include assumed debt-to-equity ratios, risk-free interest rates, and equity returns of each of the market participants in our industry.
There have been no events that we believe would result in an impairment of goodwill and intangible assets as of September 30, 2012.
Advanced Commissions
Advanced commissions consist of amounts advanced to certain third-party distributors. We began advancing commissions in November 2011. We perform ongoing credit evaluations of our distributors, all of which are located in the United States. We recover the advanced commissions from future commissions earned on premiums collected. We have not experienced any credit losses from commission advances and accordingly, have not recognized any provision for bad debt expense at September 30, 2012. A fee for the advanced commission of up to 2% of the insurance premiums advanced is charged to the distributors and recognized as other income as earned. Advanced commissions outstanding at September 30, 2012 and December 31, 2011 totaled approximately $300,000 and $24,000, respectively.
Property and Equipment
Property and equipment is carried at cost, less accumulated depreciation. As a result of the Acquisition and the related application of purchase accounting to the acquired assets and liabilities, there is a new basis of property and equipment subsequent to the acquisition date. Depreciation expense for property and equipment is computed using the straight-line method over the estimated useful lives of the respective assets, with two to three years for computer equipment and seven years for furniture and fixtures. Leasehold improvements are depreciated over the shorter of the lease term or estimated useful life. We periodically review long-lived assets for impairment whenever events or changes in business circumstances indicate that the carrying value of the assets may not be recoverable. No impairment losses were recognized for the periods presented.
Change in Accountants
On July 9, 2012, Fabricant, Weissman & Darby, P.A., whom we refer to as the Former Auditors, was dismissed as Health Plan Intermediaries, LLC’s certified public accounting firm. Mr. Kosloske, as sole member of Health Plan Intermediaries, LLC, approved their dismissal on July 9, 2012. The dismissal of the Former Auditors was effective immediately.
The Former Auditors’ audit reports on Health Plan Intermediaries, LLC’s financial statements for fiscal year 2011 and 2010 did not contain any adverse opinion or disclaimer of opinion, and were not qualified or modified as to uncertainty, audit scope or accounting principles.
During the two most recent fiscal years and through the subsequent interim period on or prior to dismissal, (a) there were no disagreements between Health Plan Intermediaries, LLC and the Former Auditors on any matter of accounting principles or practices, financial statement disclosure, or auditing scope or procedure, which disagreements, if not resolved to the satisfaction of the Former Auditors, would have caused the Former Auditors to make reference to the subject matter of the disagreement in connection with its report; and (b) no reportable events as set forth in Item 304(a)(1)(v)(A) through (D) of Regulation S-K of the Securities Act have occurred.
Effective on July 9, 2012, Mr. Kosloske, as sole member of Health Plan Intermediaries, LLC, appointed Ernst & Young LLP as its new independent registered public accounting firm for the fiscal periods from October 1, 2011 to December 31, 2011 (Successor) and January 1, 2011 to September 30, 2011 (Predecessor) and the year ended December 31, 2010 (Predecessor). During the two most recent fiscal years and the interim period preceding the engagement of Ernst & Young LLP, we did not consult with Ernst & Young LLP regarding the application of accounting principles to a specified transaction, either completed or proposed, or any of the matters or events set forth in Item 304(a)(2) of Regulation S-K.
Health Plan Intermediaries, LLC was not a SEC filer at the time of the Former Auditors’ dismissal.
78
Table of Contents
Overview
Our Company
We are a leading developer and administrator of affordable, web-based individual health insurance plans and ancillary products. Our highly scalable, proprietary, web-based technology platform allows for mass distribution of, and online enrollment in, our large and diverse portfolio of affordable health insurance offerings.
Our technology platform provides customers, who we refer to as members, immediate access to our products through our distribution partners anytime, anyplace. The health insurance products we develop are underwritten by insurance carrier companies, and we assume no underwriting, insurance or reimbursement risk. Members can price and tailor product selections to meet their needs, buy policies and print policy documents and identification cards in real-time. Our sales are executed online and offer instant electronic fulfillment. Our technology platform uses abbreviated online applications, some with health questionnaires, to provide an immediate accept or reject decision on applications for all products that we offer. Once an application is accepted, individuals can use our automated payment system to complete the enrollment process and obtain instant electronic access to their policy fulfillment documents, including the insurance policy, benefits schedule and identification cards. We receive credit card and Automated Clearing House (ACH) payments directly from members at the time of sale. Our technology platform provides significant operating leverage as we add members and reduces the costs associated with marketing, selling, underwriting and administering policies.
We are an industry leader in the sale of 12-month short-term medical, or STM, insurance plans, an alternative to traditional Individual Major Medical, or IMM, plans, which provide lifetime renewable coverage. STM plans generally offer qualifying individuals comparable benefits for fixed short-term durations of six or 12 months at approximately half the cost of IMM plans. While applications for IMM insurance may take up to 60 days to process, STM plans feature a streamlined underwriting process offering immediate coverage options. We also offer guaranteed-issue hospital indemnity plans for individuals under the age of 65, which pay fixed cash benefits for covered procedures and services, and a variety of ancillary products such as pharmacy benefit cards, dental plans, vision plans and cancer/critical illness plans that are frequently purchased as supplements to STM and hospital indemnity plans. We design and structure insurance products on behalf of insurance carrier companies, market them to individuals through our large network of distributors and manage member relations via our online member portal, which is available 24 hours a day, seven days a week. Our online enrollment process allows us to aggregate and analyze consumer data and purchasing habits to track market trends and drive product innovation. We have established relationships with several highly rated insurance carriers, including Starr Indemnity & Liability Company, Companion Life, United States Fire (a member of the Crum & Forster group), ING, Markel and CIGNA, among others. In addition, as of September 30, 2012, the large independent distribution network we access consists of 32 licensed agent call centers and 248 wholesalers, including Marsh, eHealthInsurance and MasterCard, among others, that work with over 7,300 licensed brokers. Our data-driven product design, technology platform and extensive distribution network have enabled us to grow our revenues from $11,790,000 in 2010 to $29,878,000 in 2011, and from $21,788,000 in the nine-month period ended September 30, 2011 to $30,102,000 in the nine-month period ended September 30, 2012.
We focus on the large and under-penetrated segment of the U.S. population who are uninsured or underinsured, which includes individuals who are unable to afford traditional IMM premiums, individuals not covered by employer-sponsored insurance plans, such as those who are self-employed as well as small business owners and their employees, and underserved “gap populations” that require insurance due to changes caused by life events, such as new graduates, divorcees, early retirees, military discharges, the unemployed, part-time and seasonal employees and temporary workers. Our target market consists of approximately 64 million Americans, including approximately 50 million Americans who were uninsured in 2010, according to the U.S. Census Bureau, and approximately 14 million non-elderly Americans who purchased individual health insurance plans in 2010, according to a 2010 Kaiser Family Foundation survey. As of September 30, 2012, we had approximately 24,416
79
Table of Contents
STM members. We expect the number of uninsured and underinsured to significantly increase due to the rising costs and burdensome underwriting requirements of traditional IMM plans and a decline in employer-sponsored health insurance programs.
As of September 30, 2012, we had 24,416 STM plans in force, compared with 16,838 on September 30, 2011, with an average monthly retention rate of 80% from September 30, 2011 to September 30, 2012. We earn our revenues from commissions and fees related to the sale of products to our members. Our ancillary products have created several additional revenue streams and resulted in a significant portion of our business being generated by monthly member renewals. For the nine months ended September 30, 2012, our premium equivalents, revenue and EBITDA were $54,549,000, $30,102,000 and $3,551,000, respectively, representing a 42.6%, 38.2% and 89.8% increase compared to premium equivalents, revenues and EBITDA of $38,257,000, $21,788,000 and $1,871,000, respectively, for the nine months ended September 30, 2011. See “Selected Historical Financial and Operational Data” for a discussion regarding the use of premium equivalents and EBITDA as financial measures and for reconciliations to the most directly comparable GAAP financial measures.
Health Insurance Industry and Market Opportunity
We believe ongoing changes in the health insurance industry will expand and reshape our target market. For example, the Patient Protection and Affordable Care Act, or PPACA, and the Health Care and Education Reconciliation Act of 2010, or HCERA, which we refer to, collectively, as Healthcare Reform, were signed into law on March 23, 2010. After facing a number of legal challenges, Healthcare Reform was upheld by the U.S. Supreme Court on June 28, 2012. Healthcare Reform includes a mandate requiring individuals to carry health insurance or face tax penalties; a mandate that certain employers with over 50 employees offer their employees group health insurance coverage or face tax penalties; prohibitions against insurance companies that offer traditional IMM insurance plans using pre-existing health conditions as a reason to deny an application for health insurance; and medical loss ratio, or MLR, requirements that require each health insurance carrier to spend a certain percentage of its IMM premium revenue on reimbursement for clinical services and activities that improve healthcare quality.
According to a 2011 McKinsey survey, the implementation of Healthcare Reform will likely increase the number of Americans in the individual health insurance market from 14 million to more than 100 million starting in 2014. We believe this increase will be primarily driven by two key factors: employers dropping group coverage and an additional 45 million uninsured Americans entering the individual insurance market. The McKinsey survey estimates that approximately 30% of employers would “definitely” or “probably” drop employer-sponsored insurance starting in 2014. The estimated penalty employers will face for not providing their employees coverage is $2,000 per employee for employers with over 50 employees (there is no penalty for employers with less than 50 employees), which is significantly less than the estimated price currently paid for employee coverage ($9,000 to $14,000 per employee). Assuming a 30% drop in employer-sponsored insurance, approximately 50 million Americans would join the individual health insurance market starting in 2014. In addition, because Americans will face penalties if they are uninsured, we expect that a large number of the current uninsured population of 50 million will enter the individual health insurance market. Accordingly, after 2014, we expect that the individual health insurance market will grow more than 600% to over 100 million policyholders, representing annual individual aggregate health insurance premiums in the United States of approximately $361 billion, compared with approximately $50 billion in 2010.
We believe certain dynamics in the health insurance industry present an opportunity to increase our market share in the individual health insurance market. For example, the minimum MLR thresholds require that IMM carriers use 80% of all premiums collected to pay claims. This has significantly reduced distributor commission rates on traditional IMM policies, forcing many distributors to abandon the traditional face-to-face IMM sales model. Starting in 2014, IMM carriers will also be subject to a pre-existing condition mandate, requiring them to accept all customers regardless of their pre-existing conditions. This “must-carry” pre-existing conditions
80
Table of Contents
requirement will further increase the costs of IMM coverage. Unlike traditional IMM plans, our STM products are exempt from the minimum MLR thresholds and “must-carry” pre-existing conditions requirements under Healthcare Reform, allowing us to offer attractive distributor commission rates while providing affordable products for individuals. In addition, Healthcare Reform also requires that states establish health insurance exchanges where uninsured individuals can select and purchase health insurance plans. We believe that these exchanges will further the transition from group-based insurance coverage to individual health insurance coverage, and that our STM products will be an attractive option in the non-subsidized exchange environment. Moreover, consumers are increasingly accessing the Internet to find affordable health insurance solutions. The current number of Internet users in the United States continues to grow and, according to a report published by Pew Research Center, represented 74% of the population in 2010. In addition, according to the same report, 33% of Internet users in 2010 looked online for information related to health insurance. This represents approximately 75 million Americans who used the Internet to access information related to health insurance in 2010.
We intend to aggressively pursue opportunities to help consumers identify our STM products as the right choice for healthcare coverage, and we believe our technology platform, product focus and industry expertise will allow us to gain an increasing share of this growing market.
Our Solutions
We believe that our products address a significant portion of the issues facing the healthcare system in the United States and improve access to coverage for certain underserved segments of the population.
| • | Lack of Access to Health Insurance. Due to the streamlined underwriting process for our STM plans, we are able to provide an instant decision regarding acceptance. Individuals applying for STM coverage only have to answer an abbreviated, online questionnaire regarding the status of their health to screen for risks that cannot be supported by the rate structure and design of the plan before a decision is generated. We also offer hospital indemnity plans under which members are paid fixed dollar amounts by procedure or service according to a defined schedule which includes doctor visits, lab tests, surgeries and hospitalizations. As these plans are not based on an individual’s health status, they guarantee issuance to individuals under the age of 65 and provide a viable coverage alternative for otherwise uninsurable individuals. |
| • | Growing Number of Uninsured and Underinsured Americans. We focus on the large and under-penetrated segment of the U.S. population that is uninsured or underinsured. According to the U.S. Census Bureau, 16% of Americans were uninsured in 2011, representing approximately 50 million individuals. In addition, the percentage of non-elderly Americans with employer-sponsored insurance decreased from 68% in 2000 to 59% in 2009, driving more Americans into the individual health insurance market. The number of uninsured and underinsured Americans continues to grow in part due to reductions in employer-provided health benefits. |
| • | High Cost of Health Insurance. We offer affordable alternatives to IMM. According to the U.S. Census Bureau, approximately 34 million of the 50 million uninsured Americans in 2011 were members of families with annual incomes of less than $50,000. Based on these figures, we estimate that a sizable portion of the uninsured population chooses not to purchase insurance primarily due to its high cost. According to a 2010 Kaiser Family Foundation survey, traditional IMM premiums increased an average of approximately 20% over a 12-month period, while the cost of our STM plans remained stable. In addition, as a result of Healthcare Reform, IMM premiums are expected to increase significantly in price as a result of guaranteed issue requirements for individuals with pre-existing health conditions. For individuals with pre-existing conditions, we currently offer guaranteed-issue hospital indemnity plans and, only where required by state mandate, STM plans. The implementation of Healthcare Reform will not expand our coverage of such individuals, allowing us to continue to offer attractive distributor commission rates while providing affordable products for members. |
81
Table of Contents
Our Competitive Strengths
We have the following key competitive strengths that we believe collectively provide significant barriers to entry:
| • | Value Generated for All Key Constituents. By combining extensive management experience with our technology platform, we have developed a business model that we believe enables us to create a “win-win” proposition for our key constituents. |
| • | Our Carriers. We offer carriers access to a large member base with no covered pre-existing conditions. Our technology platform connects our carriers directly to a large independent distribution network. Our platform also provides our carriers access to real-time sales and membership data. We use this information to assist our carriers in designing products that cater to their target populations. We currently utilize several carrier companies, including Starr Indemnity & Liability Company, Companion Life, United States Fire (a member of the Crum & Forster group), ING, Markel and CIGNA, among others. Our management team has long-standing relationships with most of the major carrier companies we utilize and has not lost a carrier relationship in over 10 years. |
| • | Our Distributors. At a time when commission rates on many health insurance products, including traditional IMM plans, are declining, we provide our distributors with specialized, highly sought-after product offerings and a compensation structure characterized by attractive commission rates and advance payments. We believe our long-standing relationships with most of the major carriers we utilize, as well as our technology platform, which enables real-time underwriting decisions, immediate sales conversions and access to commission data and selling tools, drive demand for distributors to partner with us. We also offer a turnkey solution that allows us to design products that best meet our distributors’ needs. This solution enables us to assist our distributors in choosing between insurance carriers on a single website and allows them to create customized products for their customers by bundling our STM and hospital indemnity products with our various ancillary products into one package. As of September 30, 2012, we utilized a network of 32 licensed agent call centers and 248 wholesalers that work with over 7,300 licensed brokers nationally. |
| • | Our Members. We provide our members with easy access to health insurance coverage at an affordable price. For qualifying individuals, our STM plans offer benefits comparable to traditional IMM plans at approximately half the cost. For example, according to a 2010 Kaiser Family Foundation survey, the average cost for an IMM plan is $3,606 for an individual and $7,102 for a family. However, the average cost for one of our 12-month STM plans is $1,800 for an individual and $3,600 for a family. Our technology platform allows our members to compare and quote prices for a broad spectrum of STM and hospital indemnity products and, after they have made informed purchase decisions, to buy and print policies online. In addition to STM and hospital indemnity plans, we allow our members the opportunity to purchase high quality ancillary products with automatic, monthly renewals at rates that fit our members’ budgets, all at the click of a button. For example, in September 2012, in addition to the 5,489 STM plans that we sold, we successfully cross-sold 3,008 new ancillary products that month. |
| • | Proprietary, Web-Based Technology Platform. We believe our technology platform represents a distinct competitive advantage as it reduces the need for customer care agents and provides significant operating leverage as we add members and product offerings. Our primary technology platform is named A.R.I.E.S. (Automated Real-Time Integrated E System). We believe our business benefits from the increasing trend of Internet use by individuals to research and purchase health insurance. The Internet offers a means of providing individuals access to health insurance products 24 hours a day, seven days a week and, for the carriers and distributors, reduces the cost and time associated with marketing, selling, underwriting and administering these products. We believe our target market is increasingly researching and applying for health insurance products online and shifting away from more traditional buying patterns. We believe our technology platform positions us for strong continued growth due to the following factors: |
| • | Plan and Product Design. Our technology platform provides real-time data that enables us, our carriers and our distributors to receive immediate information on our members, and allows us to design |
82
Table of Contents
| products that meet the changing demands of the market. Our platform also allows individuals to supplement our STM and hospital indemnity offerings with ancillary products such as pharmacy benefit cards, dental plans, vision plans and cancer/critical illness plans and makes it possible for us to instantly offer these products, which can be bundled to fit member needs. |
| • | Sales. Our technology platform combined with our customer service model drives faster sale conversions. The entire underwriting procedure is processed through our technology platform, which uses abbreviated, online health questionnaires and provides an immediate accept or reject decision, allowing for instant electronic fulfillment. Individuals can obtain full access to our technology platform through our distribution partners and can price products, buy policies and print their policy documents and identification cards anytime, anyplace. Our call centers use our technology platform to, among other functions, perform online, real-time electronic quoting, to process electronic applications and to provide instant electronic approval and fulfillment, back-office administrative support and commission reporting. |
| • | Distribution. Our technology platform allows for low cost mass distribution of our products and provides significant operating leverage. Our automated payment system allows us to collect credit card and ACH payments electronically and directly from members and to disburse commission payments to our distributors in advance, weekly or monthly. In addition, the system provides distributors with direct access to commission statements, selling tools, reporting tools (for example, information as to cancelations, failed credit card and ACH payments and persistency, renewal and cross-sell rates) and custom links to support their business. |
| • | Compliance. In addition to our A.R.I.E.S. platform, we have obtained a license to use a technology platform called HiiVe, which we use to implement a highly automated compliance program that has enhanced quality while minimizing overhead and allowed us to offer higher commissions to our distributors. The compliance program enables us to record each enrollment phone call, retrieve archived calls within seconds and score calls based on script adherence. |
| • | Established Long-Standing Insurance Carrier Relationships. Our access to carriers is essential to our business. Our management team has developed close relationships with the senior management teams of many of our insurance carriers, some lasting over 15 years. Our management team has not lost a carrier relationship in over 10 years. We believe that the nature of our relationships with our insurance carriers, combined with our product knowledge and technology platform, allow us to provide value-added products to our members. |
| • | Extensive Long-Term Relationships with Licensed Insurance Distributors. We believe our product expertise, our relationships with multiple insurance carriers, our focus on compliance and our technology platform make us a partner of choice for our distributors. We offer an appealing, incentive-based compensation structure that we believe drives demand for distributors to partner with us. We have extensive knowledge of the individual health insurance products that we design and administer, which allows us to assist our distribution partners in placing business. Our management team has built a broad distribution network and continuously adds new distributors. As of September 30, 2012, we utilized a network of 32 licensed agent call centers and 248 wholesalers that work with over 7,300 licensed brokers. Over the last 12 months, we added over 3,700 licensed brokers, 10 independent licensed broker call centers and 59 wholesalers to our national distributor network. |
| • | Seasoned Management Team. Our management team has substantial experience and long-standing relationships developed over an average of 25 years in the insurance industry. Our management team draws on its industry experience to identify opportunities to expand our business and collaborate with insurance carriers and distributors to help develop products and respond to market trends. In addition, the majority of our management team has worked together under the leadership of Michael W. Kosloske, our Chairman, President, and Chief Executive Officer, for more than a decade. |
83
Table of Contents
Our Strategy
Our objective is to continue to expand our business and increase our presence in the affordable, web-based health insurance solutions market. Our principal strategies to meet this objective are:
| • | Expand and Enhance Distributor Relationships, Distribution Channels and Lead Generation Methods. We believe we will continue to attract new distributors as the insurance marketplace continues to evolve, and we intend to continue to identify large distributor and lead relationships through the following strategies: |
| • | Advance Commission Structure. We will continue to focus on attracting additional distributors through expansion of our advance commission structure. We believe distributors increasingly demand alternative methods to fund the large and growing costs of lead generation. We estimate that these costs usually range from $2 to $20 per lead and represent a significant startup cost for our distributors. We are in the process of growing our advance commission structure, whereby we pay distributors commissions on policies sold in advance of when they would ordinarily be due to the distributor. Commissions are advanced for up to six months and are made to distributors with an established track record of selling our products. In return, we reduce subsequent commission fees payable to the distributor by up to 2% of premiums for each month that we advance commissions. We believe this structure will assist our distributors in funding their lead generation costs and will provide us with a competitive advantage in attracting and retaining distributors and will increase sales. |
| • | Call Centers. We believe we can grow our distribution network organically by developing call center managers and incentivizing them via attractive commissions. As part of this strategy, we assist in enhancing the sales model of many of our current call centers in order to increase efficiencies and maximize returns, and we established our Insurance Academy in June 2012 to expand the number of call centers selling our products. We anticipate that our Insurance Academy operations will closely resemble a “franchise model,” in that we will provide the tools (sales scripts, key metrics, lead programs, compensation programs, technology systems, etc.) for building a profitable and successful call center that focuses on selling our products and leverages our technology. Our goal is to assist in the training of owners and managers, who in return agree to enter into long-term agreements with us, under which they are required to market our products. We anticipate establishing relationships with 10 to 20 new call centers per year through our Insurance Academy initiative. We believe that this will enhance our ability to convert leads from our current distribution channels into sales. |
| • | Lead Generation and Innovative Distributor Relationships. We will continue to identify large and innovative distributor and lead relationships that we believe will increase revenue and diversify distribution. For example, in September 2012, we entered into an agreement whereby MasterCard, through its approved pre-paid card member networks, will assist us in targeting and acquiring new relationships or “leads” for marketing our products. Upon notification from MasterCard of a prospective lead, we will negotiate a separate referral fee arrangement with MasterCard at which point such prospective lead will be identified to us. We will then attempt to enter into an agreement with the prospective lead under which it will provide us with a list of its customers who hold MasterCard prepaid cards or it will directly market our products to those customers on our behalf. For example, we have entered into such an agreement with KEEPS America LLC, or KEEPS, for our prescription benefits cards. When sending their own pre-paid cards to customers, KEEPS includes our prescription benefits cards in the mailing. If the KEEPS customer uses our card, we pay KEEPS and MasterCard referral fees in connection with the distribution. To further expand our lead generation efforts, we will also continue to explore methods of screening member data for key demographic factors to identify populations for whom our products are well suited. |
| • | Increase Sales of Hospital Indemnity and Ancillary Products. We believe we have a significant opportunity to expand our market share in the hospital indemnity market. Our hospital indemnity plans in force have remained relatively stable with approximately 7,000 plans in force at December 31, 2010 and 5,841 plans in force at September 30, 2012. After the implementation of Healthcare Reform in 2014, |
84
Table of Contents
| we expect hospital indemnity plans to be increasingly used to supplement high deductible plans. In addition, our technology platform enables us to sell ancillary products that carry higher profit margins than our core STM products and that can be issued to a broader population than STM plans. Our members demand a wide range of ancillary products, including pharmacy benefit cards and dental, cancer and critical illness plans. Ancillary product policies in force grew from zero at December 31, 2010 to 23,040 at September 30, 2012. We believe we are well-positioned to take advantage of these additional opportunities at the time of sale. |
| • | Enhance Product and Name Recognition . We are focused on increasing our marketing efforts to consumers. We intend to aggressively pursue opportunities to help consumers identify our products as the right choice for health insurance coverage. We are pursuing multiple avenues to increase our brand awareness among distributors, carriers and our target market, such as through our arrangement with MasterCard that introduces our products and name to MasterCard’s large pre-paid card member networks. |
| • | Develop and Establish New and Specialized Products to Meet Consumer Needs. We plan to continue to develop and add new products to our existing portfolio of offerings. By leveraging our technology platform member data, feedback gathered by customer service agents and distributors and expertise in plan design, we believe we are well-positioned to design and bundle products that meet customer needs and add a viable source of revenue for us, our distributors and our carriers. For example, in June 2012, we introduced our cancer plan. We sold 517 of these policies in the first month, and we are currently developing new products, including fully-insured prescription cards. |
Our Products
Our differentiated product offering allows us to build leading positions in our target markets for insurance products and related services. The key products we provide include:
| • | Short-Term Medical Plans. Our STM plans cover individuals for up to six- and 12-month periods with a wide range of co-pay and deductible options at approximately half the cost of traditional IMM plans. For example, according to a 2010 Kaiser Family Foundation survey, the average cost for an IMM plan is $3,606 for an individual and $7,102 for a family. However, the average cost for one of our 12-month STM plans is $1,800 for an individual and $3,600 for a family. STM plans offer similar benefits for qualifying individuals as IMM plans. For example, both STM plans and IMM plans offer a choice of deductibles, a choice of coinsurance, coverage for emergency room care, surgeries, x-rays, lab work, diagnostics, doctor office co-payments, and preferred provider organization or “PPO” network discounts. However, while IMM plans cover prescription drugs, pre-existing conditions and preventive care, STM plans provide optional coverage for prescription drugs and do not cover pre-existing conditions or preventive care unless such coverage is mandated by the state. STM plans do not cover certain medical events such as pregnancy. Additionally, while IMM plans have guaranteed renewability and can be of a permanent duration, STM plan renewal is not guaranteed and STM plans have a limited duration of up to 12 months. Our STM plans provide up to $2 million of lifetime coverage for each insured individual, allow members to choose any doctor or hospital, offer $50 physician office and urgent care co-pays, cover foreign travel and offer phone access to physician services. As of September 30, 2012, we had 24,416 STM plans in force. For the nine months ended September 30, 2012, revenues associated with the sale of our STM plans accounted for approximately 70% of our revenues for the period. |
| • | Hospital Indemnity Plans. Our hospital indemnity plans provide a daily cash benefit for hospital treatment and doctor office visits as well as accidental injury and death or dismemberment benefits. The claims process for hospital indemnity plans is streamlined: the member simply provides proof of hospitalization and the carrier pays the benefits. These policies are primarily used by customers who do not have adequate health insurance and do not qualify for our STM plans or who wish to supplement existing coverage, typically in conjunction with high deductible plans. As of September 30, 2012, we had 5,841 hospital indemnity plans in force. For the nine months ended September 30, 2012, revenues |
85
Table of Contents
| associated with the sale of our hospital indemnity plans accounted for approximately 26% of our revenues for the period. |
| • | Ancillary Products. We provide numerous low-cost ancillary insurance products, including pharmacy benefit cards, dental plans and cancer/critical illness plans. These are typically monthly policies with automatic renewal. As of September 30, 2012, we had 23,040 ancillary product plans in force. For the nine months ended September 30, 2012, revenues associated with the sale of our ancillary products accounted for approximately 4% of our revenues for the period. |
Healthcare Laws and Regulations
Our business is subject to extensive, complex and rapidly changing federal and state laws and regulations. Various federal and state agencies have discretion to issue regulations and interpret and enforce healthcare laws. While we believe we comply in all material respects with applicable healthcare laws and regulations, these regulations can vary significantly from jurisdiction to jurisdiction, and interpretation of existing laws and regulations may change periodically. Federal and state legislatures also may enact various legislative proposals that could materially impact certain aspects of our business. The following are summaries of key federal and state laws and regulations that impact our operations:
Healthcare Reform
In March 2010, Healthcare Reform was signed into law. Healthcare Reform contains provisions that have changed and will continue to change the health insurance industry in substantial ways. For example, Healthcare Reform includes a mandate requiring individuals to be insured or face tax penalties; a mandate that employers with over 50 employees offer their employees group health insurance coverage or face tax penalties; prohibitions against insurance companies that offer traditional IMM plans using pre-existing health conditions as a reason to deny an application for health insurance; MLR requirements that require each health insurance carrier to spend a certain percentage of their premium revenue on reimbursement for clinical services and activities that improve healthcare quality; establishment of state and/or federal health insurance exchanges to facilitate access to, and the purchase of, health insurance; subsidies and cost-sharing credits to make health insurance more affordable for those below certain income levels; and expanded eligibility for Medicaid for individuals and families with incomes of up to 133% of the poverty level.
Healthcare Reform amended various provisions in many federal laws, including the Internal Revenue Code, the Employee Retirement Income Security Act of 1974 and the Public Health Services Act. Healthcare Reform is being implemented by the Department of Health and Human Services, the Department of Labor and the Department of Treasury. These agencies have already issued a number of proposed, interim final and final regulations, as well as general guidance, on key aspects of Healthcare Reform. While many aspects of Healthcare Reform do not become effective until 2014, health insurance carriers have been required to maintain MLRs of 80% in their individual and family health insurance business since the beginning of 2011.
These laws have been the subject of multiple constitutional challenges and the U.S. Supreme Court held hearings in March 2012 in National Federation of Independent Business v. Sebelius to review the constitutionality of Healthcare Reform. On June 28, 2012, the United States Supreme Court released its decision, upholding Healthcare Reform’s mandate requiring individuals to purchase health insurance. Also, under the U.S. Supreme Court’s ruling, states are able to opt out of expanding Medicaid eligibility to families and individuals with incomes up to 133% of the poverty level. Despite the decision, some uncertainty about whether parts of Healthcare Reform or Healthcare Reform in its entirety will remain in effect is expected to continue with the possibility of future litigation with respect to certain provisions as well as legislative efforts to repeal and defund portions of Healthcare Reform or Healthcare Reform in its entirety. We cannot predict the outcome of any future legislation or litigation related to Healthcare Reform. As described under “—Health Insurance Industry and Market Opportunity,” we expect Healthcare Reform to result in profound changes to the individual health insurance market and our business.
86
Table of Contents
Anti-Kickback Laws
In the United States, there are federal and state anti-kickback laws that generally prohibit the payment or receipt of kickbacks, bribes or other remuneration in exchange for the referral of patients or other health-related business. The United States federal healthcare programs’ Anti-Kickback Statute makes it unlawful for individuals or entities knowingly and willfully to solicit, offer, receive or pay any kickback, bribe or other remuneration, directly or indirectly, in exchange for or to induce the referral of an individual to a person for the furnishing or arranging for the furnishing of any item or service for which payment may be made in whole or in part under a federal healthcare program or the purchase, lease or order, or arranging for or recommending purchasing, leasing, or ordering, any good, facility, service, or item for which payment may be made in whole or in part under a federal healthcare program. Penalties for violations include criminal penalties and civil sanctions such as fines, imprisonment, and possible exclusion from federal healthcare programs.
Federal Civil False Claims Act and State False Claims Laws
The federal civil False Claims Act imposes liability on any person or entity who, among other things, knowingly presents, or causes to be presented, a false or fraudulent claim for payment by a federal healthcare program. The “qui tam” or “whistleblower” provisions of the False Claims Act allow a private individual to bring actions on behalf of the federal government alleging that the defendant has submitted a false claim to the federal government, and to share in any monetary recovery. Our future activities relating to the manner in which we sell and market our services may be subject to scrutiny under these laws.
HIPAA, Privacy and Data Security Regulations
By processing data on behalf of our clients and customers, we are subject to specific compliance obligations under privacy and data security-related laws, including the Health Insurance Portability and Accountability Act, or HIPAA, the Health Information Technology for Economic and Clinical Health Act, or the HITECH Act, and related state laws. We are also subject to federal and state security breach notification laws, as well as state laws regulating the processing of protected personal information, including laws governing the collection, use and disclosure of social security numbers and related identifiers.
The regulations that implement HIPAA and the HITECH Act establish uniform standards governing the conduct of certain electronic healthcare transactions and protecting the security and privacy of individually identifiable health information maintained or transmitted by healthcare providers, health plans, and healthcare clearinghouses, all of which are referred to as “covered entities,” and their “business associates” (which is anyone who performs a service on behalf of a covered entity involving the use or disclosure of protected health information and is not a member of the covered entity’s workforce). Our carrier companies’ and our clients’ health plans generally will be covered entities, and as their business associate they may ask us to contractually comply with certain aspects of these standards by entering into requisite business associate agreements.
As part of the payment-related aspects of our business, we may also undertake security-related obligations arising out of the Gramm-Leach-Bliley Act and the Payment Card Industry guidelines applicable to card systems. These requirements generally require safeguards for the protection of personal and other payment related information.
HIPAA Healthcare Fraud Standards
The HIPAA healthcare fraud statute created a class of federal crimes known as the “federal healthcare offenses,” including healthcare fraud and false statements relating to healthcare matters. The HIPAA healthcare fraud statute prohibits, among other things, executing a scheme to defraud any healthcare benefit program while the HIPAA false statements statute prohibits, among other things, concealing a material fact or making a materially false statement in connection with the payment for healthcare benefits, items or services. Entities that are found to have aided or abetted in a violation of the HIPAA federal healthcare offenses are deemed by statute to have committed the offense and are punishable as a principal.
87
Table of Contents
State Privacy Laws
In addition to federal regulations issued under HIPAA, some states have enacted privacy and security statutes or regulations, or State Privacy Laws, that govern the use and disclosure of a person’s medical information or records and, in some cases, are more stringent than those issued under HIPAA. These State Privacy Laws include regulation of health insurance providers and agents, regulation of organizations that perform certain administrative functions such as utilization review or third-party administration, issuance of notices of privacy practices, and reporting and providing access to law enforcement authorities. In those cases, it may be necessary to modify our operations and procedures to comply with these more stringent State Privacy Laws. If we fail to comply with applicable State Privacy Laws, we could be subject to additional sanctions.
Consumer Protection Laws
Federal and state consumer protection laws are being applied increasingly by the United States Federal Trade Commission, or FTC, and states’ attorneys general to regulate the collection, use, storage and disclosure of personal or patient information, through websites or otherwise, and to regulate the presentation of web site content. Courts may also adopt the standards for fair information practices promulgated by the FTC, which concern consumer notice, choice, security and access.
State Insurance Laws
Some of the states in which we operate have laws prohibiting unlicensed persons or business entities, including corporations, from making certain direct and indirect payments or fee-splitting arrangements with licensed insurance agents and brokers. Possible sanctions for violation of these restrictions include loss of license and civil penalties. These statutes vary from state to state, are often vague and have seldom been interpreted by the courts or regulatory agencies.
State insurance laws also require us to maintain an insurance agency or broker license in each state in which we transact health insurance business and adhere to sales, documentation and administration practices specific to that state. In addition, each of our employees who solicits, negotiates, sells or transacts health insurance business for us must maintain an individual insurance agent or broker license in one or more states. Because we transact business in the majority of states, compliance with health insurance-related laws, rules and regulations is difficult and imposes significant costs on our business.
State regulations may also require that individuals enroll in group programs or associations in order to access certain insurance products, benefits and services. We have entered into relationships with such associations in order to provide individuals access to our products. For example, we have an agreement with Med-Sense Guaranteed Association, or Med-Sense, a non-profit association that provides membership benefits to individuals and gives members access to certain of our products. Under the agreement, we primarily market membership in the association and collect certain fees and dues on its behalf. In return, we have sole access to its membership list, and Med-Sense exclusively endorses the insurance products that we offer. Under the agreement, we receive a monthly fee per member. Our agreement with Med-Sense is automatically renewable for one-year terms, unless terminated on 120 days written notice by either party. The agreement is also terminable on 15 days written notice by either party under certain circumstances, such as in the case of a breach of the agreement.
88
Table of Contents
Sales and Marketing
Our sales and marketing initiatives primarily consist of hiring seasoned sales professionals who have worked with or been referred to us by our distributors in order to strengthen our relationships with such distributors, marketing campaigns and attendance at meetings and conferences associated with acquiring new distributors. As we do not distribute insurance products to individuals, we utilize third party distributors to market our products directly to potential members, and are engaged in their own sales and marketing efforts that include investments in lead acquisition, online marketing and customer referrals. We focus on building brand awareness among our distributors and members, increasing the number of distributors and converting sales leads into buyers. Our marketing initiatives include:
Third-Party Distributors. Our third-party distributor acquisition channel consists of independent licensed agent call centers and individual insurance brokers who market directly to individuals. We have established several initiatives to assist these call centers and distributors in helping individuals select our products, including the provision of sales scripting and monitoring services through the HiiVe technology platform discussed under “—Technology.” We generally compensate our distributors for their individual health insurance sales based on the consumer submitting a health insurance application to us. If a marketing partner is licensed to sell health insurance, we may share a percentage of the commission revenue we earn from the health insurance carrier for each member referred by that distributor.
Marketing Partners. Our marketing partner member acquisition channel consists of a network of affiliate partners, including credit card companies, national banks and database marketing services who make our products available to individuals. We have established a pay-for-performance network that drives individuals to our products. These partners generally fall into one of the following categories:
| • | Financial and online services partners in industries such as credit card services, banking, insurance and mortgage and association partners; and |
| • | Employers who do not offer health insurance benefits to their employees or to one or more classes of their employees. |
Carrier Relationships
One of our core strengths is our deep integration with some of the leading insurance carriers in the United States, which enables us to offer our STM, hospital indemnity and ancillary products on our technology platform. We currently have relationships with several insurance carriers, including Starr Indemnity & Liability Company, Companion Life, United States Fire (a member of the Crum & Forster group), ING, Markel and CIGNA, among others. We have entered into written contracts with each of these carriers pursuant to which we are authorized to sell the carriers’ health plans and products in exchange for the payment of commissions that vary by carrier and by plan. These contracts are typically non-exclusive and terminable on short notice by either party for any reason. In some cases, the amendment or termination of an agreement we have with a health insurance carrier may impact the commissions we are paid on health insurance plans and products that we have already sold through the carrier.
For the nine months ended September 30, 2012, Starr Indemnity & Liability Company accounted for approximately 50% of our premium equivalents. The commission percentage used to calculate our commissions under our agreement with Starr Indemnity & Liability Company is based on net written premium and varies by the state of a member’s domicile. The agreement is terminable on 180 days written notice by either party for any reason and may be terminated on shorter notice under certain circumstances, such as in the case of a breach of the agreement.
89
Table of Contents
For the nine months ended September 30, 2012, United States Fire (a member of the Crum & Forster group) accounted for approximately 25% of our premium equivalents. The commission percentage used to calculate our commissions under our agreement with United States Fire (a member of the Crum & Forster group) is based on gross collected premium. Our agreement with United States Fire (a member of the Crum & Forster group) is for automatically renewable one year terms, unless otherwise terminated. The agreement is terminable on 120 days written notice by either party for any reason and may be terminated on shorter notice under certain circumstances, such as in the case of a breach of the agreement.
For the nine months ended September 30, 2012, Companion Life accounted for approximately 19% of our premium equivalents. The commission percentage used to calculate our commissions under our agreement with Companion Life is based on gross written premium. The agreement is terminable on 180 days written notice by either party for any reason and may be terminated on shorter notice under certain circumstances, such as in the case of a breach of the agreement.
To create an improved experience for our members, we regularly evaluate insurance carriers by comparing their market presence and brand, cost competitiveness, breadth of plans, emphasis on improving the customer experience, and ability to integrate with our data systems. We plan to continue to expand and adjust the number of insurance carriers with which we partner.
Technology
Since we began operations in 2008, we have invested significant financial and human resources in building a unique and scalable proprietary, web-based technology platform. Our technology represents a distinct competitive advantage as it reduces the need for customer care agents, the time associated with billing, underwriting, fulfillment, sale and marketing and provides significant operating leverage as we add members and product offerings. We entered into an agreement to purchase the intellectual property rights to certain of the software in August 2012.
The key components of our technology platform include:
| • | Automated Real-Time Integrated E System (A.R.I.E.S.). A.R.I.E.S. is the core of our technology platform. This proprietary technology reduces the need for the continual involvement of customer care representatives after a member has enrolled by allowing him or her to change payment information and print identification cards anytime, anyplace. A.R.I.E.S. also offers distributors an unprecedented ability to manage their business by providing direct access to real-time commission statements, commission payment and real-time sales and membership data (including cancelations, failed credit card and ACH payments, persistency, renewal and cross-sell rates). Key elements of A.R.I.E.S. include: |
| • | Quote-Buy-Print. Individuals access our technology platform through our distribution partners and can quote products and buy and print their policy documents and identification cards anytime, anyplace. |
| • | Automated Underwriting. The entire underwriting process is handled by A.R.I.E.S. through the use of health questionnaires. Because our STM products are largely targeted to healthy individuals who do not have pre-existing conditions, we do not have a traditional underwriting department. Underwriting is an immediate accept or reject decision based on a prospective member’s answers to an abbreviated online health-related questionnaire. |
| • | Multiple Value-Added Products. Consumers can purchase multiple plans and specialty products with the click of a button. Consumers are able to supplement our core STM and hospital indemnity offerings with ancillary products such as pharmacy benefit cards, dental plans, vision plans and cancer/critical illness plans. Our technology platform makes it possible for us to instantly offer these bundled products to fit member needs. |
90
Table of Contents
| • | Turn-Key Solution. Our technology platform is a turnkey solution, allowing distributors to tailor their offering to meet member needs and can be customized to enhance the experience of an affinity group or employer. |
| • | Payment. Our sales are executed online and offer instant electronic fulfillment through our platform, through which we receive credit card ACH payments directly from members at the time of sale. |
| • | Member Services. Members have the ability to log-in and change payment information and print new identification cards, all without the need of a customer service representative. |
| • | HiiVe. The HiiVe technology system streamlines compliance by providing real-time sales scripting and monitoring for distributors to ensure customers are making informed purchase decisions. The compliance system enables us to record each enrollment phone call, retrieve archived calls within seconds and score calls based on script adherence. In addition, this technology has also allowed us to automate our compliance program, enhancing quality while minimizing overhead and thereby allowing us to offer higher commissions to our distributors. |
We rely on BimSym eBusiness Solutions, Inc. and other vendors to provide various services relating to our A.R.I.E.S. technology platform, including hosting, support, maintenance and development services, for which we pay both recurring and one-off fees. A.R.I.E.S. was placed in service in March 2011 through an informal relationship with BimSym. On August 1, 2012, we entered into a software assignment agreement with BimSym pursuant to which we acquired certain proprietary rights to the A.R.I.E.S. software for a one-time payment of $45,000. On August 1, 2012, we also entered into a master services agreement with BimSym with respect to the hosting, support, maintenance and development of our A.R.I.E.S. technology platform. This agreement obligates us to make minimum future payments of $312,000 per year for the next five years. Thereafter, this agreement provides for automatic one-year renewals, unless we notify BimSym of our intent not to renew. Prior to March 2011, the Company contracted with a third party vendor, Carpe Datum L.L.C., to provide some of the services now provided through A.R.I.E.S. The HiiVe technology system is based on software we license from a third-party. For more information see “Risk Factors—We rely on third-party vendors to develop, host, maintain, service and enhance our technology platform” and “Risk Factors—Our failure to obtain, maintain and enforce the intellectual property rights on which our business depends could have a material adverse effect on our business, financial condition and results of operations.”
Seasonality
Our business of marketing individual STM insurance plans is subject to seasonal fluctuations. A large number of undergraduate and post-graduate students complete their studies during the second fiscal quarter of each year and are no longer eligible for health insurance coverage through the insurance plans of their parents or educational institutions. As a result, we experience a higher volume of new member enrollment from these demographics during the third fiscal quarter when such students purchase our products, producing a seasonal increase in revenue. During the fourth quarter of each fiscal year, many of our call centers and licensed agents are closed or maintain shorter business hours for varying periods of time due to the holiday season. We experience a lower volume of new member enrollment during the fourth quarter compared with other quarters, resulting in a seasonal decrease commission revenue. As our business matures, other seasonality trends may develop and the existing seasonality and consumer behavior that we experience may change.
91
Table of Contents
Competition
The market for selling insurance products is highly competitive and the sale of health insurance over the Internet is rapidly evolving. We compete with individuals and entities that offer and sell health insurance products utilizing traditional distribution channels, as well as the Internet. Our current or potential competitors include:
Traditional local insurance agents. There are tens of thousands of local insurance agents across the United States who sell health insurance products in their communities. We believe that the vast majority of these local agents offer health insurance without significantly utilizing the Internet or technology other than simple desktop applications such as word processing and spreadsheet programs. Some traditional insurance agents, however, utilize general agents that offer online quoting services and other tools to obtain quotes from multiple carriers and prepare electronic benefit proposals to share with their potential customers. These general agents typically offer their services only for the small and mid-sized group markets (not the individual and family markets) and operate in only a limited geographic region. Additionally, some local agents use the Internet to acquire new consumer referrals from companies that have expertise in Internet marketing. These “lead aggregator” companies utilize keyword search, primarily paid keyword search listings on Google, Bing and Yahoo! and other forms of Internet advertising, to drive Internet traffic to the lead aggregator’s website. The lead aggregator then collects and sells consumer information to agents and, to a lesser extent, to carriers, both of whom endeavor to close the referrals through traditional offline sales methods.
Health insurance carriers’ “direct-to-member” sales. Some carriers directly market and sell their plans and products to consumers through call centers and their own websites. Although we offer health insurance plans and products for many of these carriers, they also can compete with us by offering their products directly to consumers. Most of these carriers have superior brand recognition, extensive marketing budgets and significant financial resources to influence consumer preferences for searching and buying health insurance online. The carriers we choose to represent, however, do not have a competitive price advantage over us. Because individual and family plan health insurance prices are regulated in all U.S. jurisdictions, a consumer is entitled to pay the same price for a particular plan, whether the consumer purchased the plan directly from one of our carrier companies or from us.
Online agents. There are a number of agents that operate websites and provide a limited online shopping experience for consumers interested in purchasing health insurance (e.g., online quoting of health insurance product prices). Most of these online agents operate in only one or very few states, and some represent only one or a limited number of health insurance carriers. Some online agents also sell non-health insurance products such as auto insurance, life insurance and home insurance. We are one of the leading sources of STM insurance products.
National insurance brokers. Although insurance brokers have traditionally not focused on the affordable STM market, they may enter our markets and could compete with us. These large agencies have existing relationships with many of our carrier companies, are licensed nationwide and have large customer bases and significant financial, technical and marketing resources to compete in our markets. Some of these large agencies and financial services companies, such as eHealthInsurance have partnered with us in order to offer our services to their customer and member bases.
We believe the principal factors that determine our competitive advantage in the online distribution of health insurance include the following:
| • | value added healthcare products; |
| • | strength of carrier relationships and depth of technology integration with carriers; |
| • | proprietary, web-based technology platform; |
92
Table of Contents
| • | data-driven product design; |
| • | highly automated compliance program; |
| • | strength of distribution relationships; and |
| • | proven capabilities measured in years of delivering sales and creating and using reliable technology. |
Employees
As of September 30, 2012, we had 51 employees. We have not experienced any work stoppages and consider our employee relations to be good. None of our employees is represented by a labor union.
Intellectual Property
Our success depends, in part, on our ability to protect our intellectual property and proprietary technology, and to operate our business without infringing or violating the intellectual property or proprietary rights of others. We rely on a combination of copyrights, trademarks, domain names, and trade secrets, intellectual property licenses and other contractual rights (including confidentiality and non-disclosure agreements) to establish and protect our intellectual property and proprietary technology. However, these intellectual property rights may not prevent others from creating a competitive online platform or otherwise competing with us.
We may be unable to obtain, maintain and enforce the intellectual property rights on which our business depends, and assertions by third-parties that we violate their intellectual property rights could have a material adverse effect on our business, financial condition and results of operations. For more information see “Risk Factors—Our failure to obtain, maintain and enforce the intellectual property rights on which our business depends could have a material adverse effect on our business, financial condition and results of operations” and “Risk Factors—Assertions by third-parties that we violate their intellectual property rights could have a material adverse effect on our business, financial condition and results of operations.”
Facilities
We lease 7,858 square feet of space for our headquarters in Tampa, Florida under a lease that expires in 2015. In addition, we sublease approximately 4,000 square feet of space for our Insurance Academy in Boca Raton, Florida under a lease that expires in 2015. We believe that suitable additional or alternative space will be available in the future on commercially reasonable terms to accommodate our foreseeable future expansion.
Legal Proceedings
We are not currently a party to any material litigation proceedings. From time to time, however, we may be a party to litigation and subject to claims incident to the ordinary course of business. Regardless of the outcome, litigation can have an adverse impact on us because of defense and settlement costs, diversion of management resources and other factors.
93
Table of Contents
Executive Officers and Directors
The following table sets forth information regarding our executive officers and directors as of September 30, 2012:
| Name |
Age | Position | ||||
| Michael W. Kosloske |
48 | Chairman, President and Chief Executive Officer | ||||
| Michael D. Hershberger |
49 | Chief Financial Officer, Treasurer and Secretary | ||||
| Gary Raeckers |
70 | Director Nominee, Chief Operating Officer | ||||
| Scott Lingle |
44 | Chief Sales Officer | ||||
| Lori Kosloske |
36 | Chief Broker Compliance Officer | ||||
| Bryan Krul |
37 | Senior Vice President of Sales and Operations | ||||
| Paul E. Avery |
53 | Director Nominee | ||||
| Liana O’Drobinak |
49 | Director Nominee | ||||
| A. Gordon Tunstall |
68 | Director Nominee | ||||
Michael W. Kosloske, our founder, has served as our President and Chief Executive Officer since we began operations in 2008. Mr. Kosloske has served as our Chairman since 2012. Prior to founding our company, from 1987 to 2007, Mr. Kosloske was president of Health Plan Administrators, Inc., or HPA, a fully-insured niche and individual health insurance company that focused on online sales. In 2005, Mr. Kosloske sold HPA to Independence Holding Company, a New York Stock Exchange-listed holding company engaged in the life and health insurance business, and he remained president of HPA until 2007. Previously, from 1986 to 1987, Mr. Kosloske was marketing manager for Dun & Bradstreet Plan Services, Inc., a third-party administrator in Tampa, Florida. Mr. Kosloske holds a bachelor of science degree in risk management and insurance from Florida State University. Mr. Kosloske is married to our Chief Broker Compliance Officer, Lori Kosloske.
Michael D. Hershberger has served as our Chief Financial Officer since 2011. Mr. Hershberger served as senior manager at Baker Tilly, a full service accounting and advisory firm, from 2005 to 2011, where he was responsible for managing housing research. From 2009 until joining us in 2011, Mr. Hershberger also served as president of Med-Sense Guaranteed Association, a non-profit association that provides membership benefits to individuals and gives members access to certain of our products. Previously, from 1996 until 2012, Mr. Hershberger served as president of Urban Solutions, Inc. (formerly Hersh Group, Ltd), a real-estate advisory consulting firm. Prior to 2005, Mr. Hershberger served as chief financial officer of HPA from 1992 to 2002, where he was responsible for oversight of financial reporting and financial operations of certain third-party insurance administrators. From 1988 to 1992, Mr. Hershberger served as commercial loan officer at Draper & Kramer. He served as senior accountant at Coopers & Lybrand from 1985 to 1987. Mr. Hershberger holds a bachelor of science degree in accounting from Augustana College and earned his masters of science degree in urban land economics/finance from the University of Wisconsin Graduate School of Business. He is a Certified Public Accountant in the State of Illinois.
Gary Raeckers has been our Chief Operating Officer since 2010 and is a director nominee. From 2002 to 2004, Mr. Raeckers served as chief operating officer of HPA under the leadership of Mr. Kosloske. From 2009 to 2010, Mr. Raeckers served as the director of operations of Premier Administrative Solutions, where he was responsible for administration, customer service and claims processing. Prior to that, from 2005 to 2009, he served as chief operating officer and chief financial officer of Special Markets Insurance Consultants, Inc. From 2004 to 2005, Mr. Raeckers served as senior vice president of Advantec Solutions, Inc. where he was responsible for benefit administration. Prior to his service with HPA, from 1974 to 2002, Mr. Raeckers served in varying capacities, including chief executive officer and chief operating officer, at Health Plan Services, Inc. and its predecessor company, Plan Services Inc. From 1978 to 1994, Plan Services, Inc. was a wholly owned subsidiary of Dun & Bradstreet Plan Services, Inc.
94
Table of Contents
Scott Lingle serves as our Chief Sales Officer. Prior to joining us in 2011, Mr. Lingle served in various roles, including vice president of sales, at Golden Rule/United Healthcare beginning in 1992. Mr. Lingle holds a bachelor of business management degree from Olivet Nazarene University as well as a registered health underwriter, or RHU, designation from American College.
Lori Kosloske serves as our Chief Broker Compliance Officer. Mrs. Kosloske has served in various capacities with us since we began operations in 2008. Previously, Mrs. Kosloske served as our Vice President from 2011 to 2012 and our Vice President of Special Markets from 2008 to 2011. Prior to joining us, Mrs. Kosloske worked as a reinsurance broker at MarketRe (now ParkRe), a reinsurance brokerage company. From 1998 to 2003, Mrs. Kosloske held various positions at Innovative Insurance Group (InnRe), a reinsurance managing general underwriter, where she served as senior underwriter beginning in 2002. Mrs. Kosloske holds a bachelor of business administration degree from Temple University. Mrs. Kosloske is married to our Chairman, President and Chief Executive Officer, Michael W. Kosloske.
Bryan Krul has served as our Senior Vice President of Sales and Operations since 2010. Prior to joining us, Mr. Krul spent 2005 to 2010 at Independence Holding Company, a New York Stock Exchange-listed holding company engaged in the life and health insurance business, where he most recently served as vice president of eBusiness solutions. From 1998 to 2005, Mr. Krul also served in varying capacities, including director of eCommerce, at HPA under the leadership of Mr. Kosloske. Mr. Krul holds a bachelor of arts degree in communications from the University of South Florida.
Paul E. Avery is a director nominee. Mr. Avery currently serves as chief executive officer and principal of Avery Management Group, a developer of a franchisee network of Carsmetics Expert Accident Repair Centers throughout the Northeast and Texas, a position he has held since February 2010. From 2005 to 2009, Mr. Avery served as chief operating officer of OSI Restaurant Partners, Inc. In 1998, Mr. Avery was elected to the board of directors of OSI Restaurant Partners, Inc. and served as director until 2004. From 1997 to 2004, Mr. Avery served as president of Outback Steakhouse Inc. Mr. Avery holds an associate degree in hotel and restaurant management from Middlesex County College and a bachelor of science degree from Kean University.
Liana O’Drobinak is a director nominee. Ms. O’Drobinak currently serves as chief executive officer of Bay Consulting Partners, an organization focused on strategic and risk advisory consulting services, a position she has held since 2010. From 2005 to 2010, Ms. O’Drobinak served as the managing director for Florida and the vice president for the South Region of Jefferson Wells International, Inc., a subsidiary of Manpower Inc. Prior to joining Jefferson Wells, Inc., Ms. O’Drobinak founded Acclaris, Inc., a global business process outsourcing company, where she was president and chief executive officer from 2001 to 2005. From 1985 to 2001, Ms. O’Drobinak held several positions at Andersen LLP, including partner in charge, business process outsourcing (BPO) for the Southeast Region of the United States. While at Andersen LLP, Ms. O’Drobinak led SEC reporting for several initial public offerings and was involved in merger and acquisition activity across a variety of industries, qualifying her as a financial expert. In 2011, Ms. O’Drobinak was appointed to a second term as a board member of the Florida Prepaid College Board, where she currently serves as chair of a new audit committee and as a member of the investment committee. Ms. O’Drobinak also served on the board and as finance committee chair for St. Joseph’s – Baptist Hospital, served as an audit committee member of Baycare Inc. and on the board and audit committees of Acclaris, Inc. Ms. O’Drobinak holds a master of business administration and bachelor of science degree in accounting from the University of South Florida. She is a Certified Public Accountant and Certified Internal Auditor in the State of Florida.
A. Gordon Tunstall is a director nominee. Mr. Tunstall is the founder, and for more than 25 years has served as president, of Tunstall Consulting, Inc., a provider of strategic consulting and financial planning services. Mr. Tunstall currently serves as a director on the boards of Kforce Inc. and CareKinesis, and he previously served as a director for JLM Industries, Inc., Orthodontics Center of America, Inc., Discount Auto Parts, Inc., Advanced Lighting Technologies Inc., Horizon Medical Products Inc., excelleRX and L.A.T. Sportswear. Given his background as a successful strategic consultant for over 25 years advising a large number
95
Table of Contents
of companies in a variety of industries, Mr. Tunstall provides a unique point of view regarding strategy. Mr. Tunstall holds a bachelor of science degree in accounting from Widener College. We engaged Tunstall Consulting, Inc. for its consulting services in connection with this offering.
Controlled Company
For purposes of the rules of the NASDAQ Global Market, we expect to be a “controlled company” upon completion of this offering. Controlled companies under those rules are companies of which more than 50% of the voting power for the election of directors is held by an individual, a group or another company. We expect that Mr. Kosloske will beneficially own more than 50% of the combined voting power of our common stock upon completion of this offering and will continue to have the right to designate a majority of the members of our board of directors for nomination for election and the voting power to elect such directors following this offering. Accordingly, we expect to be eligible to, and we intend to, take advantage of certain exemptions from corporate governance requirements provided in rules of the NASDAQ Global Market. Specifically, as a controlled company, we would not be required to have (1) a majority of independent directors, (2) a nominating and corporate governance committee composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities, (3) a compensation committee composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities, or (4) an annual performance evaluation of the nominating and corporate governance and compensation committees. Accordingly, you will not have the same protections afforded to stockholders of companies that are subject to all of the applicable rules of the NASDAQ Global Market.
Board Structure
Upon completion of the offering, our board of directors will consist of five members. Our board has determined that each of Mr. Avery and Ms. O’Drobinak is independent under applicable NASDAQ Global Market rules.
In accordance with our amended and restated certificate of incorporation and our amended and restated bylaws that will become effective upon the completion of the offering, each of our directors will serve for a one-year term or until his or her successor is elected and qualified. At each annual meeting of our stockholders, our stockholders will elect the members of our board of directors. There will be no limit on the number of terms a director may serve on our board of directors.
Board Committees
Audit Committee
The audit committee, which is expected to consist of Ms. O’Drobinak (Chairman), Mr. Avery and Mr. Tunstall, will assist the board in overseeing our accounting and financial reporting processes and the audits of our financial statements. In addition, the audit committee will be directly responsible for the appointment, compensation, retention and oversight of the work of our independent registered public accounting firm. The board of directors has determined that Ms. O’Drobinak qualifies as an “audit committee financial expert,” as such term is defined in the rules of the SEC and that Ms. O’Drobinak and Mr. Avery qualify as independent, as such term is defined in the rules of the SEC. We will rely on the phase-in rules of the SEC and the NASDAQ Global Market with respect to the independence of our audit committee. These rules permit us to have an audit committee that has one member that is independent upon the effectiveness of the registration statement of which this prospectus forms a part, a majority of members that are independent within 90 days thereafter and all members that are independent within one year thereafter.
96
Table of Contents
Compensation Committee
Our compensation committee consists of Mr. Avery, Ms. O’Drobinak and Mr. Tunstall (Chairman). Our compensation committee is responsible for assisting our board of directors in discharging its responsibilities relating to (1) setting our compensation program and compensation of our executive officers and directors; (2) monitoring our incentive and equity-based compensation plans; and (3) preparing our compensation committee report required to be included in our proxy statement under the rules and regulations of the SEC.
Nominating and Corporate Governance Committee
Our nominating and corporate governance committee consists of Mr. Avery (Chairman), Ms. O’Drobinak and Mr. Tunstall. Our nominating and corporate governance committee assists our board of directors in identifying individuals qualified to become members of our board of directors consistent with criteria established by our board and in developing our corporate governance principles. This committee’s responsibilities include: (1) evaluating the composition, size and governance of our board of directors and its committees and making recommendations regarding the appointment of directors to our committees; (2) considering stockholder nominees for election to our board of directors; (3) evaluating and recommending candidates for election to our board of directors; (4) leading the self-evaluation process of our board of directors; (5) developing and reviewing our corporate governance guidelines and providing recommendations to the board regarding possible changes; (6) evaluating and recommending management candidates; and (7) performing any other activities the committee deems appropriate, are set forth in the corporate governance guidelines or are requested by the board.
Code of Ethics
Our board of directors will adopt a code of business conduct and ethics that applies to all of our directors, officers and other employees, including our principal executive officer, principal financial officer and principal accounting officer. Any waiver of the code for directors or executive officers may be made only by our board of directors and will be promptly disclosed to our stockholders through publication on our website, www.hiiquote.com. Amendments to the code must be approved by our board of directors and will be promptly disclosed (other than technical, administrative or non-substantive changes). A copy of our code of business conduct and ethics will be posted on our website.
Corporate Governance Guidelines
Our board of directors will adopt corporate governance guidelines that serve as a flexible framework within which our board of directors and its committees operate. These guidelines will cover a number of areas including the size and composition of the board, board membership criteria and director qualifications, director responsibilities, board agenda, roles of the Chairman of the Board, Chief Executive Officer and presiding director, meetings of independent directors, committee responsibilities and assignments, board member access to management and independent advisors, director communications with third parties, director compensation, director orientation and continuing education, evaluation of senior management and management succession planning. Additionally, our board of directors will adopt independence standards as part of our corporate governance guidelines. A copy of our corporate governance guidelines will be posted on our website, www.hiiquote.com.
Compensation Committee Interlocks and Insider Participation
None of our executive officers has served as a member of a compensation committee (or if no committee performs that function, the board of directors) of any other entity that has an executive officer serving as a member of our board of directors.
97
Table of Contents
The following table sets forth information concerning the compensation earned by our chief executive officer, our chief financial officer and our three other most highly compensated executive officers during our fiscal years ended December 31, 2011 and December 31, 2012.
Summary Compensation Table
| Name and Principal Position |
Year | Salary ($) |
Bonus ($) |
All Other Compensation ($) |
Total ($) |
|||||||||||||||
| Michael W. Kosloske (Chairman, President and Chief Executive Officer) |
2012 | 400,000 | 39,559 | (1) | 439,560 | |||||||||||||||
| 2011 | 100,000 | 615,378 | (2) | 22,962 | (3) | 738,340 | ||||||||||||||
| Michael D. Hershberger (Chief Financial Officer, Treasurer, Secretary) |
2012 | 179,762 | 179,762 | |||||||||||||||||
| 2011 | 33,333 | 33,333 | ||||||||||||||||||
| Gary Raeckers (Chief Operating Officer) |
2012 | 217,708 | 217,708 | |||||||||||||||||
| 2011 | 145,000 | 145,000 | ||||||||||||||||||
| Lori Kosloske (Chief Broker Compliance Officer) |
2012 | 170,825 | 5,000 | 23,576 | (4) | 199,402 | ||||||||||||||
| 2011 | 171,104 | 5,000 | 113,997 | (5) | 290,101 | |||||||||||||||
| Bryan Krul (Senior Vice President of Sales and Operations) |
2012 | 180,250 | 35,428 | 215,678 | ||||||||||||||||
| 2011 | 156,250 | 19,293 | 175,543 | |||||||||||||||||
| (1) | Reflects an automobile allowance of $32,857 and club dues of $6,702. |
| (2) | Reflects amounts earned in respect of the 2011 fiscal year. |
| (3) | Reflects an automobile allowance of $16,260 and club dues of $6,702. |
| (4) | Reflects an automobile allowance of $23,576. |
| (5) | Reflects an automobile allowance of $21,324 and commissions of $92,673. |
Outstanding Equity Awards at Fiscal Year End
We had no outstanding equity awards as of the end of our fiscal year ended December 31, 2011.
Severance, Retirement and Change in Control Arrangements
We intend to enter into an employment agreement with Mr. Kosloske with a term beginning on the consummation of this offering and ending on December 31, 2013. Under his agreement, Mr. Kosloske will be entitled to an annual salary of $400,000 and will be eligible to participate in our to be adopted long term incentive plan in accordance with its terms. Unless prior written notice of termination is given by either party prior to its expiration date, the term of the agreement will be automatically extended for successive one-year periods. In the event that the we determine not to extend Mr. Kosloske’s agreement, terminate Mr. Kosloske’s employment without cause (as defined in the agreement) or Mr. Kosloske terminates his employment for good reason (as defined in the agreement), Mr. Kosloske will be entitled to an amount equal to two times the sum of his annual base salary and the greater of (i) his most recently earned annual bonus and (ii) his average annual bonus earned in the three most recently completed calendar years, payable in 24 equal monthly installments beginning on the termination date, provided that Mr. Kosloske executes a general release in our favor. Mr. Kosloske will be subject to non-competition, non-disparagement and non-solicitation covenants that expire 24 months following termination of his employment. Mr. Kosloske will not be entitled to any change in control benefits.
98
Table of Contents
We intend to enter into employment agreements with Mr. Hershberger and Mrs. Kosloske with a term beginning on the consummation of this offering and ending on December 31, 2013. Under each agreement, Mr. Hershberger and Mrs. Kosloske will be entitled to annual salaries of $200,000 and $173,325, respectively. Each will be eligible to participate in our to be adopted long term incentive plan in accordance with its terms. Unless prior written notice of termination is given by either party to an agreement prior to the expiration date, the term of the agreement will be automatically extended for successive one-year periods. In the event that we determine not to extend Mr. Hershberger’s or Mrs. Kosloske’s agreement, terminate Mr. Hershberger’s or Mrs. Kosloske’s employment without cause (as defined in the agreement) or Mr. Hershberger or Ms. Kosloske terminates his or her employment for good reason (as defined in the agreement), Mr. Hershberger or Ms. Kosloske, as the case may be, will be entitled to an amount equal his or her respective annual base salary, payable in 12 equal monthly installments beginning on the termination date, provided that Mr. Hershberger or Mrs. Kosloske, as applicable, executes a general release in our favor. Mr. Hershberger and Mrs. Kosloske will each be subject to non-competition, non-disparagement and non-solicitation covenants that expire 24 months following termination of employment. Neither Mr. Hershberger nor Mrs. Kosloske will be entitled to any change in control benefits.
We are party to “at will” employment agreements with Mr. Raeckers and Mr. Krul pursuant to which each is entitled to a current annual base salary of $225,000 and $180,250, respectively. Mr. Raeckers and Mr. Krul are each subject to non-solicitation and non-competition covenants that expire 12 months after termination of employment. Neither Mr. Raeckers nor Mr. Krul is entitled to any change in control benefits.
We do not maintain any tax-qualified or supplemental retirement or pension plans. We anticipate that, in connection with this offering, we will adopt a tax-qualified 401K defined contribution plan.
Restricted Stock Agreements
Mr. Hershberger’s employment agreement also provides for the award to Mr. Hershberger of restricted shares of our Class A common stock in an amount equal to 3% of the Company’s enterprise value as determined immediately following this offering, 20% of which will vest on the six-month anniversary of this offering and 20% of which will vest on October 1 of each of 2013, 2014, 2015 and 2016, subject to Mr. Hershberger’s continued employment through the relevant vesting date; provided, however, that any unvested shares will vest upon Mr. Hershberger’s death or disability, or termination of employment without cause or for good reason. In addition, any unvested shares will vest in the event Mr. Kosloske ceases to be either our Chief Executive Officer or Chairman of our board.
Director Compensation
Our directors were appointed in connection with our formation in 2012. As a result they received no compensation for their service as a director for the year ended December 31, 2011. Following this offering, our non-employee directors are expected to receive compensation that is commensurate with arrangements offered to directors of newly public companies. We have not nor do we expect to compensate our employee directors for their service on our board of directors. We also expect to reimburse all directors for reasonable out-of-pocket expenses incurred in connection with their service as directors, in accordance with our general expense reimbursement policies. Our independent directors will also be eligible to receive stock options and other equity-based awards when, as and if determined by the nominating, governance and compensation committee.
Long Term Incentive Plan and Awards
We intend to adopt the Health Insurance Innovations, Inc. Long Term Incentive Plan, or LTIP, which will permit us to grant an array of equity-based and cash incentive awards to our named executive officers and other employees and service providers. The following is a summary of the material terms of the LTIP and such awards.
99
Table of Contents
Long Term Incentive Plan
Purpose. The purpose of the LTIP is to motivate and reward those employees and other individuals who are expected to contribute significantly to our success to perform at the highest level and to further our best interests and those of our shareholders.
Eligibility. Our employees, consultants, advisors, other service providers and non-employee directors are eligible to receive awards under the LTIP.
Authorized Shares. Subject to adjustment as described below, 1,250,000 shares of our common stock will be available for awards to be granted under the LTIP. Other than during the current calendar year, no participant may receive under the plan in any calendar year more than 200,000 shares in respect of each of the following two categories of awards: stock options and stock appreciation rights, and no participant may receive in any calendar year more than 525,000 shares in respect of restricted stock, restricted stock units and other stock-based awards. Shares underlying replacement awards (i.e., awards granted as replacements for awards granted by a company that we acquire or with which we combine) and awards that we grant on the closing of this offering will not reduce the number of shares available for issuance under the plan. If an award (other than a replacement award or an award granted on the closing of this offering) expires or is canceled or forfeited, the shares covered by the award again will be available for issuance under the plan. Shares tendered or withheld in payment of an exercise price or for withholding taxes also again will be available for issuance under the plan.
Administration. Our compensation committee will administer the LTIP and will have authority to:
| • | designate participants; |
| • | determine the types of awards to grant, the number of shares to be covered by awards, the terms and conditions of awards, whether awards may be settled or exercised in cash, shares, other awards, other property or net settlement, the circumstances under which awards may be canceled, repurchased, forfeited or suspended, and whether awards may be deferred automatically or at the election of the holder or the committee; |
| • | interpret and administer the plan and any instrument or agreement relating to, or award made under, the plan; |
| • | establish, amend, suspend or waive rules and regulations and appoint agents; and |
| • | make any other determination and take any other action that it deems necessary or desirable to administer the plan. |
Types of Awards. The LTIP will provide for grants of stock options, stock appreciation rights (SARs), restricted stock, restricted stock units (RSUs), performance awards and other stock-based awards.
| • | Stock Options. A stock option is a contractual right to purchase shares at a future date at a specified exercise price. The per share exercise price of a stock option (other than a replacement award) will be determined by our compensation committee and may not be less than the closing price of a share of our common stock on the grant date. The committee will determine the date after which each stock option may be exercised and the expiration date of each option, provided that no option will be exercisable more than ten years after the grant date. Options that are intended to qualify as incentive stock options must meet the requirements of Section 422 of the Internal Revenue Code. |
| • | SARs. SARs represent a contractual right to receive, in cash or shares, an amount equal to the appreciation of one share of our common stock from the grant date. Any SAR will be granted subject to the same terms and conditions as apply to stock options. |
| • | Restricted Stock. Restricted stock is an award of shares of our common stock that are subject to restrictions on transfer and a substantial risk of forfeiture. |
100
Table of Contents
| • | RSUs. RSUs represent a contractual right to receive the value of a share of our common stock at a future date, subject to specified vesting and other restrictions. |
| • | Performance Awards. Performance awards, which may be denominated in cash or shares, will be earned on the satisfaction of performance conditions specified by our compensation committee. The committee will have authority to specify that any other award granted under the LTIP will constitute a performance award by conditioning the exercisability or settlement of the award on the satisfaction of performance conditions. Every performance award that is intended to constitute “performance-based compensation” for purposes of Section 162(m) of the Internal Revenue Code will include a pre-established formula, such that payment, retention or vesting of the award is subject to achievement of a level of or increases in one or more of the following performance measures relating to the Company or any of its subsidiaries or business units: overhead costs, general and administration expense, market price of a share, market price appreciation of share value, cash flow, reserve value, net asset value, firm value, economic value added, earnings, earnings per share, total shareholder return, net income, operating income, cash from operations, increases in hospital indemnity plans in force, improvements in capital structure, revenue growth, margin, pre-tax income, EBIT (earnings before interest and taxes), EBITDA (earnings before interest, taxes, depreciation and amortization), net capital employed, return on assets, stockholder return, reserve replacement, return on equity, return on capital, production, assets, asset turnover, inventory turnover, unit volume, sales, sales growth, capacity utilization, market share, increase in customer base, environmental health and safety, diversity, quality, or strategic business criteria. These performance criteria may be measured on an absolute (e.g., plan or budget) or relative basis. Relative performance may be measured against a group of peer companies, a financial market index or other acceptable objective and quantifiable indices. The maximum amount of any cash-denominated performance award intended to comply with Section 162(m) that may be earned in any calendar year may not exceed $2,000,000. |
| • | Other Stock-Based Awards. Our compensation committee will be authorized to grant other stock-based awards, which may be denominated in shares of our common stock or factors that may influence the value of our shares, including convertible or exchangeable debt securities, other rights convertible or exchangeable into shares, purchase rights for shares, awards with value and payment contingent on our performance or that of our business units or any other factors that the committee designates. |
Adjustments. In the event that, as a result of any dividend or other distribution, recapitalization, stock split, reverse stock split, reorganization, merger, amalgamation, consolidation, split-up, spin-off, combination, repurchase or exchange of shares of our common stock or other securities, issuance of warrants or other rights to purchase our shares or other securities, issuance of our shares pursuant to the anti-dilution provisions of our securities, or other similar corporate transaction or event affecting our shares, an adjustment is appropriate to prevent dilution or enlargement of the benefits or potential benefits intended to be made available under the LTIP, the compensation committee will adjust equitably any or all of:
| • | the number and type of shares or other securities that thereafter may be made the subject of awards, including the aggregate and individual limits under the plan; |
| • | the number and type of shares or other securities subject to outstanding awards; and |
| • | the grant, purchase, exercise or hurdle price for any award or, if deemed appropriate, make provision for a cash payment to the holder of an outstanding award. |
Termination of Service and Change in Control. Our compensation committee will determine the effect of a termination of employment or service on outstanding awards, including whether the awards will vest, become exercisable, settle or be forfeited (including by way of repurchase by the company at par value). In the event that a participant is involuntarily terminated other than for cause, or a participant terminates employment for good reason, if applicable, in either case within 24 months following a change in control (as defined in the LTIP),
101
Table of Contents
unvested stock options and SARS shall become vested, restrictions applicable to restricted stock and restricted stock units shall lapse and performance awards shall be deemed to have been satisfied at target.
Amendment and Termination. Our board of directors may amend, alter, suspend, discontinue or terminate the LTIP, subject to approval of our shareholders if required by the rules of the stock exchange on which our shares are principally traded. Our compensation committee may amend, alter, suspend, discontinue or terminate any outstanding award. However, no such board or committee action that would materially adversely affect the rights of a holder of an outstanding award may be taken without the holder’s consent, except to the extent that such action is taken to cause the LTIP to comply with applicable law, stock market or exchange rules and regulations or accounting or tax rules and regulations. In addition, the committee may amend the LTIP in such manner as may be necessary to enable the plan to achieve its stated purposes in any jurisdiction in a tax efficient manner and in compliance with local rules and regulations.
Term. The LTIP expires after ten years, unless prior to that date the maximum number of shares available for issuance under the plan has been issued or our board of directors terminates the plan.
Awards under the LTIP
The LTIP provides that certain executives may receive SARs following the closing of this offering that will have a seven-year term and a three-year cliff vesting period. Vesting of these SARs will fully accelerate if the executive’s employment is terminated due to his death or “disability,” by us without “cause” or by him for “good reason” (as such terms are defined in his employment agreement). In addition, if we undergo a change in control, the SARs will vest on the date of the change in control. If the executive’s employment is terminated by us for cause or by him without good reason at any time, the unvested SARs will be canceled.
The LTIP provides that certain executives may also receive restricted shares following the closing of this offering that will be subject to both service and performance conditions. On the third anniversary of the grant date, the service condition applicable to these restricted shares will be deemed met, subject generally to the executive’s continued employment through each anniversary date. The performance condition will be determined prior to grant of these restricted shares.
On termination of the executive’s employment due to his death or disability, by us without cause or by him for good reason, both the service and the performance conditions of any unvested restricted shares will be deemed met. If the executive terminates his employment without good reason, any unvested restricted shares will be forfeited (or, in the committee’s sole discretion, if required pursuant to applicable law to effect such forfeiture, such shares may be repurchased at their par value). If we undergo a change in control, any unvested restricted shares will fully vest.
On vesting of any of these restricted shares, the restrictions will lapse and, subject to the restrictions on transfer that apply to our officers and directors and certain of our shareholders, and any additional restrictions under any applicable lock up agreement, the shares will be fully transferable. Prior to vesting, the executives will have the right to vote the restricted shares and to receive current payment in respect of dividends paid on shares of our common stock.
The LTIP provides that we may also issue performance-based cash incentive awards following the closing of this offering. These awards will vest one year after the grant date, subject to the performance conditions of GAAP revenues as showing the company’s audited financial statements and EBITDA. On termination of the executive’s employment due to his death or disability, a pro rata portion of the target award based on the percent of time worked will vest and become payable on the scheduled vesting date. If we undergo a change in control, the terms of the applicable employment agreement will govern the vesting of the award.
102
Table of Contents
RELATIONSHIPS AND RELATED TRANSACTIONS
In addition to the compensation arrangements with directors and executive officers described under “Executive Compensation,” the following is a description of each transaction since January 1, 2010, and each currently proposed transaction in which:
| • | we have been or are to be a participant; |
| • | the amount involved exceeded or will exceed $120,000; and |
| • | any of our directors, executive officers, beneficial holders of more than 5% of our capital stock, or any member of their immediate family or person sharing their household had or will have a direct or indirect material interest. |
Proposed Transactions with Health Insurance Innovations, Inc.
In connection with the reorganization, we will engage in certain transactions with entities controlled by Mr. Kosloske, our Chairman, President and Chief Executive Officer, that will become beneficial owner of 5% or more of our voting securities through ownership of shares of our Class B common stock. These transactions are described in detail under “The Reorganization of Our Corporate Structure.”
Amended and Restated Limited Liability Company Agreement of Health Plan Intermediaries Holdings, LLC
Following our reorganization and this offering, we will operate our business through Health Plan Intermediaries Holdings, LLC and its consolidated subsidiaries. The operations of Health Plan Intermediaries Holdings, LLC, and the rights and obligations of its members will be governed by the amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC. We will serve as sole managing member of Health Plan Intermediaries Holdings, LLC. As such, we will control its business and affairs and will be responsible for the management of its business.
The amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC will establish two classes of equity: Series A Membership Interests and Series B Membership Interests. Series A Membership Interests may be issued only to us as the sole managing member of Health Plan Intermediaries Holdings, LLC. Series B Membership Interests may be issued only to persons or entities we permit, which initially will be Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske. For a description of the Amended and Restated Limited Liability Company Agreement of Health Plan Intermediaries Holdings, LLC and the rights provided to holders of Series A Membership Interests and Series B Membership Interests thereunder, see “The Reorganization of Our Corporate Structure—Amended and Restated Limited Liability Company Agreement of Health Plan Intermediaries Holdings, LLC.”
Exchange Agreement
We will enter into an exchange agreement with the existing and certain future holders of Series B Membership Interests of Health Plan Intermediaries Holdings, LLC, which initially will be Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske. Pursuant to and subject to the terms of the exchange agreement and the amended and restated limited liability company agreement of Health Plan Intermediaries Holdings, LLC, holders of Series B Membership Interests, at any time and from time to time, may exchange one or more Series B Membership Interests, together with an equal number of shares of our Class B common stock, for shares of our Class A common stock on a one-for-one basis, subject to equitable adjustments for stock splits, stock dividends and reclassifications. For a description of the exchange agreement, see “The Reorganization of Our Corporate Structure—Amended and Restated Limited Liability Company Agreement of Health Plan Intermediaries Holdings, LLC—Exchange Agreement.”
103
Table of Contents
Tax Receivable Agreement
Assuming the underwriters do not exercise their over-allotment option, this offering is not anticipated to result in an increase in the tax basis in our share of the tangible and intangible assets of Health Plan Intermediaries Holdings, LLC. However, the purchase of Series B Membership Interests (together with an equal number of shares of our Class B common stock) with the net proceeds of the sale of any over-allotment shares, as well as subsequent exchanges of Series B Membership Interests, together with an equal number of shares of our Class B common stock, for shares of our Class A common stock, are expected to increase our tax basis in our share of Health Plan Intermediaries Holdings, LLC’s tangible and intangible assets. These increases in tax basis are expected to increase our depreciation and amortization deductions and create other tax benefits and therefore may reduce the amount of tax that we would otherwise be required to pay in the future.
After giving effect to the reorganization, we will enter into a tax receivable agreement with the existing and certain future holders of Series B Membership Interests (initially Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske). The agreement will require us to pay to such holders 85% of the cash savings, if any, in U.S. federal, state and local income tax we realize (or are deemed to realize in the case of an early termination payment, a change in control or a material breach by us of our obligations under the tax receivable agreement) as a result of any possible future increases in tax basis described above and of certain other tax benefits related to entering into the tax receivable agreement, including tax benefits attributable to payments under the tax receivable agreement itself. This will be our obligation and not an obligation of Health Plan Intermediaries Holdings, LLC. We will benefit from the remaining 15% of any realized cash savings. For a description of the tax receivable agreement, see “The Reorganization of Our Corporate Structure—Tax Receivable Agreement.”
Purchase of Membership Interest in Health Plan Intermediaries, LLC
On September 28, 2011, we entered into an agreement to purchase the units of Health Plan Intermediaries, LLC owned by Naylor Group Partners, LLC for $5,330,000 plus closing costs of $135,000. This purchase was financed with a loan from a bank for $4,250,000 and by a cash payment of $1,135,000 made by Mr. Kosloske to the Naylor Group Partners, LLC. Borrowings under the loan are secured by all of our assets, including, but not limited to, cash accounts, accounts receivable and property and equipment. The loan is further secured with a personal unlimited guarantee by Mr. Kosloske and Mrs. Kosloske and certain real properties owned by Mr. Kosloske and Mrs. Kosloske in Tampa, Florida and Keystone, Colorado.
Prior to the purchase, Health Plan Intermediaries, LLC was 50% owned by Naylor Group Partners, LLC and 50% owned by Mr. Kosloske. Following the purchase, Mr. Kosloske became the sole member of Health Plan Intermediaries, LLC.
Employment Contracts
In August 2008, we entered into an employment arrangement with Mr. Kosloske under which he receives on an annual basis all net revenues from the sale of certain prescription (Rx) contracts, in an amount not to exceed $214,000, plus commissions based on yearly revenues. This compensation is treated as guaranteed payments and totaled $615,000 for 2011 and $485,000 for 2010. Such compensation does not relate to any investment in us made by Mr. Kosloske. The employment agreement terminated on September 28, 2011. Mr. Kosloske has not received revenues from the sale of prescription contracts or commissions based on yearly revenues since October 2011, and he will not receive such revenues under any current or proposed employment contract. We will enter into a new employment contract with Mr. Kosloske in connection with this offering. See “Executive Compensation.”
104
Table of Contents
Other Relationships
During the nine months ended September 30, 2012, we paid Mr. Kosloske approximately $126,000 for unreimbursed expenses paid by Mr. Kosloske on behalf of the Company. This amount represented commissions payable to Lori Kosloske of approximately $93,000 and general business expenses of approximately $33,000.
In February 2012, we entered into a relationship with Tunstall Consulting Inc. for consulting services in connection with this offering. A. Gordon Tunstall, one of our director nominees, is the founder and president of Tunstall Consulting Inc. During the nine months ended September 30, 2012, we paid $407,000 to Tunstall Consulting Inc.
In March 2008, we entered into a relationship with Med-Sense Guaranteed Association, or Med-Sense, a non-profit association that provides membership benefits to individuals and gives members access to certain of our products. Michael D. Hershberger, our Chief Financial Officer, was president of Med-Sense until October 2011, when he resigned as president and joined us as one of our officers. We paid $434,000 and $68,000 to Med-Sense in 2011 and 2010, respectively.
Executive Management Fees
The Naylor Group Partners, LLC, the former owners of 50% of the units of the Health Plan Intermediaries, LLC, performed certain executive management services for us in 2011 and 2010. These executive management services generally consisted of advice in connection with participation in board of managers meetings. The amount paid totaled $231,000 for 2011 and $25,000 for 2010. We terminated the services arrangement with the Naylor Group Partners, LLC in connection with the transaction described under “—Purchase of Membership Interest in Health Plan Intermediaries, LLC.”
Distribution to Members
In accordance with terms of its Operating Agreement, Health Plan Intermediaries, LLC paid cash distributions in 2011 and 2010 totaling $1,301,000 ($681,000 was paid to Naylor Group Partners, LLC and $620,000 was paid to Mr. Kosloske) and $0, respectively. During the nine months ended September 30, 2012, Health Plan Intermediaries, LLC paid cash distributions of $2,763,000 to Mr. Kosloske in accordance with the terms of its Operating Agreement.
Employment Arrangements With Immediate Family Members of Our Executive Officers
Lori Kosloske, the wife of Mr. Kosloske, is employed by us. During 2012 and 2011, Mrs. Kosloske had total cash compensation of $199,402 and $290,101, respectively.
Registration Rights Agreements
In connection with the completion of this offering, we will enter into a registration rights agreement with Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, which are beneficially owned by Mr. Kosloske to register in certain circumstances for sale under the Securities Act shares of our Class A common stock to be delivered in exchange for Series B Membership Interests in certain circumstances. This agreement will provide these two entities (and their affiliates) with the right to require us to register shares of our Class A common stock held by such entities or their affiliates. For a description of these registration rights, see “The Reorganization of Our Corporate Structure—Registration Rights Agreement.”
105
Table of Contents
Policies and Procedures for Related Party Transactions
Our board of directors will adopt a written related person transaction policy, to be effective upon the closing of this offering, setting forth the policies and procedures for the review and approval or ratification of related person transactions. This policy will cover any transaction, arrangement or relationship, or any series of similar transactions, arrangements or relationships, in which we were or are to be a participant and a related person had or will have a direct or indirect material interest, as determined by the audit committee of our board of directors, including, purchases of goods or services by or from the related person or entities in which the related person has a material interest, and indebtedness, guarantees of indebtedness or employment by us of a related person. In reviewing any such proposal, our audit committee will be tasked to consider all relevant facts and circumstances, including the commercial reasonableness of the terms, the benefit or perceived benefit, or lack thereof, to us, opportunity costs of alternate transactions, the materiality and character of the related person’s direct or indirect interest and the actual or apparent conflict of interest of the related person.
All related party transactions described in this section occurred prior to adoption of this policy and as such, these transactions were not subject to the approval and review procedures set forth in the policy.
106
Table of Contents
The following table sets forth information regarding beneficial ownership of our Class A common stock and Class B common stock immediately prior to the initial public offering, after giving effect to the reorganization transactions described under “The Reorganization of Our Corporate Structure,” by:
| • | each person whom we know to own beneficially more than 5% of our Class A or Class B common stock; |
| • | each of the directors and named executive officers individually; and |
| • | all directors and executive officers as a group. |
The number of shares of Class A common stock outstanding after this offering includes 4,666,667 shares of Class A common stock being offered for sale by us in this offering and assumes no exercise of the underwriters’ over-allotment option. The percentage of beneficial ownership for the following table is based on zero shares of Class A common stock and 8,666,667 shares of Class B common stock outstanding immediately prior to the initial public offering, and 4,666,667 shares of Class A common stock and 8,666,667 shares of Class B common stock outstanding after the completion of this offering and assumes no exercise of the underwriters’ over-allotment option. To our knowledge, except as indicated in the footnotes to this table and pursuant to applicable community property laws, the persons named in the table have sole voting and investment power with respect to all shares of Class A or Class B common stock.
| Shares of Class A Common Stock Beneficially Owned |
Percentage of Shares of Class A Common Stock Beneficially Owned |
Shares of Class B Common Stock Beneficially Owned |
Percentage of Shares of Class B Common Stock Beneficially Owned |
|||||||||||||||||||||
| Name of Beneficial Owner |
Before Offering |
After Offering |
Before Offering |
After Offering |
||||||||||||||||||||
| Named executive officers and directors: |
||||||||||||||||||||||||
| Michael W. Kosloske(1) |
— | — | — | 8,666,667 | 100.0 | % | 100.0 | % | ||||||||||||||||
| Michael D. Hershberger |
— | — | — | — | — | — | ||||||||||||||||||
| Gary Raeckers |
— | — | — | — | — | — | ||||||||||||||||||
| Lori Kosloske |
— | — | — | — | — | — | ||||||||||||||||||
| Bryan Krul |
— | — | — | — | — | — | ||||||||||||||||||
| Paul E. Avery |
— | — | — | — | — | — | ||||||||||||||||||
| Liana O’Drobinak |
— | — | — | — | — | — | ||||||||||||||||||
| A. Gordon Tunstall |
— | — | — | — | — | — | ||||||||||||||||||
| All directors and executive officers as a group (eight people) |
— | — | — | 8,666,667 | 100.0 | % | 100.0 | % | ||||||||||||||||
| Greater than 5% Stockholders: |
||||||||||||||||||||||||
| Health Plan Intermediaries, LLC(1) |
— | — | — | 8,666,667 | 100.0 | % | 100.0 | % | ||||||||||||||||
| (1) | Consists of 8,580,000 shares of Class B common stock held of record by Health Plan Intermediaries, LLC and 86,667 shares of Class B common stock held by Health Plan Intermediaries Sub, LLC. As managing member of Health Plan Intermediaries Sub, LLC, Health Plan Intermediaries, LLC has sole voting and dispositive power over the shares held by Health Plan Intermediaries Sub, LLC. Michael W. Kosloske, our Chairman, President and Chief Executive Officer, is the is the sole member and primary manager of Health Plan Intermediaries, LLC and has sole voting and dispositive power over the shares held by Health Plan Intermediaries, LLC. We refer to Health Plan Intermediaries, LLC, Health Plan Intermediaries Sub, LLC and Mr. Kosloske as the Existing Stockholders. The Existing Stockholders may be deemed to have formed a “group” within the meaning of Section 13(d) under the Exchange Act, and the group may be deemed, collectively, to beneficially own all the shares of Class B common stock held of record by each of Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC. The shares of Class B common stock, together with the Series B Membership Interests of Health Plan Intermediaries Holdings, LLC owned of record by the Existing Stockholders, are exchangeable at the Existing Stockholders’ option into an equal |
107
Table of Contents
| number of shares of Class A common stock, representing 65% of the shares of Class A common outstanding stock after this offering. Under SEC rules, the Existing Stockholders are deemed the beneficial owner of such number of shares of Class A common stock. The shares of Class A common stock and Class B common stock vote together as a single class on matters submitted to a vote of our stockholders. The address of each Existing Stockholder is 15438 N. Florida Avenue, Suite 201, Tampa, Florida 33613. |
108
Table of Contents
The following descriptions are summaries of the material terms of our amended and restated certificate of incorporation and amended and restated bylaws that will be in effect upon the consummation of this offering. Reference is made to the more detailed provisions of, and the descriptions are qualified in their entirety by reference to, the amended and restated certificate of incorporation and amended and restated bylaws, forms of which are filed with the SEC as exhibits to the registration statement of which this prospectus is a part, and applicable law.
General
Following this offering, our authorized capital stock will consist of 100,000,000 shares of Class A common stock, par value $0.001 per share, 20,000,000 shares of Class B common stock, par value $0.001 per share and 5,000,000 shares of preferred stock, par value $0.001 per share.
Class A Common Stock
Class A common stock outstanding. Immediately prior to the completion of this offering, there were no outstanding shares of our Class A common stock, and all of the outstanding common stock of Health Insurance Innovations, Inc., par value $0.01 per share (which has been designated as Common Stock in our certificate of incorporation), was held of record by Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, entities beneficially owned by Michael W. Kosloske, our Chairman, President and Chief Executive Officer. There will be 4,666,667 shares of Class A common stock outstanding, assuming no exercise of the underwriters’ over-allotment option, after giving effect to the sale of the shares of Class A common stock offered hereby. All outstanding shares of Class A common stock are fully paid and non-assessable, and the shares of Class A common stock to be issued upon completion of this offering will be fully paid and non-assessable.
Voting rights. The holders of Class A common stock are entitled to one vote per share on all matters to be voted upon by the stockholders.
Dividend rights. Subject to preferences that may be applicable to any outstanding preferred stock, the holders of Class A common stock are entitled to receive ratably such dividends, if any, as may be declared from time to time by the board of directors out of funds legally available therefor. See “Dividend Policy.”
Rights upon liquidation. In the event of liquidation, dissolution or winding up of Health Insurance Innovations, Inc., the holders of Class A common stock are entitled to share ratably in all assets remaining after payment of liabilities, subject to prior distribution rights of preferred stock, if any, then outstanding.
Other rights. The holders of our Class A common stock have no preemptive or conversion rights or other subscription rights. There are no redemption or sinking fund provisions applicable to the Class A common stock. The rights, preferences and privileges of holders of our common stock will be subject to those of the holders of any shares of our preferred stock we may issue in the future.
Class B Common Stock
Issuance of Class B Common Stock with Membership Interests. Immediately prior to the completion of this offering, we intend to amend and restate our certificate of incorporation to reclassify each outstanding share of Common Stock held of record by Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, as 86,667.67 shares of Class B common stock, par value $0.001 per share. Following this offering, shares of our Class B common stock are issuable only in connection with the issuance of Series B Membership Interests of
109
Table of Contents
Health Plan Intermediaries Holdings, LLC. When a Series B Membership Interest is issued by Health Plan Intermediaries Holdings, LLC, we will issue the holder one share of our Class B common stock. Each share of our Class B common stock will be redeemed and cancelled by us if the holder exchanges one Series B Membership Interest and such share of Class B common stock for one share of Class A common stock pursuant to the terms of the exchange agreement, the form of which is filed as an exhibit to the registration statement of which this prospectus forms a part. See “The Reorganization of our Corporate Structure—Amended and Restated Limited Liability Company Agreement of Health Plan Intermediaries Holdings, LLC—Exchange Agreement.”
Voting Rights. Our Class B stockholders will be entitled to one vote for each share held of record on all matters submitted to a vote of our stockholders. Our Class A stockholders and Class B stockholders will vote together as a single class on all matters (including the election of directors) submitted to a vote of stockholders, unless otherwise required by law. Delaware law would require either our Class A stockholders and Class B stockholders to vote separately as a single class in the following circumstances:
| • | if we amend our amended and restated certificate of incorporation to increase the authorized shares of a class of stock, or to increase or decrease the par value of a class of stock, then such class would be required to vote separately to approve the proposed amendment; or |
| • | if we amend our certificate of incorporation in a manner that alters or changes the powers, preferences or special rights of a class of stock in a manner that affects holders of such class of stock adversely then such class would be required to vote separately to approve such proposed amendment. |
Dividend rights. Our Class B stockholders will not participate in any dividends declared by our board of directors.
Rights upon liquidation. In the event of any dissolution, liquidation, or winding up of our affairs, whether voluntary or involuntary, after payment of our debts and other liabilities and making provision for any holders of our preferred stock who have a liquidation preference, our Class B stockholders will not be entitled to receive any of our assets.
Other rights. In the event of our merger or consolidation with or into another company in connection with which shares of Class A common stock and Class B common stock (together with the related membership interests) are converted into, or become exchangeable for, shares of stock, other securities or property (including cash), each Class B stockholder will be entitled to receive the same number of shares of stock as is received by Class A stockholders for each share of Class A stock, and will not be entitled, for each share of Class B stock, to receive other securities or property (including cash). No shares of Class B common stock will have preemptive rights to purchase additional shares of Class B common stock.
Preferred Stock
Our board of directors has the authority to issue shares of preferred stock in one or more series and to fix the rights, preferences, privileges and restrictions thereof, including dividend rights, dividend rates, conversion rights, voting rights, terms of redemption, redemption prices, liquidation preferences and the number of shares constituting any series or the designation of such series, without further vote or action by the stockholders.
The issuance of preferred stock may have the effect of delaying, deferring or preventing a change in control of Health Insurance Innovations, Inc. without further action by the stockholders and may adversely affect the voting and other rights of the holders of Class A common stock. At present, we have no plans to issue any preferred stock.
Election and Removal of Directors; Vacancies
Our board of directors will consist of between three and nine directors, excluding any directors elected by holders of preferred stock pursuant to provisions applicable in the case of defaults. The exact number of directors
110
Table of Contents
will be fixed from time to time by resolution of the board. In accordance with our amended and restated certificate of incorporation and our amended and restated bylaws that will become effective upon the completion of the offering, each of our directors will serve for a one-year term or until his or her successor is elected and qualified. At each annual meeting of our stockholders, our stockholders will elect the members of our board of directors. There will be no limit on the number of terms a director may serve on our board of directors.
Our amended and restated certificate of incorporation and amended and restated bylaws will provide that (a) prior to the date on which Mr. Kosloske ceases to beneficially own at least a majority in voting power of all shares entitled to vote generally in the election of directors, directors may be removed with or without cause upon the affirmative vote of holders of at least a majority of the voting power of all the then outstanding shares of stock entitled to vote generally in the election of directors, and (b) on and after the date Mr. Kosloske ceases to beneficially own at least a majority in voting power of all outstanding shares entitled to vote generally in the election of directors, directors may be removed only for cause and only upon the affirmative vote of holders of at least 75% of the voting power of all the then outstanding shares of stock entitled to vote generally in the election of directors, voting together as a single class. In addition, our amended and restated bylaws will provide that any newly-created directorship on the board of directors that results from an increase in the number of directors and any vacancy occurring on the board of directors shall be filled only by a majority of the directors then in office, although less than a quorum, or by a sole remaining director.
No Cumulative Voting
The Delaware General Corporation Law, or DGCL, provides that stockholders are not entitled to the right to cumulate votes in the election of directors unless our amended and restated certificate of incorporation provides otherwise. Our amended and restated certificate of incorporation prohibits cumulative voting.
Limits on Written Consents
The DGCL permits stockholder action by written consent unless otherwise provided by our amended and restated certificate of incorporation. Our amended and restated certificate of incorporation permits stockholder action by written consent but precludes stockholder action by written consent after the date on which Mr. Kosloske ceases to beneficially own at least a majority in voting power of all shares entitled to vote generally in the election of our directors.
Stockholder Meetings
Our amended and restated certificate of incorporation and our amended and restated bylaws provide that special meetings of stockholders may be called only by the board of directors, the chairman of the board of directors or the chief executive officer; provided, however, if Mr. Kosloske beneficially owns at least a majority of all of the outstanding shares of our capital stock entitled to vote, special meetings of stockholders may be called by the holders of a majority of the total voting power of our then outstanding capital stock.
Amendment of Amended and Restated Certificate of Incorporation
Our amended and restated certificate of incorporation provides that, at any time when Mr. Kosloske is the beneficial owner of less than a majority in voting power of our outstanding common stock, the provisions of our amended and restated certificate of incorporation relating to our capital structure, voting rights, dividends, bylaws, board of directors, limited liability of directors, indemnification of directors, amendment of our amended and restated certificate of incorporation and meetings of stockholders may be amended only by the affirmative vote of holders of at least 75% of the voting power of our outstanding shares of voting stock, voting together as a
111
Table of Contents
single class. The affirmative vote of holders of at least a majority of the voting power of our outstanding shares of stock will generally be required to amend other provisions of our amended and restated certificate of incorporation.
Amendment of Amended and Restated Bylaws
Our amended and restated bylaws may generally be altered, amended or repealed, and new bylaws may be adopted, with:
| • | the affirmative vote of a majority of directors present at any regular or special meeting of the board of directors called for that purpose, provided that any alteration, amendment or repeal of, or adoption of any bylaw inconsistent with, specified provisions of the bylaws, including those related to special and annual meetings of stockholders, action of stockholders by written consent, classification of the board of directors, nomination of directors, special meetings of directors, removal of directors and committees of the board of directors, requires the affirmative vote of at least 75% of all directors in office at a meeting called for that purpose; or |
| • | the affirmative vote of holders of 75% of the voting power of our outstanding shares of voting stock, voting together as a single class. |
Other Limitations on Stockholder Actions
Our bylaws will also impose some procedural requirements on stockholders who wish to:
| • | make nominations in the election of directors; |
| • | propose that a director be removed; |
| • | propose any repeal or change in our bylaws; or |
| • | propose any other business to be brought before an annual or special meeting of stockholders. |
Under these procedural requirements, in order to bring a proposal before a meeting of stockholders, a stockholder must deliver timely notice of a proposal pertaining to a proper subject for presentation at the meeting to our corporate secretary along with the following:
| • | a description of the business or nomination to be brought before the meeting and the reasons for conducting such business at the meeting; |
| • | the stockholder’s name and address; |
| • | any material interest of the stockholder in the proposal; |
| • | the number of shares beneficially owned by the stockholder and evidence of such ownership; and |
| • | the names and addresses of all persons with whom the stockholder is acting in concert and a description of all arrangements and understandings with those persons, and the number of shares such persons beneficially own. |
To be timely, a stockholder must generally deliver notice:
| • | in connection with an annual meeting of stockholders, not less than 120 nor more than 180 days prior to the month and day corresponding to the date on which the annual meeting of stockholders was held in the immediately preceding year, but in the event that the date of the annual meeting is more than 30 days before or more than 60 days after the anniversary date of the preceding annual meeting of stockholders, a stockholder notice will be timely if received by us not later than the close of business on the later of (1) the 120th day prior to the annual meeting and (2) the 10th day following the day on which we first publicly announce the date of the annual meeting; or |
112
Table of Contents
| • | in connection with the election of a director at a special meeting of stockholders, not less than 40 nor more than 60 days prior to the date of the special meeting, but in the event that less than 55 days’ notice or prior public disclosure of the date of the special meeting of the stockholders is given or made to the stockholders, a stockholder notice will be timely if received by us not later than the close of business on the 10th day following the day on which a notice of the date of the special meeting was mailed to the stockholders or the public disclosure of that date was made. |
In order to submit a nomination for our board of directors, a stockholder must also submit any information with respect to the nominee that we would be required to include in a proxy statement, as well as some other information. If a stockholder fails to follow the required procedures, the stockholder’s proposal or nominee will be ineligible and will not be voted on by our stockholders.
Limitation of Liability of Directors and Officers
Our amended and restated certificate of incorporation will provide that no director will be personally liable to us or our stockholders for monetary damages for breach of fiduciary duty as a director, except as required by applicable law, as in effect from time to time. Currently, Delaware law requires that liability be imposed for the following:
| • | any breach of the director’s duty of loyalty to our company or our stockholders; |
| • | any act or omission not in good faith or which involved intentional misconduct or a knowing violation of law; |
| • | unlawful payments of dividends or unlawful stock repurchases or redemptions as provided in Section 174 of the Delaware General Corporation Law; and |
| • | any transaction from which the director derived an improper personal benefit. |
As a result, neither we nor our stockholders have the right, through stockholders’ derivative suits on our behalf, to recover monetary damages against a director for breach of fiduciary duty as a director, including breaches resulting from grossly negligent behavior, except in the situations described above.
Our amended and restated certificate of incorporation will provide that, to the fullest extent permitted by law, we will indemnify any officer or director of our company against all damages, claims and liabilities arising out of the fact that the person is or was our director or officer, or served any other enterprise at our request as a director, officer, employee, agent or fiduciary. We will reimburse the expenses, including attorneys’ fees, incurred by a person indemnified by this provision when we receive an undertaking to repay such amounts if it is ultimately determined that the person is not entitled to be indemnified by us. Amending this provision will not reduce our indemnification obligations relating to actions taken before an amendment.
Forum Selection
The Court of Chancery of the State of Delaware will be the sole and exclusive forum for (1) any derivative action or proceeding brought on our behalf, (2) any action asserting a claim of breach of fiduciary duty owed by any of our directors, officers or other employee to us or our stockholders, (3) any action asserting a claim arising pursuant to any provision of the Delaware General Corporation Law, or (4) any action asserting a claim governed by the internal affairs doctrine, or if such court shall not have jurisdiction, any federal court located in the State of Delaware or other Delaware state court. Any person or entity purchasing or otherwise acquiring any interest in shares of our capital stock shall be deemed to have notice of and consented to the foregoing forum selection provisions.
113
Table of Contents
Anti-Takeover Effects of Some Provisions
Some provisions of our amended and restated certificate of incorporation and bylaws could make the following more difficult:
| • | acquisition of control of us by means of a proxy contest or otherwise, or |
| • | removal of our incumbent officers and directors. |
These provisions, as well as our ability to issue preferred stock, are designed to discourage coercive takeover practices and inadequate takeover bids. These provisions are also designed to encourage persons seeking to acquire control of us to first negotiate with our board of directors. We believe that the benefits of increased protection give us the potential ability to negotiate with the proponent of an unfriendly or unsolicited proposal to acquire or restructure us, and that the benefits of this increased protection outweigh the disadvantages of discouraging those proposals, because negotiation of those proposals could result in an improvement of their terms.
Delaware Business Combination Statute
We have opted out of Section 203 of the DGCL. However, in the event that Mr. Kosloske ceases to beneficially own at least 25% of the total voting power of all the then outstanding shares of our capital stock, we will automatically become subject to Section 203 of the DGCL.
Subject to specified exceptions, Section 203 prohibits a publicly held Delaware corporation from engaging in a “business combination” with an “interested stockholder” for a period of three years after the date of the transaction in which the person became an interested stockholder. “Business combinations” include mergers, asset sales and other transactions resulting in a financial benefit to the “interested stockholder.” Subject to various exceptions, an “interested stockholder” is a person who together with his or her affiliates and associates, owns, or within three years did own, 15% or more of the corporation’s outstanding voting stock. These restrictions generally prohibit or delay the accomplishment of mergers or other takeover or change in control attempts.
Listing
We have applied to list the Class A common stock on the NASDAQ Global Market under the symbol “HIIQ.”
Transfer Agent and Registrar
The transfer agent and registrar for the Class A common stock is American Stock Transfer & Trust Company, LLC.
114
Table of Contents
U.S. FEDERAL INCOME AND ESTATE TAX CONSIDERATIONS FOR NON-U.S. HOLDERS OF CLASS A COMMON STOCK
The following is a discussion of the material U.S. federal income and estate tax consequences of the ownership and disposition of the Company’s Class A common stock by a beneficial owner that is a “non-U.S. holder”, other than a non-U.S. holder that owns, or has owned, actually or constructively, more than 5% of the Company’s Class A common stock. A “non-U.S. holder” is a person or entity that, for U.S. federal income tax purposes, is:
| • | a non-resident alien individual, other than certain former citizens and residents of the United States subject to tax as expatriates; |
| • | a corporation, or other entity treated as a corporation for U.S. federal income tax purposes, created or organized in or under the laws of a jurisdiction other than the United States or any state or political subdivision thereof or the District of Columbia; or |
| • | an estate or trust, other than an estate or trust the income of which is subject to U.S. federal income taxation regardless of its source. |
A “non-U.S. holder” does not include an individual who is present in the United States for 183 days or more in the taxable year of disposition and is not otherwise a resident of the United States for U.S. federal income tax purposes. Such an individual is urged to consult his or her own tax advisor regarding the U.S. federal income tax consequences of the sale, exchange or other disposition of the Class A common stock.
This discussion is based on the Internal Revenue Code of 1986, as amended (the “Code”), and administrative pronouncements, judicial decisions and final, temporary and proposed Treasury Regulations, changes to any of which subsequent to the date of this prospectus may affect the tax consequences described herein. This discussion does not address all aspects of U.S. federal income and estate taxation that may be relevant to non-U.S. holders in light of their particular circumstances and it does not address any tax consequences arising under the laws of any state, local or foreign jurisdiction.
If a partnership holds the Company’s Class A common stock, the tax treatment of a partner will generally depend upon the status of the partner and the activities of the partnership. If you are a partnership holding Class A common stock, or a partner in such a partnership, you should consult your tax advisors.
Prospective holders are urged to consult their tax advisors with respect to the particular tax consequences to them of owning and disposing of the Class A common stock, including the consequences under the laws of any state, local or foreign jurisdiction.
Dividends
As discussed under “Dividend Policy” above, the Company does not currently expect to pay dividends. In the event that the Company does make any distributions with respect to its shares of Class A common stock, such distributions generally will constitute dividends for U.S. federal income tax purposes to the extent paid out of the Company’s current or accumulated earnings and profits, as determined under U.S. federal income tax principles. If a distribution exceeds the Company’s current and accumulated earnings and profits as determined under U.S. federal income tax principles, the excess will be treated first as a tax-free return of the non-U.S. holder’s adjusted tax basis in the Class A common stock and thereafter as capital gain, subject to the tax treatment described below in “Gain on Disposition of the Class A Common Stock.” Dividends paid to a non-U.S. holder of the Class A common stock generally will be subject to withholding tax at a 30% rate or a reduced rate specified by an applicable income tax treaty. In order to obtain a reduced rate of withholding, a non-U.S. holder will be required to provide an Internal Revenue Service Form W-8BEN certifying its entitlement to benefits under a treaty. Additional certification requirements apply if a non-U.S. holder holds the Class A common stock through a foreign partnership or a foreign intermediary.
115
Table of Contents
The withholding tax does not apply to dividends paid to a non-U.S. holder who provides a Form W-8ECI, certifying that the dividends are effectively connected with the non-U.S. holder’s conduct of a trade or business within the United States. Instead, the effectively connected dividends will be subject to regular U.S. income tax as if the non-U.S. holder were a United States person (as defined in the Code) unless an applicable treaty provides otherwise. A non-U.S. corporation receiving effectively connected dividends may also be subject to an additional “branch profits tax” imposed at a rate of 30% (or a lower treaty rate) with respect to its effectively-connected earnings and profits attributable to such dividends and other income.
If you are a non-U.S. holder, you may obtain a refund of any excess amounts withheld by timely filing an appropriate claim for a refund with the Internal Revenue Service. Non-U.S. holders should consult their tax advisors regarding their entitlement to benefits under an appropriate income tax treaty and the specific manner of claiming the benefits of the treaty.
Gain on Disposition of the Class A Common Stock
Subject to the discussion of backup withholding below, a non-U.S. holder generally will not be subject to U.S. federal income tax on gain realized on a sale or other disposition of the Class A common stock unless:
| • | the gain is effectively connected with a trade or business of the non-U.S. holder in the United States, subject to an applicable treaty providing otherwise; or |
| • | the Company is or has been a U.S. real property holding corporation, as defined in the Code, at any time within the five-year period preceding the disposition or the non-U.S. holder’s holding period, whichever period is shorter, and the Class A common stock has ceased to be traded on an established securities market prior to the beginning of the calendar year in which the sale or disposition occurs. |
The Company believes that it is not, and does not anticipate becoming, a U.S. real property holding corporation.
Gain that is effectively connected with a U.S. trade or business will be subject to regular U.S. income tax as if the non-U.S. holder were a U.S. person, subject to an applicable treaty providing otherwise. A non-U.S. corporation with effectively connected gains may also be subject to additional “branch profits tax” imposed at a rate of 30% (or a lower treaty rate) with respect to its effectively-connected earnings and profits attributable to such gains and other income.
Information Reporting and Backup Withholding
Information returns will be filed with the Internal Revenue Service in connection with payments of dividends. This information also may be made available under a specific treaty or agreement with the tax authorities in the country in which the non-U.S. holder resides or is established. A non-U.S. holder may have to comply with certification procedures to establish that it is not a United States person in order to avoid information reporting and backup withholding with respect to payments of dividends and the proceeds from a sale or other disposition of the Class A common stock. The amount of any backup withholding from a payment to a non-U.S. holder will be allowed as a credit against such holder’s United States federal income tax liability and may entitle such holder to a refund, provided that the required information is timely furnished to the Internal Revenue Service.
Additional Withholding Rules
Recent legislation generally imposes withholding at a rate of 30% on payments to certain foreign entities of dividends on and the gross proceeds of dispositions of U.S. common stock, unless various U.S. information reporting and due diligence requirements (generally relating to ownership by U.S. persons of interests in or
116
Table of Contents
accounts with those entities) have been satisfied. An intergovernmental agreement between the United States and an applicable foreign country may modify these requirements. This withholding will apply to payments of dividends on the Class A common stock made on or after January 1, 2014 and to payments of gross proceeds from a sale or other disposition of the Class A common stock made on or after January 1, 2017. Non-U.S. holders should consult their tax advisors regarding the possible implications of this legislation on their investment in the Class A common stock.
Federal Estate Tax
Individual non-U.S. holders and entities the property of which is potentially includible in such an individual’s gross estate for U.S. federal estate tax purposes (for example, a trust funded by such an individual and with respect to which the individual has retained certain interests or powers) should note that, absent an applicable treaty benefit, the Class A common stock will be treated as U.S. situs property subject to U.S. federal estate tax.
117
Table of Contents
SHARES ELIGIBLE FOR FUTURE SALE
Prior to this offering, there has been no market for our Class A common stock. Future sales of substantial amounts of our Class A common stock in the public market or the perception that such sales might occur could adversely affect market prices prevailing from time to time. Furthermore, because only a limited number of shares will be available for sale shortly after this offering due to existing contractual and legal restrictions on resale as described below, there may be sales of substantial amounts of our Class A common stock in the public market after the restrictions lapse. This may adversely affect the prevailing market price and our ability to raise equity capital in the future.
After completion of this offering and after giving effect to the reorganization, we will have 4,666,667 shares of Class A common stock outstanding (assuming no exercise of the underwriters’ over-allotment option). All of the shares of Class A common stock sold in this offering, plus any shares sold upon exercise of the underwriters’ over-allotment option, will be freely tradable without restrictions or further registration under the Securities Act, unless the shares are purchased by our “affiliates” as that term is defined in Rule 144 under the Securities Act and except certain shares that will be subject to the lock-up period described in the next succeeding paragraph after completion of this offering. Any shares owned by our affiliates may not be resold except in compliance with Rule 144 volume limitations, manner of sale and notice requirements, pursuant to another applicable exemption from registration or pursuant to an effective registration statement. The shares of Class A common stock issuable to our Class B stockholders will be “restricted securities” as that term is defined in Rule 144 under the Securities Act. These restricted securities may be sold in the public market only if they are registered or if they qualify for an exemption from registration under Rule 144 under the Securities Act. This rule is summarized below.
In addition, at our request, the underwriters have reserved up to 233,333 shares of the 4,666,667 shares of Class A common stock offered for sale pursuant to this prospectus for sale to some of our directors, executive officers, employees and business associates in a directed shares program. Any of these directed shares purchased by our directors, executive officers and business associates, such as distributors, will be subject to the 180-day lock-up restriction described under “Underwriting.” Accordingly, the number of shares freely transferable upon completion of this offering will be reduced by the number of directed shares purchased by our directors, executive officers and business associates, and there will be a corresponding increase in the number of shares that become eligible for sale after 180 days from the date of this prospectus.
Rule 144
In general with Rule 144 as currently in effect, a person who has beneficially owned restricted shares of our Class A common stock for at least six months would be entitled to sell such securities, provided that (i) such person is not deemed to have been one of our affiliates at the time of, or at any time during the 90 days preceding, a sale and (ii) we are subject to the Exchange Act periodic reporting requirements for at least 90 days before the sale. Persons who have beneficially owned restricted shares of our Class A common stock for at least six months but who are our affiliates at the time of, or any time during the 90 days preceding, a sale, would be subject to additional restrictions, by which such person would be entitled to sell within any three-month period only a number of securities that does not exceed the greater of either of the following:
| • | 1% of the number of shares of our Class A common stock then outstanding, which will equal approximately 4,666,667 shares immediately after this offering (assuming no exercise of the underwriters’ over-allotment option); or |
| • | the average weekly trading volume of our Class A common stock on the NASDAQ Global Market during the four calendar weeks preceding the filing of a notice on Form 144 with respect to the sale; |
provided, in each case, that we are subject to the Exchange Act periodic reporting requirements for at least 90 days before the sale. Such sales both by affiliates and by non-affiliates must also comply with the manner of sale, current public information and notice provisions of Rule 144 to the extent applicable.
We are unable to estimate the number of shares that will be sold under Rule 144 since this will depend on the market price for our common stock, the personal circumstances of the stockholder and other factors.
118
Table of Contents
Class A Common Stock Issuable Upon Exchange of Membership Interests
After completion of this offering, 8,666,667 Series B Membership Interests of Health Plan Intermediaries, LLC will be outstanding (assuming no exercise of the underwriters’ over-allotment option). Each Series B Membership Interest (together with a share of Class B common stock) will be exchangeable for a share of Class A common stock. Pursuant to the registration rights agreement that we will enter into with Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC, upon request we will use our best efforts to file a registration statement for the sale of shares of Class A common stock issued to those entities in exchange for Series B Membership Interests and Class B common stock. If Health Plan Intermediaries, LLC and Health Plan Intermediaries Sub, LLC exercised all their exchange and resale rights, 8,666,667 shares of Class A common stock would be issued to them and registered for resale (representing 65% of the number of shares in our Class A common stock outstanding immediately after this offering) (assuming no exercise of the underwriters’ over-allotment option). See “The Reorganization of Our Corporate Structure—Registration Rights Agreement.”
Stock Options
1,250,000 shares of Class A common stock are available for future option grants under our to be adopted stock plans.
Prior to the consummation of the offering, we expect to approve the grant to Mr. Hershberger of an award of restricted shares of our Class A common stock in an amount equal to 3% of the Company’s enterprise value as determined immediately following this offering. These restricted shares will be granted under our to be adopted long term incentive plan on or shortly after the closing of this offering and will be subject to the vesting schedule as is described under “Executive Compensation—Restricted Stock Agreements.”
Upon completion of this offering, we intend to file a registration statement under the Securities Act covering all shares of Class A common stock issuable pursuant to our to be adopted long term incentive plan. Subject to Rule 144 volume limitations applicable to affiliates, shares registered under any registration statements will be available for sale in the open market, beginning 90 days after the date of the prospectus, except to the extent that the shares are subject to vesting restrictions with us or the contractual restrictions described below.
Lock-up Agreements
Our directors and executive officers have agreed, subject to limited exceptions, not to offer, sell, contract to sell, pledge or otherwise dispose of, directly or indirectly, any shares of our Class A Common Stock or securities convertible into or exchangeable or exercisable for any shares of our Class A Common Stock, enter into a transaction that would have the same effect, or enter into any swap, hedge or other arrangement that transfers, in whole or in part, any of the economic consequences of ownership of our Class A Common Stock, whether any of these transactions are to be settled by delivery of our Class A Common Stock or other securities, in cash or otherwise, or publicly disclose the intention to make any such offer, sale, pledge or disposition, or to enter into any such transaction, swap, hedge or other arrangement, without, in each case, the prior written consent of Credit Suisse Securities (USA) LLC and Citigroup Global Markets Inc. for a period of 180 days after the date of this prospectus.
119
Table of Contents
Under the terms and subject to the conditions contained in an underwriting agreement dated , 2013, we have agreed to sell to the underwriters named below, for whom Credit Suisse Securities (USA) LLC and Citigroup Global Markets Inc. are acting as Representatives, the following respective numbers of shares of Class A common stock:
| Underwriter |
Number of Shares |
|||
| Credit Suisse Securities (USA) LLC |
||||
| Citigroup Global Markets Inc. |
||||
| Merrill Lynch, Pierce, Fenner & Smith Incorporated |
||||
| Raymond James Financial Inc. |
||||
|
|
|
|||
| Total |
4,666,667 | |||
|
|
|
|||
The underwriting agreement provides that the underwriters are obligated to purchase all the shares of Class A common stock in the offering if any are purchased, other than those shares covered by the over-allotment option described below. The underwriting agreement also provides that if an underwriter defaults, the purchase commitments of non-defaulting underwriters may be increased or the offering may be terminated.
We have granted to the underwriters a 30-day option to purchase on a pro rata basis up to 700,000 additional shares at the initial public offering price less the underwriting discounts and commissions. The option may be exercised only to cover any over-allotments of Class A common stock.
The underwriters propose to offer the shares of Class A common stock initially at the public offering price on the cover page of this prospectus and to selling group members at that price less a selling concession of $ per share. After the initial public offering the Representatives may change the public offering price and concession.
The following table summarizes the compensation and estimated expenses we will pay (in thousands, except per share amounts):
| Per Share | Total | |||||||||||||||
| Without Over-allotment |
With Over-allotment |
Without Over-allotment |
With Over-allotment |
|||||||||||||
| Underwriting discounts and commissions paid by us |
$ | $ | $ | $ | ||||||||||||
| Expenses payable by us |
$ | $ | $ | $ | ||||||||||||
The Representatives have informed us that they do not expect sales to accounts over which the underwriters have discretionary authority to exceed 5% of the shares of Class A common stock being offered.
We have agreed that we will not, subject to certain exceptions, offer, sell, issue, contract to sell, pledge or otherwise dispose of, directly or indirectly, or file with the SEC a registration statement under the Securities Act relating to, any shares of our Class A common stock or securities convertible into or exchangeable or exercisable for any shares of our Class A common stock, or publicly disclose the intention to make any offer, sale, pledge, disposition or filing, without the prior written consent of the Representatives for a period of 180 days after the date of this prospectus. Notwithstanding the foregoing, the restrictions set forth above shall not apply to any transfer in connection with, and as contemplated by, the reorganization transactions described under “The Reorganization of Our Corporate Structure.”
120
Table of Contents
Our directors and executive officers have agreed that, subject to certain exceptions, they will not offer, sell, contract to sell, pledge or otherwise dispose of, directly or indirectly, any shares of our Class A common stock or securities convertible into or exchangeable or exercisable for any shares of our Class A common stock, enter into a transaction that would have the same effect, or enter into any swap, hedge or other arrangement that transfers, in whole or in part, any of the economic consequences of ownership of our Class A common stock, whether any of these transactions are to be settled by delivery of our Class A common stock or other securities, in cash or otherwise, or publicly disclose the intention to make any offer, sale, pledge or disposition, or to enter into any transaction, swap, hedge or other arrangement, without, in each case, the prior written consent of the Representatives for a period of 180 days after the date of this prospectus. Notwithstanding the foregoing, the restrictions set forth above shall not apply to any transfer in connection with, and as contemplated by, the reorganization transactions described under “The Reorganization of Our Corporate Structure.”
The underwriters have reserved for sale at the initial public offering price up to 233,333 shares of the Class A common stock for employees, directors and other persons associated with us who have expressed an interest in purchasing Class A common stock in the offering. The number of shares available for sale to the general public in the offering will be reduced to the extent these persons purchase the reserved shares. Any reserved shares not so purchased will be offered by the underwriters to the general public on the same terms as the other shares.
We have agreed to indemnify the underwriters against liabilities under the Securities Act, or contribute to payments that the underwriters may be required to make in that respect.
We have applied to have our Class A common stock approved for listing on the NASDAQ Global Market under the symbol “HIIQ”.
Prior to this offering, there has been no public market for our Class A common stock. The initial public offering price was determined by negotiations among us and the Representatives and will not necessarily reflect the market price of the Class A common stock following this offering. The principal factors that will be considered in determining the initial public offering price will include:
| • | the information presented in this prospectus and otherwise available to the underwriters; |
| • | the history of, and prospects for, the industry in which we will compete; |
| • | the ability of our management; |
| • | the prospects for our future earnings; |
| • | the present state of our development and our current financial condition; |
| • | the general condition of the securities markets at the time of the offering; and |
| • | the recent market prices of, and the demand for, publicly traded Class A common stock of generally comparable companies. |
We cannot assure you that the initial public offering price will correspond to the price at which the Class A common stock will trade in the public market subsequent to this offering or that an active trading market for the Class A common stock will develop and continue after this offering.
In connection with the offering the underwriters may engage in stabilizing transactions, over-allotment transactions and syndicate covering transactions in accordance with Regulation M under the Exchange Act.
| • | Stabilizing transactions permit bids to purchase the underlying security so long as the stabilizing bids do not exceed a specified maximum. |
| • | Over-allotment involves sales by the underwriters of shares in excess of the number of shares the underwriters are obligated to purchase, which creates a syndicate short position. The short position may be either a covered short position or a naked short position. In a covered short position, the number of |
121
Table of Contents
| shares over-allotted by the underwriters is not greater than the number of shares that they may purchase in the over-allotment option. In a naked short position, the number of shares involved is greater than the number of shares in the over-allotment option. The underwriters may close out any covered short position by either exercising their over-allotment option and/or purchasing shares in the open market. |
| • | Syndicate covering transactions involve purchases of the Class A common stock in the open market after the distribution has been completed in order to cover syndicate short positions. In determining the source of shares to close out the short position, the underwriters will consider, among other things, the price of shares available for purchase in the open market as compared to the price at which they may purchase shares through the over-allotment option. If the underwriters sell more shares than could be covered by the over-allotment option, a naked short position, the position can only be closed out by buying shares in the open market. A naked short position is more likely to be created if the underwriters are concerned that there could be downward pressure on the price of the shares in the open market after pricing that could adversely affect investors who purchase in the offering. |
These stabilizing transactions, syndicate covering transactions and penalty bids may have the effect of raising or maintaining the market price of our Class A common stock or preventing or retarding a decline in the market price of the Class A common stock. As a result, the price of our Class A common stock may be higher than the price that might otherwise exist in the open market. These transactions may be effected on the NASDAQ Global Market or otherwise and, if commenced, may be discontinued at any time.
A prospectus in electronic format may be made available on the web sites maintained by one or more of the underwriters, or selling group members, if any, participating in this offering and one or more of the underwriters participating in this offering may distribute prospectuses electronically. The Representatives may agree to allocate a number of shares to underwriters and selling group members for sale to their online brokerage account holders. Internet distributions will be allocated by the underwriters and selling group members that will make internet distributions on the same basis as other allocations.
Notice to Prospective Investors in the Dubai International Financial Centre
This prospectus relates to an Exempt Offer in accordance with the Offered Securities Rules of the Dubai Financial Services Authority (“DFSA”). This prospectus is intended for distribution only to persons of a type specified in the Offered Securities Rules of the DFSA. It must not be delivered to, or relied on by, any other person. The DFSA has no responsibility for reviewing or verifying any documents in connection with Exempt Offers. The DFSA has not approved this prospectus supplement nor taken steps to verify the information set forth herein and has no responsibility for the prospectus. The shares to which this prospectus relates may be illiquid and/or subject to restrictions on their resale. Prospective purchasers of the shares offered should conduct their own due diligence on the shares. If you do not understand the contents of this prospectus you should consult an authorized financial advisor.
122
Table of Contents
European Economic Area
In relation to each Member State of the European Economic Area which has implemented the Prospectus Directive (each, a “Relevant Member State”), with effect from and including the date on which the Prospectus Directive is implemented in that Relevant Member State (the “Relevant Implementation Date”), our common shares will not be offered to the public in that Relevant Member State prior to the publication of a prospectus in relation to the common shares that has been approved by the competent authority in that Relevant Member State or, where appropriate, approved in another Relevant Member State and notified to the competent authority in that Relevant Member State, all in accordance with the Prospectus Directive, except that, with effect from and including the Relevant Implementation Date, an offer of common shares may be made to the public in that Relevant Member State at any time:
| • | to any legal entity that is a qualified investor as defined in the Prospectus Directive; |
| • | to fewer than 100 or, if the Relevant Member State has implemented the relevant provision of the 2010 PD Amending Directive, 150, natural or legal persons (other than qualified investors as defined in the Prospectus Directive), as permitted under the Prospectus Directive, subject to obtaining the prior consent of the manager for any such offer; or |
| • | in any other circumstances which do not require the publication by the issuer of a prospectus pursuant to Article 3(2) of the Prospectus Directive. |
For the purposes of this provision, the expression an “offer of common shares to the public” in relation to any shares in any Relevant Member State means the communication in any form and by any means of sufficient information on the terms of the offer and the common shares to be offered so as to enable an investor to decide to purchase or subscribe the common shares, as the same may be varied in that Relevant Member State by any measure implementing the Prospectus Directive in that Relevant Member State and the expression “Prospectus Directive” means Directive 2003/71/EC (and amendments thereto, including the 2010 PD Amending Directive, to the extent implemented in the Relevant Member State), and includes any relevant implementing measure in each Relevant Member State and the expression “2010 PD Amending Directive” means Directive 2010/73/EU.
Notice to Prospective Investors in France
Neither this prospectus nor any other offering material relating to the shares described in this prospectus has been submitted to the clearance procedures of the Autorité des Marchés Financiers or of the competent authority of another member state of the European Economic Area and notified to the Autorité des Marchés Financiers. The shares have not been offered or sold and will not be offered or sold, directly or indirectly, to the public in France. Neither this prospectus nor any other offering material relating to the shares has been or will be:
| • | released, issued, distributed or caused to be released, issued or distributed to the public in France; or |
| • | used in connection with any offer for subscription or sale of the shares to the public in France. |
| • | Such offers, sales and distributions will be made in France only: |
| • | to qualified investors (investisseurs qualifiés) and/or to a restricted circle of investors (cercle restreint d’investisseurs), in each case investing for their own account, all as defined in, and in accordance with articles L.411-2, D.411-1, D.411-2, D.734-1, D.744-1, D.754-1 and D.764-1 of the French Code monétaire et financier; |
| • | to investment services providers authorized to engage in portfolio management on behalf of third parties; or |
| • | in a transaction that, in accordance with article L.411-2-II-1°-or-2°-or 3° of the French Code monétaire et financier and article 211-2 of the General Regulations (Règlement Général) of the Autorité des Marchés Financiers, does not constitute a public offer (appel public à l’épargne). |
123
Table of Contents
The shares may be resold directly or indirectly, only in compliance with articles L.411-1, L.411-2, L.412-1 and L.621-8 through L.621-8-3 of the French Code monétaire et financier.
Hong Kong
(1) We have not offered or sold and will not offer or sell our Class A common stock in Hong Kong SAR by means of this prospectus or any other document, other than to persons whose ordinary business involves buying or selling shares or debentures, whether as principal or agent or in circumstances which do not constitute an offer to the public within the meaning of the Companies Ordinance (Cap. 32 of the Laws of Hong Kong SAR), and (2) unless we are permitted to do so under the securities laws of Hong Kong SAR, we have not issued or held for the purpose of issue in Hong Kong and will not issue or hold for the purpose of issue in Hong Kong SAR this prospectus, any other offering material or any advertisement, invitation or document relating to the Class A common stock, otherwise than with respect to Class A common stock intended to be disposed of to persons outside Hong Kong SAR or only to persons whose business involves the acquisition, disposal, or holding of securities, whether as principal or as agent.
Japan
The Class A common stock offered in this prospectus has not been and will not be registered under the Financial Instruments and Exchange Law of Japan. The Class A common stock has not been offered or sold and will not be offered or sold, directly or indirectly, in Japan or to or for the account of any resident of Japan (including any corporation or other entity organized under the laws of Japan), except (i) pursuant to an exemption from the registration requirements of the Financial Instruments and Exchange Law and (ii) in compliance with any other applicable requirements of Japanese law.
Singapore
This prospectus has not been registered as a prospectus with the Monetary Authority of Singapore. Accordingly, this prospectus or any other document or material in connection with the offer or sale, or invitation for subscription or purchase, of the Class A common stock, may not be circulated or distributed, nor may the Class A common stock be offered or sold, or be made the subject of an invitation for subscription or purchase, whether directly or indirectly, to the public or any member of the public in Singapore other than (1) to an institutional investor or other person specified in Section 274 of the Securities and Futures Act, Chapter 289 of Singapore (the “SFA”), (2) to a sophisticated investor, and in accordance with the conditions, specified in Section 275 of the SFA or (3) otherwise pursuant to, and in accordance with the conditions of, any other applicable provision of the SFA.
Notice to Prospective Investors in Switzerland
The shares may not be publicly offered in Switzerland and will not be listed on the SIX Swiss Exchange (“SIX”) or on any other stock exchange or regulated trading facility in Switzerland. This document has been prepared without regard to the disclosure standards for issuance prospectuses under art. 652a or art. 1156 of the Swiss Code of Obligations or the disclosure standards for listing prospectuses under art. 27 ff. of the SIX Listing Rules or the listing rules of any other stock exchange or regulated trading facility in Switzerland. Neither this document nor any other offering or marketing material relating to the shares or the offering may be publicly distributed or otherwise made publicly available in Switzerland.
Neither this document nor any other offering or marketing material relating to the offering, the Company, the shares have been or will be filed with or approved by any Swiss regulatory authority. In particular this document will not be filed with, and the offer of shares will not be supervised by, the Swiss Financial Market
124
Table of Contents
Supervisory Authority FINMA (FINMA), and the offer of shares has not been and will not be authorized under the Swiss Federal Act on Collective Investment Schemes (“CISA”). The investor protection afforded to acquirers of interests in collective investment schemes under the CISA does not extend to acquirers of shares.
United Kingdom
Our Class A common stock may not be offered or sold and will not be offered or sold to any persons in the United Kingdom other than persons whose ordinary activities involve them in acquiring, holding, managing or disposing of investments (as principal or as agent) for the purposes of their businesses and in compliance with all applicable provisions of the Financial Services and Markets Act 2000 (“FSMA”) with respect to anything done in relation to our Class A common stock in, from or otherwise involving the United Kingdom.
In addition, each underwriter:
| • | has only communicated or caused to be communicated and will only communicate or cause to be communicated an invitation or inducement to engage in investment activity (within the meaning of section 21 of FSMA) to persons who have professional experience in matters relating to investments falling within Article 19(5) of the Financial Services and Markets Act of 2000 (Financial Promotion) Order 2005 or in circumstances in which section 21 of FSMA does not apply to the company; and |
| • | has complied with, and will comply with all applicable provisions of FSMA with respect to anything done by it in relation to the Class A common stock in, from or otherwise involving the United Kingdom. |
125
Table of Contents
Resale Restrictions
The distribution of our Class A common stock in Canada is being made only in the provinces of Ontario and Quebec on a private placement basis exempt from the requirement that we prepare and file a prospectus with the securities regulatory authorities in each province where trades of Class A common stock are made. Any resale of the Class A common stock in Canada must be made under applicable securities laws which may vary depending on the relevant jurisdiction, and which may require resales to be made under available statutory exemptions or under a discretionary exemption granted by the applicable Canadian securities regulatory authority. Purchasers are advised to seek legal advice prior to any resale of the Class A common stock.
Representations of Purchasers
By purchasing Class A common stock in Canada and accepting delivery of a purchase confirmation, a purchaser is representing to us and the dealer from whom the purchase confirmation is received that:
| • | the purchaser is resident in either the Province of Ontario or Quebec, and is not acquiring the securities for the account or benefit of any individual or entity that is resident in any province or territory of Canada other than the Province of Ontario or Quebec; |
| • | the purchaser is entitled under applicable provincial securities laws to purchase the Class A common stock without the benefit of a prospectus qualified under those securities laws as it is an “accredited investor” as defined under National Instrument 45-106 – Prospectus and Registration Exemptions; |
| • | the purchaser is a “Canadian permitted client” as defined in National Instrument 31-103 - Registration Requirements, Exemptions and Ongoing Registrant Obligations, or as otherwise interpreted and applied by the Canadian Securities Administrators; |
| • | where required by law, the purchaser is purchasing as principal and not as agent; |
| • | the purchaser has reviewed the text above under “Resale Restrictions”; and |
| • | the purchaser acknowledges and consents to the provision of specified information concerning the purchase of the Class A common stock to the regulatory authority that by law is entitled to collect the information, including certain personal information. For purchasers in Ontario, questions about such indirect collection of personal information should be directed to Administrative Support Clerk, Ontario Securities Commission, Suite 1903, Box 55, 20 Queen Street West, Toronto, Ontario M5H 3S8 or to (416) 593-3684. |
Rights of Action—Ontario Purchasers
Under Ontario securities legislation, certain purchasers who purchase a security offered by this document during the period of distribution will have a statutory right of action for damages, or while still the owner of the Class A common stock, for rescission against us in the event that this document contains a misrepresentation without regard to whether the purchaser relied on the misrepresentation. The right of action for damages is exercisable not later than the earlier of 180 days from the date the purchaser first had knowledge of the facts giving rise to the cause of action and three years from the date on which payment is made for the Class A common stock. The right of action for rescission is exercisable not later than 180 days from the date on which payment is made for the Class A common stock. If a purchaser elects to exercise the right of action for rescission, the purchaser will have no right of action for damages against us. In no case will the amount recoverable in any action exceed the price at which the Class A common stock were offered to the purchaser and if the purchaser is shown to have purchased the securities with knowledge of the misrepresentation, we will have no liability. In the case of an action for damages, we will not be liable for all or any portion of the damages that are proven to not
126
Table of Contents
represent the depreciation in value of the Class A common stock as a result of the misrepresentation relied upon. These rights are in addition to, and without derogation from, any other rights or remedies available at law to an Ontario purchaser. The foregoing is a summary of the rights available to an Ontario purchaser. Ontario purchasers should refer to the complete text of the relevant statutory provisions.
Enforcement of Legal Rights
All of our directors and officers as well as the experts named herein may be located outside of Canada and, as a result, it may not be possible for Canadian purchasers to effect service of process within Canada upon us or those persons. All or a substantial portion of our assets and the assets of those persons may be located outside of Canada and, as a result, it may not be possible to satisfy a judgment against us or those persons in Canada or to enforce a judgment obtained in Canadian courts against us or those persons outside of Canada.
Taxation and Eligibility for Investment
Canadian purchasers of Class A common stock should consult their own legal and tax advisors with respect to the tax consequences of an investment in the Class A common stock in their particular circumstances and about the eligibility of the investment by the purchaser under relevant Canadian legislation.
127
Table of Contents
The validity of the issuance of the shares of Class A common stock offered hereby will be passed upon for us by Davis Polk & Wardwell LLP, New York, New York. The underwriters have been represented by Cravath, Swaine & Moore LLP, New York, New York.
The consolidated financial statements of Health Plan Intermediaries, LLC as of September 30, 2012 (Successor) and December 31, 2011 (Successor) and for the periods from January 1, 2012 to September 30, 2012 (Successor), October 1, 2011 to December 31, 2011 (Successor) and January 1, 2011 to September 30, 2011 (Predecessor) and the year ended December 31, 2010 (Predecessor) appearing in this Prospectus and Registration Statement have been audited by Ernst & Young LLP, independent registered public accounting firm, as set forth in their report thereon appearing elsewhere herein, and are included in reliance upon such report given on the authority of such firm as experts in accounting and auditing.
WHERE YOU CAN FIND MORE INFORMATION
We have filed with the SEC, Washington, D.C. 20549, a registration statement on Form S-1 under the Securities Act with respect to the Class A common stock offered hereby. This prospectus does not contain all of the information set forth in the registration statement and the exhibits and schedules thereto. For further information with respect to the Company and its Class A common stock, reference is made to the registration statement and the exhibits and any schedules filed therewith. Statements contained in this prospectus as to the contents of any contract or other document referred to are not necessarily complete and in each instance, if such contract or document is filed as an exhibit, reference is made to the copy of such contract or other document filed as an exhibit to the registration statement, each statement being qualified in all respects by such reference. A copy of the registration statement, including the exhibits and schedules thereto, may be read and copied at the SEC’s Public Reference Room at 100 F Street, N.E., Washington, D.C. 20549. Information on the operation of the Public Reference Room may be obtained by calling the SEC at 1-800-SEC-0330. In addition, the SEC maintains an Internet site at www.sec.gov, from which interested persons can electronically access the registration statement, including the exhibits and any schedules thereto.
As a result of the offering, we will become subject to the informational requirements of the Exchange Act. We will fulfill our obligations with respect to such requirements by filing periodic reports and other information with the SEC. We intend to furnish our stockholders with annual reports containing financial statements certified by an independent public accounting firm. We also maintain an Internet site at www.hiiquote.com. Our website and the information contained therein or connected thereto shall not be deemed to be incorporated into this prospectus or the registration statement of which it forms a part.
128
Table of Contents
FINANCIAL STATEMENTS
Health Plan Intermediaries, LLC and Subsidiaries
| Page | ||||
| Audited Consolidated Financial Statements |
||||
| F-2 | ||||
| F-3 | ||||
| F-4 | ||||
| F-5 | ||||
| F-6 | ||||
| F-7 | ||||
Health Insurance Innovations, Inc.
The financial statements of Health Insurance Innovations, Inc. have been omitted from this presentation because the entity has not commenced operations, and has no activities except in connection with its formation, as described under “The Reorganization of Our Corporate Structure.”
F-1
Table of Contents
Report of Independent Registered Public Accounting Firm
The Member of Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
We have audited the accompanying consolidated balance sheets of Health Plan Intermediaries, LLC d/b/a Health Insurance Innovations and subsidiary (the Company) as of September 30, 2012 (Successor) and December 31, 2011 (Successor), and the related consolidated statements of operations, member’s equity (deficit), and cash flows for the periods from January 1, 2012 to September 30, 2012 (Successor), October 1, 2011 to December 31, 2011 (Successor) and January 1, 2011 to September 30, 2011 (Predecessor) and the year ended December 31, 2010 (Predecessor). These financial statements are the responsibility of the Company’s management. Our responsibility is to express an opinion on these financial statements based on our audits.
We conducted our audits in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement. We were not engaged to perform an audit of the Company’s internal control over financial reporting. Our audits included consideration of internal control over financial reporting as a basis for designing audit procedures that are appropriate in the circumstances, but not for the purpose of expressing an opinion on the effectiveness of the Company’s internal control over financial reporting. Accordingly, we express no such opinion. An audit also includes examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements, assessing the accounting principles used and significant estimates made by management, and evaluating the overall financial statement presentation. We believe that our audits provide a reasonable basis for our opinion.
In our opinion, the financial statements referred to above present fairly, in all material respects, the consolidated financial position of Health Plan Intermediaries, LLC d/b/a Health Insurance Innovations and subsidiary at September 30, 2012 (Successor) and December 31, 2011 (Successor), and the consolidated results of their operations and their cash flows for the periods from January 1, 2012 to September 30, 2012 (Successor), October 1, 2011 to December 31, 2011 (Successor) and January 1, 2011 to September 30, 2011 (Predecessor) and the year ended December 31, 2010 (Predecessor), in conformity with U.S. generally accepted accounting principles.
| /s/ Ernst & Young LLP |
| Certified Public Accountants |
Tampa, Florida
December 20, 2012, except for Note 16, as to which the date is January 24, 2013
F-2
Table of Contents
Health Plan Intermediaries, LLC and Subsidiaries
d/b/a Health Insurance Innovations
Consolidated Balance Sheets (Successor)
| September 30, 2012 |
December 31, 2011 |
|||||||
| Assets |
||||||||
| Current assets: |
||||||||
| Cash |
$ | 981,884 | $ | 618,109 | ||||
| Cash held on behalf of others |
3,570,510 | 3,029,774 | ||||||
| Credit card transactions receivable |
137,794 | 73,666 | ||||||
| Credit card transactions receivable for others |
846,450 | 452,518 | ||||||
| Accounts receivable |
315,396 | 196,706 | ||||||
| Notes receivable |
95,000 | — | ||||||
| Advanced commissions |
300,120 | 23,771 | ||||||
| Prepaid expenses |
26,727 | 23,339 | ||||||
| Gateway processor deposit |
— | 400,000 | ||||||
|
|
|
|
|
|||||
| Total current assets |
6,273,881 | 4,817,883 | ||||||
| Property and equipment, net of accumulated depreciation |
206,622 | 124,924 | ||||||
| Accounts receivable |
— | 57,078 | ||||||
| Deferred financing costs, net |
88,247 | 122,486 | ||||||
| Capitalized offering costs |
862,513 | — | ||||||
| Deposits |
20,514 | 8,009 | ||||||
| Goodwill |
5,906,106 | 5,906,106 | ||||||
| Intangible assets, net of accumulated amortization |
4,184,422 | 4,031,214 | ||||||
|
|
|
|
|
|||||
| Total assets |
$ | 17,542,305 | $ | 15,067,700 | ||||
|
|
|
|
|
|||||
| Liabilities and member’s equity |
||||||||
| Current liabilities: |
||||||||
| Accounts payable and accrued expenses |
$ | 1,540,207 | $ | 342,194 | ||||
| Carriers and vendors payable |
2,975,983 | 2,254,424 | ||||||
| Commissions payable |
1,440,977 | 1,255,898 | ||||||
| Unearned commissions |
196,458 | — | ||||||
| Notes payable |
110,475 | — | ||||||
| Deferred rent |
13,153 | — | ||||||
| Deferred other income |
8,434 | — | ||||||
| Current portion of long-term debt |
801,952 | 769,276 | ||||||
| Current portion of noncompete obligation |
177,372 | — | ||||||
| Current portion of capital leases |
2,467 | 5,346 | ||||||
| Due to member |
— | 125,752 | ||||||
|
|
|
|
|
|||||
| Total current liabilities |
7,267,478 | 4,752,890 | ||||||
| Capital lease obligations, less current portion |
4,331 | 9,520 | ||||||
| Long-term debt, less current portion |
2,688,136 | 3,293,466 | ||||||
| Noncompete obligation |
665,355 | — | ||||||
| Deferred rent |
48,127 | 15,925 | ||||||
|
|
|
|
|
|||||
| Total liabilities |
10,673,427 | 8,071,801 | ||||||
| Member’s equity |
6,882,114 | 6,995,899 | ||||||
| Noncontrolling interest in subsidiary |
(13,236 | ) | — | |||||
|
|
|
|
|
|||||
| Total equity |
6,868,878 | 6,995,899 | ||||||
|
|
|
|
|
|||||
| Total liabilities and equity |
$ | 17,542,305 | $ | 15,067,700 | ||||
|
|
|
|
|
|||||
See accompanying notes.
F-3
Table of Contents
Health Plan Intermediaries, LLC and Subsidiaries
d/b/a Health Insurance Innovations
Consolidated Statements of Operations
| Successor | Predecessor | |||||||||||||||||
| Nine-Month Period Ended September 30, 2012 |
Three-Month Period Ended December 31, 2011 |
Nine-Month Period Ended September 30, 2011 |
Year Ended December 31, 2010 |
|||||||||||||||
| Revenues (premium equivalents of $54,549,087, $14,949,088, $38,256,738 and $20,024,069 for the Successor period ended September 30, 2012, Successor period ended December 31, 2011, Predecessor period ended September 30, 2011, and the Predecessor year ended December 31, 2010, respectively) |
$ | 30,101,980 | $ | 8,090,116 | $ | 21,788,101 | $ | 11,790,300 | ||||||||||
| Third-party commissions |
20,093,404 | 5,600,758 | 16,102,759 | 9,009,880 | ||||||||||||||
| Credit cards and ACH fees |
692,883 | 197,128 | 473,580 | 275,640 | ||||||||||||||
| General and administrative expenses |
5,786,140 | 1,420,765 | 3,340,730 | 2,514,020 | ||||||||||||||
| Depreciation and amortization |
770,878 | 269,390 | 29,311 | 6,851 | ||||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||
| Total operating costs and expenses |
27,343,305 | 7,488,041 | 19,946,380 | 11,806,391 | ||||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||
| Income (loss) from operations |
2,758,675 | 602,075 | 1,841,721 | (16,091 | ) | |||||||||||||
| Other expenses (income): |
||||||||||||||||||
| Interest expense |
194,318 | 71,213 | — | — | ||||||||||||||
| Interest income |
— | — | — | (3,244 | ) | |||||||||||||
| Other income |
(21,603 | ) | — | — | — | |||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||
| Net income (loss) |
2,585,960 | 530,862 | 1,841,721 | (12,847 | ) | |||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||
| Net loss attributable to noncontrolling interest in subsidiary |
(63,236 | ) | — | — | — | |||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||
| Net income (loss) attributable to Health Plan Intermediaries, LLC |
$ | 2,649,196 | $ | 530,862 | $ | 1,841,721 | $ | (12,847 | ) | |||||||||
|
|
|
|
|
|
|
|
|
|||||||||||
See accompanying notes.
F-4
Table of Contents
Health Plan Intermediaries, LLC and Subsidiaries
d/b/a Health Insurance Innovations
Consolidated Statements of Member’s Equity (Deficit)
| Member’s equity |
Noncontrolling interest in subsidiary |
Total | ||||||||||
| Balance at January 1, 2010 (Predecessor) |
$ | (165,305 | ) | $ | — | $ | (165,305 | ) | ||||
| Net income (loss) |
(12,847 | ) | — | (12,847 | ) | |||||||
| Contributions from members |
101,325 | — | 101,325 | |||||||||
|
|
|
|
|
|
|
|||||||
| Balance at December 31, 2010 (Predecessor) |
(76,827 | ) | — | (76,827 | ) | |||||||
| Net income |
1,841,721 | — | 1,841,721 | |||||||||
| Distributions to members |
(1,301,000 | ) | — | (1,301,000 | ) | |||||||
|
|
|
|
|
|
|
|||||||
| Balance at September 30, 2011 (Predecessor) |
463,894 | — | 463,894 | |||||||||
| Balance at October 1, 2011 (Successor) |
463,894 | — | 463,894 | |||||||||
| Net income |
530,862 | — | 530,862 | |||||||||
| Contributions from member |
1,135,036 | — | 1,135,036 | |||||||||
| Purchase of member’s interest in Company and adjustment to member’s equity to reflect fair value |
4,866,107 | — | 4,866,107 | |||||||||
|
|
|
|
|
|
|
|||||||
| Balance at December 31, 2011 (Successor) |
6,995,899 | — | 6,995,899 | |||||||||
| Net income (loss) |
2,649,196 | (63,236 | ) | 2,585,960 | ||||||||
| Contributions from minority partner |
— | 50,000 | 50,000 | |||||||||
| Distributions to member |
(2,762,981 | ) | — | (2,762,981 | ) | |||||||
|
|
|
|
|
|
|
|||||||
| Balance at September 30, 2012 (Successor) |
$ | 6,882,114 | $ | (13,236 | ) | $ | 6,868,878 | |||||
|
|
|
|
|
|
|
|||||||
See accompanying notes.
F-5
Table of Contents
Health Plan Intermediaries, LLC and Subsidiaries
d/b/a Health Insurance Innovations
Consolidated Statements of Cash Flows
| Successor | Predecessor | |||||||||||||||||
| Nine-Month Period Ended September 30, 2012 |
Three-Month Period Ended December 31, 2011 |
Nine-Month Period Ended September 30, 2011 |
Year Ended December 31, 2010 |
|||||||||||||||
| Operating activities |
||||||||||||||||||
| Net income (loss) |
$ | 2,585,960 | $ | 530,862 | $ | 1,841,721 | $ | (12,847 | ) | |||||||||
| Adjustments to reconcile net income (loss) to net cash provided by (used in) operating activities: |
||||||||||||||||||
| Depreciation and amortization |
770,878 | 269,390 | 29,311 | 6,851 | ||||||||||||||
| Amortization of deferred financing costs |
34,239 | 12,550 | — | — | ||||||||||||||
| Change in operating assets and liabilities: |
||||||||||||||||||
| Increase in cash held on behalf of others |
(540,736 | ) | (203,900 | ) | (414,168 | ) | (2,359,698 | ) | ||||||||||
| Increase (decrease) in credit card transactions receivable |
(458,060 | ) | 17,426 | (460,672 | ) | (82,938 | ) | |||||||||||
| Increase (decrease) in accounts receivable |
(61,612 | ) | 93,285 | (179,264 | ) | (74,995 | ) | |||||||||||
| Increase in advanced commissions |
(276,349 | ) | (23,771 | ) | — | — | ||||||||||||
| Decrease (increase) in gateway processor deposit |
400,000 | — | (400,000 | ) | — | |||||||||||||
| Increase (decrease) in prepaid expenses and deposits |
4,862 | (119,879 | ) | 83,717 | (88,851 | ) | ||||||||||||
| Increase (decrease) in carriers and vendors payable |
721,559 | (155,516 | ) | 1,266,876 | 1,127,674 | |||||||||||||
| Increase (decrease) in accounts payable, accrued and deferred expenses |
1,206,802 | 18,050 | (182,083 | ) | 339,000 | |||||||||||||
| Increase in commissions payable |
185,079 | 45,497 | 411,514 | 679,690 | ||||||||||||||
| Increase in unearned commissions |
196,458 | — | — | — | ||||||||||||||
| (Decrease) increase in amounts due to members |
(125,752 | ) | 125,752 | (359,602 | ) | 435,400 | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||
| Net cash provided by (used in) operating activities |
4,643,328 | 609,746 | 1,637,350 | (30,714 | ) | |||||||||||||
| Investing activities |
||||||||||||||||||
| Purchases of property and equipment |
(118,057 | ) | (23,802 | ) | (38,453 | ) | (79,508 | ) | ||||||||||
| Loan to distributor |
(220,000 | ) | — | — | — | |||||||||||||
| Proceeds from repayment of distributor loan |
125,000 | — | — | — | ||||||||||||||
| Payments made on business acquisition |
— | (5,330,000 | ) | — | — | |||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||
| Net cash used in investing activities |
(213,057 | ) | (5,353,802 | ) | (38,453 | ) | (79,508 | ) | ||||||||||
| Financing activities |
||||||||||||||||||
| Issuance of long-term debt |
— | 4,250,000 | — | — | ||||||||||||||
| Principal payments on notes payable |
(10,280 | ) | — | — | — | |||||||||||||
| Principal payments on long-term debt |
(572,654 | ) | (187,258 | ) | — | — | ||||||||||||
| Proceeds from note payable |
100,000 | — | — | — | ||||||||||||||
| Payment of financing costs |
— | (135,036 | ) | — | — | |||||||||||||
| Payment of fees for equity issuance |
(862,513 | ) | — | — | — | |||||||||||||
| Payments on capital leases |
(8,068 | ) | (1,303 | ) | (3,771 | ) | (2,270 | ) | ||||||||||
| Capital contribution |
— | 1,135,036 | — | 101,325 | ||||||||||||||
| Proceeds from issuance of non-controlling interest in subsidiary |
50,000 | — | — | — | ||||||||||||||
| Distributions to member |
(2,762,981 | ) | — | (1,301,000 | ) | — | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||
| Net cash (used in) provided by financing activities |
(4,066,496 | ) | 5,061,439 | (1,304,771 | ) | 99,055 | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||
| Net increase in cash |
363,775 | 317,383 | 294,126 | (11,167 | ) | |||||||||||||
| Cash at beginning of period |
618,109 | 300,726 | 6,600 | 17,767 | ||||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||
| Cash at end of period |
$ | 981,884 | $ | 618,109 | $ | 300,726 | 6,600 | |||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||
| Supplemental disclosures of cash flow information |
||||||||||||||||||
| Cash paid for interest |
$ | 152,795 | $ | 55,578 | $ | — | $ | — | ||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||
| Supplemental disclosure of non-cash investing and financing activities |
||||||||||||||||||
| Equipment acquired through capital leases |
$ | — | $ | — | $ | — | $ | 22,210 | ||||||||||
| Software acquired through issuance of trade payable |
$ | 45,000 | $ | — | $ | — | $ | — | ||||||||||
| Purchase of insurance through premium financing agreement |
$ | 20,755 | $ | — | $ | — | $ | — | ||||||||||
| Noncompete agreement acquired through issuance of long-term payable |
$ | 842,727 | $ | — | $ | — | $ | — | ||||||||||
See accompanying notes.
F-6
Table of Contents
Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
Notes to Consolidated Financial Statements
September 30, 2012
1. Organization, Basis of Presentation, and Summary of Significant Accounting Policies
Description of the Company
Health Plan Intermediaries, LLC, which operates under the name Health Insurance Innovations (the Company), is a developer and administrator of affordable individual health insurance and discount benefit plans that are sold throughout the United States. The Company’s main product, short-term medical insurance, which is referred to as STM, is an alternative to traditional individual major medical plans and generally offers comparable benefits for qualifying individuals. The Company also offers guaranteed-issue hospital indemnity plans for individuals under the age of 65 and a variety of ancillary products that are frequently purchased together with the STM and hospital indemnity plans as supplements. The Company designs and structures insurance products on behalf of the Company’s contracted insurance carrier companies; markets them to individuals through a network of distributors; and manages the member relationship through customer service agents. The Company’s sales are primarily executed online and offer real-time fulfillment through a proprietary web-based technology platform, through which the Company receives credit card and automated clearing house payments directly from the purchasing customers, whom are referred to as “members,” at the time of sale. In certain cases, premiums are collected from the distributor. The plans are underwritten by contracted insurance carrier companies, and the Company assumes no underwriting or insurance risk.
The Company was formed as a Florida limited liability company in April 2003. On August 21, 2008, the Naylor Group Partners, LLC (Naylor) made a capital contribution to the Company in exchange for a 50% ownership interest in the Company. On September 28, 2011, the Company purchased all of the units owned by Naylor for $5,330,000, plus deferred financing costs of $135,000. The Company financed a portion of the purchase by entering into a loan agreement with a bank for $4,250,000. The remaining purchase price was funded with the Company’s cash and a capital contribution from Michael Kosloske (Kosloske), the current sole member of the Company.
Basis of Presentation
The September 2011 business acquisition was accounted for as a purchase and the purchase price was “pushed down” to the Company’s financial statements. When using the push-down basis of accounting, the acquired company’s financial statements reflect the new accounting basis recorded by the acquirer. Accordingly, purchase accounting adjustments have been reflected in the Company’s financial statements for the period commencing on October 1, 2011. The new basis of accounting reflects the estimated fair value of the Company’s assets and liabilities as of the date of the transaction. The Company used October 1, 2011, as the effective date of the transaction, since the operating activity between that date and the September 28, 2011 transaction date was not material.
The Company, as it existed prior to the October 1, 2011 acquisition, is referred to as “Predecessor.” The Company, as it existed on and after October 1, 2011, is referred to as the “Successor.”
The accompanying Predecessor historical financial statements for the periods ended September 30, 2011 and prior represent the financial position and corporate structure as of the dates indicated. The Predecessor’s financial statements are presented at historical cost values and do not reflect the effects of the Company’s new capital structure (debt and ownership) and accounting for the acquired intangible assets and goodwill. Therefore, the result of operations, changes in member’s equity, and cash flows for the predecessor and successor periods are not comparable.
F-7
Table of Contents
Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
Notes to Consolidated Financial Statements (continued)
1. Organization, Basis of Presentation, and Summary of Significant Accounting Policies (continued)
In June 2012, the Company and a minority partner acquired the Insurance Center for Excellence (ICE), a marketing call center. The Company owns an 80% interest in ICE, which has been consolidated in the accompanying consolidated financial statements. All intercompany accounts and transactions have been eliminated.
The accompanying financial statements have been prepared in accordance with U.S. generally accepted accounting principles (GAAP).
All dollar amounts in the footnotes are rounded to the nearest thousand.
Use of Estimates
The preparation of the financial statements in conformity with GAAP requires management to make estimates, judgments, and assumptions that affect the reported amounts of assets and liabilities at the date of the financial statements. These estimates also affect the reported amounts of revenue and expenses during the reporting periods. Actual results could differ from those estimates.
Revenue Recognition
The Company’s revenues consist of commissions earned for health insurance policies and discount benefit plans issued to members, enrollment fees paid by members, and administration fees paid by members as a direct result of the Company’s enrollment services. The member’s payment includes a combination of risk premium, fees for discount benefit plans, fees for distributors and an enrollment fee, which are collectively referred to as “Premium equivalents.” Revenues reported by the Company are net of premiums remitted to insurance carriers and fees paid for discount benefit plans. Commissions and fees attributable to the sale of six- or 12-month STM plans and hospital indemnity policies represent substantially all of the Company’s revenue for the periods presented. Revenues are net of an allowance for policies expected to be cancelled by members during a limited cancellation period. The Company establishes the allowance for estimated policy cancellations through a charge to revenue. The allowance is estimated using historical data to project future experience. Such estimates and assumptions could change in the future as more information becomes known, which could impact the amounts reported. The Company periodically reviews the adequacy of the allowance and records adjustments as necessary. The net allowance for estimated policy cancellations at September 30, 2012 (Successor) and December 31, 2011 (Successor) was $43,000 and $12,000, respectively.
Revenue is earned at the time of sale. Commission rates for all of the Company’s products are agreed to in advance with the relevant insurance carrier and vary by carrier and policy type. Under the Company’s carrier compensation arrangements, the commission rate schedule that is in effect on the policy effective date governs the commissions over the life of the policy. In addition, the Company earns enrollment and administration fees on policies issued. All amounts due to insurance carriers and discount benefit vendors are reported and paid to them according to the procedures provided for in the contractual agreements between the Company and the individual carrier or vendor. Risk premiums are typically reported and remitted to insurance carriers on the 15th of the month following the end of the month in which they are collected.
In concluding that revenues should be reported on a net basis, the Company considered ASC 605-45-45 and whether it has the responsibility to provide the goods or services to the customer or if it relies on a supplier to provide the goods or services to the customer. The Company is not the ultimate party responsible for providing the insurance coverage or discount benefits to the member and, therefore, the Company is not the primary obligor
F-8
Table of Contents
Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
Notes to Consolidated Financial Statements (continued)
1. Organization, Basis of Presentation, and Summary of Significant Accounting Policies (continued)
in the arrangement. The supplier, or insurance carrier, bears the risk for that insurance coverage. The Company therefore reports its revenue net of amounts paid to its contracted insurance carrier companies and discount benefit vendors.
Third-Party Commissions
The Company utilizes a broad network of licensed third-party distributors to sell the plans developed by the Company. The Company pays commissions to these distributors based on a percentage of the policy premium that varies by type of policy. The Company pays fees to the distributors for discount benefit plans issued.
Cash Held on Behalf of Others
In the Company’s capacity as the policy administrator, the Company collects premiums from members and distributors and, after deducting the Company’s earned commissions, remits these premiums to the Company’s contracted insurance carriers, discount benefit vendors and distributors. The Company holds the unremitted funds in a fiduciary capacity until they are disbursed and the use of such funds is restricted. The Company holds these funds in bank accounts. These unremitted amounts are reported as cash held on behalf of others in the accompanying consolidated balance sheets with the related liabilities reported as carriers and vendors payable and commissions payable. Cash held on behalf of others at September 30, 2012 (Successor) and December 31, 2011 (Successor) was approximately $3,571,000 and $3,030,000, respectively.
Accounts Receivable
Accounts receivable represent amounts due to the Company for premiums collected by a third party and are generally considered delinquent 15 days after the due date. The underlying insurance contracts are cancelled retroactively if the payment remains delinquent. The Company has not experienced any credit losses from accounts receivable and has not recognized a provision for uncollectible accounts receivable. Approximately $57,000 of accounts receivable have been excluded from current assets as of December 31, 2011 (Successor) because an agreement is in place to collect those amounts in installments through July 2013. At September 30, 2012 the entire accounts receivable balance is current.
Credit Card Transactions Receivable and Credit Card Transactions Receivable for Others
Members may pay their policy premiums to the Company by credit card or through automatic check withdrawal (ACH) transfers. The credit card vendor remits cash for these transactions to the Company periodically. Credit card transactions processed by the credit card vendor, but not yet remitted to the Company are recorded as credit card transactions receivable. A portion of the amount receivable from these transactions is related to carrier premiums, discount benefit plan fees, and commissions and is recorded as credit card transactions receivable for others in the accompanying balance sheet.
The Company incurs fees for these transactions that are expensed as incurred.
Advance Commissions
Advance commissions consist of amounts advanced to certain third-party distributors. The Company began advancing commissions in November 2011. The Company performs ongoing credit evaluations of their distributors, all of which are located in the United States. The Company recovers the advance commissions from
F-9
Table of Contents
Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
Notes to Consolidated Financial Statements (continued)
1. Organization, Basis of Presentation, and Summary of Significant Accounting Policies (continued)
future commissions earned on premiums collected. The Company has not experienced any credit losses from commission advances and accordingly, has not recognized any provision for bad debt expense for the periods presented. A fee for the advance commission of up to 2% of the insurance premium sold is charged to the distributors and recognized as interest income as earned. The interest income earned from advance commissions for the period ended September 30, 2012 (Successor) and year ended December 31, 2011 (Successor) was approximately $22,000 and $2,000, respectively. There was no interest income earned from advance commissions for the period ending September 30, 2011 (Predecessor) and year ended December 31, 2010 (Predecessor). Advance commissions outstanding at September 30, 2012 (Successor) and December 31, 2011 (Successor) totaled approximately $300,000 and $24,000, respectively.
Capitalization of Offering Costs
Capitalized offering costs are costs directly attributable to the Company’s offering of its equity securities. If the offering is not successful, the capitalized offering costs will be recorded as an expense to the consolidated statement of operations in the period that the determination is made. The Company’s capitalized offering costs as of September 30, 2012 (Successor) were approximately $863,000. The Company did not incur costs related to the offering during the period ended December 31, 2011 (Successor).
Property and Equipment
Property and equipment is recorded at cost, less accumulated depreciation, in the accompanying consolidated balance sheet. As a result of the acquisition and the related application of purchase accounting to the acquired assets and liabilities, there is a new basis of property and equipment subsequent to the acquisition date. See Note 2 for a discussion of the new basis of accounting for property and equipment. Depreciation expense for property and equipment is computed using the straight-line method over the following estimated useful lives:
| Computer equipment | 5 years | |
| Furniture and fixtures | 7 years | |
| Leasehold improvements | Shorter of the lease term or estimated useful life |
The Company periodically reviews long-lived assets for impairment whenever events or changes in business circumstances indicate that the carrying value of the assets may not be recoverable. No impairment losses were recognized for the periods presented.
Goodwill and Intangible Assets
The Company’s intangible assets arose from the purchase transactions discussed above and consist of goodwill, in-force insureds, the Company’s brand, the carrier network, and distributor relationships. Finite-lived intangible assets are amortized over their useful lives from eight months to seven years.
Goodwill and other intangible assets determined to have indefinite useful lives are not amortized, but are tested for impairment, at least annually or more frequently if indicators of impairment arise. Impairment, if any, is based on the excess of the carrying amount over the fair value of those assets. The Company performs its annual review for goodwill impairment as of October 1 of each year.
The evaluation is performed by comparing the carrying amount of these assets to their estimated fair value. If the estimated fair value is less than the carrying amount of the intangible assets, an impairment charge is
F-10
Table of Contents
Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
Notes to Consolidated Financial Statements (continued)
1. Organization, Basis of Presentation, and Summary of Significant Accounting Policies (continued)
recorded to reduce the asset to its estimated fair value. The Company’s valuation methodologies include, but are not limited to, a discounted cash flow model, which estimates the net present value of the Company’s projected cash flows, and a market approach, which evaluates comparative market multiples applied to the Company’s business to yield a second assumed value.
In estimating fair value, the Company’s methodology requires the Company to make assumptions, the most material of which are sales projections attributable to products sold with these trade names and a weighted-average discount rate. These assumptions are subject to change based on changes in the markets in which these products are sold, which reflect the Company’s projections of future revenues. Factors affecting the weighted-average discount rate include assumed debt-to-equity ratios, risk-free interest rates, and equity returns of each of the market participants in the Company’s industry.
There have been no events that the Company believes would result in an impairment of goodwill and intangible assets as of September 30, 2012 (Successor) and December 31, 2011 (Successor).
Gateway Processor Deposit
The gateway processor deposit on the accompanying consolidated balance sheet as of December 31, 2011 (Successor) represents cash that was held by a gateway credit card/ACH processor as a compensating balance and to mitigate the risk of the gateway credit card/ACH processor in case of member chargebacks. No amounts were held by any processors as of September 30, 2012 (Successor).
Fair Value of Financial Instruments
The Company measures and reports financial assets and liabilities at fair value on a recurring basis. Fair value is defined as the exchange price that would be received for an asset or paid to transfer a liability (referred to as an exit price) in the principal or most advantageous market for the asset or liability in an orderly transaction between market participants on the measurement date. Valuation techniques used to measure fair value must maximize the use of observable inputs and minimize the use of unobservable inputs. The fair value of the Company’s financial assets and liabilities is determined by using three levels of input, which are defined as follows:
| Level 1: |
Quoted prices in active markets for identical assets or liabilities | |
| Level 2: |
Quoted prices in active markets for similar assets or liabilities, quoted prices for identical or similar assets or liabilities in markets that are not active, or inputs other than quoted prices that are observable for the asset or liability | |
| Level 3: |
Unobservable inputs for the asset or liability | |
The categorization of a financial instrument within the valuation hierarchy is based upon the lowest level of input that is significant to the fair value measurement.
The Company utilizes the market approach to measure the fair value of their financial assets. The Company’s long-term debt and noncompete obligation are valued based on Level 2 inputs, and primarily valued using quoted market prices for similar instruments and nonbinding market prices that are corroborated by observable market data. The inputs and fair value are reviewed for reasonableness and may be further validated by comparison to publicly available information or compared to multiple independent valuation sources.
F-11
Table of Contents
Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
Notes to Consolidated Financial Statements (continued)
1. Organization, Basis of Presentation, and Summary of Significant Accounting Policies (continued)
The carrying amounts of financial assets and liabilities reported in the accompanying consolidated balance sheet for cash, cash held on behalf of others, credit card transactions receivable, credit card transactions receivable for others, accounts receivable, notes receivable, advance commissions, carriers and vendors payable, commissions payable, notes payable and accounts payable and accrued expenses at September 30, 2012 (Successor) and December 31, 2011 (Successor), approximate fair value because of the short-term duration of these instruments. See Note 5 to the consolidated financial statements for further discussion of the Company’s borrowings outstanding under debt agreements.
The Company’s long-term debt and noncompete obligation measured at fair value were as follows:
| Fair Value Measurements at September 30, 2012 (Successor) |
||||||||||||||||
| Carrying Value at September 30, 2012 (Successor) |
Level 1 | Level 2 | Level 3 | |||||||||||||
| Long-term debt, including current portion |
$ | 3,490,000 | $ | — | $ | 3,521,000 | $ | — | ||||||||
| Noncompete obligation, including current portion |
843,000 | — | 843,000 | — | ||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| $ | 4,333,000 | $ | — | $ | 4,364,000 | $ | — | |||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Fair Value Measurements at December 31, 2011 (Successor) |
||||||||||||||||
| Carrying Value at December 31, 2011 (Successor) |
Level 1 | Level 2 | Level 3 | |||||||||||||
| Long-term debt, including current portion |
$ | 4,063,000 | $ | — | $ | 4,078,000 | $ | — | ||||||||
|
|
|
|
|
|
|
|
|
|||||||||
2. Business Acquisitions
Acquisition of Naylor ownership
On September 28, 2011, the Company purchased the member units owned by Naylor, which represented a 50% ownership interest in the company, for $5,330,000 plus financing costs of $135,000. The Company financed a portion of the purchase price by entering into a loan agreement with a bank for $4,250,000. The remaining purchase price was funded with the Company’s cash and a special contribution from Michael Kosloske, the current sole member of the Company.
The amount of the purchase price that exceeded the fair value of the net identified tangible and intangible assets acquired is recorded as goodwill. The purchase price was allocated to the assets acquired and liabilities assumed based on their respective fair values.
F-12
Table of Contents
Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
Notes to Consolidated Financial Statements (continued)
2. Business Acquisitions (continued)
The following table summarizes the allocation of the purchase price for the Company’s business acquisition as of September 28, 2011:
| Cash |
$ | 3,127,000 | ||
| Receivables |
891,000 | |||
| Deposits |
406,000 | |||
| Property and equipment, net |
112,000 | |||
| Carriers payable |
(2,410,000 | ) | ||
| Commissions payable |
(1,210,000 | ) | ||
| Accrued expenses and other liabilities |
(452,000 | ) | ||
| Intangible asset—in-force insureds |
240,000 | |||
| Intangible asset—brand |
400,000 | |||
| Intangible asset—carrier network |
40,000 | |||
| Intangible asset—distributor relationships |
3,610,000 | |||
| Goodwill |
5,906,000 | |||
|
|
|
|||
| Total fair value |
$ | 10,660,000 | ||
|
|
|
Acquisition of Insurance Center for Excellence, LLC
On June 1, 2012, the Company and TSG Agency (“TSG”) formed Insurance Center for Excellence, LLC doing business as Insurance Academy (“ICE”). ICE is a call center training facility for the Company’s distributors. In connection with the transaction, the Company received an 80% controlling interest in ICE and was required to contribute $200,000 in capital contributions and TSG received a 20% non-controlling interest in the business and was required to contribute $50,000 in capital contributions. As of September 30, 2012 (Successor), the required contributions by the controlling and non-controlling interests were met.
ICE entered into employment agreements with employees of The Amacore Group, Inc. (“Amacore”) contemporaneously with the June 1, 2012 formation of ICE, and at the date of formation, former Amacore employees comprise the full staff of ICE. ICE additionally assumed a month-to-month lease for space that was occupied by Amacore immediately prior to the formation of ICE.
Concurrent with the formation of ICE, ICE additionally entered into a sublease agreement (“Lease Agreement”) with Amacore for additional space effective June 1, 2012. Under the Lease Agreement, ICE assumed all rights, responsibilities, obligations, terms and conditions of the original lease, which expires on April 30, 2015. Amacore agreed to transfer to ICE a security deposit previously paid by Amacore of approximately $13,000; Amacore contributed $15,000 to ICE for the purchase of property and equipment; and Amacore contributed certain office and computer equipment, and rights to certain 800 numbers, to ICE that have minimal value. The Company is recognizing the consideration provided by Amacore as a lease incentive that is being amortized over the term of the lease on a straight-line basis.
Additionally, concurrent with the June 1, 2012 formation of ICE, ICE entered into an Agent Producer Agreement and an Assignment of Commissions Agreement with Amacore (“collectively referred to as Agent Agreement”). Under the Agent Agreement, ICE assigned its commissions with respect to Assurant dental sales to Amacore in return for production incentives, training, marketing materials, commission payments and reporting, advances on commissions, ongoing sales support and 65% commission rate on sales.
The transaction with Amacore as described above is a business combination, and no assets or liabilities, including intangible assets or goodwill, were recognized other than those described above.
F-13
Table of Contents
Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
Notes to Consolidated Financial Statements (continued)
3. Property and Equipment
Property and equipment, net, are comprised of the following:
| September
30, 2012 (Successor) |
December
31, 2011 (Successor) |
|||||||
| Computer equipment |
$ | 96,000 | $ | 36,000 | ||||
| Furniture and fixtures |
74,000 | 51,000 | ||||||
| Leasehold improvements |
75,000 | 49,000 | ||||||
|
|
|
|
|
|||||
| Total property and equipment |
245,000 | 136,000 | ||||||
| Less accumulated depreciation |
(38,000 | ) | (11,000 | ) | ||||
|
|
|
|
|
|||||
| Total property and equipment, net |
$ | 207,000 | $ | 125,000 | ||||
|
|
|
|
|
|||||
Depreciation expense, including depreciation related to assets acquired through capital leases, was approximately $36,000, $11,000, $29,000, and $7,000, respectively, for the Successor period ended September 30, 2012, the Successor period ended December 31, 2011, the Predecessor period ended September 30, 2011, and the Predecessor year ended December 31, 2010.
4. Goodwill and Intangible Assets
The changes in the carrying amount of goodwill are as follows:
| Balance as of January 1, 2011 (Predecessor) |
$ | — | ||
| Goodwill acquired during the period |
— | |||
| Impairment of goodwill |
— | |||
|
|
|
|||
| Balance as of September 30, 2011 (Predecessor) |
— | |||
| Goodwill acquired during the period |
5,906,000 | |||
| Impairment of goodwill |
— | |||
|
|
|
|||
| Balance as of December 31, 2011 (Successor) |
5,906,000 | |||
| Goodwill acquired during the period |
— | |||
| Impairment of goodwill |
— | |||
|
|
|
|||
| Balance as of September 30, 2012 (Successor) |
$ | 5,906,000 | ||
|
|
|
Major classes of amortizable intangible assets at September 30, 2012 (Successor) consist of the following:
| Weighted- Average Amortization Period (In Years) |
Gross Carrying Amount |
Accumulated Amortization |
Intangible Asset, net |
|||||||||||||
| Distributor relationships |
7 | $ | 3,610,000 | $ | 516,000 | $ | 3,094,000 | |||||||||
| Carrier network |
5 | 40,000 | 8,000 | 32,000 | ||||||||||||
| Brand |
2 | 400,000 | 200,000 | 200,000 | ||||||||||||
| Capitalized software |
5 | 45,000 | 2,000 | 43,000 | ||||||||||||
| Noncompete agreement |
5 | 843,000 | 28,000 | 815,000 | ||||||||||||
|
|
|
|
|
|
|
|||||||||||
| Total intangible assets |
$ | 4,938,000 | $ | 754,000 | $ | 4,184,000 | ||||||||||
|
|
|
|
|
|
|
|||||||||||
F-14
Table of Contents
Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
Notes to Consolidated Financial Statements (continued)
4. Goodwill and Intangible Assets (continued)
Major classes of amortizable intangible assets at December 31, 2011 (Successor) consist of the following:
| Weighted- Average Amortization Period (In Years) |
Gross Carrying Amount |
Accumulated Amortization |
Intangible Asset, net |
|||||||||||||
| Distributor relationships |
7 | $ | 3,610,000 | $ | 127,000 | $ | 3,483,000 | |||||||||
| Carrier network |
5 | 40,000 | 2,000 | 38,000 | ||||||||||||
| Brand |
2 | 400,000 | 50,000 | 350,000 | ||||||||||||
| In-force insureds |
0.8 | 240,000 | 80,000 | 160,000 | ||||||||||||
|
|
|
|
|
|
|
|||||||||||
| Total intangible assets |
$ | 4,290,000 | $ | 259,000 | $ | 4,031,000 | ||||||||||
|
|
|
|
|
|
|
|||||||||||
Amortization expense for the nine months ended September 30, 2012 (Successor) and three months ended December 31, 2011 (Successor) was approximately $735,000 and $259,000, respectively. There was no amortization expense for the nine months ended September 30, 2011 (Predecessor) and year ended December 31, 2010 (Predecessor).
Amortization expense expected to be recognized subsequent to September 30, 2012 (Successor) is as follows:
| Remainder of 2012 |
$ | 225,000 | ||
| 2013 |
851,000 | |||
| 2014 |
701,000 | |||
| 2015 |
701,000 | |||
| 2016 |
699,000 | |||
| Thereafter |
1,007,000 | |||
|
|
|
|||
| Total |
$ | 4,184,000 | ||
|
|
|
5. Debt
During September 2011, the Company entered into a bank loan agreement with a principal balance of $4,250,000. The purpose of this credit loan was to finance a portion of the acquisition of the remaining 50% interest in the Company as discussed in Note 2. Borrowings under the facility are secured by all of the Company’s assets, including, but not limited to, cash accounts, accounts receivable, and property and equipment. The loan is further secured with a personal unlimited guarantee by Kosloske and certain real properties owned by Kosloske in Tampa, Florida and Keystone, Colorado. The loan is a self-amortizing five-year loan bearing fixed interest at 5.25% with equal monthly payments of approximately $81,000, which consists of principal and interest. As of September 30, 2012 (Successor) and December 31, 2011 (Successor), balances of approximately $3,490,000 and $4,063,000, respectively, were outstanding, including current portions of approximately $802,000 and $769,000, respectively.
The loan is subject to customary covenants and restrictions which, among other things, limit the Company’s ability to incur additional indebtedness. In addition, the loan agreement also includes certain nonfinancial covenants that would require immediate payment if the Company, among other things, reorganizes, merges, consolidates, or otherwise changes ownership or business structure without the bank’s prior written consent.
F-15
Table of Contents
Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
Notes to Consolidated Financial Statements (continued)
5. Debt (continued)
The loan agreement also contains customary representations and warranties and events of default. The payment of outstanding principal under the loan and accrued interest thereon may be accelerated and become immediately due and payable upon default of payment or failure to meet certain other performance obligations or failure to comply with other covenants in the loan agreement, subject to applicable notice requirements and cure periods as provided in the loan agreement.
On August 11, 2012, the Company and Health Plan Intermediaries Holdings, LLC (“HPIH”) entered into an Assumption and Reaffirmation of Loan Documents and Consent to Assignment (“Assignment”) with the lender to conditionally transfer the loan from the Company to HPIH. The Assignment required two post-closing conditions to be met. The first condition was met on September 18, 2012. The second condition was met on November 7, 2012.
At September 30, 2012 (Successor) and December 31, 2011 (Successor), the Company was in compliance with all applicable covenants.
Future principal payments on the loan subsequent to September 30, 2012 (Successor) are as follows:
| Remainder of 2012 |
$ | 196,000 | ||
| 2013 |
813,000 | |||
| 2014 |
857,000 | |||
| 2015 |
904,000 | |||
| 2016 |
720,000 | |||
|
|
|
|||
| Total minimum payments |
$ | 3,490,000 | ||
|
|
|
6. Deferred Financing Costs
Deferred financing costs consist primarily of consulting and legal fees directly related to the bank loan. These amounts are amortized over the life of the related debt using the effective interest rate method. Deferred financing costs reported on the consolidated balance sheets were approximately $88,000 and $122,000 as of September 30, 2012 (Successor) and December 31, 2011 (Successor), respectively. Amortization of the loan costs was approximately $34,000 for the nine months ended September 30, 2012 (Successor) and $13,000 for the Successor period ending December 31, 2011 (Successor). There was no amortization for the nine months ended September 30, 2011 (Predecessor) and year ended December 31, 2010 (Predecessor).
F-16
Table of Contents
Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
Notes to Consolidated Financial Statements (continued)
7. Accounts Payable and Accrued Expenses
Accounts payable and accrued expenses consisted of the following at:
| September
30, 2012 (Successor) |
December
31, 2011 (Successor) |
|||||||
| Accounts payable |
$ | 674,000 | $ | 75,000 | ||||
| Accrued professional fees |
377,000 | — | ||||||
| Accrued refunds |
242,000 | 87,000 | ||||||
| Deferred salaries |
30,000 | 10,000 | ||||||
| Accrued wages |
167,000 | 49,000 | ||||||
| Accrued credit card/ACH fees |
50,000 | 31,000 | ||||||
| Due to Naylor as a result of acquisition |
— | 80,000 | ||||||
| Other accrueds |
— | 10,000 | ||||||
|
|
|
|
|
|||||
| Total accounts payable and accrued expenses |
$ | 1,540,000 | $ | 342,000 | ||||
|
|
|
|
|
|||||
8. Segments
Operating segments are defined as components of an enterprise about which separate financial information is available that is evaluated regularly by the chief operating decision-maker, or decision-making group, in deciding how to allocate resources and in assessing performance of the Company. The Company’s chief operating decision-maker is considered to be the chief executive officer (CEO). The CEO reviews the Company’s financial information in a manner substantially similar to the accompanying consolidated financial statements. In addition, the Company’s operations, revenues, and decision-making functions are based solely in the United States. Therefore, management has concluded that the Company operates in one operating and geographic segment.
9. Related-Party Transactions
On August 22, 2012, the Company entered into a promissory note with Ivan Spinner who controls TSG, the 20% owner of Insurance Center for Excellence, LLC, in the amount of $100,000 for the purpose of funding advanced commissions. The note is non-interest bearing and requires equal monthly payments of $25,000 beginning September 20, 2012 and ending December 20, 2012. No payments on this note were made as of September 30, 2012 (Successor). Payments totaling $50,000 were made subsequent to September 30, 2012. Subsequently, this loan was modified on October 18, 2012 whereby the November and December payments were deferred to January 2, 2013 and February 1, 2013, respectively.
Under an employment agreement, Kosloske received compensation from prescription contracts plus commissions based on annual revenues. This compensation was treated as guaranteed payments during the Predecessor periods. The agreement was terminated in conjunction with the acquisition discussed in Note 2. The guaranteed payment expense totaled approximately $615,000 and $485,000 for the Predecessor period ended September 30, 2011, and the Predecessor year ending December 31, 2010, respectively, and was recorded as general and administrative expenses in the consolidated statements of operations.
The Company had an outstanding payable to Kosloske of approximately $126,000 as of December 31, 2011 (Successor) for unreimbursed expenses paid by Kosloske on behalf of the Company and is included within due to member in the consolidated balance sheet at December 31, 2011 (Successor). At September 30, 2012 (Successor), there was no amount due to member.
F-17
Table of Contents
Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
Notes to Consolidated Financial Statements (continued)
9. Related-Party Transactions (continued)
From January 1, 2010 to October 31, 2010, the Company leased office space from Kosloske. Lease payments during this period were approximately $35,000 and were recorded as general and administrative expenses in the consolidated statement of operations for the Predecessor year ended December 31, 2010.
The Company incurred management fees for accounting and administrative services performed by Naylor, in the amount of $93,000 and $50,000, which are included in general and administrative expenses on the consolidated statements of operations for the Predecessor period ended September 30, 2011 and Predecessor year ended December 31, 2010, respectively.
10. Commitments and Contingencies
Call and Put Option for ICE
In accordance with the ICE operating agreement, the Company has the right of first refusal to purchase any membership units that another member may desire to transfer. Written notice shall be provided to the Company and contain a full description of the proposed transfer including the type of transfer, the units of the proposed transfer, purchase price and payment method of proposed transfer, and the true identity of the parties involved in the proposed transfer. If the Company desires to purchase all or a portion of the units proposed to be transferred, it must give a binding written notice of the exercise of its option along with the specific number of units it intends to purchase. The Company shall have 60 days after it provides notice to close the purchase.
In the event of Ivan Spinner’s death or disability or a change of control of TSG (“Termination Event”), the Company additionally has the option to repurchase all the membership units of TSG or its affiliates. At any time a TSG Affiliate (i.e., TSG, Ivan Spinner and any permitted transferee of TSG or Ivan Spinner, collectively referred to as “TSG Affiliates”) may elect to sell to the Company all of the units owned by the TSG Affiliates by delivering a single written notice to the Company. The Company then has a period of 10 days following receipt of such notice by delivering a written notice to TSG to either (1) elect to purchase all of the TSG Affiliate units or (2) elect to sell to TSG all of the units owned by the Company and its permitted transferees. In the event the Company does not deliver the aforementioned notice, then the Company shall be deemed to have agreed to purchase all of the TSG Affiliate units. Transfers with respect to a Termination Event or TSG Affiliate are based upon fair market value as determined by a nationally recognized independent appraiser.
BimSym Agreements
On August 1, 2012, the Company entered into a software assignment agreement (“Agreement”) with BimSym eBusiness Solutions, Inc. (“BimSym”) for the Company’s exclusive ownership of all rights, title and interest in the technology platform (“ARIES System”) developed by BimSym and utilized by the Company. As a result of the executed Agreement, the Company owes BimSym a cash payment of $45,000, which is recorded as an accounts payable and accrued expense on the accompanying consolidated balance sheet as of September 30, 2012. The consideration of $45,000 was capitalized and recorded as an intangible asset. In connection with this agreement, the Company simultaneously entered into a master services agreement for the technology, under which the Company is required to make monthly payments of $26,000 for 5 years. After the five-year term, this agreement automatically renews for one-year terms unless 60 days’ notice is given by the Company.
Additionally, the Company also entered into an exclusivity agreement with BimSym whereby neither BimSym nor any of its affiliates will create, market or sell a software, system or service with the same or similar
F-18
Table of Contents
Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
Notes to Consolidated Financial Statements (continued)
10. Commitments and Contingencies (continued)
functionality as that of ARIES System under which the Company is required to make monthly payments of $16,000 for 5 years. The present value of these payments has been capitalized and recorded as an intangible asset with a corresponding liability, on the accompanying consolidated balance sheet as of September 30, 2012.
Legal Proceedings
As of September 30, 2012 (Successor) and December 31, 2011 (Successor), the Company had no significant outstanding legal proceedings. The Company is subject to certain legal proceedings and claims that may arise in the ordinary course of business. In the opinion of management, the Company does not have a potential liability related to any current legal proceedings and claims that would individually, or in the aggregate, have a material adverse effect on the Company’s financial condition, liquidity, results of operations, or cash flows.
11. Concentrations of Credit Risk and Significant Customers
Financial instruments that are potentially subject to concentrations of credit risk consist primarily of cash, credit card transactions receivable, accounts receivable, and advance commissions.
Cash is maintained in noninterest-bearing accounts at depository institutions and amounts held at these institutions were fully insured by the Federal Deposit Insurance Corporation as of September 30, 2012 (Successor) and December 31, 2011 (Successor).
The Company generally does not require collateral for credit card transactions receivable or accounts receivable. However, advance commissions are collateralized by renewal commissions. The Company has not experienced any credit losses related to these receivables and advances.
Advanced commissions were approximately $300,000 and $24,000 as of September 30, 2012 (Successor) and December 31, 2011 (Successor), respectively. As of September 30, 2012 (Successor) and December 31, 2011 (Successor) a single agency made up 44% and 93% of the advance commissions balance.
Accounts receivable were approximately $315,000 and $254,000 as of September 30, 2012 (Successor) and December 31, 2011 (Successor), respectively. As of September 30, 2012 (Successor) and December 31, 2011 (Successor), a single distributor made up 72% of the accounts receivable balance for each period.
Revenues consist of commissions earned for health insurance policies and discount benefit plans issued to members, enrollment fees paid by members, and monthly administration fees paid by members as a direct result of enrollment services provided by the Company. None of the Company’s members individually accounted for 10% or more of the Company’s revenue for the nine-month period ended September 30, 2012 (Successor), three-month period ended December 31, 2011 (Successor), nine-month period ended September 30, 2011 (Predecessor), or year ended December 31, 2010 (Predecessor).
During the nine-month period ended September 30, 2012, three carriers represented 50%, 25% and 19% of premium equivalents, respectively.
F-19
Table of Contents
Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
Notes to Consolidated Financial Statements (continued)
12. Capital Lease Obligations
The Company has entered into capital lease obligations to finance certain equipment. The leases have terms expiring beginning in 2015. As of September 30, 2012 (Successor), future cash payment commitments related to these leases are as follows:
| Remainder of 2012 |
$ | 1,000 | ||
| 2013 |
3,000 | |||
| 2014 |
3,000 | |||
| 2015 |
1,000 | |||
|
|
|
|||
| Total minimum lease payments |
8,000 | |||
| Less amounts representing interest |
(1,000 | ) | ||
|
|
|
|||
| Total capital lease obligations |
$ | 7,000 | ||
|
|
|
13. Operating Leases
The Company leases office facilities under an operating lease, which expires in 2015. The operating lease agreement contains rent holidays and rent escalation provisions. Rent holidays and rent escalation provisions are considered in determining straight-line rent expense to be recorded over the lease term. The difference between cash rent payments and straight-line rent expense is recorded as deferred rent on the balance sheet and was approximately $61,000 as of September 30, 2012 (Successor) and $16,000 as of December 31, 2011 (Successor).
Total rent expense under all operating leases, which includes equipment for the Successor period ended September 30, 2012, was approximately $132,000, $28,000, $78,000 and $71,000, for the Successor periods ended September 30, 2012 and December 31, 2011, the Predecessor period ended September 30, 2011, and the Predecessor year ended December 31, 2010, respectively, and is included in general and administrative expenses in the accompanying consolidated statements of operations.
As of September 30, 2012 (Successor), the future minimum lease payments under noncancellable operating leases were as follows:
| Remainder of 2012 |
$ | 56,000 | ||
| 2013 |
218,000 | |||
| 2014 |
222,000 | |||
| 2015 |
102,000 | |||
|
|
|
|||
| Total minimum lease payments |
$ | 598,000 | ||
|
|
|
14. Income Tax
The Company was treated as a partnership for tax purposes prior to the change in ownership on September 28, 2011. Subsequently, the Company became a single-member LLC treated as a disregarded entity not separate from its owner for income tax purposes. Income tax for the Company for both its time as a partnership and then as a single-member LLC, is the responsibility of its member. As a result, no provision for income taxes is reflected in the accompanying consolidated financial statements. Net income for financial statement purposes may differ significantly from taxable income attributable to members as a result of differences between the tax basis and the financial reporting basis of assets and liabilities.
F-20
Table of Contents
Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
Notes to Consolidated Financial Statements (continued)
15. Pro Forma Disclosure (Unaudited)
Health Insurance Innovations, Inc. will operate and control all of the businesses and affairs of Health Plan Intermediaries Holdings, LLC and its subsidiaries. Under ASC 810, Consolidation, Health Plan Intermediaries Holdings, LLC meets the definition of a variable interest entity. Further, Health Insurance Innovations, Inc. will be the primary beneficiary of Health Plan Intermediaries Holdings, LLC as a result of its 100% voting power and control over Health Plan Intermediaries Holdings, LLC and as a result of its obligation to absorb losses and its right to receive benefits of Health Plan Intermediaries Holdings, LLC that could potentially be significant to Health Plan Intermediaries Holdings, LLC. As a result, Health Insurance Innovations, Inc. is expected to consolidate the financial results of Health Plan Intermediaries Holdings, LLC and record a non-controlling interest for the economic interest in Health Plan Intermediaries Holdings, LLC held by the existing members to the extent that the book value of their interest in Health Plan Intermediaries Holdings, LLC is greater than zero. Health Insurance Innovations, Inc.’s and the non-controlling membership pro forma economic interest in Health Plan Intermediaries Holdings, LLC is estimated to be 35% and 65%, respectively, as of September 30, 2012. Pro forma net income attributable to the non-controlling interest on the statements of operations represents the portion of earnings or loss attributable to the economic interest in Health Plan Intermediaries Holdings, LLC held by the non-controlling members. Non-controlling interest on the balance sheet represents the portion of net assets of Health Plan Intermediaries Holdings, LLC attributable to the non-controlling members based on total membership interest of Health Plan Intermediaries Holdings, LLC owned by such members.
The Company has elected to be taxed as an S-Corporation under the provisions of the Internal Revenue Code. The following unaudited pro forma information reflects the reconciliation between the total statutory provision for income taxes and the total actual provision relating to the income tax expense that would have been incurred if the S-Corporation were subject to U.S. federal and state income taxes. The Company would account for income taxes under the provisions of ASC 740, Accounting for Income Taxes, which requires recognition of deferred tax assets and liabilities for the expected future consequences of events that have been included in the financial statements or tax returns. Under this method, deferred income tax assets and liabilities are determined based on the difference between the financial statement and tax bases of assets and liabilities using enacted tax rates for the year in which the differences are expected to reverse.
| Nine—Month Period Ended September 30, 2012 (Successor) |
Three—Month Period Ended December 31, 2011 (Successor) |
Nine—Month Period Ended September 30, 2011 (Predecessor) |
Year
Ended December 31, 2010 (Predecessor) |
|||||||||||||||
| Pro forma statutory tax provision |
$ | 879,000 | $ | 180,000 | $ | 626,000 | $ | (2,000 | ) | |||||||||
| State income taxes, net |
63,000 | 12,000 | 43,000 | (1,000 | ) | |||||||||||||
| Nondeductible expenses |
27,000 | 9,000 | 26,000 | 4,000 | ||||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||
| Pro forma total provision for income taxes |
$ | 969,000 | $ | 201,000 | $ | 695,000 | $ | 1,000 | ||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||
Pro forma net income per common share outstanding: Pro forma basic and diluted net income (loss) per share was computed by dividing the pro forma net income (loss) attributable to our Class A stockholders by the 4,666,667 shares of Class A common stock that we will issue and sell in this offering and the vested shares of Mr. Hershberger’s Class A restricted stock grant (assuming that the underwriters do not exercise their option to purchase an additional shares of Class A common stock to cover over-allotments). For the year ended December 31, 2011, there was no effect of dilutive restricted shares due to the pro forma net loss position. For the nine-month period ended September 30, 2012, the dilutive effect of the restricted shares was 83,845 shares. The shares of Class B common stock do not share in our earnings and are therefore not included in the weighted average shares outstanding or net income available per share.
F-21
Table of Contents
Health Plan Intermediaries, LLC
d/b/a Health Insurance Innovations
Notes to Consolidated Financial Statements (continued)
| Nine Months Ended September 30, 2012 |
Year Ended December 31, 2012 |
|||||||
| (Successor) | (Combined) (Non-GAAP) |
|||||||
| (in thousands, except shares and per share amounts) |
||||||||
| Pro forma net income (loss) |
$ | 1,100 | $ | (858 | ) | |||
| Net income (loss) attributable to non-controlling interest |
756 | (558 | ) | |||||
|
|
|
|
|
|||||
| Net income (loss) attributable to Health Insurance Innovations, Inc. |
$ | 344 | $ | (300 | ) | |||
|
|
|
|
|
|||||
| Weighted average shares Class A common stock outstanding |
||||||||
| Basic |
4,906,000 | 4,826,667 | ||||||
| Diluted |
4,982,822 | 4,826,667 | ||||||
| Net income available to Class A common stock per share |
||||||||
| Basic |
$ | 0.07 | $ | (0.06 | ) | |||
| Diluted |
$ | 0.07 | $ | (0.06 | ) | |||
16. Subsequent Events
The sole member of the Company has authorized the filing of a registration statement with the Securities and Exchange Commission for an initial public offering of Class A common stock of Health Insurance Innovations, Inc. Upon completion of the offering, Health Insurance Innovations, Inc. will be a holding company the principal asset of which will be its interest in the Company. Health Insurance Innovations, Inc. will be the sole managing member of the Company.
On October 31, 2012, in connection with the offering Health Plan Intermediaries Sub, LLC, a subsidiary of Health Plan Intermediaries, LLC, was formed.
On November 7, 2012, the Company’s assets and liabilities were transferred to another entity via a series of assignments, to facilitate the conversion of the Company to an S-Corporation.
On January 24, 2013, the Company signed a Commitment Letter with SunTrust Bank to supplement the existing bank loan agreement with SunTrust Bank with a new $2,000,000 revolving credit facility. If the Company enters into and draws on the revolving credit facility, the proceeds will be used to finance costs associated with this offering and to fund advance commission payments to distributors. The new revolving credit facility will have a total commitment for loans up to $2,000,000. The maturity of the new revolving credit facility will be 364 days from the date of closing and the loans will bear interest at a rate of LIBOR plus 3.50%. Borrowings under the revolving credit facility will be collateralized by substantially all of the assets of the Company (as well as the pledge of equity interests in Health Plan Intermediaries, LLC owned by Kosloske and a further assignment of a $4,500,000 life insurance policy on Kosloske), and SunTrust Bank will have a second lien position behind SunTrust Bank’s existing first lien on substantially all of the assets of the Company pursuant to the existing bank loan agreement. The new revolving credit facility will have customary affirmative and negative covenants including, without limitation, a Minimum Net Worth Covenant and limitations on dividends during any event of default. The commitment is conditional upon, among other things, no material adverse change in the Company’s business and final negotiation of the credit agreement. The Commitment Letter expires on March 31, 2013.
F-22
Table of Contents

Table of Contents
PART II
INFORMATION NOT REQUIRED IN PROSPECTUS
Item 13. Other Expenses of Issuance and Distribution
| Amount To Be Paid |
||||
| Registration fee |
$ | 11,764 | ||
| FINRA filing fee |
15,500 | |||
| Listing fee |
25,000 | |||
| Transfer agent’s fees |
3,500 | |||
| Printing and engraving expenses |
100,000 | |||
| Legal fees and expenses |
1,000,000 | |||
| Accounting fees and expenses |
750,000 | |||
| Blue Sky fees and expenses |
0 | |||
| Miscellaneous |
600,000 | |||
|
|
|
|||
| Total |
$ | 2,505,764 | ||
|
|
|
|||
Each of the amounts set forth above, other than the registration fee and the FINRA filing fee, is an estimate.
Item 14. Indemnification of Directors and Officers
Section 145 of the Delaware General Corporation Law provides that a corporation may indemnify directors and officers as well as other employees and individuals against expenses (including attorneys’ fees), judgments, fines and amounts paid in settlement actually and reasonably incurred by such person in connection with any threatened, pending or completed actions, suits or proceedings in which such person is made a party by reason of such person being or having been a director, officer, employee or agent to the registrant. The Delaware General Corporation Law provides that Section 145 is not exclusive of other rights to which those seeking indemnification may be entitled under any bylaw, agreement, vote of stockholders or disinterested directors or otherwise. The registrant’s amended and restated certificate of incorporation will provide for indemnification by the registrant of its directors, officers and employees to the fullest extent permitted by the Delaware General Corporation Law.
Section 102(b)(7) of the Delaware General Corporation Law permits a corporation to provide in its certificate of incorporation that a director of the corporation shall not be personally liable to the corporation or its stockholders for monetary damages for breach of fiduciary duty as a director, except for liability (1) for any breach of the director’s duty of loyalty to the corporation or its stockholders, (2) for acts or omissions not in good faith or which involve intentional misconduct or a knowing violation of law, (3) for unlawful payments of dividends or unlawful stock repurchases, redemptions or other distributions, or (4) for any transaction from which the director derived an improper personal benefit. The registrant’s amended and restated certificate of incorporation will provide for such limitation of liability.
The registrant maintains standard policies of insurance under which coverage is provided (a) to its directors and officers against loss rising from claims made by reason of breach of duty or other wrongful act, and (b) to the registrant with respect to payments which may be made by the registrant to such officers and directors pursuant to the above indemnification provision or otherwise as a matter of law.
The proposed form of underwriting agreement filed as Exhibit 1 to this registration statement provides for indemnification of directors and officers of the registrant by the underwriters against certain liabilities.
Item 15. Recent Sales of Unregistered Securities
On October 26, 2012, the registrant issued 100 shares of the registrant’s common stock, par value $0.01 per share, to Michael W. Kosloske for $1.00. The issuance of such shares of common stock was not registered under the Securities Act because the shares were offered and sold in a transaction exempt from registration under Section 4(a)(2) of the Securities Act.
II-1
Table of Contents
Item 16. Exhibits and Financial Statement Schedules
(a) The following exhibits are filed as part of this registration statement:
| Exhibit Number |
Description | |
| 1.1** | Form of Underwriting Agreement | |
| 3.1** | Certificate of Incorporation of Health Insurance Innovations, Inc., as currently in effect | |
| 3.2** | Bylaws of Health Insurance Innovations, Inc., as currently in effect | |
| 3.3** | Form of Amended and Restated Certificate of Incorporation of Health Insurance Innovations, Inc. | |
| 3.4** | Form of Amended and Restated Bylaws of Health Insurance Innovations, Inc. | |
| 4.1** | Form of Class A common stock Certificate | |
| 4.2** | Form of Registration Rights Agreement | |
| 5.1** | Opinion of Davis Polk & Wardwell LLP | |
| 10.1** | Form of Third Amended and Restated Limited Liability Company Agreement of Health Plan Intermediaries Holdings, LLC | |
| 10.2** | Contribution Agreement between Health Plan Intermediaries Holdings, LLC and Health Plan Intermediaries, LLC | |
| 10.3** | Unit Purchase Agreement among Michael W. Kosloske, Naylor Group Partners, LLC, Mathew S. Naylor and Russell R. Naylor and Health Plan Intermediaries, LLC | |
| 10.4** | Amendment to United Purchase Agreement among Michael W. Kosloske, Naylor Group Partners, LLC, Mathew S. Naylor and Russell R. Naylor and Health Plan Intermediaries, LLC | |
| 10.5** | Form of Tax Receivable Agreement | |
| 10.6** | Form of Exchange Agreement | |
| 10.7** | Loan Agreement between Health Plan Intermediaries, LLC and SunTrust Bank | |
| 10.8** | Master Service Agreement between Health Plan Intermediaries, LLC and BimSym eBusiness Solutions, Inc. | |
| 10.9** | Software Assignment Agreement between Health Plan Intermediaries, LLC and BimSym eBusiness Solutions, Inc. | |
| 10.10**† | General Manager’s Agreement between Health Plan Intermediaries, LLC and Companion Life Insurance Company | |
| 10.11**† | Agency Agreement between Health Plan Intermediaries, LLC and Starr Indemnity & Liability Company | |
| 10.12** | Administrative Services Agreement among Health Insurance Innovations, LLC, United States Fire Insurance Company and The North River Insurance Company | |
| 10.13** | Marketing/Billing Agreement between Med-Sense Guaranteed Association and Health Insurance Innovations | |
| 10.14**# | Form of Employment Agreement between Michael W. Kosloske and Health Insurance Innovations, Inc. | |
| 10.15**# | [Intentionally omitted] | |
| 10.16**# | Employment and Non-Compete Agreement between Gary Raeckers and Health Plan Intermediaries, LLC | |
| 10.17**# | Employment and Non-Compete Agreement between Scott Lingle and Health Plan Intermediaries, LLC | |
| 10.18**# | Form of Employment Agreement between Lori Kosloske and Health Insurance Innovations, Inc. | |
| 10.19**# | Employment and Non-Compete Agreement between Bryan Krul and Health Plan Intermediaries, LLC | |
| 10.20**# | Form of Health Insurance Innovations, Inc. Long Term Incentive Plan | |
| 10.21**# | Form of Restricted Stock Award Agreement pursuant to the Health Insurance Innovations, Inc. Long Term Incentive Plan between Health Insurance Innovations, Inc. and Michael D. Hershberger | |
| 10.22** | Office Lease Agreement between Health Plan Intermediaries, LLC and Magdalene Center of Tampa, LLC | |
| 10.23** | Commitment Letter between Health Plan Intermediaries Holdings, LLC and SunTrust Bank | |
| 10.24**# | Form of Employment Agreement between Michael D. Hershberger and Health Insurance Innovations, Inc. | |
| 16.1** | Letter from former accountants addressed to the Securities and Exchange Commission | |
| 21.1** | List of subsidiaries | |
| 23.1 | Consent of Ernst & Young LLP, independent registered public accounting firm | |
| 23.2** | Consent of Davis Polk & Wardwell LLP (included in Exhibit 5.1) | |
| 24.1** | Power of Attorney (included on signature page) | |
| 99.1** | [Intentionally omitted] | |
II-2
Table of Contents
| Exhibit |
Description | |
| 99.2** | Consent of Liana O’Drobinak, as director nominee | |
| 99.3** | Consent of Gordon Tunstall, as director nominee | |
| 99.4** | Consent of Paul E. Avery, as director nominee | |
| 99.5** | Consent of Gary Raeckers, as director nominee | |
| ** | Previously filed |
| # | Management contract or compensatory arrangement |
| † | Confidential treatment requested. |
(b) The following financial statement schedule is filed as part of this registration statement:
Schedules have been omitted because the information required to be set forth therein is not applicable or is shown in the financial statements or notes thereto.
Item 17. Undertakings
The undersigned registrant hereby undertakes:
(a) The undersigned registrant hereby undertakes to provide to the underwriter at the closing specified in the underwriting agreement certificates in such denominations and registered in such names as required by the underwriter to permit prompt delivery to each purchaser.
(b) Insofar as indemnification for liabilities arising under the Securities Act of 1933 may be permitted to directors, officers and controlling persons of the registrant pursuant to the provisions referenced in Item 14 of this registration statement, or otherwise, the registrant has been advised that in the opinion of the Securities and Exchange Commission such indemnification is against public policy as expressed in the Act and is, therefore, unenforceable. In the event that a claim for indemnification against such liabilities (other than the payment by the registrant of expenses incurred or paid by a director, officer, or controlling person of the registrant in the successful defense of any action, suit or proceeding) is asserted by such director, officer or controlling person in connection with the securities being registered hereunder, the registrant will, unless in the opinion of its counsel the matter has been settled by controlling precedent, submit to a court of appropriate jurisdiction the question of whether such indemnification by it is against public policy as expressed in the Act and will be governed by the final adjudication of such issue.
(c) The undersigned registrant hereby undertakes that:
(1) For purposes of determining any liability under the Securities Act of 1933, the information omitted from the form of prospectus filed as part of this registration statement in reliance upon Rule 430A and contained in a form of prospectus filed by the registrant pursuant to Rule 424(b)(1) or (4) or 497(h) under the Securities Act shall be deemed to be part of this registration statement as of the time it was declared effective.
(2) For the purpose of determining any liability under the Securities Act of 1933, each post-effective amendment that contains a form of prospectus shall be deemed to be a new registration statement relating to the securities offered therein, and the offering of such securities at that time shall be deemed to be the initial bona fide offering thereof.
II-3
Table of Contents
SIGNATURES
Pursuant to the requirements of the Securities Act of 1933, the registrant has duly caused this registration statement to be signed on its behalf by the undersigned, thereunto duly authorized, in the City of Tampa, State of Florida, on the 4th day of February, 2013.
| Health Insurance Innovations, Inc. | ||||
| By: | /s/ Michael W. Kosloske | |||
| Name: Michael W. Kosloske | ||||
| Title: Chairman, President and Chief Executive Officer | ||||
II-4
Table of Contents
KNOW ALL MEN BY THESE PRESENTS, that each person whose signature appears below constitutes and appoints Michael W. Kosloske, Michael D. Hershberger, and each of them, his or her true and lawful attorneys-in-fact and agents, with full power of substitution and resubstitution, for him or her and in his or her name, place and stead, in any and all capacities, to sign any and all amendments (including post-effective amendments) to this registration statement and any and all additional registration statements pursuant to Rule 462(b) of the Securities Act of 1933, and to file the same, with all exhibits thereto, and all other documents in connection therewith, with the Securities and Exchange Commission, granting unto each said attorney-in-fact and agents full power and authority to do and perform each and every act in person, hereby ratifying and confirming all that said attorneys-in-fact and agents or either of them or their or his or her substitute or substitutes may lawfully do or cause to be done by virtue hereof.
Pursuant to the requirements of the Securities Act of 1933, this registration statement has been signed by the following persons in the capacities and on the dates indicated.
| Signature |
Title |
Date | ||
| /s/ Michael W. Kosloske Michael W. Kosloske |
Chairman, President and Chief Executive Officer (principal executive officer) |
February 4, 2013 | ||
| /s/ Michael D. Hershberger Michael D. Hershberger |
Chief Financial Officer (principal financial officer) |
February 4, 2013 | ||
| /s/ Joan Rodgers Joan Rodgers |
Chief Accounting Officer (principal accounting officer) |
February 4, 2013 | ||
II-5
Table of Contents
EXHIBIT INDEX
| Exhibit |
Description | |
| 1.1** | Form of Underwriting Agreement | |
| 3.1** | Certificate of Incorporation of Health Insurance Innovations, Inc., as currently in effect | |
| 3.2** | Bylaws of Health Insurance Innovations, Inc., as currently in effect | |
| 3.3** | Form of Amended and Restated Certificate of Incorporation of Health Insurance Innovations, Inc. | |
| 3.4** | Form of Amended and Restated Bylaws of Health Insurance Innovations, Inc. | |
| 4.1** | Form of Class A common stock Certificate | |
| 4.2** | Form of Registration Rights Agreement | |
| 5.1** | Opinion of Davis Polk & Wardwell LLP | |
| 10.1** | Form of Third Amended and Restated Limited Liability Company Agreement of Health Plan Intermediaries Holdings, LLC | |
| 10.2** | Contribution Agreement between Health Plan Intermediaries Holdings, LLC and Health Plan Intermediaries, LLC | |
| 10.3** | Unit Purchase Agreement among Michael W. Kosloske, Naylor Group Partners, LLC, Mathew S. Naylor and Russell R. Naylor and Health Plan Intermediaries, LLC | |
| 10.4** | Amendment to United Purchase Agreement among Michael W. Kosloske, Naylor Group Partners, LLC, Mathew S. Naylor and Russell R. Naylor and Health Plan Intermediaries, LLC | |
| 10.5** | Form of Tax Receivable Agreement | |
| 10.6** | Form of Exchange Agreement | |
| 10.7** | Loan Agreement between Health Plan Intermediaries, LLC and SunTrust Bank | |
| 10.8** | Master Service Agreement between Health Plan Intermediaries, LLC and BimSym eBusiness Solutions, Inc. | |
| 10.9** | Software Assignment Agreement between Health Plan Intermediaries, LLC and BimSym eBusiness Solutions, Inc. | |
| 10.10**† | General Manager’s Agreement between Health Plan Intermediaries, LLC and Companion Life Insurance Company | |
| 10.11**† | Agency Agreement between Health Plan Intermediaries, LLC and Starr Indemnity & Liability Company | |
| 10.12** | Administrative Services Agreement among Health Insurance Innovations, LLC, United States Fire Insurance Company and The North River Insurance Company | |
| 10.13** | Marketing/Billing Agreement between Med-Sense Guaranteed Association and Health Insurance Innovations | |
| 10.14**# | Form of Employment Agreement between Michael W. Kosloske and Health Insurance Innovations, Inc. | |
| 10.15**# | [Intentionally omitted] | |
| 10.16**# | Employment and Non-Compete Agreement between Gary Raeckers and Health Plan Intermediaries, LLC | |
| 10.17**# | Employment and Non-Compete Agreement between Scott Lingle and Health Plan Intermediaries, LLC | |
| 10.18**# | Form of Employment Agreement between Lori Kosloske and Health Insurance Innovations, Inc. | |
| 10.19**# | Employment and Non-Compete Agreement between Bryan Krul and Health Plan Intermediaries, LLC | |
| 10.20**# | Form of Health Insurance Innovations, Inc. Long Term Incentive Plan | |
| 10.21**# | Form of Restricted Stock Award Agreement pursuant to the Health Insurance Innovations, Inc. Long Term Incentive Plan between Health Insurance Innovations, Inc. and Michael D. Hershberger | |
| 10.22** | Office Lease Agreement between Health Plan Intermediaries, LLC and Magdalene Center of Tampa, LLC | |
| 10.23** | Commitment Letter between Health Plan Intermediaries Holdings, LLC and SunTrust Bank | |
| 10.24**# | Form of Employment Agreement between Michael D. Hershberger and Health Insurance Innovations, Inc. | |
| 16.1** | Letter from former accountants addressed to the Securities and Exchange Commission | |
| 21.1** | List of subsidiaries | |
| 23.1 | Consent of Ernst & Young LLP, independent registered public accounting firm | |
| 23.2** | Consent of Davis Polk & Wardwell LLP (included in Exhibit 5.1) | |
| 24.1** | Power of Attorney (included on signature page) | |
| 99.1** | [Intentionally omitted] | |
| 99.2** | Consent of Liana O’Drobinak, as director nominee | |
| 99.3** | Consent of Gordon Tunstall, as director nominee | |
| 99.4** | Consent of Paul E. Avery, as director nominee | |
| 99.5** | Consent of Gary Raeckers, as director nominee | |
| ** | Previously filed |
| # | Management contract or compensatory arrangement |
| † | Confidential treatment requested. |
II-6
