Attached files
| file | filename |
|---|---|
| 8-K - FORM 8-K - MOLINA HEALTHCARE, INC. | d287700d8k.htm |
| EX-99.1 - PRESS RELEASE - MOLINA HEALTHCARE, INC. | d287700dex991.htm |
 Investor Day
2012A January 26, 2012
New York, New York
Exhibit 99.2 |
 ©
2012 Molina Healthcare, Inc.
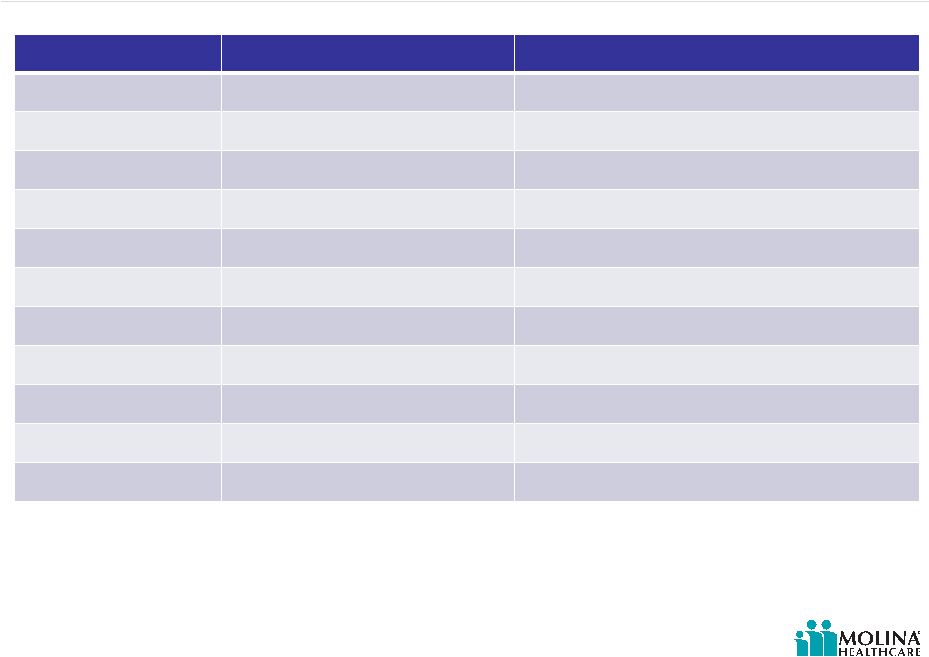
Agenda
Time
Topic
Speaker
12:30pm-12:35pm
Opening Remarks
Juan José
Orellana, VP Investor Relations
12:35pm-1:10pm
Business Overview
J. Mario Molina, MD, Chief Executive Officer
1:10pm-1:30pm
Q&A
1:30pm-1:40pm
Break
1:40pm-2:15pm
Operations Update
Terry Bayer, Chief Operating Officer
2:15pm-2:40pm
Capital Adequacy
Joseph White, Chief Accounting Officer
2:40pm-3:00pm
Q&A
3:00pm-3:15pm
Break
3:15pm-3:50pm
Outlook 2012
John Molina, Chief Financial Officer
3:50pm-4:30pm
Q&A
4:30pm
End of Program
2 |
 ©
2012 Molina Healthcare, Inc.
Cautionary Statement
3
regarding the Company’s expected results for fiscal year 2012. All of our
forward-looking statements are based on our current expectations and assumptions. Actual results could differ
materially due to the unexpected failure of our assumptions or due to adverse developments
related to numerous risk factors, including but not limited to the following: uncertainty regarding the effect of our Washington health plan’s being named an
“apparently successful bidder” by the Health Care Authority of Washington in that state’s
recent managed care procurement;
significant budget pressures on state governments which cause them to lower rates unexpectedly
or to rescind expected rates increases, or their failure to maintain existing benefit
packages or membership eligibility thresholds or criteria; uncertainties regarding the impact of the Patient Protection and Affordable Care Act,
including its possible repeal, judicial overturning of the individual insurance mandate or
Medicaid expansion, the effect of various implementing regulations, and uncertainties
regarding the impact of other federal or state health care and insurance reform
measures;
management of our medical costs, including costs associated with unexpectedly severe or
widespread illnesses such as influenza, and rates of utilization that are consistent
with our expectations;
the success of our efforts to retain existing government contracts and to obtain new
government contracts in connection with state requests for proposals (RFPs) in both
existing and new states, and our ability to grow our revenues consistent with our
expectations; the accurate estimation of incurred but not reported medical costs across our health plans;
risks associated with the continued growth in new Medicaid and Medicare enrollees, and in dual
eligible members; retroactive adjustments to premium revenue or accounting estimates which require adjustment
based upon subsequent developments; the continuation and renewal of the government contracts of both our health plans and Molina
Medicaid Solutions and the terms under which such contracts are renewed; the timing of receipt and recognition of revenue and the amortization of expense under the
state contracts of Molina Medicaid Solutions in Maine and Idaho; government audits and reviews;
changes with respect to our provider contracts and the loss of providers;
the establishment, interpretation, and implementation of a federal or state medical cost
expenditure floor as a percentage of the premiums we receive, administrative cost and
profit ceilings, and profit sharing arrangements; the interpretation and implementation of at-risk premium rules regarding the achievement
of certain quality measures; the successful integration of our acquisitions;
approval by state regulators of dividends and distributions by our health plan subsidiaries;
changes in funding under our contracts as a result of regulatory changes, programmatic
adjustments, or other reforms; high dollar claims related to catastrophic illness;
the favorable resolution of litigation, arbitration, or administrative proceedings, and the
costs associated therewith; restrictions and covenants in our credit facility;
the availability of financing to fund and capitalize our acquisitions and start-up
activities and to meet our liquidity needs and the costs and fees associated therewith; a state’s failure to renew its federal Medicaid waiver;
an inadvertent unauthorized disclosure of protected health information by us or our business
associates; changes generally affecting the managed care or Medicaid management information systems
industries; increases in government surcharges, taxes, and assessments;
changes in general economic conditions, including unemployment rates;
and numerous other risk factors, including those identified within this slide presentation
and/or our accompanying oral remarks, and those discussed in our periodic reports and filings
with the Securities and Exchange Commission. These reports can be accessed under the investor
relations tab of our Company website or on the SEC’s website at www.sec.gov. Given
these risks and uncertainties, we can give no assurances that our forward-looking
statements will prove to be accurate, or that any other results or events projected or contemplated by
our forward-looking statements will in fact occur, and we caution investors not to place
undue reliance on these statements. All forward-looking statements in this release represent our
judgment as of January 26, 2012, and we disclaim any obligation to update any
forward-looking statements to conform the statement to actual results or changes in our expectations.
Safe Harbor Statement under the Private Securities Litigation Reform Act of 1995:
This slide presentation and our accompanying oral remarks contain “forward-looking
statements” |
 Business
Overview J. Mario Molina, MD
President & Chief Executive Officer
January 26, 2012
New York, New York |
 ©
2012 Molina Healthcare, Inc.
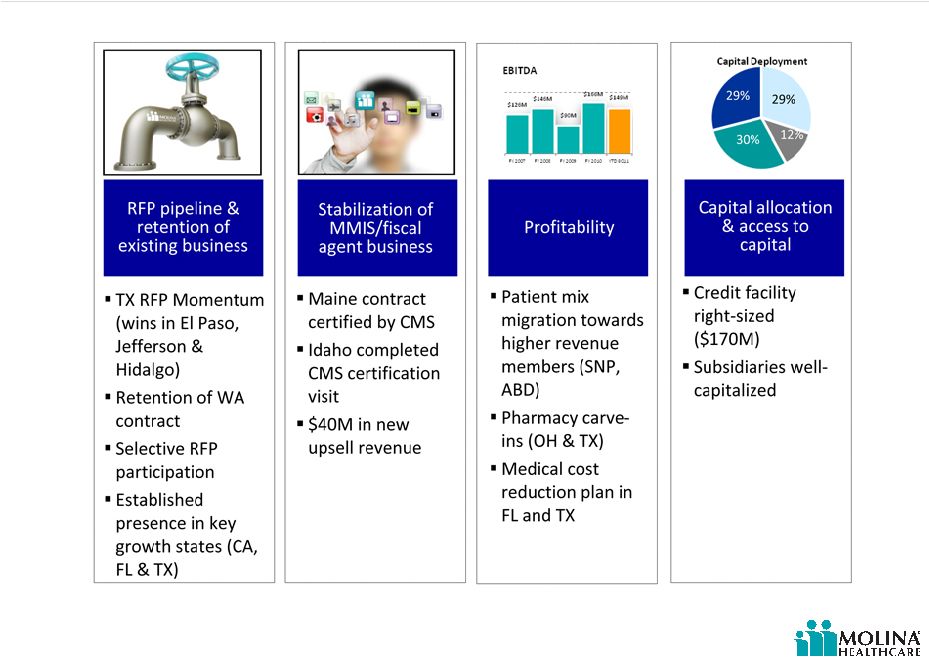
Goal setting and results
Executed on our plans for 2011
Health plan business remains stable
Medicare SNP business continues to grow
Improved profitability despite rate environment
First CMS certification achieved for fiscal agent
contract
Positioned for strong growth in 2012
New markets in Texas effective 3/12
Dual eligible care coordination integration
5
Solid progress on long-term value creation |
 ©
2012 Molina Healthcare, Inc.
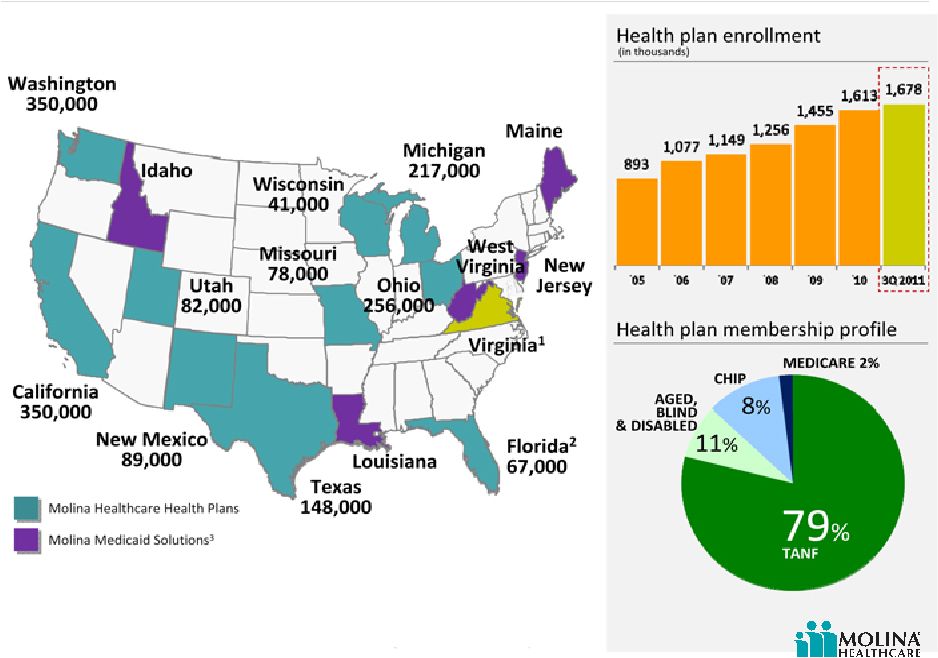
Business snapshot
Markets and members served –
3Q 2011
1.
Virginia clinics provide Direct Delivery.
2.
Florida has a managed care program as well as a Pharmacy Rebate Program.
3.
Fee based fiscal agent business.
6 |
 ©
2012 Molina Healthcare, Inc.
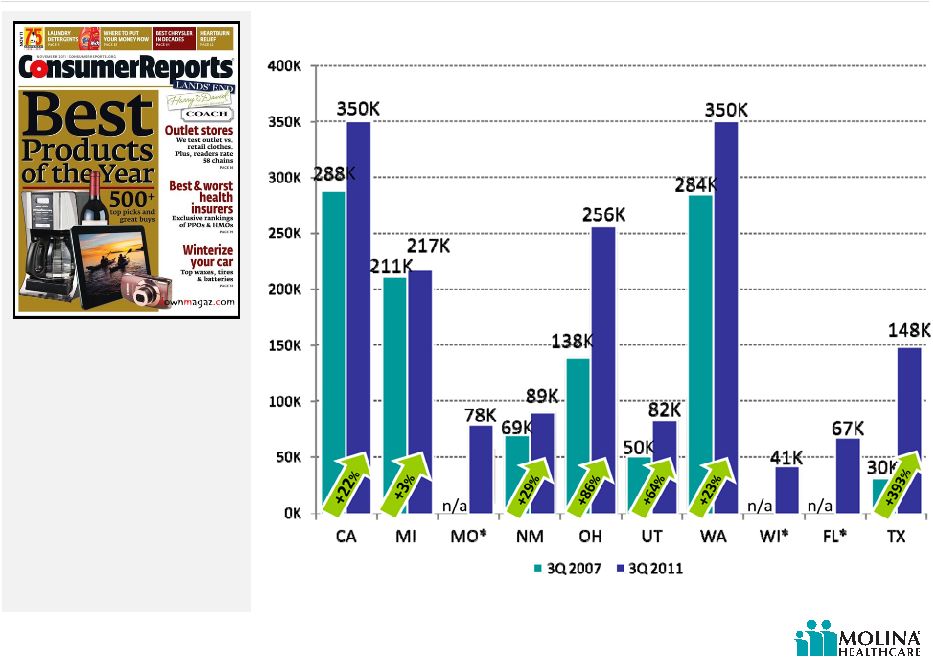
7
Delivering enrollment growth by market
As our enrollment grows,
Molina remains committed to
delivering quality health care.
Except for Wisconsin, all of
our eligible health plans have
earned NCQA accreditation.
Enrollment
(3Q 2007 –
3Q 2011)
Molina health plans ranked in Consumer Reports Magazine,
November 2011.
*Molina did not have a presence in these markets in 2007. |
 ©
2012 Molina Healthcare, Inc.
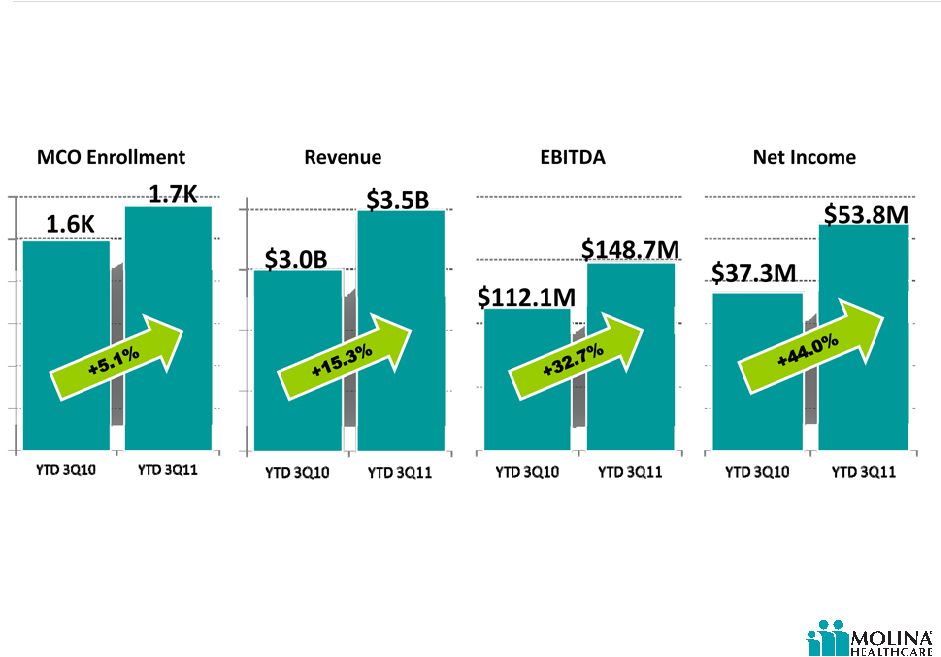
Executing on our plan
8
YTD 3Q 2010 vs. YTD 3Q 2011 |
 ©
2012 Molina Healthcare, Inc.
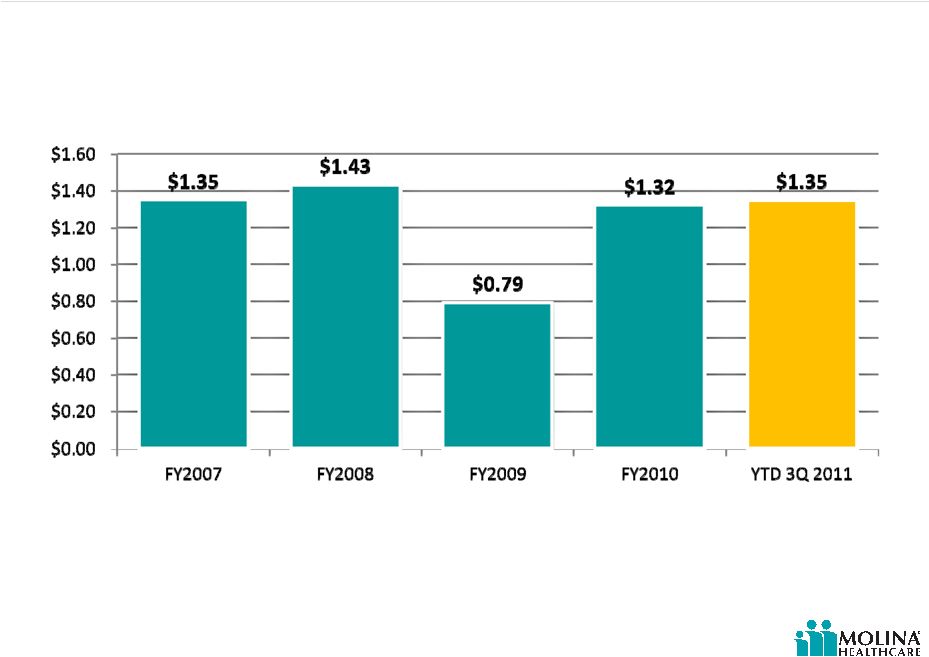
Molina earnings per share
9
Split adjusted |
 ©
2012 Molina Healthcare, Inc.
Positioned for growth
Building on momentum from new business wins and
retention of existing contracts
Leveraging established SNP (duals) growth platform
Investing in Company-owned direct delivery footprint
Continue developing and up-selling our fiscal agent
offering
Investing in corporate infrastructure (Molina Center)
10 |
 ©
2012 Molina Healthcare, Inc.
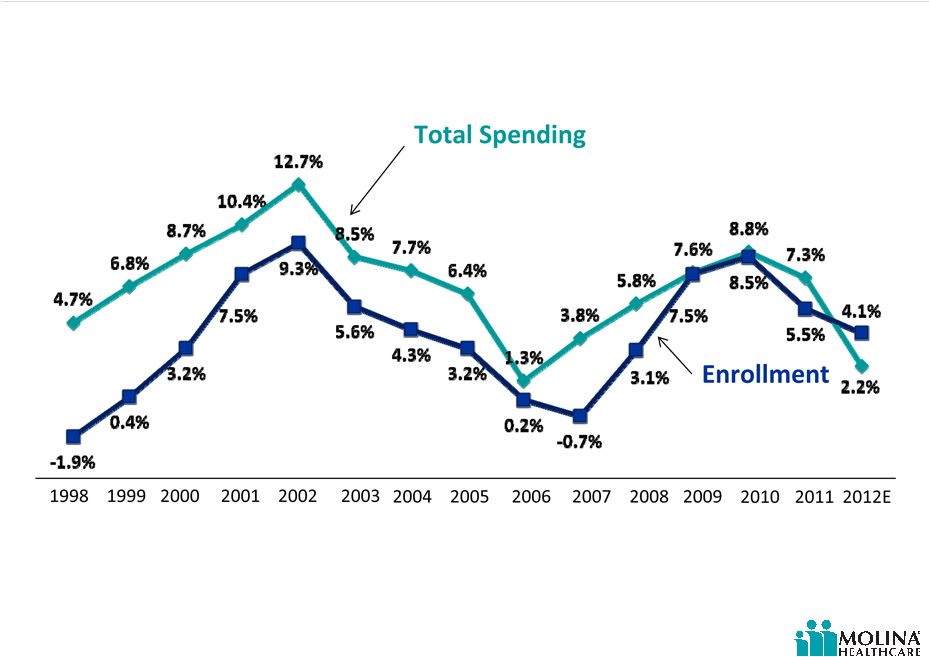
U.S. Medicaid Spending and Enrollment
Percent Changes, FY 1998 –
FY 2012E
Source:
Medicaid
Enrollment
June
2010
Data
Snapshot,
KCMU,
February
2011.
Spending
Data
from
KCMU
Analysis
of
CMS
Form
64
Data
for
Historic
Medicaid
Growth
Rates.
FY
2011
and
FY
2012
data
based
on
KCMU
survey
of
Medicaid
officials
in
50
states
and
DC
conducted
by
Health
Management
Associates,
September
2011.
Note:
Enrollment
percentage
changes
from
June
to
June
of
each
year.
Spending
growth
percentages
in
state
fiscal
year.
U.S. Medicaid spending and enrollment
11 |
 ©
2012 Molina Healthcare, Inc.
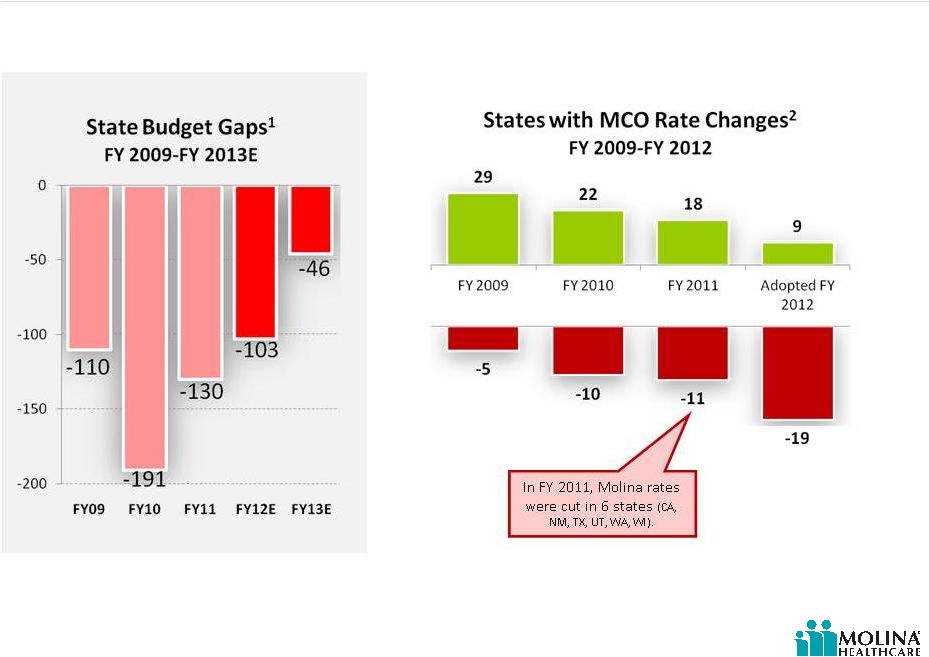
Key challenges for 2012
12
Sources:
1.
“States
Continue
to
Feel
Recession’s
Impact.”
Center
on
Budget
and
Policy
Priorities,
June
17,
2011.
2.
KMCU
survey
of
Medicaid
officials
in
50
states
and
DC
conducted
by
Health
Management
Associates,
September
2009,
September
2010,
and
September
2011.
Although some states project improved cash flows over the next few years as the economy
recovers, states’
fiscal conditions remain very weak. |
 ©
2012 Molina Healthcare, Inc.
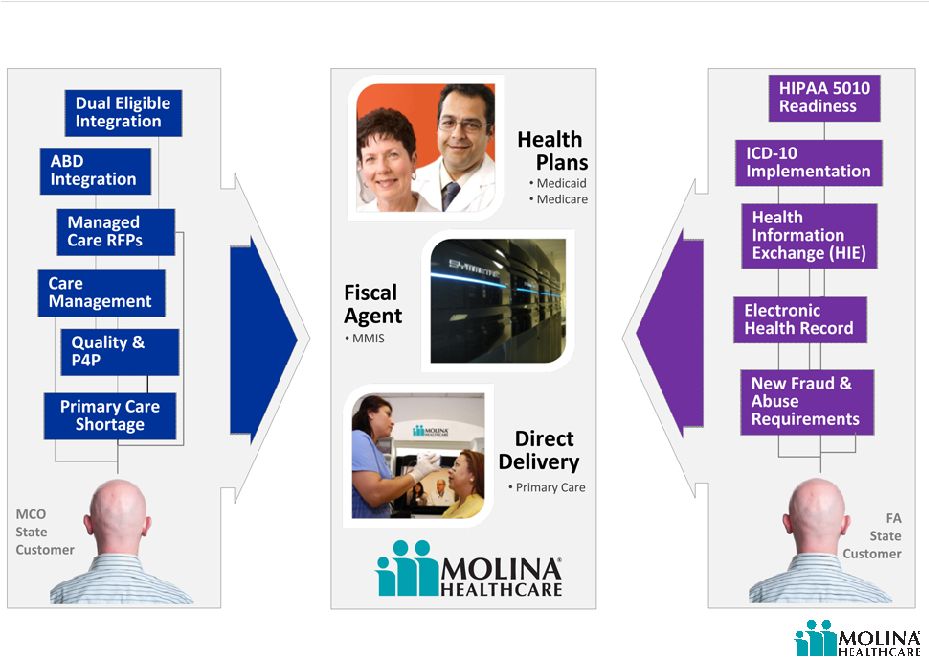
Short term growth opportunities
13
Economic, healthcare, and technology trends will translate into revenue opportunities in the
short run. |
 ©
2012 Molina Healthcare, Inc.
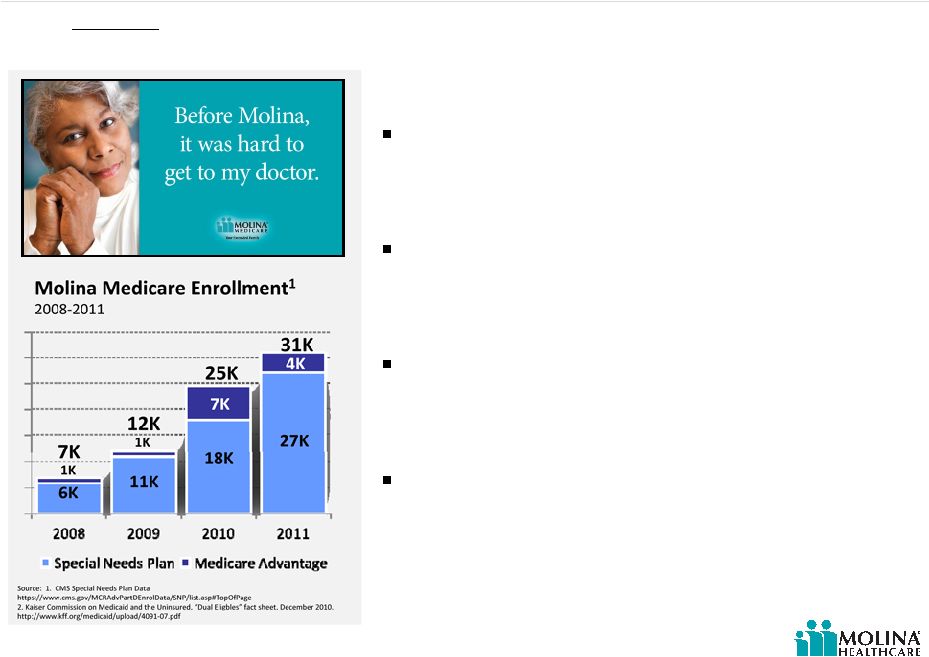
Unprecedented new focus on dual eligibles
Recognition that dual eligibles are the most
costly group of beneficiaries for both
Medicaid and Medicare
Dual eligibles account for approximately 15%
of Medicaid enrollees but contribute to 39%
of all Medicaid spending²
Medicaid/Medicare spending averages $20K
per dual per year, 5X greater than other
Medicare beneficiaries
Dual eligible population will highly benefit
from managed care
Nearly 9 million
Medicaid beneficiaries are dual eligibles: low-income seniors and younger
persons with disabilities who are enrolled in both the Medicare and Medicaid programs.
14 |
 ©
2012 Molina Healthcare, Inc.
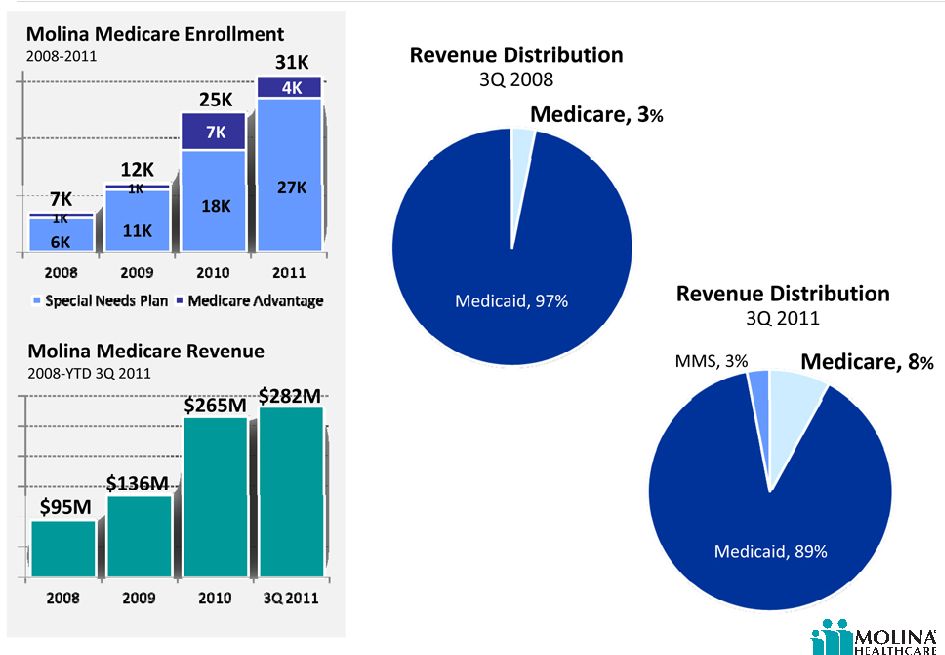
Our Medicare business is growing
15
Source: Company Data and CMS Special Needs Plan Data
https://www.cms.gov/MCRAdvPartDEnrolData/SNP/list.asp#TopOfPage |
 ©
2012 Molina Healthcare, Inc.
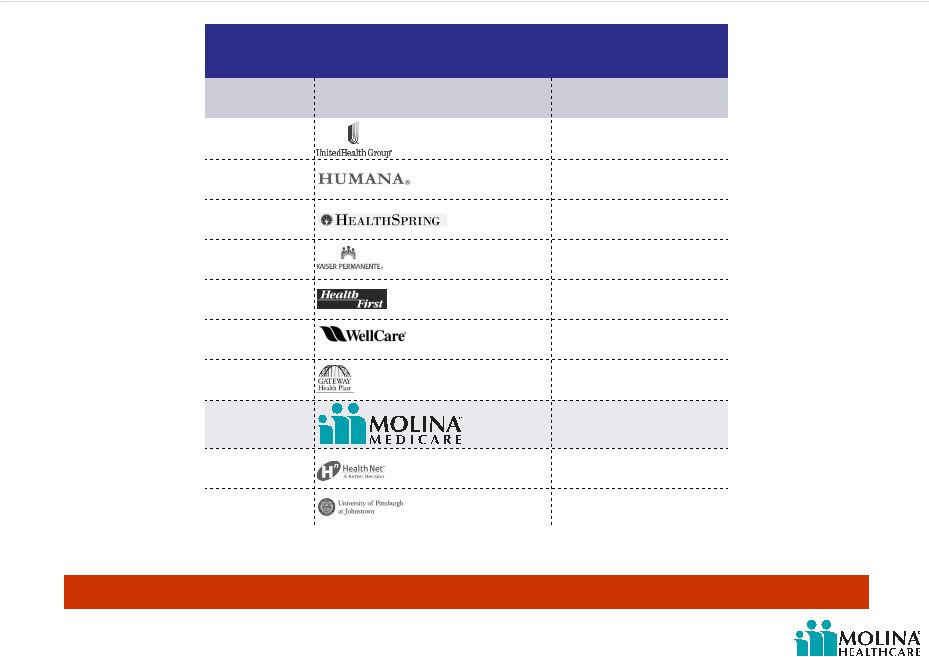
Molina’s dual eligible enrollment
16
Source: CMS Health Plan Management System as of 12/2011. Information sourced
quarterly. Top 10 SNP Dual Eligible Plans Nationwide*
Rank
Plan
Membership
1
203k
2
75k
3
75k
4
68k
5
53k
6
42k
7
28k
8
27k
9
18k
10
16k
Molina has well established SNPs serving the financially vulnerable
1.
United includes PacifiCare, Evercare, APIPA and Secure Horizons products
2.
Humana includes Arcadian, Care Plus, Arta, and MD Care.
1
2 |
 ©
2012 Molina Healthcare, Inc.
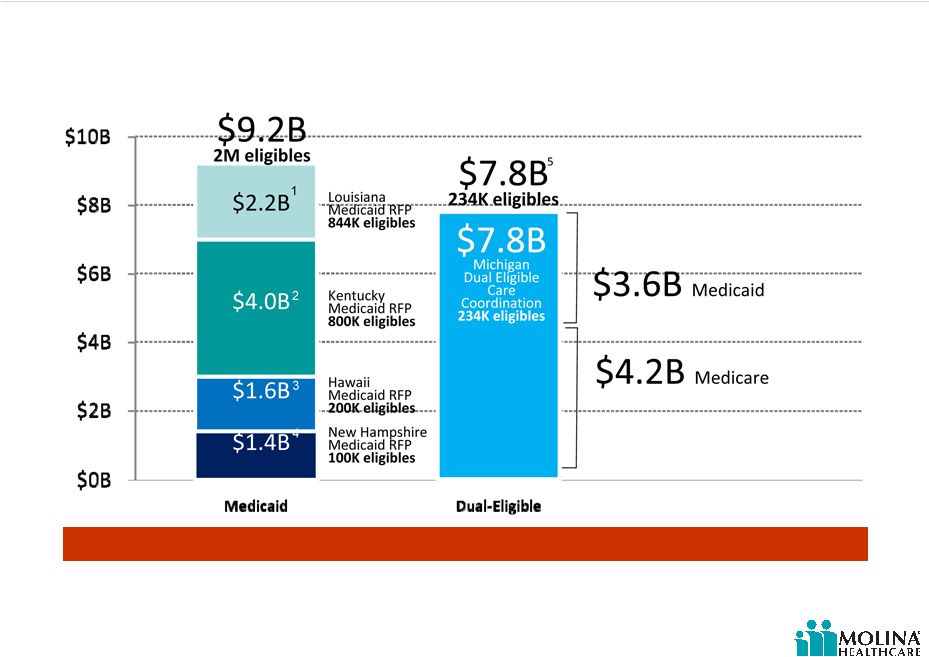
Opportunities in perspective
17
1.
The
Advocate,
“Contract
Winners
want
to
protect
data.”
August
2,
2011
2.
Insider
Louisville,
Multiple
mega
firms
pursue
Kentucky’s
$4
billion
Medicaid
contract
.”
June
23,
2011
3.
Pacific
Business
News,
$1.65B
in
Medicaid
contracts
will
expire
in
June.”
May
6,
2011.
(http://www.bizjournals.com/pacific/print-edition/2011/05/06/165-billion-in-medicaid-contracts.html)
4.
Union
Leader,
“State
reviewing
proposals
for
massive
Medicaid
contract.”
January
2,
2012.
(http://www.unionleader.com/article/20120102/NEWS06/701029974)
5.
CMS
document,
“Michigan’s
Response
to
CMS
Solicitation
State
Demonstrations
to
Integrate
Care
for
Dual
Eligible
Individuals
”
Michigan is among the 15 states selected to
receive up to $1 million to support the design
of programs
to integrate care for the dual eligible.
Select Expansion Opportunities
Molina already serves nearly 7,000 SNP beneficiaries in Michigan |
 ©
2012 Molina Healthcare, Inc.
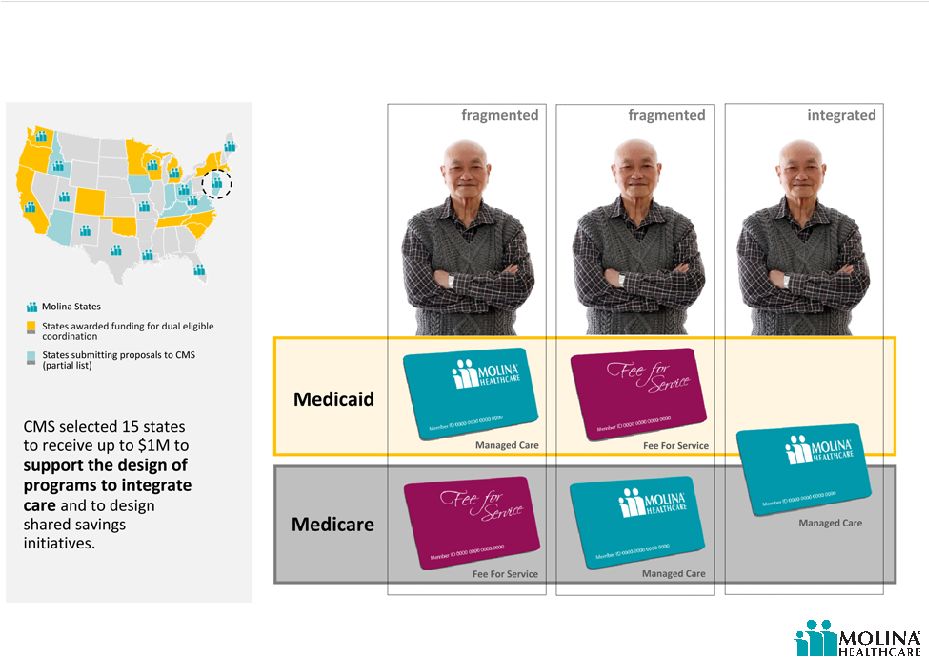
Supporting integrated care for duals
18
Medicare and Medicaid are each governed by their own policies and procedures, Dual
eligibles are forced to navigate a system with two sets of providers, benefits, and even
enrollment cards. This fragmentation can result in unnecessary,
duplicative, or missed
services. |
 ©
2012 Molina Healthcare, Inc.
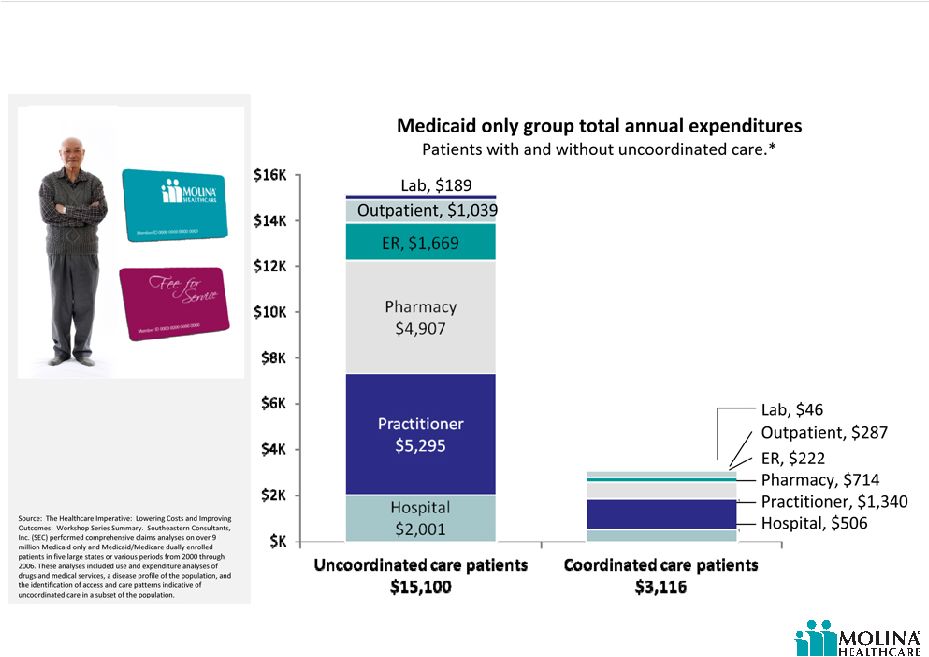
Cost of uncoordinated care
19
Medicaid patients with extremely uncoordinated care account for a disproportionate share
of costs.
These patterns are even more significant among dual patients who experience a
greater prevalence of chronic diseases and co-morbid conditions.
|
 ©
2012 Molina Healthcare, Inc.
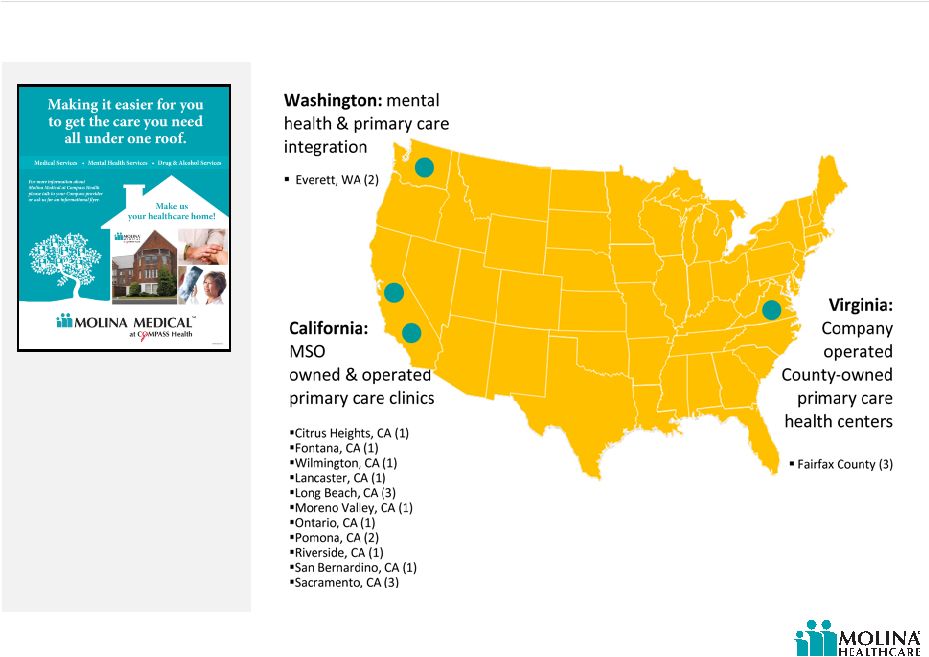
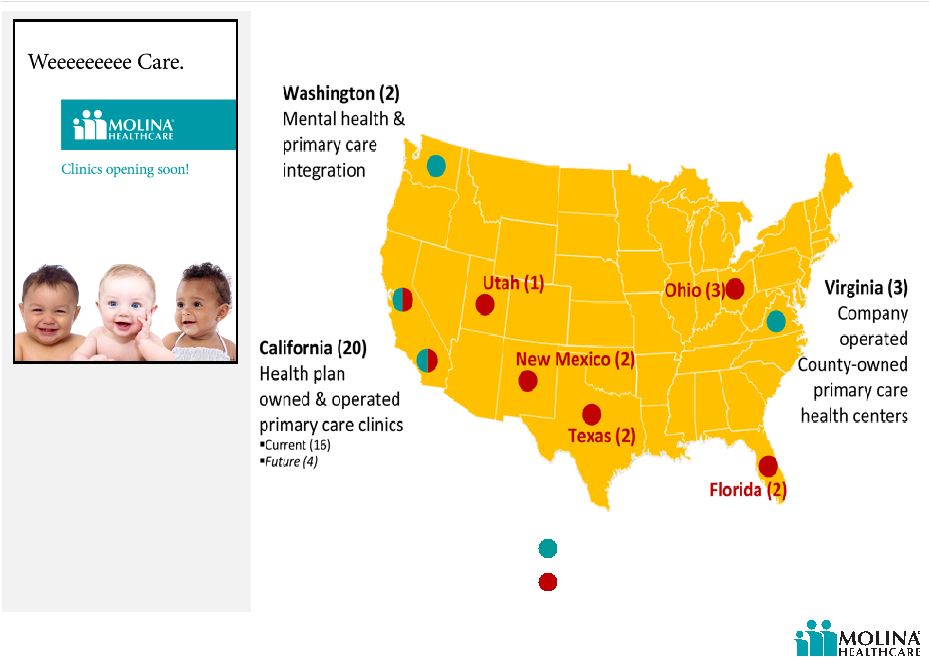
Our approach to direct delivery is flexible and can accommodate changes in local market
requirements and needs. We currently operate 21 clinics and plan
to continue expanding.
Direct Delivery
20 |
 ©
2012 Molina Healthcare, Inc.
Why build clinics at all?
21
Augment network in areas of provider scarcity
Supplement provider capacity issues
Greater emphasis on quality and outcomes
States continue to cut rates
Nurtures patient loyalty to the health plan
Brand awareness & community engagement |
 ©
2012 Molina Healthcare, Inc.
Why not build more clinics?
22
Need to augment the network not replace the network
Can be perceived as competing directly with network
providers
Identifying right locations can be a challenge
Hiring doctors to serve Medicaid patients is not easy
Get it right from the beginning |
 ©
2012 Molina Healthcare, Inc.
Direct Delivery: expanding our footprint
23
Current Molina clinics
Future Molina clinics
15 new clinics planned for 2012 |
 ©
2012 Molina Healthcare, Inc.
24
Direct Delivery –
Rx solutions
A 2007 U.S. survey reported that nearly 31% of those polled had not filled a prescription they
were given by their physician.¹
1. Source: Enhancing Prescription Medicine Adherence: A National
Action Plan, National Council on Patient Information and Education
August 2007
Molina now offers patients on-site medication
dispensing to increase the likelihood that patients
will fill their prescription and undergo the
physician’s medical treatment plan.
Value added benefit for Molina members
Acute care scripts only
Wait time: 10 -15 min
Direct member customer service line
Over 50,000 scripts already dispensed |
 ©
2012 Molina Healthcare, Inc.
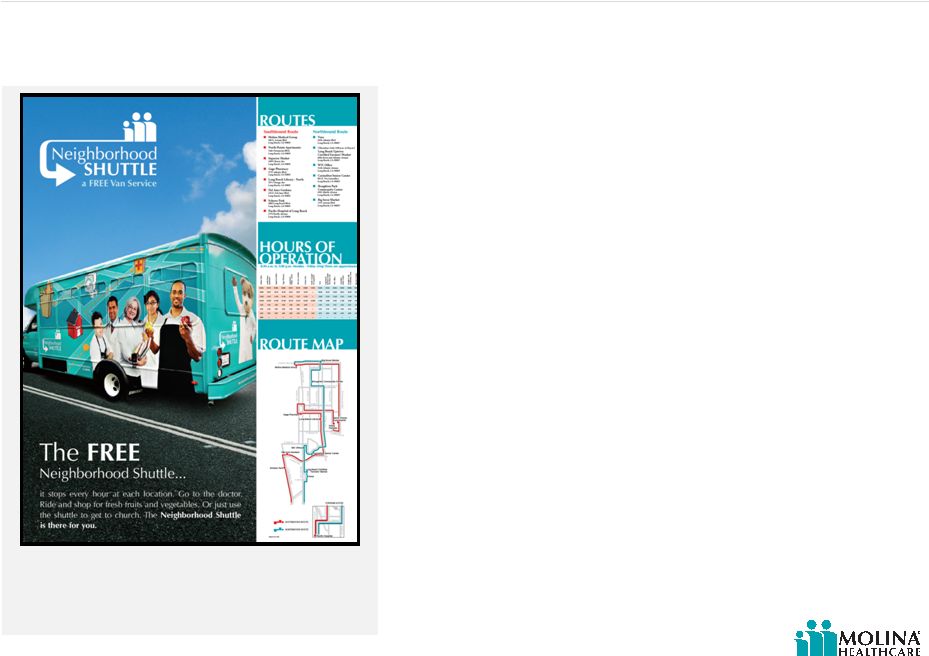
Direct Delivery –
transportation solution
25
Transportation solution
Free shuttle service offers a ride between
various key community access points,
including our clinics. (Long Beach, Inland
Empire.)
Transportation to and from a physician’s office remains a key problem for Medicaid
beneficiaries. The use of public transportation often results in missed appointments or
late arrivals. |
 ©
2012 Molina Healthcare, Inc.
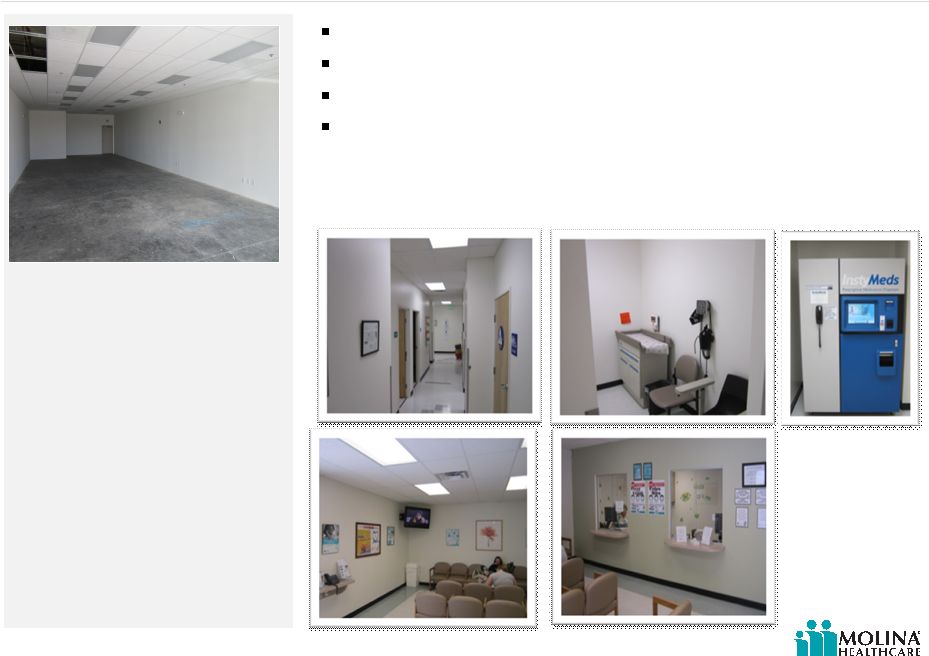
Direct Delivery –
our facilities
26
Typically leased facilities about 4,000 sq/ft
4-5 employees
1-2 Primary Care Physicians per office
Contracted: Lab, X-Ray, and Specialty services
pre build-out
after build-out |
 ©
2012 Molina Healthcare, Inc.
27
Preparation for anticipated growth
Rent vs. own decision (MOH already occupied 40%
of complex)
Advantageous real estate market conditions
Molina acquires office complex in Long Beach, California.
Purchase price of $81 million
Two connected 14-story
towers
461,263 square feet
Class A building |
 ©
2012 Molina Healthcare, Inc.
Summary of investor areas of interest
28 |
 ©
2012 Molina Healthcare, Inc.
29
Q&A |
 Operations
Update Terry Bayer
Chief Operating Officer
January 26, 2012
New York, New York |
  ©
2012 Molina Healthcare, Inc.
Operations update
Highlights from our health plans
Florida
Texas
Ohio
Washington
Dual eligible opportunity
Michigan duals
California budget
Carve-in trends
MMS certification
31 |
 ©
2012 Molina Healthcare, Inc.
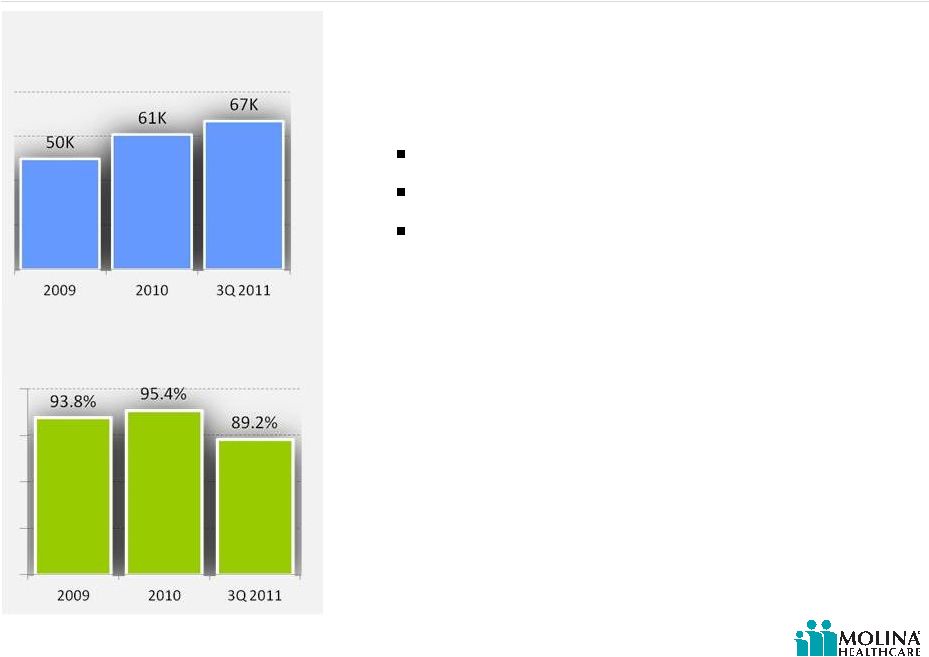
Florida
Improved financial performance due to:
Reduced unit costs
Utilization improvement
Premium rate increase effective 9/1/11
32
Molina Healthcare of Florida
Historical and YTD Enrollment
2009-3Q2011
Molina Healthcare of Florida
Historical and YTD MCR
2009-3Q2011 |
 ©
2012 Molina Healthcare, Inc.
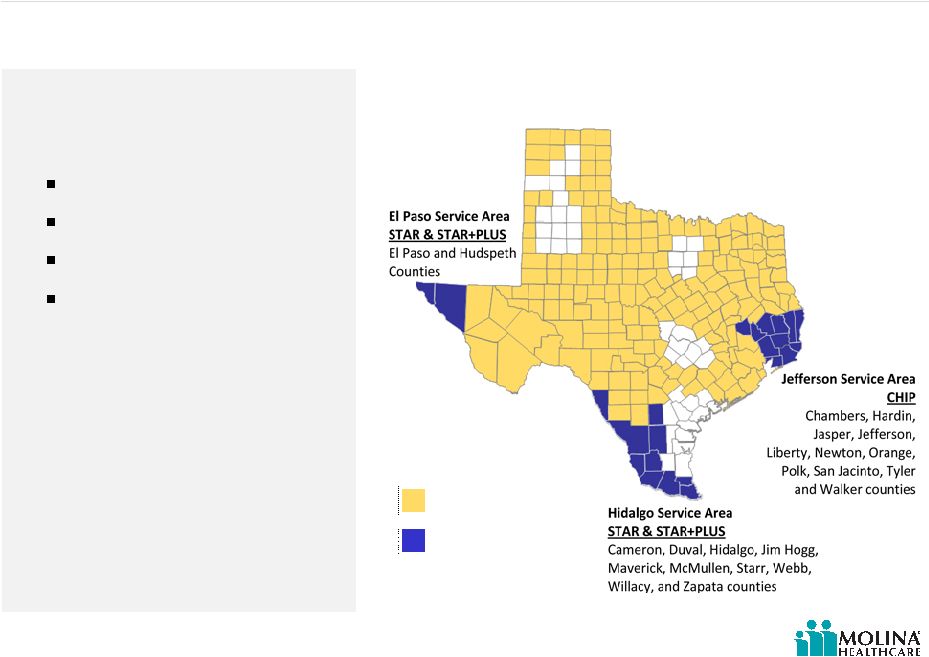
Texas overview
Existing Molina
footprint
33
Molina new SDAs effective
3/1/2012
In addition to Molina’s already expansive footprint in Texas, effective March 1, 2012,
Molina
will have three new service delivery areas (SDAs).
Source: Texas Health and Human Services Commission
Molina New SDAs
(effective 3/1/2012)
Profitability Improvement
Plan:
Rate Increases
Care Coordination
Utilization Management
Unit Costs-recontracting |
  ©
2012 Molina Healthcare, Inc.
Ohio
34
Improved financial performance due to:
Premium rate increase (effective 1/1/11)
Utilization management
Care coordination
Reducing unit costs by improving contracts
RFA issued January 11, 2011:
Re-procurement statewide
Addition of disabled children |
 ©
2012 Molina Healthcare, Inc.
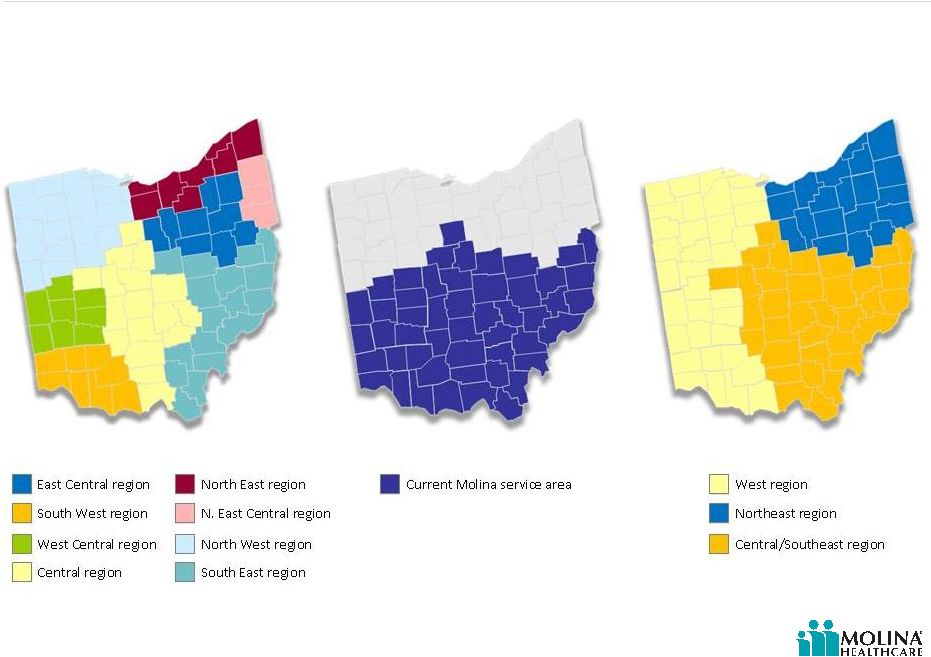
Ohio RFA
$5.1 billion rebid
Implementation expected January 1, 2013
1.5M covered families and children (CFC) lives, 125K ABD lives, and 37K
children with disabilities
Mandates ABDs, including children, into managed care
Beneficiaries currently enrolled in the covered families and children (CFC)
program will continue to be mandatorily enrolled
Divides state into three regions each with four managed care plans
Three
regions
each
with
a
unique
health
plan,
therefore
allowing
three
distinct MCOs to operate statewide.
Bids are due March 19, 2012
Not a rate bid (compliance, HEDIS, experience 60% of bid)
35
On January 11
th
, the Ohio Department of Job and Family Services issued a Request for
applications under which it will rebid the current managed care population and expand
managed care to the aged, blind, or disabled (ABD) population. |
 ©
2012 Molina Healthcare, Inc.
Post-2012 RFA
Ohio Managed Care Regions
(3 regions)
Pre-2012 RFA
Ohio Managed Care Regions
(8 regions)
Ohio RFA
Source: Ohio Department of Job and Family Services
(http://jfs.ohio.gov/rfp/JFSR1213078019/JFSR1213078019.stm)
36
Pre-2012 RFA
Current Molina Service Area
(4 regions) |
  ©
2012 Molina Healthcare, Inc.
Washington
37
RFP results announced January 17, 2012
Qualified as one of five “apparently successful”
bidders
New population:
100,000 SSI members included in Healthy
Options program effective 7/1/12.
MCO’s exiting program 7/1/12 (123,000
members)
Columbia United Providers (CUP)
Group Health
Regence
Kaiser |
 ©
2012 Molina Healthcare, Inc.
Michigan duals
38
State began enrolling dual eligibles in Medicaid
(12/11)
Dual eligibles in SNP automatically enrolled with opt-
out
Michigan Department of Community Health (MDCH)
developing Dual Eligible Integrated Care Plan
CMS submission target (4/1)
Implementation target (1/2013) |
 ©
2012 Molina Healthcare, Inc.
California Budget
Proposed changes to Medi-Cal (Medicaid)
Phased-in transfer of duals to managed care starting in January 2013. Medi-Cal
benefits transition in first year; Medicare benefits over three years. (approx.
$670M projected savings in SFY 2013)
Statewide expansion of Medi-Cal managed care starting in June 2012;
fee-for-service transition to managed care in 2014-15.
Annual open enrollment and lock-in period for Medi-Cal managed care.
Extension of gross premiums tax on Medi-Cal managed care plans and hospital fee on
hospitals. 3.61% proposed rate increase in Medi-Cal rates.
Proposed changes to Healthy Families (CHIP)
Aggregate 25.7% managed care plan rate cut effective Oct. 1, 2012. Because of varying
contract rates, the effective rate change for health plans may be significantly
different. Transfer of all Healthy Families members (approx. 875,000) to Medi-Cal
over a 9 month period beginning in Oct. 2012.
Elimination of the Managed Risk Medical Insurance Board (MRMIB) by July 2013.
Final budget terms may vary materially.
39
On January 5
th
, Governor Brown released initial California budget proposal. |
 ©
2012 Molina Healthcare, Inc.
Carve-in trends
Ohio Rx: 10/11
Texas Rx: 3/12
Texas inpatient: 3/12
40 |
 ©
2012 Molina Healthcare, Inc.
Maine MMIS certification
Certification allows state to receive maximum federal
funding for Maine Integrated Health Management
Solution (MIHMS) by meeting federal standards for claims
management system.
State of Maine can claim 75% federal reimbursement for
ongoing operations retroactive to September 1, 2010.
MIHMS was designed and implemented by Molina
Healthcare’s wholly owned subsidiary, Molina Medicaid
Solutions.
41
Centers for Medicare and Medicaid Services (CMS) awarded Molina Medicaid Solutions full
federal certification in Maine in December 2011.
Since September 1, 2010, the Maine
Integrated Health Management
Solution (MIHMS) system has been
processing approximately 1 million
claims per month and paying nearly
3,000 providers each week. |
 ©
2012 Molina Healthcare, Inc.
Molina Medicaid Solutions upsells
Item
Narrative
When Sold (Qtr/Yr)
Provider Incentive Payments
Incentive payments made to the
medical community
3Q 2011
Provider Enrollment Application
Enhancement of provider portal
application
3Q 2011
5010
HIPAA standards for installation
of 5010
3Q 2011
42
Item
Narrative
When Sold (Qtr/Yr)
InterQual
Application of InterQual criteria
to state operated facilities
1Q 2011
5010/ ICD-10
10th Revision of the International
Code of Diagnoses Compliance
Project
1Q 2011/3Q 2011
West Virginia
Louisiana
Our fiscal agent business has pursued various new revenue opportunities (upgrades, add-
ons, new services and products), producing $40M in additional sales in 2011.*
*This revenue will be recognized through 2014.
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
43
Q&A |
 ©
2012 Molina Healthcare, Inc.
Capital Adequacy
Joseph White
Chief Accounting Officer
January 26, 2012
New York, New York |
 ©
2012 Molina Healthcare, Inc.
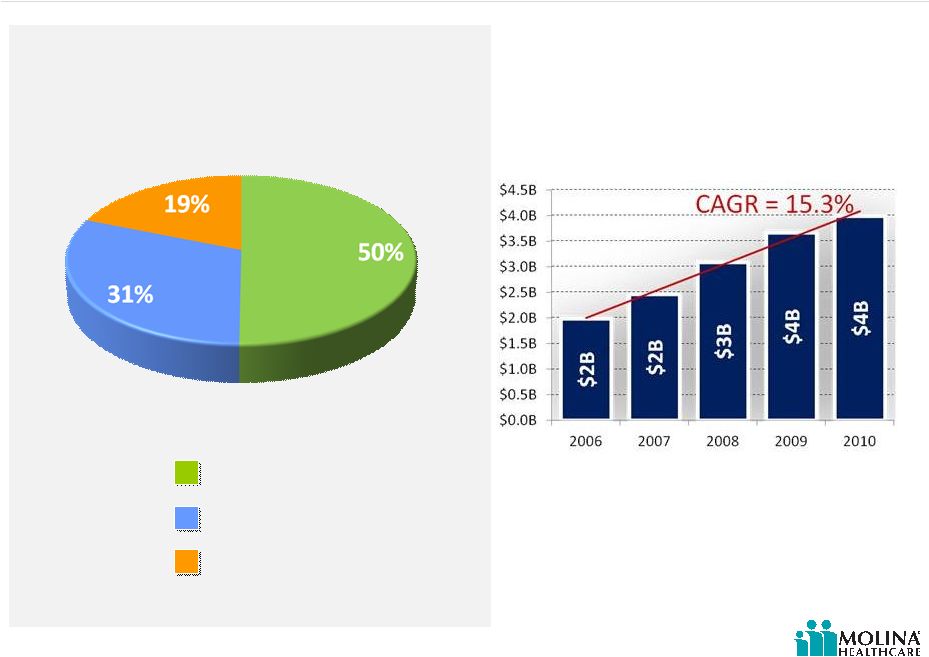
Molina earnings have funded past growth
45
Sources of Capital
2006 through 3Q2011
Common Equity
Convertible Debt
Net Income
Total Revenue
2006-2010
Source(s): SEC Filings
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
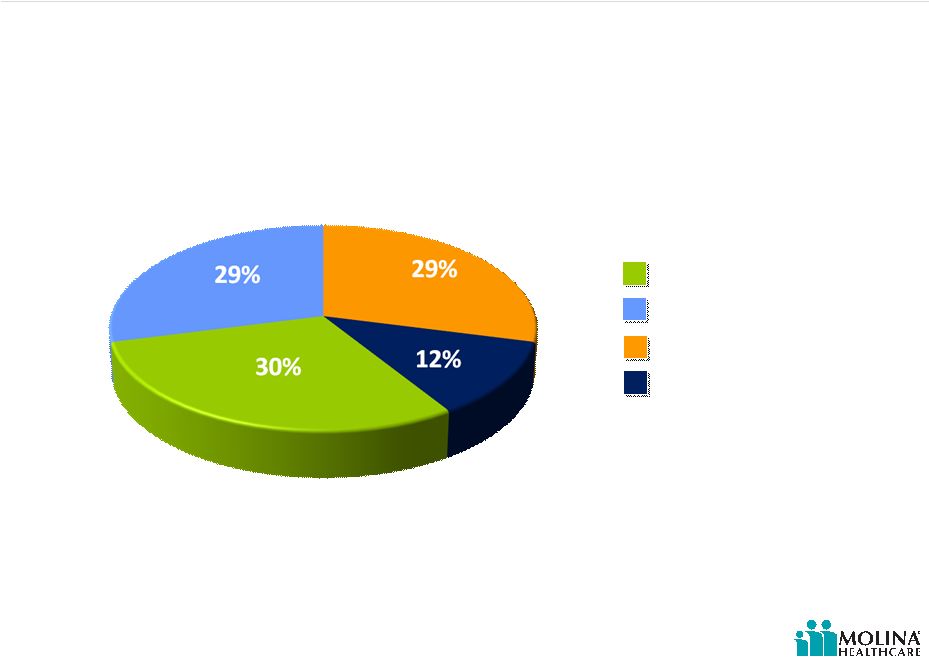
Molina has invested to grow its business
46
Capital Deployment
2006 through 3Q2011
Cash Paid for Acquisitions
Contributions to Subsidiaries
Capital Expenditures
Share Repurchases
Source(s): SEC Filings and Company Data
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
47
1997
Entered Michigan
by
acquiring Minority
Interest
1999
Acquired
controlling interest
in Michigan
Plan
2004
Entered New
Mexico by
acquiring
Health
Care Horizons the
parent company of
Cimarron Health
Plan
2004
Acquired the rights
to serve Wellness
Plan
members in
Michigan
2000
Entered
Washington
by
acquiring
Qualmed
Washington
Health Plan
2004
Acquired
members in
Washington
from Premera
Blue Cross
2005
Entered San
Diego County,
CA by acquiring
Sharp &
Universal Plan
members
2006
Acquired HCLB the
parent company
of CAPE
Health
Plan in Michigan
2007
Entered
Missouri by
acquiring
Mercy
CarePlus
2008
Entered Florida
by acquiring
Florida
NetPASS
2010
Acquired
the Health
Information
Management business
from Unisys, now
Molina Medicaid
Solutions
2010
Acquired Abri
Health Plan in
Wisconsin
2011
Acquired the
Arco Towers
in Long Beach,
CA
Capital deployment: acquisitions
Our deployment of capital has included strategic acquisitions that enable the company to
increase its market penetration in existing markets, or enter new markets and new
programs. (risk and fee based)
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
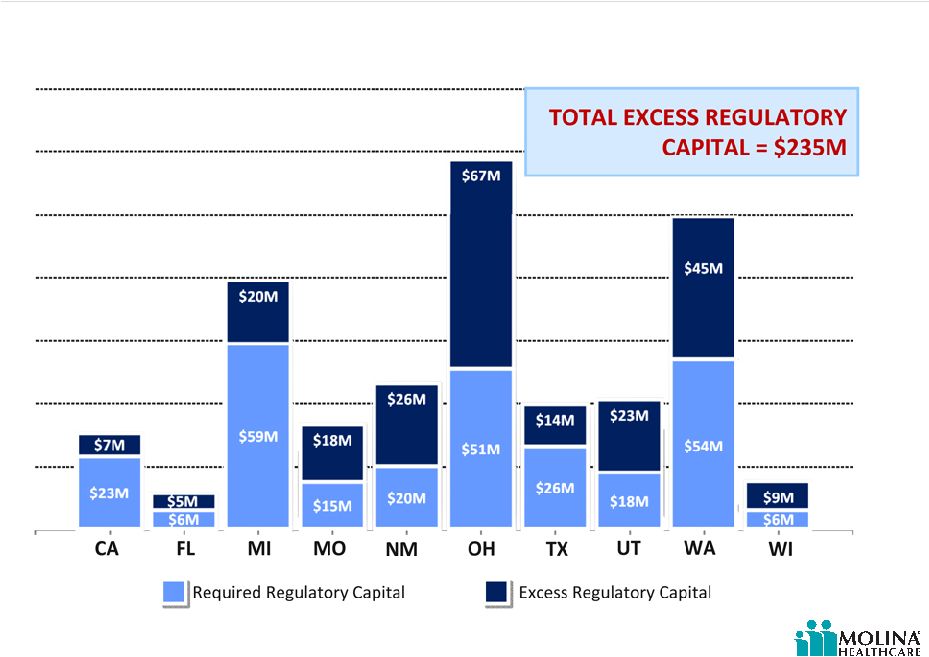
Molina health plans are well capitalized
48
*E denotes estimate.
Source(s): Company Estimates
Regulatory Capital
2011E*
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
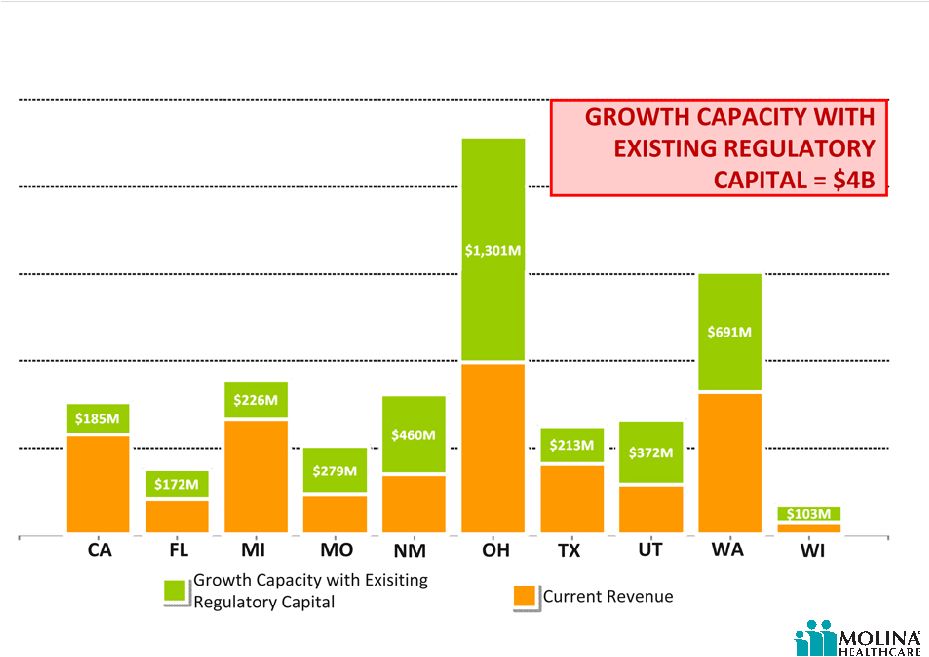
Molina health plans have capital to support growth
49
Health Plan Growth Potential without New Capital
2011E*
*E denots estimate.
Source(s): Company Estimates
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
Start-up operations need capital
Regulatory capital
Systems development and configuration
Start up costs/initial operating losses
Direct Delivery set up
Molina Medicaid Solutions development costs
50
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
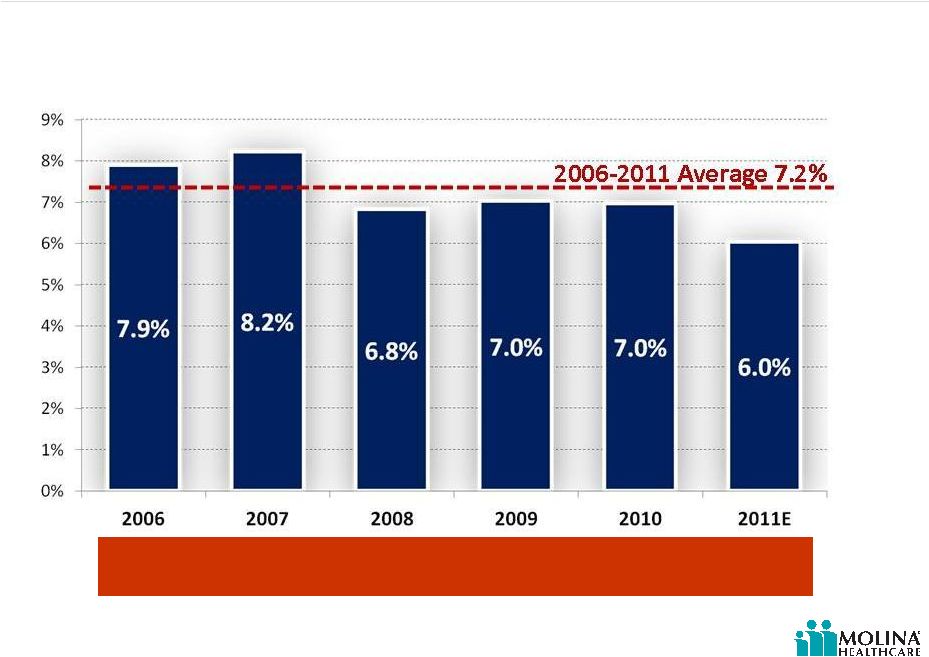
Required regulatory capital as % of revenue
51
Required Equity as % of Premium Revenue
2006-2011E*
On average our health plans need regulatory capital of approximately
7% of premium revenue.
*E denotes estimate.
Source(s): Company Data
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
Startup costs and initial operating losses
52
Molina Healthcare of Ohio
Operating Income or (Loss)
2005-3Q 2011 YTD
Source(s): NAIC Statutory Filings
“It takes time and
money to build a
profitable health plan.”
Joseph White
May 29, 2008
Molina Healthcare
Investor Day, NY
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
Other costs to start a health plan
53
Systems Development and Configuration
Approximately $2M for HMO system development and configuration
Direct Delivery set-up
On average build out cost for a typical clinic is $750K
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
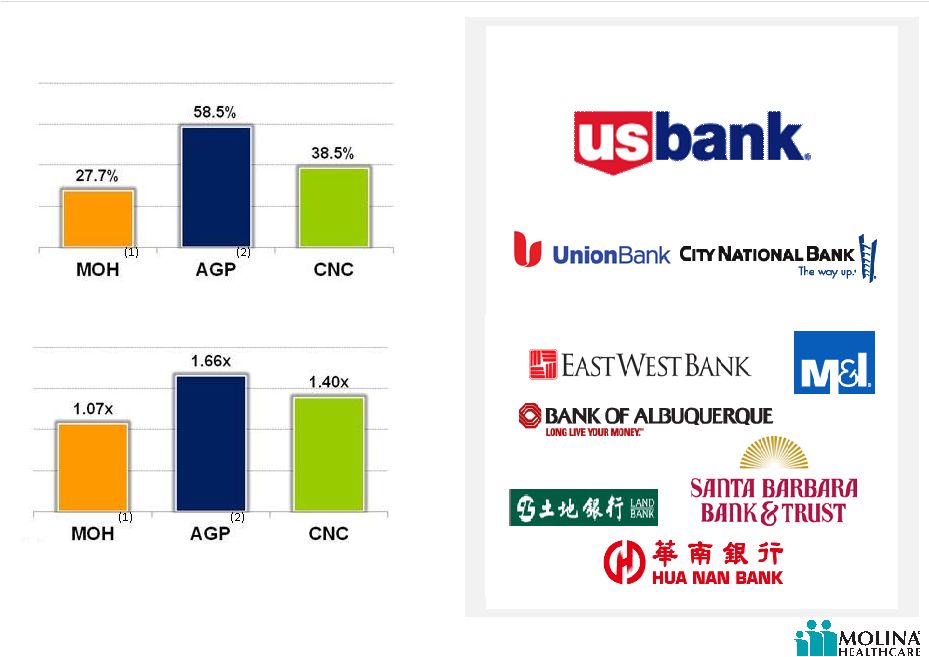
Pure Play LT Debt to Equity Ratio
Last Twelve Months as of Sept. 30, 2011
(1),(2)
Note:
(1)
MOH
Long
Term
Debt
includes
$48.6M
term
loan
issued
December
7,
2011
to
finance
the
Molina
Center
acquisition.
(2)
AGP
Long
Term
Debt
includes
$400M
Senior
Notes
issued
November
16,
2011
and
$75M
Senior
Notes
issued
January
18,
2012.
Molina $170M Credit Agreement
Pure Play Long Term Debt / EBITDA
Last Twelve Months as of Sept. 30, 2011
(1),(2)
Source(s): SEC Filings
54
Access to additional capital
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
Q&A
55 |
 Financial
Outlook 2012 John Molina
Chief Financial Officer
January 26, 2012
New York, New York |
 ©
2012 Molina Healthcare, Inc.
Cautionary Statement
57
regarding the Company’s expected results for fiscal year 2012. All of our
forward-looking statements are based on our current expectations and assumptions. Actual results could differ
materially due to the unexpected failure of our assumptions or due to adverse developments
related to numerous risk factors, including but not limited to the following: uncertainty regarding the effect of our Washington health plan’s being named an
“apparently successful bidder” by the Health Care Authority of Washington in that state’s
recent managed care procurement;
significant budget pressures on state governments which cause them to lower rates unexpectedly
or to rescind expected rates increases, or their failure to maintain existing benefit
packages or membership eligibility thresholds or criteria; uncertainties regarding the impact of the Patient Protection and Affordable Care Act,
including its possible repeal, judicial overturning of the individual insurance mandate or
Medicaid expansion, the effect of various implementing regulations, and uncertainties
regarding the impact of other federal or state health care and insurance reform
measures;
management of our medical costs, including costs associated with unexpectedly severe or
widespread illnesses such as influenza, and rates of utilization that are consistent
with our expectations;
the success of our efforts to retain existing government contracts and to obtain new
government contracts in connection with state requests for proposals (RFPs) in both
existing and new states, and our ability to grow our revenues consistent with our
expectations; the accurate estimation of incurred but not reported medical costs across our health plans;
risks associated with the continued growth in new Medicaid and Medicare enrollees, and in dual
eligible members; retroactive adjustments to premium revenue or accounting estimates which require adjustment
based upon subsequent developments; the continuation and renewal of the government contracts of both our health plans and Molina
Medicaid Solutions and the terms under which such contracts are renewed; the timing of receipt and recognition of revenue and the amortization of expense under the
state contracts of Molina Medicaid Solutions in Maine and Idaho; government audits and reviews;
changes with respect to our provider contracts and the loss of providers;
the establishment, interpretation, and implementation of a federal or state medical cost
expenditure floor as a percentage of the premiums we receive, administrative cost and
profit ceilings, and profit sharing arrangements; the interpretation and implementation of at-risk premium rules regarding the achievement
of certain quality measures; the successful integration of our acquisitions;
approval by state regulators of dividends and distributions by our health plan subsidiaries;
changes in funding under our contracts as a result of regulatory changes, programmatic
adjustments, or other reforms; high dollar claims related to catastrophic illness;
the favorable resolution of litigation, arbitration, or administrative proceedings, and the
costs associated therewith; restrictions and covenants in our credit facility;
the availability of financing to fund and capitalize our acquisitions and start-up
activities and to meet our liquidity needs and the costs and fees associated therewith; a state’s failure to renew its federal Medicaid waiver;
an inadvertent unauthorized disclosure of protected health information by us or our business
associates; changes generally affecting the managed care or Medicaid management information systems
industries; increases in government surcharges, taxes, and assessments;
changes in general economic conditions, including unemployment rates;
and numerous other risk factors, including those identified within this slide presentation
and/or our accompanying oral remarks, and those discussed in our periodic reports and filings
with the Securities and Exchange Commission. These reports can be accessed under the investor
relations tab of our Company website or on the SEC’s website at www.sec.gov. Given
these risks and uncertainties, we can give no assurances that our forward-looking
statements will prove to be accurate, or that any other results or events projected or contemplated by
our forward-looking statements will in fact occur, and we caution investors not to place
undue reliance on these statements. All forward-looking statements in this release represent our
judgment as of January 26, 2012, and we disclaim any obligation to update any
forward-looking statements to conform the statement to actual results or changes in our expectations.
Safe Harbor Statement under the Private Securities Litigation Reform Act of 1995:
This slide presentation and our accompanying oral remarks contain “forward-looking
statements” |
 ©
2012 Molina Healthcare, Inc.
2012 EPS outlook
58
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
59
2012 EPS outlook
$1.80
Guidance Issued January 26, 2012
Re-procurements in WA & MO
Benefit carve-ins in TX and OH
TX inpatient and pharmacy
Ohio full year of pharmacy
Change in mix: CA SPDs, TX STAR+PLUS & WA ABDs
TX expansion commencing March 2012
Continuing rate pressure
Infrastructure build for 2012 and beyond
Molina Center
ICD-10
Healthcare reform
Additional clinics
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
60
Note:
“G”
denote
guidance.
Amounts
are
estimates
and
subject
to
change.
Actual
results
may
differ
materially.
See
cautionary
statement.
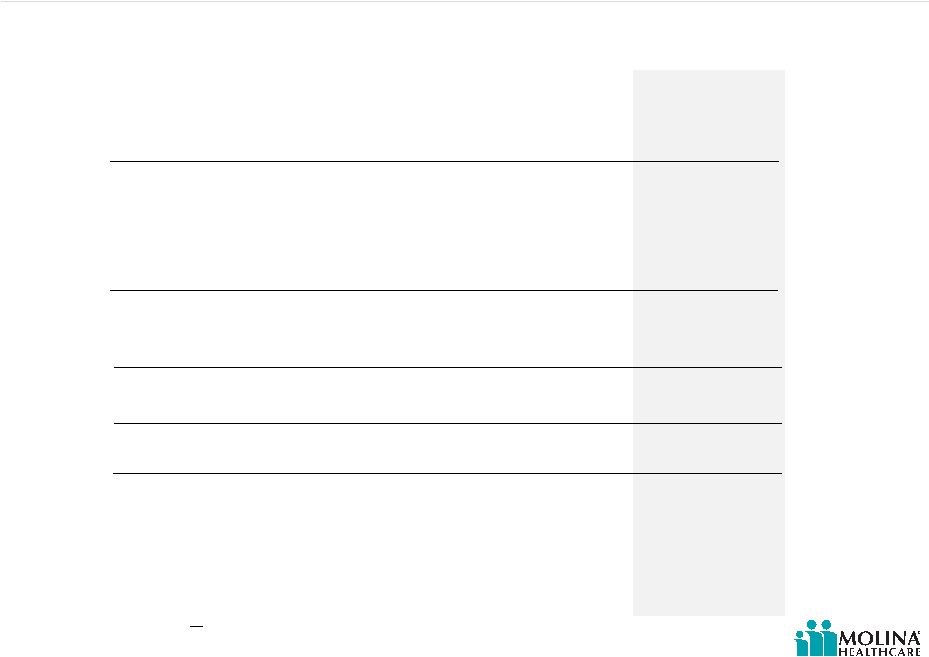
2012G*
Premium Revenue
Service Revenue
Investment Income
Total Revenue
Medical Care Costs
Medical Care Ratio
Service Costs
Service Revenue Ratio
G&A Expense
G&A Ratio
Premium Tax Expense
Depreciation
Amortization
Interest Expense
Income Before Tax
Net Income
Diluted EPS
Weighted Average Diluted Shares Outstanding
EBITDA
Effective Tax Rate
$5.9B
$185M
$6M
$6.1B
$5.1B
86%
$158M
85%
$476M
7.8%
$169M
$35M
$17M
$17M
$137M
$85M
$1.80
47.3M
$220M
38%
2012 guidance
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
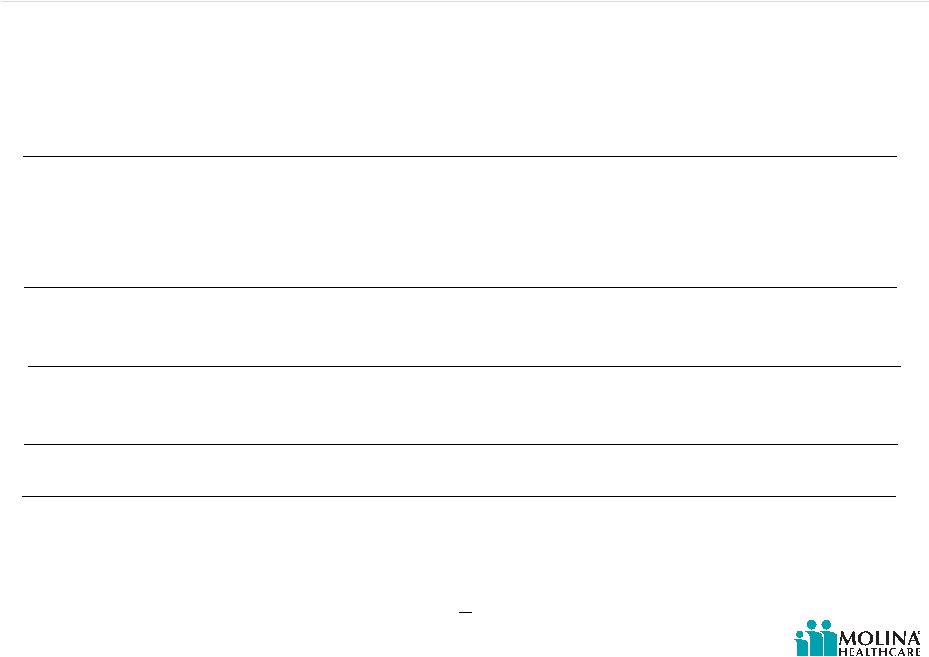
61
MMS
Total
2012 MOH segment guidance
Health Plans
Premium Revenue
Service Revenue
Investment Income
Total Revenue
Medical Care Costs
Medical Care Ratio
Service Costs
Service Revenue Ratio
G&A Expense
G&A Ratio
Premium Tax Expense
Depreciation
Amortization
Interest Expense
Income Before Tax
Net Income
Diluted EPS
Weighted Average Diluted Shares Outstanding
EBITDA
Effective Tax Rate
$5.9B
--
$6M
$5.9B
$5.1B
86%
--
--
$471M
--
$169M
$35M
$12M
$17M
$120M
$74M
--
--
$184M
--
--
$185M
--
$185M
--
--
$158M
85%
$5M
--
--
--
$5M
--
$17M
$11M
--
--
$36M
--
$5.9B
$185M
$6M
$6.1B
$5.1B
86%
$158M
85%
$476M
7.8%
$169M
$35M
$17M
$17M
$137M
$85M
$1.80
47.3M
$220M
38%
Note:
“G”
denote
guidance.
Amounts
are
estimates
and
subject
to
change.
Actual
results
may
differ
materially.
See
cautionary
statement.
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
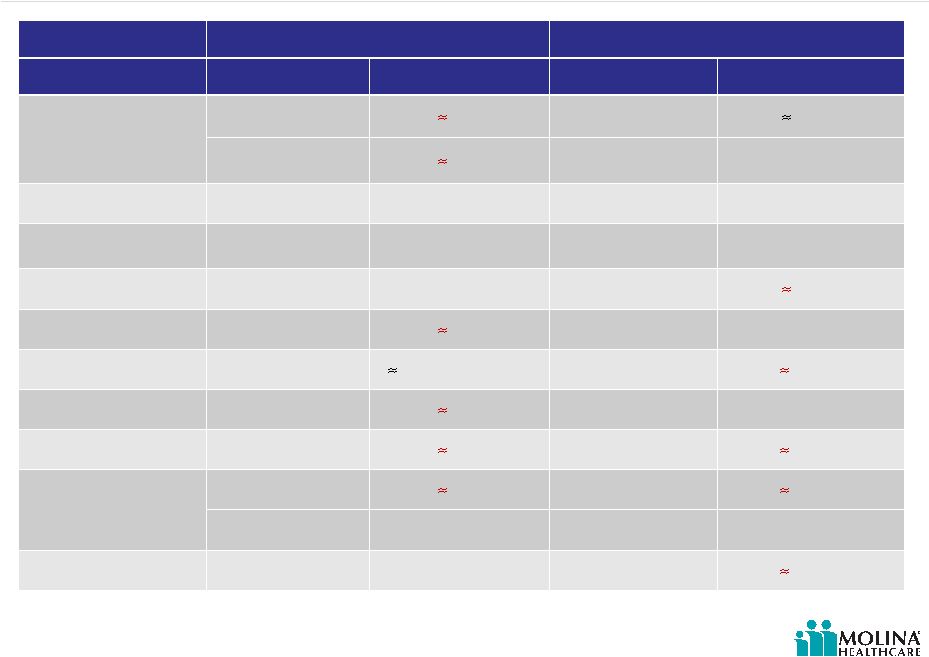
Rate change update
62
2011 CARRYOVER
2012
Health Plan
Effective Date
Revenue Change
Effective Date
Revenue Change
California
7/1/2011
(
3.5%)
1/1/2012
0.5%
(1)
10/1/2011
(
0.5%)
10/1/2012
no change
(2)
Florida
9/1/2011
˜7.5% 9/1/2012
no change
(2)
Michigan
10/1/2011
˜1.0% 10/1/2012
no change
(2)
Missouri
7/1/2011
˜5.0% 7/1/2012
(
0.5%)
(2)
New Mexico
7/1/2011
(
2.5%)
7/1/2012
no change
(2)
Ohio
10/1/2011
27.0% (Rx carve in)
1/1/2012
(
2.0%)
(1)
Texas
9/1/2011
(
2.0%)
3/1/2012
n/a
(3)
Utah
7/1/2011
(
2.0%)
7/1/2012
(
1.5%)
(2)
Washington
10/1/2011
(
0.5%)
1/1/2012
(
0.2%)
(1)
n/a
n/a
7/1/2012
n/a
(3)
Wisconsin
1/1/2011
(11.0%)
1/1/2012
(
7.5%)
(2)
Note:
(1)
Denotes known rate changes
(2)
Denotes estimated rate changes excluding new business
(3)
Rate changes not meaningful due to benefit carve ins and/or geographic population
expansion Please refer to the Company’s cautionary statements.
|
 ©
2012 Molina Healthcare, Inc.
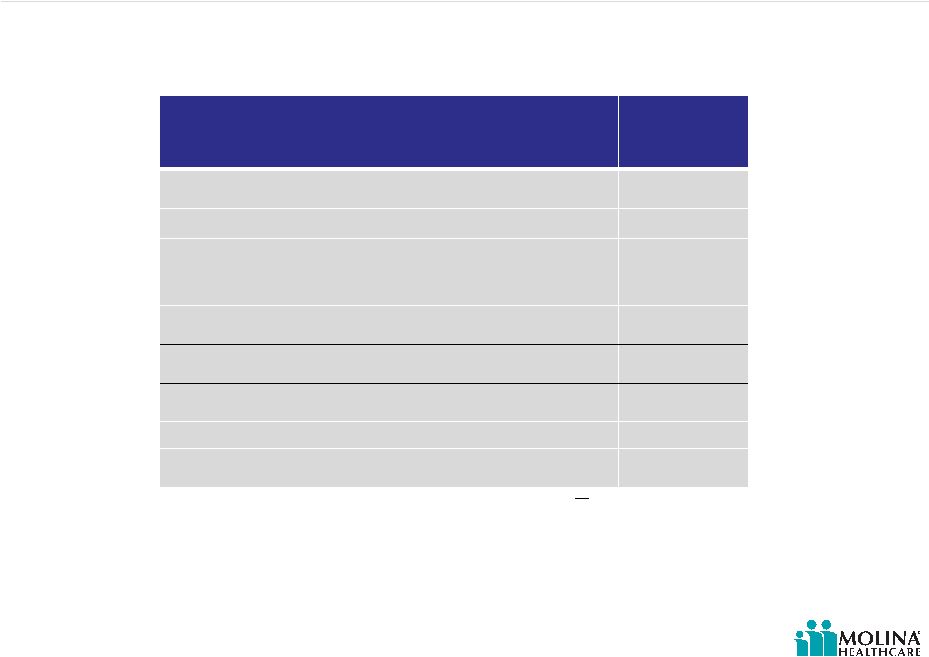
Texas expansion
63
2012
Guidance
Effective Date
3/12
MOH Expected Membership Prior to
Expansion¹
155K
MOH Expected Additional Membership
170K
Total Expected MOH Membership²
325K
MOH Expected Market Penetration² 10%
MOH Expected Incremental Revenue
$900M
1.
Denotes estimated membership at 2/29/12.
2.
Denotes
estimated
membership
at
12/31/12
.
Note:
Denotes
guidance.
Amounts
are
estimates
and
subject
to
change.
Actual
results
may
differ
materially.
See
cautionary
statements.
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
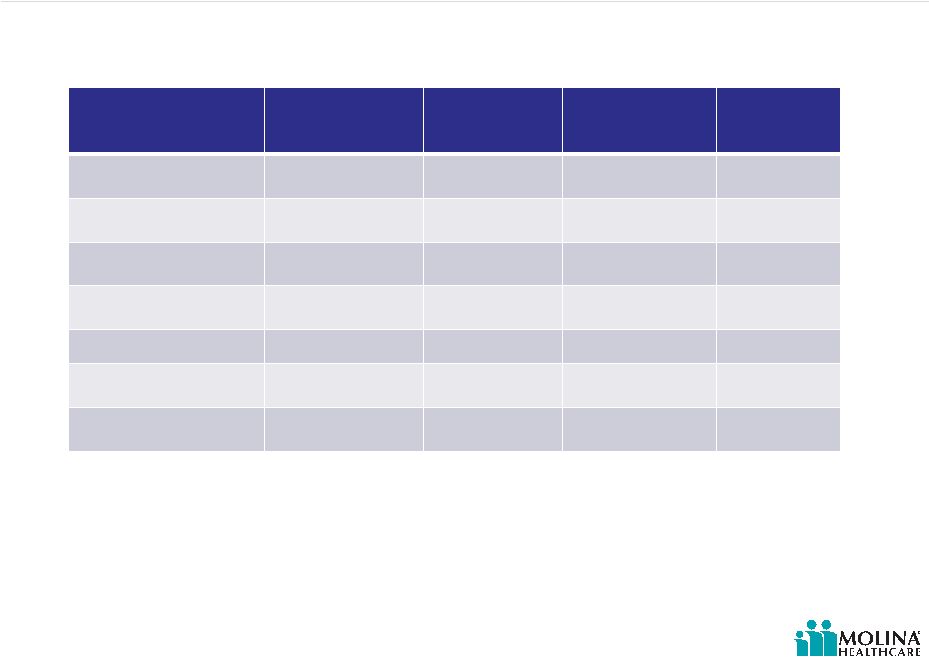
Texas March 2012 –
estimated impact of re-procurement
64
Line of Business
Dec 2011
Members
Dec 2011
Rates
Mar 2012
Members
Mar 2012
Rates
TOTAL STAR
18,000
$220
123,000
$235
TOTAL CHIP
73,000
$85
80,000
$130
TOTAL STAR PLUS
64,000
$440
100,000
$780
TOTAL
155,000
$250
303,000
$390
*Guidance assumes MCR of 90% FY 2012
Please refer to the Company’s cautionary statements. |
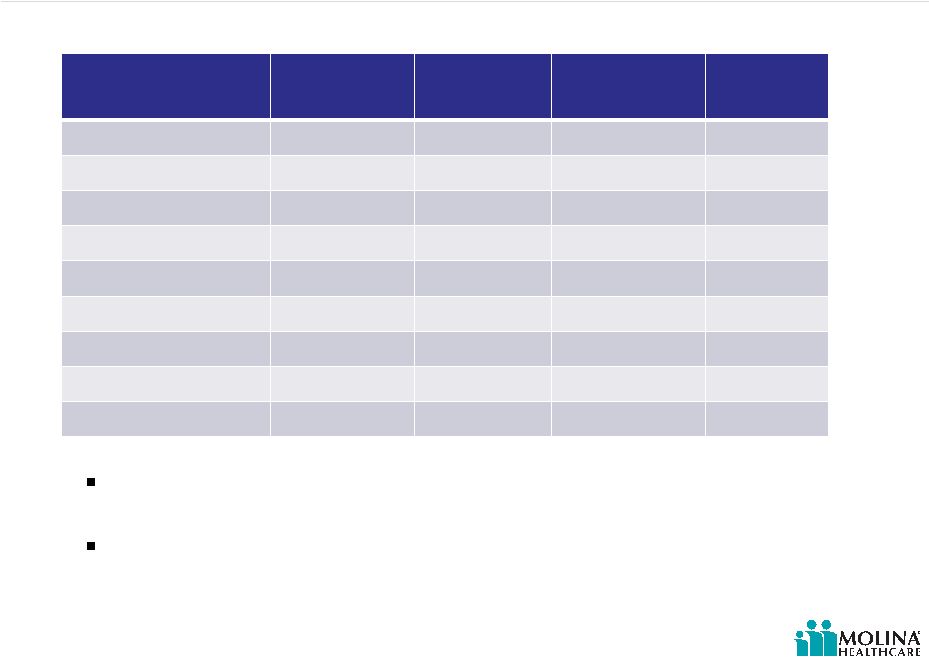 ©
2012 Molina Healthcare, Inc.
65
Line of Business
June 2012
Members
June 2012
Rates
July 2012
Members
July 2012
Rates
TANF
327,000
$160
288,000
$150
ABD
5,000
$850
12,000
$865
CHIP
11,000
$100
9,000
$95
State Funded -
BHP
8,000
$225
6,000
$240
TOTAL
351,000
$170
315,000
$180
Premium revenue excluding Medicare, is expected to drop
approximately 10% year-over-year
Guidance assumes MCR of 86% FY 2012
Washington July 2012 –
estimated impact of re-procurement
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
What could affect our 2012 number?
66
Potential headwinds:
Premium rate decreases greater than projected
Texas cost and utilization issues
Greater loss of enrollment than projected in WA
Higher than projected ABD utilization in WA
MO RFP outcome
Revenue and cost pressures in Idaho and Maine
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
What could affect our 2012 number?
Potential tailwinds:
Rate increases in markets where we are expecting
none
Cost and utilization improvement Texas
Higher than projected enrollment in CA (ABD), TX and
WA
67
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
Where is 2013 guidance?
68
Moving parts for 2013
2012 Supreme Court Decision on individual mandate
and Medicaid expansion
2012 Presidential election
Ohio RFP (goes into effect 1/2013)
Dual eligible enrollment
1
CA opportunity: 1.1M
MI opportunity: 234K
WA opportunity: 142K
Florida expansion
Georgia RFP
Sources: 1. http://www.kff.org/medicaid/upload/8215.pdf
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
Investment highlights
Attractive sector growth prospects driven by
government policies and economic conditions
Proven flexible health care services portfolio (risk-
based, fee-based and direct delivery)
Diversified geographic exposure with significant
presence in high growth regions
Focus on government-sponsored health care
programs
Seasoned management team with strong track
record of delivering earnings growth
Over 30 years of experience
69
Please refer to the Company’s cautionary statements. |
 ©
2012 Molina Healthcare, Inc.
Q&A
70 |
