Attached files
| file | filename |
|---|---|
| 8-K - LIVE FILING - AMERIGROUP CORP | htm_44063.htm |
AMENDMENT NUMBER 10
MIDDLE GRAND REGION
CONTRACTOR RISK AGREEMENT
BETWEEN
THE STATE OF TENNESSEE,
d.b.a. TENNCARE
AND
AMERIGROUP TENNESSEE, INC.
CONTRACT NUMBER: FA- 07-16936-00
For and in consideration of the mutual promises herein contained and other good and valuable consideration, the receipt and sufficiency of which is hereby acknowledged, the parties agree to clarify and/or amend the Contractor Risk Agreement (CRA) by and between the State of Tennessee TennCare Bureau, hereinafter referred to as TENNCARE, and AMERIGROUP TENNESSEE, INC., hereinafter referred to as the CONTRACTOR as specified below.
Titles and numbering of paragraphs used herein are for the purpose of facilitating use of reference only and shall not be construed to infer a contractual construction of language.
1. Section 1 shall be amended by adding the following definitions:
Abuse - Provider practices that are inconsistent with sound fiscal, business, or medical practices, and result in an unnecessary cost to the Medicaid program, or in reimbursement for services that are not medically necessary or that fail to meet professionally recognized standards for health care. It also includes recipient practices that result in unnecessary cost to the Medicaid program (see 42 CFR 455.2).
Breach (with respect to Protected Health Information (PHI)) — The acquisition, access, use, or disclosure of protected health information in a manner not permitted under the HIPAA Privacy Rule which compromises the security or privacy of the protected health information.
Fraud – An intentional deception or misrepresentation made by a person with the knowledge that the deception could result in some unauthorized benefit to himself or some other person. It includes any act that constitutes fraud under applicable Federal or State law (see 42 CFR 455.2).
Repayment – The process by which an MCO, the State of Tennessee or the Federal government, or any of their Bureaus, Agencies or Contractors recover Title XIX monies paid to an MCO, provider or enrollee.
2. Section 2.7.4.1 shall be deleted and replaced as follows:
| 2.7.4.1.1 | The CONTRACTOR shall develop programs and participate in activities to enhance the general health and well-being of members. Health education and outreach programs and activities shall include TENNderCare outreach activities (See Section 2.7.6.2) and may also include the following: |
| 3. | Section 2.7.4.2 shall be deleted and replaced by Sections 2.7.4.2 through 2.7.4.2.3 as follows: |
| 2.7.4.2 | The CONTRACTOR shall submit an Annual Community Outreach Plan no later than November 30 of each year for review and approval by TENNCARE. |
| 2.7.4.2.1 | The Annual Community Outreach Plan shall be written in accordance with guidance prepared by TENNCARE. It shall include, but is not limited to: all proposed community/health education events related to TENNderCare; community/health education events unrelated to TENNderCare; rationale for participating in these events; and a process for evaluating the benefits of the events. |
| 2.7.4.2.2 | The CONTRACTOR’s TennCare approved Annual Community Outreach Plan shall be implemented on January 1 of each year. |
| 2.7.4.2.3 | Community/health education events, both related and unrelated to TENNderCare, shall be included in the quarterly TENNderCare Report (See Section 2.30.4.4) in a format specified by TENNCARE. |
| 4. | Section 2.7.6.2.10 shall be amended by adding the reference “(See Section 2.7.4.2)” to the end of the first sentence. |
| 5. | Section 2.9.5.4.1 through 2.9.5.4.1.4 shall be deleted and replaced as follows: |
| 2.9.5.4.1 | In addition to requirements pertaining to nursing facility to community transitions (see Section 2.9.6.8), members in CHOICES Group 1 who are under the age of 21 and who are residents of a nursing facility and have requested to transition home will be provided coordination of care by the CHOICES Care Coordinator and MCO Case Management staff: |
| 2.9.5.4.1.1 | The member will be informed by the CHOICES Care Coordinator of disenrollment from CHOICES upon discharge from Nursing Facility; |
| 2.9.5.4.1.2 | Within three (3) business days of a request to transition by or on behalf of a Group 1 member under age 21, the member will be referred by the CHOICES Care Coordinator to MCO Case Management for service identification and implementation in the home setting; |
| 2.9.5.4.1.3 | The MCO Case Manager will be responsible for developing a service plan for the home setting; |
| 2.9.5.4.1.4 | The CHOICES Care Coordinator will communicate weekly via phone or face-to-face visits with the MCO Case Management staff, the member and/or his parent or guardian (as applicable and appropriate), and the nursing facility staff to ensure timely progression of the transition plan until the transition plan is complete; and |
| 6. | Section 2.9.6.1.6.1 shall be amended by adding a “)” after the word “computation”. |
| 7. | Section 2.9.6.2.5.1 shall be deleted and replaced as follows: |
| 2.9.6.2.5.1 | For members enrolled in CHOICES Group 2 who are, upon CHOICES enrollment, receiving community-based residential alternative services that are covered in CHOICES, the CONTRACTOR shall, immediately upon notice of the member’s enrollment in CHOICES, authorize such services from the current provider as of the effective date of CHOICES enrollment. In the case of those members enrolled in CHOICES Group 2 on the basis of Immediate Eligibility, community-based residential alternative services shall be authorized immediately upon notice of the member’s categorical and financial eligibility for TennCare CHOICES as of the effective date of CHOICES enrollment. The CONTRACTOR shall not transition members enrolled in CHOICES Group 2 who are, upon CHOICES enrollment, receiving services in a community-based residential alternative setting to another facility unless: (1) the member or his/her representative specifically requests to move, which shall be documented in the member’s file; (2) the member or his/her representative provides written consent to move based on quality or other concerns raised by the CONTRACTOR; or (3) the facility where the member is residing is not a contract provider; if the facility is a non-contract provider, the CONTRACTOR shall authorize medically necessary services from the non-contract provider for at least thirty (30) days which shall be extended as necessary to ensure continuity of care pending the facility’s enrollment with the CONTRACTOR or the member’s transition to a contract provider. |
| 8. | Section 2.9.6.3.7 shall be deleted and replaced as follows: |
| 2.9.6.3.7 | If the member does not meet the telephone screening criteria, the CONTRACTOR shall within five (5) business days of the screening notify the member verbally and in writing in the format prescribed by TENNCARE: (1) that he/she does not appear to meet the criteria for enrollment in CHOICES; (2) that he/she has the right to continue with the CHOICES intake process and, if determined not eligible, to receive notice of such denial, including the member’s due process right to appeal; and (3) how, if the member wishes to proceed with the CHOICES intake process, the member can submit a written request to proceed with the CHOICES intake process to the CONTRACTOR. In the event that a member does submit such written request, the CONTRACTOR shall process the request as a new referral and shall conduct a face-to-face intake visit, including level of care assessment and needs assessment, within ten (10) business days of receipt of the member’s written request, unless a later date is requested by the member, which shall be documented in writing in the CHOICES intake record. |
| 9. | Section 2.9.6.6.1.1 shall be amended by adding the word “CHOICES” in front of the word “file”. |
| 10. | Section 2.9.6.6.2.7 shall be deleted and replaced as follows: |
| 2.9.6.6.2.7 | The member’s care coordinator/care coordination team shall provide a copy of the member’s completed plan of care, including any updates, to the member, the member’s representative, as applicable, and the member’s community residential alternative provider, as applicable. The member’s care coordinator/care coordination team shall provide copies to other providers authorized to deliver care to the member upon request, and shall ensure that such providers who do not receive a copy of the plan of care are informed in writing prior to the scheduled implementation of services of all relevant information needed to ensure the provision of quality care for the member and to help ensure the member’s health, safety, and welfare, including but not limited to the tasks and functions to be performed. |
| 11. | Section 2.9.6.6.2.8 shall be amended by adding a new Section 2.9.6.6.2.8.1 which shall read as follows: |
| 2.9.6.6.2.8.1 | Within three (3) business days of updating the member’s plan of care, the member’s care coordinator/care coordination team shall provide a copy of all relevant changes to the supports broker, as applicable, and to other providers authorized to deliver care to the member. Relevant information shall include any information needed to ensure the provision of quality care for the member and to help ensure the member’s health, safety, and welfare, including but not limited to any changes in the tasks and functions to be performed. |
| 12. | Section 2.9.6.8.25.3 and Section 2.9.6.8.25.4 shall be deleted and replaced by new Sections 2.9.6.8.25.3, 2.9.6.8.25.4 and 2.9.6.8.25.4.1 as follows: |
| 2.9.6.8.25.3 | The CONTRACTOR shall conduct a census at least semi-annually at no less than one hundred twenty (120)-day intervals or as frequently as deemed necessary by TENNCARE to confirm the residency status and Group assignment of all CHOICES members (i.e., Group 1 receiving services in a NF or Group 2 receiving HCBS or short- term NF services). The CONTRACTOR shall take actions as necessary to address any discrepancies when a CHOICES member is found to no longer be receiving LTC services, or is receiving services in a different service delivery setting, e.g., NF, HCBS, or hospice in a NF, including, as appropriate, disenrollment from CHOICES and/or enrollment in a different CHOICES Group. |
| 2.9.6.8.25.4 | The CONTRACTOR shall authorize and/or reimburse short-term NF stays for Group 2 members only when the member’s stay in the facility is expected to be less than ninety (90) days and the member is expected to return to the community upon its conclusion. The CONTRACTOR shall monitor all short-term NF stays for Group 2 members and shall ensure that the member is transitioned from Group 2 to Group 1 at any time a) it is determined that the stay will not be short-term or the member will not transition back to the community; and b) prior to exhausting the ninety (90)-day short-term NF benefit covered for CHOICES Group 2 members. |
| 2.9.6.8.25.4.1 | Upon request, the CONTRACTOR shall provide to TENNCARE a member-by-member status for each Group 2 member utilizing the short-term NF stay benefit, including but not limited to the name of each Group 2 member receiving short-term NF services, the NF in which s/he currently resides, the date of admission for short-term stay, and the anticipated date of discharge back to the community. |
| 13. | Section 2.9.6.9.1.1.4 shall be amended by deleting the word “and” at the end of the text and Section 2.9.6.9.1.1.5 shall be deleted and replaced as follows: |
| 2.9.6.9.1.1.5 | In the manner prescribed by TENNCARE and in accordance with this Agreement and TENNCARE policies and protocols pertaining thereto: 1) facilitate transfers between nursing facilities which, at a minimum, includes notification to the receiving facility of the member’s level of care, and notification to DHS; and 2) facilitate transitions to CHOICES Group 2 which shall include (but is not limited to) timely notification to TENNCARE; and |
| 14. | Section 2.9.6.9.2.1.2 shall be deleted and replaced as follows: |
| 2.9.6.9.2.1.2 | During the development of the member’s plan of care and as part of the annual updates, the care coordinator shall discuss with the member his/her interest in consumer direction when eligible CHOICES HCBS are included in the plan of care; |
| 15. | Section 2.9.6.9.2.1.15 shall be amended by deleting the word “and” at the end of the text, Section 2.9.6.9.2.1.17 shall be amended by deleting the “.” and adding “; and”, and Section 2.9.6.9.2.1 shall be amended by adding a new Section 2.9.6.9.2.1.18 as follows: |
| 2.9.6.9.2.1.18 | In the manner prescribed by TENNCARE, and in accordance with this Agreement and TENNCARE policies and protocols pertaining thereto, facilitate transition to CHOICES Group 1, which shall include (but is not limited to) timely notification to TENNCARE. |
| 16. | Section 2.9.6.10.3 shall be deleted and replaced by new Sections 2.9.6.10.3 through 2.9.6.3.10.3.3 as follows: |
| 2.9.6.10.3 | If a member elects not to receive eligible CHOICES HCBS using contract providers until all necessary requirements have been fulfilled in order to implement consumer direction of eligible CHOICES HCBS: |
| 2.9.6.10.3.1 | The CONTRACTOR shall document this decision, including date and member/member’s representative’s signature, in the manner specified by TENNCARE (see Section 2.9.7.4.3.2 of this Agreement). |
| 2.9.6.10.3.2 | The member’s care coordinator shall visit the member face to face at least monthly to ensure that the member’s needs are met, and shall continue to offer eligible CHOICES HCBS through contract providers (See Section 2.9.7.4.3.3). |
| 2.9.6.10.3.3 | If eligible CHOICES HCBS are not initiated within sixty (60) days following referral to the FEA, the CONTRACTOR shall notify the member that eligible CHOICES HCBS must be initiated by contract providers unless these HCBS are not needed on an ongoing basis in order to safely meet the member’s needs in the community, in which case, the CONTRACTOR shall submit documentation to TENNCARE to begin the process of disenrollment from CHOICES Group 2. |
| 17. | Section 2.9.6.10 shall be amended by adding a new Section 2.9.6.10.11 as follows and renumbering the remaining Section accordingly, including any references thereto. |
| 2.9.6.10.11 | Within three (3) business days of updating the member’s plan of care, the member’s care coordinator/care coordination team shall provide a copy of all relevant changes to the supports broker (see Section 2.9.6.6.2.8.1. of this Agreement). |
| 18. | Section 2.9.6.11.3 through 2.9.6.11.5 shall be deleted and replaced as follows and the remaining Section shall be renumbered accordingly, including any references thereto. |
| 2.9.6.11.3 | The CONTRACTOR shall ensure that an adequate number of care coordinators are available and that sufficient staffing ratios are maintained to address the needs of CHOICES members and meet all the requirements described in this Agreement. |
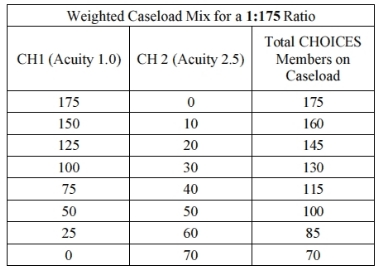
| 2.9.6.11.4 | The recommended average weighted care coordinator-to-CHOICES member staffing ratio is no more than 1:125. Such average shall be derived by dividing the total number of full-time equivalent care coordinators by the total weighted value of CHOICES members as delineated below. |
| 2.9.6.11.5 | The recommended maximum caseload for any individual care coordinator is a weighted value of no more than one hundred seventy-five (175) CHOICES members. |
| 2.9.6.11.6 | The contractor shall use the following methodology to calculate weighted care coordinatorto-CHOICES member staffing ratios and care coordinator caseloads: |
| 2.9.6.11.6.1 | Each CHOICES Group 1 member shall be factored into the weighted care coordinator-to-CHOICES member staffing ratio and weighted caseload calculations utilizing an acuity level of one (1), EXCEPT that: |
| 2.9.6.11.6.1.1 | Upon completion of a Transition Assessment which indicates that a Group 1 member is a candidate for transition to the community, such member shall be factored into the weighted caseload and staffing ratio calculations using an acuity level of two and one- half (2.5) until such time as the member is transitioned to CHOICES Group 2 or the member is no longer a candidate for transition; |
| 2.9.6.11.6.1.2 | CHOICES Group 1 members under twenty-one (21) years of age shall be factored into the weighted caseload and staffing ratio calculations utilizing an acuity level of two and one-half (2.5). |
| 2.9.6.11.6.2 | Each CHOICES Group 2 member shall be factored into the weighted caseload and staffing ratio calculations utilizing an acuity level of two and one-half (2.5); |
| 2.9.6.11.6.3 | Using the delineated acuity factors, the following provides examples of the composition of caseloads with a weighted value of 125: |

| 2.9.6.11.6.4 | Using the delineated acuity factors, the following delineates the composition of caseloads with a weighted value of 175: |
| 2.9.6.11.7 | The CONTRACTOR shall proactively plan for staff turnover and shall monitor caseload assignments and weighted care coordinator-to-CHOICES member staffing ratios and adjust hiring practices and care coordinator assignments as necessary to meet the requirements of this Agreement and to address members’ needs. |
| 2.9.6.11.8 | Upon request, the CONTRACTOR shall provide to TENNCARE documentation of such monitoring, including an itemized list by care coordinator of the total number of members assigned, and the number of Group 1 members (including members in transition and children under age 21) and Group 2 members that comprise each care coordinator’s caseload. |
| 2.9.6.11.9 | In the event that the CONTRACTOR is determined to be deficient with any requirement pertaining to care coordination as set forth in this agreement, the amount of financial sanctions assessed shall take into account whether or not the CONTRACTOR has complied with the recommended average weighted care coordinator to CHOICES member staffing ratio and the maximum weighted care coordinator caseload amounts set forth in Sections 2.9.6.11.4 and 2.9.6.11.5, based on the most recent monthly CHOICES Caseload and Staffing Ratio Report (see Section 2.30.6.8). All applicable sanctions set forth in Sections 4.20.2.2.6., 4.20.2.2.7.A.16, 4.20.2.2.7.A.18, 4.20.2.2.7.A.19, 4.20.2.2.7.A.20, 4.20.2.2.7.A.21, 4.20.2.2.7.A.22, 4.20.2.2.7.A.23, 4.20.2.2.7.A.28, 4.20.2.2.7.A.29, 4.20.2.2.7.A.30, 4.20.2.2.7.A.31, 4.20.2.2.7.B.21, and 4.20.2.2.7.C.7 of this agreement shall be multiplied by two (2) when the CONTRACTOR has not complied with these recommendations. |
| 2.9.6.11.10 | TennCare will reevaluate Care Coordinator-to-CHOICES member staffing ratio recommendations and requirements on at least an annual basis and may make adjustments based on the needs of CHOICES members, CHOICES program requirements and MCO performance. |
| 2.9.6.11.11 | TENNCARE may request changes in the CONTRACTOR’s Care Coordination Staffing Plan at any time it determines that the CONTRACTOR does not have sufficient care coordination staff to properly and timely perform its obligations under this Agreement. |
| 19. | The renumbered Section 2.9.6.11.18 shall be amended by deleting the words “at least annually”. |
| 20. | Section 2.9.6.11 shall be amended by adding a new Section 2.9.6.11.19 as follows and renumbering the remaining Section including any references thereto. |
| 2.9.6.11.19 | The CONTRACTOR shall establish an ongoing training program for care coordinators. Topics to be covered shall be determined by the CONTRACTOR based on its monitoring of care coordination (see Section 2.9.6.12) and the CHOICES program, and feedback from TENNCARE. |
| 21. | Section 2.9.6.12.7 shall be amended by adding the words “and document” as follows: |
| 2.9.6.12.7 | The CONTRACTOR shall develop and maintain an electronic case management system that includes the functionality to ensure and document compliance with all requirements specified in the Section 1115 TennCare Demonstration Waiver, federal and state laws and regulations, this Agreement, and TennCare policies and protocols, including but not limited to the following: |
| 22. | Section 2.12.4 shall be deleted and replaced as follows: |
2.12.4 LEFT BLANK INTENTIONALLY
| 23. | Section 2.12.9 shall be deleted and replaced as follows and all references to Section 2.12.9 shall be updated accordingly. |
| 2.12.9 | All provider agreements executed by the CONTRACTOR, and all provider agreements executed by subcontracting entities or organizations, shall, except as otherwise provided in Section 2.12.13, at a minimum, meet the following requirements: |
| 2.12.9.1 | Be in writing. All new provider agreements and existing provider agreements as they are renewed, shall include a signature page which contains CONTRACTOR and provider names which are typed or legibly written, provider company with titles, and dated signatures of all appropriate parties; |
| 2.12.9.2 | Specify the effective dates of the provider agreement; |
| 2.12.9.3 | Specify that the provider agreement and its attachments contain all the terms and conditions |
agreed upon by the parties;
| 2.12.9.4 | Assure that the provider shall not enter into any subsequent agreements or subcontracts forany of the work contemplated under the provider agreement without the prior written approval of the CONTRACTOR; |
| 2.12.9.5 | Identify the population covered by the provider agreement; |
| 2.12.9.6 | Specify that the provider may not refuse to provide covered medically necessary or covered preventive services to a child under the age of twenty-one (21) or a TennCare Medicaid patient under this Agreement for non-medical reasons. However, the provider shall not be required to accept or continue treatment of a patient with whom the provider feels he/she cannot establish and/or maintain a professional relationship; |
| 2.12.9.7 | Specify the functions and/or services to be provided by the provider and assure that the functions and/or services to be provided are within the scope of his/her professional/technical practice; |
| 2.12.9.8 | Specify the amount, duration and scope of services to be provided by the provider and inform the provider of TennCare non-covered services as described in Section 2.10 of this Agreement and the TennCare rules and regulations; |
| 2.12.9.9 | Provide that emergency services be rendered without the requirement of prior authorization of any kind; |
| 2.12.9.10 | Require compliance with applicable access requirements, including but not limited to appointment and wait times as referenced in Section 2.11 of the CONTRACTOR’s Agreement with TENNCARE; |
| 2.12.9.11 | Specify that unreasonable delay in providing care to a pregnant member seeking prenatal care shall be considered a material breach of the provider’s agreement with the CONTRACTOR and include the definition of unreasonable delay as described in Section 2.7.5.2.3 of this Agreement; |
| 2.12.9.12 | If the provider performs laboratory services, require the provider to meet all applicable requirements of the Clinical Laboratory Improvement Amendments (CLIA) of 1988; |
| 2.12.9.13 | Require the provider to have and maintain documentation necessary to demonstrate that |
covered services were provided in compliance with state and federal requirements;
| 2.12.9.14 | Require that an adequate record system be maintained and that all records be maintained for five (5) years from the close of the provider agreement (behavioral health records shall be maintained at the provider level for ten (10) years after the termination of the provider agreement pursuant to TCA 33-3-101) or retained until all evaluations, audits, reviews or investigations or prosecutions are completed for recording enrollee services, servicing providers, charges, dates and all other commonly accepted information elements for services rendered to enrollees pursuant to the provider agreement (including but not limited to such records as are necessary for the evaluation of the quality, appropriateness, and timeliness of services performed under the provider agreement and administrative, civil or criminal investigations and prosecutions); |
| 2.12.9.15 | Include a statement that as a condition of participation in TennCare, enrollees and providers shall give TENNCARE or its authorized representative, the Office of the Comptroller of the Treasury, and any health oversight agency, such as OIG, TBI MFCU, DHHS Office of Inspector General (DHHS OIG), and DOJ, and any other authorized state or federal agency, access to their records. Said records shall be made available and furnished immediately upon request by the provider for fiscal audit, medical audit, medical review, utilization review, and other periodic monitoring as well as for administrative, civil and criminal investigations or prosecutions upon the request of an authorized representative of the CONTRACTOR, |
TENNCARE or authorized federal, state and Office of the Comptroller of the Treasury personnel, including, but not limited to, the OIG, the TBI MFCU, the DHHS OIG and the DOJ;
2.12.9.16 Include medical records requirements found in Section 2.24.6 of this Agreement;
| 2.12.9.17 | Contain the language described in Section 2.25.6 of this Agreement regarding Audit Requirements and Section 2.25.5 of this Agreement regarding Availability of Records; |
| 2.12.9.18 | Provide that TENNCARE, DHHS OIG, Office of the Comptroller of the Treasury, OIG, TBI MFCU, and DOJ, as well as any authorized state or federal agency or entity shall have the right to evaluate through inspection, evaluation, review or request, whether announced or unannounced, or other means any records pertinent to this Agreement including, but not limited to medical records, billing records, financial records, and/or any records related to services rendered, quality, appropriateness and timeliness of services and/or any records relevant to an administrative, civil and/or criminal investigation and/or prosecution and such evaluation, inspection, review or request, and when performed or requested, shall be performed with the immediate cooperation of the provider. Upon request, the provider shall assist in such reviews including the provision of complete copies of medical records. Include a statement that HIPAA does not bar disclosure of protected health information (PHI) to health oversight agencies, including, but not limited to, OIG, TBI MFCU, DHHS OIG and DOJ. Provide that any authorized state or federal agency or entity, including, but not limited to TENNCARE, OIG, TBI MFCU, DHHS OIG, DOJ, Office of the Comptroller of the Treasury, may use these records and information for administrative, civil or criminal investigations and prosecutions; |
| 2.12.9.19 | Provide for monitoring, whether announced or unannounced, of services rendered to members; |
| 2.12.9.20 | Provide for the participation and cooperation in any internal and external QM/QI, monitoring, utilization review, peer review and/or appeal procedures established by the CONTRACTOR and/or TENNCARE; |
| 2.12.9.21 | Specify CONTRACTOR’s responsibilities under this Agreement and its agreement with the provider, including but not limited to, provision of a copy of the member handbook and provider handbook whether via web site or otherwise and requirement that the CONTRACTOR notice a provider of denied authorizations; |
| 2.12.9.22 | Specify that the CONTRACTOR shall monitor the quality of services delivered under the provider agreement and initiate corrective action where necessary to improve quality of care, in accordance with that level of medical, behavioral health, or long-term care which is recognized as acceptable professional practice in the respective community in which the provider practices and/or the standards established by TENNCARE; |
| 2.12.9.23 | Require that the provider comply with corrective action plans initiated by the CONTRACTOR; |
| 2.12.9.24 | Provide for the timely submission of all reports and clinical information required by the CONTRACTOR; |
2.12.9.25 Provide the name and address of the official payee to whom payment shall be made;
| 2.12.9.26 | Make full disclosure of the method and amount of compensation or other consideration to be received from the CONTRACTOR. However, the agreement shall not include rate methodology that provides for an automatic increase in rates; |
| 2.12.9.27 | Specify that the CONTRACTOR shall only pay providers for services (1) provided in accordance with the requirements of this Agreement, the CONTRACTOR’s policies and procedures implementing this Agreement, and state and federal law and (2) provided to TennCare enrollees who are enrolled with the CONTRACTOR; and specify that the provider is responsible for (1) ensuring that any applicable authorization requirements are met and (2) verifying that a person is eligible for TennCare on the date of service; |
| 2.12.9.28 | Provide for prompt submission of information needed to make payment. Specify that a provider shall have one hundred twenty (120) calendar days from the date of rendering a covered service to file a claim with the CONTRACTOR except in situations regarding coordination of benefits or subrogation in which case the provider is pursuing payment from a third party or if an enrollee is enrolled in the MCO with a retroactive eligibility date. In situations of third party benefits, the maximum time frames for filing a claim shall begin on the date that the third party documented resolution of the claim. In situations of enrollment in the CONTRACTOR’s MCO with a retroactive eligibility date, the time frames for filing a claim shall begin on the date that the CONTRACTOR receives notification from TENNCARE of the enrollee’s eligibility/enrollment; |
| 2.12.9.29 | Provide for payment to the provider upon receipt of a clean claim properly submitted by the provider within the required time frames as specified in TCA 56-32-126 and Section 2.22.4 of this Agreement; |
| 2.12.9.30 | Specify the provider shall accept payment or appropriate denial made by the CONTRACTOR (or, if applicable, payment by the CONTRACTOR that is supplementary to the enrollee’s third party payer) plus the amount of any applicable TennCare cost sharing responsibilities, as payment in full for covered services provided and shall not solicit or accept any surety or guarantee of payment from the enrollee in excess of the amount of applicable TennCare cost sharing responsibilities. Enrollee shall include the patient, parent(s), guardian, spouse or any other legally responsible person of the enrollee being served; |
| 2.12.9.3 | 1 Specify that in the event that TENNCARE deems the CONTRACTOR unable to timely process and reimburse claims and requires the CONTRACTOR to submit provider claims for reimbursement to an alternate claims processor to ensure timely reimbursement, the provider shall agree to accept reimbursement at the CONTRACTOR’s contracted reimbursement rate or the rate established by TENNCARE, whichever is greater; |
| 2.12.9.32 | Specify the provider’s responsibilities and prohibited activities regarding cost sharing as provided in Section 2.6.7 of this Agreement; |
| 2.12.9.33 | Specify the provider’s responsibilities regarding third party liability (TPL) , including the provider’s obligation to identify third party liability coverage, including Medicare and longterm care insurance as applicable, and, except as otherwise provided in the CONTRACTOR’s Agreement with TENNCARE, to seek such third party liability payment before submitting claims to the CONTRACTOR; |
| 2.12.9.34 | For those agreements where the provider is compensated via a capitation arrangement, language which requires: |
| 2.12.9.34.1 | That if a provider becomes aware for any reason that he or she is not entitled to a capitation payment for a particular enrollee (a patient dies, for example), the provider shall immediately notify both the CONTRACTOR and TENNCARE by certified mail, return receipt requested; and |
| 2.12.9.34.2 | The provider shall submit utilization or encounter data as specified by the CONTRACTOR so as to ensure the CONTRACTOR’s ability to submit encounter data to TENNCARE that meets the same standards of completeness and accuracy as required for proper adjudication of fee-for-service claims; |
| 2.12.9.35 | Require the provider to comply with fraud and abuse requirements described in Section 2.20 of this Agreement; |
| 2.12.9.36 | Require that the provider comply with the Affordable Care Act and TennCare policy and procedures, including but not limited to, reporting overpayments and, when it is applicable, return overpayments to the CONTRACTOR within sixty (60) days from the date the overpayment is identified. Overpayments that are not returned within sixty (60) days from the date the overpayment was identified may result in a penalty pursuant to state or federal law; |
| 2.12.9.37 | Require the provider to comply and submit to the CONTRACTOR disclosure of information in accordance with the requirements, including timeframes, specified in 42 CFR Part 455, Subpart B and TennCare policies and procedures. The timeframes for this requirement shall include, at a minimum, at the time of initial contracting, contract renewal, at any time there is a change to any of the information on the disclosure form, at least once every three (3) years, and at anytime upon request; |
| 2.12.9.38 | Any reassignment of payment must be made in accordance with 42 CFR 447.10. All tax-reporting provider entities shall not be permitted to assign TennCare funds/payments to billing agents or alternative payees without executing a billing agent or alternative payee assignment agreement. The billing agents and alternative payees are subject to initial and monthly federal exclusion (LEIE) and debarment (EPLS) screening by the assignee if the alternative payee assignment is on-going. Further, direct and indirect payments to out of country individuals and/or entities are prohibited; |
| 2.12.9.39 | Require providers to screen their employees and contractors initially and on an ongoing monthly basis to determine whether any of them has been excluded from participation in Medicare, Medicaid, SCHIP, or any Federal health care programs (as defined in Section 1 128B(f) of the Social Security Act) and not employ or contract with an individual or entity that has been excluded or debarred. The provider shall be required to immediately report to the CONTRACTOR any exclusion information discovered. The provider shall be informed by the CONTRACTOR that civil monetary penalties may be imposed against providers who employ or enter into contracts with excluded individuals or entities to provide items or services to TennCare members; |
| 2.12.9.40 | The provider, subcontractor or any other entity agrees to abide by the Medicaid laws, regulations and program instructions that apply to the provider. The provider, subcontractor or any other entity understands that payment of a claim by TennCare or a TennCare Managed Care Contractor and/or Organization is conditioned upon the claim and the underlying |
transaction complying with such laws, regulations, and program instructions (including, but not limited to, the Federal anti-kickback statute and the Stark law), and is conditioned on the provider’s, subcontractor’s or any other entity’s compliance with all applicable conditions of participation in Medicaid. The provider, subcontractor or any other entity understands and agrees that each claim the provider, subcontractor or any other entity submits to TennCare or a TennCare Managed Care Contractor and/or Organization constitutes a certification that the provider, subcontractor or any other entity has complied with all applicable Medicaid laws, regulations and program instructions (including, but not limited to, the Federal anti-kickback statute and the Stark law), in connection with such claims and the services provided therein;
| 2.12.9.41 | Require the provider to conduct background checks in accordance with state law and TennCare policy; |
| 2.12.9.42 | Require the provider to report suspected abuse, neglect, and exploitation of adults in accordance with TCA 71-6-103 and to report suspected brutality, abuse, or neglect of children in accordance with TCA 37-1-403 and TCA 37-1-605; |
| 2.12.9.43 | Require that, for CHOICES members, the provider facilitate notification of the member’s care coordinator by notifying the CONTRACTOR, in accordance with the CONTRACTOR’s processes, as expeditiously as warranted by the member’s circumstances, of any known significant changes in the member’s condition or care, hospitalizations, or recommendations for additional services; |
| 2.12.9.44 | Require hospitals, including psychiatric hospitals, to cooperate with the CONTRACTOR in developing and implementing protocols as part of the CONTRACTOR’s nursing facility diversion plan (see Section 2.9.6.7), which shall, include, at a minimum, the hospital’s obligation to promptly notify the CONTRACTOR upon admission of an eligible member regardless of payor source for the hospitalization; how the hospital will identify members who may need home health, private duty nursing, nursing facility, or CHOICES HCBS upon discharge, and how the hospital will engage the CONTRACTOR in the discharge planning process to ensure that members receive the most appropriate and cost-effective medically necessary services upon discharge; |
| 2.12.9.45 | As a condition of reimbursement for global procedures codes for obstetric care, the provider shall submit utilization or encounter data as specified by the CONTRACTOR in a timely manner to support the individual services provided; |
| 2.12.9.46 | Except as otherwise specified in Sections 2.12.11 or 2.12.12, require the provider to secure all necessary liability and malpractice insurance coverage as is necessary to adequately protect the CONTRACTOR’s members and the CONTRACTOR under the provider agreement. The provider shall maintain such insurance coverage at all times during the provider agreement and upon execution of the provider agreement furnish the CONTRACTOR with written verification of the existence of such coverage; |
| 2.12.9.47 | Specify both the CONTRACTOR and the provider agree to recognize and abide by all state and federal laws, regulations and guidelines applicable to the CONTRACTOR and the provider. Provide that the agreement incorporates by reference all applicable federal law and state laws, TennCare rules and regulations, consent decrees or court orders, and revisions of such laws, regulations, consent decrees or court orders shall automatically be incorporated into the provider agreement, as they become effective; |
| 2.12.9.48 | Specify procedures and criteria for any alterations, variations, modifications, waivers, extension of the provider agreement termination date, or early termination of the agreement and specify the terms of such change. If provision does not require amendments be valid only when reduced to writing, duly signed and attached to the original of the provider agreement, then the terms shall include provisions allowing at least thirty (30) calendar days to give notice of rejection and requiring that receipt of notification of amendments be documented (e.g., certified mail, facsimile, hand-delivered receipt, etc); |
| 2.12.9.49 | Include provisions that allow the CONTRACTOR to suspend, deny, refuse to renew or terminate any provider agreement in accordance with the terms of the CONTRACTOR’s Agreement with TENNCARE (see Section 4.4) and applicable law and regulation; |
| 2.12.9.50 | Specify that TENNCARE reserves the right to direct the CONTRACTOR to terminate or modify the provider agreement when TENNCARE determines it to be in the best interest of the State; |
| 2.12.9.51 | Specify that both parties recognize that in the event of termination of this Agreement between the CONTRACTOR and TENNCARE for any of the reasons described in Section 4.4 of this Agreement, the provider shall immediately make available, to TENNCARE, or its designated representative, in a usable form, any or all records, whether medical or financial, related to the provider’s activities undertaken pursuant to the CONTRACTOR/provider agreement. The provision of such records shall be at no expense to TENNCARE; |
| 2.12.9.52 | Specify that the TennCare Provider Independent Review of Disputed Claims process shall be available to providers to resolve claims denied in whole or in part by the CONTRACTOR as provided at TCA 56-32-126(b); |
| 2.12.9.53 | Include a Conflict of Interest clause as stated in Section 4.19 of this Agreement, Gratuities clause as stated in Section 4.23 of this Agreement, and Lobbying clause as stated in Section 4.24 of this Agreement between the CONTRACTOR and TENNCARE; |
| 2.12.9.54 | Specify that at all times during the term of the agreement, the provider shall indemnify and hold TENNCARE harmless from all claims, losses, or suits relating to activities undertaken pursuant to the Agreement between TENNCARE and the CONTRACTOR. This indemnification may be accomplished by incorporating Section 4.31 of the TENNCARE/CONTRACTOR Agreement in its entirety in the provider agreement or by use of other language developed by the CONTRACTOR and approved in writing by TENNCARE; |
| 2.12.9.55 | Require safeguarding of information about enrollees according to applicable state and federal laws and regulations and as described in Sections 2.27 and 4.33 of this Agreement; |
| 2.12.9.56 | Require the provider to comply with 42 CFR Part 438, Managed care, including but not limited to 438.6(f)(2)(i), compliance with the requirements mandating provider identification of provider-preventable conditions as a condition of payment. At a minimum, this shall mean non-payment of provider-preventable conditions as well as appropriate reporting as required by the CONTRACTOR and TENNCARE; |
2.12.9.57 Specify provider actions to improve patient safety and quality;
| 2.12.9.58 | Provide general and targeted education to providers regarding emergency appeals, including when an emergency appeal is appropriate, and procedures for providing written certification thereof, and specify that the provider shall comply with the appeal process, including but not limited to the following: |
| 2.12.9.58.1 | Assist an enrollee by providing appeal forms and contact information including the appropriate address, telephone number and/or fax number for submitting appeals for state level review; and |
| 2.12.9.58.2 | Require in advance, that providers seek prior authorization, when they feel they cannot order a drug on the TennCare PDL as well as taking the initiative to seek prior authorization or change or cancel the prescription when contacted by an enrollee or pharmacy regarding denial of a pharmacy service due to system edits (e.g., therapeutic duplication, etc.); |
| 2.12.9.59 | Require the provider to coordinate with the TennCare PBM regarding authorization and payment for pharmacy services; |
| 2.12.9.60 | Specify any liquidated damages, sanctions or reductions in payment that the CONTRACTOR may assess on the provider for specific failures to comply with contractual and/or credentialing requirements. This shall include, but may not be limited to a provider’s failure or refusal to respond to the CONTRACTOR’s request for information, the request to provide medical records, credentialing information, etc.; at the CONTRACTOR’s discretion or a directive by TENNCARE, the CONTRACTOR shall impose financial consequences against the provider as appropriate; |
| 2.12.9.61 | Require that the provider display notices of the enrollee’s right to appeal adverse action affecting services in public areas of their facility(s) in accordance with TennCare rules and regulations, subsequent amendments, or any and all consent decrees and court orders. The CONTRACTOR shall ensure that providers have a correct and adequate supply of public notices; |
| 2.12.9.62 | Include language which informs providers of the package of benefits that TENNderCare offers and which requires providers to make treatment decisions based upon children’s individual medical and behavioral health needs. TENNderCare requirements are contained in Section 2.7.6 of this Agreement. All provider agreements shall contain language that references the TENNderCare requirements in this Agreement between TENNCARE and the CONTRACTOR, and the provider agreement shall either physically incorporate these sections of the Agreement or include language to require that these sections be furnished to the provider upon request; |
| 2.12.9.63 | Include a provision which states that providers are not permitted to encourage or suggest, in any way, that TennCare children be placed into state custody in order to receive medical, behavioral, or long-term care services covered by TENNCARE; |
| 2.12.9.64 | Require that providers offer hours of operation that are no less than the hours of operation offered to commercial enrollees; |
| 2.12.9.65 | Specify that the provider have written procedures for the provision of language interpretation and translation services for any enrollee who needs such services, including but not limited to, enrollees with Limited English Proficiency; |
| 2.12.9.66 | The provider shall not use TennCare’s name or trademark for any materials intended for dissemination to their patients unless said material has been submitted to TENNCARE by the CONTRACTOR for review and has been approved by TENNCARE in accordance with Section 2.17 of this Agreement. This prohibition shall not include references to whether or not the provider accepts TennCare; and |
| 2.12.9.67 | Require that if any requirement in the provider agreement is determined by TENNCARE to conflict with the Agreement between TENNCARE and the CONTRACTOR, such requirement shall be null and void and all other provisions shall remain in full force and effect. |
| 24. | Section 2.12.12.9 shall be amended by adding a new Section 2.12.12.9.3 which shall read as follows: |
| 2.12.12.9.3 | Communicating with hospitals, discharge planners or other institutions for the purposes of soliciting potential CHOICES members that should instead be referred to the person’s MCO or AAAD, as applicable; |
| 25. | Section 2.12.12.10 shall be amended by deleting the word “and” at the end of the sentence. |
| 26. | Section 2.12.12 shall be amended by adding new Sections 2.12.12.12 and 2.12.12.13 as follows: |
| 2.12.12.12 | Prohibit CHOICES providers from altering in any manner official CHOICES or MFP brochures or other CHOICES or MFP materials unless the CONTRACTOR has submitted a request to do so to TENNCARE and obtained prior written approval from TENNCARE in accordance with Section 2.17 of this Agreement; and |
| 2.12.12.13 | Prohibit CHOICES providers from reproducing for its own use the CHOICES or MFP logos unless the CONTRACTOR has submitted a request to do so to TENNCARE and obtained prior written approval from TENNCARE in accordance with Section 2.17 of this Agreement. |
| 27. | Section 2.13.1 shall be amended by deleting and replacing Section 2.13.1.5 and adding new Sections 2.13.1.6, 2.13.1.7 and 2.13.1.8 as follows: |
| 2.13.1.5 | The CONTRACTOR shall ensure that payments are not issued to providers that have not obtained a Tennessee Medicaid provider number or for which disclosure requirements, as applicable, have not been obtained by the CONTRACTOR in accordance with 42 CFR 455.100 through 106, Section 2.12.9.37 of this Agreement, and TennCare policies and procedures. |
| 2.13.1.6 | The CONTRACTOR, as well as its subcontractors and tax-reporting provider entities shall not be permitted to assign TennCare funds/payments to billing agents or alternative payees without executing a billing agent or alternative payee assignment agreement. The billing agents and alternative payees are subject to initial and monthly federal exclusion (LEIE) and debarment (EPLS) screening by the assignee if the alternative payee assignment is on-going. Further, direct and indirect payments to out of country individuals and/or entities are prohibited. |
| 2.13.1.7 | For any entities to which the CONTRACTOR makes payment via electronic transfers, the CONTRACTOR shall have a signed EFT form that shall have 42 CFR 455.18 and 455.19 statements immediately preceding the “Signature” section. |
| 2.13.1.8 | The CONTRACTOR’s failure to implement State Budget Reductions as described by TENNCARE may, at the discretion of TENNCARE, result in the CONTRACTOR forfeiting savings that would have been realized based on the timely implementation, including the forfeiture of recoupment from providers. |
| 28. | Section 2.14.1 shall be amended by deleting and replacing Section 2.14.1.1 and adding new Sections 2.14.1.2 through 2.14.1.4. The remaining Sections shall be renumbered accordingly, including any references thereto. |
| 2.14.1.1 | The CONTRACTOR shall develop and maintain a utilization management (UM) program which shall be documented in writing. As part of this program the CONTRACTOR shall have policies and procedures with defined structures and processes. The UM program shall assign responsibility to appropriate individuals including a designated senior physician and shall involve a designated behavioral health care practitioner in the implementation of behavioral health aspects of the program and a designated long-term care professional in the implementation of the long-term care aspects of the program. |
| 2.14.1.2 | The UM program shall be supported by an associated work plan and shall be evaluated annually and updated as necessary. |
| 2.14.1.3 | The UM program description, associated work plan, and annual evaluation of the UM program shall be submitted to TENNCARE (See Section 2.30.11.1). |
| 2.14.1.4 | The UM program, including the UM program description, associated work plan, and annual evaluation shall address Emergency Department (ED) utilization and ED diversion efforts.. |
| 29. | The renumbered Section 2.14.1.16.1 shall be deleted and replaced as follows: |
| 2.14.1.16.1 | Review ED utilization data, at a minimum, every six (6) months to identify members with utilization exceeding the threshold defined by TENNCARE as ten (10) or more visits in the defined six (6) month period. The review due March 31st shall cover ED utilization during the preceding July through December; the review due September 30th shall cover ED utilization during the preceding January through June (See Section 2.30.11.7). |
| 30. | Section 2.15.6.1 shall be amended by adding a new Section 2.15.6.1.1 and 2.15.6.1.2 which shall read as follows: |
| 2.15.6.1.1 | Beginning with HEDIS 2012, the CONTRACTOR shall utilize the Hybrid methodology (i.e., gathered from administrative and medical record data) as the data collection method for any Medicaid HEDIS measure containing Hybrid Specifications as identified by NCQA. |
| 2.15.6.1.2 | The CONTRACTOR shall submit to TENNCARE by June 15 of each calendar year a |
detailed explanation for any Medicaid HEDIS measure marked as “Not Reported”.
31. Section 2.15.7 shall be deleted and replaced as follows:
2.15.7 Critical Incident Reporting and Management
2.15.7.1 CHOICES Critical Incident Reporting and Management
| 2.15.7.1.1 | The CONTRACTOR shall develop and implement a critical incident reporting and management system for incidents that occur in a home and community-based long-term care service delivery setting, including: community-based residential alternatives; adult day care centers; other CHOICES HCBS provider sites; and a member’s home, if the incident is related to the provision of covered CHOICES HCBS. |
| 2.15.7.1.2 | The CONTRACTOR shall identify and track critical incidents and shall review and analyze critical incidents to identify and address potential and actual quality of care and/or health and safety issues. The CONTRACTOR shall regularly review the number and types of incidents (including, for example, the number and type of incidents across settings, providers, and provider types) and findings from investigations (including findings from APS and CPS if available); identify trends and patterns; identify opportunities for improvement; and develop and implement strategies to reduce the occurrence of incidents and improve the quality of CHOICES HCBS. |
| 2.15.7.1.3 | Critical incidents shall include but not be limited to the following incidents when they occur in a home and community-based long-term care service delivery setting (as defined in Section 2.15.7.1.1 above): |
| 2.15.7.1.3.1 2.15.7.1.3.2 2.15.7.1.3.3 2.15.7.1.3.4 2.15.7.1.3.5 2.15.7.1.3.6 2.15.7.1.3.7 |
Unexpected death of a CHOICES member; Suspected physical or mental abuse of a CHOICES member; Theft or financial exploitation of a CHOICES member; Severe injury sustained by a CHOICES member; Medication error involving a CHOICES member; Sexual abuse and/or suspected sexual abuse of a CHOICES member; and Abuse and neglect and/or suspected abuse and neglect of a CHOICES member. |
| 2.15.7.1.4 | The CONTRACTOR shall require its staff and contract CHOICES HCBS providers to report, respond to, and document critical incidents as specified by the CONTRACTOR. This shall include, but not be limited to the following: |
2.15.7.1.4.1 Requiring that the CONTRACTOR’s staff and contract CHOICES HCBS providers
report critical incidents to the CONTRACTOR in accordance with applicable requirements. The CONTRACTOR shall develop and implement a critical incident reporting process, including the form to be used to report critical incidents and reporting timeframes. The maximum timeframe for reporting an incident to the CONTRACTOR shall be twenty-four (24) hours. The initial report of an incident within twenty-four (24) hours may be submitted verbally, in which case the person/agency/entity making the initial report shall submit a follow-up written report within forty-eight (48) hours.
| 2.15.7.1.4.2 | Requiring that suspected abuse, neglect, and exploitation of members who are adults is immediately reported in accordance with TCA 71-6-103 and suspected brutality, abuse, or neglect of members who are children is immediately reported in accordance with TCA 37-1-403 or TCA 37-1-605 as applicable. |
| 2.15.7.1.4.3 | Requiring that its staff and contract CHOICES HCBS providers immediately (which shall not exceed twenty-four hours) take steps to prevent further harm to any and all members and respond to any emergency needs of members. |
| 2.15.7.1.4.4 | Requiring that contract CHOICES HCBS providers with a critical incident conduct an internal critical incident investigation and submit a report on the investigation within the timeframe specified by the CONTRACTOR. The timeframe for submitting the report shall be as soon as possible, may be based on the severity of the incident, and, except under extenuating circumstances, shall be no more than thirty (30) days after the date of the incident. The CONTRACTOR shall review the provider’s report and follow-up with the provider as necessary to ensure that an appropriate investigation was conducted and corrective actions were implemented within applicable timeframes. |
| 2.15.7.1.4.5 | Requiring that its staff and contract CHOICES HCBS providers cooperate with any investigation conducted by the CONTRACTOR or outside agencies (e.g., TENNCARE, APS, CPS, and law enforcement). |
| 2.15.7.1.4.6 | Defining the role and responsibilities of the fiscal employer agent (see definition in Section 1) in reporting, responding to, documenting, and investigating any critical incidents, which shall include reporting incidents to the CONTRACTOR using the process developed in a accordance with Section 2.15.7.1.4.1, investigating critical incidents, submitting a report on investigations to the CONTRACTOR and reporting to the CONTRACTOR within 24 hours in accordance with the abuse and neglect plan protocols anytime there is a suspicion of abuse or neglect (see Section 2.9.7.8.6); training employees, contractors of the FEA (including supports brokers), and consumer-directed workers regarding reporting, responding to, documenting, and cooperating with the investigation of any critical incidents; and training consumers and caregivers regarding critical incident reporting and management. Such role and responsibilities shall be defined in a manner that is consistent with requirements in this Section 2.15.7.1.4 as well as TENNCARE’s contract with the fiscal employer agent and the model contract between the CONTRACTOR and the FEA. |
| 2.15.7.1.4.7 | Reviewing the FEA’s reports and investigations regarding critical incidents and follow-up with the FEA as necessary regarding corrective actions determined by the member |
and/or his/her representative to help ensure the member’s health and safety.
| 2.15.7.1.4.8 | Providing appropriate training and taking corrective action as needed to ensure its staff, contract CHOICES HCBS providers, the FEA, and workers comply with critical incident requirements. |
| 2.15.7.1.4.9 | Conducting oversight, including but not limited to oversight of its staff, contract CHOICES HCBS providers, and the FEA, to ensure that the CONTRACTOR’s policies and procedures are being followed and that necessary follow-up is being conducted in a timely manner. |
2.15.7.2 Behavioral Health Adverse Occurrences
| 2.15.7.2.1 | Adverse occurrences shall include but not be limited to the following incidents when they occur while the member is in the care of a behavioral health inpatient, residential or crisis stabilization unit: |
| 2.15.7.2.1.1 2.15.7.2.1.2 2.15.7.2.1.3 2.15.7.2.1.4 2.15.7.2.1.5 2.15.7.2.1.6 2.15.7.2.1.7 2.15.7.2.1.8 2.15.7.2.1.9 |
Suicide death Non-suicide death Death-cause unknown Homicide Homicide Attempt with significant medical intervention Suicide Attempt with significant medical intervention Allegation of Abuse/Neglect (Physical, Sexual, Verbal) Accidental Injury with significant medical intervention Use of Restraints/Seclusion (Isolation) requiring significant medical intervention; or |
| 2.15.7.2.1.10 | Treatment complications (medication errors and adverse medication reaction) requiring significant medical intervention. |
| 2.15.7.3 | The CONTRACTOR shall report to TENNCARE any death and any incident that could significantly impact the health or safety of a member (e.g., physical or sexual abuse) within twenty-four (24) hours of detection or notification. |
2.15.7.4 As specified in Sections 2.30.12.7 and 2.30.12.8, the CONTRACTOR shall submit quarterly
reports to TENNCARE regarding all critical incidents and adverse occurrences.
| 32. | Section 2.15 shall be amended by adding a new Section 2.15.8 as follows: |
2.15.8 Provider Preventable Conditions
The CONTRACTOR shall comply with 42 CFR Part 438 requirements mandating provider identification of provider-preventable conditions as a condition of payment, as well as the prohibition against payment for provider-preventable conditions as set forth in 42 CFR §434.6(a)(12) and § 447.26. The CONTRACTOR shall submit all identified Provider Preventable Conditions in a form or frequency as described by TENNCARE.
| 33. | Section 2.16.2 shall be deleted and replaced as follows: |
| 2.16.2 | The prohibition on enrollee marketing shall not apply to health education and outreach activities (see Section 2.7.4) that are described in the CONTRACTOR’s TennCare approved Annual Community Outreach Plan. |
| 34. | Section 2.17.1.1 shall be deleted and replaced as follows: |
2.17.1.1 The CONTRACTOR shall submit to TENNCARE for review and prior written approval all
materials that will be distributed to members (referred to as member materials). This includes but is not limited to member handbooks, provider directories, member newsletters, identification cards, fact sheets, notices, brochures, form letters, mass mailings, system generated letters and any other additional, but not required, materials and information provided to members designed to promote health and/or educate members.
| 35. | Section 2.17.2.7 shall be amended by adding additional text as follows: |
2.17.2.7 All written member materials shall be made available in alternative formats for persons with
special needs at no expense to the member. Alternative formats may include, but may not be limited to: Braille, large print, and audio and shall be based on the needs of the individual enrollee. The CONTRACTOR shall have processes in place to ensure that alternative format material will be made available to the enrollee within forty five (45) days of a request;
| 36. | Section 2.17.4.7.7 shall be deleted in its entirety and the remaining Section shall be renumbered accordingly, including any references thereto. |
| 37. | Section 2.18.5.3 shall be amended by deleting and replacing Section 2.18.5.3.14 and adding a new Section 2.18.5.3.15 as follows. The remaining Section shall be renumbered accordingly, including any references thereto. |
| 2.18.5.3.14 | Information for CHOICES HCBS providers regarding prohibition of facilitating CHOICES referrals with the expectation of being selected as the service provider or petitioning existing CHOICES members to change CHOICES providers (See Section 2.12.12.9); |
| 2.18.5.3.15 | Requirements regarding the prohibition of the reproduction and/or use of CHOICES and MFP materials and logos (See Sections 2.12.12.12 and 2.12.12.13). |
| 38. | Section 2.18.6.3.16 shall be amended by adding “and behavioral health” as follows: |
| 2.18.6.3.16 | Critical incident reporting and management for CHOICES HCBS and behavioral health providers; |
| 39. | Section 2.18.6 shall be amended by adding a new Section 2.18.6.9 and renumbering the remaining Section accordingly including any references thereto. |
| 2.18.6.9 | The CONTRACTOR shall provide documented and routine education and training to providers regarding proper billing. |
| 40. | Section 2.20.1 shall be deleted and replaced as follows and all references shall be updated accordingly. |
2.20.1 General
2.20.1.1 The Tennessee Bureau of Investigation, Medicaid Fraud Control Unit (TBI MFCU) is the
state agency responsible for the investigation of provider fraud and abuse in the TennCare program.
| 2.20.1.2 2.20.1.3 |
The Office of Inspector General (OIG) has the primary responsibility to investigate TennCare enrollee fraud and abuse. The CONTRACTOR shall have surveillance and utilization control programs and procedures |
(42 CFR 456.3, 456.4, 456.23) to safeguard the Medicaid funds against unnecessary or inappropriate use of Medicaid services and against improper payments. The CONTRACTOR shall have internal controls and policies and procedures in place that are designed to prevent, detect, and report known or suspected fraud and abuse activities.
2.20.1.4 The CONTRACTOR, as well as its subcontractors and providers, whether contract or non-
contract, shall comply with all federal requirements (42 CFR Part 455) on disclosure reporting. All tax-reporting provider entities that bill and/or receive TennCare funds as the result of this Agreement shall submit routine disclosures in accordance with timeframes specified in 42 CFR Part 455, Subpart B and TennCare policies and procedures, including at the time of initial contracting, contract renewal, at any time there is a change to any of the information on the disclosure form, at least once every three (3) years, and at anytime upon request.
2.20.1.5 The CONTRACTOR, as well as its subcontractors and providers, whether contract or non-
contract, shall comply with all federal requirements (42 C.F.R. § 1002) on exclusion and debarment screening. All tax-reporting provider entities that bill and/or receive TennCare funds as the result of this Agreement shall screen their owners and employees against the federal exclusion databases (such as LEIE and EPLS). Any unallowable funds made to excluded individuals as full or partial wages and/or benefits shall be refunded to and/or obtained by the State and/or the CONTRACTOR dependent upon the entity that identifies the payment of unallowable funds to excluded individuals.
2.20.1.6 The CONTRACTOR shall have adequate staffing and resources to investigate unusual
incidents and develop and implement corrective action plans to assist the CONTRACTOR in preventing and detecting potential fraud and abuse activities.
| 2.20.1.7 | The CONTRACTOR is prohibited from the repayment of funds paid by the CONTRACTOR to any provider when the issues, services or claims upon which the repayment is based meets one or more of the following: |
| 2.20.1.7.1 | Have been obtained by the State of Tennessee, either by TENNCARE directly or as part of a resolution of a state or federal investigation and/or lawsuit, including but not limited to false claims act cases; or |
2.20.1.7.2 Have been obtained by the States Recovery Audit Contractor (RAC) contractor; or
| 2.20.1.7.3 | When the issue, services or claims that are the basis of the repayment are currently being investigated by the State of Tennessee, are the subject of pending Federal or State litigation, or are being audited by the TennCare RAC. |
2.20.1.8 This prohibition described above in Section 2.20.1.7 shall be limited to a specific provider(s),
for specific dates, and for specific issues, services or claims. The CONTRACTOR shall check with the Bureau of TennCare, Program Integrity Unit before initiating any repayment of any program integrity related funds (See Section 2.20.1.7) to ensure that the repayment is permissible. In the event that the CONTRACTOR obtains funds in cases where repayment is prohibited under this section, the CONTRACTOR will return the funds to the provider.
2.20.1.9 The CONTRACTOR shall comply with all federal and state requirements regarding fraud
and abuse, including but not limited to Sections 1128, 1156, and 1 902(a)(68) of the Social Security Act.
| 41. | Section 2.20.2 shall be amended by adding the word “,subcontractors” after the word “CONTRACTOR” in Section 2.20.2.9 and by adding a new Section 2.20.2.13 as follows: |
| 2.20.2.13 | In accordance with the Affordable Care Act and TennCare policy and procedures, the CONTRACTOR shall report overpayments made by TENNCARE to the CONTRACTOR as well as overpayments made by the CONTRACTOR to a provider and/or subcontractor (See Section 2.12.9.36 and Section 3.16.5.1). |
| 42. | Sections 2.20.3.2.7 and 2.20.3.2.8 shall be amended by adding the word “Include” to the beginning of the sentence and change the following word “A” to “a”. |
| 43. | Section 2.20.3.2 shall be amended by adding new Sections 2.20.3.2.2 and 2.20.3.2.14 as follows and renumbering the remaining Section accordingly, including any references thereto. |
| 2.20.3.2.2 | Include a risk assessment of the CONTRACTOR’s various fraud and abuse/program integrity processes. A risk assessment shall also be submitted on an ‘as needed’ basis and immediately after a program integrity related action, including financial-related actions (such as overpayment, repayment and fines), is issued on a provider with concerns of fraud and abuse. The CONTRACTOR shall inform TENNCARE of such action and provide details of such financial action. The assessment shall also include a listing of the CONTRACTOR’s top three vulnerable areas and shall outline action plans in mitigating such risks; |
| 2.20.3.2.14 | Include work plans for conducting both announced and unannounced site visits and field audits to providers defined as high risk (providers with cycle/auto billing activities, providers offering DME, home health, mental health, and transportation services) to ensure services are rendered and billed correctly. |
| 44. | The renumbered Section 2.20.3.2.12 shall be amended by deleting the word “and” at the end of the sentence and the renumbered Section 2.20.3.2.13 shall be amended by deleting “.” and adding “; and” to the end of the sentence. |
| 45. | Section 2.20.3.6 shall be amended as follows: |
2.20.3.6 The CONTRACTOR shall have provisions in its Compliance Plan regarding conducting
monthly comparison of their provider files, including atypical providers, against both the Excluded Parties List System (EPLS) and the HHS-OIG List of Excluded Individuals/Entities (LEIE) and provide a report of the result of comparison to TENNCARE each month. The CONTRACTOR shall establish an electronic database to capture identifiable information on the owners, agents and managing employees listed on providers’ Disclosure forms.
| 46. | Section 2.22.2.1 shall be deleted and replaced as follows: |
2.22.2.1 The CONTRACTOR shall maintain a claims management system that can uniquely identify
the provider of the service (ensuring all billing information related to tax-reporting business entities and information related to individuals who provide services are properly reported on claims), date of receipt (the date the CONTRACTOR receives the claim as indicated by a date-stamp), real-time-accurate history of actions taken on each provider claim (i.e., paid, denied, suspended, appealed, etc.), date of payment (the date of the check or other form of payment) and all data elements as required by TENNCARE for encounter data submission (see Section 2.23), and can track and report service use against benefit limits in accordance with a methodology set by TENNCARE.
| 47. | Section 2.22.2 shall be amended by adding a new Section 2.22.2.6 as follows and renumbering the remaining Section accordingly, including any references thereto. |
2.22.2.6 For any entities to which the CONTRACTOR makes payment via electronic transfers, the
CONTRACTOR shall have a signed EFT form that shall have 42 CFR 455.18 and 455.19 statements immediately preceding the “Signature” section.
| 48. | Section 2.22 shall be amended by adding a new Section 2.22.7 as follows and renumbering the remaining Section accordingly, including any references thereto. |
2.22.7 Monthly Focused Claims Testing
2.22.7.1 In addition to the claims payment accuracy testing procedures described in Section 2.22.6, the
CONTRACTOR shall perform a monthly self test on the accuracy of claims processing based on claims judgmentally selected by TDCI. The maximum number of claims selected by TDCI each month will not exceed twenty-five (25), unless TDCI, at its discretion, determines a larger sample is warranted based on the results of the accuracy tests. The results reported by the CONTRACTOR are not intended to represent the percentage of compliance or noncompliance for the total population of claims processed by the CONTRACTOR or subcontractors.
2.22.7.2 The monthly focused claims testing procedures include:
| 2.22.7.2.1 | The CONTRACTOR shall complete the attribute sheets provided by TDCI for each claim to be tested within thirty (30) calendar days of receipt from TDCI. |
2.22.7.2.2 The CONTRACTOR shall submit a plan of correction as requested by TDCI.
| 49. | The renumbered Section 2.22.8 shall be amended by adding a new Section 2.22.8.3 as follows and renumbering the remaining Section accordingly including any references thereto. |
2.22.8.3 Identify improper payments made to invalid, missing, and/or mismatched NPIs, and/or
TINs/EINs.
| 50. | Section 2.24.4.2.4 shall be amended by deleting the reference to “Section 2.15.7.4” and replacing it with “Section 2.15.7.1.4”. |
| 51. | Section 2.26.11 shall be deleted and replaced as follows: |
2.26.11 Assignability
| 2.26.11.1 | Transportation and claims processing subcontracts shall include language requiring that the subcontract agreement shall be assignable from the CONTRACTOR to the State, or its designee: i) at the State’s discretion upon written notice to the CONTRACTOR and the affected subcontractor; or ii) upon CONTRACTOR’s request and written approval by the State. Further, the subcontract agreement shall include language by which the subcontractor agrees to be bound by any such assignment, and that the State, or its designee, shall not be responsible for past obligations of the CONTRACTOR. |
| 2.26.11.2 | Subcontractors shall not be permitted to assign TennCare funds/payments to billing agents or alternative payees without executing a billing agent or alternative payee assignment agreement. The billing agents and alternative payees are subject to initial and monthly federal exclusion (LEIE) and debarment (EPLS) screening by the assignee if the alternative payee assignment is on-going. Further, direct and indirect payments to out of country individuals and/or entities are prohibited. |
| 52. | Section 2.27 shall be deleted and replaced as follows: |
| 2.27 COMPLIANCE WITH HEALTH INSURANCE PORTABILITY AND ACCOUNTABILITY ACT (HIPAA) AND HEALTH INFORMATION | ||
| TECHNOLOGY FOR ECONOMIC AND CLINICAL HEALTH ACT (HITECH) | ||
| 2.27.1 TENNCARE and the CONTRACTOR shall comply with obligations under the Health Insurance Portability and | ||
| Accountability Act of 1996 (HIPAA) and Health Information Technology for Economic and Clinical Health Act (HITECH) | ||
| under the American Recovery and Reinvestment Act of 2009 (ARRA) and their accompanying regulations, and as amended. | ||
| 2.27.2 The CONTRACTOR warrants to TENNCARE that it is familiar with the requirements of HIPAA and HITECH and their | ||
| accompanying regulations, and shall comply with all applicable HIPAA and HITECH requirements in the course of this | ||
| Agreement including but not limited to the following: | ||
| 2.27.2.1 2.27.2.2 2.27.2.3 2.27.2.4 2.27.2.5 |
Compliance with the Privacy Rule, Security Rule, and Notification Rule; The creation of and adherence to sufficient Privacy and Security Safeguards and Policies; Timely Reporting of Violations in the Access, Use and Disclosure of PHI; and Timely Reporting of Privacy and/or Security Incidents. Failure to comply may result in actual damages that the State incurs as a result of the breach |
|
and liquidated damages in accordance with Section 4.20.
| 2.27.3 | The CONTRACTOR warrants that it shall cooperate with TENNCARE, including cooperation and coordination with TENNCARE privacy officials and other compliance officers required by HIPAA and HITECH and their accompanying regulations, in the course of performance of the Agreement so that both parties will be in compliance with HIPAA and HITECH. |
| TENNCARE and the CONTRACTOR shall sign documents, including, but not limited to, business associate agreements, as required by HIPAA and HITECH, that are reasonably necessary to keep TENNCARE and the CONTRACTOR in compliance with HIPAA and HITECH. |
| 2.27.4 | As a party to this Agreement, the CONTRACTOR hereby acknowledges its designation as a covered entity and/or business associate under the HIPAA regulations and agrees to comply with all applicable HIPAA and HITECH (hereinafter “HIPAA/HITECH”) regulations. |
| 2.27.5 | In accordance with HIPAA/HITECH regulations, the CONTRACTOR shall, at a minimum: |
| 2.27.5.1 | Comply with requirements of the Health Insurance Portability and Accountability Act of 1996 and the Health Information Technology for Economic and Clinical Health Act of 2009 (HITECH), including, but not limited to, the transactions and code sets, privacy, security, and identifier regulations, by their designated compliance dates. Compliance includes meeting all required transaction formats and code sets with the specified data sharing agreements required under the regulations; |
| 2.27.5.2 | Transmit/receive from/to its providers, subcontractors, clearinghouses and TENNCARE all transactions and code sets required by the HIPAA/HITECH regulations in the appropriate standard formats, utilizing appropriate and adequate safeguards, as specified under the law and as directed by TENNCARE so long as TENNCARE direction does not conflict with the law; |
| 2.27.5.3 | Agree that if it is not in compliance with all applicable standards defined within the transactions and code sets, privacy, security and all subsequent HIPAA/HITECH standards, that it will be in breach of this Agreement and will then take all reasonable steps to cure the breach or end the violation as applicable. Since inability to meet the transactions and code sets requirements, as well as the privacy and security requirements can bring basic business practices between TENNCARE and the CONTRACTOR and between the CONTRACTOR and its providers and/or subcontractors to a halt, if for any reason the CONTRACTOR cannot meet the requirements of this Section, TENNCARE may terminate this Agreement in accordance with the Business Associate Agreement ancillary to this Agreement; |
| 2.27.5.4 | Ensure that Protected Health Information (PHI) exchanged between the CONTRACTOR and TENNCARE is used only for the purposes of treatment, payment, or health care operations and health oversight and its related functions. All PHI not transmitted for these purposes or for purposes allowed under the federal HIPAA/HITECH regulations shall be de-identified to secure and protect the individual enrollee’s PHI; |
| 2.27.5.5 | Report to TENNCARE’s Privacy Office immediately upon becoming aware of any use or disclosure of PHI in violation of this Agreement by the CONTRACTOR, its officers, directors, employees, subcontractors or agents or by a third party to which the CONTRACTOR disclosed PHI; |
2.27.5.6 Specify in its agreements with any agent or subcontractor that will have access to PHI that
such agent or subcontractor agrees to be bound by the same restrictions, terms and conditions that apply to the CONTRACTOR pursuant to this Section;
2.27.5.7 Make available to TENNCARE enrollees the right to amend their PHI in accordance with the
federal HIPAA regulations. The CONTRACTOR shall also send information to enrollees educating them of their rights and necessary steps in this regard;
| 2.27.5.8 2.27.5.9 |
Make an enrollee’s PHI accessible to TENNCARE immediately upon request by TENNCARE; Make its internal policies and procedures, records and other documentation related to the use |
and disclosure of PHI available to the U.S. Secretary of Health and Human Services for the purposes of determining compliance with the HIPAA/HITECH regulations upon request;
| 2.27.5.10 | Create and adopt policies and procedures to periodically audit adherence to all HIPAA/HITECH regulations, and for which CONTRACTOR acknowledges and promises to perform, including but not limited to, the following obligations and actions: |
| 2.27.5.10.1 | Agree to ensure that any agent, including a subcontractor, to whom it provides PHI that was created, received, maintained, or transmitted on behalf of TENNCARE agrees to use reasonable and appropriate safeguards to protect the PHI. |
| 2.27.5.11 | If feasible, return or destroy all PHI, in whatever form or medium (including any electronic medium) and all copies of an any data or compilations derived from and allowing identification of any individual who is a subject of that PHI upon termination, cancellation, expiration or other conclusion of the Agreement, and in accordance with this Section of this Agreement. The CONTRACTOR shall complete such return or destruction as promptly as possible, but not later than thirty (30) days after the effective date of the termination, cancellation, expiration or other conclusion of the Agreement. The CONTRACTOR shall identify any PHI that cannot feasibly be returned or destroyed. Within such thirty (30) days after the effective date of the termination, cancellation, expiration or other conclusion of the Agreement, the CONTRACTOR shall: (1) certify on oath in writing that such return or destruction has been completed; (2) identify any PHI which cannot feasibly be returned or destroyed; and (3) certify that it will only use or disclose such PHI for those purposes that make its return or destruction infeasible; |
| 2.27.5.12 | Implement all appropriate administrative, physical and technical safeguards to prevent the use or disclosure of PHI other than pursuant to the terms and conditions of this Agreement and, including, but not limited to, privacy, security and confidentiality requirements in 45 CFR Parts 160 and 164; |
| 2.27.5.13 | Set up appropriate mechanisms to limit use or disclosure of PHI to the minimum necessary to accomplish the intended purpose of the use or disclosure; |
| 2.27.5.14 | Create and implement policies and procedures to address present and future HIPAA/HITECH regulatory requirements as needed, including, but not limited to: use and disclosure of data; de-identification of data; minimum necessary access; accounting of disclosures; enrollee’s right to amend, access, request restrictions; notice of privacy practices and right to file a complaint; |
| 2.27.5.15 | Provide an appropriate level of training to its staff and employees regarding HIPAA/HITECH-related policies, procedures, enrollee rights and penalties prior to the HIPAA/HITECH implementation deadlines and at appropriate intervals thereafter; |
| 2.27.5.16 | Track training of CONTRACTOR staff and employees and maintain signed acknowledgements by staff and employees of the CONTRACTOR’s HIPAA/HITECH policies; |
| 2.27.5.17 | Be allowed to use and receive information from TENNCARE where necessary for the management and administration of this Agreement and to carry out business operations where permitted under the regulations; |
2.27.5.18 Be permitted to use and disclose PHI for the CONTRACTOR’s own legal responsibilities;
| 2.27.5.19 | Adopt the appropriate procedures and access safeguards to restrict and regulate access to and use by CONTRACTOR employees and other persons performing work for the CONTRACTOR to have only minimum necessary access to PHI and personally identifiable data within their organization; |
| 2.27.5.20 | Continue to protect and secure PHI AND personally identifiable information relating to enrollees who are deceased; |
| 2.27.5.2 | 1 Be responsible for informing its enrollees of their privacy rights in the manner specified under the regulations; |
2.27.5.22 Make available PHI in accordance with 45 CFR 164.524;
| 2.27.5.23 | Make available PHI for amendment and incorporate any amendments to PHI in accordance with 45 CFR 164.526; and |
| 2.27.5.24 | Obtain a third (3rd) party certification of their HIPAA transaction compliance ninety (90) calendar days before the start date of operations. |
| 2.27.6 | The CONTRACTOR shall track all security incidents as defined by HIPAA/HITECH, and, as required by the HIPAA/HITECH Reports. The CONTRACTOR shall periodically report in summary fashion such security incidents. |
| 2.27.7 | TENNCARE and the CONTRACTOR are “information holders” as defined in TCA 47-18-2107. In the event of a breach of the security of CONTRACTOR’s information system, as defined by TCA 47-18- 2 107, the CONTRACTOR shall indemnify and hold TENNCARE harmless for expenses and/or damages related to the breach. Such obligations shall include, but not be limited to, mailing notifications to affected enrollees. Substitute notice to written notice, as defined by TCA 47-18-21 07(e)(2)and(3), shall only be permitted with TENNCARE’s express written approval. The CONTRACTOR shall notify |
TENNCARE’s Privacy Office immediately upon becoming aware of any security incident that would constitute a “breach of the security of the system” as defined in TCA 47-18-2 107.
| 2.27.8 NOTIFICATION OF BREACH & NOTIFICATION OF PROVISIONAL BREACH. The CONTRACTOR shall notify TENNCARE’s Privacy Office immediately upon becoming aware of any incident, either confirmed or provisional, that represents or may represent unauthorized access, use or disclosure of encrypted or unencrypted computerized data that materially compromises the security, confidentiality, or integrity of enrollee PHI maintained or held by the CONTRACTOR, including any unauthorized acquisition of enrollee PHI by an employee or otherwise authorized user of the CONTRACTOR’s system. This includes, but is not limited to, loss or suspected loss of remote computing or telework devices such as laptops, PDAs, Blackberrys or other Smartphones, USB drives, thumb drives, flash drives, CDs, and/or disks. |
| 53. | Section 2.28.2 and 2.28.3 shall be deleted and replaced as follows: |
| 2.28.2 | In order to demonstrate compliance with federal and state regulations of Title VI of the Civil Rights Act of 1964, Section 504 of the Rehabilitation Act of 1973, Title II of the Americans with Disabilities Act of 1990, the Age Discrimination Act of 1975 and the Omnibus Budget Reconciliation Act of 1981 (P.L. 97- 35), the Church Amendments (42 U.S.C. 300a-7), Section 245 of the Public Health Service Act (42 U.S.C. 238n.), and the Weldon Amendment (Consolidated Appropriations Act 2008, Public Law 110-161, Div. G, Sec. 508 (d), 121 Stat. 1844, 2209), the CONTRACTOR shall designate a staff person to be responsible for non-discrimination compliance as required in Section 2.29.1. |
2.28.2.1 This person shall develop a CONTRACTOR non-discrimination compliance training plan
within thirty (30) days of the implementation of this Agreement, to be approved by the Bureau of TennCare. This person shall be responsible for the provision of instruction regarding the plan to all CONTRACTOR staff within sixty (60) days of the implementation of this Agreement. This person shall be responsible for the provision of instruction regarding the plan to providers and direct service subcontractors within ninety (90) days of the implementation of this Agreement. The CONTRACTOR shall be able to show documented proof of such instruction.
| 2.28.3 | The CONTRACTOR’s non-discrimination compliance plan shall include written policies and procedures that demonstrate non-discrimination in the provision of services to members. The policy shall also demonstrate non-discrimination in the provision of services for members with Limited English Proficiency and those requiring communication assistance in alternative formats (see Section 2.18.2). These policies and procedures shall be prior approved in writing by TENNCARE. |
| 54. | Section 2.30.3 shall be deleted and replaced as follows: |
2.30.3 Annual Community Outreach Plan
The CONTRACTOR shall submit an Annual Community Outreach Plan no later than November 30 of each year for review and approval by TENNCARE. The Annual Community Outreach Plan shall be written in accordance with guidance prepared by TENNCARE. It shall include, but is not limited to: all proposed community/health education events related to TENNderCare; community/health education events unrelated to TENNderCare; rationale for participating in these events; and a process for evaluating the benefits of the events.
| 55. | Section 2.30.6 shall be amended by adding a new Section 2.30.6.8 as follows and renumbering the remaining Section accordingly, including any references thereto. |
| 2.30.6.8 | Beginning April 2012, the CONTRACTOR shall submit a monthly CHOICES Caseload and Staffing Ratio Report. |
| 2.30.6.8.1 | The report shall reflect the weighted care coordinator-to-CHOICES member staffing ratios and care coordinator caseloads on the last business day of the month prior to the report submission (e.g. the report submitted in April 2012 will reflect the weighted caseloads and staffing ratios as they appeared on March 31, 2012); |
2.30.6.8.2 The report shall include at a minimum;
2.30.6.8.2.1 The weighted average care coordinator-to CHOICES member staffing ratio; and
2.30.6.8.2.2 The weighted caseload of CHOICES member assignments to each individual care coordinator.
| 56. | Section 2.30 shall be amended by adding a new Section 2.30.7 “LEFT BLANK INTENTIONALLY”, renumbering the remaining Section accordingly including any references thereto and by deleting and replacing the renumbered Section 2.30.9 as “LEFT BLANK INTENTIONALLY. |
| 57. | The renumbered Section 2.30.11.2 shall be deleted and replaced as follows: |
| 2.30.11.2 | The CONTRACTOR shall submit quarterly Cost and Utilization Reports. These reports shall be in an Excel spreadsheet format and submitted with a ninety (90) day lag and shall be due to TENNCARE one hundred twenty (120) calendar days following the quarter for which the CONTRACTOR is reporting. These reports shall be submitted on both a cumulative year basis and on a rolling twelve (12) month basis. |
| 58. | The renumbered Section 2.30.11.7 shall be deleted and replaced as follows: |
| 2.30.11.7 | The CONTRACTOR shall submit a semi-annual Emergency Department Threshold Report (See Section 2.14.1.16.1) to TENNCARE no later than March 31st and September 30th each year identifying interventions initiated for members who exceeded the defined threshold for ED usage. |
| 59. | The renumbered Section 2.30.12 shall be amended by adding a new Section 2.30.12.5 as follows and renumbering the remaining Sections accordingly, including any references thereto. |
| 2.30.12.5 | The CONTRACTOR shall submit to TENNCARE by June 15 of each calendar year a detailed explanation for any Medicaid HEDIS measure marked as “Not Reported”. |
| 60. | The renumbered Section 2.30.12 shall be amended by adding a new Section 2.30.12.8 as follows and renumbering the remaining Sections accordingly, including any references thereto. |
| 2.30.12.8 | The CONTRACTOR shall submit a quarterly Behavioral Health Adverse Occurrences Report in accordance with Section 2.15.7.2 that provides information, by month regarding specified measures, which shall include but not be limited to the following: |
2.30.12.8.1 The number of adverse occurrences, overall and by:
2.30.12.8.1.1 Date of occurrence
2.30.12.8.1.2 Type of adverse occurrence;
2.30.12.8.1.3 Location;
2.30.12.8.1.4 Provider name; and
2.30.12.8.1.5 Action Taken by Facility/Provider.
| 61. | The renumbered Section 2.30.15.4 shall be deleted in its entirety and replaced as follows: |
| 2.30.15.4 | Effective July 1, 2012, the CONTRACTOR shall submit a quarterly Disclosure Submission Rate report which shall provide the percentage of providers for which the CONTRACTOR has obtained a complete and current disclosure form in accordance with 42 CFR 455, TennCare policies and procedures, and this Agreement (see Section 2.12.9.37). The rate shall be provided for all tax-reporting entities with billing activities during the prior quarter. The quarterly report shall include a companion listing which shall include all tax-reporting entities with reimbursement amounts received in the prior reporting quarter along with the disclosure status. For all subcontractors and providers with a signed contract and/or with billing activities, the CONTRACTOR shall maintain a minimum of ninety-five percent (9 5%) compliance on all entities excluding providers who bill under emergency provisions. Should the CONTRACTOR attain a disclosure rate below ninety-five percent (95%), the CONTRACTOR shall be subject to liquidated damages and shall submit a corrective action plan that shall address the root causes of the non–compliance. |
| 62. | The renumbered Section 2.30.15.5 shall be amended as follows: |
| 2.30.15.5 | The CONTRACTOR shall submit a monthly Program Integrity Exception List report that identifies employees or contractors (as defined in Section 2.21.9) that have been reported on the HHS-OIG LEIE (List of Excluded Individuals/Entities) (http://oig.hhs.gov/fraud/exclusions/exclusions—list.asp), the Excluded Parties List System (EPLS), and/or the listing of Monthly Disciplinary Actions issued by the Professional Health Board. |
| 63. | The renumbered Section 2.30.17 shall be amended by adding a new Section 2.30.17.2 and the renumbered Section 2.30.17.4 shall be amended by adding the phrase “number of adjustments (including repayments),” as follows. The remaining Section shall be renumbered accordingly including any references thereto. |
| 2.30.17.2 | The CONTRACTOR shall submit a monthly Focused Claims Testing Report. The report shall include the results of the self test on the accuracy of claims processing based on claims that have been judgmentally selected by TDCI (see Section 2.22.7). The CONTRACTOR shall complete the attribute sheets provided by TDCI for each claim to be tested within thirty (30) calendar days of receipt from TDCI. |
| 2.30.17.4 | The CONTRACTOR shall submit a weekly Claims Activity Report. This report shall identify the number of claims received, number of claims denied (by reason), number of claims paid, number of adjustments (including repayments), and total amount paid by the categories of service specified by TENNCARE. |
| 64. | The renumbered Section 2.30.2 1 shall be deleted and replaced as follows: |
2.30.21 HIPAA/HITECH Reports
The CONTRACTOR shall submit a Privacy/Security Incident Report. This report shall be provided at least annually, but the CONTRACTOR shall provide the report more frequently if requested by TENNCARE. The report shall include, at a minimum, the date of the incident, the date of notification to TENNCARE’s privacy officer, the nature and scope of the incident, the CONTRACTOR’s response to the incident, and the mitigating measures taken by the CONTRACTOR to prevent similar incidents in the future. Upon TENNCARE’s request, the CONTRACTOR shall provide additional details within a reasonable amount of time. “Port scans” or other unsuccessful queries to the CONTRACTOR’s information system shall not be considered a privacy/security incident for purposes of this report.
| 65. | Section 3.9.2.5 and 3.9.2.6 shall be deleted and replaced as follows: |
3.9.2.5 If TENNCARE has determined the CONTRACTOR is not in compliance with a requirement
of this Agreement in any given month, TENNCARE may issue a written notice of deficiency and TENNCARE may retain the amount withheld for the month prior to TENNCARE identifying the compliance deficiencies.
3.9.2.6 The withhold amounts for subsequent months thereafter in which the CONTRACTOR has
not cured the deficiencies may at TENNCARE’s discretion be applied in accordance with Section 3.9.2.1 as described above. If the CONTRACTOR has attained a two and one half percent (2.5%) withhold and TENNCARE subsequently determines the CONTRACTOR is not in compliance with a requirement of this Agreement, TENNCARE may provide written notice of such determination and TENNCARE may, at the discretion of TENNCARE, reinstitute the retention of the withhold as described in Section 3.9.2.1 at the next capitation payment cycle. Monthly retention of the withhold amount may continue for each subsequent month so long as the identified deficiencies have not been corrected. These funds may not be distributed to the CONTRACTOR unless it is determined by TENNCARE the CONTRACTOR has come into compliance with the Agreement requirement(s) within six (6) months of TENNCARE identifying these deficiencies. For example, if a specified deficiency(s) is corrected within four (4) months and there are no other identified deficiencies
which the CONTRACTOR has been given written notice of by TENNCARE, the withhold for the four (4) consecutive months will be paid to the CONTRACTOR upon TENNCARE determination that the deficiency(s) was corrected. However, any amounts withheld by TENNCARE for six (6) consecutive months for the same or similar compliance deficiency(s) may be permanently retained by TENNCARE on the first day after the sixth consecutive month period and may not be paid to the CONTRACTOR. If the same or similar specified deficiency(s) continues beyond six (6) consecutive months, TENNCARE may declare the MCO ineligible for future distribution of the ten percent (10%) incentive withhold and may continue to permanently retain any amounts withheld by TENNCARE for six (6) consecutive months. Such ineligibility will continue for each month TENNCARE determines the same or similar specified deficiency(s) continues to exist. Once a CONTRACTOR corrects the deficiency(s), TENNCARE may reinstate the MCO’s eligibility for distribution of the ten percent (10%) compliance incentive payment of future withholds. If TENNCARE determines that distribution of the ten percent (10%) withhold is appropriate, distribution of the ten percent (10%) shall be made at the time of the next scheduled monthly check write which includes all other payments due the CONTRACTOR.
| 66. | Section 3.16.1.1 shall be deleted and replaced as follows: |
3.16.1.1 In no event shall the maximum liability of the State under this Agreement during the original
term of the Agreement exceed five billion, one hundred eighty five million, three hundred sixty eight thousand, four hundred eighty dollars ($5,185,368,480.00).
| 67. | Section 3.16.5 shall be amended by adding a new Section 3.16.5.1 as follows and renumbering the remaining Section accordingly, including any references thereto. |
3.16.5 Return of Funds and Deductions
3.16.5.1 In accordance with the Affordable Care Act and TennCare policy and procedures, the
CONTRACTOR shall report overpayments and, when it is applicable, return overpayments to TENNCARE within sixty (60) days from the date the overpayment is identified by the CONTRACTOR. Overpayments that are not returned within sixty (60) days from the date the overpayment was identified by the CONTRACTOR may result in a penalty pursuant to state or federal law.
| 3.16.5.2 | The CONTRACTOR shall refund to TENNCARE any overpayments due or funds disallowed pursuant to this Agreement within thirty (30) calendar days of the date of written notification from TENNCARE, unless otherwise authorized by TENNCARE in writing. |
3.16.5.2 The State reserves the right to deduct from amounts which are or shall become due and
payable to the CONTRACTOR under this or any Agreement or contract between the CONTRACTOR and the State of Tennessee any amounts which are or shall become due and payable to the State of Tennessee by the CONTRACTOR.
| 68. | Section 4.3 shall be amended by adding a new Section 4.3.2 as follows and renumbering the remaining Section 4.3 accordingly, including any references thereto. |
| 4.3.2 | 42 CFR Part 438, Managed care, including but not limited to 438.6(f)(2)(i), compliance with the requirements mandating provider identification of provider-preventable conditions as a condition of payment, as well as the prohibition against payment for provider-preventable conditions as set forth in §434.6(a)(1 2) and § 447.26 of this subchapter. |
| 69. | Section 4.4.8.2 shall be amended by adding a new Section 4.4.8.2.7 as follows and renumbering the remaining Section accordingly, including any references thereto. |
| 4.4.8.2.7 | Promptly make available all signed provider agreements/contracts, including historical agreements/contracts, to TENNCARE in PDF format. (The CONTRACTOR shall have the option to submit said agreements on an on-going basis during the term of this Agreement rather than at the end of this Agreement). Upon termination of this Agreement and completion of the CONTRACTOR’s continuing obligations, the State will reserve all rights to pursue improper payments and false claims with the CONTRACTOR and/or directly with the CONTRACTOR’s subcontractors and providers. |
| 70. | Section 4.20.2.2.6 shall be amended by adding a new Section 4.20.2.2.6.1 as follows: |
| 4.20.2.2.6 | TENNCARE reserves the right to assess a general liquidated damage of five hundred dollars ($500) per occurrence with any notice of deficiency. |
4.20.2.2.6.1 In circumstances for which TENNCARE has applied this general liquidated damage to a
notice of a deficiency that is related in any way to CHOICES care coordination processes and requirements which shall be determined by TENNCARE, the amounts shall be multiplied by two (2) when the CONTRACTOR has not complied with the Caseload and Staffing recommendations as specified in Section 2.9.6.11.9 of this Agreement.
| 71. | Sections 4.20.2.2.7, Items A.16, A.18, A.19,.A.20, A.21, A.22, A.23, the renumbered Items A.28, A.29, A.30, A.31, and Item C.7 shall be amended by adding a new paragraph to the end of the existing text in the Damage column as follows: |
“These amounts shall be multiplied by two (2) when the CONTRACTOR has not complied with the Caseload and Staffing recommendations as specified in Section 2.9.6.11.9 of this Agreement.”
| 72. | Section 4.20.2.2.7 shall be amended by deleting and replacing Items A.23 through A.26 and adding a new Item A.27 as follows and renumbering the remaining Items. |
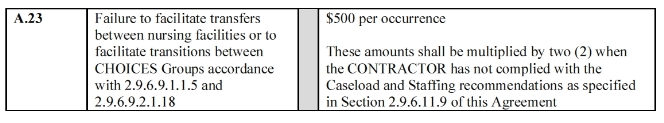
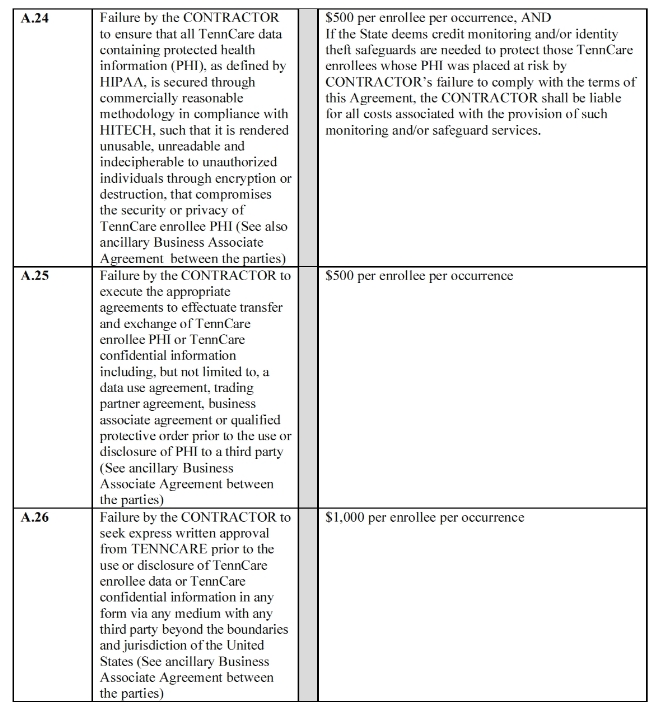
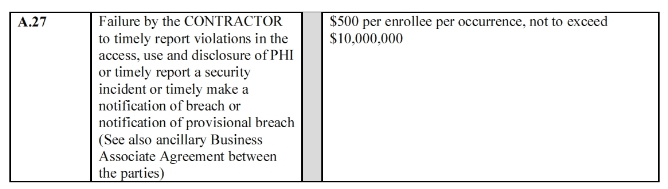
| 73. | Section 4.20.2.2.7 shall be amended by deleting and replacing Items B.15 and B.21 as follows: |
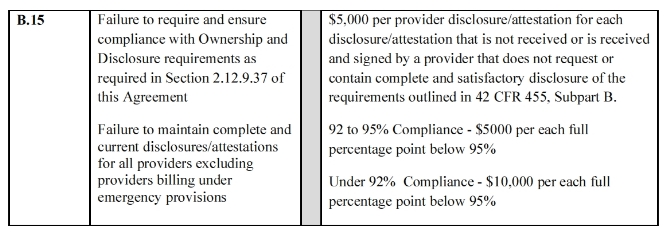
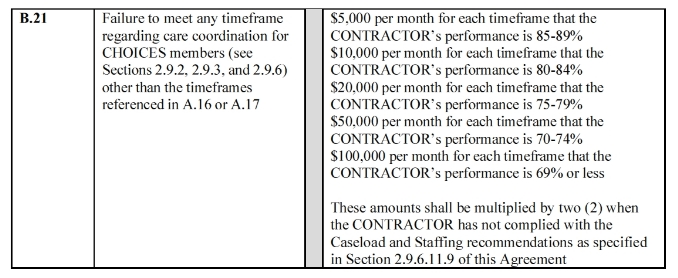
| 74. | “Mental Health Case Management” Services in Attachment I shall be deleted and replaced as follows: |
SERVICE Mental Health Case Management
DEFINITION
Mental health case management is a supportive service provided to enhance treatment effectiveness and outcomes with the goal of maximizing resilience and recovery options and natural supports for the individual. Mental health case management is consumer-centered, consumer focused and strength-based, with services provided in a timely, appropriate, effective, efficient and coordinated fashion. It consists of activities performed by a team or a single mental health case manager to support clinical services. Mental health case managers assist in ensuring the individual/family access to services.
The Case Management Society of America (CMSA) defines case management as a collaborative process of assessment, planning, facilitation and advocacy for options and services to meet an individual’s and family’s comprehensive health needs through communication and available resources to promote quality cost-effective outcomes.
Mental health case management requires that the mental health case manager and the individual and/or family have a strong productive relationship which includes viewing the individual/family as a responsible partner in identifying and obtaining the necessary services and resources. Services rendered to children and youth shall be consumer-centered and family-focused with case managers working with multiple systems (e.g. education, child welfare, juvenile justice). Mental health case management is provided in community settings, which are accessible and comfortable to the individual/family. The service should be rendered in a culturally competent manner and be outcome driven. Mental health case management shall be available 24 hours a day, 7 days a week. The service is not time limited and provides the individual/family the opportunity to improve their quality of life.
The CONTRACTOR shall ensure mental health case management is rendered in accordance with all of the service components and guidelines herein.
SERVICE DELIVERY The CONTRACTOR shall:
| • | Determine caseload size based on an average number of individuals per case manager, with the expectation being that case managers will have mixed caseloads of clients and flexibility between Levels 1and 2a and 2b (Levels 1 and 2 are defined below); and |
| • | Ensure that caseload sizes and minimum contacts are met as follows: |
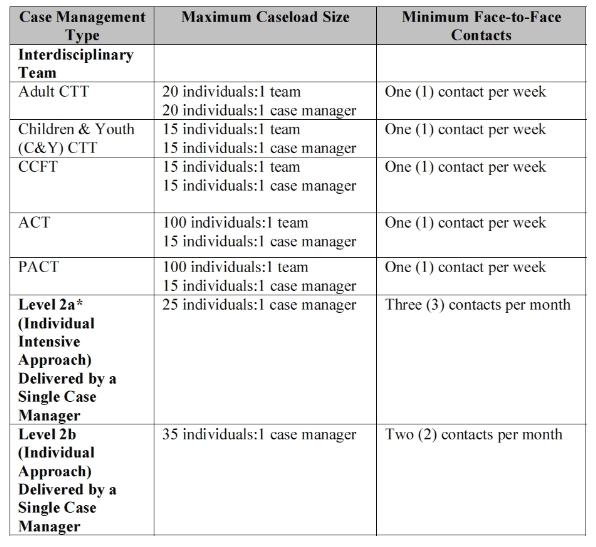
The CONTRACTOR shall ensure that the following requirements are met:
| 1) | All mental health case managers shall have, at a minimum, a bachelor’s degree or be licensed as a Registered Nurse; |
| 2) | Supervisors shall maintain no greater than a 1:30 supervisory ratio with mental health case managers; |
| 3) | Mental health case managers who are assigned to both a parent(s) and child in the same family, should have skills and experience needed for both ages; mental health case managers who are assigned to individuals with co-occurring disorders (mental illness and substance abuse disorders) should have the skills and experience to meet the needs of these individuals; |
| 4) | A minimum of fifty-one percent (51%) of all mental health case management services should take place outside the case manager’s office at the most appropriate setting; |
| 5) | The children and youth (C&Y) (under age eighteen (18)) mental health case management model shall provide a transition from C&Y services into adult services, including adult mental health case management services. The decision to serve an 18-year old youth via the C&Y case management system versus the adult system shall be a clinical one made by a provider. Transition from children’s services, including mental health case management, shall be incorporated into the child’s treatment plan; and |
| 6) | All mental health case management services shall be documented in a treatment plan. Mental health case management activities are correlated to expected outcomes and outcome achievement and shall be monitored, with progress being noted periodically in a written record. |
Level 1
Level 1 mental health case management is the most intense level of service. It provides frequent and comprehensive support to individuals with a focus on recovery and resilience. The CONTRACTOR shall ensure the provision of level 1 mental health case management to the most severely disabled adults and emotionally disturbed children and youth, including individuals who are at high risk of future hospitalization or placement out of the home and require both community support and treatment interventions. Level 1 mental health case management shall be rendered through a team approach. Team approaches may include such models as ACT, CTT, CCFT and PACT, as described below: Assertive Community Treatment (ACT)
ACT is a way of delivering comprehensive and effective services to adults diagnosed with severe mental illness and who have needs that have not been well met by traditional approaches to delivering services. The principles of ACT include:
1) Services targeted to a specific group of individuals with severe mental illness;
2) Treatment, support and rehabilitation services provided directly by the ACT team;
3) Sharing of responsibility between team members and individuals served by the team;
4) Small staff (all team staff including case managers) to individual ratios (approx. 1 to 10);
5) Comprehensive and flexible range of treatment and services;
6) Interventions occurring in community settings rather than in hospitals or clinic settings;
7) No arbitrary time limit on receiving services;
8) Individualized treatment, support and rehabilitation services;
9) Twenty-four (24) hour a day availability of services; and
10) Engagement of individuals in treatment and monitoring.
Continuous Treatment Team (CTT)
CTT is a coordinated team of staff (to include physicians, nurses, case managers, and other therapists as needed) who provide a range of intensive, integrated mental health case management, treatment, and rehabilitation services to adults and children and youth. The intent is to provide intensive treatment to families of children and youth with acute psychiatric problems in an effort to prevent removal from the home to a more restrictive level of care. An array of services are delivered in the home or in natural settings in the community, and are provided through a strong partnership with the family and other community support systems. The program provides services including crisis intervention and stabilization, counseling, skills building, therapeutic intervention, advocacy, educational services, medication management as indicated, school based counseling and consultation with teachers, and other specialized services deemed necessary and appropriate.
Comprehensive Child and Family Treatment (CCFT)
CCFT services are high intensity, time-limited services designed for children and youth to provide stabilization and deter the “imminent” risk of State custody for the individual. There is usually family instability and high-risk behaviors exhibited by the child/adolescent. CCFT services are concentrated on child, family, and parental/guardian behaviors and interaction. CCFT services are more treatment oriented and situation specific with a focus on short-term stabilization goals. The primary goal of CCFT is to reach an appropriate point of stabilization so the individual can be transitioned to a less intense outpatient service.
Program of Assertive and Community Treatment (PACT)
PACT is a service delivery model for providing comprehensive community-based treatment to adults
with severe
and persistent mental illness. It involves the use of a multi-disciplinary team of mental health
staff organized as an
accountable, mobile mental health agency or group of providers who function as a team
interchangeably to
provide the treatment, rehabilitation and support services persons with severe and/or
persistent mental illnesses need to live successfully in the community.
Level 2a and Level 2b
Level 2 mental health case management is a less intensive level of service than Level 1 and is focused on resilience and recovery. The CONTRACTOR shall ensure that level 2 mental health case management is provided to individuals whose symptoms are at least partially stabilized or reduced in order to allow treatment and rehabilitation efforts.
Where available, peer support might be used as an adjunct to the case manager in monitoring the service recipient prior to discharge from Level 2 case management. However, at no time should peer support in the form of Certified Peer Specialists, or any other form, become a substitute for case managers in the delivery of case management services.
SERVICE COMPONENTS
The CONTRACTOR shall ensure that mental health case management incorporates the following service components:
Crisis Facilitation
Crisis facilitation is provided in situations requiring immediate attention/resolution for a specific individual or other person(s) in relation to a specific individual. It is the process of accessing and coordinating services for an individual in a crisis situation to ensure the necessary services are rendered during and following the crisis episode. Most crisis facilitation activities would involve face-to-face contact with the individual.
Assessment of Daily Functioning
Assessment of daily functioning involves the on-going monitoring of how an individual is coping with life on a day to day basis for the purposes of determining necessary services to maintain community placement and improve level of functioning. Most assessments of daily functioning are achieved by face-to-face contact with the individual in his or her natural environment.
Assessment/Referral/Coordination
Assessment/referral/coordination involves assessing the needs of the individual for the purposes of referral and coordination of services that will improve functioning and/or maintain stability in the individual’s natural environment.
Mental Health Liaison
Mental health liaison services are offered to persons who are not yet assigned to mental health case management. It is a short-term service for the purposes of service referral and continuing care until other mental health services are initiated.
| 75. | The paragraph regarding “Supported Housing” in Attachment I shall be deleted and replaced as follows: |
Supported Housing
Supported housing services refers to services rendered at facilities that are staffed twenty-four (24) hours per day, seven (7) days a week with associated mental health staff supports for individuals who require treatment services and supports in a highly structured setting. These mental health services are for priority enrollees and are intended to prepare individuals for more independent living in the community while providing an environment that allows individuals to live in community settings. Given this goal, every effort should be made to place individuals in facilities near their families and other support systems and original areas of residence. Supported housing services are mental health services and do not include the payment of room and board.
| 76. | Attachment VIII shall be amended by deleting and replacing the list of DELIVERABLE ITEMS as follows: |
DELIVERABLE ITEMS
| 1. | Evidence of TDCI license for CONTRACTOR and subcontractors (as applicable) to ensure compliance with Section 2.1.1 |
| 2. | Notification that a member may satisfy any of the conditions for termination from the TennCare program in accordance with Section 2.5.4 |
| 3. | Request for prior approval/notice of use of cost effective alternative services in accordance with Section 2.6.5 |
| 4. | Request for prior approval of incentives in accordance with Section 2.6.6 |
| 5. | Policies and procedures for patient liability that ensure compliance with Section 2.6.7.2 |
| 6. | Policies and procedures for self-direction of health care tasks in accordance with Section 2.7.3 |
| 7. | Description of health education and outreach programs and activities to ensure compliance with Section 2.7.4 |
| 8. | TENNderCare policies and procedures that ensure compliance with the requirements of Section 2.7.6 |
| 9. | Policies and procedures for advance directives that ensure compliance with Section 2.7.7 |
| 10. | Disease management program policies and procedures that ensure compliance with Section 2.8 |
| 11. | Service coordination policies and procedures that ensure compliance with Section 2.9.1 |
| 12. | Policies and procedures for transition of new members that ensure compliance with the requirements of Section 2.9.2 |
| 13. | Policies and procedures for transition of member receiving long-term care services at the time of CHOICES implementation that ensure compliance with Section 2.9.3 |
| 14. | Transition of care policies and procedures that ensure compliance with Section 2.9.4 |
15. MCO case management policies and procedures that ensure compliance with Section 2.9.5
16. Care coordination policies and procedures that ensure compliance with Section 2.9.6
| 17. | Policies and procedures for consumer direction of eligible CHOICES HCBS that ensure compliance with Section 2.9.7 |
| 18. | Policies and procedures for coordination of physical health, behavioral health, and long-term care services that ensure compliance with Section 2.9.9 |
| 19. | If CONTRACTOR subcontracts for the provision of behavioral health services, agreement with the subcontractor in accordance with Section 2.9.9.2 to ensure compliance with Section 2.9.9 |
| 20. | Policies and procedures for coordination among behavioral health providers that ensure compliance with Section 2.9.10 |
| 21. | Policies and procedures for coordination of pharmacy services that ensure compliance with Section 2.9.11 |
| 22. | Policies and procedures for coordination of dental services that ensure compliance with Section 2.9.12 |
| 23. | Identification of members serving on the claims coordination committee in accordance with Section 2.9.12.5.3 |
| 24. | Policies and procedures for coordination with Medicare that ensure compliance with Section 2.9.13 |
| 25. | Policies and procedures for inter-agency coordination that ensure compliance with Section 2.9.15 |
| 26. | Policies and procedures regarding non-covered services that ensure compliance with Section 2.10 |
| 27. | Policies and procedures to develop and maintain a provider network that ensure compliance with Section 2.11.1, including policies and procedures for selection and/or retention of providers |
| 28. | Policies and procedures for PCP selection and assignment that ensure compliance with Section 2.11.2, including policies and procedures regarding change of PCP and use of specialist as PCP |
| 29. | Plan to identify, develop, or enhance existing inpatient and residential treatment capacity for adults and adolescents with co-occurring mental health and substance abuse disorders to ensure compliance with Section 2.11.5.2 |
| 30. | Credentialing manual and policies and procedures that ensure compliance with Section 2.11.8 |
| 31. | Policies and procedures that ensure compliance with notice requirements in Section 2.11.9 |
| 32. | Notice of provider and subcontractor termination and additional documentation as required by Section 2.11.9.2 |
| 33. | Provider agreement template(s) and revisions to TDCI as required in Section 2.12 |
| 34. | Indemnity language in provider agreements if different than standard indemnity language (see Section 2.12.9.54) |
| 35. | Intent to use a physician incentive plan (PIP) to TennCare Bureau and TDCI (see Section 2.13.9) |
| 36. | Any provider agreement templates or subcontracts that involve a PIP for review as a material modification (to TDCI) as required by (see Section 2.13.9) |
| 37. | Pricing policies for emergency services provided by non-contract providers that ensure compliance with Section 2.13.10.1 |
| 38. | Policies and procedures for PCP profiling to ensure compliance with Section 2.14.9 |
| 39. | Information on PCP profiling as requested by TENNCARE (see Section 2.14.9) |
| 40. | QM/QI policies and procedures to ensure compliance with Section 2.15 |
| 41. | Copy of signed contract with NCQA approved vendor to perform CAHPS as required by Section 2.15.5 |
| 42. | Copy of signed contract with NCQA approved vendor to perform HEDIS audit as required by Section 2.15.5 |
| 43. | Evidence that NCQA accreditation application submitted and fee paid (Section 2.15.5.1) |
| 44. | HEDIS BAT as required by Section 2.15.6 |
| 45. | Copy of signed NCQA survey contract as required by Section 2.15.5.1 |
| 46. | Notice of date for ISS submission and NCQA on-site review as required by Section 2.15.5.1 |
| 47. | Notice of final payment to NCQA as required by Section 2.15.5.1 |
| 48. | Notice of submission of ISS to NCQA as required by Section 2.15.5.1 |
| 49. | Copy of completed NCQA survey and final report as required by Section 2.15.5.1 |
| 50. | Notice of any revision to NCQA accreditation status |
| 51. | Policies and procedures regarding critical incident management and reporting to ensure compliance with Section 2.15.7.1 |
| 52. | Policies and procedures regarding behavioral health adverse occurrence reporting to ensure compliance with Section 2.15.7.2 |
| 53. | Report critical incidents or adverse occurrences to TENNCARE within twenty-four (24) hours pursuant to Sections 2.15.7.1, 2.15.7.2, and 2.15.7.3 |
| 54. | Provider Preventable Conditions Reporting (see Section 2.15.8) |
| 55. | If applicable, information on the use of the name of the CONTRACTOR’s TennCare MCO pursuant to Section 2.16.3 |
| 56. | Member materials as described in Section 2.17, including but not limited to, member handbook, quarterly member newsletters, identification card, and provider directory along with any required supporting materials |
| 57. | Member services phone line policies and procedures that ensure compliance with Section 2.18.1 |
| 58. | Policies and procedures regarding interpreter and translation services that ensure compliance with Section 2.18.2 |
| 59. | Provider service and phone line policies and procedures that ensure compliance with Section 2.18.4 |
| 60. | Description of 24/7 ED Assistance Line (see Section 2.18.4.7) |
| 61. | Provider handbook that is in compliance with requirements in Section 2.18.5 |
| 62. | Provider education and training plan and materials that ensure compliance with Section 2.18.6 |
| 63. | Provider relations policies and procedures in compliance with Section 2.18.7 |
| 64. | Protocols regarding one-on-one assistance to long-term care providers that ensure compliance with Section 2. 18.7.2 |
| 65. | Policies and procedures to monitor and ensure provider compliance with the Agreement (see Section 2.18.7.3) |
| 66. | Policies and procedures for a provider complaint system that ensure compliance with Section 2.18.8 |
| 67. | FEA education and training plan and materials that ensure compliance with Section 2.18.9 |
| 68. | Policies and procedures regarding member involvement with behavioral health services that ensure compliance with Section 2.18.10 |
| 69. | Appeal and complaint policies and procedures that ensure compliance with Section 2.19 |
| 70. | Fraud and abuse policies and procedures that ensure compliance with Section 2.20 |
| 71. | Report all confirmed or suspected fraud and abuse to the appropriate agency as required in Section 2.20.2 |
| 72. | Fraud and abuse compliance plan (see Section 2.20.3) |
| 73. | A risk assessment annually and “as needed” (see Section 2.20.3.2.2) |
| 74. | TPL policies and procedures that ensure compliance with Section 2.21.4 |
| 75. | Accounting policies and procedures that ensure compliance with Section 2.21.7 |
| 76. | Proof of insurance coverage (see Section 2.21.8) |
| 77. | Executed agreement for audit accounts that contains the required language (see Section 2.21.11) |
| 78. | Claims management policies and procedures that ensure compliance with Section 2.22 |
79. Internal claims dispute procedure (see Section 2.22.5)
80. EOB policies and procedures to ensure compliance with Section 2.22.8
| 81. | Systems policies and procedures, manuals, etc. to ensure compliance with Section 2.23 (see Section 2.23.10) |
| 82. | Proposed approach for remote access in accordance with Section 2.23.6.10 |
| 83. | Information security plan as required by Section 2.23.6.11 |
| 84. | Notification of Systems problems in accordance with Section 2.23.7 |
| 85. | Systems Help Desk services in accordance with Section 2.23.8 |
| 86. | Notification of changes to Systems in accordance with Section 2.23.9 |
| 87. | Notification of changes to membership of behavioral health advisory committee and current membership lists in accordance with Section 2.24.2 |
| 88. | Notification of changes to membership of CHOICES Advisory Group and current membership lists in accordance with Section 2.24.3 |
| 89. | An abuse and neglect plan in accordance with Section 2.24.4 |
| 90. | Medical record keeping policies and procedures that ensure compliance with Section 2.24.6 |
| 91. | Subcontracts (see Section 2.26) |
| 92. | HIPAA policies and procedures that ensure compliance with Section 2.27 |
| 93. | Notification of breach and provisional breach in accordance with Section 2.27 |
| 94. | Third (3rd) party certification of HIPAA transaction compliance in accordance with Section 2.27 |
| 95. | Non-discrimination policies and procedures as required by Section 2.28 |
| 96. | Names, resumes, and contact information of key staff as required by Section 2.29.1.2 |
| 97. | Changes to key staff as required by Section 2.29.1.2 |
| 98. | Staffing plan as required by Section 2.29.1.8 |
| 99. | Changes to location of staff from in-state to out-of-state as required by Section 2.29.1.9 |
| 100. | Background check policies and procedures that ensure compliance with Section 2.29.2.1 |
| 101. | List of officers and members of Board of Directors (see Section 2.29.3) |
102. Changes to officers and members of Board of Directors (see Section 2.29.3)
103. Eligibility and Enrollment Data (see Section 2.30.2.1)
104. Monthly Enrollment/Capitation Payment Reconciliation Report (see Section 2.30.2.2)
105. Quarterly Member Enrollment/Capitation Payment Report (see Section 2.30.2.3)
106. Information on members (see Section 2.30.2.4)
107. Annual Community Outreach Plan (see Section 2.30.3)
108. Psychiatric Hospital/RTF Readmission Report (see Section 2.30.4.1)
109. Post-Discharge Services Report (see Section 2.30.4.2)
110. Behavioral Health Crisis Response Report (see Section 2.30.4.3)
111. TENNderCare Report (see Section 2.30.4.4)
112. Disease Management Update Report (see Section 2.30.5.1)
113. Disease Management Report (see Section 2.30.5.2)
114. Disease Management Program Description (see Section 2.30.5.3)
115. MCO Case Management Program Description (see Section 2.30.6.1.1)
116. MCO Case Management Services Report (see Section 2.30.6.1.2)
117. MCO Case Management Update Report (see Section 2.30.6.1.3)
118. Status of Transitioning CHOICES Member Report (see Section 2.30.6.2)
119. CHOICES Nursing Facility Diversion Activities Report (see Section 2.30.6.3)
120. CHOICES Nursing Facility to Community Transition Report (see Section 2.30.6.4)
121. CHOICES HCBS Late and Missed Visits Report (see Section 2.30.6.5)
122. CHOICES Consumer Direction of eligible CHOICES HCBS Report (see Section 2.30.6.6)
123. CHOICES Care Coordination Report (see Section 2.30.6.7)
124. Monthly CHOICES Caseload and Staffing Ratio Report (see Section 2.30.6.8)
125. Quarterly MFP Participants Report (see Section 2.30.6.9)
126. Members identified as potential pharmacy lock-in candidates (see Section 2.30.6.10)
127. Pharmacy Services Report (see Section 2.30.6.11)
128. Pharmacy Services Report, On Request (see Section 2.30.6.12)
129. Provider Enrollment File (see Section 2.30.8.1)
130. Provider Compliance with Access Requirements Report (see Section 2.30.8.2)
131. PCP Assignment Report (see Section 2.30.8.3)
132. Report of Essential Hospital Services (see Section 2.30.8.4)
133. Annual Plan for the Monitoring of Behavioral Health Appointment Timeliness (see Section 2.30.8.5)
134. Quarterly Behavioral Health Appointment Timeliness Summary Report (see Section 2.30.8.6)
135. CHOICES Qualified Workforce Strategies Report (see Section 2.30.8.7)
136. FQHC Reports (see Section 2.30.8.8)
137. Related Provider Payment Report (see Section 2.30.10.1)
138. Check Run Summaries Report (see Section 2.30.10.2)
139. Claims Data Extract Report (see Section 2.30.10.3)
140. Reconciliation Payment Report (see Section 2.30.10.4)
141. Administrative Services Only Invoice Report (See Section 2.30.10.5)
142. UM program description, work plan, and evaluation (see Section 2.30.11.1)
143. Cost and Utilization Reports (see Section 2.30.11.2)
144. Cost and Utilization Summaries (see Section 2.30.11.3)
145. Identification of high-cost claimants (see Section 2.30.11.4)
146. CHOICES Utilization Report (see Section 2.30.11.5)
147. Referral Provider Listing and supporting materials (see Section 2.30.11.6)
148. Emergency Department Threshold Report (see Section 2.30.11.7)
149. QM/QI Program Description, Associated Work Plan and Annual Evaluation (see Section 2.30.12.1)
150. Report on Performance Improvement Projects (see Section 2.30.12.2)
151. NCQA Accreditation Report (see Section 2.30.12.3)
152. NCQA revaluation of accreditation status based on HEDIS scores (see Section 2.30.12.4)
| 153. | Medicaid HEDIS measures marked as “Not Reported” (see Section 2.30.12.5) |
154. Reports of Audited CAHPS Results and Audited HEDIS Results (see Section 2.30.12.6)
155. CHOICES HCBS Critical Incidents Report (see Section 2.30.12.7)
156. Behavioral Health Adverse Occurrences Report (see Section 2.30.12.8)
| 157. | Member Services, Provider Services, and Utilization Management Phone Line Report (see Section 2.30. 13. 1. 1) |
| 158. | 24/7 Nurse Triage Line Report (see Section 2.30.13.1.2) |
| 159. | ED Assistance Tracking Report (see Section 2.30.13.1.3) |
| 160. | Translation/Interpretation Services Report (see Section 2.30.13.3) |
| 161. | Provider Satisfaction Survey Report (see Section 2.30.13.4) |
| 162. | Provider Satisfaction Survey Report and CHOICES Provider Satisfaction Survey Report (see Sections 2.30.13.4 and 2.30.13.5) |
| 163. | Member Complaints Report (see Section 2.30.14) |
| 164. | Fraud and Abuse Activities Report (see Section 2.30.15.1) |
| 165. | Policies in compliance with Section 1902(a)(68) of the Social Security Act (see Section 2.30.15.3) |
| 166. | Disclosure Submission Rate Report (see Section 2.30.15.4) |
| 167. | Program Integrity Exception List Report (see Section 2.30.15.5) |
| 168. | List of Involuntary Terminations Report (see Section 2.30.15.6) |
| 169. | Recovery and Cost Avoidance Report (see Section 2.30.16.1.1) |
| 170. | Other Insurance Report (see Section 2.30.16.1.2) |
| 171. | Medical Loss Ratio (MLR) Report (see Section 2.30.16.2.1) |
| 172. | Ownership and Financial Disclosure Report (see Section 2.30.16.2.2) |
| 173. | Annual audit plan (see Section 2.30.16.2.3) |
| 174. | Financial Plan and Projection of Operating Results Report (to TDCI) (see Section 2.30.16.3.1) |
| 175. | Comparison of Actual Revenues and Expenses to Budgeted Amounts Report (to TDCI) (see Section 2.30.16.3.2) |
| 176. | Annual Financial Report (to TDCI) (see Section 2.30.16.4.3) |
| 177. | Quarterly Financial Report (to TDCI) (see Section 2.30.16.3.4) |
178. Audited Financial Statements (to TDCI) (see Section 2.30.16.3.5)
179. Claims Payment Accuracy Report (see Section 2.30.17.1)
180. EOB Report (see Section 2.30.17.2)
181. Claims Activity Report (see Section 2.30.17.3)
182. CHOICES Cost Effective Alternatives Report (see Section 2.30.17.4)
183. Systems Refresh Plan (see Section 2.30.18.1)
184. Encounter Data Files (see Section 2.30.18.2)
185. Electronic version of claims paid reconciliation (see Section 2.30.18.3)
186. Information and/or data to support encounter data submission (see Section 2.30.18.4)
187. Systems Availability and Performance Report (see Section 2.30.18.5)
188. Business Continuity and Disaster Recovery Plan (see Section 2.30.18.6)
| 189. | Reports on the Activities of the CONTRACTOR’s Behavioral Health Advisory Committee (see Section 2.30. 19. 1) |
| 190. | Report on the Activities of the CONTRACTOR’s CHOICES Advisory Group (see Section 2.30.19.2) |
| 191. | Subcontracted claims processing report (see Section 2.30.20.1) |
| 192. | HIPAA/HITECH Report (Privacy/Security Incident Report) (see Section 2.30.21) |
| 193. | Non-discrimination policy (see Section 2.30.22.1) |
| 194. | Summary Listings of Servicing Providers (see Section 2.30.22.2) |
| 195. | Non-Discrimination Compliance Plan and Assurance of Non-Discrimination (see Section 2.30.22.3) |
| 196. | Non-Discrimination Compliance Report (see Section 2.30.22.4) |
| 197. | Disclosure of conflict of interest (see Section 2.30.23.1) |
| 198. | Attestation Re: Personnel Used in Contract Performance (see Section 2.30.23.2) |
| 199. | Provider reimbursement rates for services incurred prior to the start date of operations in accordance with Section 3.7.1.2.1 |
| 200. | Return of funds in accordance with Section 3.16.5 |
| 201. | Termination plan in accordance with Section 4.4.8.2.8 |
| 202. | Policies and procedures for delivering NEMT services, including an operating procedures manual, as provided in Section A. 1 of Attachment XI |
| 77. | Attachment VI shall be deleted and replaced as follows: |
ATTACHMENT VI
FORMS FOR REPORTING FRAUD AND ABUSE
POTENTIAL FRAUD ALLEGATION REFERRAL FORM
(template with sample data)
DATE: Month/Day/Year
TO: Office of Program Integirty
FROM: Your MCE Name
Contact Person: 1st & Last name; Telephone; EMail;
SUBJECT (ENTITY/NAME/SPECIALTY): ABC Clinic, John Smith MD, Family Practice
SUBJECT ADDRESS/TELEPHONE:
100 Great Circle Rd, TN 37234 Phone: Fax:
PROVIDER INFORMATION(S):
HealthPlan IDs: 123456789 (Clinic) and 12345 (John Smith)
Medicaid ID(s): 7654321 (Clinic) and 9876543 (John Smith)
NPI(s): 1234567890 (Clinic) and 2345678900 (John Smith)
License – 1001 (John Smith)
DEA – 12345 (John Smith)
Tax ID – 621039594; SSN (2345678)
PROVIDER OPERATING REGION: East TN
PROVIDER INCOME:
$374,729 (April 2, 2007 – February 7, 2011)
DATES OF SERVICE AUDITED: November 1, 2009 – November 9, 2010
OVERPAYMENT IDENTIFIED: $ 31,861
ALLEGATION:
Provider is allegedly billing an excessive number of services per day.
SOURCE/PREDICATION:
Data analysis internal lead from the Medicaid Plan
PROCEDURE CODE and MODIFIERS: 99214 – Office/outpatient visit for the evaluation and mgmt of an estab patient Mod 25 – A significant, separately identifiable service by the same physician on the same day of the procedure or other service.
| Mod 59 – Distinct procedural service is distinct and or independent from other services performed on same day. Identifies procedures not normally reported together. |
BILLING ENTITY:
Payments are made to the group via EFT.
MEDICAL RECORD TYPE: Hard copy, hand written
SUMMARY OF PRELIMINARY INVESTIGATION ACTIONS:
Sampling:
A sample for 99214s with modifiers 25 and/or 59 for dates of service 11/1/0911/9/10 was
generated. The universe size was 430 whereas a sample 30 of dates of service was
pulled. A total of $100,000 was paid to the universe.
Medical Record Review and Findings:
On January 15, 2010 the medical record review was completed by an internal certified
professional coder (CPC). There were a total of 138 services reviewed. The following
is a summary of the services:
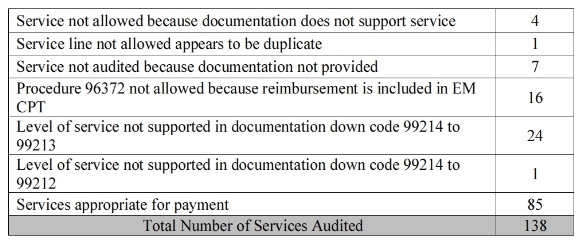
Modifier 25 was appended to the E/M services 97% of the time. It is inappropriate to append this modifier to an E/M service when it is billed in conjunction with laboratory services; 13 services were denied based on this rule.
Modifier 59 was appended on all ancillary codes (other than J codes) 100% of the time. It did not appear to be appropriately used in any instances. For example, claims for the therapeutic, prophylactic, or diagnostic injection and infusions (CPT 96365 or CPT 96372) that were appended with modifier 59 were denied 16 times.
Under certain circumstances, it may be necessary to indicate that a procedure of service was distinct or independent from other non E/M services performed on the same day. Modifier 59 is used to identify procedures/services, other than E/M services, that are not normally reported together, but are appropriate under the circumstances. However, when another already established modifier is appropriate it should be used rather than modifier 59, only if no more descriptive modifier is available, and the use of modifier 59 best explains the circumstances, should modifier 59 be used.
Note: it is not necessary to appended modifier 59 to multiple laboratory services as it does not meet the circumstances stated above.
PRIOR EDUCATIONS: None recorded
PREPAYMENT REVIEW: None
INTERAGENCY CONTACT: None
ADDITIONAL SUBJECT INFORMATION:
John Smith has hospital privileges at ABC Community Hospital.
DISCLOSURE OF OWNERSHIP and CONTROL: John Smith owns 100% of the entity.
DETERMINATION:
Based on the medical record review it has been determined that the provider is abusing “modifier
25 and 59” in order to have add on services reimbursed that are typically already covered in the
reimbursement of the E/M code.
RECOMMENDATION:
Petition for the Health Plan to pursue administratively by issuing/implementing:
Initiate pre payment review
Demand letter for repayment
Educate the provider on proper billing and medical record
documentation. Initiate a Corrective Action Plan with the provider
Continued monitoring of the provider’s billing after notification of overpayment.
TennCare Recommended MCC Referral Protocol:
1) the submission of documents related to the provider fraud and abuse referral should be via TennCare SFTP server
(path: tncare.sftp.state.tn.us/tncare/MCC###/orr/OPI/in ) with password protections on documents;
2) concurrently, a notice of submission should be e-mailed to
ProgramIntegrity.TennCare@tn.gov with a subject line stating “MCC### Notice of Referral Submission via SFTP”
along with password notices on opening documents.
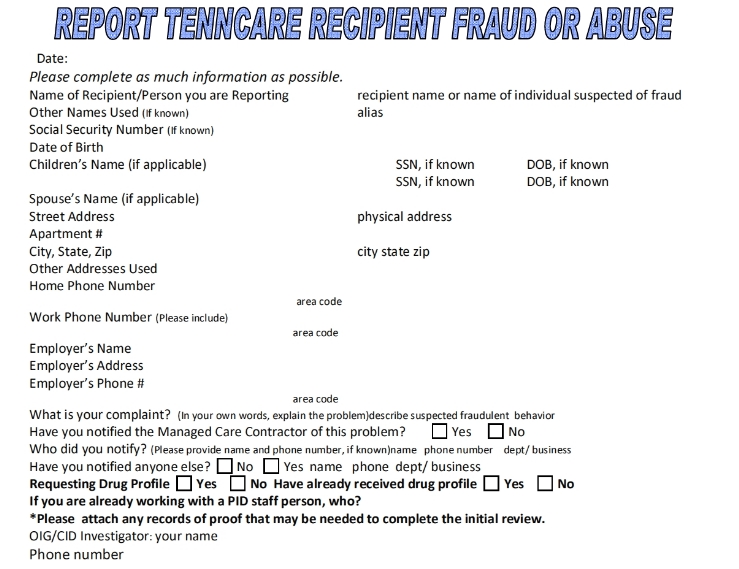
STATE OF TENNESSEE
OFFICE OF TENNCARE INSPECTOR GENERAL
PO BOX 282368
NASHVILLE, TENNESSEE 37228
FRAUD TOLL FREE HOTLINE 1-800-433-3982 • FAX (615)
256-3852
E-Mail Address: www.tennessee.gov/tenncare (follow the prompts that read
“Report Fraud Now”)
| 78. | Attachment VI shall be amended by deleting the performance standard for Non-IMD Inpatient Use in its entirety. |
| 79. | Attachment IX, Exhibit I shall be deleted and replaced with “LEFT BLANK INTENTIONALLY”. |
| 80. | The first two populations listed in Attachment IX, Exhibit K shall be deleted and replaced as follows: |
• Medicaid (Child and Adult)
• Uninsured (Child and Adult)
| 81. | Item 14 of Exhibit A of Attachment XI shall be deleted and replaced as follows: |
14. Tennessee Department of Intellectual and Developmental Disabilities (DIDD): The state
agency responsible for providing services and supports to Tennesseans with mental retardation.
DIDD is a division of the Tennessee Department of Finance and Administration.
| 82. | Attachment XII shall be amended by adding a new Exhibit G as follows: |
EXHIBIT G
CAPITATION RATES
AmeriGroup
EFFECTIVE July 1, 2011
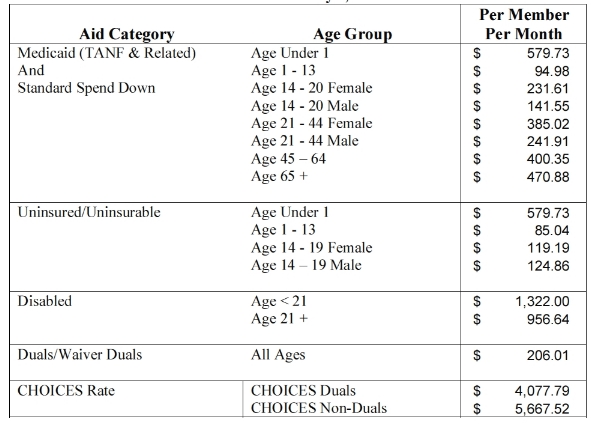 All of the provisions of the
original Agreement not specifically deleted or modified herein shall remain in full force and
effect. Unless a provision contained in this Amendment specifically indicates a different effective
date, for purposes of the provisions contained herein, this Amendment shall become effective
January 1, 2012.
All of the provisions of the
original Agreement not specifically deleted or modified herein shall remain in full force and
effect. Unless a provision contained in this Amendment specifically indicates a different effective
date, for purposes of the provisions contained herein, this Amendment shall become effective
January 1, 2012.
The CONTRACTOR, by signature of this Amendment, hereby affirms that this Amendment has not been altered and therefore represents the identical document that was sent to the CONTRACTOR by TENNCARE.
IN WITNESS WHEREOF, the parties have by their duly authorized representatives set their signatures.