Attached files
| file | filename |
|---|---|
| 8-K - 8-K - Innoviva, Inc. | a11-26866_18k.htm |
| EX-99.4 - EX-99.4 - Innoviva, Inc. | a11-26866_1ex99d4.htm |
| EX-99.1 - EX-99.1 - Innoviva, Inc. | a11-26866_1ex99d1.htm |
| EX-99.2 - EX-99.2 - Innoviva, Inc. | a11-26866_1ex99d2.htm |
Exhibit 99.3
Poster No. P822
Safety, pharmacokinetics (PK) and pharmacodynamics (PD) of single doses of GSK573719 Inhalation Powder, a new long-acting muscarinic antagonist (LAMA), in patients with COPD
R Mehta,(1) D Kelleher,(1) A Preece,(2) A Cahn(3), G Crater(1)
(1)GlaxoSmithKline, RTP, USA; (2)GlaxoSmithKline, Stockley Park, UK; (3)GlaxoSmithKline, Stevenage, UK
INTRODUCTION
· Bronchodilators are important for the management of symptoms in chronic obstructive pulmonary disease (COPD).(1)
· GSK573719 is a new, long-acting muscarinic antagonist (LAMA) offering sustained 24h bronchodilation.
OBJECTIVES
· To assess the safety/tolerability (primary), pharmacokinetics and pharmacodynamics (secondary) of single-dose inhaled GSK573719 in ipratropium-responsive COPD patients.
METHODS
· This was a phase II, randomised, double-blind, placebo-controlled, double dummy, four-way crossover study with incomplete block design.
· Patients aged 40–75 years were eligible for inclusion in the study, provided they had a history of COPD (American Thoracic Society/European Respiratory Society criteria), post-bronchodilator FEV1/FVC <0.7, FEV1 between 40% and 80% of predicted normal, and showed a minimum 25% increase in specific airways conductance (sGaw) 2h after inhaling 80mcg ipratropium bromide. Female patients had to be without childbearing potential.
· The following were considered as exclusion criteria: any past or present medical condition likely to affect the study outcome; positive pre-study drug or alcohol screen; positive test for HIV or hepatitis B or C; any medication known to be a CYP 2D6 inhibitor or substrate; and a CYP 2D6 poor metaboliser genotype.
· Four treatments were evaluated and compared with placebo: GSK573719 (250, 500 or 1000mcg), tiotropium (18mcg). Patients were randomised to receive one of twelve different sequences of study medication (Table 1). Each sequence included one dose of placebo and three of the four treatments. A 14-day washout period was scheduled between each dose.
TABLE 1. TREATMENT SEQUENCES
|
Sequence |
|
Period 1 |
|
Period 2 |
|
Period 3 |
|
Period 4 |
|
1 |
|
250mcg |
|
500mcg |
|
Tiotropium |
|
Placebo |
|
2(a) |
|
250mcg |
|
500mcg |
|
1000mcg |
|
Placebo |
|
3(a) |
|
250mcg |
|
Placebo |
|
500mcg |
|
1000mcg |
|
4(a) |
|
250mcg |
|
500mcg |
|
Placebo |
|
1000mcg |
|
5(a) |
|
Placebo |
|
250mcg |
|
500mcg |
|
1000mcg |
|
6 |
|
250mcg |
|
Placebo |
|
Tiotropium |
|
500mcg |
|
7 |
|
Placebo |
|
Tiotropium |
|
250mcg |
|
500mcg |
|
8 |
|
Tiotropium |
|
Placebo |
|
250mcg |
|
500mcg |
|
9 |
|
Tiotropium |
|
250mcg |
|
500mcg |
|
Placebo |
|
10 |
|
Tiotropium |
|
250mcg |
|
Placebo |
|
500mcg |
|
11 |
|
Placebo |
|
250mcg |
|
Tiotropium |
|
500mcg |
|
12 |
|
250mcg |
|
Placebo |
|
500mcg |
|
Tiotropium |
(a)Three subjects were randomised to each of these sequences. One subject was randomised to each of the other sequences
· GSK573719 was administered via DISKUS™ (GlaxoSmithKline plc) and tiotropium was administered via HandiHaler™ (Boehringer Ingelheim Inc.).
· Inhaled salbutamol was permitted as relief (rescue) medication. Inhaled corticosteroids (£1000mcg/day of fluticasone propionate or equivalent) were also permitted, provided the dose remained constant during the study and the preceding 4 weeks. Inhaled long acting bronchodilators were not permitted.
· Primary endpoints were: adverse events (AEs), blood pressure, heart rate (HR), electrocardiogram (ECG), 24h Holter and 4h lead II ECG monitoring, lung function and laboratory safety tests.
· Secondary endpoints were: serial post-dose measurements of sGaw, airways conductance and FEV1; plasma and urine concentrations of GSK573719; and pharmacokinetic parameters derived from the plasma and urine concentrations.
· Sample size was calculated from change in sGaw: assuming a within-subject standard deviation of 0.205 and between-subject standard deviation of 0.280, 24 subjects would be needed for 98% power to detect a 30% increase in sGaw between placebo and GSK573719 at the 5% significance level.
RESULTS
Patients
· Twenty-four patients entered the study, four of whom withdrew prematurely because of AEs. Treatments received prior to withdrawal were GSK573719 250mcg; tiotropium; placebo; and GSK573719 250mcg followed by GSK573719 500mcg.
· Except for the four withdrawals, all patients received all of their allocated doses of study medication.
· As a result, 21 patients received placebo, 22 received GSK573719 250mcg, 21 received GSK573719 500mcg, 13 received GSK573719 1000mcg and 8 received tiotropium 18mcg.
· Table 2 provides a summary of patient demographics.
TABLE 2. PATIENTS’ BASELINE CHARACTERISTICS
|
|
|
Value for the study |
|
Characteristic |
|
population (N=24) |
|
Mean age, years (range) |
|
56.0 (48–67) |
|
Male (n, %) |
|
19 (79) |
|
White/Caucasian/European (n, %) |
|
24 (100) |
|
Mean height, cm (range) |
|
174.9 (157–187) |
|
Mean weight, kg (range) |
|
80.76 (57.7–102.0) |
|
Mean body mass index, kg/m2 (range) |
|
26.37 (21.1–31.5) |
Safety and tolerability
· The proportion of patients reporting any AEs after GSK573719 ranged between 31% and 41% (Table 3). In comparison, 38% of patients reported AEs following tiotropium and 29% reported AEs after receiving placebo.
· Treatment-related AEs were reported by 5–23% of patients after receiving GSK573719, compared with 10% after receiving placebo (Table 3). No treatment-related AEs were reported following inhalation of tiotropium.
TABLE 3. SUMMARY OF AEs
|
|
|
|
|
GSK573719 |
|
Tiotropium | ||||
|
|
|
Placebo |
|
250mcg |
|
500mcg |
|
1000mcg |
|
18mcg (%) |
|
n (%) |
|
(N=21) |
|
(N=22) |
|
(N=21) |
|
(N=13) |
|
(N=8) |
|
|
|
|
|
|
|
|
|
|
|
|
|
Patients with any AE |
|
6 (29) |
|
9 (41) |
|
8 (38) |
|
4 (31) |
|
3 (38) |
|
Patients with any treatment - related AE |
|
2 (10) |
|
1 (5) |
|
4 (19) |
|
3 (23) |
|
0 |
|
Headache |
|
2 (10) |
|
1 (5) |
|
2 (10) |
|
1 (8) |
|
0 |
|
Atrial fibrillation |
|
0 |
|
0 |
|
0 |
|
1 (8) |
|
0 |
|
Dizziness |
|
0 |
|
0 |
|
2 (10) |
|
1 (8) |
|
0 |
|
Pharyngolaryngeal pain |
|
0 |
|
0 |
|
0 |
|
2 (15) |
|
0 |
|
Ventricular tachycardia |
|
0 |
|
0 |
|
1 (5) |
|
0 |
|
0 |
· The most common treatment-related AEs with GSK573719 were headache, dizziness and pharyngolaryngeal pain.
· None of the AEs associated with premature withdrawal from the study (exacerbation of COPD [n=1], respiratory distress [n=2] and intermittent atrial fibrillation [n=1]) were considered as related to study medication.
· There were no deaths or serious AEs during the study.
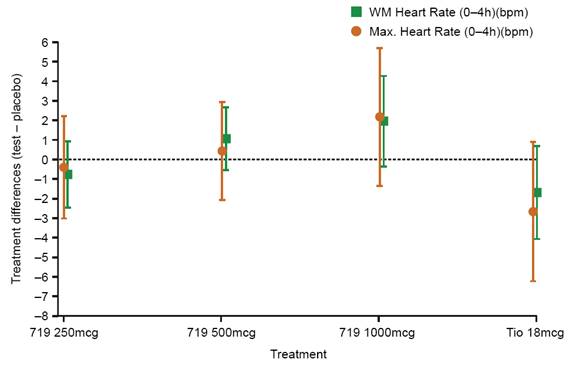
· There was no clear evidence of a difference between any of the active treatments and placebo, with respect to either weighted mean HR (0–4h) or maximum HR (0–4h) (Figure 1). There were trends towards increased values with increasing doses of GSK573719 and decreased values with tiotropium, but all 95% confidence intervals (CIs) for difference versus placebo spanned zero.
FIGURE 1. WEIGHTED MEAN AND MAXIMUM HR (0–4h): TREATMENT DIFFERENCES RELATIVE TO PLACEBO
· For the maximum and weighted mean (0–4h) systolic blood pressure, the GSK573719 250mcg and 500mcg dose groups showed decreases in both these measures, while the GSK573719 1000mcg and tiotropium 18mcg groups both showed increases. Maximum and weighted mean (0–4h) diastolic blood pressure, in general, showed decreases relative to placebo, except for GSK573719 1000mcg, where increases were seen.
· Holter parameters for maximum HR (0–24h) and mean HR (0–24h) showed a trend towards a decrease versus placebo with all active treatments. Most 95% CIs spanned zero, with the exception of those for maximum HR following GSK573719 500mcg and 1000mcg. The 1000mcg dose produced a mean decrease of 7.7bpm versus placebo (95% CI: 1.8–13.5bpm).
· There were no notable changes in mean haematology parameters, mean clinical chemistry parameters or urinalysis.
Pharmacodynamics
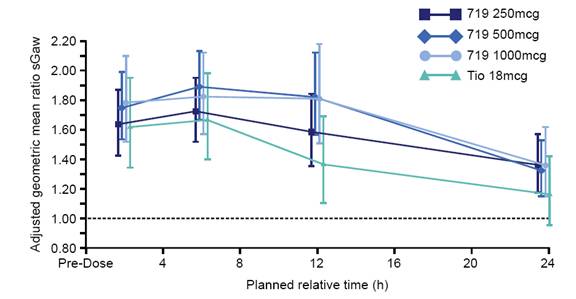
· sGaw values were higher for all active treatment groups compared with placebo over the 24h assessment period, with differences versus placebo peaking at 6h post-dose with all treatments (Figure 2). Differences versus placebo were greatest following GSK573719 500mcg and 1000mcg, and least following tiotropium.
FIGURE 2. GEOMETRIC MEAN SPECIFIC AIRWAYS CONDUCTANCE (sGaw): POST-TREATMENT DIFFERENCES RELATIVE TO PLACEBO
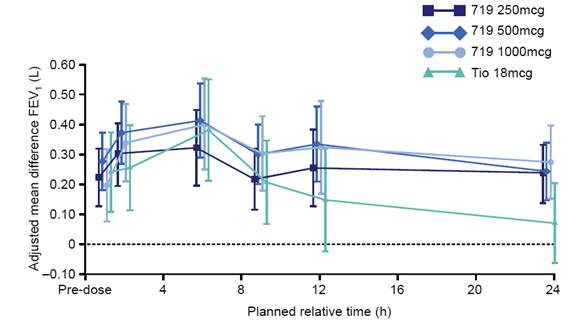
· Broadly similar results were seen with FEV1, with increases versus placebo in all active groups peaking at 6h post-treatment (Figure 3).
FIGURE 3. MEAN FEV1: POST-TREATMENT DIFFERENCES RELATIVE TO PLACEBO
Pharmacokinetics
· Pharmacokinetic data were non-quantifiable in 40–61% of plasma samples.
· Available plasma data indicated that GSK573719 was rapidly absorbed, with tmax values of 5–15min (Table 4); plasma half-life was 1–2h.
· The half-life of GSK573719 in urine was 11–12h. Renal clearance values were estimated to be 5.32, 6.40, and 6.83L/h for the 250mcg, 500mcg and 1000mcg doses, respectively.
· 1–1.3% of administered GSK573719 was excreted unchanged in the urine.
TABLE 4. PLASMA PHARMACOKINETIC PARAMETERS
|
|
|
|
|
|
|
Geometric |
|
|
|
|
|
Parameter |
|
Dose |
|
N/n |
|
mean |
|
95% CI |
|
CV (%) |
|
AUC(0-t) (h*ng/mL) |
|
250mcg |
|
22/22 |
|
0.10271 |
|
(0.07763, 0.13589) |
|
70.0 |
|
|
500mcg |
|
21/21 |
|
0.35491 |
|
(0.27070, 0.46531) |
|
65.2 | |
|
|
1000mcg |
|
13/13 |
|
0.96100 |
|
(0.81529, 1.13276) |
|
27.7 | |
|
|
|
|
|
|
|
|
|
|
|
|
|
Cmax (ng/mL) |
|
250mcg |
|
22/22 |
|
0.12615 |
|
(0.10494, 0.15164) |
|
43.4 |
|
|
500mcg |
|
21/21 |
|
0.30389 |
|
(0.25430, 0.36314) |
|
40.7 | |
|
|
1000mcg |
|
13/13 |
|
0.83228 |
|
(0.72619, 0.95386) |
|
22.9 | |
|
|
|
|
|
|
|
|
|
|
|
|
|
Tmax (h)(a) |
|
250mcg |
|
22/22 |
|
0.090 |
|
(0.08, 0.50) |
|
NA |
|
|
500mcg |
|
21/21 |
|
0.100 |
|
(0.07, 0.27) |
|
NA | |
|
|
|
1000mcg |
|
13/13 |
|
0.250 |
|
(0.08, 0.28) |
|
NA |
(a)Presented as median and range
CONCLUSIONS
· Single doses of GSK573719 were well tolerated and produced clinically significant improvements in lung function among COPD patients.
· GSK573719 was rapidly absorbed.
· Mean sGaw and FEV1 responses were significantly higher for all active treatments versus placebo.
· No correlation was observed between heart rate and Cmax, and heart rate following GSK573719 was in the same range as that following placebo.
REFERENCE
(1) Global Initiative for Chronic Obstructive Lung Disease (GOLD) guideline: Global Strategy for the diagnosis, management, and prevention of Chronic Obstructive Pulmonary Disease (updated 2010). http://www.goldcopd.com/. Accessed 14th July 2011.
ACKNOWLEDGEMENTS
· This trial was sponsored by GlaxoSmithKline (ClinicalTrials.gov: NCT00515502; AC4108123).
· The clinical phase of this study was conducted by Parexel, Berlin 14050, Germany, Pneumologisches Forschungsinstitut-Hamburg 20535, Germany and Fraunhofer-Institut (ITEM), Hannover 30625, Germany.
· Editorial support (in the form of writing assistance, assembling tables and figures, collating author comments, grammatical editing and referencing) was provided by David Cutler at Gardiner-Caldwell Communications and was funded by GlaxoSmithKline.

Presented at the European Respiratory Society (ERS) Annual Congress, Amsterdam, The Netherlands, 24–28 September 2011
