Attached files
| file | filename |
|---|---|
| EX-21 - EXHIBIT 21 - Cigna Holding Co | exhibit21.htm |
| EX-12 - EXHIBIT 12 - Cigna Holding Co | exhibit12.htm |
| EX-23 - EXHIBIT 23 - Cigna Holding Co | exhibit23.htm |
| EX-10 - EXHIBIT 10.3 - Cigna Holding Co | exhibit10_3.htm |
| EX-32 - EXHIBIT 32.1 - Cigna Holding Co | exhibit32_1.htm |
| EX-31 - EXHIBIT 31.1 - Cigna Holding Co | exhibit31_1.htm |
| EX-32 - EXHIBIT 32.2 - Cigna Holding Co | exhibit32_2.htm |
| EX-10 - EXHIBIT 10.2 - Cigna Holding Co | exhibit10_2.htm |
| EX-31 - EXHIBIT 31.2 - Cigna Holding Co | exhibit31_2.htm |
| EX-10 - EXHIBIT 10.27 - Cigna Holding Co | exhibit10_27.htm |
| EX-10 - EXHIBIT 10.26 - Cigna Holding Co | exhibit10_26.htm |
| EX-10 - EXHIBIT 10.25 - Cigna Holding Co | exhibit10_25.htm |
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
FORM 10-K
 ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 FOR THE FISCAL YEAR ENDED DECEMBER 31, 2010
ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 FOR THE FISCAL YEAR ENDED DECEMBER 31, 2010
OR
 TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 FOR THE TRANSITION PERIOD FROM ______________ TO ______________
TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 FOR THE TRANSITION PERIOD FROM ______________ TO ______________
Commission file number 1-8323

CIGNA CORPORATION
(Exact name of registrant as specified in its charter)
|
DELAWARE |
06-1059331 |
|
(State or other jurisdiction of incorporation or organization) |
(I.R.S. Employer Identification No.) |
|
Two Liberty Place, Philadelphia, Pennsylvania |
19192 |
|
(Address of principal executive offices) |
(Zip Code) |
|
(215) 761-1000 |
|
|
(Registrant’s telephone number, including area code) |
|
|
(215) 761-3596 |
|
|
(Registrant’s facsimile number, including area code) |
|
|
SECURITIES REGISTERED PURSUANT TO SECTION 12(b) OF THE ACT: |
|
|
Title of each class |
Name of each exchange on which registered |
|
Common Stock, Par Value $0.25 |
New York Stock Exchange, Inc. |
|
SECURITIES REGISTERED PURSUANT TO SECTION 12(g) OF THE ACT: |
|
None |
|
Indicate by check mark |
YES |
NO |
||
|
• if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. |
|
|
||
|
• if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act. |
|
|
||
|
• whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. |
|
|
||
|
• whether the registrant has submitted electronically and posted on its corporate Web site, if any, every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S-T during the preceding 12 months (or for such shorter period that the registrant was required to submit and post such files). |
|
|
||
|
• if disclosure of delinquent filers pursuant to Item 405 of Regulation S-K is not contained herein, and will not be contained, to the best of registrant’s knowledge, in definitive proxy or information statements incorporated by reference in Part III of this Form 10-K or any amendment to this Form 10-K. |
|
|
||
|
• whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, or a smaller reporting company. See definitions of “large accelerated filer”, “accelerated filer”, and “smaller reporting company” in Rule 12b-2 of the Exchange Act. |
||||
|
Large accelerated filer |
Accelerated filer |
Non-accelerated filer |
Smaller reporting company |
|
|
• whether the registrant is a shell company (as defined in Rule 12b-2 of the Exchange Act). |
|
|
||
The aggregate market value of the voting stock held by non-affiliates of the registrant as of June 30, 2010 was approximately $8.5 billion.
As of January 31, 2011, 271,234,488 shares of the registrant’s Common Stock were outstanding.
Part III of this Form 10-K incorporates by reference information from the registrant’s proxy statement to be dated on or about March 18, 2011.
|
Management’s Discussion and Analysis of Financial Condition and Results of Operations |
|
Changes in and Disagreements with Accountants on Accounting and Financial Disclosure |
|
Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters |
|
PART I |
ITEM 1 Business
A. Description of Business
As used in this document, “CIGNA” and the “Company” may refer to CIGNA Corporation itself, one or more of its subsidiaries, or CIGNA Corporation and its consolidated subsidiaries. CIGNA Corporation is a holding company and is not an insurance company. Its subsidiaries conduct various businesses, which are described in this Annual Report on Form 10-K for the fiscal year ended December 31, 2010 (“Form 10-K”).
CIGNA is a global health service organization with subsidiaries that are major providers of medical, dental, disability, life and accident insurance and related products and services. In the U.S., the majority of these products and services are offered through employers and other groups (e.g. unions and associations) and in selected international markets, CIGNA offers supplemental health, life and accident insurance products, expatriate benefits and international health care coverage and services to businesses, governmental and non-governmental organizations and individuals. In addition to its ongoing operations described above, the Company also has certain run-off operations, including a Run-off Reinsurance segment.
CIGNA Corporation had consolidated shareholders’ equity of $6.6 billion and assets of $45.7 billion as of December 31, 2010, and revenues of $21.3 billion for the year then ended. CIGNA Corporation was incorporated in the State of Delaware in 1981.
CIGNA’s revenues are derived principally from premiums, fees, mail order pharmacy, other revenues and investment income. The financial results of CIGNA’s businesses are reported in the following segments:
•
Health Care;
•
Disability and Life;
•
International;
•
Run-off Reinsurance; and
•
Other Operations, including Corporate-owned Life Insurance.
Available Information
CIGNA’s annual, quarterly and current reports, proxy statements and other filings, and any amendments to these filings, are made available free of charge on its website (http://www.cigna.com, under the “Investors — SEC Filings” captions) as soon as reasonably practicable after the Company electronically files these materials with, or furnishes them to, the Securities and Exchange Commission (the “SEC”). The Company uses its website as a channel of distribution for material company information. Important information, including news releases, analyst presentations and financial information regarding CIGNA is routinely posted on and accessible at www.cigna.com. See “Code of Ethics and Other Corporate Governance Disclosures” in Part III, Item 10 beginning on page 168 of this Form 10-K for additional available information.
B. Financial Information about Business Segments
The financial information included herein is in conformity with accounting principles generally accepted in the United States of America (“GAAP”), unless otherwise indicated. Certain reclassifications have been made to prior years’ financial information to conform to the 2010 presentation. Industry rankings and percentages set forth herein are for the year ended December 31, 2010, unless otherwise indicated. Unless otherwise noted, statements set forth in this document concerning CIGNA’s rank or position in an industry or particular line of business have been developed internally, based on publicly available information.
Financial data for each of CIGNA’s business segments is set forth in Note 23 to the Consolidated Financial Statements beginning on page 156 of this Form 10-K.
CIGNA CORPORATION – 2010 Form 10-K – 1
C. Strategy
As a global health service organization, CIGNA’s mission is to help the people it serves improve their health, well-being and sense of security. As part of this mission, the Company remains committed to health advocacy as a means of creating sustainable solutions for employers, improving the health of the individuals that the Company serves, and lowering the costs of health care for all constituencies.
CIGNA’s long-term growth strategy is based on: (1) growth in targeted geographies, product lines, buying segments and distribution channels; (2) improving its strategic and financial flexibility; and (3) pursuing additional opportunities in high-growth markets with particular focus on individuals. Our strategy can be summarized as follows:
•
“Go deep” with growth in targeted customer segments, geographies, buying segments and distribution channels,
•
“Go individual” by delivering high quality products and services which improve health, wellness and insurance needs that are helpful and easy to use, and
•
“Go global” by pursuing additional opportunities in high-growth markets across the globe and serving individuals regardless of where they live and work.
To achieve these goals, CIGNA expects to focus on the following which have the most potential for profitable growth:
•
Domestic Health Care segment. In this market, CIGNA is focused on expanding and deepening client and customer relationships across each segment. Specifically: (1) within key geographic segments, growing the “Select” market, which generally includes employers with more than 50 but fewer than 250 employees and the “Middle Market” segment which generally includes employers with more than 250 but less than 5,000 employees, by leveraging the Company’s customer knowledge, differentiated service model, product portfolio and distribution model, (2) engaging those national account employers who share and will benefit from the Company’s value proposition of using health advocacy and employee engagement to increase productivity, performance and the health outcomes of their employees, and (3) targeting sub-markets including industry, government and municipal entities and individuals that align closest to the Company’s stated strategy.
•
In the Disability and Life segment, CIGNA’s strategy is to grow its Disability business by fully leveraging the key components of its industry-leading disability management model to reduce costs for its clients and return their employees to work sooner through: (1) effective customer engagement and early outreach, (2) a full suite of clinical and return-to-work resources to support the employer’s ability to manage disability and work related events, and (3) specialized case management services that address an individual’s unique needs.
•
In the International segment, CIGNA continues to expand the product and geographic footprint by executing local strategies that grow supplemental, primary medical and expatriate benefits through: (1) product and channel expansion in its supplemental health, life, and accident business in key Asian geographies, (2) the introduction of new expatriate benefits products, that provide greater benefit and geographic flexibility to individual and employers (such as through the Vanbreda International acquisition); and (3) further expansion of distribution capabilities to capitalize on emerging and growing markets globally.
The Company plans to improve its strategic and financial flexibility by driving further reductions in its Health Care operating expenses, improving its medical cost competitiveness in targeted markets and effectively managing balance sheet exposures. For further discussion of the Company’s actions to manage its balance sheet exposures, see the section on “Run-off Operations” in the Introduction section of Management’s Discussion and Analysis of Financial Condition and Results of Operations (“MD&A”) beginning on page 47.
Details on the Company’s operational strategies are discussed further in the Health Care segment section of the MD&A beginning on page 63 of this Form 10-K.
CIGNA CORPORATION – 2010 Form 10-K – 2
D. Health Care
CIGNA’s Health Care segment (“CIGNA HealthCare”) offers insured and self-insured medical, dental, behavioral health, vision, and prescription drug benefit plans, health advocacy programs and other products and services that may be integrated to provide comprehensive health care benefit programs. CIGNA HealthCare companies offer these products and services in all 50 states, the District of Columbia and the U.S. Virgin Islands.
CIGNA HealthCare believes the most sustainable approach to enhancing quality and managing health care costs is to fully engage individuals in the decisions that affect their health and the health care services they receive. Accordingly, to assist individuals in making informed choices about health care for themselves and their families, CIGNA HealthCare makes available to them actionable information about health and advocacy programs, as well as about the cost and quality of health care services and supplies provided to them.
Underlying CIGNA HealthCare’s operations is a foundation of clinical expertise and an ability to provide quality service. CIGNA HealthCare’s strengths include its ability to:
•
integrate medical and specialty product offerings to achieve a more holistic and integrated approach to individuals’ health that promotes consistent care management; and
•
provide predictive modeling and other analytical tools (for example, through the Company’s exclusive access to analytical tools and algorithms developed by the University of Michigan), to assist in providing targeted outreach and health advocacy by CIGNA’s clinical professionals to CIGNA HealthCare customers.
Principal Products and Services
CIGNA offers a variety of products and services to employers and other groups that sponsor group health plans. With the exception of Health Maintenance Organization (“HMO”), Medicare, Voluntary and stop loss products, each of CIGNA HealthCare’s products is offered with alternative funding options (described below). CIGNA may sell multiple products under the same funding arrangement to the same employer. Accordingly, the revenue table included in the Health Care section of the MD&A beginning on page 63 of this Form 10-K reflects both the product type and funding arrangement. Approximately 80% of medical customers are enrolled in self-insured plans, with the remainder split fairly evenly between guaranteed cost and experience-rated insured plans. Approximately 90% of our medical customers are enrolled in self-insured and experience-rated plans, in which lower medical costs directly benefit our corporate clients and their employees.
CIGNA also offers guaranteed cost medical insurance to individuals; see the “markets and distribution” section for additional information about the Company’s offerings in the individual market.
Commercial Medical
CIGNA HealthCare provides a wide array of products and services to meet the needs of employers, other sponsors of health benefit plans and their plan participants (i.e., employees/customers and their eligible dependents), and individuals, including:
Network and Open Access Plus Plans
CIGNA HealthCare offers a product line of indemnity managed care benefit plans on an insured (guaranteed cost or experience-rated) or self-insured basis. Premiums for insurance policies written on a guaranteed cost or experience-rated basis are reported in the appropriate premium category in the revenue table included in the Health Care section of the MD&A beginning on page 63 of this Form 10-K. For self-insured plans, where a majority of the Company’s customers are enrolled, revenues consist of administrative fees and are included in fees in the revenue table.
These plans use meaningful coinsurance differences to encourage the use of “in-network” versus “out-of-network” health care providers. They also encourage the use of and give customers the option to select a primary care physician and use a national provider network, which is somewhat smaller than the national network used with the preferred provider (“PPO”) plan product line. The Network, Network Open Access, and Open Access Plus In-Network products cover only those services provided by CIGNA HealthCare participating health care professionals (“in-network”) and emergency services provided by non-participating health care professionals (“out-of-network”). The Network point of service (“POS”), Network POS Open Access and Open Access Plus plans (“OAP”) cover health care services provided by participating, and non-participating health care professionals, but the customers’ cost-sharing obligation is generally greater for out-of-network care.
CIGNA CORPORATION – 2010 Form 10-K – 3
Preferred Provider Plans
CIGNA HealthCare also offers a PPO product line that features a national network with even broader access than the Network and Open Access Plans with a somewhat higher medical cost, no option to designate a primary care physician, and in-network and out-of-network coverage with greater member cost-sharing for out-of-network services. Like Network and Open Access Plus Plans, the PPO product line is offered on an insured (guaranteed cost or experience-rated) or self-insured basis, with a majority of the customers being in self-insured plans.
Health Maintenance Organizations
In most states, Commercial and Medicare HMOs are required by law to provide coverage for all basic health services and plans may only be offered on a guaranteed cost basis. They use various tools to facilitate the appropriate use of health care services through employed and/or contracted health care professionals. HMOs control unit costs by negotiating rates of reimbursement with health care professionals and facilities and by requiring advanced authorization for coverage of certain treatments. CIGNA HealthCare offers HMO plans that require customers to obtain all non-emergency services from participating health care professionals as well as POS HMO plans that provide some level of coverage for out-of-network care from non-participating health care professionals and facilities. The out-of-network coverage is generally provided through separate insurance coverage that is sold with the HMO benefits.
Voluntary Plans
CIGNA HealthCare’s voluntary medical products are offered to employers with 51 or more eligible employees and are designed to provide hourly and part-time employees with limited coverage that is more affordable than comprehensive medical plans. CIGNA Voluntary products have annual and, in some cases, lifetime maximums, which are prohibited under the Patient Protection and Affordable Care Act effective September 23, 2010. However, the Department of Health & Human Services (HHS) has approved a one-year waiver of these limitations for plans in effect as of September 23, 2010. CIGNA intends to submit a waiver request for subsequent years through and including 2013. Annual benefit limits are prohibited beginning January 1, 2014.
CIGNA Choice Fund® suite of Consumer-Directed Products
In connection with many of the products described above, CIGNA HealthCare offers the CIGNA Choice Fund suite of consumer-directed products, including Health Reimbursement Arrangements (“HRA”), Health Savings Accounts (“HSA”) and Flexible Spending Accounts (“FSA”).
•
An HRA allows plan sponsors to choose from a variety of benefit plan designs which usually include a high deductible feature and allows employees to fund un-reimbursed health care expenses with reimbursement account funds that can be rolled over from year to year.
•
HSA plans allow plan sponsors to choose from a variety of benefit plan designs and funding options and combine a high deductible payment feature for a health plan with a tax-preferred savings account offering mutual fund investment options. Funds in an HSA can be used to pay the deductible and other eligible tax-deductible medical expenses and can be rolled over from year to year.
•
The HRA and HSA products for employers with generally more than 50 but fewer than 250 employees are now available in 49 states.
•
An FSA pays for certain health care-related expenses, that are either not covered or only partially covered by health care plans, with pre-tax contributions by employees. Unused FSA account funds cannot be rolled over from year to year; they are forfeited by the employee.
Stop Loss Coverage
CIGNA HealthCare offers stop loss insurance coverage for self-insured plans. This stop loss coverage reimburses the plan for claims in excess of a predetermined amount, either for individuals (“specific”) or the entire group (“aggregate”), or both. CIGNA HealthCare also includes stop loss features in its experience-rated policies (discussed below).
Shared Administration Services
CIGNA HealthCare provides Taft-Hartley trusts and other self-insured groups access to its national provider network and provides claim re-pricing and other services (e.g., utilization management).
Medicare
Private Fee For Service
CIGNA’s Medicare Advantage private fee-for-service plan, CIGNA Medicare Access Plan, which was offered by CIGNA through December 31, 2010, was approved by the Centers for Medicare and Medicaid Services (CMS) to be a replacement for Original Medicare. The CIGNA Medicare Access Plan offered the same benefits as Original Medicare Parts A & B, as well as supplemental benefits, including annual physicals, emergency worldwide coverage and health and wellness programs. Beginning on January 1, 2011, CIGNA no longer offers an individual Medicare Private Fee for Service Plan. To meet the needs of Medicare eligible groups desiring this coverage, CIGNA has contracted with Humana Inc. to provide group Medicare Advantage Plans underwritten and issued by Humana and reinsured by CIGNA under a 50% coinsurance agreement.
CIGNA CORPORATION – 2010 Form 10-K – 4
Medicare Part D
CIGNA’s Medicare Part D prescription drug program, CIGNA Medicare Rx®, provides a number of plan options as well as service and information support to Medicare and Medicaid eligible customers. CIGNA Medicare Rx is available in all 50 states and the District of Columbia.
Specialty
Medical Specialty
Health Advocacy
CIGNA HealthCare offers medical management, disease management, and other health advocacy services to employers and other plan sponsors. These services are offered to customers covered under CIGNA HealthCare administered plans, as well as, individuals covered under plans insured and/or administered by competing insurers/third party administrators. CIGNA offers a seamless integration of services to address the clinical and administrative challenges that are inherent in coordinating multiple vendors. Through its health advocacy programs, CIGNA HealthCare works to help: (1) healthy people stay healthy; (2) people change behaviors that are putting their health at risk; (3) people with existing health care issues access quality care and practice healthy self-care; and (4) people with a disabling illness or injury return to productive work quickly and safely.
CIGNA HealthCare offers a wide array of health advocacy programs and services to help individuals improve their health, well-being and sense of security, including:
•
early intervention by CIGNA’s network of clinical professionals;
•
CIGNA’s online health assessment, powered by analytics from the University of Michigan Health Management Research Center, which helps customers identify potential health risks and learn what they can do to live a healthier life;
•
the CIGNA Well Aware for Better Health® program, which helps patients with chronic conditions such as asthma, diabetes, depression and weight complications better manage their conditions;
•
CIGNA Health Advisor®, which provides customers with access to a personal health coach to help them reach their health and wellness goals;
•
CIGNA’s Well Informed program, which uses clinical rules-based software to identify potential gaps and omissions in customers’ health care through analysis of the Company’s integrated medical, behavioral, pharmacy and lab data allowing CIGNA HealthCare to communicate the gaps to the customer and their doctor; and
•
CIGNA’s online coaching capabilities.
CIGNA Onsite Health
CIGNA Onsite Health was formed in 2007. CIGNA operates nine onsite health centers and expects to continue to open additional onsite health clinics. In addition, the Company has expanded onsite services to include onsite pharmacies, dedicated health advocates at employer sites across the country, hourly coaching services and onsite biometric screenings through the acquisition of Kronos Optimal Health. Services and operations are projected to continue to expand throughout 2011 and beyond.
Cost Containment Service
CIGNA administers cost containment programs with respect to health care services/supplies that are covered under benefit plans. These programs, which may involve contracted vendors, are intended to control health costs through the reduction of out-of-network utilization, the auditing of provider bills and recovery of overpayments from other insurance carriers or health care professionals. CIGNA earns fees for providing or arranging these services.
Behavioral Specialty
Behavioral Health
CIGNA arranges for behavioral health care services for individuals through its network of participating behavioral health care professionals and offers behavioral health care management services, employee assistance programs, and work/life programs to employer and other groups sponsoring health benefit plans, HMOs, governmental entities and disability insurers. CIGNA Behavioral Health focuses on integrating its programs and services to facilitate customized, holistic care.
As of December 31, 2010, CIGNA’s behavioral national network had approximately 88,000 access points to independent psychiatrists, psychologists and clinical social workers and approximately 8,500 facilities and clinics that are reimbursed on a contracted fee-for-service basis.
CIGNA CORPORATION – 2010 Form 10-K – 5
CIGNA Pharmacy Management
Pharmacy
CIGNA Pharmacy Management offers prescription drug plans to its insured and self-funded customers both in conjunction with its medical products and on a stand-alone basis. With a nationwide network of over 60,000 contracted pharmacies, CIGNA Pharmacy Management is a comprehensive pharmacy benefits manager (PBM) offering clinical integration programs, specialty pharmacy solutions, and fast, efficient home delivery pharmacy capabilities.
Programs that facilitate this integration of medical, behavioral and pharmacy offerings include: Well Informed, which focuses on the chronic conditions most likely to benefit from disciplined prescription therapy, such as asthma, diabetes, back pain and high cholesterol, as well as Step Therapy, which encourages individuals who take prescription drugs to treat an ongoing medical condition to use generic and/or preferred brand drugs before progressing to higher cost brand-named drugs within the relevant therapeutic drug class. This is accomplished through claim management protocols, which may include communications with the individual and the individual’s physician.
CIGNA Specialty Pharmacy Management
Clients with CIGNA administered medical and pharmacy coverage benefit from better continuity of care, integrated reporting, and aggressive unit cost discounts on all specialty drugs — regardless of where they are administered.
TheraCare Program
CIGNA’s specialty pharmacy outcome management program, TheraCare, takes a unique approach to managing specialty conditions by lowering cost while improving health and satisfaction for our customers. CIGNA has a comprehensive list of conditions covered regardless of the pharmacy used to fill the respective prescription, or under which benefit the prescription falls. TheraCare is coordinated with other CIGNA health advocacy programs and all data is captured for analysis and reporting.
CIGNA Home Delivery Pharmacy
CIGNA also offers cost-effective mail order, telephone and on-line pharmaceutical fulfillment services through its home delivery operation. CIGNA Home Delivery Pharmacy provides an individual-focused, efficient home delivery pharmacy with high standards of quality, accuracy and individual care relating to maintenance and specialty medications. Orders may be submitted through the mail, via phone or through the internet at myCIGNA.com.
Dental Specialty
Dental
CIGNA Dental Health offers a variety of dental care products including dental health maintenance organization plans (“Dental HMO”), dental preferred provider organization (“DPPO”) plans, dental exclusive provider organization plans, traditional dental indemnity plans and a dental discount program. Employers and other groups can purchase CIGNA Dental Health products as stand-alone products or integrated with CIGNA HealthCare’s medical products. As of December 31, 2010, CIGNA Dental Health customers totaled approximately 10.3 million, representing employees at approximately 40% of all Fortune 100 companies. Most of these customers are in self-insured plans, with guaranteed cost and experience-rated insured plans accounting for the remaining membership. All dental HMO customers are in guaranteed cost insured plans. Managed dental care products are offered in 37 states for Dental HMO and 45 states and the District of Columbia for Dental PPO through a network of independent health care professionals that have contracted with CIGNA Dental Health to provide dental services.
CIGNA Dental Health customers access care from one of the largest dental HMO and dental PPO networks in the U.S., with approximately 194,200 DPPO-contracted access points (approximately 84,000 unique health care professionals) and approximately 50,600 dental HMO-contracted access points (approximately 14,900 unique health care professionals).
CIGNA Dental Health stresses preventive dentistry; it believes that promoting preventive care contributes to a healthier workforce, an improved quality of life, increased productivity and fewer treatment claims and associated costs over time. CIGNA Dental Health offers customers a dental treatment cost estimator to educate individuals on oral health and aid them in their dental health care decision-making.
CIGNA CORPORATION – 2010 Form 10-K – 6
Vision Specialty
Vision
CIGNA Vision offers flexible, cost-effective PPO coverage that includes a range of both in and out-of-network benefits for routine vision services. CIGNA’s national vision care network, which consists of over 50,100 health care professionals in approximately 22,300 locations, includes private practice ophthalmologist and optometrist offices, as well as retail eye care centers. Routine vision products are offered in conjunction with CIGNA HealthCare’s medical and dental product offerings.
Funding Arrangements, Pricing, Reserves and Reinsurance
The segment’s health care products and services are offered through the following funding arrangements:
•
Insured — Guaranteed Cost;
•
Insured — Shared ReturnsSM (Experience-rated, including minimum premium funding arrangements); and
•
Administrative Services Only.
Premiums and fees charged for HMO and most health insurance products are generally set in advance of the policy period and are typically guaranteed for one year (unless specified events occur, such as changes in benefits, significant changes in enrollment or laws affecting the coverage or costs). Premium rates for fully insured products are established either on a guaranteed cost or retrospectively experience-rated basis.
Beginning on January 1, 2011, the Patient Protection and Affordable Care Act (“Health Care Reform”) requires CIGNA HealthCare’s comprehensive medical insurance products to meet a minimum medical loss ratio (“MLR”) of 85% for large groups (generally defined as employers with more than 50 employees) and 80% for small groups and individuals. The United States Department of Health and Human Services has issued interim final regulations that specify how the MLR is to be calculated. These regulations currently require the MLR to be calculated on a state-by-state basis for each separate insurance company or HMO, and then separately within each state for large groups, small groups and individuals. The MLR is determined generally by taking the sum of claims plus expenses that improve health care quality and dividing by premiums less taxes and assessments. To the extent the MLR floors are not met for large groups, small groups or individual segments within each state, premium rebates will need to be paid to both employers and customers enrolled in the plans based on the portion of the premium each has contributed. Approximately 20% of CIGNA HealthCare’s customers are enrolled in insured plans, which are subject to the MLR requirements. These requirements are expected to have a greater near-term impact on individual and small group business.
Insured — Guaranteed Cost
Charges to policyholders under an insured, guaranteed cost policy are established at the beginning of the policy period and are not adjusted to reflect actual claim experience during the policy period. Accordingly, CIGNA HealthCare bears the risk for claims and costs. The HMO product is offered only on a guaranteed cost basis. Summarized below are the key elements of an insured, guaranteed cost funding arrangement:
•
A guaranteed cost pricing methodology reflects assumptions about future claims, health care inflation (unit cost, location of delivery of care and utilization), effective medical cost management, expenses, enrollment mix, investment returns, and profit margins.
•
Claim and expense assumptions may be based in whole or in part on prior experience of the policyholder or on a pool of accounts, depending on the policyholder’s size and the statistical credibility of the experience.
•
Generally, guaranteed cost policyholders are smaller and less statistically credible than retrospectively experience-rated groups.
•
Pricing for insurance/HMO products that use networks of contracted health care professionals reflects assumptions about the future claims impact on the reimbursement rates in the provider contracts.
•
Premium rates may vary among policyholders to reflect the underlying plan benefits, anticipated contract and demographic mix, family size, geography, industry, renewal date, and other cost-predictive factors.
•
In some states, premium rates must be approved by the state insurance department and state laws may restrict or limit the use of rating methods.
•
Premium rates for groups and individuals are subject to state and/or HHS review for unreasonable increases.
CIGNA CORPORATION – 2010 Form 10-K – 7
Insured — Shared ReturnsSM (participating, including minimum premium — also referred to as experience rated)
The key features of a Shared Returns funding arrangement are summarized below:
•
If cost experience is favorable in relation to the prospectively determined premium rates, a portion of the initial premiums may be credited to the policyholder as an experience refund. However, if claims and expenses exceed this premium (an “experience deficit”), CIGNA HealthCare generally bears the risk.
•
CIGNA HealthCare may recover an experience deficit, according to contractual provisions, through future premiums and experience settlements, provided the policy remains in force. If premiums exceed claims and expenses, any surplus amount is generally first used to offset prior deficits and otherwise generally returned to the policyholder.
•
As a result of the one-sided nature of the product, a premium that typically includes a margin to partially protect against adverse claim fluctuations is determined at the beginning of the policy period.
•
Such premiums may be adjusted for the actual claim and, in some cases, administrative cost experience of the policyholder through an experience settlement process subsequent to the policy period.
Key features of insurance policies using a minimum premium funding arrangement are summarized below:
•
Minimum premium funding arrangements combine insurance protection with an element of self-funding. The policyholder is responsible for funding all claims up to a predetermined aggregate, maximum monthly amount, and CIGNA HealthCare bears the risk for claim costs incurred in excess of that amount.
•
Instead of paying a fixed monthly premium, the group policyholder establishes and funds a bank account and must maintain an agreed upon amount in the account. The policyholder authorizes the insurer to draw upon funds in the account to pay claims and other authorized expenses.
•
The policyholder pays a significantly reduced monthly “residual” premium while the policy is in effect and a supplemental premium (to cover reserves for run-out claims and administrative expenses) upon termination.
•
As with other Shared Returns (experience-rated) insurance products, CIGNA HealthCare may recover deficits from margins in future years if the policy is renewed.
Liabilities are established for estimated experience refunds based on the results of Shared Returns (retrospectively experience-rated) policies and applicable contract terms. CIGNA HealthCare credits interest on experience refund balances to these policyholders through rates that take investment performance and market rates into consideration. Interest-crediting rates are set at CIGNA HealthCare’s discretion. Higher rates are credited to funds with longer expected payout terms reflecting the fact that higher yields are generally available on investments with longer maturities. For 2010, the rates of interest credited ranged from 1.75% to 4.0%, with a weighted average rate of approximately 2.4%.
Administrative Services Only
CIGNA HealthCare contracts with employers, unions and other groups sponsoring self-insured plans on an administrative services only (“ASO”) basis to administer claims and perform other plan related services. The key features of an ASO funding arrangement are summarized below:
•
CIGNA HealthCare collects administrative service fees in exchange for providing these self-insured plans with access to CIGNA HealthCare’s applicable participating provider network and for providing other services and programs including: claim administration; quality management; utilization management; cost containment; health advocacy; 24-hour help line; 24/7 call center; case management; disease management; pharmacy benefit management; behavioral health care management services (through its provider networks); or any combination of these services.
•
The self-insured plan sponsor is responsible for self-funding all claims, but may purchase stop loss insurance from CIGNA HealthCare or other insurers for claims in excess of a predetermined amount, for either individuals (“specific”), the entire group (“aggregate”), or both.
•
In some cases, CIGNA HealthCare provides performance guarantees associated with meeting certain service related and other performance standards. If these standards are not met, CIGNA HealthCare may be financially at risk up to a stated percentage of the contracted fee or a stated dollar amount. CIGNA HealthCare establishes liabilities for estimated payouts associated with these guarantees. See Note 24 to the Consolidated Financial Statements beginning on page 159 of this Form 10-K for details about these guarantees.
CIGNA CORPORATION – 2010 Form 10-K – 8
Pricing
Premium rates for insured funding arrangements are based on assumptions about the expected utilization levels of medical services, costs of medical services and the Company’s administrative costs. The profitability of these arrangements will vary by the actual utilization level of medical services, the cost of the services provided and the costs to administer the benefit programs. Additionally, overall profitability may be impacted by the implementation of the minimum loss ratio rebates required by Health Care Reform, as potentially favorable experience in a market will generate premium rebates instead of offsetting any unfavorable experience in other markets.
Pricing for self-funded arrangements is generally based on the expected cost to administer those arrangements and will vary by the services provided and the size and complexity of the benefit programs among other factors.
Reserves
In addition to paying current benefits and expenses under HMO and health insurance policies, CIGNA HealthCare establishes reserves for amounts estimated to fund reported claims not yet paid, as well as claims incurred, but not yet reported. As of December 31, 2010, approximately $1.5 billion, or 62% of the reserves of CIGNA HealthCare’s operations comprised liabilities that are likely to be paid within one year, primarily for medical and dental claims, as well as certain group disability and life insurance claims. The reserve amount expected to be paid within one year includes $236 million that is recoverable from certain ASO customers and from minimum premium policyholders. The remaining reserves relate primarily to contracts that are short term in nature, but have long term payouts and include liabilities for group long-term disability insurance benefits and group life insurance benefits for disabled and retired individuals, benefits paid in the form of both life and non-life contingent annuities to survivors and contractholder deposit funds.
Reinsurance
CIGNA HealthCare reduces its exposure to large catastrophic losses under group life, disability and accidental death contracts by purchasing reinsurance from unaffiliated reinsurers.
Financial information, including premiums and fees, is presented in the Health Care section of the MD&A beginning on page 63 and in Note 23 to CIGNA’s Consolidated Financial Statements beginning on page 156 of this Form 10-K.
Service and Quality
Customer Service
CIGNA HealthCare operates 12 service centers that together processed approximately 119 million medical claims in 2010. Satisfying customers is a primary business objective and critical to the Company’s success. To further this objective, in 2009, the Company made its call centers available 24 hours a day, seven days a week. As of December 31, 2010, CIGNA operates seven call centers that customers can call toll-free about their health care benefits, wellness programs and claims.
Technology
CIGNA HealthCare understands the critical importance of information technology to the level of service the Company is able to provide to its customers and to the continued growth of its health care business. The health care marketplace is evolving and the level of service that is acceptable to consumers today may not be acceptable tomorrow. Therefore, CIGNA HealthCare continues to strategically invest in its information technology infrastructure and capabilities including technology essential to fundamental claim administration and customer service, as well as tools and Internet-enabled technology that support CIGNA HealthCare’s focus on engaging customers in health care decisions.
For example, CIGNA HealthCare has developed a range of member decision support tools including:
•
myCIGNA.com, CIGNA’s consumer Internet portal. The portal is personalized with each member’s CIGNA medical, dental and pharmacy plan information;
•
myCignaPlans.com, a website that allows prospective customers to compare plan coverage and pricing options, before enrolling, based on a variety of factors. The application gives customers information on the total health care cost to them and their employer;
•
Health Risk Assessment, an online interactive tool through which customers can identify potential health risks and monitor their health status;
•
a number of interactive online cost and quality information tools that compare hospital quality and efficiency information, prescription drug choices and average price estimates and member-specific average out-of-pocket cost estimates for certain medical procedures; and
•
a special website designed for seniors that offers customized features as well as access to both the myCIGNA.com and cigna.com websites.
CIGNA CORPORATION – 2010 Form 10-K – 9
Benefit/Claim Resolution
CIGNA HealthCare customer service representatives are empowered to immediately resolve a wide range of issues to help customers obtain the most from their benefit plans. If an issue cannot be resolved informally, CIGNA HealthCare has a formal appeals process that can be initiated by telephone or in writing and involves two levels of internal review. For those matters not resolved by internal reviews, CIGNA HealthCare customers are offered the option of a voluntary external review of claims. The CIGNA HealthCare formal appeals process addresses member inquiries and appeals concerning initial coverage determinations based on medical necessity and other benefits/coverage determinations. CIGNA HealthCare’s formal appeals process meets National Committee for Quality Assurance (“NCQA”), Employee Retirement Income Security Act of 1974 (“ERISA”), Utilization Review Accreditation Commission (“URAC”) and/or applicable state regulatory requirements.
Quality Medical Care
CIGNA HealthCare’s commitment to promoting quality medical care to its customers is reflected in a variety of activities including: credentialing medical health care professionals and facilities that participate in CIGNA HealthCare’s managed care and PPO networks as well as developing the CIGNA CareSM specialist physician designation described below.
Participating Provider Network
CIGNA HealthCare has an extensive national network of participating health care professionals which, as of December 31, 2010, consisted of approximately 5,500 hospitals and approximately 640,800 health care professionals as well as other facilities, pharmacies and vendors of health care services and supplies.
In most instances, CIGNA HealthCare contracts directly with the participating hospital, health care professional or other facility to provide covered services to customers at agreed-upon rates of reimbursement. In some instances, however, CIGNA HealthCare companies contract with third parties for access to their provider networks and care management services. In addition, CIGNA HealthCare has entered into strategic alliances with several regional managed care organizations (Tufts Health Plan, HealthPartners, Inc., Health Alliance Plan, and MVP Health Plan) to gain access to their provider networks and discounts.
CIGNA Medical Group
CIGNA Medical Group (CMG) is the multi-specialty medical group practice division of CIGNA HealthCare of Arizona, Inc. which delivers primary care and certain specialty care services through 32 medical facilities and approximately 225 employed clinicians in the Phoenix, Arizona metropolitan area. Eighteen of CMG’s multi-specialty health care centers and their affiliated primary care physicians have received the top level (level 3) of Patient Centered Medical Homes (PCMH) accreditation from NCQA. CMG currently holds the highest level of this accreditation for the greatest number of practices and physicians in the state of Arizona.
CIGNA CareSM
CIGNA Care is a benefit design option available for CIGNA HealthCare administered plans in 64 service areas across the country. CIGNA Care designated physicians are a subset of participating physicians in certain specialties who are designated as CIGNA Care physicians based on specific clinical quality and cost-efficiency selection criteria. Customers pay reduced co-payments or co-insurance when they receive care from a specialist designated as a CIGNA Care provider. CIGNA participating specialists are evaluated annually for the CIGNA Care designation.
Provider Credentialing
CIGNA HealthCare credentials physicians, hospitals and other health care professionals in its participating provider networks using quality criteria which meet or exceed the standards of external accreditation or state regulatory agencies, or both. Typically, most health care professionals are re-credentialed every three years.
External Validation
CIGNA continues to demonstrate its commitment to quality and has expanded its scope of external validation of its quality programs through nationally recognized accreditation organizations. Each of CIGNA’s 23 HMO and POS plans that have undergone an accreditation review has earned Excellent or Commendable status from the NCQA, a private, nonprofit organization dedicated to improving health care quality. In addition, CIGNA’s provider transparency, wellness, utilization management, case management and demand management programs have been awarded the highest outcomes possible. From NCQA, CIGNA earned Physician & Hospital Quality Certification and Wellness and Health Promotion Accreditation. From URAC, an independent, nonprofit health care accrediting organization dedicated to promoting health care quality through accreditation, certification and commendation, CIGNA has full accreditation for Health Utilization Management.
HEDIS® Measures
In addition, CIGNA HealthCare participates in NCQA’s Health Plan Employer Data and Information Set (“HEDIS®”) Quality Compass Report. HEDIS® Effectiveness of Care measures are a standard set of metrics to evaluate the effectiveness of managed care clinical programs. CIGNA HealthCare’s national results compare favorably to industry averages.
CIGNA CORPORATION – 2010 Form 10-K – 10
Accountable Care Organizations
CIGNA has collaborated with a number of Accountable Care organizations in 2010, and expects to continue to expand these arrangements. The overall objective of these organizations is to improve the quality of care and service experience for individuals while lowering costs and improving the overall value for our customers. The goal in collaborating with an Accountable Care organization is to identify health care delivery organizations (medical groups and hospital organizations) that can coordinate end-to-end care for a defined population of patients.
Markets and Distribution
CIGNA HealthCare offers products in the following markets:
•
national accounts, which are multi-site employers generally with more than 5,000 employees;
•
middle market, which is generally defined as multi-site employers with more than 250 but fewer than 5,000 employees, and single-site employers with more than 250 employees;
•
“Select”, which generally includes employers with more than 50 but fewer than 250 employees;
•
small business; CIGNA recently made a strategic business decision to begin withdrawing its insured medical product offering from the Small Group market (defined as employers with two to 50 employees) in the following states by the end of 2011: California, Connecticut, Florida, Georgia, Hawaii, Illinois, Kansas, Missouri, New Hampshire, New York, North Carolina, Ohio, Pennsylvania, South Carolina, Texas and Virginia, as well as Washington, DC. CIGNA will continue to offer insured small group medical policies in Arizona, New Jersey, New Mexico, Tennessee, Vermont and the U.S. Virgin Islands.
•
individuals; CIGNA HealthCare actively markets insurance to individuals in ten states as of December 31, 2010, including Arizona, California, Colorado, Connecticut, Florida, Georgia, North Carolina, South Carolina, Tennessee and Texas.
•
government, which includes federal, state and local governments plans, as well as, primary and secondary schools, and colleges and universities;
•
Taft-Hartley plans, which includes customers covered by union trust funds;
•
seniors, which focuses on the health care needs of individuals 50 years and older;
•
voluntary, which focuses on employers with hourly and part-time employees; and
•
emerging markets, which includes non-CIGNA HealthCare payors to which leased network and other services are offered.
To date, the national and middle markets have comprised a significant amount of CIGNA HealthCare’s business. Following the acquisition of Great-West Healthcare in 2008, the “Select”, and emerging markets now constitute a larger share of CIGNA HealthCare’s business than before the acquisition.
CIGNA HealthCare employs sales representatives to distribute its products and services through insurance brokers and insurance consultants or directly to employers, unions and other groups. CIGNA HealthCare also employs representatives to sell utilization review services, managed behavioral health care and employee assistance services directly to insurance companies, HMOs, third party administrators and employer groups. As of December 31, 2010, the field sales force for the products and services of this segment consisted of approximately 860 sales representatives in approximately 90 field locations.
Competition
CIGNA HealthCare’s business is subject to intense competition, and industry consolidation has created an even more competitive business environment. While no one competitor dominates the health care market nationally, CIGNA HealthCare expects a continuing trend of consolidation in the industry given the current economic and political environment.
In certain geographic locations, some health care companies may have significant market share positions. A large number of health care companies and other entities compete by offering similar products. Competition in the health care market exists both for employers and other groups sponsoring plans and for the employees in those instances where the employer offers its employees a choice of products from more than one health care company. Most group policies are subject to annual review by the policyholder, who may seek competitive quotations prior to renewal.
CIGNA CORPORATION – 2010 Form 10-K – 11
The principal competitive factors are: quality and cost-effectiveness of service and provider networks; effectiveness of medical care management; product responsiveness to the needs of clients and their employees; price; cost-containment services; technology; and effectiveness of marketing and sales. Financial strength of the insurer, as indicated by ratings issued by nationally recognized rating agencies, is also a competitive factor. CIGNA HealthCare believes that its health advocacy capabilities, integrated approach to consumer engagement, breadth of product offerings, clinical care and medical management capabilities and funding options are strategic competitive advantages. These advantages allow CIGNA HealthCare to respond to the diverse needs of its customer base. CIGNA HealthCare also believes that its focus on helping to improve the health, well-being and sense of security of its customers will allow it to distinguish itself from its competitors.
CIGNA HealthCare’s principal competitors are:
•
other large insurance companies that provide group health and life insurance products;
•
Blue Cross and Blue Shield organizations;
•
stand-alone HMOs and PPOs;
•
third-party administrators;
•
HMOs affiliated with major insurance companies and hospitals; and
•
national managed pharmacy, behavioral health and utilization review services companies.
Competition also arises from smaller regional or specialty companies with strength in a particular geographic area or product line, administrative service firms and, indirectly, self-insurers. In addition to these traditional competitors, a new group of competitors is emerging. These new competitors are focused on delivering employee benefits and services through Internet-enabled technology that allows consumers to take a more active role in the management of their health. This is accomplished primarily through financial incentives, access to enhanced medical quality data and other information sharing. The effective use of the Company’s health advocacy capabilities, decision support tools (some of which are web-based) and enabling technology are critical to success in the health care industry, and CIGNA HealthCare believes they will be competitive differentiators.
Industry Developments
In the first quarter 2010, the Patient Protection and Affordable Care Act, including the Reconciliation Act of 2010, was signed into law. Many provisions became effective during 2010 and interim final regulations relating to some provisions have been issued. However there are still many provisions which will become effective in future years and regulations will continue to evolve. For more information concerning health care reform, see “Health Care Reform” in the Introduction section of the MD&A beginning on page 47 and in the Regulation section beginning on page 26.
CIGNA CORPORATION – 2010 Form 10-K – 12
E. Disability and Life
CIGNA’s Disability and Life segment (“CIGNA Disability and Life”) provides the following insurance products and their related services: group long-term and short-term disability insurance, group life insurance and accident and specialty insurance. These products and services are provided by subsidiaries of CIGNA Corporation. CIGNA Disability and Life markets products in all 50 states, the District of Columbia, Puerto Rico, the U.S. Virgin Islands and Canada.
Principal Products and Services
Disability
CIGNA Disability and Life markets group long-term and short-term disability insurance products and services. These products and services generally provide a fixed level of income to replace a portion of wages lost because of disability. CIGNA Disability and Life also provides assistance to the employee in returning to work and assistance to the employer in managing the cost of employee disability. Group disability coverage is typically employer-paid or a combination of employer and employee-paid, but may also include coverage paid for entirely by employees.
CIGNA Disability and Life is an industry leader in returning employees to work quickly. Shorter disability claim durations mean higher productivity and lower cost for employers and a better quality of life for their employees. CIGNA Disability and Life’s disability insurance products may be integrated with other disability benefit programs, behavioral programs, workers’ compensation, medical programs, social security advocacy, and leave of absence administration. CIGNA Disability and Life believes this integration provides customers with increased efficiency and effectiveness in disability claims management, enhances productivity and reduces overall costs to employers. Coordinating the administration of CIGNA Disability and Life’s disability and CIGNA HealthCare’s medical programs may provide enhanced opportunities to influence outcomes, reduce the cost of both medical and disability events and improve the return to work rate. Using information from the CIGNA HealthCare and CIGNA Disability and Life databases helps identify, treat and manage disabilities before they become chronic, longer in duration and more costly. Proactive outreach from CIGNA Behavioral Health assists employees suffering from a mental health condition, either as a primary condition or as a result of another condition. CIGNA may receive fees for providing these integrated services to customers.
Approximately 9,100 insured disability policies covering approximately 5.7 million lives were outstanding as of December 31, 2010.
Life Insurance
Group life insurance products include group term life and group universal life. Group term life insurance may be employer-paid basic life insurance, employee-paid supplemental life insurance or a combination thereof.
CIGNA Disability and Life provides group universal life insurance to employers. Group universal life insurance is a voluntary life insurance product in which the owner may accumulate cash value. The cash value earns interest at rates declared from time to time, subject to a minimum guaranteed contracted rate, and may be borrowed, withdrawn, or, within certain limits, used to fund future life insurance coverage.
Approximately 5,000 group life insurance policies covering approximately 5.1 million lives were outstanding as of December 31, 2010.
Other Products and Services
CIGNA Disability and Life offers personal accident insurance coverage, which consists primarily of accidental death and dismemberment and travel accident insurance to employers. Group accident insurance may be employer-paid or employee-paid.
CIGNA Disability and Life also offers specialty insurance services that consist primarily of disability and life, accident, and medical insurance to professional associations, financial institutions, and participant organizations. Renewal rights to CIGNA’s block of student and participant accident insurance business were sold to an unaffiliated insurer during 2009.
CIGNA CORPORATION – 2010 Form 10-K – 13
Voluntary benefits are those paid by the employee and are offered at the employer’s worksite. CIGNA Disability and Life plans provide employers, among other services, flexible enrollment options, list billing, medical underwriting, and individual record keeping. CIGNA Disability and Life designed its voluntary offerings to offer employers a complete and simple way to manage their benefits, including personalized enrollment communication and administration of the benefits program.
In 2010, CIGNA sold the workers’ compensation and case management services previously provided through its Intracorp® subsidiary. For more information on this sale, see “Acquisitions and Dispositions” in the Introduction section of the MD&A beginning on page 47.
Financial information, including premiums and fees, is presented in the Disability and Life section of the MD&A beginning on page 70 and in Note 23 to CIGNA’s Consolidated Financial Statements beginning on page 156 of this Form 10-K.
Pricing, Reserves and Reinsurance
CIGNA Disability and Life’s products and services are offered on a fully insured, experience-rated and ASO basis. Under fully insured arrangements, policyholders pay a fixed premium and CIGNA Disability and Life bears the risk for claims and costs. Under experience-rated funding arrangements, a premium that typically includes a margin to partially protect against adverse claim fluctuations is determined at the beginning of the policy period. CIGNA Disability and Life generally bears the risk if claims and expenses exceed this premium. If premiums exceed claims and expenses, any surplus amount is generally first used to offset prior deficits and is otherwise generally returned to the policyholder if surplus exceeds minimum contractual levels. With experience-rated insurance products, CIGNA Disability and Life may recover deficits from margins in future years if the policy is renewed. Under ASO arrangements, CIGNA Disability and Life contracts with groups sponsoring self-insured plans to administer claims and perform other plan related services in return for service fees. The self-insured plan sponsor is responsible for self funding all claims. The majority of CIGNA Disability and Life’s products and services are fully insured.
Premiums and fees charged for disability and life insurance products are generally established in advance of the policy period and are generally guaranteed for one to three years and selectively guaranteed for up to five years, but policies can in most cases be subject to early termination by the policyholder or by the insurance company.
Premium rates reflect assumptions about future claims, expenses, credit risk, investment returns and profit margins. Assumptions may be based in whole or in part on prior experience of the account or on a pool of accounts, depending on the group size and the statistical credibility of the experience, which varies by product.
Premiums for group universal life insurance products consist of mortality, administrative and surrender charges assessed against the policyholder’s fund balance. Interest credited and mortality charges for group universal life, and mortality charges on group variable universal life, may be adjusted prospectively to reflect expected interest and mortality experience. Mortality charges are subject to guaranteed maximum rates, based on standard mortality tables, which rates are stated in the policy.
In addition to paying current benefits and expenses, CIGNA Disability and Life establishes reserves in amounts estimated to be sufficient to pay reported claims not yet paid, as well as claims incurred but not yet reported. For liabilities with longer-term pay-out periods such as long-term disability, reserves represent the present value of future expected payments. CIGNA Disability and Life discounts these expected payments using assumptions for interest rates and the length of time over which claims are expected to be paid. The annual effective interest rate assumptions used in determining reserves for most of the long-term disability insurance business is 4.75% for claims that were incurred in 2010 and 5% for claims that were incurred in 2009. For group universal life insurance, CIGNA Disability and Life establishes reserves for deposits received and interest credited to the policyholder, less mortality and administrative charges assessed against the policyholder’s fund balance.
The profitability of this segment’s products depends on the adequacy of premiums charged and investment returns relative to claims and expenses. The effectiveness of return to work programs and mortality levels also impact the profitability of disability insurance products. CIGNA Disability and Life’s previous claim experience and industry data indicate a correlation between disability claim incidence levels and economic conditions, with submitted claims rising under adverse economic conditions, although the impact of the current adverse economic conditions is not clear. For life insurance products, the degree to which future experience deviates from mortality, morbidity and expense assumptions also affects profitability.
In order to reduce its exposure to large individual and catastrophic losses under group life, disability and accidental death policies, CIGNA Disability and Life purchases reinsurance from unaffiliated reinsurers.
CIGNA CORPORATION – 2010 Form 10-K – 14
Markets and Distribution
CIGNA Disability and Life markets the group insurance products and services described above to employers, employees, professional and other associations and groups in the following customer segments:
•
national accounts, which are multi-site employers generally with more than 5,000 employees;
•
middle market, which is generally defined as multi-site employers with more than 250 but fewer than 5,000 employees, and single-site employers with more than 250 employees; and
•
select, which generally includes employers with more than 50 but fewer than 250 employees.
In marketing these products, CIGNA Disability and Life primarily sells through insurance brokers and consultants and employs a direct sales force. As of December 31, 2010, the field sales force for the products and services of this segment consisted of approximately 200 sales professionals in 27 office locations.
Competition
The principal competitive factors that affect the CIGNA Disability and Life segment are underwriting and pricing, the quality and effectiveness of claims management, relative operating efficiency, investment and risk management, distribution methodologies and producer relations, the breadth and variety of products and services offered, and the quality of customer service.
For certain products with longer-term liabilities, such as group long-term disability insurance, the financial strength of the insurer, as indicated by ratings issued by nationally recognized rating agencies, is also a competitive factor.
The principal competitors of CIGNA’s group disability, life and accident businesses are other large and regional insurance companies that market and distribute these or similar types of products.
As of December 31, 2010, CIGNA is one of the top five providers of group disability, life and accident insurance in the United States, based on premiums.
Industry Developments and Strategic Initiatives
The group insurance market remains highly competitive as the rising cost of providing medical coverage to employees has forced companies to re-evaluate their overall employee benefit spending. Demographic shifts have further driven demand for products and services that are sufficiently flexible to meet the evolving needs of employers and employees who want innovative, cost-effective solutions to their insurance needs. Employers continue to shift towards greater employee participatory coverage and voluntary purchases.
Employers are also expressing a growing interest in employee wellness, absence management and productivity and recognizing a strong link between health, productivity and their profitability. CIGNA is well-positioned to offer employers programs that promote a healthy lifestyle, offer assistance in returning to work and integrate health care and disability programs. CIGNA believes it is well positioned to deliver integrated solutions that address these broad employer and employee needs. CIGNA also believes that its strong disability management portfolio and fully integrated programs provide employers and employees tools to improve health status. This focus on managing the employee’s total absence enables CIGNA to increase the number and likelihood of interventions and minimize disabling events.
CIGNA CORPORATION – 2010 Form 10-K – 15
F. International
CIGNA’s International segment (“CIGNA International”) offers supplemental health, life and accident insurance products as well as international health care products and services. These products and services are provided by subsidiaries of CIGNA Corporation, including foreign operating entities.
CIGNA International provides employers, affinity groups and individuals with quality local and global health care and related financial protection programs. With local licenses in over 27 countries and jurisdictions, CIGNA International offers products and services to both local citizens and globally mobile individuals. CIGNA International services expatriates virtually everywhere in the world.
Principal Products and Services
Supplemental Health, Life and Accident Insurance
CIGNA International’s supplemental health, life and accident insurance products generally provide simple, affordable coverage of risks for the health and financial security of individuals. Supplemental health products provide a specified payment for a variety of health risks and include personal accident, accidental death, critical illness, hospitalization, dental, cancer and other dread disease coverages. Term life as well as variable universal life insurance and other savings products are also included in the product portfolio. CIGNA International’s supplemental health, life and accident insurance products are offered in South Korea, Taiwan, Indonesia, Hong Kong, the European Union, China, New Zealand and Thailand.
International Health Care
CIGNA International’s health care businesses primarily consist of products and services to meet the needs of multinational companies and their expatriate employees and dependents. These products and services include insurance and administrative services for medical, dental, vision, life, accidental death and dismemberment, and disability risks. The expatriate benefits products and services are offered through guaranteed cost, experience-rated, administrative services only, and minimum premium funding arrangements. For definitions of funding arrangements, see “Funding Arrangements” in Section D beginning on page 3 of this Form 10-K. The customers of CIGNA International’s expatriate benefits business are multinational companies and intergovernmental and non-governmental organizations, headquartered in the United States, Canada, Europe, the Middle East, Hong Kong, China and other international locations. The acquisition of Vanbreda International, in the third quarter of 2010, further strengthens CIGNA International’s position in this market.
In addition, CIGNA International’s health care businesses include products and services which are primarily provided through group benefits programs to employees of businesses and other organizations in the United Kingdom and Spain. These products and services include medical indemnity insurance coverage, with some offerings having managed care or administrative service aspects. These products and services generally provide an alternative or supplement to government provided national health care programs.
In 2010, CIGNA International began offering individual private medical insurance to local citizens in Spain as well as to individual expatriates and globally mobile high net worth individuals. Local, regional or global coverage is available to these groups, adapted to local market conditions.
Financial information, including premiums and fees, is presented in the International section of the MD&A beginning on page 72 and in Note 23 to CIGNA’s Consolidated Financial Statements beginning on page 156 of this Form 10-K.
Pricing, Reserves and Reinsurance
Premium rates for CIGNA International’s supplemental health, life and accident insurance products are based on assumptions about mortality, morbidity, customer acquisition and retention, expenses and target profit margins, as well as interest rates. The profitability of these products is primarily driven by mortality, morbidity, and customer retention.
Fees for variable universal life insurance products consist of mortality, administrative, asset management and surrender charges assessed against the contractholder’s fund balance. Mortality charges on variable universal life may be adjusted prospectively to reflect expected mortality experience.
CIGNA CORPORATION – 2010 Form 10-K – 16
Premium rates and fees for CIGNA International’s health care products reflect assumptions about future claims, expenses, customer demographics, investment returns, and profit margins. For products using networks of contracted health care professionals and facilities, premiums reflect assumptions about the impact of these contracts and utilization management on future claims. Most of the premium volume for the medical indemnity business is on a guaranteed cost basis. Other premiums are established on an experience-rated basis. Most contracts permit rate changes at least annually.
The profitability of health care products is dependent upon the accuracy of projections for health care inflation (unit cost, location of delivery of care, currency of incurral and utilization), customer demographics, the adequacy of fees charged for administration and effective medical cost management.
In addition to paying current benefits and expenses, CIGNA International establishes reserves in amounts estimated to be sufficient to settle reported claims not yet paid, claims incurred but not yet reported as well as future amounts payable on experience-rated arrangements. Additionally, for some individual life insurance and supplemental health insurance products, CIGNA International establishes policy reserves which reflect the present value of expected future obligations less the present value of expected future premiums attributable to policyholder obligations. CIGNA International defers acquisition costs, such as commissions, telemarketing, direct response marketing and policy fulfillment costs, incurred in the sales of multi-year supplemental health, life, and accident products. For most products, these costs are amortized in proportion to premium revenue recognized, which is impacted by customer retention. For variable universal life products, acquisition costs are amortized in proportion to expected gross profits.
CIGNA International’s operations are diversified by line of business and geographic spread of risk. However, South Korea does represent the single largest geographic market for CIGNA International. A global approach to underwriting risk management allows for each local business to underwrite and accept risk within specified limits. Retentions are centrally managed through cost effective use of external reinsurance to limit segment liability on a per life, per risk, and per event (catastrophe) basis.
Markets and Distribution
CIGNA International’s supplemental health, life and accident insurance products are generally marketed through distribution partners with whom the individual insured has an affinity relationship. These products are sold primarily through direct marketing channels, such as outbound telemarketing and in-branch bancassurance. Marketing campaigns are conducted through these channels under a variety of arrangements with affinity partners. These affinity partners primarily include banks, credit card companies and other financial institutions. CIGNA International also distributes directly to consumers via direct response television and the Internet. CIGNA International’s supplemental health, life and accident insurance businesses are located in South Korea, Taiwan, the European Union, Hong Kong, Indonesia, China, New Zealand and Thailand. In China, CIGNA International owns a 50% interest in a joint venture through which its products and services are offered.
CIGNA International’s health care products are distributed through independent brokers and consultants, select partners, CIGNA International’s own sales personnel, telemarketing and the Internet. The customers of CIGNA International’s expatriate benefits business are multinational companies and international organizations headquartered in the United States, Canada, Europe, the Middle East, Hong Kong, China and other international locations. In addition, CIGNA International’s health care businesses include medical products, which are provided through group and individual benefits programs in the United Kingdom and Spain as well as to individual expatriates and high net worth globally mobile individuals.
For CIGNA International’s supplemental health, life and accident insurance products, a significant portion of premiums are billed and collected through credit cards. A substantial contraction in consumer credit could impact CIGNA International’s ability to retain existing policies and sell new policies. A decline in customer retention would result in both a reduction of revenue and an acceleration of the amortization of acquisition related costs. Changes in regulation around permitted distribution channels may also impact CIGNA International’s business or results. See the Regulation section beginning on page 26 and the Risk Factors section beginning on page 33 of this Form 10-K.
In 2010, South Korea generated 32% of CIGNA International’s revenues and 49% of its segment earnings. For information on the concentration of risk with respect to CIGNA International’s business in South Korea, see “Other Items Affecting International Results” in the International section of the MD&A beginning on page 72 of this Form 10-K.
CIGNA CORPORATION – 2010 Form 10-K – 17
Competition
Competitive factors in CIGNA International’s supplemental health, life and accident and health care businesses include product and distribution innovation and differentiation, efficient management of marketing processes and costs, commission levels paid to distribution partners, and quality of claims and customer services.
The principal competitive factors that affect CIGNA International’s health care businesses are underwriting and pricing, relative operating efficiency, relative effectiveness in network development and medical cost management, product innovation and differentiation, broker relations, and the quality of claims and customer service. In most overseas markets, perception of financial strength is also an important competitive factor.
For the supplemental health, life and accident insurance line of business, competitors are primarily locally based insurance companies, including insurance subsidiaries of banks primarily in Asia and Europe. Insurance company competitors in this segment primarily focus on traditional product distribution through captive agents, with direct marketing being secondary channels. CIGNA International estimates that it has less than 2% market share of the total life insurance premiums in any given market in which it operates.
The primary competitors of the expatriate benefits business include U.S.-based and European health insurance companies with global expatriate benefits operations. For the health care operations in the United Kingdom and Spain, the primary competitors are regional and local insurers, with CIGNA’s market share at less than 5% of the premiums of the total local health care market.
CIGNA International expects that the competitive environment will intensify as U.S. and Europe-based insurance and financial services providers pursue global expansion opportunities.
Industry Developments
Pressure on social health care systems and increased wealth and education in emerging markets are leading to higher demand for products providing health insurance and financial security. In the supplemental health, life and accident business, direct marketing channels are growing and attracting new competitors while industry consolidation among financial institutions and other affinity partners continues. Increased regulations requiring foreign workers to show proof of health insurance are creating opportunities for CIGNA International’s health care businesses. See “Risk Factors” beginning on page 33 of this Form 10-K for a discussion of risks related to CIGNA International.
CIGNA CORPORATION – 2010 Form 10-K – 18
G. Run-off Reinsurance
Principal Products and Services
Until 2000, CIGNA offered reinsurance coverage for part or all of the risks written by other insurance companies (or “ceding companies”) under life and annuity policies (both group and individual) and accident policies (workers’ compensation, personal accident, and catastrophe coverages). The products and services related to these operations were offered by subsidiaries of CIGNA Corporation.
In 2000, CIGNA sold its U.S. individual life, group life and accidental death reinsurance businesses. CIGNA placed its remaining reinsurance businesses (including its accident, international life, and annuity reinsurance businesses) into run-off as of June 1, 2000, and stopped underwriting new reinsurance business.
On December 31, 2010, the Company essentially exited from its workers’ compensation and personal accident reinsurance business by purchasing retrocessional coverage from a Bermuda subsidiary of Enstar Group Limited and transferring administration of this business to the reinsurer. See Note 3 to the Consolidated Financial Statements beginning on page 112 for more information.
CIGNA’s remaining exposures stem primarily from its annuity reinsurance business, including its reinsurance of guaranteed minimum death benefits (“GMDB”) and guaranteed minimum income benefits (“GMIB”) contracts.
Life and Annuity Policies
Guaranteed Minimum Death Benefit Contracts
CIGNA’s reinsurance segment reinsured GMDB (also known as variable annuity death benefits (“VADBe”)), under certain variable annuities issued by other insurance companies. These variable annuities are essentially investments in mutual funds combined with a death benefit. CIGNA has equity and other market exposures as a result of this product. The Company purchased retrocessional protection that covers approximately 5% of the assumed risks. The Company also maintains a dynamic hedge program (“GMDB equity hedge program”) to substantially reduce the equity market exposures relating to GMDB contracts by entering into exchange-traded futures contracts.
For additional information about GMDB contracts, see “Guaranteed Minimum Death Benefits” under Run-off Reinsurance section of the MD&A beginning on page 75 and Note 7 to CIGNA’s Consolidated Financial Statements beginning on page 116 of this Form 10-K.
Guaranteed Minimum Income Benefit Contracts
In certain circumstances where CIGNA’s reinsurance operations reinsured the GMDB, CIGNA also reinsured GMIB under certain variable annuities issued by other insurance companies. These variable annuities are essentially investments in mutual funds combined with minimum income and death benefits. All reinsured GMIB policies also have a GMDB benefit reinsured by the Company. When annuitants elect to receive these minimum income benefits, CIGNA may be required to make payments which will vary based on changes in underlying mutual fund values and interest rates. CIGNA has retrocessional coverage for 55% of the exposures on these contracts, provided by two external reinsurers.
For additional information about GMIB contracts, see “Guaranteed Minimum Income Benefits” under Run-off Reinsurance section of the MD&A beginning on page 75 and Note 11 to CIGNA’s Consolidated Financial Statements beginning on page 127 of this Form 10-K.
CIGNA CORPORATION – 2010 Form 10-K – 19
Markets and Distribution
These products under CIGNA’s Run-off Reinsurance segment were sold principally in North America and Europe through a small sales force and through intermediaries.
CIGNA also purchased reinsurance to reduce the risk of losses on contracts that it had written. CIGNA determines its net exposure for run-off reinsurance contracts by estimating the portion of its policy and claim reserves that it expects will be recovered from its reinsurers (or “retrocessionaires”) and reflecting these in its financial statements as Reinsurance recoverables, or, with respect to GMIB contracts discussed above, as Other assets including other intangibles.
Other Risks
For more information on policy and claim reserves see the Run-off Reinsurance section of the MD&A beginning on page 75, and Notes 8 and 11 to CIGNA’s Consolidated Financial Statements beginning on pages 119 and 127 respectively of this Form 10-K. For more information on the risk associated with Run-off Reinsurance, see the Risk Factors beginning on page 33 of this Form 10-K, and the Critical Accounting Estimates section of the MD&A beginning on page 57 of this Form 10-K.
CIGNA CORPORATION – 2010 Form 10-K – 20
H. Other Operations
CIGNA’s Other Operations segment includes the following businesses:
•
corporate owned life insurance;
•
deferred gains recognized from the 1998 sale of the individual life insurance and annuity business and the 2004 sale of the retirement benefits business; and
•
run-off settlement annuity business.
The products and services related to these operations are offered by subsidiaries of CIGNA Corporation.
Corporate-owned Life Insurance (“COLI”)
Principal Products and Services
The principal products of the COLI business are permanent insurance contracts sold to corporations to provide coverage on the lives of certain of their employees for the purpose of funding employer-paid future benefit obligations. Permanent life insurance provides coverage that, when adequately funded, does not expire after a term of years. The contracts are primarily non-participating universal life policies.
Universal life policies typically provide flexible coverage and flexible premium payments. Policy cash values fluctuate with the amount of the premiums paid, mortality and expense charges assessed, and interest credited to the policy. Variable universal life policies are universal life contracts in which the cash values vary directly with the performance of a specific pool of investments underlying the policy.
The principal services provided by the COLI business are issuance and administration of the insurance policies (e.g., maintenance of records regarding cash values and death benefits, claims processing, etc.) as well as oversight of the investment management for separate account assets that support the variable universal life product.
Product Features
COLI policies provide a death benefit for which CIGNA collects fees to cover mortality risk and pay death benefits. Mortality risk is retained according to guidelines established by CIGNA. To the extent a given policy carries mortality risk that exceeds these guidelines, reinsurance is purchased from third parties for the balance. COLI policies also allow the policy owner to borrow against a portion of their cash surrender value.
Cash values on universal life policies are credited interest at a declared interest rate that reflects the anticipated investment results of the assets backing these policies and may vary with the characteristics of each product. Universal life policies generally have a minimum guaranteed declared interest rate which may be cumulative from the issuance date of the policy. The declared interest rate may be changed monthly, but is generally changed less frequently.
Cash values on variable universal life policies vary directly with the performance of a specific pool of investments underlying the policy. A limited number of variable universal life policies guarantee that the realized investment performance for a quarter, excluding the impact of unrealized gains/losses and the impact of credit-related events, will not be negative.
Pricing, Reserves, and Reinsurance
Fees for universal life insurance products consist of mortality, administrative and surrender charges assessed against the policyholder’s fund balance. Interest credited and mortality charges for universal life and mortality charges on variable universal life may be adjusted prospectively to reflect expected interest and mortality experience. For universal life insurance, CIGNA establishes reserves for deposits received and interest credited to the contractholder, less mortality and administrative charges assessed against the contractholder’s fund balance. In order to reduce its exposure to large individual and catastrophe losses, CIGNA purchases reinsurance from unaffiliated reinsurers.
CIGNA CORPORATION – 2010 Form 10-K – 21
Markets and Distribution
The Company is actively developing and enhancing its product portfolio to pursue new business. The principal markets for COLI products are regional to national account-sized corporations, including banks. CIGNA’s COLI products are offered through a select group of independent brokers with particular expertise in the bank market and in the use of COLI for the financing of benefit plan liabilities.
Competition
The principal competitive factors that affect CIGNA’s COLI business are pricing, service, product innovation and access to third-party distribution. For CIGNA’s COLI business, competitors are primarily major life insurance companies. CIGNA expects that the competitive environment will intensify as the economy recovers and competitors develop new investment strategies and product designs, and aggressively price their offerings to build distribution capacity and gain market share.
Industry Developments and Strategic Initiatives
The COLI regulatory environment continues to evolve, with various Federal budget related proposals recommending changes in policyholder tax treatment. In addition, provisions of the Dodd-Frank financial reform legislation may limit the ability of some financial institutions to hold certain types of COLI contracts. Although regulatory and legislative activity could adversely impact our business and policyholders, management does not expect the impact to materially affect the Company’s results of operations, liquidity or financial condition.
Individual Life Insurance & Annuity and Retirement Benefits Businesses
CIGNA sold its individual life insurance and annuity business in 1998 and its retirement benefits business in 2004. Portions of the gains from these sales were deferred because the principal agreements to sell these businesses were structured as reinsurance arrangements. The deferred portion relating to the remaining reinsurance is being recognized at the rate that earnings from the sold businesses would have been expected to emerge, primarily over 15 years on a declining basis.
For more information regarding the sale of these businesses and the arrangements which secure CIGNA’s reinsurance recoverables, see Note 8 of the Consolidated Financial Statements beginning on page 119 of this Form 10-K.
Settlement Annuity Business
CIGNA’s settlement annuity business is a run-off block of contracts. These contracts are primarily liability settlements with approximately 34% of the liabilities associated with payments that are guaranteed and not contingent on survivorship. In the case of the contracts that involve non-guaranteed payments, such payments are contingent on the survival of one or more parties involved in the settlement.
The settlement annuities business is premium deficient, meaning initial premiums were not sufficient to cover all claims and profit. Liabilities are estimates of the present value of benefits to be paid less the present value of investment income generated by the assets supporting the product including realized and unrealized capital gains. The Company estimates these liabilities based on assumptions for investment yields, mortality, and administrative expenses. Refer to Note 2 to CIGNA’s Consolidated Financial Statements beginning on page 103 of this Form 10-K for additional information regarding reserves for this business.
CIGNA CORPORATION – 2010 Form 10-K – 22
I. Investments and Investment Income
CIGNA’s investment operations provide investment management and related services primarily for CIGNA’s corporate invested assets and the insurance-related invested assets in its General Account (“General Account Invested Assets”). CIGNA acquires or originates, directly or through intermediaries, various investments including private placements, public securities, commercial mortgage loans, real estate, mezzanine and private equity partnerships, policy loans and short-term investments. CIGNA’s General Account Invested Assets are managed primarily by CIGNA subsidiaries and external managers with whom CIGNA’s subsidiaries contract.
The General Account Invested Assets comprise a majority of the combined assets of the Health Care, Disability and Life, Run-off Reinsurance and Other Operations segments (collectively, the “Domestic Portfolios”). There are, in addition, portfolios containing Invested Assets that consist of the assets of the International segment (collectively, the “International Portfolios”). Additionally, CIGNA subsidiaries or external managers manage Separate Account assets on behalf of contractholders. These assets are legally segregated from the Company’s other businesses and are not included in the General Account Invested Assets. Income, gains and losses generally accrue directly to the contractholders.
Net investment income and realized investment gains (losses) are not reported separately in the investment operations. Instead, net investment income is included as a component of earnings for each of CIGNA’s operating segments (Health Care, Disability and Life, Run-off Reinsurance, Other Operations and International) and Corporate, net of the expenses attributable to the investment operations. Realized investment gains (losses) are reported for each of CIGNA’s operating segments.
CIGNA’s General Account Invested Assets under management at December 31, 2010 totaled $20.9 billion. See Schedule I to CIGNA’s Consolidated Financial Statements on page FS-3 of this Form 10-K for more information as to the allocation to types of investments.
In addition, as of December 31, 2010, CIGNA’s Separate Account assets consisted of:
•
$1.3 billion in separate account assets that are managed by the buyer of the retirement benefits business pursuant to reinsurance arrangements described in the Sales of Individual Life Insurance & Annuity and Retirement Benefits Businesses sections in Note 3 to the Consolidated Financial Statements beginning on page 112 of this Form 10-K;
•
$2.8 billion in separate account assets, which constitute a portion of the assets of the CIGNA Pension Plan; and
•
$3.8 billion in separate account assets, which primarily support certain corporate-owned life insurance, health care and disability and life products.
Types of Investments
CIGNA invests in a broad range of asset classes, including domestic and international fixed maturities and common stocks, commercial mortgage loans, real estate, mezzanine and private equity partnerships and short-term investments. Fixed maturity investments include publicly traded and private placement corporate bonds, state, local and federal government bonds, publicly traded and private placement asset-backed securities, and redeemable preferred stocks. In addition, investment assets include policy loans which are collateralized by insurance policy cash values.
For the International Portfolios, CIGNA invests primarily in publicly traded fixed maturities, short-term investments and time deposits denominated in the currency of the relevant liabilities and surplus.
Fixed Maturities
CIGNA’s fixed maturities are 92% investment grade as determined by external rating agencies (for public investments) and by CIGNA (for private investments). These assets are well diversified by individual holding and industry sector. For additional information about fixed maturities, see the “Investment Assets” section of the MD&A beginning on page 88 of this Form 10-K.
CIGNA CORPORATION – 2010 Form 10-K – 23
Commercial Mortgages and Real Estate
Commercial mortgage loan investments are subject to underwriting criteria addressing loan-to-value ratio, debt service coverage, cash flow, tenant quality, leasing, market, location and borrower’s financial strength. Such investments consist primarily of first mortgage loans on primarily completed and substantially leased commercial properties and are diversified by property type, location and borrower. Virtually all of CIGNA’s commercial mortgage loans are balloon payment loans, under which all or a substantial portion of the loan principal is due at the end of the loan term. The weighted average loan-to-value ratio of the Company’s commercial mortgage loan portfolio, based on management’s annual valuation completed in the third quarter of 2010 along with updates for subsequent portfolio activity, was approximately 74% and the weighted average debt service coverage was estimated to be 1.38. CIGNA holds no direct residential mortgage loans and does not securitize or service mortgage loans.
CIGNA enters into joint ventures with local partners to develop, lease, manage, and sell commercial real estate to maximize investment returns. CIGNA’s portfolio of real estate investments consists of properties under development and stabilized properties, and is diversified relative to property type and location. Additionally, CIGNA invests in third-party sponsored real estate funds to maximize investment returns and to maintain diversity with respect to its real estate related exposure.
CIGNA also could take possession of real estate through foreclosure of delinquent commercial mortgage loans. CIGNA rehabilitates, re-leases, and sells foreclosed properties, a process that usually takes from three to five years unless management considers a near-term sale preferable. As of December 31, 2010, CIGNA held one foreclosed property with a carrying value of $59 million.
Mezzanine and Private Equity Partnerships
CIGNA invests in limited partnership interests in partnerships formed and managed by seasoned, experienced fund managers with diverse mezzanine and private equity strategies.
Derivative Instruments
The Company uses derivative financial instruments primarily as part of a strategy to reduce the equity market exposures relating to guaranteed minimum death benefit contracts. Derivative financial instruments are also used by the Company as a part of its investment strategy to manage the characteristics of investment assets to meet the varying demands of the related insurance and contractholder liabilities. CIGNA has also written derivative instruments to minimize certain insurance customers’ market risks. For information about CIGNA’s use of derivative financial instruments, see Note 13 to CIGNA’s Consolidated Financial Statements beginning on page 142 of this Form 10-K.
See also the “Investment Assets” section of the MD&A beginning on page 88, and Notes 2, 11, 12, 14, and 15 to the Consolidated Financial Statements beginning on pages 103, 127, 136, 145, and 145, respectively, of this Form 10-K for additional information about CIGNA’s investments.
Domestic Portfolios — Investment Strategy
As of December 31, 2010, the Domestic Portfolios had $19.0 billion in General Account Invested Assets, allocated among fixed maturity investments (68%); commercial mortgage loan investments (18%); and policy loans, real estate investments, short-term investments and mezzanine and private equity partnership investments (14%).
CIGNA’s objective is to maximize risk-adjusted yields for the portfolios while generally managing the characteristics of these assets to reflect the underlying characteristics of related insurance and contractholder liabilities and capital requirements, as well as regulatory and tax considerations pertaining to those liabilities and state investment laws. CIGNA’s domestic insurance and contractholder liabilities as of December 31, 2010, excluding liabilities of businesses sold through the use of reinsurance arrangements, were associated with the following products, and the General Account Invested Assets are allocated proportionally as follows: other life and health, 51%; fully guaranteed annuity, 19%; and interest-sensitive life insurance, 30%.
CIGNA CORPORATION – 2010 Form 10-K – 24
While the businesses and products supported are described elsewhere in this Form 10-K, the General Account Invested Assets supporting the insurance and contractholder liabilities of each of the Company’s segments are as follows:
•
assets supporting CIGNA’s Health Care segment are structured to emphasize investment income, and provide the necessary liquidity to meet cash flow requirements.
•
assets supporting CIGNA’s Disability and Life segment are also structured to emphasize investment income, and provide necessary liquidity to meet cash flow requirements. Invested Assets supporting longer-term group disability insurance benefits and group life waiver of premium benefits are generally managed to an aggregate duration similar to that of the related benefit cash flows.
•
assets supporting the Run-off Reinsurance segment with respect to reinsurance provided for guaranteed minimum death benefit contracts and guaranteed minimum income benefit contracts are structured to emphasize investment income and provide the necessary liquidity to meet cash flow requirements. For information about CIGNA’s use of derivative financial instruments in the Run-off Reinsurance segment, see Notes 7 and 11 to CIGNA’s Consolidated Financial Statements beginning on pages 116 and 127 of this Form 10-K.
•
assets supporting CIGNA’s Other Operations segment are associated primarily with fully guaranteed annuities (primarily settlement annuities) and interest-sensitive life insurance (primarily corporate-owned life insurance products). Because settlement annuities generally do not permit withdrawal by policyholders prior to maturity, the amount and timing of future benefit cash flows can be reasonably estimated so funds supporting these products are invested in fixed income investments whose aggregate duration generally matches the cash flows of the related benefits. As of December 31, 2010, the average duration of assets that supported these liabilities was approximately 12 years. General Account Invested Assets supporting interest-sensitive life insurance products are primarily fixed income investments and policy loans. Fixed income investments emphasize investment yield while meeting the liquidity requirements of the related liabilities.
Investment strategy and results are affected by the amount and timing of cash available for investment, competition for investments, economic conditions, interest rates and asset allocation decisions. CIGNA routinely monitors and evaluates the status of its investments, obtaining and analyzing relevant investment-specific information as well as assessing current economic conditions, trends in capital markets and other factors. Such factors include industry sector considerations for fixed maturity investments and mezzanine and private equity partnership investments, and geographic and property-type considerations for commercial mortgage loan and real estate investments.
International Portfolios — Investment Strategy
As of December 31, 2010 the International Portfolios had $1.9 billion in Invested Assets, allocated among fixed maturity investments (93%), short-term investments (5%) and other investments (2%). The International Portfolios are primarily managed by external managers with whom CIGNA’s subsidiaries contract.
The characteristics of these assets are generally managed to reflect the underlying characteristics of related insurance and contractholder liabilities, as well as regulatory and tax considerations in the countries where CIGNA’s subsidiaries operate. CIGNA International’s Invested Assets are generally invested in the currency of related liabilities, typically the currency in which the subsidiaries operate and with an aggregate duration generally matching the duration of insurance liabilities. CIGNA’s investment policy allows the investment of subsidiary assets in U.S. dollars to the extent permitted by applicable regulation. CIGNA International’s Invested Assets as of December 31, 2010 were held primarily in support of statutory surplus and liabilities associated with the health, life and accident and healthcare products described in Section F on page 16 of this Form 10-K.
CIGNA CORPORATION – 2010 Form 10-K – 25
J. Regulation
CIGNA and its subsidiaries are subject to comprehensive federal, state and international regulations. The laws and regulations governing CIGNA’s business continue to increase each year and are subject to frequent change. CIGNA has established policies and procedures to comply with applicable requirements.
CIGNA’s insurance and HMO subsidiaries must be licensed by the jurisdictions in which they conduct business. These subsidiaries are subject to numerous state and federal regulations related to their business operations, including, but not limited to:
•
the form and content of customer contracts including benefit mandates (including special requirements for small groups, generally under 50 employees);
•
premium rates;
•
the content of agreements with participating providers of covered services;
•
producer appointment and compensation;
•
claims processing and appeals;
•
underwriting practices;
•
reinsurance arrangements;
•
unfair trade and claim practices;
•
protecting the privacy and confidentiality of the information received from members;
•
risk sharing arrangements with providers;
•
medical loss ratios;
•
advertising; and
•
the operation of consumer-directed plans (including health savings accounts, health reimbursement accounts, flexible spending accounts and debit cards).
CIGNA and its international subsidiaries comply with regulations in international jurisdictions where foreign insurers may be faced with more onerous regulations than their domestic competitors. The broader regulatory environment may include anti-corruption laws, various privacy, insurance, tax, tariff and trade laws and regulations, corporate governance, employment, intellectual property and investment laws and regulation, discriminatory licensing procedures, compulsory cessions of reinsurance, required localization of records and funds, higher premium and income taxes, and requirements for local participation in an insurer’s ownership. In addition, the expansion of CIGNA’s operations into foreign countries increases the Company’s exposure to certain U.S. laws, such as the Foreign Corrupt Practices Act of 1977 (FCPA). See page 29 for further discussion of international regulations.
The business of administering and insuring employee benefit programs, particularly health care programs, is heavily regulated by state and federal laws and administrative agencies, such as state departments of insurance and the federal departments of Labor, Health and Human Services and Justice, the Internal Revenue Service as well as the courts. Health savings accounts, health reimbursement accounts and flexible spending accounts are also regulated by the U.S. Department of the Treasury and the Internal Revenue Service.
CIGNA’s operations, accounts and other books and records are subject to examination at regular intervals by regulatory agencies, including state health, insurance and managed care departments, state boards of pharmacy and the Center for Medicare & Medicaid Services to assess compliance with applicable laws and regulations. In addition, CIGNA’s current and past business practices are subject to review by, and from time to time the Company receives subpoenas and other requests of information from, various state insurance and health care regulatory authorities, attorneys general, the Office of Inspector General, and other state and federal authorities, including inquiries by, and testimony before committees and subcommittees of the U.S. Congress regarding certain of its business practices. These examinations, reviews, subpoenas and requests may result in changes to or clarifications of CIGNA’s business practices, as well as fines, penalties or other sanctions.
CIGNA CORPORATION – 2010 Form 10-K – 26
Regulatory and Legislative Developments
The federal and state governments in the U.S. as well as governments in other countries where CIGNA does business continue to enact and seriously consider many broad-based legislative and regulatory proposals that could materially impact various aspects of CIGNA’s business.
During the first quarter of 2010, the Patient Protection and Affordable Care Act and the Health Care and Education Reconciliation Act of 2010 were signed into law. This legislation is far-reaching and is intended to expand access to health insurance coverage over time. This legislation includes a requirement that most individuals maintain a minimum level of health insurance coverage beginning in 2014 and also a requirement that most large employers offer coverage to their employees or they will be required to pay a financial penalty.
In addition, the legislation imposes an excise tax on high-cost employer-sponsored coverage and an annual fee on insurance companies and HMOs which will not be deductible for income tax purposes. It also limits the amount of compensation for executives of insurers that is tax deductible. The Patient Protection and Affordable Care Act also imposes new regulations on the health insurance sector, including, but not limited to, guaranteed coverage and renewal requirements, prohibitions on some annual and all lifetime benefit limits, increased restrictions on rescinding coverage, minimum medical loss ratio and customer rebate requirements, a requirement to cover preventive services on a first dollar basis, greater controls on premium rate increases for health insurance, and a requirement to establish state insurance exchanges.
Some of the health insurance reform provisions in the new law became effective immediately upon enactment while others take effect for group health plans and individual insurance policies with the first policy or plan year occurring on and after September 23, 2010 (six months from the enactment of the legislation) including those requiring coverage of preventive services with no enrollee cost-sharing, banning the use of lifetime and certain limits on benefits, increasing restrictions on rescinding coverage and extending coverage of dependents to the age of 26. Minimum medical loss ratio requirements commenced in January 2011 for health insurance companies and HMOs. Other significant changes, including the annual fees on health insurance companies, the excise tax on high-cost employer-sponsored coverage, the guaranteed issue and renewal requirements and the requirement that individuals maintain coverage, do not become effective until 2014 or later.
The Patient Protection and Affordable Care Act left many of the details of the new law to be established through regulations. While federal agencies have published interim final regulations with respect to many requirements, many issues remain unresolved. For example, the Department of Health and Human Services released interim final regulations in November 2010 which provided a special methodology for calculating medical loss ratios for 2011 for expatriate insurance business and limited benefit plans while also stating that it intends to study the data in determining whether special accommodations will be made for these plans in 2012 and future years. In addition to acting to comply with applicable requirements of the legislation, CIGNA is closely monitoring regulatory developments and keeping its clients apprised of changes that may affect them. (See further Health Care reform discussion beginning on page 50.)
In 2010, Congress also enacted the Dodd-Frank Wall-Street Reform and Consumer Protection Act which provides for a number of reforms and regulations in the corporate governance, financial reporting and disclosure, investments, tax and enforcement areas that will affect CIGNA. The full impact of this legislation may not be known for several years until regulations become fully effective. CIGNA is closely monitoring how these regulations will impact the Company.
Regulation of Insurance Companies
Financial Reporting
Regulators closely monitor the financial condition of licensed insurance companies and HMOs. States regulate the form and content of statutory financial statements, the type and concentration of permitted investments, and corporate governance over financial reporting. CIGNA’s insurance and HMO subsidiaries are required to file periodic financial reports and schedules with regulators in most of the jurisdictions in which they do business as well as annual financial statements audited by independent certified public accountants. Certain insurance and HMO subsidiaries are required to file an annual report of internal control over financial reporting with most jurisdictions in which they do business. Insurance and HMO subsidiaries’ operations and accounts are subject to examination by such agencies.
CIGNA CORPORATION – 2010 Form 10-K – 27
Guaranty Associations, Indemnity Funds, Risk Pools and Administrative Funds
Most states and certain non-U.S. jurisdictions require insurance companies to support guaranty associations or indemnity funds, which are established to pay claims on behalf of insolvent insurance companies. In the United States, these associations levy assessments on member insurers licensed in a particular state to pay such claims.
Several states also require HMOs to participate in guaranty funds, special risk pools and administrative funds. For additional information about guaranty fund and other assessments, see Note 24 to CIGNA’s Consolidated Financial Statements beginning on page 159 of this Form 10-K.
Some states also require health insurers and HMOs to participate in assigned risk plans, joint underwriting authorities, pools or other residual market mechanisms to cover risks not acceptable under normal underwriting standards.
Solvency and Capital Requirements
Many states have adopted some form of the National Association of Insurance Commissioners (“NAIC”) model solvency-related laws and risk-based capital rules (“RBC rules”) for life and health insurance companies. The RBC rules recommend a minimum level of capital depending on the types and quality of investments held, the types of business written and the types of liabilities incurred. If the ratio of the insurer’s adjusted surplus to its risk-based capital falls below statutory required minimums, the insurer could be subject to regulatory actions ranging from increased scrutiny to conservatorship.
In addition, various non-U.S. jurisdictions prescribe minimum surplus requirements that are based upon solvency, liquidity and reserve coverage measures. During 2010, CIGNA’s HMOs and life and health insurance subsidiaries, as well as non-U.S. insurance subsidiaries, were compliant with applicable RBC and non-U.S. surplus rules.
Effective December 31, 2009, the Company’s principal life insurance subsidiary, Connecticut General Life Insurance Company (“CGLIC”), implemented the NAIC’s Actuarial Guideline XLIII (also known as AG 43 or VACARVM), which is applicable to CGLIC’s statutory reserves for GMDB and GMIB contracts totaling $1.5 billion as of December 31, 2010. As provided under this guidance, CGLIC received approval from the State of Connecticut to grade-in the full effect of the guideline over a 3-year period beginning in 2009. At December 31, 2010, statutory reserves for CGLIC were higher than the pre-AG 43 reserves by $123 million. If the guidance had been fully implemented at December 31, 2010, statutory reserves would have been higher by an additional $63 million. Management does not anticipate that VACARVM will have a material impact on the amount of dividends expected to be paid by CGLIC to the parent company in 2011. In addition, VACARVM has no impact on measurement of the Company’s results of operations or financial condition as determined under GAAP.
Holding Company Laws
CIGNA’s domestic insurance companies and certain of its HMOs are subject to state laws regulating subsidiaries of insurance holding companies. Under such laws, certain dividends, distributions and other transactions between an insurance or HMO subsidiary and its affiliates may require notification to, or approval by, one or more state insurance commissioners.
Marketing, Advertising and Products
In most states, CIGNA’s insurance companies and HMO subsidiaries are required to certify compliance with applicable advertising regulations on an annual basis. CIGNA’s insurance companies and HMO subsidiaries are also required in most states to file and secure regulatory approval of products prior to the marketing, advertising, and sale of such products. State and/or federal regulatory scrutiny of life and health insurance company and HMO marketing and advertising practices, including the adequacy of disclosure regarding products and their administration, may result in increased regulation. Products offering limited coverage, such as those CIGNA issues through the Star HRG business acquired in July 2006, continue to attract increased regulatory scrutiny.
CIGNA CORPORATION – 2010 Form 10-K – 28
Licensing Requirements
Pharmacy Licensure Laws
Certain CIGNA subsidiaries are pharmacies, which dispense prescription drugs to participants of benefit plans administered or insured by CIGNA subsidiary HMOs and insurance companies. These pharmacy-subsidiaries are subject to state licensing requirements and regulation.
International Licensure Laws
CIGNA International subsidiaries are often required to be licensed when entering new markets or starting new operations in certain jurisdictions. The licensure requirements for these CIGNA subsidiaries vary by country and are subject to change.
Claim Administration, Utilization Review and Related Services
Certain CIGNA subsidiaries contract for the provision of claim administration, utilization management and other related services with respect to the administration of self-insured benefit plans. These CIGNA subsidiaries may be subject to state third-party administration and other licensing requirements and regulation.
International Regulations
An increasing portion of CIGNA’s revenue is derived from operations outside the United States, which exposes the Company to laws of multiple jurisdictions and the rules and regulations of various governing bodies and regulators, including those related to financial and other disclosures, corporate governance, privacy, data protection, data mining, data transfer, labor and employment, consumer protection and anti-corruption. The operations in countries outside the United States:
•
are subject to local regulations in the place in which CIGNA subsidiaries conduct business;
•
in some cases, are subject to regulations in the places in which customers are located; and
•
in all cases are subject to FCPA.
FCPA prohibits offering, promising, providing or authorizing others to give anything of value to a foreign government official to obtain or retain business or otherwise secure a business advantage. CIGNA is also subject to applicable anti-corruption laws in the jurisdictions in which it operates. Additionally, in many countries outside of the U.S., health care professionals are employed by the government. Therefore, CIGNA’s dealings with them are subject to regulation under the FCPA. Violations of the FCPA and other anti-corruption laws may result in severe criminal and civil sanctions as well as other penalties and the SEC and Department of Justice have increased their enforcement activities with respect to FCPA. The UK Bribery Act of 2010 is an anti-corruption law that applies to all companies with a nexus to the United Kingdom and whose scope is even broader than the FCPA. It is yet to be seen how the UK Bribery Act will be implemented and enforced, but any voluntary disclosures of FCPA violations may be shared with the UK authorities, thus potentially exposing companies to liability and potential penalties in multiple jurisdictions. CIGNA has internal control policies and procedures and has implemented training and compliance programs for its employees to deter prohibited practices. However, if CIGNA’s employees or agents fail to comply with applicable laws governing its international operations, the Company may face investigations, prosecutions and other legal proceedings and actions which could result in civil penalties, administrative remedies and criminal sanctions. See the Risk Factors section beginning on page 33 for a discussion of the risks related to operating globally.
Federal Regulations
Employee Retirement Income Security Act
CIGNA subsidiaries sell most of their products and services to sponsors of employee benefit plans that are governed by ERISA. CIGNA subsidiaries are subject to requirements imposed by ERISA affecting claim and appeals procedures for health plans and are expected to comply with these requirements on behalf of the dental, disability, life and accident plans they administer.
CIGNA CORPORATION – 2010 Form 10-K – 29
Medicare Regulations
Several CIGNA subsidiaries engage in businesses that are subject to federal Medicare regulations such as:
•
those offering individual and group Medicare Advantage (HMO) coverage in Arizona;
•
contractual arrangements with the federal government for the processing of certain Medicare claims and other administrative services; and
•
those offering Medicare Pharmacy (Part D) and Medicare Advantage Private Fee For Service products that are subject to federal Medicare regulations.
Several CIGNA subsidiaries are also subject to reporting requirements pursuant to Section 111 of the Medicare, Medicaid and SCHIP Extension Act of 2007.
Federal Audits of Government Sponsored Health Care Programs
Participation in government sponsored health care programs subjects CIGNA to a variety of federal laws and regulations and risks associated with audits conducted under these programs. These audits may occur in years subsequent to CIGNA providing the relevant services under audit. These risks may include reimbursement claims as well as potential fines and penalties. For example, the federal government requires Medicare and Medicaid providers to file detailed cost reports for health care services provided. These reports may be audited in subsequent years. CIGNA HMOs that contract to provide community-rated coverage to participants in the Federal Employees Health Benefit Plan may be required to reimburse the federal government if, following an audit, it is determined that a federal employee group did not receive the benefit of a discount offered by a CIGNA HMO to one of the two groups closest in size to the federal employee group. See “Health Care” in Section D beginning on page 3 of this Form 10-K for additional information about CIGNA’s participation in government health-related programs.
The Federal government has made investigating and prosecuting health care fraud and abuse a priority. Fraud and abuse prohibitions encompass a wide range of activities, including kickbacks for referral of members, billing for unnecessary medical services, improper marketing, and violation of patient privacy rights. The regulations and contractual requirements in this area are complex and subject to change and compliance will continue to require significant resources.
Health Insurance Portability and Accountability Act Regulations
The federal Health Insurance Portability and Accountability Act of 1996 and its implementing regulations (“HIPAA”) impose several different requirements on health insurers, HMOs, health plans, health care providers and clearinghouses. Health insurers and HMOs are further subject to regulations related to guaranteed issuance (for groups with 50 or fewer lives), guaranteed renewal, and portability of health insurance.
HIPAA also imposes minimum standards for health plans, health insurers, health care providers and their vendors to safeguard the privacy and security of individually identifiable or protected health information (“PHI”). HIPAA’s privacy and security requirements were expanded by the Health Information Technology for Economic and Clinical Health Act (“HITECH”) which enhanced penalties for HIPAA violations and required regulated entities to provide notice of breaches of unsecured PHI.
HIPAA also establishes rules to standardize the format and content of certain electronic transactions, including, but not limited to, eligibility and claims. Federal regulations were issued requiring entities subject to HIPAA to update their transaction formats for electronic data interchange from the current HIPAA 4010 standards to new HIPAA 5010 standards with a compliance date of January 1, 2012. Regulations were also issued requiring a conversion from the ICD-9 diagnosis and procedure code sets to the ICD-10 diagnosis and procedure code sets. The IDC-10 code set conversion is dependent upon implementation of the HIPAA 5010 standards. CIGNA has related project plans underway to deliver ICD-10 capabilities by the October 1, 2013 effective date.
CIGNA CORPORATION – 2010 Form 10-K – 30
Other Confidentiality Requirements
The federal Gramm-Leach-Bliley Act generally places restrictions on the disclosure of non-public information to non-affiliated third parties, and requires financial institutions, including insurers, to provide customers with notice regarding how their non-public personal information is used, including an opportunity to “opt out” of certain disclosures. State departments of insurance and certain federal agencies adopted implementing regulations as required by federal law. A number of states have also adopted data security laws and/or regulations, regulating data security and/or requiring security breach notification, which may apply to CIGNA in certain circumstances.
Antitrust Regulations
CIGNA subsidiaries are also engaged in activities that may be scrutinized under federal and state antitrust laws and regulations. These activities include the administration of strategic alliances with competitors, information sharing with competitors and provider contracting.
Anti-Money Laundering Regulations
Certain CIGNA products (“Covered Products” as defined in the Bank Secrecy Act) are subject to U.S. Department of the Treasury anti-money laundering regulations. CIGNA has implemented anti-money laundering policies designed to ensure that its Covered Products are underwritten and sold in compliance with these regulations.
Office of Foreign Assets Control
The Company is also subject to regulation put forth by the Office of Foreign Assets Control (OFAC) of the U.S. Department of the Treasury which administers and enforces economic and trade sanctions based on U.S. foreign policy and national security goals against targeted foreign countries and regimes, terrorists, international narcotics traffickers, those engaged in activities related to the proliferation of weapons of mass destruction, and other threats to the national security, foreign policy or economy of the United States.
Investment-Related Regulations
Depending upon their nature, CIGNA’s investment management activities are subject to U.S. federal securities laws, ERISA, and other federal and state laws governing investment related activities. In many cases, the investment management activities and investments of individual insurance companies are subject to regulation by multiple jurisdictions.
CIGNA CORPORATION – 2010 Form 10-K – 31
K. Miscellaneous
CIGNA and its principal subsidiaries are not dependent on business from one or a few customers. No one customer accounted for 10% or more of CIGNA’s consolidated revenues in 2010. CIGNA and its principal subsidiaries are not dependent on business from one or a few brokers or agents. In addition, CIGNA’s insurance businesses are generally not committed to accept a fixed portion of the business submitted by independent brokers and agents, and generally all such business is subject to its approval and acceptance.
CIGNA had approximately 30,600, 29,300, and 30,300 employees as of December 31, 2010, 2009 and 2008, respectively.
CIGNA CORPORATION – 2010 Form 10-K – 32
ITEM 1A Risk Factors
As a large company operating in a complex industry, CIGNA encounters a variety of risks and uncertainties including those identified in this Risk Factor discussion and elsewhere in this report. CIGNA devotes resources to developing enterprise-wide risk management processes, in addition to the risk management processes within its businesses. These factors represent risks and uncertainties that could have a material adverse effect on CIGNA’s business, liquidity, results of operations or financial condition. These risks and uncertainties are not the only ones CIGNA faces. Other risks and uncertainties that CIGNA does not know about now, or that the Company does not now think are significant and does not appropriately identify and manage, may impair its business or the trading price of its securities. The following are significant risks identified by CIGNA.
Business Risks
Future performance of CIGNA’s business will depend on the Company’s ability to execute on its strategic and operational initiatives effectively.
The future performance of CIGNA’s business will depend in large part on CIGNA’s ability to implement and execute effectively its growth strategy. These strategic and operational initiatives include: (1) growth in targeted geographies, product lines, buying segments and distribution channels; (2) improving its strategic and financial flexibility; and (3) pursuing additional opportunities in high-growth markets with particular focus on individuals.
Successful execution of these strategic and operational initiatives depends on a number of factors including:
•
differentiating CIGNA’s products and services from those of its competitors by leveraging its health advocacy capabilities and other strengths in targeted markets, geographies and buyer segments;
•
developing and introducing new products or programs, because of the inherent risks and uncertainties associated with product development, particularly in response to government regulation or the increased focus on consumer directed products;
•
identifying and introducing the proper mix or integration of products that will be accepted by the marketplace;
•
attracting and retaining sufficient numbers of qualified employees;
•
effectively managing balance sheet exposures, including evaluating potential solutions for the Company’s run-off reinsurance business and pension funding obligation;
•
improving medical cost competitiveness in targeted markets; and
•
reducing CIGNA HealthCare’s medical operating expenses to achieve sustainable benefits.
If these initiatives fail or are not executed effectively, it could harm the Company’s consolidated financial position and results of operations. For example, the plan to reduce operating expenses while maintaining the necessary resources and the Company’s talent pool is important to the Company and if not managed effectively could have long-term effects on the business by decreasing or slowing improvements in its products and limiting its ability to retain or hire key personnel. In addition, in order to succeed, the Company must align its organization to its evolving strategy. CIGNA must effectively integrate its operations, actively work to ensure consistency throughout the organization, and promote a global mind-set. If the Company fails to do so, it may be unable to grow as planned, and the result of expansion may be unsatisfactory. Also, the current competitive, economic and regulatory environment will require CIGNA’s organization to adapt rapidly and nimbly to new opportunities and challenges. The Company will be unable to do so if it does not make important decisions quickly, define its appetite for risk specifically, implement new governance, managerial and organizational processes smoothly and communicate roles and responsibilities clearly.
As a multi-national company, CIGNA’s international operations face political, legal, operational, regulatory, economic and other risks that present challenges and could negatively affect those operations or our long-term growth.
CIGNA’s growth strategy involves expanding our foreign operations including South Korea, China, Spain, Turkey, Indonesia and India and entering into targeted new markets outside of the U.S. As a result, CIGNA’s business is increasingly exposed to risks inherent in foreign operations. These risks, which can vary substantially by market, include political, legal, operational, regulatory, economic and other risks, including government intervention and censorship that the Company does not face in its U.S. operations. The global nature of CIGNA’s business and operations presents challenges, including but not limited to those arising from:
•
varying regional and geopolitical business conditions and demands;
•
discriminatory regulation, nationalization or expropriation of assets;
CIGNA CORPORATION – 2010 Form 10-K – 33
•
price controls or other pricing issues and exchange controls or other restrictions that prevent it from transferring funds from these operations out of the countries in which it operates or converting local currencies that CIGNA International holds into U.S. dollars or other currencies;
•
foreign currency exchange rates and fluctuations that may have an impact on the future costs or on future sales and cash flows from the Company’s international operations, and any measures that it may implement to reduce the effect of volatile currencies and other risks of its international operations may not be effective;
•
reliance on local sales forces for some of its operations in these countries that may have labor problems and less flexible employee relationships which can be difficult and expensive to terminate, or where changes in local regulation or law may disrupt the business operations. In some countries, CIGNA International voluntarily operates or is required to operate with local business partners with the resulting risk of managing partner relationships to the business objectives;
•
challenges associated with managing more geographically diverse operations and projects;
•
the need to provide sufficient levels of technical support in different locations;
•
political instability or acts of war, terrorism, natural disasters, pandemics in locations where CIGNA operates. For example, CIGNA International’s largest geographic market is South Korea which has recently been subject to increased tension and disputes with North Korea; and
•
general economic and political conditions.
These factors may increase in importance as we continue to expand globally. Further, expansion into new markets may require considerable management time before any significant revenues and earnings are generated.
International operations also require the Company to devote significant management resources to implement its controls and systems in new markets, to comply with the U.S. anti-bribery and anti-corruption as well as anti-money laundering provisions and similar laws in local jurisdictions and to overcome logistical and other challenges based on differing languages, cultures and time zones. Violations of these laws and regulations could result in fines, criminal sanctions against the Company, its officers or employees, and prohibitions on the conduct of its business. CIGNA must regularly reassess the size, capability and location of its global infrastructure and make appropriate changes, and must have effective change management processes and internal controls in place to address changes in its business and operations. CIGNA’s success depends, in part, on its ability to anticipate these risks and manage these difficulties. The Company monitors its international operations and investigates allegations of improprieties relating to transactions and the way in which such transactions are recorded. Where circumstances warrant, we provide information and report our findings to government authorities, but no assurance can be given that action will not be taken by such authorities.
Successful management of CIGNA’s outsourcing projects and key vendors is important to its business.
To improve operating costs, productivity and efficiencies, CIGNA outsources selected functions to third parties. CIGNA takes steps to monitor and regulate the performance of independent third parties who provide services or to whom the Company delegates selected functions. These third parties include information technology system providers, independent practice associations, call center and claim service providers and types of service providers.
Arrangements with key vendors may make CIGNA’s operations vulnerable if third parties fail to satisfy their obligations to the Company as a result of their performance, changes in their own operations, financial condition, or other matters outside of CIGNA’s control, including their obligations to maintain and protect the security and confidentiality of the Company’s information and data. In addition, to the extent CIGNA outsources selected services or selected functions to third parties in foreign jurisdictions, the Company could be exposed to risks inherent in conducting business outside of the United States, including international economic and political conditions, additional costs associated with complying with foreign laws and fluctuations in currency values. The expanding role of third party providers may also require changes to CIGNA’s existing operations and the adoption of new procedures and processes for retaining and managing these providers, as well as redistributing responsibilities as needed, in order to realize the potential productivity and operational efficiencies. Effective management, development and implementation of its outsourcing strategies are important to CIGNA’s business and strategy. If there are delays or difficulties in enhancing business processes or its third party providers do not perform as anticipated, CIGNA may not fully realize on a timely basis the anticipated economic and other benefits of the outsourcing projects or other relationships it enters into with key vendors, which could result in substantial costs, divert management’s attention from other strategic activities, negatively affect employee morale or create other operational or financial problems for the Company. Terminating or transitioning arrangements with key vendors could result in additional costs and a risk of operational delays, potential errors and possible control issues as a result of the termination or during the transition phase.
CIGNA CORPORATION – 2010 Form 10-K – 34
In 2006, CIGNA entered into an agreement with IBM to operate certain software applications and significant portions of CIGNA’s information technology infrastructure, including the provision of services relating to its call center application, enterprise content management, risk-based capital analytical infrastructure and voice and data communications network. This contract includes several service level agreements, or SLAs, related to issues such as performance and job disruption with significant financial penalties if these SLAs are not met. However, the Company may not be adequately indemnified against all possible losses through the terms and conditions of the agreement and the fees paid could be a subject of dispute between the parties. In addition, some of CIGNA’s termination rights are contingent upon payment of a fee, which may be significant. If CIGNA’s relationship with IBM is abruptly terminated, the Company’s customers may experience disruption of service.
Effective investment in and execution of improvements in the Company’s information technology infrastructure and functionality are important to its strategy and failure to do so may impede its ability to deliver the services required in the evolving marketplace at a competitive cost or to strategically implement new information systems.
CIGNA’s information technology strategy and execution are critical to the continued success of the Company. Increasing regulatory and legislative mandated changes will place additional demands on CIGNA’s information technology infrastructure which could have direct impact on available resources for projects more directly tied to strategic initiatives. The marketplace is evolving and the level of service that is acceptable to customers today will not necessarily be acceptable tomorrow. The Company must continue to invest in long-term solutions that will enable it to meet customer expectations, enhance the customer experience and act as a differentiator in the market. CIGNA’s success is dependent, in large part, on maintaining the effectiveness of existing technology systems and continuing to deliver and enhance technology systems that support the Company’s business processes in a cost-efficient and resource-efficient manner. CIGNA also must develop new systems to meet the current market standard and keep pace with continuing changes in information processing technology, evolving industry and regulatory standards and customer needs. System development projects are long term in nature, may be more costly than expected to complete and may not deliver the expected benefits upon completion.
CIGNA’s business depends on its ability to properly maintain the integrity or security of its data.
CIGNA’s business depends on effective information systems and the integrity and timeliness of the data it uses to run its business. CIGNA’s business strategy requires providing members and providers with Internet-enabled products and information to meet their needs. CIGNA’s ability to adequately price its products and services, establish reserves, provide effective and efficient service to its customers, and to timely and accurately report its financial results also depends significantly on the integrity of the data in its information systems. If the information CIGNA relies upon to run its businesses were found to be inaccurate or unreliable due to fraud or other error, or if CIGNA were to fail to maintain effectively its information systems and data integrity, the Company could have problems with, among other things: operational disruptions, which may impact customers, physicians and other health care providers; determining medical cost estimates and establishing appropriate pricing; retaining and attracting customers; and regulatory compliance.
Maintaining the security of any sensitive data residing on the Company’s systems is critical to CIGNA’s reputation. Failure to do so could expose the Company to litigation or other actions, fines or penalties.
CIGNA operates a pharmacy benefit management business, onsite clinics, and medical facilities, which are subject to a number of risks and uncertainties, in addition to those CIGNA faces with its health care business.
CIGNA’s pharmacy benefit management business is subject to federal and state regulation, including federal and state anti-remuneration laws, ERISA, HIPAA and laws related to the operation of Internet and mail-service pharmacies.
The Company’s pharmacy benefit management business would also be adversely affected by an inability to contract on favorable terms with pharmaceutical manufacturers and could suffer claims and reputational harm in connection with purported errors by CIGNA’s mail order or retail pharmacy businesses. Disruptions at any of the Company’s pharmacy business facilities due to failure of technology or any other failure or disruption to these systems or to the infrastructure due to fire, electrical outage, natural disaster, acts of terrorism or some other catastrophic event could reduce CIGNA’s ability to process and dispense prescriptions and provide products and services to customers.
CIGNA CORPORATION – 2010 Form 10-K – 35
The Company employs physicians, nurse practitioners, nurses and other health care professionals at onsite low acuity and primary care clinics it operates for the Company’s customers (as well as certain clinics for Company employees). The Company also owns and operates medical facilities in the Phoenix, Arizona metropolitan area, including multispecialty health care centers, outpatient surgery and urgent care centers, low acuity clinics, laboratory, pharmacy and other operations that employ primary care as well as specialty care physicians and other types of health care professionals. As a direct employer of health care professionals and as an operator of primary and low-acuity care clinics and other types of medical facilities, the Company is subject to liability for negligent acts, omissions, or injuries occurring at one of its clinics or caused by one of its employees. Even if any claims brought against the Company were unsuccessful or without merit, it would have to defend against such claims. The defense of any such actions may be time-consuming and costly, and may distract management’s attention. As a result, CIGNA may incur significant expenses and the Company’s financial results could be adversely affected.
CIGNA faces competitive pressure, particularly price competition, which could result in premiums which are insufficient to cover the cost of the healthcare services delivered to its members and inadequate medical claims reserves.
While health plans compete on the basis of many factors, including service quality of clinical resources, claims administration services and medical management programs, and quality, sufficiency and cost effectiveness of health care professional network relationships, CIGNA expects that price will continue to be a significant basis of competition. CIGNA’s customer contracts are subject to negotiation as customers seek to contain their costs, and customers may elect to reduce benefits in order to constrain increases in their benefit costs. Such an election may result in lower premiums for the Company’s products, although it may also reduce CIGNA’s costs. Alternatively, the Company’s customers may purchase different types of products that are less profitable, or move to a competitor to obtain more favorable premiums.
Factors such as business consolidations, strategic alliances, legislative reform and marketing practices create pressure to contain premium price increases, despite increasing medical costs. For example, the Gramm-Leach-Bliley Act gives banks and other financial institutions the ability to affiliate with insurance companies, which may lead to new competitors with significant financial resources in the insurance and health benefits fields.
The Company’s product margins and growth depend, in part on its ability to compete effectively in its markets, set rates appropriately in highly competitive markets to keep or increase its market share, increase membership as planned, and avoid losing accounts with favorable medical cost experience while retaining or increasing membership in accounts with unfavorable medical cost experience.
CIGNA’s profitability depends, in part, on its ability to accurately predict and control future health care costs through underwriting criteria, provider contracting, utilization management and product design. Premiums in the health care business are generally fixed for one-year periods. Accordingly, future cost increases in excess of medical cost projections reflected in pricing cannot generally be recovered in the current contract year through higher premiums. Although CIGNA bases the premiums it charges on its estimate of future health care costs over the fixed premium period, actual costs may exceed what was estimated and reflected in premiums. Factors that may cause actual costs to exceed premiums include: medical cost inflation; higher than expected utilization of medical services; the introduction of new or costly treatments and technology; and membership mix.
CIGNA records medical claims reserves for estimated future payments. The Company continually reviews estimates of future payments relating to medical claims costs for services incurred in the current and prior periods and makes necessary adjustments to its reserves. However, actual health care costs may exceed what was estimated.
Public perception of the health benefits industry, if negative, could reduce enrollment in CIGNA’s health benefits programs.
The health care industry in general is subject to negative publicity, which can arise either from perceptions regarding the industry and its business practices or products. This risk may be increased as the industry offers new products, such as products with limited benefits or develops new types of arrangements with business partners beyond those in which it traditionally has operated. Negative publicity related to the industry may adversely impact the CIGNA brand, its ability to market its products and services and its relationships with its healthcare professionals, which could reduce the number of enrollees in CIGNA’s health benefits programs.
CIGNA CORPORATION – 2010 Form 10-K – 36
Acquisitions involve risks that could adversely affect CIGNA’s business.
As part of our growth strategy, CIGNA regularly considers strategic transactions, including acquisitions. For example, in 2010, the Company acquired Vanbreda International and Kronos Optimal Health Company with the expectation that these acquisitions will result in various benefits, including, among others, a broader distribution network in certain geographic areas, an expanded range of health benefits and products, cost savings, and increased profitability of the acquired businesses by improving operating efficiencies. Achieving the anticipated benefits is subject to a number of uncertainties, including whether CIGNA integrates its acquired companies in an efficient and effective manner, and general competitive factors in the marketplace. Failure to achieve these anticipated benefits could result in increased costs, decreases in the amount of expected revenues and diversion of management’s time and energy.
In addition, effective internal controls are necessary for the Company to provide reliable and accurate financial reports and to effectively prevent fraud. The integration of acquired businesses is likely to result in CIGNA’s systems and controls becoming increasingly complex and more difficult to manage. The Company devotes significant resources and time to comply with the internal control over financial reporting requirements of the Sarbanes-Oxley Act of 2002. However, CIGNA cannot be certain that these measures will ensure that it designs, implements and maintains adequate control over its financial processes and reporting in the future, especially in the context of acquisitions of other businesses. Any difficulties in the assimilation of acquired businesses into the Company’s control system could harm its operating results or cause it to fail to meet its financial reporting obligations. Inferior internal controls could also cause investors to lose confidence in the Company’s reported financial information, which could have a negative effect on the trading price of CIGNA’s stock and its access to capital.
Regulatory and Litigation Risks
CIGNA faces risks related to litigation and regulatory investigations.
CIGNA is routinely involved in numerous claims, lawsuits, regulatory audits, investigations and other legal matters arising in the ordinary course of business, including that of administering and insuring employee benefit programs. Such legal matters include benefit claims, breach of contract actions, tort claims, disputes regarding reinsurance arrangements, employment and employment discrimination-related suits, employee benefit claims, wage and hour claims, and intellectual property and real estate related disputes. In addition, CIGNA incurs and likely will continue to incur liability for claims related to its health care business, such as failure to pay for or provide health care, poor outcomes for care delivered or arranged, provider disputes, including disputes over compensation, and claims related to self-funded business. Also, there are currently, and may be in the future, attempts to bring class action lawsuits against the industry.
Court decisions and legislative activity may increase CIGNA’s exposure for any of these types of claims. In some cases, substantial non-economic or punitive damages may be sought. CIGNA currently has insurance coverage for some of these potential liabilities. Other potential liabilities may not be covered by insurance, insurers may dispute coverage or the amount of insurance may not be sufficient to cover the entire damages awarded. In addition, certain types of damages, such as punitive damages, may not be covered by insurance, and insurance coverage for all or certain forms of liability may become unavailable or prohibitively expensive in the future. It is possible that the resolution of one or more of the legal matters and claims described could result in losses material to CIGNA’s consolidated results of operations, liquidity or financial condition.
A description of material legal actions and other legal matters in which CIGNA is currently involved is included under “Legal Proceedings” in Item 3 beginning on page 43, Note 24 to CIGNA’s Consolidated Financial Statements beginning on page 159 of this Form 10-K and “Regulation” in Section J beginning on page 26. The outcome of litigation and other legal matters is always uncertain, and outcomes that are not justified by the evidence or existing law can occur. CIGNA believes that it has valid defenses to the legal matters pending against it and is defending itself vigorously.
In addition, there is heightened review by federal and state regulators of health care and group disability insurance industry business and reporting practices. CIGNA is frequently the subject of regulatory market conduct and other reviews, audits and investigations by state insurance and health and welfare departments, attorneys general, Centers for Medicare and Medicaid Services and, the Office of Inspector General. These regulatory reviews could result in changes to or clarifications of our business practices, and also could result in significant fines, penalties, civil liabilities, criminal liabilities or other sanctions. For example, in February 2009, CIGNA and the New York Attorney General announced an agreement relating to an industry-wide investigation into certain payment practices with respect to out-of-network providers. As a result of that agreement, CIGNA contributed $10 million towards the establishment of a new non-profit company that would compile and create an independent database system to provide fee information regarding out-of-network reimbursement rates.
CIGNA CORPORATION – 2010 Form 10-K – 37
CIGNA’s business is subject to substantial government regulation, which, along with new regulation, could increase its costs of doing business and could adversely affect its profitability.
CIGNA’s business is regulated at the international, federal, state and local levels. The laws and rules governing CIGNA’s business and related interpretations are increasing in number and complexity, subject to frequent change and can be inconsistent or even conflicting with each other. As a public company with global operations, CIGNA is subject to the laws of multiple jurisdictions and the rules and regulations of various governing bodies, including those related to financial and other disclosures, corporate governance, privacy, data protection, labor and employment, consumer protection and anti-corruption. CIGNA must identify, assess and respond to new trends in the legislative and regulatory environments as well as effectively comply with the various existing regulations applicable to its business. Existing or future laws and rules could force CIGNA to change how it does business, restrict revenue and enrollment growth, increase health care, technology and administrative costs including pension costs and capital requirements, require enhancements to the Company’s compliance infrastructure and internal controls environment, take other actions such as changing its reserve levels with respect to certain reinsurance contracts, change business practices in disability payments and increase CIGNA’s liability in federal and state courts for coverage determinations, contract interpretation and other actions.
In addition, CIGNA must obtain and maintain regulatory approvals to market many of its products, to increase prices for certain regulated products and to consummate some of its acquisitions and divestitures. Delays in obtaining or failure to obtain or maintain these approvals could reduce the Company’s revenue or increase its costs. For further information on regulatory matters relating to CIGNA, see “Regulation” in Section J beginning on page 26 and “Legal Proceedings” in Item 3 beginning on page 43 of this Form 10-K.
Health care reform legislation, as well as potential additional changes in federal or state regulations could adversely affect CIGNA’s business, results of operations, financial condition and liquidity.
During the first quarter of 2010, the Patient Protection and Affordable Care Act as well as the Health Care and Education Reconciliation Act of 2010 were signed into law, which will result in significant changes to the current U.S. health care system. The legislation is far-reaching and is intended to expand access to health insurance coverage over time. The legislation includes a requirement that most individuals maintain a minimum level of health insurance coverage beginning in 2014 and also a requirement that most large employers offer coverage to their employees or they will be required to pay a financial penalty.
In addition, the legislation imposes an excise tax on high-cost employer-sponsored coverage and an annual fee on insurance companies and HMOs which will not be deductible for income tax purposes. It also limits the amount of compensation for executives of insurers that this tax deductible. The Patient Protection and Affordable Care Act also imposes new regulations on the health insurance sector, including, but not limited to, guaranteed coverage/renewal requirements, prohibitions on some annual and all lifetime benefit limits, increased restrictions on rescinding coverage, establishment of minimum medical loss ratio/enrollee rebate requirements, a requirement to cover preventive services on a first dollar basis, the establishment of state insurance exchanges and essential benefit packages and greater controls on premium rate increases for health insurance.
Some of the health insurance reform provisions in the new law became effective immediately upon enactment while others take effect for group health plans and individual insurance policies with the first policy or plan year occurring on and after September 23, 2010 (six months from the enactment of the legislation) including those requiring coverage of preventive services with no enrollee cost-sharing, banning the use of lifetime and certain limits on benefits, increasing restrictions on rescinding coverage and extending coverage of dependents to the age of 26. The minimum medical loss ratio requirements for health insurance companies and HMOs became effective beginning in January 2011. Other significant changes, including the annual fees on health insurance companies, the excise tax on high-cost employer-sponsored coverage, the guaranteed issue and renewal requirements and the requirement that individuals maintain coverage, do not become effective until 2014 or later. These changes could impact the Company significantly through:
•
potential disruption to the employer based market, which is currently the primary business model for the Company’s Health Care segment;
•
potential cost shifting in the health care delivery system to health insurance companies and HMOs; and
•
limitations on the ability to increase premiums to meet costs.
CIGNA CORPORATION – 2010 Form 10-K – 38
The Patient Protection and Affordable Care Act left many of the details of the new law to be established through regulations. While federal agencies have published interim final regulations with respect to many requirements, many issues remain unresolved. For example, the Department of Health and Human Services released interim final regulations in November 2010 which provided a special methodology for calculating medical loss ratios for 2011 for the expatriate insurance business and limited benefit plans while also stating that it intends to study the data in determining whether special accommodations will be made for these plans in 2012 and future years. While health care reform presents the Company with new business opportunities which may increase membership in CIGNA’s health plans, it may also cause employers to drop health care coverage for their employees; it is possible that the Company’s business operations and financial results could be adversely affected by health care reform.
Financial Risks
CIGNA’s equity hedge program for its guaranteed minimum death benefits contracts could fail to reduce the risk of stock market declines.
As part of its Run-off Reinsurance business, CIGNA reinsured a guaranteed minimum death benefit under certain variable annuities issued by other insurance companies. CIGNA maintains a hedge program to reduce equity market risks related to these contracts by selling domestic and foreign-denominated exchange-traded futures contracts. The purpose of this program is to reduce the adverse effects of potential future domestic and international stock market declines on CIGNA’s liabilities for these contracts. Under the program, increases in liabilities under the annuity contracts from a declining equity market are offset by gains on the futures contracts. However, the program will not perfectly offset the change in the liability in part because the market does not offer futures contracts that exactly match the diverse mix of equity fund investments held by contractholders. The impact of this mismatch may be higher in periods of significant volatility and may result in higher losses to the Company. In addition, the number of futures contracts used in the program is adjusted only when certain tolerances are exceeded and in periods of highly volatile equity markets when actual volatility exceeds the expected volatility assumed in the liability calculation, losses will result. Further, CIGNA could have difficulty in entering into appropriate futures contracts. See “Run-off Reinsurance” in Section G beginning on page 19 of this Form 10-K for more information on the program.
Actual experience could differ significantly from CIGNA’s assumptions used in estimating CIGNA’s liabilities for reinsurance contracts covering guaranteed minimum death benefits or minimum income benefits.
CIGNA estimates reserves for guaranteed minimum death benefit and minimum income benefit exposures based on assumptions regarding lapse, partial surrender, mortality, interest rates, volatility, reinsurance recoverables, and, for minimum income benefit exposures, annuity income election rates. These estimates are currently based on CIGNA’s experience and future expectations. CIGNA monitors actual experience to update these reserve estimates as necessary. CIGNA regularly evaluates the assumptions used in establishing reserves and changes its estimates if actual experience or other evidence suggests that earlier assumptions should be revised. In addition, the Company could have losses attributable to its inability to recover amounts from retrocessionaires. See Notes 7 and 11 to CIGNA’s Consolidated Financial Statements beginning on pages 116 and 127, respectively of this Form 10-K, for more information on assumptions used for the Company’s guaranteed minimum death benefit and minimum income benefit exposures.
Significant stock market declines could result in larger net liabilities for guaranteed minimum death benefit contracts or for guaranteed minimum income benefit contracts, the recognition of additional pension obligations, increased funding for those obligations, and increased pension plan expenses.
The Company calculates a provision for expected future partial surrenders as part of the liability for guaranteed minimum death benefit contracts. As equity markets decline, the amount of guaranteed death benefit exposure increases and the equity hedge program is designed to offset the corresponding change in the liability. If a contractholder withdraws substantially all of its mutual fund investments, the liability increases reflecting the lower assumed future premiums, the lower likelihood of lapsation, and the lower likelihood of account values recovering sufficiently to reduce death benefit exposure in future periods. These effects are not covered by the Company’s equity hedge program. Thus if equity markets decline, the provision for expected future partial surrenders increases and there is no corresponding offset from the hedge program.
As equity markets decline, the claim amounts that the Company expects to pay out for the guaranteed minimum income benefit business increases resulting in increased net liabilities and related losses.
CIGNA CORPORATION – 2010 Form 10-K – 39
CIGNA currently has unfunded obligations in its frozen pension plan. A significant decline in the value of the plan’s equity and fixed income investments or unfavorable changes in applicable laws or regulations could materially increase CIGNA’s expenses and change the timing and amount of required plan funding, which could reduce the cash available to CIGNA, including its subsidiaries. See Note 10 to CIGNA’s Consolidated Financial Statements beginning on page 122 of this Form 10-K for more information on the Company’s obligations under the pension plan.
Significant changes in market interest rates affect the value of CIGNA’s financial instruments that promise a fixed return or benefit and the value of particular assets and liabilities.
As an insurer, CIGNA has substantial investment assets that support insurance and contractholder deposit liabilities. Generally low levels of interest rates on investments, such as those experienced in United States financial markets during recent years, have negatively impacted the level of investment income earned by the Company in recent periods, and such lower levels of investment income would continue if these lower interest rates were to continue.
Substantially all of the Company’s investment assets are in fixed interest-yielding debt securities of varying maturities, fixed redeemable preferred securities and commercial mortgage loans. The value of these investment assets can fluctuate significantly with changes in market conditions. A rise in interest rates could reduce the value of the Company’s investment portfolio and increase interest expense if CIGNA were to access its available lines of credit.
The Company is also exposed to interest rate and equity risk associated with the Company’s pension and other post-retirement obligations. Sustained declines in interest rates could have an adverse impact on the funded status of the Company’s pension plans and the Company’s re-investment yield on new investments.
Changes in interest rates may also impact the discount rate and expected long-term rate of return assumptions associated with the Company’s guaranteed minimum death benefit liabilities. Significant, sustained declines in interest rates could cause the Company to reduce these long-term assumptions, resulting in increased liabilities.
In addition, changes in interest rates impact the assumed market returns and the discount rate used in the fair value calculations for the Company’s liabilities for guaranteed minimum income benefits. Significant interest rate declines could significantly increase the Company’s liabilities for these contracts.
As the 7-year Treasury rate (claim interest rate) declines, the claim amounts that the Company expects to pay out for the guaranteed minimum income benefit business increases. For a subset of the business, there is a contractually guaranteed floor of 3% for the claim interest rate. Significant interest rate declines could significantly increase the Company’s net liabilities for guaranteed minimum income benefit contracts because of increased exposures.
A downgrade in the financial strength ratings of CIGNA’s insurance subsidiaries could adversely affect new sales and retention of current business, and a downgrade in CIGNA’s debt ratings would increase the cost of borrowed funds and affect ability to access capital.
Financial strength, claims paying ability and debt ratings by recognized rating organizations are an important factor in establishing the competitive position of insurance companies and health benefits companies. Ratings information by nationally recognized ratings agencies is broadly disseminated and generally used throughout the industry. CIGNA believes the claims paying ability and financial strength ratings of its principal insurance subsidiaries are an important factor in marketing its products to certain of CIGNA’s customers. In addition, CIGNA Corporation’s debt ratings impact both the cost and availability of future borrowings, and accordingly, its cost of capital. Each of the rating agencies reviews CIGNA’s ratings periodically and there can be no assurance that current ratings will be maintained in the future. In addition, a downgrade of these ratings could make it more difficult to raise capital and to support business growth at CIGNA’s insurance subsidiaries.
CIGNA CORPORATION – 2010 Form 10-K – 40
Insurance ratings represent the opinions of the rating agencies on the financial strength of a company and its capacity to meet the obligations of insurance policies. The principal agencies that rate CIGNA’s insurance subsidiaries characterize their insurance rating scales as follows:
•
A.M. Best Company, Inc. (“A.M. Best”), A++ to S (“Superior” to “Suspended”);
•
Moody’s Investors Service (“Moody’s”), Aaa to C (“Exceptional” to “Lowest”);
•
Standard & Poor’s Corp. (“S&P”), AAA to R (“Extremely Strong” to “Regulatory Action”); and
•
Fitch, Inc. (“Fitch”), AAA to D (“Exceptionally Strong” to “Order of Liquidation”).
As of February 25, 2011, the insurance financial strength ratings for CIGNA subsidiaries, CGLIC and Life Insurance Company of North America (“LINA”) were as follows:
|
CGLIC Insurance Ratings (1) |
LINA Insurance Ratings (1) |
|
|
A.M. Best |
A (“Excellent”, 3rd of 16) |
A (“Excellent”, 3rd of 16) |
|
Moody’s |
A2 (“Good”, 6th of 21) |
A2 (“Good”, 6th of 21) |
|
S&P |
A (“Strong”, 6th of 21) |
(Not Rated) |
|
Fitch |
A (“Strong”, 6th of 24) |
A (“Strong”, 6th of 24) |
|
(1) Includes the rating assigned, the agency’s characterization of the rating and the position of the rating in the agency’s rating scale (e.g., CGLIC’s rating by A.M. Best is the 3rd highest rating awarded in its scale of 16). |
||
Global market, economic and geopolitical conditions may cause fluctuations in equity market prices, interest rates and credit spreads which could impact the Company’s ability to raise or deploy capital as well as affect the Company’s overall liquidity.
If the capital markets and credit market experience extreme volatility and disruption, there could be downward pressure on stock prices and credit capacity for certain issuers without regard to those issuers’ underlying financial strength. Extreme disruption in the credit markets could adversely impact the Company’s availability and cost of credit in the future. In addition, unpredictable or unstable market conditions could result in reduced opportunities to find suitable opportunities to raise capital.
Operational and Other Risks
CIGNA’s business depends on the uninterrupted operation of its systems and business functions, including information technology and other business systems.
CIGNA’s business is highly dependent upon its ability to perform, in an efficient and uninterrupted fashion, its necessary business functions, such as: claims processing and payment; internet support and customer call centers; and the processing of new and renewal business. A power outage, pandemic, or failure of one or more of information technology, telecommunications or other systems could cause slower system response times resulting in claims not being processed as quickly as clients desire, decreased levels of client service and client satisfaction, and harm to CIGNA’s reputation. In addition, because CIGNA’s information technology and telecommunications systems interface with and depend on third-party systems, CIGNA could experience service denials if demand for such service exceeds capacity or a third-party system fails or experiences an interruption. If sustained or repeated, such a business interruption, systems failure or service denial could result in a deterioration of CIGNA’s ability to pay claims in a timely manner, provide customer service, write and process new and renewal business, or perform other necessary corporate functions. This could result in a materially adverse effect on CIGNA’s business results and liquidity.
CIGNA CORPORATION – 2010 Form 10-K – 41
A security breach of CIGNA’s computer systems could also interrupt or damage CIGNA’s operations or harm CIGNA’s reputation. In addition, CIGNA could be subject to liability if sensitive customer information is misappropriated from CIGNA’s computer systems. These systems may be vulnerable to physical break-ins, computer viruses, programming errors, attacks by third parties or similar disruptive problems. Any publicized compromise of security could result in a loss of customers or a reduction in the growth of customers, increased operating expenses, financial losses, additional litigation or other claims, which could have a material adverse effect on CIGNA’s business.
CIGNA is focused on further developing its business continuity program to address the continuation of core business operations. While CIGNA continues to test and assess its business continuity program to satisfy the needs of CIGNA’s core business operations and addresses multiple business interruption events, there is no assurance that core business operations could be performed upon the occurrence of such an event.
Effective prevention, detection or control systems are critical to maintain regulatory compliance or prevent fraud and failure to have these systems in place could adversely affect the Company.
Failure of CIGNA’s prevention, detection or control systems related to regulatory compliance and compliance with CIGNA’s internal policies, including data systems security and unethical conduct by managers and employees, could adversely affect CIGNA’s reputation and also expose it to litigation and other proceedings, fines and penalties. Federal and state governments have made investigating and prosecuting health care and other insurance fraud and abuse a priority. Fraud and abuse prohibitions encompass a wide range of activities, including kickbacks for referral of members, billing for unnecessary medical services, improper marketing, and violations of patient privacy rights. The regulations and contractual requirements applicable to the Company are complex and subject to change. Although the Company believes its compliance efforts are adequate, ongoing vigorous law enforcement, a highly technical regulatory scheme and recent adoption of the Dodd-Frank legislation enhancing regulators’ enforcement powers and whistleblower incentives and protections mean that its compliance efforts in this area will continue to require significant resources.
In addition, provider or member fraud that is not prevented or detected could impact CIGNA’s medical costs or those of its self-insured customers. Further, during an economic downturn, CIGNA’s segments, including HealthCare, Disability and Life and International, may see increased fraudulent claims volume which may lead to additional cost because of an increase in disputed claims and litigation.
CIGNA also faces other risks that may adversely affect our business, results of operations, or financial condition, including but not limited to:
•
a material weakness in our internal controls over financial reporting;
•
requirements to restate financial results due to inappropriate or changing interpretation of the application of accounting principles that would have a significant effect on CIGNA’s reported results of operations and financial condition;
•
large scale natural disasters, public health epidemics or other geopolitical events that could cause CIGNA’s covered medical and disability expenses, pharmacy costs and mortality experience to rise significantly or cause operational disruption; and
•
competition faced by the Company to attract and retain key people to effectively execute the Company’s key initiatives and business strategy.
CIGNA CORPORATION – 2010 Form 10-K – 42
ITEM 1B Unresolved Staff Comments
None.
ITEM 2 Properties
CIGNA’s global real estate portfolio consists of approximately 6.6 million square feet of owned and leased properties. Our domestic portfolio has approximately 5.8 million square feet in 37 states, District of Columbia, and Puerto Rico. Our International properties contain approximately 800,000 square feet located throughout the following countries:
Belgium, Canada, China, France, Germany, Hong Kong, Indonesia, Ireland, Italy, Netherlands, New Zealand, Portugal, Singapore, South Korea, Spain, Sweden, Switzerland, Taiwan, Thailand, Turkey, United Arab Emirates, United Kingdom, and Vietnam.
Our principal, domestic office locations, including staff support operations, along with CIGNA Disability and Life Insurance, the domestic office of CIGNA International, and CIGNA HealthCare, are the Wilde Building located at 900 Cottage Grove Road in Bloomfield, Connecticut and Two Liberty Place located at 1601 Chestnut Street in Philadelphia, Pennsylvania. The Wilde Building is owned with approximately 825,000 square feet and Two Liberty Place contains approximately 460,000 square feet of leased office space.
CIGNA believes its properties are adequate and suitable for our business as presently conducted. The foregoing does not include information on investment properties.
ITEM 3 Legal Proceedings
The information contained under “Litigation and Other Legal Matters” in Note 24 to CIGNA’s Financial Statements beginning on page 159 of this Form 10-K, is incorporated herein by reference.
CIGNA CORPORATION – 2010 Form 10-K – 43
Executive Officers of the Registrant
All officers are elected to serve for a one-year term or until their successors are elected. Principal occupations and employment during the past five years are listed below.
WILLIAM L. ATWELL, 60, President of CIGNA International beginning September 2008; and Managing Director of Atwell and Associates, LLC from January 2006 until August 2008.
DAVID M. CORDANI, 45, Chief Executive Officer of CIGNA beginning December 2009; President of CIGNA beginning June 2008; Chief Operating Officer of CIGNA from June 2008 until December 2009; President of CIGNA HealthCare from July 2005 until June 2008; and a Director of CIGNA since October 2009.
PHILIP D. EMOND, 55, Executive Vice President and Chief Information Officer of CIGNA beginning October 2010; Senior Vice President of CIGNA’s Information Technology Applications from June 2008 until October 2010; and Executive Vice President of Canadian Imperial Bank of Commerce from August 2000 until March 2005.
THOMAS A. MCCARTHY, 54, Acting Chief Financial Officer of CIGNA beginning September 1, 2010; Vice President of CIGNA responsible for CIGNA’s strategy and corporate development, including mergers and acquisitions and corporate risk management beginning April 2003; and Treasurer of CIGNA from July 2008 until January 2011.
MATTHEW G. MANDERS, 49, President of CIGNA, US Service, Clinical and Specialty beginning January 2010; President of CIGNA HealthCare, Total Health, Productivity, Network & Middle Market from June 2009 until January 2010; Customer Segments from July 2006 until June 2009; and President of CIGNA HealthCare, Middle Market Segment from August 2004 until July 2006.
JOHN M. MURABITO, 52, Executive Vice President of CIGNA beginning August 2003, with responsibility for Human Resources and Services.
CAROL ANN PETREN, 58, Executive Vice President and General Counsel of CIGNA beginning May 2006, Corporate Secretary of CIGNA beginning May 2010; and Senior Vice President and Deputy General Counsel of MCI from August 2003 until March 2006.
BERTRAM L. SCOTT, 58, President of CIGNA, US Commercial beginning June 2010; Executive Vice President and Chief Development and Sales Officer of TIAA-CREF from August 2008 until June 2010; Executive Vice President, Strategy, Implementation and Policy of TIAA-CREF from September 2006 until August 2008; and Executive Vice President, Product Management of TIAA-CREF from November 2003 until September 2006.
CIGNA CORPORATION – 2010 Form 10-K – 44
|
PART II |
ITEM 5 Market for registrant’s common equity, related stockholder matters and issuer purchases of equity securities
The information under the caption “Quarterly Financial Data — Stock and Dividend Data” appears on page 166 and the number of shareholders of record as of December 31, 2010 appears under the caption “Highlights” on page 46 of this Form 10-K. CIGNA’s common stock is listed with, and trades on, the New York Stock Exchange under the symbol “CI”.
Issuer Purchases of Equity Securities
The following table provides information about CIGNA’s share repurchase activity for the quarter ended December 31, 2010:
ISSUER PURCHASES OF EQUITY SECURITIES
|
Period |
Total # of shares purchased (1) |
Average price paid per share |
Total # of shares purchased |
Approximate dollar value of shares that may yet be purchased as part of publicly announced program (3) |
|
October 1-31, 2010 |
224 |
$36.15 |
0 |
$247,329,268 |
|
November 1-30, 2010 |
2,391 |
$37.32 |
0 |
$247,329,268 |
|
December 1-31, 2010 |
598 |
$37.32 |
0 |
$247,329,268 |
|
TOTAL |
3,213 |
$37.24 |
0 |
N/A |
|
(1) Includes shares tendered by employees as payment of taxes withheld on the exercise of stock options and the vesting of restricted stock granted under the Company’s equity compensation plans. Employees tendered 224 shares in October, 2,391 shares in November, and 598 shares in December. (2) CIGNA has had a repurchase program for many years, and has had varying levels of repurchase authority and activity under this program. The program has no expiration date. CIGNA suspends activity under this program from time to time, generally without public announcement. Through February 25, 2011, the Company had repurchased approximately 1.8 million shares for approximately $73 million. On February 23, 2011, the Board of Directors increased share repurchase authority by $500 million. Remaining authorization under the program was $247 million as of December 31, 2010 and $674 million as of February 25, 2011. (3) Approximate dollar value of shares is as of the last date of the applicable month. |
||||
CIGNA CORPORATION – 2010 Form 10-K – 45
ITEM 6 Selected Financial Data
Highlights
|
(Dollars in millions, except per share amounts) |
2010 |
2009 |
2008 |
2007 |
2006 |
|
Revenues | |||||
|
Premiums and fees and other revenues |
$18,653 |
$16,161 |
$17,004 |
$15,376 |
$13,987 |
|
Net investment income |
1,105 |
1,014 |
1,063 |
1,114 |
1,195 |
|
Mail order pharmacy revenues |
1,420 |
1,282 |
1,204 |
1,118 |
1,145 |
|
Realized investment gains (losses) |
75 |
(43) |
(170) |
16 |
219 |
|
TOTAL REVENUES |
$21,253 |
$18,414 |
$19,101 |
$17,624 |
$16,546 |
|
Results of Operations: | |||||
|
Health Care |
$861 |
$731 |
$664 |
$679 |
$653 |
|
Disability and Life |
291 |
284 |
273 |
254 |
226 |
|
International |
243 |
183 |
182 |
176 |
138 |
|
Run-off Reinsurance |
26 |
185 |
(646) |
(11) |
(14) |
|
Other Operations |
85 |
86 |
87 |
109 |
106 |
|
Corporate |
(211) |
(142) |
(162) |
(97) |
(95) |
|
Realized investment gains (losses), net of taxes and noncontrolling interest |
50 |
(26) |
(110) |
10 |
145 |
|
Shareholders’ income from continuing operations |
1,345 |
1,301 |
288 |
1,120 |
1,159 |
|
Income from continuing operations attributable to noncontrolling interest |
4 |
3 |
2 |
3 |
- |
|
Income from continuing operations |
1,349 |
1,304 |
290 |
1,123 |
1,159 |
|
Income (loss) from discontinued operations, net of taxes |
- |
1 |
4 |
(5) |
(4) |
|
NET INCOME |
$1,349 |
$1,305 |
$294 |
$1,118 |
$1,155 |
|
Shareholders’ income per share from continuing operations: | |||||
|
Basic |
$4.93 |
$4.75 |
$1.04 |
$3.91 |
$3.46 |
|
Diluted |
$4.89 |
$4.73 |
$1.03 |
$3.86 |
$3.43 |
|
Shareholders’ net income per share: | |||||
|
Basic |
$4.93 |
$4.75 |
$1.05 |
$3.89 |
$3.45 |
|
Diluted |
$4.89 |
$4.73 |
$1.05 |
$3.84 |
$3.42 |
|
Common dividends declared per share |
$0.04 |
$0.04 |
$0.04 |
$0.04 |
$0.03 |
|
Total assets |
$45,682 |
$43,013 |
$41,406 |
$40,065 |
$42,399 |
|
Long-term debt |
$2,288 |
$2,436 |
$2,090 |
$1,790 |
$1,294 |
|
Shareholders’ equity |
$6,645 |
$5,417 |
$3,592 |
$4,748 |
$4,330 |
|
Per share |
$24.44 |
$19.75 |
$13.25 |
$16.98 |
$14.63 |
|
Common shares outstanding (in thousands) |
271,880 |
274,257 |
271,036 |
279,588 |
98,654 |
|
Shareholders of record |
8,568 |
8,888 |
9,014 |
8,696 |
9,117 |
|
Employees |
30,600 |
29,300 |
30,300 |
26,600 |
27,100 |
Beginning in 2010, the Company began reporting the expense associated with its frozen pension plans in Corporate. Prior periods were not restated. The effect on prior periods was not material.
In 2008, the Company recorded significant charges related to the guaranteed minimum income benefits and guaranteed minimum death benefits businesses as well as an after-tax litigation charge of $52 million in Corporate related to the CIGNA pension plan. For additional information, see the Run-off Reinsurance section of the Management’s Discussion and Analysis beginning on page 75 and Note 24 to the Consolidated Financial Statements.
During 2007, CIGNA completed a three-for-one stock split of CIGNA’s common shares. Per share figures for 2006 reflect the stock split. Pro forma common shares outstanding, calculated as if the stock split had occurred at the beginning of 2006, were 295,963 in 2006.
CIGNA CORPORATION – 2010 Form 10-K – 46
ITEM 7 Management’s Discussion and Analysis of Financial Condition and Results of Operations
Index
|
|
|
|
|
|
|
|
|
|
|
|
Introduction
As used in this document, “CIGNA” and the “Company” may refer to CIGNA Corporation itself, one or more of its subsidiaries, or CIGNA Corporation and its consolidated subsidiaries. CIGNA Corporation is a holding company and is not an insurance company. Its subsidiaries conduct various businesses, which are described in this Annual Report on Form 10-K for the fiscal year ended December 31, 2010 (“Form 10-K”).
In this filing and in other marketplace communications, the Company makes certain forward-looking statements relating to the Company’s financial condition and results of operations, as well as to trends and assumptions that may affect the Company. Generally, forward-looking statements can be identified through the use of predictive words (e.g., “Outlook for 2010”). Actual results may differ from the Company’s predictions. Some factors that could cause results to differ are discussed throughout Management’s Discussion and Analysis (“MD&A”), including in the Cautionary Statement beginning on page 95. The forward-looking statements contained in this filing represent management’s current estimate as of the date of this filing. Management does not assume any obligation to update these estimates.
The following discussion addresses the financial condition of the Company as of December 31, 2010, compared with December 31, 2009, and a comparison of results of operations for the years ended December 31, 2010, 2009 and 2008.
CIGNA is a global health service organization with subsidiaries that are major providers of medical, dental, disability, life and accident insurance and related products and services. In the U.S., the majority of these products and services are offered through employers and other groups (e.g. unions and associations) and in selected international markets, CIGNA offers supplemental health, life and accident insurance products, expatriate benefits and international health care coverage and services to businesses, governmental and non-governmental organizations and individuals. In addition to its ongoing operations described above, the Company also has certain run-off operations, including a Run-off Reinsurance segment.
Unless otherwise indicated, financial information in the MD&A is presented in accordance with accounting principles generally accepted in the United States (“GAAP”). Certain reclassifications have been made to prior period amounts to conform to the presentation of 2010 amounts. See Note 2 to the Consolidated Financial Statements for additional information.
CIGNA CORPORATION – 2010 Form 10-K – 47
Overview of 2010 Results
Summarized below are the key highlights for 2010. For additional information, see the remaining sections of this MD&A, which discuss both consolidated and segment results in more detail.
Key Consolidated Financial Data
|
(Dollars in millions) |
2010 |
2009 |
2008 |
|
Revenues |
$21,253 |
$18,414 |
$19,101 |
|
Medical membership (in thousands) (1) |
12,473 |
11,669 |
12,338 |
|
Adjusted income from operations (2) |
$1,277 |
$1,097 |
$946 |
|
Shareholders’ income from continuing operations |
$1,345 |
$1,301 |
$398 |
|
Cash flows from operating activities |
$1,743 |
$745 |
$1,656 |
|
Shareholders’ equity |
$6,645 |
$5,417 |
$3,592 |
|
(1) Includes medical members of the Company’s Health Care segment as well as the International health care business, including expatriate benefits. (2) For a definition of adjusted income from operations, see the “Consolidated Results of Operations” section of this MD&A beginning on page 53. |
|||
Results of Operations
•
Revenues rose significantly in 2010, reflecting strong premium growth in the Company’s ongoing operating segments due to solid growth in each of the Company’s targeted markets. Net investment income and realized investment results also improved significantly primarily reflecting improving economic conditions.
•
Medical membership increased, reflecting the acquisition of Vanbreda International as well as the strength of the Company’s value proposition centered around health advocacy and its focus on growth in targeted markets, primarily the middle market and select segments.
•
Adjusted income from operations increased significantly in 2010, reflecting focused execution of the Company’s business strategy, which includes a growing global customer base.
•
Shareholders’ income from continuing operations also increased, but at a lower rate than adjusted income from operations. This is primarily due to significantly lower results in the Company’s run-off GMIB business. Results from this business are volatile, as key market inputs to the valuation of these assets and liabilities, such as interest rates, are adjusted each quarter.
•
Cash flows from operating activities remain strong, reflecting solid underlying earnings as well as business growth. Strong operating cash flows enabled the Company to contribute $212 million to its pension plan as well as to repurchase 6.2 million shares of stock for $201 million.
Liquidity and Financial Condition
During 2010, the Company entered into several transactions to position itself to execute on its strategy as well as to strengthen its liquidity and financial condition.
•
The recent acquisition of Vanbreda International in the third quarter of 2010 positions the Company to be a global leader in the delivery of expatriate benefits.
•
The Company sold its workers’ compensation and case management business to GENEX Holdings.
•
The Company reduced its balance sheet exposure in the run-off reinsurance operations by reinsuring its run-off workers’ compensation and personal accident business.
•
The Company retired portions of its long-term debt through a tender offer process, and issued replacement debt at a significantly lower interest rate.
Shareholders’ equity increased substantially during 2010, reflecting strong shareholders’ net income as well as increased invested asset values (primarily fixed maturities) reflecting lower market yields. Those favorable impacts were partially offset by the unfavorable effects of the pension plan liability on shareholders’ equity due to changes in the discount rate and mortality assumptions. The Company’s commercial mortgage loan portfolio continued to perform well, with minimal write-downs and stabilizing real estate valuations.
CIGNA CORPORATION – 2010 Form 10-K – 48
Business Strategy
As a global health service organization, CIGNA’s mission is to help the people it serves improve their health, well-being and sense of security. As part of this mission, the Company remains committed to health advocacy as a means of creating sustainable solutions for employers, improving the health of the individuals that the Company serves, and lowering the costs of health care for all constituencies.
CIGNA’s long-term growth strategy is based on: (1) growth in targeted geographies, product lines, buying segments and distribution channels; (2) improving its strategic and financial flexibility; and (3) pursuing additional opportunities in high-growth markets with particular focus on individuals. Our strategy can be summarized as follows:
•
“Go deep” with growth in targeted customer segments, geographies, buying segments and distribution channels;
•
“Go individual” by delivering high quality products and services which improve health, wellness and insurance needs that are helpful and easy to use; and
•
“Go global” by pursuing additional opportunities in high-growth markets across the globe and serving individuals regardless of where they live and work.
To achieve these goals, CIGNA expects to focus on the following which have the most potential for profitable growth:
•
Domestic Health Care segment. In this market, CIGNA is focused on expanding and deepening client and customer relationships across each segment. Specifically: (1) within key geographic segments, growing the “Select” market, which generally includes employers with more than 50 but fewer than 250 employees and the “Middle Market” segment which generally includes employers with more than 250 but less than 5,000 employees, by leveraging the Company’s customer knowledge, differentiated service model, product portfolio and distribution model; (2) engaging those national account employers who share and will benefit from the Company’s value proposition of using health advocacy and employee engagement to increase productivity, performance and the health outcomes of their employees; and (3) targeting sub-markets including industry, government and municipal entities and individuals that align closest to the Company’s stated strategy.
•
In the Disability and Life segment, CIGNA’s strategy is to grow its Disability business by fully leveraging the key components of its industry-leading disability management model to reduce costs for its clients and return their employees to work sooner through: (1) effective customer engagement and early outreach; (2) a full suite of clinical and return-to-work resources to support the employer’s ability to manage disability and work related events; and (3) specialized case management services that address an individual’s unique needs.
•
In the International segment, CIGNA continues to expand the product and geographic footprint by executing local strategies that grow supplemental, primary medical and expatriate benefits through: (1) product and channel expansion in its supplemental health, life and accident business in key Asian geographies; (2) the introduction of new expatriate benefits products, that provide greater benefit and geographic flexibility to individual and employers (such as through the Vanbreda International acquisition); and (3) further expansion of distribution capabilities to capitalize on emerging and growing markets globally.
The Company plans to improve its strategic and financial flexibility by driving further reductions in its Health Care operating expenses, improving its medical cost competitiveness in targeted markets and effectively managing balance sheet exposures.
See the “Run-off operations” section below for further discussion of the Company’s actions to manage its balance sheet exposures. The Company’s operational strategies are discussed further in the Health Care segment section of the MD&A beginning on page 63.
The Company’s ability to increase revenue, shareholders’ net income and operating cash flows from ongoing operations is directly related to progress on the execution of its strategy as described above as well as other key factors, including the Company’s ability to:
•
profitably price products and services at competitive levels that reflect emerging experience;
•
cross sell its various health and related benefit products;
•
invest available cash at attractive rates of return for appropriate durations; and
•
effectively deploy capital.
CIGNA CORPORATION – 2010 Form 10-K – 49
In addition to the Company-specific factors cited above, overall results are influenced by a range of economic and other factors, especially:
•
cost trends and inflation for medical and related services;
•
utilization patterns of medical and other services;
•
employment levels;
•
the tort liability system;
•
developments in the political environment both domestically and internationally, including U.S. health care reform;
•
interest rates, equity market returns, foreign currency fluctuations and credit market volatility, including the availability and cost of credit in the future; and
•
federal, state and international regulation.
The Company regularly monitors the trends impacting operating results from the above mentioned key factors to appropriately respond to economic and other factors affecting its operations, both in its ongoing and run-off operations.
Run-off Operations
The Company’s run-off reinsurance operations have significant exposures, primarily for its guaranteed minimum death benefits (“GMDB”, also known as “VADBe”) and guaranteed minimum income benefits (“GMIB”) products. As part of its strategy to effectively manage these exposures, the Company operates an equity hedge program to substantially reduce the impact of equity market movements on the liability for the GMDB business. The Company actively monitors the performance of the hedge program, and evaluates the cost/benefit of hedging other risks, including interest rate risk.
These products are also influenced by a range of economic and behavioral factors that were not hedged as of December 31, 2010, including:
•
equity markets for GMIB contracts;
•
interest rates;
•
future partial surrender elections for GMDB contracts;
•
annuity election rates for guaranteed minimum income benefits (“GMIB”) contracts;
•
annuitant lapse rates; and
•
the collection of amounts recoverable from retrocessionaires.
In order to manage these factors, the Company:
•
actively studies policyholder behavior experience and adjusts future expectations based on the results of the studies, as warranted;
•
implemented a partial hedge in February 2011 for a portion of the equity market risk for GMIB contracts and a portion of the interest rate risk for GMDB and GMIB contracts, and will continue to evaluate further adjustments to the hedging program;
•
performs regular audits of ceding companies to ensure compliance with agreements as well as to help maximize the collection of receivables from retrocessionaires; and
•
monitors the financial strength and credit standing of its retrocessionaires and establishes or collects collateral when warranted.
Health Care Reform
In the first quarter of 2010, the Patient Protection and Affordable Care Act, including the Reconciliation Act of 2010, (“Health Care Reform”) was signed into law. Health Care Reform mandates broad changes in the delivery of health care benefits that may impact the Company’s current business model, including its relationship with current and future customers, producers and health care providers, products, services, processes and technology. Health Care Reform includes, among others, provisions for mandatory coverage of benefits, a minimum medical loss ratio for insured business, eliminates lifetime and annual benefit limits and creates health insurance exchanges. The provisions of the law take effect over the next several years from 2010 to 2018. Many provisions of Health Care Reform have become effective during 2010, and interim final regulations have been issued, however there are still many provisions which have yet to become effective, and it is possible that the ultimate impact of Health Care Reform could have a material impact on the Company’s results of operations. The Company is evaluating potential business opportunities resulting from Health Care Reform that will enable it to leverage the strengths and capabilities of its broad health and wellness portfolio.
CIGNA CORPORATION – 2010 Form 10-K – 50
Health Care Reform will require the assessment of fees and excise taxes on health services companies such as CIGNA and others in the health care industry to help fund the additional insurance benefits and coverages provided by this legislation. The amount which the Company will be required to pay starting in 2013 and 2014 for these fees and excise taxes will result in charges to the Company’s financial statements in future periods. In addition, since these fees and excise taxes will not be tax deductible, the Company’s effective tax rate is expected to increase in future periods. However, the Company is unable to estimate the amount of these fees and excise taxes or the increase in the effective tax rate because guidance for the calculation has not been finalized.
Health Care Reform also changes certain tax laws which affected the Company’s 2010 financial statements. Although these provisions do not become effective until 2013, they are expected to limit the tax deductibility of certain future retiree benefit and compensation-related payments earned after 2009. The Company recorded after-tax charges of approximately $10 million for the twelve months ended December 31, 2010 related to these changes. The Company will continue to evaluate the impact of these tax laws as further guidance is made available.
During 2010, the Company incurred total after-tax costs of approximately $25 million related to Health Care Reform comprised of:
•
$10 million of additional income tax related to the impact of the tax law changes as described previously, and
•
$15 million of costs related to building the infrastructure necessary to comply with the provisions of Health Care Reform which were effective in 2010 and 2011 of which $7 million were incremental costs. The remaining $8 million reflected the estimated cost of internal staff redeployed to work on Health Care Reform initiatives.
Many provisions of Health Care Reform are not effective until future years and the Company will continue to implement these provisions. On January 1, 2011, the minimum loss ratio became effective and will require payment of premium rebates beginning in 2012 to employers and customers covered under the Company’s comprehensive medical insurance if certain minimum medical loss ratios are not met. Management estimates charges for rebates to approximate $25 million after-tax for the year ending December 31, 2011. This estimate followed the most current regulatory guidance for the calculation of rebates and was developed using assumptions about the amount and distribution for claim experience, enrollment and premiums earned by state and market segment. Actual rebates could differ substantially from management’s estimates if actual experience differs from the assumptions.
Management is currently unable to estimate the full impact of Health Care Reform on the Company’s future results of operations, and its financial condition and liquidity due to uncertainties related to interpretation, implementation and timing of its many provisions. It is possible; however, that this impact could be material to future results of operations. Management, through its internal task force, continues to closely monitor implementation of the law, report on the Company’s compliance with Health Care Reform, actively engage with regulators to assist with the ongoing conversion of legislation to regulation and assess potential opportunities arising from Health Care Reform.
Acquisitions and Dispositions
In line with its growth strategy, the Company has strengthened its market position and reduced balance sheet exposures through the following acquisition and disposition transactions.
Reinsurance of Run-off Workers’ Compensation and Personal Accident Business
On December 31, 2010, the Company essentially exited from its workers’ compensation and personal accident reinsurance business by purchasing retrocessional coverage from a Bermuda subsidiary of Enstar Group Limited and transferring administration of this business to the reinsurer. See Note 3 to the Consolidated Financial Statements for additional information.
Sale of Workers’ Compensation and Case Management Business
On December 1, 2010 the Company completed the sale of its workers’ compensation and case management business to GENEX Holdings, Inc. The Company recognized an after-tax gain on sale of $11 million ($18 million before tax) which was reported in other revenues in the Disability and Life segment. See Note 3 to the Consolidated Financial Statements for additional information.
Acquisition of Vanbreda International
On August 31, 2010, the Company acquired 100% of the voting stock of Vanbreda International NV (“Vanbreda International”), based in Antwerp, Belgium for a cash purchase price of $412 million. See Note 3 to the Consolidated Financial Statements for additional information about the acquisition of Vanbreda International.
CIGNA CORPORATION – 2010 Form 10-K – 51
Acquisition of Great-West Healthcare
On April 1, 2008, the Company acquired the Health care division of Great-West Life and Annuity, Inc. (“Great-West Healthcare”). See Note 3 to the Consolidated Financial Statements for additional information.
Initiatives to Lower Operating Expenses
As part of its strategy, the Company has undertaken several initiatives to realign its organization and consolidate support functions in an effort to increase efficiency and responsiveness to customers and to reduce costs.
During 2008 and 2009, the Company conducted a comprehensive review to reduce certain operating expenses of its ongoing businesses (“cost reduction program”). As a result, the Company recognized severance-related and real estate charges in other operating expenses.
Severance charges in 2008 and 2009 resulted from reductions of approximately 2,350 positions in the Company’s workforce. Cost reduction activities associated with these charges are substantially complete as of December 31, 2010 with severance expected to be paid by the end of the second quarter of 2011. In 2010, the Company recorded an incremental pre-tax charge of $6 million ($4 million after-tax) to reflect actual severance experience differing from prior assumptions.
Cost reduction activity for 2008, 2009 and 2010 was as follows:
|
(In millions) |
Severance |
Real Estate |
Total |
|
Fourth Quarter 2008 charge (balance carried to January 1, 2009) |
$44 |
$11 |
$55 |
|
Second Quarter |
14 |
- |
14 |
|
Third Quarter |
10 |
- |
10 |
|
Fourth Quarter |
20 |
- |
20 |
|
Subtotal — 2009 charges |
44 |
- |
44 |
|
Less: Payments |
55 |
3 |
58 |
|
Balance, December 31, 2009 |
33 |
8 |
41 |
|
Add: change in estimate to severance accrual |
6 |
- |
6 |
|
Less: 2010 Payments | |||
|
First Quarter |
10 |
1 |
11 |
|
Second Quarter |
8 |
5 |
13 |
|
Third Quarter |
7 |
1 |
8 |
|
Fourth Quarter |
5 |
1 |
6 |
|
Balance, December 31, 2010 |
$9 |
$- |
$9 |
The Health Care segment reported substantially all of the 2010 charge, $37 million pre-tax ($24 million after-tax) of the 2009 charges and $44 million pre-tax ($27 million after-tax) of the 2008 charge. The remainder of the 2009 and 2008 charges were reported as follows: Disability and Life: $5 million pre-tax ($4 million after-tax) in 2009 and $3 million pre-tax ($2 million after-tax) in 2008; and International: $2 million pre-tax ($1 million after-tax) in 2009 and $8 million pre-tax ($6 million after-tax) in 2008.
The Company expects annualized after-tax savings from this cost reduction program to be approximately $130 million in 2011 and beyond. A portion of the savings was realized in 2009 while most was realized in 2010.
CIGNA CORPORATION – 2010 Form 10-K – 52
Consolidated Results of Operations
The Company measures the financial results of its segments using “segment earnings (loss)”, which is defined as shareholders’ income (loss) from continuing operations before after-tax realized investment results. Adjusted income from operations is defined as consolidated segment earnings (loss) excluding special items (defined below) and the results of the GMIB business. Adjusted income from operations is another measure of profitability used by the Company’s management because it presents the underlying results of operations of the Company’s businesses and permits analysis of trends in underlying revenue, expenses and shareholders’ net income. This measure is not determined in accordance with GAAP and should not be viewed as a substitute for the most directly comparable GAAP measure, which is shareholders’ income from continuing operations.
Summarized below is a reconciliation between shareholders’ income from continuing operations and adjusted income from operations.
|
Financial Summary (In millions) |
2010 |
2009 |
2008 |
|
Premiums and fees |
$18,393 |
$16,041 |
$16,253 |
|
Net investment income |
1,105 |
1,014 |
1,063 |
|
Mail order pharmacy revenues |
1,420 |
1,282 |
1,204 |
|
Other revenues |
260 |
120 |
751 |
|
Realized investment gains (losses) |
75 |
(43) |
(170) |
|
Total revenues |
21,253 |
18,414 |
19,101 |
|
Benefits and expenses |
19,383 |
16,516 |
18,719 |
|
Income from continuing operations before taxes |
1,870 |
1,898 |
382 |
|
Income taxes |
521 |
594 |
92 |
|
Income from continuing operations |
1,349 |
1,304 |
290 |
|
Less: income from continuing operations attributable to noncontrolling interest |
4 |
3 |
2 |
|
Shareholders’ income from continuing operations |
1,345 |
1,301 |
288 |
|
Less: realized investment gains (losses), net of taxes |
50 |
(26) |
(110) |
|
SEGMENT EARNINGS |
1,295 |
1,327 |
398 |
|
Less: adjustments to reconcile to adjusted income from operations: | |||
|
Results of GMIB business (after-tax): | |||
|
Charge on adoption of fair value measurements for GMIB contracts |
- |
- |
(131) |
|
Results of GMIB business excluding charge on adoption |
(24) |
209 |
(306) |
|
Special items (after-tax): | |||
|
Resolution of a federal tax matter (See Note 20 to the Consolidated Financial Statements) |
101 |
- |
- |
|
Loss on early extinguishment of debt (See Note 16 to the Consolidated Financial Statements) |
(39) |
- |
- |
|
Loss on reinsurance transaction (See Note 3 to the Consolidated Financial Statements) |
(20) |
- |
- |
|
Curtailment gain (See Note 10 to the Consolidated Financial Statements) |
- |
30 |
- |
|
Cost reduction charges (See Note 6 to the Consolidated Financial Statements) |
- |
(29) |
(35) |
|
Completion of IRS examination (See Note 20 to the Consolidated Financial Statements) |
- |
20 |
- |
|
Charges related to litigation matters (See Note 24 to the Consolidated Financial Statements) |
- |
- |
(76) |
|
ADJUSTED INCOME FROM OPERATIONS |
$1,277 |
$1,097 |
$946 |
Summarized below is adjusted income from operations by segment:
|
Adjusted Income (Loss) From Operations (In millions) |
2010 |
2009 |
2008 |
|
Health Care |
$861 |
$729 |
$715 |
|
Disability and Life |
291 |
279 |
275 |
|
International |
243 |
182 |
188 |
|
Run-off Reinsurance |
(27) |
(24) |
(209) |
|
Other Operations |
85 |
85 |
87 |
|
Corporate |
(176) |
(154) |
(110) |
|
TOTAL |
$1,277 |
$1,097 |
$946 |
CIGNA CORPORATION – 2010 Form 10-K – 53
Overview of 2010 Consolidated Results of Operations
Adjusted income from operations increased 16% in 2010 compared with 2009 primarily due to strong earnings growth in the ongoing business segments (Health Care, Disability and Life and International), reflecting focused execution of the Company’s strategy, which includes a growing global customer base as well as higher net investment income reflecting improved economic conditions and asset growth. See the individual segment sections of this MD&A for further discussion.
Shareholders’ income from continuing operations increased 3% in 2010 compared with 2009, reflecting strong growth in adjusted income from operations as explained above as well as significant improvement in realized investment results, partially offset by a loss in the GMIB business in 2010 compared with a significant gain in 2009. See the Run-off Reinsurance section of the MD&A beginning on page 75 for additional information on GMIB results.
Overview of 2009 Consolidated Results of Operations
Adjusted income from operations increased 16% in 2009 compared with 2008 primarily reflecting significantly improved results in the Run-off Reinsurance segment due to a lower amount of reserve strengthening required for the GMDB business in 2009 compared with 2008. This result was primarily due to improved equity market conditions in 2009. Also, in the aggregate, adjusted income from operations from the Company’s ongoing operating segments (Health Care, Disability and Life, and International) improved slightly in 2009 over 2008. These favorable effects were partially offset by higher unallocated costs (including interest) reported in Corporate.
Shareholders’ income from continuing operations for the year ended December 31, 2009 was significantly higher than 2008, reflecting improved adjusted income from operations, as explained above, as well as the following:
•
substantially improved results in the GMIB business due to improved equity market conditions and generally higher interest rates;
•
improved realized investment results, also reflecting better market conditions during 2009; and
•
the favorable year over year impact of the following special items as detailed in the table above: completion of the IRS examination; the curtailment gain on the pension plan; and the absence of litigation charges in 2009.
Special Items and GMIB
Management does not believe that the special items noted in the table above are representative of the Company’s underlying results of operations. Accordingly, the Company excluded these special items from adjusted income from operations in order to facilitate an understanding and comparison of results of operations and permit analysis of trends in underlying revenue, expenses and shareholders’ income from continuing operations.
Special items for 2010 included:
•
a gain resulting from the resolution of a federal income tax matter, consisting of a $97 million release of a deferred tax valuation allowance and $4 million of accrued interest. See Note 20 for further information;
•
a loss on the extinguishment of debt resulting from the decision of certain holders of the Company’s 8.5% Notes due 2019 and 6.35% Notes due 2018 to accept the Company’s tender offer to redeem these Notes for cash. See Note 16 for further information; and
•
a loss on reinsurance of the run-off workers’ compensation and personal accident reinsurance businesses to Enstar. See Note 3 for further information.
Special items for 2009 included a curtailment gain resulting from the decision to freeze the pension plan (see Note 10 to the Consolidated Financial Statements for additional information), cost reduction charges related to the 2008 cost reduction program (see the Introduction section of the MD&A beginning on page 47 of this Form 10-K), and benefits resulting from the completion of the 2005 and 2006 IRS examinations (see Note 20 to the Consolidated Financial Statements for additional information).
Special items for 2008 included a cost reduction charge related to the 2008 cost reduction program (see the Introduction section of the MD&A beginning on page 47 of this Form 10-K), a litigation matter related to the CIGNA Pension Plan (see Note 24 to the Consolidated Financial Statements for additional information) reported in Corporate and charges related to certain other litigation matters, which are reported in the Health Care segment.
CIGNA CORPORATION – 2010 Form 10-K – 54
The Company also excludes the results of the GMIB business from adjusted income from operations because the fair value of GMIB assets and liabilities must be recalculated each quarter using updated capital market assumptions. The resulting changes in fair value, which are reported in shareholders’ net income, are volatile and unpredictable. See the Critical Accounting Estimates section of the MD&A beginning on page 57 of this Form 10-K for more information on the effect of capital market assumption changes on shareholders’ net income. Because of this volatility, and since the GMIB business is in run-off, management does not believe that its results are meaningful in assessing underlying results of operations. The loss for the GMIB business in 2010 primarily reflects the impact of declining interest rates, partially offset by favorable equity market performance, whereas the gain in 2009 primarily reflected increases in interest rates combined with favorable equity market performance. See the Run-off Reinsurance section of the MD&A beginning on page 75 for further information on the GMIB business.
Outlook for 2011
The Company expects 2011 adjusted income from operations to be approximately level with 2010. This outlook includes an assumption that GMDB (also known as “VADBe”) results will be approximately break-even for 2011, which assumes that actual experience, including capital market performance, will be consistent with long-term reserve assumptions. See Note 7 to the Consolidated Financial Statements and the Critical Accounting Estimates section of this MD&A beginning on page 57 for more information on the potential effect of capital market and other assumption changes on shareholders’ net income.
Information is not available for management to reasonably estimate the future results of the GMIB business or realized investment results due in part to interest rate and stock market volatility and other internal and external factors. In addition, the Company is not able to identify or reasonably estimate the financial impact of special items in 2011 however they may include potential adjustments associated with cost reduction, litigation, tax and assessment-related matters.
The Company’s outlook for 2011 is subject to the factors cited above and in the Cautionary Statement beginning on page 95 of this Form 10-K and the sensitivities discussed in the Critical Accounting Estimates section of the MD&A beginning on page 57 of this Form 10-K. If unfavorable equity market and interest rate movements occur, the Company could experience losses related to investment impairments and the GMIB and GMDB businesses. These losses could adversely impact the Company’s consolidated results of operations and financial condition by potentially reducing the capital of the Company’s insurance subsidiaries and reducing their dividend-paying capabilities.
Revenues
Total revenues increased by 15% in 2010, compared with 2009, and decreased by 4% in 2009 compared with 2008. Changes in the components of total revenue are described in more detail below.
Premiums and Fees
Premiums and fees increased by 15% in 2010, compared with 2009, primarily reflecting membership growth in the Health Care segment’s risk businesses as well as growth in the International segment. Premiums and fees increased by 10% in 2010 compared with 2009 after excluding the Medicare Private Fee for Service (“Medicare PFFS”) Individual business, from which the Company has exited beginning in 2011.
Premiums and fees decreased by 1% in 2009, compared with 2008, primarily reflecting membership declines in Health Care resulting from higher unemployment and the unfavorable effect of foreign currency translation in International, offset by the absence of premium and fees from Great West Healthcare in the first quarter of 2008 since this business was acquired April 1, 2008.
Net Investment Income
Net investment income increased by 9% in 2010, compared with 2009, primarily reflecting improved results from security partnerships and real estate investments and higher assets due to business growth, partially offset by lower reinvestment yields.
Net investment income decreased by 5% in 2009, compared with 2008, primarily reflecting lower income from real estate investments and security partnerships, unfavorable foreign exchange rates and lower investment yields, partially offset by higher invested assets due to business growth.
CIGNA CORPORATION – 2010 Form 10-K – 55
Mail Order Pharmacy Revenues
Mail order pharmacy revenues increased by 11% in 2010, compared with 2009, primarily reflecting increases in volume and, to a lesser extent, price increases and by 6% in 2009, compared with 2008, primarily due to price increases.
Other Revenues
Other revenues include the impact of futures contracts associated with the GMDB equity hedge program. Losses on futures contracts reflect stock market gains, whereas gains reflect stock market losses. The Company reported losses associated with the GMDB equity hedge program of $157 million in 2010 and $282 million in 2009 compared with gains of $333 million in 2008. Excluding the impact of the futures contracts associated with the GMDB equity hedge program, Other revenues increased 4% in 2010, compared with 2009 primarily reflecting the pre-tax gain on the sale of the workers’ compensation and case management business of $18 million.
Excluding the impact of the futures contracts associated with the GMDB equity hedge program, Other revenues decreased 4% in 2009, compared with 2008, primarily reflecting declines in amortization of deferred gains on the sales of the retirement benefits and individual life insurance and annuity business.
Realized Investment Results
Realized investment results in 2010 were significantly higher than in 2009 primarily due to:
•
lower impairments on fixed maturities and real estate funds in 2010;
•
increased prepayment fees on fixed maturities received in 2010 as a result of favorable market conditions and issuer specific business circumstances; and
•
gains on sales of real estate held in joint ventures and other investments in 2010.
These favorable effects were partially offset by an increase in commercial mortgage loan impairments recorded in 2010, reflecting continued weakness in the commercial real estate market.
Realized investment results in 2009 were significantly improved compared to 2008, primarily due to:
•
lower asset write-downs on fixed maturities largely reflecting improved market conditions;
•
gains on sales of fixed maturities and equities in 2009 compared with losses in 2008; and
•
gains on hybrid securities in 2009 compared with losses in 2008 (changes in fair value for these securities are reported in realized investment results).
These favorable effects were partially offset by higher impairments of investments in real estate entities and commercial mortgage loans in 2009 due to the impact of the continued weak economic environment on the commercial real estate market and the absence of significant gains on the sales of real estate ventures reported during 2008.
See Note 15 to the Consolidated Financial Statements for additional information.
CIGNA CORPORATION – 2010 Form 10-K – 56
Critical Accounting Estimates
The preparation of consolidated financial statements in accordance with GAAP requires management to make estimates and assumptions that affect reported amounts and related disclosures in the consolidated financial statements. Management considers an accounting estimate to be critical if:
•
it requires assumptions to be made that were uncertain at the time the estimate was made; and
•
changes in the estimate or different estimates that could have been selected could have a material effect on the Company’s consolidated results of operations or financial condition.
Management has discussed the development and selection of its critical accounting estimates with the Audit Committee of the Company’s Board of Directors and the Audit Committee has reviewed the disclosures presented below.
In addition to the estimates presented in the following table, there are other accounting estimates used in the preparation of the Company’s consolidated financial statements, including estimates of liabilities for future policy benefits other than those identified in the following table, as well as estimates with respect to goodwill, unpaid claims and claim expenses, postemployment and postretirement benefits other than pensions, certain compensation accruals, and income taxes.
Management believes the current assumptions used to estimate amounts reflected in the Company’s consolidated financial statements are appropriate. However, if actual experience differs from the assumptions used in estimating amounts reflected in the Company’s consolidated financial statements, the resulting changes could have a material adverse effect on the Company’s consolidated results of operations, and in certain situations, could have a material adverse effect on the Company’s liquidity and financial condition.
See Note 2 to the Consolidated Financial Statements for further information on significant accounting policies that impact the Company.
|
Balance Sheet Caption/Nature of Critical Accounting Estimate |
Assumptions/Approach Used |
Effect if Different Assumptions Used |
|
Future policy benefits — Guaranteed minimum death benefits (“GMDB” also known as “VADBe”) These liabilities are estimates of the present value of net amounts expected to be paid, less the present value of net future premiums expected to be received. The amounts to be paid represent the excess of the guaranteed death benefit over the values of contractholders’ accounts. The death benefit coverage in force at December 31, 2010 (representing the amount payable if all of approximately 530,000 contractholders had submitted death claims as of that date) was approximately $5 billion. Liabilities for future policy benefits for these contracts as of December 31 were as follows (in millions): • 2010 — $1,138 • 2009 — $1,285 |
The Company estimates these liabilities based on assumptions for lapse, partial surrender, claim mortality (deaths that result in claims), interest rates (mean investment performance and discount rate), and volatility. These assumptions are based on the Company’s experience and future expectations over the long-term period. The Company monitors actual experience to update these estimates as necessary.
Lapse: the full surrender of an annuity prior to a contractholder’s death.
Partial surrender: most contractholders have the ability to withdraw substantially all of their mutual fund investments while retaining death benefit coverage in effect at withdrawal. A partial surrender causes the value of the reinsured liability to increase reflecting lower future assumed premiums, a lower likelihood of lapse, and a lower likelihood that account values will recover sufficiently to reduce the death benefit exposure in the future. These effects are not covered by the Company’s GMDB equity hedge program. Market declines expose the Company to higher death benefit exposure and higher anticipated election rates of future partial surrenders. Thus, if equity markets decline, the Company’s liability for partial surrenders increases and there is no corresponding offset from the hedge program. The election rate for expected future partial surrenders is updated quarterly based on emerging experience.
Interest rates: include both: (a) the mean investment performance assumption, and (b) the liability discount rate assumption. The mean investment performance for underlying equity mutual funds considers the Company’s GMDB equity hedge program which reflects the average short-term interest rate to be earned over the life of the program and considers the current low level of interest rates. The mean investment performance for underlying fixed income mutual funds considers the expected market return over the life of the contracts.
Volatility: the degree of variation of future market returns of the underlying mutual fund investments. |
Current assumptions used to estimate these liabilities are detailed in Note 7 to the Consolidated Financial Statements. Based on current and historical market, industry and Company-specific experience and management’s judgment, the Company believes that it is reasonably likely that the unfavorable changes in the key assumptions and/or conditions described below could occur. If these unfavorable assumption changes were to occur, the approximate after-tax decrease in shareholders’ net income would be as follows: • 5% increase in claim mortality rates — $30 million; • 10% decrease in lapse rates — $20 million; • 10% increase in election rates for future partial surrenders — $5 million; • 50 basis point decrease in interest rates: Mean Investment Performance — $25 million, Discount Rate — $30 million; • 10% increase in volatility — $25 million. As of December 31, 2010, if contractholder account values invested in underlying equity mutual funds declined by 10% due to equity market performance, the after-tax decrease in shareholders’ net income resulting from an increase in the provision for partial surrenders would be approximately $10 million. As of December 31, 2010, if contractholder account values invested in underlying bond/money market mutual funds declined by 3% due to bond/money market performance, the after-tax decrease in shareholders’ net income resulting from an increase in the provision for partial surrenders and an increase in unhedged exposure would be approximately $10 million. The amounts would be reflected in the Run-off Reinsurance segment. |
CIGNA CORPORATION – 2010 Form 10-K – 57
|
Balance Sheet Caption/Nature of Critical Accounting Estimate |
Assumptions/Approach Used |
Effect if Different Assumptions Used |
|
Health Care medical claims payable Medical claims payable for the Health Care segment include both reported claims and estimates for losses incurred but not yet reported. Liabilities for medical claims payable as of December 31 were as follows (in millions): • 2010 — gross $1,246; net $1,010 • 2009 — gross $921; net $715 These liabilities are presented above both gross and net of reinsurance and other recoverables. These liabilities generally exclude amounts for administrative services only business. See Note 5 to the Consolidated Financial Statements for additional information. |
The Company develops estimates for Health Care medical claims payable using actuarial principles and assumptions consistently applied each reporting period, and recognizes the actuarial best estimate of the ultimate liability within a level of confidence, as required by actuarial standards of practice, which require that the liabilities be adequate under moderately adverse conditions. The liability is primarily calculated using “completion factors” (a measure of the time to process claims), which are developed by comparing the date claims were incurred, generally the date services were provided, to the date claims were paid. The Company uses historical completion factors combined with an analysis of current trends and operational factors to develop current estimates of completion factors. The Company estimates the liability for claims incurred in each month by applying the current estimates of completion factors to the current paid claims data. This approach implicitly assumes that historical completion rates will be a useful indicator for the current period. It is possible that the actual completion rates for the current period will develop differently from historical patterns, which could have a material impact on the Company’s medical claims payable and shareholders’ net income. Completion factors are impacted by several key items including changes in: 1) electronic (auto-adjudication) versus manual claim processing, 2) provider claims submission rates, 3) membership and 4) the mix of products. In addition, for the more recent months, the Company also relies on medical cost trend analysis, which reflects expected claim payment patterns and other relevant operational considerations. Medical cost trend is primarily impacted by medical service utilization and unit costs, which are affected by changes in the level and mix of medical benefits offered, including inpatient, outpatient and pharmacy, the impact of copays and deductibles, changes in provider practices and changes in consumer demographics and consumption behavior. Despite reflecting both historical and emerging trends in setting reserves, it is possible that the actual medical trend for the current period will develop differently from the expected, which could have a material impact on the Company’s medical claims payable and shareholders’ net income. For each reporting period, the Company evaluates key assumptions by comparing the assumptions used in establishing the medical claims payable to actual experience. When actual experience differs from the assumptions used in establishing the liability, medical claims payable are increased or decreased through current period shareholders’ net income. Additionally, the Company evaluates expected future developments and emerging trends which may impact key assumptions. The estimation process involves considerable judgment, reflecting the variability inherent in forecasting future claim payments. These estimates are highly sensitive to changes in the Company’s key assumptions, specifically completion factors, and medical cost trends. |
For the year ended December 31, 2010, actual experience differed from the Company’s key assumptions as of December 31, 2009, resulting in $93 million of favorable incurred claims related to prior years’ medical claims payable or 1.3% of the current year incurred claims as reported for the year ended December 31, 2009. For the year ended December 31, 2009, actual experience differed from the Company’s key assumptions as of December 31, 2008, resulting in $43 million of favorable incurred claims related to prior years’ medical claims, or 0.6% of the current year incurred claims reported for the year ended December 31, 2008. Specifically, the favorable impact is due to faster than expected completion factors and lower than expected medical cost trends, both of which included an assumption for moderately adverse experience. The impact of this favorable prior year development was an increase to shareholders’ net income of $26 million after-tax ($39 million pre-tax) for the year ended December 31, 2010. The change in the amount of the incurred claims related to prior years in the medical claims payable liability does not directly correspond to an increase or decrease in shareholders’ net income as explained in Note 5 to the Consolidated Financial Statements. |
CIGNA CORPORATION – 2010 Form 10-K – 58
|
Balance Sheet Caption/Nature of Critical Accounting Estimate |
Assumptions/Approach Used |
Effect if Different Assumptions Used |
|
Accounts payable, accrued expenses and other liabilities, and Other assets, including other intangibles — Guaranteed minimum income benefits These liabilities are calculated with a complex internal model using many scenarios to determine the fair value of amounts estimated to be paid, less the fair value of net future premiums estimated to be received, adjusted for risk and profit charges that the Company anticipates a hypothetical market participant would require to assume this business. The amounts estimated to be paid represent the excess of the anticipated value of the income benefit over the value of the annuitants’ accounts at the time of annuitization. The assets associated with these contracts represent receivables in connection with reinsurance that the Company has purchased from two external reinsurers, which covers 55% of the exposures on these contracts. Liabilities related to these contracts as of December 31, were as follows (in millions): • 2010 — $903 • 2009 — $903 As of December 31, estimated amounts receivable related to these contracts from two external reinsurers, were as follows (in millions): • 2010 — $480 • 2009 — $482 |
The Company considers the various assumptions used to estimate the fair values of assets and liabilities associated with these contracts in two categories: 1) capital market inputs; and 2) future annuitant behavior and other assumptions.
Capital market inputs include market returns and discount rates, claim interest rates and market volatility. This group of assumptions is largely based on market-observable inputs.
Interest rates include (a) market returns, (b) the liability discount rate assumption and (c) the projected interest rates used to calculate the reinsured income benefit at the time of annuitization (claim interest rate).
Volatility: the degree of variation of future market returns of the underlying mutual fund investments.
Future annuitant behavior and other inputs: these assumptions include annuity election rates, lapse, mortality, nonperformance risk (for both the Company and its retrocessionaires), and a risk and profit charge. This group of assumptions is based on the Company’s experience, industry data, and management’s judgment.
Annuity election rates: the proportion of annuitants who elect to receive their income benefit as an annuity.
Lapse: the full surrender of an annuity prior to annuitization of the policy.
Nonperformance risk: the market’s perception that either the Company will not fulfill its GMIB liability (own credit) or the Company will not collect on its GMIB retrocessional coverage (reinsurer credit risk).
Risk and profit charge: the amount that a hypothetical market participant would include in the valuation to cover the uncertainty of outcomes and the desired return on capital. |
Current assumptions used to estimate these liabilities are detailed in Note 11 to the Consolidated Financial Statements. The Company’s results of operations are expected to be volatile in future periods because most capital market assumptions will be based largely on market-observable inputs at the close of each period including interest rates and market implied volatilities. Based on current and historical market, industry and Company-specific experience and management’s judgment, the Company believes that it is reasonably likely that the unfavorable changes in the key assumptions and/or conditions described below could occur. If these unfavorable assumption changes were to occur, the approximate after-tax decrease in shareholders’ net income, net of estimated amounts receivable from reinsurers, would be as follows: • 50 basis point decrease in interest rates (which are aligned with LIBOR) used for projecting market returns and discounting — $15 million; • 50 basis point decrease in interest rates used for projecting claim exposure (7-year Treasury rates) — $25 million; • 20% increase in implied market volatility — $10 million; • 5% decrease in mortality — $1 million; • 10% increase in annuity election rates — $3 million; • 10% decrease in lapse rates — $5 million; • 10% increase to the risk and profit charge — $2 million. Market declines expose the Company to a larger net liability. Decreases in annuitants’ account values resulting from a 10% equity market decline could decrease shareholders’ net income by approximately $20 million. Decreases in annuitants’ account values resulting from a 3% decline due to bond/money market performance could decrease shareholders’ net income by approximately $2 million. If credit default swap spreads used to evaluate the nonperformance risk of the Company were to narrow or the credit rating of its principal life insurance subsidiary were to improve, it would cause a decrease in the discount rate of the GMIB liability, resulting in an unfavorable impact to earnings. If the discount rate decreased by 25 bps due to this, the decrease in shareholders’ net income would be approximately $10 million. |
CIGNA CORPORATION – 2010 Form 10-K – 59
|
Balance Sheet Caption/Nature of Critical Accounting Estimate |
Assumptions/Approach Used |
Effect if Different Assumptions Used |
|
Accounts payable, accrued expenses and other liabilities, and Other assets including other intangibles — Guaranteed minimum income benefits (continued) |
If credit default swap spreads used to evaluate the nonperformance risk of the Company’s GMIB retrocessionaires were to widen or the retrocessionaires’ credit ratings were to weaken, it would cause an increase in the discount rate of the GMIB asset, resulting in an unfavorable impact to earnings. If the discount rate increased by 25 bps due to this, the decrease in shareholders’ net income would be approximately $2 million. All of these estimated impacts due to unfavorable changes in assumptions could vary from quarter to quarter depending on actual reserve levels, the actual market conditions or changes in the anticipated view of a hypothetical market participant as of any future valuation date. The amounts would be reflected in the Run-off Reinsurance segment in GMIB expense. |
|
|
Accounts payable, accrued expenses and other liabilities — pension liabilities These liabilities are estimates of the present value of the qualified and nonqualified pension benefits to be paid (attributed to employee service to date) net of the fair value of plan assets. The accrued pension benefit liability as of December 31 was as follows (in millions): • 2010 — $1,528 • 2009 — $1,513 See Note 10 to the Consolidated Financial Statements for additional information. |
The Company estimates these liabilities and the related expense with actuarial models using various assumptions including discount rates and an expected long-term return on plan assets. Discount rates are set by applying actual annualized yields at various durations from the Citigroup Pension Liability curve, without adjustment, to the expected cash flows of the pension liabilities. The expected long-term return on plan assets for the domestic qualified pension plan is developed considering actual historical returns, expected long-term market conditions, plan asset mix and management’s investment strategy. In addition, to measure pension costs the Company uses a market-related asset value method for domestic qualified pension plan assets invested in non-fixed income investments, which are approximately 80% of total plan assets. This method recognizes the difference between actual and expected returns in the non-fixed income portfolio over 5 years, a method that reduces the short-term impact of market fluctuations on pension cost. At December 31, 2010, the market-related asset value was approximately $3.4 billion compared with a market value of $3.2 billion. The accumulated unrecognized actuarial loss of $1.8 billion at December 31, 2010 primarily reflects the significant decline in the value of equity securities during 2008 and, to a lesser extent, a decline in the discount rate and change in mortality assumption during 2010. The actuarial loss is adjusted for unrecognized changes in market-related asset values and amortized over the average remaining life expectancy of plan participants if the adjusted loss exceeds 10% of the market-related value of plan assets or 10% of the projected benefit obligation, whichever is greater. As of December 31, 2010, approximately $1.1 billion of the adjusted actuarial loss exceeded 10% of the projected benefit obligation. As a result, approximately $25 million after-tax of the unrecognized loss will be expensed in 2011 shareholders’ net income. For the year ended December 31, 2010, $18 million after-tax of the unrecognized loss was expensed in shareholders’ net income. |
Using past experience, the Company expects that it is reasonably possible that a favorable or unfavorable change in these key assumptions of 50 basis points could occur. An unfavorable change is a decrease in these key assumptions with resulting impacts as discussed below. If discount rates for the qualified and nonqualified pension plans decreased by 50 basis points: • annual pension costs for 2011 would decrease by approximately $3 million, after-tax; and • the accrued pension benefit liability would increase by approximately $225 million as of December 31, 2010 resulting in an after-tax decrease to shareholders’ equity of approximately $145 million as of December 31, 2010. If the expected long-term return on domestic qualified pension plan assets decreased by 50 basis points, annual pension costs for 2011 would increase by approximately $10 million after-tax. If the Company used the market value of assets to measure pension costs as opposed to the market-related value, annual pension cost for 2011 would increase by approximately $15 million after-tax. If the December 31, 2010 fair values of domestic qualified plan assets decreased by 10%, the accrued pension benefit liability would increase by approximately $315 million as of December 31, 2010 resulting in an after-tax decrease to shareholders’ equity of approximately $205 million. An increase in these key assumptions would result in impacts to annual pension costs, the accrued pension liability and shareholders’ equity in an opposite direction, but similar amounts. |
CIGNA CORPORATION – 2010 Form 10-K – 60
|
Balance Sheet Caption/Nature of Critical Accounting Estimate |
Assumptions/Approach Used |
Effect if Different Assumptions Used |
|
Investments — Fixed maturities Recognition of losses from “other- than-temporary” impairments of public and private placement fixed maturities To assess whether a fixed maturity’s decline in fair value below its amortized cost is other than temporary, the Company evaluates the expected recovery in value and its intent to sell or the likelihood of a required sale of the fixed maturity prior to an expected recovery. When the Company does not expect to recover a fixed maturity’s amortized cost, its fair value and expected future cash flows must be estimated by management to record an impairment loss. The credit portion of an impairment loss is recognized in shareholders’ net income and measured as the difference between a fixed maturity’s amortized cost and the net present value of its projected future cash flows. The non-credit portion, if any, is recognized in a separate component of shareholders’ equity. See Note 2 (C) to the Consolidated Financial Statements for additional information regarding the Company’s accounting policies for fixed maturities. |
When evaluating whether a loss is other than temporary, the Company considers factors including: • length of time and severity of decline; • financial health and specific near term prospects of the issuer; • changes in the regulatory, economic or general market environment of the issuer’s industry or geographic region; and • the Company’s intent to sell or the likelihood of a required sale prior to recovery. Management estimates other-than-temporary impairments based on fair values using quoted market prices for public securities with active markets and generally the present value of future cash flows for private placement bonds and other public securities. Expected future cash flows for each fixed maturity are based on the Company’s assessment of qualitative and quantitative factors, including the probability of default, and the estimated timing and amount of any recovery in value. See Note 11 to the Consolidated Financial Statements for a discussion of the Company’s fair value measurements. The Company recognized other -than- temporary impairments of investments in fixed maturities as follows (in millions, after-tax): • 2010 — $1 • 2009 — $31 • 2008 — $138 See Note 12 to the Consolidated Financial Statements for a discussion of the Company’s review of declines in fair value. |
For all fixed maturities with cost in excess of their fair value, if this excess was determined to be other-than-temporary, shareholders’ net income for the year ended December 31, 2010 would have decreased by approximately $51 million after-tax. For private placement bonds considered impaired, a decrease of 10% of all expected future cash flows for the impaired bonds would reduce shareholders’ net income by less than $1 million after-tax. |
CIGNA CORPORATION – 2010 Form 10-K – 61
|
Balance Sheet Caption/Nature of Critical Accounting Estimate |
Assumptions/Approach Used |
Effect if Different Assumptions Used |
|
Investments — Commercial Mortgage Loans — Valuation Reserves Recognition of losses from valuation reserves for impaired commercial mortgage loans To determine whether a commercial mortgage loan is impaired, the Company evaluates the likelihood of collecting all interest and principal payments in accordance with the contractual terms of the original loan agreement. When it is probable that the Company will not collect amounts due according to the terms of the original loan agreement, a loan is considered impaired and the Company must estimate the fair value of the underlying property to measure an impairment loss. An impairment loss is recorded using a valuation allowance for an impaired commercial mortgage loan’s carrying value in excess of the estimated fair value of its underlying property. Changes to valuation reserves are recorded in Realized investment gains (losses). See Note 2 (C) to the Consolidated Financial Statements for additional information regarding the Company’s accounting policies for commercial mortgage loans. |
The Company’s evaluation of the likelihood of collecting all contractual payments and the collateral fair value for commercial mortgage loans is a qualitative and quantitative process which is subject to uncertainties. The Company carefully evaluates all facts and circumstances for each loan and its supporting collateral. When evaluating the likelihood of collecting the contractual payments of a commercial mortgage loan, the Company considers factors including: • financial statements, budgets and operating plans for the property; • inspection reports of the property completed by third party servicers; • debt service coverage and loan-to-value ratio of the underlying collateral; • the borrower’s continuing financial commitment to the property; and • conditions and factors pertinent to the property and its local market. When it becomes probable that all contractual payments will not be collected according to the terms of the original loan agreement, the Company calculates the estimated fair value of the underlying property based on a 10-year discounted cash flow analysis. Factors key to this valuation include the following: • net operating income of the property; • rental and growth rates for the property and its local market; • capital requirements for the property; and • current market discount and capitalization rates. These evaluations are based primarily on an in-depth review of the commercial mortgage loan portfolio which is completed annually in the third quarter. The Company updates this annual review as material changes in these factors are identified. The Company recognized impairment losses from commercial mortgage loan valuation reserves as follows (in millions, after-tax): • 2010 — $15 • 2009 — $11 • 2008 — $0 See the Investment Assets section of the MD&A beginning on page 88 for discussion of the Company’s problem and potential problem mortgage loans and Note 12 to the Consolidated Financial Statements for further information surrounding impaired commercial mortgage loans. |
If loans with carrying values in excess of the fair value of their underlying property were considered impaired as of December 31, 2010, shareholders’ net income would decrease by approximately $11 million after-tax. If property values declined by 10% across the commercial mortgage loan portfolio as of December 31, 2010, approximately 18% of the portfolio’s loans would have carrying values in excess of their underlying properties’ fair values totaling approximately $80 million. And if each of these loans were considered impaired as of December 31, 2010, shareholders’ net income would decrease by approximately $52 million after-tax. If underlying property values declined by 10% for impaired commercial mortgage loans with valuation reserves as of December 31, 2010, shareholders’ net income would decrease by approximately $2 million after-tax. |
CIGNA CORPORATION – 2010 Form 10-K – 62
Segment Reporting
Operating segments generally reflect groups of related products, but the International segment is generally based on geography. The Company measures the financial results of its segments using “segment earnings (loss)”, which is defined as shareholders’ income (loss) from continuing operations excluding after-tax realized investment gains and losses. “Adjusted income from operations” for each segment is defined as segment earnings excluding special items and the results of the Company’s GMIB business. Adjusted income from operations is another measure of profitability used by the Company’s management because it presents the underlying results of operations of the segment and permits analysis of trends. This measure is not determined in accordance with GAAP and should not be viewed as a substitute for the most directly comparable GAAP measure, which is segment earnings. Each segment provides a reconciliation between segment earnings and adjusted income from operations.
Beginning in 2010, the Company began reporting the expense associated with its frozen pension plans in Corporate. Prior periods were not restated; the effect on prior periods is not material.
Health Care Segment
Segment Description
The Health Care segment offers insured and self-insured medical, dental, behavioral health, vision, and prescription drug benefit plans, health advocacy programs and other products and services that may be integrated to provide comprehensive health care benefit programs. CIGNA HealthCare companies offer these products and services in all 50 states, the District of Columbia and the U.S. Virgin Islands. These products and services are offered through a variety of funding arrangements such as guaranteed cost, retrospectively experience-rated and administrative services only arrangements.
The Company measures the operating effectiveness of the Health Care segment using the following key factors:
•
segment earnings and adjusted income from operations;
•
membership growth;
•
sales of specialty products to core medical customers;
•
changes in operating expenses per member; and
•
medical expense as a percentage of premiums (medical care ratio) in the guaranteed cost business.
Results of Operations
|
Financial Summary (In millions) |
2010 |
2009 |
2008 |
|
Premiums and fees |
$13,319 |
$11,384 |
$11,665 |
|
Net investment income |
243 |
181 |
200 |
|
Mail order pharmacy revenues |
1,420 |
1,282 |
1,204 |
|
Other revenues |
266 |
262 |
267 |
|
Segment revenues |
15,248 |
13,109 |
13,336 |
|
Mail order pharmacy cost of goods sold |
1,169 |
1,036 |
961 |
|
Benefits and other expenses |
12,742 |
10,943 |
11,359 |
|
Benefits and expenses |
13,911 |
11,979 |
12,320 |
|
Income before taxes |
1,337 |
1,130 |
1,016 |
|
Income taxes |
476 |
399 |
352 |
|
SEGMENT EARNINGS |
861 |
731 |
664 |
|
Less: special items (after-tax) included in segment earnings: | |||
|
Curtailment gain (See Note 10 to the Consolidated Financial Statements) |
- |
25 |
- |
|
Cost reduction charge (See Note 6 to the Consolidated Financial Statements) |
- |
(24) |
(27) |
|
Completion of IRS examination (See Note 20 to the Consolidated Financial Statements) |
- |
1 |
- |
|
Charge related to litigation matters (See Note 24 to the Consolidated Financial Statements) |
- |
- |
(24) |
|
ADJUSTED INCOME FROM OPERATIONS |
$861 |
$729 |
$715 |
|
Realized investment gains (losses), net of taxes |
$26 |
$(19) |
$(13) |
CIGNA CORPORATION – 2010 Form 10-K – 63
The Health Care segment’s adjusted income from operations increased 18% in 2010, as compared with 2009 reflecting:
•
revenue growth in the commercial risk businesses, particularly in the targeted market segments, as evidenced by a 15% increase in commercial risk membership. In addition, adjusted income from operations was favorably impacted by increased penetration of our specialty products;
•
a lower guaranteed cost medical care ratio driven by lower medical cost trend, reflecting lower utilization levels, as well as favorable prior year development; and
•
higher investment income due to higher security partnership results, higher real estate income and increased assets driven by membership growth.
Operating expense efficiencies were achieved by successful execution of cost reduction initiatives including staffing, real estate and pension changes, resulting in an approximately 3% decrease in the operating expense ratio. Despite this decline in the expense ratio, adjusted income from operations was reduced in 2010 by increased expenses related to business growth, investment in segment expansion, compliance and higher management incentive compensation.
The Health Care segment’s adjusted income from operations in 2009, as compared with 2008, was favorably impacted by the absence of a $7 million after-tax adjustment related to a large experience-rated life and non-medical account in run-out recorded in the first quarter of 2008.
Excluding this item, adjusted income from operations for 2009 was slightly higher than 2008 reflecting:
•
lower operating expenses, excluding the impact of an additional quarter from the Great-West Healthcare acquisition (effective April 1, 2008), primarily driven by cost reduction initiatives and pension plan changes, partially offset by higher management incentive compensation and higher information technology spend;
•
higher stop loss earnings largely from the Great-West Healthcare acquisition (effective April 1, 2008), tempered by lower margins on the remaining book; and
•
improved specialty earnings.
These favorable effects were largely offset by:
•
lower membership;
•
lower guaranteed cost earnings primarily reflecting a higher medical care ratio driven by unfavorable prior year development, as well as higher in-year claims due, in part to H1N1 flu-related claims; and
•
lower investment income primarily reflecting lower income from real estate funds.
CIGNA CORPORATION – 2010 Form 10-K – 64
Revenues
The table below shows premiums and fees for the Health Care segment:
|
(In millions) |
2010 |
2009 |
2008 |
|
Medical: | |||
|
Guaranteed cost (1) (2) |
$3,929 |
$3,380 |
$3,704 |
|
Experience-rated (2) (3) |
1,823 |
1,699 |
1,953 |
|
Stop loss |
1,287 |
1,274 |
1,197 |
|
Dental |
804 |
731 |
785 |
|
Medicare |
1,470 |
595 |
400 |
|
Medicare Part D |
558 |
342 |
327 |
|
Other (4) |
543 |
515 |
518 |
|
Total medical |
10,414 |
8,536 |
8,884 |
|
Life and other non-medical |
103 |
179 |
184 |
|
Total premiums |
10,517 |
8,715 |
9,068 |
|
Fees (2) (5) |
2,802 |
2,669 |
2,597 |
|
TOTAL PREMIUMS AND FEES |
$13,319 |
$11,384 |
$11,665 |
|
(1) Includes guaranteed cost premiums primarily associated with open access and commercial HMO, as well as other risk-related products. (2) Premiums and/or fees associated with certain specialty products are also included. (3) Includes minimum premium arrangements with a risk profile similar to experience-rated funding arrangements. The risk portion of minimum premium revenue is reported in experience-rated medical premium whereas the self funding portion of minimum premium revenue is recorded in fees. Also, includes certain non-participating cases for which special customer level reporting of experience is required. (4) Other medical premiums include risk revenue and specialty products. (5) Represents administrative service fees for medical members and related specialty product fees for non-medical members as well as fees related to Medicare Part D of $57 million in 2010, $41 million in 2009, and $69 million in 2008. |
|||
Premiums and fees increased by 17% in 2010 (10% excluding the Medicare PFFS Individual business, which the Company has exited beginning in 2011), compared with 2009, primarily reflecting membership growth in most risk-based products, including Medicare, and to a lesser extent rate increases. The membership growth was driven by strong retention and new sales in targeted market segments. The increase in fees primarily reflects growth in specialty products. These increases reflect the success of the Company’s efforts to enhance customer access, improve the quality of care and provide cost effective products and services.
Premiums and fees decreased 2% in 2009, compared with 2008, primarily reflecting lower membership largely due to disenrollment resulting from higher unemployment. This impact was partially offset by:
•
rate actions across all products;
•
increases in fees relating to specialty products;
•
membership growth in the Medicare private fee for service and Voluntary products; and
•
the impact of the Great-West Healthcare acquisition (effective April 1, 2008).
Net investment income increased by 34% in 2010 compared with 2009 primarily reflecting higher security partnership results, higher real estate income and increased invested assets driven by business growth. Net investment income decreased by 10% in 2009 compared with 2008 primarily reflecting lower income from real estate funds partially offset by higher invested assets.
Other revenues for the Health Care segment consist of revenues earned on direct channel sales of certain specialty products, including behavioral health and disease management.
CIGNA CORPORATION – 2010 Form 10-K – 65
Benefits and Expenses
Health Care segment benefits and expenses consist of the following:
|
(In millions) |
2010 |
2009 |
2008 |
|
Medical claims expense |
$8,570 |
$6,927 |
$7,252 |
|
Other benefit expenses |
100 |
169 |
193 |
|
Mail order pharmacy cost of goods sold |
1,169 |
1,036 |
961 |
|
Other operating expenses |
4,072 |
3,847 |
3,914 |
|
TOTAL BENEFITS AND EXPENSES |
$13,911 |
$11,979 |
$12,320 |
Medical claims expense increased by 24% in 2010 (13% excluding the Medicare PFFS Individual business, which the Company has exited beginning in 2011), compared with 2009 largely due to higher medical membership, particularly in the commercial risk and Medicare PFFS Individual business, the latter resulted in an increase of approximately $725 million for the year ended December 31, 2010 compared with last year. The increase also reflects medical cost inflation.
Medical claims expense decreased by 4% in 2009 compared with 2008 largely due to lower membership, particularly in the experience-rated and guaranteed cost businesses. This impact was partially offset by growth in Medicare membership and increases in medical expenses due to medical cost inflation as well as H1N1 flu-related claims.
Other operating expenses increased in 2010, compared with 2009, primarily due to increased membership in risk products, investment in segment expansion, compliance and higher management incentive compensation, partially offset by cost reduction initiatives including staffing, real estate and pension changes.
Excluding special items, other operating expenses increased slightly in 2009 compared with 2008, primarily due to expenses related to the Great-West Healthcare acquisition (effective April 1, 2008), higher management incentive compensation and higher information technology spend, mostly offset by cost reduction initiatives and pension plan changes as a result of the comprehensive review of ongoing expenses, as well as lower volume-related expenses.
Other Items Affecting Health Care Results
Health Care Medical Claims Payable
Medical claims payable increased $325 million for the year ended December 31, 2010 largely driven by medical membership growth, particularly in the Medicare PFFS and commercial risk businesses as noted above (see Note 5 to the Consolidated Financial Statements for additional information). The Medicare PFFS reserve balance was $167 million as of December 31, 2010. It is expected that a substantial portion of this reserve will be settled by December 31, 2011.
Medical Membership
A medical member reported within the Health Care segment (excluding members in the International and Disability and Life segments) is defined as a person who falls within one of the following categories:
•
is covered under an insurance policy or service agreement issued by the Company;
•
has access to the Company’s provider network for covered services under their medical plan;
•
has medical claims that are administered by the Company; or
•
is covered under an insurance policy that is (i) marketed by the Company, and (ii) for which the Company assumes reinsurance of at least 50%.
CIGNA CORPORATION – 2010 Form 10-K – 66
As of December 31, estimated medical membership was as follows:
|
(In thousands) |
2010 |
2009 |
2008 |
|
Guaranteed cost (1) |
1,177 |
1,001 |
1,092 |
|
Experience-rated (2) |
849 |
761 |
864 |
|
Total commercial risk |
2,026 |
1,762 |
1,956 |
|
Medicare |
145 |
52 |
35 |
|
Total risk |
2,171 |
1,814 |
1,991 |
|
Service |
9,266 |
9,226 |
9,688 |
|
TOTAL MEDICAL MEMBERSHIP (3) |
11,437 |
11,040 |
11,679 |
|
(1) Includes members primarily associated with open access, commercial HMO and voluntary/limited benefits as well as other risk-related products. (2) Includes minimum premium members, who have a risk profile similar to experience-rated members. Also, includes certain non-participating cases for which special customer level reporting of experience is required. (3) Excludes members in the International and Disability and Life Segments. |
|||
The Health Care segment’s medical membership increased 3.6% as of December 31, 2010 when compared with December 31, 2009. The increase was primarily driven by new business sales in targeted market segments: middle market, select and individual, as well as improved persistency in the risk businesses and lower disenrollment across all funding arrangements. The net decrease in the Health Care segment’s medical membership was 5.5% as of December 31, 2009 when compared with December 31, 2008. The decrease was primarily driven by disenrollment across all funding arrangements as a result of higher unemployment.
Operational Strategies
The Health Care segment is focused on several operational strategies including improving the efficiency of its operations, while growing its customer base in targeted markets and focusing on the needs of its customers. Savings generated from the reduction of operating expenses will provide the financial flexibility and capital to make investments that will enable the Company to enhance its capabilities, particularly in product development and the delivery of customer service, health advocacy and related technology. These capabilities are critical to enabling the Health Care segment to execute on its strategies to achieve profitable growth and retain customers. Successful execution of these operational strategies is critical to maintaining and improving its competitive position in the health care marketplace.
The operational strategies currently underway are discussed below.
Delivering superior service to customers and health care professionals
The Company is focused on delivering consistent, reliable and superior service to customers, health care professionals and clients. The Company believes that further enhancing service can improve customer retention and, when combined with useful health information and tools, can help motivate customers to become more engaged in their personal health. This will help to promote healthy outcomes thereby removing cost from the health care system. The evolution of the consumer-driven health care market is driving increased product and service complexity and is raising customers’ expectations with respect to service levels, which is expected to require significant investment, management attention and heightened interaction with customers.
The Company continues to focus on the development and enhancement of its service model that is capable of meeting the challenges brought on by the increasing product and service complexity and the heightened expectations of health care customers. The Company continues to make significant investments in the development and implementation of systems and technology to improve the provider service experience for customers and health care professionals (e.g. opening its Call Center 24/7), thereby enhancing its capabilities and improving its competitive position.
CIGNA CORPORATION – 2010 Form 10-K – 67
Profitable growth and customer retention
The Health Care segment continues to focus on retaining profitable relationships, expanding on those relationships and growing profitable new business by focusing on:
•
targeted market segments where buyers value our health improvement capabilities;
•
targeted geographic regions where the Company already has a strong market presence and competitive networks;
•
providing a diverse product portfolio that meets current market needs, as well as emerging consumer-directed trends;
•
developing and implementing the systems, information technology and infrastructure to deliver member service that keeps pace with the emerging consumer-directed market trends; and
•
increasing penetration of our specialty health care programs and services and cross-selling products sold primarily by other segments of the Company.
The Health Care segment is focused on market segment and product expansion. With respect to market segment expansion, the focus is predominantly in the “Middle Market” (employers with generally more than 250 but fewer than 5,000 employees), “Select” (employers with generally more than 50 but fewer than 250 employees), and “Individual” market segments. The Health Care segment is focusing on several strategic growth industries and targeting key geographic markets within the Select and Middle Market segments that align with our competitive strengths. The Health Care segment expects to grow its presence in these market segments by leveraging its customer knowledge, differentiated service model, product portfolio and distribution model. The Health Care segment continues to increase its penetration into the Individual market segment and will refine its strategy for this market segment based on the evolution of health care reform. In the “National” market segment (multi-site, multi-state commercial employers with generally more than 5,000 employees), the Company will selectively focus on clients that value its differentiated product offering. These clients include those seeking engagement and incentive based programs designed to improve health, and those that purchase multiple products and services from a single company.
Driving additional cross-selling is also key to the Company’s integrated benefits value proposition. The Company is expanding network access for its dental product and improving network flexibility to drive better alignment with customers’ needs including increasing disability and pharmacy penetration across the entire book.
Offering products that meet emerging customer and market trends
In addition to designing lower cost plan offerings to meet emerging customer and market trends, enhancements to the Company’s suite of products (CIGNA Choice Fund® CIGNA Health Advisor, CIGNA Incentive Points Program, CIGNA Choicelinx) offer various options to customers and employers that are key to our customer engagement strategy. By providing tools to our customers which will facilitate access and greater understanding of their health care choices, customers are better equipped to make effective health related decisions. CIGNA’s Cost of Care Estimator, Quicken Health and improvements to customer Explanation of Benefits and Health Statements are a part of the Company’s strategy to engage the individual by making information more available and easier to understand. In addition to operating clinics at employer sites, the Company has expanded their onsite health services to include onsite pharmacies, dedicated health advocates, hourly coaching services and onsite biometric screenings through the acquisition of Kronos.
Effectively managing medical costs
The Health Care segment operates under a centralized medical management model, which helps improve the health, well being and sense of security of its members, while reducing infrastructure expenses and driving productivity.
The Health Care segment is focused on continuing to effectively manage medical utilization and unit costs. The Company believes that by increasing the quality of medical care and improving access to care it can drive reductions in total medical cost and better outcomes, resulting in healthier members. To help achieve this, the Company continues to focus on contracting with health care professionals to strengthen its networks in targeted markets, enhancing clinical capabilities and engaging its customers and clients/employers.
Improving operating expense efficiency
The Company operates in an intensely competitive marketplace. The Company continues to be focused on improving its operating expense efficiency while balancing strategic investments to achieve its enterprise strategy. Within the Health care segment, the Company is focused on driving operating efficiency within its primary operating functions while investing prudently in technology, segment expansion and specialty products expense.
CIGNA CORPORATION – 2010 Form 10-K – 68
The Health Care segment’s operating expenses are comprised of three components and are approximately allocated as follows: health care (70%), specialty and market segment expansion (20%), and premium taxes and commissions (10%).
•
The health care component is the primary focus of improving operating expense efficiency. This component includes:
•
fulfillment activities, which are comprised of service operations, technology, and medical and network management;
•
customer acquisition, which represent costs for sales and account management, underwriting, and marketing and product development; and
•
staff functions, which represent finance, legal and human resources.
•
The specialty and market segment expansion and the premium tax/commission expense components would increase over time as revenues grow. Specialty includes disease management, pharmacy, dental, behavioral, and seniors coverages.
The Health Care segment expects to drive efficiencies and competitively manage its operating expenses while remaining focused on its other business strategies including investing in areas that are critical to the Company’s growth initiatives and segment expansions, ensuring continued excellence in customer service and clinical programs, and leveraging technology to drive further operating efficiencies.
CIGNA CORPORATION – 2010 Form 10-K – 69
Disability and Life Segment
Segment Description
The Disability and Life segment includes group disability, life, accident and specialty insurance.
Key factors for this segment are:
•
premium growth, including new business and customer retention;
•
net investment income;
•
benefits expense as a percentage of earned premium (loss ratio); and
•
other operating expense as a percentage of earned premiums and fees (expense ratio).
Results of Operations
|
Financial Summary (In millions) |
2010 |
2009 |
2008 |
|
Premiums and fees |
$2,667 |
$2,634 |
$2,562 |
|
Net investment income |
261 |
244 |
256 |
|
Other revenues |
123 |
113 |
117 |
|
Segment revenues |
3,051 |
2,991 |
2,935 |
|
Benefits and expenses |
2,640 |
2,598 |
2,553 |
|
Income before taxes |
411 |
393 |
382 |
|
Income taxes |
120 |
109 |
109 |
|
SEGMENT EARNINGS |
291 |
284 |
273 |
|
Less: special items (after-tax) included in segment earnings: | |||
|
Curtailment gain (See Note 10 to the Consolidated Financial Statements) |
- |
4 |
- |
|
Cost reduction charge (See Note 6 to the Consolidated Financial Statements) |
- |
(4) |
(2) |
|
Completion of IRS examination (See Note 20 to the Consolidated Financial Statements) |
- |
5 |
- |
|
ADJUSTED INCOME FROM OPERATIONS |
$291 |
$279 |
$275 |
|
Realized investment gains (losses), net of taxes |
$12 |
$(1) |
$(48) |
The Disability and Life segment’s adjusted income from operations increased 4% in 2010 compared to 2009 reflecting:
•
higher net investment income; and
•
the $11 million after-tax gain on the sale of the workers’ compensation and case management business.
Largely offsetting these factors were:
•
less favorable claims experience in the disability insurance business, primarily related to lower short-term disability underwriting margins. These results include the favorable after-tax impact of disability reserve studies of $29 million in 2010 compared with $20 million in 2009, which reflect continued strong disability claims management programs;
•
slightly less favorable accident claims experience including the less favorable after-tax impact of reserve studies of $3 million in 2010 compared with $5 million in 2009; and
•
lower earnings in specialty products.
The Disability and Life segment’s adjusted income from operations increased 1% in 2009 compared to 2008 reflecting:
•
favorable claims experience in the disability insurance business including the favorable after-tax impact of disability reserve studies of $20 million in 2009 compared with $8 million in 2008. The results in 2008 also included a $3 million favorable after-tax impact of a reinsurance settlement. The favorable claims experience and reserve study impacts are largely driven by continued strong disability claims management programs;
•
improved claims experience in the accident business including the more favorable after-tax impact of reserve studies of $5 million in 2009 compared with $3 million in 2008; and
•
higher premiums and fees in the disability and life businesses.
CIGNA CORPORATION – 2010 Form 10-K – 70
Largely offsetting these factors were:
•
lower results in the group life insurance business in 2009 primarily due to less favorable current year life claims experience, partially offset by the favorable after-tax impact of reserve studies of $9 million in 2009 compared with $3 million in 2008;
•
a higher operating expense ratio, including a litigation expense charge of $4 million;
•
lower net investment income; and
•
the absence of the 2008 favorable after-tax impact of specialty reserve studies of $2 million.
Revenues
Premiums and fees increased 1% in 2010 compared with 2009. The segment’s revenue growth was somewhat tempered by the Company’s exit from two large, non-strategic assumed government life insurance programs and the sale of the renewal rights for the student and participant accident business. Excluding the impact of these items, premiums and fees increased 7% as a result of disability and life sales growth combined with solid persistency.
Premiums and fees increased by 3% in 2009 compared with 2008 reflecting disability and life sales growth and solid persistency, partially offset by lower employment levels at the customers we serve, the Company’s exit from a large, low-margin assumed government life reinsurance program and the sale of the renewal rights for the student and participant accident business.
Net investment income increased by 7% in 2010 reflecting higher income from security and real estate partnerships and higher assets. Net investment income decreased by 5% in 2009 reflecting lower yields and lower security and real estate partnership income.
Other revenues include the $18 million pre-tax gain on the sale of the workers’ compensation and case management business in 2010.
Benefits and Expenses
Benefits and expenses increased 2% in 2010 compared with 2009, primarily reflecting:
•
disability and life business growth; and
•
less favorable claims experience in the short-term disability insurance business. These results reflect the favorable pre-tax impact of disability reserve studies of $43 million in 2010 compared with $29 million in 2009, largely driven by continued strong disability claims management programs.
These effects were partially offset by:
•
the Company’s exit from two large, non-strategic assumed government life insurance programs and the sale of the renewal rights for the student and participant accident business.
Benefits and expenses increased 2% in 2009 compared with 2008, primarily reflecting:
•
disability and life business growth;
•
less favorable life claims experience driven by the higher average size of death claims; and
•
a higher expense ratio in 2009 compared with 2008 reflecting strategic investments in the claim operations and information technology initiatives partially offset by a continued focus on operating expense management and lower disability and workers’ compensation case management expenses.
These effects were partially offset by:
•
more favorable disability claims experience including the favorable pre-tax impact of disability reserve studies of $29 million in 2009 compared with $15 million in 2008 resulting from higher resolutions driven by strong disability management programs partially offset by higher new claims;
•
more favorable accident claim experience, driven by lower new claims; and
•
the Company’s exit from a government life insurance program and sale of the renewal rights for the student and participant accident business.
CIGNA CORPORATION – 2010 Form 10-K – 71
International Segment
Segment Description
The International segment includes supplemental health, life and accident insurance products and international health care products and services, including those offered to expatriate employees of multinational corporations and other organizations.
The key factors for this segment are:
•
premium growth, including new business and customer retention;
•
benefits expense as a percentage of earned premium (loss ratio);
•
operating expense as a percentage of earned premium (expense ratio); and
•
impact of foreign currency movements.
Results of Operations
|
Financial Summary (In millions) |
2010 |
2009 |
2008 |
|
Premiums and fees |
$2,268 |
$1,882 |
$1,870 |
|
Net investment income |
82 |
69 |
79 |
|
Other revenues |
31 |
22 |
18 |
|
Segment revenues |
2,381 |
1,973 |
1,967 |
|
Benefits and expenses |
2,039 |
1,717 |
1,679 |
|
Income before taxes |
342 |
256 |
288 |
|
Income taxes |
95 |
70 |
104 |
|
Income attributable to noncontrolling interest |
4 |
3 |
2 |
|
SEGMENT EARNINGS |
243 |
183 |
182 |
|
Less: special items (after-tax) included in segment earnings: | |||
|
Cost reduction charge (See Note 6 to the Consolidated Financial Statements) |
- |
(1) |
(6) |
|
Curtailment gain (See Note 10 to the Consolidated Financial Statements) |
- |
1 |
- |
|
Completion of IRS examination (See Note 20 to the Consolidated Financial Statements) |
- |
1 |
- |
|
ADJUSTED INCOME FROM OPERATIONS |
$243 |
$182 |
$188 |
|
Impact of foreign currency movements using 2009 rates |
$13 | ||
|
Impact of foreign currency movements using 2008 rates |
$11 |
$(15) | |
|
Impact of permanent investment in overseas earnings: | |||
|
Implementation effect |
$5 |
$14 |
$- |
|
Effect of recording taxes at the tax rates of respective foreign jurisdictions |
25 |
8 |
- |
|
TOTAL |
$30 |
$22 |
$- |
|
Realized investment gains (losses), net of taxes |
$2 |
$2 |
$(3) |
Excluding the impact of the tax adjustments discussed below and foreign currency movements (presented in the table above), the International segment’s adjusted income from operations increased 25% for 2010, compared with 2009. The increase was primarily due to strong revenue growth and higher persistency in the supplemental health, life and accident insurance business, particularly in South Korea, as well as favorable loss ratios and membership growth in the expatriate employee benefits business and higher net investment income, partially offset by higher administrative expenses. Both businesses continue to deliver attractive margins.
Excluding the impact of the tax adjustments discussed below and foreign currency movements (presented in the table above), the International segment’s adjusted income from operations decreased 7% for 2009, compared with 2008. The decrease was primarily driven by unfavorable claims experience in the supplemental health, life and accident insurance business and the expatriate employee benefits business. The unfavorable effects were partially offset by revenue growth and competitively strong margins in both businesses.
CIGNA CORPORATION – 2010 Form 10-K – 72
During the first quarter of 2010, the Company’s International segment implemented a capital management strategy to permanently invest the earnings of its Hong Kong operation overseas. Income taxes for this operation, and the South Korean operation that implemented a similar strategy in the second quarter of 2009, are recorded at the tax rate of the respective foreign jurisdiction. See the Financial Summary table for the effect of these capital management strategies on International’s adjusted income from operations for each applicable period. The increase in the effect of recording taxes at the tax rates of respective foreign jurisdictions in 2010 primarily reflects higher pre-tax earnings in South Korea and, to a lesser extent, the addition of Hong Kong in 2010.
Throughout this discussion, the impact of foreign currency movements was calculated by comparing the reported results to what the results would have been had the exchange rates remained constant with the prior year’s comparable period exchange rates. The favorable impact in 2010 using 2009 rates, as well as the unfavorable change in 2009 using 2008 rates, primarily reflects the movement between the U.S. dollar and the South Korean won.
Revenues
Premiums and fees. Excluding the effect of foreign currency movements, premiums and fees were $2.2 billion in 2010, compared with reported premiums and fees of $1.9 billion in 2009, an increase of 16%. The increase was primarily attributable to new sales growth in the supplemental health, life and accident insurance operations, particularly in South Korea, and rate increases and membership growth in the expatriate employee benefits business. Excluding the effect of foreign currency movements, premiums and fees were $2.0 billion in 2009, compared with reported premiums and fees of $1.9 billion in 2008, an increase of 9%. The increase was primarily attributable to new sales growth in the supplemental health, life and accident insurance operations, particularly in Taiwan and South Korea, and rate actions in the expatriate employee benefits business.
Net investment income increased by 19% in 2010, compared with 2009. The increase was primarily due to favorable foreign currency movements and asset growth, particularly in South Korea. Net investment income decreased by 13% in 2009, compared with 2008. The decrease was primarily due to unfavorable foreign currency movements, primarily in South Korea.
Benefits and Expenses
Excluding the impact of foreign currency movements, benefits and expenses were $2.0 billion in 2010, compared with reported benefits and expenses of $1.7 billion in 2009, an increase of 15%. These increases were primarily due to business growth and higher claims in the supplemental health, life and accident insurance business, particularly in South Korea. Excluding the impact of foreign currency movements, benefits and expenses were $1.8 billion in 2009, compared with reported benefits and expenses of $1.7 billion in 2008, an increase of 9%. The increase was primarily driven by higher loss ratios, business growth, and increased amortization of deferred acquisition costs.
Loss ratios were higher in the supplemental health, life and accident insurance business in 2010, compared with 2009, reflecting less favorable claims experience. Loss ratios were lower in the expatriate benefits business in 2010, compared with 2009, reflecting favorable claim experience and rate increases on renewal business.
Policy acquisition expenses increased in 2010, compared with 2009, reflecting business growth and foreign currency movements. Policy acquisition costs decreased in 2009, compared to 2008, reflecting foreign currency movements partially offset by business growth and higher amortization of acquisition costs associated with lower persistency in the supplemental health, life and accident insurance business.
Expense ratios increased in 2010, compared with 2009, reflecting the acquisition costs associated with the purchase of Vanbreda International as well as the impact of the higher expense ratios associated with the acquired business. Expense ratios decreased in 2009, compared with 2008, reflecting effective expense management.
CIGNA CORPORATION – 2010 Form 10-K – 73
Other Items Affecting International Results
For the Company’s International segment, South Korea is the single largest geographic market. South Korea generated 32% of the segment’s revenues and 49% of the segment’s earnings in 2010. South Korea generated 29% of the segment’s revenues and 49% of the segment’s earnings in 2009. Due to the concentration of business in South Korea, the International segment is exposed to potential losses resulting from economic and geopolitical developments in that country, as well as foreign currency movements affecting the South Korean currency, which could have a significant impact on the segment’s results and the Company’s consolidated financial results.
As discussed in Note 3 to the Consolidated Financial Statements, the Company acquired Vanbreda International in August of 2010. This acquisition further strengthens CIGNA International’s position in the expatriate benefits market. Since the acquisition, earnings from Vanbreda International have been immaterial to results of operations. The Company expects Vanbreda International’s earnings to be accretive in 2011.
In China, CIGNA International owns a 50% interest in a joint venture through which its products and services are offered. The Company accounts for this joint venture using the equity method, recording its share of the joint venture’s net income in other revenues.
CIGNA CORPORATION – 2010 Form 10-K – 74
Run-off Reinsurance Segment
Segment Description
The Company’s reinsurance operations were discontinued and are now an inactive business in run-off mode since the sale of the U.S. individual life, group life and accidental death reinsurance business in 2000. This segment is predominantly comprised of GMDB, GMIB, workers’ compensation and personal accident reinsurance products. On December 31, 2010, the Company essentially exited from its workers compensation and personal accident reinsurance business by purchasing retrocessional coverage from a Bermuda subsidiary of Enstar Group Limited and transferring the ongoing administration of this business to the reinsurer. The 2010 special item loss reflects the after-tax costs of this transaction.
The determination of liabilities for GMDB and GMIB requires the Company to make critical accounting estimates. In 2008, the Company updated the assumptions for GMIB and the effects of hypothetical changes in those assumptions in connection with the implementation of the FASB’s fair value disclosure and measurement guidance (ASC 820). The Company describes the assumptions used to develop the reserves for GMDB in Note 7 to the Consolidated Financial Statements and for the assets and liabilities associated with GMIB in Note 11 to the Consolidated Financial Statements. The Company also provides the effects of hypothetical changes in those assumptions in the Critical Accounting Estimates section of the MD&A beginning on page 57 of this Form 10-K.
The Company excludes the results of the GMIB business from adjusted income from operations because the fair value of GMIB assets and liabilities must be recalculated each quarter using updated capital market assumptions. The resulting changes in fair value, which are reported in shareholders’ net income, are volatile and unpredictable.
Results of Operations
|
Financial Summary (In millions) |
2010 |
2009 |
2008 |
|
Premiums and fees |
$25 |
$29 |
$43 |
|
Net investment income |
114 |
113 |
104 |
|
Other revenues |
(158) |
(283) |
331 |
|
Segment revenues |
(19) |
(141) |
478 |
|
Benefits and expenses |
91 |
(419) |
1,499 |
|
Income (loss) before income taxes (benefits) |
(110) |
278 |
(1,021) |
|
Income taxes (benefits) |
(136) |
93 |
(375) |
|
SEGMENT EARNINGS (LOSS) |
26 |
185 |
(646) |
|
Less: special items (after-tax) included in segment earnings: | |||
|
Resolution of federal tax matters (See Note 20 to the Consolidated Financial Statements) |
97 |
- |
- |
|
Loss on Reinsurance transaction (See Note 3 to the Consolidated Financial Statements) |
(20) |
- |
- |
|
Less: results of GMIB business: | |||
|
Charge on adoption of fair value measurements for GMIB contracts |
- |
- |
(131) |
|
Results of GMIB business excluding charge on adoption |
(24) |
209 |
(306) |
|
ADJUSTED LOSS FROM OPERATIONS |
$(27) |
$(24) |
$(209) |
|
Realized investment gains (losses), net of taxes |
$5 |
$(2) |
$(19) |
The adjusted loss from operations for Run-off Reinsurance was larger in 2010 compared with 2009 due to reduced favorable after-tax impact of reserve studies ($6 million for 2010 compared to $16 million for 2009) and settlements and commutations ($3 million for 2010 compared to $11 million in 2009) for workers compensation and personal accident businesses, partially offset by reduced charges in 2010 to strengthen GMDB reserves ($34 million after-tax for 2010, compared to $47 million after-tax for 2009).
Segment earnings declined significantly in 2010 compared with 2009, primarily due to the reduction in earnings from the GMIB business, partially offset by the gain resulting from the resolution of a federal tax matter.
Adjusted income from operations for Run-off Reinsurance improved significantly in 2009 compared with 2008 due to significantly reduced charges in the GMDB business to strengthen reserves ($47 million after-tax for 2009, compared with $263 million for 2008) resulting from a substantially lower amount of reserve strengthening. The improvement in GMDB results in 2009 primarily reflected the recovery and stabilization of the financial markets. Adjusted income from operations also included the favorable after-tax impact of reserve studies for the workers compensation and personal accident business of $16 million in 2009 and $30 million in 2008.
CIGNA CORPORATION – 2010 Form 10-K – 75
Segment earnings were significantly higher in 2009, compared with 2008, due in part to the improvement in adjusted income from operations as discussed above and the significant improvement in GMIB results in 2009 (significant gains) compared with 2008 (significant losses).
For additional discussion of GMIB results, see “Benefits and Expenses” below.
Other Revenues
Other revenues included pre-tax losses from futures contracts used in the GMDB equity hedge program (see Note 7 to the Consolidated Financial Statements) of $157 million in 2010 and $282 million in 2009 compared with pre-tax gains of $333 million in 2008. Amounts reflecting corresponding changes in liabilities for GMDB contracts were included in benefits and expenses consistent with GAAP when a premium deficiency exists (see below “Other Benefits and Expenses”). The Company held futures contract positions related to this program with a notional amount of $0.9 billion at December 31, 2010.
Benefits and Expenses
Benefits and expenses were comprised of the following:
|
(In millions) |
2010 |
2009 |
2008 |
|
GMIB fair value (gain) loss |
$55 |
$(304) |
$690 |
|
Other benefits and expenses |
36 |
(115) |
809 |
|
BENEFITS AND EXPENSES |
$91 |
$(419) |
$1,499 |
GMIB fair value (gain) loss. Under the GAAP guidance for fair value measurements, the Company’s results of operations are expected to be volatile in future periods because capital market assumptions needed to estimate the assets and liabilities for the GMIB business are based largely on market-observable inputs at the close of each reporting period including interest rates (LIBOR swap curve) and market-implied volatilities. See Note 11 to the Consolidated Financial Statements for additional information about assumptions and asset and liability balances related to GMIB.
GMIB fair value losses of $55 million for 2010, were primarily due to declining interest rates, partially offset by increases in underlying account values resulting from favorable equity and bond fund returns, which result in decreased exposures.
GMIB fair value gains of $304 million for 2009, were primarily due to increases in interest rates and increases in underlying account values in the period resulting from favorable equity market and bond fund returns, resulting in reduced exposures. These favorable effects were partially offset by increases to the annuitization assumption and updates to the lapse assumptions.
GMIB fair value losses of $690 million for 2008 include a pre-tax charge of $202 million for the adoption of the FASB’s fair value disclosure and measurement guidance, which is discussed in Notes 2(B) and 11 to the Consolidated Financial Statements. Excluding the charge on adoption, the GMIB fair value losses of $488 million were primarily due to declines in interest rates, the impact of declines in underlying account values driven by declines in equity markets and bond fund returns, resulting in increased exposures, and unfavorable annuitization and lapse experience.
The GMIB liabilities and related assets are calculated using a complex internal model and assumptions from the viewpoint of a hypothetical market participant. This resulting liability (and related asset) is higher than the Company believes will ultimately be required to settle claims primarily because market-observable interest rates are used to project growth in account values of the underlying mutual funds to estimate fair value from the viewpoint of a hypothetical market participant. The Company’s payments for GMIB claims are expected to occur over the next 15 to 20 years and will be based on actual values of the underlying mutual funds and the 7-year Treasury rate at the dates benefits are elected. Management does not believe that current market-observable interest rates reflect actual growth expected for the underlying mutual funds over that timeframe, and therefore believes that the recorded liability and related asset do not represent what management believes will ultimately be required as this business runs off.
However, significant declines in mutual fund values that underlie the contracts (increasing the exposure to the Company) together with declines in the 7-year treasury rates (used to determine claim payments) similar to what occurred periodically during the last few years would increase the expected amount of claims that would be paid out for contractholders who choose to annuitize. It is also possible that such unfavorable market conditions would have an impact on the level of contractholder annuitizations, particularly if these unfavorable market conditions persisted for an extended period.
CIGNA CORPORATION – 2010 Form 10-K – 76
Other Benefits and Expenses are comprised of the following:
|
(In millions) |
2010 |
2009 |
2008 |
|
Equity market movements (corresponding change due to GMDB futures results) |
$(157) |
$(282) |
$333 |
|
GMDB reserve strengthening |
52 |
73 |
406 |
|
Other GMDB, primarily accretion of discount |
85 |
87 |
83 |
|
GMDB benefit expense (income) |
(20) |
(122) |
822 |
|
Loss on reinsurance of workers’ compensation and personal accident business |
31 |
- |
- |
|
Other, including operating expenses |
25 |
7 |
(13) |
|
OTHER BENEFITS AND EXPENSES (INCOME) |
$36 |
$(115) |
$809 |
Other Benefits and Expenses
Equity market movements
The reduction in benefits expense in 2010 and 2009 reflects favorable equity market performance, while the increase in 2008 reflects the significant decline in equity markets. As explained in Other revenues above, these changes do not affect shareholders’ net income because they are offset by gains or losses on futures contracts used to hedge equity market performance.
GMDB reserve strengthening
The following highlights the impacts of GMDB reserve strengthening:
•
2010: Primarily reflects management’s consideration of the anticipated impact of the continued low level of current short-term interest rates and, to a lesser extent, a reduction in assumed lapse rates for policies that have taken or are assumed to take significant partial withdrawals.
•
2009: Primarily due to an increase in the provision for future partial surrenders due to overall market declines, adverse volatility-related impacts due to turbulent equity market conditions and adverse interest rate impacts.
•
2008: Primarily due to the adverse impacts of overall market declines, volatility related impacts due to turbulent equity market conditions, and to a lesser extent, adverse interest rate impacts.
See Note 7 to the Consolidated Financial Statements for additional information about assumptions and reserve balances related to GMDB.
Other, including operating expenses
The increases were due to the reduced favorable impacts of reserve studies in each successive year, and additionally for 2010, the reduced impact of favorable settlements and commutations.
Segment Summary
The Company’s payment obligations for underlying reinsurance exposures assumed by the Company under these contracts are based on ceding companies’ claim payments. For GMDB and GMIB, claim payments vary because of changes in equity markets and interest rates, as well as mortality and policyholder behavior. Any of these claim payments can extend many years into the future, and the amount of the ceding companies’ ultimate claims, and therefore the amount of the Company’s ultimate payment obligations and corresponding ultimate collection from retrocessionaires may not be known with certainty for some time.
The Company’s reserves for underlying reinsurance exposures assumed by the Company, as well as for amounts recoverable from retrocessionaires, are considered appropriate as of December 31, 2010, based on current information. However, it is possible that future developments, which could include but are not limited to worse than expected claim experience and higher than expected volatility, could have a material adverse effect on the Company’s consolidated results of operations and could have a material adverse effect on the Company’s financial condition. The Company bears the risk of loss if its payment obligations to cedents increase or if its retrocessionaires are unable to meet, or successfully challenge, their reinsurance obligations to the Company.
CIGNA CORPORATION – 2010 Form 10-K – 77
Other Operations Segment
Segment Description
CIGNA’s Other Operations segment includes the results of the following businesses:
•
corporate-owned life insurance (“COLI”);
•
deferred gains recognized from the 1998 sale of the individual life insurance and annuity business and the 2004 sale of the retirement benefits business; and
•
run-off settlement annuity business.
COLI has contributed the majority of earnings in Other Operations for the periods presented and management expects this trend to continue in future periods as deferred gain amortization continues to decline from the sold businesses. The COLI regulatory environment continues to evolve, with various federal budget related proposals recommending changes in policyholder tax treatment. In addition, provisions of the Dodd-Frank financial reform legislation may limit the ability of some financial institutions to hold certain types of COLI contracts. Although regulatory and legislative activity could adversely impact our business and policyholders, management does not expect the impact to materially affect the Company’s results of operations, liquidity or financial condition.
Results of Operations
|
Financial Summary (In millions) |
2010 |
2009 |
2008 |
|
Premiums and fees |
$114 |
$112 |
$113 |
|
Net investment income |
404 |
407 |
414 |
|
Other revenues |
60 |
64 |
71 |
|
Segment revenues |
578 |
583 |
598 |
|
Benefits and expenses |
454 |
466 |
468 |
|
Income before taxes |
124 |
117 |
130 |
|
Income taxes |
39 |
31 |
43 |
|
SEGMENT EARNINGS |
85 |
86 |
87 |
|
Completion of IRS examination (See Note 20 to the Consolidated Financial Statements) |
- |
1 |
- |
|
ADJUSTED INCOME FROM OPERATIONS |
$85 |
$85 |
$87 |
|
Realized investment gains (losses), net of taxes |
$5 |
$(6) |
$(27) |
Adjusted income from operations for Other Operations was flat in 2010 compared with 2009, reflecting an increase in COLI earnings driven by higher investment income and favorable mortality, primarily offset by the continued decline in deferred gain amortization associated with the sold businesses.
Adjusted income from operations for Other Operations declined in 2009 compared with 2008, reflecting a continued decline in deferred gain amortization associated with the sold businesses offset by increased COLI earnings driven by higher investment income and improved operating expenses.
Revenues
Net investment income
Net investment income decreased 1% in 2010 compared with 2009, primarily reflecting lower yields, offset by higher average invested assets of the COLI business and improved income from real estate and security partnerships. Net investment income decreased 2% in 2009 compared with 2008 primarily reflecting lower average invested assets and lower real estate income.
Other revenues
Other revenues decreased 6% in 2010 compared with 2009 and decreased 10% in 2009 compared with 2008 primarily due to lower deferred gain amortization related to the sold retirement benefits and individual life insurance and annuity businesses.
For more information regarding the sale of these businesses see Note 8 of the Consolidated Financial Statements beginning on page 119 of this Form 10-K.
CIGNA CORPORATION – 2010 Form 10-K – 78
Corporate
Description
Corporate reflects amounts not allocated to other segments, such as net interest expense (defined as interest on corporate debt less net investment income on investments not supporting segment operations), interest on uncertain tax positions, certain litigation matters, intersegment eliminations, compensation cost for stock options and certain corporate overhead expenses such as directors’ expenses and, beginning in 2010, pension expense related to the Company’s frozen pension plans.
|
Financial Summary (In millions) |
2010 |
2009 |
2008 |
|
SEGMENT LOSS |
$(211) |
$(142) |
$(162) |
|
Less: special items (after-tax) included in segment loss: | |||
|
Resolution of Federal Tax Matter |
4 |
- |
- |
|
Loss on early extinguishment of debt |
(39) |
- |
- |
|
Charge related to litigation matter (See Note 24 to the Consolidated Financial Statements) |
- |
- |
(52) |
|
Completion of IRS examination (See Note 20 to the Consolidated Financial Statements) |
- |
12 |
- |
|
ADJUSTED LOSS FROM OPERATIONS |
$(176) |
$(154) |
$(110) |
Corporate’s adjusted loss from operations was higher in 2010, compared with 2009, primarily reflecting:
•
higher net interest expense, primarily driven by a higher long-term debt balance;
•
tax adjustments related to postretirement benefits and compensation resulting from health care reform; and
•
pension expense related to the Company’s frozen pension plans which was reported in Corporate beginning in 2010.
These unfavorable effects were partially offset by lower spending on strategic initiatives and lower directors’ deferred compensation expense.
Corporate’s adjusted loss from operations was higher in 2009, compared with 2008, primarily reflecting:
•
higher net interest expense attributable to lower average invested assets and increased debt used for general corporate purposes, including the repayment of some of the Company’s outstanding commercial paper issued to finance the acquisition of Great West Healthcare;
•
higher directors’ deferred compensation expenses caused by an increase in the Company’s stock price during 2009 compared with a decrease during 2008; and
•
spending on certain strategic initiatives.
CIGNA CORPORATION – 2010 Form 10-K – 79
Liquidity and Capital Resources
|
Financial Summary (In millions) |
2010 |
2009 |
2008 |
|
Short-term investments |
$174 |
$493 |
$236 |
|
Cash and cash equivalents |
$1,605 |
$924 |
$1,342 |
|
Short-term debt |
$552 |
$104 |
$301 |
|
Long-term debt |
$2,288 |
$2,436 |
$2,090 |
|
Shareholders’ equity |
$6,645 |
$5,417 |
$3,592 |
Liquidity
The Company maintains liquidity at two levels: the subsidiary level and the parent company level.
Liquidity requirements at the subsidiary level generally consist of:
•
claim and benefit payments to policyholders; and
•
operating expense requirements, primarily for employee compensation and benefits.
The Company’s subsidiaries normally meet their operating requirements by:
•
maintaining appropriate levels of cash, cash equivalents and short-term investments;
•
using cash flows from operating activities;
•
selling investments;
•
matching investment durations to those estimated for the related insurance and contractholder liabilities; and
•
borrowing from its parent company.
Liquidity requirements at the parent level generally consist of:
•
debt service and dividend payments to shareholders; and
•
pension plan funding.
The parent normally meets its liquidity requirements by:
•
maintaining appropriate levels of cash, cash equivalents and short-term investments;
•
collecting dividends from its subsidiaries;
•
using proceeds from issuance of debt and equity securities; and
•
borrowing from its subsidiaries.
Cash flows for the years ended December 31, were as follows:
|
(In millions) |
2010 |
2009 |
2008 |
|
Operating activities |
$1,743 |
$745 |
$1,656 |
|
Investing activities |
$(1,342) |
$(1,485) |
$(2,572) |
|
Financing activities |
$274 |
$307 |
$314 |
Cash flows from operating activities consist of cash receipts and disbursements for premiums and fees, mail order pharmacy and other revenues, gains (losses) recognized in connection with the Company’s GMDB equity hedge program, investment income, taxes, and benefits and expenses.
Because certain income and expense transactions do not generate cash, and because cash transactions related to revenue and expenses may occur in periods different from when those revenues and expenses are recognized in shareholders’ net income, cash flows from operating activities can be significantly different from shareholders’ net income.
CIGNA CORPORATION – 2010 Form 10-K – 80
Cash flows from investing activities generally consist of net investment purchases or sales and net purchases of property and equipment, which includes capitalized software, as well as cash used to acquire businesses.
Cash flows from financing activities are generally comprised of issuances and re-payment of debt at the parent level, proceeds on the issuance of common stock resulting from stock option exercises, and stock repurchases. In addition, the subsidiaries report net deposits/withdrawals to/from investment contract liabilities (which include universal life insurance liabilities) because such liabilities are considered financing activities with policyholders.
2010
Operating activities
For the year ended December 31, 2010, cash flows from operating activities were greater than net income by $394 million. Net income contains certain income and expense items which neither provide nor use operating cash flow, including:
•
GMIB fair value loss of $55 million;
•
a pre-tax loss on the transfer of the workers’ compensation and personal accident business of $31 million;
•
tax benefits related to resolution of a federal tax matter of $101 million;
•
depreciation and amortization charges of $292 million; and
•
realized investment gains of $75 million.
Cash flows from operating activities were greater than net income excluding the items noted above by $192 million. Excluding cash outflows of $157 million associated with the GMDB equity hedge program, (which did not affect shareholders’ net income) cash flows from operating activities were higher than net income by $349 million. This result primarily reflects premium growth in the Health Care segment’s risk businesses due to significant new business in 2010 and tax payments lower than expense due to favorable effects of benefit plans (primarily pension) and deferred foreign earnings, partially offset by pension contributions of $212 million.
Cash flows from operating activities increased by $998 million in 2010 compared with 2009. Excluding the results of the GMDB equity hedge program (which did not affect net income), cash flows from operating activities increased by $873 million. This increase in 2010 primarily reflects premium growth in the Health Care segment’s risk businesses as noted above and earnings growth in the Health Care, Disability and Life and International segments as well as lower contributions to the qualified domestic pension plan ($212 million in 2010, compared with $410 million in 2009). These favorable effects were partially offset by higher management compensation and income tax payments in 2010 compared with 2009.
Investing activities
Cash used in investing activities was $1.3 billion. This use of cash primarily consisted of net purchases of investments of $503 million, cash used to fund acquisitions (net of cash acquired) of $344 million, net cash used to transfer the run-off workers’ compensation and personal accident assumed reinsurance business via a reinsurance transaction of $190 million, and net purchases of property and equipment of $300 million.
Financing activities
Cash provided from financing activities primarily consisted of net proceeds from the issuance of long-term debt of $543 million, partially offset by debt repayments of $270 million primarily to retire a portion of the 8.5% Notes due 2019 and the 6.35% Notes due 2018 as a result of the tender offers to bondholders. See the Capital Resources section for more information. Financing activities also included net deposits to contractholder deposit funds of $90 million and proceeds on issuances of common stock of $64 million. These inflows were partially offset by common stock repurchases of $201 million.
CIGNA CORPORATION – 2010 Form 10-K – 81
2009
Operating activities
For the year ended December 31, 2009, cash flows from operating activities were less than net income by $560 million. Net income contains certain non-cash income and expense items, which neither provide nor use operating cash flow, including:
•
GMIB fair value gain of $304 million;
•
net pre-tax charges related to special items of $7 million;
•
tax benefits related to the IRS examination of $29 million;
•
depreciation and amortization charges of $268 million; and
•
realized investment losses of $43 million.
Cash flows from operating activities were lower than net income excluding the non-cash items noted above by $545 million. This decrease was primarily due to pre-tax cash outflows of $282 million associated with the GMDB equity hedge program which did not affect shareholders’ net income and pre-tax contributions to the domestic pension plans of approximately $410 million, partially offset by the favorable effect of the pension contributions on tax payments.
Cash flows from operating activities decreased by $911 million in 2009 compared with 2008. Excluding the results of the GMDB equity hedge program (which did not affect net income), cash flows from operating activities decreased by $296 million. This decrease in 2009 primarily reflects pre-tax contributions to the qualified domestic pension plan of approximately $410 million for 2009 compared with none for 2008, partially offset by the favorable effect of the pension contributions on tax payments.
Investing activities
Cash used in investing activities was $1.5 billion. This use of cash primarily consisted of net purchases of investments of $1.2 billion and net purchases of property and equipment of $307 million.
Financing activities
Cash provided from financing activities primarily consisted of net proceeds from the issuance of long-term debt of $346 million, partially offset by repayments of short-term debt, principally commercial paper, of $199 million. Financing activities also included net deposits to contractholder deposit funds of $89 million and proceeds on issuances of common stock of $30 million.
Interest Expense
Interest expense on long-term debt, short-term debt and capital leases was as follows:
|
(In millions) |
2010 |
2009 |
2008 |
|
Interest expense |
$182 |
$166 |
$146 |
The increase in interest expense in 2010 was primarily due to higher long-term debt (including current maturities) outstanding in 2010, resulting from the issuance of debt in May 2010 and May 2009 used for general corporate purposes.
The increase in interest expense in 2009 was primarily due to the issuance of debt used for general corporate purposes, including the repayment of some of the Company’s outstanding commercial paper issued to finance the Great-West Healthcare acquisition.
Capital Resources
The Company’s capital resources (primarily retained earnings and the proceeds from the issuance of debt and equity securities) provide protection for policyholders, furnish the financial strength to underwrite insurance risks and facilitate continued business growth.
Management, guided by regulatory requirements and rating agency capital guidelines, determines the amount of capital resources that the Company maintains. Management allocates resources to new long-term business commitments when returns, considering the risks, look promising and when the resources available to support existing business are adequate.
CIGNA CORPORATION – 2010 Form 10-K – 82
The Company prioritizes its use of capital resources to:
•
provide capital necessary to support growth and maintain or improve the financial strength ratings of subsidiaries;
•
consider acquisitions that are strategically and economically advantageous; and
•
return capital to investors through share repurchase.
The availability of capital resources will be impacted by equity and credit market conditions. Extreme volatility in credit or equity market conditions may reduce the Company’s ability to issue debt or equity securities.
Sources of Capital
On December 8, 2010, the Company issued $250 million of 4.375% Notes ($249 net of debt discount, with an effective interest rate of 5.1%). The difference between the stated and effective interest rates primarily reflects the effect of treasury locks. See Note 13 to the Consolidated Financial Statements for further information. Interest is payable on June 15 and December 15 of each year beginning December 15, 2010. These Notes will mature on December 15, 2020. The proceeds of this debt were used to fund the tender offer for the Company’s 8.5% Senior Notes due 2019 and the 6.35% Senior Notes due 2018 (described further below under uses of capital).
On May 12, 2010, the Company issued $300 million of 5.125% Notes ($299 million, net of debt discount, with an effective interest rate of 5.36% per year). Interest is payable on June 15 and December 15 of each year beginning December 15, 2010. These Notes will mature on June 15, 2020. The proceeds of this debt were used for general corporate purposes.
On May 4, 2009, the Company issued $350 million of 8.5% Notes ($349 million, net of debt discount, with an effective interest rate of 9.90% per year). The difference between the stated and effective interest rates primarily reflects the effect of treasury locks. See Note 13 to the Consolidated Financial Statements for further information. Interest is payable on May 1 and November 1 of each year beginning November 1, 2009. The proceeds of this debt were used for general corporate purposes, including the repayment of some of the Company’s outstanding commercial paper. These Notes will mature on May 1, 2019. As explained further under Uses of Capital below, the Company repurchased a portion of these Notes under a tender offer dated December 1, 2010.
On March 4, 2008, the Company issued $300 million of 6.35% Notes (with an effective interest rate of 6.68% per year). The difference between the stated and effective interest rates primarily reflects the effect of treasury locks. Interest is payable on March 15 and September 15 of each year beginning September 15, 2008. The proceeds of this debt were used for general corporate purposes, including financing the acquisition of Great-West Healthcare. These Notes will mature on March 15, 2018. As explained further under Uses of Capital below, the Company repurchased a portion of these Notes under a tender offer dated December 9, 2010.
The Company may redeem these Notes, at any time, in whole or in part, at a redemption price equal to the greater of:
•
100% of the principal amount of the Notes to be redeemed; or
•
the present value of the remaining principal and interest payments on the Notes being redeemed discounted at the applicable Treasury Rate plus 25 basis points for the 4.375% and 5.125% Notes due 2020, 50 basis points for the 8.5% Notes due 2019, or 40 basis points for the 6.35% Notes due 2018.
On March 14, 2008, the Company entered into a commercial paper program (“the Program”). Under the Program, the Company is authorized to sell short-term unsecured commercial paper notes from time to time up to a maximum of $500 million. The proceeds are used for general corporate purposes, including working capital, capital expenditures, acquisitions and share repurchases. The Company uses the credit facility described below as back-up liquidity to support the outstanding commercial paper. If at any time funds are not available on favorable terms under the Program, the Company may use the Credit Agreement (see below) for funding. In October 2008, the Company added an additional dealer to its Program. As of December 31, 2010, the Company had $100 million in commercial paper outstanding, at a weighted average interest rate of 0.38% and remaining maturities ranging from 11 to 35 days.
In June 2007, the Company amended and restated its five-year committed revolving credit and letter of credit agreement for $1.75 billion, which permits up to $1.25 billion to be used for letters of credit. This agreement is diversified among 22 banks, with three banks each having 11% of the commitment and the other 19 banks having the remaining 67% of the commitment. The credit agreement includes options, which are subject to consent by the administrative agent and the committing banks, to increase the commitment amount up to $2.0 billion and to extend the term of the agreement. The Company entered into the agreement for general corporate purposes, including support for the issuance of commercial paper and to obtain statutory reserve credit for certain reinsurance arrangements. There were letters of credit in the amount of $82 million issued as of December 31, 2010.
CIGNA CORPORATION – 2010 Form 10-K – 83
Uses of Capital
Pension funding
The Company contributed $212 million to the domestic qualified pension plans, of which $69 million was required and $143 million was voluntary.
Acquisition of Vanbreda International
In 2010, the Company acquired Vanbreda International for $412 million. The acquisition was funded from available cash. See Note 3 for further information.
Repayments of long-term debt
On December 1, 2010 the Company offered to settle its 8.5% Notes due 2019, including accrued interest from November 1 through the settlement date. The tender price equaled the present value of the remaining principal and interest payments on the Notes being redeemed, discounted at a rate equal to the 10 year treasury rate plus a fixed spread of 100 basis points. The tender offer priced at a yield of 4.128% and principal of $99 million was tendered, with $251 million remaining outstanding. The Company paid $130 million, including accrued interest and expenses, to settle the Notes, resulting in an after-tax loss on early debt extinguishment of $21 million.
On December 9, 2010 the Company offered to settle its 6.35% Notes due 2018, including accrued interest from September 16 through the settlement date. The tender price equaled the present value of the remaining principal and interest payments on the Notes being redeemed, discounted at a rate equal to the 10 year treasury rate plus a fixed spread of 45 basis points. The tender offer priced at a yield of 3.923% and principal of $169 million was tendered, with $131 million remaining outstanding. The Company paid $198 million, including accrued interest and expenses, to settle the Notes, resulting in an after-tax loss on early debt extinguishment of $18 million.
Share Repurchase
The Company maintains a share repurchase program, which was authorized by its Board of Directors. The decision to repurchase shares depends on market conditions and alternate uses of capital. The Company has, and may continue from time to time, to repurchase shares on the open market through a Rule 10b5-1 plan which permits a company to repurchase its shares at times when it otherwise might be precluded from doing so under insider trading laws or because of self-imposed trading blackout periods. The Company suspends activity under this program from time to time and also removes such suspensions, generally without public announcement.
The Company repurchased 6.2 million shares for $201 million during 2010, and an additional 1.8 million shares for $73 million through February 25, 2011. On February 23, 2011, the Board of Directors increased share repurchase authority by $500 million. The total remaining share repurchase authorization as of February 25, 2011 was $674 million.
The Company did not repurchase any shares during 2009 and repurchased 10.0 million shares for $378 million in 2008.
Liquidity and Capital Resources Outlook
At December 31, 2010, there was approximately $810 million in cash available at the parent company level. In 2011, the parent company’s cash obligations are expected to consist of the following:
•
scheduled interest payments of $167 million on outstanding short-term and long-term debt of $2.8 billion at December 31, 2010;
•
scheduled maturities of long-term debt of $448 million;
•
contributions to the domestic qualified pension plan of $250 million, of which approximately 50% are expected to be required; and
•
approximately $100 million of commercial paper that will mature over the next three months. The Company expects to either repay the commercial paper or refinance it either by issuing long-term debt or re-issuing commercial paper.
The Company expects, based on cash on hand, current projections for dividends from the Company’s subsidiaries, as well as its ability to issue debt or equity securities in the capital markets to have sufficient liquidity to meet its obligations.
CIGNA CORPORATION – 2010 Form 10-K – 84
However, the Company’s cash projections may not be realized and the demand for funds could exceed available cash if:
•
ongoing businesses experience unexpected shortfalls in earnings;
•
regulatory restrictions or rating agency capital guidelines reduce the amount of dividends available to be distributed to the parent company from the insurance and HMO subsidiaries (including the impact of equity market deterioration and volatility on subsidiary capital);
•
significant disruption or volatility in the capital and credit markets reduces the Company’s ability to raise capital or creates unexpected losses related to the GMDB and GMIB businesses;
•
a substantial increase in funding over current projections is required for the Company’s pension plan; or
•
a substantial increase in funding is required for the Company’s GMDB and GMIB equity and interest rate hedge programs.
In those cases, the Company expects to have the flexibility to satisfy liquidity needs through a variety of measures, including intercompany borrowings and sales of liquid investments. The parent company may borrow up to $600 million from CGLIC without prior state approval. In addition, the Company may use short-term borrowings, such as the commercial paper program and the committed line of credit agreement of up to $1.7 billion subject to the maximum debt leverage covenant in its line of credit agreement. As of December 31, 2010, the Company had $1.7 billion of borrowing capacity within the maximum debt leverage covenant in the line of credit agreement in addition to the $2.8 billion of debt outstanding.
Though the Company believes it has adequate sources of liquidity, significant disruption or volatility in the capital and credit markets could affect the Company’s ability to access those markets for additional borrowings or increase costs associated with borrowing funds.
Solvency regulation
Many states have adopted some form of the National Association of Insurance Commissioners (“NAIC”) model solvency-related laws and risk-based capital rules (“RBC rules”) for life and health insurance companies. The RBC rules recommend a minimum level of capital depending on the types and quality of investments held, the types of business written and the types of liabilities incurred. If the ratio of the insurer’s adjusted surplus to its risk-based capital falls below statutory required minimums, the insurer could be subject to regulatory actions ranging from increased scrutiny to conservatorship.
In addition, various non-U.S. jurisdictions prescribe minimum surplus requirements that are based upon solvency, liquidity and reserve coverage measures. During 2010, the Company’s HMOs and life and health insurance subsidiaries, as well as non-U.S. insurance subsidiaries, were compliant with applicable RBC and non-U.S. surplus rules.
Effective December 31, 2009 the Company’s principal life insurance subsidiary, CGLIC, implemented the NAIC’s Actuarial Guideline XLIII (also known as AG 43 or VACARVM), which is applicable to CGLIC’s statutory reserves for GMDB and GMIB contracts totaling $1.5 billion as of December 31, 2010. As provided under this guidance, CGLIC received approval from the State of Connecticut to grade-in the full effect of the guideline over a 3-year period beginning in 2009. At December 31, 2010, statutory reserves for CGLIC were higher than the pre-AG 43 reserves by $123 million. If the guidance had been fully implemented at December 31, 2010, statutory reserves would have been higher by an additional $62 million. Management does not anticipate that VACARVM will have a material impact on the amount of dividends expected to be paid by CGLIC to the parent company in 2011. In addition, VACARVM has no impact on measurement of the Company’s results of operations or financial condition as determined under GAAP.
Unfunded Pension Plan Liability
As of December 31, 2010, the unfunded pension liability was $1.5 billion, substantially unchanged from December 31, 2009, reflecting a decline in the discount rate of approximately 50 basis points as well as an update to mortality assumptions during 2010 to better reflect recent experience, entirely offset by contributions of $212 million during 2010 and favorable investment asset performance in 2010. Although the GAAP funded status did not decline as a result of the contributions made in 2010, required pension contributions in 2011 under the Pension Protection Act of 2006 are not expected to significantly change from previous estimates, since discount rates used for funding purposes are based on a 24-month moving average which is less susceptible to volatility than the rate required to be used to compute the liability for the financial statements.
CIGNA CORPORATION – 2010 Form 10-K – 85
Guarantees and Contractual Obligations
The Company is contingently liable for various contractual obligations entered into in the ordinary course of business. The maturities of the Company’s primary contractual cash obligations, as of December 31, 2010, are estimated to be as follows:
|
(In millions, on an undiscounted basis) |
Total |
Less than 1 year |
1-3 years |
4-5 years |
After 5 years |
|
On-Balance Sheet: | |||||
|
Insurance liabilities: | |||||
|
Contractholder deposit funds |
$7,293 |
$677 |
$875 |
$769 |
$4,972 |
|
Future policy benefits |
11,182 |
459 |
846 |
891 |
8,986 |
|
Health Care medical claims payable |
1,246 |
1,213 |
22 |
2 |
9 |
|
Unpaid claims and claims expenses |
4,445 |
1,374 |
847 |
583 |
1,641 |
|
Short-term debt |
574 |
574 |
- |
- |
- |
|
Long-term debt |
4,390 |
146 |
299 |
313 |
3,632 |
|
Other long-term liabilities |
1,274 |
556 |
220 |
132 |
366 |
|
Off-Balance Sheet: | |||||
|
Purchase obligations |
1,284 |
578 |
446 |
173 |
87 |
|
Operating leases |
496 |
105 |
163 |
104 |
124 |
|
TOTAL |
$32,184 |
$5,682 |
$3,718 |
$2,967 |
$19,817 |
On-Balance Sheet
•
Insurance liabilities. Contractual cash obligations for insurance liabilities, excluding unearned premiums and fees, represent estimated net benefit payments for health, life and disability insurance policies and annuity contracts. Recorded contractholder deposit funds reflect current fund balances primarily from universal life customers. Contractual cash obligations for these universal life contracts are estimated by projecting future payments using assumptions for lapse, withdrawal and mortality. These projected future payments include estimated future interest crediting on current fund balances based on current investment yields less the estimated cost of insurance charges and mortality and administrative fees. Actual obligations in any single year will vary based on actual morbidity, mortality, lapse, withdrawal, investment and premium experience. The sum of the obligations presented above exceeds the corresponding insurance and contractholder liabilities of $16 billion recorded on the balance sheet because the recorded insurance liabilities reflect discounting for interest and the recorded contractholder liabilities exclude future interest crediting, charges and fees. The Company manages its investment portfolios to generate cash flows needed to satisfy contractual obligations. Any shortfall from expected investment yields could result in increases to recorded reserves and adversely impact results of operations. The amounts associated with the sold retirement benefits and individual life insurance and annuity businesses, as well as the reinsured workers’ compensation and personal accident businesses are excluded from the table above as net cash flows associated with them are not expected to impact the Company. The total amount of these reinsured reserves excluded is approximately $6 billion.
•
Short-term debt represents commercial paper, current maturities of long-term debt, and current obligations under capital leases.
•
Long-term debt includes scheduled interest payments. Capital leases are included in long-term debt and represent obligations for software licenses.
•
Other long-term liabilities. These items are presented in accounts payable, accrued expenses and other liabilities in the Company’s Consolidated Balance Sheets. This table includes estimated payments for GMIB contracts, pension and other postretirement and postemployment benefit obligations, supplemental and deferred compensation plans, interest rate and foreign currency swap contracts, and certain tax and reinsurance liabilities.
Estimated payments of $113 million for deferred compensation, non-qualified and International pension plans and other postretirement and postemployment benefit plans are expected to be paid in less than one year. The Company’s best estimate is that contributions to the qualified domestic pension plan during 2011 will be approximately $250 million. The Company expects to make payments subsequent to 2011 for these obligations, however subsequent payments have been excluded from the table as their timing is based on plan assumptions which may materially differ from actual activities (see Note 10 to the Consolidated Financial Statements for further information on pension and other postretirement benefit obligations).
CIGNA CORPORATION – 2010 Form 10-K – 86
The above table also does not contain $177 million of gross liabilities for uncertain tax positions because the Company cannot reasonably estimate the timing of their resolution with the respective taxing authorities. See Note 20 to the Consolidated Financial Statements for the year ended December 31, 2010 for further information.
Off-Balance Sheet
•
Purchase obligations. As of December 31, 2010, purchase obligations consisted of estimated payments required under contractual arrangements for future services and investment commitments as follows:
|
(In millions) | |
|
Fixed maturities |
$14 |
|
Commercial mortgage loans |
63 |
|
Real estate |
11 |
|
Limited liability entities (other long-term investments) |
521 |
|
Total investment commitments |
609 |
|
Future service commitments |
675 |
|
TOTAL PURCHASE OBLIGATIONS |
$1,284 |
The Company had commitments to invest in limited liability entities that hold real estate, loans to real estate entities or securities. See Note 12(D) to the Consolidated Financial Statements for additional information.
Future service commitments include an agreement with IBM for various information technology (IT) infrastructure services. The Company’s remaining commitment under this contract is approximately $268 million over the next 3 years. The Company has the ability to terminate this agreement with 90 days notice, subject to termination fees.
The Company’s remaining estimated future service commitments primarily represent contracts for certain outsourced business processes and IT maintenance and support. The Company generally has the ability to terminate these agreements, but does not anticipate doing so at this time. Purchase obligations exclude contracts that are cancelable without penalty and those that do not specify minimum levels of goods or services to be purchased.
•
Operating leases. For additional information, see Note 22 to the Consolidated Financial Statements.
Guarantees
The Company, through its subsidiaries, is contingently liable for various financial and other guarantees provided in the ordinary course of business. See Note 24 to the Consolidated Financial Statements for additional information on guarantees.
CIGNA CORPORATION – 2010 Form 10-K – 87
Investment Assets
The Company’s investment assets do not include separate account assets. Additional information regarding the Company’s investment assets and related accounting policies is included in Notes 2, 11, 12, 13, 14, 15 and 18 to the Consolidated Financial Statements.
Fixed Maturities
Investments in fixed maturities include publicly-traded and privately placed debt securities, mortgage and other asset-backed securities, preferred stocks redeemable by the investor, hybrid and trading securities. Fair values are based on quoted market prices when available. When market prices are not available, fair value is generally estimated using discounted cash flow analyses, incorporating current market inputs for similar financial instruments with comparable terms and credit quality. In instances where there is little or no market activity for the same or similar instruments, the Company estimates fair value using methods, models and assumptions that the Company believes a hypothetical market participant would use to determine a current transaction price.
The Company performs ongoing analyses of prices used to value the Company’s invested assets to determine that they represent appropriate estimates of fair value. This process involves quantitative and qualitative analysis including reviews of pricing methodologies, judgments of valuation inputs, the significance of any unobservable inputs, pricing statistics and trends. The Company also performs sample testing of sales values to confirm the accuracy of prior fair value estimates.
The Company’s fixed maturity portfolio continues to be diversified by issuer and industry type, with no single industry constituting more than 10% of total invested assets as of December 31, 2010.
|
(In millions) |
2010 |
2009 |
|
Federal government and agency |
$687 |
$571 |
|
State and local government |
2,467 |
2,521 |
|
Foreign government |
1,169 |
1,070 |
|
Corporate |
9,632 |
8,585 |
|
Federal agency mortgage-backed |
10 |
34 |
|
Other mortgage-backed |
88 |
121 |
|
Other asset-backed |
656 |
541 |
|
TOTAL |
$14,709 |
$13,443 |
As of December 31, 2010, $13.5 billion, or 92%, of the fixed maturities in the Company’s investment portfolio were investment grade (Baa and above, or equivalent), and the remaining $1.2 billion were below investment grade. The majority of the bonds that are below investment grade are rated at the higher end of the non-investment grade spectrum. These quality characteristics have not materially changed during the year.
The net appreciation of the Company’s fixed maturity portfolio increased nearly $400 million during 2010, driven by a decline in market yields. Although asset values are well in excess of amortized cost, there are specific securities with amortized cost in excess of fair value by approximately $80 million as of December 31, 2010.
Corporate fixed maturities includes private placement investments of $4.7 billion, which are generally less marketable than publicly-traded bonds, but yields on these investments tend to be higher than yields on publicly-traded bonds with comparable credit risk. The Company performs a credit analysis of each issuer, diversifies investments by industry and issuer and requires financial and other covenants that allow the Company to monitor issuers for deteriorating financial strength and pursue remedial actions, if warranted.
The Company’s investment in state and local government securities is diversified by issuer and geography with no single exposure greater than $30 million. The Company focuses on the underlying issuer’s credit quality with 94% rated A3 or better excluding guarantees by monoline bond insurers, consistent with the prior year. As of December 31, 2010, 63%, or $1,542 million, of the Company’s total investments in state and local government securities were guaranteed by monoline bond insurers, providing additional credit quality support. The quality ratings of these investments with and without this guaranteed support as of December 31, 2010 were as follows:
CIGNA CORPORATION – 2010 Form 10-K – 88
|
(In millions) |
Quality Rating |
As of December 31, 2010 |
|
|
Fair Value |
|||
|
With Guarantee |
Without Guarantee |
||
|
State and local governments |
Aaa |
$79 |
$78 |
|
Aa1-Aa3 |
1,172 |
1,092 |
|
|
A1-A3 |
232 |
278 |
|
|
Baa1-Baa3 |
59 |
42 |
|
|
Not available |
- |
52 |
|
|
TOTAL STATE AND LOCAL GOVERNMENTS |
|
$1,542 |
$1,542 |
The Company invests in high quality foreign government obligations, with an average quality rating of AA as of December 31, 2010. The diversification of these investments was consistent with the geographic distribution of the international business operations.
As of December 31, 2010, the Company’s investments in other asset and mortgage-backed securities totaling $754 million included $477 million of investment grade private placement securities guaranteed by monoline bond insurers. Quality ratings without considering the guarantees for these other asset-backed securities were not available.
As of December 31, 2010, the Company had no direct investments in monoline bond insurers. Guarantees provided by various monoline bond insurers for certain of the Company’s investments in state and local governments and other asset-backed securities as of December 31, 2010 were:
|
Guarantor (In millions) |
As of December 31, 2010 |
|
Indirect Exposure |
|
|
National Public Finance Guarantee (formerly MBIA, Inc.) |
$1,217 |
|
Assured Guaranty Municipal Corp (formerly Financial Security Assurance) |
589 |
|
AMBAC |
176 |
|
Financial Guaranty Insurance Co. |
37 |
|
TOTAL |
$2,019 |
AMBAC filed for bankruptcy during the fourth quarter of 2010. However, the Company does not expect this action to materially impact valuations of guaranteed securities given the high quality of underlying issuer credit without this guaranteed support.
Commercial Mortgage Loans
The Company’s commercial mortgage loans are fixed rate loans, diversified by property type, location and borrower to reduce exposure to potential losses. Loans are secured by high quality commercial property and are generally made at less than 75% of the property’s value at origination of the loan. In addition to property value, debt service coverage, which is the ratio of the estimated cash flows from the property to the required loan payments (principal and interest), is an important underwriting consideration. The Company holds no direct residential mortgage loans and does not securitize or service mortgage loans.
The Company completed its annual in depth review of its commercial mortgage loan portfolio in July, 2010. This review included an analysis of each property’s most recent annual financial statements, rent rolls and operating plans and budgets for 2010, a physical inspection of the property and other pertinent factors. Based on property values and cash flows estimated as part of this review, along with updates for portfolio activity subsequent to the review, the portfolio’s average loan-to-value ratio improved to 74% as of December 31, 2010 from 77% as of December 31, 2009. The portfolio’s debt service coverage was estimated to be 1.38 as of December 31, 2010, down from 1.48 as of December 31, 2009.
Values estimated for the properties in CIGNA’s mortgage portfolio reflect improving commercial real estate capital markets, with stabilizing, and in some instances, increasing values, for well leased, quality commercial real estate located in strong institutional markets, the quality reflected by the vast majority of properties securing the mortgages. The deterioration in property cash flows (and resulting debt service coverage levels) estimated as part of the review reflects generally weak fundamentals (higher vacancy and reduced rental rates) across property types and markets. While commercial real estate capital markets improved during 2010 and there are some signs of improvement in fundamentals, a sustained recovery will be dependent on continued improvement in local markets and the broader national economy.
CIGNA CORPORATION – 2010 Form 10-K – 89
The following table reflects the commercial mortgage loan portfolio as of December 31, 2010 summarized by loan-to-value ratio based on the annual loan review completed in July, 2010.
LOAN-TO-VALUE DISTRIBUTION
|
Loan-to-Value Ratios |
Amortized Cost |
% of Mortgage Loans |
||
|
Senior |
Subordinated |
Total |
||
|
Below 50% |
$195 |
$157 |
$352 |
10% |
|
50% to 59% |
486 |
33 |
519 |
15% |
|
60% to 69% |
600 |
64 |
664 |
19% |
|
70% to 79% |
310 |
30 |
340 |
10% |
|
80% to 89% |
805 |
33 |
838 |
24% |
|
90% to 99% |
544 |
27 |
571 |
16% |
|
100% or above |
202 |
- |
202 |
6% |
|
TOTALS |
$3,142 |
$344 |
$3,486 |
100% |
As summarized above, $344 million or 10% of the commercial mortgage loan portfolio is comprised of subordinated notes and loans, including $310 million of loans secured by first mortgages, which were fully underwritten and originated by the Company using its standard underwriting procedures. Senior interests in these first mortgage loans were then sold to other institutional investors. This strategy allowed the Company to effectively utilize its origination capabilities to underwrite high quality loans with strong borrower sponsorship, limit individual loan exposures, and achieve attractive risk adjusted yields. In the event of a default, the Company would pursue remedies up to and including foreclosure jointly with the holders of the senior interests, but would receive repayment only after satisfaction of the senior interest.
There are seven loans where the aggregate carrying value of the mortgage loans exceeds the value of the underlying properties by $17 million. Five of these loans have current debt service coverage of 1.0 or greater and two with debt service coverage below 1.0 have other risk mitigating factors including strong borrower sponsorship. As of December 31, 2010, the mortgage portfolio contains approximately 170 loans and all but four of these loans (totaling $86 million and considered problem commercial mortgage loans) continue to perform under their contractual terms, resulting in an aggregate default rate of 2.5%. The Company has $518 million of loans maturing in the next twelve months. Given the quality and diversity of the underlying real estate, positive debt service coverage and significant borrower cash investment averaging nearly 30%, the Company remains confident that the vast majority of borrowers will continue to perform as required. While considered unlikely, if property values were to decrease 10% from those levels estimated during the annual in-depth loan review, this would cause approximately 18% of the portfolio’s carrying values to exceed the fair values of their underlying properties, totaling $80 million.
Other Long-term Investments
The Company’s other long-term investments include $682 million in securities partnership and real estate funds as well as direct investments in real estate joint ventures. The funds typically invest in mezzanine debt or equity of privately held companies (securities partnerships) and equity real estate. Because these investments have a subordinate position in the capital structure, the Company assumes a higher level of risk for higher expected returns. Although the total fair values of these investments exceeded their carrying values as of December 31, 2010, the fair value of the Company’s ownership interest in certain funds (those carried at cost) was less than its carrying value by $50 million. During 2010 these investment values improved, but remained at depressed levels reflecting the impact of declines in value experienced predominantly during 2008 and 2009 due to economic weakness and disruption in the capital markets, particularly in the commercial real estate market. The Company believes these declines in value are temporary and expects to recover its carrying value over the remaining lives of the funds. To mitigate risk, these investments are diversified across approximately 65 separate partnerships, and approximately 40 general partners who manage one or more of these partnerships. Also, the funds’ underlying investments are diversified by industry sector or property type, and geographic region. No single investment exceeds 6% of the Company’s securities and real estate partnership portfolio. Given the current economic environment, future impairments are possible; however, management does not expect those losses to have a material effect on the Company’s results of operations, financial condition or liquidity.
CIGNA CORPORATION – 2010 Form 10-K – 90
Problem and Potential Problem Investments
“Problem” bonds and commercial mortgage loans are either delinquent by 60 days or more or have been restructured as to terms, which could include concessions by the Company for modification of interest rate, principal payment or maturity date. “Potential problem” bonds and commercial mortgage loans are considered current (no payment more than 59 days past due), but management believes they have certain characteristics that increase the likelihood that they may become problems. The characteristics management considers include, but are not limited to, the following:
•
request from the borrower for restructuring;
•
principal or interest payments past due by more than 30 but fewer than 60 days;
•
downgrade in credit rating;
•
collateral losses on asset-backed securities; and
•
for commercial mortgages, deterioration of debt service coverage below 1.0 or value declines resulting in estimated loan-to-value ratios increasing to 100% or more.
The Company recognizes interest income on problem bonds and commercial mortgage loans only when payment is actually received because of the risk profile of the underlying investment. The amount that would have been reflected in net income if interest on non-accrual investments had been recognized in accordance with the original terms was not significant for 2010 or 2009.
The following table shows problem and potential problem investments at amortized cost, net of valuation reserves and write-downs:
|
(In millions) |
December 31, 2010 |
December 31, 2009 |
||||
|
Gross |
Reserve |
Net |
Gross |
Reserve |
Net |
|
|
Problem bonds |
$86 |
$(39) |
$47 |
$103 |
$(49) |
$54 |
|
Problem commercial mortgage loans |
90 |
(4) |
86 |
169 |
(11) |
158 |
|
Foreclosed real estate |
59 |
- |
59 |
59 |
- |
59 |
|
TOTAL PROBLEM INVESTMENTS |
$235 |
$(43) |
$192 |
$331 |
$(60) |
$271 |
|
Potential problem bonds |
$40 |
$(10) |
$30 |
$94 |
$(10) |
$84 |
|
Potential problem commercial mortgage loans |
305 |
(8) |
297 |
245 |
(6) |
239 |
|
TOTAL POTENTIAL PROBLEM INVESTMENTS |
$345 |
$(18) |
$327 |
$339 |
$(16) |
$323 |
Net problem investments represent 1.0% of total investments excluding policy loans. The Company actively managed its problem asset exposure during 2010. Net problem investments decreased $79 million during 2010 reflecting:
•
$98 million reduction from the foreclosure and subsequent sale or partial sale of three assets. These partial sales represented assets transferred to joint ventures and recapitalized with contributions of new equity from third-party investors, resulting in the reclassification of the retained ownership interests in these assets from foreclosed real estate to other long-term investments;
•
$7 million reduction to problem bonds due to redemption activity; and
•
$26 million of additions related to two new problem mortgage loans.
Additionally, two mortgage loans totaling $53 million were identified as problem loans in 2010 and subsequently disposed of through a direct sale and a partial sale subsequent to foreclosure.
Realized investment gains and losses from the disposal of problem assets were not material to the Company’s results of operations.
CIGNA CORPORATION – 2010 Form 10-K – 91
Net potential problem investments represent 1.7% of total investments excluding policy loans. Net potential problem investments increased $4 million during 2010 reflecting:
•
$188 million increase due to the addition of eight commercial mortgage loans, five of which were identified as a result of management’s in-depth portfolio loan review completed in July 2010. These loans were exhibiting signs of distress such as an elevated loan-to-value ratio or a low or negative debt service coverage. Seven of the loans continue to perform according to their original contractual terms as of December 31, 2010, while one of the loans was reclassified to problem status;
•
$96 million reduction for commercial mortgage loans that were sold, foreclosed, reclassified to problem commercial mortgage loans or paid down;
•
$34 million reduction for commercial mortgage loans that were reclassified to loans in good standing; and
•
$54 million decline in potential problem bonds due to improved bond performance as well as redemption activity.
Commercial mortgage loans are considered impaired when it is probable that the Company will not collect amounts due according to the terms of the original loan agreement. Problem and potential problem commercial mortgage loans totaling $95 million (net of valuation reserves), presented in the above table, are considered impaired. During 2010, the Company recorded a $24 million pre-tax ($15 million after-tax) charge to increase valuation reserves on impaired commercial mortgage loans. See Note 12 to the Consolidated Financial Statements and the Critical Accounting Estimates section of the MD&A beginning on page 57 of this Form 10-K for additional information regarding impaired commercial mortgage loans.
Summary
The Company recorded after-tax realized investment losses for investment asset write-downs and changes in valuation reserves as follows:
|
(In millions) |
2010 |
2009 |
|
Credit-related (1) |
$24 |
$61 |
|
Other (2) |
1 |
8 |
|
TOTAL (3) |
$25 |
$69 |
|
(1) Credit-related losses include other-than-temporary declines in value of fixed maturities and equity securities, and impairments of commercial mortgage loans and real estate entities. The amount related to credit losses on fixed maturities for which a portion of the impairment was recognized in other comprehensive income was not significant. (2) Prior to adoption of new GAAP guidance for other-than-temporary impairments on April 1, 2009, Other primarily represented the impact of rising market yields on investments where the Company could not demonstrate the intent and ability to hold until recovery. (3) Other-than-temporary impairments on fixed maturities in 2010 were not significant. Other-than-temporary impairments on fixed maturities in 2009 were $31 million and are included in both the credit-related and other categories above. |
||
The financial credit markets improved during 2010, with appreciation in asset values reflecting lower market yields. In the current economic environment, risks in the Company’s investment portfolio, while declining, remain elevated. Continued economic weakness for an extended period could cause default rates to increase and recoveries to decline resulting in additional impairment losses for the Company. Future realized and unrealized investment results will be impacted largely by future market conditions that are not reasonably predictable. Management believes that the vast majority of the Company’s fixed maturity investments will continue to perform under their contractual terms, and that declines in their fair values below carrying value are temporary. Based on the strategy to match the duration of invested assets to the duration of insurance and contractholder liabilities, the Company expects to hold a significant portion of these assets for the long term. While future credit-related losses could have a material adverse impact on results of operations, such losses are not expected to have a material adverse effect on the Company’s financial condition or liquidity.
While management believes the commercial mortgage loan portfolio is positioned to perform well due to its solid aggregate loan-to-value ratio (including minimal loans with carrying values exceeding the fair value of collateral) and strong debt service coverage, the commercial real estate market continues to exhibit significant signs of distress and if these conditions remain for an extended period or worsen substantially, it could result in an increase in problem and potential problem loans. Given the current economic environment, future impairments could have a material adverse effect on results of operations; however, management does not expect those losses to have a material adverse effect on the Company’s financial condition or liquidity.
CIGNA CORPORATION – 2010 Form 10-K – 92
Market Risk
Financial Instruments
The Company’s assets and liabilities include financial instruments subject to the risk of potential losses from adverse changes in market rates and prices. The Company’s primary market risk exposures are:
•
Interest-rate risk on fixed-rate, domestic, medium-term instruments. Changes in market interest rates affect the value of instruments that promise a fixed return and impact the value of liabilities for reinsured GMDB and GMIB contracts.
•
Foreign currency exchange rate risk of the U.S. dollar primarily to the South Korean won, euro, Taiwan dollar, British pound, New Zealand dollar, and Hong Kong dollar. An unfavorable change in exchange rates reduces the carrying value of net assets denominated in foreign currencies.
•
Equity price risk for domestic equity securities and for the value of reinsured GMDB and GMIB contracts resulting from unfavorable changes in variable annuity account values based on underlying mutual fund investments.
For further discussion of reinsured contracts, see Note 7 for GMDB contracts and Note 11 for GMIB contracts in the Consolidated Financial Statements.
The Company’s Management of Market Risks
The Company predominantly relies on three techniques to manage its exposure to market risk:
•
Investment/liability matching. The Company generally selects investment assets with characteristics (such as duration, yield, currency and liquidity) that correspond to the underlying characteristics of its related insurance and contractholder liabilities so that the Company can match the investments to its obligations. Shorter-term investments support generally shorter-term life and health liabilities. Medium-term, fixed-rate investments support interest-sensitive and health liabilities. Longer-term investments generally support products with longer pay out periods such as annuities and long-term disability liabilities.
•
Use of local currencies for foreign operations. The Company generally conducts its international business through foreign operating entities that maintain assets and liabilities in local currencies. While this technique does not reduce the Company’s foreign currency exposure of its net assets, it substantially limits exchange rate risk to those net assets.
•
Use of derivatives. The Company generally uses derivative financial instruments to minimize certain market risks.
See Notes 2(C) and 13 to the Consolidated Financial Statements for additional information about financial instruments, including derivative financial instruments.
Effect of Market Fluctuations on the Company
The examples that follow illustrate the effect of hypothetical changes in market rates or prices on the fair value of certain financial instruments including:
•
hypothetical changes in market interest rates, primarily for fixed maturities and commercial mortgage loans, partially offset by liabilities for long-term debt and GMIB contracts;
•
hypothetical changes in market rates for foreign currencies, primarily for the net assets of foreign subsidiaries denominated in a foreign currency; and
•
hypothetical changes in market prices for equity exposures, primarily for equity securities and GMIB contracts.
In addition, hypothetical effects of changes in equity indices and foreign exchange rates are presented separately for futures contracts used in the GMDB equity hedge program.
CIGNA CORPORATION – 2010 Form 10-K – 93
Management believes that actual results could differ materially from these examples because:
•
these examples were developed using estimates and assumptions;
•
changes in the fair values of all insurance-related assets and liabilities have been excluded because their primary risks are insurance rather than market risk;
•
changes in the fair values of investments recorded using the equity method of accounting and liabilities for pension and other postretirement and postemployment benefit plans (and related assets) have been excluded, consistent with the disclosure guidance; and
•
changes in the fair values of other significant assets and liabilities such as goodwill, deferred policy acquisition costs, taxes, and various accrued liabilities have been excluded; because they are not financial instruments, their primary risks are other than market risk.
The effects of hypothetical changes in market rates or prices on the fair values of certain of the Company’s financial instruments, subject to the exclusions noted above (particularly insurance liabilities), would have been as follows as of December 31:
|
Market scenario for certain non-insurance financial instruments (in millions) |
Loss in fair value |
|
|
2010 |
2009 |
|
|
100 basis point increase in interest rates |
$700 |
$700 |
|
10% strengthening in U.S. dollar to foreign currencies |
$190 |
$160 |
|
10% decrease in market prices for equity exposures |
$50 |
$50 |
The Company’s foreign operations hold investment assets, such as fixed maturities, that are generally invested in the currency of the related liabilities. Due to the increase in the fair value of these investments in 2010, which are primarily denominated in the South Korean won, the effect of a hypothetical 10% strengthening in U.S. dollar to foreign currencies at December 31, 2010 was greater than that effect at December 31, 2009.
The effect of a hypothetical increase in interest rates was determined by estimating the present value of future cash flows using various models, primarily duration modeling and, for GMIB contracts, stochastic modeling. The effect of a hypothetical strengthening of the U.S. dollar relative to the foreign currencies held by the Company was estimated to be 10% of the U.S. dollar equivalent fair value. The effect of a hypothetical decrease in the market prices of equity exposures was estimated based on a 10% decrease in the equity mutual fund values underlying guaranteed minimum income benefits reinsured by the Company and a 10% decrease in the value of equity securities held by the Company. See Note 11 to the Consolidated Financial Statements for additional information.
The Company uses futures contracts as part of a GMDB equity hedge program to substantially reduce the effect of equity market changes on certain reinsurance contracts that guarantee minimum death benefits based on unfavorable changes in underlying variable annuity account values. The hypothetical effect of a 10% increase in the S&P 500, S&P 400, Russell 2000, NASDAQ, TOPIX (Japanese), EUROSTOXX and FTSE (British) equity indices and a 10% weakening in the U.S. dollar to the Japanese yen, British pound and euro would have been a decrease of approximately $80 million in the fair value of the futures contracts outstanding under this program as of December 31, 2010. A corresponding decrease in liabilities for GMDB contracts would result from the hypothetical 10% increase in these equity indices and 10% weakening in the U.S. dollar. See Note 7 to the Consolidated Financial Statements for further discussion of this program and related GMDB contracts.
As noted above, the Company manages its exposures to market risk by matching investment characteristics to its obligations.
Stock Market Performance
The performance of equity markets can have a significant effect on the Company’s businesses, including on:
•
risks and exposures associated with GMDB (see Note 7 to the Consolidated Financial Statements) and GMIB contracts (see Note 11 to the Consolidated Financial Statements); and
•
pension liabilities since equity securities comprise a significant portion of the assets of the Company’s employee pension plans.
CIGNA CORPORATION – 2010 Form 10-K – 94
Cautionary Statement for Purposes of the “Safe Harbor” Provisions of the Private Securities Litigation Reform Act of 1995
CIGNA Corporation and its subsidiaries (the “Company”) and its representatives may from time to time make written and oral forward-looking statements, including statements contained in press releases, in the Company’s filings with the Securities and Exchange Commission, in its reports to shareholders and in meetings with analysts and investors. Forward-looking statements may contain information about financial prospects, economic conditions, trends and other uncertainties. These forward-looking statements are based on management’s beliefs and assumptions and on information available to management at the time the statements are or were made. Forward-looking statements include but are not limited to the information concerning possible or assumed future business strategies, financing plans, competitive position, potential growth opportunities, potential operating performance improvements, trends and, in particular, the Company’s strategic initiatives, litigation and other legal matters, operational improvement initiatives in the health care operations, and the outlook for the Company’s full year 2011 and beyond results. Forward-looking statements include all statements that are not historical facts and can be identified by the use of forward-looking terminology such as the words “believe”, “expect”, “plan”, “intend”, “anticipate”, “estimate”, “predict”, “potential”, “may”, “should” or similar expressions.
By their nature, forward-looking statements: (i) speak only as of the date they are made, (ii) are not guarantees of future performance or results and (iii) are subject to risks, uncertainties and assumptions that are difficult to predict or quantify. Therefore, actual results could differ materially and adversely from those forward-looking statements as a result of a variety of factors. Some factors that could cause actual results to differ materially from the forward-looking statements include:
1.
increased medical costs that are higher than anticipated in establishing premium rates in the Company’s Health Care operations, including increased use and costs of medical services;
2.
increased medical, administrative, technology or other costs resulting from new legislative and regulatory requirements imposed on the Company’s businesses;
3.
challenges and risks associated with implementing operational improvement initiatives and strategic actions in the ongoing operations of the businesses, including those related to: (i) growth in targeted geographies, product lines, buying segments and distribution channels, (ii) offering products that meet emerging market needs, (iii) strengthening underwriting and pricing effectiveness, (iv) strengthening medical cost and medical membership results, (v) delivering quality member and provider service using effective technology solutions, (vi) lowering administrative costs and (vii) transitioning to an integrated operating company model, including operating efficiencies related to the transition;
4.
risks associated with pending and potential state and federal class action lawsuits, disputes regarding reinsurance arrangements, other litigation and regulatory actions challenging the Company’s businesses, including disputes related to payments to health care professionals, government investigations and proceedings, and tax audits and related litigation;
5.
heightened competition, particularly price competition, which could reduce product margins and constrain growth in the Company’s businesses, primarily the Health Care business;
6.
risks associated with the Company’s mail order pharmacy business which, among other things, includes any potential operational deficiencies or service issues as well as loss or suspension of state pharmacy licenses;
7.
significant changes in interest rates or sustained deterioration in the commercial real estate markets;
8.
downgrades in the financial strength ratings of the Company’s insurance subsidiaries, which could, among other things, adversely affect new sales, retention of current business as well as a downgrade in financial strength ratings of reinsurers which could result in increased statutory reserve or capital requirements;
9.
limitations on the ability of the Company’s insurance subsidiaries to dividend capital to the parent company as a result of downgrades in the subsidiaries’ financial strength ratings, changes in statutory reserve or capital requirements or other financial constraints;
10.
inability of the program adopted by the Company to substantially reduce equity market risks for reinsurance contracts that guarantee minimum death benefits under certain variable annuities (including possible market difficulties in entering into appropriate futures contracts and in matching such contracts to the underlying equity risk);
11.
adjustments to the reserve assumptions (including lapse, partial surrender, mortality, interest rates and volatility) used in estimating the Company’s liabilities for reinsurance contracts covering guaranteed minimum death benefits under certain variable annuities;
12.
adjustments to the assumptions (including annuity election rates and amounts collectible from reinsurers) used in estimating the Company’s assets and liabilities for reinsurance contracts covering guaranteed minimum income benefits under certain variable annuities;
13.
significant stock market declines, which could, among other things, result in increased expenses for guaranteed minimum income benefit contracts, guaranteed minimum death benefit contracts and the Company’s pension plans in future periods as well as the recognition of additional pension obligations;
14.
significant deterioration in economic conditions and significant market volatility, which could have an adverse effect on the Company’s operations, investments, liquidity and access to capital markets;
CIGNA CORPORATION – 2010 Form 10-K – 95
15.
significant deterioration in economic conditions and significant market volatility, which could have an adverse effect on the businesses of our customers (including the amount and type of health care services provided to their workforce, loss in workforce and our customers’ ability to pay receivables) and our vendors (including their ability to provide services);
16.
adverse changes in state, federal and international laws and regulations, including health care reform legislation and regulation which could, among other items, affect the way the Company does business, increase cost, limit the ability to effectively estimate, price for and manage medical costs, and affect the Company’s products, services, market segments, technology and processes;
17.
amendments to income tax laws, which could affect the taxation of employer provided benefits, the taxation of certain insurance products such as corporate-owned life insurance, or the financial decisions of individuals whose variable annuities are covered under reinsurance contracts issued by the Company;
18.
potential public health epidemics, pandemics and bio-terrorist activity, which could, among other things, cause the Company’s covered medical and disability expenses, pharmacy costs and mortality experience to rise significantly, and cause operational disruption, depending on the severity of the event and number of individuals affected;
19.
risks associated with security or interruption of information systems, which could, among other things, cause operational disruption;
20.
challenges and risks associated with the successful management of the Company’s outsourcing projects or key vendors, including the agreement with IBM for provision of technology infrastructure and related services;
21.
the ability to successfully complete the integration of acquired businesses; and
22.
the unique political, legal, operational, regulatory and other challenges associated with expanding our business globally.
This list of important factors is not intended to be exhaustive. Other sections of the Form 10-K, including the “Risk Factors” section, and other documents filed with the Securities and Exchange Commission include both expanded discussion of these factors and additional risk factors and uncertainties that could preclude the Company from realizing the forward-looking statements. The Company does not assume any obligation to update any forward-looking statements, whether as a result of new information, future events or otherwise, except as required by law.
CIGNA CORPORATION – 2010 Form 10-K – 96
Management’s Annual Report on Internal Control over Financial Reporting
Management of CIGNA Corporation is responsible for establishing and maintaining adequate internal controls over financial reporting. The Company’s internal controls were designed to provide reasonable assurance to the Company’s management and Board of Directors that the Company’s consolidated published financial statements for external purposes were prepared in accordance with generally accepted accounting principles. The Company’s internal control over financial reporting include those policies and procedures that:
(i)
pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets and liabilities of the Company;
(ii)
provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the Company are being made only in accordance with authorization of management and directors of the Company; and
(iii)
provide reasonable assurance regarding prevention or timely detection of unauthorized acquisitions, use or disposition of the Company’s assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements.
Management assessed the effectiveness of the Company’s internal controls over financial reporting as of December 31, 2010. In making this assessment, Management used the criteria set forth by the Committee of Sponsoring Organizations of the Treadway Commission (“COSO”) in Internal Control-Integrated Framework. Based on management’s assessment and the criteria set forth by COSO, it was determined that the Company’s internal controls over financial reporting are effective as of December 31, 2010.
The Company’s independent registered public accounting firm, PricewaterhouseCoopers, has audited the effectiveness of the Company’s internal control over financial reporting, as stated in their report located on page 165 in this Form 10-K.
CIGNA CORPORATION – 2010 Form 10-K – 97
ITEM 7A Quantitative and Qualitative Disclosures About Market Risk
The information contained under the caption “Market Risk” in the MD&A section of this Form 10-K is incorporated by reference.
CIGNA CORPORATION – 2010 Form 10-K – 98
ITEM 8 Financial Statements and Supplementary Data
CIGNA Corporation
Consolidated Statements of Income
|
For the years ended December 31, (In millions, except per share amounts) |
2010 |
2009 |
2008 |
|
Revenues | |||
|
Premiums and fees |
$18,393 |
$16,041 |
$16,253 |
|
Net investment income |
1,105 |
1,014 |
1,063 |
|
Mail order pharmacy revenues |
1,420 |
1,282 |
1,204 |
|
Other revenues |
260 |
120 |
751 |
|
Realized investment gains (losses) | |||
|
Other-than-temporary impairments on fixed maturities, net |
(1) |
(47) |
(213) |
|
Other realized investment gains |
76 |
4 |
43 |
|
Total realized investment gains (losses) |
75 |
(43) |
(170) |
|
TOTAL REVENUES |
21,253 |
18,414 |
19,101 |
|
Benefits and Expenses | |||
|
Health Care medical claims expense |
8,570 |
6,927 |
7,252 |
|
Other benefit expenses |
3,663 |
3,407 |
4,285 |
|
Mail order pharmacy cost of goods sold |
1,169 |
1,036 |
961 |
|
GMIB fair value (gain) loss |
55 |
(304) |
690 |
|
Other operating expenses |
5,926 |
5,450 |
5,531 |
|
TOTAL BENEFITS AND EXPENSES |
19,383 |
16,516 |
18,719 |
|
Income from Continuing Operations before Income Taxes |
1,870 |
1,898 |
382 |
|
Income taxes (benefits): | |||
|
Current |
331 |
275 |
313 |
|
Deferred |
190 |
319 |
(221) |
|
TOTAL TAXES |
521 |
594 |
92 |
|
Income from Continuing Operations |
1,349 |
1,304 |
290 |
|
Income from Discontinued Operations, Net of Taxes |
- |
1 |
4 |
|
Net Income |
1,349 |
1,305 |
294 |
|
Less: Net Income Attributable to Noncontrolling Interest |
4 |
3 |
2 |
|
SHAREHOLDERS’ NET INCOME |
$1,345 |
$1,302 |
$292 |
|
Basic Earnings Per Share: | |||
|
Shareholders' income from continuing operations |
$4.93 |
$4.75 |
$1.04 |
|
Shareholders' income from discontinued operations |
- |
- |
0.01 |
|
SHAREHOLDERS’ NET INCOME |
$4.93 |
$4.75 |
$1.05 |
|
Diluted Earnings Per Share: | |||
|
Shareholders’ income from continuing operations |
$4.89 |
$4.73 |
$1.03 |
|
Shareholders’ income from discontinued operations |
- |
- |
0.02 |
|
SHAREHOLDERS’ NET INCOME |
$4.89 |
$4.73 |
$1.05 |
|
Dividends Declared Per Share |
$0.04 |
$0.04 |
$0.04 |
|
Amounts Attributable to CIGNA: | |||
|
Shareholders’ income from continuing operations |
$1,345 |
$1,301 |
$288 |
|
Shareholders’ income from discontinued operations |
- |
1 |
4 |
|
SHAREHOLDERS’ NET INCOME |
$1,345 |
$1,302 |
$292 |
|
The accompanying Notes to the Consolidated Financial Statements are an integral part of these statements. |
|||
CIGNA CORPORATION – 2010 Form 10-K – 99
CIGNA Corporation
Consolidated Balance Sheets
|
As of December 31, (In millions, except per share amounts) |
2010 |
2009 |
|
ASSETS | ||
|
Investments: | ||
|
Fixed maturities, at fair value (amortized cost, $13,445; $12,580) |
$14,709 |
$13,443 |
|
Equity securities, at fair value (cost, $144; $137) |
127 |
113 |
|
Commercial mortgage loans |
3,486 |
3,522 |
|
Policy loans |
1,581 |
1,549 |
|
Real estate |
112 |
124 |
|
Other long-term investments |
759 |
595 |
|
Short-term investments |
174 |
493 |
|
Total investments |
20,948 |
19,839 |
|
Cash and cash equivalents |
1,605 |
924 |
|
Accrued investment income |
235 |
238 |
|
Premiums, accounts and notes receivable, net |
1,318 |
1,361 |
|
Reinsurance recoverables |
6,495 |
6,597 |
|
Deferred policy acquisition costs |
1,122 |
943 |
|
Property and equipment |
912 |
862 |
|
Deferred income taxes, net |
782 |
1,029 |
|
Goodwill |
3,119 |
2,876 |
|
Other assets, including other intangibles |
1,238 |
1,056 |
|
Separate account assets |
7,908 |
7,288 |
|
TOTAL ASSETS |
$45,682 |
$43,013 |
|
LIABILITIES | ||
|
Contractholder deposit funds |
$8,509 |
$8,484 |
|
Future policy benefits |
8,147 |
8,136 |
|
Unpaid claims and claim expenses |
4,017 |
3,968 |
|
Health Care medical claims payable |
1,246 |
921 |
|
Unearned premiums and fees |
416 |
427 |
|
Total insurance and contractholder liabilities |
22,335 |
21,936 |
|
Accounts payable, accrued expenses and other liabilities |
5,936 |
5,797 |
|
Short-term debt |
552 |
104 |
|
Long-term debt |
2,288 |
2,436 |
|
Nonrecourse obligations |
- |
23 |
|
Separate account liabilities |
7,908 |
7,288 |
|
TOTAL LIABILITIES |
39,019 |
37,584 |
|
Contingencies — Note 24 | ||
|
SHAREHOLDERS’ EQUITY | ||
|
Common stock (par value per share, $0.25; shares issued, 351; authorized, 600) |
88 |
88 |
|
Additional paid-in capital |
2,534 |
2,514 |
|
Net unrealized appreciation, fixed maturities |
529 |
378 |
|
Net unrealized appreciation, equity securities |
3 |
4 |
|
Net unrealized depreciation, derivatives |
(24) |
(30) |
|
Net translation of foreign currencies |
25 |
(12) |
|
Postretirement benefits liability adjustment |
(1,147) |
(958) |
|
Accumulated other comprehensive loss |
(614) |
(618) |
|
Retained earnings |
9,879 |
8,625 |
|
Less treasury stock, at cost |
(5,242) |
(5,192) |
|
TOTAL SHAREHOLDERS’ EQUITY |
6,645 |
5,417 |
|
Noncontrolling interest |
18 |
12 |
|
TOTAL EQUITY |
6,663 |
5,429 |
|
Total liabilities and equity |
$45,682 |
$43,013 |
|
SHAREHOLDERS’ EQUITY PER SHARE |
$24.44 |
$19.75 |
|
The accompanying Notes to the Consolidated Financial Statements are an integral part of these statements. |
||
CIGNA CORPORATION – 2010 Form 10-K – 100
CIGNA Corporation
Consolidated Statements of Comprehensive Income and Changes in Total Equity
|
For the years ended December 31, (In millions, except per share amounts) |
2010 |
2009 |
2008 |
|||
|
Comprehensive Income |
Total Equity |
Comprehensive Income |
Total Equity |
Comprehensive Income |
Total Equity |
|
|
Common Stock, beginning and end of year |
|
$88 |
|
$88 |
|
$88 |
|
Additional Paid-In Capital, beginning of year |
|
2,514 |
|
2,502 |
|
2,474 |
|
Effect of issuance of stock for employee benefit plans |
20 |
12 |
28 |
|||
|
Additional Paid-In Capital, end of year |
|
2,534 |
|
2,514 |
|
2,502 |
|
Accumulated Other Comprehensive Income (Loss), beginning of year |
|
(618) |
|
(1,074) |
|
51 |
|
Implementation effect of updated guidance on other-than-temporary impairments (see Note 2) |
- |
(18) |
- |
|||
|
Net unrealized appreciation (depreciation), fixed maturities |
$151 |
151 |
$543 |
543 |
$(287) |
(287) |
|
Net unrealized depreciation, equity securities |
(1) |
(1) |
(3) |
(3) |
- |
- |
|
Net unrealized appreciation (depreciation) on securities |
150 |
540 |
(287) | |||
|
Net unrealized appreciation (depreciation), derivatives |
6 |
6 |
(17) |
(17) |
6 |
6 |
|
Net translation of foreign currencies |
37 |
37 |
48 |
48 |
(121) |
(121) |
|
Postretirement benefits liability adjustment |
(189) |
(189) |
(97) |
(97) |
(723) |
(723) |
|
Other comprehensive income (loss) |
4 |
474 |
(1,125) | |||
|
Accumulated Other Comprehensive Loss, end of year |
|
(614) |
|
(618) |
|
(1,074) |
|
Retained Earnings, beginning of year |
|
8,625 |
|
7,374 |
|
7,113 |
|
Implementation effect of updated guidance on other-than-temporary impairments (See Note 2) |
- |
18 |
- |
|||
|
Shareholders’ net income |
1,345 |
1,345 |
1,302 |
1,302 |
292 |
292 |
|
Effect of issuance of stock for employee benefit plans |
(80) |
(58) |
(20) |
|||
|
Common dividends declared (per share: $0.04; $0.04; $0.04) |
(11) |
(11) |
(11) |
|||
|
Retained Earnings, end of year |
|
9,879 |
|
8,625 |
|
7,374 |
|
Treasury Stock, beginning of year |
|
(5,192) |
|
(5,298) |
|
(4,978) |
|
Repurchase of common stock |
(201) |
- |
(378) |
|||
|
Other, primarily issuance of treasury stock for employee benefit plans |
151 |
106 |
58 |
|||
|
Treasury Stock, end of year |
|
(5,242) |
|
(5,192) |
|
(5,298) |
|
Shareholders’ Comprehensive Income (Loss) and Shareholders’ Equity |
1,349 |
6,645 |
1,776 |
5,417 |
(833) |
3,592 |
|
Noncontrolling interest, beginning of year |
|
12 |
|
6 |
|
6 |
|
Net income attributable to noncontrolling interest |
4 |
4 |
3 |
3 |
2 |
2 |
|
Accumulated other comprehensive income attributable to noncontrolling interest |
2 |
2 |
3 |
3 |
(2) |
(2) |
|
Noncontrolling interest, end of year |
6 |
18 |
6 |
12 |
- |
6 |
|
TOTAL COMPREHENSIVE INCOME AND TOTAL EQUITY |
$1,355 |
$6,663 |
$1,782 |
$5,429 |
$(833) |
$3,598 |
|
The accompanying Notes to the Consolidated Financial Statements are an integral part of these statements. |
||||||
CIGNA CORPORATION – 2010 Form 10-K – 101
CIGNA Corporation
Consolidated Statements of Cash Flows
|
For the years ended December 31, (In millions) |
2010 |
2009 |
2008 |
|
Cash Flows from Operating Activities | |||
|
Net income |
$1,349 |
$1,305 |
$294 |
|
Adjustments to reconcile net income to net cash provided by operating activities: | |||
|
Depreciation and amortization |
292 |
268 |
244 |
|
Realized investment (gains) losses |
(75) |
43 |
170 |
|
Deferred income taxes |
190 |
319 |
(221) |
|
Gains on sales of businesses (excluding discontinued operations) |
(13) |
(32) |
(38) |
|
(Income) from discontinued operations |
- |
(1) |
(4) |
|
Net changes in assets and liabilities, net of non-operating effects: | |||
|
Premiums, accounts and notes receivable |
62 |
49 |
219 |
|
Reinsurance recoverables |
37 |
30 |
63 |
|
Deferred policy acquisition costs |
(156) |
(109) |
(74) |
|
Other assets |
(3) |
452 |
(860) |
|
Insurance liabilities |
325 |
(357) |
485 |
|
Accounts payable, accrued expenses and other liabilities |
(272) |
(1,321) |
1,466 |
|
Current income taxes |
2 |
55 |
(72) |
|
Other, net |
5 |
44 |
(16) |
|
NET CASH PROVIDED BY OPERATING ACTIVITIES |
1,743 |
745 |
1,656 |
|
Cash Flows from Investing Activities | |||
|
Proceeds from investments sold: | |||
|
Fixed maturities |
822 |
927 |
1,459 |
|
Equity securities |
4 |
22 |
6 |
|
Commercial mortgage loans |
63 |
61 |
48 |
|
Other (primarily short-term and other long-term investments) |
1,102 |
910 |
492 |
|
Investment maturities and repayments: | |||
|
Fixed maturities |
1,084 |
1,100 |
872 |
|
Commercial mortgage loans |
70 |
94 |
98 |
|
Investments purchased: | |||
|
Fixed maturities |
(2,587) |
(2,916) |
(2,681) |
|
Equity securities |
(12) |
(14) |
(18) |
|
Commercial mortgage loans |
(239) |
(175) |
(488) |
|
Other (primarily short-term and other long-term investments) |
(810) |
(1,187) |
(776) |
|
Property and equipment purchases |
(300) |
(307) |
(257) |
|
Acquisitions, net of cash acquired |
(344) |
- |
(1,319) |
|
Other (primarily dispositions) |
(195) |
- |
(8) |
|
NET CASH USED IN INVESTING ACTIVITIES |
(1,342) |
(1,485) |
(2,572) |
|
Cash Flows from Financing Activities | |||
|
Deposits and interest credited to contractholder deposit funds |
1,295 |
1,312 |
1,305 |
|
Withdrawals and benefit payments from contractholder deposit funds |
(1,205) |
(1,223) |
(1,214) |
|
Change in cash overdraft position |
59 |
53 |
(17) |
|
Net change in short-term debt, primarily commercial paper |
- |
(199) |
298 |
|
Net proceeds on issuance of long-term debt |
543 |
346 |
297 |
|
Repayment of long-term debt |
(270) |
(1) |
- |
|
Repurchase of common stock |
(201) |
- |
(378) |
|
Issuance of common stock |
64 |
30 |
37 |
|
Common dividends paid |
(11) |
(11) |
(14) |
|
NET CASH PROVIDED BY FINANCING ACTIVITIES |
274 |
307 |
314 |
|
Effect of foreign currency rate changes on cash and cash equivalents |
6 |
15 |
(26) |
|
Net increase (decrease) in cash and cash equivalents |
681 |
(418) |
(628) |
|
Cash and cash equivalents, beginning of year |
924 |
1,342 |
1,970 |
|
Cash and cash equivalents, end of year |
$1,605 |
$924 |
$1,342 |
|
Supplemental Disclosure of Cash Information: | |||
|
Income taxes paid, net of refunds |
$326 |
$220 |
$366 |
|
Interest paid |
$180 |
$158 |
$140 |
|
The accompanying Notes to the Consolidated Financial Statements are an integral part of these statements. |
|||
CIGNA CORPORATION – 2010 Form 10-K – 102
Notes to the Consolidated Financial Statements
NOTE 1 Description of Business
As used in this document, “CIGNA” and the “Company” may refer to CIGNA Corporation itself, one or more of its subsidiaries, or CIGNA Corporation and its consolidated subsidiaries. CIGNA Corporation is a holding company and is not an insurance company. Its subsidiaries conduct various businesses, which are described in this Annual Report on Form 10-K for the fiscal year ended December 31, 2010 (“Form 10-K”).
The Company is a global health service organization with subsidiaries that are major providers of medical, dental, disability, life and accident insurance and related products and services. In the U.S., the majority of these products and services are offered through employers and other groups (e.g. unions and associations) and in selected international markets, the Company offers supplemental health, life and accident insurance products, expatriate benefits and international health care coverage and services to businesses, governmental and non-governmental organizations and individuals. In addition to its ongoing operations described above, the Company also has certain run-off operations, including a Run-off Reinsurance segment.
NOTE 2 Summary of Significant Accounting Policies
A. Basis of Presentation
The Consolidated Financial Statements include the accounts of CIGNA Corporation and its significant subsidiaries. Intercompany transactions and accounts have been eliminated in consolidation.
These Consolidated Financial Statements were prepared in conformity with accounting principles generally accepted in the United States of America (“GAAP”). Amounts recorded in the Consolidated Financial Statements necessarily reflect management’s estimates and assumptions about medical costs, investment valuation, interest rates and other factors. Significant estimates are discussed throughout these Notes; however, actual results could differ from those estimates. The impact of a change in estimate is generally included in earnings in the period of adjustment.
In preparing these Consolidated Financial Statements, the Company has evaluated events that occurred between the balance sheet date and February 25, 2011 and determined there were no other items to disclose.
Certain reclassifications have been made to prior period amounts to conform to the current presentation. In addition, certain amounts have been restated as a result of the adoption of new accounting pronouncements.
Variable interest entities
As of December 31, 2010 and 2009 the Company determined it was not a primary beneficiary in any variable interest entities.
B. Recent Accounting Pronouncements
Deferred acquisition costs
In October 2010, the Financial Accounting Standards Board (“FASB”) amended guidance (ASU 2010-26) for the accounting of costs related to the acquisition or renewal of insurance contracts to require costs such as certain sales compensation or telemarketing costs that are related to unsuccessful efforts and any indirect costs to be expensed as incurred. This new guidance must be implemented on January 1, 2012 or may be implemented earlier and any changes to the Company’s Consolidated Financial Statements may be recognized prospectively for acquisition costs incurred beginning in 2012 or through retrospective adjustment of comparative prior periods. The Company’s deferred acquisition costs arise from sales and renewal activities primarily in its International segment and, to a lesser extent, the Health Care and corporate-owned life insurance businesses. Because the new requirements further restrict the types of costs that are deferrable, the Company expects more of its acquisition costs to be expensed when incurred under the new guidance. The Company continues to evaluate these new requirements to determine the timing, method and estimated effects of their implementation.
Credit quality disclosures
Effective December 31, 2010, the Company adopted the FASB’s updated guidance (ASU 2010-20) that requires disclosures about the credit quality and risks inherent in financing receivables, including how credit risk is analyzed and assessed on a disaggregated basis (by portfolio segment and class). The Company determined it has one portfolio segment and one class of mortgage loans because all loans are subject to the same monitoring and risk assessment process, and are made exclusively to commercial borrowers. Financing receivables other than mortgage loans are immaterial. See Note 12 (B) for additional information.
CIGNA CORPORATION – 2010 Form 10-K – 103
Variable interest entities
Effective January 1, 2010, the Company adopted the FASB’s amended guidance that requires ongoing qualitative analysis to determine whether a variable interest entity must be consolidated based on the entity’s purpose and design, the Company’s ability to direct the entity’s activities that most significantly impact its economic performance, and the Company’s right or obligation to participate in that performance (ASC 810). A variable interest entity is insufficiently capitalized or is not controlled by its equity owners through voting or similar rights. These amendments must be applied to qualifying special-purpose entities and troubled debt restructures formerly excluded from such analysis. On adoption and through December 31, 2010, the Company was not required to consolidate any variable interest entities and there were no effects to its results of operations or financial condition. Although consolidation was not required, disclosures about the Company’s involvement with variable interest entities have been provided in Note 14.
Transfers of financial assets
Effective January 1, 2010, the Company adopted the FASB’s guidance for accounting for transfers of financial assets (ASC 860) that changes the requirements for recognizing the transfer of financial assets and requires additional disclosures about a transferor’s continuing involvement in transferred assets. The guidance also eliminates the concept of a “qualifying special purpose entity” when assessing transfers of financial instruments. On adoption, there were no effects to the Company’s results of operations or financial condition.
Fair value measurements
The Company adopted the FASB’s updated guidance on fair value measurements (ASU 2010-06) in the first quarter of 2010, which requires separate disclosures of significant transfers between levels in the fair value hierarchy. See Note 11 for additional information.
Effective January 1, 2008, the Company adopted the FASB’s fair value disclosure and measurement guidance (ASC 820) that expands disclosures about fair value measurements and clarifies how to measure fair value by focusing on the price that would be received when selling an asset or paid to transfer a liability (exit price). At adoption, the Company was required to change certain assumptions used to estimate the fair values of GMIB assets and liabilities. Because there is no market for these contracts, the assumptions used to estimate their fair values at adoption were determined using a hypothetical market participant’s view of exit price, rather than using historical market data and actual experience to establish the Company’s future expectations. Certain of these assumptions (primarily related to annuitant behavior) have limited or no observable market data so determining an exit price requires the Company to exercise significant judgment and make critical accounting estimates. On adoption, the Company recorded a charge of $131 million after-tax, net of reinsurance ($202 million pre-tax), in Run-off Reinsurance. The Company’s results of operations related to this business are expected to continue to be volatile in future periods because several underlying assumptions (primarily interest rates) will be based on current market-observable inputs which will likely change each period.
Amendments to this guidance in 2008 and 2009 had no effect on the Company’s Consolidated Financial Statements. See Note 11 for additional information.
Other-than-temporary impairments
On April 1, 2009, the Company adopted the FASB’s updated guidance for evaluating whether an impairment is other than temporary for fixed maturities with declines in fair value below amortized cost (ASC 320). A reclassification adjustment from retained earnings to accumulated other comprehensive income was required for previously impaired fixed maturities that had a non-credit loss as of the date of adoption, net of related tax effects.
The cumulative effect of adoption increased the Company’s retained earnings in 2009 with an offsetting decrease to accumulated other comprehensive income of $18 million, with no overall change to shareholders’ equity. See Note 12 (A) for information on the Company’s other-than-temporary impairments including additional required disclosures.
Noncontrolling interests in subsidiaries
Effective January 1, 2009, the Company adopted the FASB’s updated guidance on accounting for noncontrolling interests (ASC 810) through retroactive restatement of prior financial statements and reclassified $3 million of noncontrolling interest as of January 1, 2007 from Accounts payable, accrued expenses and other liabilities to Noncontrolling interest in total equity. In addition, net income attributable to the noncontrolling interest of $2 million in 2008 and $3 million in 2007 has been reclassified to be included in net income, with a reduction to net income to determine net income attributable to the Company’s shareholders (“shareholders’ net income”).
Earnings per share
Effective January 1, 2009, the Company adopted the FASB’s updated earnings per share guidance (ASC 260) for determining participating securities that requires unvested restricted stock awards containing rights to nonforfeitable dividends to be included in the denominator of both basic and diluted earnings per share (“EPS”) calculations. Prior period EPS data were restated in 2009 to reflect the adoption of this guidance. As part of this restatement, basic EPS for the full year 2008 was adjusted to $1.04 per share (originally reported as $1.05 per share).
CIGNA CORPORATION – 2010 Form 10-K – 104
C. Investments
The Company’s accounting policies for investment assets are discussed below:
Fixed maturities and equity securities
Fixed maturities primarily include bonds, mortgage and other asset-backed securities and preferred stocks redeemable by the investor. Equity securities include common stocks and preferred stocks that are non-redeemable or redeemable only at the option of the issuer. These investments are primarily classified as available for sale and are carried at fair value with changes in fair value recorded in accumulated other comprehensive income (loss) within shareholders’ equity. Beginning April 1, 2009, when the Company determines it does not expect to recover the amortized cost basis of fixed maturities with declines in fair value (even if it does not intend to sell or will not be required to sell these fixed maturities), the credit portion of the impairment loss is recognized in net income and the non-credit portion, if any, is recognized in a separate component of shareholders’ equity. The credit portion is the difference between the amortized cost basis of the fixed maturity and the net present value of its projected future cash flows. Projected future cash flows are based on qualitative and quantitative factors, including probability of default, and the estimated timing and amount of recovery. For mortgage and asset-backed securities, estimated future cash flows are based on assumptions about the collateral attributes including prepayment speeds, default rates and changes in value. Equity securities and, prior to April 1, 2009, fixed maturities were considered impaired, and their cost basis was written down to fair value through earnings, when management did not expect to recover the amortized cost, or if the Company could not demonstrate its intent or ability to hold the investment until full recovery. Fixed maturities and equity securities also include trading and certain hybrid securities that are carried at fair value with changes in fair value reported in realized investment gains and losses. The Company has irrevocably elected the fair value option for these securities to simplify accounting and mitigate volatility in results of operations and financial condition. Hybrid securities include certain preferred stock and debt securities with call or conversion options.
Commercial mortgage loans
Mortgage loans held by the Company are made exclusively to commercial borrowers. Generally, commercial mortgage loans are carried at unpaid principal balances and are issued at a fixed rate of interest. Commercial mortgage loans are considered impaired when it is probable that the Company will not collect amounts due according to the terms of the original loan agreement. The Company assesses the impairment of loans individually for all loans in the portfolio. Impaired loans are carried at the lower of unpaid principal or fair value of the underlying collateral. Valuation reserves reflect any changes in fair value. The Company estimates the fair value of the underlying collateral using internal valuations generally based on discounted cash flow analyses.
Policy loans
Policy loans are carried at unpaid principal balances plus accumulated interest. The loans are collateralized by insurance policy cash values and therefore have no exposure to credit loss.
Real estate
Investment real estate can be “held and used” or “held for sale”. The Company accounts for real estate as follows:
•
Real estate “held and used” is expected to be held longer than one year and includes real estate acquired through the foreclosure of commercial mortgage loans. The Company carries real estate held and used at depreciated cost less any write-downs to fair value due to impairment and assesses impairment when cash flows indicate that the carrying value may not be recoverable. Depreciation is generally calculated using the straight-line method based on the estimated useful life of the particular real estate asset.
•
Real estate is “held for sale” when a buyer’s investigation is completed, a deposit has been received and the sale is expected to be completed within the next year. Real estate held for sale is carried at the lower of carrying value or current fair value, less estimated costs to sell, and is not depreciated. Valuation reserves reflect any changes in fair value.
•
The Company uses several methods to determine the fair value of real estate, but relies primarily on discounted cash flow analyses and, in some cases, third-party appraisals.
At the time of foreclosure, properties are reclassified from commercial mortgage loans to real estate or other long-term investments depending on the ownership of the underlying assets. The Company rehabilitates, re-leases and sells foreclosed properties. This process usually takes from three to five years unless management considers a near-term sale preferable. When foreclosed real estate is recapitalized through a joint venture including a contribution of new equity from a third-party investor, the asset is accounted for as a partnership investment in good standing reported in other long-term investments.
CIGNA CORPORATION – 2010 Form 10-K – 105
Other long-term investments
Other long-term investments include investments in unconsolidated entities. These entities include certain limited partnerships and limited liability companies holding real estate, securities or loans. These investments are carried at cost plus the Company’s ownership percentage of reported income or loss in cases where the Company has significant influence, otherwise the investment is carried at cost. Income from certain entities is reported on a one quarter lag depending on when their financial information is received. Also included in other long-term investments are loans to unconsolidated real estate entities secured by the equity interests of these real estate entities, which are carried at unpaid principal balances (mezzanine loans). These other long-term investments are considered impaired, and written down to their fair value, when cash flows indicate that the carrying value may not be recoverable. Fair value is generally determined based on a discounted cash flow analysis.
Additionally, other long-term investments include interest rate and foreign currency swaps carried at fair value. See Note 13 for information on the Company’s accounting policies for these derivative financial instruments.
Short-term investments
Investments with maturities of greater than 90 days but less than one year from time of purchase are classified as short-term, available for sale and carried at fair value, which approximates cost.
Derivative financial instruments
Note 13 discusses the Company’s accounting policies for derivative financial instruments.
Net investment income
When interest and principal payments on investments are current, the Company recognizes interest income when it is earned. The Company stops recognizing interest income when interest payments are delinquent based on contractual terms or when certain terms (interest rate or maturity date) of the investment have been restructured. Net investment income on these investments is only recognized when interest payments are actually received. Interest and dividends on trading and hybrid securities are included in net investment income when they are earned.
Investment gains and losses
Realized investment gains and losses result from sales, investment asset write-downs, changes in the fair values of trading and hybrid securities and certain derivatives and changes in valuation reserves, based on specifically identified assets. Realized investment gains and losses on the disposition of certain directly owned real estate investments are eliminated from ongoing operations and reported in discontinued operations when the operations and cash flows of the underlying assets are clearly distinguishable and the Company has no significant continuing involvement in their operations.
Unrealized gains and losses on fixed maturities and equity securities carried at fair value (excluding trading and hybrid securities) and certain derivatives are included in accumulated other comprehensive income (loss), net of:
•
amounts required to adjust future policy benefits for the run-off settlement annuity business; and
•
deferred income taxes.
D. Cash and Cash Equivalents
Cash equivalents consist of short-term investments with maturities of three months or less from the time of purchase that are classified as held to maturity and carried at amortized cost. The Company reclassifies cash overdraft positions to accounts payable, accrued expenses and other liabilities when the legal right of offset does not exist.
E. Premiums, Accounts and Notes Receivable and Reinsurance Recoverables
Premiums, accounts and notes receivable are reported net of an allowance for doubtful accounts of $49 million as of December 31, 2010 and $43 million as of December 31, 2009. Reinsurance recoverables are estimates of amounts that the Company will receive from reinsurers and are recorded net of an allowance for unrecoverable reinsurance of $10 million as of December 31, 2010 and $15 million as of December 31, 2009. The Company estimates these allowances for doubtful accounts for premiums, accounts and notes receivable, as well as for reinsurance recoverables, using management’s best estimate of collectibility, taking into consideration the aging of these amounts, historical collection patterns and other economic factors.
CIGNA CORPORATION – 2010 Form 10-K – 106
F. Deferred Policy Acquisition Costs
Acquisition costs include sales compensation, commissions, direct response marketing, telemarketing, premium taxes and other costs that the Company incurs in connection with new and renewal business. Depending on the product line they relate to, the Company records acquisition costs in different ways. Acquisition costs for:
•
Universal life products are deferred and amortized in proportion to the present value of total estimated gross profits over the expected lives of the contracts.
•
Supplemental health, life and accident insurance (primarily individual international products) and group health and accident insurance products are deferred and amortized, generally in proportion to the ratio of periodic revenue to the estimated total revenues over the contract periods.
•
Other products are expensed as incurred.
For universal life and other individual products, management estimates the present value of future revenues less expected payments. For group health and accident insurance products, management estimates the sum of unearned premiums and anticipated net investment income less future expected claims and related costs. If management’s estimates of these sums are less than the deferred costs, the Company reduces deferred policy acquisition costs and records an expense. The Company recorded amortization for policy acquisition costs of $312 million in 2010, $299 million in 2009 and $314 million in 2008 in other operating expenses. There are no deferred policy acquisition costs attributable to the sold individual life insurance and annuity and retirement businesses or the run-off reinsurance operations.
G. Property and Equipment
Property and equipment is carried at cost less accumulated depreciation. When applicable, cost includes interest, real estate taxes and other costs incurred during construction. Also included in this category is internal-use software that is acquired, developed or modified solely to meet the Company’s internal needs, with no plan to market externally. Costs directly related to acquiring, developing or modifying internal-use software are capitalized.
The Company calculates depreciation and amortization principally using the straight-line method generally based on the estimated useful life of each asset as follows: buildings and improvements, 10 to 40 years; purchased software, one to five years; internally developed software; three to seven years and furniture and equipment (including computer equipment); three to 10 years. Improvements to leased facilities are depreciated over the remaining lease term or the estimated life of the improvement. If the Company determines the carrying value of a long-lived asset is not recoverable, an impairment charge is recorded. See Note 9 for additional information.
H. Goodwill
Goodwill represents the excess of the cost of businesses acquired over the fair value of their net assets. Goodwill primarily relates to the Health Care segment ($2.9 billion) and, to a lesser extent, the International segment ($240 million). The Company evaluates goodwill for impairment at least annually during the third quarter at the reporting unit level, based on discounted cash flow analyses and writes it down through results of operations if impaired. Consistent with prior years, the Company’s evaluations of goodwill associated with the Health Care segment used the best information available at the time, including reasonable assumptions and projections consistent with those used in its annual planning process. The discounted cash flow analyses used a range of discount rates that correspond with the Company’s weighted average cost of capital, consistent with that used for investment decisions considering the specific and detailed operating plans and strategies within the Health Care segment. The resulting discounted cash flow analysis indicated an estimated fair value for the Health Care segment exceeding its carrying value, including goodwill and other intangibles. Finally, the Company determined that no events or circumstances occurred subsequent to the annual evaluation of goodwill that would more likely than not reduce the fair value of its reporting units below their carrying values. See Note 9 for additional information.
I. Other Assets, including Other Intangibles
Other assets consist of various insurance-related assets and the gain position of certain derivatives, primarily GMIB assets. The Company’s other intangible assets include purchased customer and producer relationships, provider networks, and trademarks. The Company amortizes other intangibles on an accelerated or straight-line basis over periods from 1 to 30 years. Management revises amortization periods if it believes there has been a change in the length of time that an intangible asset will continue to have value. Costs incurred to renew or extend the terms of these intangible assets are generally expensed as incurred. See Note 9 for additional information.
CIGNA CORPORATION – 2010 Form 10-K – 107
J. Separate Account Assets and Liabilities
Separate account assets and liabilities are contractholder funds maintained in accounts with specific investment objectives. The assets of these accounts are legally segregated and are not subject to claims that arise out of any of the Company’s other businesses. These separate account assets are carried at fair value with equal amounts for related separate account liabilities. The investment income, gains and losses of these accounts generally accrue to the contractholders and are not included in the Company’s revenues and expenses. Fees earned for asset management services are reported in premiums and fees.
K. Contractholder Deposit Funds
Liabilities for contractholder deposit funds primarily includes deposits received from customers for investment-related and universal life products and investment earnings on their fund balances. These liabilities are adjusted to reflect administrative charges and, for universal life fund balances, mortality charges. In addition, this caption includes premium stabilization reserves that are insurance experience refunds for group contracts that are left with the Company to pay future premiums, deposit administration funds that are used to fund nonpension retiree insurance programs, retained asset accounts and annuities or supplementary contracts without significant life contingencies. Interest credited on these funds is accrued ratably over the contract period.
L. Future Policy Benefits
Future policy benefits are liabilities for the present value of estimated future obligations under long-term life and supplemental health insurance policies and annuity products currently in force. These obligations are estimated using actuarial methods and primarily consist of reserves for annuity contracts, life insurance benefits, guaranteed minimum death benefit (“GMDB”) contracts and certain life, accident and health insurance products in our International operations.
Obligations for annuities represent specified periodic benefits to be paid to an individual or groups of individuals over their remaining lives. Obligations for life insurance policies represent benefits to be paid to policyholders, net of future premiums to be received. Management estimates these obligations based on assumptions as to premiums, interest rates, mortality and surrenders, allowing for adverse deviation. Mortality, morbidity, and surrender assumptions are based on either the Company’s own experience or actuarial tables. Interest rate assumptions are based on management’s judgment considering the Company’s experience and future expectations, and range from 1.25% to 10%. Obligations for the run-off settlement annuity business include adjustments for investment returns consistent with requirements of GAAP when a premium deficiency exists.
Certain reinsurance contracts contain GMDB under variable annuities issued by other insurance companies. These obligations represent the guaranteed death benefit in excess of the contractholder’s account values (based on underlying equity and bond mutual fund investments). These obligations are estimated based on assumptions regarding lapse, partial surrenders, mortality, interest rates (mean investment performance and discount rate), market volatility as well as investment returns and premiums, consistent with the requirements of GAAP when a premium deficiency exists. Lapse, partial surrenders, mortality, interest rates and volatility are based on management’s judgment considering the Company’s experience and future expectations. The results of futures contracts used in the GMDB equity hedge program are reflected in the liability calculation as a component of investment returns. See also Note 7 for additional information.
M. Unpaid Claims and Claims Expenses
Liabilities for unpaid claims and claim expenses are estimates of payments to be made under insurance coverages (primarily long-term disability, workers’ compensation and life and health) for reported claims and for losses incurred but not yet reported.
The Company develops these estimates for losses incurred but not yet reported using actuarial principles and assumptions based on historical and projected claim incidence patterns, claim size, subrogation recoveries and the length of time over which payments are expected to be made. The Company consistently applies these actuarial principles and assumptions each reporting period, with consideration given to the variability of these factors, and recognizes the actuarial best estimate of the ultimate liability within a level of confidence, as required by actuarial standards of practice, which require that the liabilities be adequate under moderately adverse conditions.
CIGNA CORPORATION – 2010 Form 10-K – 108
The Company’s estimate of the liability for disability claims reported but not yet paid is primarily calculated as the present value of expected benefit payments to be made over the estimated time period that a policyholder remains disabled. The Company estimates the expected time period that a policyholder may be disabled by analyzing the rate at which an open claim is expected to close (claim resolution rate). Claim resolution rates may vary based upon the length of time a policyholder is disabled, the covered benefit period, cause of disability, benefit design and the policyholder’s age, gender and income level. The Company uses historical resolution rates combined with an analysis of current trends and operational factors to develop current estimates of resolution rates. The reserve for the gross monthly disability benefits due to a policyholder is reduced (offset) by the income that the policyholder receives under other benefit programs, such as Social Security Disability Income, worker’s compensation, statutory disability or other group disability benefit plans. For awards of such offsets that have not been finalized, the Company estimates the probability and amount of the offset based on the Company’s experience over the past three to five years.
The Company discounts certain claim liabilities related to group long-term disability and workers’ compensation because benefit payments may be made over extended periods. Discount rate assumptions are based on projected investment returns for the asset portfolios that support these liabilities and range from 3.80% to 7.25%. When estimates change, the Company records the adjustment in benefits and expenses in the period in which the change in estimate is identified. Discounted liabilities associated with the long-term disability and certain workers’ compensation businesses were $3.1 billion at December 31, 2010 and December 31, 2009.
N. Health Care Medical Claims Payable
Medical claims payable for the Health Care segment include both reported claims and estimates for losses incurred but not yet reported.
The Company develops estimates for Health Care medical claims payable using actuarial principles and assumptions consistently applied each reporting period, and recognizes the actuarial best estimate of the ultimate liability within a level of confidence, as required by actuarial standards of practice, which require that the liabilities be adequate under moderately adverse conditions.
The liability is primarily calculated using “completion factors” (a measure of the time to process claims), which are developed by comparing the date claims were incurred, generally the date services were provided, to the date claims were paid. The Company uses historical completion factors combined with an analysis of current trends and operational factors to develop current estimates of completion factors. The Company estimates the liability for claims incurred in each month by applying the current estimates of completion factors to the current paid claims data. This approach implicitly assumes that historical completion rates will be a useful indicator for the current period. It is possible that the actual completion rates for the current period will develop differently from historical patterns, which could have a material impact on the Company’s medical claims payable and shareholders’ net income.
Completion factors are impacted by several key items including changes in: 1) electronic (auto-adjudication) versus manual claim processing, 2) provider claims submission rates, 3) membership and 4) the mix of products. As noted, the Company uses historical completion factors combined with an analysis of current trends and operational factors to develop current estimates of completion factors.
In addition, for the more recent months, the Company also relies on medical cost trend analysis, which reflects expected claim payment patterns and other relevant operational considerations. Medical cost trend is primarily impacted by medical service utilization and unit costs, which are affected by changes in the level and mix of medical benefits offered, including inpatient, outpatient and pharmacy, the impact of copays and deductibles, changes in provider practices and changes in consumer demographics and consumption behavior.
Despite reflecting both historical and emerging trends in setting reserves, it is possible that the actual medical trend for the current period will develop differently from expectations, which could have a material impact on the Company’s medical claims payable and shareholders’ net income.
For each reporting period, the Company evaluates key assumptions by comparing the assumptions used in establishing the medical claims payable to actual experience. When actual experience differs from the assumptions used in establishing the liability, medical claims payable are increased or decreased through current period shareholders’ net income. Additionally, the Company evaluates expected future developments and emerging trends which may impact key assumptions. The estimation process involves considerable judgment, reflecting the variability inherent in forecasting future claim payments. These estimates are highly sensitive to changes in the Company’s key assumptions, specifically completion factors, and medical cost trends.
CIGNA CORPORATION – 2010 Form 10-K – 109
O. Unearned Premiums and Fees
Premiums for life, accident and health insurance are recognized as revenue on a pro rata basis over the contract period. Fees for mortality and contract administration of universal life products are recognized ratably over the coverage period. The unrecognized portion of these amounts received is recorded as unearned premiums and fees.
P. Accounts Payable, Accrued Expenses and Other Liabilities
Accounts payable, accrued expenses and other liabilities consist principally of liabilities for pension, other postretirement and postemployment benefits (see Note 10), self-insured exposures, incentive compensation and various insurance-related items, including amounts related to reinsurance contracts and insurance-related assessments that management can reasonably estimate. Accounts payable, accrued expenses and other liabilities also include certain overdraft positions and the loss position of certain derivatives, primarily for GMIB contracts (see Note 13). Legal costs to defend the Company’s litigation and arbitration matters are expensed when incurred in cases for which the Company cannot reasonably estimate the ultimate cost to defend. In cases for which the Company can reasonably estimate the cost to defend, these costs are recognized when the claim is reported.
Q. Translation of Foreign Currencies
The Company generally conducts its international business through foreign operating entities that maintain assets and liabilities in local currencies, which are generally their functional currencies. The Company uses exchange rates as of the balance sheet date to translate assets and liabilities into U.S. dollars. Translation gains or losses on functional currencies, net of applicable taxes, are recorded in accumulated other comprehensive income (loss). The Company uses average monthly exchange rates during the year to translate revenues and expenses into U.S. dollars.
R. Premiums and Fees, Revenues and Related Expenses
Premiums for group life, accident and health insurance and managed care coverages are recognized as revenue on a pro rata basis over the contract period. Benefits and expenses are recognized when incurred. Premiums and fees include revenue from experience-rated contracts where revenue is based on the estimated ultimate claim, and in some cases, administrative cost experience of the contract. For these contracts, premium revenue includes an adjustment for experience-rated refunds which is calculated according to contract terms and using the customer’s experience (including estimates of incurred but not reported claims).
Premiums for individual life, accident and health insurance and annuity products, excluding universal life and investment-related products, are recognized as revenue when due. Benefits and expenses are matched with premiums.
Premiums and fees received for CIGNA’s Medicare Advantage Plans and Medicare Part D products from customers and the Centers for Medicare and Medicaid Services (CMS) are recognized as revenue ratably over the contract period. CMS provides risk adjusted premium payments for the Medicare Advantage Plans and Medicare Part D products, based on the demographics and health severity of enrollees. The Company recognizes periodic changes to risk adjusted premiums as revenue when the amounts are determinable and collection is reasonably assured. Additionally, Medicare Part D includes payments from CMS for risk sharing adjustments. The risk sharing adjustments, which are estimated quarterly based on claim experience, compare actual incurred drug benefit costs to estimated costs submitted in original contracts and may result in more or less revenue from CMS. Final revenue adjustments are determined through an annual settlement with CMS that occurs after the contract year.
Revenue for investment-related products is recognized as follows:
•
Net investment income on assets supporting investment-related products is recognized as earned.
•
Contract fees, which are based upon related administrative expenses, are recognized in premiums and fees as they are earned ratably over the contract period.
Benefits and expenses for investment-related products consist primarily of income credited to policyholders in accordance with contract provisions.
Revenue for universal life products is recognized as follows:
•
Net investment income on assets supporting universal life products is recognized as earned.
•
Fees for mortality and surrender charges are recognized as assessed, which is as earned.
•
Administration fees are recognized as services are provided.
CIGNA CORPORATION – 2010 Form 10-K – 110
Benefits and expenses for universal life products consist of benefit claims in excess of policyholder account balances. Expenses are recognized when claims are submitted, and income is credited to policyholders in accordance with contract provisions.
Contract fees and expenses for administrative services only programs and pharmacy programs and services are recognized as services are provided. Mail order pharmacy revenues and cost of goods sold are recognized as each prescription is shipped.
S. Stock Compensation
The Company records compensation expense for stock awards and options over their vesting periods primarily based on the estimated fair value at the grant date. Compensation expense is recorded for stock options over their vesting period based on fair value at the grant date which is calculated using an option-pricing model. Compensation expense is recorded for restricted stock grants and units over their vesting periods based on fair value, which is equal to the market price of the Company’s common stock on the date of grant. Compensation expense for strategic performance shares is recorded over the performance period. For strategic performance shares with payment dependent on market condition, fair value is determined at the grant date using a Monte Carlo simulation model and not subsequently adjusted regardless of the final outcome. For strategic performance shares with payment dependent on performance conditions, expense is initially accrued based on the most likely outcome, but evaluated for adjustment each period for updates in the expected outcome. At the end of the performance period, expense is trued up to the actual outcome (number of shares awarded times the share price at the grant date).
T. Participating Business
The Company’s participating life insurance policies entitle policyholders to earn dividends that represent a portion of the earnings of the Company’s life insurance subsidiaries. Participating insurance accounted for approximately 1% of the Company’s total life insurance in force at the end of 2010 and 2009, and approximately 2% of the Company’s total life insurance in force at the end of 2008.
U. Income Taxes
The Company and its domestic subsidiaries file a consolidated United States federal income tax return. The Company’s foreign subsidiaries file tax returns in accordance with foreign law. U.S. taxation of these foreign subsidiaries may differ in timing and amount from taxation under foreign laws. Reportable amounts, including credits for foreign tax paid by these subsidiaries, are reflected in the U.S. tax return of the affiliates’ domestic parent.
The Company recognizes deferred income taxes when the financial statement and tax-based carrying values of assets and liabilities are different and recognizes deferred income tax liabilities on the unremitted earnings of foreign subsidiaries that are not permanently invested overseas. For subsidiaries whose earnings are considered permanently invested overseas, income taxes are accrued at the local foreign tax rate. The Company establishes valuation allowances against deferred tax assets if it is more likely than not that the deferred tax asset will not be realized. The need for a valuation allowance is determined based on the evaluation of various factors, including expectations of future earnings and management’s judgment. Note 20 contains detailed information about the Company’s income taxes.
The Company recognizes interim period income taxes by estimating an annual effective tax rate and applying it to year-to-date results. The estimated annual effective tax rate is periodically updated throughout the year based on actual results to date and an updated projection of full year income. Although the effective tax rate approach is generally used for interim periods, taxes on significant, unusual and infrequent items are recognized at the statutory tax rate entirely in the period the amounts are realized.
CIGNA CORPORATION – 2010 Form 10-K – 111
NOTE 3 Acquisitions and Dispositions
The Company may from time to time acquire or dispose of assets, subsidiaries or lines of business. Significant transactions are described below.
A. Reinsurance of Run-off Workers’ Compensation and Personal Accident Business
On December 31, 2010, the Company essentially exited from its workers’ compensation and personal accident reinsurance business by purchasing retrocessional coverage from a Bermuda subsidiary of Enstar Group Limited and transferring administration of this business to the reinsurer. Under the reinsurance agreement, CIGNA is indemnified for liabilities with respect to its workers’ compensation and personal accident reinsurance business to the extent that these liabilities do not exceed 190% of the December 31 net reserves. The Company believes that the risk of loss beyond this maximum aggregate is remote. The reinsurance arrangement is secured by assets held in trust. Cash consideration paid to the reinsurer was $190 million. The net effect of this transaction was an after-tax loss of $20 million ($31 million pre-tax), primarily reported in other operating expenses in the Run-off Reinsurance segment.
B. Sale of Workers’ Compensation and Case Management Business
On December 1, 2010 the Company completed the sale of its workers’ compensation and case management business to GENEX Holdings, Inc. The Company recognized an after-tax gain on sale of $11 million ($18 million pre-tax) which was reported in other revenues in the Disability and Life segment. Proceeds of the sale were received in preferred stock of GENEX Holdings, Inc., resulting in the Company becoming a minority shareholder in GENEX Holdings, Inc. This investment is classified in other long-term investments and accounted for using the equity method of accounting.
C. Acquisition of Vanbreda International
On August 31, 2010, the Company acquired 100% of the voting stock of Vanbreda International NV (Vanbreda International), based in Antwerp, Belgium for a cash purchase price of $412 million. Vanbreda International specializes in providing worldwide medical insurance and employee benefits to intergovernmental and non-governmental organizations, including international humanitarian operations, as well as corporate clients. Vanbreda International’s strong presence in Europe complements the Company’s position in providing expatriate benefits primarily to corporate clients in North America, as well as in Europe and Asia.
In accordance with GAAP, the total purchase price has been allocated to the tangible and intangible net assets acquired based on management’s estimates of their fair values. Accordingly, approximately $210 million was allocated to intangible assets, primarily customer relationships. The weighted average amortization period is 15 years. The condensed balance sheet at the acquisition date was as follows:
|
(In millions) | |
|
Investments |
$39 |
|
Cash and cash equivalents |
73 |
|
Premiums, accounts and notes receivable |
22 |
|
Property and equipment |
1 |
|
Deferred income taxes |
(71) |
|
Goodwill |
229 |
|
Other assets, including other intangibles |
220 |
|
Total assets acquired |
513 |
|
Accounts payable, accrued expenses and other liabilities |
101 |
|
Total liabilities acquired |
101 |
|
Net assets acquired |
$412 |
Goodwill is allocated to the International segment. For foreign tax purposes, the acquisition of Vanbreda International is being treated as a stock purchase. Accordingly, goodwill and other intangible assets will not be amortized for foreign tax purposes but may reduce the taxability of earnings repatriated to the U.S. by Vanbreda International.
The results of Vanbreda International are included in the Company’s Consolidated Financial Statements from the date of acquisition. The pro forma effect on total revenues and net income assuming the acquisition had occurred as of January 1, 2009 was not material to the Company’s total revenues and shareholders’ net income for the years ended December 31, 2010 or 2009.
CIGNA CORPORATION – 2010 Form 10-K – 112
D. Great-West Healthcare Acquisition
On April 1, 2008, the Company acquired the Healthcare division of Great-West Life and Annuity, Inc. (“Great-West Healthcare”) through 100% indemnity reinsurance agreements and the acquisition of certain affiliates and other assets and liabilities of Great-West Healthcare. The purchase price of approximately $1.5 billion consisted of a payment to the seller of approximately $1.4 billion for the net assets acquired and the assumption of net liabilities under the reinsurance agreement of approximately $0.1 billion. Great-West Healthcare primarily sells medical plans on a self-funded basis with stop loss coverage to select and regional employer groups. Great-West Healthcare’s offerings also include the following specialty products: stop loss, life, disability, medical, dental, vision, prescription drug coverage, and accidental death and dismemberment insurance. The acquisition, which was accounted for as a purchase, was financed through a combination of cash and the issuance of both short and long-term debt.
In accordance with the FASB’s guidance on accounting for business combinations, the Company completed its allocation of the total purchase price to the tangible and intangible net assets acquired based on management’s estimates of their fair values. Accordingly, approximately $290 million was allocated to intangible assets, primarily customer relationships and internal-use software. The weighted average amortization period was 9 years for customer relationships and 6 years for internal-use software. The remainder, net of tangible net assets acquired, was goodwill which approximated $1.1 billion and was allocated entirely to the Health Care segment. Substantially all of the goodwill is tax deductible and is being amortized over 15 years for federal income tax purposes.
NOTE 4 Earnings Per Share
Basic and diluted earnings per share were computed as follows:
|
(Dollars in millions, except per share amounts) |
Basic |
Effect of Dilution |
Diluted |
|
2010 | |||
|
Shareholders’ income from continuing operations |
$1,345 |
$- |
$1,345 |
|
Shares (in thousands): | |||
|
Weighted average |
272,866 |
- |
272,866 |
|
Common stock equivalents |
2,421 |
2,421 |
|
|
Total shares |
272,866 |
2,421 |
275,287 |
|
EPS |
$4.93 |
$(0.04) |
$4.89 |
|
2009 | |||
|
Shareholders’ income from continuing operations |
$1,301 |
$- |
$1,301 |
|
Shares (in thousands): | |||
|
Weighted average |
274,058 |
- |
274,058 |
|
Common stock equivalents |
1,299 |
1,299 |
|
|
Total shares |
274,058 |
1,299 |
275,357 |
|
EPS |
$4.75 |
$(0.02) |
$4.73 |
|
2008 | |||
|
Shareholders’ income from continuing operations |
$288 |
$- |
$288 |
|
Shares (in thousands): | |||
|
Weighted average |
277,317 |
- |
277,317 |
|
Common stock equivalents |
1,526 |
1,526 |
|
|
Total shares |
277,317 |
1,526 |
278,843 |
|
EPS |
$1.04 |
$(0.01) |
$1.03 |
As described in Note 2, effective in 2009, the Company adopted the FASB’s new guidance for determining participating securities which requires the Company’s unvested restricted stock awards to be included in weighted average shares instead of being considered a common stock equivalent and restated 2008 EPS.
CIGNA CORPORATION – 2010 Form 10-K – 113
The following outstanding employee stock options were not included in the computation of diluted earnings per share because their effect would have increased diluted earnings per share (antidilutive) as their exercise price was greater than the average share price of the Company’s common stock for the period.
|
(In millions) |
2010 |
2009 |
2008 |
|
Antidilutive options |
6.3 |
8.8 |
6.3 |
NOTE 5 Health Care Medical Claims Payable
Medical claims payable for the Health Care segment reflects estimates of the ultimate cost of claims that have been incurred but not yet reported, those which have been reported but not yet paid (reported claims in process) and other medical expense payable, which primarily comprises accruals for provider incentives and other amounts payable to providers. Incurred but not yet reported comprises the majority of the reserve balance as follows:
|
(In millions) |
2010 |
2009 |
|
Incurred but not yet reported |
$1,067 |
$790 |
|
Reported claims in process |
164 |
114 |
|
Other medical expense payable |
15 |
17 |
|
MEDICAL CLAIMS PAYABLE |
$1,246 |
$921 |
Activity in medical claims payable was as follows:
|
(In millions) |
2010 |
2009 |
2008 |
|
Balance at January 1, |
$921 |
$924 |
$975 |
|
Less: Reinsurance and other amounts recoverable |
206 |
211 |
258 |
|
Balance at January 1, net |
715 |
713 |
717 |
|
Acquired April 1, net |
- |
- |
90 |
|
Incurred claims related to: | |||
|
Current year |
8,663 |
6,970 |
7,312 |
|
Prior years |
(93) |
(43) |
(60) |
|
Total incurred |
8,570 |
6,927 |
7,252 |
|
Paid claims related to: | |||
|
Current year |
7,682 |
6,278 |
6,716 |
|
Prior years |
593 |
647 |
630 |
|
Total paid |
8,275 |
6,925 |
7,346 |
|
Balance at December 31, net |
1,010 |
715 |
713 |
|
Add: Reinsurance and other amounts recoverable |
236 |
206 |
211 |
|
Balance at December 31, |
$1,246 |
$921 |
$924 |
Reinsurance and other amounts recoverable reflect amounts due from reinsurers and policyholders to cover incurred but not reported and pending claims for minimum premium products and certain administrative services only business where the right of offset does not exist. See Note 8 for additional information on reinsurance. For the year ended December 31, 2010, actual experience differed from the Company’s key assumptions resulting in favorable incurred claims related to prior years’ medical claims payable of $93 million, or 1.3% of the current year incurred claims as reported for the year ended December 31, 2009. Actual completion factors resulted in a reduction in medical claims payable of $51 million, or 0.7% of the current year incurred claims as reported for the year ended December 31, 2009 for the insured book of business. Actual medical cost trend resulted in a reduction in medical claims payable of $42 million, or 0.6% of the current year incurred claims as reported for the year ended December 31, 2009 for the insured book of business.
For the year ended December 31, 2009, actual experience differed from the Company’s key assumptions, resulting in favorable incurred claims related to prior years’ medical claims payable of $43 million, or 0.6% of the current year incurred claims as reported for the year ended December 31, 2008. Actual completion factors resulted in a reduction of the medical claims payable of $21 million, or 0.3% of the current year incurred claims as reported for the year ended December 31, 2008 for the insured book of business. Actual medical cost trend resulted in a reduction of the medical claims payable of $22 million, or 0.3% of the current year incurred claims as reported for the year ended December 31, 2008 for the insured book of business.
CIGNA CORPORATION – 2010 Form 10-K – 114
The favorable impact in 2010 is primarily due to lower utilization levels that occurred in late 2009 and the release of the provision for moderately adverse conditions. This provision is a component of the assumptions for both completion factors and medical cost trend, established for claims incurred related to prior years. The release was substantially offset by the provision for moderately adverse conditions established for claims incurred related to the current year. The favorable impact in 2009 was primarily due to the release of the provision for moderately adverse conditions.
The corresponding impact of prior year development was an increase to shareholders’ net income of $26 million after-tax ($39 million pre-tax) for the year ended December 31, 2010 and was not material to shareholders’ net income for the year ended December 31, 2009. The change in the amount of the incurred claims related to prior years in the medical claims payable liability does not directly correspond to an increase or decrease in the Company’s shareholders’ net income recognized for the following reasons:
First, the Company consistently recognizes the actuarial best estimate of the ultimate liability within a level of confidence, as required by actuarial standards of practice, which require that the liabilities be adequate under moderately adverse conditions. As the Company establishes the liability for each incurral year, the Company ensures that its assumptions appropriately consider moderately adverse conditions. When a portion of the development related to the prior year incurred claims is offset by an increase determined appropriate to address moderately adverse conditions for the current year incurred claims, the Company does not consider that offset amount as having any impact on shareholders’ net income.
Second, while changes in reserves for the Company’s guaranteed cost products do directly affect shareholders’ net income, changes in reserves for the Company’s retrospectively experience-rated business do not always impact shareholders’ net income. For the Company’s retrospectively experience-rated business only adjustments to medical claims payable on accounts in deficit affect shareholders’ net income. An increase or decrease to medical claims payable on accounts in deficit, in effect, accrues to the Company and directly impacts shareholders’ net income. An account is in deficit when the accumulated medical costs and administrative charges, including profit charges, exceed the accumulated premium received. Adjustments to medical claims payable on accounts in surplus accrue directly to the policyholder with no impact on the Company’s shareholders’ net income. An account is in surplus when the accumulated premium received exceeds the accumulated medical costs and administrative charges, including profit charges.
NOTE 6 Initiatives to Lower Operating Expenses
As part of its strategy, the Company has undertaken several initiatives to realign its organization and consolidate support functions in an effort to increase efficiency and responsiveness to customers and to reduce costs.
During 2008 and 2009, the Company conducted a comprehensive review to reduce the operating expenses of its ongoing businesses (“cost reduction program”). As a result, the Company recognized severance-related and real estate charges in other operating expenses.
Severance charges in 2008 and 2009 resulted from reductions of approximately 2,350 positions in the Company’s workforce. Cost reduction activities associated with these charges are substantially complete as of December 31, 2010. In 2010, the Company recorded an incremental pre-tax charge of $6 million ($4 million after-tax) to reflect actual severance experience differing from prior assumptions.
CIGNA CORPORATION – 2010 Form 10-K – 115
Cost reduction activity for 2008, 2009 and 2010 was as follows:
|
Pre-tax (In millions) |
Severance |
Real Estate |
Total |
|
Fourth Quarter 2008 charge (balance carried to January 1, 2009) |
$44 |
$11 |
$55 |
|
Second Quarter |
14 |
- |
14 |
|
Third Quarter |
10 |
- |
10 |
|
Fourth Quarter |
20 |
- |
20 |
|
Subtotal — 2009 charges |
44 |
- |
44 |
|
Less: Payments |
55 |
3 |
58 |
|
Balance, December 31, 2009 |
33 |
8 |
41 |
|
Add: change in estimate to severance accrual |
6 |
- |
6 |
|
Less: 2010 Payments | |||
|
First Quarter |
10 |
1 |
11 |
|
Second Quarter |
8 |
5 |
13 |
|
Third Quarter |
7 |
1 |
8 |
|
Fourth Quarter |
5 |
1 |
6 |
|
Balance, December 31, 2010 |
$9 |
$- |
$9 |
The Health Care segment recorded substantially all of the 2010 charge, $37 million pre-tax ($24 million after-tax) of the 2009 charges and $44 million pre-tax ($27 million after-tax) of the 2008 charge. The remainder of the 2009 and 2008 charges were reported as follows: Disability and Life: $5 million pre-tax ($4 million after-tax) in 2009 and $3 million pre-tax ($2 million after-tax) in 2008; and International: $2 million pre-tax ($1 million after-tax) in 2009 and $8 million pre-tax ($6 million after-tax) in 2008. Substantially all severance is expected to be paid by the end of the second quarter of 2011.
NOTE 7 Guaranteed Minimum Death Benefit Contracts
The Company’s reinsurance operations, which were discontinued in 2000 and are now an inactive business in run-off mode, reinsured a guaranteed minimum death benefit (“GMDB”), also known as variable annuity death benefits (“VADBe”), under certain variable annuities issued by other insurance companies. These variable annuities are essentially investments in mutual funds combined with a death benefit. The Company has equity and other market exposures as a result of this product. In periods of declining equity markets and in periods of flat equity markets following a decline, the Company’s liabilities for these guaranteed minimum death benefits increase. Conversely, in periods of rising equity markets, the Company’s liabilities for these guaranteed minimum death benefits decrease.
In order to substantially reduce the equity market exposures relating to guaranteed minimum death benefit contracts, the Company operates a dynamic hedge program (“GMDB equity hedge program”), using exchange-traded futures contracts. The hedge program is designed to offset both positive and negative impacts of changes in equity markets on the GMDB liability. In addition, the Company uses foreign currency futures contracts to reduce the international equity market and foreign currency risks associated with this business. The hedge program involves detailed, daily monitoring of equity market movements and rebalancing the futures contracts within established parameters. While the hedge program is actively managed, it may not exactly offset changes in the GMDB liability due to, among other things, divergence between the performance of the underlying mutual funds and the hedge instruments, high levels of volatility in the equity markets, and differences between actual contractholder behavior and what is assumed. The performance of the underlying mutual funds compared to the hedge instruments is further impacted by a time lag, since the data is not reported and incorporated into the required hedge position on a real time basis. Although this hedge program does not qualify for GAAP hedge accounting, it is an economic hedge because it is designed to reduce and is effective in reducing equity market exposures resulting from this product. The results of the futures contracts are included in other revenue and amounts reflecting corresponding changes in liabilities for these GMDB contracts are included in benefits and expenses. The notional amount of futures contract positions held by the Company at December 31, 2010 was $0.9 billion. The Company recorded in other revenues pre-tax losses of $157 million in 2010 and $282 million in 2009, compared with pre-tax gains of $333 million in 2008 from these futures contracts.
In 2000, the Company determined that the GMDB reinsurance business was premium deficient because the recorded future policy benefit reserve was less than the expected present value of future claims and expenses less the expected present value of future premiums and investment income using revised assumptions based on actual and expected experience. The Company tests for premium deficiency by reviewing its reserve each quarter using current market conditions and its long-term assumptions. Under premium deficiency accounting, if the recorded reserve is determined insufficient, an increase to the reserve is reflected as a charge to current period income. Consistent with GAAP, the Company does not recognize gains on premium deficient long duration products.
CIGNA CORPORATION – 2010 Form 10-K – 116
The Company had future policy benefit reserves for GMDB contracts of $1.1 billion as of December 31, 2010, and $1.3 billion as of December 31, 2009. The determination of liabilities for GMDB requires the Company to make critical accounting estimates. The Company estimates its liabilities for GMDB exposures using a complex internal model run using many scenarios and based on assumptions regarding lapse, future partial surrenders, claim mortality (deaths that result in claims), interest rates (mean investment performance and discount rate) and volatility. Lapse refers to the full surrender of an annuity prior to a contractholder’s death. Future partial surrender refers to the fact that most contractholders have the ability to withdraw substantially all of their mutual fund investments while retaining the death benefit coverage in effect at the time of the withdrawal. Mean investment performance for underlying equity mutual funds refers to market rates expected to be earned on the hedging instruments over the life of the GMDB equity hedge program, and for underlying fixed income mutual funds refers to the expected market return over the life of the contracts. Market volatility refers to market fluctuation. These assumptions are based on the Company’s experience and future expectations over the long-term period, consistent with the long-term nature of this product. The Company regularly evaluates these assumptions and changes its estimates if actual experience or other evidence suggests that assumptions should be revised. If actual experience differs from the assumptions (including lapse, future partial surrenders, claim mortality, interest rates and volatility) used in estimating these liabilities, the result could have a material adverse effect on the Company’s consolidated results of operations, and in certain situations, could have a material adverse effect on the Company’s financial condition.
The following provides information about the Company’s reserving methodology and assumptions for GMDB as of December 31, 2010:
•
The reserves represent estimates of the present value of net amounts expected to be paid, less the present value of net future premiums. Included in net amounts expected to be paid is the excess of the guaranteed death benefits over the values of the contractholders’ accounts (based on underlying equity and bond mutual fund investments).
•
The reserves include an estimate for partial surrenders that essentially lock in the death benefit for a particular policy based on annual election rates that vary from 0 to 15% depending on the net amount at risk for each policy and whether surrender charges apply.
•
The assumed mean investment performance for the underlying equity mutual funds considers the Company’s GMDB equity hedge program using futures contracts, and is based on the Company’s view that short-term interest rates will average 5% over future periods, but considers that current short-term rates are less than 5%. The mean investment performance assumption for the underlying fixed income mutual funds (bonds and money market) is 5% based on a review of historical returns. The investment performance for underlying equity and fixed income mutual funds is reduced by fund fees ranging from 1 to 3% across all funds.
•
The volatility assumption is based on a review of historical monthly returns for each key index (e.g. S&P 500) over a period of at least ten years. Volatility represents the dispersion of historical returns compared to the average historical return (standard deviation) for each index. The assumption is 16% to 26%, varying by equity fund type; 4% to 10%, varying by bond fund type; and 2% for money market funds. These volatility assumptions are used along with the mean investment performance assumption to project future return scenarios.
•
The discount rate is 5.75%.
•
The claim mortality assumption is 65% to 89% of the 1994 Group Annuity Mortality table, with 1% annual improvement beginning January 1, 2000. The assumption reflects that for certain contracts, a spousal beneficiary is allowed to elect to continue a contract by becoming its new owner, thereby postponing the death claim rather than receiving the death benefit currently. For certain issuers of these contracts, the claim mortality assumption depends on age, gender, and net amount at risk for the policy.
•
The lapse rate assumption is 0% to 24%, depending on contract type, policy duration and the ratio of the net amount at risk to account value.
During 2010, the Company performed its periodic review of assumptions resulting in a charge of $52 million pre-tax ($34 million after-tax) to strengthen GMDB reserves. During 2010, current short-term interest rates had declined from the level anticipated at December 31, 2009, leading the Company to increase reserves. Interest rate risk is not covered by the GMDB equity hedge program discussed above. The Company also updated the lapse assumption for policies that have already taken or may take a significant partial withdrawal, which had a lesser reserve impact.
During 2009, the Company reported a charge of $73 million pre-tax ($47 million after-tax) to strengthen GMDB reserves. The reserve strengthening primarily reflected an increase in the provision for future partial surrenders due to market declines, adverse volatility-related impacts due to turbulent equity market conditions, and interest rate impacts.
During 2008, the Company recorded additional benefits expenses of $406 million pre-tax ($263 million after-tax) to strengthen GMDB reserves following an analysis of experience and reserve assumptions. The amounts were primarily due to adverse impacts of overall market declines of $210 million pre-tax ($136 million after-tax), adverse volatility-related impacts due to turbulent equity market conditions totaling $182 million pre-tax ($118 million after-tax) and adverse interest rate impacts of $14 million pre-tax ($9 million after-tax).
CIGNA CORPORATION – 2010 Form 10-K – 117
Activity in future policy benefit reserves for these GMDB contracts was as follows:
|
(In millions) |
2010 |
2009 |
2008 |
|
Balance at January 1, |
$1,285 |
$1,609 |
$848 |
|
Add: Unpaid Claims |
36 |
34 |
21 |
|
Less: Reinsurance and other amounts recoverable |
53 |
83 |
19 |
|
Balance at January 1, net |
1,268 |
1,560 |
850 |
|
Add: Incurred benefits |
(20) |
(122) |
822 |
|
Less: Paid benefits |
124 |
170 |
112 |
|
Ending balance, net |
1,124 |
1,268 |
1,560 |
|
Less: Unpaid Claims |
37 |
36 |
34 |
|
Add: Reinsurance and other amounts recoverable |
51 |
53 |
83 |
|
Balance at December 31, |
$1,138 |
$1,285 |
$1,609 |
Benefits paid and incurred are net of ceded amounts. Incurred benefits reflect the (favorable) or unfavorable impact of a rising or falling equity market on the liability, and include the charges discussed above. Losses or gains have been recorded in other revenues as a result of the GMDB equity hedge program to reduce equity market exposures.
The majority of the Company’s exposure arises under annuities that guarantee that the benefit received at death will be no less than the highest historical account value of the related mutual fund investments on a contractholder’s anniversary date. Under this type of death benefit, the Company is liable to the extent the highest historical anniversary account value exceeds the fair value of the related mutual fund investments at the time of a contractholder’s death. Other annuity designs that the Company reinsured guarantee that the benefit received at death will be:
•
the contractholder’s account value as of the last anniversary date (anniversary reset); or
•
no less than net deposits paid into the contract accumulated at a specified rate or net deposits paid into the contract.
The table below presents the account value, net amount at risk and average attained age of underlying contractholders for guarantees in the event of death, by type of benefit as of December 31. The net amount at risk is the death benefit coverage in force or the amount that the Company would have to pay if all contractholders died as of the specified date, and represents the excess of the guaranteed benefit amount over the fair value of the underlying mutual fund investments.
|
(Dollars in millions) |
2010 |
2009 |
|
Highest anniversary annuity value | ||
|
Account value |
$13,336 |
$13,890 |
|
Net amount at risk |
$4,372 |
$5,953 |
|
Average attained age of contractholders (weighted by exposure) |
70 |
69 |
|
Anniversary value reset | ||
|
Account value |
$1,396 |
$1,403 |
|
Net amount at risk |
$52 |
$113 |
|
Average attained age of contractholders (weighted by exposure) |
63 |
61 |
|
Other | ||
|
Account value |
$1,864 |
$1,918 |
|
Net amount at risk |
$755 |
$914 |
|
Average attained age of contractholders (weighted by exposure) |
69 |
68 |
|
Total | ||
|
Account value |
$16,596 |
$17,211 |
|
Net amount at risk |
$5,179 |
$6,980 |
|
Average attained age of contractholders (weighted by exposure) |
70 |
69 |
|
Number of contractholders (approx.) |
530,000 |
590,000 |
The Company has also written reinsurance contracts with issuers of variable annuity contracts that provide annuitants with certain guarantees related to minimum income benefits. All reinsured GMIB policies also have a GMDB benefit reinsured by the Company. See Note 11 for further information.
CIGNA CORPORATION – 2010 Form 10-K – 118
NOTE 8 Reinsurance
The Company’s insurance subsidiaries enter into agreements with other insurance companies to assume and cede reinsurance. Reinsurance is ceded primarily to limit losses from large exposures and to permit recovery of a portion of direct losses. Reinsurance is also used in acquisition and disposition transactions where the underwriting company is not being acquired. Reinsurance does not relieve the originating insurer of liability. The Company regularly evaluates the financial condition of its reinsurers and monitors its concentrations of credit risk.
Retirement benefits business
The Company had reinsurance recoverables of $1.7 billion as of December 31, 2010, and December 31, 2009 from Prudential Retirement Insurance and Annuity Company resulting from the 2004 sale of the retirement benefits business, which was primarily in the form of a reinsurance arrangement. The reinsurance recoverable, which is reduced as the Company’s reinsured liabilities are paid or directly assumed by the reinsurer, is secured primarily by fixed maturities equal to or greater than 100% of the reinsured liabilities. These fixed maturities are held in a trust established for the benefit of the Company. As of December 31, 2010, the fair value of trust assets exceeded the reinsurance recoverable.
Individual life and annuity reinsurance
The Company had reinsurance recoverables totaling $4.3 billion as of December 31, 2010 and $4.4 billion as of December 31, 2009 from The Lincoln National Life Insurance Company and Lincoln Life & Annuity of New York resulting from the 1998 sale of the Company’s individual life insurance and annuity business through indemnity reinsurance arrangements. At December 31, 2010, the $3.9 billion reinsurance recoverable from The Lincoln National Life Insurance Company was secured by assets held in a trust established for the benefit of the Company, and was less than the market value of the trust assets. The remaining recoverable from Lincoln Life & Annuity of New York of $402 million is currently unsecured, however if this reinsurer does not maintain a specified minimum credit or claims paying rating, it is required to fully secure the outstanding balance. As of December 31, 2010 both companies had ratings sufficient to avoid triggering a contractual obligation.
Other Ceded and Assumed Reinsurance
Ceded Reinsurance: Ongoing operations
The Company’s insurance subsidiaries have reinsurance recoverables from various reinsurance arrangements in the ordinary course of business for its Health Care, Disability and Life, and International segments as well as the corporate-owned life insurance business. Reinsurance recoverables of $282 million as of December 31, 2010 are expected to be collected from more than 70 reinsurers.
The Company reviews its reinsurance arrangements and establishes reserves against the recoverables in the event that recovery is not considered probable. As of December 31, 2010, the Company’s recoverables related to these segments were net of a reserve of $9 million.
Assumed and Ceded reinsurance: Run-off Reinsurance segment
The Company’s Run-off Reinsurance operations assumed risks related to GMDB contracts, GMIB contracts, workers’ compensation, and personal accident business. The Company’s Run-off Reinsurance operations also purchased retrocessional coverage to reduce the risk of loss on these contracts. In December 2010, the Company entered into reinsurance arrangements to transfer the remaining liabilities and administration of the workers’ compensation and personal accident businesses to a subsidiary of Enstar Group Limited. Under this arrangement, the new reinsurer also assumes the future risk of collection from prior reinsurers. See Note 3 for further details regarding this arrangement.
Liabilities related to GMDB, workers’ compensation and personal accident are included in future policy benefits and unpaid claims. Because the GMIB contracts are treated as derivatives under GAAP, the asset related to GMIB is recorded in the Other assets, including other intangibles caption and the liability related to GMIB is recorded in Accounts payable, accrued expenses, and other liabilities on the Company’s Consolidated Balance Sheets (see Notes 11 and 24 for additional discussion of the GMIB assets and liabilities).
The reinsurance recoverables for GMDB, workers’ compensation, and personal accident total $261 million as of December 31, 2010. Of this amount, approximately 77% are secured by assets in trust or letters of credit.
The Company reviews its reinsurance arrangements and establishes reserves against the recoverables in the event that recovery is not considered probable. As of December 31, 2010, the Company’s recoverables related to this segment were net of a reserve of $1 million.
CIGNA CORPORATION – 2010 Form 10-K – 119
The Company’s payment obligations for underlying reinsurance exposures assumed by the Company under these contracts are based on the ceding companies’ claim payments. For GMDB, claim payments vary because of changes in equity markets and interest rates, as well as mortality and contractholder behavior. Any of these claim payments can extend many years into the future, and the amount of the ceding companies’ ultimate claims, and therefore the amount of the Company’s ultimate payment obligations and corresponding ultimate collection from retrocessionaires, may not be known with certainty for some time.
Summary
The Company’s reserves for underlying reinsurance exposures assumed by the Company, as well as for amounts recoverable from reinsurers/retrocessionaires for both ongoing operations and the run-off reinsurance operation, are considered appropriate as of December 31, 2010, based on current information. However, it is possible that future developments could have a material adverse effect on the Company’s consolidated results of operations and, in certain situations, such as if actual experience differs from the assumptions used in estimating reserves for GMDB, could have a material adverse effect on the Company’s financial condition. The Company bears the risk of loss if its retrocessionaires do not meet or are unable to meet their reinsurance obligations to the Company.
In the Company’s Consolidated Income Statements, Premiums and fees were presented net of ceded premiums, and Total benefits and expenses were presented net of reinsurance recoveries, in the following amounts:
|
(In millions) |
2010 |
2009 |
2008 |
|
Premiums and Fees | |||
|
Short-duration contracts: | |||
|
Direct |
$16,611 |
$13,886 |
$13,969 |
|
Assumed |
496 |
1,076 |
1,221 |
|
Ceded |
(187) |
(192) |
(242) |
|
16,920 |
14,770 |
14,948 |
|
|
Long-duration contracts: | |||
|
Direct |
1,687 |
1,499 |
1,521 |
|
Assumed |
36 |
33 |
53 |
|
Ceded: | |||
|
Individual life insurance and annuity business sold |
(195) |
(209) |
(220) |
|
Other |
(55) |
(52) |
(49) |
|
1,473 |
1,271 |
1,305 |
|
|
TOTAL |
$18,393 |
$16,041 |
$16,253 |
|
Reinsurance recoveries | |||
|
Individual life insurance and annuity business sold |
$321 |
$322 |
$368 |
|
Other |
156 |
178 |
282 |
|
TOTAL |
$477 |
$500 |
$650 |
The decrease in assumed premiums in 2010 primarily reflects the effect of the Company’s exit from two large, non-strategic assumed government life insurance programs as well as the transfer of policies assumed in the acquisition of Great-West Healthcare directly to one of the Company’s insurance subsidiaries in 2010. The effects of reinsurance on written premiums and fees for short-duration contracts were not materially different from the recognized premium and fee amounts shown in the above table.
NOTE 9 Goodwill, Other Intangibles, and Property and Equipment
Goodwill primarily relates to the Health Care segment ($2.9 billion) and, to a lesser extent, the International segment ($240 million) and increased by approximately $230 million during 2010 as a result of the acquisition of Vanbreda International and foreign currency translation after the acquisition. The fair value of the Company’s reporting units is substantially in excess of their carrying value therefore the risk for future impairment is unlikely.
CIGNA CORPORATION – 2010 Form 10-K – 120
Other intangible assets were comprised of the following at December 31:
|
(Dollars in millions) |
Cost |
Accumulated Amortization |
Net Carrying Value |
Weighted Average Amortization Period (Years) |
|
2010 | ||||
|
Customer relationships |
$587 |
$277 |
$310 |
12 |
|
Other |
70 |
22 |
48 |
14 |
|
Total reported in other assets, including other intangibles |
657 |
299 |
358 |
|
|
Internal-use software reported in property and equipment |
1,379 |
875 |
504 |
5 |
|
TOTAL OTHER INTANGIBLE ASSETS |
$2,036 |
$1,174 |
$862 |
|
|
2009 | ||||
|
Customer relationships |
$386 |
$254 |
$132 |
9 |
|
Other |
46 |
12 |
34 |
10 |
|
Total reported in other assets, including other intangibles |
432 |
266 |
166 | |
|
Internal-use software reported in property and equipment |
1,168 |
692 |
476 |
4 |
|
TOTAL OTHER INTANGIBLE ASSETS |
$1,600 |
$958 |
$642 |
|
The increase in intangible assets in 2010 primarily relates to the acquisition of Vanbreda International.
Property and equipment was comprised of the following as of December 31:
|
(Dollars in millions) |
Cost |
Accumulated Amortization |
Net Carrying Value |
|
|
2010 | ||||
|
Internal-use software |
$1,379 |
$875 |
$504 |
|
|
Other property and equipment |
1,190 |
782 |
408 |
|
|
TOTAL PROPERTY AND EQUIPMENT |
$2,569 |
$1,657 |
$912 |
|
|
2009 | ||||
|
Internal-use software |
$1,168 |
$692 |
$476 |
|
|
Other property and equipment |
1,194 |
808 |
386 |
|
|
TOTAL PROPERTY AND EQUIPMENT |
$2,362 |
$1,500 |
$862 |
|
Depreciation and amortization was comprised of the following for the years ended December 31:
|
(Dollars in millions) |
2010 |
2009 |
2008 |
|
Internal-use software |
$161 |
$147 |
$143 |
|
Other property and equipment |
99 |
91 |
76 |
|
Depreciation and amortization of property and equipment |
260 |
238 |
219 |
|
Other intangibles |
32 |
30 |
25 |
|
TOTAL DEPRECIATION AND AMORTIZATION |
$292 |
$268 |
$244 |
The Company estimates annual pre-tax amortization for intangible assets, including internal-use software, over the next five calendar years to be as follows: $214 million in 2011, $179 million in 2012, $139 million in 2013, $84 million in 2014, and $53 million in 2015.
CIGNA CORPORATION – 2010 Form 10-K – 121
NOTE 10 Pension and Other Postretirement Benefit Plans
A. Pension and Other Postretirement Benefit Plans
The Company and certain of its subsidiaries provide pension, health care and life insurance defined benefits to eligible retired employees, spouses and other eligible dependents through various domestic and foreign plans. The effect of its foreign pension and other post retirement benefit plans is immaterial to the Company’s results of operations, liquidity and financial position. Effective July 1, 2009, the Company froze its primary domestic defined benefit pension plans. A curtailment of benefits occurred as a result of this action since it eliminated the accrual of benefits for the future service of active employees enrolled in these domestic pension plans. Accordingly, the Company recognized a pre-tax curtailment gain of $46 million ($30 million after-tax) in 2009.
The Company measures the assets and liabilities of its domestic pension and other postretirement benefit plans as of December 31. The following table summarizes the projected benefit obligations and assets related to the Company’s domestic and international pension and other postretirement benefit plans as of, and for the year ended, December 31:
|
(In millions) |
Pension Benefits |
Other Postretirement Benefits |
||
|
2010 |
2009 |
2010 |
2009 |
|
|
Change in benefit obligation | ||||
|
Benefit obligation, January 1 |
$4,363 |
$4,101 |
$419 |
$376 |
|
Service cost |
2 |
43 |
1 |
1 |
|
Interest cost |
240 |
250 |
22 |
24 |
|
Loss from past experience |
379 |
255 |
36 |
59 |
|
Benefits paid from plan assets |
(258) |
(247) |
(2) |
(4) |
|
Benefits paid - other |
(35) |
(30) |
(32) |
(37) |
|
Translation of foreign currencies |
— |
1 |
— |
— |
|
Amendments |
— |
5 |
— |
— |
|
Curtailment |
— |
(15) |
— |
— |
|
Benefit obligation, December 31 |
4,691 |
4,363 |
444 |
419 |
|
Change in plan assets | ||||
|
Fair value of plan assets, January 1 |
2,850 |
2,248 |
24 |
24 |
|
Actual return on plan assets |
357 |
436 |
1 |
2 |
|
Benefits paid |
(258) |
(247) |
(2) |
(2) |
|
Translation of foreign currencies |
— |
1 |
— |
— |
|
Contributions |
214 |
412 |
— |
— |
|
Fair value of plan assets, December 31 |
3,163 |
2,850 |
23 |
24 |
|
Funded Status |
$(1,528) |
$(1,513) |
$(421) |
$(395) |
The postretirement benefits liability adjustment included in accumulated other comprehensive loss consisted of the following as of December 31:
|
(In millions) |
Pension Benefits |
Other Postretirement Benefits |
||
|
2010 |
2009 |
2010 |
2009 |
|
|
Unrecognized net gain (loss) |
$(1,805) |
$(1,558) |
$(14) |
$22 |
|
Unrecognized prior service cost |
(5) |
(5) |
51 |
69 |
|
POSTRETIREMENT BENEFITS LIABILITY ADJUSTMENT |
$(1,810) |
$(1,563) |
$37 |
$91 |
CIGNA CORPORATION – 2010 Form 10-K – 122
During 2010, the Company’s postretirement benefits liability adjustment increased by $301 million pre-tax ($189 million after-tax) resulting in a decrease to shareholders’ equity. The increase in the liability was primarily due to a decrease in the discount rate, and an update to the mortality assumption to provide for mortality improvement, partially offset by 2010 investment returns in excess of expectations. As a result of the adoption of the Patient Protection and Affordable Care Act (“Health Care Reform”) in 2010, the Company has decided to discontinue its Medicare Advantage Private Fee for Service benefits for certain retirees effective in 2011. As a result, the postretirement benefits liability adjustment increased by $8 million after-tax at December 31, 2010. Although the adoption of Health Care Reform affects other aspects of the Company’s postretirement medical plan, their effects were not material to the Company’s results of operations or liquidity.
Pension benefits
The Company’s pension plans were underfunded by $1.5 billion in 2010 and 2009 and had related accumulated benefit obligations of $4.7 billion as of December 31, 2010 and $4.3 billion as of December 31, 2009.
The Company funds its qualified pension plans at least at the minimum amount required by the Employee Retirement Income Security Act of 1974 and the Pension Protection Act of 2006. For 2011, the Company expects to make minimum required and voluntary contributions totaling approximately $250 million. Future years’ contributions will ultimately be based on a wide range of factors including but not limited to asset returns, discount rates, and funding targets.
Components of net pension cost for the years ended December 31 were as follows:
|
(In millions) |
2010 |
2009 |
2008 |
|
Service cost |
$2 |
$43 |
$74 |
|
Interest cost |
240 |
250 |
242 |
|
Expected long-term return on plan assets |
(253) |
(239) |
(234) |
|
Amortization of: | |||
|
Net loss from past experience |
28 |
34 |
57 |
|
Prior service cost |
— |
(4) |
(11) |
|
Curtailment |
— |
(46) |
— |
|
NET PENSION COST |
$17 |
$38 |
$128 |
The Company expects to recognize pre-tax losses of $38 million in 2011 from amortization of past experience. This estimate is based on a weighted average amortization period for the frozen and inactive plans of approximately 30 years, as this period is now based on the average expected remaining life of plan participants.
Other postretirement benefits
Unfunded retiree health benefit plans had accumulated benefit obligations of $296 million at December 31, 2010, and $268 million at December 31, 2009. Retiree life insurance plans had accumulated benefit obligations of $148 million as of December 31, 2010 and $150 million as of December 31, 2009.
Components of net other postretirement benefit cost for the years ended December 31 were as follows:
|
(In millions) |
2010 |
2009 |
2008 |
|
Service cost |
$1 |
$1 |
$1 |
|
Interest cost |
22 |
24 |
24 |
|
Expected long-term return on plan assets |
(1) |
(1) |
(1) |
|
Amortization of: | |||
|
Net gain from past experience |
— |
(5) |
(8) |
|
Prior service cost |
(18) |
(18) |
(17) |
|
NET OTHER POSTRETIREMENT BENEFIT COST |
$4 |
$1 |
$(1) |
The Company expects to recognize in 2011 pre-tax gains of $16 million related to amortization of prior service cost and no pre-tax losses from amortization of past experience. The original amortization period is based on an average remaining service period of active employees associated with the other postretirement benefit plans of approximately 9 years. The weighted average remaining amortization period for prior service cost is approximately 3 years.
CIGNA CORPORATION – 2010 Form 10-K – 123
The estimated rate of future increases in the per capita cost of health care benefits is 8.5% in 2011, decreasing by 0.50% per year to 5% in 2018 and beyond. This estimate reflects the Company’s current claim experience and management’s estimate that rates of growth will decline in the future. A 1% increase or decrease in the estimated rate would change 2010 reported amounts as follows:
|
(In millions) |
Increase |
Decrease |
|
Effect on total service and interest cost |
$1 |
$1 |
|
Effect on postretirement benefit obligation |
$14 |
$13 |
Plan assets
The target investment allocation percentages (57% equity securities, 20% fixed income, 8% real estate and 15% other) are developed by management as guidelines, although the fair values of each asset category are expected to vary as a result of changes in market conditions. The pension plan asset portfolio has been most heavily weighted towards equity securities, consisting of domestic and international investments, in an effort to earn a higher rate of return on pension plan investments over the long-term payout period of the pension benefit obligations. The diversification of the pension plan assets into other investments is intended to mitigate the volatility in returns, while also providing adequate liquidity to fund benefit distributions.
As of December 31, 2010, pension plan assets included $2.8 billion invested in the separate accounts of Connecticut General Life Insurance Company (“CGLIC”) and Life Insurance Company of North America, which are subsidiaries of the Company, as well as an additional $0.4 billion invested directly in funds offered by the buyer of the retirement benefits business.
The fair values of plan assets by category and by hierarchy as defined by GAAP are as follows. See Note 11 for a definition of the levels within the fair value hierarchy.
|
December 31, 2010 (In millions) |
Quoted Prices in Active Markets for Identical Assets (Level 1) |
Significant Other Observable Inputs (Level 2) |
Significant Unobservable Inputs (Level 3) |
Total |
|
Plan assets at fair value: | ||||
|
Fixed maturities: | ||||
|
Federal government and agency |
$— |
$8 |
$— |
$8 |
|
Corporate |
— |
158 |
24 |
182 |
|
Mortgage and other asset-backed |
— |
4 |
— |
4 |
|
Fund investments and pooled separate accounts (1) |
— |
372 |
2 |
374 |
|
TOTAL FIXED MATURITIES |
— |
542 |
26 |
568 |
|
Equity securities: | ||||
|
Domestic |
1,445 |
— |
20 |
1,465 |
|
International, including funds and pooled separate accounts (1) |
208 |
218 |
— |
426 |
|
TOTAL EQUITY SECURITIES |
1,653 |
218 |
20 |
1,891 |
|
Real estate, including pooled separate accounts (1) |
— |
— |
240 |
240 |
|
Securities partnerships |
— |
— |
347 |
347 |
|
Guaranteed deposit account contract |
— |
— |
24 |
24 |
|
Cash equivalents |
— |
93 |
— |
93 |
|
TOTAL PLAN ASSETS AT FAIR VALUE |
$1,653 |
$853 |
$657 |
$3,163 |
|
(1) A pooled separate account has several participating benefit plans and each owns a share of the total pool of investments. |
||||
CIGNA CORPORATION – 2010 Form 10-K – 124
|
December 31, 2009 (In millions) |
Quoted Prices in Active Markets for Identical Assets (Level 1) |
Significant Other Observable Inputs (Level 2) |
Significant Unobservable Inputs (Level 3) |
Total |
|
Plan assets at fair value: | ||||
|
Fixed maturities: | ||||
|
Federal government and agency |
$— |
$6 |
$— |
$6 |
|
Corporate |
— |
114 |
26 |
140 |
|
Mortgage and other asset-backed |
— |
22 |
— |
22 |
|
Fund investments and pooled separate accounts (1) |
— |
300 |
118 |
418 |
|
TOTAL FIXED MATURITIES |
— |
442 |
144 |
586 |
|
Equity securities: | ||||
|
Domestic |
1,341 |
1 |
23 |
1,365 |
|
International, including funds and pooled separate accounts (1) |
171 |
195 |
— |
366 |
|
TOTAL EQUITY SECURITIES |
1,512 |
196 |
23 |
1,731 |
|
Real estate, including pooled separate accounts (1) |
— |
— |
160 |
160 |
|
Securities partnerships |
— |
— |
257 |
257 |
|
Guaranteed deposit account contract |
— |
— |
29 |
29 |
|
Cash equivalents |
— |
87 |
— |
87 |
|
TOTAL PLAN ASSETS AT FAIR VALUE |
$1,512 |
$725 |
$613 |
$2,850 |
|
(1) A pooled separate account has several participating benefit plans and each owns a share of the total pool of investments. |
||||
Plan assets in Level 1 include exchange-listed equity securities. Level 2 assets primarily include:
•
fixed income and international equity funds priced using their daily net asset value which is the exit price; and
•
fixed maturities valued using recent trades of similar securities or pricing models as described below.
Because many fixed maturities do not trade daily, fair values are often derived using recent trades of securities with similar features and characteristics. When recent trades are not available, pricing models are used to determine these prices. These models calculate fair values by discounting future cash flows at estimated market interest rates. Such market rates are derived by calculating the appropriate spreads over comparable U.S. Treasury securities, based on the credit quality, industry and structure of the asset.
Plan assets classified in Level 3 include securities partnerships and equity real estate generally valued based on the pension plan’s ownership share of the equity of the investee including changes in the fair values of its underlying investments. In addition, as of December 31, 2009, investments in pooled separate accounts principally invested in equity real estate and fixed income funds that are priced using the net asset value are classified in Level 3 due to restrictions on withdrawal.
The following table summarizes the changes in pension plan assets classified in Level 3 for the years ended December 31, 2010 and December 31, 2009. Actual return on plan assets in this table may include changes in fair value that are attributable to both observable and unobservable inputs.
|
(In millions) |
Fixed Maturities |
Equity Securities |
Mortgage Loans & Real Estate |
Securities Partnerships |
Guaranteed |
Total |
|
Balance at January 1, 2010 |
$144 |
$23 |
$160 |
$257 |
$29 |
$613 |
|
Actual return on plan assets: | ||||||
|
Assets still held at the reporting date |
(14) |
(1) |
16 |
53 |
2 |
56 |
|
Assets sold during the period |
14 |
— |
— |
— |
— |
14 |
|
Total actual return on plan assets |
— |
(1) |
16 |
53 |
2 |
70 |
|
Purchases, sales, settlements, net |
(121) |
2 |
64 |
37 |
(7) |
(25) |
|
Transfers into Level 3 |
6 |
— |
— |
— |
— |
6 |
|
Transfers out of Level 3 |
(3) |
(4) |
— |
— |
— |
(7) |
|
Balance at December 31, 2010 |
$26 |
$20 |
$240 |
$347 |
$24 |
$657 |
CIGNA CORPORATION – 2010 Form 10-K – 125
|
(In millions) |
Fixed Maturities |
Equity Securities |
Real Estate |
Securities Partnerships |
Guaranteed |
Total |
|
Balance at January 1, 2009 |
$31 |
$14 |
$208 |
$264 |
$32 |
$549 |
|
Actual return on plan assets: | ||||||
|
Assets still held at the reporting date |
8 |
— |
(104) |
(31) |
8 |
(119) |
|
Assets sold during the period |
5 |
— |
— |
— |
— |
5 |
|
Total actual return on plan assets |
13 |
— |
(104) |
(31) |
8 |
(114) |
|
Purchases, sales, settlements, net |
(75) |
9 |
56 |
24 |
(11) |
3 |
|
Transfers into Level 3 |
175 |
— |
— |
— |
— |
175 |
|
Balance at December 31, 2009 |
$144 |
$23 |
$160 |
$257 |
$29 |
$613 |
The assets related to other postretirement benefit plans are invested in deposit funds with interest credited based on fixed income investments in the general account of CGLIC. As there are significant unobservable inputs used in determining the fair value of these assets, they are classified as Level 3. During 2010, these assets earned a return of $1 million, offset by a net withdrawal from the fund of $2 million, while during 2009, they earned a return of $2 million, offset by a net withdrawal of $2 million.
Assumptions for pension and other postretirement benefit plans
Management determined the present value of the projected benefit obligation and the accumulated other postretirement benefit obligation and related benefit costs based on the following weighted average assumptions as of and for the years ended December 31:
|
2010 |
2009 |
|
|
Discount rate: | ||
|
Pension benefit obligation |
5.00% |
5.50% |
|
Other postretirement benefit obligation |
4.75% |
5.25% |
|
Pension benefit cost |
5.50% |
6.25% |
|
Other postretirement benefit cost |
5.25% |
6.25% |
|
Expected long-term return on plan assets: | ||
|
Pension benefit cost |
8.00% |
8.00% |
|
Other postretirement benefit cost |
5.00% |
5.00% |
|
Expected rate of compensation increase: | ||
|
Projected pension benefit obligation |
— |
3.50% |
|
Pension benefit cost |
— |
3.50% |
|
Other postretirement benefit obligation |
3.00% |
3.00% |
|
Other postretirement benefit cost |
3.00% |
3.00% |
Discount rates are set by applying actual annualized yields at various durations from the Citigroup Pension Liability curve, without adjustment, to the expected cash flows of the postretirement benefits liabilities. The Company believes that the Citigroup Pension Liability curve is the most representative curve to use because it is derived from a broad array of bonds in various industries throughout the domestic market for high quality bonds. Further, Citigroup monitors the bond portfolio to ensure that only high quality issues are included. Accordingly, the Company does not believe that any adjustment is required to the Citigroup curve.
Expected long-term rates of return on plan assets were developed considering actual long-term historical returns, expected long-term market conditions, plan asset mix and management’s investment strategy, which includes a significant allocation of domestic and foreign equity securities. Expected long-term market conditions take into consideration certain key macroeconomic trends including expected domestic and foreign GDP growth, employment levels and inflation. Based on the Company’s current outlook, the expected return assumption is considered reasonable. Actual and target investment allocations are very similar at December 31, 2010.
CIGNA CORPORATION – 2010 Form 10-K – 126
To measure pension costs, the Company uses a market-related asset valuation for domestic pension plan assets invested in non-fixed income investments. The market-related value of pension assets recognizes the difference between actual and expected long-term returns in the portfolio over 5 years , a method that reduces the short-term impact of market fluctuations. At December 31, 2010, the market-related asset value was approximately $3.4 billion compared with a market value of approximately $3.2 billion.
Benefit payments
The following benefit payments, including expected future services, are expected to be paid in:
|
(In millions) |
Pension Benefits |
Other Postretirement Benefits |
|
|
Gross |
Net of Medicare |
||
|
2011 |
$507 |
$45 |
$41 |
|
2012 |
$342 |
$42 |
$40 |
|
2013 |
$328 |
$42 |
$40 |
|
2014 |
$332 |
$41 |
$39 |
|
2015 |
$321 |
$40 |
$38 |
|
2016-2020 |
$1,579 |
$179 |
$172 |
B. 401(k) Plans
The Company sponsors a 401(k) plan in which the Company matches a portion of employees’ pre-tax contributions. Another 401(k) plan with an employer match was frozen in 1999. Participants in the active plan may invest in a fund that invests in the Company’s common stock, several diversified stock funds, a bond fund and a fixed-income fund. In conjunction with the action to freeze the domestic defined benefit pension plans, effective January 1, 2010, the Company increased its matching contributions to 401(k) plan participants.
The Company may elect to increase its matching contributions if the Company’s annual performance meets certain targets. A substantial amount of the Company’s matching contributions are invested in the Company’s common stock. The Company’s expense for these plans was $69 million for 2010, $36 million for 2009 and $34 million for 2008.
NOTE 11 Fair Value Measurements
The Company carries certain financial instruments at fair value in the financial statements including fixed maturities, equity securities, short-term investments and derivatives. Other financial instruments are measured at fair value under certain conditions, such as when impaired.
Fair value is defined as the price at which an asset could be exchanged in an orderly transaction between market participants at the balance sheet date. A liability’s fair value is defined as the amount that would be paid to transfer the liability to a market participant, not the amount that would be paid to settle the liability with the creditor.
Fair values are based on quoted market prices when available. When market prices are not available, fair value is generally estimated using discounted cash flow analyses, incorporating current market inputs for similar financial instruments with comparable terms and credit quality. In instances where there is little or no market activity for the same or similar instruments, the Company estimates fair value using methods, models and assumptions that the Company believes a hypothetical market participant would use to determine a current transaction price. These valuation techniques involve some level of estimation and judgment by the Company which becomes significant with increasingly complex instruments or pricing models.
The Company’s financial assets and liabilities carried at fair value have been classified based upon a hierarchy defined by GAAP. The hierarchy gives the highest ranking to fair values determined using unadjusted quoted prices in active markets for identical assets and liabilities (Level 1) and the lowest ranking to fair values determined using methodologies and models with unobservable inputs (Level 3). An asset’s or a liability’s classification is based on the lowest level of input that is significant to its measurement. For example, a financial asset or liability carried at fair value would be classified in Level 3 if unobservable inputs were significant to the instrument’s fair value, even though the measurement may be derived using inputs that are both observable (Levels 1 and 2) and unobservable (Level 3).
CIGNA CORPORATION – 2010 Form 10-K – 127
The Company performs ongoing analyses of prices used to value the Company’s invested assets to determine that they represent appropriate estimates of fair value. This process involves quantitative and qualitative analysis including reviews of pricing methodologies, judgments of valuation inputs, the significance of any unobservable inputs, pricing statistics and trends. The Company also performs sample testing of sales values to confirm the accuracy of prior fair value estimates.
Financial Assets and Financial Liabilities Carried at Fair Value
The following tables provide information as of December 31, 2010 and December 31, 2009 about the Company’s financial assets and liabilities carried at fair value. Similar disclosures for separate account assets, which are also recorded at fair value on the Company’s Consolidated Balance Sheets, are provided separately as gains and losses related to these assets generally accrue directly to policyholders. In addition, Note 10 contains similar disclosures for the Company’s pension plan assets.
|
December 31, 2010 (In millions) |
Quoted Prices in Active Markets for Identical Assets (Level 1) |
Significant Other Observable Inputs (Level 2) |
Significant Unobservable Inputs (Level 3) |
Total |
|
Financial assets at fair value: | ||||
|
Fixed maturities: | ||||
|
Federal government and agency |
$133 |
$550 |
$4 |
$687 |
|
State and local government |
— |
2,467 |
— |
2,467 |
|
Foreign government |
— |
1,152 |
17 |
1,169 |
|
Corporate |
— |
9,252 |
380 |
9,632 |
|
Federal agency mortgage-backed |
— |
10 |
— |
10 |
|
Other mortgage-backed |
— |
85 |
3 |
88 |
|
Other asset-backed |
— |
161 |
495 |
656 |
|
Total fixed maturities (1) |
133 |
13,677 |
899 |
14,709 |
|
Equity securities |
6 |
87 |
34 |
127 |
|
Subtotal |
139 |
13,764 |
933 |
14,836 |
|
Short-term investments |
— |
174 |
— |
174 |
|
GMIB assets (2) |
— |
— |
480 |
480 |
|
Other derivative assets (3) |
— |
19 |
— |
19 |
|
TOTAL FINANCIAL ASSETS AT FAIR VALUE, EXCLUDING SEPARATE ACCOUNTS |
$139 |
$13,957 |
$1,413 |
$15,509 |
|
Financial liabilities at fair value: | ||||
|
GMIB liabilities |
$— |
$— |
$903 |
$903 |
|
Other derivative liabilities (3) |
— |
32 |
— |
32 |
|
TOTAL FINANCIAL LIABILITIES AT FAIR VALUE |
$— |
$32 |
$903 |
$935 |
|
(1) Fixed maturities include $443 million of net appreciation required to adjust future policy benefits for the run-off settlement annuity business including $74 million of appreciation for securities classified in Level 3. (2) The GMIB assets represent retrocessional contracts in place from two external reinsurers which cover 55% of the exposures on these contracts. The assets are net of a liability of $15 million for the future cost of reinsurance. (3) Other derivative assets include $16 million of interest rate and foreign currency swaps qualifying as cash flow hedges and $3 million of interest rate swaps not designated as accounting hedges. Other derivative liabilities reflect foreign currency and interest rate swaps qualifying as cash flow hedges. See Note 13 for additional information. |
||||
CIGNA CORPORATION – 2010 Form 10-K – 128
|
December 31, 2009 (In millions) |
Quoted Prices in Active Markets for Identical Assets (Level 1) |
Significant Other Observable Inputs (Level 2) |
Significant Unobservable Inputs (Level 3) |
Total |
|
Financial assets at fair value: | ||||
|
Fixed maturities: | ||||
|
Federal government and agency |
$43 |
$527 |
$1 |
$571 |
|
State and local government |
— |
2,521 |
— |
2,521 |
|
Foreign government |
— |
1,056 |
14 |
1,070 |
|
Corporate |
— |
8,241 |
344 |
8,585 |
|
Federal agency mortgage-backed |
— |
34 |
— |
34 |
|
Other mortgage-backed |
— |
114 |
7 |
121 |
|
Other asset-backed |
— |
92 |
449 |
541 |
|
Total fixed maturities (1) |
43 |
12,585 |
815 |
13,443 |
|
Equity securities |
2 |
81 |
30 |
113 |
|
Subtotal |
45 |
12,666 |
845 |
13,556 |
|
Short-term investments |
— |
493 |
— |
493 |
|
GMIB assets (2) |
— |
— |
482 |
482 |
|
Other derivative assets (3) |
— |
16 |
— |
16 |
|
TOTAL FINANCIAL ASSETS AT FAIR VALUE, EXCLUDING SEPARATE ACCOUNTS |
$45 |
$13,175 |
$1,327 |
$14,547 |
|
Financial liabilities at fair value: |
|
|
|
|
|
GMIB liabilities |
$— |
$— |
$903 |
$903 |
|
Other derivative liabilities (3) |
— |
30 |
— |
30 |
|
TOTAL FINANCIAL LIABILITIES AT FAIR VALUE |
$— |
$30 |
$903 |
$933 |
|
(1) Fixed maturities include $274 million of net appreciation required to adjust future policy benefits for the run-off settlement annuity business including $38 million of appreciation for securities classified in Level 3. (2) The GMIB assets represent retrocessional contracts in place from two external reinsurers which cover 55% of the exposures on these contracts. The assets are net of a liability of $15 million for the future cost of reinsurance. (3) Other derivative assets include $12 million of interest rate and foreign currency swaps qualifying as cash flow hedges and $4 million of interest rate swaps not designated as accounting hedges. Other derivative liabilities reflect foreign currency and interest rate swaps qualifying as cash flow hedges. See Note 13 for additional information. |
||||
Level 1 Financial Assets
Inputs for instruments classified in Level 1 include unadjusted quoted prices for identical assets in active markets accessible at the measurement date. Active markets provide pricing data for trades occurring at least weekly and include exchanges and dealer markets.
Assets in Level 1 include actively-traded U.S. government bonds and exchange-listed equity securities. Given the narrow definition of Level 1 and the Company’s investment asset strategy to maximize investment returns, a relatively small portion of the Company’s investment assets are classified in this category.
Level 2 Financial Assets and Financial Liabilities
Inputs for instruments classified in Level 2 include quoted prices for similar assets or liabilities in active markets, quoted prices from those willing to trade in markets that are not active, or other inputs that are market observable or can be corroborated by market data for the term of the instrument. Such other inputs include market interest rates and volatilities, spreads and yield curves. An instrument is classified in Level 2 if the Company determines that unobservable inputs are insignificant.
CIGNA CORPORATION – 2010 Form 10-K – 129
Fixed maturities and equity securities. Approximately 93% of the Company’s investments in fixed maturities and equity securities are classified in Level 2 including most public and private corporate debt and equity securities, federal agency and municipal bonds, non-government asset and mortgage-backed securities and preferred stocks. Because many fixed maturities and preferred stocks do not trade daily, fair values are often derived using recent trades of securities with similar features and characteristics. When recent trades are not available, pricing models are used to determine these prices. These models calculate fair values by discounting future cash flows at estimated market interest rates. Such market rates are derived by calculating the appropriate spreads over comparable U.S. Treasury securities, based on the credit quality, industry and structure of the asset. Typical inputs and assumptions to pricing models include, but are not limited to, a combination of benchmark yields, reported trades, issuer spreads, liquidity, benchmark securities, bids, offers, reference data, and industry and economic events. For mortgage-backed securities, inputs and assumptions may also include characteristics of the issuer, collateral attributes, prepayment speeds and credit rating.
Nearly all of these instruments are valued using recent trades or pricing models. Less than 1% of the fair value of investments classified in Level 2 represents foreign bonds that are valued, consistent with local market practice, using a single unadjusted market-observable input derived by averaging multiple broker-dealer quotes.
Short-term investments are carried at fair value, which approximates cost. On a regular basis the Company compares market prices for these securities to recorded amounts to validate that current carrying amounts approximate exit prices. The short-term nature of the investments and corroboration of the reported amounts over the holding period support their classification in Level 2.
Other derivatives classified in Level 2 represent over-the-counter instruments such as interest rate and foreign currency swap contracts. Fair values for these instruments are determined using market observable inputs including forward currency and interest rate curves and widely published market observable indices. Credit risk related to the counterparty and the Company is considered when estimating the fair values of these derivatives. However, the Company is largely protected by collateral arrangements with counterparties, and determined that no adjustment for credit risk was required as of December 31, 2010 or December 31, 2009. The nature and use of these other derivatives are described in Note 13.
Level 3 Financial Assets and Financial Liabilities
Certain inputs for instruments classified in Level 3 are unobservable (supported by little or no market activity) and significant to their resulting fair value measurement. Unobservable inputs reflect the Company’s best estimate of what hypothetical market participants would use to determine a transaction price for the asset or liability at the reporting date.
The Company classifies certain newly issued, privately placed, complex or illiquid securities, as well as assets and liabilities relating to GMIB, in Level 3.
Fixed maturities and equity securities. Approximately 6% of fixed maturities and equity securities are priced using significant unobservable inputs and classified in this category, including:
|
(In millions) |
December 31, 2010 |
December 31, 2009 |
|
Other asset and mortgage-backed securities — valued using pricing models |
$498 |
$456 |
|
Corporate and government bonds — valued using pricing models |
328 |
288 |
|
Corporate bonds — valued at transaction price |
73 |
71 |
|
Equity securities — valued at transaction price |
34 |
30 |
|
TOTAL |
$933 |
$845 |
Fair values of mortgage and asset-backed securities and corporate bonds are determined using pricing models that incorporate the specific characteristics of each asset and related assumptions including the investment type and structure, credit quality, industry and maturity date in comparison to current market indices, spreads and liquidity of assets with similar characteristics. For mortgage and asset-backed securities, inputs and assumptions to pricing may also include collateral attributes and prepayment speeds. Recent trades in the subject security or similar securities are assessed when available, and the Company may also review published research, as well as the issuer’s financial statements, in its evaluation. Certain subordinated corporate bonds and private equity investments are valued at transaction price in the absence of market data indicating a change in the estimated fair values.
CIGNA CORPORATION – 2010 Form 10-K – 130
Guaranteed minimum income benefit contracts. Because cash flows of the GMIB liabilities and assets are affected by equity markets and interest rates but are without significant life insurance risk and are settled in lump sum payments, the Company reports these liabilities and assets as derivatives at fair value. The Company estimates the fair value of the assets and liabilities for GMIB contracts using assumptions regarding capital markets (including market returns, interest rates and market volatilities of the underlying equity and bond mutual fund investments), future annuitant behavior (including mortality, lapse, and annuity election rates), and non-performance risk, as well as risk and profit charges. As certain assumptions (primarily related to future annuitant behavior) used to estimate fair values for these contracts are largely unobservable, the Company classifies GMIB assets and liabilities in Level 3. The Company considered the following in determining the view of a hypothetical market participant:
•
that the most likely transfer of these assets and liabilities would be through a reinsurance transaction with an independent insurer having a market capitalization and credit rating similar to that of the Company; and
•
that because this block of contracts is in run-off mode, an insurer looking to acquire these contracts would have similar existing contracts with related administrative and risk management capabilities.
These GMIB assets and liabilities are calculated with a complex internal model using many scenarios to determine the fair value of net amounts estimated to be paid, less the fair value of net future premiums estimated to be received, adjusted for risk and profit charges that the Company anticipates a hypothetical market participant would require to assume this business. Net amounts estimated to be paid represent the excess of the anticipated value of the income benefits over the values of the annuitants’ accounts at the time of annuitization. Generally, market return, interest rate and volatility assumptions are based on market observable information. Assumptions related to annuitant behavior reflect the Company’s belief that a hypothetical market participant would consider the actual and expected experience of the Company as well as other relevant and available industry resources in setting policyholder behavior assumptions. The significant assumptions used to value the GMIB assets and liabilities as of December 31, 2010 were as follows:
•
The market return and discount rate assumptions are based on the market-observable LIBOR swap curve.
•
The projected interest rate used to calculate the reinsured income benefits is indexed to the 7-year Treasury Rate at the time of annuitization (claim interest rate) based on contractual terms. That rate was 2.71% at December 31, 2010 and must be projected for future time periods. These projected rates vary by economic scenario and are determined by an interest rate model using current interest rate curves and the prices of instruments available in the market including various interest rate caps and zero-coupon bonds. For a subset of the business, there is a contractually guaranteed floor of 3% for the claim interest rate.
•
The market volatility assumptions for annuitants’ underlying mutual fund investments that are modeled based on the S&P 500, Russell 2000 and NASDAQ Composite are based on the market-implied volatility for these indices for three to seven years grading to historical volatility levels thereafter. For the remaining 54% of underlying mutual fund investments modeled based on other indices (with insufficient market-observable data), volatility is based on the average historical level for each index over the past 10 years. Using this approach, volatility ranges from 17% to 31% for equity funds, 4% to 12% for bond funds, and 1% to 2% for money market funds.
•
The mortality assumption is 70% of the 1994 Group Annuity Mortality table, with 1% annual improvement beginning January 1, 2000.
•
The annual lapse rate assumption reflects experience that differs by the company issuing the underlying variable annuity contracts, ranges from 2% to 17% at December 31, 2010, and depends on the time since contract issue and the relative value of the guarantee.
•
The annual annuity election rate assumption reflects experience that differs by the company issuing the underlying variable annuity contracts and depends on the annuitant’s age, the relative value of the guarantee and whether a contractholder has had a previous opportunity to elect the benefit. Immediately after the expiration of the waiting period, the assumed probability that an individual will annuitize their variable annuity contract is up to 80%. For the second and subsequent annual opportunities to elect the benefit, the assumed probability of election is up to 30%. Actual data is still emerging for the Company as well as the industry and the estimates are based on this limited data.
•
The nonperformance risk adjustment is incorporated by adding an additional spread to the discount rate in the calculation of both (1) the GMIB liability to reflect a hypothetical market participant’s view of the risk of the Company not fulfilling its GMIB obligations, and (2) the GMIB asset to reflect a hypothetical market participant’s view of the reinsurers’ credit risk, after considering collateral. The estimated market-implied spread is company-specific for each party involved to the extent that company-specific market data is available and is based on industry averages for similarly rated companies when company-specific data is not available. The spread is impacted by the credit default swap spreads of the specific parent companies, adjusted to reflect subsidiaries’ credit ratings relative to their parent company and any available collateral. The additional spread over LIBOR incorporated into the discount rate ranged from 5 to 110 basis points for the GMIB liability and from 10 to 85 basis points for the GMIB reinsurance asset for that portion of the interest rate curve most relevant to these policies.
•
The risk and profit charge assumption is based on the Company’s estimate of the capital and return on capital that would be required by a hypothetical market participant.
CIGNA CORPORATION – 2010 Form 10-K – 131
The Company regularly evaluates each of the assumptions used in establishing these assets and liabilities by considering how a hypothetical market participant would set assumptions at each valuation date. Capital markets assumptions are expected to change at each valuation date reflecting currently observable market conditions. Other assumptions may also change based on a hypothetical market participant’s view of actual experience as it emerges over time or other factors that impact the net liability. If the emergence of future experience or future assumptions differs from the assumptions used in estimating these assets and liabilities, the resulting impact could be material to the Company’s consolidated results of operations, and in certain situations, could be material to the Company’s financial condition.
GMIB liabilities are reported in the Company’s Consolidated Balance Sheets in Accounts payable, accrued expenses and other liabilities. GMIB assets associated with these contracts represent net receivables in connection with reinsurance that the Company has purchased from two external reinsurers and are reported in the Company’s Consolidated Balance Sheets in Other assets, including other intangibles.
Changes in Level 3 Financial Assets and Financial Liabilities Carried at Fair Value
The following tables summarize the changes in financial assets and financial liabilities classified in Level 3 for the years ended December 31, 2010 and 2009. These tables exclude separate account assets as changes in fair values of these assets accrue directly to policyholders. Gains and losses reported in this table may include changes in fair value that are attributable to both observable and unobservable inputs.
|
(In millions) |
Fixed Maturities & Equity Securities |
GMIB Assets |
GMIB Liabilities |
GMIB Net |
|
Balance at 1/1/2010 |
$845 |
$482 |
$(903) |
$(421) |
|
Gains (losses) included in income: | ||||
|
GMIB fair value gain/(loss) |
— |
57 |
(112) |
(55) |
|
Other |
27 |
— |
— |
— |
|
Total gains (losses) included in shareholders’ net income |
27 |
57 |
(112) |
(55) |
|
Gains included in other comprehensive income |
10 |
— |
— |
— |
|
Gains required to adjust future policy benefits for settlement annuities (1) |
34 |
— |
— |
— |
|
Purchases, issuances, settlements, net |
(74) |
(59) |
112 |
53 |
|
Transfers into/(out of) Level 3: | ||||
|
Transfers into Level 3 |
155 |
— |
— |
— |
|
Transfers out of Level 3 |
(64) |
— |
— |
— |
|
Total transfers into/(out of) Level 3 |
91 |
— |
— |
— |
|
Balance at 12/31/2010 |
$933 |
$480 |
$(903) |
$(423) |
|
Total gains (losses) included in shareholders’ net income attributable to instruments held at the reporting date |
$18 |
$57 |
$(112) |
$(55) |
|
(1) Amounts do not accrue to shareholders. |
||||
CIGNA CORPORATION – 2010 Form 10-K – 132
|
(In millions) |
Fixed Maturities & Equity Securities |
GMIB Assets |
GMIB Liabilities |
GMIB Net |
|
Balance at 1/1/2009 |
$889 |
$953 |
$(1,757) |
$(804) |
|
Gains (losses) included in income: | ||||
|
GMIB fair value gain/(loss) |
— |
(365) |
669 |
304 |
|
Other |
(18) |
— |
— |
— |
|
Total gains (losses) included in shareholders’ net income |
(18) |
(365) |
669 |
304 |
|
Gains included in other comprehensive income |
59 |
— |
— |
— |
|
Losses required to adjust future policy benefits for settlement annuities (1) |
(72) |
— |
— |
— |
|
Purchases, issuances, settlements, net |
(29) |
(106) |
185 |
79 |
|
Transfers into/(out of) Level 3: | ||||
|
Transfers into Level 3 |
276 |
— |
— |
— |
|
Transfers out of Level 3 |
(260) |
— |
— |
— |
|
Total transfers into/(out of) Level 3 |
16 |
— |
— |
— |
|
Balance at 12/31/2009 |
$845 |
$482 |
$(903) |
$(421) |
|
Total gains (losses) included in shareholders’ net income attributable to instruments held at the reporting date |
$(20) |
$(365) |
$669 |
$304 |
|
(1) Amounts do not accrue to shareholders. |
||||
As noted in the tables above, total gains and losses included in net income are reflected in the following captions in the Consolidated Statements of Income:
•
Realized investment gains (losses) and net investment income for amounts related to fixed maturities and equity securities; and
•
GMIB fair value (gain) loss for amounts related to GMIB assets and liabilities.
Reclassifications impacting Level 3 financial instruments are reported as transfers in or out of the Level 3 category as of the beginning of the quarter in which the transfer occurs. Therefore gains and losses in income only reflect activity for the quarters the instrument was classified in Level 3.
Transfers into or out of the Level 3 category occur when unobservable inputs, such as the Company’s best estimate of what a market participant would use to determine a current transaction price, become more or less significant to the fair value measurement. For the years ended December 31, 2010 and 2009, transfer activity between Level 3 and Level 2 primarily reflects changes in the level of unobservable inputs used to value certain private corporate bonds, principally related to credit risk of the issuers.
The Company provided reinsurance for other insurance companies that offer a guaranteed minimum income benefit, and then retroceded a portion of the risk to other insurance companies. These arrangements with third-party insurers are the instruments still held at the reporting date for GMIB assets and liabilities in the table above. Because these reinsurance arrangements remain in effect at the reporting date, the Company has reflected the total gain or loss for the period as the total gain or loss included in income attributable to instruments still held at the reporting date. However, the Company reduces the GMIB assets and liabilities resulting from these reinsurance arrangements when annuitants lapse, die, elect their benefit, or reach the age after which the right to elect their benefit expires.
Under FASB’s guidance for fair value measurements, the Company’s GMIB assets and liabilities are expected to be volatile in future periods because the underlying capital markets assumptions will be based largely on market-observable inputs at the close of each reporting period including interest rates and market-implied volatilities.
GMIB fair value losses of $55 million for 2010, were primarily due to declining interest rates, partially offset by increases in underlying account values resulting from favorable equity and bond fund returns, which resulted in decreased exposures.
GMIB fair value gains of $304 million for 2009, were primarily due to increases in interest rates and increases in underlying account values in the period resulting from favorable equity market and bond fund returns, resulting in reduced exposures. These favorable effects were partially offset by updates to the annuitization assumption (to assume that a greater percentage of contractholders will annuitize) and updates to the lapse assumption.
CIGNA CORPORATION – 2010 Form 10-K – 133
Separate account assets
Fair values and changes in the fair values of separate account assets generally accrue directly to the policyholders and are excluded from the Company’s revenues and expenses. As of December 31, 2010 and December 31, 2009 separate account assets were as follows:
|
December 31, 2010 (In millions) |
Quoted Prices in Active Markets for Identical Assets (Level 1) |
Significant Other Observable Inputs (Level 2) |
Significant |
Total |
|
Guaranteed separate accounts (See Note 24) |
$286 |
$1,418 |
$— |
$1,704 |
|
Non-guaranteed separate accounts (1) |
1,947 |
3,663 |
594 |
6,204 |
|
TOTAL SEPARATE ACCOUNT ASSETS |
$2,233 |
$5,081 |
$594 |
$7,908 |
|
(1) Non-guaranteed separate accounts include $2.8 billion in assets supporting the Company’s pension plan, including $557 million classified in Level 3. |
||||
|
December 31, 2009 (In millions) |
Quoted Prices in Active Markets for Identical Assets (Level 1) |
Significant Other Observable Inputs (Level 2) |
Significant (Level 3) |
Total |
|
Guaranteed separate accounts (See Note 24) |
$275 |
$1,480 |
$— |
$1,755 |
|
Non-guaranteed separate accounts (1) |
1,883 |
3,100 |
550 |
5,533 |
|
TOTAL SEPARATE ACCOUNT ASSETS |
$2,158 |
$4,580 |
$550 |
$7,288 |
|
(1) Non-guaranteed separate accounts include $2.6 billion in assets supporting the Company’s pension plan, including $517 million classified in Level 3. |
||||
Separate account assets in Level 1 include exchange-listed equity securities. Level 2 assets primarily include:
•
corporate and structured bonds valued using recent trades of similar securities or pricing models that discount future cash flows at estimated market interest rates as described above; and
•
actively-traded institutional and retail mutual fund investments and separate accounts priced using the daily net asset value which is the exit price.
Separate account assets classified in Level 3 include investments primarily in securities partnerships and real estate generally valued based on the separate account’s ownership share of the equity of the investee including changes in the fair values of its underlying investments. In addition, in 2009, certain fixed income funds priced using their net asset values are classified in Level 3 due to restrictions on their withdrawal.
The following tables summarize the change in separate account assets reported in Level 3 for the years ended December 31, 2010 and 2009.
|
(In millions) | |
|
Balance at 1/1/2010 |
$550 |
|
Policyholder gains (1) |
71 |
|
Purchases, issuances, settlements, net |
(10) |
|
Transfers into/(out of) Level 3: | |
|
Transfers into Level 3 |
9 |
|
Transfers out of Level 3 |
(26) |
|
Total transfers into/(out of) Level 3: |
(17) |
|
Balance at 12/31/2010 |
$594 |
|
(1) Included in this amount are gains of $53 million attributable to instruments still held at the reporting date. |
|
CIGNA CORPORATION – 2010 Form 10-K – 134
|
(In millions) | |
|
Balance at 1/1/2009 |
$475 |
|
Policyholder losses (1) |
(86) |
|
Purchases, issuances, settlements, net |
4 |
|
Transfers into/(out of) Level 3: | |
|
Transfers into Level 3 |
176 |
|
Transfers out of Level 3 |
(19) |
|
Total transfers into/(out of) Level 3: |
157 |
|
Balance at 12/31/2009 |
$550 |
|
(1) Included in this amount are losses of $92 million attributable to instruments still held at the reporting date. |
|
For the year ended December 31, 2009, transfers into Level 3 primarily represented fixed income funds that are priced using the net asset value where restrictions were placed on withdrawal.
Assets and Liabilities Measured at Fair Value under Certain Conditions
Some financial assets and liabilities are not carried at fair value each reporting period, but may be measured using fair value only under certain conditions, such as investments in commercial mortgage loans and real estate entities when they become impaired. During 2010, impaired commercial mortgage loans with carrying values of $158 million were written down to their fair values of $134 million, resulting in pre-tax realized investment losses of $24 million. Also during 2010, impaired real estate entities carried at cost of $35 million were written down to their fair values of $21 million, resulting in pre-tax realized investment losses of $14 million.
During 2009, impaired commercial mortgage loans with carrying values of $143 million were written down to their fair values of $126 million, resulting in pre-tax realized investment losses of $17 million. Also during 2009, impaired real estate entities with carrying values of $48 million were written down to their fair values of $12 million, resulting in pre-tax realized investment losses of $36 million.
These fair values were calculated by discounting the expected future cash flows at estimated market interest rates. Such market rates were derived by calculating the appropriate spread over comparable U.S. Treasury rates, based on the characteristics of the underlying collateral, including the type, quality and location of the assets. The fair value measurements were classified in Level 3 because these cash flow models incorporate significant unobservable inputs.
Fair Value Disclosures for Financial Instruments Not Carried at Fair Value
Most financial instruments that are subject to fair value disclosure requirements are carried in the Company’s Consolidated Financial Statements at amounts that approximate fair value. The following table provides the fair values and carrying values of the Company’s financial instruments not recorded at fair value that are subject to fair value disclosure requirements at December 31, 2010 and December 31, 2009.
|
(In millions) |
December 31, 2010 |
December 31, 2009 |
||
|
Fair Value |
Carrying Value |
Fair Value |
Carrying Value |
|
|
Commercial mortgage loans |
$3,470 |
$3,486 |
$3,323 |
$3,522 |
|
Contractholder deposit funds, excluding universal life products |
$1,001 |
$989 |
$940 |
$941 |
|
Long-term debt, including current maturities, excluding capital leases |
$2,926 |
$2,709 |
$2,418 |
$2,427 |
The fair values presented in the table above have been estimated using market information when available. The following is a description of the valuation methodologies and inputs used by the Company to determine fair value.
CIGNA CORPORATION – 2010 Form 10-K – 135
Commercial mortgage loans. The Company estimates the fair value of commercial mortgage loans generally by discounting the contractual cash flows at estimated market interest rates that reflect the Company’s assessment of the credit quality of the loans. Market interest rates are derived by calculating the appropriate spread over comparable U.S. Treasury rates, based on the property type, quality rating and average life of the loan. The quality ratings reflect the relative risk of the loan, considering debt service coverage, the loan-to-value ratio and other factors. Fair values of impaired mortgage loans are based on the estimated fair value of the underlying collateral generally determined using an internal discounted cash flow model.
Contractholder deposit funds, excluding universal life products. Generally, these funds do not have stated maturities. Approximately 45% of these balances can be withdrawn by the customer at any time without prior notice or penalty. The fair value for these contracts is the amount estimated to be payable to the customer as of the reporting date, which is generally the carrying value. Most of the remaining contractholder deposit funds are reinsured by the buyers of the individual life insurance and annuity and retirement benefits businesses. The fair value for these contracts is determined using the fair value of these buyers’ assets supporting these reinsured contracts. The Company had a reinsurance recoverable equal to the carrying value of these reinsured contracts.
Long-term debt, including current maturities, excluding capital leases. The fair value of long-term debt is based on quoted market prices for recent trades. When quoted market prices are not available, fair value is estimated using a discounted cash flow analysis and the Company’s estimated current borrowing rate for debt of similar terms and remaining maturities.
Fair values of off-balance sheet financial instruments were not material.
NOTE 12 Investments
A. Fixed Maturities and Equity Securities
Securities in the following table are included in fixed maturities and equity securities on the Company’s Consolidated Balance Sheets. These securities are carried at fair value with changes in fair value reported in other realized investment gains (losses) and interest and dividends reported in net investment income. The Company’s hybrid investments include certain preferred stock or debt securities with call or conversion features.
|
(In millions) |
2010 |
2009 |
|
Included in fixed maturities: | ||
|
Trading securities (amortized cost: $3; $8) |
$3 |
$8 |
|
Hybrid securities (amortized cost: $45; $37) |
52 |
43 |
|
TOTAL |
$55 |
$51 |
|
Included in equity securities: | ||
|
Hybrid securities (amortized cost: $108; $109) |
$86 |
$81 |
Fixed maturities included $98 million at December 31, 2010 and $197 million at December 31, 2009, which were pledged as collateral to brokers as required under certain futures contracts. These fixed maturities were primarily corporate securities.
The following information about fixed maturities excludes trading and hybrid securities. The amortized cost and fair value by contractual maturity periods for fixed maturities were as follows at December 31, 2010:
|
(In millions) |
Amortized Cost |
Fair Value |
|
Due in one year or less |
$776 |
$789 |
|
Due after one year through five years |
4,509 |
4,804 |
|
Due after five years through ten years |
4,835 |
5,256 |
|
Due after ten years |
2,619 |
3,052 |
|
Mortgage and other asset-backed securities |
658 |
753 |
|
TOTAL |
$13,397 |
$14,654 |
Actual maturities could differ from contractual maturities because issuers may have the right to call or prepay obligations, with or without penalties. Also, in some cases the Company may extend maturity dates.
CIGNA CORPORATION – 2010 Form 10-K – 136
Gross unrealized appreciation (depreciation) on fixed maturities by type of issuer is shown below (excluding trading securities and hybrid securities with a fair value of $55 million at December 31, 2010 and $51 million at December 31, 2009).
|
(In millions) |
December 31, 2010 |
|||
|
Amortized Cost |
Unrealized Appreciation |
Unrealized Depreciation |
Fair Value |
|
|
Federal government and agency |
$459 |
$229 |
$(1) |
$687 |
|
State and local government |
2,305 |
172 |
(10) |
2,467 |
|
Foreign government |
1,109 |
64 |
(4) |
1,169 |
|
Corporate |
8,866 |
761 |
(49) |
9,578 |
|
Federal agency mortgage-backed |
9 |
1 |
— |
10 |
|
Other mortgage-backed |
80 |
10 |
(3) |
87 |
|
Other asset-backed |
569 |
99 |
(12) |
656 |
|
TOTAL |
$13,397 |
$1,336 |
$(79) |
$14,654 |
|
(In millions) |
December 31, 2009 |
|||
|
Amortized Cost |
Unrealized Appreciation |
Unrealized Depreciation |
Fair Value |
|
|
Federal government and agency |
$398 |
$174 |
$(1) |
$571 |
|
State and local government |
2,341 |
188 |
(8) |
2,521 |
|
Foreign government |
1,040 |
38 |
(8) |
1,070 |
|
Corporate |
8,104 |
529 |
(98) |
8,535 |
|
Federal agency mortgage-backed |
33 |
1 |
— |
34 |
|
Other mortgage-backed |
125 |
5 |
(10) |
120 |
|
Other asset-backed |
494 |
55 |
(8) |
541 |
|
TOTAL |
$12,535 |
$990 |
$(133) |
$13,392 |
The above table includes investments with a fair value of $2.5 billion supporting the Company’s run-off settlement annuity business, with gross unrealized appreciation of $476 million and gross unrealized depreciation of $33 million at December 31, 2010. Such unrealized amounts are required to support future policy benefit liabilities of this business and, as such, are not included in accumulated other comprehensive income. At December 31, 2009, investments supporting this business had a fair value of $2.3 billion, gross unrealized appreciation of $326 million and gross unrealized depreciation of $52 million.
As of December 31, 2010, the Company had commitments to purchase $14 million of fixed maturities bearing interest at a fixed market rate.
Review of declines in fair value
Management reviews fixed maturities with a decline in fair value from cost for impairment based on criteria that include:
•
length of time and severity of decline;
•
financial health and specific near term prospects of the issuer;
•
changes in the regulatory, economic or general market environment of the issuer’s industry or geographic region; and
•
the Company’s intent to sell or the likelihood of a required sale prior to recovery.
CIGNA CORPORATION – 2010 Form 10-K – 137
Excluding trading and hybrid securities, as of December 31, 2010, fixed maturities with a decline in fair value from amortized cost (which were primarily investment grade corporate bonds) were as follows, including the length of time of such decline:
|
(Dollars in millions) |
December 31, 2010 |
|||
|
Fair Value |
Amortized Cost |
Unrealized Depreciation |
Number of Issues |
|
|
Fixed maturities: | ||||
|
One year or less: | ||||
|
Investment grade |
$957 |
$988 |
$(31) |
311 |
|
Below investment grade |
$104 |
$108 |
$(4) |
64 |
|
More than one year: | ||||
|
Investment grade |
$296 |
$334 |
$(38) |
63 |
|
Below investment grade |
$40 |
$46 |
$(6) |
17 |
As of December 31, 2010, the unrealized depreciation of investment grade fixed maturities is primarily due to increases in market yields since purchase.
B. Commercial Mortgage Loans
Mortgage loans held by the Company are made exclusively to commercial borrowers and are diversified by property type, location and borrower. Loans are secured by high quality, primarily completed and substantially leased operating properties and are generally carried at unpaid principal balances and are issued at a fixed rate of interest.
At December 31, commercial mortgage loans were distributed among the following property types and geographic regions:
|
(In millions) |
2010 |
2009 |
|
Property type | ||
|
Office buildings |
$1,043 |
$1,101 |
|
Apartment buildings |
835 |
901 |
|
Industrial |
619 |
551 |
|
Hotels |
533 |
499 |
|
Retail facilities |
418 |
426 |
|
Other |
38 |
44 |
|
TOTAL |
$3,486 |
$3,522 |
|
Geographic region | ||
|
Pacific |
$931 |
$965 |
|
South Atlantic |
752 |
735 |
|
New England |
585 |
566 |
|
Central |
519 |
518 |
|
Middle Atlantic |
385 |
408 |
|
Mountain |
314 |
330 |
|
TOTAL |
$3,486 |
$3,522 |
At December 31, 2010, scheduled commercial mortgage loan maturities were as follows (in millions): $518 in 2011, $547 in 2012, $612 in 2013, $274 in 2014 and $1,535 thereafter. Actual maturities could differ from contractual maturities for several reasons: borrowers may have the right to prepay obligations, with or without prepayment penalties: the maturity date may be extended; and loans may be refinanced.
As of December 31, 2010, the Company had commitments to extend credit under commercial mortgage loan agreements of $63 million that were diversified by property type and geographic region.
CIGNA CORPORATION – 2010 Form 10-K – 138
Credit Quality
The Company applies a consistent and disciplined approach to evaluating and monitoring credit risk, beginning with the initial underwriting of a mortgage loan and continuing throughout the investment holding period. Mortgage origination professionals employ an internal rating system developed from the Company’s experience in real estate investing and mortgage lending. A quality rating, designed to evaluate the relative risk of the transaction, is assigned at each loan’s origination and is updated each year as part of the annual portfolio loan review. The Company monitors credit quality on an ongoing basis, classifying each loan as a loan in good standing, potential problem loan or problem loan.
Quality ratings are based on internal evaluations of each loan’s specific characteristics considering a number of key inputs, including real estate market-related factors such as rental rates and vacancies, and property-specific inputs such as growth rate assumptions and lease rollover statistics. However, the two most significant contributors to the credit quality rating are the debt service coverage and loan-to-value ratios. The debt service coverage ratio measures the amount of property cash flow available to meet annual interest and principal payments on debt. A debt service coverage ratio below 1.0 indicates that there is not enough cash flow to cover the loan payments. The loan-to-value ratio, commonly expressed as a percentage, compares the amount of the loan to the fair value of the underlying property collateralizing the loan. Based on property valuations and cash flows estimated as part of the most recent annual review completed in July, 2010, and considering updates for loans where material changes were subsequently identified, the portfolio’s aggregate debt service coverage ratio was 1.38 and loan-to-value ratio was 74% as of December 31, 2010. As of December 31, 2009, the portfolio’s aggregate debt service coverage ratio was 1.48 and loan-to-value ratio was 77%.
The following table summarizes the credit risk profile of the Company’s commercial mortgage loan portfolio based on loan-to-value and debt service coverage ratios, as of December 31, 2010:
|
Loan-to-Value Ratios (Dollars in millions) |
Debt Service Coverage Ratio |
Total |
||||
|
1.30x or Greater |
1.20x to 1.29x |
1.10x to 1.19x |
1.00x to 1.09x |
Less than 1.00x |
||
|
Below 50% |
$324 |
$— |
$— |
$— |
$29 |
$353 |
|
50% to 59% |
409 |
54 |
56 |
— |
— |
519 |
|
60% to 69% |
533 |
73 |
5 |
28 |
25 |
664 |
|
70% to 79% |
138 |
79 |
57 |
55 |
11 |
340 |
|
80% to 89% |
267 |
186 |
165 |
151 |
69 |
838 |
|
90% to 99% |
15 |
54 |
181 |
185 |
135 |
570 |
|
100% or above |
— |
— |
47 |
43 |
112 |
202 |
|
TOTAL |
$1,686 |
$446 |
$511 |
$462 |
$381 |
$3,486 |
The Company’s annual in-depth review of its commercial mortgage loan investments is the primary mechanism for identifying emerging risks in the portfolio. This review is performed by the Company’s investment professionals and includes an analysis of each underlying property’s most recent annual financial statements, rent rolls, operating plans, budgets, a physical inspection of the property and other pertinent factors. Based on historical results, current leases, lease expirations and rental conditions in each market, the Company estimates the current year and future stabilized property income and fair value, and categorizes the investments as loans in good standing, potential problem loans or problem loans. Quality ratings are adjusted between annual reviews if new property information is received or events such as delinquency or a borrower request for restructure cause management to believe that the Company’s estimate of financial performance, fair value or the risk profile of the underlying property has been impacted.
Potential problem mortgage loans are considered current (no payment more than 59 days past due), but exhibit certain characteristics that increase the likelihood of future default. The characteristics management considers include, but are not limited to, the deterioration of debt service coverage below 1.0, estimated loan-to-value ratios increasing to 100% or more, downgrade in quality rating and request from the borrower for restructuring. In addition, loans are considered potential problems if principal or interest payments are past due by more than 30 but less than 60 days. Problem mortgage loans are either in default by 60 days or more or have been restructured as to terms, which could include concessions on interest rate, principal payment or maturity date. The Company monitors each problem and potential problem mortgage loan on an ongoing basis, and updates the loan categorization and quality rating when warranted.
Problem and potential problem mortgage loans totaled $383 million at December 31, 2010 and $397 million at December 31, 2009, with no significant concentrations by property type or geographic region in either year.
CIGNA CORPORATION – 2010 Form 10-K – 139
Impaired Commercial Mortgage Loans
A commercial mortgage loan is considered impaired when it is probable that the Company will not collect all amounts due (principal and interest) according to the terms of the original loan agreement. The Company assesses each loan individually for impairment, utilizing the information obtained from the quality review process discussed above. Impaired loans are carried at the lower of unpaid principal balance or the fair value of the underlying collateral. Certain commercial mortgage loans without valuation reserves are considered impaired because the Company will not collect all interest due according to the terms of the original agreements; however, the Company does expect to recover their remaining carrying value primarily because it is less than the fair value of the underlying property.
As of December 31, the carrying value of the Company’s impaired commercial mortgage loans and related valuation reserves were as follows:
|
(In millions) |
2010 |
2009 |
|||||
|
Gross |
Reserves |
Net |
Gross |
Reserves |
Net |
||
|
Impaired commercial mortgage loans with valuation reserves |
$47 |
$(12) |
$35 |
$143 |
$(17) |
$126 |
|
|
Impaired commercial mortgage loans with no valuation reserves |
60 |
— |
60 |
96 |
— |
96 |
|
|
TOTAL |
$107 |
$(12) |
$95 |
|
$239 |
$(17) |
$222 |
During 2010, the Company recorded a $24 million pre-tax ($15 million after-tax) increase in valuation reserves on impaired commercial mortgage loans primarily due to decreased valuations of certain office properties collateralizing the loans. The average recorded investment in impaired loans was $169 million during 2010 and $116 million during 2009. The Company recognizes interest income on problem mortgage loans only when payment is actually received because of the risk profile of the underlying investment. Interest income that would have been reflected in net income if interest on non-accrual commercial mortgage loans had been received in accordance with the original terms was not significant for 2010 or 2009. Interest income on impaired commercial mortgage loans was not significant for 2010 or 2009.
The following table summarizes the changes in valuation reserves for commercial mortgage loans:
|
(In millions) |
2010 |
2009 |
|
Reserve balance, January 1, |
$17 |
$— |
|
Increase in valuation reserves |
24 |
17 |
|
Charge-offs upon sales and repayments, net of recoveries |
(12) |
— |
|
Transfers to foreclosed real estate |
(17) |
— |
|
RESERVE BALANCE, DECEMBER 31, |
$12 |
$17 |
C. Real Estate
As of December 31, 2010 and 2009, real estate investments consisted primarily of office and industrial buildings in California. Investments with a carrying value of $49 million as of December 31, 2010 and $55 million as of December 31, 2009 were non-income producing during the preceding twelve months. As of December 31, 2010, the Company had commitments to contribute additional equity of $11 million to real estate investments.
D. Other Long-term Investments
As of December 31, other long-term investments consisted of the following:
|
(In millions) |
2010 |
2009 |
|
Real estate entities |
$394 |
$289 |
|
Securities partnerships |
288 |
272 |
|
Interest rate and foreign currency swaps |
19 |
16 |
|
Mezzanine loans |
13 |
13 |
|
Other |
45 |
5 |
|
TOTAL |
$759 |
$595 |
CIGNA CORPORATION – 2010 Form 10-K – 140
Investments in real estate entities and securities partnerships with a carrying value of $169 million at December 31, 2010 and $121 million at December 31, 2009 were non-income producing during the preceding twelve months.
As of December 31, 2010, the Company had commitments to contribute:
•
$224 million to limited liability entities that hold either real estate or loans to real estate entities that are diversified by property type and geographic region; and
•
$297 million to entities that hold securities diversified by issuer and maturity date.
The Company expects to disburse approximately 55% of the committed amounts in 2011.
E. Short-Term Investments and Cash Equivalents
Short-term investments and cash equivalents included corporate securities of $1.1 billion, federal government securities of $137 million and money market funds of $40 million as of December 31, 2010. The Company’s short-term investments and cash equivalents as of December 31, 2009 included corporate securities of $624 million, federal government securities of $402 million and money market funds of $104 million.
F. Concentration of Risk
As of December 31, 2010 and 2009, the Company did not have a concentration of investments in a single issuer or borrower exceeding 10% of shareholders’ equity.
CIGNA CORPORATION – 2010 Form 10-K – 141
NOTE 13 Derivative Financial Instruments
The Company uses derivative financial instruments primarily as part of a strategy to reduce the equity market exposures relating to guaranteed minimum death benefit contracts. Derivative financial instruments are also used by the Company as a part of its investment strategy to manage the characteristics of investment assets (such as duration, yield, currency and liquidity) to meet the varying demands of the related insurance and contractholder liabilities (such as paying claims, investment returns and withdrawals). Derivatives are typically used under this strategy to minimize interest rate and foreign currency risks. The Company routinely monitors exposure to credit risk associated with derivatives and diversifies the portfolio among approved dealers of high credit quality to minimize this risk. In addition, the Company has written or sold contracts to guarantee minimum income benefits.
The Company uses hedge accounting when derivatives are designated, qualify and are highly effective as hedges. Effectiveness is formally assessed and documented at inception and each period throughout the life of a hedge using various quantitative methods appropriate for each hedge, including regression analysis and dollar offset. Under hedge accounting, the changes in fair value of the derivative and the hedged risk are generally recognized together and offset each other when reported in shareholders’ net income.
The Company accounts for derivative instruments as follows:
•
Derivatives are reported on the balance sheet at fair value with changes in fair values reported in shareholders’ net income or accumulated other comprehensive income.
•
Changes in the fair value of derivatives that hedge market risk related to future cash flows — and that qualify for hedge accounting — are reported in a separate caption in accumulated other comprehensive income. These hedges are referred to as cash flow hedges.
•
A change in the fair value of a derivative instrument may not always equal the change in the fair value of the hedged item; this difference is referred to as hedge ineffectiveness. Where hedge accounting is used, the Company reflects hedge ineffectiveness in shareholders’ net income (generally as part of realized investment gains and losses).
Certain of the Company’s over-the-counter derivative instruments contain provisions requiring either the Company or the counterparty to post collateral depending on the amount of the net liability position and predefined financial strength or credit rating thresholds. The collateral posting requirements vary by counterparty. The aggregate fair value of derivative instruments with such credit-risk-related contingent features where the Company was in a net liability position was $25 million at December 31, 2010 and $29 million at December 31, 2009 for which the Company was not required to post collateral with its counterparties. If the various contingent features underlying the agreements were triggered as of the balance sheet date, the Company would be required to post collateral equal to the total net liability. The Company is a party to certain other derivative instruments that contain termination provisions for which the counterparties could demand immediate payment of the total net liability position if the financial strength rating of the Company were to decline below specified levels. As of December 31, 2010 and 2009, there was no net liability position under such derivative instruments.
See Note 7 for a discussion of derivatives associated with GMDB contracts and Note 11 for a discussion of derivatives arising from GMIB contracts. The effects of other derivatives were not material to the Company’s consolidated results of operations, liquidity or financial condition for the years ended December 31, 2010 and 2009.
The following tables present information about the nature and accounting treatment of the Company’s primary derivative financial instruments including the Company’s purpose for entering into specific derivative transactions, and their locations in and effect on the financial statements as of and for the periods ended December 31, 2010 and 2009. Derivatives in the Company’s separate accounts are excluded from the tables because associated gains and losses generally accrue directly to policyholders.
CIGNA CORPORATION – 2010 Form 10-K – 142
|
Instrument/Volume of Activity |
Primary Risk |
Purpose |
Cash Flows |
Accounting Policy |
|||
|
Derivatives Designated as Accounting Hedges-Cash Flow Hedges |
|||||||
|
Interest rate swaps — $153 million (2010) and $160 million (2009) of par value of related investments
Foreign currency swaps — $159 million (2010) and $179 million (2009) of U.S. dollar equivalent par value of related investments
Combination swaps (interest rate and foreign currency) — $64 million (2010) and $54 million (2009) of U.S. dollar equivalent par value of related investments |
Interest rate and foreign currency |
To hedge the interest and/or foreign currency cash flows of fixed maturities and commercial mortgage loans to match associated liabilities. Currency swaps are primarily euros, Australian dollars, Canadian dollars and British pounds for periods of up to 11 years. |
The Company periodically exchanges cash flows between variable and fixed interest rates and/or between two currencies for both principal and interest. Net interest cash flows are reported in operating activities. |
Using cash flow hedge accounting, fair values are reported in other long-term investments or other liabilities and accumulated other comprehensive income and amortized into net investment income or reported in other realized investment gains and losses as interest or principal payments are received. |
|||
|
Fair Value Effect on the Financial Statements (in millions) |
|||||||
|
Instrument |
Other Long-Term Investments |
Accounts Payable, Accrued Expenses and Other Liabilities |
Gain (Loss) Recognized in Other Comprehensive Income (1) |
||||
|
As of December 31, |
As of December 31, |
For the years ended December 31, |
|||||
|
2010 |
2009 |
2010 |
2009 |
2010 |
2009 |
||
|
Interest rate swaps |
$10 |
$8 |
$- |
$- |
$2 |
$(5) |
|
|
Foreign currency swaps |
6 |
4 |
20 |
24 |
10 |
(24) |
|
|
Interest rate and foreign currency swaps |
- |
- |
12 |
6 |
(7) |
(12) |
|
|
TOTAL |
$16 |
$12 |
$32 |
$30 |
$5 |
$(41) |
|
|
(1) Other comprehensive income for foreign currency swaps excludes amounts required to adjust future policy benefits for the run-off settlement annuity business. |
|||||||
|
Purchased options — $312 million of cash surrender value of related life insurance policies |
Interest rate |
To hedge the possibility of early policyholder cash surrender when the amortized cost of underlying invested assets is greater than their fair values. |
The Company pays a fee and may receive or pay cash, based on the difference between the amortized cost and fair values of underlying invested assets at the time of policyholder surrender. These cash flows will be reported in financing activities. |
Using cash flow hedge accounting, fair values are reported in other assets or other liabilities, with changes in fair value reported in accumulated other comprehensive income and amortized to other benefit expenses over the life of the underlying invested assets. |
|||
|
Fair Value Effect on the Financial Statements |
|||||||
|
Fair values reported in other assets and other comprehensive income were not significant. |
|||||||
|
Treasury lock |
Interest rate |
To hedge the variability of and fix at inception date, the benchmark Treasury rate component of future interest payments on debt to be issued. |
The Company paid the fair value of the contract at the expiration. Cash flows were reported in operating activities. |
Using cash flow hedge accounting, fair values are reported in other assets or other liabilities, with changes in fair value reported in accumulated other comprehensive income and amortized to interest expense over the period of expected cash flows. |
|||
|
Fair Value Effect on the Financial Statements |
|||||||
|
In the first quarter of 2009, all treasury locks matured and the Company recognized a gain of $14 million in other comprehensive income, resulting in net cumulative losses of $26 million, to be amortized to interest expense over the life of the debt. In the second quarter of 2009, the Company issued debt and began amortizing this loss to interest expense over the period of expected cash flows. |
|||||||
The amount of gains (losses) reclassified from accumulated other comprehensive income into income was not significant. No gains (losses) were recognized due to ineffectiveness and no amounts were excluded from the assessment of hedge ineffectiveness.
CIGNA CORPORATION – 2010 Form 10-K – 143
|
Instrument/Volume of Activity |
Primary Risk |
Purpose |
Cash Flows |
Accounting Policy |
||||
|
Derivatives Not Designated As Accounting Hedges |
||||||||
|
Futures — $892 million (2010) and $1,058 million (2009) of U.S. dollar equivalent market price of outstanding contracts |
Equity and foreign currency |
To reduce domestic and international equity market exposures for certain reinsurance contracts that guarantee minimum death benefits (GMDB) resulting from changes in variable annuity account values based on underlying mutual funds. Currency futures are primarily euros, Japanese yen and British pounds. |
The Company receives (pays) cash daily in the amount of the change in fair value of the futures contracts. Cash flows are included in operating activities. |
Fair value changes are reported in other revenues. Amounts not yet settled from the previous day’s fair value change (daily variation margin) are reported in premiums, accounts and notes receivable, net or accounts payable, accrued expenses and other liabilities. |
||||
|
Fair Value Effect on the Financial Statements (in millions) |
||||||||
|
Other Revenues |
||||||||
|
2010 |
2009 |
|||||||
|
Futures |
$(157) |
$(283) |
||||||
|
Interest rate swaps — $45 million (2010) and $76 million (2009) of par value of related investments |
Interest rate |
To hedge the interest cash flows of fixed maturities to match associated liabilities. |
The Company periodically exchanges cash flows between variable and fixed interest rates and these cash flows are included in investing activities. |
Fair values are reported in other long-term investments or other liabilities, with changes in fair value reported in other realized investment gains and losses. |
||||
|
Fair Value Effect on the Financial Statements (in millions) |
||||||||
|
Other Long-Term Investments |
Other Realized Investment Gains (Losses) |
|||||||
|
As of December 31, |
For the years ended December 31, |
|||||||
|
2010 |
2009 |
2010 |
2009 |
|||||
|
Interest rate swaps |
$3 |
$4 |
$(2) |
$(1) |
||||
|
Written options (GMIB liability) — $1,134 million (2010) and $1,183 million (2009) of maximum potential undiscounted future payments as defined in Note 24
Purchased options (GMIB asset) — $624 million (2010) and $651 million (2009) of maximum potential undiscounted future receipts as defined in Note 24 |
Equity and interest rate |
The Company has written reinsurance contracts with issuers of variable annuity contracts that provide annuitants with certain guarantees of minimum income benefits, resulting from the level of variable annuity account values compared with a contractually guaranteed amount. Payment by the Company depends on the actual account value in the underlying mutual funds and the level of interest rates when the contractholders elect to receive minimum income payments. The Company purchased reinsurance contracts to reduce a portion of the market risk assumed. These contracts are accounted for as written and purchased options. |
The Company periodically receives (pays) fees based on either contractholders’ account values or deposits increased at a contractual rate. The Company will also pay (receive) cash depending on changes in account values and interest rates when contractholders first elect to receive minimum income payments. These cash flows are reported in operating activities. |
Fair values are reported in other liabilities (GMIB liability) and other assets (GMIB asset). Changes in fair value are reported in GMIB fair value (gain)/loss. |
||||
|
Fair Value Effect on the Financial Statements (in millions) |
||||||||
|
Instrument |
Other Assets, including other intangibles |
Accounts Payable, Accrued Expenses and Other Liabilities |
GMIB Fair Value (Gain)/Loss |
|||||
|
As of December 31, |
As of December 31, |
For the years ended December 31, |
||||||
|
2010 |
2009 |
2010 |
2009 |
2010 |
2009 |
|||
|
Written options (GMIB liability) |
$— |
$— |
$903 |
$903 |
$112 |
$(669) |
||
|
Purchased options (GMIB asset) |
480 |
482 |
— |
— |
(57) |
365 |
||
|
TOTAL |
$480 |
$482 |
$903 |
$903 |
$55 |
$(304) |
||
CIGNA CORPORATION – 2010 Form 10-K – 144
NOTE 14 Variable Interest Entities
When the Company becomes involved with a variable interest entity and when the nature of the Company’s involvement with the entity changes, in order to determine if the Company is the primary beneficiary and must consolidate the entity, it evaluates:
•
the structure and purpose of the entity;
•
the risks and rewards created by and shared through the entity; and
•
the entity’s participants’ ability to direct the activities, receive its benefits and absorb its losses. Participants include the entity’s sponsors, equity holders, guarantors, creditors and servicers.
In the normal course of its investing activities, the Company makes passive investments in securities that are issued by variable interest entities for which the Company is not the sponsor or manager. These investments are predominantly asset-backed securities primarily collateralized by foreign bank obligations and commercial mortgage-backed securities. The asset-backed securities largely represent fixed-rate debt securities issued by trusts which hold perpetual floating-rate subordinated notes issued by foreign banks. The commercial mortgage-backed securities represent senior interests in pools of commercial or residential mortgages created and held by special-purpose entities to provide investors with diversified exposure to these assets. The Company owns senior securities issued by several entities and receives fixed-rate cash flows from the underlying assets in the pools. The Company is not the primary beneficiary and does not consolidate any of these entities because either:
•
it had no power to direct the activities that most significantly impact the entities’ economic performance; or
•
it had no right to receive benefits nor obligation to absorb losses that could be significant to these variable interest entities.
The Company has not provided, and does not intend to provide, financial support to these entities. The Company performs ongoing qualitative analyses of its involvement with these variable interest entities to determine if consolidation is required. The Company’s maximum potential exposure to loss related to these entities is limited to the carrying amount of its investment reported in fixed maturities and equity securities, and its aggregate ownership interest is insignificant relative to the total principal amount issued by these entities. See Note 12A for a discussion of the Company’s process for assessing fixed maturities and equity securities for impairment.
NOTE 15 Investment Income and Gains and Losses
A. Net Investment Income
The components of pre-tax net investment income for the years ended December 31 were as follows:
|
(In millions) |
2010 |
2009 |
2008 |
|
Fixed maturities |
$788 |
$748 |
$729 |
|
Equity securities |
6 |
7 |
8 |
|
Commercial mortgage loans |
221 |
223 |
219 |
|
Policy loans |
90 |
92 |
86 |
|
Real estate |
(2) |
(1) |
1 |
|
Other long-term investments |
29 |
(30) |
6 |
|
Short-term investments and cash |
11 |
10 |
43 |
|
1,143 |
1,049 |
1,092 |
|
|
Less investment expenses |
38 |
35 |
29 |
|
NET INVESTMENT INCOME |
$1,105 |
$1,014 |
$1,063 |
Net investment income for separate accounts (which is not reflected in the Company’s revenues) was $163 million for 2010, $22 million for 2009, and $148 million for 2008.
CIGNA CORPORATION – 2010 Form 10-K – 145
B. Realized Investment Gains and Losses
The following realized gains and losses on investments for the years ended December 31 exclude amounts required to adjust future policy benefits for the run-off settlement annuity business.
|
(In millions) |
2010 |
2009 |
2008 |
|
Fixed maturities |
$87 |
$2 |
$(237) |
|
Equity securities |
5 |
12 |
(31) |
|
Commercial mortgage loans |
(23) |
(20) |
(2) |
|
Real estate |
3 |
— |
— |
|
Other investments, including derivatives |
3 |
(37) |
100 |
|
Realized investment gains (losses), before income taxes |
75 |
(43) |
(170) |
|
Less income taxes (benefits) |
25 |
(17) |
(60) |
|
Net realized investment gains (losses) |
$50 |
$(26) |
$(110) |
Included in pre-tax realized investment gains (losses) above were asset write-downs and changes in valuation reserves as follows:
|
(in millions) |
2010 |
2009 |
2008 |
|
Credit related (1) |
$38 |
$93 |
$67 |
|
Other (2) |
1 |
13 |
150 |
|
TOTAL (3) |
$39 |
$106 |
$217 |
|
(1) Credit-related losses include other-than-temporary declines in fair value of fixed maturities and equity securities, and impairments of commercial mortgage loans and real estate entities. The amount related to credit losses on fixed maturities for which a portion of the impairment was recognized in other comprehensive income was not significant. (2) Prior to adoption of new GAAP guidance for other-than-temporary impairments on April 1, 2009, other primarily represented the impact of rising market yields on investments where the Company could not demonstrate the intent and ability to hold until recovery. (3) Other-than-temporary impairments on fixed maturities in 2010 were not significant. Other-than-temporary impairments on fixed maturities of $47 million in 2009 and $213 million in 2008 are included in both the credit related and other categories above. |
|||
The Company recognized pre-tax gains of $7 million in 2010 and $13 million in 2009, compared with pre-tax losses of $31 million in 2008 on hybrid securities.
Realized investment losses in 2009 in other investments, including derivatives primarily represent impairments of real estate entities. In 2008, gains primarily represented gains on the sales of real estate properties held in joint ventures.
Realized investment gains and (losses) that are not reflected in the Company’s revenues for the years ended December 31 were as follows:
|
(In millions) |
2010 |
2009 |
2008 |
|
Separate accounts |
$191 |
$(25) |
$(146) |
|
Investment gains required to adjust future policy benefits for the run-off settlement annuity business |
$18 |
$51 |
$8 |
Sales information for available-for-sale fixed maturities and equity securities, for the years ended December 31 were as follows:
|
(In millions) |
2010 |
2009 |
2008 |
|
Proceeds from sales |
$826 |
$949 |
$1,465 |
|
Gross gains on sales |
$46 |
$51 |
$13 |
|
Gross losses on sales |
$(3) |
$(9) |
$(53) |
CIGNA CORPORATION – 2010 Form 10-K – 146
NOTE 16 Debt
|
(In millions) |
2010 |
2009 |
|
Short-term: | ||
|
Commercial paper |
$100 |
$100 |
|
Current maturities of long-term debt |
452 |
4 |
|
TOTAL SHORT-TERM DEBT |
$552 |
$104 |
|
Long-term: | ||
|
Uncollateralized debt: | ||
|
7% Notes due 2011 |
$— |
$222 |
|
6.375% Notes due 2011 |
— |
226 |
|
5.375% Notes due 2017 |
250 |
250 |
|
6.35% Notes due 2018 |
131 |
300 |
|
8.5% Notes due 2019 |
251 |
349 |
|
4.375% Notes due 2020 |
249 |
— |
|
5.125% Notes due 2020 |
299 |
— |
|
6.37% Notes due 2021 |
78 |
78 |
|
7.65% Notes due 2023 |
100 |
100 |
|
8.3% Notes due 2023 |
17 |
17 |
|
7.875% Debentures due 2027 |
300 |
300 |
|
8.3% Step Down Notes due 2033 |
83 |
83 |
|
6.15% Notes due 2036 |
500 |
500 |
|
Other |
30 |
11 |
|
TOTAL LONG-TERM DEBT |
$2,288 |
$2,436 |
In the fourth quarter of 2010, the Company entered into the following transactions related to its long-term debt:
•
On December 1, 2010 the Company offered to settle its 8.5% Notes due 2019, including accrued interest from November 1 through the settlement date. The tender price equaled the present value of the remaining principal and interest payments on the Notes being redeemed, discounted at a rate equal to the 10-year treasury rate plus a fixed spread of 100 basis points. The tender offer priced at a yield of 4.128% and principal of $99 million was tendered, with $251 million remaining outstanding. The Company paid $130 million, including accrued interest and expenses, to settle the Notes, resulting in an after-tax loss on early debt extinguishment of $21 million.
•
On December 9, 2010 the Company offered to settle its 6.35% Notes due 2018, including accrued interest from September 16 through the settlement date. The tender price equaled the present value of the remaining principal and interest payments on the Notes being redeemed, discounted at a rate equal to the 10-year treasury rate plus a fixed spread of 45 basis points. The tender offer priced at a yield of 3.923% and principal of $169 million was tendered, with $131 million remaining outstanding. The Company paid $198 million, including accrued interest and expenses, to settle the Notes, resulting in an after-tax loss on early debt extinguishment of $18 million.
•
On December 8, 2010, the Company issued $250 million of 4.375% Notes ($249 million net of debt discount, with an effective interest rate of 5.1%). The difference between the stated and effective interest rates primarily reflects the effect of treasury locks. See Note 13 to the Consolidated Financial Statements for further information. Interest is payable on June 15 and December 15 of each year beginning in 2010. These Notes will mature on December 15, 2020. The proceeds of this debt were used to fund the tender offer for the 8.5% Senior Notes due 2019 and the 6.35% Senior Notes due 2018 described above.
During 2010, the 7% Notes and 6.375% Notes due 2011 were reclassified into current maturities of long-term debt since they will mature in less than one year.
On May 12, 2010, the Company issued $300 million of 5.125% Notes ($299 million, net of debt discount, with an effective interest rate of 5.36% per year). Interest is payable on June 15 and December 15 of each year beginning December 15, 2010. These Notes will mature on June 15, 2020. The proceeds of this debt were used for general corporate purposes.
CIGNA CORPORATION – 2010 Form 10-K – 147
On May 4, 2009 the Company issued $350 million of 8.5% Notes ($349 million, net of debt discount, with an effective interest rate of 9.90% per year). The difference between the stated and effective interest rates primarily reflects the effect of treasury locks. See Note 13 for further information. Interest is payable on May 1 and November 1 of each year beginning November 1, 2009. These Notes will mature on May 1, 2019. As described above, a portion of these Notes were settled in 2010 through a tender offer.
The Company may redeem the Notes issued in 2010 and 2009 at any time, in whole or in part, at a redemption price equal to the greater of:
•
100% of the principal amount of the Notes to be redeemed; or
•
the present value of the remaining principal and interest payments on the Notes being redeemed discounted at the applicable Treasury Rate plus 25 basis points for the 4.375% and 5.125% Notes due 2020 and 50 basis points for the 8.5% Notes due 2019.
Maturities of debt and capital leases are as follows (in millions): $452 in 2011, $3 in 2012 and 2013, $23 in 2014 and the remainder in years after 2014. Interest expense on long-term debt, short-term debt and capital leases was $182 million in 2010, $166 million in 2009, and $146 million in 2008.
On March 14, 2008, the Company entered into a commercial paper program (“the Program”). Under the Program, the Company is authorized to sell from time to time short-term unsecured commercial paper notes up to a maximum of $500 million. The proceeds are used for general corporate purposes, including working capital, capital expenditures, acquisitions and share repurchases. The Company uses the credit facility entered into in June 2007, as back-up liquidity to support the outstanding commercial paper. If at any time funds are not available on favorable terms under the Program, the Company may use its credit facility for funding. In October 2008, the Company added an additional dealer to its Program. As of December 31, 2010, the Company had $100 million in commercial paper outstanding, at a weighted average interest rate of 0.38%.
In June 2007, the Company amended and restated its five-year revolving credit and letter of credit agreement for $1.75 billion, which permits up to $1.25 billion to be used for letters of credit. The agreement includes options, which are subject to consent by the administrative agent and the committing bank, to increase the commitment amount up to $2.0 billion and to extend the term of the agreement. The Company entered into the agreement for general corporate purposes, including the support for the issuance of commercial paper and to obtain statutory reserve credit for certain reinsurance arrangements. There were letters of credit issued in the amount of $82 million as of December 31, 2010. As of December 31, 2010, the Company had an additional $1.7 billion of borrowing capacity within the maximum debt leverage covenant in the line of credit agreement in addition to the $2.8 billion of short-term and long-term debt outstanding.
NOTE 17 Common and Preferred Stock
As of December 31, the Company had issued the following shares:
|
(Shares in thousands) |
2010 |
2009 |
|
Common: Par value $0.25 | ||
|
600,000 shares authorized | ||
|
Outstanding — January 1 |
274,257 |
271,036 |
|
Issued for stock option and other benefit plans |
3,805 |
3,221 |
|
Repurchase of common stock |
(6,182) |
— |
|
Outstanding — December 31 |
271,880 |
274,257 |
|
Treasury stock |
79,066 |
76,689 |
|
ISSUED — DECEMBER 31 |
350,946 |
350,946 |
The Company maintains a share repurchase program, which was authorized by its Board of Directors. The decision to repurchase shares depends on market conditions and alternative uses of capital. The Company has, and may continue from time to time, to repurchase shares on the open market through a Rule 10b5-1 plan that permits a company to repurchase its shares at times when it otherwise might be precluded from doing so under insider trading laws or because of self-imposed trading blackout periods.
The Company has authorized a total of 25 million shares of $1 par value preferred stock. No shares of preferred stock were outstanding at December 31, 2010 or 2009.
CIGNA CORPORATION – 2010 Form 10-K – 148
NOTE 18 Accumulated Other Comprehensive Income (Loss)
Accumulated other comprehensive income (loss) excludes amounts required to adjust future policy benefits for the run-off settlement annuity business.
Changes in accumulated other comprehensive income (loss) were as follows:
|
2010 (In millions) |
Pre-Tax |
Tax (Expense) Benefit |
After- Tax |
|
Net unrealized appreciation, securities: | |||
|
Net unrealized appreciation on securities arising during the year |
$319 |
$(109) |
$210 |
|
Reclassification adjustment for (gains) included in shareholders’ net income |
(92) |
32 |
(60) |
|
Net unrealized appreciation, securities |
$227 |
$(77) |
$150 |
|
Net unrealized appreciation, derivatives |
$8 |
$(2) |
$6 |
|
Net translation of foreign currencies |
$48 |
$(11) |
$37 |
|
Postretirement benefits liability adjustment: | |||
|
Reclassification adjustment for amortization of net losses from past experience and prior service costs |
$10 |
$(4) |
$6 |
|
Net change arising from assumption and plan changes and experience |
(311) |
116 |
(195) |
|
Net postretirement benefits liability adjustment |
$(301) |
$112 |
$(189) |
|
2009 (In millions) |
Pre-Tax |
Tax (Expense) Benefit |
After- Tax |
|
Net unrealized appreciation, securities: | |||
|
Implementation effect of updated guidance on other-than-temporary impairments |
$(27) |
$9 |
$(18) |
|
Net unrealized appreciation on securities arising during the year |
843 |
(292) |
551 |
|
Reclassification adjustment for (gains) included in net income |
(14) |
3 |
(11) |
|
Net unrealized appreciation, securities |
$802 |
$(280) |
$522 |
|
Net unrealized depreciation, derivatives |
$(30) |
$13 |
$(17) |
|
Net translation of foreign currencies |
$76 |
$(28) |
$48 |
|
Postretirement benefits liability adjustment: | |||
|
Reclassification adjustment for amortization of net losses from past experience and prior service costs |
$7 |
$(3) |
$4 |
|
Curtailment gain |
(46) |
16 |
(30) |
|
Reclassification adjustment included in shareholders’ net income |
(39) |
13 |
(26) |
|
Net change arising from assumption and plan changes and experience |
(107) |
36 |
(71) |
|
Net postretirement benefits liability adjustment |
$(146) |
$49 |
$(97) |
CIGNA CORPORATION – 2010 Form 10-K – 149
|
2008 (In millions) |
Pre-Tax |
Tax (Expense) Benefit |
After- Tax |
|
Net unrealized depreciation, securities: | |||
|
Net unrealized depreciation on securities arising during the year |
$(706) |
$245 |
$(461) |
|
Reclassification adjustment for losses included in net income |
268 |
(94) |
174 |
|
Net unrealized depreciation, securities |
$(438) |
$151 |
$(287) |
|
Net unrealized appreciation, derivatives |
$9 |
$(3) |
$6 |
|
Net translation of foreign currencies |
$(183) |
$62 |
$(121) |
|
Postretirement benefits liability adjustment: |
|
|
|
|
Reclassification adjustment for amortization of net losses from past experience and prior service costs |
$21 |
$(7) |
$14 |
|
Net change arising from assumption and plan changes and experience |
(1,134) |
397 |
(737) |
|
Net postretirement benefits liability adjustment |
$(1,113) |
$390 |
$(723) |
NOTE 19 Shareholders’ Equity and Dividend Restrictions
State insurance departments and foreign jurisdictions that regulate certain of the Company’s subsidiaries prescribe accounting practices (which differ in some respects from GAAP) to determine statutory net income and surplus. The Company’s life insurance and HMO company subsidiaries are regulated by such statutory requirements. The statutory net income for the years ended, and statutory surplus as of, December 31 of the Company’s life insurance and HMO subsidiaries were as follows:
|
(In millions) |
2010 |
2009 |
2008 |
|
Net income |
$1,697 |
$1,088 |
$420 |
|
Surplus |
$5,107 |
$4,728 |
$3,638 |
As of December 31, 2010, statutory surplus for each of the Company’s life insurance and HMO subsidiaries is sufficient to meet the minimum required by regulators. As of December 31, 2010, the Company’s life insurance and HMO subsidiaries had investments on deposit with state departments of insurance with statutory carrying values of $319 million. The Company’s life insurance and HMO subsidiaries are also subject to regulatory restrictions that limit the amount of annual dividends or other distributions (such as loans or cash advances) insurance companies may extend to the parent company without prior approval of regulatory authorities. The maximum dividend distribution that the Company’s life insurance and HMO subsidiaries may make during 2011 without prior approval is approximately $1.5 billion. Restricted net assets of the Company as of December 31, 2010, were approximately $5 billion. One of the Company’s life insurance subsidiaries is permitted to loan up to $600 million to the parent company without prior approval.
CIGNA CORPORATION – 2010 Form 10-K – 150
NOTE 20 Income Taxes
A. Income Tax Expense
The components of income taxes for the years ended December 31 were as follows:
|
(In millions) |
2010 |
2009 |
2008 |
|
Current taxes | |||
|
U.S. income |
$267 |
$211 |
$255 |
|
Foreign income |
45 |
48 |
57 |
|
State income |
19 |
16 |
1 |
|
331 |
275 |
313 |
|
|
Deferred taxes (benefits) | |||
|
U.S. income |
182 |
279 |
(224) |
|
Foreign income |
15 |
39 |
2 |
|
State income |
(7) |
1 |
1 |
|
190 |
319 |
(221) |
|
|
TOTAL INCOME TAXES |
$521 |
$594 |
$92 |
Total income taxes for the years ended December 31 were different from the amount computed using the nominal federal income tax rate of 35% for the following reasons:
|
(In millions) |
2010 |
2009 |
2008 |
|
Tax expense at nominal rate |
$655 |
$664 |
$135 |
|
Tax-exempt interest income |
(31) |
(31) |
(32) |
|
Effect of permanently invested foreign earnings |
(31) |
(23) |
— |
|
Dividends received deduction |
(3) |
(3) |
(3) |
|
Resolution of federal tax matters |
— |
(27) |
(1) |
|
State income tax (net of federal income tax benefit) |
9 |
12 |
1 |
|
Change in valuation allowance |
(94) |
(2) |
(15) |
|
Other |
16 |
4 |
7 |
|
TOTAL INCOME TAXES |
$521 |
$594 |
$92 |
Effect of Permanently Invested Foreign Earnings
The Company has historically accrued U. S. income taxes on the undistributed earnings of its foreign subsidiaries. However, the Company recently began computing income taxes attributable to the South Korea and Hong Kong operations using the tax rates of the foreign jurisdictions, as compared to the higher U. S. statutory tax rate. This change, adopted in 2009 for South Korea and earlier in 2010 for Hong Kong, was based upon a determination that the prospective earnings of these operations would be permanently invested overseas.
As a result, shareholders’ net income for the year ended December 31, 2010, increased by $31 million, which included $20 million relative to South Korea and $11 million relative to Hong Kong. The Hong Kong amount includes $6 million associated with first quarter transition. Shareholders’ net income for the year ended December 31, 2009 increased by $23 million, all attributable to South Korea. Permanent investment of foreign operation earnings has resulted in cumulative unrecognized deferred tax liabilities of $54 million though December 31, 2010.
Change in Valuation Allowance
The decline in the valuation allowance primarily reflects the resolution of a disputed federal income tax matter. See the “Deferred Income Taxes” section of this footnote for further discussion.
CIGNA CORPORATION – 2010 Form 10-K – 151
B. Deferred Income Taxes
Deferred income tax assets and liabilities as of December 31 are shown below.
|
(In millions) |
2010 |
2009 |
|
Deferred tax assets | ||
|
Employee and retiree benefit plans |
$746 |
$774 |
|
Investments, net |
100 |
111 |
|
Other insurance and contractholder liabilities |
391 |
430 |
|
Deferred gain on sale of business |
58 |
67 |
|
Policy acquisition expenses |
143 |
144 |
|
Loss carryforwards |
76 |
104 |
|
Other accrued liabilities |
107 |
111 |
|
Bad debt expense |
18 |
16 |
|
Other |
37 |
34 |
|
Deferred tax assets before valuation allowance |
1,676 |
1,791 |
|
Valuation allowance for deferred tax assets |
(23) |
(116) |
|
Deferred tax assets, net of valuation allowance |
1,653 |
1,675 |
|
Deferred tax liabilities | ||
|
Depreciation and amortization |
314 |
291 |
|
Foreign operations, net |
267 |
151 |
|
Unrealized appreciation on investments and foreign currency translation |
290 |
204 |
|
Total deferred tax liabilities |
871 |
646 |
|
NET DEFERRED INCOME TAX ASSETS |
$782 |
$1,029 |
Management believes consolidated taxable income expected to be generated in the future will be sufficient to support realization of the Company’s net deferred tax assets. This determination is based upon the Company’s consistent overall earnings history and future earnings expectations. Other than deferred tax benefits attributable to operating loss carryforwards, there are no time constraints within which the Company’s deferred tax assets must be realized. Federal operating losses of $205 million were available to offset taxable income of the generating companies, and begin to expire in 2022. As of December 31, 2010, the Company had no foreign tax credit carryforwards.
The Company’s deferred tax asset is net of a federal and state valuation allowance. The valuation allowance reflects management’s assessment that certain deferred tax assets may not be realizable. As described above, the significant decline in the valuation allowance was primarily due to the resolution of a disputed federal income tax matter through an administrative appeals process, as well as an available tax planning strategy, which indicated that future recognition of the underlying operating loss in the run-off reinsurance operations is now more likely than not.
C. Uncertain Tax Positions
A reconciliation of unrecognized tax benefits for the years ended December 31 is as follows:
|
(In millions) |
2010 |
2009 |
2008 |
|
Balance at January 1, |
$214 |
$164 |
$260 |
|
Increase (decrease) due to prior year positions |
(55) |
5 |
(119) |
|
Increase due to current year positions |
34 |
76 |
34 |
|
Reduction related to settlements with taxing authorities |
(13) |
(28) |
(5) |
|
Reduction related to lapse of applicable statute of limitations |
(3) |
(3) |
(6) |
|
BALANCE AT DECEMBER 31, |
$177 |
$214 |
$164 |
CIGNA CORPORATION – 2010 Form 10-K – 152
Unrecognized tax benefits decreased during 2010 primarily due to the resolution of the disputed federal income tax matter for tax years 2005 and 2006 previously described as contributing to the decline in the valuation allowance.
The December 31, 2010 balance included $29 million that would increase shareholders’ net income if recognized. The Company has determined it is reasonably possible that within the next twelve months the level of unrecognized tax benefits could change significantly, subject to the development of IRS specific matters. These changes are not expected to have a material impact on shareholders’ net income.
The Company classifies net interest expense on uncertain tax positions and any applicable penalties as a component of income tax expense, but excludes these amounts from the liability for uncertain tax positions. The Company’s liability for net interest and penalties was $14 million at December 31, 2010, $13 million at December 31, 2009 and $19 million at December 31, 2008. The 2009 decline included $13 million associated with the completion of an IRS examination.
During the first quarter of 2009, the IRS completed its examination of the Company’s 2005 and 2006 consolidated federal income tax returns, resulting in an increase to shareholders’ net income of $21 million ($20 million in continuing operations and $1 million in discontinued operations). The increase reflected a reduction in net unrecognized tax benefits of $8 million, ($17 million reported in income tax expense, partially offset by a $9 million pre-tax charge) and a reduction of interest and penalties of $13 million (reported in income tax expense).
D. Federal Income Tax Examinations, Litigation and Other Matters
One disputed matter remains unresolved related to the IRS examination of the 2003 and 2004 consolidated federal income tax returns and on June 4, 2009 the Company initiated litigation of this matter by filing a petition in the United States Tax Court. Due to the nature of the litigation process, timing of the resolution of this matter is uncertain. This same issue also remains unresolved in the IRS examination of the 2005 and 2006 consolidated federal income tax returns. Though the Company expects to prevail, unfavorable resolution of this litigation would result in a charge to shareholders’ net income of up to $22 million, representing net interest expense on the cumulative incremental tax for all affected years.
The IRS is currently in the latter stages of its examination of the Company’s 2007 and 2008 consolidated federal income tax returns, which is expected to be completed in the first quarter of 2011. The Company conducts business in numerous states and foreign jurisdictions, and may be engaged in multiple audit proceedings at any given time. Generally, no further state or foreign audit activity for years prior to 2002 is expected.
The recently enacted Patient Protection & Affordable Care Act, including the Reconciliation Act of 2010, included provisions limiting the tax deductibility of certain future retiree benefit and compensation related payments that were earned after 2009. The effect of these provisions reduced shareholders’ net income for the twelve months ended December 31, 2010 by $10 million. The Company will continue to evaluate the tax effect of these provisions.
NOTE 21 Employee Incentive Plans
The People Resources Committee (“the Committee”) of the Board of Directors awards stock options, restricted stock, deferred stock and, beginning in 2010, strategic performance shares to certain employees. To a very limited extent, the Committee has issued common stock instead of cash compensation and dividend equivalent rights as part of restricted and deferred stock units. The Company issues shares from Treasury stock for option exercises, awards of restricted stock and payment of deferred and restricted stock units.
Compensation cost and related tax benefits for these awards were as follows:
|
(In millions) |
2010 |
2009 |
2008 |
|
Compensation cost |
$49 |
$42 |
$41 |
|
Tax benefits |
$12 |
$15 |
$14 |
The Company had the following number of shares of common stock available for award at December 31: 7.5 million in 2010, 23.3 million in 2009 and 28.5 million in 2008.
Stock options. The Company awards options to purchase the Company’s common stock at the market price of the stock on the grant date. Options vest over periods ranging from one to five years and expire no later than 10 years after the grant date.
CIGNA CORPORATION – 2010 Form 10-K – 153
The table below shows the status of, and changes in, common stock options during the last three years:
|
(Options in thousands) |
2010 |
2009 |
2008 |
|||
|
Options |
Weighted Average Exercise Price |
Options |
Weighted Average Exercise Price |
Options |
Weighted Average Exercise Price |
|
|
Outstanding — January 1 |
13,751 |
$29.34 |
12,258 |
$35.48 |
11,430 |
$32.69 |
|
Granted |
1,846 |
$34.64 |
4,709 |
$14.15 |
2,311 |
$46.53 |
|
Exercised |
(2,565) |
$24.31 |
(1,167) |
$25.32 |
(1,058) |
$27.40 |
|
Expired or canceled |
(939) |
$30.86 |
(2,049) |
$33.42 |
(425) |
$40.67 |
|
Outstanding — December 31 |
12,093 |
$31.10 |
13,751 |
$29.34 |
12,258 |
$35.48 |
|
Options exercisable at year-end |
7,656 |
$34.42 |
8,578 |
$33.53 |
8,687 |
$31.19 |
Compensation expense of $18 million related to unvested stock options at December 31, 2010 will be recognized over the next two years (weighted average period).
The table below summarizes information for stock options exercised during the last three years :
|
(In millions) |
2010 |
2009 |
2008 |
|
Intrinsic value of options exercised |
$30 |
$7 |
$23 |
|
Cash received for options exercised |
$62 |
$30 |
$26 |
|
Excess tax benefits realized from options exercised |
$5 |
$— |
$6 |
The following table summarizes information for outstanding common stock options at December 31, 2010:
|
(Dollars in millions, except per share amounts) |
Options Outstanding |
Options Exercisable |
|
Number (in thousands) |
12,093 |
7,656 |
|
Total intrinsic value |
$99 |
$44 |
|
Weighted average exercise price |
$31.10 |
$34.42 |
|
Weighted average remaining contractual life |
5.8 years |
4.3 years |
The weighted average fair value of options granted under employee incentive plans was $11.56 for 2010, $4.60 for 2009 and $14.33 for 2008, using the Black-Scholes option-pricing model and the following assumptions:
|
2010 |
2009 |
2008 |
|
|
Dividend yield |
0.1% |
0.3% |
0.1% |
|
Expected volatility |
40.0% |
40.0% |
35.0% |
|
Risk-free interest rate |
1.9% |
1.6% |
2.2% |
|
Expected option life |
4 years |
4 years |
4 years |
The expected volatility reflects the Company’s past daily stock price volatility. The Company does not consider volatility implied in the market prices of traded options to be a good indicator of future volatility because remaining maturities of traded options are less than one year. The risk-free interest rate is derived using the four-year U.S. Treasury bond yield rate as of the award date for the primary grant. Expected option life reflects the Company’s historical experience.
CIGNA CORPORATION – 2010 Form 10-K – 154
Restricted stock. The Company awards restricted stock to its employees or directors with vesting periods ranging from two to five years. These awards are generally in one of two forms: restricted stock grants or restricted stock units. Restricted stock grants are the most widely used form of restricted stock awards and are used for substantially all U.S.-based employees receiving such awards. Recipients of restricted stock grants are entitled to earn dividends and to vote during the vesting period, but forfeit their awards if their employment terminates before the vesting date. Awards of restricted stock units are generally limited to international employees. A restricted stock unit represents a right to receive a common share of stock when the unit vests. Recipients of restricted stock units are entitled to receive hypothetical dividends, but cannot vote during the vesting period. They forfeit their units if their employment terminates before the vesting date.
The table below shows the status of, and changes in, restricted stock grants and units during the last three years:
|
(Awards in thousands) |
2010 |
2009 |
2008 |
|||
|
Grants/Units |
Weighted Average Fair Value at Award Date |
Grants/Units |
Weighted Average Fair Value at Award Date |
Grants/Units |
Weighted Average Fair Value at Award Date |
|
|
Outstanding — January 1 |
4,113 |
$27.65 |
2,347 |
$40.53 |
2,482 |
$34.28 |
|
Awarded |
1,155 |
$34.63 |
2,678 |
$18.14 |
820 |
$43.90 |
|
Vested |
(541) |
$40.87 |
(557) |
$32.00 |
(760) |
$23.81 |
|
Forfeited |
(421) |
$29.28 |
(355) |
$33.79 |
(195) |
$40.47 |
|
OUTSTANDING — DECEMBER 31 |
4,306 |
$27.70 |
4,113 |
$27.65 |
2,347 |
$40.53 |
The fair value of vested restricted stock was: $18 million in 2010, $10 million in 2009 and $35 million in 2008.
At the end of 2010, approximately 3,000 employees held 4.3 million restricted stock grants and units with $65 million of related compensation expense to be recognized over the next three years (weighted average period).
Strategic Performance Shares. The Company awards strategic performance shares to its executives generally with a performance period of three years. Strategic performance shares are divided into two broad groups: 50% are subject to a market condition (total shareholder return relative to industry peer companies) and 50% are subject to a performance conditions (revenue growth and cumulative adjusted net income). These targets are set by the Committee. At the end of the performance period, holders of strategic performance shares will be awarded anywhere from 0 to 200% of the original grant of strategic performance shares in CIGNA common stock.
The table below shows the status of, and changes in, strategic performance shares during 2010:
|
(Awards in thousands) |
2010 |
|
|
Grants/Units |
Weighted Average Fair Value at Award Date |
|
|
Awarded |
480 |
$34.73 |
|
Forfeited |
(50) |
$34.65 |
|
OUTSTANDING — DECEMBER 31 |
430 |
$34.73 |
At the end of 2010, 61 employees held approximately 430,000 strategic performance shares and $11 million of related compensation expense expected to be recognized over the next two years. For strategic performance shares subject to a performance condition, the amount of expense may vary based on actual performance in 2011 and 2012.
CIGNA CORPORATION – 2010 Form 10-K – 155
NOTE 22 Leases, Rentals and Outsourced Service Arrangements
Rental expenses for operating leases, principally for office space, amounted to $127 million in 2010, $138 million in 2009 and $131 million in 2008. As of December 31, 2010, future net minimum rental payments under non-cancelable operating leases were approximately $496 million, payable as follows (in millions): $105 in 2011, $93 in 2012, $70 in 2013, $56 in 2014, $48 in 2015 and $124 thereafter.
The Company also has several outsourced service arrangements with third parties, primarily for human resource and information technology support services. The initial service periods under these arrangements range from seven to eight years and their related costs are reported consistent with operating leases over the service period based on the pattern of use. The Company recorded in other operating expense $114 million in 2010, $115 million in 2009 and $113 million in 2008 for these arrangements.
NOTE 23 Segment Information
The Company’s operating segments generally reflect groups of related products, except for the International segment which is generally based on geography. In accordance with GAAP, operating segments that do not require separate disclosure were combined in “Other Operations”. The Company measures the financial results of its segments using “segment earnings (loss)”, which is defined as shareholders’ income (loss) from continuing operations before after-tax realized investment results.
Consolidated pre-tax income from continuing operations is primarily attributable to domestic operations. Consolidated pre-tax income from continuing operations generated by the Company’s foreign operations was approximately 13% in 2010, 9% in 2009 and 36% in 2008.
The Company determines segment earnings (loss) consistent with accounting policies used in preparing the consolidated financial statements, except that amounts included in Corporate are not allocated to segments. The Company allocates certain other operating expenses, such as systems and other key corporate overhead expenses, on systematic bases. Income taxes are generally computed as if each segment were filing a separate income tax return. The Company does not report total assets by segment since this is not a metric used to allocate resources or evaluate segment performance.
The Company presents segment information as follows:
Health Care includes medical, dental, behavioral health, prescription drug and other products and services that may be integrated to support consumer-focused health care programs. This segment also includes group disability and life insurance products that were historically sold in connection with certain experience-rated medical products.
Disability and Life includes group:
•
disability insurance;
•
life insurance;
•
accident; and
•
specialty insurance.
International includes:
•
supplemental health, life and accident insurance products; and
•
international health care products and services including those offered to expatriate employees of multinational corporations.
Run-off Reinsurance includes accident, workers’ compensation, international life and health, GMDB and GMIB reinsurance businesses. The Company stopped underwriting new reinsurance business in 2000 and essentially exited the accident and workers’ compensation business in 2010.
The Company also reports results in two other categories.
CIGNA CORPORATION – 2010 Form 10-K – 156
Other Operations consist of:
•
corporate-owned life insurance (COLI);
•
deferred gains recognized from the 1998 sale of the individual life insurance and annuity business and the 2004 sale of the retirement benefits business; and
•
the run-off settlement annuity business.
Corporate reflects amounts such as interest expense on corporate debt and on uncertain tax positions, net investment income on investments not supporting segment operations, intersegment eliminations, compensation cost for stock options and certain corporate overhead expenses. Beginning in 2010, the Company began reporting the expense associated with its frozen pension plans in Corporate. Prior periods were not restated as the effect on prior periods was not material.
Summarized segment financial information for the years ended December 31 was as follows:
|
(In millions) |
2010 |
2009 |
2008 |
|
Health Care | |||
|
Premiums and fees: | |||
|
Medical: | |||
|
Guaranteed cost (1)(2) |
$3,929 |
$3,380 |
$3,704 |
|
Experience-rated (2)(3) |
1,823 |
1,699 |
1,953 |
|
Stop loss |
1,287 |
1,274 |
1,197 |
|
Dental |
804 |
731 |
785 |
|
Medicare |
1,470 |
595 |
400 |
|
Medicare Part D |
558 |
342 |
327 |
|
Other (4) |
543 |
515 |
518 |
|
Total medical |
10,414 |
8,536 |
8,884 |
|
Life and other non-medical |
103 |
179 |
184 |
|
Total premiums |
10,517 |
8,715 |
9,068 |
|
Fees (2)(5) |
2,802 |
2,669 |
2,597 |
|
Total premiums and fees |
13,319 |
11,384 |
11,665 |
|
Mail order pharmacy revenues |
1,420 |
1,282 |
1,204 |
|
Other revenues |
266 |
262 |
267 |
|
Net investment income |
243 |
181 |
200 |
|
Segment revenues |
$15,248 |
$13,109 |
$13,336 |
|
Income taxes |
$476 |
$399 |
$352 |
|
Segment earnings |
$861 |
$731 |
$664 |
|
(1) Includes guaranteed cost premiums primarily associated with open access and commercial HMO, as well as other risk-related products. (2) Premiums and/or fees associated with certain specialty products are also included. (3) Includes minimum premium arrangements with a risk profile similar to experience-rated funding arrangements. The risk portion of minimum premium revenue is reported in experience-rated medical premium whereas the self funding portion of minimum premium revenue is recorded in fees. Also includes certain non-participating cases for which special customer level reporting of experience is required. (4) Other medical premiums include risk revenue for specialty products. (5) Represents administrative service fees for medical members and related specialty product fees for non-medical members as well as fees related to Medicare Part D of $57 million in 2010, $41 million in 2009 and $69 million in 2008. |
|||
CIGNA CORPORATION – 2010 Form 10-K – 157
|
(In millions) |
2010 |
2009 |
2008 |
|
Disability and Life | |||
|
Premiums and fees: | |||
|
Life |
$1,238 |
$1,301 |
$1,261 |
|
Disability |
1,167 |
1,057 |
1,004 |
|
Other |
262 |
276 |
297 |
|
Total |
2,667 |
2,634 |
2,562 |
|
Other revenues |
123 |
113 |
117 |
|
Net investment income |
261 |
244 |
256 |
|
Segment revenues |
$3,051 |
$2,991 |
$2,935 |
|
Income taxes |
$120 |
$109 |
$109 |
|
Segment earnings |
$291 |
$284 |
$273 |
|
International | |||
|
Premiums and fees: | |||
|
Health Care |
$1,037 |
$884 |
$856 |
|
Supplemental Health, Life, and Accident |
1,231 |
998 |
1,014 |
|
Total |
2,268 |
1,882 |
1,870 |
|
Other revenues |
31 |
22 |
18 |
|
Net investment income |
82 |
69 |
79 |
|
Segment revenues |
$2,381 |
$1,973 |
$1,967 |
|
Income taxes |
$95 |
$70 |
$104 |
|
Equity in income of investees |
$14 |
$11 |
$8 |
|
Segment earnings |
$243 |
$183 |
$182 |
|
Run-off Reinsurance | |||
|
Premiums and fees and other revenues |
$(133) |
$(254) |
$374 |
|
Net investment income |
114 |
113 |
104 |
|
Segment revenues |
$(19) |
$(141) |
$478 |
|
Income taxes (benefits) |
$(136) |
$93 |
$(375) |
|
Segment earnings (loss) |
$26 |
$185 |
$(646) |
|
Other Operations | |||
|
Premiums and fees and other revenues |
$174 |
$176 |
$184 |
|
Net investment income |
404 |
407 |
414 |
|
Segment revenues |
$578 |
$583 |
$598 |
|
Income taxes |
$39 |
$31 |
$43 |
|
Segment earnings |
$85 |
$86 |
$87 |
|
Corporate | |||
|
Other revenues and eliminations |
$(62) |
$(58) |
$(53) |
|
Net investment income |
1 |
— |
10 |
|
Segment revenues |
$(61) |
$(58) |
$(43) |
|
Income tax benefits |
$(98) |
$(91) |
$(81) |
|
Segment loss |
$(211) |
$(142) |
$(162) |
|
Realized investment gains (losses) | |||
|
Realized investment gains (losses) |
$75 |
$(43) |
$(170) |
|
Income taxes (benefits) |
25 |
(17) |
(60) |
|
Realized investment gains (losses), net of taxes and noncontrolling interest |
$50 |
$(26) |
$(110) |
|
Total | |||
|
Premiums and fees and other revenues |
$18,653 |
$16,161 |
$17,004 |
|
Mail order pharmacy revenues |
1,420 |
1,282 |
1,204 |
|
Net investment income |
1,105 |
1,014 |
1,063 |
|
Realized investment gains (losses) |
75 |
(43) |
(170) |
|
Total revenues |
$21,253 |
$18,414 |
$19,101 |
|
Income taxes |
$521 |
$594 |
$92 |
|
Segment earnings |
$1,295 |
$1,327 |
$398 |
|
Realized investment gains (losses), net of taxes and noncontrolling interest |
$50 |
$(26) |
$(110) |
|
Shareholders’ income from continuing operations |
$1,345 |
$1,301 |
$288 |
CIGNA CORPORATION – 2010 Form 10-K – 158
Premiums and fees, mail order pharmacy revenues and other revenues by product type were as follows for the years ended December 31:
|
(In millions) |
2010 |
2009 |
2008 |
|
Medical |
$14,253 |
$12,089 |
$12,337 |
|
Disability |
1,162 |
1,063 |
994 |
|
Supplemental Health, Life, and Accident |
2,839 |
2,748 |
2,766 |
|
Mail order pharmacy |
1,420 |
1,282 |
1,204 |
|
Other |
399 |
261 |
907 |
|
TOTAL |
$20,073 |
$17,443 |
$18,208 |
Concentration of risk. For the Company’s International segment, South Korea is the single largest geographic market. South Korea generated 32% of the segment’s revenues and 49% of the segment’s earnings in 2010. South Korea generated 29% of the segment’s revenues and 49% of the segment’s earnings in 2009. Due to the concentration of business in South Korea, the International segment is exposed to potential losses resulting from economic and geopolitical developments in that country, as well as foreign currency movements affecting the South Korean currency, which could have a significant impact on the segment’s results and the Company’s consolidated financial results.
NOTE 24 Contingencies and Other Matters
The Company, through its subsidiaries, is contingently liable for various guarantees provided in the ordinary course of business.
A. Financial Guarantees Primarily Associated with the Sold Retirement Benefits Business
Separate account assets are contractholder funds maintained in accounts with specific investment objectives. The Company records separate account liabilities equal to separate account assets. In certain cases, primarily associated with the sold retirement benefits business (which was sold in April 2004), the Company guarantees a minimum level of benefits for retirement and insurance contracts, written in separate accounts. The Company establishes an additional liability if management believes that the Company will be required to make a payment under these guarantees.
The Company guarantees that separate account assets will be sufficient to pay certain retiree or life benefits. The sponsoring employers are primarily responsible for ensuring that assets are sufficient to pay these benefits and are required to maintain assets that exceed a certain percentage of benefit obligations. This percentage varies depending on the asset class within a sponsoring employer’s portfolio (for example, a bond fund would require a lower percentage than a riskier equity fund) and thus will vary as the composition of the portfolio changes. If employers do not maintain the required levels of separate account assets, the Company or an affiliate of the buyer has the right to redirect the management of the related assets to provide for benefit payments. As of December 31, 2010, employers maintained assets that exceeded the benefit obligations. Benefit obligations under these arrangements were $1.3 billion as of December 31, 2010. As of December 31, 2010, approximately 75% of these guarantees are reinsured by an affiliate of the buyer of the retirement benefits business. The remaining guarantees are provided by the Company with minimal reinsurance from third parties. There were no additional liabilities required for these guarantees as of December 31, 2010. Separate account assets supporting these guarantees are classified in Levels 1 and 2 of the GAAP fair value hierarchy. See Note 11 for further information on the fair value hierarchy.
The Company does not expect that these financial guarantees will have a material effect on the Company’s consolidated results of operations, liquidity or financial condition.
B. Guaranteed Minimum Income Benefit Contracts
The Company’s reinsurance operations, which were discontinued in 2000 and are now an inactive business in run-off mode, reinsured minimum income benefits under certain variable annuity contracts issued by other insurance companies. A contractholder can elect the guaranteed minimum income benefit (“GMIB”) within 30 days of any eligible policy anniversary after a specified contractual waiting period. The Company’s exposure arises when the guaranteed annuitization benefit exceeds the annuitization benefit based on the policy’s current account value. At the time of annuitization, the Company pays the excess (if any) of the minimum benefit guaranteed under the contract over the benefit based on the current account value in a lump sum to the direct writing insurance company.
In periods of declining equity markets or declining interest rates, the Company’s GMIB liabilities increase. Conversely, in periods of rising equity markets and rising interest rates, the Company’s liabilities for these benefits decrease.
CIGNA CORPORATION – 2010 Form 10-K – 159
The Company estimates the fair value of the GMIB assets and liabilities using assumptions for market returns and interest rates, volatility of the underlying equity and bond mutual fund investments, mortality, lapse, annuity election rates, non-performance risk, and risk and profit charges. See Note 11 for additional information on how fair values for these liabilities and related receivables for retrocessional coverage are determined.
The Company is required to disclose the maximum potential undiscounted future payments for GMIB contracts. Under these guarantees, the future payment amounts are dependent on equity and bond fund market and interest rate levels prior to and at the date of annuitization election, which must occur within 30 days of a policy anniversary, after the appropriate waiting period. Therefore, the future payments are not fixed and determinable under the terms of the contract. Accordingly, the Company has estimated the maximum potential undiscounted future payments using hypothetical adverse assumptions, defined as follows:
•
no annuitants surrendered their accounts;
•
all annuitants lived to elect their benefit;
•
all annuitants elected to receive their benefit on the next available date (2011 through 2017); and
•
all underlying mutual fund investment values remained at the December 31, 2010 value of $1.3 billion with no future returns.
The maximum potential undiscounted payments that the Company would make under those assumptions would aggregate $1.1 billion before reinsurance recoveries. The Company expects the amount of actual payments to be significantly less than this hypothetical undiscounted aggregate amount. The Company has retrocessional coverage in place from two external reinsurers which covers 55% of the exposures on these contracts. The Company bears the risk of loss if its retrocessionaires do not meet or are unable to meet their reinsurance obligations to the Company.
C. Certain Other Guarantees
The Company had indemnification obligations to lenders of up to $168 million as of December 31, 2010 related to borrowings by certain real estate joint ventures which the Company either records as an investment or consolidates. These borrowings, which are nonrecourse to the Company and are secured by the joint ventures’ real estate properties with fair values in excess of the loan amounts and mature at various dates beginning in 2011 through 2017. The Company’s indemnification obligations would require payment to lenders for any actual damages resulting from certain acts such as unauthorized ownership transfers, misappropriation of rental payments by others or environmental damages. Based on initial and ongoing reviews of property management and operations, the Company does not expect that payments will be required under these indemnification obligations. Any payments that might be required could be recovered through a refinancing or sale of the assets. In some cases, the Company also has recourse to partners for their proportionate share of amounts paid. There were no liabilities required for these indemnification obligations as of December 31, 2010.
As part of the reinsurance and administrative service arrangements, the Company pays claims for the group medical and long-term disability business of Great-West Healthcare and collects related amounts due from their third-party reinsurers. Any uncollected amounts will represent additional assumed liabilities of the Company and decrease its shareholders’ net income if and when these amounts are determined uncollectible. At December 31, 2010, there were no receivables recorded for paid claims due from third-party reinsurers for this business and unpaid claims related to this business were estimated at $19 million.
As of December 31, 2010, the Company guaranteed that it would compensate the lessors for a shortfall of up to $44 million in the market value of certain leased equipment at the end of each lease. Guarantees of $28 million expire in 2012 and $16 million expire in 2016. The Company had recorded additional liabilities for these guarantees of $11 million as of December 31, 2010.
The Company had indemnification obligations as of December 31, 2010 in connection with acquisition and disposition transactions. These indemnification obligations are triggered by the breach of representations or covenants provided by the Company, such as representations for the presentation of financial statements, the filing of tax returns, compliance with law or the identification of outstanding litigation. These obligations are typically subject to various time limitations, defined by the contract or by operation of law, such as statutes of limitation. In some cases, the maximum potential amount due is subject to contractual limitations based on a percentage of the transaction purchase price, while in other cases limitations are not specified or applicable. The Company does not believe that it is possible to determine the maximum potential amount due under these obligations, since not all amounts due under these indemnification obligations are subject to limitation. There were no liabilities required for these indemnification obligations as of December 31, 2010.
CIGNA CORPORATION – 2010 Form 10-K – 160
The Company has agreements with certain banks that provide banking services to settle claim checks processed by the Company for administrative services only and certain minimum premium customers. The customers are responsible for adequately funding their accounts as claim checks are presented for payment. Under these agreements, the Company guarantees that the banks will not incur a loss if a customer fails to properly fund its account. The amount of the guarantee fluctuates daily. As of December 31, 2010, the aggregate maximum exposure under these guarantees was approximately $366 million and there were no liabilities required. After-tax charges related to these guarantees were approximately $3 million for the year ended December 31, 2010 and there were no charges in 2009. Through February 1, 2011, the exposure that existed at December 31, 2010 has been reduced by approximately 92% through customers’ funding of claim checks when presented for payment. In addition, the Company can limit its exposure under these guarantees by suspending claim payments for any customer who has not adequately funded their bank account.
The Company contracts on an administrative services only basis with customers who fund their own claims. The Company charges these customers administrative fees based on the expected cost of administering their self-funded programs. In some cases, the Company provides performance guarantees associated with meeting certain service related and other performance standards. If these standards are not met, the Company may be financially at risk up to a stated percentage of the contracted fee or a stated dollar amount. The Company establishes liabilities for estimated payouts associated with these guarantees. Approximately 13% of these reported fees were at risk for the periods reported, with actual reimbursements of generally less than 1% of these reported fees in 2010, 2009, and 2008.
The Company does not expect that these certain other guarantees will have a material adverse effect on the Company’s consolidated results of operations, liquidity or financial condition.
D. Regulatory and Industry Developments
Employee benefits regulation. The business of administering and insuring employee benefit programs, particularly health care programs, is heavily regulated by federal and state laws and administrative agencies, such as state departments of insurance and the Federal Departments of Health and Human Services, Labor and Justice, as well as the courts. Regulation and judicial decisions have resulted in changes to industry and the Company’s business practices and will continue to do so in the future. In addition, the Company’s subsidiaries are routinely involved with various claims, lawsuits and regulatory and IRS audits and investigations that could result in financial liability, changes in business practices, or both. Health care regulation in its various forms could have an adverse effect on the Company’s health care operations if it inhibits the Company’s ability to respond to market demands or results in increased medical or administrative costs without improving the quality of care or services.
Other possible regulatory and legislative changes or judicial decisions that could have an adverse effect on the Company’s employee benefits businesses include:
•
additional mandated benefits or services that increase costs;
•
legislation that would grant plan participants broader rights to sue their health plans;
•
changes in public policy and in the political environment, which could affect state and federal law, including legislative and regulatory proposals related to health care issues, which could increase cost and affect the market for the Company’s health care products and services; and pension legislation, which could increase pension cost;
•
changes in Employee Retirement Income Security Act of 1974 (“ERISA”) regulations resulting in increased administrative burdens and costs;
•
additional restrictions on the use of prescription drug formularies and rulings from pending purported class action litigation, which could result in adjustments to or the elimination of the average wholesale price or “AWP” of pharmaceutical products as a benchmark in establishing certain rates, charges, discounts, guarantees and fees for various prescription drugs;
•
additional privacy legislation and regulations that interfere with the proper use of medical information for research, coordination of medical care and disease and disability management;
•
additional variations among state laws mandating the time periods and administrative processes for payment of health care provider claims;
•
legislation that would exempt independent physicians from antitrust laws; and
•
changes in federal tax laws, such as amendments that could affect the taxation of employer provided benefits.
CIGNA CORPORATION – 2010 Form 10-K – 161
The employee benefits industry remains under scrutiny by various state and federal government agencies and could be subject to government efforts to bring criminal actions in circumstances that could previously have given rise only to civil or administrative proceedings.
Guaranty fund assessments. The Company operates in a regulatory environment that may require the Company to participate in assessments under state insurance guaranty association laws. The Company’s exposure to assessments is based on its share of business it writes in the relevant jurisdictions for certain obligations of insolvent insurance companies to policyholders and claimants. For the years ended December 31, 2010, 2009 and 2008, charges related to guaranty fund assessments were not material to the Company’s results of operations.
The Company is aware of an insurer that is in rehabilitation, an intermediate action before insolvency. As of December 31, 2010, the regulator had petitioned the state court for liquidation and the Company believes it is likely that the state court will rule on insolvency for this insurer within the next twelve months. If the insurer is declared insolvent and placed in liquidation, the Company and other insurers may be required to pay a portion of policyholder claims through guaranty fund assessments from various states in which the Company’s insurance subsidiaries write premiums. Based on current information available, which is subject to change, the Company has estimated that potential future assessments could decrease its future results of operations by up to $40 million after-tax. The ultimate amount and timing of any future charges for this potential insolvency will depend on several factors, including the declaration of insolvency and the amount of the potential insolvency, the basis, amount and timing of associated estimated future guaranty fund assessments and the availability and amount of any potential premium tax and other offsets. Cash payments, if any, by the Company’s insurance subsidiaries are likely to extend over several years. The Company will continue to monitor the outcome of the court’s deliberations and may record a liability and expense in a future reporting period.
E. Litigation and Other Legal Matters
The Company is routinely involved in numerous claims, lawsuits, regulatory and IRS audits, investigations and other legal matters arising, for the most part, in the ordinary course of the business of administering and insuring employee benefit programs including payments to providers and benefit level disputes. Litigation of income tax matters is accounted for under FASB’s accounting guidance for uncertainty in income taxes. Further information can be found in Note 20. The outcome of litigation and other legal matters is always uncertain, and outcomes that are not justified by the evidence can occur. The Company believes that it has valid defenses to the legal matters pending against it and is defending itself vigorously.
In accordance with applicable accounting guidance, when litigation and regulatory matters present loss contingencies that are both probable and estimable, the Company accrues the estimated loss by a charge to income. In such cases, there may also be an exposure to loss in excess of the amounts accrued. If it is reasonably possible that a material adverse outcome could develop in excess of any amounts accrued, the matter is disclosed. In many proceedings, however, it is inherently difficult to determine whether any loss is probable or even possible or to estimate the amount of any loss. As a litigation or regulatory matter develops, the Company monitors the matter for further developments that could affect the amount previously accrued, if any, and updates such amount accrued or disclosures previously provided as appropriate.
Based upon its current knowledge, and taking into consideration its current accruals, the Company believes that the legal actions, proceedings and investigations currently pending against it should not have a material adverse effect on the Company’s results of operation, financial condition or liquidity other than possibly the matters referred to in the following paragraphs. However, in light of the uncertainties involved in these matters, there is no assurance that their ultimate resolution will not exceed the amounts currently accrued by the Company and that an adverse outcome in one or more of these matters could be material to the Company’s financial statements, results of operation, financial condition or liquidity for any particular period.
CIGNA CORPORATION – 2010 Form 10-K – 162
Broker compensation. Beginning in 2004, the Company, other insurance companies and certain insurance brokers received subpoenas and inquiries from various regulators, including the New York and Connecticut Attorneys General, the Florida Office of Insurance Regulation, the U.S. Attorney’s Office for the Southern District of California and the U.S. Department of Labor relating to their investigations of insurance broker compensation. CIGNA cooperated with the inquiries and investigations.
On August 1, 2005, two CIGNA subsidiaries, Connecticut General Life Insurance Company and Life Insurance Company of North America, were named as defendants in a multi-district litigation proceeding, In re Insurance Brokerage Antitrust Litigation, consolidated in the United States District Court for the District of New Jersey. The complaint alleges that brokers and insurers conspired to hide commissions, thus increasing the cost of employee benefit plans, and seeks treble damages and injunctive relief. Numerous insurance brokers and other insurance companies are named as defendants. In 2008, the court ordered the clerk to enter judgment against plaintiffs and in favor of the defendants. Plaintiffs appealed. On August 16, 2010, the Third Circuit Court of Appeals affirmed that decision as to employee benefit companies. No appeal was taken. On September 27, 2010, the District Court entered final judgment against plaintiffs consistent with the Third Circuit Court of Appeals’ opinion. Accordingly, the risk of loss is immaterial. This matter is closed and will no longer be reported.
Amara cash balance pension plan litigation. On December 18, 2001, Janice Amara filed a class action lawsuit, captioned Janice C. Amara, Gisela R. Broderick, Annette S. Glanz, individually and on behalf of all others similarly situated v. CIGNA Corporation and CIGNA Pension Plan, in the United States District Court for the District of Connecticut against CIGNA Corporation and the CIGNA Pension Plan on behalf of herself and other similarly situated participants in the CIGNA Pension Plan affected by the 1998 conversion to a cash balance formula. The plaintiffs allege various ERISA violations including, among other things, that the Plan’s cash balance formula discriminates against older employees; the conversion resulted in a wear away period (during which the pre-conversion accrued benefit exceeded the post-conversion benefit); and these conditions are not adequately disclosed in the Plan.
In 2008, the court issued a decision finding in favor of CIGNA Corporation and the CIGNA Pension Plan on the age discrimination and wear away claims. However, the court found in favor of the plaintiffs on many aspects of the disclosure claims and ordered an enhanced level of benefits from the existing cash balance formula for the majority of the class, requiring class members to receive their frozen benefits under the pre-conversion CIGNA Pension Plan and their accrued benefits under the post-conversion CIGNA Pension Plan. The court also ordered, among other things, pre-judgment and post-judgment interest. Both parties appealed the court’s decisions to the United States Court of Appeals for the Second Circuit which issued a decision on October 6, 2009 affirming the District Court’s judgment and order on all issues. On January 4, 2010, the Company and the plaintiffs filed separate petitions for a writ of certiorari to the United States Supreme Court. CIGNA’s petition was granted on June 28, 2010 and was argued on November 30, 2010. The United States Supreme Court held the plaintiffs’ petition for writ of certiorari and the Company expects it to be disposed of when an opinion is issued. The implementation of the judgment is currently stayed. The Company will continue to vigorously defend itself in this case. As of December 31, 2010, the Company is carrying a liability of $82 million pre-tax ($53 million after-tax), which principally reflects the Company’s best estimate of the liabilities related to the court order.
CIGNA CORPORATION – 2010 Form 10-K – 163
Ingenix. On February 13, 2008, State of New York Attorney General Andrew M. Cuomo announced an industry-wide investigation into the use of data provided by Ingenix, Inc., a subsidiary of UnitedHealthcare, used to calculate payments for services provided by out-of-network providers. The Company received four subpoenas from the New York Attorney General’s office in connection with this investigation and responded appropriately. On February 17, 2009, the Company entered into an Assurance of Discontinuance resolving the investigation. In connection with the industry-wide resolution, the Company contributed $10 million to the establishment of a new non-profit company that will compile and provide the data currently provided by Ingenix. In addition, on March 28, 2008, the Company received a voluntary request for production of documents from the Connecticut Attorney General’s office seeking certain out-of-network claim payment information. The Company has responded appropriately. Since January 2009, the Company has received and responded to inquiries regarding the use of Ingenix data from the Illinois and Texas Attorneys General and the Departments of Insurance in Illinois, Florida, Vermont, Georgia, Pennsylvania, Connecticut, and Alaska.
The Company was named as a defendant in a number of putative nationwide class actions asserting that due to the use of data from Ingenix, Inc., the Company improperly underpaid claims, an industry-wide issue. Three actions were brought on behalf of members, (Franco v. CIGNA Corp. et al., Chazen v. CIGNA Corp. et al. and Nelson v. Connecticut General Life Insurance Co. et al.), and three remaining actions were brought on behalf of providers, (American Medical Association et al. v. CIGNA Corp. et al., Shiring et al. v. CIGNA Corp. et al.; and North Peninsula Surgical Center v. Connecticut General Life Insurance Co. et al.), all of which were consolidated into the Franco case pending in the United States District Court for the District of New Jersey. The consolidated amended complaint, filed on August 7, 2009, asserts claims under ERISA, the RICO statute, the Sherman Antitrust Act and New Jersey state law. CIGNA filed a motion to dismiss the consolidated amended complaint on September 9, 2009, which is fully briefed and pending. Plaintiffs filed a motion for class certification on May 28, 2010, which is also fully briefed and pending. Fact and expert discovery have been completed.
On June 9, 2009, CIGNA filed motions in the United States District Court for the Southern District of Florida to enforce a previous settlement, In re Managed Care Litigation, by enjoining the RICO and antitrust causes of action asserted by the provider and medical association plaintiffs in the Ingenix litigation on the ground that they arose prior to and were released in the prior settlement. On November 30, 2009, the Court granted the motions and ordered the provider and association plaintiffs to withdraw their RICO and antitrust claims from the Ingenix litigation by December 21, 2009. The plaintiffs filed notices of appeal with the United States Court of Appeals for the Eleventh Circuit on December 10 and 11, 2009. On April 21, 2010 and June 16, 2010, the appeals were dismissed for lack of appellate jurisdiction. Plaintiffs’ motion for reconsideration was denied on August 18, 2010.
It is reasonably possible that others could initiate additional litigation or additional regulatory action against the Company with respect to use of data provided by Ingenix, Inc. The Company denies the allegations asserted in the investigations and litigation and will vigorously defend itself in these matters.
Due to numerous uncertain and unpredictable factors presented in these cases, including the lack of any clear basis to determine whether and to what extent the claimants have been injured, it is not possible to estimate a range of loss at this time.
In its Form 10-Q for the quarter ended September 30, 2010, CIGNA described the Managed Care cases. The Company believes that any remaining liabilities related to the unresolved Managed Care cases are immaterial to the Company’s results of operation, financial condition or liquidity.
CIGNA CORPORATION – 2010 Form 10-K – 164
Report of Independent Registered Public Accounting Firm
To the Board of Directors and Shareholders of CIGNA Corporation
In our opinion, the accompanying consolidated balance sheets and the related consolidated statements of income, comprehensive income and changes in total equity and cash flows present fairly, in all material respects, the financial position of CIGNA Corporation and its subsidiaries («the Company») at December 31, 2010 and December 31, 2009, and the results of their operations and their cash flows for each of the three years in the period ended December 31, 2010 in conformity with accounting principles generally accepted in the United States of America. Also in our opinion, the Company maintained, in all material respects, effective internal control over financial reporting as of December 31, 2010, based on criteria established in Internal Control - Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (COSO). The Company’s management is responsible for these financial statements, for maintaining effective internal control over financial reporting and for its assessment of the effectiveness of internal control over financial reporting, included in Management’s Annual Report on Internal Control over Financial Reporting. Our responsibility is to express opinions on these financial statements and on the Company’s internal control over financial reporting based on our integrated audits. We conducted our audits in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audits to obtain reasonable assurance about whether the financial statements are free of material misstatement and whether effective internal control over financial reporting was maintained in all material respects. Our audits of the financial statements included examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements, assessing the accounting principles used and significant estimates made by management, and evaluating the overall financial statement presentation. Our audit of internal control over financial reporting included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, and testing and evaluating the design and operating effectiveness of internal control based on the assessed risk. Our audits also included performing such other procedures as we considered necessary in the circumstances. We believe that our audits provide a reasonable basis for our opinions.
A company’s internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company’s internal control over financial reporting includes those policies and procedures that (i) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (ii) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (iii) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company’s assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
/s/ PricewaterhouseCoopers LLP
Philadelphia, Pennsylvania
February 25, 2011
CIGNA CORPORATION – 2010 Form 10-K – 165
Quarterly Financial Data (unaudited)
The following unaudited quarterly financial data is presented on a consolidated basis for each of the years ended December 31, 2010 and 2009. Quarterly financial results necessarily rely heavily on estimates. This and certain other factors, such as the seasonal nature of portions of the insurance business, suggest the need to exercise caution in drawing specific conclusions from quarterly consolidated results.
|
(In millions, except per share amounts) |
Three Months Ended |
||||
|
March 31 |
June 30 |
Sept. 30 |
Dec. 31 |
||
|
Consolidated Results | |||||
|
2010 | |||||
|
Total revenues |
$5,205 |
$5,353 |
$5,266 |
$5,429 |
|
|
Income from continuing operations before income taxes |
422 |
439 |
464 |
545 |
|
|
Shareholders’ net income |
283(1) |
294(2) |
307(3) |
461(4) |
|
|
Shareholders’ net income per share: | |||||
|
Basic |
1.03 |
1.07 |
1.13 |
1.71 |
|
|
Diluted |
1.02 |
1.06 |
1.13 |
1.69 |
|
|
2009 | |||||
|
Total revenues |
$4,773 |
$4,488 |
$4,517 |
$4,636 |
|
|
Income from continuing operations before income taxes |
273 |
630 |
487 |
508 |
|
|
Shareholders’ net income (loss) |
208(5) |
435(6) |
329(7) |
330(8) |
|
|
Shareholders’ net income (loss) per share: | |||||
|
Basic |
0.76 |
1.59 |
1.20 |
1.20 |
|
|
Diluted |
0.76 |
1.58 |
1.19 |
1.19 |
|
|
Stock and Dividend Data | |||||
|
2010 | |||||
|
Price range of common stock |
— high |
$39.26 |
$37.61 |
$36.03 |
$38.53 |
|
— low |
$32.00 |
$30.78 |
$29.12 |
$34.33 |
|
|
Dividends declared per common share |
$0.040 |
$— |
$— |
$— |
|
|
2009 | |||||
|
Price range of common stock |
— high |
$23.06 |
$25.60 |
$33.00 |
$38.12 |
|
— low |
$12.68 |
$16.84 |
$23.10 |
$26.83 |
|
|
Dividends declared per common share |
$0.040 |
$— |
$— |
$— |
|
|
(1) The first quarter of 2010 includes an after-tax gain of $5 million for the GMIB business. (2) The second quarter of 2010 includes an after-tax loss of $104 million for the GMIB business. (3) The third quarter of 2010 includes an after-tax loss of $10 million for the GMIB business. (4) The fourth quarter of 2010 includes an after-tax gain of $85 million for the GMIB business, an after-tax charge of $20 million for the loss on a reinsurance transaction, a net tax benefit of $101 million related to the resolution of a Federal tax matter, and an after-tax charge of $39 million related to the early extinguishment of debt. (5) The first quarter of 2009 includes an after-tax gain of $23 million for the GMIB business, an after-tax benefit of $20 million associated with the completion of the 2005 and 2006 IRS examinations and an after-tax charge of $47 million to strengthen GMDB reserves. (6) The second quarter of 2009 includes an after-tax gain of $110 million for the GMIB business, an after-tax benefit of $30 million associated with a pension curtailment gain, and an after-tax charge of $9 million for the cost reduction program. (7) The third quarter of 2009 includes an after-tax gain of $16 million for the GMIB business and an after-tax charge of $7 million for the cost reduction program. (8) The fourth quarter of 2009 includes an after-tax gain of $60 million for the GMIB business and an after-tax charge of $13 million for the cost reduction program. |
|||||
CIGNA CORPORATION – 2010 Form 10-K – 166
FIVE-YEAR CUMULATIVE TOTAL SHAREHOLDER RETURN*
December 30, 2005 — December 31, 2010
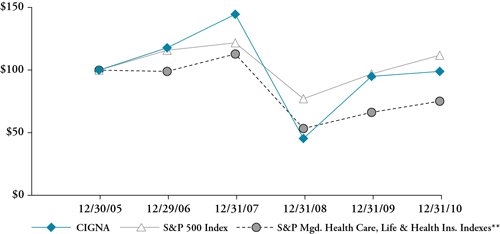
|
12/30/2005 |
12/29/2006 |
12/31/2007 |
12/31/2008 |
12/31/2009 |
12/31/2010 |
|
|
CIGNA |
$100 |
$118 |
$145 |
$45 |
$95 |
$99 |
|
S&P 500 Index |
$100 |
$116 |
$122 |
$77 |
$97 |
$112 |
|
S&P Mgd. Health Care, Life & Health Ins. Indexes** |
$100 |
$99 |
$113 |
$53 |
$66 |
$75 |
|
* Assumes that the value of the investment in CIGNA common stock and each index was $100 on December 30, 2005 and that all dividends were reinvested. ** Weighted average of S&P Managed Health Care (75%) and Life & Health Insurance (25%) Indexes. |
||||||
CIGNA CORPORATION – 2010 Form 10-K – 167
ITEM 9 Changes in and Disagreements with Accountants on Accounting and Financial Disclosure
None.
ITEM 9A Controls and Procedures
A. Disclosure Controls and Procedures
Based on an evaluation of the effectiveness of CIGNA’s disclosure controls and procedures conducted under the supervision and with the participation of CIGNA’s management, CIGNA’s Chief Executive Officer and Acting Chief Financial Officer concluded that, as of the end of the period covered by this report, CIGNA’s disclosure controls and procedures are effective to ensure that information required to be disclosed by CIGNA in the reports that it files or submits under the Exchange Act is recorded, processed, summarized and reported, within the time periods specified in the SEC’s rules and forms.
B. Internal Control Over Financial Reporting
Management’s Annual Report on Internal Control over Financial Reporting
The Company’s management report on internal control over financial reporting under the caption “Management’s Annual Report on Internal Control over Financial Reporting” on page 97 in this Form 10-K.
Attestation Report of the Registered Public Accounting Firm
The attestation report of CIGNA’s independent registered public accounting firm, on the effectiveness of CIGNA’s internal control over financial reporting appears under the caption “Report of Independent Registered Public Accounting Firm” on page 165 of this Form 10-K.
Changes in Internal Control Over Financial Reporting
There have been no changes in CIGNA’s internal control over financial reporting identified in connection with the evaluation described in the above paragraph that have materially affected, or are reasonably likely to materially affect, CIGNA’s internal control over financial reporting.
ITEM 9B Other Information
None.
|
PART III |
ITEM 10 Directors and Executive Officers of the Registrant
A. Directors of the Registrant
The information under the captions “The Board of Directors’ Nominees for Terms to Expire in April 2013”, “Directors Who Will Continue in Office”, “Board of Directors and Committee Meetings, Membership, Attendance and Independence” (as it relates to Audit Committee disclosure), and “Section 16(a) Beneficial Ownership Reporting Compliance” in CIGNA’s proxy statement to be dated on or about March 18, 2011 is incorporated by reference.
B. Executive Officers of the Registrant
See PART I — “Executive Officers of the Registrant on page 44 in this Form 10-K.”
CIGNA CORPORATION – 2010 Form 10-K – 168
C. Code of Ethics and Other Corporate Governance Disclosures
CIGNA’s Code of Ethics is the Company’s code of business conduct and ethics, and applies to CIGNA’s directors, officers (including the chief executive officer, acting chief financial officer and chief accounting officer) and employees. The Code of Ethics is posted on the Corporate Governance section found on the “About Us” page of the Company’s website, www.cigna.com. In the event the Company substantively amends its Code of Ethics or waives a provision of the Code, CIGNA intends to disclose the amendment or waiver on the Corporate Governance section of the Company’s website.
In addition, the Company’s corporate governance guidelines (Board Practices) and the charters of its board committees (audit, corporate governance, executive, finance and people resources) are available on the Corporate Governance section of the Company’s website. These corporate governance documents, as well as the Code of Ethics, are available in print to any shareholder who requests them.
ITEM 11 Executive Compensation
The information under the captions “Director Compensation”, “Report of the People Resources Committee”, “Compensation Discussion and Analysis” and “Executive Compensation” in CIGNA’s proxy statement to be dated on or about March 18, 2011 is incorporated by reference.
CIGNA CORPORATION – 2010 Form 10-K – 169
ITEM 12 Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters
The following table presents information regarding CIGNA’s equity compensation plans as of December 31, 2010:
|
Plan Category |
(a)(1) Securities To Be Issued Upon Exercise Of Outstanding Options, Warrants And Rights |
(b)(2) Weighted Average Exercise Price Per Share Of Outstanding Options, Warrants And Rights |
(c)(3) Securities Remaining Available For Future Issuance Under Equity Compensation Plans (Excluding Securities Reflected In Column (a)) |
|
Equity Compensation Plans Approved by Security Holders |
13,189,506 |
$31.10 |
7,548,136 |
|
Equity Compensation Plans Not Approved by Security Holders |
— |
— |
— |
|
TOTAL |
13,189,506 |
$31.10 |
7,548,136 |
|
(1) In addition to outstanding options, includes 112,524 restricted stock units, 82,297 deferred shares, 41,457 director deferred share units that settle in shares, and 860,004 strategic performance shares which are reported at the maximum 200% payout rate. (2) The weighted-average exercise price is based only on outstanding options. (3) Includes 448,790 shares of common stock available as of the close of business December 31, 2010 for future issuance under the CIGNA Directors Equity Plan; and 2,644,719 shares of common stock available as of the close of business on December 31, 2010 for future issuance under the CIGNA Long-Term Incentive Plan as shares of restricted stock, shares in payment of dividend equivalent rights, shares in lieu of cash payable under a Qualifying Plan, or shares in payment of strategic performance units or strategic performance shares. |
|||
The information under the captions “Stock held by Directors, Nominees and Executive Officers” and “Largest Security Holders” in CIGNA’s proxy statement to be dated on or about March 18, 2011 is incorporated by reference.
ITEM 13 Certain Relationships and Related Transactions
The information under the caption “Certain Transactions” in CIGNA’s proxy statement to be dated on or about March 18, 2011 is incorporated by reference.
ITEM 14 Principal Accounting Fees and Services
The information under the captions “Policy for the Pre-Approval of Audit and Non-Audit Services” and “Fees to Independent Registered Public Accounting Firm” in CIGNA’s proxy statement to be dated on or about March 18, 2011 is incorporated by reference.
CIGNA CORPORATION – 2010 Form 10-K – 170
|
PART IV |
ITEM 15 Exhibits and Financial Statement Schedules
|
(a) |
1. The following Financial Statements appear on pages 99 through 165: |
|
|
Consolidated Statements of Income for the years ended December 31, 2010, 2009 and 2008. |
||
|
Consolidated Balance Sheets as of December 31, 2010 and 2009. |
||
|
Consolidated Statements of Comprehensive Income and Changes in Total Equity for the years ended December 31, 2010, 2009 and 2008. |
||
|
Consolidated Statements of Cash Flows for the years ended December 31, 2010, 2009 and 2008. |
||
|
Notes to the Consolidated Financial Statements. |
||
|
Report of Independent Registered Public Accounting Firm. |
||
|
2. The financial statement schedules are listed in the Index to Financial Statement Schedules on page FS1. |
||
|
3. The exhibits are listed in the Index to Exhibits beginning on page E1. |
||
CIGNA CORPORATION – 2010 Form 10-K – 171
Signatures
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized.
|
CIGNA CORPORATION |
|
|
Date: |
February 25, 2011 |
|
By: |
/s/ THOMAS A. MCCARTHY |
|
Name: |
Thomas A. McCarthy |
|
Title: |
Acting Chief Financial Officer (Principal Financial Officer) |
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed below by the following persons on behalf of the registrant and in the capacities indicated as of February 25, 2011.
|
Signature |
Title |
|
/s/ DAVID M. CORDANI |
|
|
David M. Cordani |
Chief Executive Officer and Director (Principal Executive Officer) |
|
/s/ THOMAS A. MCCARTHY |
|
|
Thomas A. McCarthy |
Acting Chief Financial Officer (Principal Financial Officer) |
|
/s/ MARY T. HOELTZEL |
|
|
Mary T. Hoeltzel |
Vice President and Chief Accounting Officer (Principal Accounting Officer) |
|
/s/ ISAIAH HARRIS, JR. |
|
|
Isaiah Harris, Jr. |
Chairman of the Board |
|
/s/ JANE E. HENNEY, M.D. |
|
|
Jane E. Henney, M.D. |
Director |
|
/s/ ROMAN MARTINEZ IV |
|
|
Roman Martinez IV |
Director |
|
/s/ JOHN M. PARTRIDGE |
|
|
John M. Partridge |
Director |
CIGNA CORPORATION – 2010 Form 10-K – 172
|
Signature |
Title |
|
/s/ JAMES E. ROGERS |
|
|
James E. Rogers |
Director |
|
/s/ JOSEPH P. SULLIVAN |
|
|
Joseph P. Sullivan |
Director |
|
/s/ CAROL COX WAIT |
|
|
Carol Cox Wait |
Director |
|
/s/ ERIC C. WISEMAN |
|
|
Eric C. Wiseman |
Director |
|
/s/ DONNA F. ZARCONE |
|
|
Donna F. Zarcone |
Director |
|
/s/ WILLIAM D. ZOLLARS |
|
|
William D. Zollars |
Director |
CIGNA CORPORATION – 2010 Form 10-K – 173
{THIS PAGE INTENTIONALLY LEFT BLANK}
CIGNA CORPORATION – 2010 Form 10-K – 174
|
Report of Independent Registered Public Accounting Firm on Financial Statement Schedules |
Schedules
|
I Summary of Investments — Other Than Investments in Related Parties as of December 31, 2010 |
|
II Condensed Financial Information of CIGNA Corporation (Registrant) |
Schedules other than those listed above are omitted because they are not required or are not applicable, or the required information is shown in the financial statements or notes thereto.
CIGNA CORPORATION – 2010 Form 10-K – FS-1
Report of Independent Registered Public Accounting Firm on Financial Statement Schedules
To the Board of Directors and Shareholders of CIGNA Corporation
Our audits of the consolidated financial statements and of the effectiveness of internal control over financial reporting referred to in our report dated February 25, 2011 (which report and consolidated financial statements are included under Item 8 in this Annual Report on Form 10-K) also included an audit of the financial statement schedules listed in Item 15(a)(2) of this Form 10-K. In our opinion, these financial statement schedules present fairly, in all material respects, the information set forth therein when read in conjunction with the related consolidated financial statements.
|
/s/ PricewaterhouseCoopers LLP |
|
Philadelphia, Pennsylvania |
|
February 25, 2011 |
CIGNA CORPORATION – 2010 Form 10-K – FS-2
CIGNA Corporation and Subsidiaries Schedule I — Summary of Investments — Other than Investments in Related Parties — December 31, 2010 (In millions)
|
Type of Investment |
Cost |
Fair Value |
Amount at which shown in the Consolidated Balance Sheet |
|
Fixed maturities: | |||
|
Bonds: | |||
|
United States government and government agencies and authorities |
$459 |
$687 |
$687 |
|
States, municipalities and political subdivisions |
2,305 |
2,467 |
2,467 |
|
Foreign governments |
1,109 |
1,169 |
1,169 |
|
Public utilities |
88 |
93 |
93 |
|
All other corporate bonds |
8,801 |
9,516 |
9,516 |
|
Asset backed securities: | |||
|
United States government agencies mortgage-backed |
9 |
10 |
10 |
|
Other mortgage-backed |
81 |
88 |
88 |
|
Other asset-backed |
569 |
656 |
656 |
|
Redeemable preferred stocks |
24 |
23 |
23 |
|
TOTAL FIXED MATURITIES |
13,445 |
14,709 |
14,709 |
|
Equity securities: | |||
|
Common stocks: | |||
|
Industrial, miscellaneous and all other |
27 |
32 |
32 |
|
Non redeemable preferred stocks |
117 |
95 |
95 |
|
TOTAL EQUITY SECURITIES |
144 |
127 |
127 |
|
Commercial mortgage loans on real estate |
3,486 |
3,486 |
|
|
Policy loans |
1,581 |
1,581 |
|
|
Real estate investments |
112 |
112 |
|
|
Other long-term investments |
705 |
759 |
|
|
Short-term investments |
174 |
174 |
|
|
TOTAL INVESTMENTS |
$19,647 |
|
$20,948 |
CIGNA CORPORATION – 2010 Form 10-K – FS-3
CIGNA Corporation and Subsidiaries Schedule II — Condensed Financial Information of CIGNA Corporation (Registrant)
Statements of Income
|
(In millions) |
For the year ended December 31, |
||
|
2010 |
2009 |
2008 |
|
|
Operating expenses: | |||
|
Interest |
$176 |
$160 |
$140 |
|
Intercompany interest |
26 |
80 |
220 |
|
Other |
129 |
68 |
108 |
|
TOTAL OPERATING EXPENSES |
331 |
308 |
468 |
|
Loss before income taxes |
(331) |
(308) |
(468) |
|
Income tax benefit |
(106) |
(118) |
(161) |
|
Loss of parent company |
(225) |
(190) |
(307) |
|
Equity in income of subsidiaries from continuing operations |
1,570 |
1,491 |
595 |
|
Shareholders’ income from continuing operations |
1,345 |
1,301 |
288 |
|
Income from discontinued operations, net of taxes |
— |
1 |
4 |
|
SHAREHOLDERS’ NET INCOME |
$1,345 |
$1,302 |
$292 |
|
See Notes to Financial Statements on pages FS-7 through FS-9. |
|||
CIGNA CORPORATION – 2010 Form 10-K – FS-4
CIGNA Corporation and Subsidiaries Schedule II — Condensed Financial Information of CIGNA Corporation (Registrant)
Balance Sheets
|
(In millions) |
As of December 31, |
|||
|
2010 |
2009 |
|||
|
ASSETS: | ||||
|
Investments in subsidiaries |
$14,384 |
$13,674 |
||
|
Other assets |
568 |
586 |
||
|
TOTAL ASSETS |
$14,952 |
|
$14,260 |
|
|
LIABILITIES: | ||||
|
Intercompany |
$3,718 |
$4,517 |
||
|
Short-term debt |
548 |
100 |
||
|
Long-term debt |
2,180 |
2,347 |
||
|
Other liabilities |
1,861 |
1,879 |
||
|
TOTAL LIABILITIES |
|
8,307 |
|
8,843 |
|
SHAREHOLDERS’ EQUITY: | ||||
|
Common stock (shares issued, 351; authorized, 600) |
88 |
88 |
||
|
Additional paid-in capital |
2,534 |
2,514 |
||
|
Net unrealized appreciation — fixed maturities |
$529 |
$378 | ||
|
Net unrealized appreciation — equity securities |
3 |
4 | ||
|
Net unrealized depreciation — derivatives |
(24) |
(30) | ||
|
Net translation of foreign currencies |
25 |
(12) | ||
|
Postretirement benefits liability adjustment |
(1,147) |
(958) | ||
|
Accumulated other comprehensive loss |
(614) |
(618) |
||
|
Retained earnings |
9,879 |
8,625 |
||
|
Less treasury stock, at cost |
(5,242) |
(5,192) |
||
|
TOTAL SHAREHOLDERS’ EQUITY |
|
6,645 |
|
5,417 |
|
TOTAL LIABILITIES AND SHAREHOLDERS’ EQUITY |
|
$14,952 |
|
$14,260 |
|
See Notes to Financial Statements on pages FS-7 through FS-9. |
||||
CIGNA CORPORATION – 2010 Form 10-K – FS-5
CIGNA Corporation and Subsidiaries Schedule II — Condensed Financial Information of CIGNA Corporation (Registrant)
Statements of Cash Flows
|
(In millions) |
For the year ended December 31, |
||
|
2010 |
2009 |
2008 |
|
|
Cash Flows from Operating Activities: | |||
|
Shareholders’ Net Income |
$1,345 |
$1,302 |
$292 |
|
Adjustments to reconcile shareholders’ net income to net cash provided by operating activities: | |||
|
Equity in income of subsidiaries |
(1,574) |
(1,494) |
(595) |
|
(Income) from discontinued operations |
— |
(1) |
(4) |
|
Dividends received from subsidiaries |
1,050 |
650 |
535 |
|
Other liabilities |
(294) |
(401) |
74 |
|
Other, net |
162 |
356 |
(116) |
|
Net cash provided by operating activities |
689 |
412 |
186 |
|
Cash Flows from Financing Activities: | |||
|
Net change in intercompany debt |
(816) |
(579) |
(426) |
|
Net change in short-term debt |
— |
(199) |
299 |
|
Net proceeds on issuance of long-term debt |
543 |
346 |
297 |
|
Repayment of long-term debt |
(268) |
— |
— |
|
Issuance of common stock |
64 |
30 |
37 |
|
Common dividends paid |
(11) |
(11) |
(14) |
|
Repurchase of common stock |
(201) |
— |
(378) |
|
Net cash used in financing activities |
(689) |
(413) |
(185) |
|
Net increase (decrease) in cash and cash equivalents |
— |
(1) |
1 |
|
Cash and cash equivalents, beginning of year |
— |
1 |
— |
|
Cash and cash equivalents, end of year |
$— |
$— |
$1 |
|
See Notes to Financial Statements on pages FS-7 through FS-9. |
|||
CIGNA CORPORATION – 2010 Form 10-K – FS-6
CIGNA Corporation and Subsidiaries Schedule II — Condensed Financial Information of CIGNA Corporation (Registrant)
Notes to Condensed Financial Statements
The accompanying condensed financial statements should be read in conjunction with the Consolidated Financial Statements and the accompanying notes thereto in the Annual Report on Form 10-K.
Note 1 — For purposes of these condensed financial statements, CIGNA Corporation’s (the Company) wholly owned and majority owned subsidiaries are recorded using the equity basis of accounting. Certain reclassifications have been made to prior years’ amounts to conform to the 2010 presentation.
Note 2 — Short-term and long-term debt consisted of the following at December 31:
|
(In millions) |
2010 |
2009 |
|
Short-term: | ||
|
Commercial Paper |
$100 |
$100 |
|
Current maturities of long-term debt |
448 |
— |
|
TOTAL SHORT-TERM DEBT |
$548 |
$100 |
|
Long-term: | ||
|
Uncollateralized debt: | ||
|
7% Notes due 2011 |
$— |
$222 |
|
6.375% Notes due 2011 |
— |
226 |
|
5.375% Notes due 2017 |
250 |
250 |
|
6.35% Notes due 2018 |
131 |
300 |
|
8.5% Notes due 2019 |
251 |
349 |
|
4.38% Notes due 2020 |
249 |
— |
|
5.13% Notes due 2020 |
299 |
— |
|
7.65% Notes due 2023 |
100 |
100 |
|
8.3% Notes due 2023 |
17 |
17 |
|
7.875% Debentures due 2027 |
300 |
300 |
|
8.3% Step Down Notes due 2033 |
83 |
83 |
|
6.15% Notes due 2036 |
500 |
500 |
|
TOTAL LONG-TERM DEBT |
$2,180 |
$2,347 |
On December 1, 2010 the Company offered to settle its 8.5% Notes due 2019, including accrued interest from November 1 through the settlement date. The tender price equaled the present value of the remaining principal and interest payments on the Notes being redeemed, discounted at a rate equal to the 10-year treasury rate plus a fixed spread of 100 basis points. The tender offer priced at a yield of 4.128% and principal of $99 million was tendered, with $251 million remaining outstanding. The Company paid $130 million, including accrued interest and expenses, to settle the Notes, resulting in an after-tax loss on early debt extinguishment of $21 million.
On December 9, 2010 the Company offered to settle its 6.35% Notes due 2018, including accrued interest from September 16 through the settlement date. The tender price equaled the present value of the remaining principal and interest payments on the Notes being redeemed, discounted at a rate equal to the 10-year treasury rate plus a fixed spread of 45 basis points. The tender offer priced at a yield of 3.923% and principal of $169 million was tendered, with $131 million remaining outstanding. The Company paid $198 million, including accrued interest and expenses, to settle the Notes, resulting in an after-tax loss on early debt extinguishment of $18 million.
On December 8, 2010, the Company issued $250 million of 4.375% Notes ($249 million net of debt discount, with an effective interest rate of 5.1%). The difference between the stated and effective interest rates primarily reflects the effect of treasury locks. Interest is payable on June 15 and December 15 of each year beginning in 2010. These Notes will mature on December 15, 2020. The proceeds of this debt were used to fund the tender offer for the 8.5% Senior Notes due 2019 and the 6.35% Senior Notes due 2018 described above.
CIGNA CORPORATION – 2010 Form 10-K – FS-7
During 2010, the 7% Notes and 6.375% Notes due 2011 were reclassified into current maturities of long-term debt since they will mature in less than one year.
On May 12, 2010, the Company issued $300 million of 5.125% Notes ($299 million, net of debt discount, with an effective interest rate of 5.36% per year). Interest is payable on June 15 and December 15 of each year beginning December 15, 2010. These Notes will mature on June 15, 2020. The proceeds of this debt were used for general corporate purposes.
On May 4, 2009 the Company issued $350 million of 8.5% Notes ($349 million, net of debt discount, with an effective interest rate of 9.90% per year). The difference between the stated and effective interest rates primarily reflects the effect of treasury locks. Interest is payable on May 1 and November 1 of each year beginning November 1, 2009. These Notes will mature on May 1, 2019. As described above, a portion of these Notes were settled in 2010 through a tender offer.
The Company may redeem the Notes issued in May of 2010 and 2009, at any time, in whole or in part, at a redemption price equal to the greater of:
•
100% of the principal amount of the Notes to be redeemed; or
•
the present value of the remaining principal and interest payments on the Notes being redeemed discounted at the applicable Treasury Rate plus 25 basis points 4.375% and 5.125% Notes due 2020 and 50 basis points for the 8.5% Notes due 2019.
Maturities of debt are as follows (in millions): $448 in 2011, none in 2012, 2013 and 2014 and the remainder in years after 2014. Interest expense on short-term and long-term debt was $176 million in 2010, $160 million in 2009, and $140 million in 2008.
Interest paid on short-term and long-term debt amounted to $175 million, $153 million and $135 million for 2010, 2009 and 2008, respectively.
On March 14, 2008, the Company entered into a commercial paper program (“the Program”). Under the Program, the Company is authorized to sell from time to time short-term unsecured commercial paper notes up to a maximum of $500 million. The proceeds are used for general corporate purposes, including working capital, capital expenditures, acquisitions and share repurchases. The Company uses the credit facility entered into in June 2007, as back-up liquidity to support the outstanding commercial paper. If at any time funds are not available on favorable terms under the Program, the Company may use its credit facility for funding. In October 2008, the Company added an additional dealer to its Program. As of December 31, 2010, the Company had $100 million in commercial paper outstanding, at a weighted average interest rate of 0.38%, used for corporate purposes.
In June 2007, the Company amended and restated its five-year revolving credit and letter of credit agreement for $1.75 billion, which permits up to $1.25 billion to be used for letters of credit. The agreement includes options, which are subject to consent by the administrative agent and the committing bank, to increase the commitment amount up to $2.0 billion and to extend the term of the agreement. The Company entered into the agreement for general corporate purposes, including the support for the issuance of commercial paper and to obtain statutory reserve credit for certain reinsurance arrangements. There were letters of credit issued in the amount of $82 million as of December 31, 2010. As of December 31, 2010, the Company had an additional $1.7 billion of borrowing capacity within the maximum debt leverage covenant in the line of credit agreement in addition to the $2.7 billion of short-term and long-term debt outstanding.
Note 3 — Intercompany liabilities consist primarily of loans payable to CIGNA Holdings, Inc. of $3.7 billion as of December 31, 2010 and $4.6 billion as of December 31, 2009. Interest was accrued at an average monthly rate of 0.61% and 1.56% for 2010 and 2009, respectively.
CIGNA CORPORATION – 2010 Form 10-K – FS-8
Note 4 — As of December 31, 2010, the Company had guarantees and similar agreements in place to secure payment obligations or solvency requirements of certain wholly owned subsidiaries as follows:
•
The Company has arranged for bank letters of credit in the amount of $37 million in support of its indirect wholly owned subsidiaries. As of December 31, 2010, approximately $33 million of the letters of credit were issued to support CIGNA Global Reinsurance Company, an indirect wholly owned subsidiary domiciled in Bermuda. These letters of credit primarily secure the payment of insureds’ claims from run-off reinsurance operations. As of December 31, 2010, approximately $4 million of the letters of credit were issued to provide collateral support for various other indirectly wholly owned subsidiaries of the Company.
•
The Company has provided a capital commitment deed in an amount up to $185 million in favor of CIGNA Global Reinsurance Company. This deed is equal to the letters of credit securing the payment of insureds’ claims from run-off reinsurance operations. This deed is required by Bermuda regulators to have these letters of credit for the London run-off reinsurance operations included as admitted assets.
•
Various indirect, wholly owned subsidiaries have obtained surety bonds in the normal course of business. If there is a claim on a surety bond and the subsidiary is unable to pay, the Company guarantees payment to the company issuing the surety bond. The aggregate amount of such surety bonds as of December was $61 million.
•
The Company is obligated under a $27 million letter of credit required by the insurer of its high-deductible self-insurance programs to indemnify the insurer for claim liabilities that fall within deductible amounts for policy years dating back to 1994.
•
The Company also provides solvency guarantees aggregating $34 million under state and federal regulations in support of its indirect wholly owned medical HMOs in several states.
•
The Company has arranged a $55 million letter of credit in support of CIGNA Europe Insurance Company, an indirect wholly owned subsidiary. The Company has agreed to indemnify the banks providing the letters of credit in the event of any draw. CIGNA Europe Insurance Company is the holder of the letters of credit.
•
In addition, the Company has agreed to indemnify payment of losses included in CIGNA Europe Insurance Company’s reserves on the assumed reinsurance business transferred from ACE. As of December 31, 2010, the reserve was $95 million.
In 2010, no payments have been made on these guarantees and none are pending. The Company provided other guarantees to subsidiaries that, in the aggregate, do not represent a material risk to the Company’s results of operations, liquidity or financial condition.
CIGNA CORPORATION – 2010 Form 10-K – FS-9
CIGNA Corporation and Subsidiaries Schedule III — Supplementary Insurance Information
|
Segment (In millions) |
Deferred policy acquisition costs |
Future policy benefits and contractholder deposit funds |
Medical claims payable and unpaid claims |
Unearned premiums and fees |
|
Year Ended December 31, 2010: | ||||
|
Health Care |
$54 |
$488 |
$1,400 |
$80 |
|
Disability and Life |
2 |
1,066 |
3,180 |
17 |
|
International |
998 |
1,173 |
288 |
288 |
|
Run-off Reinsurance |
— |
1,139 |
244 |
— |
|
Other Operations |
68 |
12,790 |
159 |
31 |
|
Corporate |
— |
— |
(8) |
— |
|
TOTAL |
$1,122 |
$16,656 |
$5,263 |
$416 |
|
Year Ended December 31, 2009: | ||||
|
Health Care |
$60 |
$507 |
$1,098 |
$76 |
|
Disability and Life |
6 |
1,023 |
3,122 |
32 |
|
International |
808 |
1,003 |
228 |
282 |
|
Run-off Reinsurance |
— |
1,287 |
288 |
— |
|
Other Operations |
69 |
12,800 |
161 |
37 |
|
Corporate |
— |
— |
(8) |
— |
|
TOTAL |
$943 |
$16,620 |
$4,889 |
$427 |
|
Year Ended December 31, 2008: | ||||
|
Health Care |
$60 |
$551 |
$1,138 |
$70 |
|
Disability and Life |
7 |
956 |
3,104 |
36 |
|
International |
650 |
843 |
205 |
265 |
|
Run-off Reinsurance |
— |
1,611 |
356 |
— |
|
Other Operations |
72 |
13,332 |
158 |
43 |
|
Corporate |
— |
— |
— |
— |
|
TOTAL |
$789 |
$17,293 |
$4,961 |
$414 |
CIGNA CORPORATION – 2010 Form 10-K – FS-10
|
Premiums and fees (1) |
Net investment income (2) |
Benefit |
Amortization of deferred policy |
Other operating expenses (4) |
|
$13,319 |
$243 |
$8,670 |
$155 |
$5,086 |
|
2,667 |
261 |
1,935 |
6 |
699 |
|
2,268 |
82 |
1,255 |
145 |
639 |
|
25 |
114 |
(22) |
— |
113 |
|
114 |
404 |
395 |
6 |
53 |
|
— |
1 |
— |
— |
248 |
|
$18,393 |
$1,105 |
$12,233 |
$312 |
$6,838 |
|
$11,384 |
$181 |
$7,096 |
$141 |
$4,742 |
|
2,634 |
244 |
1,922 |
6 |
670 |
|
1,882 |
69 |
1,080 |
146 |
491 |
|
29 |
113 |
(146) |
— |
(273) |
|
112 |
407 |
398 |
6 |
62 |
|
— |
— |
(16) |
— |
191 |
|
$16,041 |
$1,014 |
$10,334 |
$299 |
$5,883 |
|
$11,665 |
$200 |
$7,445 |
$138 |
$4,737 |
|
2,562 |
256 |
1,914 |
6 |
633 |
|
1,870 |
79 |
1,003 |
164 |
512 |
|
43 |
104 |
782 |
— |
717 |
|
113 |
414 |
408 |
6 |
54 |
|
— |
10 |
(15) |
— |
215 |
|
$16,253 |
$1,063 |
$11,537 |
$314 |
$6,868 |
|
(1) Amounts presented are shown net of the effects of reinsurance. See Note 8 to the Consolidated Financial Statements included in CIGNA’s 2010 Annual Report on Form 10-K. (2) The allocation of net investment income is based upon the investment year method, the identification of certain portfolios with specific segments, or a combination of both. (3) Benefit expenses include Health Care medical claims expense and other benefit expenses. (4) Other operating expenses include mail order pharmacy cost of goods sold, GMIB fair value (gain) loss and other operating expenses, and excludes amortization of deferred policy acquisition expenses. |
||||
CIGNA CORPORATION – 2010 Form 10-K – FS-11
CIGNA Corporation and Subsidiaries Schedule IV — Reinsurance
|
(In millions) |
Gross amount |
Ceded to other companies |
Assumed from other companies |
Net amount |
Percentage of amount assumed to net |
|
Year Ended December 31, 2010: | |||||
|
Life insurance in force |
$566,841 |
$44,335 |
$9,734 |
$532,240 |
1.8% |
|
Premiums and fees: | |||||
|
Life insurance and annuities |
$2,026 |
$264 |
$107 |
$1,869 |
5.7% |
|
Accident and health insurance |
16,272 |
173 |
425 |
16,524 |
2.6% |
|
TOTAL |
$18,298 |
$437 |
$532 |
$18,393 |
2.9% |
|
Year Ended December 31, 2009: | |||||
|
Life insurance in force |
$544,687 |
$50,011 |
$71,107 |
$565,783 |
12.6% |
|
Premiums and fees: | |||||
|
Life insurance and annuities |
$1,909 |
$297 |
$305 |
$1,917 |
15.9% |
|
Accident and health insurance |
13,476 |
156 |
804 |
14,124 |
5.7% |
|
TOTAL |
$15,385 |
$453 |
$1,109 |
$16,041 |
6.9% |
|
Year Ended December 31, 2008: | |||||
|
Life insurance in force |
$392,803 |
$44,116 |
$108,106 |
$456,793 |
23.7% |
|
Premiums and fees: | |||||
|
Life insurance and annuities |
$1,885 |
$281 |
$333 |
$1,937 |
17.2% |
|
Accident and health insurance |
13,605 |
230 |
941 |
14,316 |
6.6% |
|
TOTAL |
$15,490 |
$511 |
$1,274 |
$16,253 |
7.8% |
CIGNA CORPORATION – 2010 Form 10-K – FS-12
CIGNA Corporation and Subsidiaries Schedule V — Valuation and Qualifying Accounts and Reserves
|
Description (In millions) |
Balance at beginning of period |
Charged (Credited) to costs and expenses (1) |
Charged (Credited) to other accounts |
Other deductions —describe (2) |
Balance at end of period |
|
2010: | |||||
|
Investment asset valuation reserves: | |||||
|
Commercial mortgage loans |
$17 |
$24 |
$— |
$(29) |
$12 |
|
Allowance for doubtful accounts: | |||||
|
Premiums, accounts and notes receivable |
$43 |
$11 |
$— |
$(5) |
$49 |
|
Deferred tax asset valuation allowance |
$116 |
$(93) |
$— |
$— |
$23 |
|
Reinsurance recoverables |
$15 |
$(5) |
$— |
$— |
$10 |
|
2009: | |||||
|
Investment asset valuation reserves: | |||||
|
Commercial mortgage loans |
$3 |
$17 |
$— |
$(3) |
$17 |
|
Allowance for doubtful accounts: | |||||
|
Premiums, accounts and notes receivable |
$50 |
$(2) |
$— |
$(5) |
$43 |
|
Deferred tax asset valuation allowance |
$126 |
$(2) |
$— |
$(8) |
$116 |
|
Reinsurance recoverables |
$23 |
$(7) |
$— |
$(1) |
$15 |
|
2008: | |||||
|
Investment asset valuation reserves: | |||||
|
Commercial mortgage loans |
$1 |
$2 |
$— |
$— |
$3 |
|
Allowance for doubtful accounts: | |||||
|
Premiums, accounts and notes receivable |
$54 |
$12 |
$1 |
$(17) |
$50 |
|
Deferred tax asset valuation allowance |
$150 |
$(15) |
$— |
$(9) |
$126 |
|
Reinsurance recoverables |
$27 |
$(3) |
$— |
$(1) |
$23 |
|
(1) 2010 amount for deferred tax asset valuation allowance primarily reflects the resolution of a federal tax matter. See Note 20 to the Consolidated Financial Statements. (2) 2010 amount for commercial mortgage loans primarily reflects charge-offs upon sales and repayments, as well as transfers to foreclosed real estate. |
|||||
CIGNA CORPORATION – 2010 Form 10-K – FS-13
Index to Exhibits
|
Number |
Description |
Method of Filing |
|
3.1 |
Restated Certificate of Incorporation of the registrant as last amended April 23, 2008 |
Filed as Exhibit 3.1 to the registrant’s Form 10-Q for the quarterly period ended March 31, 2008 and incorporated herein by reference. |
|
3.2 |
By-Laws of the registrant as last amended and restated October 20, 2010 |
Filed as Exhibit 3.1 to the registrant’s Form 8-K on October 26, 2010 and incorporated herein by reference. |
|
4.1 (a) |
Indenture dated August 16, 2006 between CIGNA Corporation and U.S. Bank National Association |
Filed as Exhibit 4.1 to the registrant’s Form S-3ASR on August 17, 2006 and incorporated herein by reference. |
|
(b) |
Supplemental Indenture No. 3 dated March 7, 2008 between CIGNA Corporation and U.S. Bank National Association |
Filed as Exhibit 4.1 to the registrant’s Form 8-K on March 10, 2008 and incorporated herein by reference. |
|
4.2 |
Indenture dated January 1, 1994 between CIGNA Corporation and Marine Midland Bank |
Filed as Exhibit 4.2 to the registrant’s Form 10-K for the year ended December 31, 2009 and incorporated herein by reference |
|
4.3 |
Indenture dated June 30, 1988 between CIGNA Corporation and Bankers Trust |
Filed as Exhibit 4.3 to the registrant’s Form 10-K for the year ended December 31, 2009 and incorporated herein by reference |
|
Exhibits 10.1 through 10.28 are identified as compensatory plans, management contracts or arrangements pursuant to Item 15 of Form 10-K. |
||
|
10.1 |
Deferred Compensation Plan for Directors of CIGNA Corporation, as amended and restated January 1, 1997 |
Filed as Exhibit 10.1 to the registrant’s Form 10-K for the year ended December 31, 2006 and incorporated herein by reference. |
|
10.2 |
Deferred Compensation Plan of 2005 for Directors of CIGNA Corporation, Amended and Restated effective April 28, 2010 |
Filed herewith. |
|
10.3 |
CIGNA Corporation Non-Employee Director Compensation Program amended and restated effective January 1, 2011 |
Filed herewith. |
|
10.4 |
CIGNA Restricted Share Equivalent Plan for Non-Employee Directors as amended and restated effective January 1, 2008 |
Filed as Exhibit 10.3 to the registrant’s Form 10-K for the year ended December 31, 2007 and incorporated herein by reference |
|
10.5 |
CIGNA Corporation Director Equity Plan |
Filed as Exhibit 10.3 to the registrant’s Form 10-Q for the quarterly period ended March 31, 2010 and incorporated herein by reference. |
CIGNA CORPORATION – 2010 Form 10-K – E-1
|
Number |
Description |
Method of Filing |
|
10.6 |
CIGNA Corporation Compensation Program for Independent Vice Chairman/Chairman of the Board of Directors |
Filed as Exhibit 10.1 to the registrant’s Form 10-Q for the quarterly period ended September 30, 2009 and incorporated herein by reference. |
|
10.7 |
CIGNA Corporation Stock Plan, as amended and restated through July 2000 |
Filed as Exhibit 10.7 to the registrant’s Form 10-K for the year ended December 31, 2009 and incorporated herein by reference. |
|
10.8 (a) |
CIGNA Stock Unit Plan, as amended and restated effective July 22, 2008 |
Filed as Exhibit 10.1 to the registrant’s Form 10-Q for the quarterly period ended September 30, 2008 and incorporated herein by reference. |
|
(b) |
Amendment No. 1 to the CIGNA Stock Unit Plan, as amended and restated effective July 22, 2008 |
Filed as Exhibit 10.3 to the registrant’s Form 10-Q for the quarterly period ended June 30, 2010 and incorporated herein by reference. |
|
10.9 |
CIGNA Executive Severance Benefits Plan as amended and restated effective April 27, 2010 |
Filed as Exhibit 10.2 to the registrant’s Form 10-Q for the quarterly period ended June 30, 2010 and incorporated herein by reference. |
|
10.10 |
Description of Severance Benefits for Executives in Non-Change of Control Circumstances |
Filed as Exhibit 10.10 to the registrant’s Form 10-K for the year ended December 31, 2009 and incorporated herein by reference. |
|
10.11 |
Description of CIGNA Corporation Strategic Performance Share Program |
Filed as Exhibit 10.1 to the registrant’s Form 10-Q for the quarterly period ended March 31, 2010 and incorporated herein by reference. |
|
10.12 |
CIGNA Executive Incentive Plan amended and restated as of January 1, 2008 |
Filed as Exhibit 10.8 to the registrant’s Form 10-K for the year ended December 31, 2007 and incorporated herein by reference. |
|
10.13 (a) |
CIGNA Long-Term Incentive Plan as amended and restated effective as of April 28, 2010 |
Filed as Exhibit 10.2 to the registrant’s Form 10-Q for the quarterly period ended March 31, 2010 and incorporated herein by reference. |
|
(b) |
Amendment No. 1 to the CIGNA Long-Term Incentive Plan as amended and restated effective as of April 28, 2010 |
Filed as Exhibit 10.1 to the registrant’s Form 10-Q for the quarterly period ended June 30, 2010 and incorporated herein by reference. |
|
10.14 |
CIGNA Deferred Compensation Plan, as amended and restated October 24, 2001 |
Filed as Exhibit 10.10 to the registrant’s Form 10-K for the year ended December 31, 2006 and incorporated herein by reference. |
CIGNA CORPORATION – 2010 Form 10-K – E-2
|
Number |
Description |
Method of Filing |
|
10.15 |
CIGNA Deferred Compensation Plan of 2005 effective as of January 1, 2005 |
Filed as Exhibit 10.12 to the registrant’s Form 10-K for the year ended December 31, 2007 and incorporated herein by reference. |
|
10.16 (a) |
CIGNA Supplemental Pension Plan as amended and restated effective August 1, 1998 |
Filed as Exhibit 10.15(a) to the registrant’s Form 10-K for the year ended December 31, 2009 and incorporated herein by reference. |
|
(b) |
Amendment No. 1 to the CIGNA Supplemental Pension Plan, amended and restated effective as of September 1, 1999 |
Filed as Exhibit 10.15(a) to the registrant’s Form 10-K for the year ended December 31, 2009 and incorporated herein by reference. |
|
(c) |
Amendment No. 2 dated December 6, 2000 to the CIGNA Supplemental Pension |
Filed as Exhibit 10.12(c) to the registrant’s Form 10-K for the year ended December 31, 2006 and incorporated herein by reference. |
|
10.17 (a) |
CIGNA Supplemental Pension Plan of 2005 effective as of January 1, 2005 |
Filed as Exhibit 10.15 to the registrant’s Form 10-K for the year ended December 31, 2007 and incorporated herein by reference. |
|
(b) |
Amendment No. 1 to the CIGNA Supplemental Pension Plan of 2005 |
Filed as Exhibit 10.1 to the registrant’s Form 10-Q for the quarterly period ended June 30, 2009 and incorporated herein by reference. |
|
10.18 |
CIGNA Supplemental 401(k) Plan effective January 1, 2010 |
Filed as Exhibit 10.17 to the registrant’s Form 10-K for the year ended December 31, 2009 and incorporated herein by reference. |
|
10.19 |
Description of CIGNA Corporation Financial Services Program |
Filed as Exhibit 10.18 to the registrant’s Form 10-K for the year ended December 31, 2009 and incorporated herein by reference. |
|
10.20 |
Description of Mandatory Deferral of Non-Deductible Executive Compensation Arrangement |
Filed as Exhibit 10.14 to the registrant’s Form 10-K for the year ended December 31, 2006 and incorporated herein by reference. |
|
10.21 |
Agreement and Release dated December 9, 2009 with Mr. Hanway |
Filed as Exhibit 10.1 to the registrant’s Form 8-K filed on December 9, 2009 and incorporated herein by reference. |
CIGNA CORPORATION – 2010 Form 10-K – E-3
|
Number |
Description |
Method of Filing |
|
10.22 |
Schedule regarding Amended Deferred Stock Unit Agreements effective December 31, 2008 with Messrs, Hanway and Murabito and Form of Amended Deferred Stock Unit Agreement |
Filed as Exhibit 10.20 to the registrant’s Form 10-K for the year ended December 31, 2008 and incorporated herein by reference. |
|
10.23 |
Agreement and Release dated August 31, 2010 with Ms. Hagan |
Filed as Exhibit 10.1 to the registrant’s Form 8-K filed on September 1, 2010 and incorporated herein by reference. |
|
10.24 |
Agreement and Release dated September 20, 2010 with Mr. Woeller |
Filed as Exhibit 10.1 to the registrant’s Form 8-K filed on September 20, 2010 and incorporated herein by reference. |
|
10.25 |
Form of CIGNA Long-Term Incentive Plan: Nonqualified Stock Option and Grant Letter |
Filed herewith. |
|
10.26 |
Form of CIGNA Long-Term Incentive Plan: Restricted Stock Grant and Grant Letter |
Filed herewith. |
|
10.27 |
Form of CIGNA Long-Term Incentive Plan: Restricted Stock Unit Grant and Grant Letter |
Filed herewith. |
|
10.28 |
Asset and Stock Purchase Agreement by and among Great-West Life & Annuity Insurance Company, et al and Connecticut General Life Insurance Company |
Filed as Exhibit 10.23 to the registrant’s Form 10-K for the period ended December 31, 2007 and incorporated herein by reference. |
|
12 |
Computation of Ratios of Earnings to Fixed Charges |
Filed herewith. |
|
21 |
Subsidiaries of the Registrant |
Filed herewith. |
|
23 |
Consent of Independent Registered Public Accounting Firm |
Filed herewith |
|
31.1 |
Certification of Chief Executive Officer of CIGNA Corporation pursuant to Rule 13a-14(a) or Rule 15d-14(a) of the Securities Exchange Act of 1934 |
Filed herewith. |
CIGNA CORPORATION – 2010 Form 10-K – E-4
|
Number |
Description |
Method of Filing |
|
31.2 |
Certification of Chief Financial Officer of CIGNA Corporation pursuant to Rule 13a-14(a) or Rule 15d-14(a) of the Securities Exchange Act of 1934 |
Filed herewith. |
|
32.1 |
Certification of Chief Executive Officer of CIGNA Corporation pursuant to Rule 13a-14(b) or Rule 15d-14(b) and 18 U.S.C. Section 1350 |
Furnished herewith. |
|
32.2 |
Certification of Chief Financial Officer of CIGNA Corporation pursuant to Rule 13a-14(b) or Rule 15d-14(b) and 18 U.S.C. Section 1350 |
Furnished herewith. |
The registrant will furnish to the Commission upon request of any other instruments defining the rights of holders of long-term debt.
Shareholders may obtain copies of exhibits by writing to CIGNA Corporation, Shareholder Services Department, 1601 Chestnut Street, TL18, Philadelphia, PA 19192
CIGNA CORPORATION – 2010 Form 10-K – E-5
