Attached files
Table of Contents
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, DC 20549
FORM 10-K
(Mark One)
þ ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934
For the fiscal year ended December 31, 2010
OR
¨ TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934
Commission File Number: 001-14057
KINDRED HEALTHCARE, INC.
(Exact name of registrant as specified in its charter)
| Delaware | 61-1323993 | |
| (State or other jurisdiction of incorporation or organization) |
(I.R.S. Employer Identification Number) | |
| 680 South Fourth Street Louisville, Kentucky |
40202-2412 | |
| (Address of principal executive offices) | (Zip Code) | |
(502) 596-7300
(Registrant’s telephone number, including area code)
Securities registered pursuant to Section 12(b) of the Act:
| Title of Each Class |
Name of Each Exchange on which Registered | |
| Common Stock, par value $0.25 per share | New York Stock Exchange |
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes þ No ¨
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act. Yes ¨ No þ
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes þ No ¨
Indicate by check mark whether the registrant has submitted electronically and posted on its corporate Web site, if any, every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S-T (§232.405 of this chapter) during the preceding 12 months (or for such shorter period that the registrant was required to submit and post such files). Yes ¨ No ¨
Indicate by check mark if disclosure of delinquent filers pursuant to Item 405 of Regulation S-K (§229.405 of this chapter) is not contained herein, and will not be contained, to the best of registrant’s knowledge, in definitive proxy or information statements incorporated by reference in Part III of this Annual Report on Form 10-K or any amendment of this Annual Report on Form 10-K. þ
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, or a smaller reporting company. See the definitions of “large accelerated filer,” “accelerated filer” and “smaller reporting company” in Rule 12b-2 of the Exchange Act.
Large accelerated filer ¨ Accelerated filer þ Non-accelerated filer ¨ Smaller reporting company ¨
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Act). Yes ¨ No þ
The aggregate market value of the shares of the registrant held by non-affiliates of the registrant, based on the closing price of such stock on the New York Stock Exchange on June 30, 2010, was approximately $493,000,000. For purposes of the foregoing calculation only, all directors and executive officers of the registrant have been deemed affiliates.
As of January 31, 2011, there were 39,495,320 shares of the registrant’s common stock, $0.25 par value, outstanding.
DOCUMENTS INCORPORATED BY REFERENCE
Part III of this Annual Report on Form 10-K incorporates by reference from the registrant’s 2010 definitive proxy statement, which will be filed no later than 120 days after December 31, 2010.
Table of Contents
| Page | ||||||
| PART I | ||||||
| Item 1. |
3 | |||||
| Item 1A. |
44 | |||||
| Item 1B. |
66 | |||||
| Item 2. |
66 | |||||
| Item 3. |
66 | |||||
| Item 4. |
67 | |||||
| PART II |
||||||
| Item 5. |
68 | |||||
| Item 6. |
70 | |||||
| Item 7. |
Management’s Discussion and Analysis of Financial Condition and Results of Operations |
71 | ||||
| Item 7A. |
91 | |||||
| Item 8. |
92 | |||||
| Item 9. |
Changes in and Disagreements With Accountants on Accounting and Financial Disclosure |
92 | ||||
| Item 9A. |
92 | |||||
| Item 9B. |
93 | |||||
| PART III | ||||||
| Item 10. |
94 | |||||
| Item 11. |
95 | |||||
| Item 12. |
Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters |
95 | ||||
| Item 13. |
Certain Relationships and Related Transactions, and Director Independence |
95 | ||||
| Item 14. |
96 | |||||
| PART IV |
||||||
| Item 15. |
97 | |||||
2
Table of Contents
PART I
| Item 1. | Business |
GENERAL
Kindred Healthcare, Inc. is a healthcare services company that through its subsidiaries operates hospitals, nursing and rehabilitation centers, assisted living facilities and a contract rehabilitation services business across the United States. At December 31, 2010, our hospital division operated 89 long-term acute care (“LTAC”) hospitals (6,887 licensed beds) in 24 states. Our nursing center division operated 226 nursing and rehabilitation centers and seven assisted living facilities (27,905 licensed beds) in 28 states. We also operated a contract rehabilitation services business that provides rehabilitative services primarily in long-term care settings. All references in this Annual Report on Form 10-K to “Kindred,” “Company,” “we,” “us,” or “our” mean Kindred Healthcare, Inc. and, unless the context otherwise requires, our consolidated subsidiaries.
All financial and statistical information presented in this Annual Report on Form 10-K reflects the continuing operations of our businesses for all periods presented unless otherwise indicated.
RehabCare Acquisition. On February 7, 2011, we entered into an Agreement and Plan of Merger (the “Merger Agreement”) with RehabCare Group, Inc. (“RehabCare”), providing for the acquisition of RehabCare by Kindred. Subject to the terms and conditions of the Merger Agreement, RehabCare will be merged with and into Kindred (the “Merger”), with Kindred surviving the Merger.
At December 31, 2010, RehabCare operated 29 LTAC hospitals, five inpatient rehabilitation hospitals and provided rehabilitation therapy services in 116 acute care hospitals and 1,112 skilled nursing facilities in 42 states. RehabCare reported consolidated revenues of approximately $1.3 billion and net income from continuing operations of approximately $65 million in fiscal 2010.
The Merger will form the largest post-acute healthcare services company in the United States with over $6 billion in annual revenues and operations in 46 states. The combined company will be a leading operator of LTAC hospitals, nursing and rehabilitation centers, skilled and acute care rehabilitation therapy contract services and inpatient rehabilitation facilities. This transaction, valued at approximately $1.3 billion, will further our cluster market strategy, add to our existing LTAC hospital and skilled nursing contract rehabilitation therapy businesses and expand our service offerings to include the acute care inpatient rehabilitation therapy business.
We believe that the RehabCare acquisition will be highly accretive to our earnings and cash flows, provide significant long-term strategic benefits and further enhance our future growth prospects. The RehabCare acquisition is also consistent with our strategy of developing clinical and operational expertise across the post-acute continuum of healthcare services.
At the effective time of the Merger, each share of RehabCare common stock outstanding immediately prior to the effective time (subject to certain exceptions) will be converted into the right to receive 0.471 of a share of Kindred common stock and $26.00 in cash, without interest (the “Merger Consideration”). No fractional shares of Kindred common stock will be issued in the Merger, and RehabCare’s stockholders will receive cash in lieu of fractional shares. The Merger Agreement also provides for the vesting and conversion of certain employee stock options and restricted shares of RehabCare. Outstanding Kindred common stock will not be affected by the Merger. Upon completion of the transaction, RehabCare stockholders will own approximately 22% of our outstanding common stock.
The consummation of the Merger is subject to certain conditions, including the adoption by the RehabCare and Kindred stockholders of the Merger Agreement; clearance under the Hart-Scott-Rodino Antitrust Improvements Act of 1976, as amended; receipt of certain other licensure and regulatory approvals; receipt of the proceeds of the financing described below; and other customary closing conditions.
3
Table of Contents
The Merger Agreement contains customary representations, warranties and covenants, including covenants providing for each of the parties (i) to use reasonable best efforts to cause the transaction to be consummated and (ii) to call and hold a stockholders’ meeting and recommend adoption of the Merger Agreement, subject to fiduciary duties. The Merger Agreement also requires RehabCare to conduct its operations in all material respects according to the ordinary course of business consistent with past practice until the closing of the Merger. RehabCare is subject to customary “no-shop” restrictions on its ability to solicit acquisition proposals from third parties and to provide information to and engage in discussions with third parties about acquisition proposals, subject to a “fiduciary duty” exception in certain circumstances prior to adoption of the Merger Agreement by RehabCare’s stockholders.
The Merger Agreement also contains certain termination rights and provides that (i) upon termination of the Merger Agreement under specified circumstances, including a change in the recommendation of the board of directors of RehabCare or termination of the Merger Agreement to enter into a written definitive agreement for a “superior proposal,” RehabCare must pay us a termination fee of $26 million and (ii) upon the termination of the Merger Agreement under specified circumstances, including a change in the recommendation of our board of directors or our failure to complete the financing discussed below, after all other closing conditions have been met, we must pay RehabCare a cash termination fee of $62 million.
We have obtained a financing commitment (the “Commitment Letter”) from JPMorgan Chase Bank, N.A., J.P. Morgan Securities LLC, Morgan Stanley Senior Funding, Inc. and Citigroup Global Markets Inc. in connection with the pending transaction. These funds and existing cash balances are expected to be sufficient to fund the cash consideration to RehabCare stockholders and to refinance certain existing Kindred and RehabCare debt. Subject to certain conditions, we expect to have in place approximately $1.9 billion of long-term financing, of which approximately $1.6 billion is expected to be outstanding at the time of consummation of the pending transaction.
The foregoing summaries of the Merger Agreement and the Commitment Letter, and the transactions contemplated thereby do not purport to be complete and are subject to, and qualified in their entirety by, the full text of such agreements, which have previously been filed with the Securities and Exchange Commission (the “SEC”). See “Item 1A – Risk Factors – Risk Factors Relating to the RehabCare Acquisition.”
Vista Acquisition. On November 1, 2010, we completed the acquisition of five LTAC hospitals from Vista Healthcare, LLC (“Vista”) for a purchase price of $179 million in cash (the “Vista Acquisition”). The Vista Acquisition was financed with proceeds from our revolving credit facility.
The Vista Acquisition included four freestanding hospitals and one hospital-in-hospital with a total of 250 beds, all of which are located in southern California. We did not acquire the working capital of Vista or assume any of its liabilities. All of the Vista hospitals are leased.
Spin-Off Transaction. On July 31, 2007, we completed the spin-off of our former institutional pharmacy business, Kindred Pharmacy Services, Inc. (“KPS”), and the immediate subsequent combination of KPS with the former institutional pharmacy business of AmerisourceBergen Corporation (“AmerisourceBergen”) to form a new, independent, publicly traded company named PharMerica Corporation (“PharMerica”) (the “Spin-off Transaction”). Immediately prior to the Spin-off Transaction, KPS incurred $125 million of bank debt, the proceeds of which were distributed to us. Immediately after the Spin-off Transaction, our stockholders and the stockholders of AmerisourceBergen each held approximately 50% of the outstanding common stock of PharMerica.
For accounting purposes, the assets and liabilities of KPS were eliminated from our balance sheet effective at the close of business on July 31, 2007, and since August 1, 2007, the future operating results of KPS are no longer included in our operating results. In accordance with the authoritative guidance for accounting for the impairment or disposal of long-lived assets, the historical operating results of KPS are not reported as a discontinued operation of us because of the significance of the expected continuing cash flows between
4
Table of Contents
PharMerica and us under pharmacy services contracts for services to be provided by PharMerica to our hospitals and nursing and rehabilitation centers. Accordingly, for periods prior to August 1, 2007, the historical operating results of KPS are included in our historical continuing operations.
In addition to the pharmacy services contracts noted above, we also entered into new agreements with PharMerica for information systems services, transition services and certain tax matters.
Commonwealth Transaction. In February 2006, we acquired the operations of the LTAC hospitals, nursing and rehabilitation centers and assisted living facilities operated by Commonwealth Communities Holdings LLC and certain of its affiliates for a total purchase price of $124 million in cash (the “Commonwealth Transaction”).
The Commonwealth Transaction included five freestanding LTAC hospitals and one hospital-in-hospital with a total of 421 licensed hospital beds. Three of these hospitals also operate co-located sub-acute units and skilled nursing units with a total of 168 licensed beds. In addition, we acquired the operations of nine nursing and rehabilitation centers containing 1,316 licensed beds and four assisted living facilities with a total of 215 licensed beds. In the transaction, we also acquired the right to develop 95 additional licensed hospital beds in Massachusetts. In September 2008, we closed one of the freestanding LTAC hospitals acquired in the Commonwealth Transaction and relinquished the related licensed beds to the Commonwealth of Massachusetts. See “– Discontinued Operations.”
Spin-off from Ventas. On May 1, 1998, Ventas, Inc. (“Ventas”) completed the spin-off of its healthcare operations to its stockholders through the distribution of our former common stock. Ventas retained ownership of substantially all of its real property and leases a portion of such real property to us. In anticipation of the spin-off from Ventas, we were incorporated on March 27, 1998 as a Delaware corporation. For accounting purposes, the consolidated historical financial statements of Ventas became our historical financial statements following the spin-off.
Risk Factors. This Annual Report on Form 10-K includes forward-looking statements within the meaning of Section 27A of the Securities Act of 1933, as amended (the “Securities Act”), and Section 21E of the Securities Exchange Act of 1934, as amended (the “Exchange Act”). See “Item 1A – Risk Factors.”
Discontinued Operations
In recent years, we have completed several transactions related to the divestiture of unprofitable hospitals and nursing and rehabilitation centers.
In June 2009, we purchased for resale six under-performing nursing and rehabilitation centers (the “Nursing Centers”) previously leased from Ventas for $55.7 million. In addition, we paid Ventas a lease termination fee of $2.3 million. The Nursing Centers were included in our Master Lease Agreements (as defined below under “– Master Lease Agreements”) with Ventas and we do not have the ability to terminate a lease of an individual facility under the Master Lease Agreements. The aggregate annual rent for the Nursing Centers was approximately $6 million for the year ended December 31, 2008. The Nursing Centers, which contained 777 licensed beds, generated pretax losses of $0.1 million, $0.5 million and $2.5 million for 2010, 2009 and 2008, respectively. We recorded a pretax gain of $2.1 million ($1.3 million net of income taxes) during 2010 and a pretax loss of $39.5 million ($24.3 million net of income taxes) during 2009 related to these divestitures. We disposed of the Nursing Centers during 2009 and 2010 for $27.2 million.
In September 2008, we purchased for resale a LTAC hospital for $22.3 million that was previously leased. We recorded a pretax loss of $36.9 million ($22.7 million net of income taxes) in 2008 resulting from the losses related to the purchase, closure and planned divestiture of the hospital, including the impairment of a certificate of need intangible asset ($15.2 million), the impairment of property and equipment ($17.3 million) and other costs ($4.4 million). In addition, we recorded a pretax loss of $2.6 million ($1.6 million net of income taxes) in 2010 resulting from a reduction to the fair market value of the property.
5
Table of Contents
In September 2008, we also announced our intention to dispose of another LTAC hospital and its related operations. We recorded a pretax loss of $7.4 million ($4.6 million net of income taxes) during 2008 related to the impairment of the hospital’s building and equipment. In addition, we recorded a pretax loss of $0.5 million ($0.3 million net of income taxes) in 2010 resulting from a reduction to the fair market value of the property.
These two hospitals generated pretax losses of $1.5 million in 2010, $3.3 million in 2009 and $8.0 million in 2008.
We also discontinued the operations of a hospital in 2008 after terminating the hospital operating lease and ceasing operations.
For accounting purposes, the operating results of these businesses and the losses or impairments associated with these transactions have been classified as discontinued operations in the accompanying consolidated statement of operations for all periods presented. Assets not sold at December 31, 2010 have been measured at the lower of carrying value or estimated fair value less costs of disposal and have been classified as held for sale in the accompanying consolidated balance sheet. See notes 3 and 4 of the notes to consolidated financial statements.
HEALTHCARE OPERATIONS
We are organized into three operating divisions: the hospital division, the nursing center division and the rehabilitation division. The hospital division operates LTAC hospitals. The nursing center division operates nursing and rehabilitation centers and assisted living facilities. The rehabilitation division primarily provides rehabilitation services primarily in long-term care settings. We believe that the independent focus of each division on the unique aspects of its business enhances its ability to attract patients, residents and non-affiliated customers, improve the quality of its operations and achieve operating efficiencies.
HOSPITAL DIVISION
Our hospital division provides long-term acute care services to medically complex patients through the operation of a national network of 89 hospitals with 6,887 licensed beds located in 24 states as of December 31, 2010. We operate the largest network of LTAC hospitals in the United States based upon fiscal 2010 revenues of approximately $2.0 billion (before eliminations). As a result of our commitment to the LTAC hospital business, we have developed a comprehensive program of care for medically complex patients that allows us to deliver high quality care in a cost-effective manner.
A number of the hospital division’s hospitals also provide skilled nursing, sub-acute and outpatient services. Outpatient services may include diagnostic services, rehabilitation therapy, CT scanning, one-day surgery and laboratory.
In our hospitals, we treat medically complex patients, including the critically ill, suffering from multiple organ system failures, most commonly of the cardiovascular, pulmonary, kidney, gastro-intestinal and cutaneous (skin) systems. In particular, we have a core competency in treating patients with cardio-pulmonary disorders, skin and wound conditions, and life-threatening infections. Prior to being admitted to our hospitals, many of our patients have undergone a major surgical procedure or developed a neurological disorder following head and spinal cord injury, cerebrovascular incident or metabolic instability. Our expertise lies in the ability to simultaneously deliver comprehensive and coordinated medical interventions directed at all affected organ systems, while maintaining a patient-centered, integrated care plan. Medically complex patients are characteristically dependent on technology for continued life support, including mechanical ventilation, total parenteral nutrition, respiratory or cardiac monitors and kidney dialysis machines. During 2010, the average length of stay for patients in our hospitals was approximately 30 days.
6
Table of Contents
Our hospital division patients generally have conditions that require a high level of monitoring and specialized care, yet may not need the services of a traditional intensive care unit. These patients are not clinically appropriate for admission to other post-acute settings because their severe medical conditions are periodically or chronically unstable. By providing a range of services required for the care of medically complex patients, we believe that our LTAC hospitals provide our patients with high quality, cost-effective care.
Our LTAC hospitals employ a comprehensive program of care for their patients that draws upon the talents of interdisciplinary teams, including physician specialists. The teams evaluate patients upon admission to determine treatment programs. Our hospital division has developed specialized treatment programs focused on the needs of medically complex patients. In addition to traditional medical services, most of our patients receive individualized treatment plans in rehabilitation, skin integrity management and clinical pharmacology. Where appropriate, the treatment programs may involve the services of several disciplines, such as pulmonary medicine, infectious disease and physical medicine.
Hospital Division Strategy
Our goal is to be the leading operator of LTAC hospitals in terms of both quality of care and operating efficiency. Our strategies for achieving this goal include:
Maintaining High Quality of Care. The hospital division differentiates its hospitals through its ability to care for medically complex patients in a high quality, cost-effective setting. We are committed to maintaining and improving the quality of our patient care by dedicating appropriate resources at each facility and continuing to refine our clinical initiatives and objectives. We continue to take steps to improve our quality indicators and maintain the quality of care at our hospitals, including:
| • | attracting and retaining high quality professional staff within each market. The hospital division believes that its future success will depend in part upon its continued ability to hire and retain qualified healthcare personnel and to promote leadership and development training, |
| • | maintaining an integrated quality assurance and improvement program, administered by the hospital division’s chief medical officer and senior vice president of clinical operations, which encompasses utilization review, quality improvement, infection control and risk management, |
| • | promoting best practices through our hospitals and standardizing products and services to promote better care, |
| • | expanding our service excellence programs to further embed a culture of caring in each of our hospitals, |
| • | maintaining clinical outcome programs, which include concurrent reviews of all of our patient population against quality screenings, outcome reporting and patient and family satisfaction surveys, |
| • | maintaining a program whereby our hospitals are reviewed by internal quality auditors for compliance with standards of The Joint Commission (the “Joint Commission”) or the American Osteopathic Association (the “AOA”), national organizations that establish standards relating to the physical plant, administration, quality of patient care and operation of medical staffs of hospitals, |
| • | engaging quality councils at the divisional, regional, district and hospital levels to analyze data, set quality goals and oversee all quality assurance and quality improvement activities throughout the division, |
| • | incorporating the clinical advice of the hospital division’s chief medical officer, medical advisory board and other physicians into our operational procedures, and |
| • | implementing an integrated risk management plan to improve quality and expand existing patient safety initiatives. |
7
Table of Contents
Improving Operating Efficiency. The hospital division is continually focused on improving operating efficiency and controlling costs while maintaining quality patient care. Our hospital division seeks to improve operating efficiencies and control costs by standardizing key operating procedures and optimizing the skill mix of its staff based upon the clinical needs of each hospital’s patients. The initiatives we have undertaken to control our costs and improve efficiency include:
| • | managing labor costs by adjusting staffing to patient acuity and fluctuations in patient census, |
| • | increasing the standardization of operating processes, procedures and equipment, |
| • | improving physician participation in resource consumption, medical record documentation and intensity of service management, |
| • | managing pharmacy costs through the use of a medication control program and evaluating medical utilization through our pharmacy and therapeutic committees in each hospital, |
| • | centralizing administrative functions such as accounting, payroll, legal, reimbursement, compliance, tax and information systems, |
| • | utilizing management information technology to aid in financial and clinical reporting as well as billing and collections, and |
| • | centralizing business office operations and collaborating on sales and marketing and managed care strategies in our cluster markets. |
Growing Through Business Development and Acquisitions. Our growth strategy is focused on the development and expansion of our services:
| • | Growing Through Selective Acquisitions – We seek growth opportunities through strategic acquisitions in selected target markets, particularly where an acquisition may assist us in scaling our operations more rapidly and efficiently than internal growth. In 2010, we acquired four freestanding hospitals and one hospital-in-hospital with a total of 250 beds as part of the Vista Acquisition. Our planned acquisition of RehabCare will significantly expand the scope of our hospital division by adding 29 LTAC hospitals (1,605 licensed beds). |
| • | Freestanding Hospitals – At December 31, 2010, we operated 72 freestanding hospitals (6,157 licensed beds). During 2010, we opened one freestanding hospital and two replacement hospitals which added a total of 46 licensed hospital beds. During 2009 and 2008, we opened two new freestanding hospitals which added a total of 130 licensed hospital beds. The maturation of these hospitals is a key component of our growth strategy. We have one new freestanding hospital under development which will add 50 licensed hospital beds to our capacity. Pursuant to the Medicare, Medicaid and SCHIP Extension Act of 2007 (the “SCHIP Extension Act”), a three-year moratorium, beginning December 29, 2007, was imposed on the establishment of a LTAC hospital or satellite facility, subject to exceptions for facilities under development. The moratorium on the establishment of a LTAC hospital or satellite facility was extended from three years to five years by the Patient Protection and Affordable Care Act (enacted on March 23, 2010) and the Healthcare Education and Reconciliation Act (enacted on March 30, 2010) (collectively, the “ACA”). We believe the freestanding hospital under development is exempt from the moratorium. |
| • | Sub-Acute Development – We are well positioned to develop sub-acute units in several of our hospitals to broaden our scope of services, promote higher quality care and take advantage of unused capacity. We operate seven sub-acute units with 409 licensed beds and we have five hospital-based sub-acute units with approximately 150 licensed beds currently under development. |
| • | Cluster Market Development – We are increasingly focused on the opportunities available to us in markets where we operate multiple hospitals or in which we have affiliated nursing and rehabilitation centers. These cluster markets present opportunities for our hospitals and nursing and rehabilitation centers to share centralized business office operations and collaborate on their sales and marketing and |
8
Table of Contents
| managed care strategies. These cluster markets also allow us to better coordinate and manage the continuum of care for each of our patients, implement physician services strategies and reduce re-hospitalizations. We believe a more market focused approach will increase admissions over time, better educate the marketplace on our ability to care for post-acute patients and enhance our capabilities to care for patients across various post-acute settings. |
| • | Hospital-in-Hospital – We have contracts with non-Kindred short-term acute care and other hospitals to operate LTAC hospitals with a host hospital (“HIH”). Under these arrangements, we lease space and purchase certain ancillary services from the host hospital and provide it with the option to discharge a portion of its clinically appropriate patients into the care of our hospital. These HIHs also receive patients from general short-term acute care hospitals in addition to the host hospital. During 2010, we acquired one HIH with 30 licensed hospital beds. At December 31, 2010, we operated 17 HIHs with 730 licensed beds. We currently have a 50-bed HIH under development which we believe is exempt from the LTAC moratorium. |
Expanding Program Development. We are a leading provider of long-term acute care to patients with pulmonary dysfunction. In addition, we have developed and continue to expand other inpatient and outpatient service areas such as wound care, post-surgical care, acute rehabilitation, pain management, as well as new intensive care units, where we believe opportunities exist to position our hospitals as centers of excellence in given markets. We continue to broaden our expertise beyond pulmonary services and to leverage our leadership position in pulmonary care to expand our market strength to other clinical services. We also continue to expand our sub-acute programs in selected markets.
Increasing Patient Volume, Particularly Commercial Patients. We continue to expand our sales and marketing function to grow same-facility admissions and to take advantage of available capacity. We generally receive higher reimbursement rates from commercial insurers as a group than from the Medicare and Medicaid programs. As a result, we work to expand relationships with insurers and to enhance their understanding of our services in order to increase commercial patient volume. Each of our hospitals employs specialized staff to focus on patient admissions and the patient referral process. We have enhanced our sales and marketing function and implemented new technologies to increase the speed of referrals and admissions.
Improving Relationships with Referring Providers. Substantially all of the acute and medically complex patients admitted to our hospitals are transferred to us by other healthcare providers such as general short-term acute care hospitals, intensive care units, managed care programs, physicians, nursing centers and home care settings. Accordingly, we are focused on maintaining strong relationships with these providers as well as developing more comprehensive relationships with physician groups. In order to maintain these relationships, we employ clinical liaisons that are responsible for coordinating admissions and assessing the nature of services necessary for the proper care of the patient. The clinical liaisons also are responsible for educating healthcare professionals at the referral sources about the unique nature of the services provided by our LTAC hospitals.
9
Table of Contents
Selected Hospital Division Operating Data
The following table sets forth certain operating and financial data for the hospital division (dollars in thousands, except statistics):
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Revenues |
$ | 1,973,321 | $ | 1,932,892 | $ | 1,837,322 | ||||||
| Operating income |
$ | 357,100 | $ | 363,811 | $ | 345,367 | ||||||
| Hospitals in operation at end of period |
89 | 83 | 82 | |||||||||
| Licensed beds at end of period |
6,887 | 6,580 | 6,482 | |||||||||
| Admissions |
45,559 | 45,019 | 43,936 | |||||||||
| Patient days |
1,385,669 | 1,381,350 | 1,395,049 | |||||||||
| Average length of stay |
30.4 | 30.7 | 31.8 | |||||||||
| Revenues per admission |
$ | 43,313 | $ | 42,935 | $ | 41,818 | ||||||
| Revenues per patient day |
$ | 1,424 | $ | 1,399 | $ | 1,317 | ||||||
| Medicare case mix index (discharged patients only) |
1.19 | 1.21 | 1.15 | |||||||||
| Average daily census |
3,796 | 3,785 | 3,812 | |||||||||
| Occupancy % |
65.1 | 64.7 | 64.8 | |||||||||
| Annualized employee turnover % |
22.0 | 22.1 | 25.2 | |||||||||
| Assets at end of period |
$ | 1,100,138 | $ | 867,332 | $ | 847,394 | ||||||
| Capital expenditures: |
||||||||||||
| Routine |
$ | 36,967 | $ | 26,716 | $ | 35,932 | ||||||
| Development |
41,140 | 42,371 | 33,285 | |||||||||
The term “operating income” is defined as earnings before interest, income taxes, depreciation, amortization, rent and corporate overhead. A reconciliation of “operating income” to our consolidated results of operations is included in note 6 of the notes to consolidated financial statements. The term “licensed beds” refers to the maximum number of beds permitted in a facility under its license regardless of whether the beds are actually available for patient care. “Patient days” refers to the total number of days of patient care provided for the periods indicated. “Average length of stay” is computed by dividing each facility’s patient days by the number of admissions in the respective period. “Medicare case mix index” is the sum of the individual patient diagnostic related group weights for the period divided by the sum of the discharges for the same period. “Average daily census” is computed by dividing each facility’s patient days by the number of calendar days in the respective period. “Occupancy %” is computed by dividing average daily census by the number of operational licensed beds, adjusted for the length of time each facility was in operation during each respective period. “Annualized employee turnover %” is calculated by dividing full-time and part-time terminations by the active employee count at the beginning of the year. Routine capital expenditures include expenditures at existing facilities that generally do not result in the expansion of services. Development capital expenditures include expenditures for the development of new facilities or the expansion of services or capacity at existing facilities.
10
Table of Contents
Sources of Hospital Revenues
The hospital division receives payment for its services from third party payors, including government reimbursement programs such as Medicare and Medicaid and non-government sources such as Medicare Advantage, commercial insurance companies, health maintenance organizations, preferred provider organizations and contracted providers. Patients covered by non-government payors generally are more profitable to the hospital division than those covered by the Medicare and Medicaid programs. The following table sets forth the approximate percentages of our hospital admissions, patient days and revenues derived from the payor sources indicated:
| Year ended |
Medicare | Medicaid | Medicare Advantage | Commercial insurance and other |
||||||||||||||||||||||||||||||||||||||||||||
| Admissions | Patient days |
Revenues | Admissions | Patient days |
Revenues | Admissions | Patient days |
Revenues | Admissions | Patient days |
Revenues | |||||||||||||||||||||||||||||||||||||
| 2010 |
64 | % | 56 | % | 56 | % | 9 | % | 13 | % | 9 | % | 9 | % | 10 | % | 10 | % | 18 | % | 21 | % | 25 | % | ||||||||||||||||||||||||
| 2009 |
64 | 56 | 55 | 9 | 15 | 10 | 9 | 10 | 10 | 18 | 19 | 25 | ||||||||||||||||||||||||||||||||||||
| 2008 |
66 | 58 | 55 | 10 | 15 | 10 | 8 | 8 | 9 | 16 | 19 | 26 | ||||||||||||||||||||||||||||||||||||
For the year ended December 31, 2010, revenues of the hospital division totaled approximately $2.0 billion or 42% of our total revenues (before eliminations). For more information regarding the reimbursement for our hospital services, see “– Governmental Regulation – Hospital Division – Overview of Hospital Division Reimbursement.”
Hospital Facilities
The following table lists by state the number of hospitals and related licensed beds we operated as of December 31, 2010:
| Number of facilities | ||||||||||||||||||||
| State |
Licensed beds |
Owned by us |
Leased from Ventas (2) |
Leased from other parties |
Total | |||||||||||||||
| Arizona |
217 | – | 2 | 2 | 4 | |||||||||||||||
| California |
1,097 | 4 | 5 | 6 | 15 | |||||||||||||||
| Colorado |
68 | – | 1 | – | 1 | |||||||||||||||
| Florida (1) |
745 | 2 | 6 | 2 | 10 | |||||||||||||||
| Georgia (1) |
72 | – | – | 1 | 1 | |||||||||||||||
| Illinois (1) |
582 | 1 | 4 | 1 | 6 | |||||||||||||||
| Indiana |
119 | 1 | 1 | – | 2 | |||||||||||||||
| Kentucky (1) |
414 | – | 1 | 1 | 2 | |||||||||||||||
| Louisiana |
168 | – | 1 | – | 1 | |||||||||||||||
| Massachusetts (1) |
676 | 3 | 2 | 2 | 7 | |||||||||||||||
| Missouri (1) |
265 | – | 2 | 1 | 3 | |||||||||||||||
| Nevada |
238 | 1 | 1 | 1 | 3 | |||||||||||||||
| New Jersey (1) |
117 | – | – | 3 | 3 | |||||||||||||||
| New Mexico |
61 | – | 1 | – | 1 | |||||||||||||||
| North Carolina (1) |
124 | – | 1 | – | 1 | |||||||||||||||
| Ohio |
250 | – | – | 3 | 3 | |||||||||||||||
| Oklahoma |
93 | – | 1 | 1 | 2 | |||||||||||||||
| Pennsylvania |
393 | 2 | 2 | 3 | 7 | |||||||||||||||
| South Carolina (1) |
59 | – | – | 1 | 1 | |||||||||||||||
| Tennessee (1) |
109 | – | 1 | 1 | 2 | |||||||||||||||
| Texas |
818 | 1 | 6 | 4 | 11 | |||||||||||||||
| Virginia (1) |
60 | – | – | 1 | 1 | |||||||||||||||
| Washington (1) |
80 | 1 | – | – | 1 | |||||||||||||||
| Wisconsin |
62 | – | – | 1 | 1 | |||||||||||||||
| Totals |
6,887 | 16 | 38 | 35 | 89 | |||||||||||||||
| (1) | These states have certificate of need regulations. See “– Governmental Regulation – Federal, State and Local Regulation.” |
| (2) | See “– Master Lease Agreements.” |
11
Table of Contents
Quality Assessment and Improvement
The hospital division maintains a clinical outcomes and customer service program which includes a review of its patient population measured against utilization and quality standards, clinical outcomes data collection and patient/family, employee and physician satisfaction surveys. In addition, our hospitals have integrated quality assurance and improvement programs administered by a director of quality management, which encompass quality improvement, infection control and risk management. The objective of these programs is to ensure that patients are managed appropriately in our hospitals and that quality healthcare is provided in a cost-effective manner.
The hospital division has implemented a program whereby its hospitals are reviewed by internal quality auditors for compliance with standards of the Joint Commission or the AOA. The purposes of this internal review process are to (1) ensure ongoing compliance with industry recognized standards for hospitals, (2) assist management in analyzing each hospital’s operations and (3) provide consulting and educational programs for each hospital to identify opportunities to improve patient care.
Hospital Division Management and Operations
Each of our hospitals has a fully credentialed, multi-specialty medical staff to meet the needs of the medically complex, long-term acute patient. Our hospitals offer a broad range of physician services including pulmonology, internal medicine, infectious diseases, neurology, nephrology, cardiology, radiology and pathology. In addition, our hospitals have a multi-disciplinary team of healthcare professionals, including a professional nursing staff trained to care for long-term acute patients, respiratory, physical, occupational and speech therapists, pharmacists, registered dietitians and social workers, to address the needs of medically complex patients.
Each hospital utilizes a pre-admission assessment system to evaluate clinical needs and other information in determining the appropriateness of each potential patient admission. After admission, each patient’s case is reviewed by the hospital’s interdisciplinary team to determine a care plan. Typically, and where appropriate, the care plan involves the services of several disciplines, such as pulmonary medicine, infectious disease and physical medicine.
A hospital chief executive officer or administrator supervises and is responsible for the day-to-day operations at each of our hospitals. Each hospital or network of hospitals also employs a chief financial officer who monitors the financial matters of the hospital or network. Within selected markets having a significant concentration of hospitals, administrative functions such as billing and collections may be shared to improve efficiency. In addition, each hospital or network of hospitals employs a chief clinical officer to oversee the clinical operations and a director of quality management to oversee our quality assurance programs. We provide centralized services in the areas of information systems design and development, training, reimbursement expertise, legal advice, tax, technical accounting support, purchasing and facilities management to each of our hospitals. We believe that this centralization improves efficiency, promotes the standardization of certain processes and allows hospital staff to focus more attention on patient care.
A division president and a chief financial officer manage the hospital division. The operations of the hospitals are divided into an east region, a central region and a west region, each headed by a senior officer of the division who reports to the division president. The clinical issues and quality concerns of the hospital division are managed by the division’s chief medical officer and senior vice president of clinical operations.
Hospital Division Competition
In each geographic market that we serve, there are generally several competitors that provide similar services to those provided by our hospital division. In addition, several of the markets in which the hospital division operates have other LTAC hospitals that provide services comparable to those offered by our hospitals.
12
Table of Contents
Certain competing hospitals are operated by not-for-profit, non-taxpaying or governmental agencies, which can finance capital expenditures on a tax-exempt basis and receive funds and charitable contributions unavailable to our hospital division.
Competition for patients covered by non-government reimbursement sources is intense. The primary competitive factors in the LTAC hospital business include quality of services, charges for services and responsiveness to the needs of patients, families, payors and physicians. Other companies have entered the LTAC hospital business with licensed hospitals that compete with our hospitals. The competitive position of any hospital also is affected by the ability of its management to negotiate contracts with purchasers of group healthcare services, including managed care companies, preferred provider organizations and health maintenance organizations. Such organizations attempt to obtain discounts from established hospital charges. The importance to a hospital’s competitive position of obtaining contracts with preferred provider organizations, health maintenance organizations and other organizations that finance healthcare varies from market to market, depending on the number and market strength of such organizations.
NURSING CENTER DIVISION
Our nursing center division provides quality, cost-effective care through the operation of a national network of 226 nursing and rehabilitation centers and seven assisted living facilities (27,905 licensed beds) located in 28 states. We are the largest publicly held operator of nursing and rehabilitation centers in the United States based upon our fiscal 2010 revenues of approximately $2.2 billion (before eliminations). Through our nursing and rehabilitation centers, we provide short stay patients and long stay residents with a full range of medical, nursing, rehabilitative, pharmacy and routine services, including daily dietary, social and recreational services.
Consistent with industry trends, patients and residents admitted to our nursing and rehabilitation centers arrive with greater medical complexity and require a more extensive and costly level of care. This is particularly true with our Medicare population for whom the average length of stay in 2010 was 34 days. To appropriately care for a higher acuity short stay patient population and a more frail and unstable long stay resident population, we are taking steps to improve the delivery of the clinical and hospitality services offered to our patients and residents by adjusting the level of clinical and hospitality staffing, assisting physician oversight through the selective use of nurse practitioners, enhancing nursing skills via ongoing education and competency evaluations and improving clinical case management through the employment of clinical case managers.
We have developed transitional care units at approximately half of our nursing and rehabilitation centers. These units within our nursing and rehabilitation centers typically consist of 20 to 50 beds offering skilled nursing services and a range of rehabilitation services including physical, occupational and speech therapy to patients recovering from a variety of surgical procedures such as joint replacements, amputations, bariatric procedures, wound closure/repair procedures as well as medical conditions such as stroke, and cardiac and respiratory ailments. Several of our nursing and rehabilitation centers have clinical programs focused primarily upon a short stay patient population arriving for recovery, recuperation and rehabilitation resulting in a transitional care patient population that comprises a significant portion of the patients treated in the nursing and rehabilitation center. We refer to these types of nursing and rehabilitation centers as transitional care centers since this higher level of care encompasses a significant portion of the clinical activities of the center.
At a number of our nursing and rehabilitation centers, we offer specialized programs for residents with Alzheimer’s disease and other dementias through our Reflections units. We have developed specific certification criteria for these units. These units are operated by teams of professionals that are dedicated to addressing the unique problems experienced by residents with Alzheimer’s disease or other dementias. We believe that we are a leading provider of nursing care to residents with Alzheimer’s disease and dementia based upon the specialization and size of our program.
13
Table of Contents
We also monitor and enhance the quality of care and customer service at our nursing and rehabilitation centers through the use of performance improvement committees as well as family satisfaction surveys. Our performance improvement committees oversee resident healthcare needs and resident and staff safety. Physician medical directors serve on these committees and advise on healthcare policies and practices. We regularly conduct surveys of residents and their families, and these surveys are reviewed by our performance improvement committees at each center to promote quality care and customer service. An increasingly important performance improvement initiative is a division-wide focus on reducing potentially avoidable hospitalizations. The clinical leadership of each center is actively engaged in improving nursing competencies and communication skills, developing specific clinical programs to address acute care needs that may arise on site and working collaboratively with the medical community to coordinate monitoring and treatment.
Substantially all of our nursing and rehabilitation centers are certified to provide services under the Medicare and Medicaid programs. Our nursing and rehabilitation centers have been certified because the quality of our services, accommodations, equipment, safety, personnel, physical environment and policies and procedures meet or exceed the standards of certification set by those programs.
Nursing Center Division Strategy
Our goal is to become the provider of choice in the markets we serve, which we believe will allow us to increase our patient census and enhance our payor mix. We are employing several initiatives to improve the quality of our services and to address the needs of a more acute patient population. The principal elements of our nursing center division strategy are:
Providing Quality, Clinical-Based Services. The nursing center division is focused on qualitative and quantitative clinical performance indicators with the goal of providing quality care under the cost containment objectives imposed by government and private payors. In an effort to continually improve the quality of our services and enhance our ability to care for complex and higher acuity residents, we pursue initiatives to:
| • | improve recruitment, retention, management development, succession planning and employee satisfaction, |
| • | expand the involvement of our medical directors, engage the services of more primary care and specialty physicians and increase the use of nurse practitioners, |
| • | expand our therapy services, wound care, complex medical care and palliative care programs to improve our ability to care for a more acute patient population, |
| • | improve our processes to monitor and promote our patient care objectives and align financial incentives with quality care and customer service goals, |
| • | increase the number of our transitional care and sub-acute units to treat patients with rehabilitation and complex medical needs, |
| • | develop medical advisory boards at select transitional care centers to enhance our clinical programming and review case studies to improve care, |
| • | improve our Reflections units to care for residents with Alzheimer’s disease and other dementias, |
| • | maximize quality outcomes by implementing the collaborative advice and recommendations of the nursing center division’s chief medical officer, senior clinical operations staff and rehabilitation therapists, and |
| • | implement recommendations of our performance improvement committees established at the division, regional and district levels that analyze data, set quality goals and oversee all quality assurance and quality improvement activities throughout the division. |
14
Table of Contents
Enhancing Sales and Marketing Programs. We conduct our nursing and rehabilitation center marketing efforts, which focus on the quality of care provided at our nursing and rehabilitation centers, at the local market level through our nursing and rehabilitation center executive directors, clinical liaisons, admissions coordinators and/or other center-based sales and marketing personnel. The marketing efforts of our nursing and rehabilitation center personnel are supplemented by strategies provided by our divisional, regional and district marketing staffs. We also continue to refocus our marketing efforts to address the difference between the needs of short-term rehabilitation patients and those seeking long-term care. To better promote our services we are:
| • | concentrating our sales and marketing resources toward our transitional care, sub-acute and Alzheimer’s units, |
| • | working to improve our relationships with existing local referral sources and identifying and developing new referral sources and promoting our value proposition, |
| • | expanding the number of clinical liaisons and admission coordinators, particularly at the nursing and rehabilitation center level, and implementing community outreach programs, |
| • | focusing on improving the recruiting, training and retention of sales and marketing personnel and improving accountability, and |
| • | reconfiguring and streamlining our admission documentation process to address a higher volume of short-term admissions. |
Increasing Operating Efficiency. The nursing center division continually seeks to improve operating efficiency with a view to maintaining high quality care. We believe that operating efficiency is critical to maintaining our position as a leading provider of nursing center services in the United States. To improve operating efficiency we strive to:
| • | increase our average patient occupancy levels, which leverages higher revenues over the fixed costs associated with operating our nursing and rehabilitation centers, |
| • | manage our labor costs by improving nurse and other staff retention, maintaining competitive labor rates and reducing reliance on overtime compensation and temporary nursing agency services, |
| • | centralize administrative functions such as accounting, payroll, legal, reimbursement, compliance and information systems, |
| • | enhance our quality assurance, risk management and liability claims defense initiatives to address professional liability and workers compensation costs, |
| • | enhance monitoring of our ancillary expenses, such as rehabilitation and pharmacy costs, that grow in an environment of increased admissions and higher acuity patients, and |
| • | continue to upgrade our management information systems to provide financial and clinical reporting, and improve billing and collections. |
Nursing and Rehabilitation Center Development. The nursing center division continually seeks ways to improve its existing portfolio. We have:
| • | acquired four nursing and rehabilitation centers with a total of 510 nursing and rehabilitation center beds and one assisted living facility with 136 assisted living beds during 2010, |
| • | repositioned our portfolio by divesting six underperforming nursing and rehabilitation centers with approximately 800 licensed beds in the last three years, |
| • | increased our focus on the opportunities available to us in markets where we operate multiple nursing and rehabilitation centers or in which we have affiliated hospitals. These cluster markets present opportunities for our nursing and rehabilitation centers and hospitals to share centralized business office operations and collaborate on their sales and marketing and managed care strategies. These cluster markets also allow us to better coordinate and manage the continuum of care for each of our |
15
Table of Contents
| patients and residents, implement physician services strategies and reduce re-hospitalizations. We believe a more market focused approach will increase admissions over time, better educate the marketplace on our ability to care for post-acute patients and enhance our capabilities to care for patients across various post-acute settings, |
| • | continued to seek additional growth opportunities through strategic acquisitions in selected target markets, particularly where an acquisition may assist us in scaling our operations more rapidly and efficiently than internal growth, and |
| • | expanded our transitional care centers and transitional care units to address the needs of more Medicare and managed care short term patients. |
Selected Nursing Center Division Operating Data
The following table sets forth certain operating and financial data for the nursing center division (dollars in thousands, except statistics):
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Revenues |
$ | 2,187,885 | $ | 2,150,342 | $ | 2,093,297 | ||||||
| Operating income |
$ | 302,672 | $ | 305,590 | $ | 321,814 | ||||||
| Facilities in operation at end of period: |
||||||||||||
| Nursing and rehabilitation centers: |
||||||||||||
| Owned or leased |
222 | 218 | 218 | |||||||||
| Managed |
4 | 4 | 4 | |||||||||
| Assisted living facilities |
7 | 6 | 6 | |||||||||
| Licensed beds at end of period: |
||||||||||||
| Nursing and rehabilitation centers: |
||||||||||||
| Owned or leased |
26,957 | 26,711 | 26,935 | |||||||||
| Managed |
485 | 485 | 485 | |||||||||
| Assisted living facilities |
463 | 327 | 317 | |||||||||
| Patient days (a) |
8,675,214 | 8,810,288 | 8,921,598 | |||||||||
| Revenues per patient day (a) |
$ | 252 | $ | 244 | $ | 235 | ||||||
| Average daily census (a) |
23,768 | 24,138 | 24,376 | |||||||||
| Admissions (a) |
76,451 | 72,801 | 69,986 | |||||||||
| Occupancy % (a) |
87.4 | 89.0 | 89.1 | |||||||||
| Medicare average length of stay (a,b) |
34.0 | 35.4 | 35.5 | |||||||||
| Annualized employee turnover % |
39.6 | 38.9 | 48.9 | |||||||||
| Assets at end of period |
$ | 647,355 | $ | 566,592 | $ | 574,710 | ||||||
| Capital expenditures: |
||||||||||||
| Routine |
$ | 37,024 | $ | 39,663 | $ | 44,627 | ||||||
| Development |
26,701 | 5,687 | 5,466 | |||||||||
| (a) | Excludes managed facilities. |
| (b) | Computed by dividing total Medicare discharge patient days by total Medicare discharges. |
Sources of Nursing and Rehabilitation Center Revenues
Nursing and rehabilitation center revenues are derived principally from the Medicare and Medicaid programs and from private and other payors. Consistent with the nursing center industry, changes in the mix of the patient and resident population among these three categories significantly affect the profitability of our nursing and rehabilitation center operations. Although higher acuity patients generally produce the most revenue per patient day, profitability with respect to higher acuity patients is impacted by the costs associated with the higher level of nursing care and other services generally required. In addition, these patients usually have a significantly shorter length of stay.
16
Table of Contents
The following table sets forth the approximate percentages of nursing and rehabilitation center patient days and revenues derived from the payor sources indicated:
| Medicare | Medicaid | Medicare Advantage |
Private and other | |||||||||||||||||||||||||||||
| Year ended December 31, |
Patient days |
Revenues | Patient days |
Revenues | Patient days |
Revenues | Patient days |
Revenues | ||||||||||||||||||||||||
| 2010 |
16 | % | 35 | % | 60 | % | 40 | % | 4 | % | 7 | % | 20 | % | 18 | % | ||||||||||||||||
| 2009 |
17 | 34 | 61 | 42 | 4 | 6 | 18 | 18 | ||||||||||||||||||||||||
| 2008 |
17 | 34 | 61 | 43 | 3 | 5 | 19 | 18 | ||||||||||||||||||||||||
For the year ended December 31, 2010, revenues of the nursing center division totaled approximately $2.2 billion or 47% of our total revenues (before eliminations). For more information regarding the reimbursement for our nursing and rehabilitation center services, see “– Governmental Regulation – Nursing Center Division – Overview of Nursing Center Division Reimbursement.”
Nursing and Rehabilitation Center Facilities
The following table lists by state the number of nursing and rehabilitation centers and assisted living facilities and related licensed beds we operated as of December 31, 2010:
| Number of facilities | ||||||||||||||||||||||||
| State |
Licensed beds |
Owned by us |
Leased from Ventas (2) |
Leased from other parties |
Managed | Total | ||||||||||||||||||
| Alabama (1) |
464 | – | 2 | 1 | – | 3 | ||||||||||||||||||
| Arizona |
562 | – | 3 | 1 | – | 4 | ||||||||||||||||||
| California |
2,437 | 4 | 6 | 11 | – | 21 | ||||||||||||||||||
| Colorado |
464 | – | 4 | – | – | 4 | ||||||||||||||||||
| Connecticut (1) |
522 | – | 5 | – | – | 5 | ||||||||||||||||||
| Georgia (1) |
520 | – | 4 | – | – | 4 | ||||||||||||||||||
| Idaho |
695 | 1 | 7 | – | – | 8 | ||||||||||||||||||
| Indiana |
3,542 | 10 | 13 | 1 | – | 24 | ||||||||||||||||||
| Kentucky (1) |
1,571 | 2 | 10 | 1 | – | 13 | ||||||||||||||||||
| Maine (1) |
756 | – | 8 | 2 | – | 10 | ||||||||||||||||||
| Massachusetts (1) |
4,818 | 2 | 26 | 12 | 3 | 43 | ||||||||||||||||||
| Missouri (1) |
240 | – | – | 3 | – | 3 | ||||||||||||||||||
| Montana (1) |
276 | – | 2 | – | – | 2 | ||||||||||||||||||
| Nevada |
174 | – | 2 | – | – | 2 | ||||||||||||||||||
| New Hampshire (1) |
512 | – | 3 | – | – | 3 | ||||||||||||||||||
| North Carolina (1) |
2,063 | – | 16 | 3 | – | 19 | ||||||||||||||||||
| Ohio (1) |
2,053 | 5 | 9 | 2 | – | 16 | ||||||||||||||||||
| Oregon (1) |
205 | – | 2 | – | – | 2 | ||||||||||||||||||
| Pennsylvania |
103 | – | 1 | – | – | 1 | ||||||||||||||||||
| Rhode Island (1) |
197 | – | 2 | – | – | 2 | ||||||||||||||||||
| Tennessee (1) |
1,065 | – | 3 | 5 | – | 8 | ||||||||||||||||||
| Texas |
405 | 3 | – | – | – | 3 | ||||||||||||||||||
| Utah |
411 | – | 4 | – | – | 4 | ||||||||||||||||||
| Vermont (1) |
300 | – | 1 | – | 1 | 2 | ||||||||||||||||||
| Virginia (1) |
601 | – | 4 | – | – | 4 | ||||||||||||||||||
| Washington (1) |
656 | – | 7 | – | – | 7 | ||||||||||||||||||
| Wisconsin (1) |
1,922 | – | 11 | 1 | – | 12 | ||||||||||||||||||
| Wyoming |
371 | – | 4 | – | – | 4 | ||||||||||||||||||
| Totals |
27,905 | 27 | 159 | 43 | 4 | 233 | ||||||||||||||||||
| (1) | These states have certificate of need regulations. See “– Governmental Regulation – Federal, State and Local Regulation.” |
| (2) | See “– Master Lease Agreements.” |
17
Table of Contents
Nursing Center Division Management and Operations
Each of our nursing and rehabilitation centers is managed by a state-licensed executive director who is supported by other professional personnel, including a director of nursing, nursing assistants, licensed practical nurses, staff development coordinator, activities director, social services director, clinical liaisons, admissions coordinator and business office manager. The directors of nursing are state-licensed nurses who supervise our nursing staffs that include registered nurses, licensed practical nurses and nursing assistants. Staff size and composition vary depending on the size and occupancy of each nursing and rehabilitation center, the types of services provided and the acuity level of the patients and residents. The nursing and rehabilitation centers contract with physicians who provide medical director services and serve on performance improvement committees. We provide our centers with centralized information systems, federal and state reimbursement expertise, state licensing and Medicare and Medicaid certification and maintenance support, as well as legal, finance, accounting, purchasing and facilities management support. The centralization of these services improves operating efficiencies, promotes the standardization of certain processes and permits our healthcare staff to focus on the delivery of quality care.
Our nursing center division is managed by a division president and a chief financial officer. Our nursing center operations are divided into three geographic regions, each of which is headed by an operational senior vice president. These three operational senior vice presidents report to the division president. The clinical issues and quality concerns of the nursing center division are overseen by the division’s chief medical officer and a divisional medical director as well as a senior vice president of clinical and nursing operations with assistance from our regional and district teams. The sales and marketing efforts for the division are led by our senior vice president of sales and marketing with assistance from our regional and district teams. Divisional, regional and/or district staff also support the nursing center division in the areas of nursing, dietary services, federal and state reimbursement, human resources management, maintenance and financial services.
Quality Assessment and Improvement
Quality of care is monitored and enhanced by our clinical operations personnel as well as our performance improvement committees and family satisfaction surveys. Our performance improvement committees oversee resident healthcare needs and resident and staff safety. Additionally, physician medical directors serve on these committees and advise on healthcare policies and procedures. Regional and district nursing professionals visit our nursing and rehabilitation centers periodically to review practices and recommend improvements where necessary in the level of care provided and to ensure compliance with requirements under applicable Medicare and Medicaid regulations. Surveys of residents’ families are conducted on a regular basis and provide an opportunity for families to rate various aspects of our service and the physical condition of our nursing and rehabilitation centers. These surveys are reviewed by performance improvement committees at each nursing and rehabilitation center to promote and improve resident care.
The nursing center division provides training programs for nursing center executive directors, business office and other department managers, nurses and nursing assistants. These programs are designed to maintain high levels of quality patient and resident care, with an orientation towards regulatory compliance.
Substantially all of our nursing and rehabilitation centers are certified to provide services under the Medicare and Medicaid programs. A nursing center’s qualification to participate in such programs depends upon many factors, such as accommodations, equipment, clinical services, safety, personnel, physical environment and adequacy of policies and procedures.
Nursing Center Division Competition
Our nursing and rehabilitation centers compete with other nursing centers and similar long-term care facilities primarily on the basis of quality of care, reputation, location and physical appearance and, in the case of private payment residents, the charges for our services. Our nursing and rehabilitation centers also compete on a
18
Table of Contents
local and regional basis with other nursing centers as well as with facilities providing similar services, including hospitals, extended care centers, assisted living facilities, home health agencies and similar institutions. Some competitors may operate newer facilities and may provide services that we do not offer. Our competitors include government-owned, religious organization-owned, secular not-for-profit and for-profit institutions. Many of these competitors have greater financial and other resources than we do. Although there is limited, if any, price competition with respect to Medicare and Medicaid residents (since revenues received for services provided to these residents are based generally on fixed rates), there is substantial price competition for private payment residents.
REHABILITATION DIVISION
Our rehabilitation division provides rehabilitative services including physical and occupational therapies and speech pathology services, to residents and patients of nursing centers, acute and long-term acute care hospitals, outpatient clinics, home health agencies, assisted living facilities, school districts and hospice providers. We provide rehabilitative services to 541 nursing centers, 97 hospitals and 58 other locations in 40 states under the name “Peoplefirst Rehabilitation.” Approximately 61% of the rehabilitation division’s revenues in 2010 were generated from therapy services contracts with our hospitals and nursing and rehabilitation centers.
Our rehabilitation division employs approximately 10,000 therapists and had revenues of approximately $505 million (before eliminations) in 2010. We are organized into seven geographic regions.
Our rehabilitation division provides specialized rehabilitation programs designed to meet the individual needs of the residents and patients we serve. Our specialized care programs address complex medical needs, such as wound care, pain management, cognitive retraining, in addition to neurologic, orthopedic, cardiac and pulmonary recovery.
Peoplefirst Rehabilitation provides clinical education and programming which is developed and supported by our clinical experts. These programs are implemented in an effort to ensure clinical practices that support the provision of quality rehabilitation services in accordance with applicable standards of care.
Peoplefirst Rehabilitation recruits and retains qualified professionals with the clinical expertise to provide quality patient care and measurable rehabilitation outcomes. Peoplefirst Rehabilitation also provides regulatory expertise and compliance support that benefits our clients and their residents and patients.
Rehabilitation Division Strategy
Our goals are to be the leading rehabilitation services provider and employer of choice in the markets we serve and to increase our market share and name recognition through contract growth. Our strategies for achieving these goals include:
Improving Quality Care and Customer Satisfaction. Our rehabilitation division is committed to providing effective and efficient care to the residents and patients to whom we provide rehabilitation services. We have implemented the following measures in an effort to improve the operations of our customers with the goal of enhancing the quality of care provided to their residents and patients:
| • | we have specialized rehabilitation programs to promote quality care. Such programs focus on residents and patients with Alzheimer’s disease and other forms of dementia, pain management and medically complex, orthopedic and neurological rehabilitation needs; |
| • | we promote the competencies of our therapists by providing extensive training and implementing a best practices approach to the provision of rehabilitation services; |
19
Table of Contents
| • | we take an integrated approach to delivering rehabilitation services as a key member of our customer’s interdisciplinary care team and work to enhance our customer’s quality care objectives; |
| • | we have developed a proprietary nationwide rehabilitation information system that allows us to access management and clinical reports which provide quality assurance measures, identify industry trends, track patient outcomes and streamline invoicing; and |
| • | we have implemented the use of technological enhancements, such as handheld devices for capturing information related to the provision of rehabilitation services. These devices increase the efficiency of our therapists and support compliance with the regulations which govern documentation of rehabilitation services. |
Effective Recruiting and Retention of Qualified Therapists. The healthcare industry is facing a significant shortage of qualified therapists. In an effort to provide quality care to the patients and residents to whom we provide rehabilitation services, we continuously strive to recruit and retain qualified therapists. We offer competitive incentive and recognition programs for our therapists and have increased our recruiting infrastructure to reduce open positions, decrease contract labor and improve productivity. We also promote continuing education opportunities to enhance the personal knowledge and growth of our therapists and encourage our therapists’ participation in nurturing a culture of quality and customer service.
Increasing Operating Efficiency. We seek to improve our operating efficiency by increasing the productivity of our therapists and other rehabilitation staff. We have developed standard division-wide labor productivity tools to monitor and better manage therapist productivity as well as our staffing models. In an effort to enable our therapists to focus their attention on providing quality rehabilitation services to patients and residents, we have implemented the use of technological enhancements and clinical protocols that promote best practices.
Growing Through Business Development and External Contract Sales. Our growth strategy is focused on the enhancement of rehabilitation programs for the customers we serve and the expansion of our business in strategic markets. These markets include locations in which we already have a significant presence, where demand may exist for our services, or where we wish to expand the provision of our services. Our efforts will continue to target customers in both the acute and post-acute care settings. In order to increase market share, our initiatives include demonstrating our value proposition to customers in the areas of clinical excellence and programming, staff recruitment and retention, regulatory and reimbursement support, census development and committed customer service. In addition, we continue to promote a greater awareness of the services we provide by enhancing sales and marketing strategies and through the use of our Peoplefirst website.
Growth Through Selective Acquisitions. We seek growth opportunities through strategic acquisitions in selected target markets, particularly where an acquisition may assist us in scaling our operations more rapidly and efficiently than internal growth. The RehabCare acquisition will substantially expand our rehabilitation business.
Growth Through Home Care and Hospice Operations. We have continued to expand our presence into the home care and hospice markets, and now provide services in four states through 15 offices. In connection with this expansion, we acquired a hospice business in 2009 and a home health company in 2010 that operates in ten locations. Revenues from our home care and hospice operations totaled approximately $18 million in fiscal 2010.
Capital Investments. We are expanding our operational and capital programs to refurbish and expand gym space, upgrade equipment and enhance our brand image in several of the sub-acute units, transitional care centers and transitional care units in which we provide services.
20
Table of Contents
Selected Rehabilitation Division Operating Data
The following table sets forth certain operating and financial data for the rehabilitation division (dollars in thousands):
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Revenues: |
||||||||||||
| Company-operated |
$ | 306,464 | $ | 288,265 | $ | 268,663 | ||||||
| Non-affiliated |
198,491 | 186,773 | 158,657 | |||||||||
| $ | 504,955 | $ | 475,038 | $ | 427,320 | |||||||
| Operating income |
$ | 51,923 | $ | 50,592 | $ | 38,071 | ||||||
| Number of customer contracts: |
||||||||||||
| Company-operated |
315 | 306 | 310 | |||||||||
| Non-affiliated |
381 | 316 | 345 | |||||||||
| Revenue per site |
$ | 777,069 | $ | 730,345 | $ | 651,895 | ||||||
| Therapist productivity % |
82.0 | 84.2 | 81.4 | |||||||||
| Annualized employee turnover % |
14.4 | 12.8 | 13.3 | |||||||||
| Assets at end of period |
$ | 87,853 | $ | 53,856 | $ | 45,733 | ||||||
| Routine capital expenditures |
$ | 2,715 | $ | 1,043 | $ | 1,162 | ||||||
“Therapist productivity %” is computed by dividing labor minutes related to patient care by total labor minutes for the period.
Sources of Rehabilitation Division Revenues
The rehabilitation division receives payment for the rehabilitation services it provides to residents and patients of the customers that we serve. The payments are based upon negotiated patient per diem rates, negotiated per minute rates, or a negotiated fee schedule based upon the types of services rendered. For the year ended December 31, 2010, revenues of the rehabilitation division totaled approximately $505 million or 11% of our total revenues (before eliminations). As a provider of services to healthcare providers, trends and developments in healthcare reimbursement will impact our revenues and growth. Changes in the reimbursement provided by Medicare or Medicaid to our customers can impact the demand and pricing for our services. For more information regarding the reimbursement for our rehabilitation services, see “– Governmental Regulation – Rehabilitation Division – Overview of Rehabilitation Division Revenues,” “– Governmental Regulation – Hospital Division – Overview of Hospital Division Reimbursement,” and “– Governmental Regulation – Nursing Center Division – Overview of Nursing Center Division Reimbursement.”
21
Table of Contents
Geographic Coverage
The following table lists by state the number of hospitals, nursing centers and other rehabilitation customer contracts we serviced as of December 31, 2010:
| Hospitals | Nursing centers | Other | Total | |||||||||||||||||||||||||
| State |
Company operated |
Non-affiliated | Company operated |
Non-affiliated | Non-affiliated | Company operated |
Non-affiliated | |||||||||||||||||||||
| Alabama |
– | – | 3 | 1 | – | 3 | 1 | |||||||||||||||||||||
| Arizona |
4 | – | 4 | 1 | 2 | 8 | 3 | |||||||||||||||||||||
| California |
15 | – | 21 | 6 | – | 36 | 6 | |||||||||||||||||||||
| Colorado |
1 | – | 4 | – | 3 | 5 | 3 | |||||||||||||||||||||
| Connecticut |
– | – | 6 | 8 | – | 6 | 8 | |||||||||||||||||||||
| Delaware |
– | – | – | 1 | – | – | 1 | |||||||||||||||||||||
| Florida |
10 | – | – | 4 | 3 | 10 | 7 | |||||||||||||||||||||
| Georgia |
1 | – | 4 | 9 | – | 5 | 9 | |||||||||||||||||||||
| Idaho |
– | – | 8 | 1 | 5 | 8 | 6 | |||||||||||||||||||||
| Illinois |
6 | – | – | 30 | 4 | 6 | 34 | |||||||||||||||||||||
| Indiana |
2 | – | 24 | 5 | 13 | 26 | 18 | |||||||||||||||||||||
| Iowa |
– | – | – | 1 | – | – | 1 | |||||||||||||||||||||
| Kentucky |
2 | – | 13 | 19 | 5 | 15 | 24 | |||||||||||||||||||||
| Louisiana |
1 | – | – | – | – | 1 | – | |||||||||||||||||||||
| Maine |
– | – | 8 | 4 | – | 8 | 4 | |||||||||||||||||||||
| Maryland |
– | – | – | 20 | – | – | 20 | |||||||||||||||||||||
| Massachusetts |
7 | 1 | 42 | 7 | – | 49 | 8 | |||||||||||||||||||||
| Michigan |
– | 1 | – | – | – | – | 1 | |||||||||||||||||||||
| Missouri |
3 | – | 2 | 3 | – | 5 | 3 | |||||||||||||||||||||
| Montana |
– | – | 2 | – | 3 | 2 | 3 | |||||||||||||||||||||
| Nebraska |
– | – | – | 2 | – | – | 2 | |||||||||||||||||||||
| Nevada |
3 | 1 | 2 | 2 | 1 | 5 | 4 | |||||||||||||||||||||
| New Hampshire |
– | – | 3 | 1 | 1 | 3 | 2 | |||||||||||||||||||||
| New Jersey |
2 | – | – | – | – | 2 | – | |||||||||||||||||||||
| New Mexico |
1 | 1 | – | – | – | 1 | 1 | |||||||||||||||||||||
| North Carolina |
1 | – | 19 | 43 | 3 | 20 | 46 | |||||||||||||||||||||
| Ohio |
3 | 2 | 14 | 42 | 7 | 17 | 51 | |||||||||||||||||||||
| Oklahoma |
2 | – | – | – | – | 2 | – | |||||||||||||||||||||
| Oregon |
– | – | 2 | 1 | – | 2 | 1 | |||||||||||||||||||||
| Pennsylvania |
7 | – | 1 | 11 | – | 8 | 11 | |||||||||||||||||||||
| Rhode Island |
– | – | 2 | 4 | – | 2 | 4 | |||||||||||||||||||||
| South Carolina |
1 | – | – | – | – | 1 | – | |||||||||||||||||||||
| Tennessee |
1 | – | 8 | 9 | – | 9 | 9 | |||||||||||||||||||||
| Texas |
11 | 4 | 3 | 22 | 5 | 14 | 31 | |||||||||||||||||||||
| Utah |
– | – | 4 | – | – | 4 | – | |||||||||||||||||||||
| Vermont |
– | – | 2 | 3 | – | 2 | 3 | |||||||||||||||||||||
| Virginia |
1 | – | 4 | 30 | – | 5 | 30 | |||||||||||||||||||||
| Washington |
1 | – | 7 | 9 | 3 | 8 | 12 | |||||||||||||||||||||
| Wisconsin |
1 | – | 12 | 14 | – | 13 | 14 | |||||||||||||||||||||
| Wyoming |
– | – | 4 | – | – | 4 | – | |||||||||||||||||||||
| Totals |
87 | 10 | 228 | 313 | 58 | 315 | 381 | |||||||||||||||||||||
22
Table of Contents
Sales and Marketing
The rehabilitation division’s sales and marketing strategy focuses on the outsourcing needs of long-term care facilities and hospitals by emphasizing the broad range of rehabilitation programs, clinical expertise, and competitive pricing that we can provide. The rehabilitation division’s new business efforts are led by the vice president of business development and five directors of business development in geographically defined regions.
Rehabilitation Division Management and Operations
We have four nursing center and three hospital regions organized predominantly by the geographic location of our customers. Each of our rehabilitation programs has an on-site manager that reports to an area rehabilitation director. The area director is responsible for the overall management of eight to 12 on-site managers. The area directors report to their respective division vice president of rehabilitation operations.
We provide our program staff with centralized information systems, federal and state reimbursement expertise, professional licensing support, as well as legal, finance, accounting and purchasing support. The centralization of these services improves operating efficiencies, promotes the standardization of certain processes and permits program staff to focus on the delivery of quality, medically necessary rehabilitation services.
A division president and a chief financial officer manage our rehabilitation division. Our operations are divided between the nursing center line of business and hospital line of business and each is headed by an officer of the division who reports to the division president. A senior vice president of clinical operations manages the clinical education of our therapists and our quality care initiatives.
Rehabilitation Division Competition
In the geographic markets that we serve, there are national, regional and local rehabilitation services providers that offer rehabilitation services comparable to ours. A number of our competitors may have greater financial and other resources than us, may be more established in the markets in which we compete and may be willing to provide services at lower prices. In addition, a number of long-term care facilities and hospitals may elect not to outsource rehabilitation services thereby reducing our potential customer base. While there are several large rehabilitation providers, the market generally is highly fragmented and is primarily comprised of smaller independent providers.
We believe our rehabilitation division generally competes on its reputation for providing quality rehabilitation services, qualified therapists and competitive pricing.
GOVERNMENTAL REGULATION
Various healthcare reform provisions became law upon enactment of the ACA. The reforms contained in the ACA will impact each of our businesses in some manner. Several of the reforms are very significant and could ultimately change the nature of our services, the methods of payment for our services and the underlying regulatory environment. The reforms include possible modifications to the conditions of qualification for payment, bundling payments to cover both acute and post-acute care and the imposition of enrollment limitations on new providers. The ACA creates a series of robust transparency and reporting requirements for skilled nursing facilities including requirements to disclose information on organizational structures, financial, clinical and other related data as well as information on officers, directors, trustees or managing employees. Skilled nursing facilities are required to certify to the Secretary of the U.S. Department of Health and Human Services (“HHS”) and the U.S. Department of Health and Human Services Office of Inspector General (the “OIG”) that the information submitted is accurate and current. In addition, the primary goals of healthcare reform are to increase quality and reduce costs. The ACA includes reductions in the reimbursement paid to us and other healthcare providers as well as additional reductions for failure to meet certain quality standards. Moreover, healthcare
23
Table of Contents
reform could negatively impact insurance companies, other third party payors, our customers, as well as other healthcare providers, which may in turn negatively impact our business. As such, these healthcare reforms or other similar healthcare reforms could have a material adverse effect on our business, financial position, results of operations and liquidity.
Medicare and Medicaid
Medicare is a federal program that provides certain hospital and medical insurance benefits to persons age 65 and over and certain disabled persons. Medicaid is a medical assistance program administered by each state funded with federal and state funds pursuant to which healthcare benefits are available to certain indigent or disabled patients. Within the Medicare and Medicaid statutory framework, there are substantial areas subject to administrative rulings, interpretations and discretion that may affect payments made under Medicare and Medicaid. A substantial portion of our revenues are derived from patients covered by the Medicare and Medicaid programs. See “Hospital Division – Sources of Hospital Revenues,” “Nursing Center Division – Sources of Nursing and Rehabilitation Center Revenues” and “Rehabilitation Division – Sources of Rehabilitation Division Revenues.”
We could be affected adversely by the continuing efforts of governmental and private third party payors to contain healthcare costs. We cannot assure you that reimbursement payments under governmental and private third party payor programs, including Medicare supplemental insurance policies, will remain at levels comparable to present levels or will be sufficient to cover the costs allocable to patients eligible for reimbursement pursuant to these programs. Medicare reimbursement in LTAC hospitals and nursing centers are subject to fixed payments under the Medicare prospective payment systems. Medicaid reimbursement rates in many states in which we operate nursing and rehabilitation centers also are based upon fixed payment systems. Generally, these rates are adjusted annually for inflation. However, these adjustments may not reflect the actual increase in the costs of providing healthcare services. In addition, Medicaid reimbursement can be impacted negatively by state budgetary pressures, which may lead to reduced reimbursement or delays in receiving payments. In addition, we cannot assure you that the facilities operated by us, or the provision of goods and services offered by us, will meet the requirements for participation in such programs.
The ACA requires reductions to updates in the standard federal rate to LTAC hospitals beginning in the 2010 rate year and productivity adjustment reductions in updates to payments for LTAC hospitals and nursing and rehabilitation centers beginning in fiscal year 2012, which in each case may cause reimbursement to be less than in the prior year. In addition, under the ACA, Medicare payments to hospitals, including LTAC hospitals, are reduced if the hospital fails to meet certain quality data or fails to comply with new value based purchasing programs. Nursing and rehabilitation centers also will be subject to reductions in reimbursement if they fail to meet the standards in new value based purchasing programs.
In addition, there are continuing efforts to reform governmental healthcare programs that could result in major changes in the healthcare delivery and reimbursement systems on a national and state level and we cannot assure you that healthcare reform, future healthcare legislation or other changes in the administration or interpretation of governmental healthcare programs will not have a material adverse effect on our business, financial position, results of operations and liquidity. See “Item 1A – Risk Factors – Risk Factors Relating to Reimbursement and Regulation of Our Business – Changes in the reimbursement rates or methods or timing of payment from third party payors, including the Medicare and Medicaid programs, or the implementation of other measures to reduce reimbursement for our services and products could result in a substantial reduction in our revenues and operating margins.”
Federal, State and Local Regulations
The extensive federal, state and local regulations affecting the healthcare industry include, but are not limited to, regulations relating to licensure, conduct of operations, ownership of facilities, addition of facilities, allowable costs, services and prices for services, facility staffing requirements, and the privacy and security of
24
Table of Contents
health-related information. In addition, various anti-fraud and abuse laws, including physician self-referral laws, anti-kickback laws and laws regarding filing of false claims, codified under the Social Security Act and other statutes, prohibit certain business practices and relationships in connection with healthcare services for patients whose care will be paid by Medicare, Medicaid or other governmental programs. Sanctions for violating these anti-fraud and abuse laws include criminal penalties, civil penalties and possible exclusion from government programs such as Medicare and Medicaid.
In the ordinary course of our business, we are subject regularly to inquiries, investigations and audits by federal and state agencies that oversee applicable healthcare program participation and payment regulations, including enhanced medical necessity review of LTAC hospital cases pursuant to the SCHIP Extension Act and audits under the Centers for Medicare and Medicaid Services (“CMS”) Recovery Audit Contractor (“RAC”) program which was expanded pursuant to the Tax Relief and Health Care Act of 2006.
We believe that the regulatory environment surrounding most segments of the healthcare industry remains intense. Federal and state governments continue to impose intensive enforcement policies resulting in a significant number of inspections, citations of regulatory deficiencies and other regulatory penalties including demands for refund of overpayments, terminations from the Medicare and Medicaid programs, bars on Medicare and Medicaid payments for new admissions and civil monetary penalties. These enforcement policies, along with the costs incurred to respond to and defend reviews, audits and investigations, could have a material adverse effect on our business, financial position, results of operations and liquidity. We vigorously contest such penalties where appropriate; however, these cases can involve significant legal and other expenses and consume our resources.
Section 1877 of the Social Security Act, commonly known as the “Stark Law,” provides that a physician may not refer a Medicare or Medicaid patient for a “designated health service” to an entity with which the physician or an immediate family member has a financial relationship unless the financial arrangement meets an exception under the Stark Law or its regulations. Designated health services include inpatient and outpatient hospital services, physical, occupational, and speech therapy, durable medical equipment, prosthetics, orthotics and supplies, diagnostic imaging, enteral and parenteral feeding and supplies and clinical laboratory services. Under the Stark Law, a “financial relationship” is defined as an ownership or investment interest or a compensation arrangement. If such a financial relationship exists and does not meet a Stark Law exception, the entity is prohibited from submitting or claiming payment under the Medicare or Medicaid programs or from collecting from the patient. Many of the compensation arrangements exceptions permit referrals if, among other things, the arrangement is set forth in a written agreement signed by the parties, the compensation to be paid is set in advance, is consistent with fair market value and is not determined in a manner that takes into account the volume or value of any referrals or other business generated between the parties. Exceptions may have other requirements. Any funds collected for an item or service resulting from a referral that violates the Stark Law must be repaid to Medicare, any other third party payor and the patient. In addition, a civil monetary penalty of up to $15,000 for each service may be imposed for presenting or causing to be presented, a claim for a service rendered in violation of the Stark Law. Many states have enacted healthcare provider referral laws that go beyond physician self-referrals or apply to a greater range of services than just the designated health services under the Stark Law.
The federal anti-kickback statute set forth in Section 1128B(b) of the Social Security Act (the “Anti-Kickback Statute”), prohibits the knowing and willful offer, payment, solicitation or receipt of any remuneration, directly or indirectly, overtly or covertly, in cash or in kind, to induce the referral of an individual, in return for recommending, or to arrange for, the referral of an individual for any item or service payable under any federal healthcare program, including Medicare or Medicaid. The OIG has issued regulations that create “safe harbors” for certain conduct and business relationships that are deemed protected under the Anti-Kickback Statute. In order to receive safe harbor protection, all of the requirements of a safe harbor must be met. The fact that a given business arrangement does not fall within one of these safe harbors, however, does not render the arrangement per se illegal. Business arrangements of healthcare service providers that fail to satisfy the applicable safe harbor criteria, if investigated, will be evaluated based on all facts and circumstances and risk
25
Table of Contents
increased scrutiny and possible sanctions by enforcement authorities. The Anti-Kickback Statute is a criminal statute, with penalties of up to $25,000, up to five years in prison, or both. The OIG can pursue a civil claim for violation of the Anti-Kickback Statute under the Civil Monetary Penalty Statute of up to $50,000 per claim and up to three times the amount received from the government for the items or services. We believe that business practices of providers and financial relationships between providers have become subject to increased scrutiny as healthcare reform efforts continue on the federal and state levels. State Medicaid programs are required to enact an anti-kickback statute. Many states have adopted or are considering similar legislative proposals, some of which extend beyond the Medicaid program, to prohibit the payment or receipt of remuneration for the referral of patients regardless of the source of payment for the care.
The U.S. Department of Justice (the “DOJ”) may bring an action under the federal False Claims Act (the “FCA”), alleging that a healthcare provider has defrauded the government by submitting a claim for items or services not rendered as claimed, which may include coding errors, billing for services not provided and submitting false cost reports. The Fraud Enforcement and Recovery Act of 2009 expanded the scope of the FCA by, among other things, creating liability for knowingly and improperly avoiding repayment of an overpayment received from the government and broadening protections for whistleblowers. The ACA clarifies that if an item or service is provided in violation of the Anti-Kickback Statute, the claim submitted for those items or services is a false claim that may be prosecuted under the FCA as a false claim. Civil penalties under the FCA are between $5,500 and $11,000 for each claim and up to three times of the amount claimed. Under the qui tam or “whistleblower” provisions of the FCA, a private individual with knowledge of fraud may bring a claim on behalf of the federal government and receive a percentage of the federal government’s recovery. Due to these whistleblower incentives, lawsuits have become more frequent.
In addition to the penalties described above, violation of any of these laws may subject us to exclusion from participation in any federal or state healthcare program. These fraud and abuse laws and regulations are complex, and we do not always have the benefit of significant regulatory or judicial interpretation of these laws and regulations. While we do not believe our arrangements are in violation of these prohibitions, we cannot assure you that governmental officials charged with the responsibility for enforcing the provisions of these prohibitions will not assert that one or more of our arrangements are in violation of the provisions of such laws and regulations.
The Balanced Budget Act of 1997 (the “Balanced Budget Act”) also includes a number of anti-fraud and abuse provisions. The Balanced Budget Act contains additional civil monetary penalties for violations of the Anti-Kickback Statute discussed above and imposes an affirmative duty on healthcare providers to ensure that they do not employ or contract with persons excluded from the Medicare program. The Balanced Budget Act also provides a minimum ten-year period for exclusion from participation in federal healthcare programs for persons or entities convicted of a prior healthcare offense.
Various states in which we operate hospitals and nursing and rehabilitation centers have established minimum staffing requirements or may establish minimum staffing requirements in the future. The implementation of these staffing requirements in some states is not contingent upon any additional appropriation of state funds in any budget act or other statute. Our ability to satisfy such staffing requirements will depend upon our ability to attract and retain qualified healthcare professionals, including nurses, certified nurse’s assistants, therapists and other staff. Failure to comply with such minimum staffing requirements may result in the imposition of fines or other sanctions. If states do not appropriate sufficient additional funds to pay for any additional operating costs resulting from such minimum staffing requirements, our profitability may be materially adversely affected. See “Item 1A – Risk Factors – Risk Factors Relating to Our Operations – We could experience significant legal actions, fines and increases in our operating costs if we fail to comply with state minimum staffing requirements.”
The International Classification of Diseases (“ICD”) is a classification system for diseases and signs, symptoms, abnormal findings, complaints, social circumstances and external causes of injury or diseases,
26
Table of Contents
promulgated by the World Health Organization. HHS has mandated that healthcare payors and providers and their vendors must convert from the current ICD-9 coding system to the materially different ICD-10 coding system by October 1, 2013. ICD-10 is the first major change in diagnosis and procedure coding in three decades.
HIPAA. The federal Health Insurance Portability and Accountability Act of 1996, commonly known as “HIPAA,” among other requirements, broadened the scope of existing fraud and abuse laws and mandated the adoption of administrative simplification regulations aimed at standardizing transaction formats and billing codes for documenting medical services, dealing with claims submissions and protecting the privacy and security of individually identifiable health information. HIPAA regulations that standardize transactions and code sets require standard formatting for healthcare providers, like us, that submit claims electronically.
The HIPAA privacy regulations apply to “protected health information,” which is defined generally as individually identifiable health information transmitted or maintained in any form or medium, excluding certain types of records such as education records. The privacy regulations seek to limit the use and disclosure of most paper and oral communications, as well as those in electronic form, regarding an individual’s past, present or future physical or mental health or condition, or relating to the provision of healthcare to the individual or payment for that healthcare, if the individual can or may be identified by such information. HIPAA provides for the imposition of civil and/or criminal penalties if protected health information is improperly disclosed.
HIPAA’s security regulations require us to ensure the confidentiality, integrity, and availability of all electronically protected health information that we create, receive, maintain or transmit. We must protect against reasonably anticipated threats or hazards to the security of such information and the unauthorized use or disclosure of such information. The HIPAA unique health identifier standards require us to obtain and use national provider identifiers.
The Health Information Technology for Economic and Clinical Health Act, known as the “HITECH Act,” was passed in 2009 and instituted new HIPAA requirements regarding providing individuals with notification of breaches of their unsecured protected health information and reporting to the media of violations involving more than 500 individuals in a single jurisdiction, as well as immediate reporting to HHS of any violation involving more than 500 individuals for publication on the HHS website. The HITECH Act also imposed new requirements on HIPAA business associates and strengthened HIPAA enforcement provisions, including civil monetary penalty amounts.
We believe we are in substantial compliance with the HIPAA regulations. We cannot assure you that potential non-compliance by us with HIPAA regulations will not have a material adverse effect on our business, financial position, results of operations and liquidity.
Certificates of Need and State Licensing. Certificate of need, or CON, regulations control the development and expansion of healthcare services and facilities in certain states. Certain states also require regulatory approval prior to certain changes in ownership of a hospital or nursing center. Certain states that do not have CON programs may have other laws or regulations that limit or restrict the development or expansion of healthcare facilities. We operate hospitals in 12 states and nursing and rehabilitation centers in 18 states that require state approval for the expansion of our facilities and services under CON programs. To the extent that CONs or other similar approvals are required for expansion of the operations of our hospitals or nursing and rehabilitation centers, either through facility acquisitions, expansion or provision of new services or other changes, such expansion could be affected adversely by the failure or inability to obtain the necessary approvals, changes in the standards applicable to such approvals or possible delays and expenses associated with obtaining such approvals.
We are required to obtain state licenses to operate each of our hospitals and nursing and rehabilitation centers and to ensure their participation in government programs. Once a hospital or nursing and rehabilitation center becomes licensed and operational, it must continue to comply with federal, state and local licensing requirements in addition to local building and life-safety codes. All of our hospitals and nursing and
27
Table of Contents
rehabilitation centers have the necessary licenses. Failure of our hospitals and nursing and rehabilitation centers to satisfy applicable licensure and certification requirements could have a material adverse effect on our business, financial position, results of operations and liquidity.
Hospital Division
General Regulations. The hospital division is subject to various federal and state regulations. In order to receive Medicare reimbursement, each hospital must meet the applicable conditions of participation set forth by HHS relating to the type of hospital, its equipment, personnel and standard of medical care, as well as comply with state and local laws and regulations. We have developed a management system to facilitate our compliance with these various standards and requirements. Among other things, each hospital employs a person who is responsible for leading an ongoing quality assessment and improvement program. Hospitals undergo periodic on-site Medicare certification surveys, which generally are limited in frequency if the hospital is accredited by the Joint Commission. As of December 31, 2010, 88 hospitals operated by the hospital division were certified as Medicare LTAC providers and one hospital has a pending certification as a Medicare short-term acute care provider. In addition, 76 hospitals also were certified by their respective state Medicaid programs. Loss of certification could affect adversely a hospital’s ability to receive payments from the Medicare and Medicaid programs.
As noted above, the hospital division also is subject to federal and state laws that govern financial and other arrangements between healthcare providers. These laws prohibit, among other things, certain direct and indirect payments for the referral of patients, certain referrals by physicians if they or their immediate family members have a financial relationship with the hospital, or fee-splitting arrangements between healthcare providers that are designed to induce or encourage the referral of patients to, or the recommendation of, a particular provider for medical products and services. Such laws include the Anti-Kickback Statute, the Stark Law and the FCA. In addition, some states restrict certain business relationships between physicians and ancillary service providers and some states prohibit business corporations from providing, or holding themselves out as a provider of, medical care. Possible sanctions for violation of any of these restrictions or prohibitions include loss of licensure or eligibility to participate in reimbursement programs as well as civil and criminal penalties. These laws vary considerably from state to state.
Accreditation by the Joint Commission or the AOA. Hospitals may receive accreditation from the Joint Commission or the AOA, national organizations that establish standards relating to the physical plant, administration, quality of patient care and operation of medical staffs of hospitals. With respect to accreditation by the Joint Commission, hospitals and certain other healthcare facilities are generally required to have been in operation at least four months in order to be eligible. After conducting on-site surveys, the Joint Commission awards accreditation for up to three years to hospitals found to be in substantial compliance with Joint Commission standards. Accredited hospitals also are periodically resurveyed, at the option of the Joint Commission, upon a major change in facilities or organization and after merger or consolidation. With respect to the AOA, the accreditation process includes and in-depth review of both open and closed patient records as well as on-site surveys, including direct observation of the care being provided. As of December 31, 2010, all of the hospitals operated by the hospital division were accredited by either the Joint Commission or the AOA or were in the process of seeking accreditation. The hospital division intends to seek and obtain Joint Commission or AOA accreditation for any additional facilities it may operate in the future.
Peer Review. Federal regulations provide that admission to and utilization of hospitals by Medicare and Medicaid patients must be reviewed by peer review organizations or quality improvement organizations in order to ensure efficient utilization of hospitals and services. A quality improvement organization may conduct such review either prospectively or retrospectively and may, as appropriate, recommend denial of payments for services provided to a patient. The review is subject to administrative and judicial appeals. Each of the hospitals operated by our hospital division employs a clinical professional to administer the hospital’s integrated quality assurance and improvement program. Denials by third party utilization review organizations historically have not had a material adverse effect on the hospital division’s operating results.
28
Table of Contents
Overview of Hospital Division Reimbursement
Medicare Reimbursement of Short-term Acute Care Hospitals – Medicare reimburses general short-term acute care hospitals under a prospective payment system (“IPPS”). Under IPPS, Medicare inpatient costs are reimbursed based upon a fixed payment amount per discharge using medical severity diagnostic related groups (“MS-DRGs”). The MS-DRG payment under IPPS is based upon the national average cost of treating a Medicare patient’s condition. Although the average length of stay varies for each MS-DRG, we believe that the average stay for all Medicare patients subject to IPPS is approximately six days. An additional outlier payment is made for patients with higher treatment costs but these payments are designed only to cover marginal costs. Hospitals that are certified by Medicare as LTAC hospitals are excluded from the IPPS.
Medicare Reimbursement of Long-term Acute Care Hospitals – Since October 2002, the Medicare payment system for LTAC hospitals has been based upon the Long-Term Acute Care Prospective Payment System (“LTAC PPS”), a prospective payment system specifically for LTAC hospitals. LTAC PPS maintains LTAC hospitals as a distinct provider type, separate from short-term acute care hospitals. Only providers certified as LTAC hospitals may be paid under this system. To maintain certification under LTAC PPS, the average length of stay of Medicare patients must be greater than 25 days.
CMS has, for a number of years, considered the development of facility and patient certification criteria for LTAC hospitals, potentially as an alternative to the current certification system pursuant to which LTAC hospitals must maintain an average Medicare length of stay of 25 days. In 2004, the Medicare Payment Advisory Commission, a commission chartered by Congress to advise it on Medicare payment issues (“MedPAC”), recommended to Congress the adoption by CMS of new facility staffing and services criteria and patient clinical characteristics and treatment requirements for LTAC hospitals in order to ensure that only appropriate patients are admitted to these facilities. Since the MedPAC recommendation, CMS has initiated studies to examine such recommendations and those studies are ongoing. Implementation of additional criteria that may limit the population of patients eligible for our hospital services or change the basis on which we are paid could have a material adverse effect on our business, financial position, results of operations and liquidity.
On August 1, 2007, CMS issued final regulations regarding Medicare hospital inpatient payments to short-term acute care hospitals as well as certain provisions affecting LTAC hospitals. These regulations adopt a new system for LTAC hospitals for classifying patients into diagnostic categories called Medicare Severity Diagnosis Related Groups or more specifically, for LTAC hospitals, “MS-LTC-DRGs.” LTAC PPS is based upon discharged-based MS-LTC-DRGs similar to the system used to pay short-term acute care hospitals. This new MS-LTC-DRG system replaced the previous diagnostic related group system for LTAC hospitals and became effective for discharges occurring on or after October 1, 2007. The MS-LTC-DRG system created additional severity-adjusted categories for most diagnoses.
While the clinical system which groups procedures and diagnoses is identical to the prospective payment system for short-term acute care hospitals, LTAC PPS utilizes different rates and formulas. Three types of payments are used in this system: (a) short-stay outlier payment, which provides for patients whose length of stay is less than 5/6th of the geometric mean length of stay for that MS-LTC-DRG, based upon the lesser of (1) a per diem based upon the average payment for that MS-LTC-DRG, (2) the estimated costs, (3) the full MS-LTC-DRG payment, or (4) a blend of an amount comparable to what would otherwise be paid under IPPS computed as a per diem, capped at the full IPPS MS-DRG comparable payment amount and a per diem based upon the average payment for that MS-LTC-DRG under LTAC PPS; (b) MS-LTC-DRG fixed payment which provides a single payment for all patients with a given MS-LTC-DRG, regardless of length of stay, cost of care or place of discharge; and (c) high cost outlier that will provide a partial coverage of costs for patients whose cost of care far exceeds the MS-LTC-DRG reimbursement. For patients in the high cost outlier category, Medicare will reimburse 80% of the costs incurred above a threshold, defined as the MS-LTC-DRG reimbursement plus a fixed loss amount per discharge.
29
Table of Contents
On July 31, 2008, CMS issued final regulations regarding the re-weighting of MS-LTC-DRGs for discharges occurring on or after October 1, 2008. CMS announced that this update was made in a budget neutral manner, and that estimated aggregate LTAC Medicare payments would be unaffected by these regulations. Based upon our experience under these final regulations, it appears that the re-weighting increased payments for the care of higher acuity patients.
On May 29, 2009, CMS issued an interim final rule that revised the October 1, 2008 payment weights. Effective June 3, 2009, CMS reduced MS-LTC-DRG payment weights by 3.9%, resulting in approximately a 0.9% reduction of the estimated total LTAC PPS payments in the federal fiscal year ending September 30, 2009. No retroactive adjustments to payments were made. On July 31, 2009, CMS finalized this interim rule.
LTAC PPS provides for an adjustment for differences in area wages resulting from salary and benefit variations. There also are additional rules for payment for patients who are transferred from a LTAC hospital to another healthcare setting and are subsequently re-admitted to the LTAC hospital. The LTAC PPS payment rates also are subject to annual adjustments.
Medicare regulations require that when two or more hospital facilities share the same provider number and are considered to be a single hospital, the “remote” or “satellite” facility must meet certain criteria with respect to the “main” facility. These criteria relate largely to demonstrating a high level of integration between the two facilities. If the criteria are not met, each facility would need to meet all Medicare requirements independently, including, for example, the minimum average length of patient stay for LTAC hospital qualification. It is advantageous for certain satellite facilities that may not independently be able to meet these Medicare requirements to maintain provider-based status so that they will be reimbursed at the higher rate for LTAC hospitals under Medicare. If CMS determines that facilities claiming to be provider-based and being reimbursed accordingly do not meet the integration requirements of the regulations, CMS may recover the amount of any excess reimbursements based upon that claimed status. We have several hospitals in which multiple facilities share a Medicare provider number, and the failure of any one or more of them to meet the provider-based status regulations could materially and adversely affect our business, financial position, results of operations and liquidity.
The LTAC PPS system is subject to significant change. Slight variations in patient acuity or length of stay could significantly change Medicare revenues generated under LTAC PPS. In addition, our hospitals may not be able to appropriately adjust their operating costs to changes in patient acuity and length of stay or to changes in reimbursement rates. In addition, we cannot assure you that LTAC PPS will not have a material adverse effect on revenues from commercial third party payors. Various factors, including a reduction in average length of stay, have negatively impacted revenues from commercial third party payors in recent years.
SCHIP Extension Act.
The SCHIP Extension Act became law on December 29, 2007. This legislation provides for, among other things:
| (1) | a mandated study by the Secretary of HHS on the establishment of LTAC hospital certification criteria; |
| (2) | enhanced medical necessity review of LTAC hospital cases; |
| (3) | a three-year moratorium on the establishment of a LTAC hospital or satellite facility, subject to exceptions for facilities under development; |
| (4) | a three-year moratorium on an increase in the number of licensed beds at a LTAC hospital or satellite facility, subject to exceptions for states where there is only one other LTAC hospital and upon request following the closure or decrease in the number of licensed beds at a LTAC hospital within the state; |
30
Table of Contents
| (5) | a three-year moratorium on the application of a one-time budget neutrality adjustment to payment rates to LTAC hospitals under LTAC PPS; |
| (6) | a three-year moratorium on very short-stay outlier payment reductions to LTAC hospitals initially implemented on May 1, 2007; |
| (7) | a three-year moratorium on the application of the so-called “25 Percent Rule” (described below) to freestanding LTAC hospitals; |
| (8) | a three-year period during which LTAC hospitals that are co-located with another hospital may admit up to 50% of their patients from their co-located hospital and still be paid according to LTAC PPS; |
| (9) | a three-year period during which LTAC hospitals that are co-located with an urban single hospital or a hospital that generates more than 25% of the Medicare discharges in a metropolitan statistical area (“MSA Dominant hospital”) may admit up to 75% of their patients from such urban single hospital or MSA Dominant hospital and still be paid according to LTAC PPS; and |
| (10) | the elimination of the July 1, 2007 market basket increase in the standard federal payment rate of 0.71%, effective for discharges occurring on or after April 1, 2008. |
The three year moratorium beginning on December 29, 2007 on the establishment and classification of new LTAC hospitals, LTAC satellite facilities and LTAC beds in existing LTAC hospitals or satellite hospitals does not apply to LTAC hospitals that, before December 29, 2007, (1) began the qualifying period for payment under LTAC PPS, (2) had a written agreement with an unrelated party for the construction, renovation, lease or demolition for a LTAC hospital and had expended at least 10% of the estimated cost of the project or $2,500,000, or (3) had obtained an approved certificate of need. The moratorium also does not apply to an increase in beds in an existing hospital or satellite facility if the LTAC hospital is located in a state where there is only one other LTAC hospital and the LTAC hospital requests an increase in beds following the closure or the decrease in the number of beds of the other LTAC hospital.
The ACA revised certain provisions of the SCHIP Extension Act. The moratoriums on the establishment of new LTAC hospitals or satellites and bed increases at LTAC hospitals or satellites, the application of a one-time budget neutrality adjustment to rates, the payment reductions due to the very short-stay outlier provisions and application of the “25 Percent Rule” to freestanding hospitals were extended from three years to five years. In addition, the periods during which LTAC hospitals may admit up to 50% of their patients from co-located hospitals and during which LTAC hospitals may admit up to 75% of their patients from a MSA Dominant hospital were extended from three years to five years as well.
Recent Medicare Rate Adjustments.
On May 1, 2007, CMS issued regulatory changes regarding Medicare reimbursement for LTAC hospitals (the “2007 Final Rule”). In the 2007 Final Rule, the policy known as the “25 Percent Rule” was expanded to all LTAC hospitals, regardless of whether they are co-located with another hospital. Under the 2007 Final Rule, all LTAC hospitals were to be paid LTAC PPS rates for admissions from a single referral source up to 25% of aggregate Medicare admissions. Patients reaching high cost outlier status in the short-term hospital were not to be counted when computing the 25% limit. Admissions beyond the 25% threshold were to be paid at a lower amount based upon short-term acute care hospital rates. However, as set forth above, the SCHIP Extension Act initially placed a three-year moratorium on the expansion of the “25 Percent Rule” to freestanding hospitals. That moratorium was extended to five years by the ACA. In addition, the SCHIP Extension Act initially provided for a three-year period during which (1) LTAC hospitals may admit up to 50% of their patients from their co-located hospitals and still be paid according to LTAC PPS; and (2) LTAC hospitals that are co-located with an urban single hospital or a MSA Dominant hospital may admit up to 75% of their patients from such urban single or MSA Dominant hospital and still be paid according to LTAC PPS. Those periods also were extended to five years under the ACA. The five-year moratorium of the “25 Percent Rule” threshold payment adjustment for
31
Table of Contents
freestanding hospitals and grandfathered hospitals with a host hospital will expire for cost reporting periods beginning on or after July 1, 2012. The expansion of the admission limit to 50% for non-grandfathered LTAC hospitals from their co-located hospital will expire for cost reports beginning on or after October 1, 2012, the same time at which the 75% limit for MSA Dominant hospitals will expire.
On May 2, 2008, CMS issued regulatory changes regarding Medicare reimbursement for LTAC hospitals (the “2008 Final Rule”) that became effective for discharges occurring on or after July 1, 2008. The 2008 Final Rule projected an overall increase in payments to all Medicare certified LTAC hospitals of approximately 2.5%. Included in the 2008 Final Rule were (1) an increase to the standard federal payment rate of 2.7% (as compared to the adjusted federal rate for discharges occurring on or after April 1, 2008 by the SCHIP Extension Act); (2) adjustments to the wage index component of the federal payment resulting in projected reductions in payments of 0.1%; (3) an increase in the high cost outlier threshold per discharge to $22,960; and (4) an extension of the rate year cycle for one year to September 30, 2009, in order to be consistent thereafter with the federal fiscal year that begins October 1 of each year.
CMS has regulations governing payments to LTAC hospitals that are co-located with another hospital, such as a HIH. The rules generally limit Medicare payments to the HIH if the Medicare admissions to the HIH from its co-located hospital exceed 25% of the total Medicare discharges for the HIH’s cost reporting period, the “25 Percent Rule.” There are limited exceptions for admissions from rural, urban single and MSA Dominant hospitals. Admissions that exceed this “25 Percent Rule” are paid using IPPS. Patients transferred after they have reached the short-term acute care outlier payment status are not counted toward the admission threshold. Patients admitted prior to meeting the admission threshold, as well as Medicare patients admitted from a non co-located hospital, are eligible for the full payment under LTAC PPS. If the HIH’s admissions from the co-located hospital exceed the limit in a cost reporting period, Medicare will pay the lesser of (1) the amount payable under LTAC PPS; or (2) the amount payable under IPPS. At December 31, 2010, we operated 17 HIHs with 730 licensed beds.
On August 1, 2007, CMS issued final regulations regarding Medicare hospital inpatient payments to short-term acute care hospitals as well as certain provisions affecting LTAC hospitals. These regulations adopt a new system for LTAC hospitals for classifying patients into diagnostic categories called Medicare Severity Diagnosis Related Groups or more specifically, for LTAC hospitals, “MS-LTC-DRGs.” LTAC PPS is based upon discharged-based MS-LTC-DRGs similar to the system used to pay short-term acute care hospitals. This new MS-LTC-DRG system replaced the previous diagnostic related group system for LTAC hospitals and became effective for discharges occurring on or after October 1, 2007. The MS-LTC-DRG system created additional severity-adjusted categories for most diagnoses.
On July 31, 2008, CMS issued final regulations regarding the re-weighting of MS-LTC-DRGs for discharges occurring on or after October 1, 2008. CMS announced that this update was made in a budget neutral manner, and that estimated aggregate LTAC Medicare payments would be unaffected by these regulations. Based upon our experience under these final regulations, it appears that the re-weighting increased payments for the care of higher acuity patients.
On May 29, 2009, CMS issued an interim final rule that revised the October 1, 2008 payment weights. Effective June 3, 2009, CMS reduced MS-LTC-DRG payment weights by 3.9%, resulting in approximately a 0.9% reduction of the estimated total LTAC PPS payments in the federal fiscal year ending September 30, 2009. No retroactive adjustments to payments were made. On July 31, 2009, CMS finalized this interim rule.
On July 31, 2009, CMS issued final regulations regarding Medicare reimbursement for LTAC hospitals for the fiscal year beginning October 1, 2009. Included in those final regulations is (1) a market basket increase to the standard federal payment rate of 2.5%; (2) an offset of 0.5% applied to the standard federal payment rate to account for the effect of documentation and coding changes; (3) adjustments to area wage indexes; and (4) a decrease in the high cost outlier threshold per discharge to $18,425. These final regulations also include a recalibration of the MS-LTC-DRG payment weights. CMS indicated that all of these changes will result in a
32
Table of Contents
3.3% increase to average Medicare payments to LTAC hospitals. The 2.7% annualized reduction that resulted from a recalibration of MS-LTC-DRG payment weights on June 3, 2009 is incorporated into the final October 1, 2009 payment weights. On April 1, 2010, CMS reduced the October 1, 2009 standard federal payment rate by 0.25% as mandated by the ACA. In addition to specific market basket reductions, Congress has mandated that the annual market basket payment update for a variety of providers, including LTAC hospitals, be reduced for a “productivity adjustment” determined by CMS. These productivity adjustments may vary and will be determined annually by CMS. The productivity adjustments for LTAC hospitals are scheduled to be implemented on October 1, 2011.
On July 30, 2010, CMS issued final regulations regarding Medicare reimbursement for LTAC hospitals for the fiscal year beginning October 1, 2010. Included in those final regulations is (1) a market basket increase to the standard federal payment rate of 2.5%; (2) an offset of 2.5% applied to the standard federal payment rate to account for the effect of documentation and coding changes; (3) an offset of 0.5% applied to the standard federal payment rate as mandated by the ACA; (4) adjustments to area wage indexes; and (5) an increase in the high cost outlier threshold per discharge to $18,785. CMS indicated that all of these changes will result in a 0.5% increase to average Medicare payments to LTAC hospitals.
The LTAC PPS system is subject to significant change. Slight variations in patient acuity or length of stay could significantly change Medicare revenues generated under LTAC PPS. In addition, our hospitals may not be able to appropriately adjust their operating costs to changes in patient acuity and length of stay or to changes in reimbursement rates. In addition, we cannot assure you that LTAC PPS will not have a material adverse effect on revenues from commercial third party payors. Various factors, including a reduction in average length of stay, have negatively impacted revenues from commercial third party payors in recent years.
Medicaid Reimbursement of Long-term Acute Care Hospitals – The Medicaid program is designed to provide medical assistance to individuals unable to afford care. Medicaid payments are made under a number of different systems, which include cost-based reimbursement, prospective payment systems or programs that negotiate payment levels with individual hospitals. Medicaid programs are subject to statutory and regulatory changes, administrative rulings, interpretations of policy by state agencies and certain government funding limitations, all of which may increase or decrease the level of payments to our hospitals.
Non-government Payments – The hospital division seeks to maximize the number of non-government payment patients admitted to its hospitals, including those covered under commercial insurance and managed care health plans. Non-government payment patients typically have financial resources (including insurance coverages) to pay for their services and do not rely on government programs for support. It is important to our business to establish relationships with commercial insurers, managed care health plans and other private payors and to maintain our reputation with such payors as a provider of quality patient care. We negotiate contracts with purchasers of group healthcare services, including private employers, commercial insurers and managed care companies. Some payor organizations attempt to obtain discounts from established charges. We focus on demonstrating to these payors how our services can provide them and their customers with the most viable pricing arrangements in circumstances where they may otherwise be faced with funding treatment at higher rates at other healthcare providers. The importance of obtaining contracts with commercial insurers, managed care health plans and other private payors varies among markets, depending on such factors as the number of commercial payors and their relative market strength. Failure to obtain contracts with certain commercial insurers and managed care health plans or reductions in payments for our services provided to individuals covered by commercial insurance could have a material adverse effect on our business, financial position, results of operations and liquidity.
Nursing Center Division
General Regulations. The development and operation of nursing and rehabilitation centers and the provision of healthcare services are subject to federal, state and local laws relating to the adequacy of medical
33
Table of Contents
care, equipment, personnel, operating policies, fire prevention, rate-setting and compliance with building codes and environmental laws. Nursing and rehabilitation centers are subject to periodic inspection by governmental and other authorities to ensure continued compliance with various standards, continued licensing under state law, certification under the Medicare and Medicaid programs and continued participation in the Veterans Administration program. The failure to obtain, maintain or renew any required regulatory approvals or licenses could adversely affect nursing and rehabilitation center operations including their financial results.
As noted above, the nursing center division also is subject to federal and state laws that govern financial and other arrangements between healthcare providers. These laws prohibit, among other things, certain direct and indirect payments or fee-splitting arrangements between healthcare providers that are designed to induce or encourage the referral of patients to, or the recommendation of, a particular provider for medical products and services and prohibit referrals from physicians that have certain financial relationships with the provider. Such laws include the Anti-Kickback Statute, the Stark Law and the FCA. In addition, some states restrict certain business relationships between physicians and ancillary service providers and some states prohibit business corporations from providing, or holding themselves out as a provider of, medical care. Possible sanctions for violation of any of these restrictions or prohibitions include loss of licensure or eligibility to participate in reimbursement programs as well as civil and criminal penalties. These laws vary considerably from state to state.
In certain circumstances, federal law mandates that conviction for certain abusive or fraudulent behavior with respect to one nursing center may subject other facilities under common control or ownership to disqualification from participation in the Medicare and Medicaid programs. In addition, some regulations provide that all nursing and rehabilitation centers under common control or ownership within a state are subject to being delicensed if any one or more of such facilities are delicensed.
Licensure and Requirements for Participation. The nursing and rehabilitation centers operated and managed by the nursing center division are licensed either on an annual or bi-annual basis and generally are certified annually for participation in Medicare and Medicaid programs through various regulatory agencies that determine compliance with federal, state and local laws. These legal requirements relate to compliance with the laws and regulations governing the operation of nursing and rehabilitation centers including the quality of nursing care, the qualifications of the administrative and nursing personnel, and the adequacy of the physical plant and equipment. Federal regulations determine the survey process for nursing and rehabilitation centers that is followed by state survey agencies. The state survey agencies recommend to CMS the imposition of federal sanctions and impose state sanctions on facilities for noncompliance with certain requirements. Available sanctions include, but are not limited to, imposition of civil monetary penalties, temporary suspension of payment for new admissions, appointment of a temporary manager, suspension of payment for eligible patients and suspension or decertification from participation in the Medicare and Medicaid programs.
We believe that substantially all of our nursing and rehabilitation centers are in substantial compliance with applicable Medicare and Medicaid requirements of participation. In the ordinary course of business, however, our nursing and rehabilitation centers periodically receive statements of deficiencies from regulatory agencies. In response, the nursing and rehabilitation centers implement plans of correction to address the alleged deficiencies. In most instances, the regulatory agency accepts the nursing and rehabilitation center’s plan of correction and places the nursing and rehabilitation center back into compliance with regulatory requirements. In some cases, the regulatory agency may take a number of adverse actions against the nursing and rehabilitation center, including the imposition of fines, temporary suspension of payment for admission of new residents to the nursing and rehabilitation center, decertification from participation in the Medicaid and/or Medicare programs and, in extreme circumstances, revocation of the nursing and rehabilitation center’s license.
Overview of Nursing Center Division Reimbursement
Medicare – The Medicare Part A program provides reimbursement for extended care services furnished to Medicare beneficiaries who are admitted to nursing and rehabilitation centers after at least a three-day stay in an
34
Table of Contents
acute care hospital. Covered services include supervised nursing care, room and board, social services, physical, speech and occupational therapies, certain pharmaceuticals and supplies and other necessary services provided by nursing and rehabilitation centers. Medicare payments to our nursing and rehabilitation centers are based upon certain resource utilization grouping (“RUG”) payment rates developed by CMS that provide various levels of reimbursement based upon patient acuity.
The Balanced Budget Act established a Medicare prospective payment system (“PPS”) for nursing centers for cost reporting periods beginning on or after July 1, 1998. The payments received under PPS cover substantially all services for Medicare residents including all ancillary services, such as respiratory therapy, physical therapy, occupational therapy, speech therapy and certain covered pharmaceuticals.
Medicare Part B provides reimbursement for certain physician services, limited drug coverage and other outpatient services, such as therapy and other services, outside of a Medicare Part A covered patient stay. Payment for these services is determined according to the Medicare Physician Fee Schedule (“MPFS”). Annually since 1997, the MPFS has been subject to a sustainable growth rate adjustment (“SGR”) intended to keep spending growth in line with allowable spending. Each year since the SGR was enacted, this adjustment produced a scheduled negative update to payment for physicians, therapists and other healthcare providers paid under the MPFS. Annually, since 2002, Congress has stepped in with so-called “doc fix” legislation to stop payment cuts to physicians. In December 2010, Congress passed the Medicare and Medicaid Extenders Act of 2010 (“MMEA”) which again suspended the payment cut for 2011.
Since 2006, federal legislation has provided for an annual Medicare Part B outpatient therapy cap. In succeeding years, CMS subsequently increased the amount of the therapy cap. Legislation also was passed that required CMS to implement a broad process for reviewing medically necessary therapy claims, creating an exception to the cap. Legislation has annually extended the Medicare Part B outpatient therapy cap exception process. The Medicare Improvements for Patients and Providers Act of 2008, enacted on July 15, 2008, extended the therapy cap exception process from July 1, 2008 to December 31, 2009. The ACA provided that the exception process remain in effect from January 1, 2010 through December 31, 2010. MMEA extended the therapy cap exception process through December 31, 2011. Patients in our facilities whose stay is not reimbursed by Medicare must seek reimbursement for their therapy under Medicare Part B and are subject to the therapy cap.
On January 1, 2006, the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (“Medicare Part D”) implemented a major expansion of the Medicare program through the introduction of a prescription drug benefit. Under Medicare Part D, dual eligible patients have their outpatient prescription drug costs covered by this new Medicare benefit, subject to certain limitations. Most of our nursing and rehabilitation center patients whose drug costs were previously covered by state Medicaid programs are dual eligible patients who qualify for the Medicare drug benefit. Accordingly, Medicaid is no longer a primary payor for the pharmacy services provided to these residents.
Recent Medicare Rate Adjustments
On July 31, 2009, CMS issued final regulations regarding Medicare reimbursement for nursing centers for the fiscal year beginning October 1, 2009. Included in these regulations are (1) a market basket increase to the federal payment rates of 2.2%; (2) updates to the wage indexes which adjust the federal payment; and (3) a reduction in the RUG indexes attributed to a CMS forecast error in a prior year, resulting in a 3.3% reduction in payments. CMS estimated that these changes will result in a net decrease in Medicare payments to nursing and rehabilitation centers of 1.1%. In addition to specific market basket reductions, Congress has mandated that the annual market basket payment update for a variety of providers, including nursing centers, be reduced for a “productivity adjustment” determined by CMS. These productivity adjustments may vary and will be determined annually by CMS. The productivity adjustments for nursing centers are scheduled to be implemented on October 1, 2011.
35
Table of Contents
On July 16, 2010, CMS issued a notice that updates the payment rates for nursing centers for the fiscal year beginning October 1, 2010. That notice provided for an increase in rates of 1.7%, which is comprised of a market basket increase of 2.3% less a forecast error adjustment of 0.6%.
On November 2, 2010, CMS issued a final rule related to rate changes to Medicare Part B therapy services included in the MPFS rule. The rule became effective January 1, 2011. The rule provides for a rate reduction for reimbursement of therapy expenses for secondary procedures when multiple therapy services are provided on the same day. CMS projects that the rule will result in an approximate 7% rate reduction for Medicare Part B therapy services in calendar year 2011. Based upon our historical Medicare Part B therapy services data, we estimate that this rule will reduce our Medicare revenues related to Part B therapy services by approximately $7 million per year beginning in 2011.
In addition, for the fiscal year beginning October 1, 2010, CMS finalized provisions that increase the number of RUG categories for nursing centers from 53 to 66 (i.e., RUGs IV) and amend the criteria, including the provision of therapy services, used to classify patients into these categories. CMS has indicated that these changes will be enacted in a budget neutral manner.
The therapy time requirements to qualify for rehabilitation RUG categories are unchanged under RUGs IV, however the allocation of minutes has changed as a result of the most recent clinical assessment tool of the minimum data set (“MDS 3.0”). Rather than count all therapy time that a nursing center patient receives, rehabilitation providers must now allocate therapy minutes between the patients being served during concurrent therapy sessions. In addition, the number of patients that a therapist/assistant may treat concurrently is limited to two patients. Additional tracking provisions also require therapists to track and report different delivery modes of therapy (individual, concurrent and group therapy) on MDS 3.0. Our rehabilitation division has hired additional therapists to facilitate the provision of additional individual minutes. Effective October 1, 2010, CMS began paying claims using the RUGs IV system.
Medicaid – Medicaid is a state-administered program financed by state funds and matching federal funds. The program provides for medical assistance to the indigent and certain other eligible persons. Although administered under broad federal regulations, states are given flexibility to construct programs and payment methods consistent with their individual goals. Accordingly, these programs differ in many respects from state to state.
The nursing center division provides to eligible individuals Medicaid-covered services consisting of nursing care, room and board and social services. In addition, states may at their option cover other services such as physical, occupational and speech therapies and pharmaceuticals. Medicaid programs also are subject to statutory and regulatory changes, administrative rulings, interpretations of policy by the state agencies and certain government funding limitations, all of which may materially increase or decrease the level of program payments to nursing and rehabilitation centers operated by the nursing center division. We believe that the payments under many of these programs may not be sufficient on an overall basis to cover the costs of serving certain patients participating in these programs. In addition, the downturn in the United States economy over the past few years has accentuated budgetary pressures impacting state fiscal budgets, thereby further reducing Medicaid payments to our nursing and rehabilitation centers from current levels.
Under the American Recovery & Reinvestment Act of 2009, state Medicaid programs were granted a temporary increase in federal medical assistance percentage (“FMAP”) funding. As a result of the economic downturn experienced by most states, the practical effect of the increase in FMAP funding meant the payments for services in nursing and rehabilitation centers in most states were either frozen or increased nominally relative to annual adjustments normally associated with the Medicaid budget process. After various legislative extensions, the enhanced FMAP rate is set to expire June 30, 2011.
36
Table of Contents
There continue to be legislative and regulatory proposals that would impose further limitations on government and private payments to providers of healthcare services. The Balanced Budget Act eased existing impediments on the ability of states to reduce their Medicaid reimbursement levels. Many states are considering or have enacted measures that are designed to reduce their Medicaid expenditures and to make certain changes to private healthcare insurance. As states face budgetary issues, we anticipate further pressure on Medicaid rates that could negatively impact payments to our nursing and rehabilitation centers.
In addition, some states seek to increase the levels of funding contributed by the federal government to their Medicaid programs through a mechanism known as a provider tax. Under these programs, states levy a tax on healthcare providers, which increases the amount of state revenue available to expend on the Medicaid program. This increase in program revenues increases the payment made by the federal government to the state in the form of matching funds. Consequently, the state then has more funds available to support Medicaid rates for providers of Medicaid covered services. However, states may not necessarily use these funds to increase payments to nursing center providers. Provider tax plans are subject to approval by the federal government and were included as a provision in the Tax Relief and Health Care Act of 2006, codifying the maximum Medicaid provider tax rate at 5.5% through fiscal year 2011. Although these plans have been approved in the past, we cannot assure you that such plans will be approved by the federal government in the future.
Non-government Payments – The nursing center division seeks to maximize the number of non-government payment residents admitted to our nursing and rehabilitation centers, including those covered under private insurance and managed care health plans. Non-government payment residents typically have financial resources (including insurance coverages) to pay for their services and do not rely on government programs for support. It is important to our business to establish relationships with commercial insurers, managed care health plans and other private payors and to maintain our reputation with such payors as a provider of quality patient and resident care. We negotiate contracts with purchasers of group healthcare services, including private employers, commercial insurers and managed care companies. Some payor organizations attempt to obtain discounts from established charges. We focus on demonstrating to these payors how our services can provide them and their customers with the most viable pricing arrangements in circumstances where they may otherwise be faced with funding treatment at higher rates at other healthcare providers. The importance of obtaining contracts with commercial insurers, managed care health plans and other private payors varies among markets, depending on such factors as the number of commercial payors and their relative market strength. Failure to obtain contracts with certain commercial insurers and managed care health plans or reductions in payments for our services provided to individuals covered by commercial insurance could have a material adverse effect on our business, financial position, results of operations and liquidity.
Rehabilitation Division
General Regulations. The rehabilitation division is subject to various federal and state regulations. Therapists and other healthcare professionals that we employ are required to be individually licensed or certified pursuant to applicable state and federal laws. We have processes in place in an effort to ensure that our therapists and other healthcare professionals are licensed or certified in accordance with applicable federal and state laws. In addition, we require our therapists and other employees to participate in continuing education programs. The failure of a therapist or other healthcare professional to obtain, maintain or renew required licenses or certifications could adversely affect a client’s and our operations, including negatively impacting our financial results.
As noted above, the rehabilitation division is subject to federal and state laws that govern financial and other arrangements between healthcare providers. These laws prohibit, among other things, certain direct and indirect payments or fee-splitting arrangements between healthcare providers that are designed to induce or encourage the referral of patients to, or the recommendation of, a particular provider for medical products and services. Such laws include the anti-fraud and anti-kickback laws discussed previously. In addition, some states restrict certain business relationships between physicians and ancillary service providers. Some states also prohibit for-profit
37
Table of Contents
corporations from providing rehabilitation services through therapists who are directly employed by the corporation or otherwise providing, or holding themselves out as a provider of, medical care. Possible sanctions for violation of any of these restrictions or prohibitions include loss of eligibility to contract with long-term care facilities, hospitals and other providers participating in Medicare, Medicaid and other federal healthcare programs as well as civil and criminal penalties. These laws vary considerably from state to state.
Overview of Rehabilitation Division Revenues
The rehabilitation division receives payment for the services it provides to patients and residents of the nursing centers, acute and long-term acute care hospitals, outpatient clinics, home health agencies, assisted living facilities, school districts and hospice providers that it serves. The payments are based upon negotiated patient per diem rates, negotiated per minute rates or a fee schedule based upon the type of service rendered.
As noted above, various federal and state laws and regulations govern reimbursement to long-term care facilities, hospitals and other healthcare providers participating in Medicare, Medicaid and other federal healthcare programs. Though these laws and regulations are generally not directly applicable to our rehabilitation division, they are applicable to our customers. If our customers fail to comply with these laws and regulations they could be subject to possible sanctions, including loss of licensure or eligibility to participate in reimbursement programs as well as civil and criminal penalties, which could materially and adversely affect our business, financial position, results of operations and liquidity. If our arrangements with our customers are found to violate the Anti-Kickback Statute or other fraud and abuse laws, we could be subject to criminal and civil penalties as well as exclusion from participation in federal and state healthcare programs. In addition, there continue to be legislative and regulatory proposals to contain healthcare costs by imposing further limitations on government and private payments to providers of healthcare services.
Medicare Part B provides reimbursement for certain physician services, limited drug coverage and other outpatient services, such as therapy and other services, outside of a Medicare Part A covered patient stay. Payment for these services is determined according to the MPFS. Annually since 1997, the MPFS has been subject to the SGR, intended to keep spending growth in line with allowable spending. Each year since the SGR was enacted, this adjustment produced a scheduled negative update to payment for physicians, therapists and other healthcare providers paid under the MPFS. Annually, since 2002, Congress has stepped in with so-called “doc fix” legislation to stop payment cuts to physicians. In December 2010, Congress passed MMEA which again suspended the payment cut for 2011.
Since 2006, federal legislation has provided for an annual Medicare Part B outpatient therapy cap. In succeeding years, CMS subsequently increased the amount of the therapy cap. Legislation also was passed that required CMS to implement a broad process for reviewing medically necessary therapy claims, creating an exception to the cap. Legislation has annually extended the Medicare Part B outpatient therapy cap exception process. The Medicare Improvements for Patients and Providers Act of 2008, enacted on July 15, 2008, extended the therapy cap exception process from July 1, 2008 to December 31, 2009. The ACA provided that the exception process remain in effect from January 1, 2010 through December 31, 2010. MMEA extended the therapy cap exception process through December 31, 2011.
On July 16, 2010, CMS issued a notice that updates the payment rates for nursing centers for the fiscal year beginning October 1, 2010. That notice provided for an increase in rates of 1.7%, which is comprised of a market basket increase of 2.3% less a forecast error adjustment of 0.6%.
On November 2, 2010, CMS issued a final rule related to rate changes to Medicare Part B therapy services included in the MPFS rule. The rule became effective January 1, 2011. The rule provides for a rate reduction for reimbursement of therapy expenses for secondary procedures when multiple therapy services are provided on the same day. CMS projects that the rule will result in an approximate 7% rate reduction for Medicare Part B therapy
38
Table of Contents
services in calendar year 2011. Based upon our historical Medicare Part B therapy services data, we estimate that this rule will reduce our Medicare revenues related to Part B therapy services by approximately $7 million per year beginning in 2011.
In addition, for the fiscal year beginning October 1, 2010, CMS finalized provisions that increase the number of RUG categories for nursing centers from 53 to 66 (i.e., RUGs IV) and amend the criteria, including the provision of therapy services, used to classify patients into these categories. CMS has indicated that these changes will be enacted in a budget neutral manner. While we are unable to estimate the impact of these changes, the operating results of our contract rehabilitation services business may be adversely affected.
The therapy time requirements to qualify for rehabilitation RUG categories are unchanged under RUGs IV, however the allocation of minutes has changed as a result of MDS 3.0. Rather than count all therapy time that a nursing center patient receives, rehabilitation providers must now allocate therapy minutes between the patients being served during concurrent therapy sessions. In addition, the number of patients that a therapist/assistant may treat concurrently is limited to two patients. Additional tracking provisions also require therapists to track and report different delivery modes of therapy (individual, concurrent and group therapy) on MDS 3.0. Our rehabilitation division has hired additional therapists to facilitate the provision of additional individual minutes. Effective October 1, 2010, CMS began paying claims using the RUGs IV system.
Reductions in the reimbursement provided to our customers by Medicare or Medicaid could negatively impact the demand and price for our services and could have a material adverse effect on our rehabilitation revenues and growth prospects.
MASTER LEASE AGREEMENTS
At December 31, 2010, we leased from Ventas and its affiliates 38 LTAC hospitals and 159 nursing and rehabilitation centers under four master lease agreements (as amended, the “Master Lease Agreements”). Under the Master Lease Agreements, Ventas has a right to sever properties from the existing leases in order to create additional leases, a device adopted to facilitate its financing flexibility. In such circumstances, our aggregate lease obligations remain unchanged.
On April 30, 2009, we entered into agreements with Ventas to renew the leases for 86 nursing and rehabilitation centers and 22 LTAC hospitals (collectively, the “2010 Renewal Facilities”) for an additional five years. The initial lease term for the 2010 Renewal Facilities was set to expire in April 2010.
The following summary description of the Master Lease Agreements is qualified in its entirety by reference to the Master Lease Agreements filed with the SEC.
Term and Renewals
Each Master Lease Agreement includes land, buildings, structures and other improvements on the land, easements and similar appurtenances to the land and improvements, and permanently affixed equipment, machinery and other fixtures relating to the operation of the leased properties. There are several bundles of leased properties under each Master Lease Agreement, with each bundle containing approximately six to 20 leased properties.
Under the Master Lease Agreements, the base term for 28 nursing and rehabilitation center and eight LTAC hospital leases (which are contained in four renewal bundles) is scheduled to expire in April 2013 (the “2013 Lease Renewals”). At our option, the 2013 Lease Renewals may be extended for one five-year renewal term
39
Table of Contents
beyond the base term at the then existing rental rate plus the then existing escalation amount per annum. If we elect to renew, all, but not less than all, of the facilities in a renewal bundle must be renewed.
The base terms for 45 nursing and rehabilitation centers and eight LTAC hospitals as well as the 2010 Renewal Facilities were initially set to expire in April 2008 and 2010, respectively, but were each renewed for additional five-year terms. We may further extend the term of these leases for two additional five-year renewal terms beyond the first renewal term at the greater of (1) the then existing rental rate plus the then existing escalation amount per annum or (2) the then fair market value rental rate. The fair market value rental rate is determined through an appraisal procedure set forth in the Master Lease Agreements. The then fair market value rental rate may be materially higher than the existing rental rate. In such a situation we may be forced to either not exercise the renewal or pay the higher rental rate, either of which could have a material adverse effect on our business, financial position, results of operations and liquidity. If we elect to renew, all, but not less than all, of the facilities in a renewal bundle must be renewed.
The following chart sets forth the remaining lease renewals under the Master Lease Agreements:
| Facility renewals | ||||||||||||||
| Expiration date |
Renewal date |
Nursing and |
Hospitals |
Renewal bundles |
||||||||||
| April 30, 2013 |
November 1, 2011 – April 29, 2012 |
28 | 8 | 4 | ||||||||||
| April 30, 2013 |
November 1, 2011 – April 29, 2012 |
45 | 8 | 6 | ||||||||||
| April 30, 2015 |
November 1, 2013 – April 29, 2014 |
86 | 22 | 10 | ||||||||||
We may not extend the Master Lease Agreements beyond the base term or any previously exercised renewal term if, at the time we seek such extension and at the time such extension takes effect, (1) an event of default has occurred and is continuing or (2) a Medicare/Medicaid event of default (as described below) and/or a licensed bed event of default (as described below) has occurred and is continuing with respect to three or more leased properties subject to a particular Master Lease Agreement. The base term and renewal term of each Master Lease Agreement are subject to termination upon default by us (subject to certain exceptions) and certain other conditions described in the Master Lease Agreements.
Rental Amounts and Escalators
Each Master Lease Agreement is commonly known as a triple-net lease or an absolute-net lease. Accordingly, in addition to rent, we are required to pay the following: (1) all insurance required in connection with the leased properties and the business conducted on the leased properties, (2) certain taxes levied on or with respect to the leased properties (other than taxes on the income of Ventas) and (3) all utilities and other services necessary or appropriate for the leased properties and the business conducted on the leased properties.
We paid rents to Ventas (including amounts classified as discontinued operations) approximating $246 million for the year ended December 31, 2010, $243 million for the year ended December 31, 2009 and $239 million for the year ended December 31, 2008.
Each Master Lease Agreement provides for rent escalations each May 1 if the patient revenues for the leased properties meet certain criteria as measured using the preceding calendar year revenues as compared to the base period. All annual rent escalators are payable in cash. In connection with the exercise of the rent reset by Ventas in 2006, the rent escalations were modified. The contingent annual rent escalator is 2.7% for Master Lease
40
Table of Contents
Agreements Nos. 1, 3 and 4. The contingent annual rent escalator for Master Lease Agreement No. 2 is based upon the Consumer Price Index with a floor of 2.25% and a ceiling of 4%. In 2010, the contingent annual rent escalator for Master Lease Agreement No. 2 was 2.25%.
Use of the Leased Property
The Master Lease Agreements require that we utilize the leased properties solely for the provision of healthcare services and related uses and as Ventas may otherwise consent. We are responsible for maintaining or causing to be maintained all licenses, certificates and permits necessary for the leased properties to comply with various healthcare and other regulations. We also are obligated to operate continuously each leased property as a provider of healthcare services.
Events of Default
Under each Master Lease Agreement, an “Event of Default” will be deemed to occur if, among other things:
| • | we fail to pay rent or other amounts within five days after notice, |
| • | we fail to comply with covenants, which failure continues for 30 days or, so long as diligent efforts to cure such failure are being made, such longer period (not over 180 days) as is necessary to cure such failure, |
| • | certain bankruptcy or insolvency events occur, including filing a petition of bankruptcy or a petition for reorganization under the bankruptcy code, |
| • | an event of default arises from our failure to pay principal or interest on any indebtedness exceeding $50 million, |
| • | the maturity of any indebtedness exceeding $50 million is accelerated, |
| • | we cease to operate any leased property as a provider of healthcare services for a period of 30 days, |
| • | a default occurs under any guaranty of any lease or the indemnity agreements with Ventas, |
| • | we or our subtenant lose any required healthcare license, permit or approval or fail to comply with any legal requirements as determined by a final unappealable determination, |
| • | we fail to maintain insurance, |
| • | we create or allow to remain certain liens, |
| • | we breach any material representation or warranty, |
| • | a reduction occurs in the number of licensed beds in a facility, generally in excess of 10% (or less than 10% if we have voluntarily “banked” licensed beds) of the number of licensed beds in the applicable facility on the commencement date (a “licensed bed event of default”), |
| • | Medicare or Medicaid certification with respect to a participating facility is revoked and re-certification does not occur for 120 days (plus an additional 60 days in certain circumstances) (a “Medicare/Medicaid event of default”), |
| • | we become subject to regulatory sanctions as determined by a final unappealable determination and fail to cure such regulatory sanctions within the specified cure period for any facility, |
| • | we fail to cure a breach of any permitted encumbrance within the applicable cure period and, as a result, a real property interest or other beneficial property right of Ventas is at material risk of being terminated, or |
41
Table of Contents
| • | we fail to cure the breach of any of the obligations of Ventas as lessee under any existing ground lease within the applicable cure period and, if such breach is a non-monetary, non-material breach, such existing ground lease is at material risk of being terminated. |
Remedies for an Event of Default
Except as noted below, upon an Event of Default under one of the Master Lease Agreements, Ventas may, at its option, exercise the following remedies:
(1) after not less than ten days notice to us, terminate the Master Lease Agreement to which such Event of Default relates, repossess any leased property, relet any leased property to a third party and require that we pay to Ventas, as liquidated damages, the net present value of the rent for the balance of the term, discounted at the prime rate,
(2) without terminating the Master Lease Agreement to which such Event of Default relates, repossess the leased property and relet the leased property with us remaining liable under such Master Lease Agreement for all obligations to be performed by us thereunder, including the difference, if any, between the rent under such Master Lease Agreement and the rent payable as a result of the reletting of the leased property, and
(3) seek any and all other rights and remedies available under law or in equity.
In addition to the remedies noted above, under the Master Lease Agreements, in the case of a facility-specific event of default, Ventas may terminate a Master Lease Agreement as to the leased property to which the Event of Default relates, and may, but need not, terminate the entire Master Lease Agreement. Each of the Master Lease Agreements includes special rules relative to Medicare/Medicaid events of default and a licensed bed event of default. In the event a Medicare/Medicaid event of default and/or a licensed bed event of default occurs and is continuing (a) with respect to not more than two properties at the same time under a Master Lease Agreement that covers 41 or more properties and (b) with respect to not more than one property at the same time under a Master Lease Agreement that covers 21 to and including 40 properties, Ventas may not exercise termination or dispossession remedies against any property other than the property or properties to which the event of default relates. Thus, in the event Medicare/Medicaid events of default and licensed bed events of default would occur and be continuing (a) with respect to one property under a Master Lease Agreement that covers less than 20 properties, (b) with respect to two or more properties at the same time under a Master Lease Agreement that covers 21 to and including 40 properties, or (c) with respect to three or more properties at the same time under a Master Lease Agreement that covers 41 or more properties, then Ventas would be entitled to exercise all rights and remedies available to it under the Master Lease Agreements.
Assignment and Subletting
Except as noted below, the Master Lease Agreements provide that we may not assign, sublease or otherwise transfer any leased property or any portion of a leased property as a whole (or in substantial part), including by virtue of a change of control, without the consent of Ventas, which may not be unreasonably withheld if the proposed assignee (1) is a creditworthy entity with sufficient financial stability to satisfy its obligations under the related Master Lease Agreement, (2) has not less than four years experience in operating healthcare facilities for the purpose of the applicable facility’s primary intended use, (3) has a favorable business and operational reputation and character, and (4) has all licenses, permits, approvals and authorizations to operate the facility and agrees to comply with the use restrictions in the related Master Lease Agreement. The obligation of Ventas to consent to a subletting or assignment is subject to the reasonable approval rights of any mortgagee and/or the lenders under its credit agreement. We may sublease up to 20% of each leased property for restaurants, gift shops and other stores or services customarily found in hospitals or nursing and rehabilitation centers without the consent of Ventas, subject, however, to there being no material alteration in the character of the leased property or in the nature of the business conducted on such leased property.
42
Table of Contents
In addition, each Master Lease Agreement allows us to assign or sublease (a) without the consent of Ventas, 10% of the nursing and rehabilitation center facilities in each Master Lease Agreement and (b) with Ventas’ consent (which consent will not be unreasonably withheld, delayed or conditioned), two hospitals in each Master Lease Agreement, if either (i) the applicable regulatory authorities have threatened to revoke our Medicaid or Medicare certification or an authorization necessary to operate such leased property or (ii) we cannot profitably operate such leased property. Any such proposed assignee/sublessee must satisfy the requirements listed above and it must have all licenses, permits, approvals and other authorizations required to operate the leased properties in accordance with the applicable permitted use. With respect to any assignment or sublease made under this provision, Ventas agrees to execute a nondisturbance and attornment agreement with such proposed assignee or subtenant. Upon any assignment or subletting, we will not be released from our obligations under the applicable Master Lease Agreement.
Subject to certain exclusions, we must pay to Ventas 80% of any consideration received by us on account of an assignment and 80% (50% in the case of existing subleases) of sublease rent payments (approximately equal to revenue net of specified allowed expenses attributable to a sublease, and specifically defined in the Master Lease Agreements), provided that Ventas’s right to such payments will be subordinate to that of our lenders.
Ventas will have the right to approve the purchaser at a foreclosure of one or more of our leasehold mortgages by our lenders. Such approval will not be unreasonably withheld so long as such purchaser is creditworthy, reputable and has four years experience in operating healthcare facilities. Any dispute regarding whether Ventas has unreasonably withheld its consent to such purchaser will be subject to expedited arbitration.
ADDITIONAL INFORMATION
Employees
As of December 31, 2010, we had approximately 40,600 full-time and 16,200 part-time and per diem employees. We had approximately 3,100 unionized employees at 35 of our facilities as of December 31, 2010.
The market for qualified nurses, therapists and other healthcare professionals is highly competitive. We, like other healthcare providers, have experienced difficulties in attracting and retaining qualified personnel such as nurses, certified nurse’s assistants, nurse’s aides, therapists and other providers of healthcare services. Our hospitals and nursing and rehabilitation centers are particularly dependent on nurses for patient care. Our rehabilitation division continues to seek qualified therapists to fill open positions. The difficulty we have experienced in hiring and retaining qualified personnel has increased our average wage rates and may force us to increase our use of contract personnel. We expect to continue to experience increases in our labor costs primarily due to higher wages and greater benefits required to attract and retain qualified healthcare personnel. Salaries, wages and benefits were approximately 57% of our consolidated revenues for the year ended December 31, 2010. Our ability to manage labor costs will significantly affect our future operating results.
Professional and General Liability Insurance
Our healthcare operations are primarily insured for professional and general liability risks by our wholly owned limited purpose insurance subsidiary, Cornerstone Insurance Company (“Cornerstone”). Cornerstone insures initial losses up to specified coverage levels per occurrence. On a per claim basis, coverages for losses in excess of those insured by Cornerstone are maintained through unaffiliated commercial insurance carriers. Cornerstone insures all claims in all states up to a per occurrence limit without the benefit of any aggregate coverage limit through unaffiliated commercial insurance carriers, thereby increasing our financial risk.
We believe that our insurance is adequate in amount and coverage. There can be no assurance that in the future such insurance will be available at a reasonable price or that we will be able to maintain adequate levels of professional and general liability insurance coverage.
43
Table of Contents
Where You Can Find More Information
We file annual, quarterly and current reports, proxy statements and other information with the SEC under the Exchange Act.
Our filings with the SEC are available to the public free of charge on the SEC website at http://www.sec.gov, which contains reports, proxy and information statements and other information. You also may read or obtain copies of this information in person or by mail from the SEC’s Public Reference Room, 100 F Street, NE, Room 1580, Washington, D.C. 20549. Please call the SEC at 1-800-SEC-0330 for further information on the operation of the Public Reference Room.
Our filings with the SEC, including our Annual Report on Form 10-K, Quarterly Reports on Form 10-Q, Current Reports on Form 8-K and any amendments thereto, are available free of charge on our website, through a link to the SEC’s website, as soon as reasonably practicable after they are electronically filed with or furnished to the SEC. Our website is www.kindredhealthcare.com. Information made available on our website is not a part of this document.
| Item 1A. | Risk Factors |
Certain statements made in this Annual Report on Form 10-K and the documents we incorporate by reference in this Annual Report on Form 10-K include forward-looking statements within the meaning of Section 27A of the Securities Act and Section 21E of the Exchange Act. All statements regarding our expected future financial position, results of operations, cash flows, financing plans, business strategy, budgets, capital expenditures, competitive positions, growth opportunities, plans and objectives of management and statements containing the words such as “anticipate,” “approximate,” “believe,” “plan,” “estimate,” “expect,” “project,” “could,” “should,” “will,” “intend,” “may” and other similar expressions, are forward-looking statements.
Such forward-looking statements are inherently uncertain, and stockholders and other potential investors must recognize that actual results may differ materially from our expectations as a result of a variety of factors, including, without limitation, those discussed below. Such forward-looking statements are based upon management’s current expectations and include known and unknown risks, uncertainties and other factors, many of which we are unable to predict or control, that may cause our actual results or performance to differ materially from any future results or performance expressed or implied by such forward-looking statements. These statements involve risks, uncertainties and other factors discussed below and detailed from time to time in our filings with the SEC. Factors that may affect our plans or results include, without limitation:
| • | our ability to integrate the operations of the acquired hospitals and rehabilitation services operations and realize the anticipated revenues, economies of scale, cost synergies and productivity gains in connection with the RehabCare acquisition and any other acquisitions that may be undertaken during 2011, as and when planned, including the potential for unanticipated issues, expenses and liabilities associated with those acquisitions and the risk that RehabCare fails to meet its expected financial and operating targets, |
| • | the receipt of all required licensure and regulatory approvals and the satisfaction of the closing conditions to the RehabCare acquisition, including approval of the pending transaction by the stockholders of the respective companies, and our ability to complete the required financing as contemplated by the financing commitment, |
| • | the potential for diversion of management time and resources in seeking to complete the RehabCare acquisition and integrate its operations, |
| • | the potential failure to retain key employees of RehabCare, |
| • | the impact of our significantly increased levels of indebtedness as a result of the RehabCare acquisition on our funding costs, operating flexibility and ability to fund ongoing operations with additional borrowings, particularly in light of ongoing volatility in the credit and capital markets, |
44
Table of Contents
| • | the potential for dilution to our stockholders as a result of the RehabCare acquisition, |
| • | the impact of pending or future litigation relating to the RehabCare acquisition, |
| • | the impact of healthcare reform, which will initiate significant reforms to the United States healthcare system, including potential material changes to the delivery of healthcare services and the reimbursement paid for such services by the government or other third party payors. Healthcare reform will impact each of our businesses in some manner. Due to the substantial regulatory changes that will need to be implemented by CMS and others, and the numerous processes required to implement these reforms, we cannot predict which healthcare initiatives will be implemented at the federal or state level, the timing of any such reforms, or the effect such reforms or any other future legislation or regulation will have on our business, financial position, results of operations and liquidity, |
| • | changes in the reimbursement rates or the methods or timing of payment from third party payors, including commercial payors and the Medicare and Medicaid programs, changes arising from and related to LTAC PPS, including potential changes in the Medicare payment rules, the Medicare Prescription Drug, Improvement, and Modernization Act of 2003, and changes in Medicare and Medicaid reimbursements for nursing centers, and the expiration of the Medicare Part B therapy cap exception process, |
| • | the effects of additional legislative changes and government regulations, interpretation of regulations and changes in the nature and enforcement of regulations governing the healthcare industry, |
| • | our ability to successfully pursue our development activities, including through acquisitions, and successfully integrate new operations, including the realization of anticipated revenues, economies of scale, cost savings and productivity gains associated with such operations, |
| • | the impact of the SCHIP Extension Act, including the ability of our hospitals to adjust to potential LTAC certification, medical necessity reviews and the moratorium on future hospital development, |
| • | the impact of the expiration of several moratoriums under the SCHIP Extension Act which could impact the short stay rules, the budget neutrality adjustment as well as implement the policy known as the “25 Percent Rule,” which would limit certain patient admissions, |
| • | failure of our facilities to meet applicable licensure and certification requirements, |
| • | the further consolidation and cost containment efforts of managed care organizations and other third party payors, |
| • | our ability to meet our rental and debt service obligations, |
| • | our ability to operate pursuant to the terms of our debt obligations, including our obligations under financings undertaken to complete the RehabCare acquisition, and our ability to operate pursuant to our Master Lease Agreements, |
| • | the condition of the financial markets, including volatility and weakness in the equity, capital and credit markets, which could limit the availability and terms of debt and equity financing sources to fund the requirements of our businesses, or which could negatively impact our investment portfolio, |
| • | national and regional economic, financial, business and political conditions, including their effect on the availability and cost of labor, credit, materials and other services, |
| • | our ability to control costs, particularly labor and employee benefit costs, |
| • | increased operating costs due to shortages in qualified nurses, therapists and other healthcare personnel, |
| • | our ability to attract and retain key executives and other healthcare personnel, |
45
Table of Contents
| • | the increase in the costs of defending and insuring against alleged professional liability and other claims and the ability to predict the estimated costs related to such claims, including the impact of differences in actuarial assumptions and estimates compared to eventual outcomes, |
| • | our ability to successfully reduce (by divestiture of operations or otherwise) our exposure to professional liability and other claims, |
| • | our ability to successfully dispose of unprofitable facilities, |
| • | events or circumstances which could result in the impairment of an asset or other charges, |
| • | changes in generally accepted accounting principles or practices, and changes in tax accounting or tax laws (or authoritative interpretations relating to any of these matters), and |
| • | our ability to maintain an effective system of internal control over financial reporting. |
Many of these factors are beyond our control. We caution you that any forward-looking statements made by us are not guarantees of future performance. We disclaim any obligation to update any such factors or to announce publicly the results of any revisions to any of the forward-looking statements to reflect future events or developments.
You should consider carefully all the risks described below, together with all of the information included in this Annual Report on Form 10-K, in evaluating our Company and our common stock. To facilitate your consideration of all of the risks described below, these risks are organized under headings and subheadings for your convenience. If any of the risks described in this Annual Report on Form 10-K were to occur, it could have a material adverse effect on our business, financial position, results of operations, liquidity and stock price.
Risk Factors Relating to the RehabCare Acquisition
There are risks associated with our pending acquisition of RehabCare.
On February 7, 2011, we executed the Merger Agreement in which we agreed to acquire RehabCare for cash and shares of our common stock. While we agreed to acquire RehabCare because we believe the acquisition will be beneficial to us and our stockholders, there are risks associated with the acquisition, which include:
| • | whether we will be able to complete our planned financing of the RehabCare acquisition on the terms and the timetable that we expect; |
| • | whether our stockholders and those of RehabCare will approve the Merger; |
| • | any issuance of our shares in the RehabCare acquisition will result in dilution of the ownership percentage of our existing stockholders, and any economic benefits that we realize as a result of the acquisition may not be sufficient to offset the ownership dilution; |
| • | potential delays or unanticipated costs associated with our efforts to obtain licensure and regulatory approvals with respect to the RehabCare acquisition, as well as the approval by RehabCare’s stockholders, including the possibility that licensure or regulatory approvals may be granted subject to conditions, such as divestitures of existing assets or businesses or restrictions on the conduct of the combined company, that could affect our operations, financial results and prospects; |
| • | the impact and outcome of litigation challenging the terms of the RehabCare acquisition, including pending class action litigation against us, which could entail claims for damages and significant cost and delay the consummation of the RehabCare acquisition; |
| • | the risks associated with our efforts to integrate the operations of RehabCare with our own and achieve the cost and other synergies we expect, as described below; |
| • | the impact of our increased level of indebtedness after the RehabCare acquisition on our financial and operating flexibility, our future access to the credit markets and our funding costs; and |
46
Table of Contents
| • | the possibility that the market price of our common stock may decline as a result of investor perceptions about the terms or benefits of the RehabCare acquisition. |
In addition, we may be required to pay RehabCare a termination fee of $62 million upon the termination of the Merger Agreement under specified circumstances, including a change in the recommendation of our board of directors or our failure to complete the financing, after all other closing conditions have been met.
Any of these and the other risks discussed below could jeopardize our ability to complete the RehabCare acquisition or realize its anticipated benefits as and when planned, which could in turn have a material adverse effect on our stock price, financial condition, results of operations and business prospects.
We may not be able to successfully integrate RehabCare’s operations with our own or realize the anticipated benefits of the RehabCare acquisition, which could materially and adversely affect our financial condition, results of operations and business prospects.
Even if we complete the RehabCare acquisition, we may not be able to successfully integrate its operations with our own, and we may not realize all or any of the expected benefits of the acquisition as and when planned. The integration of RehabCare’s operations with our own will be complex, costly and time-consuming. We expect that it will require significant attention from senior management and will impose substantial demands on our operations and personnel, potentially diverting attention from other important pending projects. The difficulties and risks associated with the integration of RehabCare include:
| • | the possibility that we will fail to implement our business plans for the combined company, including as a result of new legislation or regulation in the healthcare industry that affects the timing or costs associated with the operations of the combined company or our integration plan; |
| • | possible inconsistencies in the standards, controls, procedures, policies and compensation structures of the two companies; |
| • | limitations prior to the consummation of the acquisition on our ability to work with RehabCare management to develop an integration plan; |
| • | the increased scope and complexity of our operations; |
| • | the potential loss of key employees and the costs associated with our efforts to retain key employees; |
| • | provisions in our and RehabCare’s contracts with third parties that may limit our flexibility to take certain actions; |
| • | risks and limitations on our ability to consolidate corporate and administrative infrastructures of the two companies; |
| • | the possibility that we may have failed to discover liabilities of RehabCare during our due diligence investigation as part of the acquisition for which we, as a successor owner, may be responsible; |
| • | obligations that we will have to joint venture partners and other counterparties of RehabCare that arise as result of the change in control of RehabCare; |
| • | obligations that we will have to our lenders under the new financing arrangements to be put in place upon the closing of the merger, including our obligations to comply with significant new financial covenants; and |
| • | the possibility of unanticipated delays, costs or inefficiencies associated with the integration of RehabCare’s operations with our own. |
As a result of these difficulties and risks, we may not accomplish the integration of RehabCare’s business smoothly, successfully or within our budgetary expectations and anticipated timetable. Accordingly, we may fail to realize some or all of the anticipated benefits of the RehabCare acquisition, such as increase in our scale, diversification, cash flows and operational efficiency and meaningful accretion to our diluted earnings per share.
47
Table of Contents
We must obtain governmental and regulatory approvals to consummate the RehabCare acquisition, which, if delayed, not granted or granted with unacceptable conditions, may jeopardize or delay its consummation, result in additional expenditure of time and resources and reduce the anticipated benefits of the acquisition.
The proposed acquisition of RehabCare is conditioned on the receipt of all material governmental authorizations, consents, orders and approvals, including U.S. antitrust clearance and state licensure and regulatory approvals. If we do not receive these approvals, or do not receive them on terms that satisfy the conditions set forth in the Merger Agreement, then we will not be obligated to consummate the proposed acquisition.
The governmental agencies from which we will seek these approvals have broad discretion in administering the relevant regulations. As a condition to their approval of the RehabCare acquisition, they may impose requirements, limitations or costs or require divestitures or place restrictions on the conduct of the business of the combined company. These requirements, limitations, costs, divestitures or restrictions could jeopardize or delay the consummation of the RehabCare acquisition and could reduce its anticipated benefits to us. We cannot assure you that we will obtain all of the required approvals or that we can obtain them on any particular terms.
We may be unable to realize anticipated cost synergies or may incur additional and/or unexpected costs in order to realize them.
We expect to realize approximately $40 million of operating synergies within a period of two years following the completion of the RehabCare acquisition, with approximately $25 million expected in the first year after closing. We may be unable to realize all of these cost synergies within the timeframe expected, or at all, and we may incur additional and/or unexpected costs in order to realize them.
Risk Factors Relating to Reimbursement and Regulation of Our Business
Healthcare reform has initiated significant reforms to the United States healthcare system.
Various healthcare reform provisions became law upon enactment of the ACA. The reforms contained in the ACA will impact each of our businesses in some manner. Several of the reforms are very significant and could ultimately change the nature of our services, the methods of payment for our services and the underlying regulatory environment. The reforms include possible modifications to the conditions of qualification for payment, bundling payments to cover both acute and post-acute care and the imposition of enrollment limitations on new providers. The ACA creates a series of robust transparency and reporting requirements for skilled nursing facilities including requirements to disclose information on organizational structures, financial, clinical and other related data as well as information on officers, directors, trustees or managing employees. Skilled nursing facilities are required to certify to the Secretary of HHS and the OIG that the information submitted is accurate and current. In addition, a primary goal of healthcare reform is to reduce costs, which includes reductions in the reimbursement paid to us and other healthcare providers. Moreover, healthcare reform could negatively impact insurance companies, other third party payors, our customers, as well as other healthcare providers, which may in turn negatively impact our business. As such, these healthcare reforms or other similar healthcare reforms could have a material adverse effect on our business, financial position, results of operations and liquidity.
Changes in the reimbursement rates or methods or timing of payment from third party payors, including the Medicare and Medicaid programs, or the implementation of other measures to reduce reimbursement for our services and products could result in a substantial reduction in our revenues and operating margins.
We depend on reimbursement from third party payors, including the Medicare and Medicaid programs, for substantially all of our revenues. For the year ended December 31, 2010, we derived approximately 63% of our total revenues (before eliminations) from the Medicare and Medicaid programs and the balance from other third party payors, such as commercial insurance companies, health maintenance organizations, preferred provider
48
Table of Contents
organizations and contracted providers. The Medicare and Medicaid programs are highly regulated and subject to frequent and substantial changes. See “Item 1 – Business.”
There are continuing efforts to reform governmental healthcare programs, both as part of the ACA enacted in 2010 and otherwise, that could result in major changes in the healthcare delivery and reimbursement system on a national and state level. Potential reforms include changes directly impacting the government and private reimbursement systems for our LTAC hospitals, our nursing and rehabilitation centers as well as our rehabilitation operations. Reforms or other changes to the payment systems, including modifications to the conditions of qualification for payment, bundling payments to cover both acute and post-acute care or the imposition of enrollment limitations on new providers, may be proposed or could be adopted by Congress or CMS in the future.
Moreover, weak economic conditions also could adversely affect the budgets of individual states and of the federal government. This could result in attempts to reduce or eliminate payments for federal and state healthcare programs, including Medicare and Medicaid, and could result in an increase in taxes and assessments on our activities. In addition, private third party payors are continuing their efforts to control healthcare costs through direct contracts with healthcare providers, increased utilization review and greater enrollment in managed care programs and preferred provider organizations. These private payors increasingly are demanding discounted fee structures and are requesting that healthcare providers assume more financial risk.
Though we cannot predict what reform proposals will be adopted or finally implemented, healthcare reform and regulations may have a material adverse effect on our business, financial position, results of operations and liquidity through, among other things, decreasing funds available for our services or increased operating costs. We could be affected adversely by the continuing efforts of governmental and private third party payors to contain healthcare costs. We cannot assure you that reimbursement payments under governmental and private third party payor programs, including Medicare supplemental insurance policies, will remain at levels comparable to present levels or will be sufficient to cover the costs allocable to patients eligible for reimbursement pursuant to these programs. Future changes in third party payor reimbursement rates or methods, including the Medicare and Medicaid programs, or the implementation of other measures to reduce reimbursement for our services and products could result in a material reduction in our revenues. Our operating margins continue to be under pressure because of deterioration in pricing flexibility, changes in payor mix, changes in length of stay and growth in operating expenses in excess of increases in payments by third party payors. In addition, as a result of competitive pressures, our ability to maintain operating margins through price increases to private patients or commercial payors remains limited. These results could have a material adverse effect on our business, financial position, results of operations and liquidity.
Future cost containment initiatives undertaken by third party payors may limit our revenues and profitability.
Initiatives undertaken by major insurers and managed care companies to contain healthcare costs or to respond to healthcare reform could affect the profitability of our services. These payors attempt to control healthcare costs by contracting with providers of healthcare to obtain services on a discounted basis. We believe that this trend will continue and intensify and may further limit reimbursements for healthcare services. If insurers or managed care companies from whom we receive substantial payments reduce the amounts they pay for services, our profit margins may decline, or we may lose patients if we choose not to renew our contracts with these insurers at lower rates. These results could have a material adverse effect on our business, financial position, results of operations and liquidity.
Further consolidation of managed care organizations and other third party payors may adversely affect our profits.
Managed care organizations and other third party payors have continued to consolidate in order to enhance their ability to influence the delivery and cost structure of healthcare services. Consequently, the healthcare needs
49
Table of Contents
of a large percentage of the United States population are increasingly served by a smaller number of managed care organizations. These organizations generally enter into service agreements with a limited number of providers for needed services. In addition, third party payors, including managed care payors, increasingly are demanding discounted fee structures. To the extent that these organizations terminate us as a preferred provider, engage our competitors as a preferred or exclusive provider or demand discounted fee structures, our business, financial position, results of operations and liquidity could be materially and adversely affected.
We conduct business in a heavily regulated industry, and changes in regulations, the enforcement thereof or violations of regulations may result in increased costs or sanctions that reduce our revenues and profitability.
In the ordinary course of our business, we are subject regularly to inquiries and audits by federal and state agencies that oversee applicable healthcare program participation and payment regulations. We also have been subject to government investigations. We believe that the regulatory environment surrounding most segments of the healthcare industry will remain intense.
The extensive federal, state and local regulations affecting the healthcare industry include, but are not limited to, regulations relating to licensure, conduct of operations, ownership of facilities, addition of facilities, allowable costs, services and prices for services, facility staffing requirements, qualifications and licensure of staff, environmental and occupational health and safety, and the confidentiality and security of health-related information. In particular, various laws including anti-kickback, anti-fraud and abuse amendments codified under the Social Security Act prohibit certain business practices and relationships that might affect the provision and cost of healthcare services reimbursable under Medicare and Medicaid, including the payment or receipt of remuneration for the referral of patients whose care will be paid by Medicare or other governmental programs. Sanctions for violating the anti-kickback, anti-fraud and abuse amendments under the Social Security Act include criminal penalties, civil sanctions, fines and possible exclusion from government programs such as Medicare and Medicaid. See “Item 1 – Business – Governmental Regulation.”
Federal and state governments continue to pursue intensive enforcement policies resulting in a significant number of inspections, audits, citations of regulatory deficiencies and other regulatory sanctions including demands for refund of overpayments, terminations from the Medicare and Medicaid programs, bans on Medicare and Medicaid payments for new admissions and civil monetary penalties. RAC audits and other audits evaluating the medical necessity of services provided are expected to further intensify the regulatory environment surrounding the healthcare industry as third party firms engaged by CMS commence extensive reviews of claims data and medical and other records to identify improper payments to healthcare providers under the Medicare program. If we fail to comply with the extensive laws and regulations applicable to our businesses, we could become ineligible to receive government program reimbursement, suffer civil or criminal penalties or be required to make significant changes to our operations. In addition, we could be forced to expend considerable resources responding to investigations, audits or other enforcement actions under these laws or regulations. Furthermore, should we lose the licenses for one or more of our facilities as a result of regulatory action or otherwise, we could be in default under our Master Lease Agreements and our revolving credit facility. Failure of our staff to satisfy applicable licensure requirements or of our hospitals and nursing and rehabilitation centers to satisfy applicable licensure and certification requirements could have a material adverse effect on our business, financial position, results of operations and liquidity.
We are unable to predict the future course of federal, state and local regulation or legislation, including Medicare and Medicaid statutes and regulations, or the intensity of federal and state enforcement actions. Changes in the regulatory framework, including those associated with healthcare reform, and sanctions from various enforcement actions could have a material adverse effect on our business, financial position, results of operations and liquidity.
50
Table of Contents
We face and are currently subject to reviews, audits and investigations under our contracts with federal and state government agencies and other payors, and these reviews, audits and investigations could have adverse findings that may negatively impact our business.
As a result of our participation in the Medicare and Medicaid programs, we face and are currently subject to various governmental reviews, audits and investigations to verify our compliance with these programs and applicable laws and regulations. An increasing level of governmental and private resources is being devoted to the investigation of allegations of fraud and abuse in the Medicare and Medicaid programs, and federal and state regulatory authorities are taking an increasingly strict view of the requirements on healthcare providers by the Social Security Act and Medicare and Medicaid programs. We are routinely subject to audits under various government programs, including the RAC program, in which third party firms engaged by CMS conduct extensive reviews of claims data and medical and other records to identify potential improper payments to healthcare providers under the Medicare program. In addition, we, like other nursing center operators, are subject to ongoing investigations by the OIG into the billing of rehabilitation services provided to Medicare patients and general compliance with conditions of participation with Medicare and Medicaid. Private pay sources also often reserve the right to conduct audits. Our costs to respond to and defend reviews, audits and investigations are significant and are likely to increase in the current enforcement environment. In the past, some of these audits and investigations have required us to refund or retroactively adjust amounts that have been paid under the relevant program or from other payors. We may be subject to similar obligations in the future. Moreover, an adverse review, audit or investigation could also result in other adverse consequences, particularly if the underlying conduct is found to be systemic. These consequences include:
| • | state or federal agencies imposing fines, penalties and other sanctions on us; |
| • | loss of our right to participate in the Medicare or Medicaid programs or one or more third party payor networks; or |
| • | damage to our reputation in various markets, which could adversely affect our ability to attract patients, residents and employees. |
If they were to occur, these consequences could have a material adverse effect on our business, financial position, results of operations and liquidity.
We are subject to extensive and complex federal and state government laws and regulations which govern and restrict our relationships with physicians and other referral sources.
The Anti-Kickback Statute, the federal physician self-referral laws (commonly called the Stark Law), the FCA and similar state laws materially restrict our relationships with physicians and other referral sources. We have a variety of financial relationships with physicians and others who either refer or influence the referral of patients to our healthcare facilities, and these laws govern those relationships. The OIG has enacted safe harbor regulations that outline practices deemed protected from prosecution under the Anti-Kickback Statute. While we endeavor to comply with the safe harbors, certain of our current arrangements, including with physicians and other referral sources, may not qualify for safe harbor protection. Failure to qualify for a safe harbor does not mean the arrangement necessarily violates the Anti-Kickback Statute, but may subject the arrangement to greater scrutiny. However, we cannot offer assurance that practices outside of a safe harbor will not be found to violate the Anti-Kickback Statute. Allegations of violations of the Anti-Kickback Statute may be brought under federal civil monetary penalty laws, which require a lower burden of proof than other fraud and abuse laws, including the Anti-Kickback Statute.
Our financial relationships with referring physicians and their immediate family members must comply with the Stark Law by meeting an exception. We attempt to structure our relationships to meet an exception to the Stark Law, but the regulations implementing the exceptions are detailed and complex, and we cannot provide assurance that every relationship complies fully with the Stark Law. Unlike the Anti-Kickback Statute, failure to
51
Table of Contents
meet an exception under the Stark Law results in a violation of the Stark Law, even if such violation is technical in nature.
Additionally, if we violate the Anti-Kickback Statute or the Stark Law, or if we improperly bill for our services, we may be found to violate the FCA, either under a suit brought by the government or by a private person under a qui tam, or “whistleblower”, lawsuit.
If we fail to comply with the Anti-Kickback Statute, the Stark Law, the FCA or other applicable laws and regulations, we could be subjected to liabilities, including civil penalties (including the loss of our licenses to operate one or more facilities), exclusion of one or more facilities from participation in the Medicare, Medicaid and other federal and state healthcare programs and, for violations of certain laws and regulations, and criminal penalties.
We do not always have the benefit of significant regulatory or judicial interpretation of these laws and regulations. In the future, different interpretations or enforcement of these laws and regulations could subject our current or past practices to allegations of impropriety or illegality or could require us to make changes in our facilities, equipment, personnel, services, capital expenditure programs and operating expenses. A determination that we have violated these laws, or the public announcement that we are being investigated for possible violations of these laws, could have a material adverse effect on our business, financial position, results of operations and liquidity, and our business reputation could suffer significantly. In addition, other legislation or regulations at the federal or state level may be adopted that adversely affect our business.
If our LTAC hospitals fail to maintain their certification as long-term acute care hospitals, our profitability would decline.
If our LTAC hospitals, satellite LTAC facilities or HIHs fail to meet or maintain the standards for certification as LTAC hospitals, such as average minimum length of patient stay, they will receive payments under the prospective payment system applicable to general acute care hospitals rather than payment under the system applicable to LTAC hospitals. Payments at rates applicable to general acute care hospitals would result in our LTAC hospitals receiving less Medicare reimbursement than they currently receive for patient services and our profitability would decline. In addition, implementation of additional LTAC hospital certification criteria and medical necessity reviews may limit the population of patients eligible for our services or change the basis upon which we are paid, which could have a material adverse effect on our business, financial position, results of operations and liquidity.
Implementation of additional patient or facility criteria for LTAC hospitals that limit the population of patients eligible for our hospital services or change the basis upon which we are paid could adversely affect our revenues and profitability.
CMS has, for a number of years, considered the development of facility and patient certification criteria for LTAC hospitals, potentially as an alternative to the current payment system under LTAC PPS. In 2004, MedPAC recommended to Congress the adoption by CMS of new facility staffing and services criteria and patient clinical characteristics and treatment requirements for LTAC hospitals in order to ensure that only appropriate patients are admitted to these facilities. Since the MedPAC recommendation, CMS has initiated studies to examine such recommendations and those studies are ongoing. Implementation of additional criteria that may limit the population of patients eligible for our hospital services or change the basis upon which we are paid could have a material adverse effect on our business, financial position, results of operations and liquidity.
52
Table of Contents
The temporary moratorium on the Medicare certification of new LTAC hospitals and beds in existing LTAC hospitals will limit our ability to increase LTAC hospital bed capacity, expand into new areas or increase services in existing areas we serve.
The SCHIP Extension Act imposed a three-year moratorium beginning on December 29, 2007 on the establishment and classification of new LTAC hospitals, LTAC satellite facilities and LTAC beds in existing LTAC hospitals or satellite hospitals. The ACA extended this moratorium to five years. The moratorium does not apply to LTAC hospitals that, before December 29, 2007, (1) began the qualifying period for payment under LTAC PPS, (2) had a written agreement with an unrelated party for the construction, renovation, lease or demolition for a LTAC hospital and had expended at least 10% of the estimated cost of the project or $2,500,000 or (3) had obtained an approved certificate of need. The moratorium also does not apply to an increase in beds in an existing hospital or satellite facility if the LTAC hospital is located in a state where there is only one other LTAC hospital and the LTAC hospital requests an increase in beds following the closure or the decrease in the number of beds of the other LTAC hospital. This moratorium may adversely affect our ability to increase LTAC bed capacity, expand into new areas or increase bed capacity in existing markets that we serve.
Expiration of the moratorium imposed on certain federal regulations otherwise applicable to LTAC hospitals, including HIHs and satellite hospitals, will have an adverse effect on our future revenues and profitability.
The SCHIP Extension Act, among other things, placed a three-year moratorium beginning on December 29, 2007 on (1) the application of a one-time budget neutrality adjustment to payment rates to LTAC hospitals under LTAC PPS, and (2) the very short stay outlier payment reductions to LTAC hospitals. The ACA extended this moratorium to five years. The expiration of this moratorium could have a material adverse effect on our business, financial position, results of operations and liquidity.
CMS has regulations governing payments to LTAC hospitals that are co-located with another hospital, such as a HIH. The rules generally limit Medicare payments to the HIH if the Medicare admissions to the HIH from its co-located hospital exceed 25% of the total Medicare discharges for the HIH’s cost reporting period. There are limited exceptions for admissions from rural, urban single and MSA Dominant hospitals. Patients transferred after they have reached the short-term acute care outlier payment status are not counted toward the admission threshold. Patients admitted prior to meeting the admission threshold, as well as Medicare patients admitted from a non co-located hospital, are eligible for the full payment under LTAC PPS. If the HIH’s admissions from the co-located hospital exceed the limit in a cost reporting period, Medicare will pay the lesser of (1) the amount payable under LTAC PPS or (2) the amount payable under IPPS.
In 2007, CMS expanded the “25 Percent Rule” to all LTAC hospitals, regardless of whether they are co-located with another hospital. Under the 2007 Final Rule, all LTAC hospitals were to be paid LTAC PPS rates for admissions from a single referral source up to 25% of aggregate Medicare admissions. Patients reaching high cost outlier status in the short-term hospital were not to be counted when computing the 25% limit. Admissions beyond the 25% threshold were to be paid at a lower amount based upon IPPS rates.
Under the 2007 Final Rule, the 25% threshold was to be phased in over three years. Hospitals having fiscal years beginning on or after July 1, 2007 and before July 1, 2008, including most of our hospitals, had their admission cap initially established at the lesser of 75% of Medicare referrals or the actual percentage of Medicare referrals received from a primary referral source for that hospital in the base year of 2005. For most of our hospitals, this initial first year cap began on September 1, 2007. Beginning on September 1, 2008, the cap would have been reduced to the lesser of 50% of Medicare referrals or the actual percentage of Medicare referrals for that hospital in the 2005 base year. The fully phased-in cap of 25% would have applied to most of our hospitals after September 1, 2009.
The SCHIP Extension Act initially placed a three-year moratorium on the expansion of the “25 Percent Rule” to freestanding hospitals. That moratorium was extended to five years by the ACA. In addition, the SCHIP
53
Table of Contents
Extension Act initially provided for a three-year period during which (1) LTAC hospitals may admit up to 50% of their patients from their co-located hospitals and still be paid according to LTAC PPS; and (2) LTAC hospitals that are co-located with an urban single hospital or a MSA Dominant hospital may admit up to 75% of their patients from such urban single or MSA Dominant hospital and still be paid according to LTAC PPS. Those periods also were extended to five years under the ACA. The five-year moratorium of the “25 Percent Rule” threshold payment adjustment for freestanding hospitals and grandfathered hospitals with a host hospital will expire for cost reporting periods beginning on or after July 1, 2012. The expansion of the admission limit to 50% for non-grandfathered LTAC hospitals from their co-located hospital will expire for cost reports beginning on or after October 1, 2012, the same time at which the 75% limit for MSA Dominant hospitals will expire.
Since these rules are complex and are based on the volume of Medicare admissions and the source of those admissions, we cannot predict with any certainty the impact on our future revenues or operations from these regulations. If the “25 Percent Rule” is applied as currently written, it could have a material adverse effect on our business, financial position, results of operations and liquidity when the moratorium expires.
Healthcare reform and other regulations could adversely affect the liquidity of our customers, which could have an adverse effect on their ability to make timely payments to us for our products and services.
The ACA and other laws and regulations that limit or restrict Medicare and Medicaid payments to our customers could adversely impact the liquidity of our customers, resulting in their inability to pay us, or to timely pay us, for our products and services. In addition, if our customers fail to comply with applicable laws and regulations they could be subject to possible sanctions, including loss of licensure or eligibility to participate in reimbursement programs as well as civil and criminal penalties. These developments could have a material adverse effect on our business, financial position, results of operations and liquidity.
Risks Factors Relating to Our Capital and Liquidity
We may not be able to meet our substantial rent and debt service requirements.
A substantial portion of our cash flows from operations is dedicated to the payment of rents related to our leased properties as well as principal and interest obligations on our outstanding indebtedness, including our revolving credit facility. Subject to certain restrictions, we also have the ability to incur substantial additional borrowings under our revolving credit facility. In addition, we intend to incur substantial additional indebtedness in connection with the RehabCare acquisition. If we are unable to generate sufficient funds to meet our obligations or our revolving credit facility otherwise becomes due and payable, we may be required to refinance, restructure or otherwise amend some or all of such obligations, sell assets or raise additional cash through the sale of our equity. We cannot assure you that we would be able to obtain such refinancing on terms as favorable as our current financing or that such restructuring activities, sales of assets or issuances of equity can be accomplished or, if accomplished, would raise sufficient funds to meet these obligations. In addition, our Master Lease Agreements and/or our revolving credit facility:
| • | require us to dedicate a substantial portion of our cash flow to payments on our rent and interest obligations, thereby reducing the availability of cash flow to fund working capital, capital expenditures and other general corporate activities, |
| • | require us to pledge as collateral substantially all of our assets, |
| • | require us to maintain a certain defined fixed payment ratio at a specified level, thereby reducing our financial flexibility, |
| • | require us to limit the amount of capital expenditures we can incur in any fiscal year and also limit the aggregate amount we can expend on acquisitions, and |
| • | require us to operate continuously each leased property despite its level of profitability and otherwise restrict our operational flexibility. |
54
Table of Contents
These provisions:
| • | could have a material adverse effect on our ability to withstand competitive pressures or adverse economic conditions (including adverse regulatory changes), |
| • | could adversely affect our ability to make material acquisitions, obtain future financing or take advantage of business opportunities that may arise, and |
| • | could increase our vulnerability to a downturn in general economic conditions or in our business. |
Our failure to pay rent or otherwise comply with the provisions of any of our Master Lease Agreements could materially adversely affect our business, financial position, results of operations and liquidity.
We lease 38 of our hospitals and 159 of our nursing and rehabilitation centers from Ventas under our Master Lease Agreements. Our failure to pay the rent or otherwise comply with the provisions of any of our Master Lease Agreements would result in an “Event of Default” under such Master Lease Agreement and also would result in a default under our revolving credit facility. Upon an Event of Default, remedies available to Ventas include, without limitation, terminating such Master Lease Agreement, repossessing and reletting the leased properties and requiring us to remain liable for all obligations under such Master Lease Agreement, including the difference between the rent under such Master Lease Agreement and the rent payable as a result of reletting the leased properties, or requiring us to pay the net present value of the rent due for the balance of the term of such Master Lease Agreement. The exercise of such remedies would have a material adverse effect on our business, financial position, results of operations and liquidity.
For additional information on the Master Lease Agreements, see “Item 1 – Business – Master Lease Agreements.”
The condition of the financial markets, including volatility and weakness in the equity, capital and credit markets, could limit the availability and terms of debt and equity financing sources to fund the capital and liquidity requirements of our businesses, including financing we must undertake in connection with the RehabCare acquisition.
Financial markets experienced significant disruptions over the past few years. These disruptions have impacted liquidity in the debt markets, making financing terms for borrowers less attractive and, in certain cases, significantly reducing the availability of certain types of debt financing. Despite the instability over the past few years within the financial markets nationally and globally, we have not experienced any individual lender limitations to extend credit under our revolving credit facility. However, the obligations of each of the lending institutions in our revolving credit facility are separate and the availability of future borrowings under our revolving credit facility could be impacted by further volatility and disruptions in the financial credit markets or other events. While the term of our revolving credit facility expires in July 2012, we cannot assure you that a prolonged downturn in the credit markets or other circumstances will not impact our ability to access our revolving credit facility or to refinance the revolving credit facility. Our inability to access our revolving credit facility or refinance the revolving credit facility would have a material adverse effect on our business, financial position, results of operations and liquidity. We believe that the revolving credit facility included in the financing arrangements we will undertake for purposes of the RehabCare acquisition will include substantially similar terms and therefore continue to expose us to the risks identified above.
Interest rates under our revolving credit facility are based, at our option, upon (a) the London Interbank Offered Rate (“LIBOR”) plus the applicable margin or (b) the applicable margin plus the higher of the prime rate or 0.5% over the federal funds rate. Higher interest rates could have a material adverse effect on our business, financial position, results of operations and liquidity. Moreover, our level of leverage, particularly after the completion of the RehabCare acquisition, may limit our ability to refinance or amend our existing revolving credit facility.
55
Table of Contents
Our revolving credit facility is collateralized by substantially all of our assets including certain owned real property and is guaranteed by substantially all of our subsidiaries. The terms of our revolving credit facility include one financial covenant and certain other provisions that limit acquisitions and annual capital expenditures. We were in compliance with the terms of our revolving credit facility at December 31, 2010. However, a downturn in operating earnings or events beyond our control could impair our ability to comply with the covenants contained within our revolving credit facility. If we anticipated a potential financial or other covenant violation, however, we would seek relief from our lenders, which likely would include some cost to us, and such relief may not be on terms as favorable as those in our existing revolving credit facility. Under these circumstances, there is also the potential that our lenders would not grant relief to us. A default due to the violation of a financial or other covenant contained within our revolving credit facility or the occurrence of an “Event of Default” under the Master Lease Agreements could require us to immediately repay all amounts then outstanding under the revolving credit facility.
Our inability to access external sources of financing when our revolving credit facility terminates could have a material adverse effect on our business, financial position, results of operations and liquidity.
Prior to the termination of our revolving credit facility, we will need to enter into a new revolving credit facility to continue to operate our business. There can be no assurance that we will be successful in our effort to enter into a new revolving credit facility in the future. Many lenders have been adversely impacted by events over the past few years in the United States and international financial markets and, as a result, have ceased certain lending practices or reduced the amount of lending they have made available to borrowers. While we expect there to be alternatives available to us to enter into a new revolving credit facility, we cannot assure you that any of these alternatives will be successfully implemented.
We depend on our revolving credit facility to meet our cash requirements to operate our business. If we repay our revolving credit facility upon its termination and are unable to enter into a new revolving credit facility on terms acceptable to us, or at all, we may be forced to reduce our operations and may not be able to respond to changing business conditions or competitive pressures. As a result, our business, financial position, results of operations and liquidity could be adversely affected.
In connection with the RehabCare acquisition, we obtained the Commitment Letter from JPMorgan Chase Bank, N.A., J.P. Morgan Securities LLC, Morgan Stanley Senior Funding, Inc. and Citigroup Global Markets Inc. Subject to certain conditions, we expect to have in place approximately $1.9 billion of long-term financing, of which approximately $1.6 billion is expected to be outstanding at the time of consummation of the RehabCare transaction. If we were unable to complete these financings, it would have a material adverse effect on our business, financial position, results of operations and liquidity.
If we have future capital needs that cannot be funded from operating cash flows, any future issuances of equity securities may dilute the value of our common stock and any additional issuances of debt may increase our leverage.
Though we anticipate that the cash amounts generated internally, together with amounts available under our revolving credit facility, will be sufficient to implement our business plan for the foreseeable future, we may need additional capital if a substantial acquisition or other growth opportunity becomes available or if unexpected events occur or opportunities arise. Moreover, we intend to incur substantial additional indebtedness in connection with the RehabCare acquisition. We cannot assure you that additional capital will be available, or available on terms favorable to us. If capital is not available, we may not be able to fund internal or external business expansion or respond to competitive pressures or other market conditions. If available, we may obtain additional capital through the public or private sale of debt or equity securities. However, our ability to access the public debt or equity capital markets, on terms favorable to us or at all, may be limited by further disruptions in these markets or other events. If we sell equity securities, the transaction could be dilutive to our existing shareholders. Furthermore, these securities could have rights, preferences and privileges more favorable than
56
Table of Contents
those of our common stock. If we incur additional debt, our leverage may increase and could have a material adverse effect on our business, financial position, results of operations and liquidity.
Disruptions in the financial markets could negatively impact our investment portfolio.
The financial market disruptions over the past few years have impacted the value of equity investments, bonds and other securities. We regularly hold cash in depository and money market accounts. If the financial institutions holding or managing these accounts fail or experience other disruptions, we could lose a portion or all of our cash which could have a material adverse effect on our business, financial position, results of operations and liquidity.
In addition, we hold a substantial investment portfolio in our limited purpose insurance subsidiary. Investments held in our limited purpose insurance subsidiary consist principally of cash and cash equivalents, debt securities, equities and commercial paper that are held to satisfy the payment of claims and expenses related to professional liability and workers compensation risks. Our investment policy governing insurance subsidiary investments precludes the investment portfolio managers from selling any security at a loss without prior authorization from us. The investment managers also limit the exposure to any one issue, issuer or type of investment. We intend, and have the ability, to hold insurance subsidiary investments for a long duration without the necessity of selling securities to fund the underwriting needs of our insurance subsidiary. This ability to hold securities allows sufficient time for recovery of temporary declines in the market value of equity securities and the par value of debt securities as of their stated maturity date. We cannot assure you, however, that we will recover declines in the market value of our investments. There is a continuing risk that declines in fair value may occur and additional material realized losses from sales or other-than-temporary impairments may be recorded in the future. Furthermore, we cannot assure you that declines in the market value of our investments will not require us to further capitalize our limited purpose insurance subsidiary or otherwise have a material adverse effect on our business, financial position, results of operations and liquidity.
Our stock price is volatile and fluctuations in our operating results, quarterly earnings and other factors may result in declines in the price of our common stock.
Equity markets are prone to, and in the last few years have experienced, extreme price and volume fluctuations. Volatility over the past few years has had a significant impact on the market price of securities issued by many companies, including us and other companies in the healthcare industry. If we are unable to operate our businesses as profitably as we have in the past or as our stockholders expect us to in the future, the market price of our common stock will likely decline as stockholders could sell shares of our common stock when it becomes apparent that the market expectations may not be realized. In addition to our operating results, many economic and other factors beyond our control could have an adverse effect on the price of our common stock, including:
| • | general economic conditions; |
| • | quarterly variations in operating results; |
| • | changes in financial estimates and recommendations by securities analysts; |
| • | operating and stock price performance of other companies that investors may deem comparable; |
| • | press releases or negative publicity relating to our competitors or us or relating to trends in healthcare; |
| • | regulatory changes and adverse outcomes from litigation and government or regulatory investigations; |
| • | sales of stock by insiders; |
| • | changes in our credit ratings; |
57
Table of Contents
| • | natural disasters, terrorist attacks and pandemics; and |
| • | limitations on our ability to repurchase our common stock. |
Market volatility and declines in the price of our common stock could have a material adverse effect on our ability to obtain capital or complete acquisitions through the public or private sale or issuance of our equity securities.
In addition, security holders often institute class action litigation following periods of volatility in the price of a company’s securities. If the market value of our common stock experiences adverse fluctuations and we become a party to this type of litigation, regardless of the outcome, we could incur substantial legal costs and our management’s attention could be diverted from the operation of our business, causing our business to decline.
Risk Factors Relating to Our Operations
Acquisitions, investments and strategic alliances that we have made or may make in the future may use significant resources, may be unsuccessful and could expose us to unforeseen liabilities.
We intend to continue to selectively pursue strategic acquisitions of, investments in, and strategic alliances with LTAC hospitals, nursing centers, rehabilitation operations and other related healthcare operations, particularly where an acquisition may assist us in scaling our operations more rapidly and efficiently than internal growth. Acquisitions may involve significant cash expenditures, debt incurrence, additional operating losses, amortization of certain intangible assets of acquired companies, dilutive issuances of equity securities and expenses that could have a material adverse effect on our business, financial position, results of operations and liquidity. Our ability to pursue attractive acquisition targets, at least in the near term, may be adversely affected by the significant resources and management attention that we expect to devote to completion of the RehabCare acquisition.
Acquisitions, investments and strategic alliances involve numerous risks, which can be more significant if we complete additional acquisitions while still completing the integration of RehabCare if that acquisition is completed. These risks include:
| • | limitations on our ability to identify acquisitions that meet our target criteria and limitations on our ability to complete such acquisitions on reasonable terms and valuations, |
| • | limitations on our ability to access equity or capital to fund acquisitions, including difficulty in obtaining financing for acquisitions at a reasonable cost, or that such financing will not contain restrictive covenants that limit our operating flexibility or ability to access additional capital when needed, |
| • | entry into markets or businesses in which we may have limited or no experience, |
| • | difficulties integrating acquired operations, personnel and information systems, and in realizing projected efficiencies and cost savings, particularly in the case of significant acquisitions, |
| • | diversion of management’s time from existing operations, |
| • | potential loss of key employees or customers of acquired companies, |
| • | inaccurate assessment of assets and liabilities and exposure to undisclosed or unforeseen liabilities of acquired companies, including liabilities for failure to comply with healthcare laws, |
| • | inability to operate acquired facilities profitably or succeed in achieving improvements in their financial performance, and |
| • | impairment of acquired goodwill and intangible assets. |
We continue to seek acquisitions and other strategic opportunities for each of our businesses that may negatively impact our business, financial position, results of operations and liquidity.
We continue to seek acquisitions and other strategic opportunities for each of our businesses, particularly where an acquisition may assist us in scaling our operations more rapidly and efficiently than internal growth.
58
Table of Contents
Accordingly, we are often engaged in evaluating potential transactions and other strategic alternatives, some of which may be significant in size, such as the RehabCare acquisition, and we engage in preliminary discussions that may result in one or more transactions. Although there is uncertainty that any of our discussions will result in definitive agreements or the timing of announcement or completion of any transaction, our business, short-term and long-term financial position, results of operations and liquidity may be impacted if we announce or complete any such transaction or if we incur substantial costs or other losses in connection with such transaction, whether or not it is completed. Moreover, although we intend to enter into transactions that enhance long-term shareholder value, our ability to achieve this objective would be subject to integration risks, the ability to retain and attract key personnel, the ability to realize synergies and other risks, all of which would be more material with transactions of significant size.
In addition to acquisitions, we also may pursue strategic opportunities involving the construction of new hospitals or nursing and rehabilitation centers. The construction of new facilities involves numerous risks, including construction delays, cost over-runs, and the satisfaction of zoning and other regulatory requirements. We may be unable to operate newly constructed facilities profitably and such facilities may involve significant cash expenditures, debt incurrence, additional operating losses, and expenses that could have a material adverse effect on our business, financial position, results of operations and liquidity.
We could experience significant increases to our operating costs due to shortages of qualified nurses, therapists and other healthcare professionals or union activity.
The market for qualified nurses, therapists and other healthcare professionals is highly competitive. We, like other healthcare providers, have experienced difficulties in attracting and retaining qualified personnel such as nurses, certified nurse’s assistants, nurse’s aides, therapists and other providers of healthcare services. Our hospitals and nursing and rehabilitation centers are particularly dependent on nurses for patient care. Our rehabilitation division continues to seek qualified therapists to fill open positions. The difficulty we have experienced in hiring and retaining qualified personnel has increased our average wage rates and may force us to increase our use of contract personnel.
In addition, healthcare providers are continuing to see an increase in the amount of union activity across the country. At December 31, 2010, approximately 3,100 of the employees at 35 of our facilities were unionized. Though we cannot predict the degree to which we will be affected by future union activity, there are continuing legislative proposals that could result in increased union activity. We could experience an increase in labor and other costs from such union activity.
We expect to continue to experience increases in our labor costs primarily due to higher wages and greater benefits required to attract and retain qualified healthcare personnel. Salaries, wages and benefits were approximately 57% of our consolidated revenues for the year ended December 31, 2010. Our ability to manage labor costs will significantly affect our future operating results.
We could experience significant legal actions, fines and increases in our operating costs if we fail to comply with state minimum staffing requirements.
Various states in which we operate hospitals and nursing and rehabilitation centers have established minimum staffing requirements or may establish minimum staffing requirements in the future. Staffing requirements in some states is not contingent upon any additional appropriation of state funds in any budget act or other statute. Our ability to satisfy such staffing requirements will, among other things, depend upon our ability to attract and retain qualified healthcare professionals.
While we seek to comply with all applicable staffing requirements, the regulations in this area are complex and we may experience compliance issues from time to time. Failure to comply with such minimum staffing requirements may result in one or more facilities failing to meet the conditions of participation under relevant
59
Table of Contents
federal and state healthcare programs and the imposition of fines or other sanctions. Private litigation involving these matters has also become more common, and certain of our facilities are the subject of litigation involving claims brought in 2010 that we did not meet relevant staffing requirements from time to time since 2006.
Moreover, a portion of the staffing costs we incur is funded by states through Medicaid program appropriations or otherwise. If states do not appropriate sufficient additional funds to pay for any additional operating costs resulting from such minimum staffing requirements, our profitability may be materially adversely affected.
If we lose our key management personnel, we may not be able to successfully manage our business and achieve our objectives.
Our future success depends in large part upon the leadership and performance of our executive management team and key employees and our ability to retain and motivate these individuals. Competition for these individuals is intense and there can be no assurance that we will retain our key officers and employees or that we can attract or retain other highly qualified individuals in the future. If we lose the services of one or more of our key officers or employees, or if one or more of them decides to join a competitor or otherwise compete directly or indirectly with us, we may not be able to successfully manage our business or achieve our business objectives and we may not be able to replace them with similarly qualified personnel. If we lose key personnel, we may be unable to replace them with personnel of comparable experience, reputation in the industry or skills. The loss of any of our key officers or employees could have a material adverse effect on our business, financial position, results of operations and liquidity.
If we fail to attract patients and residents and compete effectively with other healthcare providers or if our referral sources fail to view us as an attractive long-term healthcare provider, our revenues and profitability may decline.
The long-term healthcare services industry is highly competitive. Our hospitals face competition from healthcare providers that provide services comparable to those offered by our hospitals. Many competing hospitals are larger and more established than our hospitals. We may experience increased competition from existing hospitals as well as hospitals converted, in whole or in part, to specialized care facilities. Our nursing and rehabilitation centers compete on a local and regional basis with other nursing centers and other long-term healthcare providers. Some of our competitors operate newer facilities and may offer services not provided by us or are operated by entities having greater financial and other resources than us. Our rehabilitation division competes with national, regional and local rehabilitation service providers within our markets. Several of these competitors may have greater financial and other resources than us, may be more established in the markets in which we compete and may be willing to provide services at lower prices. We cannot assure you that increased competition in the future will not adversely affect our business, financial position, results of operations and liquidity.
In addition, we rely significantly on appropriate referrals from physicians, hospitals and other healthcare providers in the communities in which we deliver our services to attract appropriate patients and residents. Our referral sources are not obligated to refer business to us and may refer business to other healthcare providers. We believe many of our referral sources refer patients and residents to us as a result of the quality of our patient services and our efforts to establish and build a relationship with them. If any of our facilities fail to achieve or maintain a reputation for providing high quality care, or are perceived to provide a lower quality of care than comparable facilities within the same geographic area, or customers of our rehabilitation therapy services perceive that they could receive higher quality services from other providers, our ability to attract and retain patients and customers could be adversely affected. We believe that the perception of our quality of care by potential residents or patients or their families seeking our services is influenced by a variety of factors, including physician and other healthcare professional referrals, community information and referral services, newspapers and other print and electronic media, results of patient surveys, recommendations from family and friends, and
60
Table of Contents
published quality care statistics compiled by CMS or other industry data. If we lose, or fail to maintain, existing relationships with our referral resources, fail to develop new relationships or if we are perceived by our referral sources for any reason as not providing high quality patient care, our patient volumes and the quality of our patient mix could suffer and our revenue and profitability could decline.
Significant legal actions could subject us to increased operating costs and substantial uninsured liabilities, which could materially and adversely affect our business, financial position, results of operations and liquidity.
We incur significant costs to investigate and defend against a variety of claims, including professional liability, wage and hour, and minimum staffing claims, among others, particularly in our hospital and nursing and rehabilitation center operations. In addition to large compensatory claims, plaintiffs’ attorneys increasingly are seeking, and have sometimes been successful in obtaining, significant fines and punitive damages and attorneys’ fees. Furthermore, there are continuing efforts to limit the ability of healthcare providers to utilize arbitration as a process to resolve these claims. As a result of these factors, our defense costs and potential liability exposure are significant, unpredictable, and likely to increase. We also are subject to lawsuits under the FCA and comparable state laws for submitting fraudulent bills for services to the Medicare and Medicaid programs. These lawsuits, which may be initiated by “whistleblowers”, can involve significant monetary damages, fines, attorneys’ fees and the award of bounties to private plaintiffs who successfully bring these suits and to the government programs. We are also subject to payment obligations under contracts we enter into with our rehabilitation division customers to indemnify them against claim denials associated with our services.
While we are able to insure against certain of these costs and liabilities, such as our professional liability risks described below, we are not able to do so in many other cases. In the absence of insurance proceeds, we must fund these costs and liabilities from operating cash flows, which can reduce our operating margins and our funds available for investment in our business, and otherwise limit our operating and financial flexibility.
We insure a substantial portion of our professional liability risks primarily through our limited purpose insurance subsidiary. Provisions for loss for our professional liability risks are based upon management’s best available information including actuarially determined estimates. The allowance for professional liability risks includes an estimate of the expected cost to settle reported claims and an amount, based upon past experiences, for losses incurred but not reported. These liabilities are necessarily based upon estimates and, while management believes that the provision for loss is adequate, the ultimate liability may be in excess of, or less than, the amounts recorded. Changes in the number of professional liability claims and the cost to settle these claims significantly impact the allowance for professional liability risks. A relatively small variance between our estimated and actual number of claims or average cost per claim could have a material impact, either favorable or unfavorable, on the adequacy of the allowance for professional liability risks. Differences between the ultimate claims costs and our historical provisions for loss and actuarial assumptions and estimates could have a material adverse effect on our business, financial position, results of operations and liquidity.
Our limited purpose insurance subsidiary insures initial losses up to specified coverage levels per occurrence and in the aggregate. On a per claim basis, coverages for losses in excess of those insured by the limited purpose insurance subsidiary are maintained through unaffiliated commercial insurance carriers. Our limited purpose insurance subsidiary insures all claims in all states up to a per occurrence limit without the benefit of any aggregate coverage limit through unaffiliated commercial insurance carriers, thereby increasing our financial risk. We maintain professional and general liability insurance in amounts and coverage that management believes are sufficient for our operations. However, our insurance may not cover all claims against us or the full extent of our liability nor continue to be available at a reasonable cost. Moreover, the cost of insurance coverage maintained with unaffiliated commercial insurance carriers is costly and may continue to increase. If we are unable to maintain adequate insurance coverage or are required to pay punitive damages that are uninsured, we may be exposed to substantial liabilities.
61
Table of Contents
Federal and state employment-related laws and regulations could increase our cost of doing business and subject us to significant back pay awards, fines and lawsuits.
Our operations are subject to a variety of federal and state employment-related laws and regulations, including, but not limited to, the U.S. Fair Labor Standards Act which governs such matters as minimum wages, overtime pay, compensable time, recordkeeping and other working conditions, the Americans with Disabilities Act (ADA) and similar state laws that provide civil rights protections to individuals with disabilities in the context of employment, public accommodations and other areas, the National Labor Relations Act, regulations of the Equal Employment Opportunity Commission, regulations of the Office of Civil Rights, regulations of state Attorneys General, federal and state wage and hour laws, family leave mandates and a variety of similar laws enacted by the federal and state governments that govern these and other employment-related matters. Accordingly, we are subject to employee-related claims, lawsuits and proceedings in connection with our operations, including, but not limited to, those related to wrongful discharge, discrimination or violations of equal employment or federal and state wage and hour laws. Because labor represents such a large portion of our operating costs, compliance with these evolving federal and state laws and regulations could substantially increase our cost of doing business and subject us to significant back pay awards, fines and lawsuits. In addition, federal proposals to introduce a system of mandated health insurance and flexible work time and other similar initiatives could, if implemented, adversely affect our operations. Our failure to comply with federal and state employment-related laws and regulations could have a material adverse effect on our business, financial position, results of operations and liquidity.
We have limited operational and strategic flexibility since we lease a substantial number of our facilities.
We lease a substantial number of our facilities from Ventas and other third parties. Under our leases, we generally are required to operate continuously our leased properties as a provider of healthcare services. In addition, these leases generally limit or restrict our ability to assign the lease to another party. Our failure to comply with these lease provisions would result in an event of default under the leases and subject us to material damages, including potential defaults under our revolving credit facility. Given these restrictions, we may be forced to continue operating unprofitable facilities to avoid defaults under our leases. See “Item 1 – Business – Master Lease Agreements.”
Possible changes in the acuity of residents and patients as well as payor mix and payment methodologies may significantly affect our profitability.
The sources and amount of our revenues are determined by a number of factors, including the occupancy rates of our facilities, length of stay, the payor mix of residents and patients, rates of reimbursement among payors and patient acuity. Changes in patient acuity as well as payor mix among private pay, Medicare and Medicaid can significantly affect our profitability. In particular, any significant decrease in our population of high acuity patients or any significant increase in our Medicaid population could have a material adverse effect on our business, financial position, results of operations and liquidity, especially if state Medicaid programs continue to limit, or more aggressively seek limits on, reimbursement rates.
We may be unable to reduce costs to offset completely any decreases in our revenues.
Reduced levels of occupancy in our facilities and reductions in reimbursements from Medicare, Medicaid or other payors would adversely impact our revenues and liquidity. We may be unable to put in place corresponding reductions in costs in response to declines in census or other revenue shortfalls. The inability to timely adjust our operations to address a decrease in our revenues could have a material adverse effect on our business, financial position, results of operations and liquidity.
62
Table of Contents
We are exposed to the credit risk of our payors which in the future may cause us to make larger allowances for doubtful accounts or incur bad debt write-offs.
Due to weak economic conditions or other factors, commercial payors and customers may default on their payments to us and individual patients may default on co-payments and deductibles for which they are responsible under the terms of either commercial insurance programs or Medicare. Although we review the credit risk of our commercial payors and customers regularly, such risks may arise from events or circumstances that are difficult to anticipate or control, such as a general economic downturn. If our payors default on their payments to us in the future, we may have to record higher provisions for allowances for doubtful accounts or incur bad debt write-offs, both of which could have a material adverse effect on our business, financial position, results of operations and liquidity.
Delays in collection of our accounts receivable could adversely affect our business, financial position, results of operations and liquidity.
Prompt billing and collection are important factors in our liquidity. Billing and collection of our accounts receivable are subject to the complex regulations that govern Medicare and Medicaid reimbursement and rules imposed by non-government payors. Our inability, or the inability of our customers, to bill and collect on a timely basis pursuant to these regulations and rules could subject us to payment delays that could negatively impact our business, financial position, results of operations and liquidity. In addition, we may experience delays in reimbursement as a result of the failure to receive prompt approvals related to change of ownership applications for acquired or other facilities or from delays caused by our or other third parties’ information system failures.
If we are found to have violated laws protecting the confidentiality of patient health information, we could be subject to civil or criminal penalties, which could increase our liabilities and harm our reputation or our business.
There are a number of federal and state laws protecting the confidentiality of certain patient health information, including patient records, and restricting the use and disclosure of that protected information. In particular, the privacy rules under HIPAA protect medical records and other personal health information by limiting their use and disclosure, giving individuals the right to access, amend and seek accounting of their own health information and limiting most use and disclosures of health information to the minimum amount reasonably necessary to accomplish the intended purpose. If we are found to be in violation of the privacy or security rules under HIPAA or other federal or state laws protecting the confidentiality of patient health information, we could be subject to sanctions and civil or criminal penalties, which could increase our liabilities, harm our reputation and have a material adverse effect on our business, financial position, results of operations and liquidity.
We depend on the proper function and availability of our information systems.
We are dependent on the proper function and availability of our information systems. Though we have taken steps to protect the safety and security of our information systems and the data maintained within those systems, there can be no assurance that our safety and security measures and disaster recovery plan will prevent damage or interruption of our systems and operations and we may be vulnerable to losses associated with the improper functioning, security breach or unavailability of our information systems. Failure to maintain proper function and availability of our information systems could have a material adverse effect on our business, financial position, results of operations and liquidity.
In addition, certain software supporting our business and information systems are licensed to us by independent software developers. Our inability, or the inability of these developers, to continue to maintain and upgrade our information systems and software could disrupt or reduce the efficiency of our operations. In
63
Table of Contents
addition, costs and potential problems and interruptions associated with the implementation of new or upgraded systems and technology or with maintenance or adequate support of existing systems also could disrupt or reduce the efficiency of our operations and could have a material adverse effect on our business, financial position, results of operations and liquidity.
Terrorist attacks, pandemics or natural disasters could negatively impact our business, financial position, results of operations and liquidity.
Terrorist attacks, pandemics, or acts of nature, such as floods, fires, hurricanes, tornadoes or earthquakes, may cause damage or disruption to us, our employees and our facilities, which could have an adverse impact on our residents and patients. In order to provide care for our residents and patients, we are dependent upon consistent and reliable delivery of food, pharmaceuticals, power and other products to our facilities and the availability of employees to provide services at our facilities. If the delivery of goods or the ability of employees to reach our facilities were interrupted due to a natural disaster, pandemic or a terrorist attack, it could have a significant negative impact on our business. Furthermore, the impact, or impending threat, of a natural disaster has in the past and may in the future require that we evacuate one or more facilities, which would be costly and would involve substantial risks to our operations and potentially to our residents and patients. The impact of natural disasters, pandemics and terrorist attacks is inherently uncertain. Such events could severely damage or destroy one or more of our facilities, harm our business, reputation and financial performance or otherwise have a material adverse effect on our business, financial position, results of operations and liquidity.
Climate change poses both regulatory and physical risks that could adversely impact our business, financial position, results of operations and liquidity.
Climate change could have a potential economic impact on us and climate change mitigation programs and regulations could increase our costs. Energy costs could be higher as a result of climate change regulations. Our costs could increase if utility companies pass on their costs, such as those associated with carbon taxes, emission cap and trade programs, or renewable portfolio standards. In addition, climate change may increase the frequency or intensity of natural disasters. As such, we cannot assure you that climate change will not adversely impact our business, financial position, results of operations and liquidity.
Certain events or circumstances could result in the impairment of our assets or other charges, including, without limitation, impairments of goodwill and identifiable intangible assets that result in material charges to earnings.
We regularly review the carrying value of certain long-lived assets and identifiable finite lived intangible assets with respect to any events or circumstances that indicate an impairment or an adjustment to the amortization period may be necessary, such as when the market value of our common stock is below book equity value. On an ongoing basis, we also evaluate, based upon the fair value of our reporting units, whether the carrying value of our goodwill is impaired. If circumstances suggest that the recorded amounts of any of these assets cannot be recovered based upon estimated future cash flows, the carrying values of such assets are reduced to fair value. If the carrying value of any of these assets is impaired, we may incur a material charge to earnings.
Although we have determined that there were no goodwill or other indefinite lived intangible asset impairments as of December 31, 2010, adverse changes in the operating environment and related key assumptions used to determine the fair value of our reporting units and indefinite lived intangible assets or continued declines in the value of our common stock may result in future impairment charges for a portion or all of these assets. Moreover, the value of our goodwill and other indefinite lived assets could be negatively impacted by potential healthcare reforms. An impairment charge could have a material adverse effect on our business, financial position and results of operations.
64
Table of Contents
The inability or failure of management in the future to conclude that we maintain effective internal control over financial reporting, or the inability of our independent registered public accounting firm to issue a report of our internal control over financial reporting, could have a material adverse effect on our business, financial position, results of operations and liquidity.
We report annually on the effectiveness of our internal control over financial reporting, and our independent registered public accounting firm must also audit the effectiveness of our internal control over financial reporting on an annual basis. If we fail to have, or management or our independent registered public accounting firm is unable to conclude that we maintain, effective internal controls and procedures for financial reporting, we could be unable to provide timely and reliable financial information which could have a material adverse effect on our business, financial position, results of operations and liquidity.
Different interpretations of accounting principles or changes in generally accepted accounting principles could have a material adverse effect on our business, financial position, results of operations and liquidity.
Generally accepted accounting principles are complex, continually evolving and changing and may be subject to varied interpretation by third parties, including the SEC. Such varied interpretations could result from differing views related to specific facts and circumstances. Differences in interpretation of generally accepted accounting principles or changes in generally accepted accounting principles could have a material adverse effect on our business, financial position, results of operations and liquidity.
Risk Factors Relating to the KPS Spin-Off
If the Spin-off Transaction does not qualify as a tax-free transaction, tax could be imposed on us and our shareholders.
As a condition to closing the Spin-off Transaction in 2007, we received a private letter ruling from the Internal Revenue Service (the “IRS”) that the spin-off of KPS and the subsequent merger of KPS and distribution of PharMerica common stock qualified for tax-free treatment to holders of our common stock (except with respect to cash received in lieu of a fractional share) and, generally, to us.
The IRS ruling does not address all of the issues that are relevant to determining whether the Spin-off Transaction will qualify for tax-free treatment because the IRS will not rule on certain issues. As a condition to closing, we received an opinion of counsel that the Spin-off Transaction generally qualifies for tax-free treatment to us and our shareholders. The opinion of counsel is intended to address certain of those matters that the ruling does not. The IRS ruling and opinion of counsel do not address, however, state, local or foreign tax consequences of the Spin-off Transaction, merger and distribution of PharMerica common stock.
The IRS ruling and the opinion of counsel relied on representations, assumptions and undertakings made by us and PharMerica (and its subsidiaries), including representations and undertakings from PharMerica regarding the conduct of its business and other matters after the closing of the Spin-off Transaction. If such representations, assumptions or undertakings are incorrect, neither the IRS ruling nor the opinion of counsel would be valid. In addition, current law generally creates a presumption that the spin-off of KPS in the Spin-off Transaction would be taxable to us, but not to our shareholders, if PharMerica or its shareholders were to engage in certain transactions that result in a change in ownership of its stock during the four-year period beginning two years before the Spin-off Transaction, unless it is established that the Spin-off Transaction and such transactions were not part of a plan or series of related transactions to effect a change in ownership of the stock of PharMerica.
Furthermore, notwithstanding the IRS private letter ruling and the opinion of counsel, the IRS could determine that the Spin-off Transaction should be treated as a taxable transaction to us and our shareholders if it determines that any of the representations, assumptions or undertakings that were included in the request for the private letter ruling are false or have been violated or if it disagrees with the conclusions in the opinion of counsel that are not covered by the IRS ruling. If the spin-off of KPS in the Spin-off Transaction fails to qualify
65
Table of Contents
for tax-free treatment, the deemed receipt of shares of KPS will be treated as a taxable distribution to our shareholders. In addition, events occurring after the distribution of common stock of PharMerica could cause us to recognize a gain on the spin-off of KPS.
| Item 1B. | Unresolved Staff Comments |
None.
| Item 2. | Properties |
For information concerning the hospitals and nursing and rehabilitation centers operated by us, see “Item 1 – Business – Hospital Division – Hospital Facilities,” “Item 1 – Business – Nursing Center Division – Nursing and Rehabilitation Center Facilities,” and “Item 1 – Business – Master Lease Agreements.” We believe that our facilities are adequate for our future needs in such locations.
Our corporate headquarters is located in a 287,000 square foot building in Louisville, Kentucky.
We are subject to various federal, state and local laws and regulations governing the use, discharge and disposal of hazardous materials, including medical waste products. Compliance with these laws and regulations is not expected to have a material adverse effect on us. It is possible, however, that environmental issues may arise in the future which we cannot predict.
| Item 3. | Legal Proceedings |
We are a party to various legal actions (some of which are not insured), and regulatory and other governmental audits and investigations in the ordinary course of our business. We cannot predict the ultimate outcome of pending litigation and regulatory and other governmental audits and investigations. These matters could potentially subject us to sanctions, damages, recoupments, fines and other penalties. The DOJ, CMS or other federal and state enforcement and regulatory agencies may conduct additional investigations related to our businesses in the future that may, either individually or in the aggregate, have a material adverse effect on our business, financial position, results of operations and liquidity. See “Item 1A – Risk Factors – Risk Factors Relating to Our Operations – “We could experience significant legal actions, fines and increases in our operating costs if we fail to comply with state minimum staffing requirements,” “Significant legal actions could subject us to increased operating costs and substantial uninsured liabilities, which could materially and adversely affect our business, financial position, results of operations and liquidity,” and “Federal and state employment-related laws and regulations could increase our cost of doing business and subject us to significant back pay awards, fines and lawsuits.”
On February 10, 2011, a purported class action complaint relating to the RehabCare acquisition was filed in the Circuit Court of St. Louis County, Missouri, against RehabCare and certain of its directors and officers, as well as us, by Arthur I. Murray, Jr., individually and on behalf of all of our stockholders, excluding the defendants and their affiliates. The complaint alleges, among other allegations, that the consideration that RehabCare’s stockholders will receive in connection with the proposed transaction is inadequate and that the individual RehabCare defendants breached their fiduciary duties to stockholders in approving the Merger Agreement. The complaint further alleges that the individual RehabCare defendants were aided and abetted in such breaches by RehabCare and us. The complaint seeks various forms of relief, including injunctive relief that would, if granted, prevent the RehabCare acquisition from being consummated in accordance with the agreed-upon terms. The case is styled Arthur I. Murray, Jr. v. RehabCare Group, Inc., et al. (No. I.I.S.L. – CC00566, Circuit Court, St. Louis Co., MO). Another purported class action complaint, styled Norfolk County Retirement System v. Harry E. Rich, et al. (C.A. No. 6197 (DE (Wilmington) Court of Chancery) and filed on February 15, 2011, asserts substantially identical claims and seeks similar relief against RehabCare, certain of its directors and
66
Table of Contents
officers and us, on behalf of all of our stockholders, excluding the defendants and their affiliates. We believe that these complaints are without merit and intend to defend them vigorously.
| Item 4. | Removed and Reserved |
67
Table of Contents
PART II
| Item 5. | Market for Registrant’s Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities |
MARKET PRICE FOR COMMON STOCK
AND DIVIDEND HISTORY
Our common stock is quoted on the New York Stock Exchange (the “NYSE”) under the ticker symbol “KND.” The prices in the table below, for the calendar quarters indicated, represent the high and low sale prices for our common stock as reported on the NYSE.
| Sales price of common stock |
||||||||
| 2010 |
High | Low | ||||||
| First quarter |
$ | 19.76 | $ | 16.01 | ||||
| Second quarter |
$ | 18.83 | $ | 12.75 | ||||
| Third quarter |
$ | 13.75 | $ | 11.50 | ||||
| Fourth quarter |
$ | 19.59 | $ | 12.52 | ||||
| 2009 |
High | Low | ||||||
| First quarter |
$ | 18.57 | $ | 11.51 | ||||
| Second quarter |
$ | 17.83 | $ | 10.70 | ||||
| Third quarter |
$ | 17.27 | $ | 11.83 | ||||
| Fourth quarter |
$ | 20.00 | $ | 13.80 | ||||
Our revolving credit facility contains covenants that limit, among other things, our ability to pay dividends. Any determination to pay dividends in the future will be dependent upon our results of operations, financial position, contractual restrictions, restrictions imposed by applicable laws and other factors deemed relevant by our Board of Directors. We have not paid, and do not anticipate that we will pay in the foreseeable future, any cash dividends on our common stock. Accordingly, investors must rely on sales of their common stock after price appreciation which may never occur, as the only way to realize any future gains on their investment. Investors seeking cash dividends should not purchase our common stock.
As of January 31, 2011, there were 470 holders of record of our common stock.
See “Part III – Item 12 – Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters,” for disclosures regarding our equity compensation plans.
68
Table of Contents
PERFORMANCE GRAPH
The following graph summarizes the cumulative total return to shareholders of our common stock from December 30, 2005 to December 31, 2010, compared to the cumulative total return on the Standard & Poor’s 500 Stock Index (the “S&P Composite Index”) and the Standard & Poor’s 1500 Health Care Index (the “S&P 1500 Health Care Index”). The graph assumes an investment of $100 in each of our common stock, the S&P Composite Index, and the S&P 1500 Health Care Index on December 30, 2005, and also assumes the reinvestment of all cash dividends. In accordance with SEC rules, the July 31, 2007 distribution of the KPS shares to our shareholders in connection with the Spin-off Transaction is treated for purposes of the following graph as a special stock dividend in calculating shareholder return and prior period prices have been adjusted accordingly.
COMPARISON OF CUMULATIVE TOTAL RETURN
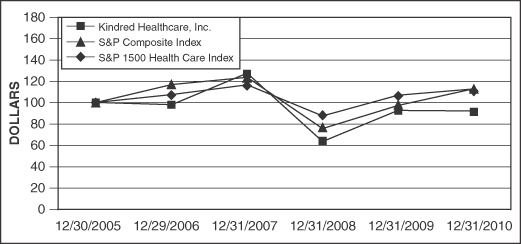
| 12/30/05 | 12/29/06 | 12/31/07 | 12/31/08 | 12/31/09 | 12/31/10 | |||||||||||||||||||
| Kindred Healthcare, Inc. |
$ | 100.00 | $ | 98.02 | $ | 125.78 | $ | 65.56 | $ | 92.95 | $ | 92.50 | ||||||||||||
| S&P Composite Index |
100.00 | 115.79 | 122.16 | 76.96 | 97.33 | 111.99 | ||||||||||||||||||
| S&P 1500 Health Care Index |
100.00 | 106.97 | 115.55 | 88.09 | 106.37 | 111.90 | ||||||||||||||||||
69
Table of Contents
| Item 6. | Selected Financial Data |
KINDRED HEALTHCARE, INC.
SELECTED FINANCIAL DATA
(In thousands, except per share amounts)
| Year ended December 31, | ||||||||||||||||||||
| 2010 | 2009 | 2008 | 2007 | 2006 | ||||||||||||||||
| Statement of Operations Data: |
||||||||||||||||||||
| Revenues |
$ | 4,359,697 | $ | 4,270,007 | $ | 4,093,864 | $ | 4,128,649 | $ | 4,041,786 | ||||||||||
| Salaries, wages and benefits |
2,505,690 | 2,483,086 | 2,374,163 | 2,325,417 | 2,185,316 | |||||||||||||||
| Supplies |
342,197 | 333,056 | 317,149 | 542,986 | 669,023 | |||||||||||||||
| Rent |
357,372 | 348,248 | 338,673 | 337,769 | 289,080 | |||||||||||||||
| Other operating expenses |
948,609 | 886,205 | 854,383 | 730,965 | 650,045 | |||||||||||||||
| Other income |
(11,422 | ) | (11,512 | ) | (17,407 | ) | (7,701 | ) | – | |||||||||||
| Depreciation and amortization |
121,552 | 125,730 | 120,022 | 118,574 | 115,057 | |||||||||||||||
| Interest expense |
7,090 | 7,880 | 15,373 | 17,044 | 13,920 | |||||||||||||||
| Investment income |
(1,245 | ) | (4,413 | ) | (7,096 | ) | (16,105 | ) | (14,488 | ) | ||||||||||
| 4,269,843 | 4,168,280 | 3,995,260 | 4,048,949 | 3,907,953 | ||||||||||||||||
| Income from continuing operations before income taxes |
89,854 | 101,727 | 98,604 | 79,700 | 133,833 | |||||||||||||||
| Provision for income taxes |
33,708 | 39,115 | 38,144 | 36,567 | 52,739 | |||||||||||||||
| Income from continuing operations |
56,146 | 62,612 | 60,460 | 43,133 | 81,094 | |||||||||||||||
| Discontinued operations, net of income taxes: |
||||||||||||||||||||
| Income (loss) from operations |
798 | 931 | (3,399 | ) | (12,982 | ) | (2,351 | ) | ||||||||||||
| Loss on divestiture of operations |
(453 | ) | (23,432 | ) | (20,776 | ) | (77,021 | ) | (32 | ) | ||||||||||
| Net income (loss) |
$ | 56,491 | $ | 40,111 | $ | 36,285 | $ | (46,870 | ) | $ | 78,711 | |||||||||
| Earnings (loss) per common share: |
||||||||||||||||||||
| Basic: |
||||||||||||||||||||
| Income from continuing operations |
$ | 1.42 | $ | 1.61 | $ | 1.56 | $ | 1.09 | $ | 2.02 | ||||||||||
| Discontinued operations: |
||||||||||||||||||||
| Income (loss) from operations |
0.02 | 0.02 | (0.09 | ) | (0.33 | ) | (0.06 | ) | ||||||||||||
| Loss on divestiture of operations |
(0.01 | ) | (0.60 | ) | (0.53 | ) | (1.94 | ) | – | |||||||||||
| Net income (loss) |
$ | 1.43 | $ | 1.03 | $ | 0.94 | $ | (1.18 | ) | $ | 1.96 | |||||||||
| Diluted: |
||||||||||||||||||||
| Income from continuing operations |
$ | 1.42 | $ | 1.60 | $ | 1.54 | $ | 1.06 | $ | 1.95 | ||||||||||
| Discontinued operations: |
||||||||||||||||||||
| Income (loss) from operations |
0.02 | 0.02 | (0.09 | ) | (0.32 | ) | (0.06 | ) | ||||||||||||
| Loss on divestiture of operations |
(0.01 | ) | (0.60 | ) | (0.53 | ) | (1.90 | ) | – | |||||||||||
| Net income (loss) |
$ | 1.43 | $ | 1.02 | $ | 0.92 | $ | (1.16 | ) | $ | 1.89 | |||||||||
| Shares used in computing earnings (loss) per common share: |
||||||||||||||||||||
| Basic |
38,738 | 38,339 | 37,830 | 38,791 | 39,108 | |||||||||||||||
| Diluted |
38,954 | 38,502 | 38,397 | 39,558 | 40,677 | |||||||||||||||
| Financial Position: |
||||||||||||||||||||
| Working capital |
$ | 214,654 | $ | 241,032 | $ | 403,917 | $ | 294,878 | $ | 295,389 | ||||||||||
| Total assets |
2,337,415 | 2,022,224 | 2,181,761 | 2,079,552 | 2,016,127 | |||||||||||||||
| Long-term debt |
365,556 | 147,647 | 349,433 | 275,814 | 130,090 | |||||||||||||||
| Stockholders’ equity |
1,031,759 | 966,594 | 914,975 | 862,124 | 995,578 | |||||||||||||||
70
Table of Contents
| Item 7. | Management’s Discussion and Analysis of Financial Condition and Results of Operations |
You should read the following discussion together with the selected financial data in Item 6 and our consolidated financial statements and the notes thereto included in this Annual Report on Form 10-K. All financial and operating data presented in Items 6 and 7 reflects the continuing operations of our business for all periods presented unless otherwise indicated.
Overview
We are a healthcare services company that through our subsidiaries operates hospitals, nursing and rehabilitation centers, assisted living facilities and a contract rehabilitation services business across the United States. At December 31, 2010, our hospital division operated 89 LTAC hospitals with 6,887 licensed beds in 24 states. Our nursing center division operated 226 nursing and rehabilitation centers and seven assisted living facilities with 27,905 licensed beds in 28 states. We also operated a contract rehabilitation services business that provides rehabilitative services primarily in long-term care settings.
In recent years, we have completed several strategic divestitures to improve our future operating results. For accounting purposes, the operating results of these businesses and the losses or impairments associated with these transactions have been classified as discontinued operations in the accompanying consolidated statement of operations for all periods presented. Assets not sold at December 31, 2010 have been measured at the lower of carrying value or estimated fair value less costs of disposal and have been classified as held for sale in the accompanying consolidated balance sheet. See notes 3 and 4 of the notes to consolidated financial statements.
The operating results of acquired businesses have been included in our accompanying consolidated financial statements from the respective acquisition dates.
RehabCare Acquisition
On February 7, 2011, we entered into the Merger Agreement with RehabCare, providing for our acquisition of RehabCare, with Kindred as the surviving entity.
At December 31, 2010, RehabCare operated 29 LTAC hospitals, five inpatient rehabilitation hospitals and provided rehabilitation therapy services in 116 acute care hospitals and 1,112 skilled nursing facilities in 42 states. RehabCare reported consolidated revenues of approximately $1.3 billion and net income from continuing operations of approximately $65 million in fiscal 2010.
The Merger will form the largest post-acute healthcare services company in the United States with over $6 billion in annual revenues and operations in 46 states. The combined company will be a leading operator of LTAC hospitals, nursing and rehabilitation centers, skilled and acute care rehabilitation therapy contract services and inpatient rehabilitation facilities. This transaction, valued at approximately $1.3 billion, will further our cluster market strategy, add to our existing LTAC hospital and skilled nursing contract rehabilitation therapy businesses and expand our service offerings to include the acute care inpatient rehabilitation therapy business.
We believe that the RehabCare acquisition will be highly accretive to our earnings and cash flows, provide significant long-term strategic benefits and further enhance our future growth prospects. The RehabCare acquisition is also consistent with our strategy of developing clinical and operational expertise across the post-acute continuum of healthcare services.
At the effective time of the Merger, each share of RehabCare common stock outstanding immediately prior to the effective time (subject to certain exceptions) will be converted into the right to receive the Merger Consideration. Outstanding Kindred common stock will not be affected by the Merger. Upon completion of the transaction, RehabCare stockholders will own approximately 22% of our outstanding common stock.
71
Table of Contents
The consummation of the Merger is subject to certain conditions, including the adoption by the RehabCare and Kindred stockholders of the Merger Agreement; clearance under the Hart-Scott-Rodino Antitrust Improvements Act of 1976, as amended; receipt of certain other licensure and regulatory approvals; receipt of the proceeds of the financing described below; and other customary closing conditions.
The Merger Agreement contains customary representations, warranties and covenants, including covenants providing for each of the parties (i) to use reasonable best efforts to cause the transaction to be consummated and (ii) to call and hold a stockholders’ meeting and recommend adoption of the Merger Agreement, subject to fiduciary duties. The Merger Agreement also requires RehabCare to conduct its operations in all material respects according to the ordinary course of business consistent with past practice until the closing of the Merger. RehabCare is subject to customary “no-shop” restrictions on its ability to solicit acquisition proposals from third parties and to provide information to and engage in discussions with third parties about acquisition proposals, subject to a “fiduciary duty” exception in certain circumstances prior to adoption of the Merger Agreement by RehabCare’s stockholders.
The Merger Agreement also contains certain termination rights and provides that (i) upon termination of the Merger Agreement under specified circumstances, including a change in the recommendation of the board of directors of RehabCare or termination of the Merger Agreement to enter into a written definitive agreement for a “superior proposal,” RehabCare must pay us a termination fee of $26 million and (ii) upon the termination of the Merger Agreement under specified circumstances, including a change in the recommendation of our board of directors or our failure to complete the financing discussed below, after all other closing conditions have been met, we must pay RehabCare a cash termination fee of $62 million.
We have obtained the Commitment Letter from JPMorgan Chase Bank, N.A., J.P. Morgan Securities LLC, Morgan Stanley Senior Funding, Inc. and Citigroup Global Markets Inc. in connection with the pending transaction. These funds and existing cash balances are expected to be sufficient to fund the cash consideration to RehabCare stockholders and to refinance certain existing Kindred and RehabCare debt. Subject to certain conditions, we expect to have in place approximately $1.9 billion of long-term financing, of which approximately $1.6 billion is expected to be outstanding at the time of consummation of the pending transaction. See “Item 1A – Risk Factors – Risk Factors Relating to the RehabCare Acquisition.”
Vista Acquisition
On November 1, 2010, we completed the Vista Acquisition, which was financed with proceeds from our revolving credit facility.
The Vista Acquisition included four freestanding hospitals and one hospital-in-hospital with a total of 250 beds, all of which are located in southern California. We did not acquire the working capital of Vista or assume any of its liabilities. All of the Vista hospitals are leased.
Critical Accounting Policies
Our discussion and analysis of financial condition and results of operations are based upon our consolidated financial statements which have been prepared in accordance with accounting principles generally accepted in the United States. The preparation of these financial statements requires the use of estimates and judgments that affect the reported amounts and related disclosures of commitments and contingencies. We rely on historical experience and on various other assumptions that we believe to be reasonable under the circumstances to make judgments about the carrying values of assets and liabilities that are not readily apparent from other sources. Actual results may differ materially from these estimates.
We believe the following critical accounting policies, among others, affect the more significant judgments and estimates used in the preparation of our consolidated financial statements.
72
Table of Contents
Revenue recognition
We have agreements with third party payors that provide for payments to each of our operating divisions. These payment arrangements may be based upon prospective rates, reimbursable costs, established charges, discounted charges or per diem payments. Net patient service revenue is recorded at the estimated net realizable amounts from Medicare, Medicaid, Medicare Advantage, other third party payors and individual patients for services rendered. Retroactive adjustments that are likely to result from future examinations by third party payors are accrued on an estimated basis in the period the related services are rendered and adjusted as necessary in future periods based upon new information or final settlements.
We recorded income of approximately $8 million in 2008 related to the favorable settlement of a prior year nursing and rehabilitation center Medicaid cost report dispute.
A summary of revenues by payor type follows (in thousands):
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Medicare |
$ | 1,882,365 | $ | 1,817,117 | $ | 1,743,447 | ||||||
| Medicaid |
1,059,118 | 1,086,901 | 1,075,645 | |||||||||
| Medicare Advantage |
345,026 | 321,437 | 263,699 | |||||||||
| Other |
1,379,652 | 1,332,817 | 1,275,148 | |||||||||
| 4,666,161 | 4,558,272 | 4,357,939 | ||||||||||
| Eliminations |
(306,464 | ) | (288,265 | ) | (264,075 | ) | ||||||
| $ | 4,359,697 | $ | 4,270,007 | $ | 4,093,864 | |||||||
Collectibility of accounts receivable
Accounts receivable consist primarily of amounts due from the Medicare and Medicaid programs, other government programs, managed care health plans, commercial insurance companies and individual patients and customers. Estimated provisions for doubtful accounts are recorded to the extent it is probable that a portion or all of a particular account will not be collected.
In evaluating the collectibility of accounts receivable, we consider a number of factors, including the age of the accounts, changes in collection patterns, the composition of patient accounts by payor type, the status of ongoing disputes with third party payors and general industry conditions. Actual collections of accounts receivable in subsequent periods may require changes in the estimated provision for loss. Changes in these estimates are charged or credited to the results of operations in the period of the change.
The provision for doubtful accounts totaled $24 million for 2010, $29 million for 2009 and $31 million for 2008.
Allowances for insurance risks
We insure a substantial portion of our professional liability risks and workers compensation risks through our limited purpose insurance subsidiary. Provisions for loss for these risks are based upon management’s best available information including actuarially determined estimates.
The allowance for professional liability risks includes an estimate of the expected cost to settle reported claims and an amount, based upon past experiences, for losses incurred but not reported. These liabilities are necessarily based upon estimates and, while management believes that the provision for loss is adequate, the ultimate liability may be in excess of, or less than, the amounts recorded. To the extent that expected ultimate claims costs vary from historical provisions for loss, future earnings will be charged or credited.
73
Table of Contents
Provisions for loss for professional liability risks retained by our limited purpose insurance subsidiary have been discounted based upon actuarial estimates of claim payment patterns using a discount rate of 1% to 5% depending upon the policy year. The discount rate was 1% for the 2010 policy year, 2% for the 2009 policy year, 3% for the 2008 policy year and 5% for all prior policy years. The discount rates are based upon the risk free interest rate for the respective year. Amounts equal to the discounted loss provision are funded annually. We do not fund the portion of professional liability risks related to estimated claims that have been incurred but not reported. Accordingly, these liabilities are not discounted. The allowance for professional liability risks aggregated $249 million at December 31, 2010 and $242 million at December 31, 2009. If we did not discount any of the allowances for professional liability risks, these balances would have approximated $253 million at December 31, 2010 and $247 million at December 31, 2009.
As a result of improved professional liability underwriting results of our limited purpose insurance subsidiary, we received distributions of $22 million in 2010, $34 million in 2009 and $39 million in 2008 from our limited purpose insurance subsidiary in accordance with applicable regulations. These distributions had no impact on earnings and the proceeds were used primarily to repay borrowings under our revolving credit facility.
Changes in the number of professional liability claims and the cost to settle these claims significantly impact the allowance for professional liability risks. A relatively small variance between our estimated and actual number of claims or average cost per claim could have a material impact, either favorable or unfavorable, on the adequacy of the allowance for professional liability risks. For example, a 1% variance in the allowance for professional liability risks at December 31, 2010 would impact our operating income by approximately $2 million.
The provision for professional liability risks (continuing operations), including the cost of coverage maintained with unaffiliated commercial insurance carriers, aggregated $55 million for 2010, $48 million for 2009 and $33 million for 2008. Changes in estimates for prior year professional liability costs reduced professional liability costs by approximately $20 million, $27 million and $38 million in 2010, 2009 and 2008, respectively.
With respect to our discontinued operations, we recorded favorable pretax adjustments of $5 million in 2010, $11 million in 2009 and $10 million in 2008 resulting from changes in estimates for professional liability reserves related to prior years.
Provisions for loss for workers compensation risks retained by our limited purpose insurance subsidiary are not discounted and amounts equal to the loss provision are funded annually. The allowance for workers compensation risks aggregated $84 million at December 31, 2010 and $82 million at December 31, 2009. The provision for workers compensation risks (continuing operations), including the cost of coverage maintained with unaffiliated commercial insurance carriers, aggregated $43 million for 2010, $36 million for 2009 and $30 million for 2008.
See notes 4 and 8 of the notes to consolidated financial statements.
Accounting for income taxes
The provision for income taxes is based upon our annual reported income or loss for each respective accounting period. We recognize an asset or liability for the deferred tax consequences of temporary differences between the tax bases of assets and liabilities and their reported amounts in the financial statements. These temporary differences will result in taxable or deductible amounts in future years when the reported amounts of the assets are recovered or liabilities are settled. We also recognize as deferred tax assets the future tax benefits from net operating losses (“NOLs”) and capital loss carryforwards. A valuation allowance is provided for these deferred tax assets if it is more likely than not that some portion or all of the net deferred tax assets will not be realized.
74
Table of Contents
Our effective income tax rate was 37.5% in 2010, 38.5% in 2009 and 38.7% in 2008. We recorded favorable income tax adjustments related to the resolution of certain income tax contingencies from prior years that reduced the provision for income taxes by approximately $3 million in 2010 and approximately $2 million in each of 2009 and 2008.
There are significant uncertainties with respect to capital loss carryforwards that could affect materially the realization of certain deferred tax assets. Accordingly, we have recognized deferred tax assets to the extent it is more likely than not they will be realized and a valuation allowance is provided for deferred tax assets to the extent that it is uncertain that the deferred tax asset will be realized. We recognized net deferred tax assets totaling $102 million at December 31, 2010 and $154 million at December 31, 2009.
We identified deferred income tax assets for state income tax NOLs of $42 million and $38 million at December 31, 2010 and 2009, respectively, and a corresponding deferred income tax valuation allowance of $38 million and $34 million at December 31, 2010 and 2009, respectively, for that portion of the net deferred income tax assets that we will likely not realize in the future.
After our emergence from bankruptcy in 2001, the realization of pre-reorganization deferred tax assets and the resolution of certain income tax contingencies eliminated in full the goodwill recorded in connection with fresh-start accounting. After the fresh-start accounting goodwill was eliminated in full, the excess of approximately $1 million in 2008 was treated as an increase to capital in excess of par value and a reduction in the pre-emergence deferred tax valuation allowance and pre-emergence income tax liability.
We are subject to various federal and state income tax audits in the ordinary course of business. Such audits could result in increased tax payments, interest and penalties. While we believe our tax positions are appropriate, we cannot assure you that the various authorities engaged in the examination of our income tax returns will not challenge our positions.
We record accrued interest and penalties associated with uncertain tax positions as income tax expense in the consolidated statement of operations. Accrued interest related to uncertain tax provisions totaled $0.2 million as of December 31, 2010 and $0.1 million as of December 31, 2009.
To the extent the unrecognized income tax benefits become realized or the related accrued interest is no longer necessary, our provision for income taxes would be favorably impacted. The amount, if recognized, that would favorably impact our results of operations approximates $3 million.
The federal statute of limitations remains open for tax years 2007 through 2009 and we are currently under examination by the IRS for each of these years. See note 7 of the notes to consolidated financial statements.
State jurisdictions generally have statutes of limitations for tax returns ranging from three to five years. The state impact of federal income tax changes remains subject to examination by various states for a period of up to one year after formal notification to the states. We currently have various state income tax returns under examination.
We received approval from the IRS for an accounting method change for income tax purposes that resulted in a non-recurring reduction in income tax payments of approximately $25 million during 2010. Our earnings were not impacted by this transaction.
Valuation of long-lived assets and goodwill
We regularly review the carrying value of certain long-lived assets and identifiable finite lived intangible assets with respect to any events or circumstances that indicate an impairment or an adjustment to the amortization period is necessary. If circumstances suggest that the recorded amounts cannot be recovered based upon estimated future undiscounted cash flows, the carrying values of such assets are reduced to fair value.
75
Table of Contents
In assessing the carrying values of long-lived assets, we estimate future cash flows at the lowest level for which there are independent, identifiable cash flows. For this purpose, these cash flows are aggregated based upon the contractual agreements underlying the operation of the facility or group of facilities. Generally, an individual facility is considered the lowest level for which there are independent, identifiable cash flows. However, to the extent that groups of facilities are leased under a master lease agreement in which the operations of a facility and compliance with the lease terms are interdependent upon other facilities in the agreement (including our ability to renew the lease or divest a particular property), we define the group of facilities under a master lease agreement as the lowest level for which there are independent, identifiable cash flows. Accordingly, the estimated cash flows of all facilities within a master lease agreement are aggregated for purposes of evaluating the carrying values of long-lived assets.
Our other intangible assets with finite lives are amortized in accordance with the authoritative guidance for goodwill and other intangible assets using the straight-line method over their estimated useful lives ranging from one to 20 years.
In accordance with the authoritative guidance for goodwill and other intangible assets, we are required to perform an impairment test for goodwill and indefinite lived intangible assets at least annually or more frequently if adverse events or changes in circumstances indicate that the asset may be impaired. During 2010 and 2009, the market value of our common stock was below our book equity value. Management believes that the difference between our market equity value and our book equity during 2010 was generally attributable to uncertainty in equity markets related to certain Medicare regulatory changes that went into effect October 1, 2010 for our nursing center division and rehabilitation services division and uncertainty related to the enactment of healthcare reform legislation during 2010. Some of the uncertainty surrounding the 2010 Medicare regulatory changes and its impact on us was alleviated on December 15, 2010 when we updated earnings guidance for the fourth quarter of 2010 and provided 2011 earnings guidance for the first time. The earnings guidance, which included the impact of the regulatory changes for both periods, provided a stronger earnings outlook than expected by investors. Management believes that the difference between our market equity value and our book equity value during 2009 was generally attributable to uncertainty in the equity markets related to proposed federal healthcare reform legislation and certain Medicare revenue reductions announced by CMS during the year. The difference between the book equity value and the market value of our common stock during 2010 and 2009 was a potential indication that the carrying value of our goodwill may have been impaired but was not viewed as a triggering event.
We perform our annual goodwill impairment test at the end of each fiscal year for each of our reporting units. A reporting unit is either an operating segment or one level below the operating segment, referred to as a component. When the components within our operating segments have similar economic characteristics, we aggregate the components of our operating segments into one reporting unit. Accordingly, we have determined that our reporting units are hospitals, nursing and rehabilitation centers, rehabilitation services, home health and hospice. The carrying value of goodwill for each of our reporting units at December 31, 2010 and 2009 were as follows (in thousands):
| December 31, | ||||||||
| 2010 | 2009 | |||||||
| Hospitals |
$ | 213,200 | $ | 68,577 | ||||
| Nursing and rehabilitation centers |
6,080 | 889 | ||||||
| Rehabilitation services |
3,363 | 3,363 | ||||||
| Home health |
11,383 | – | ||||||
| Hospice |
8,394 | 8,394 | ||||||
| $ | 242,420 | $ | 81,223 | |||||
76
Table of Contents
The goodwill impairment test involves a two-step process. The first step is a comparison of each reporting unit’s fair value to its carrying value. If the carrying value of the reporting unit is greater than its fair value, there is an indication that impairment may exist and the second step must be performed to measure the amount of impairment loss. Based upon the results of the step one impairment test for goodwill and the impairment test of indefinite lived intangible assets in each of the last three years, no impairment charges were recorded in connection with our annual impairment tests.
Since quoted market prices for our reporting units are not available, we applied judgment in determining the fair value of these reporting units for purposes of performing the goodwill impairment test. We relied on widely accepted valuation techniques, including equally weighted discounted cash flow and market multiple analyses approaches, which capture both the future income potential of the reporting unit and the market behaviors and actions of market participants in the industry that includes the reporting unit. These types of analyses require us to make assumptions and estimates regarding future cash flows, industry-specific economic factors and the profitability of future business strategies. The discounted cash flow approach uses a projection of estimated operating results and cash flows that are discounted using a weighted average cost of capital. Under the discounted cash flow approach, the projection uses management’s best estimates of economic and market conditions over the projected period for each reporting unit including growth rates in the number of admissions, patient days, reimbursement rates, operating costs, rent expense and capital expenditures. Other significant estimates and assumptions include terminal value growth rates, changes in working capital requirements and weighted average cost of capital. The market multiple analysis estimates fair value by applying cash flow multiples to the reporting unit’s operating results. The multiples are derived from comparable publicly traded companies with similar operating and investment characteristics to the reporting units.
Our analysis indicated that the estimated fair value of each reporting unit exceeded its book equity value. Our conclusions were supported by both quantitative and qualitative factors, including the estimate of an implied control premium for acquisitions in our industry, our fourth quarter operating results that exceeded investment analyst expectations and consideration of our updated business expectations at December 31, 2010 and 2009. We do not believe that any of our reporting units were at risk for failing the step one impairment test at December 31, 2010.
Our indefinite lived intangible assets consist primarily of certificates of need, which are estimated primarily using an excess earnings method, a form of discounted cash flows, which is based upon the concept that net after-tax cash flows provide a return supporting all of the assets of a business enterprise. The carrying value of our certificates of need at December 31, 2010 was $66 million. The fair values of our indefinite lived intangible assets are derived from current market data and projections at a facility level which include management’s best estimates of economic and market conditions over the projected period including growth rates in the number of admissions, patient days, reimbursement rates, operating costs, rent expense and capital expenditures. Other significant estimates and assumptions include terminal value growth rates, changes in working capital requirements and weighted average cost of capital. At December 31, 2010, the fair value of our certificates of need intangible assets exceeded its carrying value. We do not believe that any of our certificates of need were at risk for failing the impairment test at December 31, 2010. In conjunction with two acquisitions consummated in November 2010, we also acquired Medicare certifications with indefinite lives totaling $18 million. However, an impairment analysis was not conducted because there were no triggering events between the acquisition dates and December 31, 2010. See note 2 of the notes to consolidated financial statements.
Although we have determined that there was no goodwill or other indefinite lived intangible asset impairments as of December 31, 2010, adverse changes in the operating environment and related key assumptions used to determine the fair value of our reporting units and indefinite lived intangible assets or declines in the value of our common stock may result in future impairment charges for a portion or all of these assets. Specifically, if the rate of growth of government and commercial revenues earned by our reporting units were to be less than projected or if healthcare reforms were to negatively impact our business, an impairment
77
Table of Contents
charge for a portion or all of the assets may be required. An impairment charge could have a material adverse effect on our business, financial position and results of operations, but would not be expected to have an impact on our cash flows or liquidity.
Recently Issued Accounting Requirements
In December 2010, the Financial Accounting Standards Board (the “FASB”) issued authoritative guidance related to goodwill and other intangibles. The provisions of the guidance modify Step 1 of the goodwill impairment test for reporting units with zero or negative carrying amounts. For those reporting units, an entity is required to perform Step 2 of the goodwill impairment test if it is more likely than not that a goodwill impairment exists. In determining if it is more likely than not that a goodwill impairment exists, an entity should consider whether there are any adverse qualitative factors indicating that an impairment may exist. The guidance is effective for all interim and annual reporting periods beginning after December 15, 2010. The adoption of the guidance is not expected to have a material impact on our business, financial position, results of operations or liquidity.
In December 2010, the FASB issued authoritative guidance related to business combinations. The provisions of the guidance specify that if a public entity presents comparative financial statements, the entity should disclose revenue and earnings of the combined entity as though the business combination(s) that occurred during the current year had occurred as of the beginning of the comparable prior year annual reporting period only. Supplemental pro forma disclosures have also been expanded to include a description of the nature and amount of material, non-recurring pro forma adjustments included in the pro forma financial statements. The guidance is effective prospectively for business combinations with an acquisition date on or after the beginning of the first annual reporting period beginning on or after December 15, 2010. The adoption of the guidance is not expected to have a material impact on our business, financial position, results of operations or liquidity.
In January 2010, the FASB issued authoritative guidance related to fair value measurements and disclosures. The provisions of the guidance require new disclosures related to transfers in and out of Levels 1 and 2 classifications (as described in note 16 of the notes to consolidated financial statements). The provisions also require a reconciliation of the activity in Level 3 (as described in note 16 of the notes to consolidated financial statements) recurring fair value measurements. Existing disclosures also were expanded to include Level 2 fair value measurement valuation techniques and inputs. The guidance is effective for all interim and annual reporting periods beginning after December 15, 2009, except for the disclosures for Level 3 activity which is effective for fiscal years beginning after December 15, 2010. The adoption of the guidance did not, and is not expected to, have a material impact on our business, financial position, results of operations or liquidity.
In June 2009, the FASB issued revised authoritative guidance related to the consolidation criteria for variable interest entities (“VIE”). The guidance, among other things, requires a qualitative rather than a quantitative analysis to determine the primary beneficiary of a VIE; requires continuous assessments of whether an enterprise is the primary beneficiary of a VIE; enhances disclosures regarding an enterprise’s involvement with a VIE; and amends certain guidance for determining whether an entity is a VIE. Under the guidance, a VIE must be consolidated if the enterprise has both (a) the power to direct the activities of the VIE that most significantly impact the entity’s economic performance, and (b) the obligation to absorb losses or the right to receive benefits from the VIE that could potentially be significant to the VIE. The guidance was effective as of January 1, 2010. The adoption of the guidance did not, and is not expected to, have a material impact on our business, financial position, results of operations or liquidity.
Upon adoption of the VIE guidance on January 1, 2010, we reassessed our three investment partnerships and lease agreements under the new accounting guidance. Although the investment partnerships were determined to be VIEs, they do not require us to absorb losses or receive benefits that could potentially be significant to the VIEs, nor can we direct the activities that most significantly impact the VIEs’ economic performance. As a
78
Table of Contents
result, the investment partnerships continue to be accounted for under the equity method of accounting and are not consolidated. We also determined that three of our lease agreements were considered VIEs. However, we are not the primary beneficiary of these leases as we lack the power to direct activities of the lessor that most significantly impact the economic performance under these leases. In addition, our investments and involvement in lease arrangements related to these VIEs were not significant to our consolidated financial statements.
Impact of Medicare and Medicaid Reimbursement
We depend on reimbursement from third party payors, including the Medicare and Medicaid programs, for a substantial portion of our revenues. For the year ended December 31, 2010, we derived approximately 63% of our total revenues (before eliminations) from the Medicare and Medicaid programs and the balance from other third party payors, such as commercial insurance companies, health maintenance organizations, preferred provider organizations and contracted providers.
The Medicare and Medicaid programs are highly regulated and subject to frequent and substantial changes. See “Part I – Item 1 – Business – Governmental Regulation” for an overview of the reimbursement systems impacting our businesses and “Part I – Item 1A – Risk Factors.”
Results of Operations – Continuing Operations
For the years ended December 31, 2010, 2009 and 2008
A summary of our operating data follows (dollars in thousands, except statistics):
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Revenues: |
||||||||||||
| Hospital division |
$ | 1,973,321 | $ | 1,932,892 | $ | 1,837,322 | ||||||
| Nursing center division |
2,187,885 | 2,150,342 | 2,093,297 | |||||||||
| Rehabilitation division |
504,955 | 475,038 | 427,320 | |||||||||
| 4,666,161 | 4,558,272 | 4,357,939 | ||||||||||
| Eliminations |
(306,464 | ) | (288,265 | ) | (264,075 | ) | ||||||
| $ | 4,359,697 | $ | 4,270,007 | $ | 4,093,864 | |||||||
| Income from continuing operations: |
||||||||||||
| Operating income (loss): |
||||||||||||
| Hospital division |
$ | 357,100 | $ | 363,811 | $ | 345,367 | ||||||
| Nursing center division |
302,672 | 305,590 | 321,814 | |||||||||
| Rehabilitation division |
51,923 | 50,592 | 38,071 | |||||||||
| Corporate: |
||||||||||||
| Overhead |
(133,919 | ) | (134,636 | ) | (133,019 | ) | ||||||
| Insurance subsidiary |
(3,153 | ) | (6,185 | ) | (6,657 | ) | ||||||
| (137,072 | ) | (140,821 | ) | (139,676 | ) | |||||||
| Operating income |
574,623 | 579,172 | 565,576 | |||||||||
| Rent |
(357,372 | ) | (348,248 | ) | (338,673 | ) | ||||||
| Depreciation and amortization |
(121,552 | ) | (125,730 | ) | (120,022 | ) | ||||||
| Interest, net |
(5,845 | ) | (3,467 | ) | (8,277 | ) | ||||||
| Income from continuing operations before income taxes |
89,854 | 101,727 | 98,604 | |||||||||
| Provision for income taxes |
33,708 | 39,115 | 38,144 | |||||||||
| $ | 56,146 | $ | 62,612 | $ | 60,460 | |||||||
79
Table of Contents
A summary of our consolidating statement of operations follows (in thousands):
| Year ended December 31, 2010 | ||||||||||||||||||||||||
| Hospital division |
Nursing center division |
Rehabilitation division |
Corporate | Eliminations | Consolidated | |||||||||||||||||||
| Revenues |
$ | 1,973,321 | $ | 2,187,885 | $ | 504,955 | $ | – | $ | (306,464 | ) | $ | 4,359,697 | |||||||||||
| Salaries, wages and benefits |
894,702 | 1,080,344 | 431,224 | 99,480 | (60 | ) | 2,505,690 | |||||||||||||||||
| Supplies |
228,157 | 110,266 | 3,217 | 557 | – | 342,197 | ||||||||||||||||||
| Rent |
152,986 | 198,105 | 6,136 | 145 | – | 357,372 | ||||||||||||||||||
| Other operating expenses |
493,362 | 694,603 | 18,591 | 48,457 | (306,404 | ) | 948,609 | |||||||||||||||||
| Other income |
– | – | – | (11,422 | ) | – | (11,422 | ) | ||||||||||||||||
| Depreciation and amortization |
51,639 | 45,471 | 2,709 | 21,733 | – | 121,552 | ||||||||||||||||||
| Interest expense |
5 | 131 | – | 6,954 | – | 7,090 | ||||||||||||||||||
| Investment income |
(3 | ) | (70 | ) | (6 | ) | (1,166 | ) | – | (1,245 | ) | |||||||||||||
| 1,820,848 | 2,128,850 | 461,871 | 164,738 | (306,464 | ) | 4,269,843 | ||||||||||||||||||
| Income from continuing operations before income taxes |
$ | 152,473 | $ | 59,035 | $ | 43,084 | $ | (164,738 | ) | $ | – | 89,854 | ||||||||||||
| Provision for income taxes |
33,708 | |||||||||||||||||||||||
| Income from continuing operations |
$ | 56,146 | ||||||||||||||||||||||
| Capital expenditures, excluding acquisitions (including discontinued operations): |
||||||||||||||||||||||||
| Routine |
$ | 36,967 | $ | 37,024 | $ | 2,715 | $ | 32,190 | $ | – | $ | 108,896 | ||||||||||||
| Development |
41,140 | 26,701 | – | – | – | 67,841 | ||||||||||||||||||
| $ | 78,107 | $ | 63,725 | $ | 2,715 | $ | 32,190 | $ | – | $ | 176,737 | |||||||||||||
80
Table of Contents
Consolidating statement of operations (in thousands) (Continued):
| Year ended December 31, 2009 | ||||||||||||||||||||||||
| Hospital division |
Nursing center division |
Rehabilitation division |
Corporate | Eliminations | Consolidated | |||||||||||||||||||
| Revenues |
$ | 1,932,892 | $ | 2,150,342 | $ | 475,038 | $ | – | $ | (288,265 | ) | $ | 4,270,007 | |||||||||||
| Salaries, wages and benefits |
875,788 | 1,102,975 | 402,986 | 101,337 | – | 2,483,086 | ||||||||||||||||||
| Supplies |
221,529 | 108,038 | 2,827 | 664 | (2 | ) | 333,056 | |||||||||||||||||
| Rent |
147,494 | 194,835 | 5,778 | 141 | – | 348,248 | ||||||||||||||||||
| Other operating expenses |
471,764 | 633,739 | 18,633 | 50,332 | (288,263 | ) | 886,205 | |||||||||||||||||
| Other income |
– | – | – | (11,512 | ) | – | (11,512 | ) | ||||||||||||||||
| Depreciation and amortization |
51,932 | 48,631 | 2,291 | 22,876 | – | 125,730 | ||||||||||||||||||
| Interest expense |
2 | 130 | 1 | 7,747 | – | 7,880 | ||||||||||||||||||
| Investment income |
(7 | ) | (111 | ) | (8 | ) | (4,287 | ) | – | (4,413 | ) | |||||||||||||
| 1,768,502 | 2,088,237 | 432,508 | 167,298 | (288,265 | ) | 4,168,280 | ||||||||||||||||||
| Income from continuing operations before income taxes |
$ | 164,390 | $ | 62,105 | $ | 42,530 | $ | (167,298 | ) | $ | – | 101,727 | ||||||||||||
| Provision for income taxes |
39,115 | |||||||||||||||||||||||
| Income from continuing operations |
$ | 62,612 | ||||||||||||||||||||||
| Capital expenditures, excluding acquisitions (including discontinued operations): |
||||||||||||||||||||||||
| Routine |
$ | 26,716 | $ | 39,663 | $ | 1,043 | $ | 30,128 | $ | – | $ | 97,550 | ||||||||||||
| Development |
42,371 | 5,687 | – | – | – | 48,058 | ||||||||||||||||||
| $ | 69,087 | $ | 45,350 | $ | 1,043 | $ | 30,128 | $ | – | $ | 145,608 | |||||||||||||
81
Table of Contents
Consolidating statement of operations (in thousands) (Continued):
| Year ended December 31, 2008 | ||||||||||||||||||||||||
| Hospital division |
Nursing center division |
Rehabilitation division |
Corporate | Eliminations | Consolidated | |||||||||||||||||||
| Revenues |
$ | 1,837,322 | $ | 2,093,297 | $ | 427,320 | $ | – | $ | (264,075 | ) | $ | 4,093,864 | |||||||||||
| Salaries, wages and benefits |
842,018 | 1,068,648 | 371,248 | 92,249 | – | 2,374,163 | ||||||||||||||||||
| Supplies |
210,962 | 103,626 | 1,744 | 821 | (4 | ) | 317,149 | |||||||||||||||||
| Rent |
146,316 | 186,612 | 5,555 | 190 | – | 338,673 | ||||||||||||||||||
| Other operating expenses |
438,975 | 599,209 | 16,257 | 64,013 | (264,071 | ) | 854,383 | |||||||||||||||||
| Other income |
– | – | – | (17,407 | ) | – | (17,407 | ) | ||||||||||||||||
| Depreciation and amortization |
48,150 | 48,645 | 1,965 | 21,262 | – | 120,022 | ||||||||||||||||||
| Interest expense |
326 | 133 | – | 14,914 | – | 15,373 | ||||||||||||||||||
| Investment income |
(43 | ) | (160 | ) | (48 | ) | (6,845 | ) | – | (7,096 | ) | |||||||||||||
| 1,686,704 | 2,006,713 | 396,721 | 169,197 | (264,075 | ) | 3,995,260 | ||||||||||||||||||
| Income from continuing operations before income taxes |
$ | 150,618 | $ | 86,584 | $ | 30,599 | $ | (169,197 | ) | $ | – | 98,604 | ||||||||||||
| Provision for income taxes |
38,144 | |||||||||||||||||||||||
| Income from continuing operations |
$ | 60,460 | ||||||||||||||||||||||
| Capital expenditures, excluding acquisitions (including discontinued operations): |
||||||||||||||||||||||||
| Routine |
$ | 35,932 | $ | 44,627 | $ | 1,162 | $ | 28,205 | $ | – | $ | 109,926 | ||||||||||||
| Development |
33,285 | 5,466 | – | – | – | 38,751 | ||||||||||||||||||
| $ | 69,217 | $ | 50,093 | $ | 1,162 | $ | 28,205 | $ | – | $ | 148,677 | |||||||||||||
82
Table of Contents
Operating data:
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Hospital data: |
||||||||||||
| End of period data: |
||||||||||||
| Number of hospitals |
89 | 83 | 82 | |||||||||
| Number of licensed beds |
6,887 | 6,580 | 6,482 | |||||||||
| Revenue mix %: |
||||||||||||
| Medicare |
56 | 55 | 55 | |||||||||
| Medicaid |
9 | 10 | 10 | |||||||||
| Medicare Advantage |
10 | 10 | 9 | |||||||||
| Commercial insurance and other |
25 | 25 | 26 | |||||||||
| Admissions: |
||||||||||||
| Medicare |
28,966 | 28,696 | 29,028 | |||||||||
| Medicaid |
4,043 | 4,254 | 4,233 | |||||||||
| Medicare Advantage |
4,242 | 4,030 | 3,587 | |||||||||
| Commercial insurance and other |
8,308 | 8,039 | 7,088 | |||||||||
| 45,559 | 45,019 | 43,936 | ||||||||||
| Admissions mix %: |
||||||||||||
| Medicare |
64 | 64 | 66 | |||||||||
| Medicaid |
9 | 9 | 10 | |||||||||
| Medicare Advantage |
9 | 9 | 8 | |||||||||
| Commercial insurance and other |
18 | 18 | 16 | |||||||||
| Patient days: |
||||||||||||
| Medicare |
776,299 | 779,359 | 806,427 | |||||||||
| Medicaid |
188,875 | 202,290 | 208,423 | |||||||||
| Medicare Advantage |
134,578 | 132,262 | 117,945 | |||||||||
| Commercial insurance and other |
285,917 | 267,439 | 262,254 | |||||||||
| 1,385,669 | 1,381,350 | 1,395,049 | ||||||||||
| Average length of stay: |
||||||||||||
| Medicare |
26.8 | 27.2 | 27.8 | |||||||||
| Medicaid |
46.7 | 47.6 | 49.2 | |||||||||
| Medicare Advantage |
31.7 | 32.8 | 32.9 | |||||||||
| Commercial insurance and other |
34.4 | 33.3 | 37.0 | |||||||||
| Weighted average |
30.4 | 30.7 | 31.8 | |||||||||
| Revenues per admission: |
||||||||||||
| Medicare |
$ | 38,272 | $ | 37,436 | $ | 35,127 | ||||||
| Medicaid |
43,266 | 44,465 | 43,816 | |||||||||
| Medicare Advantage |
45,979 | 47,141 | 45,148 | |||||||||
| Commercial insurance and other |
59,553 | 59,647 | 66,345 | |||||||||
| Weighted average |
43,313 | 42,935 | 41,818 | |||||||||
| Revenues per patient day: |
||||||||||||
| Medicare |
$ | 1,428 | $ | 1,378 | $ | 1,264 | ||||||
| Medicaid |
926 | 935 | 890 | |||||||||
| Medicare Advantage |
1,449 | 1,436 | 1,373 | |||||||||
| Commercial insurance and other |
1,730 | 1,793 | 1,793 | |||||||||
| Weighted average |
1,424 | 1,399 | 1,317 | |||||||||
| Medicare case mix index (discharged patients only) |
1.19 | 1.21 | 1.15 | |||||||||
| Average daily census |
3,796 | 3,785 | 3,812 | |||||||||
| Occupancy % |
65.1 | 64.7 | 64.8 | |||||||||
| Annualized employee turnover % |
22.0 | 22.1 | 25.2 | |||||||||
83
Table of Contents
Operating data (Continued):
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Nursing and rehabilitation center data: |
||||||||||||
| End of period data: |
||||||||||||
| Number of facilities: |
||||||||||||
| Nursing and rehabilitation centers: |
||||||||||||
| Owned or leased |
222 | 218 | 218 | |||||||||
| Managed |
4 | 4 | 4 | |||||||||
| Assisted living facilities |
7 | 6 | 6 | |||||||||
| 233 | 228 | 228 | ||||||||||
| Number of licensed beds: |
||||||||||||
| Nursing and rehabilitation centers: |
||||||||||||
| Owned or leased |
26,957 | 26,711 | 26,935 | |||||||||
| Managed |
485 | 485 | 485 | |||||||||
| Assisted living facilities |
463 | 327 | 317 | |||||||||
| 27,905 | 27,523 | 27,737 | ||||||||||
| Revenue mix %: |
||||||||||||
| Medicare |
35 | 34 | 34 | |||||||||
| Medicaid |
40 | 42 | 43 | |||||||||
| Medicare Advantage |
7 | 6 | 5 | |||||||||
| Private and other |
18 | 18 | 18 | |||||||||
| Patient days (a): |
||||||||||||
| Medicare |
1,423,106 | 1,463,445 | 1,523,090 | |||||||||
| Medicaid |
5,182,145 | 5,375,605 | 5,466,653 | |||||||||
| Medicare Advantage |
365,722 | 333,775 | 272,517 | |||||||||
| Private and other |
1,704,241 | 1,637,463 | 1,659,338 | |||||||||
| 8,675,214 | 8,810,288 | 8,921,598 | ||||||||||
| Patient day mix %: |
||||||||||||
| Medicare |
16 | 17 | 17 | |||||||||
| Medicaid |
60 | 61 | 61 | |||||||||
| Medicare Advantage |
4 | 4 | 3 | |||||||||
| Private and other |
20 | 18 | 19 | |||||||||
| Revenues per patient day: |
||||||||||||
| Medicare Part A |
$ | 485 | $ | 461 | $ | 437 | ||||||
| Total Medicare (including Part B) |
533 | 503 | 474 | |||||||||
| Medicaid |
170 | 167 | 163 | |||||||||
| Medicare Advantage |
409 | 394 | 373 | |||||||||
| Private and other |
233 | 235 | 229 | |||||||||
| Weighted average |
252 | 244 | 235 | |||||||||
| Average daily census |
23,768 | 24,138 | 24,376 | |||||||||
| Admissions (a) |
76,451 | 72,801 | 69,986 | |||||||||
| Occupancy % |
87.4 | 89.0 | 89.1 | |||||||||
| Medicare average length of stay |
34.0 | 35.4 | 35.5 | |||||||||
| Annualized employee turnover % |
39.6 | 38.9 | 48.9 | |||||||||
| Rehabilitation data: |
||||||||||||
| Revenue mix %: |
||||||||||||
| Company-operated |
61 | 61 | 63 | |||||||||
| Non-affiliated |
39 | 39 | 37 | |||||||||
| Sites of service (at end of period) |
696 | 622 | 655 | |||||||||
| Revenue per site |
$ | 777,069 | $ | 730,345 | $ | 651,895 | ||||||
| Therapist productivity % |
82.0 | 84.2 | 81.4 | |||||||||
| Annualized employee turnover % |
14.4 | 12.8 | 13.3 | |||||||||
| (a) | Excludes managed facilities. |
84
Table of Contents
The Year in Review
Fiscal 2010 was a year of significant transition and change, including the enactment of landmark legislation related to national healthcare policy and reform. While many of the provisions of healthcare reform will become effective several years in the future, it has prompted many discussions in our local markets between short-term acute care hospitals, post-acute providers, managed care plans, physicians and others to begin to address potential changes in healthcare delivery that the marketplace will demand.
Revenues in 2010 increased 2% to $4.4 billion, while income from continuing operations declined 10% to $56 million, or $1.42 per diluted share, from $63 million or $1.60 per diluted share in 2009. Despite a decline in earnings, we reported robust operating cash flows in excess of $200 million for the second consecutive year. More importantly, we achieved a number of operational, development and financial goals that have positioned us for earnings growth in 2011 and beyond.
We entered 2010 with the expectation of reduced earnings prompted by volume weakness in our two major divisions and reimbursement rate pressures from both federal and state programs as well as commercial payors and managed care plans. The confluence of both rate and volume pressure required a more intense focus on cost management and efficiencies at every level of the organization. Despite several operational challenges during the year, we did not waiver from our strategic operational and growth plan centered on improving our quality, taking care of our people, pursuing operational efficiencies, maximizing our operating cash flows and continued execution of our cluster market strategy.
We also entered the year facing significant regulatory changes that would become effective in the fourth quarter. In our nursing and rehabilitation centers, significant changes in the Medicare patient classification system known as “RUGs IV” and related changes in patient clinical data collection (“MDS 3.0”) required extensive planning, training and infrastructure investments across the organization. In our Peoplefirst rehabilitation therapy business, Medicare-related changes in billing for concurrent therapy services posed significant clinical and operational challenges that would affect the profitability of the rehabilitation services business as well as the operational results of our affiliated and unaffiliated nursing center clients.
Our fourth quarter transition to the new rules for RUGs IV, MDS 3.0 and concurrent therapy was successful from both a clinical and operational perspective. While we are in the early stages of these Medicare reimbursement policy changes, we believe that we are properly positioned to provide higher levels of care to medically complex patients who require more nursing, rehabilitation therapy and other ancillary services. Our successful transition resulted from outstanding clinical and operational leadership and collaboration across our lines of business that showed the strength of our organization and its ability to adapt rapidly to change. Our fourth quarter consolidated operating results were significantly higher than the same period in 2009, bolstering our expectations for further growth in fiscal 2011.
Our acquisition and development program produced four transactions in 2010 that furthered our cluster market strategy. These acquisitions included five LTAC hospitals in southern California, three nursing and rehabilitation centers in the Dallas/Fort Worth market, a combined nursing and rehabilitation center and assisted living facility in Cleveland, Ohio and a home health operation in central Ohio, each of which should provide additional earnings growth going forward.
RehabCare acquisition
On February 8, 2011, we announced an agreement to acquire RehabCare to form the largest post-acute healthcare services company in the United States with over $6 billion in annual revenues and operations in 46 states. The combined company will be a leading operator of LTAC hospitals, nursing and rehabilitation centers, skilled and acute care rehabilitation therapy contract services and inpatient rehabilitation facilities. This transaction, valued at approximately $1.3 billion, will further our cluster market strategy, add to our existing LTAC hospital and skilled nursing contract rehabilitation therapy businesses and expand our service offerings to include the acute care inpatient rehabilitation therapy business.
85
Table of Contents
Hospital division
Revenues increased 2% in 2010 to $2.0 billion and 5% in 2009 to $1.9 billion. During each of the past two years, revenue growth was primarily a result of increases in admissions, ongoing development of new hospitals and increases in Medicare reimbursement rates. For the year ended December 31, 2010, the Vista Acquisition contributed $24 million in revenues.
Aggregate admissions increased 1% in 2010 and 2% in 2009. On a same-facility basis, aggregate admissions were relatively unchanged in 2010 and rose 3% in 2009. Medicare same-facility admissions declined 1% in each of 2010 and 2009, while non-government same-facility admissions increased 3% and 14% in the respective periods.
Hospital operating margins were 18.1% in 2010 compared to 18.8% in both 2009 and 2008. Despite sluggish admission volumes in 2010, low wage rate growth and changes to employee benefit programs stabilized overall compensation costs as a percentage of revenues at 45% for both 2010 and 2009. However, growth in physician service costs and professional liability costs lead to an operating margin decline in 2010. Physician service costs rose 10% to $34 million in 2010 while professional liability costs grew 29% to $27 million in 2010.
Average hourly wage rates were relatively unchanged in 2010 and rose 2% in 2009 compared to the previous year. As a result of certain plan changes in 2010, employee benefit costs increased 1% in 2010 following a 7% increase in 2009 compared to 2008.
Nursing center division
Revenues increased 2% in 2010 and 3% in 2009. Revenue growth in each of the past two years was primarily attributable to reimbursement rate increases that reflected both inflationary adjustments and higher patient acuity levels. Revenues for 2008 included pretax income of approximately $8 million related to the favorable settlement of a prior year nursing and rehabilitation center Medicaid cost report dispute.
On a same-facility basis, nursing center admissions increased 4% in 2010 and 3% in 2009 compared to prior periods, while same-facility patient days declined 2% in 2010 and 1% in 2009 compared to prior periods as a result of declines in average length of stay.
Nursing center operating margins were 13.8% in 2010 compared to 14.2% in 2009 and 15.4% in 2008. While we have generally executed well in our strategy to attract higher acuity Medicare and managed care (including Medicare Advantage) patients, increases in rehabilitation therapy and pharmacy costs have reduced our operating margins. Rehabilitation therapy and pharmacy costs rose 5% to $315 million in 2010 and 7% to $300 million in 2009. In addition, Medicaid rate pressures in many states also have contributed to lower operating margins.
During 2010, we outsourced certain facility maintenance functions which resulted in a decline of approximately $24 million in salaries, wages and benefits costs and a corresponding increase in other operating expenses. Average hourly wage rates increased 3% in 2010 and 2% in 2009 compared to the previous year. As a result of certain plan changes in 2010, employee benefit costs declined 3% in 2010 following an 8% increase in 2009 compared to 2008.
86
Table of Contents
Rehabilitation division
Revenues increased 6% to $505 million in 2010 and 11% to $475 million in 2009. The increase in revenues was primarily attributable to growth in new customers in 2010, and the volume of services provided to existing customers in both 2010 and 2009. Revenues derived from non-affiliated customers aggregated $199 million in 2010, $187 million in 2009 and $158 million in 2008.
During 2010, the division added 108 new non-affiliated rehabilitation services contracts with annualized revenues of approximately $52 million. During 2009 and 2008, the division added 54 and 59 new non-affiliated contracts, respectively.
Operating margins declined to 10.3% in 2010 from 10.7% in 2009, primarily as a result of the Medicare-related changes in billing for concurrent therapy services which became effective on October 1, 2010. Operating margins in 2009 increased from 8.9% in 2008, primarily due to improvements in labor productivity levels and the volume of services provided to existing customers. Management believes that rehabilitation therapy operating margins will decline in 2011 primarily as a result of the Medicare concurrent therapy rule changes that became effective in the fourth quarter of 2010.
Corporate overhead
Operating income for our operating divisions excludes allocations of corporate overhead. These costs aggregated $134 million in 2010, $135 million in 2009 and $133 million in 2008. As a percentage of consolidated revenues, corporate overhead totaled 3.1% in 2010, 3.2% in 2009 and 3.2% in 2008. Corporate overhead in 2010 included approximately $1 million related to retirement costs.
We recorded approximately $11 million in each of 2010 and 2009 and $17 million in 2008 in other income related to the information systems and transition services agreements with PharMerica.
Capital costs
Rent expense increased 3% to $357 million in 2010 and 3% to $348 million in 2009. The increase in rent expense in both periods resulted primarily from contractual inflation and contingent rent increases.
Depreciation and amortization expense was $122 million in 2010, $126 million in 2009 and $120 million in 2008. The decrease in 2010 was primarily the result of an increasing number of older assets becoming fully depreciated. The increase in 2009 was primarily a result of our ongoing capital expenditure program and hospital development projects.
Interest expense aggregated $7 million in 2010 compared to $8 million in 2009 and $15 million in 2008. The decrease in 2010 and 2009 was primarily attributable to lower interest rates and lower average borrowing levels under our revolving credit facility compared to 2008.
Investment income related primarily to our insurance subsidiary investments totaled $1 million in 2010 compared to $5 million in 2009 and $7 million in 2008. Investment income in all three years was negatively impacted by declining investment yields and by pretax other-than-temporary impairments of investments of approximately $1 million, $0.4 million and $2 million for 2010, 2009 and 2008, respectively, held in our insurance subsidiary investment portfolio.
Income taxes
The provision for income taxes is based upon our annual reported income or loss for each respective accounting period and includes the effect of certain non-taxable and non-deductible items. Our effective income tax rate was 37.5% in 2010, 38.5% in 2009 and 38.7% in 2008. We recorded favorable income tax adjustments related to the resolution of state income tax contingencies from prior years that reduced the provision for income taxes by approximately $3 million in 2010 and approximately $2 million in each of 2009 and 2008.
87
Table of Contents
Consolidated results
Income from continuing operations before income taxes declined 12% to $90 million in 2010 and increased 3% to $102 million in 2009 from $99 million in 2008. Income from continuing operations declined 10% to $56 million in 2010 from $63 million in 2009 and increased 4% in 2009 from $60 million in 2008.
Results of Operations – Discontinued Operations
Income from discontinued operations was $1 million in each of 2010 and 2009 compared to a loss from discontinued operations of $3 million in 2008. Discontinued operations included favorable pretax adjustments of $5 million ($3 million net of income taxes) in 2010, $11 million ($7 million net of income taxes) in 2009 and $10 million ($6 million net of income taxes) in 2008 resulting from changes in estimates for professional liability reserves related to prior years.
We recorded a pretax loss on divestiture of operations of $0.7 million ($0.4 million net of income taxes) during 2010 related to assets held for sale. We recorded a pretax loss on divestiture of operations of $39 million ($24 million net of income taxes) during 2009 related to the planned divestiture of the Nursing Centers. We recorded a pretax loss on divestiture of operations of $44 million ($27 million net of income taxes) during 2008 related to the planned divestiture of two LTAC hospitals. We recorded a pretax gain on divestiture of operations of $10 million ($6 million net of income taxes) during 2008 related to the sale of three previously leased facilities purchased for resale from Ventas in 2007.
See notes 3, 4 and 8 of the notes to consolidated financial statements.
Liquidity
Operating cash flows and capital expenditures
Cash flows provided by operations (including discontinued operations) aggregated $210 million for 2010, $234 million for 2009 and $172 million for 2008. During each year, we maintained sufficient liquidity to finance our routine capital expenditures, our ongoing development programs, and our acquisition and strategic divestiture activities.
Fluctuations in operating cash flows during the past three years were primarily attributable to changes in accounts receivable collections and the timing of income tax payments. Income tax payments were favorably impacted by realized losses on sales of discontinued operations and a tax accounting method change approved by the IRS in 2010. Our operating cash flows in each of the last three years exceeded our routine and development capital spending.
We utilize our revolving credit facility to meet working capital needs and finance our acquisition and development programs. As a result, we typically carry minimal amounts of cash on our consolidated balance sheet. Based upon our expected operating cash flows, the availability of borrowings under our revolving credit facility ($235 million at December 31, 2010) and the Commitment Letter, we believe that we have the necessary financial resources to satisfy our expected short-term and long-term liquidity needs.
Revolving credit facility and financing activities
During 2010, we amended our revolving credit facility to (i) increase the aggregate amount of the credit from $500 million to $600 million and (ii) increase the amount permitted for acquisitions and certain investments by $250 million. The term of our revolving credit facility expires in July 2012. See “Item 1A – Risk Factors – Risk Factors Relating to Our Capital and Liquidity.”
Interest rates under our revolving credit facility are based, at our option, upon (a) LIBOR plus the applicable margin or (b) the applicable margin plus the higher of the prime rate or 0.5% over the federal funds rate. Our revolving credit facility is collateralized by substantially all of our assets including certain owned real property
88
Table of Contents
and is guaranteed by substantially all of our subsidiaries. The terms of our revolving credit facility include a certain defined fixed payment ratio covenant and covenants which limit acquisitions and annual capital expenditures. We were in compliance with the terms of our revolving credit facility at December 31, 2010.
Despite the instability within the financial markets both nationally and globally, we have not experienced any individual lender limitations to extend credit under our revolving credit facility. However, the obligations of each of the lending institutions in our revolving credit facility are separate and the availability of future borrowings under our revolving credit facility could be impacted by further volatility and disruptions in the financial credit markets or other events, including the bankruptcy of a lending institution. At December 31, 2008, we maintained significant excess cash balances in the event that one or more of our lenders was unable to extend credit under our revolving credit facility.
We have obtained the Commitment Letter from JPMorgan Chase Bank, N.A., J.P. Morgan Securities LLC, Morgan Stanley Senior Funding, Inc. and Citigroup Global Markets Inc. in connection with the pending RehabCare acquisition. These funds and existing cash balances are expected to be sufficient to fund the cash consideration to RehabCare stockholders and to refinance certain existing Kindred and RehabCare debt. Subject to certain conditions, we expect to have in place approximately $1.9 billion of long-term financing, of which approximately $1.6 billion is expected to be outstanding at the time of consummation of the pending acquisition.
As a result of improved professional liability underwriting results of our limited purpose insurance subsidiary, we received distributions of $22 million in 2010, $34 million in 2009 and $39 million in 2008 from our limited purpose insurance subsidiary in accordance with applicable regulations. These distributions had no impact on earnings and the proceeds were used primarily to repay borrowings under our revolving credit facility.
Debt and lease obligations
Future payments of principal and interest due under long-term debt agreements and lease obligations as of December 31, 2010 follows (in thousands):
| Payments due by period | ||||||||||||||||||||||||
| Revolving credit facility (a) |
Other long-term debt |
Non-cancelable operating leases | Total | |||||||||||||||||||||
| Year |
Ventas (b) | Other | Subtotal | |||||||||||||||||||||
| 2011 |
$ | 10,408 | $ | 128 | $ | 251,836 | $ | 75,882 | $ | 327,718 | $ | 338,254 | ||||||||||||
| 2012 |
370,703 | 127 | 256,953 | 70,420 | 327,373 | 698,203 | ||||||||||||||||||
| 2013 |
– | 127 | 178,966 | 69,101 | 248,067 | 248,194 | ||||||||||||||||||
| 2014 |
– | 127 | 141,519 | 66,695 | 208,214 | 208,341 | ||||||||||||||||||
| 2015 |
– | 128 | 47,399 | 62,302 | 109,701 | 109,829 | ||||||||||||||||||
| Thereafter |
– | 138 | – | 199,092 | 199,092 | 199,230 | ||||||||||||||||||
| $ | 381,111 | $ | 775 | $ | 876,673 | $ | 543,492 | $ | 1,420,165 | $ | 1,802,051 | |||||||||||||
| (a) | Revolving credit facility interest is based upon the weighted average interest rate of 2.8% as of December 31, 2010. |
| (b) | See “Part I – Business – Master Lease Agreements – Rental Amounts and Escalators.” |
As of December 31, 2010, we had approximately $3 million of total gross unrecognized tax benefits and $0.2 million of accrued interest related to uncertain tax positions. Because future cash outflows related to these unrecognized tax benefits are uncertain, they are excluded from the table above.
Capital Resources
Excluding acquisitions, routine capital expenditures (expenditures necessary to maintain existing facilities that generally do not increase capacity or add services) totaled $109 million in 2010, $98 million in 2009 and $110 million in 2008. Hospital development capital expenditures (primarily new facility construction) totaled $41 million in 2010, $42 million in 2009 and $33 million in 2008. Nursing and rehabilitation center development
89
Table of Contents
capital expenditures (primarily the addition of transitional care services for higher acuity patients and new facility construction) totaled $27 million in 2010 and $6 million in each of 2009 and 2008. These capital expenditures were financed primarily through internally generated funds. At December 31, 2010, the estimated cost to complete and equip construction in progress approximated $45 million. We believe that our capital expenditure program is adequate to improve and equip our existing facilities.
Expenditures for acquisitions totaled $280 million in 2010, $83 million in 2009 and $49 million in 2008. To the extent that these expenditures were not financed through the use of operating cash flows, we utilized our revolving credit facility to finance these transactions.
The more significant acquisitions in the past three years included the Vista Acquisition in November 2010 ($179 million), the purchase of three nursing and rehabilitation centers in September 2010 ($38 million) and the acquisition of previously leased facilities in each of the last three years ($75 million).
In 2009, we purchased the Nursing Centers from Ventas for approximately $58 million and subsequently sold these facilities for $27 million. See “Part 1 – Item 1 – Business – Discontinued Operations.”
In 2008, we purchased for resale a LTAC hospital for $22 million that was previously leased and announced our intention to dispose of another LTAC hospital and its related operations. These two facilities are classified as assets held for sale in our consolidated balance sheet at December 31, 2010.
Other Information
Effects of inflation and changing prices
We derive a substantial portion of our revenues from the Medicare and Medicaid programs. Congress and certain state legislatures have enacted or may enact additional significant cost containment measures limiting our ability to recover our cost increases through increased pricing of our healthcare services. Medicare revenues in LTAC hospitals and nursing centers are subject to fixed payments under the Medicare prospective payment systems.
Medicaid reimbursement rates in many states in which we operate nursing and rehabilitation centers also are based upon fixed payment systems. Generally, these rates are adjusted annually for inflation. However, these adjustments may not reflect the actual increase in the costs of providing healthcare services.
Various healthcare reform provisions became law upon enactment of the ACA. The reforms contained in the ACA will impact each of our businesses in some manner. Several of the reforms are very significant and could ultimately change the nature of our services, the methods of payment for our services and the underlying regulatory environment. The reforms include possible modifications to the conditions of qualification for payment, bundling payments to cover both acute and post-acute care and the imposition of enrollment limitations on new providers. In addition, a primary goal of healthcare reform is to reduce costs, which includes reductions in the reimbursement paid to us and other healthcare providers. Moreover, healthcare reform could negatively impact insurance companies, other third party payors, our customers, as well as other healthcare providers, which may in turn negatively impact our business. As such, these healthcare reforms or other similar healthcare reforms could have a material adverse effect on our business, financial position, results of operations and liquidity.
There are continuing efforts to reform governmental healthcare programs, both as part of the ACA enacted in 2010 and otherwise, that could result in major changes in the healthcare delivery and reimbursement system on a national and state level. Potential reforms include changes directly impacting the government and private reimbursement systems for our LTAC hospitals, our nursing and rehabilitation centers as well as our rehabilitation operations. Reforms or other changes to the payment systems, including modifications to the conditions of qualification for payment, bundling payments to cover both acute and post-acute care or the imposition of enrollment limitations on new providers, may be proposed or could be adopted by Congress or CMS in the future.
90
Table of Contents
Moreover, weak economic conditions also could adversely affect the budgets of individual states and of the federal government. This could result in attempts to reduce or eliminate payments for federal and state healthcare programs, including Medicare and Medicaid, and could result in an increase in taxes and assessments on our activities. In addition, private third party payors are continuing their efforts to control healthcare costs through direct contracts with healthcare providers, increased utilization review and greater enrollment in managed care programs and preferred provider organizations. These private payors increasingly are demanding discounted fee structures and are requesting that healthcare providers assume more financial risk.
Though we cannot predict what reform proposals will be adopted or finally implemented, healthcare reform and regulations may have a material adverse effect on our business, financial position, results of operations and liquidity through, among other things, decreasing funds available for our services or increased operating costs. We could be affected adversely by the continuing efforts of governmental and private third party payors to contain healthcare costs. We cannot assure you that reimbursement payments under governmental and private third party payor programs, including Medicare supplemental insurance policies, will remain at levels comparable to present levels or will be sufficient to cover the costs allocable to patients eligible for reimbursement pursuant to these programs. Future changes in third party payor reimbursement rates or methods, including the Medicare and Medicaid programs, or the implementation of other measures to reduce reimbursement for our services and products could result in a material reduction in our revenues. Our operating margins may continue to be under pressure because of deterioration in pricing flexibility, changes in payor mix, changes in length of stay and growth in operating expenses in excess of increases in payments by third party payors. In addition, as a result of competitive pressures, our ability to maintain operating margins through price increases to private patients or commercial payors remains limited. These results could have a material adverse effect on our business, financial position, results of operations and liquidity.
We believe that our operating margins will also continue to be under pressure as the growth in operating expenses, particularly professional liability, labor and employee benefits costs, exceeds payment increases from third party payors. In addition, as a result of competitive pressures, our ability to maintain operating margins through price increases to private patients is limited.
See “Part I – Item 1 – Business – Governmental Regulation” for a detailed discussion of Medicare and Medicaid reimbursement regulations. Also see “Part I – Item 1A – Risk Factors.”
| Item 7A. | Quantitative and Qualitative Disclosures About Market Risk |
The following discussion of our exposure to market risk contains “forward-looking statements” that involve risks and uncertainties. Given the unpredictability of interest rates as well as other factors, actual results could differ materially from those projected in such forward-looking information.
Our exposure to market risk relates to changes in the prime rate, federal funds rate and LIBOR which affect the interest paid on certain borrowings.
The following table provides information about our financial instruments as of December 31, 2010 that are sensitive to changes in interest rates. The table presents principal cash flows and related weighted average interest rates by expected maturity date.
91
Table of Contents
Interest Rate Sensitivity
Principal (Notional) Amount by Expected Maturity
Average Interest Rate
(Dollars in thousands)
| Expected maturities | Fair value 12/31/10 |
|||||||||||||||||||||||||||||||
| 2011 | 2012 | 2013 | 2014 | 2015 | Thereafter | Total | ||||||||||||||||||||||||||
| Liabilities: |
||||||||||||||||||||||||||||||||
| Long-term debt, including amounts due within one year: |
||||||||||||||||||||||||||||||||
| Fixed rate |
$ | 91 | $ | 96 | $ | 102 | $ | 109 | $ | 116 | $ | 133 | $ | 647 | $ | 640 | (a) | |||||||||||||||
| Average interest rate |
6.0 | % | 6.0 | % | 6.0 | % | 6.0 | % | 6.0 | % | 6.0 | % | ||||||||||||||||||||
| Variable rate (b) |
$ | – | $ | 365,000 | $ | – | $ | – | $ | – | $ | – | $ | 365,000 | $ | 365,000 | ||||||||||||||||
| (a) | Calculated based upon the net present value of future principal and interest payments using a discount rate of 6%. |
| (b) | Interest on borrowings under our revolving credit facility is payable, at our option, at (1) LIBOR plus an applicable margin ranging from 1.75% to 2.50% or (2) the applicable margin ranging from 0.75% to 1.50% plus the higher of the prime rate or 0.5% over the federal funds rate. The applicable margin is based upon our average daily excess availability as defined in our revolving credit facility. |
| Item 8. | Financial Statements and Supplementary Data |
The information required by this Item 8 is included in appendix pages F-2 through F-42 of this Annual Report on Form 10-K and incorporated herein by reference.
| Item 9. | Changes in and Disagreements With Accountants on Accounting and Financial Disclosure |
None.
| Item 9A. | Controls and Procedures |
Evaluation of Disclosure Controls and Procedures and Changes in Internal Control over Financial Reporting
We have carried out an evaluation under the supervision and with the participation of our management, including the Chief Executive Officer and Chief Financial Officer, of the effectiveness of the design and operation of our disclosure controls and procedures. There are inherent limitations to the effectiveness of any system of disclosure controls and procedures, including the possibility of human error and the circumvention or overriding of the controls and procedures. Accordingly, even effective disclosure controls and procedures can only provide reasonable assurance of achieving their control objectives. Based upon our evaluation, the Chief Executive Officer and Chief Financial Officer have concluded that, as of December 31, 2010, the disclosure controls and procedures, as defined in Rule 13a-15(e) under the Exchange Act, are effective.
There has been no change in our internal control over financial reporting during the quarter ended December 31, 2010, that has materially affected, or is reasonably likely to materially affect, our internal control over financial reporting.
Management’s Annual Report on Internal Control over Financial Reporting
Our management is responsible for establishing and maintaining adequate internal control over financial reporting as defined in Rules 13a-15(f) and 15d-15(f) under the Exchange Act. Our internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and
92
Table of Contents
the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. Our internal control over financial reporting includes those policies and procedures that:
| (i) | pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the Company; |
| (ii) | provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the Company are being made only in accordance with authorizations of management and directors of the Company; and |
| (iii) | provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use or disposition of the Company’s assets that could have a material effect on the financial statements. |
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
Our management assessed the effectiveness of the Company’s internal control over financial reporting as of December 31, 2010. In making this assessment, management used the criteria set forth by the Committee of Sponsoring Organizations of the Treadway Commission (COSO) in Internal Control-Integrated Framework.
Based upon our assessment and those criteria, management has concluded that the Company maintained effective internal control over financial reporting as of December 31, 2010.
The effectiveness of the Company’s internal control over financial reporting as of December 31, 2010 has been audited by PricewaterhouseCoopers LLP, our independent registered public accounting firm, who also audited our consolidated financial statements included in this Annual Report on Form 10-K, as stated in their report which appears in our consolidated financial statements.
| Item 9B. | Other Information |
Not applicable.
93
Table of Contents
PART III
| Item 10. | Directors, Executive Officers and Corporate Governance |
EXECUTIVE OFFICERS OF THE REGISTRANT
Set forth below are the names, ages (as of January 1, 2011) and present and past positions of our current executive officers:
| Name |
Age |
Position | ||
| Paul J. Diaz | 49 | President and Chief Executive Officer | ||
| Benjamin A. Breier | 39 | Chief Operating Officer | ||
| Richard A. Lechleiter | 52 | Executive Vice President and Chief Financial Officer | ||
| Lane M. Bowen | 60 | Executive Vice President and President, Nursing Center Division | ||
| Jeffrey P. Winter | 54 | Executive Vice President and President, Hospital Division | ||
| Richard E. Chapman | 62 | Executive Vice President and Chief Administrative and Information Officer | ||
| Christopher M. Bird | 46 | President, Peoplefirst Rehabilitation Division | ||
| William M. Altman | 51 | Senior Vice President, Strategy and Public Policy | ||
| Joseph L. Landenwich | 46 | Senior Vice President of Corporate Legal Affairs and Corporate Secretary | ||
| Gregory C. Miller | 41 | Chief Development Officer | ||
| M. Suzanne Riedman | 59 | General Counsel and Chief Diversity Officer |
Paul J. Diaz has served as one of our directors since May 2002, as our Chief Executive Officer since January 1, 2004 and as our President since January 2002. Mr. Diaz served as our Chief Operating Officer from January 2002 to December 31, 2003.
Benjamin A. Breier has served as our Chief Operating Officer since August 31, 2010. He served as our Executive Vice President and President, Hospital Division from March 2008 until August 2010, and as President, Peoplefirst Rehabilitation division from August 2005 to March 2008. Prior to joining us, Mr. Breier served as Senior Vice President, Operations for Concentra, Inc., a leading provider of workers compensation and occupational health services, from December 2003 to August 2005.
Richard A. Lechleiter, a certified public accountant, has served as our Executive Vice President and Chief Financial Officer since February 2005. He served as Senior Vice President and Chief Financial Officer from February 2002 to February 2005.
Lane M. Bowen has served as our Executive Vice President since February 2005 and as President, Nursing Center Division since October 2002.
Jeffrey P. Winter has served as our Executive Vice President and President, Hospital Division, since November 1, 2010. Prior to joining us, he served as Chief Administrative Officer of Providence Health and Services, California Region. Prior to joining Providence in 2009, Mr. Winter was with Catholic Healthcare West for ten years, most recently as President of Group Operations.
Richard E. Chapman has served as our Executive Vice President and Chief Administrative and Information Officer since February 2005. He served as Chief Administrative and Information Officer and Senior Vice President from January 2001 to February 2005.
Christopher M. Bird has served as our President, Peoplefirst Rehabilitation division since April 2008. Prior to joining us, Mr. Bird served as Vice President, Operations and Business Development, Outpatient Services Division with Tenet Healthcare Corp., which owns and operates acute care hospitals and related ancillary healthcare businesses, from May 2006 to April 2008. Mr. Bird served as Division Vice President, Western Division, with DaVita, Inc., a provider of dialysis services for patients suffering from chronic kidney failure, from December 2001 to April 2006.
94
Table of Contents
William M. Altman, an attorney, has served as our Senior Vice President, Strategy and Public Policy since January 1, 2008. He served as Senior Vice President, Compliance and Government Programs from April 2002 to December 2007.
Joseph L. Landenwich, an attorney and certified public accountant, has served as our Senior Vice President of Corporate Legal Affairs and Corporate Secretary since December 2003. Mr. Landenwich served as Vice President of Corporate Legal Affairs and Corporate Secretary from November 1999 to December 2003.
Gregory C. Miller has served as our Chief Development Officer since February 16, 2011. He served as Senior Vice President, Corporate Development and Financial Planning from January 2005 to February 2011. He served as our Vice President, Corporate Development and Financial Planning from January 2004 to January 2005.
M. Suzanne Riedman, an attorney, has served as our General Counsel since August 1999 and as our Chief Diversity Officer since December 2010. She also held the title of Senior Vice President from August 1999 to February 2011.
As a result of decreased Medicare and Medicaid reimbursement rates introduced by the Balanced Budget Act and other issues associated with our Company, we were unable to meet our then existing financial obligations, including rent payable to the Company’s largest landlord, Ventas, and debt service obligations under our then existing indebtedness. Accordingly, on September 13, 1999, we filed voluntary petitions for protection under the Bankruptcy Code. On March 1, 2001, the Bankruptcy Court approved our Fourth Amended Joint Plan of Reorganization. From the date of our bankruptcy filing until we emerged from bankruptcy on April 20, 2001, we operated our businesses as a debtor-in-possession subject to the jurisdiction of the Bankruptcy Court. Messrs. Chapman and Lechleiter and Ms. Riedman were each executive officers of the Company at the time of our bankruptcy filing.
The information required by this Item, other than the information set forth above under “Executive Officers of the Registrant,” is omitted because we are filing a definitive proxy statement, which includes the required information, pursuant to Regulation 14A not later than 120 days after the end of the fiscal year covered by this Annual Report on Form 10-K. The required information contained in our proxy statement is incorporated herein by reference.
| Item 11. | Executive Compensation |
The information required by this Item is omitted because we are filing a definitive proxy statement, which includes the required information, pursuant to Regulation 14A not later than 120 days after the end of the fiscal year covered by this Annual Report on Form 10-K. The required information contained in our proxy statement is incorporated herein by reference.
| Item 12. | Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters |
The information required by this Item is omitted because we are filing a definitive proxy statement, which includes the required information, pursuant to Regulation 14A not later than 120 days after the end of the fiscal year covered by this Annual Report on Form 10-K. The required information contained in our proxy statement is incorporated herein by reference.
| Item 13. | Certain Relationships and Related Transactions, and Director Independence |
The information required by this Item is omitted because we are filing a definitive proxy statement, which includes the required information, pursuant to Regulation 14A not later than 120 days after the end of the fiscal year covered by this Annual Report on Form 10-K. The required information contained in our proxy statement is incorporated herein by reference.
95
Table of Contents
| Item 14. | Principal Accounting Fees and Services |
The information required by this Item is omitted because we are filing a definitive proxy statement, which includes the required information, pursuant to Regulation 14A not later than 120 days after the end of the fiscal year covered by this Annual Report on Form 10-K. The required information contained in our proxy statement is incorporated herein by reference.
96
Table of Contents
PART IV
| Item 15. | Exhibits and Financial Statement Schedules |
(a)(1) and (a)(2) Index to Consolidated Financial Statements and Financial Statement Schedules:
| Page | ||||
| Report of Independent Registered Public Accounting Firm |
F-2 | |||
| Consolidated Financial Statements: |
||||
| Consolidated Statement of Operations for the years ended December 31, 2010, 2009 and 2008 |
F-3 | |||
| Consolidated Balance Sheet, December 31, 2010 and 2009 |
F-4 | |||
| Consolidated Statement of Stockholders’ Equity for the years ended December 31, 2010, 2009 and 2008 |
F-5 | |||
| Consolidated Statement of Cash Flows for the years ended December 31, 2010, 2009 and 2008 |
F-6 | |||
| Notes to Consolidated Financial Statements |
F-7 | |||
| Quarterly Consolidated Financial Information (Unaudited) |
F-40 | |||
| Financial Statement Schedule (a): |
||||
| Schedule II – Valuation and Qualifying Accounts for the years ended December 31, 2010, 2009 and 2008 |
F-42 | |||
| (a) | All other schedules have been omitted because the required information is not present or not present in material amounts. |
97
Table of Contents
(a)(3) Index to Exhibits:
| Exhibit |
Description of document | |
| 2.1 | Fourth Amended Joint Plan of Reorganization of Vencor, Inc. and Affiliated Debtors under Chapter 11 of the Bankruptcy Code. Exhibit 2.1 to the Current Report on Form 8-K of the Company dated March 19, 2001 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 2.2 | Order Confirming the Fourth Amended Joint Plan of Reorganization of Vencor, Inc. and Affiliated Debtors under Chapter 11 of the Bankruptcy Code, as entered by the United States Bankruptcy Court for the District of Delaware on March 16, 2001. Exhibit 2.2 to the Current Report on Form 8-K of the Company dated March 19, 2001 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 2.3 | Purchase and Sale Agreement by and among those entities listed on Schedule P thereto as buying entities, those entities listed on Schedule P thereto as selling entities and Jeffrey A. Goldshine, Douglas B. Noble, and Mary Catherine Rumsey, and solely for purposes of Article III thereof and the Guaranty, Kindred Healthcare Operating, Inc., dated as of October 24, 2005. Exhibit 2.1 to the Company’s Current Report on Form 8-K dated October 24, 2005 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 2.4* | Master Transaction Agreement, dated as of October 25, 2006, by and among AmerisourceBergen Corporation, PharMerica, Inc., Kindred Healthcare, Inc., Kindred Healthcare Operating, Inc., Kindred Pharmacy Services, Inc., Safari Holding Corporation, Hippo Merger Corporation and Rhino Merger Corporation. Exhibit 10.1 to the Company’s Current Report on Form 8-K dated October 25, 2006 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 2.5 | Amendment No. 1 To Master Transaction Agreement, dated as of June 4, 2007, among AmerisourceBergen Corporation, PharMerica, Inc., Kindred Healthcare, Inc., Kindred Healthcare Operating, Inc., Kindred Pharmacy Services, Inc., Safari Holding Corporation, Hippo Merger Corporation and Rhino Merger Corporation. Exhibit 10.1 to the Company’s Current Report on Form 8-K dated June 4, 2007 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 2.6* | Amendment No. 2 To Master Transaction Agreement, dated as of July 31, 2007, among AmerisourceBergen Corporation, PharMerica Long-Term Care, Inc. (formerly named PharMerica, Inc.), Kindred Healthcare, Inc., Kindred Healthcare Operating, Inc., Kindred Pharmacy Services, Inc., PharMerica Corporation (formerly named Safari Holding Corporation), Hippo Merger Corporation and Rhino Merger Corporation. Exhibit 2.1 to the Company’s Form 10-Q for the quarterly period ended September 30, 2007 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 2.7 | Asset Purchase Agreement, dated as of August 23, 2010, by and among (i) (a) KND Development 52, L.L.C., KND Development 53, L.L.C., KND Development 54, L.L.C., and KND Development 55, L.L.C., (ii) Kindred Healthcare Operating, Inc., (iii) (a) Vista Healthcare Holdings, LLC, (b) Vista Healthcare, LLC, (c) Vista Hospital of South Bay, LP, (d) South Bay Community Hospital, Inc., (e) Rancho Cucamonga Community Hospital, LLC, (f) Vista Specialty Hospital of Southern California, LP, (g) Perris Valley Community Hospital, LLC, and (h) Vista Hospital of South Bay, LLC, (iv) (a) Ara Tavitian, M.D., (b) J. Vartan Hovsepian, (c) Marc Ferrell, (d) Marc Furstman, (e) Vista Hospital Management Group, Inc., (f) the Ara Tavitian 2010 GRAT, (g) Vista Partnership Holding, LLC, and (v) Tavitian Holdings, LLC. Exhibit 2.1 to the Company’s Current Report on Form 8-K dated August 23, 2010 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
98
Table of Contents
| Exhibit |
Description of document | |
| 2.8 | Amendment No. 1 to the Asset Purchase Agreement, entered into as of October 21, 2010, by and among (i) (a) KND Development 52, L.L.C., KND Development 53, L.L.C., KND Development 54, L.L.C., and KND Development 55, L.L.C., (ii) Kindred Healthcare Operating, Inc., (iii) (a) Vista Healthcare Holdings, LLC, (b) Vista Healthcare, LLC, (c) Vista Hospital of South Bay, LP, (d) South Bay Community Hospital, Inc., (e) Rancho Cucamonga Community Hospital, LLC, (f) Vista Specialty Hospital of Southern California, LP, (g) Perris Valley Community Hospital, LLC, and (h) Vista Hospital of South Bay, LLC, (iv) (a) Ara Tavitian, M.D., (b) J. Vartan Hovsepian, (c) Marc Ferrell, (d) Marc Furstman, (e) Vista Hospital Management Group, Inc., (f) the Ara Tavitian 2010 GRAT, (g) Vista Partnership Holding, LLC, and (v) Tavitian Holdings, LLC. Exhibit 2.1 to the Company’s Current Report on Form 8-K dated October 21, 2010 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 2.9 | Amendment No. 2 to the Asset Purchase Agreement, entered into as of October 30, 2010, by and among (i) (a) KND Development 52, L.L.C., KND Development 53, L.L.C., KND Development 54, L.L.C., and KND Development 55, L.L.C., (ii) Kindred Healthcare Operating, Inc., (iii) (a) Vista Healthcare Holdings, LLC, (b) Vista Healthcare, LLC, (c) Vista Hospital of South Bay, LP, (d) South Bay Community Hospital, Inc., (e) Rancho Cucamonga Community Hospital, LLC, (f) Vista Specialty Hospital of Southern California, LP, (g) Perris Valley Community Hospital, LLC, and (h) Vista Hospital of South Bay, LLC, (iv) (a) Ara Tavitian, M.D., (b) J. Vartan Hovsepian, (c) Marc Ferrell, (d) Marc Furstman, (e) Vista Hospital Management Group, Inc., (f) the Ara Tavitian 2010 GRAT, (g) Vista Partnership Holding, LLC, and (v) Tavitian Holdings, LLC. Exhibit 2.1 to the Company’s Current Report on Form 8-K dated October 30, 2010 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 2.10 | Agreement and Plan of Merger, dated as of February 7, 2011, among Kindred Healthcare, Inc., Kindred Healthcare Development, Inc. and RehabCare Group, Inc. Exhibit 2.1 to the Company’s Current Report on Form 8-K dated February 7, 2011 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 3.1 | Amended and Restated Certificate of Incorporation of the Company. Exhibit 4.1 to the Company’s Registration Statement on Form S-3 filed August 31, 2001 (Comm. File No. 333-68838) is hereby incorporated by reference. | |
| 3.2 | Certificate of Amendment of Amended and Restated Certificate of Incorporation. Exhibit 3.1 to the Company’s Form 10-Q for the quarterly period ended March 31, 2002 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 3.3 | Amended and Restated Bylaws of the Company. Exhibit 3.1 to the Company’s Current Report on Form 8-K dated March 20, 2009 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 4.1 | Articles IV, IX, X and XII of the Restated Certificate of Incorporation of the Company is included in Exhibit 3.1. | |
| 10.1 | Second Amended and Restated Credit Agreement dated as of July 18, 2007 among the Company, the Lenders party thereto, JPMorgan Chase Bank, N.A., as Administrative Agent and Collateral Agent, J.P. Morgan Securities Inc., as Sole Bookrunner and Sole Lead Arranger, Citicorp USA, Inc., as Syndication Agent, and General Electric Capital Corporation, The CIT Group/Business Credit, Inc. and Wells Fargo Foothill, as Co-Documentation Agents. Exhibit 10.1 to the Company’s Form 10-Q for the quarterly period ended September 30, 2007 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.2 | Amendment No. 1, dated as of September 23, 2010, to the Second Amended and Restated Credit Agreement dated as of July 18, 2007 among Kindred Healthcare, Inc., the Lenders party thereto, and JPMorgan Chase Bank, N.A., as Administrative Agent and Collateral Agent. Exhibit 10.1 to the Company’s Current Report on Form 8-K dated September 23, 2010 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
99
Table of Contents
| Exhibit |
Description of document | |
| 10.3 | Amendment No. 2 and Joinder Agreement to the Second Amended and Restated Credit Agreement dated as of July 18, 2007 among the Company, the Lenders party thereto, and JPMorgan Chase Bank, N.A., as Administrative Agent and Collateral Agent. Exhibit 10.1 to the Company’s Current Report on Form 8-K dated December 10, 2010 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.4 | Tax Allocation Agreement dated as of April 30, 1998 by and between Vencor, Inc. and Ventas, Inc. Exhibit 10.9 to the Company’s Form 10-Q for the quarterly period ended June 30, 1998 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.5 | Agreement of Indemnity-Third Party Leases dated as of April 30, 1998 by and between Vencor, Inc. and its subsidiaries and Ventas, Inc. Exhibit 10.11 to the Company’s Form 10-Q for the quarterly period ended June 30, 1998 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.6 | Agreement of Indemnity-Third Party Contracts dated as of April 30, 1998 by and between Vencor, Inc. and its subsidiaries and Ventas, Inc. Exhibit 10.12 to the Company’s Form 10-Q for the quarterly period ended June 30, 1998 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.7 | Form of Indemnification Agreement between the Company and certain of its officers and employees. Exhibit 10.31 to the Ventas, Inc. Form 10-K for the year ended December 31, 1995 (Comm. File No. 1-10989) is hereby incorporated by reference. | |
| 10.8 | Form of Indemnification Agreement between the Company and each member of its Board of Directors. Exhibit 10.21 to the Company’s Form 10-K for the year ended December 31, 2001 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.9** | Kindred Deferred Compensation Plan, Third Amendment and Restatement effective as of January 1, 2009. Exhibit 10.4 to the Company’s Form 10-Q for the quarterly period ended September 30, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.10 | Tax Refund Escrow Agreement and First Amendment to the Tax Allocation Agreement made and entered into as of the 20th of April 2001 by and between the Company and each of its subsidiaries and Ventas, Inc., Ventas Realty Limited Partnership and Ventas LP Realty, L.L.C. Exhibit 10.31 to the Company’s Form 10-K for the year ended December 31, 2001 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.11** | Vencor, Inc. Supplemental Executive Retirement Plan dated January 1, 1998, as amended. Exhibit 10.27 to the Company’s Registration Statement on Form S-4 (Reg. No. 333-57953) is hereby incorporated by reference. | |
| 10.12** | Amendment No. Two to Supplemental Executive Retirement Plan dated as of January 15, 1999. Exhibit 10.48 to the Company’s Form 10-K for the year ended December 31, 1999 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.13** | Amendment No. Three to Supplemental Executive Retirement Plan dated as of December 31, 1999. Exhibit 10.49 to the Company’s Form 10-K for the year ended December 31, 1999 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.14** | Amendment No. 4 to Supplemental Executive Retirement Plan. Exhibit 10.3 to the Company’s Form 10-Q for the quarterly period ended March 31, 2001 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
100
Table of Contents
| Exhibit |
Description of document | |
| 10.15** | Amendment No. 5 to Supplemental Executive Retirement Plan. Exhibit 10.6 to the Company’s Form 10-Q for the quarterly period ended September 30, 2006 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.16** | Amendment No. 6 to Supplemental Executive Retirement Plan. Exhibit 10.5 to the Company’s Form 10-Q for the quarterly period ended September 30, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.17** | Amended and Restated Kindred Healthcare, Inc. Long-Term Incentive Plan. Exhibit 10.5 to the Company’s Form 10-Q for the quarterly period ended March 31, 2009 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.18** | Amended and Restated Kindred Healthcare, Inc. Short-Term Incentive Plan. Exhibit 10.3 to the Company’s Form 10-Q for the quarterly period ended September 30, 2008
(Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.19** | Agreement dated as of March 20, 2009 by and between Kindred Healthcare, Inc. and Edward L. Kuntz. Exhibit 10.1 to the Company’s Current Report on Form 8-K dated March 20, 2009 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.20** | Employment Agreement dated as of December 18, 2008 by and between Kindred Healthcare Operating, Inc. and Paul J. Diaz. Exhibit 10.3 to the Company’s Current Report on Form 8-K dated December 18, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.21** | Change-in-Control Severance Agreement dated as of November 13, 2009 by and between Kindred Healthcare Operating, Inc. and Paul J. Diaz. Exhibit 10.1 to the Company’s Current Report on Form 8-K dated November 13, 2009 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.22** | Employment Agreement dated as of December 18, 2008 by and between Kindred Healthcare Operating, Inc. and Richard E. Chapman. Exhibit 10.21 to the Company’s Form 10-K for the year ended December 31, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.23** | Change-in-Control Severance Agreement dated as of November 13, 2009 by and between Kindred Healthcare Operating, Inc. and Richard E. Chapman. Exhibit 10.21 to the Company’s Form 10-K for the year ended December 31, 2009 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.24** | Agreement and Release of Claims dated as of August 31, 2010 by and between Kindred Healthcare, Inc. and Frank J. Battafarano. Exhibit 10.1 to the Company’s Current Report on Form 8-K dated August 31, 2010 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.25** | Employment Agreement dated as of December 18, 2008 by and between Kindred Healthcare Operating, Inc. and M. Suzanne Riedman. Exhibit 10.25 to the Company’s Form 10-K for the year ended December 31, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.26** | Change-in-Control Severance Agreement dated as of November 13, 2009 by and between Kindred Healthcare Operating, Inc. and M. Suzanne Riedman. Exhibit 10.25 to the Company’s Form 10-K for the year ended December 31, 2009 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.27** | Employment Agreement dated as of December 18, 2008 by and between Kindred Healthcare Operating, Inc. and Richard A. Lechleiter. Exhibit 10.5 to the Company’s Current Report on Form 8-K dated December 18, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.28** | Change-in-Control Severance Agreement dated as of November 13, 2009 by and between Kindred Healthcare Operating, Inc. and Richard A. Lechleiter. Exhibit 10.2 to the Company’s Current Report on Form 8-K dated November 13, 2009 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
101
Table of Contents
| Exhibit |
Description of document | |
| 10.29** | Employment Agreement dated as of December 18, 2008 by and between Kindred Healthcare Operating, Inc. and William M. Altman. Exhibit 10.29 to the Company’s Form 10-K for the year ended December 31, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.30** | Change-in-Control Severance Agreement dated as of November 13, 2009 by and between Kindred Healthcare Operating, Inc. and William M. Altman. Exhibit 10.29 to the Company’s Form 10-K for the year ended December 31, 2009 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.31** | Employment Agreement dated as of December 18, 2008 by and between Kindred Healthcare Operating, Inc. and Lane M. Bowen. Exhibit 10.9 to the Company’s Current Report on Form 8-K dated December 18, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.32** | Change-in-Control Severance Agreement dated as of November 13, 2009 by and between Kindred Healthcare Operating, Inc. and Lane M. Bowen. Exhibit 10.4 to the Company’s Current Report on Form 8-K dated November 13, 2009 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.33** | Employment Agreement dated as of December 18, 2008 by and between Kindred Healthcare Operating, Inc. and Joseph L. Landenwich. Exhibit 10.33 to the Company’s Form 10-K for the year ended December 31, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.34** | Change-in-Control Severance Agreement dated as of November 13, 2009 by and between Kindred Healthcare Operating, Inc. and Joseph L. Landenwich. Exhibit 10.33 to the Company’s Form 10-K for the year ended December 31, 2009 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.35** | Employment Agreement dated as of March 30, 2010 by and between Kindred Healthcare Operating, Inc. and Benjamin A. Breier. Exhibit 10.1 to the Company’s Current Report on Form 8-K dated March 30, 2010 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.36** | Change-in-Control Severance Agreement dated as of November 13, 2009 by and between Kindred Healthcare Operating, Inc. and Benjamin A. Breier. Exhibit 10.35 to the Company’s Form 10-K for the year ended December 31, 2009 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.37** | Employment Agreement dated as of December 18, 2008 by and between Kindred Healthcare Operating, Inc. and Gregory C. Miller. Exhibit 10.37 to the Company’s Form 10-K for the year ended December 31, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.38** | Change-in-Control Severance Agreement dated as of November 13, 2009 by and between Kindred Healthcare Operating, Inc. and Gregory C. Miller. Exhibit 10.37 to the Company’s Form 10-K for the year ended December 31, 2009 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.39** | Employment Agreement dated as of December 18, 2008 by and between Kindred Healthcare Operating, Inc. and Christopher M. Bird. Exhibit 10.39 to the Company’s Form 10-K for the year ended December 31, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.40** | Change-in-Control Severance Agreement dated as of November 13, 2009 by and between Kindred Healthcare Operating, Inc. and Christopher M. Bird. Exhibit 10.39 to the Company’s Form 10-K for the year ended December 31, 2009 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.41** | Employment Agreement dated as of November 1, 2010 by and between Kindred Healthcare Operating, Inc. and Jeffrey P. Winter. Exhibit 10.3 to the Company’s Form 10-Q for the quarterly period ended September 30, 2010 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
102
Table of Contents
| Exhibit |
Description of document | |
| 10.42** | Change-in-Control Severance Agreement dated as of November 1, 2010 by and between Kindred Healthcare Operating, Inc. and Jeffrey P. Winter. Exhibit 10.4 to the Company’s Form 10-Q for the quarterly period ended September 30, 2010 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.43 | Second Amended and Restated Master Lease Agreement No. 1 dated as of April 27, 2007 for Lease Executed by Ventas Realty, Limited Partnership, as Lessor and Kindred Healthcare, Inc. and Kindred Healthcare Operating, Inc. as Tenant. Exhibit 10.3 to the Company’s Form 10-Q for the quarterly period ended June 30, 2007 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.44 | Amendment to Memorandum of Lease and Specific Property Lease Amendment dated as of June 8, 2007 by and between Ventas Realty, Limited Partnership, as Lessor and Kindred Healthcare, Inc. and Kindred Healthcare Operating, Inc. as Tenant. Exhibit 10.47 to the Company’s Form 10-K for the year ended December 31, 2007 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.45 | Amendment to Master Lease and Memorandum of Lease dated as of January 16, 2009 by and between Ventas Realty, Limited Partnership, as Lessor and Kindred Healthcare, Inc. and Kindred Healthcare Operating, Inc. as Tenant. Exhibit 10.1 to the Company’s Form 10-Q for the quarterly period ended March 31, 2009 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.46 | Amendment to Memorandum of Lease and Specific Property Lease Amendment dated as of October 14, 2009 by and between Ventas Realty, Limited Partnership, as Lessor and Kindred Healthcare, Inc. and Kindred Healthcare Operating, Inc. as Tenant. Exhibit 10.43 to the Company’s Form 10-K for the year ended December 31, 2009 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.47 | Second Amended and Restated Master Lease Agreement No. 2 dated as of April 27, 2007 for Lease Executed by Ventas Realty, Limited Partnership, as Lessor and Kindred Healthcare, Inc. and Kindred Healthcare Operating, Inc. as Tenant. Exhibit 10.4 to the Company’s Form 10-Q for the quarterly period ended June 30, 2007 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.48 | Second Amended and Restated Master Lease Agreement No. 3 dated as of April 27, 2007 for Lease Executed by Ventas Realty, Limited Partnership, as Lessor and Kindred Healthcare, Inc. and Kindred Healthcare Operating, Inc. as Tenant. Exhibit 10.5 to the Company’s Form 10-Q for the quarterly period ended June 30, 2007 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.49 | Amendment to Memorandum of Lease and Specific Property Lease Amendment dated as of January 9, 2009 by and between Ventas Realty, Limited Partnership, as Lessor and Kindred Healthcare, Inc. and Kindred Healthcare Operating, Inc. as Tenant. Exhibit 10.2 to the Company’s Form 10-Q for the quarterly period ended March 31, 2009 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.50 | Second Amended and Restated Master Lease Agreement No. 4 dated as of April 27, 2007 for Lease Executed by Ventas Realty, Limited Partnership, as Lessor and Kindred Healthcare, Inc. and Kindred Healthcare Operating, Inc. as Tenant. Exhibit 10.6 to the Company’s Form 10-Q for the quarterly period ended June 30, 2007 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.51 | Amendment to Master Lease and Memorandum of Lease dated as of August 7, 2007 by and among Ventas Realty, Limited Partnership, as Lessor and Kindred Healthcare, Inc. and Kindred Healthcare Operating, Inc. as Tenant. Exhibit 10.51 to the Company’s Form 10-K for the year ended December 31, 2007 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
103
Table of Contents
| Exhibit |
Description of document | |
| 10.52 | Renewal Notice to Lessor dated April 30, 2009 regarding the Second Amended and Restated Master Lease Agreements Nos. 1-4 between Ventas Realty, Limited Partnership, as Lessor and Kindred Healthcare, Inc. and Kindred Healthcare Operating, Inc. as Tenant. Exhibit 10.1 to the Company’s Form 10-Q for the quarterly period ended June 30, 2009 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.53 | Master Lease among Health Care Property Investors, Inc. and Health Care Property Partners, collectively, as Lessor and Kindred Nursing Centers East, L.L.C., Kindred Nursing Centers West, L.L.C. and Kindred Nursing Centers Limited Partnership, collectively, as Lessee, dated May 16, 2001. Exhibit 10.11 to the Company’s Form 10-Q for the quarterly period ended June 30, 2001 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.54 | First Amendment to Master Lease dated effective August 1, 2001 by and among Health Care Property Investors, Inc., Health Care Property Partners and Indiana HCP, L.P., collectively, as Lessor and Kindred Nursing Centers East, L.L.C., Kindred Nursing Centers West, L.L.C. and Kindred Nursing Centers Limited Partnership, collectively, as Lessee. Exhibit 10.53 to the Company’s Form 10-K for the year ended December 31, 2007 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.55 | Second Amendment to Master Lease dated as of November 18, 2003 by and among Health Care Property Investors, Inc., Health Care Property Partners and Indiana HCP, L.P., collectively, as Lessor and Kindred Nursing Centers East, L.L.C., Kindred Nursing Centers West, L.L.C. and Kindred Nursing Centers Limited Partnership, collectively, as Lessee. Exhibit 10.54 to the Company’s Form 10-K for the year ended December 31, 2007 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.56 | Third Amendment to Master Lease dated and effective as of June 30, 2004 by and among Health Care Property Investors, Inc. and Health Care Property Partners, collectively, as Lessor and Kindred Nursing Centers East, L.L.C., Kindred Nursing Centers West, L.L.C. and Kindred Nursing Centers Limited Partnership, collectively, as Lessee. Exhibit 10.55 to the Company’s Form 10-K for the year ended December 31, 2007 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.57 | Fourth Amendment to Master Lease by and among Health Care Property Investors, Inc. and Health Care Property Partners, collectively, as Lessor and Kindred Nursing Centers East, L.L.C., Kindred Nursing Centers West, L.L.C. and Kindred Nursing Centers Limited Partnership, collectively, as Lessee, dated February 28, 2006. Exhibit 10.71 to the Company’s Form 10-K for the year ended December 31, 2006 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.58 | Fifth Amendment to Master Lease by and among Health Care Property Investors, Inc., Health Care Property Partners, and Texas HCP Holding, L.P., collectively, as Lessor and Kindred Nursing Centers East, L.L.C., Kindred Nursing Centers West, L.L.C., Kindred Nursing Centers Limited Partnership, Kindred Hospitals Limited Partnership and Transitional Hospitals Corporation of Wisconsin, Inc., collectively, as Lessee, dated January 31, 2007. Exhibit 10.72 to the Company’s Form 10-K for the year ended December 31, 2006 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.59 | Sixth Amendment to Master Lease by and among HCP, Inc. f/k/a Health Care Property Investors, Inc., Health Care Property Investors, Inc., Health Care Property Partners, and Texas HCP Holding, L.P., collectively, as Lessor and Kindred Nursing Centers East, L.L.C., Kindred Nursing Centers West, L.L.C., Kindred Nursing Centers Limited Partnership and Transitional Hospitals Corporation of Wisconsin, Inc., collectively, as Lessee, dated December 8, 2008. Exhibit 10.53 to the Company’s Form 10-K for the year ended December 31, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
104
Table of Contents
| Exhibit |
Description of document | |
| 10.60 | Master Lease Agreement dated as of February 28, 2006 by and between HCRI Massachusetts Properties Trust II, as Lessor and Kindred Nursing Centers East, L.L.C., as Tenant. Exhibit 10.6 to the Company’s Form 10-Q for the quarterly period ended March 31, 2006 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.61 | First Amendment to Master Lease Agreement dated as of June 20, 2007 by and between HCRI Massachusetts Properties Trust II, as Lessor and Kindred Nursing Centers East, L.L.C., as Tenant. Exhibit 10.59 to the Company’s Form 10-K for the year ended December 31, 2007 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.62 | Termination of Lease and Notice of Lease dated as of January 22, 2010 by and among HCRI Massachusetts Properties Trust, HCRI Massachusetts Properties Trust II and Kindred Hospitals East, L.L.C. Exhibit 10.1 to the Company’s Form 10-Q for the quarterly period ended March 31, 2010 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.63 | Termination of Lease and Notice of Lease dated as of January 22, 2010 by and among HCRI Massachusetts Properties Trust, HCRI Massachusetts Properties Trust II, Kindred Hospitals East, L.L.C. and KND Real Estate 26, L.L.C. Exhibit 10.2 to the Company’s Form 10-Q for the quarterly period ended March 31, 2010 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.64 | Agreement and Plan of Reorganization between the Company and Ventas, Inc. Exhibit 10.1 to the Company’s Form 10, as amended, dated April 27, 1998 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.65** | The Company’s 2000 Stock Option Plan. Exhibit 4.1 to the Company’s Registration Statement on Form S-8 (Reg. No. 333-59598) is hereby incorporated by reference. | |
| 10.66** | The Company’s Restricted Share Plan. Exhibit 4.2 to the Company’s Registration Statement on Form S-8 (Reg. No. 333-59598) is hereby incorporated by reference. | |
| 10.67** | Kindred Healthcare, Inc. 2001 Stock Incentive Plan, Amended and Restated. Exhibit 10.1 to the Company’s Current Report on Form 8-K dated May 22, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.68** | Form of Kindred Healthcare, Inc. Non-Qualified Stock Option Grant Agreement under the 2001 Stock Incentive Plan, Amended and Restated. Exhibit 10.64 to the Company’s Form 10-K for the year ended December 31, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.69** | Form of Kindred Healthcare, Inc. Incentive Stock Option Grant Agreement under the 2001 Stock Incentive Plan, Amended and Restated. Exhibit 10.65 to the Company’s Form 10-K for the year ended December 31, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.70** | Form of Kindred Healthcare, Inc. Restricted Share Award Agreement under the 2001 Stock Incentive Plan, Amended and Restated. Exhibit 10.66 to the Company’s Form 10-K for the year ended December 31, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.71** | Form of Kindred Healthcare, Inc. Stock Bonus Award Agreement under the 2001 Stock Incentive Plan, Amended and Restated. Exhibit 10.4 to the Company’s Form 10-Q for the quarterly period ended March 31, 2009 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.72** | Form of Kindred Healthcare, Inc. Performance Unit Award Agreement under the 2001 Stock Incentive Plan, Amended and Restated. Exhibit 10.68 to the Company’s Form 10-K for the year ended December 31, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.73** | Kindred Healthcare, Inc. 2001 Equity Plan for Non-Employee Directors (Amended and Restated). Exhibit 10.69 to the Company’s Form 10-K for the year ended December 31, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
105
Table of Contents
| Exhibit |
Description of document | |
| 10.74** | Form of Kindred Healthcare, Inc. Non-Qualified Stock Option Grant Agreement under the 2001 Equity Plan for Non-Employee Directors (Amended and Restated). Exhibit 10.70 to the Company’s Form 10-K for the year ended December 31, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.75** | Form of Kindred Healthcare, Inc. Restricted Share Award Agreement under the 2001 Equity Plan for Non-Employee Directors (Amended and Restated). Exhibit 10.71 to the Company’s Form 10-K for the year ended December 31, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.76** | Form of Amendment No. 1 to Non-Discretionary Non-Qualified Stock Option Grant Agreement under the 2001 Equity Plan for Non-Employee Directors (Amended and Restated). Exhibit 10.72 to the Company’s Form 10-K for the year ended December 31, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.77** | Form of Amendment No. 1 to Discretionary Non-Qualified Stock Option Grant Agreement under the 2001 Equity Plan for Non-Employee Directors (Amended and Restated). Exhibit 10.73 to the Company’s Form 10-K for the year ended December 31, 2008 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.78 | Tax Matters Agreement, by and among AmerisourceBergen Corporation, PharMerica, Inc., Kindred Healthcare, Inc., Kindred Pharmacy Services, Inc. and Safari Holding Corporation, in each case on behalf of itself and its Affiliates. Exhibit 10.2 to the Company’s Current Report on Form 8-K dated October 25, 2006 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.79 | Commitment Letter, dated as of February 7, 2011, by and among JPMorgan Chase Bank, N.A., J.P. Morgan Securities LLC, Morgan Stanley Senior Funding, Inc., Citigroup Global Markets Inc. and Kindred Healthcare, Inc.. Exhibit 10.1 to the Company’s Current Report on Form 8-K dated February 7, 2011 (Comm. File No. 001-14057) is hereby incorporated by reference. | |
| 10.80 | Other Debt Instruments – Copies of debt instruments for which the related debt is less than 10% of total assets will be furnished to the SEC upon request. | |
| 21 | List of Subsidiaries. | |
| 23.1 | Consent of Independent Registered Public Accounting Firm. | |
| 31 | Rule 13a-14(a)/15d-14(a) Certifications. | |
| 32 | Section 1350 Certifications. | |
| * | The Company will furnish supplementally to the SEC upon request a copy of any omitted exhibit or annex. |
| ** | Compensatory plan or arrangement required to be filed as an exhibit pursuant to Item 15(b) of this Annual Report on Form 10-K. |
(b) Exhibits.
The response to this portion of Item 15 is submitted as a separate section of this Annual Report on Form 10-K.
(c) Financial Statement Schedules.
The response to this portion of Item 15 is included in appendix page F-42 of this Annual Report on Form 10-K.
106
Table of Contents
SIGNATURES
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized.
| Date: February 23, 2011 |
KINDRED HEALTHCARE, INC. | |||
| By: | /s/ Paul J. Diaz | |||
| Paul J. Diaz President and Chief Executive Officer | ||||
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed below by the following persons on behalf of the registrant and in the capacities and on the dates indicated.
| Signature |
Title |
Date | ||
| /s/ Joel Ackerman Joel Ackerman |
Director | February 23, 2011 | ||
| /s/ Ann C. Berzin Ann C. Berzin |
Director | February 23, 2011 | ||
| /s/ Jonathan D. Blum Jonathan D. Blum |
Director | February 23, 2011 | ||
| /s/ Thomas P. Cooper, M.D. Thomas P. Cooper, M.D. |
Director | February 23, 2011 | ||
| /s/ Isaac Kaufman Isaac Kaufman |
Director | February 23, 2011 | ||
| /s/ Frederick J. Kleisner Frederick J. Kleisner |
Director | February 23, 2011 | ||
| /s/ Eddy J. Rogers, Jr. Eddy J. Rogers, Jr. |
Director | February 23, 2011 | ||
| /s/ Phyllis R. Yale Phyllis R. Yale |
Director | February 23, 2011 | ||
| /s/ Edward L. Kuntz Edward L. Kuntz |
Chairman of the Board |
February 23, 2011 | ||
| /s/ Paul J. Diaz Paul J. Diaz |
Director, President and Chief Executive Officer (Principal Executive Officer) |
February 23, 2011 | ||
| /s/ Richard A. Lechleiter Richard A. Lechleiter |
Executive Vice President and Chief Financial Officer (Principal Financial Officer) |
February 23, 2011 | ||
| /s/ John J. Lucchese John J. Lucchese |
Senior Vice President and Corporate Controller (Principal Accounting Officer) |
February 23, 2011 | ||
107
Table of Contents
INDEX TO CONSOLIDATED FINANCIAL STATEMENTS
AND FINANCIAL STATEMENT SCHEDULES
| Page | ||||
| F-2 | ||||
| Consolidated Financial Statements: |
||||
| Consolidated Statement of Operations for the years ended December 31, 2010, 2009 and 2008 |
F-3 | |||
| F-4 | ||||
| Consolidated Statement of Stockholders’ Equity for the years ended December 31, 2010, 2009 and 2008 |
F-5 | |||
| Consolidated Statement of Cash Flows for the years ended December 31, 2010, 2009 and 2008 |
F-6 | |||
| F-7 | ||||
| F-40 | ||||
| Financial Statement Schedule (a): |
||||
| Schedule II – Valuation and Qualifying Accounts for the years ended December 31, 2010, 2009 and 2008 |
F-42 | |||
| (a) | All other schedules have been omitted because the required information is not present or not present in material amounts. |
F-1
Table of Contents
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
To the Board of Directors and Shareholders
of Kindred Healthcare, Inc.:
In our opinion, the consolidated financial statements listed in the index appearing under Item 15(a)(1) present fairly, in all material respects, the financial position of Kindred Healthcare, Inc. and its subsidiaries at December 31, 2010 and 2009, and the results of their operations and their cash flows for each of the three years in the period ended December 31, 2010 in conformity with accounting principles generally accepted in the United States of America. In addition, in our opinion, the financial statement schedule listed in the index appearing under Item 15(a)(2) presents fairly, in all material respects, the information set forth therein when read in conjunction with the related consolidated financial statements. Also in our opinion, the Company maintained, in all material respects, effective internal control over financial reporting as of December 31, 2010, based on criteria established in Internal Control — Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (COSO). The Company’s management is responsible for these financial statements and financial statement schedule, for maintaining effective internal control over financial reporting and for its assessment of the effectiveness of internal control over financial reporting, included in Management’s Annual Report on Internal Control over Financial Reporting under Item 9A. Our responsibility is to express opinions on these financial statements, on the financial statement schedule, and on the Company’s internal control over financial reporting based on our integrated audits. We conducted our audits in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audits to obtain reasonable assurance about whether the financial statements are free of material misstatement and whether effective internal control over financial reporting was maintained in all material respects. Our audits of the financial statements included examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements, assessing the accounting principles used and significant estimates made by management, and evaluating the overall financial statement presentation. Our audit of internal control over financial reporting included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, and testing and evaluating the design and operating effectiveness of internal control based on the assessed risk. Our audits also included performing such other procedures as we considered necessary in the circumstances. We believe that our audits provide a reasonable basis for our opinions.
A company’s internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company’s internal control over financial reporting includes those policies and procedures that (i) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (ii) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (iii) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company’s assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
/S/ PRICEWATERHOUSECOOPERS LLP
Louisville, Kentucky
February 23, 2011
F-2
Table of Contents
KINDRED HEALTHCARE, INC.
CONSOLIDATED STATEMENT OF OPERATIONS
(In thousands, except per share amounts)
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Revenues |
$ | 4,359,697 | $ | 4,270,007 | $ | 4,093,864 | ||||||
| Salaries, wages and benefits |
2,505,690 | 2,483,086 | 2,374,163 | |||||||||
| Supplies |
342,197 | 333,056 | 317,149 | |||||||||
| Rent |
357,372 | 348,248 | 338,673 | |||||||||
| Other operating expenses |
948,609 | 886,205 | 854,383 | |||||||||
| Other income |
(11,422 | ) | (11,512 | ) | (17,407 | ) | ||||||
| Depreciation and amortization |
121,552 | 125,730 | 120,022 | |||||||||
| Interest expense |
7,090 | 7,880 | 15,373 | |||||||||
| Investment income |
(1,245 | ) | (4,413 | ) | (7,096 | ) | ||||||
| 4,269,843 | 4,168,280 | 3,995,260 | ||||||||||
| Income from continuing operations before income taxes |
89,854 | 101,727 | 98,604 | |||||||||
| Provision for income taxes |
33,708 | 39,115 | 38,144 | |||||||||
| Income from continuing operations |
56,146 | 62,612 | 60,460 | |||||||||
| Discontinued operations, net of income taxes: |
||||||||||||
| Income (loss) from operations |
798 | 931 | (3,399 | ) | ||||||||
| Loss on divestiture of operations |
(453 | ) | (23,432 | ) | (20,776 | ) | ||||||
| Net income |
$ | 56,491 | $ | 40,111 | $ | 36,285 | ||||||
| Earnings per common share: |
||||||||||||
| Basic: |
||||||||||||
| Income from continuing operations |
$ | 1.42 | $ | 1.61 | $ | 1.56 | ||||||
| Discontinued operations: |
||||||||||||
| Income (loss) from operations |
0.02 | 0.02 | (0.09 | ) | ||||||||
| Loss on divestiture of operations |
(0.01 | ) | (0.60 | ) | (0.53 | ) | ||||||
| Net income |
$ | 1.43 | $ | 1.03 | $ | 0.94 | ||||||
| Diluted: |
||||||||||||
| Income from continuing operations |
$ | 1.42 | $ | 1.60 | $ | 1.54 | ||||||
| Discontinued operations: |
||||||||||||
| Income (loss) from operations |
0.02 | 0.02 | (0.09 | ) | ||||||||
| Loss on divestiture of operations |
(0.01 | ) | (0.60 | ) | (0.53 | ) | ||||||
| Net income |
$ | 1.43 | $ | 1.02 | $ | 0.92 | ||||||
| Shares used in computing earnings per common share: |
||||||||||||
| Basic |
38,738 | 38,339 | 37,830 | |||||||||
| Diluted |
38,954 | 38,502 | 38,397 | |||||||||
See accompanying notes.
F-3
Table of Contents
KINDRED HEALTHCARE, INC.
(In thousands, except per share amounts)
| December 31, 2010 |
December 31, 2009 |
|||||||
| ASSETS | ||||||||
| Current assets: |
||||||||
| Cash and cash equivalents |
$ | 17,168 | $ | 16,303 | ||||
| Cash–restricted |
5,494 | 5,820 | ||||||
| Insurance subsidiary investments |
76,753 | 106,834 | ||||||
| Accounts receivable less allowance for loss of $13,584 – 2010 and $20,156 – 2009 |
631,877 | 610,959 | ||||||
| Inventories |
24,327 | 22,303 | ||||||
| Deferred tax assets |
13,439 | 42,791 | ||||||
| Income taxes |
42,118 | 17,447 | ||||||
| Other |
24,862 | 21,194 | ||||||
| 836,038 | 843,651 | |||||||
| Property and equipment, at cost: |
||||||||
| Land |
65,431 | 47,912 | ||||||
| Buildings |
950,957 | 787,803 | ||||||
| Equipment |
669,365 | 613,344 | ||||||
| Construction in progress |
68,417 | 66,641 | ||||||
| 1,754,170 | 1,515,700 | |||||||
| Accumulated depreciation |
(857,623 | ) | (765,602 | ) | ||||
| 896,547 | 750,098 | |||||||
| Goodwill |
242,420 | 81,223 | ||||||
| Intangible assets less accumulated amortization of $3,731 – 2010 and $2,647 – 2009 |
92,883 | 64,491 | ||||||
| Assets held for sale |
7,167 | 8,806 | ||||||
| Insurance subsidiary investments |
101,210 | 100,223 | ||||||
| Deferred tax assets |
88,816 | 110,930 | ||||||
| Other |
72,334 | 62,802 | ||||||
| $ | 2,337,415 | $ | 2,022,224 | |||||
| LIABILITIES AND STOCKHOLDERS’ EQUITY | ||||||||
| Current liabilities: |
||||||||
| Accounts payable |
$ | 174,495 | $ | 161,066 | ||||
| Salaries, wages and other compensation |
291,116 | 287,772 | ||||||
| Due to third party payors |
27,115 | 28,261 | ||||||
| Professional liability risks |
41,555 | 47,076 | ||||||
| Other accrued liabilities |
87,012 | 78,358 | ||||||
| Long-term debt due within one year |
91 | 86 | ||||||
| 621,384 | 602,619 | |||||||
| Long-term debt |
365,556 | 147,647 | ||||||
| Professional liability risks |
207,669 | 195,126 | ||||||
| Deferred credits and other liabilities |
111,047 | 110,238 | ||||||
| Commitments and contingencies |
||||||||
| Stockholders’ equity: |
||||||||
| Preferred stock, $0.25 par value; authorized 1,000 shares; none issued and outstanding |
– | – | ||||||
| Common stock, $0.25 par value; authorized 175,000 shares; issued 39,495 shares – 2010 and 39,104 shares – 2009 |
9,874 | 9,776 | ||||||
| Capital in excess of par value |
828,593 | 820,407 | ||||||
| Accumulated other comprehensive income (loss) |
135 | (423 | ) | |||||
| Retained earnings |
193,157 | 136,834 | ||||||
| 1,031,759 | 966,594 | |||||||
| $ | 2,337,415 | $ | 2,022,224 | |||||
See accompanying notes.
F-4
Table of Contents
KINDRED HEALTHCARE, INC.
CONSOLIDATED STATEMENT OF STOCKHOLDERS’ EQUITY
(In thousands)
| Shares of common stock |
Par value common stock |
Capital in excess of par value |
Accumulated other comprehensive income/(loss) |
Retained earnings |
Total | |||||||||||||||||||
| Balances, December 31, 2007 |
38,339 | $ | 9,585 | $ | 790,367 | $ | 1,250 | $ | 60,922 | $ | 862,124 | |||||||||||||
| Comprehensive income: |
||||||||||||||||||||||||
| Net income |
36,285 | 36,285 | ||||||||||||||||||||||
| Net unrealized investment losses, net of income taxes |
(3,044 | ) | (3,044 | ) | ||||||||||||||||||||
| Other |
(1,825 | ) | (1,825 | ) | ||||||||||||||||||||
| Comprehensive income |
31,416 | |||||||||||||||||||||||
| Grant of non-vested restricted stock |
166 | 41 | (41 | ) | – | |||||||||||||||||||
| Issuance of common stock in connection with employee benefit plans |
504 | 126 | 9,016 | (277 | ) | 8,865 | ||||||||||||||||||
| Shares tendered by employees for statutory tax withholdings upon issuance of common stock |
(100 | ) | (25 | ) | (2,326 | ) | (53 | ) | (2,404 | ) | ||||||||||||||
| Stock-based compensation amortization |
12,637 | 12,637 | ||||||||||||||||||||||
| Pre-emergence income tax liability adjustment |
1,385 | 1,385 | ||||||||||||||||||||||
| Income tax benefit in connection with the issuance of common stock under employee benefit plans |
1,103 | 1,103 | ||||||||||||||||||||||
| Other |
(151 | ) | (151 | ) | ||||||||||||||||||||
| Balances, December 31, 2008 |
38,909 | 9,727 | 812,141 | (3,619 | ) | 96,726 | 914,975 | |||||||||||||||||
| Comprehensive income: |
||||||||||||||||||||||||
| Net income |
40,111 | 40,111 | ||||||||||||||||||||||
| Net unrealized investment gains, net of income taxes |
1,230 | 1,230 | ||||||||||||||||||||||
| Other |
1,966 | 1,966 | ||||||||||||||||||||||
| Comprehensive income |
43,307 | |||||||||||||||||||||||
| Grant of non-vested restricted stock |
196 | 49 | (49 | ) | – | |||||||||||||||||||
| Issuance of common stock in connection with employee benefit plans |
104 | 26 | 931 | 957 | ||||||||||||||||||||
| Shares tendered by employees for statutory tax withholdings upon issuance of common stock |
(105 | ) | (26 | ) | (1,512 | ) | (3 | ) | (1,541 | ) | ||||||||||||||
| Stock-based compensation amortization |
9,905 | 9,905 | ||||||||||||||||||||||
| Income tax provision in connection with the issuance of common stock under employee benefit plans |
(1,009 | ) | (1,009 | ) | ||||||||||||||||||||
| Balances, December 31, 2009 |
39,104 | 9,776 | 820,407 | (423 | ) | 136,834 | 966,594 | |||||||||||||||||
| Comprehensive income: |
||||||||||||||||||||||||
| Net income |
56,491 | 56,491 | ||||||||||||||||||||||
| Net unrealized investment gains, net of income taxes |
1,229 | 1,229 | ||||||||||||||||||||||
| Other |
(671 | ) | (671 | ) | ||||||||||||||||||||
| Comprehensive income |
57,049 | |||||||||||||||||||||||
| Grant of non-vested restricted stock |
425 | 106 | (106 | ) | – | |||||||||||||||||||
| Issuance of common stock in connection with employee benefit plans |
96 | 24 | 25 | 49 | ||||||||||||||||||||
| Shares tendered by employees for statutory tax withholdings upon issuance of common stock |
(130 | ) | (32 | ) | (2,147 | ) | (168 | ) | (2,347 | ) | ||||||||||||||
| Stock-based compensation amortization |
10,714 | 10,714 | ||||||||||||||||||||||
| Income tax provision in connection with the issuance of common stock under employee benefit plans |
(300 | ) | (300 | ) | ||||||||||||||||||||
| Balances, December 31, 2010 |
39,495 | $ | 9,874 | $ | 828,593 | $ | 135 | $ | 193,157 | $ | 1,031,759 | |||||||||||||
See accompanying notes.
F-5
Table of Contents
KINDRED HEALTHCARE, INC.
CONSOLIDATED STATEMENT OF CASH FLOWS
(In thousands)
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Cash flows from operating activities: |
||||||||||||
| Net income |
$ | 56,491 | $ | 40,111 | $ | 36,285 | ||||||
| Adjustments to reconcile net income to net cash provided by operating activities: |
||||||||||||
| Depreciation and amortization |
121,552 | 126,404 | 122,265 | |||||||||
| Amortization of stock-based compensation costs |
10,714 | 9,905 | 12,637 | |||||||||
| Provision for doubtful accounts |
24,397 | 29,320 | 32,336 | |||||||||
| Deferred income taxes |
21,446 | 10,876 | 20,793 | |||||||||
| Loss on divestiture of discontinued operations |
453 | 23,432 | 20,776 | |||||||||
| Other |
252 | (1,186 | ) | 1,029 | ||||||||
| Change in operating assets and liabilities: |
||||||||||||
| Accounts receivable |
(45,232 | ) | (29,247 | ) | (46,610 | ) | ||||||
| Inventories and other assets |
(14,294 | ) | (17,386 | ) | (11,489 | ) | ||||||
| Accounts payable |
9,446 | (4,088 | ) | (13,953 | ) | |||||||
| Income taxes |
3,462 | 35,009 | 9,052 | |||||||||
| Due to third party payors |
1,213 | (6,369 | ) | (8,309 | ) | |||||||
| Other accrued liabilities |
20,088 | 16,939 | (2,527 | ) | ||||||||
| Net cash provided by operating activities |
209,988 | 233,720 | 172,285 | |||||||||
| Cash flows from investing activities: |
||||||||||||
| Routine capital expenditures |
(108,896 | ) | (97,550 | ) | (109,926 | ) | ||||||
| Development capital expenditures |
(67,841 | ) | (48,058 | ) | (38,751 | ) | ||||||
| Acquisitions |
(279,794 | ) | (83,432 | ) | (48,824 | ) | ||||||
| Sale of assets |
649 | 25,967 | 27,984 | |||||||||
| Purchase of insurance subsidiary investments |
(43,913 | ) | (103,477 | ) | (121,693 | ) | ||||||
| Sale of insurance subsidiary investments |
82,736 | 122,410 | 119,810 | |||||||||
| Net change in insurance subsidiary cash and cash equivalents |
(8,521 | ) | 22,005 | 31,064 | ||||||||
| Change in other investments |
2 | 2,002 | 7,002 | |||||||||
| Other |
962 | 3,538 | 2,568 | |||||||||
| Net cash used in investing activities |
(424,616 | ) | (156,595 | ) | (130,766 | ) | ||||||
| Cash flows from financing activities: |
||||||||||||
| Proceeds from borrowings under revolving credit |
2,030,800 | 1,214,400 | 1,498,000 | |||||||||
| Repayment of borrowings under revolving credit |
(1,812,800 | ) | (1,416,100 | ) | (1,424,300 | ) | ||||||
| Repayment of capital lease obligation |
– | – | (16,268 | ) | ||||||||
| Payment of deferred financing costs |
(2,831 | ) | (855 | ) | (508 | ) | ||||||
| Issuance of common stock |
49 | 957 | 8,865 | |||||||||
| Other |
275 | (19 | ) | 610 | ||||||||
| Net cash provided by (used in) financing activities |
215,493 | (201,617 | ) | 66,399 | ||||||||
| Change in cash and cash equivalents |
865 | (124,492 | ) | 107,918 | ||||||||
| Cash and cash equivalents at beginning of period |
16,303 | 140,795 | 32,877 | |||||||||
| Cash and cash equivalents at end of period |
$ | 17,168 | $ | 16,303 | $ | 140,795 | ||||||
| Supplemental information: |
||||||||||||
| Interest payments |
$ | 5,261 | $ | 6,122 | $ | 14,661 | ||||||
| Income tax payments (refunds) |
11,961 | (4,480 | ) | 7,590 | ||||||||
| Rental payments to Ventas, Inc. |
246,392 | 243,011 | 239,367 | |||||||||
See accompanying notes.
F-6
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS
NOTE 1 – ACCOUNTING POLICIES
Reporting entity
Kindred Healthcare, Inc. is a healthcare services company that through its subsidiaries operates hospitals, nursing and rehabilitation centers, assisted living facilities and a contract rehabilitation services business across the United States (collectively, “Kindred” or the “Company”).
Basis of presentation
The consolidated financial statements include all subsidiaries. All intercompany transactions have been eliminated. Investments in affiliates in which the Company has a 50% or less interest are accounted for by either the equity or cost method.
In recent years, the Company has completed several transactions related to the divestiture of unprofitable hospitals and nursing and rehabilitation centers. For accounting purposes, the operating results of these businesses and the losses or impairments associated with these transactions have been classified as discontinued operations in the accompanying consolidated statement of operations for all periods presented. Assets not sold at December 31, 2010 have been measured at the lower of carrying value or estimated fair value less costs of disposal and have been classified as held for sale in the accompanying consolidated balance sheet. See Notes 3 and 4.
The consolidated financial statements have been prepared in accordance with generally accepted accounting principles and include amounts based upon the estimates and judgments of management. Actual amounts may differ from those estimates.
Recently issued accounting requirements
In December 2010, the Financial Accounting Standards Board (the “FASB”) issued authoritative guidance related to goodwill and other intangibles. The provisions of the guidance modify Step 1 of the goodwill impairment test for reporting units with zero or negative carrying amounts. For those reporting units, an entity is required to perform Step 2 of the goodwill impairment test if it is more likely than not that a goodwill impairment exists. In determining if it is more likely than not that a goodwill impairment exists, an entity should consider whether there are any adverse qualitative factors indicating that an impairment may exist. The guidance is effective for all interim and annual reporting periods beginning after December 15, 2010. The adoption of the guidance is not expected to have a material impact on the Company’s business, financial position, results of operations or liquidity.
In December 2010, the FASB issued authoritative guidance related to business combinations. The provisions of the guidance specify that if a public entity presents comparative financial statements, the entity should disclose revenue and earnings of the combined entity as though the business combination(s) that occurred during the current year had occurred as of the beginning of the comparable prior year annual reporting period only. Supplemental pro forma disclosures have also been expanded to include a description of the nature and amount of material, non-recurring pro forma adjustments included in the pro forma financial statements. The guidance is effective prospectively for business combinations with an acquisition date on or after the beginning of the first annual reporting period beginning on or after December 15, 2010. The adoption of the guidance is not expected to have a material impact on the Company’s business, financial position, results of operations or liquidity.
In January 2010, the FASB issued authoritative guidance related to fair value measurements and disclosures. The provisions of the guidance require new disclosures related to transfers in and out of Levels 1 and 2 classifications (as described in Note 16). The provisions also require a reconciliation of the activity in Level 3 (as described in Note 16) recurring fair value measurements. Existing disclosures also were expanded to include Level 2 fair value measurement valuation techniques and inputs. The guidance is effective for all interim and
F-7
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 1 – ACCOUNTING POLICIES (Continued)
Recently issued accounting requirements (Continued)
annual reporting periods beginning after December 15, 2009, except for the disclosures for Level 3 activity which is effective for fiscal years beginning after December 15, 2010. The adoption of the guidance did not, and is not expected to, have a material impact on the Company’s business, financial position, results of operations or liquidity.
In June 2009, the FASB issued revised authoritative guidance related to the consolidation criteria for variable interest entities (“VIE”). The guidance, among other things, requires a qualitative rather than a quantitative analysis to determine the primary beneficiary of a VIE; requires continuous assessments of whether an enterprise is the primary beneficiary of a VIE; enhances disclosures regarding an enterprise’s involvement with a VIE; and amends certain guidance for determining whether an entity is a VIE. Under the guidance, a VIE must be consolidated if the enterprise has both (a) the power to direct the activities of the VIE that most significantly impact the entity’s economic performance, and (b) the obligation to absorb losses or the right to receive benefits from the VIE that could potentially be significant to the VIE. The guidance was effective as of January 1, 2010. The adoption of the guidance did not, and is not expected to, have a material impact on the Company’s business, financial position, results of operations or liquidity.
Upon adoption of the VIE guidance on January 1, 2010, the Company reassessed its three investment partnerships and its lease agreements under the new accounting guidance. Although the investment partnerships were determined to be VIEs, they do not require the Company to absorb losses or receive benefits that could potentially be significant to the VIEs, nor can the Company direct the activities that most significantly impact the VIEs’ economic performance. As a result, the investment partnerships continue to be accounted for under the equity method of accounting and are not consolidated. The Company also determined that three of its lease agreements were considered VIEs. However, the Company is not the primary beneficiary of these leases as it lacks the power to direct activities of the lessor that most significantly impact the economic performance under these leases. In addition, the Company’s investments and involvement in lease arrangements related to these VIEs were not significant to its consolidated financial statements.
Reclassifications
Certain prior year amounts have been reclassified to conform with the current year presentation.
Revenues
Revenues are recorded based upon estimated amounts due from patients and third party payors for healthcare services provided, including anticipated settlements under reimbursement agreements with Medicare, Medicaid, Medicare Advantage and other third party payors.
A summary of revenues by payor type follows (in thousands):
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Medicare |
$ | 1,882,365 | $ | 1,817,117 | $ | 1,743,447 | ||||||
| Medicaid |
1,059,118 | 1,086,901 | 1,075,645 | |||||||||
| Medicare Advantage |
345,026 | 321,437 | 263,699 | |||||||||
| Other |
1,379,652 | 1,332,817 | 1,275,148 | |||||||||
| 4,666,161 | 4,558,272 | 4,357,939 | ||||||||||
| Eliminations |
(306,464 | ) | (288,265 | ) | (264,075 | ) | ||||||
| $ | 4,359,697 | $ | 4,270,007 | $ | 4,093,864 | |||||||
F-8
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 1 – ACCOUNTING POLICIES (Continued)
Cash and cash equivalents
Cash and cash equivalents include highly liquid investments with an original maturity of three months or less when purchased.
Insurance subsidiary investments
The Company maintains investments for the payment of claims and expenses related to professional liability and workers compensation risks. These investments have been categorized as available-for-sale and are reported at fair value. The fair value of publicly traded debt and equity securities and money market funds are based upon quoted market prices or observable inputs such as interest rates using either a market or income valuation approach. Since the Company’s insurance subsidiary investments are restricted for a limited purpose, they are classified in the accompanying consolidated balance sheet based upon the expected current and long-term cash requirements of the limited purpose insurance subsidiary.
The Company follows the authoritative guidance related to the meaning of other-than-temporary impairment and its application to certain investments to assess whether the Company’s investments with unrealized loss positions are other-than-temporarily impaired. Unrealized gains and losses, net of deferred income taxes, are reported as a component of accumulated other comprehensive income (loss). Realized gains and losses and declines in value judged to be other-than-temporary are determined using the specific identification method and are reported in the Company’s statement of operations. See Note 9.
Accounts receivable
Accounts receivable consist primarily of amounts due from the Medicare and Medicaid programs, other government programs, managed care health plans, commercial insurance companies and individual patients and customers. Estimated provisions for doubtful accounts are recorded to the extent it is probable that a portion or all of a particular account will not be collected.
In evaluating the collectibility of accounts receivable, the Company considers a number of factors, including the age of the accounts, changes in collection patterns, the composition of patient accounts by payor type, the status of ongoing disputes with third party payors and general industry conditions. Actual collections of accounts receivable in subsequent periods may require changes in the estimated provision for loss. Changes in these estimates are charged or credited to the results of operations in the period of change.
The provision for doubtful accounts totaled $24.2 million for 2010, $28.7 million for 2009 and $30.8 million for 2008.
Due to third party payors
The Company’s hospitals and nursing and rehabilitation centers are required to submit cost reports at least annually to various state and federal agencies administering the respective reimbursement programs. In many instances, interim cash payments to the Company are only an estimate of the amount due for services provided. Any overpayment to the Company arising from the completion of a cost report is recorded as a liability.
Inventories
Inventories consist primarily of pharmaceutical and medical supplies and are stated at the lower of cost (first-in, first-out) or market.
F-9
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 1 – ACCOUNTING POLICIES (Continued)
Property and equipment
Property and equipment is carried at cost less accumulated depreciation. Depreciation expense, computed by the straight-line method, was $120.3 million for 2010, $124.8 million for 2009 and $119.1 million for 2008. Depreciation rates for buildings range generally from 20 to 45 years. Leasehold improvements are depreciated over their estimated useful lives or the remaining lease term, whichever is shorter. Estimated useful lives of equipment vary from five to 15 years. Depreciation expense is not recorded for property and equipment classified as held for sale.
Interest costs incurred during the construction of the Company’s development projects are capitalized. Capitalized interest for the years ended December 31, 2010, 2009 and 2008 was $1.3 million, $2.2 million and $2.9 million, respectively. Repairs and maintenance are expensed as incurred.
The Company separates capital expenditures into two categories, routine and development, in the accompanying consolidated statement of cash flows. Purchases of routine property and equipment include expenditures at existing facilities that generally do not result in increased capacity or the expansion of services. Development capital expenditures include expenditures for the development of new facilities or the expansion of services or capacity at existing facilities.
Long-lived assets
The Company regularly reviews the carrying value of certain long-lived assets and identifiable finite lived intangible assets with respect to any events or circumstances that indicate an impairment or an adjustment to the amortization period is necessary. If circumstances suggest that the recorded amounts cannot be recovered based upon estimated future undiscounted cash flows, the carrying values of such assets are reduced to fair value.
In assessing the carrying values of long-lived assets, the Company estimates future cash flows at the lowest level for which there are independent, identifiable cash flows. For this purpose, these cash flows are aggregated based upon the contractual agreements underlying the operation of the facility or group of facilities. Generally, an individual facility is considered the lowest level for which there are independent, identifiable cash flows. However, to the extent that groups of facilities are leased under a master lease agreement in which the operations of a facility and compliance with the lease terms are interdependent upon other facilities in the agreement (including the Company’s ability to renew the lease or divest a particular property), the Company defines the group of facilities under a master lease agreement as the lowest level for which there are independent, identifiable cash flows. Accordingly, the estimated cash flows of all facilities within a master lease agreement are aggregated for purposes of evaluating the carrying values of long-lived assets.
Goodwill and other intangible assets
Intangible assets are comprised primarily of goodwill, certificates of need, Medicare certifications and trade names primarily originating from business combinations accounted for as purchase transactions.
A summary of goodwill by reporting unit follows (in thousands):
| Hospitals | Nursing and rehabilitation centers |
Rehabilitation services |
Home health |
Hospice | Total | |||||||||||||||||||
| Balances, December 31, 2008 |
$ | 68,577 | $ | 639 | $ | 1,863 | $ | – | $ | 1,165 | $ | 72,244 | ||||||||||||
| Acquisitions |
– | – | – | – | 6,917 | 6,917 | ||||||||||||||||||
| Other |
– | 250 | 1,500 | – | 312 | 2,062 | ||||||||||||||||||
| Balances, December 31, 2009 |
68,577 | 889 | 3,363 | – | 8,394 | 81,223 | ||||||||||||||||||
| Acquisitions |
144,325 | 5,191 | – | 11,383 | – | 160,899 | ||||||||||||||||||
| Other |
298 | – | – | – | – | 298 | ||||||||||||||||||
| Balances, December 31, 2010 |
$ | 213,200 | $ | 6,080 | $ | 3,363 | $ | 11,383 | $ | 8,394 | $ | 242,420 | ||||||||||||
F-10
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 1 – ACCOUNTING POLICIES (Continued)
Goodwill and other intangible assets (Continued)
In accordance with the authoritative guidance for goodwill and other intangible assets, the Company is required to perform an impairment test for goodwill and indefinite lived intangible assets at least annually or more frequently if adverse events or changes in circumstances indicate that the asset may be impaired.
The Company performs its annual goodwill impairment test at the end of each fiscal year for each of its reporting units. A reporting unit is either an operating segment or one level below the operating segment, referred to as a component. When the components within the Company’s operating segments have similar economic characteristics, the Company aggregates the components of its operating segments into one reporting unit. Accordingly, the Company has determined that its reporting units are hospitals, nursing and rehabilitation centers, rehabilitation services, home health and hospice.
The goodwill impairment test involves a two-step process. The first step is a comparison of each reporting unit’s fair value to its carrying value. If the carrying value of the reporting unit is greater than its fair value, there is an indication that impairment may exist and the second step must be performed to measure the amount of impairment loss. Based upon the results of the step one impairment test for goodwill and the impairment test of indefinite lived intangible assets in each of the last three years, no impairment charges were recorded in connection with the Company’s annual impairment tests.
Since quoted market prices for the Company’s reporting units are not available, the Company applied judgment in determining the fair value of these reporting units for purposes of performing the goodwill impairment test. The Company relied on widely accepted valuation techniques, including equally weighted discounted cash flow and market multiple analyses approaches, which capture both the future income potential of the reporting unit and the market behaviors and actions of market participants in the industry that includes the reporting unit. These types of analyses require the Company to make assumptions and estimates regarding future cash flows, industry-specific economic factors and the profitability of future business strategies. The discounted cash flow approach uses a projection of estimated operating results and cash flows that are discounted using a weighted average cost of capital. Under the discounted cash flow approach, the projection uses management’s best estimates of economic and market conditions over the projected period for each reporting unit including growth rates in the number of admissions, patient days, reimbursement rates, operating costs, rent expense and capital expenditures. Other significant estimates and assumptions include terminal value growth rates, changes in working capital requirements and weighted average cost of capital. The market multiple analysis estimates fair value by applying cash flow multiples to the reporting unit’s operating results. The multiples are derived from comparable publicly traded companies with similar operating and investment characteristics to the reporting units.
The Company’s analysis indicated that the estimated fair value of each reporting unit exceeded its book equity value. The Company’s conclusions were supported by both quantitative and qualitative factors, including the estimate of an implied control premium for acquisitions in the Company’s industry, the Company’s fourth quarter operating results that exceeded investment analyst expectations and consideration of the Company’s updated business expectations at December 31, 2010 and 2009.
The Company’s indefinite lived intangible assets consist primarily of certificates of need, which are estimated primarily using an excess earnings method, a form of discounted cash flows, which is based upon the concept that net after-tax cash flows provide a return supporting all of the assets of a business enterprise. The carrying value of the Company’s certificates of need at December 31, 2010 was $66.5 million. The fair values of the Company’s indefinite lived intangible assets are derived from current market data and projections at a facility level which include management’s best estimates of economic and market conditions over the projected period including growth rates in the number of admissions, patient days, reimbursement rates, operating costs, rent
F-11
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 1 – ACCOUNTING POLICIES (Continued)
Goodwill and other intangible assets (Continued)
expense and capital expenditures. Other significant estimates and assumptions include terminal value growth rates, changes in working capital requirements and weighted average cost of capital. At December 31, 2010, the fair value of the Company’s certificates of need intangible assets exceeded its carrying value. In conjunction with two acquisitions consummated in November 2010, the Company also acquired Medicare certifications with indefinite lives totaling $18.1 million. However, an impairment analysis was not conducted because there were no triggering events between the acquisition dates and December 31, 2010.
The Company’s other intangible assets include both finite and indefinite lived intangible assets. The Company’s other intangible assets with finite lives are amortized under the authoritative guidance for goodwill and other intangible assets using the straight-line method over their estimated useful lives ranging from one to 20 years. A summary of intangible assets at December 31 follows (in thousands):
| 2010 | 2009 | |||||||||||||||||||||||||||||||
| Cost | Accumulated amortization |
Carrying value |
Weighted average life |
Cost | Accumulated amortization |
Carrying value |
Weighted average life |
|||||||||||||||||||||||||
| Current: |
||||||||||||||||||||||||||||||||
| Employment contracts |
$ | 945 | $ | (278 | ) | $ | 667 | 1 year | $ | 186 | $ | (182 | ) | $ | 4 | 1 year | ||||||||||||||||
| Non-current: |
||||||||||||||||||||||||||||||||
| Certificates of need (indefinite life) |
66,453 | – | 66,453 | 61,856 | – | 61,856 | ||||||||||||||||||||||||||
| Medicare certifications (indefinite life) |
18,979 | – | 18,979 | 919 | – | 919 | ||||||||||||||||||||||||||
| Leasehold interests |
1,100 | (51 | ) | 1,049 | 4 years | – | – | – | ||||||||||||||||||||||||
| Customer relationship assets |
1,044 | (805 | ) | 239 | 4 years | 1,044 | (558 | ) | 486 | 4 years | ||||||||||||||||||||||
| Non-compete agreements |
4,033 | (2,726 | ) | 1,307 | 5 years | 2,994 | (2,076 | ) | 918 | 5 years | ||||||||||||||||||||||
| Trade names |
5,005 | (149 | ) | 4,856 | 13 years | 325 | (13 | ) | 312 | 10 years | ||||||||||||||||||||||
| 96,614 | (3,731 | ) | 92,883 | 67,138 | (2,647 | ) | 64,491 | |||||||||||||||||||||||||
| $ | 97,559 | $ | (4,009 | ) | $ | 93,550 | $ | 67,324 | $ | (2,829 | ) | $ | 64,495 | |||||||||||||||||||
Amortization expense computed by the straight-line method totaled $1.3 million for 2010 and $0.9 million for both 2009 and 2008.
Estimated annual amortization expense for intangible assets at December 31, 2010 will approximate $1.9 million, $1.0 million, $0.9 million, $0.6 million and $0.6 million for the years 2011, 2012, 2013, 2014 and 2015, respectively.
Insurance risks
Provisions for loss for professional liability risks and workers compensation risks are based upon management’s best available information including actuarially determined estimates. The provisions for loss related to professional liability risks retained by the Company’s wholly owned limited purpose insurance subsidiary are discounted based upon actuarial estimates of claim payment patterns. Provisions for loss related to workers compensation risks retained by the Company’s limited purpose insurance subsidiary are not discounted. To the extent that expected ultimate claims costs vary from historical provisions for loss, future earnings will be charged or credited. See Notes 4 and 8.
F-12
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 1 – ACCOUNTING POLICIES (Continued)
Earnings per common share
Earnings per common share are based upon the weighted average number of common shares outstanding during the respective periods. The diluted calculation of earnings per common share includes the dilutive effect of stock options and performance-based restricted shares. On January 1, 2009, the Company adopted the provisions of the authoritative guidance for determining whether instruments granted in share-based payment transactions are participating securities for purposes of calculating earnings per common share. See Note 5.
Stock option accounting
The Company recognizes compensation expense in its consolidated financial statements using a Black-Scholes option valuation model for non-vested stock options. See Note 13.
Other information
The Company has performed an evaluation of subsequent events through the date on which the financial statements were issued.
NOTE 2 – ACQUISITIONS
The following is a summary of the Company’s significant acquisition activities. The operating results of the acquired businesses have been included in the accompanying consolidated financial statements of the Company from the respective acquisition dates. The purchase price of the acquired businesses and acquired leased facilities resulted from negotiations with each of the sellers that were based upon both the historical and expected future cash flows of the respective businesses and real estate values. All of these acquisitions were financed through operating cash flows or borrowings under the Company’s revolving credit facility. Unaudited pro forma operating results are only provided for newly acquired businesses that are material to the Company’s consolidated financial statements.
Vista Acquisition
In November 2010, the Company acquired five LTAC hospitals from Vista Healthcare, LLC (“Vista”) for a purchase price of $179.0 million in cash (the “Vista Acquisition”). The Vista Acquisition included four freestanding hospitals and one hospital-in-hospital with a total of 250 beds, all of which are located in southern California. The Company did not acquire the working capital of Vista or assume any of its liabilities. All of the Vista hospitals are leased.
Vista’s results of operations have been included in the Company’s consolidated financial statements since November 1, 2010 and consisted of revenues of $24.3 million and pretax income of $1.5 million. Vista’s operations have been included in the hospital division business segment.
The purchase price was allocated to the estimated fair value of tangible and intangible assets, with the remainder allocated to goodwill. The primary factors in the decision to acquire Vista were the opportunity to meet the growing demand for the Company’s services in southern California and expand the Company’s hospital operations. The Vista hospitals also provide several clinical service offerings not currently available in the Company’s hospitals providing an opportunity to expand its clinical services as well as attract new sources of business.
The purchase price included consideration of $10 million held in escrow associated with the representations, warranties and covenants of the seller for 24 months following the acquisition date.
F-13
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 2 – ACQUISITIONS (Continued)
Vista Acquisition (Continued)
The following is the Vista Acquisition purchase price allocation (in thousands):
| Inventory |
$ | 1,546 | ||
| Property and equipment |
11,710 | |||
| Identifiable intangible assets: |
||||
| Medicare certifications (indefinite life) |
17,160 | |||
| Trade name |
1,830 | |||
| Leasehold interests |
1,100 | |||
| Non-compete agreements |
720 | |||
| Deposits and other |
620 | |||
| Goodwill |
144,325 | |||
| $ | 179,011 | |||
The weighted average life of the definite lived intangible assets is four years.
The total goodwill arising from the acquisition is based upon the expected future cash flows of the Vista operations which reflects both growth expectations and cost savings from combining the operations of the Company and Vista. Goodwill is expected to be deductible for income tax purposes over a life of 15 years. All of the goodwill was assigned to the Company’s hospital reporting unit.
The unaudited pro forma net effect of the Vista Acquisition assuming the acquisition occurred as of January 1, 2008 is as follows (in thousands except per share amounts):
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Revenues |
$ | 4,489,092 | $ | 4,416,342 | $ | 4,228,081 | ||||||
| Income from continuing operations |
66,195 | 73,452 | 66,521 | |||||||||
| Net income |
66,540 | 50,951 | 42,346 | |||||||||
| Earnings per common share: |
||||||||||||
| Basic: |
||||||||||||
| Income from continuing operations |
$ | 1.68 | $ | 1.88 | $ | 1.72 | ||||||
| Net income |
$ | 1.69 | $ | 1.30 | $ | 1.10 | ||||||
| Diluted: |
||||||||||||
| Income from continuing operations |
$ | 1.67 | $ | 1.88 | $ | 1.70 | ||||||
| Net income |
$ | 1.68 | $ | 1.30 | $ | 1.08 | ||||||
The unaudited pro forma financial data has been derived by combining the historical financial results of the Company and the operations acquired in the Vista Acquisition for the periods presented.
Other 2010 acquisitions
In November 2010, the Company acquired a home health company for $12.9 million, which included $11.4 million of goodwill, $1.4 million of identifiable intangible assets and $0.1 million of other assets.
In September 2010, the Company acquired three nursing and rehabilitation centers for $37.7 million, which included $5.0 million of goodwill, $2.5 million of identifiable intangible assets and $30.2 million of property and equipment and other assets.
F-14
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 2 – ACQUISITIONS (Continued)
Other 2010 acquisitions (Continued)
In March 2010, the Company acquired a combined nursing and rehabilitation center and assisted living facility for $16.6 million, which included $0.2 million of goodwill, $2.2 million of identifiable intangible assets and $14.2 million of property and equipment and other assets.
In January 2010, the Company acquired the real estate of two previously leased hospitals and two previously leased nursing and rehabilitation centers for $31.1 million in cash and $2.4 million in unamortized prepaid rent. Annual rents associated with these four facilities aggregated $2.9 million.
During 2010, the Company incurred $4.6 million in acquisition-related costs. These costs were charged to the Company’s business segments as follows:
| Hospital division |
$ | 3,257 | ||
| Nursing center division |
704 | |||
| Rehabilitation division |
683 | |||
| $ | 4,644 | |||
The fair value of each of the acquisitions completed during the year ended December 31, 2010 were measured using primarily discounted cash flow methodologies, a Level 3 (as described in Note 16) measurement technique.
2009 acquisitions
In July 2009, the Company acquired a hospice business for $8.0 million, which included $6.9 million of goodwill, $0.9 million of identifiable intangible assets and $0.2 million of equipment. The fair value of the assets acquired were measured using primarily discounted cash flow methodologies, a Level 3 (as described in Note 16) measurement technique.
In March 2009, the Company also acquired the real estate of a previously leased hospital for $15.6 million in cash and $1.6 million in unamortized prepaid rent. Annual rent associated with this facility aggregated $1.8 million. The fair value of the assets acquired were measured using Level 2 (as described in Note 16) observable inputs, including replacement costs and direct sales comparisons of similar properties in the same geographic market or region.
2008 acquisitions
In April 2008, the Company acquired the real estate of four previously leased nursing and rehabilitation centers for $23.9 million. Annual rents associated with these facilities approximated $2.6 million. The fair value of the assets acquired were measured using Level 2 (as described in Note 16) observable inputs, including replacement costs and direct sales comparisons of similar properties in the same geographic market or region.
NOTE 3 – DIVESTITURES
In recent years, the Company has completed certain strategic divestitures to improve its future operating results. For accounting purposes, the operating results of these businesses and the losses or impairments associated with these transactions have been classified as discontinued operations in the accompanying consolidated statement of operations for all periods presented. See Note 4.
F-15
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 3 – DIVESTITURES (Continued)
2009 divestitures
In June 2009, the Company purchased for resale six under-performing nursing and rehabilitation centers (the “Nursing Centers”) previously leased from Ventas, Inc. (“Ventas”) for $55.7 million. In addition, the Company paid Ventas a lease termination fee of $2.3 million. The Nursing Centers were included in the Company’s Master Lease Agreements (as defined in Note 10) with Ventas and the Company does not have the ability to terminate a lease of an individual facility under the Master Lease Agreements. The aggregate annual rent for the Nursing Centers was approximately $6 million for the year ended December 31, 2008. The Nursing Centers, which contained 777 licensed beds, generated pretax losses of $0.1 million, $0.5 million and $2.5 million for 2010, 2009 and 2008, respectively. The Company recorded a pretax gain of $2.1 million ($1.3 million net of income taxes) for the year ended December 31, 2010 and a pretax loss of $39.5 million ($24.3 million net of income taxes) for the year ended December 31, 2009 related to these divestitures.
2008 divestitures
In September 2008, the Company purchased for resale a LTAC hospital for $22.3 million that was previously leased. The Company recorded a pretax loss of $36.9 million ($22.7 million net of income taxes) in 2008 resulting from the losses related to the purchase, closure and planned divestiture of the hospital, including the impairment of a certificate of need intangible asset ($15.2 million), the impairment of property and equipment ($17.3 million) and other costs ($4.4 million). In addition, the Company recorded a pretax loss of $2.6 million ($1.6 million net of income taxes) in 2010 resulting from a reduction to the fair market value of the property.
In September 2008, the Company also announced its intention to dispose of another LTAC hospital and its related operations. The Company recorded a pretax loss of $7.4 million ($4.6 million net of income taxes) during 2008 related to the impairment of the hospital’s building and equipment. In addition, the Company recorded a pretax loss of $0.5 million ($0.3 million net of income taxes) in 2010 resulting from a reduction to the fair market value of the property.
These two hospitals generated pretax losses of $1.5 million in 2010, $3.3 million in 2009 and $8.0 million in 2008.
The Company also discontinued the operations of a hospital in 2008 after terminating the hospital operating lease and ceasing operations.
Assets not sold at December 31, 2010 have been measured at the lower of carrying value or estimated fair value less costs of disposal and have been classified as held for sale in the accompanying consolidated balance sheet. See Note 4.
NOTE 4 – DISCONTINUED OPERATIONS
In accordance with the authoritative guidance for the impairment or disposal of long-lived assets, the divestiture of unprofitable businesses discussed in Notes 1 and 3 have been accounted for as discontinued operations. Accordingly, the results of operations of these businesses for all periods presented and the losses or impairments related to these divestitures have been classified as discontinued operations, net of income taxes, in the accompanying consolidated statement of operations. At December 31, 2010, the Company held for sale two hospitals reported as discontinued operations.
F-16
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 4 – DISCONTINUED OPERATIONS (Continued)
Discontinued operations included favorable pretax adjustments of $5.1 million ($3.1 million net of income taxes) in 2010, $11.1 million ($6.8 million net of income taxes) in 2009 and $9.7 million ($6.0 million net of income taxes) in 2008 resulting from changes in estimates for professional liability reserves related to prior years.
A summary of discontinued operations follows (in thousands):
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Revenues |
$ | 13,507 | $ | 56,249 | $ | 104,698 | ||||||
| Salaries, wages and benefits |
9,893 | 33,945 | 63,567 | |||||||||
| Supplies |
773 | 3,426 | 7,802 | |||||||||
| Rent |
132 | 3,572 | 9,161 | |||||||||
| Other operating expenses |
1,438 | 13,122 | 27,462 | |||||||||
| Depreciation |
– | 674 | 2,243 | |||||||||
| Interest expense |
1 | 9 | 2 | |||||||||
| Investment income |
(27 | ) | (12 | ) | (13 | ) | ||||||
| 12,210 | 54,736 | 110,224 | ||||||||||
| Income (loss) from operations before income taxes |
1,297 | 1,513 | (5,526 | ) | ||||||||
| Provision (benefit) for income tax |
499 | 582 | (2,127 | ) | ||||||||
| Income (loss) from operations |
798 | 931 | (3,399 | ) | ||||||||
| Loss on divestiture of operations, net of income taxes |
(453 | ) | (23,432 | ) | (20,776 | ) | ||||||
| $ | 345 | $ | (22,501 | ) | $ | (24,175 | ) | |||||
The following table sets forth certain discontinued operations data by business segment (in thousands):
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Revenues: |
||||||||||||
| Hospital division |
$ | 181 | $ | 4,850 | $ | 33,687 | ||||||
| Nursing center division |
13,326 | 51,399 | 71,011 | |||||||||
| $ | 13,507 | $ | 56,249 | $ | 104,698 | |||||||
| Operating income (loss): |
||||||||||||
| Hospital division |
$ | (1,139 | ) | $ | (2,759 | ) | $ | (5,470 | ) | |||
| Nursing center division |
2,542 | 8,515 | 11,337 | |||||||||
| $ | 1,403 | $ | 5,756 | $ | 5,867 | |||||||
| Rent: |
||||||||||||
| Hospital division |
$ | 121 | $ | 208 | $ | 2,858 | ||||||
| Nursing center division |
11 | 3,364 | 6,303 | |||||||||
| $ | 132 | $ | 3,572 | $ | 9,161 | |||||||
| Depreciation: |
||||||||||||
| Hospital division |
$ | – | $ | – | $ | 852 | ||||||
| Nursing center division |
– | 674 | 1,391 | |||||||||
| $ | – | $ | 674 | $ | 2,243 | |||||||
F-17
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 4 – DISCONTINUED OPERATIONS (Continued)
A summary of the net assets held for sale follows (in thousands):
| December 31, | ||||||||
| 2010 | 2009 | |||||||
| Long-term assets: |
||||||||
| Property and equipment, net |
$ | 7,062 | $ | 8,723 | ||||
| Other |
105 | 83 | ||||||
| 7,167 | 8,806 | |||||||
| Current liabilities (included in other accrued liabilities) |
(72 | ) | (422 | ) | ||||
| $ | 7,095 | $ | 8,384 | |||||
NOTE 5 – EARNINGS PER SHARE
Earnings per common share are based upon the weighted average number of common shares outstanding during the respective periods. The diluted calculation of earnings per common share includes the dilutive effect of stock options and performance-based restricted shares. On January 1, 2009, the Company adopted the provisions of the authoritative guidance for determining whether instruments granted in share-based payment transactions are participating securities, which requires that unvested restricted stock that entitles the holder to receive nonforfeitable dividends before vesting be included as a participating security in the basic and diluted earnings per common share calculation pursuant to the two-class method.
F-18
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 5 – EARNINGS PER SHARE (Continued)
A computation of the earnings per common share follows (in thousands, except per share amounts):
| Year ended December 31, | ||||||||||||||||||||||||
| 2010 | 2009 | 2008 | ||||||||||||||||||||||
| Basic | Diluted | Basic | Diluted | Basic | Diluted | |||||||||||||||||||
| Earnings: |
||||||||||||||||||||||||
| Income from continuing operations: |
||||||||||||||||||||||||
| As reported in Statement of Operations |
$ | 56,146 | $ | 56,146 | $ | 62,612 | $ | 62,612 | $ | 60,460 | $ | 60,460 | ||||||||||||
| Allocation to participating unvested restricted stockholders |
(1,015 | ) | (1,009 | ) | (1,094 | ) | (1,090 | ) | (1,374 | ) | (1,355 | ) | ||||||||||||
| Available to common stockholders |
$ | 55,131 | $ | 55,137 | $ | 61,518 | $ | 61,522 | $ | 59,086 | $ | 59,105 | ||||||||||||
| Discontinued operations, net of income taxes: |
||||||||||||||||||||||||
| Income (loss) from operations: |
||||||||||||||||||||||||
| As reported in Statement of Operations |
$ | 798 | $ | 798 | $ | 931 | $ | 931 | $ | (3,399 | ) | $ | (3,399 | ) | ||||||||||
| Allocation to participating unvested restricted stockholders |
(14 | ) | (14 | ) | (16 | ) | (16 | ) | 77 | 76 | ||||||||||||||
| Available to common stockholders |
$ | 784 | $ | 784 | $ | 915 | $ | 915 | $ | (3,322 | ) | $ | (3,323 | ) | ||||||||||
| Loss on divestiture of operations: |
||||||||||||||||||||||||
| As reported in Statement of Operations |
$ | (453 | ) | $ | (453 | ) | $ | (23,432 | ) | $ | (23,432 | ) | $ | (20,776 | ) | $ | (20,776 | ) | ||||||
| Allocation to participating unvested restricted stockholders |
8 | 8 | 409 | 408 | 472 | 466 | ||||||||||||||||||
| Available to common stockholders |
$ | (445 | ) | $ | (445 | ) | $ | (23,023 | ) | $ | (23,024 | ) | $ | (20,304 | ) | $ | (20,310 | ) | ||||||
| Net income: |
||||||||||||||||||||||||
| As reported in Statement of Operations |
$ | 56,491 | $ | 56,491 | $ | 40,111 | $ | 40,111 | $ | 36,285 | $ | 36,285 | ||||||||||||
| Allocation to participating unvested restricted stockholders |
(1,021 | ) | (1,015 | ) | (701 | ) | (698 | ) | (825 | ) | (813 | ) | ||||||||||||
| Available to common stockholders |
$ | 55,470 | $ | 55,476 | $ | 39,410 | $ | 39,413 | $ | 35,460 | $ | 35,472 | ||||||||||||
| Shares used in the computation: |
||||||||||||||||||||||||
| Weighted average shares outstanding – basic computation |
38,738 | 38,738 | 38,339 | 38,339 | 37,830 | 37,830 | ||||||||||||||||||
| Dilutive effect of employee stock options |
135 | 128 | 567 | |||||||||||||||||||||
| Dilutive effect of performance-based restricted shares |
81 | 35 | – | |||||||||||||||||||||
| Adjusted weighted average shares outstanding – diluted computation |
38,954 | 38,502 | 38,397 | |||||||||||||||||||||
| Earnings per common share: |
||||||||||||||||||||||||
| Income from continuing operations |
$ | 1.42 | $ | 1.42 | $ | 1.61 | $ | 1.60 | $ | 1.56 | $ | 1.54 | ||||||||||||
| Discontinued operations: |
||||||||||||||||||||||||
| Income (loss) from operations |
0.02 | 0.02 | 0.02 | 0.02 | (0.09 | ) | (0.09 | ) | ||||||||||||||||
| Loss on divestiture of operations |
(0.01 | ) | (0.01 | ) | (0.60 | ) | (0.60 | ) | (0.53 | ) | (0.53 | ) | ||||||||||||
| Net income |
$ | 1.43 | $ | 1.43 | $ | 1.03 | $ | 1.02 | $ | 0.94 | $ | 0.92 | ||||||||||||
| Number of antidilutive stock options excluded from shares used in the diluted earnings per common share computation |
2,466 | 2,986 | 1,310 | |||||||||||||||||||||
F-19
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 6 – BUSINESS SEGMENT DATA
At December 31, 2010, the Company operated three business segments: the hospital division, the nursing center division and the rehabilitation division. The hospital division operates LTAC hospitals, the nursing center division operates nursing and rehabilitation centers and assisted living facilities, and the rehabilitation division provides rehabilitation therapy services primarily in long-term care settings. For segment purposes, the Company defines operating income as earnings before interest, income taxes, depreciation, amortization and rent. Operating income reported for each of the Company’s business segments excludes the allocation of corporate overhead. The accounting policies of each of the segments are the same and are described in Note 1.
The Company identifies its segments in accordance with the aggregation provisions of the authoritative guidance for segment reporting. This information is consistent with information used by the Company in managing its businesses and aggregates businesses with similar economic characteristics. The Company includes operating data for its home health and hospice businesses in the rehabilitation division.
The following table sets forth certain data by business segment (in thousands):
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Revenues: |
||||||||||||
| Hospital division |
$ | 1,973,321 | $ | 1,932,892 | $ | 1,837,322 | ||||||
| Nursing center division |
2,187,885 | 2,150,342 | 2,093,297 | |||||||||
| Rehabilitation division |
504,955 | 475,038 | 427,320 | |||||||||
| 4,666,161 | 4,558,272 | 4,357,939 | ||||||||||
| Eliminations |
(306,464 | ) | (288,265 | ) | (264,075 | ) | ||||||
| $ | 4,359,697 | $ | 4,270,007 | $ | 4,093,864 | |||||||
| Income from continuing operations: |
||||||||||||
| Operating income (loss): |
||||||||||||
| Hospital division |
$ | 357,100 | $ | 363,811 | $ | 345,367 | ||||||
| Nursing center division |
302,672 | 305,590 | 321,814 | |||||||||
| Rehabilitation division |
51,923 | 50,592 | 38,071 | |||||||||
| Corporate: |
||||||||||||
| Overhead |
(133,919 | ) | (134,636 | ) | (133,019 | ) | ||||||
| Insurance subsidiary |
(3,153 | ) | (6,185 | ) | (6,657 | ) | ||||||
| (137,072 | ) | (140,821 | ) | (139,676 | ) | |||||||
| Operating income |
574,623 | 579,172 | 565,576 | |||||||||
| Rent |
(357,372 | ) | (348,248 | ) | (338,673 | ) | ||||||
| Depreciation and amortization |
(121,552 | ) | (125,730 | ) | (120,022 | ) | ||||||
| Interest, net |
(5,845 | ) | (3,467 | ) | (8,277 | ) | ||||||
| Income before income taxes |
89,854 | 101,727 | 98,604 | |||||||||
| Provision for income taxes |
33,708 | 39,115 | 38,144 | |||||||||
| $ | 56,146 | $ | 62,612 | $ | 60,460 | |||||||
F-20
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 6 – BUSINESS SEGMENT DATA (Continued)
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Rent: |
||||||||||||
| Hospital division |
$ | 152,986 | $ | 147,494 | $ | 146,316 | ||||||
| Nursing center division |
198,105 | 194,835 | 186,612 | |||||||||
| Rehabilitation division |
6,136 | 5,778 | 5,555 | |||||||||
| Corporate |
145 | 141 | 190 | |||||||||
| $ | 357,372 | $ | 348,248 | $ | 338,673 | |||||||
| Depreciation and amortization: |
||||||||||||
| Hospital division |
$ | 51,639 | $ | 51,932 | $ | 48,150 | ||||||
| Nursing center division |
45,471 | 48,631 | 48,645 | |||||||||
| Rehabilitation division |
2,709 | 2,291 | 1,965 | |||||||||
| Corporate |
21,733 | 22,876 | 21,262 | |||||||||
| $ | 121,552 | $ | 125,730 | $ | 120,022 | |||||||
| Capital expenditures, excluding acquisitions (including discontinued operations): |
||||||||||||
| Hospital division: |
||||||||||||
| Routine |
$ | 36,967 | $ | 26,716 | $ | 35,932 | ||||||
| Development |
41,140 | 42,371 | 33,285 | |||||||||
| 78,107 | 69,087 | 69,217 | ||||||||||
| Nursing center division: |
||||||||||||
| Routine |
37,024 | 39,663 | 44,627 | |||||||||
| Development |
26,701 | 5,687 | 5,466 | |||||||||
| 63,725 | 45,350 | 50,093 | ||||||||||
| Rehabilitation division |
2,715 | 1,043 | 1,162 | |||||||||
| Corporate: |
||||||||||||
| Information systems |
29,786 | 28,441 | 26,363 | |||||||||
| Other |
2,404 | 1,687 | 1,842 | |||||||||
| $ | 176,737 | $ | 145,608 | $ | 148,677 | |||||||
| Assets at end of period: |
||||||||||||
| Hospital division |
$ | 1,100,138 | $ | 867,332 | ||||||||
| Nursing center division |
647,355 | 566,592 | ||||||||||
| Rehabilitation division |
87,853 | 53,856 | ||||||||||
| Corporate |
502,069 | 534,444 | ||||||||||
| $ | 2,337,415 | $ | 2,022,224 | |||||||||
| Goodwill: |
||||||||||||
| Hospital division |
$ | 213,200 | $ | 68,577 | ||||||||
| Nursing center division |
6,080 | 889 | ||||||||||
| Rehabilitation division |
23,140 | 11,757 | ||||||||||
| $ | 242,420 | $ | 81,223 | |||||||||
F-21
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 7 – INCOME TAXES
The provision for income taxes is based upon the Company’s annual reported income or loss for each respective accounting period. The Company recognizes an asset or liability for the deferred tax consequences of temporary differences between the tax bases of assets and liabilities and their reported amounts in the financial statements. These temporary differences will result in taxable or deductible amounts in future years when the reported amounts of the assets are recovered or liabilities are settled. The Company also recognizes as deferred tax assets the future tax benefits from net operating and capital loss carryforwards. A valuation allowance is provided for these deferred tax assets if it is more likely than not that some portion or all of the net deferred tax assets will not be realized.
Provision for income taxes consists of the following (in thousands):
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Current: |
||||||||||||
| Federal |
$ | 12,538 | $ | 23,246 | $ | 21,218 | ||||||
| State |
2,316 | 4,227 | 3,769 | |||||||||
| 14,854 | 27,473 | 24,987 | ||||||||||
| Deferred |
18,854 | 11,642 | 13,157 | |||||||||
| $ | 33,708 | $ | 39,115 | $ | 38,144 | |||||||
Reconciliation of federal statutory tax expense to the provision for income taxes follows (in thousands):
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Income tax expense at federal rate |
$ | 31,449 | $ | 35,605 | $ | 34,511 | ||||||
| State income tax expense, net of federal income tax expense |
3,145 | 3,560 | 3,451 | |||||||||
| Prior year contingencies |
(2,917 | ) | (1,769 | ) | (2,104 | ) | ||||||
| Other items, net |
2,031 | 1,719 | 2,286 | |||||||||
| $ | 33,708 | $ | 39,115 | $ | 38,144 | |||||||
A summary of net deferred income tax assets by source included in the accompanying consolidated balance sheet at December 31 follows (in thousands):
| 2010 | 2009 | |||||||||||||||
| Assets | Liabilities | Assets | Liabilities | |||||||||||||
| Property and equipment |
$ | 867 | $ | – | $ | 19,227 | $ | – | ||||||||
| Insurance |
53,914 | – | 53,885 | – | ||||||||||||
| Accounts receivable allowances |
– | 14,421 | 12,179 | – | ||||||||||||
| Compensation |
45,183 | – | 39,685 | – | ||||||||||||
| Net operating losses |
42,205 | – | 37,924 | – | ||||||||||||
| Assets held for sale |
10,072 | – | 15,336 | – | ||||||||||||
| Other |
2,866 | – | 10,555 | – | ||||||||||||
| 155,107 | $ | 14,421 | 188,791 | $ | – | |||||||||||
| Reclassification of deferred tax liabilities |
(14,421 | ) | – | |||||||||||||
| Net deferred tax assets |
140,686 | 188,791 | ||||||||||||||
| Valuation allowance |
(38,431 | ) | (35,070 | ) | ||||||||||||
| $ | 102,255 | $ | 153,721 | |||||||||||||
F-22
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 7 – INCOME TAXES (Continued)
Deferred income taxes totaling $13.5 million and $42.8 million at December 31, 2010 and 2009, respectively, were classified as current assets, and deferred income taxes totaling $88.8 million and $110.9 million at December 31, 2010 and 2009, respectively, were classified as noncurrent assets.
After the Company’s emergence from bankruptcy in 2001, the realization of pre-reorganization deferred tax assets (amounts which had been considered “more likely than not” to be realized by the Company) and the resolution of certain income tax contingencies eliminated in full the goodwill recorded in connection with fresh-start accounting. After the fresh-start accounting goodwill was eliminated in full, the excess of $1.4 million in 2008 was treated as an increase to capital in excess of par value and a reduction in the pre-emergence deferred tax valuation allowance and pre-emergence income tax liability.
The Company identified deferred income tax assets for state income tax NOLs of $42.2 million and $37.9 million at December 31, 2010 and 2009, respectively, and a corresponding deferred income tax valuation allowance of $37.8 million and $34.0 million at December 31, 2010 and 2009, respectively, for that portion of the net deferred income tax assets that the Company will likely not realize in the future.
The Company follows the provisions of the authoritative guidance for accounting for uncertainty in income taxes which clarifies the accounting for uncertain income tax issues recognized in an entity’s financial statements. The guidance prescribes a recognition threshold and measurement attribute for the financial statement recognition and measurement of a tax position taken or expected to be taken in an income tax return.
A reconciliation of unrecognized tax benefits follows (in thousands):
| Balance, December 31, 2007 |
$ | 9,213 | ||
| Additions based upon tax positions related to the current year |
2,796 | |||
| Reductions due to lapses of applicable statute of limitations |
(2,456 | ) | ||
| Balance, December 31, 2008 |
9,553 | |||
| Additions based upon tax positions related to the current year |
232 | |||
| Reductions due to lapses of applicable statute of limitations |
(2,042 | ) | ||
| Balance, December 31, 2009 |
7,743 | |||
| Additions based upon tax positions related to the current year |
100 | |||
| Reductions due to lapses of applicable statute of limitations |
(4,616 | ) | ||
| Balance, December 31, 2010 |
$ | 3,227 | ||
The Company records accrued interest and penalties associated with uncertain tax positions as income tax expense in the consolidated statement of operations. Accrued interest related to uncertain tax provisions totaled $0.2 million as of December 31, 2010 and $0.1 million as of December 31, 2009.
To the extent the unrecognized income tax benefits become realized or the related accrued interest is no longer necessary, the company’s provision for income taxes would be favorably impacted. The amount, if recognized, that would favorably impact the Company’s results of operations approximates $3.2 million.
The federal statute of limitations remains open for tax years 2007 through 2009 and the Company is currently under examination by the Internal Revenue Service (the “IRS”) for each of these years.
F-23
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 7 – INCOME TAXES (Continued)
State jurisdictions generally have statutes of limitations for tax returns ranging from three to five years. The state impact of federal income tax changes remains subject to examination by various states for a period of up to one year after formal notification to the states. The Company currently has various state income tax returns under examination.
The Company received approval from the IRS for an accounting method change for income tax purposes that resulted in a non-recurring reduction in income tax payments of approximately $25 million during 2010. The Company’s earnings were not impacted by this transaction.
NOTE 8 – INSURANCE RISKS
The Company insures a substantial portion of its professional liability risks and workers compensation risks through its limited purpose insurance subsidiary. Provisions for loss for these risks are based upon management’s best available information including actuarially determined estimates.
The allowance for professional liability risks includes an estimate of the expected cost to settle reported claims and an amount, based upon past experiences, for losses incurred but not reported. These liabilities are necessarily based upon estimates and, while management believes that the provision for loss is adequate, the ultimate liability may be in excess of, or less than, the amounts recorded. To the extent that expected ultimate claims costs vary from historical provisions for loss, future earnings will be charged or credited. The provision for professional liability risks has reflected favorable adjustments related to prior year changes in estimates in each of the last three years.
The provision for loss for insurance risks, including the cost of coverage maintained with unaffiliated commercial insurance carriers, follows (in thousands):
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Professional liability: |
||||||||||||
| Continuing operations |
$ | 55,612 | $ | 48,478 | $ | 33,117 | ||||||
| Discontinued operations |
(4,289 | ) | (4,590 | ) | (6,287 | ) | ||||||
| Workers compensation: |
||||||||||||
| Continuing operations |
$ | 42,634 | $ | 35,505 | $ | 30,082 | ||||||
| Discontinued operations |
(1,329 | ) | (904 | ) | 1,189 | |||||||
F-24
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 8 – INSURANCE RISKS (Continued)
Changes in the allowance for professional liability risks and workers compensation risks for the years ended December 31 follow (in thousands) (including discontinued operations):
| 2010 | 2009 | |||||||||||||||||||||||
| Professional liability |
Workers compensation |
Total | Professional liability |
Workers compensation |
Total | |||||||||||||||||||
| Allowance for insurance risks at beginning of year |
$ | 242,202 | $ | 82,122 | $ | 324,324 | $ | 243,251 | $ | 83,341 | $ | 326,592 | ||||||||||||
| Provision for loss for insurance risks: |
||||||||||||||||||||||||
| Current year |
63,886 | 39,677 | 103,563 | 68,978 | 35,595 | 104,573 | ||||||||||||||||||
| Prior years |
(24,311 | ) | (6,936 | ) | (31,247 | ) | (38,072 | ) | (8,206 | ) | (46,278 | ) | ||||||||||||
| 39,575 | 32,741 | 72,316 | 30,906 | 27,389 | 58,295 | |||||||||||||||||||
| Provision for commercial insurance, administrative and overhead costs |
11,748 | 8,564 | 20,312 | 12,982 | 7,212 | 20,194 | ||||||||||||||||||
| Discount accretion |
2,811 | – | 2,811 | 5,891 | – | 5,891 | ||||||||||||||||||
| Contributions from managed facilities |
71 | 255 | 326 | 74 | 212 | 286 | ||||||||||||||||||
| Payments for insurance risks: |
||||||||||||||||||||||||
| Current year |
(3,157 | ) | (11,714 | ) | (14,871 | ) | (5,270 | ) | (10,913 | ) | (16,183 | ) | ||||||||||||
| Prior years |
(44,951 | ) | (20,416 | ) | (65,367 | ) | (44,929 | ) | (19,937 | ) | (64,866 | ) | ||||||||||||
| (48,108 | ) | (32,130 | ) | (80,238 | ) | (50,199 | ) | (30,850 | ) | (81,049 | ) | |||||||||||||
| Payments for commercial insurance, administrative and overhead costs |
(11,748 | ) | (8,564 | ) | (20,312 | ) | (12,982 | ) | (7,212 | ) | (20,194 | ) | ||||||||||||
| Change in reinsurance and other recoverables |
12,673 | 1,192 | 13,865 | 12,279 | 2,030 | 14,309 | ||||||||||||||||||
| Allowance for insurance risks at end of year |
$ | 249,224 | $ | 84,180 | $ | 333,404 | $ | 242,202 | $ | 82,122 | $ | 324,324 | ||||||||||||
A summary of the assets and liabilities related to insurance risks included in the accompanying consolidated balance sheet at December 31 follows (in thousands):
| 2010 | 2009 | |||||||||||||||||||||||
| Professional liability |
Workers compensation |
Total | Professional liability |
Workers compensation |
Total | |||||||||||||||||||
| Assets: |
||||||||||||||||||||||||
| Current: |
||||||||||||||||||||||||
| Insurance subsidiary investments |
$ | 54,162 | $ | 22,591 | $ | 76,753 | $ | 84,953 | $ | 21,881 | $ | 106,834 | ||||||||||||
| Reinsurance recoverables |
265 | – | 265 | 89 | – | 89 | ||||||||||||||||||
| Other |
– | 319 | 319 | – | 321 | 321 | ||||||||||||||||||
| 54,427 | 22,910 | 77,337 | 85,042 | 22,202 | 107,244 | |||||||||||||||||||
| Non-current: |
||||||||||||||||||||||||
| Insurance subsidiary investments |
38,635 | 62,575 | 101,210 | 43,272 | 56,951 | 100,223 | ||||||||||||||||||
| Reinsurance and other recoverables |
41,752 | 3,222 | 44,974 | 29,446 | 2,030 | 31,476 | ||||||||||||||||||
| Deposits |
3,000 | 1,313 | 4,313 | 5,000 | 1,410 | 6,410 | ||||||||||||||||||
| Other |
– | 44 | 44 | – | 36 | 36 | ||||||||||||||||||
| 83,387 | 67,154 | 150,541 | 77,718 | 60,427 | 138,145 | |||||||||||||||||||
| $ | 137,814 | $ | 90,064 | $ | 227,878 | $ | 162,760 | $ | 82,629 | $ | 245,389 | |||||||||||||
| Liabilities: |
||||||||||||||||||||||||
| Allowance for insurance risks: |
||||||||||||||||||||||||
| Current |
$ | 41,555 | $ | 24,676 | $ | 66,231 | $ | 47,076 | $ | 23,934 | $ | 71,010 | ||||||||||||
| Non-current |
207,669 | 59,504 | 267,173 | 195,126 | 58,188 | 253,314 | ||||||||||||||||||
| $ | 249,224 | $ | 84,180 | $ | 333,404 | $ | 242,202 | $ | 82,122 | $ | 324,324 | |||||||||||||
F-25
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 8 – INSURANCE RISKS (Continued)
Provisions for loss for professional liability risks retained by the Company’s limited purpose insurance subsidiary have been discounted based upon actuarial estimates of claim payment patterns using a discount rate of 1% to 5% depending upon the policy year. The discount rate was 1% for the 2010 policy year, 2% for the 2009 policy year, 3% for the 2008 policy year and 5% for all prior policy years. The discount rates are based upon the risk free interest rate for the respective year. Amounts equal to the discounted loss provision are funded annually. The Company does not fund the portion of professional liability risks related to estimated claims that have been incurred but not reported. Accordingly, these liabilities are not discounted. If the Company did not discount any of the allowances for professional liability risks, these balances would have approximated $252.6 million at December 31, 2010 and $247.3 million at December 31, 2009.
Provisions for loss for workers compensation risks retained by the Company’s limited purpose insurance subsidiary are not discounted and amounts equal to the loss provision are funded annually.
NOTE 9 – INSURANCE SUBSIDIARY INVESTMENTS
The Company maintains investments, consisting principally of cash and cash equivalents, debt securities, equities and commercial paper for the payment of claims and expenses related to professional liability and workers compensation risks. These investments have been categorized as available-for-sale and are reported at fair value.
The amortized cost and estimated fair value of the Company’s insurance subsidiary investments at December 31 follow (in thousands):
| 2010 | 2009 | |||||||||||||||||||||||||||||||
| Amortized cost |
Unrealized gains |
Unrealized losses |
Fair value |
Amortized cost |
Unrealized gains |
Unrealized losses |
Fair value |
|||||||||||||||||||||||||
| Cash and cash equivalents (a) |
$ | 104,664 | $ | – | $ | – | $ | 104,664 | $ | 96,143 | $ | – | $ | – | $ | 96,143 | ||||||||||||||||
| Debt securities: |
||||||||||||||||||||||||||||||||
| Corporate bonds |
32,174 | 542 | (40 | ) | 32,676 | 47,528 | 770 | (102 | ) | 48,196 | ||||||||||||||||||||||
| Debt securities issued by U.S. government agencies |
17,906 | 113 | (27 | ) | 17,992 | 37,788 | 223 | (43 | ) | 37,968 | ||||||||||||||||||||||
| U.S. Treasury notes |
2,482 | 11 | – | 2,493 | 2,801 | 19 | – | 2,820 | ||||||||||||||||||||||||
| Debt securities issued by foreign governments |
2,081 | 15 | – | 2,096 | 624 | – | (5 | ) | 619 | |||||||||||||||||||||||
| Commercial mortgage-backed securities |
307 | 19 | – | 326 | 610 | 27 | – | 637 | ||||||||||||||||||||||||
| 54,950 | 700 | (67 | ) | 55,583 | 89,351 | 1,039 | (150 | ) | 90,240 | |||||||||||||||||||||||
| Equities by industry: |
||||||||||||||||||||||||||||||||
| Financial services |
1,284 | 209 | (66 | ) | 1,427 | 1,284 | 162 | (155 | ) | 1,291 | ||||||||||||||||||||||
| Healthcare |
1,572 | 20 | (235 | ) | 1,357 | 1,573 | 16 | (171 | ) | 1,418 | ||||||||||||||||||||||
| Oil and gas |
921 | 142 | (37 | ) | 1,026 | 1,257 | 8 | (303 | ) | 962 | ||||||||||||||||||||||
| Real estate |
148 | 9 | – | 157 | 147 | 2 | (24 | ) | 125 | |||||||||||||||||||||||
| Other |
7,446 | 867 | (269 | ) | 8,044 | 8,470 | 80 | (1,132 | ) | 7,418 | ||||||||||||||||||||||
| 11,371 | 1,247 | (607 | ) | 12,011 | 12,731 | 268 | (1,785 | ) | 11,214 | |||||||||||||||||||||||
| Commercial paper |
5,705 | 2 | (2 | ) | 5,705 | 9,449 | 14 | (3 | ) | 9,460 | ||||||||||||||||||||||
| $ | 176,690 | $ | 1,949 | $ | (676 | ) | $ | 177,963 | $ | 207,674 | $ | 1,321 | $ | (1,938 | ) | $ | 207,057 | |||||||||||||||
| (a) | Includes $2.6 million and $4.7 million of money market funds at December 31, 2010 and 2009, respectively. |
F-26
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 9 – INSURANCE SUBSIDIARY INVESTMENTS (Continued)
The fair value by maturity periods at December 31, 2010 of available-for-sale investments of the Company’s insurance subsidiary follows. Equities generally do not have maturity dates.
| (In thousands) |
Contractual maturities |
|||
| Within one year |
$ | 126,045 | ||
| One year to five years |
39,548 | |||
| After five years |
359 | |||
| Equities |
12,011 | |||
| $ | 177,963 | |||
Since the Company’s insurance subsidiary investments are restricted for a limited purpose, they are classified in the accompanying consolidated balance sheet based upon the expected current and long-term cash requirements of the limited purpose insurance subsidiary.
Net investment income earned by the Company’s insurance subsidiary investments follows (in thousands):
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Interest income |
$ | 1,986 | $ | 3,393 | $ | 8,107 | ||||||
| Net amortization of premium and accretion of discount |
(394 | ) | (298 | ) | (141 | ) | ||||||
| Gains on sale of investments |
524 | 1,598 | 1,244 | |||||||||
| Losses on sale of investments |
(84 | ) | (346 | ) | (194 | ) | ||||||
| Other-than-temporary impairment on investments |
(728 | ) | (444 | ) | (2,311 | ) | ||||||
| Investment expenses |
(148 | ) | (168 | ) | (242 | ) | ||||||
| $ | 1,156 | $ | 3,735 | $ | 6,463 | |||||||
The available-for-sale investments of the Company’s insurance subsidiary which have unrealized losses at December 31, 2010 and 2009 are shown below. The investments are categorized by the length of time that individual securities have been in a continuous unrealized loss position at December 31, 2010 and 2009.
| December 31, 2010 |
Less than one year | One year or greater | Total | |||||||||||||||||||||
| (In thousands) |
Fair value |
Unrealized losses |
Fair value |
Unrealized losses |
Fair value |
Unrealized losses |
||||||||||||||||||
| Debt securities: |
||||||||||||||||||||||||
| Corporate bonds |
$ | 5,003 | $ | 36 | $ | 678 | $ | 4 | $ | 5,681 | $ | 40 | ||||||||||||
| Debt securities issued by U.S. government agencies |
5,635 | 27 | – | – | 5,635 | 27 | ||||||||||||||||||
| Debt securities issued by foreign governments |
– | – | – | – | – | – | ||||||||||||||||||
| 10,638 | 63 | 678 | 4 | 11,316 | 67 | |||||||||||||||||||
| Equities by industry: |
||||||||||||||||||||||||
| Financial services |
199 | 17 | 150 | 49 | 349 | 66 | ||||||||||||||||||
| Healthcare |
361 | 11 | 874 | 224 | 1,235 | 235 | ||||||||||||||||||
| Oil and gas |
114 | 31 | 251 | 6 | 365 | 37 | ||||||||||||||||||
| Real estate |
– | – | – | – | – | – | ||||||||||||||||||
| Other |
855 | 109 | 1,215 | 160 | 2,070 | 269 | ||||||||||||||||||
| 1,529 | 168 | 2,490 | 439 | 4,019 | 607 | |||||||||||||||||||
| Commercial paper |
2,503 | 2 | – | – | 2,503 | 2 | ||||||||||||||||||
| $ | 14,670 | $ | 233 | $ | 3,168 | $ | 443 | $ | 17,838 | $ | 676 | |||||||||||||
F-27
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 9 – INSURANCE SUBSIDIARY INVESTMENTS (Continued)
| December 31, 2009 |
Less than one year | One year or greater | Total | |||||||||||||||||||||
| (In thousands) |
Fair value |
Unrealized losses |
Fair value |
Unrealized losses |
Fair value |
Unrealized losses |
||||||||||||||||||
| Debt securities: |
||||||||||||||||||||||||
| Corporate bonds |
$ | 13,269 | $ | 42 | $ | 1,806 | $ | 60 | $ | 15,075 | $ | 102 | ||||||||||||
| Debt securities issued by U.S. government agencies |
10,769 | 43 | – | – | 10,769 | 43 | ||||||||||||||||||
| Debt securities issued by foreign governments |
619 | 5 | – | – | 619 | 5 | ||||||||||||||||||
| 24,657 | 90 | 1,806 | 60 | 26,463 | 150 | |||||||||||||||||||
| Equities by industry: |
||||||||||||||||||||||||
| Financial services |
525 | 113 | 315 | 42 | 840 | 155 | ||||||||||||||||||
| Healthcare |
303 | 68 | 719 | 103 | 1,022 | 171 | ||||||||||||||||||
| Oil and gas |
124 | 10 | 451 | 293 | 575 | 303 | ||||||||||||||||||
| Real estate |
– | – | 119 | 24 | 119 | 24 | ||||||||||||||||||
| Other |
2,027 | 76 | 3,207 | 1,056 | 5,234 | 1,132 | ||||||||||||||||||
| 2,979 | 267 | 4,811 | 1,518 | 7,790 | 1,785 | |||||||||||||||||||
| Commercial paper |
1,847 | 3 | – | – | 1,847 | 3 | ||||||||||||||||||
| $ | 29,483 | $ | 360 | $ | 6,617 | $ | 1,578 | $ | 36,100 | $ | 1,938 | |||||||||||||
The unrealized losses on equities totaling $0.6 million at December 31, 2010 were due generally to market fluctuations. Accordingly, the Company believes these unrealized losses are temporary in nature.
The Company’s investment policy governing insurance subsidiary investments precludes the investment portfolio managers from selling any security at a loss without prior authorization from the Company. The investment managers also limit the exposure to any one issue, issuer or type of investment. The Company intends, and has the ability, to hold insurance subsidiary investments for a long duration without the necessity of selling securities to fund the underwriting needs of its insurance subsidiary. This ability to hold securities allows sufficient time for recovery of temporary declines in the market value of equity securities and the par value of debt securities as of their stated maturity date.
The Company considered the severity and duration of its unrealized losses and recognized $0.7 million, $0.4 million and $2.3 million pretax other-than-temporary impairments in 2010, 2009 and 2008, respectively, for various investments held in its insurance subsidiary investment portfolio. These investments were determined to be impaired after considering the duration of the declines in value and the likelihood of near term price recovery of each investment. Because the Company considered the remaining unrealized losses at December 31, 2010 and 2009 to be temporary, the Company did not record any additional impairment losses related to these investments.
As a result of improved professional liability underwriting results of the Company’s limited purpose insurance subsidiary, the Company received distributions of $22 million in 2010, $34 million in 2009 and $39 million in 2008 from its limited purpose insurance subsidiary in accordance with applicable regulations. These distributions had no impact on earnings and the proceeds were used primarily to repay borrowings under the Company’s revolving credit facility.
F-28
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 10 – LEASES
The Company leases real estate and equipment under cancelable and non-cancelable arrangements. The following table sets forth rent expense by business segment (in thousands):
| Year ended December 31, | ||||||||||||
| 2010 | 2009 | 2008 | ||||||||||
| Hospital division: |
||||||||||||
| Buildings: |
||||||||||||
| Ventas |
$ | 93,372 | $ | 91,218 | $ | 86,871 | ||||||
| Other landlords |
33,172 | 31,501 | 34,089 | |||||||||
| Equipment |
26,442 | 24,775 | 25,356 | |||||||||
| 152,986 | 147,494 | 146,316 | ||||||||||
| Nursing center division: |
||||||||||||
| Buildings: |
||||||||||||
| Ventas |
156,101 | 152,436 | 144,723 | |||||||||
| Other landlords |
39,825 | 39,876 | 39,373 | |||||||||
| Equipment |
2,179 | 2,523 | 2,516 | |||||||||
| 198,105 | 194,835 | 186,612 | ||||||||||
| Rehabilitation division: |
||||||||||||
| Buildings |
445 | 245 | 161 | |||||||||
| Equipment |
5,691 | 5,533 | 5,394 | |||||||||
| 6,136 | 5,778 | 5,555 | ||||||||||
| Corporate: |
||||||||||||
| Buildings |
107 | 99 | 155 | |||||||||
| Equipment |
38 | 42 | 35 | |||||||||
| 145 | 141 | 190 | ||||||||||
| $ | 357,372 | $ | 348,248 | $ | 338,673 | |||||||
Various facility leases include contingent annual rent escalators based upon a change in the Consumer Price Index or other agreed upon terms such as a patient revenue test. These contingent rents are included in rent expense in the year incurred. The Company recorded contingent rent of $0.6 million, $0.5 million and $3.9 million for the years ended December 31, 2010, 2009 and 2008, respectively.
Future minimum payments under non-cancelable operating leases are as follows (in thousands):
| Minimum payments | ||||||||||||
| Ventas | Other | Total | ||||||||||
| 2011 |
$ | 251,836 | $ | 75,882 | $ | 327,718 | ||||||
| 2012 |
256,953 | 70,420 | 327,373 | |||||||||
| 2013 |
178,966 | 69,101 | 248,067 | |||||||||
| 2014 |
141,519 | 66,695 | 208,214 | |||||||||
| 2015 |
47,399 | 62,302 | 109,701 | |||||||||
| Thereafter |
– | 199,092 | 199,092 | |||||||||
At December 31, 2010, the Company leased from Ventas and its affiliates 38 LTAC hospitals and 159 nursing and rehabilitation centers under four master lease agreements (the “Master Lease Agreements”).
F-29
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 10 – LEASES (Continued)
Under the Master Lease Agreements, the base term for 28 nursing and rehabilitation center and eight LTAC hospital leases (which are contained in four renewal bundles) is scheduled to expire in April 2013 (the “2013 Lease Renewals”). At the Company’s option, the 2013 Lease Renewals may be extended for one five-year renewal term beyond the base term at the then existing rental rate plus the then existing escalation amount per annum. If the Company elects to renew, all, but not less than all, of the facilities in a renewal bundle must be renewed.
In April 2009, the Company entered into agreements with Ventas to renew the Master Lease Agreements for an additional five years for 86 nursing and rehabilitation centers and 22 LTAC hospitals (collectively, the “2010 Renewal Facilities”). The initial lease term for the 2010 Renewal Facilities was scheduled to expire in April 2010. The Company’s option to renew the leases on the 2010 Renewal Facilities would have expired on April 30, 2009. No additional rent or other consideration was paid in connection with these renewals.
The base terms for 45 nursing and rehabilitation centers and eight LTAC hospitals as well as the 2010 Renewal Facilities were initially set to expire in April 2008 and 2010, respectively, but were each renewed for additional five-year terms. The Company may further extend the term of these leases for two additional five-year renewal terms beyond the first renewal term at the greater of (1) the then existing rental rate plus the then existing escalation amount per annum or (2) the then fair market value rental rate. The fair market value rental rate is determined through an appraisal procedure set forth in the Master Lease Agreements. The then fair market value rental rate may be materially higher than the existing rental rate. In such a situation the Company may be forced to either not exercise the renewal or pay the higher rental rate, either of which could have a material adverse effect on the Company’s business, financial position, results of operations and liquidity. If the Company elects to renew, all, but not less than all, of the facilities in a renewal bundle must be renewed.
NOTE 11 – LONG-TERM DEBT
Capitalization
A summary of long-term debt at December 31 follows (in thousands):
| 2010 | 2009 | |||||||
| Revolving credit facility due 2012 |
$ | 365,000 | $ | 147,000 | ||||
| Other |
647 | 733 | ||||||
| Total debt, average life of 2 years (weighted average rate 2.8% for 2010 and 2.4% for 2009) |
365,647 | 147,733 | ||||||
| Amounts due within one year |
(91 | ) | (86 | ) | ||||
| Long-term debt |
$ | 365,556 | $ | 147,647 | ||||
During 2010, the Company amended its revolving credit facility to (i) increase the aggregate amount of the credit from $500 million to $600 million and (ii) increase the amount permitted for acquisitions and certain investments by $250 million. The term of the Company’s revolving credit facility expires in July 2012.
Interest rates under the Company’s revolving credit facility are based, at the Company’s option, upon (a) the London Interbank Offered Rate plus the applicable margin or (b) the applicable margin plus the higher of the prime rate or 0.5% over the federal funds rate. The Company’s revolving credit facility is collateralized by substantially all of the Company’s assets including certain owned real property and is guaranteed by substantially
F-30
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 11 – LONG-TERM DEBT (Continued)
Capitalization (Continued)
all of the Company’s subsidiaries. The terms of the Company’s revolving credit facility include a certain defined fixed payment ratio covenant and covenants which limit acquisitions and annual capital expenditures. The Company was in compliance with the terms of its revolving credit facility at December 31, 2010.
Other information
In April 2008, the Company repaid a capital lease obligation of $16.3 million in connection with the exercise of a purchase option under a hospital lease agreement.
The following table summarizes scheduled maturities of long-term debt for the years 2011 through 2015 (in thousands):
| Revolving credit facility |
Other | Total | ||||||||||
| 2011 |
$ | – | $ | 91 | $ | 91 | ||||||
| 2012 |
365,000 | 96 | 365,096 | |||||||||
| 2013 |
– | 102 | 102 | |||||||||
| 2014 |
– | 109 | 109 | |||||||||
| 2015 |
– | 116 | 116 | |||||||||
The estimated fair value of the Company’s long-term debt at December 31, 2010 and 2009 approximated the respective carrying amounts.
NOTE 12 – CONTINGENCIES
Management continually evaluates contingencies based upon the best available information. In addition, allowances for losses are provided currently for disputed items that have continuing significance, such as certain third party reimbursements and deductions that continue to be claimed in current cost reports and tax returns.
Management believes that allowances for losses have been provided to the extent necessary and that its assessment of contingencies is reasonable.
Principal contingencies are described below:
Revenues – Certain third party payments are subject to examination by agencies administering the various reimbursement programs. The Company is contesting certain issues raised in audits of prior year cost reports.
Professional liability risks – The Company has provided for loss for professional liability risks based upon management’s best available information including actuarially determined estimates. Ultimate claims costs may differ from the provisions for loss. See Notes 4 and 8.
Income taxes – The Company is subject to various federal and state income tax audits in the ordinary course of business. Such audits could result in increased tax payments, interest and penalties. In 2007, the Company completed the spin-off of its former institutional pharmacy business and is a party to a tax matters agreement which sets forth the Company’s rights and obligations related to taxes for periods before and after the spin-off transaction.
F-31
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 12 – CONTINGENCIES (Continued)
Litigation – The Company is a party to various legal actions (some of which are not insured), and regulatory and other governmental audits and investigations in the ordinary course of business. The Company cannot predict the ultimate outcome of pending litigation and regulatory and other governmental audits and investigations. These matters could potentially subject the Company to sanctions, damages, recoupments, fines and other penalties. The U.S. Department of Justice (the “DOJ”), the Centers for Medicare and Medicaid Services (“CMS”) or other federal and state enforcement and regulatory agencies may conduct additional investigations related to the Company’s businesses in the future which may, either individually or in the aggregate, have a material adverse effect on the Company’s business, financial position, results of operations and liquidity.
Other indemnifications – In the ordinary course of business, the Company enters into contracts containing standard indemnification provisions and indemnifications specific to a transaction such as a disposal of an operating facility. These indemnifications may cover claims related to employment-related matters, governmental regulations, environmental issues and tax matters, as well as patient, third party payor, supplier and contractual relationships. Obligations under these indemnities generally are initiated by a breach of the terms of a contract or by a third party claim or event.
NOTE 13 – CAPITAL STOCK
The Company’s shareholders approved an additional 1.5 million shares of common stock in May 2008 that could be issued under the Company’s incentive compensation plans.
Plan descriptions
The Company maintains plans under which approximately ten million service-based restricted shares, performance-based restricted shares and options to purchase common stock may be granted to directors, officers and other key employees. Exercise provisions vary, but most stock options are exercisable in whole or in part beginning one to four years after grant and ending seven to ten years after grant. Shares of common stock available for future grants were 1,049,230, 1,699,946 and 2,201,688 at December 31, 2010, 2009 and 2008, respectively.
Stock options
There were no stock option grants during the year ended December 31, 2010.
The fair value of each stock option is estimated at the date of grant using a Black-Scholes option valuation model with the following weighted average assumptions for stock option grants in 2009 and 2008:
| Year ended December 31, | ||||
| 2009 | 2008 | |||
| Risk-free interest rate |
1.75% | 2.80% | ||
| Expected dividend yield |
None | None | ||
| Expected term |
5 years | 5 years | ||
| Expected volatility |
50% | 40% | ||
| Weighted average fair value at grant date |
$6.45 | $9.05 | ||
The expected term represents the period of time that stock options granted are estimated to be outstanding and was determined using the simplified method under the authoritative guidance for stock-based compensation. The expected volatility is based upon the historical prices of the Company’s common stock. An estimate of expected forfeitures was determined and compensation expense was recognized only for those stock options expected to vest.
F-32
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 13 – CAPITAL STOCK (Continued)
Stock options (Continued)
At December 31, 2010, unearned compensation costs related to non-vested stock options aggregated $0.4 million. These costs will be expensed over the remaining weighted average vesting period of approximately two years. Compensation expense related to stock options approximated $1.2 million ($1.0 million net of income taxes) for the year ended December 31, 2010, $2.7 million ($2.3 million net of income taxes) for the year ended December 31, 2009 and $3.5 million ($2.9 million net of income taxes) for the year ended December 31, 2008.
Activity in the various plans is summarized below:
| Shares under option |
Option price per share |
Weighted average exercise price |
||||||||||
| Balances, December 31, 2009 |
3,449,525 | $ | 4.89 to $28.41 | $ | 18.55 | |||||||
| Exercised |
(3,683 | ) | 8.43 to 16.81 | 13.34 | ||||||||
| Canceled |
(80,114 | ) | 6.10 to 25.83 | 18.41 | ||||||||
| Balances, December 31, 2010 |
3,365,728 | $ | 4.89 to $28.41 | $ | 18.56 | |||||||
The intrinsic value of the stock options exercised during 2010 was immaterial and for 2009 and 2008 approximated $0.6 million and $5.7 million, respectively. Cash received from stock option exercises in 2010, 2009 and 2008 totaled $0.1 million, $1.0 million and $8.9 million, respectively.
A summary of stock options outstanding at December 31, 2010 follows:
| Options outstanding | Options exercisable | |||||||||||||||||||
| Range of exercise prices |
Number outstanding at December 31, 2010 |
Weighted average remaining contractual life |
Weighted average exercise price |
Number exercisable at December 31, 2010 |
Weighted average exercise price |
|||||||||||||||
| $4.89 to $8.44 |
190,845 | 2 years | $ | 7.95 | 190,845 | $ | 7.95 | |||||||||||||
| $11.53 to $15.29 |
988,979 | 3 years | 14.15 | 774,282 | 14.01 | |||||||||||||||
| $16.81 to $22.72 |
1,084,683 | 3 years | 18.53 | 1,074,393 | 18.51 | |||||||||||||||
| $23.25 to $28.41 |
1,101,221 | 2 years | 24.38 | 1,010,205 | 24.26 | |||||||||||||||
| 3,365,728 | 3 years | $ | 18.56 | 3,049,725 | $ | 18.61 | ||||||||||||||
The intrinsic value of the stock options outstanding and stock options that are exercisable as of December 31, 2010 approximated $6.8 million and $6.0 million, respectively.
Service-based restricted shares
At December 31, 2010, unearned compensation costs related to non-vested service-based restricted shares aggregated $5.3 million. These costs will be expensed over the remaining weighted average vesting period of approximately three years. Compensation expense related to these awards approximated $6.1 million ($3.8 million net of income taxes) for the year ended December 31, 2010, $5.9 million ($3.6 million net of income taxes) for the year ended December 31, 2009 and $9.1 million ($5.6 million net of income taxes) for the year ended December 31, 2008.
F-33
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 13 – CAPITAL STOCK (Continued)
Service-based restricted shares (Continued)
A summary of non-vested service-based restricted shares follows:
| Non-vested service-based restricted shares |
Weighted average fair value at date of grant |
|||||||
| Balances, December 31, 2009 |
598,692 | $ | 24.92 | |||||
| Granted |
446,934 | 17.95 | ||||||
| Vested |
(324,435 | ) | 25.77 | |||||
| Canceled |
(22,174 | ) | 17.08 | |||||
| Balances, December 31, 2010 |
699,017 | $ | 20.32 | |||||
The fair value of restricted shares vested during 2010, 2009 and 2008 was $5.9 million, $5.4 million and $8.0 million, respectively.
Performance-based restricted shares
Performance-based restricted share awards vest over a three-year period based upon the attainment of various performance measures in each performance period. Compensation expense related to these awards approximated $3.4 million ($2.1 million net of income taxes) for the year ended December 31, 2010 and $1.3 million ($0.8 million net of income taxes) for the year ended December 31, 2009. No material compensation costs were recorded in 2008 for these awards because none of the performance measures for the 2008 performance period were attained.
A summary of non-vested performance-based restricted shares follows:
| Non-vested performance-based restricted shares |
Weighted average fair value at date of grant |
|||||||
| Balances, December 31, 2009 |
220,186 | |||||||
| Granted |
308,449 | $ | 18.01 | |||||
| Vested |
(92,273 | ) | 14.93 | |||||
| Canceled |
(2,379 | ) | $ | 17.87 | ||||
| Balances, December 31, 2010 |
433,983 | |||||||
The performance measures and fair value for each vesting period of a performance-based restricted share award are established annually. The performance measures and fair value for the non-vested performance-based restricted shares have not been established for vesting periods with performance measures determined after December 31, 2010.
NOTE 14 – EMPLOYEE BENEFIT PLANS
The Company maintains defined contribution retirement plans covering employees who meet certain minimum eligibility requirements. Benefits are determined as a percentage of a participant’s contributions and generally are vested based upon length of service. Retirement plan expense was $2.5 million for 2010, $9.7 million for 2009 and $9.4 million for 2008. During 2010, the Company reduced the benefits under the plans. Amounts equal to retirement plan expense are funded annually.
F-34
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 15 – ACCRUED LIABILITIES
A summary of other accrued liabilities at December 31 follows (in thousands):
| 2010 | 2009 | |||||||
| Taxes other than income |
$ | 40,318 | $ | 29,880 | ||||
| Patient accounts |
34,735 | 36,546 | ||||||
| Other |
11,959 | 11,932 | ||||||
| $ | 87,012 | $ | 78,358 | |||||
NOTE 16 – FINANCIAL INSTRUMENTS AND FAIR VALUE MEASUREMENTS
The Company follows the provisions of the authoritative guidance for fair value measurements, which addresses how companies should measure fair value when they are required to use a fair value measure for recognition or disclosure purposes under generally accepted accounting principles.
Fair value is defined as the exchange price that would be received for an asset or paid to transfer a liability in the principal or most advantageous market for the asset or liability in an orderly transaction between market participants on the measurement date. The guidance related to fair value measures referenced in Note 1 establishes a fair value hierarchy that requires an entity to maximize the use of observable inputs and minimize the use of unobservable inputs when measuring fair value. The guidance describes three levels of inputs that may be used to measure fair value:
| Level 1 |
Quoted prices in active markets for identical assets or liabilities. Level 1 assets and liabilities include debt and equity securities and derivative contracts that are traded in an active exchange market, as well as certain U.S. Treasury, other U.S. Government and agency asset backed debt securities that are highly liquid and are actively traded in over-the-counter markets. | |
| Level 2 |
Observable inputs other than Level 1 prices, such as quoted prices for similar assets or liabilities, quoted prices in markets that are not active, and other inputs that are observable or can be corroborated by observable market data for substantially the full term of the assets or liabilities. | |
| Level 3 |
Unobservable inputs that are supported by little or no market activity and that are significant to the fair value of the assets or liabilities. Level 3 assets and liabilities include financial instruments whose value is determined using pricing models, discounted cash flow methodologies, or similar techniques, as well as instruments for which the determination of fair value requires significant management judgment or estimation. | |
F-35
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 16 – FINANCIAL INSTRUMENTS AND FAIR VALUE MEASUREMENTS (Continued)
The Company’s assets and liabilities measured at fair value on a recurring and non-recurring basis and any associated losses for the twelve months ended December 31, 2010 and 2009 are summarized below (in thousands):
| Fair value measurements | Assets/ liabilities at fair value |
Total losses |
||||||||||||||||||
| Level 1 | Level 2 | Level 3 | ||||||||||||||||||
| December 31, 2010: |
||||||||||||||||||||
| Recurring: |
||||||||||||||||||||
| Assets: |
||||||||||||||||||||
| Available-for-sale debt securities: |
||||||||||||||||||||
| Corporate bonds |
$ | – | $ | 32,676 | $ | – | $ | 32,676 | $ | – | ||||||||||
| Debt securities issued by U.S. government agencies |
– | 17,992 | – | 17,992 | – | |||||||||||||||
| U.S. Treasury notes |
2,493 | – | – | 2,493 | – | |||||||||||||||
| Debt securities issued by foreign governments |
– | 2,096 | – | 2,096 | – | |||||||||||||||
| Commercial mortgage-backed securities |
– | 326 | – | 326 | – | |||||||||||||||
| 2,493 | 53,090 | – | 55,583 | – | ||||||||||||||||
| Available-for-sale equity securities |
12,011 | – | – | 12,011 | – | |||||||||||||||
| Commercial paper |
– | 5,705 | – | 5,705 | – | |||||||||||||||
| Money market funds |
2,581 | – | – | 2,581 | – | |||||||||||||||
| Total available-for-sale investments |
17,085 | 58,795 | – | 75,880 | – | |||||||||||||||
| Deposits held in money market funds |
7,238 | 3,001 | – | 10,239 | – | |||||||||||||||
| $ | 24,323 | $ | 61,796 | $ | – | $ | 86,119 | $ | – | |||||||||||
| Liabilities |
$ | – | $ | – | $ | – | $ | – | $ | – | ||||||||||
| Non-recurring: |
||||||||||||||||||||
| Assets: |
||||||||||||||||||||
| Hospitals available for sale |
$ | – | $ | – | $ | 5,605 | $ | 5,605 | $ | (1,880 | ) | |||||||||
| Liabilities |
$ | – | $ | – | $ | – | $ | – | $ | – | ||||||||||
| December 31, 2009: |
||||||||||||||||||||
| Recurring: |
||||||||||||||||||||
| Assets: |
||||||||||||||||||||
| Available-for-sale debt securities: |
||||||||||||||||||||
| Corporate bonds |
$ | – | $ | 48,196 | $ | – | $ | 48,196 | $ | – | ||||||||||
| Debt securities issued by U.S. government agencies |
– | 37,968 | – | 37,968 | – | |||||||||||||||
| U.S. Treasury notes |
2,820 | – | – | 2,820 | – | |||||||||||||||
| Debt securities issued by foreign governments |
– | 619 | – | 619 | – | |||||||||||||||
| Commercial mortgage-backed securities |
– | 637 | – | 637 | – | |||||||||||||||
| 2,820 | 87,420 | – | 90,240 | – | ||||||||||||||||
| Available-for-sale equity securities |
11,214 | – | – | 11,214 | – | |||||||||||||||
| Commercial paper |
– | 9,460 | – | 9,460 | – | |||||||||||||||
| Money market funds |
4,692 | – | – | 4,692 | – | |||||||||||||||
| Total available-for-sale investments |
18,726 | 96,880 | – | 115,606 | – | |||||||||||||||
| Deposits held in money market funds |
351 | 3,000 | – | 3,351 | – | |||||||||||||||
| $ | 19,077 | $ | 99,880 | $ | – | $ | 118,957 | $ | – | |||||||||||
| Liabilities |
$ | – | $ | – | $ | – | $ | – | $ | – | ||||||||||
| Non-recurring: |
||||||||||||||||||||
| Assets: |
||||||||||||||||||||
| Acquired previously leased hospital |
$ | – | $ | 18,000 | $ | – | $ | 18,000 | $ | – | ||||||||||
| Nursing and rehabilitation centers available for sale |
– | – | 1,000 | 1,000 | (21,870 | ) | ||||||||||||||
| $ | – | $ | 18,000 | $ | 1,000 | $ | 19,000 | $ | (21,870 | ) | ||||||||||
| Liabilities |
$ | – | $ | – | $ | – | $ | – | $ | – | ||||||||||
F-36
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 16 – FINANCIAL INSTRUMENTS AND FAIR VALUE MEASUREMENTS (Continued)
Recurring measurements
The Company’s available-for-sale investments are held by its limited purpose insurance subsidiary and consist of debt securities, equities, commercial paper and money market funds. These available-for-sale investments and the insurance subsidiary’s cash and cash equivalents of $102.1 million as of December 31, 2010 and $91.5 million as of December 31, 2009, classified as insurance subsidiary investments, are maintained for the payment of claims and expenses related to professional liability and workers compensation risks.
The Company’s deposits held in money market funds consist primarily of cash and cash equivalents held for general corporate purposes.
The fair value of actively traded debt and equity securities and money market funds are based upon quoted market prices and are generally classified as Level 1. The fair value of inactively traded debt securities and commercial paper are based upon either quoted market prices of similar securities or observable inputs such as interest rates using either a market or income valuation approach and are generally classified as Level 2. The Company’s investment advisors obtain and review pricing for each security. The Company is responsible for the determination of fair value and as such the Company reviews the pricing information from its advisors in determining reasonable estimates of fair value. Based upon the Company’s internal review procedures, there were no adjustments to the prices during 2010 or 2009.
The following table presents the carrying amounts and estimated fair values of the Company’s financial instruments. The carrying value is equal to fair value for financial instruments that are based upon quoted market prices or current market rates.
| 2010 | 2009 | |||||||||||||||
| (In thousands) |
Carrying value |
Fair value |
Carrying value |
Fair value |
||||||||||||
| Cash and cash equivalents |
$ | 17,168 | $ | 17,168 | $ | 16,303 | $ | 16,303 | ||||||||
| Cash–restricted |
5,494 | 5,494 | 5,820 | 5,820 | ||||||||||||
| Insurance subsidiary investments |
177,963 | 177,963 | 207,057 | 207,057 | ||||||||||||
| Tax refund escrow investments |
213 | 213 | 215 | 215 | ||||||||||||
| Long-term debt, including amounts due within one year |
365,647 | 365,640 | 147,733 | 147,724 | ||||||||||||
Non-recurring measurements
In December 2010, the Company reduced the fair value of hospitals held for sale, which resulted in a pretax loss of $3.1 million recorded in discontinued operations. The primary reason for the reduction was the general deterioration in the real estate markets where the hospitals are located. The fair value of the assets were measured using Level 3 unobservable inputs, including sales comparisons of similar properties in the same geographic market or region, which were then adjusted.
In March 2009, the Company acquired a previously leased hospital for $15.6 million in cash and $1.6 million in unamortized prepaid rent. The fair value of the assets was measured using Level 2 observable inputs, including replacement costs and direct sales comparisons of similar properties in the same geographic market or region.
In June 2009, the Company purchased the Nursing Centers from Ventas for $55.7 million. In addition, the Company paid Ventas a lease termination fee of $2.3 million. The Company used unobservable inputs for the valuation methodology that are significant to the fair value measurement and required management’s judgment
F-37
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 16 – FINANCIAL INSTRUMENTS AND FAIR VALUE MEASUREMENTS (Continued)
Non-recurring measurements (Continued)
related to the assumptions market participants would use in pricing the assets. The valuation of these assets also included sales comparisons of similar properties and past transactions, in addition to expected proceeds negotiated with potential purchasers. In aggregate, the assets had a carrying value of $61.4 million and were adjusted to a fair value of $27.2 million, less expected selling costs of $1.4 million, resulting in an impairment charge of $35.6 million ($21.9 million net of income taxes).
During 2010, the Company sold one of the Nursing Centers held for sale for $1.0 million. During 2009, the Company sold five of the Nursing Centers for $26.2 million and also recorded additional costs of $3.9 million ($2.4 million net of income taxes) related to the disposal of the Nursing Centers.
NOTE 17 – LITIGATION
The Company is a party to various legal actions (some of which are not insured), and regulatory and other governmental audits and investigations in the ordinary course of its business. The Company cannot predict the ultimate outcome of pending litigation and regulatory and other governmental audits and investigations. These matters could potentially subject the Company to sanctions, damages, recoupments, fines and other penalties. The DOJ, CMS or other federal and state enforcement and regulatory agencies may conduct additional investigations related to the Company’s businesses in the future that may, either individually or in the aggregate, have a material adverse effect on the Company’s business, financial position, results of operations and liquidity.
NOTE 18 – SUBSEQUENT EVENT
On February 7, 2011, the Company entered into an Agreement and Plan of Merger (the “Merger Agreement”) with RehabCare Group, Inc. (“RehabCare”), providing for the acquisition of RehabCare by Kindred. Subject to the terms and conditions of the Merger Agreement, RehabCare will be merged with and into Kindred (the “Merger”), with Kindred surviving the Merger.
At December 31, 2010, RehabCare operated 29 LTAC hospitals, five inpatient rehabilitation hospitals and provided rehabilitation therapy services in 116 acute care hospitals and 1,112 skilled nursing facilities in 42 states. RehabCare reported consolidated revenues of approximately $1.3 billion and net income from continuing operations of approximately $65 million in fiscal 2010.
The Merger will form the largest post-acute healthcare services company in the United States with over $6 billion in annual revenues and operations in 46 states. The combined company will be a leading operator of LTAC hospitals, nursing and rehabilitation centers, skilled and acute care rehabilitation therapy contract services and inpatient rehabilitation facilities. This transaction, valued at approximately $1.3 billion, will further the Company’s cluster market strategy, add to its existing LTAC hospital and skilled nursing contract rehabilitation therapy businesses and expand the Company’s service offerings to include the acute care inpatient rehabilitation therapy business.
At the effective time of the Merger, each share of RehabCare common stock outstanding immediately prior to the effective time (subject to certain exceptions) will be converted into the right to receive 0.471 of a share of Kindred common stock and $26.00 in cash, without interest (the “Merger Consideration”). No fractional shares of Kindred common stock will be issued in the Merger, and RehabCare’s stockholders will receive cash in lieu of fractional shares. The Merger Agreement also provides for the vesting and conversion of certain employee stock options and restricted shares of RehabCare. Outstanding Kindred common stock will not be affected by the Merger. Upon completion of the transaction, RehabCare stockholders will own approximately 22% of Kindred’s outstanding common stock.
F-38
Table of Contents
KINDRED HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
NOTE 18 – SUBSEQUENT EVENT (Continued)
The consummation of the Merger is subject to certain conditions, including the adoption by the RehabCare and Kindred stockholders of the Merger Agreement; clearance under the Hart-Scott-Rodino Antitrust Improvements Act of 1976, as amended; receipt of certain other licensure and regulatory approvals; receipt of the proceeds of the financing described below; and other customary closing conditions.
The Merger Agreement contains customary representations, warranties and covenants, including covenants providing for each of the parties (i) to use reasonable best efforts to cause the transaction to be consummated and (ii) to call and hold a stockholders’ meeting and recommend adoption of the Merger Agreement, subject to fiduciary duties. The Merger Agreement also requires RehabCare to conduct its operations in all material respects according to the ordinary course of business consistent with past practice until the closing of the Merger. RehabCare is subject to customary “no-shop” restrictions on its ability to solicit acquisition proposals from third parties and to provide information to and engage in discussions with third parties about acquisition proposals, subject to a “fiduciary duty” exception in certain circumstances prior to adoption of the Merger Agreement by RehabCare’s stockholders.
The Merger Agreement also contains certain termination rights and provides that (i) upon termination of the Merger Agreement under specified circumstances, including a change in the recommendation of the board of directors of RehabCare or termination of the Merger Agreement to enter into a written definitive agreement for a “superior proposal,” RehabCare must pay Kindred a termination fee of $26 million and (ii) upon the termination of the Merger Agreement under specified circumstances, including a change in the recommendation of the board of directors of Kindred or Kindred’s failure to complete the financing discussed below, after all other closing conditions have been met, Kindred must pay RehabCare a cash termination fee of $62 million.
Kindred has obtained a financing commitment from JPMorgan Chase Bank, N.A., J.P. Morgan Securities LLC, Morgan Stanley Senior Funding, Inc. and Citigroup Global Markets Inc. in connection with the pending acquisition. These funds and existing cash balances are expected to be sufficient to fund the cash consideration to RehabCare stockholders and to refinance certain existing Kindred and RehabCare debt. Subject to certain conditions, Kindred expects to have in place approximately $1.9 billion of long-term financing, of which approximately $1.6 billion is expected to be outstanding at the time of consummation of the pending acquisition.
On February 10, 2011, a purported class action complaint relating to the RehabCare acquisition was filed in the Circuit Court of St. Louis County, Missouri, against RehabCare and certain of its directors and officers, as well as the Company, by Arthur I. Murray, Jr., individually and on behalf of all of the Company’s stockholders, excluding the defendants and their affiliates. The complaint alleges, among other allegations, that the consideration that RehabCare’s stockholders will receive in connection with the proposed transaction is inadequate and that the individual RehabCare defendants breached their fiduciary duties to stockholders in approving the Merger Agreement. The complaint further alleges that the individual RehabCare defendants were aided and abetted in such breaches by RehabCare and the Company. The complaint seeks various forms of relief, including injunctive relief that would, if granted, prevent the RehabCare acquisition from being consummated in accordance with the agreed-upon terms. The case is styled Arthur I. Murray, Jr. v. RehabCare Group, Inc., et al. (No. I.I.S.L. – CC00566, Circuit Court, St. Louis Co., MO). Another purported class action complaint, styled Norfolk County Retirement System v. Harry E. Rich, et al. (C.A. No. 6197 (DE (Wilmington) Court of Chancery) and filed on February 15, 2011, asserts substantially identical claims and seeks similar relief against RehabCare, certain of its directors and officers and the Company, on behalf of all of the Company’s stockholders, excluding the defendants and their affiliates. The Company believes that these complaints are without merit and intends to defend them vigorously.
F-39
Table of Contents
KINDRED HEALTHCARE, INC.
QUARTERLY CONSOLIDATED FINANCIAL INFORMATION (UNAUDITED)
(In thousands, except per share amounts)
The following table represents summary quarterly consolidated financial information (unaudited) for the years ended December 31, 2010 and 2009:
| 2010 (a) | ||||||||||||||||
| First | Second | Third | Fourth | |||||||||||||
| Revenues |
$ | 1,089,837 | $ | 1,081,364 | $ | 1,053,012 | $ | 1,135,484 | ||||||||
| Net income: |
||||||||||||||||
| Income from continuing operations |
15,155 | 16,136 | 5,100 | 19,755 | ||||||||||||
| Discontinued operations, net of income taxes: |
||||||||||||||||
| Income (loss) from operations |
(154 | ) | 87 | (260 | ) | 1,125 | ||||||||||
| Gain (loss) on divestiture of operations |
(137 | ) | 54 | 86 | (456 | ) | ||||||||||
| Net income |
14,864 | 16,277 | 4,926 | 20,424 | ||||||||||||
| Earnings per common share: |
||||||||||||||||
| Basic: |
||||||||||||||||
| Income from continuing operations |
0.38 | 0.41 | 0.13 | 0.50 | ||||||||||||
| Discontinued operations: |
||||||||||||||||
| Income (loss) from operations |
– | – | (0.01 | ) | 0.03 | |||||||||||
| Gain (loss) on divestiture of operations |
– | – | – | (0.01 | ) | |||||||||||
| Net income |
0.38 | 0.41 | 0.12 | 0.52 | ||||||||||||
| Diluted: |
||||||||||||||||
| Income from continuing operations |
0.38 | 0.41 | 0.13 | 0.50 | ||||||||||||
| Discontinued operations: |
||||||||||||||||
| Income (loss) from operations |
– | – | (0.01 | ) | 0.03 | |||||||||||
| Gain (loss) on divestiture of operations |
– | – | – | (0.01 | ) | |||||||||||
| Net income |
0.38 | 0.41 | 0.12 | 0.52 | ||||||||||||
| Shares used in computing earnings per common share: |
||||||||||||||||
| Basic |
38,626 | 38,756 | 38,778 | 38,790 | ||||||||||||
| Diluted |
38,859 | 38,914 | 38,838 | 39,089 | ||||||||||||
| Market prices: |
||||||||||||||||
| High |
19.76 | 18.83 | 13.75 | 19.59 | ||||||||||||
| Low |
16.01 | 12.75 | 11.50 | 12.52 | ||||||||||||
| 2009 (a) | ||||||||||||||||
| First | Second | Third | Fourth | |||||||||||||
| Revenues |
$ | 1,069,474 | $ | 1,073,054 | $ | 1,057,488 | $ | 1,069,991 | ||||||||
| Net income (loss): |
||||||||||||||||
| Income from continuing operations |
23,341 | 17,538 | 5,388 | 16,345 | ||||||||||||
| Discontinued operations, net of income taxes: |
||||||||||||||||
| Income (loss) from operations |
(581 | ) | (897 | ) | 13 | 2,396 | ||||||||||
| Gain (loss) on divestiture of operations |
– | (24,051 | ) | 52 | 567 | |||||||||||
| Net income (loss) |
22,760 | (7,410 | ) | 5,453 | 19,308 | |||||||||||
| Earnings (loss) per common share: |
||||||||||||||||
| Basic: |
||||||||||||||||
| Income from continuing operations |
0.60 | 0.45 | 0.14 | 0.42 | ||||||||||||
| Discontinued operations: |
||||||||||||||||
| Income (loss) from operations |
(0.02 | ) | (0.02 | ) | – | 0.06 | ||||||||||
| Gain (loss) on divestiture of operations |
– | (0.62 | ) | – | 0.01 | |||||||||||
| Net income (loss) |
0.58 | (0.19 | ) | 0.14 | 0.49 | |||||||||||
| Diluted: |
||||||||||||||||
| Income from continuing operations |
0.60 | 0.45 | 0.14 | 0.42 | ||||||||||||
| Discontinued operations: |
||||||||||||||||
| Income (loss) from operations |
(0.02 | ) | (0.02 | ) | – | 0.06 | ||||||||||
| Gain (loss) on divestiture of operations |
– | (0.62 | ) | – | 0.01 | |||||||||||
| Net income (loss) |
0.58 | (0.19 | ) | 0.14 | 0.49 | |||||||||||
| Shares used in computing earnings (loss) per common share: |
||||||||||||||||
| Basic |
38,184 | 38,307 | 38,398 | 38,465 | ||||||||||||
| Diluted |
38,315 | 38,415 | 38,524 | 38,693 | ||||||||||||
| Market prices: |
||||||||||||||||
| High |
18.57 | 17.83 | 17.27 | 20.00 | ||||||||||||
| Low |
11.51 | 10.70 | 11.83 | 13.80 | ||||||||||||
| (a) | See accompanying discussion of certain quarterly items. |
F-40
Table of Contents
KINDRED HEALTHCARE, INC.
QUARTERLY CONSOLIDATED FINANCIAL INFORMATION (UNAUDITED) (Continued)
SIGNIFICANT QUARTERLY ADJUSTMENTS
The following is a description of significant quarterly adjustments recorded during 2010 and 2009:
Fourth quarter 2010
Operating results for the fourth quarter of 2010 included pretax charges related to acquisition-related costs of $2.1 million.
Third quarter 2010
Operating results for the third quarter of 2010 included pretax charges related to acquisition-related costs of $0.8 million. The provision for income taxes included a favorable adjustment of $2.9 million related to the resolution of state income tax contingencies from prior years.
Second quarter 2010
Operating results for the second quarter of 2010 included pretax charges related to acquisition-related costs of $0.9 million.
First quarter 2010
Operating results for the first quarter of 2010 included pretax charges related to severance and retirement costs of $2.9 million and acquisition-related costs of $0.8 million.
Third quarter 2009
The provision for income taxes included a favorable adjustment of $1.7 million related to the resolution of state income tax contingencies from prior years.
F-41
Table of Contents
KINDRED HEALTHCARE, INC.
SCHEDULE II — VALUATION AND QUALIFYING ACCOUNTS
FOR THE YEARS ENDED DECEMBER 31, 2010, 2009 AND 2008
(In thousands)
| Additions | ||||||||||||||||||||
| Balance at beginning of period |
Charged to costs and expenses |
Other | Deductions or payments |
Balance at end of period |
||||||||||||||||
| Allowance for loss on accounts receivable: |
||||||||||||||||||||
| Year ended December 31, 2008 |
$ | 33,305 | $ | 32,336 | $ | – | $ | (38,093 | ) | $ | 27,548 | |||||||||
| Year ended December 31, 2009 |
27,548 | 29,320 | – | (36,712 | ) | 20,156 | ||||||||||||||
| Year ended December 31, 2010 |
20,156 | 24,397 | – | (30,969 | ) | 13,584 | ||||||||||||||
| Allowance for deferred taxes: |
||||||||||||||||||||
| Year ended December 31, 2008 |
$ | 11,328 | $ | – | $ | 34,012 | (a) | $ | (9,788 | ) | $ | 35,552 | ||||||||
| Year ended December 31, 2009 |
35,552 | – | – | (482 | ) | 35,070 | ||||||||||||||
| Year ended December 31, 2010 |
35,070 | – | 3,833 | (a) | (472 | ) | 38,431 | |||||||||||||
| (a) | The Company identified deferred income tax assets for state income tax NOLs of $42.2 million, $37.9 million and $34.0 million at December 31, 2010, December 31, 2009 and December 31, 2008, respectively, and a corresponding deferred income tax valuation allowance of $37.8 million at December 31, 2010 and $34.0 million at December 31, 2009 and 2008 after determining that a portion of these net deferred income tax assets were not realizable. |
F-42
