Attached files
| file | filename |
|---|---|
| 8-K - FORM 8-K - AMEDISYS INC | d8k.htm |
Exhibit 99.1

| ||||
| Open Letter to Shareholders | ||||
| July 15, 2010 | ||||

www.amedisys.com
07/10
Dear Shareholders,
As you may be aware, The Wall Street Journal (WSJ) published an article on April 26, 2010 that questions the home health industry therapy utilization trends. This one press report has led to an inquiry of Amedisys and other home health agencies by the Senate Finance Committee (SFC), which has requested documents and information relating to our therapy utilization trends. Since the SFC announced its inquiry, the Securities and Exchange Commission (SEC) also has requested documents and information from us. Amedisys is cooperating with both the SFC and the SEC.
As we promised during Tuesday’s investor update call, enclosed is a summary of some of the key data points we included in our submission to the SFC regarding our therapy utilization trends. We have also included some additional information we believe is appropriate to share with you at this time.
We believe this information will provide helpful insight regarding how Amedisys cares for the patients entrusted to our care, and in particular, how we use therapy to improve the outcomes of our patients.
In summary:
| • | Our therapy visits are consistent with standard ranges of therapy utilization in our industry. Amedisys, like all providers, has a responsibility to provide its patients all care that is medically necessary. Our therapy distribution falls within the ranges published in The Guide to Physical Therapy Practice and other recognized sources. CMS’ studies analyzing the data of therapy provided in the outpatient setting from 2002, 2004, 2006, 2007 and 2008 also support our therapy trends. |
| • | Our therapy visits track patient acuity. Sicker, more complex, patients generally require higher levels of therapy than healthier patients. Our therapy distribution tracks the acuity (or sickness) of our patients, with sicker patients receiving more therapy than their healthier counterparts. |
| • | Therapy trends are not based on a static patient population year-over-year. In fact, our patient population from 2007 – 2008 was impacted by several key factors, including: |
| a) | an influx of patients from Inpatient Rehabilitation Facilities to home health as a result of the 75 Percent Rule; |
| b) | our Balanced for LifeSM falls prevention program reaching scale; |
| c) | we completed our largest acquisition to date, TLC Healthcare Services, Inc., which brought a more diverse mix of patients into our care; and |
| d) | we began to implement other multidisciplinary programs focused on specific patient needs including wound care and stroke recovery |

|
1 |
| • | Amedisys provides more therapy above Medicare payment thresholds – we simply deliver the care patients need and their doctors prescribe. We exceeded the national average for providing uncompensated therapy visits in excess of 10 per episode by three percent in 2006 and 2007. We exceeded the national average by 7.1% in providing uncompensated 21-plus visit episodes in 2008 and 2009. Amedisys’ uncompensated visits in these years totaled more than $95 million. |
| • | Only licensed therapists may recommend therapy, and only physicians may approve it. Our policies respect that recommending and ordering therapy are strictly clinical responsibilities, and prohibit our business people from improperly interfering or attempting to influence these matters. |
| • | Our physician consultants are not compensated for referrals. Amedisys has structured its physician consultant compensation to exceed the standards required under federal law. In 2009, the average Amedisys physician consultant compensation totaled no more than $2,600 for the year. We believe our physician consultants serve in this capacity not primarily to make money, but to better serve their patients. |
| • | We deliver quality care for our patients and save Medicare dollars. In fact, in May of this year, CMS recognized the quality of our care by awarding us $3.4 million based upon our performance during our first year of participating in the Medicare Home Health Pay for Performance (HHP4P) demonstration out of the total $15.4 million paid by CMS to the entire industry. CMS is sharing savings in the program with agencies that either maintained high levels of quality or made significant improvements in quality of care. |
Before addressing these matters in more detail, we would first like to provide you some more general information concerning our Company.
About Amedisys
Amedisys has been and will continue to be a leader in the home health care and hospice industries, working to improve patient outcomes, drive better practices and use state of the art technologies.
We believe in our organization and our people, and we are not letting these matters distract us from our mission. We remain intensely focused on our goal of delivering quality, cost effective care for the 35,000 patients we serve across the country every day. We are proud of the clinical outcomes we have achieved for our home health care patients, which are among the best in the industry.
Our views are supported by the “Home Health Compare” data collected and reported by the Centers for Medicare & Medicaid Services (CMS) on 12 quality indicators, which show that we met or exceeded the average in 11 of the 12 measurement categories in the geographic footprint we serve and 9 of the 12 measurement categories on a national basis.

|
2 |
CMS measures home health quality outcomes using a federally mandated assessment and data collection instrument at specified time points in a patient’s encounter with home health. This instrument is known as OASIS (Outcomes Assessment Information Set). CMS’s intent is that this data collection instrument helps home health agencies systematically plan for using resources and evaluate how their patients fare during an episode of care.
In addition to our focus on quality, we have been leading innovations in the modern home health movement.
| • | We were one of the first health care companies to develop and bring to market a multidisciplinary approach to falls prevention with our Balanced for LifeSM program. |
| • | We were the first home health care services company to develop advanced chronic care management programs for diabetes, cardiac disease, wound care, COPD, stroke and seven other illnesses. |
| • | We were the first in the home health services industry to adopt technology to provide better, more efficient care for our patients including a patient call center (Encore), laptop point-of-care (POC) systems that enable us to provide a uniform standard of high quality care and the first to design a method of communicating electronically with our patient’s supervising physicians to provide better, more responsive care (MercuryDoc). |
| • | We were the first in the home health services industry to design and launch a national hospital care transitions and readmission reduction program (called Care Transitions); and the first to combine all the resources mentioned above into a comprehensive care coordination and management delivery model – C4M™ : Comprehensive, Continuous, Chronic Care Management. |
And, we do all of this as an investment in the promise that we are a part of the solution to solving one of nation’s most pressing health care issues – caring for the growing population of the aging and chronically ill. We have done this at our own expense. We do not receive any incremental reimbursement for Encore or Care Transitions or Mercury Doc. We have done these things because it’s what’s right for our patients.
Our goal is to continue to lead the industry in quality, improved patient outcomes and efficiency.

|
3 |
Our Response to Recent Developments
Leaders in complex and highly regulated industries such as ours sometimes become targets of criticism.
We have received some inquiries from you seeking our perspective on these issues, as well as many letters of support, which we truly appreciate. We believe our shareholders deserve transparency from us so we want to provide you with our current perspective on these matters and also clarify some key points.
Senate Finance Committee Inquiry: We have made a number of submissions to the Senate Finance Committee, and expect to make additional submissions as we cooperate with its inquiry. We are confident that our responses will aid the SFC in better understanding our complex industry and therapy utilization in general. We believe the information we have provided, and will provide, will underscore for the SFC the significant value that Amedisys and the home health care industry brings to patients, their families, and the nation’s healthcare system.
SEC Investigation: We also have received a subpoena from the Securities and Exchange Commission for documents that appear to relate to the matters under review by the Senate Finance Committee. Given the public nature of these matters it is possible that we could receive questions and interest from other regulatory authorities. We intend to cooperate with, and present our views and perspectives regarding these matters in connection with, any such inquiry.
Shareholder Lawsuits: As you may know, putative shareholder class action lawsuits and a shareholder derivative suit have been filed following the WSJ article. Regrettably, we are not surprised by the filing of these lawsuits. These types of lawyer-driven lawsuits are an unfortunate reality in today’s environment whenever a publicly traded company becomes a target of criticism and experiences a stock price decline. Amedisys intends to vigorously defend the company against claims made based on a news article that we believe did not present all of the facts.
Wall Street Journal Article: We stand by the integrity of our company and our employees. We believe the WSJ article is based upon an inaccurate understanding of a very complex industry and the ever-changing population that we serve, and that it overlooked some important facts, which we’ve pointed out to the SFC.

|
4 |
We worked extensively with the WSJ reporter, explaining in detail our business model, innovations, clinical outcomes and focus on quality. In fact, we provided the reporter with an opportunity to meet with our patients, visit our offices and speak with our staff. Despite our efforts, we were disappointed that she presented what we believe is an unbalanced story, excluding much of the data we shared with her in the spirit of full cooperation.
For example, the WSJ article focused upon the change in therapy utilization in the home health industry from 2007 to 2008, appearing to suggest that providers in the industry changed their therapy utilization to take advantage of the new Medicare reimbursement methodology that CMS implemented in 2008, without giving proper consideration to whether patients needed the care.
However, the WSJ story appeared to assume a static patient population when in fact the needs of the patients under our care in 2008 were quite different from those of the patients under our care in 2007, including a more diverse distribution of patients based upon primary diagnoses and acuity mix. The key factors impacting our shifting patient population include the trend that Amedisys has been taking care of patients who are increasingly sicker and debilitated, and therefore who need more therapy visits. At the same time, other factors have resulted in Amedisys also taking care of more lower acuity patients who require relatively fewer visits.
We believe a number of factors have contributed to these trends, including the following:
| • | In 2008, we began to reach significant scale with our roll-out of Balanced for Life™ (BFL), a multidisciplinary falls prevention program that impacted the patient population mix and therapy utilization trends. We believe the BFL program explains to a significant extent both our increase in visits (a) at the higher end (greater than 13 therapy visits per episode) of the care spectrum, because BFL is a multidisciplinary program that generally requires intensive therapy for complex patients having co-morbidities, and (b) at the lower end (less than 10 therapy visits per episode) of the care spectrum, as some patients who enter the BFL program have only a single disorder, typically of the vestibular system, and often may be treated successfully in approximately six visits . Our clinical outcomes from BFL for our patients have been positive. Our data analysis demonstrates that we’re lowering the risk of falls and also decreasing hospitalization – goals that we share with the medical community, patients, their families and legislators alike. |
| • | Also in 2008, we completed our largest acquisition to date, TLC Healthcare Services, Inc., which expanded our geographic footprint and brought a more diverse distribution of patients, |

|
5 |
specifically as it relates to primary diagnoses and acuity mix. We believe this acquisition significantly increased our number of patients with lower acuity who required fewer than 10 therapy visits.
| • | In 2008, consistent with federal health policy goals, we began to implement other multidisciplinary programs focused on specific patient needs. These included, for example, wound care, stroke recovery, patients with cognition, speech and swallowing therapy needs. Because these programs typically supplement, not supplant, the need for traditional physical therapy, we believe they had the effect of increasing overall therapy usage per episode significantly. |
| • | The 75 Percent Rule, which changed how Medicare reimbursed rehab facilities also continued to impact our patient population during this period. The effect, in our view, was a continuing influx of therapy patients previously seen in rehab facilities into home health. From the 2004 to 2009 time period, major joint replacement at Inpatient Rehab Facilities (IRFs) went from 24% of patients to 11%. Likewise, the share of hospital major joint replacement discharges to IRF’s went from 28% to 14% over the 2004 – 2008 time period. Over this same time period, home health’s share of these discharges went from 21% to 30%. We believe the 75% rule substantially changed our patient mix, particularly at the ten-visit and above level. |
In an effort to be more granular and transparent, we are providing key data that we highlighted to the Senate Finance Committee.

|
6 |
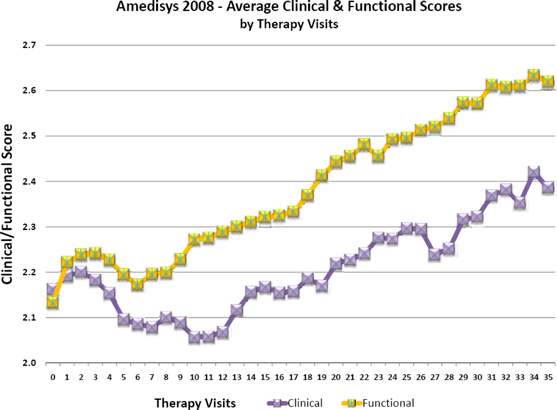
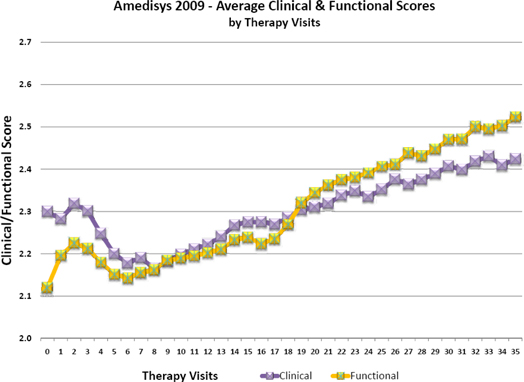
Data Point 1—Therapy Tracks Patient Acuity
Sicker, more complex patients generally need and receive more therapy than healthier patients. We believe our therapy visits track patient acuity (or sickness), plain and simple. Patient acuity is measured by tracking our patients’ clinical and functional scores, measures of patient health formulated by CMS. We believe that our therapy utilization trends in general correlate with patient acuity, which is linked to these objective clinical benchmarks.
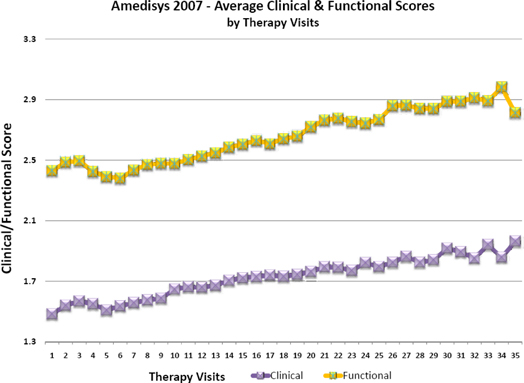

|
7 |

|
8 |

|
9 |
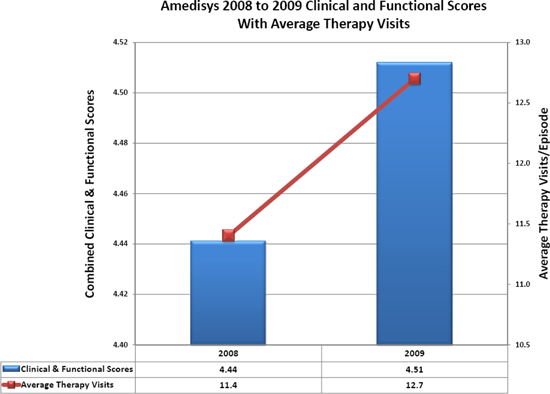
Data Point 2—Patient Acuity Changed From 2007 through 2009, with Increasing Acuity Driving More Therapy Visits
The health or acuity of our patient population has changed over time. We believe the change in therapy utilization from 2007 to 2008 is explained to a significant degree by this fact. Medication utilization is a good indicator of patient complexity, and as the corresponding chart shows there were significant year over year changes in medication over the 2007 through 2009 period, a variable that is completely dictated by the patient’s physicians. We believe that the increasing levels of patient acuity during this period drove greater numbers of therapy visits per episode.
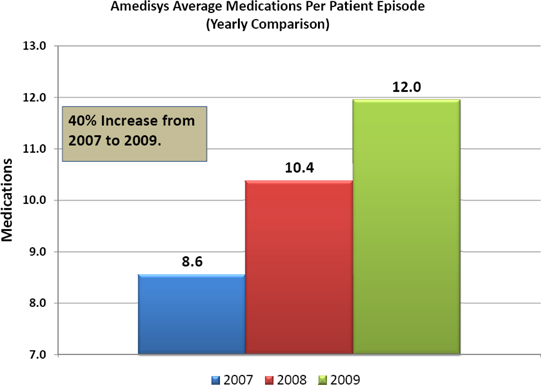
Note: Chart includes data for Home Health Medicare patients for the full years reported.
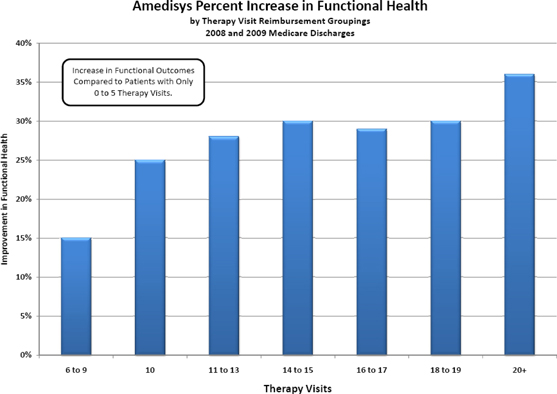
Data Point 3—Appropriate Therapy Levels Yield Positive Outcomes
Appropriate levels of therapy are necessary to yield positive patient outcomes. When we separated our therapy visits into the current nine PPS reimbursement rate categories, we found that each one of these categories was related to a significant increase in patient functioning. Thus, 6 to 9 therapy visits, 10 therapy visits, 11 to 13 therapy visits, 14 to 15 therapy visits, 16 to 17 therapy visits, 18 to 19 therapy visits, and 20 and over therapy visits were all independently related to an increase in functional scores compared to the 0 to 5 therapy visits category.

|
10 |
While the results of these aggregate models are illustrative (see chart below) we are mindful that the specific amount of therapy prescribed for each patient is unique depending on his or her combination of functional and clinical complexity. Again, sicker patients generally need and receive more therapy than those who are less sick; and therapy is recommended according to the patient’s unique needs as determined by the therapist in the exercise of his or her professional judgment, and as approved by the attending physician. These data points demonstrate that providing appropriate levels of therapy is necessary to yield positive patient outcomes.
We believe this is what CMS had in mind when it implemented reimbursement systems designed to incent providers—in the words of the CMS official quoted in the WSJ story—not to “stint on therapy.” We believe this data also attests to the efficacy of the therapy we provide to our patients.

|
11 |
Data Point 4—Balanced for LifeSM Has Yielded Very Good Patient Outcomes
We were disappointed the Wall Street Journal reporter failed to mention our successful Balanced for LifeSM program. While our BFL program is now called into question, in an ironic twist, over the last several years Congress has focused on legislation relating to falls prevention, culminating in 2007 when President Bush signed the Safety of Seniors Act. In addition, CMS’ Home Health Quality Improvement National Campaign (HHQI) demonstration taking place this month has falls prevention focus. Among older adults, falls are the most common cause of nonfatal injuries and hospital admissions for trauma, and the leading cause of injury deaths. As a result, OASIS-C, the new assessment document (implemented in January 2010) that CMS requires all home health agencies to use in evaluating patients upon admission, now incorporates elements related to fall prevention.
Amedisys has been leading the way in falls prevention with BFL for three years – the only multidisciplinary program of its kind that has leading-edge clinical outcomes.

|
12 |
BFL Yields Positive Patient Outcomes
Upon admission to the BFL program, 81% of our patients are at a high fall risk as indicated by their scores on the Tinetti Performance Oriented Mobility Assessment, a widely recognized clinical instrument used to measure fall risk. At discharge from the BFL program, only 20% of our patients remain at a high fall risk and 94% of our patients improve their balance by at least two points.
Amedisys BFL Outcomes (December 2007-December 2009)
Based on submission of over 37,000 patient outcomes who completed the Balanced for Life program.
| Fall Screening Tool |
Total Possible Score |
Initial Score |
Discharge Score |
Points Improved |
% Improved | |||||
| Tinetti POMA |
28 points | 14 | 22 | 8 points | 57% | |||||
| 4-item DGI |
12 points | 5 | 9 | 4 points | 80% | |||||
| Functional Reach |
n/a | 5.8 | 8.8 | 3 inches | 52% | |||||
| Modified Falls Efficacy Scale |
10 points | 5 | 8 | 3 points | 60% | |||||
| Loss of Protective Sensation |
10 points | 3 | 5 | 2 points | 66% | |||||
| Modified Clinical Test of Sensory Integration on Balance |
4 points | 1.2 | 2.9 | 1.7 positions |
141% |

|
13 |
Data Point 5—Amedisys Provided Significant Levels of Uncompensated Therapy, Generally Exceeding Industry Averages
Amedisys is focused on doing the right thing, at the right time, for every patient.
While our therapy utilization generally tracks the industry average, there are some notable differences.
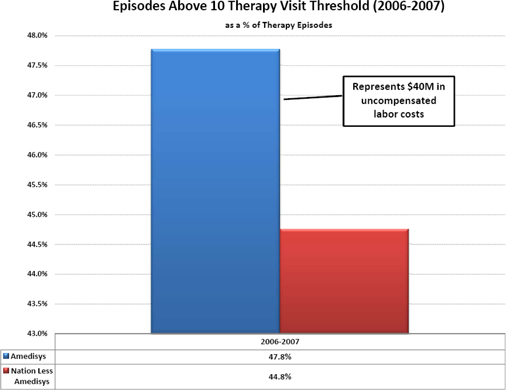
Prior to 2008, home health providers who provided fewer than 10 visits received no additional reimbursement for providing such therapy, and those providing in excess of 10 visits received no additional reimbursement for any of the visits provided in excess of 10. In 2006 and 2007, our provision of 11 or more therapy visits per episode exceeded the national average by three percent, and we incurred approximately $40 million of labor cost in providing these visits for which we received no additional compensation. We also provided a considerable volume of the therapy visits below the ten-visit threshold, for which we received no incremental compensation. The labor cost of these visits was approximately $5.2 million.
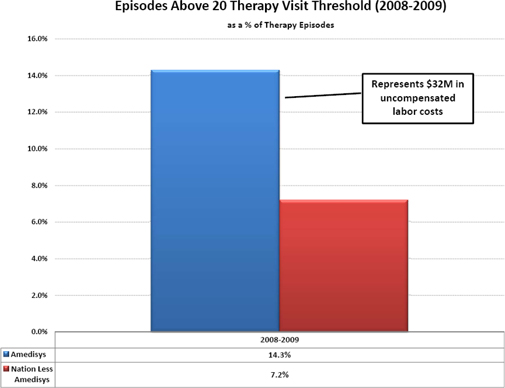
Similarly, under the new PPS system implemented in 2008, a provider has no financial incentive to provide more than 20 therapy visits in any episode. Again, Amedisys exceeded the national average by 7.1% in providing these unprofitable 21-plus visit episodes during 2008 and 2009. It is notable that our provision of uncompensated visits is trending upward. Looking at 2009 standing alone, we exceeded the national average by 11%. The labor cost to Amedisys of providing these uncompensated visits during 2008 and 2009 was approximately $32 million. We also provided a considerable volume of the therapy visits below the six-visit threshold, for which we received no incremental compensation. The labor cost of these visits was approximately $18.6 million.
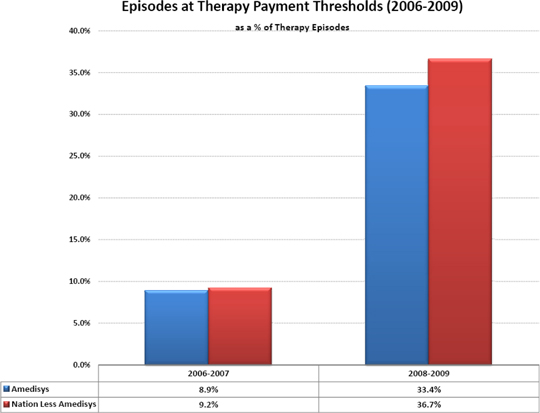
The charts on the following pages compare Amedisys’ visits performed at the therapy threshold level during the relevant time periods with those provided by the rest of the home health industry, showing that Amedisys had a lower incidence of visits that hit the threshold level than its competitors during the periods of 2006-2007 and 2008-2009.

|
14 |
Data Point 5A: Amedisys had a lower incidence of visits that hit the threshold level (and therefore, a much higher incidence of uncompensated visits).

|
15 |
Data Point 5B: Amedisys had a lower incidence of visits that hit the threshold level

|
16 |
Data Point 6—Amedisys’ Relationships with Physicians Exceed the Standards Required by Law
We will not stand idly by and allow the physicians who help us ensure quality and compliance face scrutiny without due cause.
Amedisys contracts with physicians to serve as Medical Directors or Medical Advisors. Collectively, we refer to all of these physicians as “Physician Consultants.” These experts serve an important role in ensuring our patients receive the highest quality care including providing supervision, management and oversight to the services provided by each agency to ensure that the professional services rendered meet or exceed accepted standards of care.
Amedisys has specifically structured its physician consultant compensation to exceed the standards required under federal law.
Prior to 2001, federal law limited physicians’ financial relationships with home health agencies to $25,000 or less annually. Although the enactment of Stark II regulations in 2001 eliminated this $25,000 cap, Amedisys elected to voluntarily retain this compensation ceiling for any physician consultant relationship.
Additionally, we have implemented strict contracting standards for our hourly payments to physician consultants. First, we commissioned one of the four physician compensation services recognized by the federal government in the Stark II Phase II regulations as an appropriate arbiter of fair market valuation for physician services, to conduct the first of its kind, national compensation survey for medical directors of home health and hospice.
Furthermore, we retained a national coding and reimbursement expert to analyze Medicare’s billing code for physician care plan oversight of home health services (G0181) and identify the relative value units attributable to the physician’s expertise and convert this to an hourly equivalent.
It should be noted that both of these valuations were paid for entirely by Amedisys, and in the case of the national compensation survey, the results were shared at no cost with other agencies who contributed data. The results of these two studies provide the basis for our compensation of Physician Consultants.

|
17 |
Based on the nature of the questions that have been raised regarding our financial relationships with physician consultants, one might believe that payments to physicians, and in particular to Medical Directors, were assumed to drive therapy referrals. We believe that is simply not the case.
In 2009, the average Amedisys physician consultant compensation totaled no more than $2,600 for the year. We believe this is not a role a physician takes for profit. Rather, we believe it is a role they take on as part of their responsibility to patients.
Additional Important Considerations
When considering our therapy utilization, we believe it is important to consider these additional points:
Therapists Not Incented Under Our Policies to Hit Reimbursement Thresholds.
Under our policies, employee compensation is not computed based upon any therapist or agency reaching any of the past or present Medicare reimbursement thresholds for therapy. In fact, under our policies, therapists and other employees are compensated regardless of whether Amedisys receives any reimbursement from Medicare for the therapy they perform.
Physicians Must Order Therapy.
All therapy services we deliver must be prescribed for the patient by the patient’s attending physician. Our therapists make recommendations to the patient’s attending physician concerning the number of therapy visits they project the patient will need, but under our policies the physician must approve the entire care plan, including the prescribed number of therapy visits. This includes any changes to the initially prescribed plan of care (e.g., if a therapist determines a patient actually requires fewer visits than prescribed).
Only Licensed Therapists May Recommend Therapy.
Our operating procedures respect that only the licensed therapist and the patient’s attending physician are qualified and legally permitted to make clinical judgments about how many visits a patient is to receive. Our policies do not provide for managers or business office employees to prescribe any particular number of visits for any particular patient.

|
18 |
Our Compliance Program Prohibits Improper Manipulation of Therapy.
We are serious about compliance. Our compliance program includes all elements recommended by the Office of Inspector General of the Department of Health and Human Services, and is run by a seasoned former state Medicaid fraud and abuse prosecutor, Jeffrey Jeter. We have a Zero Tolerance Policy for fraud and abuse, and manipulation of therapy thresholds is and has been an express violation of our compliance policies. We routinely audit agencies that have high therapy utilization, and conduct hundreds of clinical audits each quarter. We maintain a compliance hotline for reporting concerns.
I believe these considerations support the view that Amedisys is providing patients the therapy they need, and is doing so effectively, so as to improve patient outcomes.
In closing, I would like to make it clear that I stand by our organization and our people.
President Obama has stated that the rising cost of health care is the nation’s number one deficit problem – “nothing else even comes close.” (Speech by President Barack Obama. September 9, 2009)
Health care costs are sky rocketing, especially as it relates to Medicare’s complex patients. Amedisys is a part of the solution.
In the United States 96 percent of Medicare beneficiaries are suffering from more than one chronic illness. Chronic diseases affect approximately 133 million Americans regardless of their age, race or economic status. Over the next twenty years, the number of Americans with chronic conditions is expected to increase by 37 percent.
Currently, 12 percent of the Medicare population accounts for 69 percent of costs because they have complex, chronic illnesses. This is the exact population that Amedisys’ national network is designed to serve. And we are working with passion to position Amedisys to take advantage of opportunities presented by the recent health care reform legislation, with an eye toward becoming the undisputed leader in chronic care management of this fragile and rapidly growing population.

|
19 |
Consider this: Recent health care reforms included 16 measures that focus on the need to improve patient outcomes and reduce Medicare costs and waste by:
(a) providing chronic care coordination services to high cost Medicare beneficiaries
> Amedisys’ C4M™ model
(b) providing better transitions from hospital to home and reducing re-hospitalization rates
> Amedisys’ National Care Transitions Program
(c) moving away from fee-for-service reimbursement to paying for good results
> Amedisys’ recent CMS pay-for-performance award
(d) providing more involvement of primary care physicians including removing the artificial barriers between physicians and other providers barriers
> Amedisys’ MercuryDoc patient care portal and our AMS3 platform will facilitate this as well as the medical home and
Independence at Home model
(e) better integration of healthcare
> Again, our C4M™ model
We are building the continuum of care that Americans need. Legislation alone will not get us there. Amedisys’ resources, knowledge and skilled clinicians can.
We hope that this letter containing our perspectives as of today is helpful in providing you more information about our Company. Home health care is a critical part of the solution to our nation’s growing health care issues and Amedisys will continue to lead the way.
Thank you,
| /s/ William F. Borne |
| William F. Borne |
| Chairman & CEO, Amedisys, Inc. |

|
20 |
