Attached files
Table of Contents
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
Form 10-K
| x | ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the fiscal year ended December 31, 2009
or
| ¨ | TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the transition period from to
Commission file number: 0-8082
LHC GROUP, INC.
(Exact name of registrant as specified in its charter)
| Delaware | 71-0918189 | |
| (State or other jurisdiction of incorporation or organization) |
(I.R.S. Employer Identification No.) |
420 West Pinhook Rd, Suite A
Lafayette, Louisiana 70503
(Address of principal executive offices)
(337) 233-1307
(Registrant’s telephone number, including area code)
Securities registered pursuant to Section 12(b) of the Exchange Act:
| Common Stock, par value $.01 per share | NASDAQ Global Select Market | |
| (Title of each class) | (Name of each exchange on which registered) |
Securities registered pursuant to Section 12(g) of the Exchange Act:
None
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined by Rule 405 of the Securities Act. Yes ¨ No x
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act. Yes ¨ No x
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes x No ¨
Indicate by checkmark whether the registrant has submitted electronically and posted on its corporate Web site, in any, every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S-T (Section 232.405) during the preceding 12 months (or for such shorter period that the registrant was required to submit and post such files). Yes ¨ No ¨
Indicate by check mark if disclosure of delinquent filers pursuant to Item 405 of Regulation S-K (Section 229.405) is not contained herein, and will not be contained, to the best of registrant’s knowledge, in definitive proxy or information statements incorporated by reference in Part III of this Form 10-K or any amendment to this Form 10-K. x
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, or a smaller reporting company. See definitions of “large accelerated filer,” “accelerated filer” and “smaller reporting company” in Rule 12b-2 of the Exchange Act.
| Large accelerated filer | ¨ | Accelerated filer | x | |||
| Non-accelerated filer | ¨ | Smaller reporting company | ¨ | |||
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Act). Yes ¨ No x
As of June 30, 2009, the aggregate market value of the registrant’s common stock held by non-affiliates of the registrant was $354.3 million based on the closing sale price as reported on the NASDAQ Global Select Market. For purposes of this determination shares beneficially owned by officers, directors and ten percent shareholders have been excluded, which does not constitute a determination that such persons are affiliates.
There were 18,597,579 shares of common stock, $.01 par value, issued and outstanding as of March 8, 2010.
DOCUMENTS INCORPORATED BY REFERENCE
Portions of the Registrant’s Annual Report to stockholders for the fiscal year ended December 31, 2009 are incorporated by reference in Part II of this Annual Report on Form 10-K. Portions of the Registrant’s Proxy Statement for its 2010 Annual Meeting of Stockholders are incorporated by reference in Part III of this Annual Report on Form 10-K.
Table of Contents
TABLE OF CONTENTS
2
Table of Contents
CAUTIONARY STATEMENT REGARDING FORWARD-LOOKING STATEMENTS
This Annual Report on Form 10-K and the information incorporated by reference herein, contain certain statements and information that may constitute “forward-looking statements” within the meaning of Section 27A of the Securities Act of 1933 and Section 21E of the Securities Exchange Act of 1934 (the “Exchange Act”). Forward-looking statements relate to future plans and strategies, anticipated events or trends, future financial performance and expectations and beliefs concerning matters that are not historical facts or that necessarily depend upon future events. The words “may,” “will,” “should,” “could,” “would,” “expect,” “plan,” “anticipate,” “believe,” “foresee,” “estimate,” “predict,” “potential,” “intend” and similar expressions are intended to identify forward-looking statements. Specifically, this Annual Report on Form 10-K contains, among others, forward-looking statements about:
| • | our expectations regarding financial condition or results of operations for periods after December 31, 2009; |
| • | our critical accounting policies; |
| • | our business strategies and our ability to grow our business; |
| • | our participation in the Medicare and Medicaid programs; |
| • | the reimbursement levels of Medicare and other third-party payors; |
| • | the prompt receipt of payments from Medicare and other third-party payors; |
| • | our future sources of and needs for liquidity and capital resources; |
| • | the effect of any changes in market rates on our operating and cash flows; |
| • | our ability to obtain financing; |
| • | our ability to make payments as they become due; |
| • | the outcomes of various routine and non-routine governmental reviews, audits and investigations; |
| • | our expansion strategy, the successful integration of recent acquisitions and, if necessary, the ability to relocate or restructure our current facilities; |
| • | the value of our propriety technology; |
| • | the impact of legal proceedings; |
| • | our insurance coverage; |
| • | the costs of medical supplies; |
| • | our competitors and our competitive advantages; |
| • | our ability to attract and retain valuable employees; |
| • | the price of our stock; |
| • | our compliance with environmental, health and safety laws and regulations; |
| • | our compliance with health care laws and regulations; |
3
Table of Contents
| • | our compliance with Securities and Exchange Commission laws and regulations and Sarbanes-Oxley requirements; |
| • | the impact of federal and state government regulation on our business; and |
| • | the impact of changes in or future interpretations of fraud, anti-kickback or other laws. |
The forward-looking statements included in this report reflect our current views and assumptions only as of the date this report is filed with the Securities and Exchange Commission. Except as required by law, we assume no responsibility and do not intend to release updates or revisions to forward-looking statements after the date they are made, whether as a result of new information, future events or otherwise. The occurrence of any of the events described in Part I, Item 1A, Risk Factors in this Annual Report on Form 10-K or incorporated by reference into this Annual Report on Form 10-K, and other events that we have not predicted or assessed could have a material adverse effect on our earnings, financial condition and business, and any such forward-looking statements should not be relied on as a prediction of future events. Many factors, beyond our ability to control or predict could cause actual results or achievements to materially differ from any future results or achievements expressed in or implied by our forward-looking statements.
We qualify all of our forward-looking statements by these cautionary statements. In addition, with respect to all of our forward-looking statements, we claim the protection of the safe harbor for forward-looking statements contained in the Private Securities Litigation Reform Act of 1995.
You should read this Annual Report on Form 10-K, the information incorporated by reference into this Annual Report on Form 10-K and the documents filed as exhibits to this Annual Report on Form 10-K completely and with the understanding that our actual future results or achievements may differ materially from what we expect or anticipate.
Unless otherwise indicated, “LHC Group,” “we,” “us,” “our” and “the Company” refer to LHC Group, Inc. and its consolidated subsidiaries.
| Item 1. | Business. |
Overview
We provide post-acute health care services to patients through our home nursing agencies, hospices and long-term acute care hospitals (“LTACHs”). Through our wholly and majority owned subsidiaries, equity joint ventures and controlled affiliates, we currently operate in Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, Missouri, North Carolina, Ohio, Oklahoma, Oregon, Tennessee, Texas, Virginia, West Virginia, and Washington. We operate in two segments: home-based services and facility-based services. As of December 31, 2009, we owned and operated 264 home-based service locations, with 230 home nursing agency locations, 21 hospices, two diabetes management companies, three specialty agencies and four private duty agencies. As of December 31, 2009, we also managed the operations of four home nursing agencies in which we do not have an ownership interest. Our facility-based services included five long-term acute care hospitals with eight locations, a pharmacy, one medical equipment location and a family health center. We also managed the operations of one inpatient rehabilitation facility and an LTACH in which we have no ownership interest.
We provide home-based post-acute health care services through our home nursing agencies and hospices. Our home nursing locations offer a wide range of services, including skilled nursing, medically-oriented social services and physical, occupational and speech therapy. The nurses, home health aides and therapists in our home nursing agencies work closely with patients and their families to design and implement individualized treatments in accordance with a physician-prescribed plan of care. Our hospices provide end-of-life care to patients with terminal illnesses through interdisciplinary teams of physicians, nurses, home health aides, counselors and volunteers. Of the 264 home-based services locations, 139 are wholly-owned by us, 113 are majority-owned or controlled by us through joint ventures, eight are operated through license lease arrangements, and we manage the operations of four home nursing agencies in which we have no ownership interest.
Our LTACH locations, seven of which are located within host hospitals, provide services primarily to patients with complex medical conditions who have transitioned out of a hospital intensive care unit but whose conditions
4
Table of Contents
remain too severe for treatment in a non-acute setting. As of December 31, 2009, our hospitals had 188 licensed beds. Of our 13 facility-based services locations, four are wholly-owned by us and seven are majority-owned or controlled by us through joint ventures and we manage the operations of two locations in which we have no ownership.
Our net service revenue by segment for the years ended December 31, 2009, 2008 and 2007 was as follows (amounts in thousands):
| Year Ended December 31, | |||||||||
| 2009 | 2008 | 2007 | |||||||
| Home-Based Services | $ | 469,470 | $ | 326,041 | $ | 244,107 | |||
| Facility-Based Services | 62,510 | 56,550 | 52,910 | ||||||
| Consolidated Net Service Revenue | $ | 531,980 | $ | 382,591 | $ | 297,017 | |||
Our founders began operations in September 1994 as St. Landry Home Health, Inc. in Palmetto, Louisiana. After several years of expansion, our founders reorganized their business and began operating as Louisiana Healthcare Group, Inc. in June 2000. In March 2001, Louisiana Healthcare Group, Inc. reorganized and became a wholly owned subsidiary of The Healthcare Group, Inc., a Louisiana business corporation. In December 2002, The Healthcare Group, Inc. merged into LHC Group, LLC, a Louisiana limited liability company, with LHC Group, LLC being the surviving entity. In January 2005, LHC Group, LLC established a wholly owned Delaware subsidiary, LHC Group, Inc. and on February 9, 2005, LHC Group, LLC merged into LHC Group, Inc., a Delaware corporation. Our principal executive offices are located at 420 West Pinhook Road, Suite A, Lafayette, Louisiana, 70503. Our telephone number is (337) 233-1307. Our website is www.lhcgroup.com; information contained on our website is not part of or incorporated by reference into this Annual Report on Form 10-K.
5
Table of Contents
Industry and Market Opportunity
According to Centers for Disease Control and Prevention (“CDC”), approximately 86% of the Medicare population has one chronic condition, 66% have two or more chronic conditions, and 40% have three or more chronic conditions. Chronic diseases, such as asthma, cancer, diabetes and heart disease, are the leading causes of death and disability in the United States and account for the vast majority of healthcare spending. They affect the quality of life for 133 million Americans and are responsible for seven out of every ten deaths in the U.S. – killing more than 1.7 million Americans every year. Chronic diseases are also the primary driver of healthcare costs – accounting for more than 75 cents of every dollar we spend on healthcare in this country, as reported by the CDC. In 2007, this amounted to $1.65 trillion of the $2.2 trillion spent on healthcare.
According to a study conducted by Avalere Health in 2009, Medicare patients with diabetes, chronic obstructive pulmonary disease, or congestive heart failure that used home healthcare within 3 months of being discharged from a hospital cost the program $1.7 billion less and had 24,000 fewer re-hospitalizations than similar patients that used other forms of post-acute care over a two-year period. The analysis also found that if cumulated to the full set of Medicare beneficiaries in the study group that utilized other forms of post-acute care, the program would have saved an additional $1.7 billion. About 8.9% of Medicare fee-for-service beneficiaries currently use home health services. Based on this Avalere report and the ever rising costs of treating chronic illness, we believe there is a significant opportunity for home health to serve an expanded role in the treatment of chronic disease.
In addition to the opportunity for home care to serve an expanded role in the treatment of chronic disease, we believe there is significant opportunity for growth in the home care industry that will be driven by:
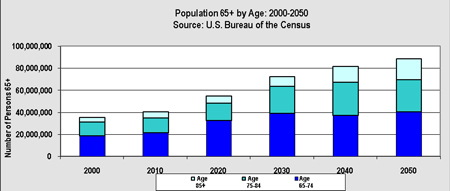
| • | a U.S. population that is getting older and living longer. According to the U.S. Bureau of the Census, the population 65 and older will increase from 35 million people in 2000 to a projected to 88.5 million in 2050. |
| • | patient preference for less restrictive care settings; |
| • | incentives for general acute care hospitals to discharge patients into less intensive treatment settings as quickly as medically appropriate; |
| • | higher incidences of chronic conditions and disease; and |
| • | a continued movement of institutionalized people into home- and community-based care. |
We also believe our post-acute service provides valuable alternatives to an underserved, rural patient population. According to the National Rural Health Association (“NRHA”), rural areas have a higher percentage of residents over the age of 65, who accounted for 18.0% of the total population in rural markets compared to 15.0% in urban
6
Table of Contents
markets. Additionally, according to NRHA, rural areas typically do not offer the range of post-acute health care services that are available in urban or suburban markets. As such, patients in rural markets face challenges in accessing health care in a convenient and appropriate setting. For example, NRHA estimates that although approximately 25% of Americans live in rural areas, less than 10% of the nation’s physicians practice in rural areas. According to NRHA, individuals in rural areas may also have difficulty reaching health care facilities due to greater travel time or a lack of public transportation. The economic characteristics and population dispersion of rural markets also make these markets less attractive to health maintenance organizations and other managed care payors. Government studies cited by NRHA have shown rural residents also tend to have more health complications than urban residents. Additionally, NRHA has noted that residents in rural areas are less likely to use preventive screening services and have a higher prevalence of disabilities, heart disease, cancer, diabetes and other chronic conditions when compared to urban residents. At December 31, 2009, 50% of our patient population lives in rural areas as designated by the Core Based Statistical Area (“CBSA”) population classification by the U.S. Office of Management and Budget (“OMB”).
We believe we are well positioned to build and maintain long-term relationships with local hospitals, physicians and other health care providers and to become the highest quality post-acute provider in our markets. In our experience, because most rural areas have the population size to support only one or two general acute care hospitals, the local hospital often plays a significant role in rural market health care delivery systems. Rural patients who require home nursing frequently receive care from a small home care agency or an agency that, while owned and run by the hospital, is not an area of focus for that hospital. Similarly, patients in these markets who require services typically offered by long-term acute care hospitals are more likely to remain in the community hospital because it is often the only local facility equipped to deal with severe, complex medical conditions. By entering these markets through affiliations with local hospitals, competition for the services we provide is minimal.
Business Strategy
Our objective is to become the leading provider of post-acute services to Medicare beneficiaries in the United States. To achieve this objective, we intend to:
Drive internal growth in existing markets. We intend to drive internal growth in our current markets by increasing the number of health care providers in each market from whom we receive referrals and by expanding the breadth of our services. We intend to achieve this growth by: (1) continuing to educate health care providers about the benefits of our services; (2) reinforcing the position of our agencies and facilities as community assets; (3) maintaining our emphasis on high-quality medical care for our patients; and (4) providing a superior work environment for our employees.
Achieve margin improvement through the active management of costs. The majority of our net service revenue is generated under Medicare prospective payment systems (“PPS”) through which we are paid pre-determined rates based upon the clinical condition and severity of the patients in our care. Because our profitability in a fixed payment system depends upon our ability to manage the costs of providing care, we continue to pursue initiatives to improve our margins and net income.
Expand into new markets. We intend to continue expanding into new markets by developing de novo locations and by acquiring existing Medicare-certified home nursing agencies in attractive markets throughout the United States. We will continue our unique strategy of partnering with non-profit hospitals in home health services, as these ventures provide significant return on investment. We also plan to look to acquire larger freestanding agencies that can serve as growth platforms in markets we do not currently serve, in order to support our growth into new states.
Pursue strategic acquisitions. We will continue to identify and evaluate opportunities for strategic acquisitions in new and existing markets that will enhance our market position, increase our referral base and expand the breadth of services we offer.
Develop joint ventures. We endeavor to joint venture with hospitals to provide post-acute services, such as home health and hospice services in communities served by hospitals already operating Medicare- certified home health agencies.
7
Table of Contents
Services
We provide post-acute care services in the United States by providing quality cost-effective health care services to patients within the comfort and privacy of their home or place of residence. Our services can be broadly classified into two principal categories: (1) home-based services offered through our home nursing agencies and hospices; and (2) facility-based services offered through our long-term acute care hospitals and inpatient rehabilitation facility.
Home-Based Services
Home Nursing. Our registered and licensed practical nurses provide a variety of medically necessary services to homebound patients who are suffering from acute or chronic illness, recovering from injury or surgery, or who otherwise require care, teaching or monitoring. These services include wound care and dressing changes, cardiac rehabilitation, infusion therapy, pain management, pharmaceutical administration, skilled observation and assessment and patient education. We have also designed guidelines to treat chronic diseases and conditions, including diabetes, hypertension, arthritis, Alzheimer’s disease, low vision, spinal stenosis, Parkinson’s disease, osteoporosis, complex wound care and chronic pain. Our home health aides provide assistance with daily living activities such as light housekeeping, simple meal preparation, medication management, bathing and walking. Through our medical social workers, we counsel patients and their families with regard to financial, personal and social concerns that arise from a patient’s health-related problems. We provide skilled nursing, ventilator and tracheotomy services, extended care specialties, medication administration and management and patient and family assistance and education. We also provide management services to third-party home nursing agencies, often as an interim solution until proper state and regulatory approvals for an acquisition can be obtained.
Our physical, occupational and speech therapists provide therapy services to patients in their home. Our therapists coordinate multi-disciplinary treatment plans with physicians, nurses and social workers to restore basic mobility skills such as getting out of bed and walking safely with crutches or a walker. As part of the treatment and rehabilitation process, a therapist will stretch and strengthen muscles, test balance and coordination abilities and teach home exercise programs. Our therapists assist patients and their families with improving and maintaining a patient’s ability to perform functional activities of daily living, such as the ability to dress, cook, clean and manage other activities safely in the home environment. Our speech and language therapists provide corrective and rehabilitative treatment to patients who suffer from physical or cognitive deficits or disorders that create difficulty with verbal communication or swallowing.
All of our home nursing agencies offer 24-hour personal emergency response and support services through Philips Lifeline (“Lifeline”) for qualified patients who require close medical monitoring but who want to maintain an independent lifestyle. These services consist principally of a communicator that connects to the telephone line in the subscriber’s home and a personal help button that is worn or carried by the individual subscriber, which when activated, initiates a telephone call from the subscriber’s communicator to Lifeline’s central monitoring facilities. Lifeline’s trained personnel identify the nature and extent of the subscriber’s particular need and notify the subscriber’s family members, neighbors and/or emergency personnel, as needed. We believe our use of the Lifeline system increases patient satisfaction and loyalty by providing our patients a point of contact between scheduled nursing visits. As a result, we provide a more complete regimen of care management than our competitors in the markets in which we operate by offering this service to qualified patients as part of their home health plan of care.
Hospice. Our Medicare-certified hospice operations provide a full range of hospice services designed to meet the individual physical, spiritual and psychosocial needs of terminally ill patients and their families. Our hospice services are primarily provided in a patient’s home but can also be provided in a nursing home, assisted living facility or hospital. Key services provided include pain and symptom management accompanied by palliative medication, emotional and spiritual support, spiritual counseling and family bereavement counseling, inpatient and respite care, homemaker services, dietary counseling and social worker visits for up to 13 months after a patient’s death.
Facility-Based Services
Long-term Acute Care Hospitals. Our LTACHs treat patients with severe medical conditions who require a high-level of care and frequent monitoring by physicians and other clinical personnel. Patients who receive our services in an LTACH are too medically unstable to be treated in a non-acute setting. Examples of these medical conditions include respiratory failure, neuromuscular disorders, cardiac disorders, non-healing wounds, renal disorders, cancer, head and neck injuries and mental disorders. These impairments often are associated with accidents, strokes, heart attacks and other serious medical conditions. We also treat patients diagnosed with musculoskeletal impairments that restrict their ability to perform normal activities of daily living. As part of our facility-based services, we operate an institutional pharmacy, which focuses on providing a full array of services to our long-term acute care hospitals and inpatient rehabilitation facility.
8
Table of Contents
Rehabilitation Services. In our facilities and through our contractual relationships, we provide physical, occupational and speech rehabilitation services. We also provide certain specialized services such as hand therapy or sports performance enhancement to treat sports and work related injuries, musculoskeletal disorders, chronic or acute pain and orthopedic conditions. Our patients are often diagnosed with musculoskeletal impairments that restrict their ability to perform normal activities of daily living. These impairments are often associated with accidents, sports injuries, strokes, heart attacks and other medical conditions. Our rehabilitation services are designed to help these patients minimize physical and cognitive impairments and maximize functional ability. We also design services to prevent short-term disabilities from becoming chronic conditions. Our rehabilitation services are provided by our physical, occupational and respiratory therapists and speech-language pathologists. We also provide management services to one inpatient rehabilitation facility and operate one health and wellness center.
Operations
Financial information relating to the home- and facility- based segments of our business is found in Note 11 to the Consolidated Financial Statements included in this Annual Report on Form 10-K. All of our operations are based in the United States.
Home-Based Services
Each of our home nursing agencies is staffed with experienced clinical home health professionals who provide a wide range of patient care services. Our home nursing agencies are managed by a Director of Nursing or Branch Manager who is also a licensed registered nurse. Our Directors of Nursing and Branch Managers are overseen by State Directors who report to Division Vice Presidents. The Senior Vice President of Home Health Operations is accountable for the oversight of the Division Vice Presidents and directly reports to the Chief Operating Officer of the Company. Our patient care operating model for our home nursing agencies is structured on a base model that requires a Medicare patient minimum census of 50 patients. At the base model level, one registered nurse is responsible for all aspects of the management of each patient’s plan of care. A home nursing agency based on this model is staffed with an office manager, a field-registered nurse, a field-licensed professional nurse and a home health aide. We also contract with local community therapists and other clinicians, as appropriate, to provide additional required services. As the size and patient census of a particular home nursing agency grows, these staffing patterns are increased appropriately.
Our home nursing agencies use our Service Value Point system, a proprietary clinical resource allocation model and cost management system. The system is a quantitative tool that assigns a target level of resource units to a group of patients based upon their initial assessment and estimated skilled nursing and therapy needs. The Service Value Point system allows the Director of Nursing or Branch Manager to allocate adequate resources throughout the group of patients assigned to his or her care, rather than focusing on the profitability of an individual patient.
Patient care is handled at the home nursing agency level. Functions that are centralized into the home office include payroll, accounting, financial reporting, billing, collections, regulatory and legal compliance, risk management, pharmacy, information technology and general clinical oversight accomplished by periodic on-site surveys. Each of our home nursing agencies is licensed and certified by the state and federal governments, and 119 agencies are accredited by the Joint Commission, a nationwide commission that establishes standards relating to the physical plant, administration, quality of patient care and operation of medical staffs of hospitals. Those not yet accredited are working towards achieving this accreditation, a process which can take up to six months. By the end of 2010, we expect to have an additional 219 agencies accredited by the Joint Commission.
Facility-Based Services
Long-Term Acute Care Hospitals. Each of our LTACH locations is managed by a Hospital Administrator, while the clinical operations are directed by a Director of Nursing who is a licensed registered nurse. The individual Hospital Administrators are responsible for managing the day-to-day operating activities of the hospital within appropriate budgetary constraints. Each Hospital Administrator reports to the Senior Vice President of Facility-Based Services. Each Director of Nursing reports directly to his or her respective hospital administrator as well as indirectly to our Director of Clinical Services responsible for the oversight of the quality of patient care services. The medical management of each patient is overseen by a Medical Director who is responsible for ensuring the appropriateness of admissions, as well as leading weekly patient care conferences.
9
Table of Contents
Our facility-based services follow a clinical approach under which each patient is discussed in weekly, multidisciplinary team meetings. In these meetings, patient progress is assessed, compared to goals and future goals are set. We believe that this model results in higher quality care, predictable discharge patterns and the avoidance of unnecessary delays.
All coding, medical records, human resources, case management, utilization review and medical staff credentialing are provided at the hospital level. Centralized functions that are provided by the home office include payroll, accounting, financial reporting, billing, collections, regulatory and legal compliance, risk management, pharmacy, information technology and general clinical oversight accomplished by periodic on-site surveys.
Rehabilitation Services. Our rehabilitation services are overseen by an administrator, who is a licensed physical therapist.
As with our LTACHs, all coding, medical records, human resources, charge/data entry, front end collections and marketing for our rehabilitation centers are provided at the individual center level. Centralized functions provided by the home office include payroll, accounting, financial reporting, billing, collections, regulatory and legal compliance, risk management, information technology and general clinical oversight accomplished by periodic on-site surveys.
Joint Ventures
As of December 31, 2009, we had 63 joint venture agreements for 120 of our agencies.
| Type of Services |
||
| Home Nursing Agencies |
105 | |
| Hospice |
8 | |
| LTACH |
7 | |
| 120 |
Our joint ventures are structured either as equity joint ventures or agency leasing arrangements, as permitted by applicable state laws and subject to business considerations. As of December 31, 2009, we had 63 equity joint ventures and four agency leasing arrangements. Of the 63 equity joint ventures, we have joint ventured with 55 hospitals, with physicians on four and with other parties on the remaining four. With respect to our four joint ventures with physicians, three involve the ownership and operation of LTACHs and one involves the ownership of a rural home nursing agency.
Equity Joint Ventures
As of December 31, 2009, we have 63 equity joint ventures for the ownership and operation of home nursing agencies, hospices, and LTACHs. Our equity joint ventures are structured as limited liability companies in which we own a majority equity interest and our partners own a minority equity interest ranging from 1% to 49%. At the time of formation, we and our partners each contribute capital to the equity joint venture in the form of cash or property. We believe that the amount contributed by each party to the equity joint venture represents their pro rata portion of the fair market value of the equity joint venture. None of our partners are required to make or influence referrals to our equity joint ventures. In fact, each of our hospital joint venture partners must follow the same Medicare discharge planning regulations, which, among other things, requires them to offer each Medicare patient a list of available Medicare-certified home nursing agency options and to allow the patient to choose his or her own provider.
We serve as the manager for our equity joint ventures and oversee their day-to-day operations. From a governance perspective, our equity joint ventures are either manager-managed or board managed. In our manager-managed joint ventures, we are designated as the manager, and, in our board managed joint ventures, we hold a majority of the votes required to take action. We possess a majority of the total votes available to be cast by the members of the management committee. However, in three of these joint ventures where we have partnered with not-for-profit hospitals, the hospital controls a majority
10
Table of Contents
of the total management committee votes. In such instances we possess the right to withdraw from the equity joint venture at any time upon notice to our partner in exchange for the receipt of a payment in an amount calculated in accordance with a predetermined fair market value formula. The members of our equity joint ventures participate in profits and losses in proportion to their equity interests. Distributions from our equity joint ventures are made pro-rata based on percentage ownership interests and are not based on referrals made to the equity joint venture by any of the members.
The 63 equity joint ventures individually contribute between 0.1% and 6.0% of our total net service revenue and only two of the equity joint ventures account for greater than 5.0% of our total net service revenue for the 12 months ended December 31, 2009. Extended Care Hospital of Lafayette, LLC, a LTACH in which we own 87.3% of the membership interests, contributed 5.0% to net service revenue, for the year ended December 31, 2009. Mississippi HomeCare of Jackson, LLC, in which we have a 66.67% ownership interest, contributed 6.0% to our consolidated net service revenue for the year ended December 31, 2009. This joint venture was converted from a license lease arrangement (discussed below) to an equity joint venture in October 2007.
Several of our equity joint ventures include a buy/sell option that grants to us and our joint venture partners the right to require the other joint venture party to either purchase all of the exercising member’s membership interests or sell to the exercising member all of the non-exercising member’s membership interests, at the non-exercising member’s option, within 30 days of the receipt of notice of the exercise of the buy/sell option. In some instances, the purchase price under these buy/sell provisions is based on a multiple of the historical or future earnings before income taxes, depreciation and amortization of the equity joint venture at the time the buy/sell option is exercised. In other instances, the buy/sell purchase price will be negotiated by the partners but will be subject to a fair market valuation process.
License Leasing Agreements
As of December 31, 2009, we have four agreements to lease, through our wholly-owned subsidiaries, the right to use the home health licenses necessary to operate five of our home nursing agencies and three hospice agencies. These leases are entered into in instances when state law would otherwise prohibit the alienation and sale of home nursing agencies. The table below details the monthly fees and termination dates of the leasing agreements. Two of the agreements are based on net quarterly projections with a cap of $160,000 per year.
| 2009 Current Monthly Fee |
Increase in Monthly Fee |
Initial Term Dates | ||
| Based on net quarterly projections with a cap of $160,000. | None |
2010 with a 5 year automatic renewal | ||
| $16,000 | 5% increase every three years | 2017 with a 2 year automatic renewal | ||
| $5,000 | Renegotiated after five years (2013) | 2017 with a 5 year automatic renewal |
In all four leasing arrangements, we have a right of first refusal in the event that the lessor intends to sell the leased agency to a third party.
Management Services Agreements
As of December 31, 2009, we have six management services agreements under which we manage the operations of four home nursing agencies, an inpatient rehabilitation facility and one LTACH, which we entered into in 2009. We currently have no ownership interest in the agencies and facilities subject to these management services agreements. As described in the agreements we provide billing, management and other consulting services suited to and designed for the efficient operation of the applicable home nursing agency, inpatient rehabilitation facility or LTACH. We are responsible for the costs associated with the locations and personnel required for the provision of services. We are compensated through one arrangement based on a percentage of cash collections, a flat fee on another arrangement and reimbursed for operating expenses and compensated based on a percentage of operating net income for the remaining two arrangements. The term of these arrangements is typically five years, with an option to renew for an additional five-year term. The termination dates for our management services agreements range from August 31, 2010 to August 31, 2014.
We record management services revenue as services are provided in accordance with the various management services agreements.
11
Table of Contents
Competition
The home health care market is highly fragmented. According to MedPac, there were approximately 10,000 Medicare-certified home nursing agencies in the United States in 2009, of which approximately 32% were hospital-based or not-for-profit, freestanding agencies. MedPAC estimates that 19% of these home nursing agencies are located in rural markets. Although there are a small number of public home nursing companies with significant home nursing operations, they generally do not compete with us in the rural markets that we currently serve. As we expand into new markets, we may encounter public companies that have greater resources or greater access to capital. Competition in our markets comes primarily from small local and regional providers. These providers include facility- and hospital-based providers, visiting nurse associations and nurse registries. We are unaware of any competitor offering our breadth of services and focusing on the needs of rural markets.
We have also entered into various joint ventures with nonprofit hospitals for the ownership and management of home nursing agencies and LTACHs. We are unaware of any competitor with this type of ownership mix.
Although several public and private national and regional companies own or manage long-term acute care hospitals, they generally do not operate in the rural markets that we serve. Generally, the competition in our markets comes from local health care providers. We believe our principal competitive advantages over these local providers are our diverse service offerings, our collaborative approach to working with health care providers, our focus on rural markets and our patient-oriented operating model.
Quality Control
In March 2008, we established the LHC Group Quality Council (“The Council”). The Council is responsible for formulating quality of care indicators, identifying performance improvement priorities, and facilitating best-practices for quality care. As part of this council, we adopted the Plan, Do, Check, Act methodology. We also set forth a quality platform for home care that reviews the following:
| • | performance improvement audits; |
| • | joint commission; |
| • | state and regulatory surveys; |
| • | home health compare; and |
| • | patient perception of care. |
The Council also has the responsibility to ensure that the infrastructure of the quality initiatives throughout the Company is appropriate, to oversee and evaluate the effectiveness of the quality plans and initiatives and to recommend appropriate quality and performance improvement initiatives.
In 2009, we established the Clinical Quality Committee of the Board of Directors (“The Committee”). The Committee is responsible for advising the Company’s clinical leadership, monitoring the performance of our locations based on internal and external benchmarks, overseeing and evaluating the effectiveness of the performance improvement and quality plans, facilitating best-practices based on internal and external comparisons and fostering enhanced awareness of clinical performance by the Board of Directors.
We have approximately 48 Performance Improvement Coordinators and 20 Performance Improvement Assistants that are all trained using a performance improvement specific orientation program and mentorship.
As part of our ongoing quality control, internal auditing and monitoring programs, we conduct internal regulatory audits and mock surveys at each of our agencies and facilities at least once a year. If an agency or facility does not achieve a satisfactory rating, we require that it prepare and implement a plan of correction. We then follow-up to verify that all deficiencies identified in the initial audit and survey have been corrected.
As required under the Medicare conditions of participation, we have a continuous quality improvement program, which involves:
| • | ongoing education of staff and quarterly continuous quality improvement meetings at each of our agencies and facilities and at our home office; |
12
Table of Contents
| • | monthly comprehensive audits of patient charts performed at each of our agencies and facilities; |
| • | at least annually, a comprehensive audit of patient charts performed on each of our agencies and facilities by our home office staff; |
| • | review of Home Health Compare scores; |
| • | assessment of patient’s perception of care using Press Ganey exit survey; and |
| • | assessment of infection control practices and risk events. |
If an agency or facility fails to achieve a satisfactory rating on a patient chart audit, we require that it prepare and implement a plan of correction.
We continually expand and refine our quality improvement programs. Specific written policies, procedures, training and educational materials and programs, as well as auditing and monitoring activities, have been prepared and implemented to address the functional and operational aspects of our business. Our programs also address specific problem areas identified through regulatory interpretation and enforcement activities. We believe our consistent focus on continuous quality improvement programs provide us with a competitive advantage in the market.
Compliance
We have established and maintain a comprehensive corporate compliance program that is designed to assist all of our employees to meet or exceed applicable standards established by federal and state laws and regulations and industry practice. Although we first established our corporate compliance program in 1996, in 2009 we redesigned and enhanced several aspects of our corporate compliance program. Our 2009 redesign and enhancement involved several initiatives to further our goal of fostering and maintaining the highest standards of compliance, ethics, integrity and professionalism in every aspect of our business dealings.
The purpose of our corporate compliance program is to focus on compliance with applicable legal and regulatory requirements; the requirements of the Medicare and Medicaid programs and other government healthcare programs; industry standards; our Code of Conduct and Ethics; and our policies and procedures that support and enhance overall compliance within our company. The primary focus of our corporate compliance program is on regulations related to the federal False Claims Act, Stark Law, Anti-Kickback Law, billing and overall adherence to health care regulations.
To ensure the independence of our compliance department staff, the following measures have been implemented:
| • | our Chief Compliance Officer reports has direct oversight by the Audit Committee of our Board of Directors; |
| • | the compliance department has its own operating budget; and |
| • | the compliance department has the authority to independently investigate any compliance or ethical concerns, including, when deemed necessary, the authority to interview any company personnel, access any company property (including electronic communications) and engage counsel to assist in any investigation. |
Among other activities, our compliance department staff is responsible for the following activities:
| • | drafting and revising company policies and procedures related to compliance and ethics issues; |
| • | reviewing, making recommended revisions to, disseminating and tracking attestations to our Code of Conduct and Ethics; |
| • | measuring compliance with our policies and procedures, Code of Conduct and Ethics and legal and regulatory requirements related to the Medicare and Medicaid programs and other government healthcare programs, laws and regulations; |
| • | developing and providing compliance-related training and education to all of our employees and, as appropriate, directors, contractors and other representatives and agents, including, new-hire compliance training for all new employees, annual compliance training for all employees, sales compliance training to all members of our sales team, billing compliance training to all members of our billing and revenue cycle team and other job-specific and role-based compliance training of certain employees; |
13
Table of Contents
| • | performing an annual company-wide risk assessment; |
| • | implementing an annual compliance auditing and monitoring work plan and performing and following up on various risk-based auditing and monitoring activities, including both clinical and non-clinical auditing and monitoring activities at the corporate level and at the local agency/facility level; |
| • | developing, implementing and overseeing our Health Insurance Portability and Accountability Act of 1996 (“HIPAA”) privacy compliance program; |
| • | monitoring, responding to and overseeing the resolution of issues and concerns raised through our anonymous compliance hotline; |
| • | monitoring, responding to and resolving all compliance and ethics-related issues and concerns raised through any other form of communication; and |
| • | ensuring that we take appropriate corrective and disciplinary action when noncompliant or improper conduct is identified. |
Our Chief Compliance Officer is a member of and meets with and provides a weekly report on our compliance initiatives, investigations and other activities to our Senior Management team. We have also developed a corporate compliance committee that is chaired by our Chief Compliance Officer and also includes our Chief Executive Officer, Chief Operating Officer, Chief Financial Officer, General Counsel, Chief Corporate Development Officer, Chief Administrative Officer, Senior Counsel of Legislative and Regulatory Affairs, VP of Quality and Performance Improvement, VP of Corporate Education, Associate General Counsel, Director of Revenue Cycle, Director of Internal Audit and Director of Financial Reporting. Our corporate compliance committee meets on a quarterly basis or as called by the Chief Compliance Officer to establish the agenda for compliance initiatives and review the status of compliance initiatives, investigations and other activities, as well as the operations of our Compliance Department. Our Chief Compliance Officer also meets with and provides a quarterly report on our compliance initiatives, investigations and other activities to the Audit Committee of our Board of Directors.
All employees are required to report incidents, issues or other concerns that they believe in good faith may be in violation of our Code of Conduct and Ethics, our policies and procedures, applicable legal and regulatory requirements or the requirements of the Medicare and Medicaid programs and other government healthcare programs. All employees are encouraged to either contact our Chief Compliance Officer directly or to contact our 24-hour toll-free compliance hotline when they have questions or concerns about any compliance or ethics issues. All reports to our compliance hotline are kept confidential to the extent allowed by law, and employees have the option to remain anonymous. In cases reported to our compliance hotline that involve a compliance or ethics issue or any possible violation of law or regulation, the matter is referred to the compliance department for investigation. Retaliation against employees in connection with reporting compliance or ethical concerns is considered a serious violation of our Code of Conduct and Ethics, and, if it occurs, it will result in discipline, up to and including termination of employment.
We continually expand and refine our compliance and ethics programs. We promote a culture of compliance, ethics, integrity and professionalism within our company through persistent messages from our senior leadership concerning the necessity of strict compliance with legal requirements and company policies and procedures. We believe our consistent focus on our compliance and ethics programs provide us with a competitive advantage in the markets we serve.
Technology and Intellectual Property
Our Service Value Point system is a proprietary information system that assists us in, among other things, monitoring use and other cost factors, supporting our health care management techniques, internal benchmarking, clinical analysis, outcomes monitoring and claims generation, revenue cycle management and revenue reporting. We were notified by the U.S. Patent and Trademark Office that the patent for our Service Value Points system was finalized during 2009. This proprietary home nursing clinical resource and cost management system is a quantitative tool that assigns a target level of resource units to each patient based upon his or her initial assessment and estimated skilled nursing and therapy needs. We designed this system to empower our direct care employees to make appropriate day-to-day clinical care decisions while also allowing us to manage the quality and delivery of care across our system and to monitor the cost of providing that care both on a patient-specific and agency-specific basis.
In addition to our Service Value Point system, our business is substantially dependent on non-proprietary software. We utilize a third-party software information system for billing and maintaining patient claim receivables
14
Table of Contents
for our LTACHs. Our various home nursing agency databases primarily utilize one billing and patient claim system. We have kept certain acquisitions on their legacy system where we determined it was more advantageous to do so and where we obtained expertise on the legacy system in the acquisition. Three such legacy systems are also utilized in our operations. By using these systems and the expertise obtained we maintain accuracy, reliability and efficiency of processing and management reporting.
Technology plays a key role in our organization’s ability to expand operations and maintain effective managerial control. The software we use is based on client-server technology and is highly scalable. We believe our software and systems are flexible, easy-to-use and allow us to accommodate growth without difficulty. We believe that building and enhancing our information and software systems provides us with a competitive advantage that allows us to grow our business in a more cost-efficient manner and results in better patient care.
We continue to implement, evaluate and refine our point of care (“POC”) roll out strategy and will be conducting beta tests on POC throughout 2010. We currently have 28 locations on POC. Compared to 5 years ago when 30%-40% of home health agencies and 5% of hospices utilized POC, today 65% of home health agencies and 30% of hospices utilize POC. POC tools now have predictive and disease management capabilities built in. Today, 55% of all Americans have broadband access at home, which is up from 47% in 2007, according to a July Pew Internet & American Life Project report. The study also found that 38% of rural Americans now have broadband at home, an increase of 23% from 2007. $7.2 billion of the $787 billion federal stimulus package is set aside to expand the reach of broadband to rural areas. This supports the increasing ability for real time transfer of information from the field to the office and presents a more compelling quality and efficiency return on investment.
Reimbursement
Medicare
The federal government’s Medicare program, governed by the Social Security Act of 1965, reimburses health care providers for services furnished to Medicare beneficiaries. These beneficiaries generally include persons age 65 and older and those who are chronically disabled. The program is primarily administered by the Department of Health and Human Services (“HHS”) and the Centers for Medicare & Medicaid Services (“CMS”). Medicare payments accounted for 81.7%, 83.2% and 81.7% of our net service revenue for the years ended December 31, 2009, 2008 and 2007, respectively. Medicare reimburses us based upon the setting in which we provide our services or the Medicare category in which those services fall.
Home Nursing. The Medicare home nursing benefit is available to patients who need care following discharge from a hospital, as well as patients who suffer from chronic conditions that require ongoing but intermittent care. The services received need not be rehabilitative or of a finite duration; however, patients who require full-time skilled nursing for an extended period of time generally do not qualify for Medicare home nursing benefits. As a condition of coverage under Medicare, beneficiaries must: (1) be homebound in that they are unable to leave their home without considerable effort; (2) require intermittent skilled nursing, physical therapy, or speech therapy services that are covered by Medicare; and (3) receive treatment under a plan of care that is established and periodically reviewed by a physician. Qualifying patients also may receive reimbursement for occupational therapy, medical social services and home health aide services if these additional services are part of a plan of care prescribed by a physician.
We receive a standard prospective Medicare payment for delivering care over a base 60-day period, referred to as an episode of care. There is no limit to the number of episodes a beneficiary may receive as long as he or she remains eligible. Most patients complete treatment within one payment episode. The base episode payment, established through federal legislation, is a flat rate that is adjusted upward or downward based upon differences in the expected resource needs of individual patients as indicated by clinical severity, functional severity and service utilization. The magnitude of the adjustment is determined by each patient’s categorization into one of 153 payment groups, known as home health resource groups and the costliness of care for patients in each group relative to the average patient. Our payment is further adjusted for differences in local prices using the hospital wage index. We bill and are reimbursed for services in two stages: an initial request for advance payment when the episode commences and a final claim when it is completed. We submit all Medicare claims through the Medicare Administrative Contractors for the federal government. We receive 60% of the estimated payment for a patient’s initial episode up-front (after the initial assessment is completed and upon initial billing) and the remaining 40% upon completion of the episode and after all final treatment orders are signed by the physician. In the event of subsequent episodes, reimbursement timing is 50% up-front and 50% upon completion of the episode.
15
Table of Contents
Final payments may reflect one of four retroactive adjustments to ensure the adequacy and effectiveness of the total reimbursement: (1) an outlier payment if the patient’s care was unusually costly; (2) a low utilization adjustment if the number of visits was fewer than five; (3) a partial payment if the patient transferred to another provider before completing the episode; or (4) a payment adjustment based upon the level of therapy services required in the population base. Because such adjustments are determined upon the completion date of the episode, retroactive adjustments could impact our financial results up to 60 days in advance of the effective date and recognition of the change.
We verify a patient’s eligibility for home health benefits at the time of admission. Through the verification process we are able to determine the payor source and eligibility for reimbursement of each patient. Accordingly, we do not have any material reimbursement amounts that are pending approval based on the eligibility of a patient to receive reimbursement from the applicable payor program. Further, we provide only limited services to patients who are ineligible for reimbursement from a third party payor. Therefore, we do not have any material reimbursement from patients who are self-pay.
The base payment rate for Medicare home nursing in 2009 was $2,272 per 60-day episode. Since the inception of the prospective payment system in October 2000, the base episode payment rate has varied due to both the impact of annual market-basket based increases and Medicare-related legislation. Home health payment rates are updated annually by either the full home health market basket percentage, or by the home health market basket percentage as adjusted by Congress. CMS establishes the home health market basket index, which measures inflation in the prices of an appropriate mix of goods and services included in home health services.
The Office of Inspector General (“OIG”) of HHS has a responsibility to report both to the Secretary of HHS and to Congress any program or management problems related to programs such as Medicare. The OIG’s duties are carried out through a nationwide network of audits, investigations and inspections. The OIG has recently undertaken a study with respect to Medicare reimbursement for home health services. No estimate can be made at this time regarding the impact, if any, of the OIG’s findings.
Hospice. In order for a Medicare beneficiary to qualify for the Medicare hospice benefit, two physicians must certify that, in the best judgment of the physician or medical director, the beneficiary has less than six months to live, assuming the beneficiary’s disease runs its normal course. In addition, the Medicare beneficiary must affirmatively elect hospice care and waive any rights to other Medicare benefits related to his or her terminal illness. For each benefit period, a physician must recertify that the Medicare beneficiary’s life expectancy is six months or less in order for the beneficiary to continue to qualify for and to receive the Medicare hospice benefit. The first two benefit periods are measured at 90-day intervals and subsequent benefit periods are measured at 60-day intervals. A Medicare beneficiary may revoke his or her election at any time and resume receiving traditional Medicare benefits. There is no limit on how long a Medicare beneficiary can receive hospice benefits and services, provided that the beneficiary continues to meet Medicare hospice eligibility criteria.
Medicare reimburses for hospice care using a prospective payment system. Under that system, we receive one of four predetermined daily or hourly rates based upon the level of care we furnish to the beneficiary. These rates are subject to annual adjustments based on inflation and geographic wage considerations. Our base Medicare rates depend upon which of the following four levels of care we provide:
| • | Routine Care. This level of care includes care that is not classified under any of the other levels of care, such as the work of social workers or home health aides. |
| • | General Inpatient Care. This level of care is available for pain control or acute or chronic symptom management that cannot be managed in a setting other than an inpatient Medicare certified facility, such as a hospital, skilled nursing facility or hospice inpatient facility. |
| • | Continuous Home Care. This level of care is provided when a patient is experiencing a medical crisis and requires nursing services to achieve palliation and symptom control. For services to qualify for this level of care, the agency must provide a minimum of eight hours of care within a 24-hour period. |
| • | Respite Care. This level of care is provided on a short-term, inpatient basis to give temporary relief to the person who regularly provides care to the patient. |
Medicare limits the reimbursement we may receive for inpatient care services of hospice patients. Under the “80-20 rule,” if the number of inpatient care days furnished by us to Medicare beneficiaries exceeds 20% of the total days of hospice care furnished by us to Medicare beneficiaries, Medicare payments to us for inpatient care days exceeding the inpatient cap will be reduced to the routine home care rate. This determination is made annually based
16
Table of Contents
on the 12-month period beginning on November 1st each year. This limit is computed on a program-by-program basis. Our hospices have not exceeded the cap on inpatient care services during 2008 or 2007. We have not received notification that any of our hospices have exceeded the cap on inpatient care services during 2009.
Our Medicare hospice reimbursement is also subject to a cap amount calculated by the Medicare fiscal intermediary at the end of the hospice cap period, which runs from November 1st through October 31st of the following year. We have not received notification that any of our hospices have exceeded the cap on per beneficiary limits during 2009.
The two caps include an inpatient cap and overall payment cap, detailed below:
| • | Inpatient Cap. This cap limits the number of days of inpatient care (both respite and general) under a provider number to 20% of the total number of days of hospice care (both inpatient and in-home) furnished to all patients served. The daily payment rate for any inpatient days of service in excess of the cap amount is calculated at the routine home care rate, with excess amounts due back to Medicare; and |
| • | Overall Payment Cap. This cap is calculated by the Medicare fiscal intermediary at the end of each hospice cap period to determine the maximum allowable payments per provider number. On a monthly and quarterly basis, we estimate our potential cap exposure using information available for both inpatient day limits as well as per beneficiary cap amounts. The total cap amount for each provider is calculated by multiplying the number of beneficiaries electing hospice care from September 28, 2008 to September 27, 2009 by a statutory amount that is indexed for inflation. The per beneficiary cap amount was $23,014 for the twelve-month period ended October 31, 2009 and $22,386 for the twelve month period ended October 31, 2008. There will be a cap liability if actual payments per the Provider Statistical and Reimbursement report for the period of November 1, 2008 to October 31, 2009 exceed the beneficiary cap amount. |
Long-term Acute Care Hospitals. All Medicare payments to our LTACHs are made in accordance with a prospective payment system specifically applicable to long term acute care hospitals, referred to as “LTACH-PPS.” Proposed rules specifically related to LTACHs are generally published in January, finalized in May and effective on July 1st of each year. Additionally, LTACHs are subject to annual updates to the rules related to the inpatient prospective payment system, or “IPPS,” that are typically proposed in May, finalized in August and effective on October 1st of each year. In the annual payment rate update for the 2009 fiscal year, CMS consolidated the two historical annual updates into one annual update. The final rule adopted a 15-month rate update for fiscal year 2009 and moves the LTACH-PPS from a July-June update cycle to an October-September cycle. Beginning fiscal year 2010 the LTACH rate year will begin October 1, coinciding with the start of the federal fiscal year.
August 2004 Final Rule. On August 11, 2004, CMS published final regulations applicable to LTACHs that are operated as “hospital within hospitals” or as “satellites.” We collectively refer to hospital within hospitals and satellites as “HwHs,” and we refer to the CMS final regulations as the “final regulations.” HwHs are separate hospitals located in space leased from, and located in or on the same campus of, another hospital. We refer to such other hospitals as “host” hospitals. Effective for hospital cost reporting periods beginning on or after October 1, 2004, subject to certain exceptions, the final regulations provide lower rates of reimbursement to HwHs for those Medicare patients admitted from their host hospitals that are in excess of a specified percentage threshold. For HwHs opened after October 1, 2004, the Medicare admissions threshold has been established at 25% except for HwHs located in rural areas or co-located with “MSA dominant” hospitals or single urban hospitals where the percentage is no more than 50%, nor less than 25%. For HwHs that met specified criteria and were in existence as of October 1, 2004, the Medicare admissions thresholds were to have been phased in over a four year period starting with hospital cost reporting periods that began on or after October 1, 2004. However, as described below, many of these changes have been postponed for a three year period by the Medicare, Medicaid, and SCHIP Extension Act of 2007, or “SCHIP Extension Act,” and further clarified in the American Recovery and Reinvestment Act of 2009, or “ARRA.”
May 2007 Final Rule. On May 11, 2007, CMS published its annual payment rate update for the 2008 LTACH-PPS rate year, or “RY 2008” (affecting discharges and cost reporting periods beginning on or after July 1, 2007 and before July 1, 2008). The May 2007 final rule made several changes to LTACH-PPS payment methodologies and amounts during RY 2008 although, as described below, many of these changes have been postponed for a three year period by the SCHIP Extension Act.
17
Table of Contents
For cost reporting periods beginning on or after July 1, 2007, the May 2007 final rule expanded the Medicare HWH admissions threshold to apply to Medicare patients admitted from any individual hospital. Previously, the admissions threshold was applicable only to Medicare HWH admissions from hospitals co-located with an LTACH or satellite of an LTACH. Under the May 2007 final rule, free-standing LTACHs and grandfathered HwHs would be subject to the Medicare admission thresholds, as well as HwHs and satellites that admit Medicare patients from non-co-located hospitals. To the extent that any LTACH’s or LTACH satellite facility’s discharges that are admitted from an individual hospital (regardless of whether the referring hospital is co-located with the LTACH or LTACH satellite) exceed the applicable percentage threshold during a particular cost reporting period, the payment rate for those discharges would be subject to a downward payment adjustment. Cases admitted in excess of the applicable threshold would be reimbursed at a rate comparable to that under general acute care IPPS, which is generally lower than LTACH-PPS rates. Cases that reach outlier status in the discharging hospital would not count toward the limit and would be paid under LTACH-PPS. CMS estimated the impact of the expansion of the Medicare admission thresholds would result in a reduction of 2.2% of the aggregate payments to all LTACHs in RY 2008.
The applicable percentage threshold is generally 25% after the completion of the phase-in period described below. The percentage threshold for LTACH discharges from a referring hospital that is an MSA dominant hospital or a single urban hospital is the percentage of total Medicare discharges in the MSA that are from the referring hospital, but no less than 25% nor more than 50%. For Medicare discharges from LTACHs or LTACH satellites located in rural areas, as defined by the Office of Management and Budget, the percentage threshold is 50% from any individual referring hospital. The expanded 25% rule is being phased in over a three year period. The three year transition period starts with cost reporting periods beginning on or after July 1, 2007 and before July 1, 2008, when the threshold is the lesser of 75% or the percentage of the LTACH’s or LTACH satellite’s admissions discharged from the referring hospital during its cost reporting period beginning on or after July 1, 2004 and before July 1, 2005, or “RY 2005.” For cost reporting periods beginning on or after July 1, 2008 and before July 1, 2009, the threshold is the lesser of 50% or the percentage of the LTACH’s or LTACH satellite’s admissions from the referring hospital, during its RY 2005 cost reporting period. For cost reporting periods beginning on or after July 1, 2009, all LTACHs will be subject to the 25% threshold (or applicable threshold for rural, urban-single, or MSA dominant hospitals). The SCHIP Extension Act, as amended by the ARRA, postponed the application of the percentage threshold to all free-standing and grandfathered HwHs for a three year period commencing on an LTACH’s first cost reporting period on or after July 1, 2007. However, the SCHIP Extension Act did not postpone the application of the percentage threshold, or the transition period stated above, to those Medicare patients discharged from an LTACH HWH or HWH satellite that were admitted from a non-co-located hospital. The SCHIP Extension Act only postpones the expansion of the admission threshold in the May 2007 final rule to free-standing LTACHs and grandfathered HwHs.
The May 2007 final rule further revised the payment adjustment formula for short stay outlier, or “SSO” cases. Beginning with discharges on or after July 1, 2007, for cases with a length of stay that is less than the average length of stay plus one standard deviation for the same DRG under IPPS, referred to as the so-called “IPPS comparable threshold,” the rule effectively lowers the LTACH payment to a rate based on the general acute care hospital IPPS. SSO cases with covered lengths of stay that exceed the IPPS comparable threshold would continue to be paid under the SSO payment policy described above under the May 2006 final rule. Cases with a covered length of stay less than or equal to the IPPS comparable threshold and less than five-sixths of the geometric average length of stay for that LTC-DRG would be paid at an amount comparable to the IPPS per diem. The SCHIP Extension Act also postponed, for the three year period beginning on December 29, 2007, the SSO policy changes made in the May 2007 final rule.
The May 2007 final rule increased the standard federal rate by 0.71% for RY 2008. As a result, the federal rate for RY 2008 is equal to $38,356.45, compared to $38,086.04 for RY 2007. Subsequently, the SCHIP Extension Act eliminated the update to the standard federal rate that occurred for RY 2008 effective April 1, 2008. This adjustment to the standard federal rate was applied prospectively on April 1, 2008 and reduced the federal rate back to $38,086.04. In a technical correction to the May 2007 final rule, CMS increased the fixed-loss amount for high cost outlier in RY 2008 to $20,738, compared to $14,887 in RY 2007. CMS projected an estimated 0.4% decrease in LTACH payments in RY 2008 due to this change in the fixed-loss amount and the overall impact of the May 2007 final rule to be a 1.2% decrease in total estimated LTACH-PPS payments for RY 2008.
The May 2007 final rule provided that beginning with the annual payment rate updates to the LTC-DRG classifications and relative weights for the fiscal year 2008, or “FY 2008” (affecting discharges beginning on or after October 1, 2007 and before September 30, 2008), annual updates to the LTC-DRG classification and relative weights are to have a budget neutral impact. Under the May 2007 final rule, future LTC-DRG reclassification and recalibrations, by themselves, should neither increase nor decrease the estimated aggregated LTACH-PPS payments.
18
Table of Contents
The May 2007 final rule is complex and the SCHIP Extension Act postponed the implementation of certain portions of the May 2007 final rule. While we cannot predict the ultimate long-term impact of LTACH-PPS because the payment system remains subject to significant change, if the May 2007 final rule becomes effective as currently written, after the expiration of the applicable provisions of the SCHIP Extension Act, our future net operating revenues and profitability could be adversely affected.
August 2007 Final Rule. On August 22, 2007, CMS published the IPPS final rule for FY 2008, which created a new patient classification system with categories referred to as MS-DRGs and MS-LTC-DRGs, respectively, for hospitals reimbursed under IPPS and LTACH-PPS. Beginning with discharges on or after October 1, 2007, the new classification categories take into account the severity of the patient’s condition. CMS assigned proposed relative weights to each MS-DRG and MS-LTC-DRG to reflect their relative use of medical care resources.
The August 2007 final rule published a budget neutral update to the MS-LTC-DRG classification and relative weights. In the preamble to the IPPS final rule for FY 2008 CMS restated that it intends to continue to update the LTC-DRG weights annually in the IPPS rulemaking and those weights would be modified by a budget neutrality adjustment factor to ensure that estimated aggregate LTACH payments after reweighting are equal to estimated aggregate LTACH payments before reweighting.
Medicare, Medicaid, and SCHIP Extension Act of 2007. On December 29, 2007, President Bush signed into law the SCHIP Extension Act. Among other changes in the federal health care programs, the SCHIP Extension Act makes significant changes to Medicare policy for LTACHs including a new statutory definition of an LTACH, a report to Congress on new LTACH patient criteria, relief from certain LTACH-PPS payment policies for three years, a three year moratorium on the establishment and classification of new LTACHs and LTACH beds, elimination of the payment update for the last quarter of RY 2008 and new medical necessity reviews by Medicare contractors through at least October 1, 2010.
The SCHIP Extension Act precludes the Secretary from implementing, during the three year moratorium period, the provisions added by the May 2007 final rule that extended the 25% rule to free-standing LTACHs and grandfathered HwHs. The SCHIP Extension Act also modifies, during the moratorium, the effect of the 25% rule for non-grandfathered LTACH HwHs, non-grandfathered satellites and grandfathered LTACH HwHs, as it applies to admissions from co-located hospitals. For HwHs and satellite facilities, the applicable percentage threshold is set at 50% and not phased in to the 25% level. For those HwHs and satellite facilities located in rural areas and those which receive referrals from MSA dominant hospitals or single urban hospitals, the percentage threshold is set at no more than 75%. The ARRA, as discussed below further revises the SCHIP Extension Act to postpone the percentage limitations established in the SCHIP Extension Act to the three cost reporting periods beginning on or after July 1, 2007 for freestanding LTACHs, grandfathered HwHs and grandfathered satellites and on or after October 1, 2007 for non-grandfathered LTACH HwHs and non-grandfathered satellites.
The SCHIP Extension Act also precludes the Secretary from implementing, for the three year period beginning on December 29, 2007, a one-time adjustment to the LTACH standard federal rate. This rule, established in the original LTACH-PPS regulations, permits CMS to restate the standard federal rate to reflect the effect of changes in coding since the LTACH-PPS base year. In the preamble to the May 2007 final rule, CMS discussed making a one-time prospective adjustment to the LTACH-PPS rates for the 2009 rate year. In addition, the SCHIP Extension Act reduced the Medicare payment update for the portion of RY 2008 from April 1, 2008 to June 30, 2008 to the same base rate applied to LTACH discharges during RY 2007.
For the three calendar years following December 29, 2007, the Secretary must impose a moratorium on the establishment and classification of new LTACHs, LTACH satellite facilities, and LTACH beds in existing LTACH or satellite facilities. This moratorium does not apply to LTACHs that, before the date of enactment, (1) began the qualifying period for payment under the LTACH-PPS, (2) have a written agreement with an unrelated party for the construction, renovation, lease or demolition for a LTACH and have expended at least 10% of the estimated cost of the project or $2,500,000, or (3) have obtained an approved certificate of need.
May 6, 2008 Interim Final Rule. On May 6, 2008, CMS published an interim final rule with comment period, which implemented portions of the SCHIP Extension Act. The May 6, 2008 interim final rule addressed: (1) the payment adjustment for very short-stay outliers, (2) the standard federal rate for the last three months of RY 2008, (3) adjustment of the high cost outlier fixed-loss amount for the last three months of RY 2008, and (4) made references to the SCHIP Extension Act in the discussion of the basis and scope of the LTACH-PPS rules.
19
Table of Contents
May 9, 2008 Final Rule. On May 9, 2008, CMS published its annual payment rate update for the 2009 LTACH-PPS rate year, or “RY 2009” (affecting discharges and cost reporting periods beginning on or after July 1, 2008). The final rule adopts a 15-month rate update, from July 1, 2008 through September 30, 2009 and moves LTACH-PPS from a July-June update cycle to the same update cycle as the general acute care hospital inpatient rule (October — September). For RY 2009, the rule establishes a 2.7% update to the standard federal rate. The rule increases the fixed-loss amount for high cost outlier cases to $22,960, which is $2,222 higher than the 2008 LTACH-PPS rate year. The final rule provides that CMS may make a one-time reduction in the LTACH-PPS rates to reflect a budget neutrality adjustment no earlier than December 29, 2010 and no later than October 1, 2012. CMS estimated this reduction will be approximately 3.75%.
May 22, 2008 Interim Final Rule. On May 22, 2008, CMS published an interim final rule with comment period, which implements portions of the SCHIP Extension Act not addressed in the May 6, 2008 interim final rule. Among other things, the May 22, 2008 interim final rule establishes a definition for “free-standing” LTACHs as a hospital that: (1) has a Medicare provider agreement, (2) has an average length of stay of greater than 25 days, (3) does not occupy space in a building used by another hospital, (4) does not occupy space in one or more separate or entire buildings located on the same campus as buildings used by another hospital and (5) is not part of a hospital that provides inpatient services in a building also used by another hospital.
August 2008 Final Rule. On August 19, 2008, CMS published the IPPS final rule for FY 2009 (affecting discharges and cost reports beginning on or after October 1, 2008 and before October 1, 2009), which made limited revisions to the classifications of cases in MS-LTC-DRGs. The final rule also includes a number of hospital ownership and physician referral provisions, including expansion of a hospital’s disclosure obligations by requiring physician-owned hospitals to disclose ownership or investment interests held by immediate family members of a referring physician. The final rule requires physician-owned hospitals to furnish to patients, on request, a list of physicians or immediate family members who own or invest in the hospital. Moreover, a physician-owned hospital must require all physician owners or investors who are also active members of the hospital’s medical staff to disclose in writing their ownership or investment interests in the hospital to all patients they refer to the hospital. CMS can terminate the Medicare provider agreement of a physician-owned hospital if it fails to comply with these disclosure provisions or with the requirement that a hospital disclose in writing to all patients whether there is a physician on-site at the hospital 24 hours per day, 7 days per week.
The American Recovery and Reinvestment Act of 2009. On February 17, 2009, President Obama signed into law the American Recovery and Reinvestment Act of 2009, the “ARRA.” The ARRA makes several technical corrections to the SCHIP Extension Act, including a clarification that, during the moratorium period established by the SCHIP Extension Act, the percentage threshold for grandfathered satellites is set at 50% and not phased in to the 25% level for admissions from a co-located hospital. In addition, the ARRA clarifies that the application of the percentage threshold is postponed for a LTACH HWH or satellite that was co-located with a provider-based, off-campus location of an IPPS hospital that did not deliver services payable under IPPS. The ARRA also provides that the postponement of the percentage threshold established in the SCHIP Extension Act will be effective for cost reporting periods beginning on or after July 1, 2007 for freestanding LTACHs and grandfathered HwHs and satellites and on or after October 1, 2007 for other LTACH HwHs and satellites.
June 3, 2009 Interim Final Rule. On June 3, 2009, CMS published an interim final rule in which CMS adopted a new table of MS-LTC-DRG relative weights that will apply to the remainder of fiscal year 2009 (through September 30, 2009). This interim final rule revises the MS-LTC-DRG relative weights for payment under the LTACH-PPS for FY 2009 due to CMS’s misapplication of its established methodology in the calculation of the budget neutrality factor. This error resulted in relative weights that are higher, by approximately 3.9 percent for all of FY 2009 (October 1, 2008 through September 30, 2009) which has the effect of reducing reimbursement by approximately 3.9%. However, CMS is only applying the corrected weights to the remainder of fiscal year 2009 (that is, from June 3, 2009 through September 30, 2009).
July 31, 2009 Final Rule. On July 31, 2009, CMS released its annual payment rate update for the LTACH PPS for “FY 2010” (affecting discharges and cost reporting periods beginning on or after October 1, 2009 and before September 30, 2010). For FY 2010 CMS adopted a 2.5% increase in payments under the LTACH PPS. As a result, the standard federal rate for FY 2010 is set at $39,896.65, an increase from $39,114.36 in FY 2009. The increase in the standard federal rate uses a 2.0% update factor based on the market basket update of 2.5% less an adjustment of 0.5% to account for changes in documentation and coding practices. The fixed loss amount for high cost outlier cases is set at $18,425. This is a decrease from the fixed loss amount in the 2009 rate year of $22,960.
20
Table of Contents
The July 31, 2009 annual payment rate update also included an interim final rule with comment period implementing provisions of the ARRA discussed above, including amendments to provisions of the SCHIP Extension Act relating to payments to LTACHs and LTACH satellite facilities and increases in beds in existing LTACHs and LTACH satellite facilities under the LTACH PPS.
In the same federal register, CMS finalized three interim final rules with comment period that it previously published but had yet to respond to public comment. First, CMS finalized the June 3, 2009 interim final rule that adopted a new table of MS-LTC-DRG relative weights for the period between June 3, 2009 and September 30, 2009. Second, CMS finalized the May 6, 2008 interim final rule that implemented changes to LTACH PPS mandated by the SCHIP Extension Act addressing: (1) payment adjustments for certain short-stay outliers, (2) the federal standard rate for the last three months of rate year 2008, and (3) adjustment of the high cost outlier fixed-loss amount. Finally, CMS finalized the May 22, 2008 interim final rule that implemented changes to LTACH PPS mandated by the SCHIP Extension Act modifying the percentage threshold policy for certain LTACHs and addressing the three-year moratorium on the establishment of new LTACHs and bed increases at existing LTACHs and LTACH satellites.
We currently have a total of eight LTACHs. Seven of our hospitals are classified as HwHs and one as freestanding remote site. Of the seven HwH facilities, four are located in rural or non-MSAs. Three of our seven HwH facilities are located in MSA or urban areas. Of these seven locations classified as HwHs, one facility is a satellite location of a parent hospital located in an MSA and one facility is a satellite location of a parent hospital located in a non-MSA. We also have one location that is a freestanding remote site of a parent located in an MSA. Based on our discussions with CMS, we believe each of our satellite and remote locations will be viewed as being located in a non-MSA regardless of the location of its parent hospital and will be treated independently from its parent for purposes of calculating its compliance with the admissions limitations. If the “25% rule” is extended, as planned, to freestanding LTACHs after the three-year delay (established in the MMSEA), our current freestanding facility would not likely be affected because we currently do not receive more than 25% of our Medicare admissions from any single referring hospital.
For the 12 months ended December 31, 2009, on an individual basis, the admission of six of our LTACHs were under the proper threshold as of the current cost report year date of August 31, 2009. Our new LTACH acquired in 2009 is a grandfathered LTACH and, therefore, has no limitations under MMSEA with respect to the number of patients that can be admitted from the host hospital. Our remaining LTACH is not an HwH; therefore, it is not subject to these limits on host hospital referrals, but maintains compliance with non-co-located hospital referral thresholds.
Medicaid
Medicaid is a joint federal and state funded health insurance program for certain low-income individuals. Medicaid reimburses health care providers using a number of different systems, including cost-based, prospective payment and negotiated rate systems. Rates are also subject to adjustment based on statutory and regulatory changes, administrative rulings, government funding limitations and interpretations of policy by individual state agencies.
Non-Governmental Payors
A portion of our net service revenue comes from private payor sources. These sources include insurance companies, workers’ compensation programs, health maintenance organizations, preferred provider organizations, other managed care companies and employers, as well as patients directly. Patients are generally not responsible for any difference between customary charges for our services and amounts paid by Medicare and Medicaid programs and the non-governmental payors, but are responsible for services not covered by these programs or plans, as well as for deductibles and co-insurance obligations of their coverage. The amount of these deductibles and co-insurance obligations on patients has increased in recent years. Collection of amounts due from individuals is typically more difficult than collection of amounts due from government or business payors. However, the majority of our billed services are paid in full by Medicare, Medicaid or private insurance. Accordingly, co-payments from patients do not represent a material portion of our billed revenue and corresponding accounts receivable. To further reduce their
21
Table of Contents
health care costs, most insurance companies, health maintenance organizations, preferred provider organizations and other managed care companies have negotiated discounted fee structures or fixed amounts for services performed, rather than paying health care providers the amounts billed.
In response to the challenges associated with collecting from commercial payors and the unprofitable reimbursement rates paid by many commercial payors, we terminated or sent notice of termination to 285 commercial payors for home health services in the fourth quarter of 2007. These 285 commercial payors had reimbursement rates averaging 26% below cost, representing approximately 8% of our home health revenue, 16% of our home health admissions and 44% of our bad debt write-offs against home health revenue in 2007. In 2009, approximately 13.3% of our home health revenue was derived from commercial payors. During 2008 and 2009, we successfully negotiated higher reimbursement rates with a majority of our commercial payors. We currently have three national contracts and five regional contracts. However, if we are unable to continue negotiating higher reimbursement rates with commercial payors or if commercial payors continue to reduce health care costs through reduction in home health reimbursement, it could have a material adverse impact on our financial results.
Government Regulations
General
The health care industry is highly regulated and we are required to comply with federal, state and local laws, which significantly affect our business. These laws and regulations are extremely complex and, in many instances, the industry does not have the benefit of significant regulatory or judicial interpretation. Regulations and policies frequently change, and we monitor these changes through trade and governmental publications and associations. The significant areas of federal and state regulatory laws that could affect our ability to conduct our business include the following:
| • | Medicare and Medicaid participation and reimbursement; |
| • | the federal Anti-Kickback Statute and similar state laws; |
| • | the federal Stark Law and similar state laws; |
| • | false and other improper claims; |
| • | the Health Insurance Portability and Accountability Act of 1996 (“HIPAA”); |
| • | civil monetary penalties; |
| • | environmental health and safety laws; |
| • | licensing; and |
| • | certificates of need and permits of approval. |
If we fail to comply with these applicable laws and regulations, we could suffer civil or criminal penalties, including the loss of our licenses to operate and our ability to participate in federal and state health care programs, which would materially adversely affect our financial condition and results of operations. Although we believe we are in material compliance with all applicable laws, these laws are complex and a review of our practices by a court or law enforcement or regulatory authority could result in an adverse determination that could harm our business. Furthermore, the laws applicable to us are subject to change, interpretation and amendment, which could adversely affect our ability to conduct our business.
Office of Inspector General
The OIG has a responsibility to report any program or management problems related to programs such as Medicare to the Secretary of HHS and Congress. The OIG’s duties are carried out through a nationwide network of audits, investigations and inspections. Each year, the OIG outlines areas it intends to study relating to a wide range of providers. In fiscal year 2009, the OIG indicated its intent to study topics relating to, among others, home health, hospice and long-term care hospitals. No estimate can be made at this time regarding the impact, if any, of the OIG’s findings.
22
Table of Contents
Medicare Participation
During the years ended December 31, 2009, 2008 and 2007, we received 81.7%, 83.2% and 81.7%, respectively, of our net service revenue from Medicare. We expect to continue to receive the majority of our net service revenue from serving Medicare beneficiaries. Medicare is a federally funded and administered health insurance program, primarily for individuals entitled to social security benefits who are 65 or older or who are disabled. To participate in the Medicare program and receive Medicare payments, our agencies and facilities must comply with regulations promulgated by CMS. Among other things, these requirements, known as “conditions of participation,” relate to the type of facility, its personnel and its standards of medical care. Although we intend to continue to participate in the Medicare reimbursement programs, we cannot guarantee that our agencies and programs will continue to qualify for participation.
Under Medicare rules, the designation “provider-based” refers to circumstances in which a subordinate facility (e.g., a separately-certified Medicare provider, a department of a provider or a satellite facility) is treated as part of another provider, called the “main” provider, for Medicare payment purposes. In these cases, the services of the subordinate facility are included in the “main” provider’s cost report and overhead costs of the main provider can be allocated to the subordinate facility, to the extent that such costs are shared. We operate three LTACHs that are treated as provider-based satellites of certain of our other facilities. We also provide contract rehabilitation and management services to hospital rehabilitation departments that may be treated as provider-based. These facilities are required to satisfy certain operational standards in order to retain their provider-based status. Although we intend to continue to operate these facilities as provider-based, we cannot guarantee that they will continue to qualify as provider-based entities.
Anti-Kickback Statute
Provisions of the Social Security Act of 1965, commonly referred to as the Anti-Kickback Statute, prohibit the payment or receipt of anything of value in return for the referral of patients or arranging for the referral of patients, or in return for the recommendation, arrangement, purchase, lease or order of items or services that are covered by a federal health care program such as Medicare and Medicaid. Violation of the Anti-Kickback Statute is a felony and sanctions include imprisonment of up to five years, criminal fines of up to $25,000, civil monetary penalties of up to $50,000 per act plus three times the amount claimed or three times the remuneration offered and exclusion from federal health care programs (including the Medicare and Medicaid programs). Many states have adopted similar prohibitions against payments intended to induce referrals of Medicaid and other third-party payor patients.
The OIG has published numerous “safe harbors” that exempt some practices from enforcement action under the federal Anti-Kickback Statute. These safe harbors exempt specified activities, including bona-fide employment relationships, contracts for the rental of space or equipment, personal service arrangements and management contracts, so long as all of the requirements of the safe harbor are met. The OIG has recognized that the failure of an arrangement to satisfy all of the requirements of a particular safe harbor does not necessarily mean that the arrangement violates the Anti-Kickback Statute. Instead, each arrangement is analyzed on a case-by-case basis, which is very fact specific. We cannot guarantee that all our arrangements will satisfy a safe harbor or will ultimately be viewed as being compliant with the Anti-Kickback Statute.
We are required under the Medicare conditions of participation and some state licensing laws to contract with numerous health care providers and practitioners, including physicians, hospitals and nursing homes and to arrange for these individuals or entities to provide services to our patients. In addition, we have contracts with other suppliers, including pharmacies, ambulance services and medical equipment companies. We have also entered into various joint ventures with hospitals and physicians for the ownership and management of home nursing agencies and LTACHs. Some of these individuals or entities may refer, or be in a position to refer, patients to us and we may refer, or be in a position to refer, patients to these individuals or entities. We attempt to structure these arrangements in a manner that meets the requirements of a safe harbor. However, some of these arrangements may not meet all of the requirements of a safe harbor. We believe that our contracts and arrangements with providers, practitioners and suppliers do not violate the Anti-Kickback Statute or similar state laws. We cannot guarantee, however, that governmental agencies and bodies will interpret these laws in the same manner as we do.
23
Table of Contents
From time to time, various federal and state agencies, such as HHS and CMS, issue pronouncements, including fraud alerts, that identify practices that may be subject to heightened scrutiny. For example, the OIG’s FY 2009 Work Plan describes, among other things, the government’s intention to examine Medicare Part B payments for therapy services, accuracy of claims coding for Medicare home health resources groups, examining trends in utilization patterns and Medicare reimbursement for services ordered by referring physicians, the incidence of Medicare home health services outlier payments for insulin injections, and analysis of Home Health Agency claims under CMS’ Comprehensive Error Rate Testing Program to determine whether payments for services and items were adequately documented, medically necessary and coded correctly.
In June 1995, the OIG issued a special fraud alert that focused on the home nursing industry and identified some of the illegal practices the OIG has uncovered. In March 1998, the OIG issued a special fraud alert titled, Fraud and Abuse in Nursing Home Arrangements with Hospices. This special fraud alert focused on payments received by nursing homes from hospices. We believe, but cannot assure you, that our operations comply with the principles expressed by the OIG in these special fraud alerts.
We endeavor to conduct our operations in compliance with federal and state health care fraud and abuse laws, including the Anti-Kickback Statute and similar state laws. However, our practices may be challenged in the future and the fraud and abuse laws may be interpreted in a way that finds us in violation of these laws. If we are found to be in violation of the Anti-Kickback Statute, we could be subject to civil and criminal penalties and we could be excluded from participating in federal health care programs such as Medicare and Medicaid. The occurrence of any of these events could significantly harm our business and financial condition.
Stark Law
Congress has passed significant prohibitions against physician referrals of patients for certain health care services. These prohibitions are commonly known as the Stark Law. The Stark Law prohibits a physician from making referrals for particular health care services (called designated health services) to entities with which the physician, or an immediate family member of the physician, has a financial relationship.
The term “financial relationship” is defined very broadly to include most types of ownership or compensation relationships. The Stark Law also prohibits the entity receiving the referral from seeking payment under the Medicare and Medicaid programs for services rendered pursuant to a prohibited referral. If an entity is paid for services rendered pursuant to a prohibited referral, it may incur civil penalties and could be excluded from participating in the Medicare or Medicaid programs. If an arrangement is covered by the Stark Law, the requirements of a Stark Law exception must be met for the physician to be able to make referrals to the entity for designated health services and for the entity to be able to bill for these services.
“Designated health services” under the Stark Law is defined to include clinical laboratory services; physical therapy services; occupational therapy services; radiology services, including magnetic resonance imaging, computerized axial tomography scans and ultrasound services; radiation therapy services and supplies; durable medical equipment and supplies; parenteral and enteral nutrients, equipment and supplies; prosthetics, orthotics and prosthetic devices and supplies; home health services; outpatient prescription drugs; and inpatient and outpatient hospital services. The Stark Law defines a financial relationship to include: (1) a physician’s ownership or investment interest in an entity and (2) a compensation relationship between a physician and an entity. Under the Stark Law, financial relationships include both direct and indirect relationships.
Physicians refer patients to us for several Stark Law designated health services, including home health services, inpatient and outpatient hospital services and physical therapy services. We have compensation arrangements with some of these physicians or their professional practices in the form of medical director and consulting agreements. We also have operations owned by joint ventures in which physicians have an investment interest. In addition, other physicians who refer patients to our agencies and facilities may own our stock. As a result of these relationships, we could be deemed to have a financial relationship with physicians who refer patients to our facilities and agencies for designated health services. If so, the Stark Law would prohibit the physicians from making those referrals and would prohibit us from billing for the services unless a Stark Law exception applies.
The Stark Law contains exceptions for certain physician ownership or investment interests in and certain physician compensation arrangements with entities. If a compensation arrangement or investment relationship between a physician, or a physician’s immediate family member, and an entity satisfies all requirements for a Stark Law exception, the Stark Law will not prohibit the physician from referring patients to the entity for designated health services. The exceptions for compensation arrangements cover employment relationships, personal services
24
Table of Contents
contracts and space and equipment leases, among others. The exceptions for a physician investment relationship include ownership in an entire hospital and ownership in rural providers. We believe our compensation arrangements with referring physicians and our physician investment relationships meet the requirements for an exception under the Stark Law and that our operations comply with the Stark Law.
The Stark Law also includes an exception for a physician’s ownership or investment interest in certain entities through the ownership of stock. If a physician owns stock in an entity and the stock is listed on a national exchange or is quoted on NASDAQ and the ownership meets certain other requirements, the Stark Law will not apply to prohibit the physician from referring to the entity for designated health services. The requirements for this Stark Law exception include a requirement that the entity issuing the stock have at least $75.0 million in stockholders’ equity at the end of its most recent fiscal year or on average during the previous three fiscal years. As of December 31, 2009, 2008 and 2007, we have exceeded $75.0 million in stockholders’ equity.
If an entity violates the Stark Law, it could be subject to civil penalties of up to $15,000 per prohibited claim and up to $100,000 for knowingly entering into certain prohibited referral schemes. The entity also may be excluded from participating in federal health care programs (including Medicare and Medicaid). There are no criminal penalties for violations of Stark Law. If the Stark Law was found to apply to our relationships with referring physicians and those relationships did not meet the requirement of an exception under the Stark Law, we would be required to restructure these relationships or refuse to accept referrals for designated health services from these physicians. If we were found to have submitted claims to Medicare or Medicaid for services provided pursuant to a referral prohibited by the Stark Law, we would be required to repay any amounts we received from Medicare for those services and could be subject to civil monetary penalties. Further, we could be excluded from participating in Medicare and Medicaid. If we were required to repay any amounts to Medicare, subjected to fines, or excluded from the Medicare and Medicaid Programs, our business and financial condition would be harmed significantly.
Many states have physician relationship and referral statutes that are similar to the Stark Law. Some of these laws generally apply regardless of payor. We believe that our operations are structured to comply with applicable state laws with respect to physician relationships and referrals. However, any finding that we are not in compliance with these state laws could require us to change our operations or could subject us to penalties. This, in turn, could have a negative impact on our operations.
False and Improper Claims
The submission of claims to a federal or state health care program for items and services that are “not provided as claimed” may lead to the imposition of civil monetary penalties, criminal fines and imprisonment and/or exclusion from participation in state and federally funded health care programs, including the Medicare and Medicaid programs. These false claims statutes include the Federal False Claims Act. Under the Federal False Claims Act, actions against a provider can be initiated by the federal government or by a private party on behalf of the federal government. These private parties are often referred to as qui tam relators, and relators are entitled to share in any amounts recovered by the government. Both direct enforcement activity by the government and qui tam actions have increased significantly in recent years. This development has increased the risk that a health care company like us will have to defend a false claims action, pay fines or be excluded from the Medicare and Medicaid programs as a result of an investigation arising out of false claims laws. Many states have enacted similar laws providing for the imposition of civil and criminal penalties for the filing of fraudulent claims. Because of the complexity of the government regulations applicable to our industry, we cannot assure that we will not be the subject of an action under the Federal False Claims Act or similar state law.
Anti-fraud Provisions of the HIPAA
In an effort to combat health care fraud, Congress included several anti-fraud measures in HIPAA. Among other things, HIPAA broadened the scope of certain fraud and abuse laws, extended criminal penalties for Medicare and Medicaid fraud to other federal health care programs and expanded the authority of the OIG to exclude persons and entities from participating in the Medicare and Medicaid programs. HIPAA also extended the Medicare and Medicaid civil monetary penalty provisions to other federal health care programs, increased the amounts of civil monetary penalties and established a criminal health care fraud statute.
Federal health care offenses under HIPAA include health care fraud and making false statements relating to health care matters. Under HIPAA, among other things, any person or entity that knowingly and willfully defrauds or attempts to defraud a health care benefit program is subject to a fine, imprisonment or both. Also under HIPAA,
25
Table of Contents
any person or entity that knowingly and willfully falsifies or conceals or covers up a material fact or makes any materially false or fraudulent statements in connection with the delivery of or payment of health care services by a health care benefit plan is subject to a fine, imprisonment or both. HIPAA applies not only to governmental plans but also to private payors.
Administrative Simplification Provisions of HIPAA
HHS’s final regulations governing electronic transactions involving health information are part of the administrative simplification provisions of HIPAA, commonly referred to as the Transaction Standards rule. The rule establishes standards for eight of the most common health care transactions by reference to technical standards promulgated by recognized standards publishing organizations. Under the standards, any party transmitting or receiving health transactions electronically must send and receive data in a single format, rather than the large number of different data formats currently used. This rule applies to us in connection with submitting and processing health claims. The Transaction Standards rule also applies to many of our payors and to our relationships with those payors. Because many of our payors might not have been able to accept transactions in the format required by the Transaction Standards rule by the original compliance date, we filed a timely compliance extension plan with HHS. We believe that our operations materially comply with the Transaction Standards rule.
HHS also has final regulations implementing HIPAA that set forth standards for the privacy of individually-identifiable health information, referred to as protected health information. These regulations cover health care providers, health care clearinghouses and health plans. The privacy regulations require companies covered by the regulations to use and disclose protected health information only as allowed by the privacy regulations. Specifically, the privacy regulations require companies, including us, to do the following, among other things:
| • | obtain patient authorization prior to certain uses or disclosures of protected health information; |
| • | provide notice of privacy practices to patients and obtain an acknowledgement that the patient has received the notice; |
| • | respond to requests from patients for access to or to obtain a copy of their protected health information; |
| • | respond to patient requests for amendments of their protected health information; |
| • | provide an accounting to patients of certain disclosure of their protected health information; |
| • | enter into agreements with the companies’ business associates through which the business associates agree to use and disclose protected health information only as permitted by the agreement and the requirements of the privacy regulations; |
| • | train the companies’ workforce in privacy compliance; |
| • | designate a privacy officer; |
| • | use and disclose only the minimum necessary information to accomplish a particular purpose; and |
| • | establish policies and procedures with respect to uses and disclosures of protected health information. |
These regulatory requirements impose significant administrative and financial obligations on companies that use or disclose individually identifiable health information relating to the health of a patient. We have implemented policies and procedures to maintain patient privacy and comply with HIPAA’s privacy regulations. However, the privacy regulations are extensive, and we may need to change some of our practices to comply with them as they are interpreted.
In February 2003, HHS published the final security regulations implementing HIPAA that govern the security of health information. The compliance date for the security regulations was April 21, 2005. The security regulations require the implementation of policies and procedures that establish administrative, physical and technical safeguards for electronic protected health information. Companies covered by the security regulations are required to ensure the confidentiality, integrity and availability of electronic protected health information. Specifically, among others things, companies subject to the security regulations, including us, are required to:
| • | conduct a thorough assessment of the potential risks and vulnerabilities to confidentiality, integrity and availability of electronic protected health information and to reduce the risks and vulnerabilities to a reasonable and appropriate level as required by the security regulations; |
26
Table of Contents
| • | designate a security officer; |
| • | establish policies relating to access by the companies’ workforce to electronic protected health information; |
| • | enter into agreements with the companies’ business associates whereby business associates agree to establish administrative, physical and technical safeguards for electronic protected health information received from or on behalf of the companies; |
| • | create a disaster and contingency plan to ensure the availability of electronic protected health information; |
| • | train the companies’ workforce in security compliance; |
| • | establish physical controls for electronic devices and media containing or transmitting electronic protected health information; |
| • | establish policies and procedures regarding the use of workstations with access to electronic protected health information; and |
| • | establish technical controls for the information systems maintaining or transmitting electronic protected health information. |
In addition, in 2009, the American Reinvestment and Recovery Act of 2009 expanded some of our obligations under the existing HIPAA privacy and security provisions, including:
| • | requirements to notify individuals and governmental agencies when security breaches occur with respect to unsecured information; |
| • | limitations on our ability to use or disclose protected health information for marketing or soliciting charitable contributions; |
| • | expansion of certain privacy and security requirements to our vendors and business associates; and |
| • | requirements for providing an accounting of disclosures of electronic health records. |
These regulatory requirements impose significant administrative and financial obligations on companies like us that use or disclose electronic health information. We have implemented policies and procedures to comply with the security regulations.
Civil Monetary Penalties
The Secretary of HHS may impose civil monetary penalties on any person or entity that presents, or causes to be presented, certain ineligible claims for medical items or services. The amount of penalties varies depending on the offense, from $2,000 to $50,000 per violation, plus treble damages for the amount at issue and may include exclusion from federal health care programs (including Medicare and Medicaid).
HHS also can impose penalties on a person or entity who offers inducements to beneficiaries for program services, who violates rules regarding the assignment of payments, or who knowingly gives false or misleading information that could reasonably influence the discharge of patients from a hospital. Persons who have been excluded from a federal health care program and who retain ownership in a participating entity and persons who contract with excluded persons may be penalized.
HHS also can impose penalties for false or fraudulent claims and those that include services not provided as claimed. In addition, HHS may impose penalties on claims:
| • | for physician services that the person or entity knew or should have known were rendered by a person who was unlicensed, or by a person who misrepresented either (1) his or her qualifications in obtaining his or her license or (2) his or her certification in a medical specialty; |
27
Table of Contents
| • | for services furnished by a person who was, at the time the claim was made, excluded from the program to which the claim was made; or |
| • | that show a pattern of medically unnecessary items or services. |
Penalties also are applicable in certain other cases, including violations of the federal Anti-Kickback Statute, payments to limit certain patient services and improper execution of statements of medical necessity.
Environmental Health and Safety Laws
We are subject to federal, state and local regulations governing the storage, use and disposal of materials and waste products. Although we believe that our safety procedures for storing, handling and disposing of these hazardous materials comply with the standards prescribed by law and regulation, we cannot completely eliminate the risk of accidental contamination or injury from those hazardous materials. In the event of an accident, we could be held liable for any damages that result and any liability could exceed the limits or fall outside the coverage of our insurance. We may not be able to maintain insurance on acceptable terms, or at all. We could incur significant costs and the diversion of our management’s attention to comply with current or future environmental laws and regulations. We do not have any violations related to compliance with environmental, health and safety laws through 2009.
Licensing
Our agencies and facilities are subject to state and local licensing regulations ranging from the adequacy of medical care to compliance with building codes and environmental protection laws. To assure continued compliance with these various regulations, governmental and other authorities periodically inspect our agencies and facilities. Additionally, health care professionals at our agencies and facilities are required to be individually licensed or certified under applicable state law. We take steps to ensure that our employees and agents possess all necessary licenses and certifications.
The institutional pharmacy operations within our facility-based services segment are also subject to regulation by the various states in which we conduct the pharmacy business, as well as by the federal government. The pharmacies are regulated under the Food, Drug and Cosmetic Act and the Prescription Drug Marketing Act, which are administered by the United States Food and Drug Administration. Under the Comprehensive Drug Abuse Prevention and Control Act of 1970, administered by the United States Drug Enforcement Administration, dispensers of controlled substances must register with the Drug Enforcement Administration, file reports of inventories and transactions and provide adequate security measures. Failure to comply with such requirements could result in civil or criminal penalties. We do not have any violations related to the Comprehensive Drug Abuse Prevention and Control Act of 1970 through 2009.
Accreditation
The Joint Commission is a nationwide commission that establishes standards relating to the physical plant, administration, quality of patient care and operation of medical staffs of health care organizations. Currently, Joint Commission accreditation of home nursing and hospice agencies is voluntary. However, some managed care organizations use Joint Commission accreditation as a credentialing standard for regional and state contracts. As of December 31, 2009, the Joint Commission had accredited 119 of our agencies. Those not yet accredited are working towards achieving this accreditation. By the end of 2010, we expect to have 219 agencies accredited by the Joint Commission.
Certificate of Need and Permit of Approval Laws
In addition to state licensing laws, some states require a provider to obtain a certificate of need or permit of approval prior to establishing or expanding certain health services or facilities. States with certificate of need or permit of approval laws place limits on both the construction and acquisition of health care facilities and operations and the expansion of existing facilities and services. In these states, approvals are required for capital expenditures
28
Table of Contents
exceeding certain amounts that involve certain facilities or services, including home nursing agencies. The certificate of need or permit of approval issued by the state determines the service areas for the applicable agency or program. The following states issue certificate of need or permits of approval: Alabama, Alaska, Arkansas, Georgia, Hawaii, Kentucky, Maryland, Mississippi, Montana, New Jersey, New York, North Carolina, South Carolina, Tennessee, Vermont, Washington, West Virginia and the District of Columbia. In addition, the state of Louisiana has imposed a moratorium on the issuance of new licenses for home nursing agencies that we expect to remain in effect for 2010.
State certificate of need and permit of approval laws generally provide that, prior to the addition of new capacity, the construction of new facilities or the introduction of new services, a designated state health planning agency must determine that a need exists for those beds, facilities or services. The process is intended to promote comprehensive health care planning, assist in providing high quality health care at the lowest possible cost and avoid unnecessary duplication by ensuring that only needed health care facilities and operations will be built and opened.
Employees
As of December 31, 2009 we had 6,998 employees, of which 4,713 were full-time and 2,285 were part-time, and approximately 825 independent contractors. None of our employees are subject to a collective bargaining agreement. We consider our relationships with our employees and independent contractors to be good.
Insurance
We are subject to claims and legal actions in the ordinary course of our business. To cover claims that may arise, we maintain professional malpractice liability insurance, general liability insurance, automobile liability insurance and workers’ compensation/employer’s liability insurance in amounts that we believe are appropriate and sufficient for our operations. We maintain professional malpractice and general liability insurance that provide primary coverage on a claims-made basis of $1.0 million per incident and $3.0 million in annual aggregate amounts. We maintain workers’ compensation insurance that meets state statutory requirements with a primary employer liability limit of $1.0 million for Louisiana, Mississippi, Alabama, Arkansas, Texas, Tennessee, Georgia, Florida, Kentucky, Missouri, Oklahoma, Virginia, West Virginia, Oregon and North Carolina. There are no limits to employer liability in Ohio and Washington. We maintain automobile liability insurance for all owned, hired and non-owned autos with a primary limit of $2.0 million. In addition, we currently maintain multiple layers of umbrella coverage in the aggregate amount of $25.0 million that provides excess coverage for professional malpractice, general liability, automobile liability and employer’s liability. We maintain directors and officers liability insurance in the aggregate amount of $25.0 million. The cost and availability of insurance coverage has varied widely in recent years. While we believe that our insurance policies and coverage are adequate for a business enterprise of our type, we cannot guarantee that our insurance coverage is sufficient to cover all future claims or that it will continue to be available in adequate amounts or at a reasonable cost.
Available Information
Our Annual Reports on Form 10-K, Quarterly Reports on Form 10-Q, Current Reports on Form 8-K, proxy statements and amendments to those reports are available free of charge on our internet website at www.lhcgroup.com as soon as reasonably practicable after such reports are electronically filed with or furnished to the Securities and Exchange Commission (“SEC”). The SEC also maintains an internet site at www.sec.gov that contains reports, proxy and information statements and other information regarding issuers that file electronically with the SEC. These reports may also be obtained at the SEC’s Public Reference Room at 100 F Street NE, Washington, D.C. 20549. Information on the operation of the Public Reference Room is available by calling the SEC at (800) SEC-0330.
| Item 1A. | Risk Factors. |
The risks and uncertainties described below and elsewhere in this Annual Report on Form 10-K could cause our actual results to differ materially from past or expected results and are not the only ones we face. Other risks and uncertainties that we have not predicted or assessed may also adversely affect us.
If any of the following risks occurs, our earnings, financial condition or business could be materially harmed and the trading price of our common stock could decline, resulting in the loss of all or part of investments.
29
Table of Contents
Risk Factors Related to Reimbursement and Government Regulation
We derive more than 80% of our net service revenue from Medicare. If there are changes in Medicare rates or methods governing Medicare payments for our services, or if we are unable to control our costs, our results of operations and cash flows could decline materially.
For the years ended December 31, 2009, 2008 and 2007, we received 81.7%, 83.2% and 81.7%, respectively, of our net service revenue from Medicare. Reductions in Medicare rates or changes in the way Medicare pays for services could cause our net service revenue and net income to decline, perhaps materially. Reductions in Medicare reimbursement could be caused by many factors, including:
| • | administrative or legislative changes to the base rates under the applicable prospective payment systems; |
| • | the reduction or elimination of annual rate increases; |
| • | the imposition or increase by Medicare of mechanisms, such as co-payments, shifting more responsibility for a portion of payment to beneficiaries; |
| • | adjustments to the relative components of the wage index used in determining reimbursement rates; |
| • | changes to case mix or therapy thresholds; |
| • | the reclassification of home health resource groups or long-term care diagnosis-related groups; or |
| • | further limitations on referrals to long-term acute care hospitals from host hospitals. |
We receive fixed payments from Medicare for our services based on the level of care provided to our patients. Consequently, our profitability largely depends upon our ability to manage the cost of providing these services. Medicare currently provides for an annual adjustment of the various payment rates, such as the base episode rate for our home nursing services, based upon the increase or decrease of the medical care expenditure category of the Consumer Price Index, which may be less than actual inflation. This adjustment could be eliminated or reduced in any given year. Our base episode rate for home nursing services is also subject to an annual market basket adjustment. For 2009 and 2008, the home health market basket percentage increase was 2.9% and 3.0%, respectively. Further, Medicare routinely reclassifies home health resource groups and long-term care diagnosis-related groups. As a result of those reclassifications, we could receive lower reimbursement rates depending on the case mix of the patients we service. If our cost of providing services increases by more than the annual Medicare price adjustment, or if these reclassifications result in lower reimbursement rates, our results of operations, net income and cash flows could be adversely impacted.
Proposed Healthcare Reform, if passed into law, could reduce our revenue and profitability.
Both houses of the U.S. Congress have passed bills that would reform the structure and funding of the U.S. healthcare system. However, the two bills have not been reconciled with each other and signed into law.
We cannot predict if any of these proposals will ultimately become law, or, if enacted, what their terms or the regulations promulgated pursuant to such laws will be. Any health care reforms may be phased in over a number of years but, if enacted, could reduce our revenues, increase our costs, expose us to expanded liability and require us to revise the ways in which we conduct business or put us at risk for loss of business. In addition, our results of operations and our financial position, including our ability to maintain the value of our goodwill and cash flows could be materially adversely affected by such changes.
We are subject to extensive government regulation. Any changes in the laws and regulations governing our business, or the interpretation and enforcement of those laws or regulations, could require us to modify our operations and could negatively impact our operating results and cash flows.
As a provider of health care services, we are subject to extensive regulation on the federal, state and local levels, including with regard to:
| • | licensure and certificates of need and permits of approval; |
30
Table of Contents
| • | coding and billing for services; |
| • | conduct of operations, including financial relationships among health care providers, Medicare fraud and abuse and physician self-referral; |
| • | maintenance and protection of records, including HIPAA; |
| • | environmental protection, health and safety; |
| • | certification of additional agencies or facilities by the Medicare program; and |
| • | payment for services. |
The laws and regulations governing our operations, along with the terms of participation in various government programs, regulate how we do business, the services we offer and our interactions with patients and other providers. These laws and regulations, and their interpretations, are subject to frequent change. Changes in existing laws, regulations, their interpretations or the enactment of new laws or regulations could increase our costs of doing business and cause our net income to decline. If we fail to comply with these applicable laws and regulations, we could suffer civil or criminal penalties, including the loss of our licenses to operate and our ability to participate in federal and state reimbursement programs.
We are also subject to various routine and non-routine governmental reviews, audits and investigations. These audits include those conducted through the recovery audit contractor program, in which third party firms engaged by CMS conduct extensive reviews of claims data and non-medical and other records to identify potential improper payments under the Medicare Program. In recent years, federal and state civil and criminal enforcement agencies have heightened and coordinated their oversight efforts related to the health care industry, including with respect to referral practices, cost reporting, billing practices, joint ventures and other financial relationships among health care providers. Although we have invested substantial time and effort in implementing policies and procedures to comply with laws and regulations, we could be subject to liabilities arising from violations. A violation of the laws governing our operations, or changes in the interpretation of those laws, could result in the imposition of fines, civil or criminal penalties, the termination of our rights to participate in federal and state-sponsored programs or the suspension or revocation of our licenses to operate. If we become subject to material fines or if other sanctions or other corrective actions are imposed upon us, we may suffer a substantial reduction in net income.
Current economic conditions and continued decline in spending by the Federal and State governments could harm our results of operations and cash flows.
Worldwide economic conditions have significantly declined and will likely remain depressed for the foreseeable future. While our services are not typically sensitive to general declines in the federal and state economies, the erosion in the tax base caused by the general economic downturn has caused, and will likely continue to cause, restrictions on the federal and state governments’ ability to obtain financing and a decline in spending. As a result, we may face reimbursement rate cuts or reimbursement delays from Medicare and Medicaid and other governmental payors, which could adversely impact our results of operations and cash flows.
If any of our agencies or facilities fail to comply with the conditions of participation in the Medicare program, that agency or facility could be terminated from Medicare, which could adversely affect our net service revenue and net income.
Our agencies and facilities must comply with the extensive conditions of participation in the Medicare program. These conditions of participation vary depending on the type of agency or facility, but, in general, require our agencies and facilities to meet specified standards relating to personnel, patient rights, patient care, patient records, administrative reporting and legal compliance. If an agency or facility fails to meet any of the Medicare conditions of participation, that agency or facility may receive a notice of deficiency from the applicable state surveyor. If that agency or facility then fails to institute and comply with a plan of correction to correct the deficiency within the time period provided by the state surveyor, that agency or facility could be terminated from the Medicare program. We respond in the ordinary course to deficiency notices issued by state surveyors and none of our facilities or agencies have ever been terminated from the Medicare program for failure to comply with the conditions of participation. Any termination of one or more of our agencies or facilities from the Medicare program for failure to satisfy the Medicare conditions of participation could adversely affect our net service revenue and net income.
31
Table of Contents
The inability of our long-term acute care hospitals to maintain their certification as long-term acute care hospitals could have an adverse affect on our results of operations and cash flows.
If our LTACHs fail to meet or maintain the standards for Medicare certification as LTACHs, such as for average minimum length of patient stay, they will receive reimbursement under the prospective payment system applicable to general acute care hospitals rather than the system applicable to long-term acute care hospitals. Payments at rates applicable to general acute care hospitals would likely result in our long-term acute care hospitals receiving less Medicare reimbursement than they currently receive for their patient services. Moreover, all but one of our LTACHs are subject to additional Medicare criteria because they operate as separate hospitals located in space leased from and located in a general acute care hospital, known as a host hospital. This is known as a “hospital within a hospital” model. These additional criteria include requirements concerning financial and operational separateness from the host hospital. If any of our LTACHs were subject to payment as general acute care hospitals or failed to comply with the separateness requirements, our net service revenue and net income would decline.
CMS has adopted regulations that could materially and adversely affect the results of operations and cash flows of our long-term acute care hospitals.
In a final rule released on May 1, 2007, CMS expanded the Medicare admissions threshold to apply not only to long-term acute care hospitals within hospitals and satellites but also to freestanding LTACHs and grandfathered LTACHs. The policy also applies to HwHs and satellites that admit Medicare patients from non-co-located hospitals. While this policy change was supposed to take effect for cost reporting periods beginning on or after July 1, 2007, the MMSEA delayed the implementation of the policy for three years with respect to freestanding LTACHs and grandfathered LTACHs. Further, the MMSEA set the percentage threshold at 50% for three years for HwHs and satellites located in urban areas that would otherwise be subject to a transition period and it established a 75% ceiling for HwHs and satellite facilities located in rural areas and those that receive referrals from MSA dominant hospitals or urban single hospitals.
We currently have a total of eight LTACHs. Seven of our hospitals are classified as HwHs and one as freestanding. Of the seven HwH facilities, four are located in rural or non-MSAs and are, therefore, subject to a final admission percentage of 50% at the end of the phase-in period. Three of our seven HwH facilities are located in MSA or urban areas and will be subject to a final admission percentage of 25% at the end of the phase-in period. Of the seven locations classified as HwHs, three facilities are satellite locations of a parent hospital located in an MSA and one is a satellite location of a parent hospital located in a non-MSA. Based on our discussions with CMS, we believe each of these satellite locations will be viewed as being located in a non-MSA regardless of the location of its parent hospital and will be treated independently from its parent for purposes of calculating its compliance with the admissions limitations. If the “25 percent rule” is extended, as planned, to freestanding LTACHs after the three-year delay established in the MMSEA, our current freestanding facility would not likely be affected because we currently do not receive more than 25% of our Medicare admissions from any single referring hospital.
For the 12 months ended December 31, 2009, on an individual basis, six of our LTACH locations admitted between 50% and 75% of their patients from their host hospitals. These hospitals came under the proper threshold as of their cost report year, August 31, 2009. Our new LTACH acquired in 2009, is a grandfathered LTACH and, , has no limitations under MMSEA with respect to the number of patients that can be admitted from the host hospital. Our remaining LTACH is not an HwH; therefore, it is not subject to these limits on host hospital referrals.
Our ability to quantify the potential reduction in our reimbursement rates resulting from the implementation of these new regulations is contingent upon a variety of factors, such as our ability to reduce the percentage of admissions that are derived from our host hospitals and, if necessary, our ability to relocate our existing long-term acute care hospitals to freestanding locations. We may not be able to successfully restructure or relocate these operations without incurring significant expense or in a manner that avoids reimbursement reductions. If these new regulations result in lower reimbursement rates, our net service revenue and net income could decline. As a result of these new rules, we do not intend to expand the number of HwH long-term acute care hospitals that we operate.
We are reimbursed by Medicare for services we provide in our long-term acute care hospitals based on the long-term care diagnosis-related group assigned to each patient. CMS establishes these long-term care diagnosis-related groups by grouping diseases by diagnosis to reflect the amount of resources needed to treat a given disease. The
32
Table of Contents
May 2007 CMS final rules reclassifies certain long-term care diagnosis-related groups, which could result in a decrease in reimbursement rates. Further, the rule kept in place the financial penalties associated with the failure to limit the total number of Medicare patients discharged from a host hospital and subsequently readmitted to a long-term acute care hospital located within the host hospital to no greater than 5.0%. If we fail to comply with these readmission rates or if our reimbursement rates decline due to the reclassification of certain long-term care diagnosis-related groups, our net service revenue and net income could decline.
Legislative initiatives could negatively impact our operations and financial results.
In recent years, an increasing number of legislative initiatives have been introduced or proposed in Congress and in state legislatures that would result in major changes in the health care system, either at the national or state level. Many of these proposals have been introduced in an effort to reduce costs. For example, the Medicare Modernization Act of 2003 (“MMA”) allocated significant additional funds to Medicare managed care providers in order to promote greater participation in those plans by Medicare beneficiaries. If these increased funding levels achieve their intended result, the rate of growth in the Medicare fee-for-service market could decline. For the years ended December 31, 2009, 2008 and 2007, we received 81.7%, 83.2% and 81.7%, respectively, of our net service revenue from the Medicare fee-for-service market. Among other proposals that have been introduced are insurance market reforms to increase the availability of group health insurance to small businesses, requirements that all businesses offer health insurance coverage to their employees and the creation of government health insurance or plans that would cover all citizens and increase payments by beneficiaries. We cannot predict whether any of the above proposals, or any other future proposals, will be adopted. If adopted, we could be forced to expend considerable resources to comply with and implement such reforms, which may place us at a competitive disadvantage.
If the structures or operations of our joint ventures are found to violate the law, it could have a material adverse impact on our financial condition and consolidated results of operations.
As of December 31, 2009, 51.4% of our net service revenue was derived from our joint ventures. Our joint ventures are structured either as equity joint ventures or agency leasing arrangements, as permitted by applicable state laws and subject to business considerations. As of December 31, 2009, we had 63 equity joint ventures and four agency leasing arrangements. Of these 63 joint ventures, 55 are with hospitals, four are with physicians and four are with other parties. With respect to our four joint ventures with physicians, three are for the ownership and operation of long-term acute care hospitals and one is for the ownership of a rural home nursing agency.
Several of our joint ventures are with hospitals and physicians, which are governed by the Anti-Kickback Statute and similar state laws. These anti-kickback statutes prohibit the payment or receipt of anything of value in return for referrals of patients or services covered by governmental health care programs, such as Medicare. The OIG has published numerous safe harbors that exempt qualifying arrangements from enforcement under the Anti-Kickback Statute. We have sought to satisfy as many safe harbor requirements as possible in structuring our joint ventures. For example, each of our equity joint ventures with hospitals and physicians is structured in accordance with the following principles:
| • | the investment interest offered is not based upon actual or expected referrals by the hospital or physician; |
| • | our joint venture partners are not required to make or influence referrals to the joint venture; |
| • | at the time the joint venture is formed, each hospital or physician joint venture partner is required to make an actual capital contribution to the joint venture equal to the fair market value of his or her investment interest and is at risk to lose its investment; |
| • | neither we nor the joint venture entity lends funds to or guarantees a loan to acquire interests in the joint venture for a hospital or physician; and |
| • | distributions to our joint venture partners are based solely on their equity interests and are not affected by referrals from the hospital or physician. |
Despite our efforts to meet the safe harbor requirements where possible, our joint ventures may not satisfy all elements of the safe harbor requirements.
33
Table of Contents
Our five joint ventures with physicians are also governed by the Stark Law and similar state laws, which restrict physicians from making referrals for particular health care services to entities with which the physicians or their families have a financial relationship. We also believe we have structured our physician joint ventures in a way that meets applicable exceptions under the Stark Law and similar state physician referral laws. For example, we believe our one physician joint venture for a home nursing agency complies with the rural provider exception to the Stark Law and that our four physician joint ventures for LTACHs comply with the whole hospital exception to the Stark Law.
If any of our joint ventures were found to be in violation of federal or state anti-kickback or physician referral laws, we could be required to restructure them or refuse to accept referrals from the physicians or hospitals with which we have entered into a joint venture. We also could be required to repay to Medicare amounts we have received pursuant to any prohibited referrals, and we could suffer civil or criminal penalties, including the loss of our licenses to operate and our ability to participate in federal and state health care programs. If any of our joint ventures were subject to any of these penalties, our business could be materially adversely affected. If the structure of any of our joint ventures were found to violate federal or state anti-kickback statutes or physician referral laws, we may be unable to implement our growth strategy, which could have an adverse impact on our future net income and consolidated results of operations.
The application of state certificate of need and permit of approval regulations and compliance with federal and state licensing requirements could substantially limit our ability to operate and grow our business.
Our ability to expand operations in a state will depend on our ability to obtain a state license to operate. States may have a limit on the number of licenses they issue. For example, as of December 31, 2009, we operated 54 home nursing agencies in Louisiana. Louisiana currently has a moratorium on the issuance of new home nursing agency licenses through 2009. We cannot predict whether this moratorium will be extended beyond this date or whether any other states in which we currently operate, or may wish to operate in the future, may adopt a similar moratorium.
We currently operate in ten states that require health care providers to obtain prior approval, known as a certificate of need or a permit of approval, for the purchase, construction or expansion of health care facilities, to make certain capital expenditures or to make changes in services or bed capacity. The states that currently issue certificate of need or permits of approval are: Alabama, Alaska, Arkansas, Georgia, Hawaii, Kentucky, Maryland, Mississippi, Montana, New Jersey, New York, North Carolina, South Carolina, Tennessee, Vermont, Washington, West Virginia and the District of Columbia. In granting approval, these states consider the need in the service area for additional or expanded health care facilities or services. The failure to obtain any requested certificate of need, permit of approval or other license could impair our ability to operate or expand our business.
Risk Factors Related to Capital and Liquidity
The adverse changes and uncertainty in the capital and credit markets may negatively affect our ability to access financing. Without such financing we may be unable to achieve our objectives for strategic acquisitions and internal growth.
The disruption of the global financial and credit markets and the related instability in the global financial system may have an effect on our long term liquidity and financial conditions. While we have been able to achieve our current acquisition strategy through operating cash and without long term borrowing on our Credit Facility, the need may arise to obtain additional funding.
At December 31, 2009, we had $394,000 in cash. Based on our current plan of operations, including acquisitions, we believe this amount, when combined with expected cash flows from operations and amounts available under our revolving line of credit, will be sufficient to fund our growth strategy and to meet our anticipated operating expenses, capital expenditures and debt service obligations for at least the next 12 months. If our future net service revenue or cash flow from operations is less than we currently anticipate, we may not have sufficient funds to implement our growth strategy. Further, we cannot readily predict the timing, size and success of our acquisition and internal development efforts and the associated capital commitments. If we do not have sufficient cash resources, our growth could be limited unless we are able to obtain additional equity or debt financing.
We do not believe our availability of funds under our Credit Facility is at risk; however, we continue to monitor our lenders. If the availability of funds under our Credit Facility decreases we may need to consider adjusting our growth strategy.
34
Table of Contents
The agreement governing our credit facility contains, and future debt agreements may contain, various covenants that limit our discretion in the operation of our business.
The agreement and instruments governing our outstanding Credit Facility, and the agreements and instruments governing future debt agreements may contain various restrictive covenants that, among other things, require us to comply with or maintain certain financial tests and ratios that may restrict our ability to:
| • | incur more debt; |
| • | redeem or repurchase stock, pay dividends or make other distributions; |
| • | make certain investments; |
| • | create liens; |
| • | enter into transactions with affiliates; |
| • | make unapproved acquisitions; |
| • | merge or consolidate; |
| • | transfer or sell assets; and |
| • | make fundamental changes in our corporate existence and principal business. |
In addition, events beyond our control could affect our ability to comply with and maintain these financial tests and ratios. Any failure by us to comply with or maintain all applicable financial tests and ratios and to comply with all applicable covenants could result in an event of default with respect to our credit facility or any other future debt agreements. An event of default could lead to the acceleration of the maturity of any outstanding loans and the termination of the commitments to make further extensions of credit. Even if we are able to comply with all applicable covenants, the restrictions on our ability to operate our business at our sole discretion could harm our business by, among other things, limiting our ability to take advantage of financing, mergers, acquisitions and other corporate opportunities.
Our net service revenue is concentrated in a small number of states, which makes us sensitive to regulatory and economic changes in those states.
Our net service revenue is particularly sensitive in the 18 states in which we provide services - Louisiana, Mississippi, Kentucky, Arkansas, Alabama, Virginia, West Virginia, Texas, Tennessee, Florida, Georgia, Ohio, Missouri, North Carolina, Maryland, Oklahoma, Oregon and Washington. The Company’s Louisiana facilities accounted for approximately 34.0%, 41.9% and 50.9% of net service revenue during the years ended December 31, 2009, 2008 and 2007 respectively. Accordingly, any changes in the current demographic, economic, competitive, or regulatory conditions in these states could have an adverse effect on our business, financial condition, results of operations and cash flows. Medicaid changes in these states could also have a material adverse effect on our results of operations or cash flows.
Hurricanes or other adverse weather events could negatively affect the local economies in which we operate or disrupt our operations, which could have an adverse effect on our business or results of operations.
Our operations along coastal areas in the southern United States are particularly susceptible to hurricanes. Such weather events can disrupt our operations, result in damage to our properties and negatively affect the local economies in which we operate. In late summer 2008, Hurricane Ike and Hurricane Gustav struck the Gulf Coast region of the United States and caused extensive and catastrophic physical damage to those areas. While we have recovered from the effects of Hurricane Ike and Hurricane Gustav, future hurricanes could affect our operations or the economies in those market areas and result in damage to certain of our facilities, the equipment located at such facilities or equipment rented to patients in those areas. Our business or results of operations may be adversely affected by these and other negative effects of future hurricanes. Although we maintain insurance coverage, we
35
Table of Contents
cannot guarantee that our insurance coverage will be adequate to cover any losses or that we will be able to maintain insurance at a reasonable cost in the future. If our losses from business interruption or property damage exceed the amount for which we are insured, our results of operations and financial condition would be adversely affected.
Delays in reimbursement may cause liquidity problems.
Our business is characterized by delays in reimbursement from the time we request payment for our services to the time we receive reimbursement or payment. A portion of our estimated reimbursement (60.0% for an initial episode of care and 50.0% for subsequent episodes of care) for each Medicare episode is billed at the commencement of the episode and we typically receive payment within approximately 12 days. The remaining reimbursement is billed upon completion of the episode and is typically paid within 14 to 17 days from the billing date. If we have information system problems or issues arise with Medicare or other payors, we may encounter further delays in our payment cycle. For example, in the past we have experienced delays resulting from problems arising out of the implementation by Medicare of new or modified reimbursement methodologies or as a result of natural disasters, such as hurricanes. We have also experienced delays in reimbursement resulting from our implementation of new information systems related to our accounts receivable and billing functions. Any future timing delay may cause working capital shortages. As a result, working capital management, including prompt and diligent billing and collection, is an important factor in our consolidated results of operations and liquidity. Our working capital management procedures may not successfully negate this risk. Significant delays in payment or reimbursement could have an adverse impact on our liquidity and financial condition.
Risk Factors Related to Operations and our Growth Strategy
We could be required to record a material non-cash charge to income if our recorded goodwill or intangible assets are impaired.
As of December 31, 2009, we have recorded $139.5 million to goodwill and $46.9 million to intangible assets, net, on our consolidated balance sheet. Goodwill and other intangibles are assessed for impairment annually for each of our reporting units. The assessment includes comparing the fair value of each reporting unit to the carrying value of the assets assigned to the reporting unit. If the carrying value of the reporting unit were to exceed our estimate of fair value of the reporting unit, we would be required to estimate the fair value of the individual assets and liabilities within the reporting unit to ascertain the fair value of goodwill. If we determine that the fair value is less than our book value, we could be required to record a non-cash impairment charge to our consolidated statements of income, which could have a material adverse effect on our earnings.
Our allowance for contractual adjustments and doubtful accounts may not be sufficient to cover uncollectible amounts.
On an ongoing basis, we estimate the amount of Medicare, Medicaid and private insurance receivables that we will not be able to collect. This allows us to calculate the expected loss on our receivables for the period we are reporting. Our allowance for contractual adjustments and doubtful accounts may underestimate actual unpaid receivables for various reasons, including:
| • | adverse changes in our estimates as a result of changes in payor mix and related collection rates; |
| • | inability to collect funds due to missed filing deadlines or inability to prove that timely filings were made; |
| • | adverse changes in the economy generally exceeding our expectations; or |
| • | unanticipated changes in reimbursement from Medicare, Medicaid and private insurance companies. |
If our allowance for contractual adjustments and doubtful accounts is insufficient to cover losses on our receivables, our business, financial position and results of operations could be materially adversely affected.
Changes in the case mix of patients, as well as payor mix and payment methodologies, may have a material adverse effect on our results of operations and cash flows.
The sources and amounts of our patient revenue are determined by a number of factors, including the mix of patients and the rates of reimbursement among payors. Generally, we receive higher reimbursement for Medicare. Changes in the case mix of the patients, payment methodologies or payor mix among private pay, Medicare and Medicaid may significantly affect our results of operations and cash flows.
36
Table of Contents
Shortages in qualified nurses and other health care professionals could increase our operating costs significantly or constrain our ability to grow.
We rely on our ability to attract and retain qualified nurses and other health care professionals. The availability of qualified nurses nationwide has declined in recent years and competition for these and other health care professionals has increased, while salary and benefit costs have risen accordingly. Our ability to attract and retain nurses and other health care professionals depends on several factors, including our ability to provide desirable assignments and competitive benefits and salaries. We may not be able to attract and retain qualified nurses or other health care professionals in the future. In addition, the cost of attracting and retaining these professionals and providing them with attractive benefit packages may be higher than anticipated which could cause our net income to decline. Moreover, if we are unable to attract and retain qualified professionals, the quality of services offered to our patients may decline or our ability to grow may be constrained.
If we are required to either repurchase or sell a substantial portion of the equity interests in our joint ventures, our capital resources and financial condition could be materially adversely impacted.
Upon the occurrence of fundamental changes to the laws and regulations applicable to our joint ventures, or if a substantial number of our joint venture partners were to exercise the buy/sell provisions contained in many of our joint venture agreements, we may be obligated to purchase or sell the equity interests held by us or our joint venture partners. In some instances, the purchase price under these buy/sell provisions is based on a multiple of the historical or future earnings before income taxes, depreciation and amortization of the equity joint venture at the time the buy/sell option is exercised. In other instances, the buy/sell purchase price will be negotiated by the partners but will be subject to a fair market valuation process. In the event the buy/sell provisions are exercised and we lack sufficient capital to purchase the interest of our joint venture partners, we may be obligated to sell our equity interest in these joint ventures. If we are forced to sell our equity interest, we will lose the benefit of those particular joint venture operations. If these buy/sell provisions are exercised and we choose to purchase the interest of our joint venture partners, we may be obligated to expend significant capital in order to complete such acquisitions. If either of these events occurs, our net service revenue and net income could decline or we may not have sufficient capital necessary to implement our growth strategy.
If we are unable to maintain relationships with existing referral sources or establish new referral sources, our growth and net income could be adversely affected.
Our success depends significantly on referrals from physicians, hospitals and other health care providers in the communities in which we deliver our services. Our referral sources are not obligated to refer business to us and may refer business to other health care providers. We believe many of our referral sources refer business to us as a result of the quality of patient care provided by our local employees in the communities in which our agencies and facilities are located. If we are unable to retain these employees, our referral sources may refer business to other health care providers. Our loss of, or failure to maintain, existing relationships or our failure to develop new relationships could affect adversely our ability to expand our operations and operate profitably.
We face competition, including from competitors with greater resources, which may make it difficult for us to compete effectively as a provider of post-acute health care services.
We compete with local and regional home nursing and hospice companies, hospitals and other businesses that provide post-acute health care services, some of which are large established companies that have significantly greater resources than we do. Our primary competition comes from local operators in each of our markets. We expect our competitors to develop joint ventures with providers, referral sources and payors, which could result in increased competition. The introduction by our competitors of new and enhanced service offerings, in combination with industry consolidation and the development of competitive joint ventures, could cause a decline in net service revenue, loss of market acceptance of our services or make our services less attractive. Future increases in competition from existing competitors or new entrants may limit our ability to maintain or increase our market share. We may not be able to compete successfully against current or future competitors and competitive pressures may have a material, adverse impact on our business, financial condition and results of operations.
37
Table of Contents
Future acquisitions may be unsuccessful and could expose us to unforeseen liabilities. Further, our acquisition and internal development activity may impose strains on our existing resources.
Our growth strategy involves the acquisition of home nursing agencies throughout the United States. These acquisitions involve significant risks and uncertainties, including difficulties integrating acquired personnel and other corporate cultures into our business, the potential loss of key employees or patients of acquired agencies and the assumption of liabilities and exposure to unforeseen liabilities of acquired agencies. We may not be able to fully integrate the operations of the acquired businesses with our current business structure in an efficient and cost-effective manner. The failure to effectively integrate any of these businesses could have a material adverse effect on our operations.
We generally structure our acquisitions as asset purchase transactions in which we expressly state that we are not assuming any pre-existing liabilities of the seller and obtain indemnification rights from the previous owners for acts or omissions arising prior to the date of such acquisitions. However, the allocation of liability arising from such acts or omissions between the parties could involve the expenditure of a significant amount of time, manpower and capital. Further, the former owners of the agencies and facilities we acquire may not have the financial resources necessary to satisfy our indemnification claims relating to pre-existing liabilities. If we were unsuccessful in a claim for indemnification from a seller, the liability imposed could materially, adversely affect our operations.
In addition, as we continue to expand our markets, our growth could strain our resources, including management, information and accounting systems, regulatory compliance, logistics and other internal controls. Our resources may not keep pace with our anticipated growth. If we do not manage our expected growth effectively, our future prospects could be affected adversely.
We may face increased competition for attractive acquisition and joint venture candidates.
We intend to continue growing through the acquisition of additional home nursing agencies and the formation of joint ventures with hospitals for the operation of home nursing agencies. We face competition for acquisition and joint venture candidates, which may limit the number of acquisition and joint venture opportunities available to us or lead to the payment of higher prices for our acquisitions and joint ventures. Recently, we have observed an increase in the acquisition prices for select home nursing agencies. We cannot guarantee that we will be able to identify suitable acquisition or joint venture opportunities in the future or that any such opportunities, if identified, will be consummated on favorable terms, if at all. Without successful acquisitions or joint ventures, our future growth rate could decline. In addition, we cannot guarantee that any future acquisitions or joint ventures, if consummated, will result in further growth.
Federal regulation may impair our ability to consummate acquisitions or open new agencies.
Changes in Federal laws or regulations may materially adversely impact our ability to acquire agencies or open new start-up agencies. For example, CMS recently adopted a regulation known as the “36 Month Rule” that is applicable to home health agency acquisitions. The 36 Month Rule prohibits buyers of certain home health agencies – those that either enrolled in Medicare or underwent a change in ownership fewer than 36 months prior to the acquisitions – from assuming the Medicare billing privileges of the acquired agency. Instead, the acquired agencies must enroll as new providers with Medicare. As a result, the 36 Month Rule may further increase competition for acquisition targets that are not subject to the rule, and may cause significant Medicare billing delays for the purchases of agencies that are subject to the rule.
If we are subject to substantial malpractice or other similar claims, it could materially adversely impact our results of operations and financial condition flows.
The services we offer have an inherent risk of professional liability and substantial damage awards. We, and the nurses and other health care professionals who provide services on our behalf, may be the subject of medical malpractice claims. These nurses and other health care professionals could be considered our agents and, as a result, we could be held liable for their medical negligence. We cannot predict the effect that any claims of this nature, regardless of their ultimate outcome, could have on our business or reputation or on our ability to attract and retain patients and employees. We maintain malpractice liability insurance that provides primary coverage on a claims-made basis of $1.0 million per incident and $3.0 million in annual aggregate amounts. In addition, we maintain multiple layers of umbrella coverage in the aggregate amount of $25.0 million that provide excess coverage for professional malpractice and other liabilities. We are responsible for deductibles and amounts in excess of the limits
38
Table of Contents
of our coverage. Claims that could be made in the future in excess of the limits of such insurance, if successful, could materially adversely affect our financial condition. In addition, our insurance coverage may not continue to be available to us at commercially reasonable rates, in adequate amounts or on satisfactory terms.
Failure of, or problems with, our critical software or information systems could harm our business and operating results.
In addition to our Service Value Point system, our business is also substantially dependent on non-proprietary software. We utilize a third-party software information system for billing and maintaining patient claim receivables for our LTACHs. Our various home nursing agency databases are fully consolidated into an enterprise-wide system. Problems with, or the failure of, these systems could negatively impact our clinical performance and our management and reporting capabilities. Any such problems or failure could materially and adversely affect our operations and reputation, result in significant costs to us, cause delays in our ability to bill Medicare or other payors for our services, or impair our ability to provide our services in the future. The costs incurred in correcting any errors or problems with regard to our proprietary and non-proprietary software may be substantial and could adversely affect our net income.
Our information systems are networked via public network infrastructure and standards based encryption tools that meet regulatory requirements for transmission of protected health care information over such networks. However, threats from computer viruses, instability of the public network on which our data transit relies, or other instances that might render those networks unstable or disabled would create operational difficulties for us, including difficulties effectively transmitting claims and maintaining efficient clinical oversight of our patients, as well as disrupting revenue reporting and billing and collections management, which could adversely affect our business or operations.
Risk Factors Related to our Ownership and Management
Start-up agencies can be delayed from opening in a timely manner due to processing or regulatory approvals.
There can be delays associated with opening a de novo agency. These delays are the result of processing delays with the state regulatory bodies as well as processing delays by the associated fiscal intermediaries that serve as billing liaisons between the agency and CMS. To initiate operations at a de novo agency, we must submit the necessary applications along with the required documentation to the appropriate state and Federal regulatory bodies. However, CMS has issued a memorandum which prioritizes the initial surveys for new Medicare providers as lowest priority for the state regulatory bodies. Moreover, depending on state requirements the fiscal intermediary may need to receive the state license before the approval process can move forward. Once the necessary application and documentation has been submitted to the state and Federal regulatory bodies, there is a testing period of transmitting data from the applicant to CMS. Once complete, the agency receives a provider agreement and corresponding number and can begin billing. If we are unable to obtain regulatory approval for our de novo agencies in a timely manner, such delays could have a material adverse effect on our business and our consolidated financial condition, results of operations and cash flows.
As a holding company, we have no material assets or operations of our own.
We are a holding company with no material assets or operations of our own. Accordingly, our ability to service our debt and pay dividends, if any, is dependent upon the earnings from the business conducted by our subsidiaries. The distributions of those earnings or advances or other distributions of funds by these subsidiaries to us are contingent upon the subsidiaries’ earnings and are subject to various business considerations. In addition, distributions by subsidiaries could be subject to statutory restrictions, including state laws requiring that the subsidiary be solvent, or contractual restrictions. If our subsidiaries are unable to make sufficient distributions or advances to us, we may not have the cash resources necessary to service our debt or pay dividends.
The loss of certain senior management could have a material adverse effect on our operations and financial performance.
Our success depends upon the continued employment of certain members of our senior management, including our co-founder, President and Chief Executive Officer, Keith G. Myers, our Executive Vice President and Chief Operating Officer, Donald D. Stelly and our Executive Vice President and Chief Financial Officer, Peter J. Roman. We have entered into an employment agreement with each of these officers in an effort to further secure their employment. The loss of service of any of these officers could have a material adverse effect on our operations if we were unable to find a suitable replacement.
39
Table of Contents
Our executive officers and directors and their affiliates hold a substantial portion of our stock and could exercise significant influence over matters requiring stockholder approval, regardless of the wishes of other stockholders.
Our executive officers and directors and individuals or entities affiliated with them, beneficially own an aggregate of approximately 16.5% of our outstanding common stock as of December 31, 2009. The interests of these stockholders may differ from other stockholders’ interests. If they were to act together, these affiliated stockholders would be able to significantly influence all matters that our stockholders vote upon, including the election of directors, business combinations, the amendment of our certificate of incorporation and other significant corporate actions.
Certain provisions of our charter, bylaws, Delaware law and our stockholder’s rights plan may delay or prevent a change in control of the Company.
Delaware law and our corporate documents contain provisions that may enable our board of directors to resist a change in control of the Company. These provisions include:
| • | a staggered board of directors; |
| • | limitations on persons authorized to call a special meeting of stockholders; |
| • | the authorization of undesignated preferred stock, the terms of which may be established and shares of which may be issued without stockholder approval; |
| • | advance notice procedures required for stockholders to nominate candidates for election as directors or to bring matters before an annual meeting of stockholders; and |
| • | a stockholder’s rights plan that includes a 20% threshold for triggering events, a three-year term for directors, an independent director evaluation provision (commonly known as a “TIDE” provision) and a stockholder redemption feature allowing stockholders to vote at a special meeting that would be called to consider qualified takeover offers. |
These anti-takeover defenses could discourage, delay or prevent a transaction involving a change in control of the Company. These provisions could also discourage proxy contests and make it more difficult for stockholders to elect directors or cause us to take other corporate actions.
We have implemented other anti-takeover provisions or provisions that could have an anti-takeover effect, including a stockholder rights plan, also known as a “poison pill.” This provision and others that our Board of Directors may adopt hereafter, may discourage offers to acquire us and may permit our board of directors to choose not to entertain offers to purchase us, even if such offers include a substantial premium to the market price of out stock. Therefore, our stockholders may be deprived of opportunities to profit from a sale of control.
Our stock is thinly traded, which may cause volatility in our stock price, including a decline in value.
We have a relatively low volume of daily trades in our common stock on the Nasdaq Global Select Market. For example, the average daily trading volume of our common stock on NASDAQ over the three-month trading period ending March 4, 2010 was approximately 190,000 shares per day. Because our common stock is traded infrequently, the price per share of our common stock can fluctuate more significantly from day-to-day than a widely held stock that is actively traded on a daily basis. For example, trading of a large volume of our common stock may have a significant impact on the trading price of our stock. In addition, future issuances of our common stock, including the exercise of any options or the vesting of any restricted stock that we may grant to directors, executive officers and other employees in the future and the issuance of common stock in connection with acquisitions, could have an adverse effect on the market price of our common stock.
If we identify deficiencies in our internal control over financial reporting, our business and our stock price could be adversely affected.
40
Table of Contents
We are required to report on the effectiveness of our internal control over financial reporting as required by Section 404 of Sarbanes-Oxley. Under Section 404, we are required to assess the effectiveness of our internal control over financial reporting and report our conclusion in our annual report. Our independent auditor is also required to report its conclusion regarding the effectiveness of our internal control over financial reporting. The existence of one or more material weaknesses would require us and our auditor to conclude that our internal control over financial reporting is not effective. If there are identified deficiencies in our internal control over financial reporting, we could be subject to regulatory scrutiny and a loss of public confidence in our financial reporting, which could have an adverse effect on our business and our stock price.
| Item 1B. | Unresolved Staff Comments |
We have no unresolved written comments from the staff of the SEC regarding our periodic or current reports filed under the Exchange Act.
| Item 2. | Properties. |
As of December 31, 2009, we owned or managed facilities in the following locations:
| Louisiana |
66 | |
| Tennessee |
36 | |
| Mississippi |
28 | |
| Kentucky |
27 | |
| Alabama |
20 | |
| Arkansas |
20 | |
| West Virginia |
16 | |
| Washington |
14 | |
| Texas |
12 | |
| Maryland |
11 | |
| Florida |
5 | |
| Georgia |
5 | |
| Missouri |
5 | |
| Oregon |
3 | |
| North Carolina |
2 | |
| Ohio |
2 | |
| Virginia |
4 | |
| Oklahoma |
1 | |
| 277 |
Our home office is located in Lafayette, Louisiana in 19,159 square feet of leased office space under a lease that commenced on March 1, 2004 and expires February 28, 2014. Our 264 owned home-based service locations are located in leased facilities. Generally, the leases for our home-based service locations have initial terms of one year, but range from one to five years. Most of the leases either contain multiple options to extend the lease period in one-year increments or convert to a month-to-month lease upon the expiration of the initial term. Seven of our LTACHs are hospitals within a hospital, meaning we have a lease or sublease for space with the host hospital, which are also our joint venture partners. Generally, our leases or subleases for LTACHs have initial terms of five years, but range from three to ten years. Most of our leases and subleases for our LTACHs contain multiple options to extend the term in one-year increments.
| Item 3. | Legal Proceedings. |
On July 13, 2009, the Company filed a Current Report on Form 8-K regarding an administrative subpoena from the Inspector General of the Office of Personnel Management (“OPM”). OPM is an administrative agency responsible for overseeing the Federal Employees Health Benefit Program (“FEHBP”). Although the subpoena was issued by OPM, the Company learned on July 9, 2009 that the scope of the review is not limited to the FEHBP and, also extends to services provided to Medicare beneficiaries. The focus of the review is on third-party quality improvement audits performed on the Company’s behalf by a third party consultant from 2005 to present. The Company will continue to cooperate and provide responsive information for the OPM review.
41
Table of Contents
On April 14, 2009, the Company filed a Current Report on Form 8-K regarding a qui tam lawsuit filed on March 20, 2009 in the Middle District Court of Tennessee entitled United States of America ex rel Sally Christine Summers v. LHC Group, Inc. which alleged a violation of the False Claims Act at a single agency. On June 11, 2009, the Company filed a Current Report on Form 8-K, reporting the district court’s order dismissing the case. The plaintiff is now appealing the court’s dismissal, and the Company continues to respond as necessary and appropriate.
| Item 4. | Reserved |
| Item 5. | Market for Registrant’s Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities. |
Sales of Unregistered Common Stock
None
Market Information and Holders
The Company’s common stock trades on the NASDAQ Global Select Market (“NASDAQ”) under the symbol “LHCG.” As of March 8, 2009, there were approximately 211 registered holders of record of the Company’s common stock.
Dividend Policy
The Company has not paid any dividends on its common stock since its initial public offering in 2005 and does not anticipate paying dividends in the foreseeable future. We currently intend to retain future earnings, if any, to support the development and growth of our business. Payment of future dividends, if any, will be at the discretion of our board of directors and subject to any requirements under our Credit Facility or any future credit facility.
Price Range of Common Stock
The following table provides the high and low prices of the Company’s Common Stock during 2009 and 2008 as quoted by NASDAQ.
| High | Low | |||||
| 2009 |
||||||
| Fourth Quarter |
$ | 34.74 | $ | 27.70 | ||
| Third Quarter |
32.01 | 21.15 | ||||
| Second Quarter |
28.54 | 20.25 | ||||
| First Quarter |
34.98 | 17.00 | ||||
| High | Low | |||||
| 2008 |
||||||
| Fourth Quarter |
$ | 36.83 | $ | 22.46 | ||
| Third Quarter |
31.42 | 21.50 | ||||
| Second Quarter |
23.64 | 13.55 | ||||
| First Quarter |
25.48 | 15.04 | ||||
The closing price of our common stock as reported by NASDAQ on March 8, 2010 was $31.85.
42
Table of Contents
Performance Graph
This item is incorporated by reference from our annual report to stockholders for the fiscal year ended December 31, 2009.
43
Table of Contents
| Item 6. | Selected Financial Data. |
The selected consolidated financial data presented below is derived from our audited consolidated financial statements included in this Annual Report on Form 10-K as of and for each of the years ended December 31, 2009, 2008 and 2007. The selected consolidated financial data presented below as of and for each of the years ended December 31, 2006 and 2005 is derived from our audited consolidated financial statements not included in this Annual Report on Form 10-K. The financial data for the years ended December 31, 2009, 2008 and 2007 should be read together with our Consolidated Financial Statements and related notes included in Part II, Item 8-Financial Statements and Supplementary Data and Item 7. Management’s Discussion and Analysis of Financial Condition and Consolidated Results of Operations included herein.
| Year Ended December 31, | ||||||||||||||||
| 2009 | 2008(2) | 2007(2) | 2006(2) | 2005(2) | ||||||||||||
| (In thousands except share and per share data) | ||||||||||||||||
| Consolidated Statements of Income Data: |
||||||||||||||||
| Net service revenue |
$ | 531,980 | $ | 382,591 | $ | 297,017 | $ | 217,418 | $ | 154,610 | ||||||
| Gross margin |
261,465 | 196,337 | 146,979 | 107,394 | 73,778 | |||||||||||
| Operating income |
85,046 | 60,492 | 38,781 | 35,521 | 22,544 | |||||||||||
| Income from continuing operations |
57,900 | 42,654 | 27,286 | 21,549 | 22,090 | |||||||||||
| Net Income attributable to LHC Group, Inc. |
43,841 | 30,202 | 19,589 | 20,594 | 10,103 | |||||||||||
| Change in the redemption value of redeemable noncontrolling interests |
45 | 31 | 193 | 1,163 | (1,476 | ) | ||||||||||
| Net income available to LHC Group, Inc.’s common stockholders |
$ | 43,886 | $ | 30,233 | $ | 19,782 | $ | 21,757 | $ | 8,626 | ||||||
| Net income attributable to LHC Group Inc., per basic share(1): |
$ | 2.44 | $ | 1.69 | $ | 1.11 | $ | 1.27 | $ | 0.59 | ||||||
| Net income attributable to LHC Group Inc., per diluted share(1): |
$ | 2.43 | $ | 1.69 | $ | 1.11 | $ | 1.27 | $ | 0.59 | ||||||
| Weighted average shares outstanding(1): |
||||||||||||||||
| Basic |
17,960,376 | 17,855,634 | 17,760,432 | 17,090,583 | 14,628,737 | |||||||||||
| Diluted |
18,069,897 | 17,899,087 | 17,827,444 | 17,104,650 | 14,684,639 | |||||||||||
| Cash dividends declared per common share |
— | — | — | — | $ | 0.009 | ||||||||||
| As of December 31, | |||||||||||||||
| 2009 | 2008 | 2007 | 2006 | 2005 | |||||||||||
| (In Thousands) | |||||||||||||||
| Consolidated Balance Sheet Data: |
|||||||||||||||
| Cash |
$ | 394 | $ | 3,511 | $ | 1,155 | $ | 26,877 | $ | 17,398 | |||||
| Total assets |
306,233 | 243,400 | 174,985 | 152,694 | 104,418 | ||||||||||
| Total debt |
11,802 | 5,116 | 3,431 | 3,837 | 5,427 | ||||||||||
| Total LHC Group, Inc. stockholders’ equity |
$ | 221,172 | $ | 176,821 | $ | 143,371 | $ | 121,889 | $ | 78,444 | |||||
| (1) | All references to shares and per share amounts have been retroactively restated to reflect our incorporation in the State of Delaware in 2005 and to give effect to a three-for-two stock split with respect to our common stock as if such events occurred as of the beginning of the earliest period presented. |
| (2) | Amounts have been restated to reflect the Company’s outpatient rehabilitation clinic, which was sold in September 2009, as discontinued operations. |
| Item 7. | Management’s Discussion and Analysis of Financial Condition and Results of Operations. |
The following discussion and analysis contains forward-looking statements about our future revenues, operating results, plans and expectations. Forward-looking statements are based on a number of assumptions and estimates that are inherently subject to significant risks and uncertainties and our results could differ materially from the results anticipated by our forward-looking statements as a result of many known or unknown factors, including, but not limited to, those factors discussed in Part I, Item 1A –, Risk Factors. Also, please read the “Cautionary Statements Regarding Forward-Looking Statements” set forth at the beginning of this Annual Report on Form 10-K.
44
Table of Contents
Please read the following discussion in conjunction with Part 1 of this Form 10-K as well as our Consolidated Financial Statements and the related notes contained elsewhere in this Annual Report on Form 10-K.
Overview
We provide post-acute health care services primarily to Medicare beneficiaries throughout the United States, through our home nursing agencies, hospices and LTACHs. Our net service revenue increased $149.4 million to $532.0 million for the year ending December 31, 2009 from $382.6 million for the period ending December 31, 2008. During 2009, we acquired 13 home nursing agencies, two hospice agencies and one LTACH. We also initiated the operations of 13 home health agencies. We currently operate 277 locations in the following 18 states: Louisiana, Mississippi, Arkansas, Alabama, Texas, Kentucky, Florida, Tennessee, Georgia, North Carolina, Virginia, West Virginia, Ohio, Missouri, Oklahoma, Maryland, Washington and Oregon.
Segments
We operate in two segments for financial reporting purposes: home-based services and facility-based services. We derived 88.2%, 85.2% and 82.2% of our net service revenue during the years ended December 31, 2009, 2008 and 2007, respectively, from our home-based services segment and derived the balance of our net service revenue from our facility-based services segment.
Through our home-based services segment we offer a wide range of services, including skilled nursing, private duty nursing, physical, occupational and speech therapy, medically-oriented social services and hospice care. As of December 31, 2009, the home-based services segment comprised the following locations:
| Type of Service |
||
| Home Health |
230 | |
| Hospice |
21 | |
| Diabetes Management Company |
2 | |
| Private Duty |
4 | |
| Specialty Services |
3 | |
| Management Companies |
4 | |
| 264 |
Of our 264 home-based services locations, 139 are wholly-owned by us, 113 are majority-owned or controlled by us through joint ventures, eight are controlled by us through license lease arrangements and the remaining four are management companies in which we have no ownership interest. We intend to increase the number of home nursing agencies that we operate through continued acquisitions and organic development. As we acquire and develop home nursing agencies, we anticipate the percentage of our net service revenue and operating income derived from our home-based services segment will continue to increase.
We provide facility-based services principally through our LTACHs. As of December 31, 2009, we owned and operated five LTACHs with eight locations, of which all but one are located within host hospitals. We also owned and operated a pharmacy, one medical equipment company, a health and fitness center and we manage the operations of one inpatient rehabilitation facility and one LTACH in which we have no ownership interest. Of these 13 facility-based services locations, four are wholly-owned by us and seven are majority-owned or controlled by us through joint ventures and two are managed companies.
Development Activities
The following table provides a summary of our acquisitions, divestitures and internal development activities from January 1, 2007 through December 31, 2009. This table does not include the six management services agreements under which we manage the operations of four home nursing agencies, one inpatient rehabilitation facility and one LTACH.
45
Table of Contents
| Home-Based Services | Facility-Based Services | ||||||||||||
| Home Nursing Agencies |
Hospice Agencies |
Specialty and Private Duty |
Long-Term Acute Care Hospitals, Critical Access Hospitals and Inpatient Rehabilitation Facilities |
Specialty and Outpatient Rehabilitation Clinics |
|||||||||
| Year |
|||||||||||||
| Total at January 1, 2007 |
100 | 6 | 3 | 8 | 4 | ||||||||
| Developed |
18 | — | — | — | — | ||||||||
| Acquired |
20 | 3 | — | — | — | ||||||||
| Divested/Closed |
(1 | ) | — | — | (1 | ) | — | ||||||
| Total at January 1, 2008 |
137 | 9 | 3 | 7 | 4 | ||||||||
| Developed |
19 | 1 | — | — | — | ||||||||
| Acquired |
50 | 9 | 6 | — | — | ||||||||
| Total at December 31, 2008 |
206 | 19 | 9 | 7 | 4 | ||||||||
| Developed |
13 | — | — | — | — | ||||||||
| Acquired |
13 | 2 | — | 1 | — | ||||||||
| Divested/Closed |
(2 | ) | — | — | — | (1 | ) | ||||||
| Total at December 31, 2009 |
230 | 21 | 9 | 8 | 3 | ||||||||
Recent Developments
Home-Based Services
Home Nursing. The base payment rate for Medicare home nursing in calendar year (“CY”) 2009 was $2,271.92 per 60-day episode. The standard federal rate is increased or decreased based on each Medicare patient’s case mix index which measures the severity of the patient’s condition. Since the inception of the prospective payment system in October 2000, the base episode rate payment has varied due to both the impact of annual market basket based increases and Medicare-related legislation. Home health payment rates are updated annually by either the full home health market basket percentage, or by the home health market basket percentage as adjusted by Congress. CMS establishes the home health market basket index, which measures inflation in the prices of an appropriate mix of goods and services included in home health services.
On October 30, 2009, CMS issued the CY 2010 final rule covering agency payment rates for home health services. The final rule provides for the following adjustments to the base rate: a 2.2% market basket increase, a 2.75% coding adjustment decrease, and a 2.5% increase resulting from a modification to the current outlier policy. The CY 2010 outlier policy caps outlier payments at 10% per agency and targets total aggregate outlier payments at 2.5% of total home health payments. The CY 2009 aggregate target was 5.0% and there was no per agency limit.
The combined effects of the market basket increase, the coding adjustment decrease and the modification of the outlier policy are estimated to increase payment to home nursing in CY 2010 by 1.8%. The base payment rate for Medicare home nursing in CY 2010 is $2,312.94 per 60-day episode.
The United States Congress is currently working on legislation as part of the healthcare reform that could impact the amounts that we are paid by Medicare for services provided to Medicare eligible patients. As of the date of this filing, the legislation has not been finalized and thus we cannot estimate the impact of such potential changes, if any.
Hospice. The following table shows the hospice Medicare payment rates for fiscal year (“FY”) 2009 which began on October 1, 2008 and ended September 30, 2009:
| Description |
Rate per patient day | ||
| Routine Home Care |
$ | 139.97 | |
| Continuous Home Care |
$ | 816.94 | |
| Inpatient Respite Care |
$ | 144.79 | |
| General Inpatient Care |
$ | 622.66 | |
46
Table of Contents
On August 6, 2009 CMS issued a final rule, effective October 1, 2009, to update the Medicare Hospice Wage Index for fiscal year FY 2010. This rule revises the phase-out of the hospice wage index budget neutrality adjustment factor (BNAF), which was finalized in the FY 2009 final rule, to now occur over 7 years. As a result of this final rule, the BNAF will be reduced by 10% in FY 2010, and 15 percent each year from FY 2011 through FY 2016. The combined effects of a 10% reduction to the BNAF in the FY 2010 Hospice Wage Index and a 2.1% hospital market basket update are estimated to increase payment to hospices in FY 2010 by 1.4%. In addition, this final rule requires hospice physicians to provide a short narrative as part of hospice certifications and recertifications of terminal illness. The final rule also set the FY 2009 hospice aggregate cap amount at $23, 014.50.
The following table shows the hospice Medicare payment rates for FY 2010:
| Description |
Rate per patient day | ||
| Routine Home Care |
$ | 142.91 | |
| Continuous Home Care |
$ | 834.10 | |
| Inpatient Respite Care |
$ | 147.83 | |
| General Inpatient Care |
$ | 635.74 | |
Facility-Based Services
LTACHs. The federal standard rate for 2009 LTACH-PPS rate year (“RY”) was $39,114 per Medicare discharge and the high cost outlier threshold was $22,960. The standard federal rate for LTACH-PPS is increased or decreased based on each Medicare patient’s case mix index, which measures the severity of the patient’s condition. The high cost outlier threshold is the limit that triggers additional high cost outlier payments to an LTACH.
On May 9, 2008, CMS published its annual payment rate update for RY 2009 (affecting discharges and cost reporting periods beginning on or after July 1, 2008). The May 2008 final rule adopted a 15-month rate update, from July 1, 2008 through September 30, 2009 and moved LTACH-PPS from a July-June update cycle to the same update cycle as the general acute care hospital inpatient rule, currently October to September. For RY 2009, the rule increased the Medicare base rate 2.7%, to $39,114.34 from $38,086.04. The rule also increased the fixed-loss amount for high cost outlier cases to $22,960, which is $2,222 higher than the RY 2008 LTACH-PPS. The final rule provided that CMS may make a one-time reduction in the LTACH-PPS rates to reflect a budget neutrality adjustment no earlier than December 29, 2010 and no later than October 1, 2012. CMS estimates this reduction will be approximately 3.75%.
On July 30, 2009, CMS published its final rule updating payments to LTACHs for RY 2010. The July final rule adopted a 2.5% inflation update which will apply to discharges and cost reporting periods beginning October 1, 2009 and, ending September 30, 2010.
The federal standard rate will be $39,896 per Medicare discharge and the high cost outlier threshold will be lowered from $22,960 to $18,425. These developments should have a small positive impact on reimbursement in RY 2010.
To recap, the standard federal rate uses a 2.0% update factor based on a market basket update of 2.5% less an adjustment of 0.5% to account for changes in documentation and coding.
2009 and 2008 Operational Data
The following table sets forth, for the period indicated, data regarding aggregate admissions and Medicare admissions to our home-based segment and patient days for our facility-based segment. Certain historical data has been included in order to present a more comparative analysis of the statistical data.
47
Table of Contents
| Three Months Ended March 31, 2009 |
Three Months Ended June 30, 2009 |
Three Months Ended September 30, 2009 |
Three Months Ended December 31, 2009 |
Year Ended December 31, 2009 | ||||||
| Home-Based Services Data: |
||||||||||
| Average census |
27,834 | 29,182 | 28,150 | 29,706 | 28,721 | |||||
| Average Medicare census |
22,363 | 23,592 | 22,486 | 23,512 | 22,994 | |||||
| Admissions |
18,104 | 19,779 | 21,485 | 21,798 | 81,166 | |||||
| Medicare admissions |
12,242 | 14,721 | 14,927 | 15,126 | 57,016 | |||||
| Facility-Based Services Data: |
||||||||||
| Patient days |
11,981 | 12,880 | 13,043 | 13,331 | 51,235 |
| Three Months Ended March 31, 2008 |
Three Months Ended June 30, 2008 |
Three Months Ended September 30, 2008 |
Three Months Ended December 31, 2008 |
Year Ended December 31, 2008 | ||||||
| Home-Based Services Data: |
||||||||||
| Average census |
18,958 | 20,469 | 21,733 | 24,675 | 21,519 | |||||
| Average Medicare census |
14,876 | 16,544 | 17,810 | 19,987 | 17,355 | |||||
| Admissions |
13,367 | 13,688 | 14,113 | 15,462 | 56,630 | |||||
| Medicare admissions |
9,774 | 10,053 | 10,482 | 11,402 | 41,711 | |||||
| Facility-Based Services Data: |
||||||||||
| Patient days |
12,034 | 11,298 | 10,930 | 11,928 | 46,190 |
Consolidated Results of Operations
The following table sets forth, for the periods indicated, net service revenue, cost of service revenue, general and administrative expenses, and operating income by segment (amounts in thousands). The table also includes data regarding total admissions and Medicare admissions for our home-based services segment and patient days for our facility-based services segment.
| Year Ended December 31, | |||||||||
| 2009 | 2008 | 2007 | |||||||
| Home-Based Services Data: |
|||||||||
| Net service revenue |
$ | 469,470 | $ | 326,041 | $ | 244,107 | |||
| Cost of service revenue |
234,131 | 154,376 | 116,962 | ||||||
| Gross margin |
235,339 | 171,665 | 127,145 | ||||||
| Provision for bad debts |
4,199 | 10,208 | 9,426 | ||||||
| General and administrative expenses |
155,670 | 109,917 | 80,595 | ||||||
| Operating income |
$ | 75,470 | $ | 51,540 | $ | 37,124 | |||
| Average census |
28,721 | 21,519 | 16,635 | ||||||
| Average Medicare census |
22,994 | 17,355 | 12,560 | ||||||
| Total admissions |
81,166 | 56,630 | 43,736 | ||||||
| Total Medicare admissions |
57,016 | 41,771 | 30,751 | ||||||
48
Table of Contents
| Year Ended December 31, | |||||||||
| 2009 | 2008 | 2007 | |||||||
| Facility-Based Services Data: |
|||||||||
| Net service revenue |
$ | 62,510 | $ | 56,550 | $ | 52,910 | |||
| Cost of service revenue |
36,384 | 31,878 | 33,076 | ||||||
| Gross margin |
26,126 | 24,672 | 19,834 | ||||||
| Provision for bad debts |
525 | 1,563 | 2,822 | ||||||
| General and administrative expenses |
16,025 | 14,157 | 15,355 | ||||||
| Operating income |
$ | 9,576 | $ | 8,952 | $ | 1,657 | |||
| Patient days |
51,235 | 46,190 | 45,818 | ||||||
The growth in home-based services in 2009 primarily relates to our acquisitions and development of de-novo locations during 2009. The relationship between the Company’s expenses and net service revenue provides a more comparative analysis of the financial information. The following table sets forth, for the periods indicated, certain items included in our consolidated statement of income as a percentage of our net service revenue:
| Year Ended December 31, | |||||||||
| 2009 | 2008 | 2007 | |||||||
| Net service revenue |
100.0 | % | 100.0 | % | 100.0 | % | |||
| Cost of service revenue |
50.9 | 48.7 | 50.5 | ||||||
| Gross margin |
49.1 | 51.3 | 49.5 | ||||||
| Provision for bad debts |
0.9 | 3.1 | 4.1 | ||||||
| General and administrative expenses |
32.3 | 32.4 | 32.3 | ||||||
| Operating income |
15.9 | 15.8 | 13.1 | ||||||
| Interest expense |
0.0 | (0.1 | ) | (0.1 | ) | ||||
| Non-operating income (loss), including gain on sales of entities and assets |
0.0 | 0.4 | 0.4 | ||||||
| Income tax expense |
5.0 | 4.9 | 4.1 | ||||||
| Noncontrolling interest expense |
2.6 | 3.1 | 1.8 | ||||||
| Income from continuing operations |
8.3 | % | 8.1 | % | 7.5 | % | |||
Year Ended December 31, 2009 Compared to Year Ended December 31, 2008
Net Service Revenue
Consolidated net service revenue for the year ended December 31, 2009 was $532.0 million, an increase of 39.0% or $149.4 million, from $382.6 million for the same period ending December 31, 2008. The growth in home-based services net service revenue contributed $143.4 million of the increase in consolidated net service revenue between 2009 and 2008. Net service revenue was comprised of the following for the periods ending December 31:
| 2009 | 2008 | |||||
| Home-based services |
88.2 | % | 85.2 | % | ||
| Facility-based services |
11.8 | 14.8 | ||||
| 100.0 | % | 100.0 | % | |||
Revenue derived from Medicare represented 81.7% and 83.2% of consolidated net service revenue for the years ended December 31, 2009 and 2008, respectively.
Home-Based Services. Net service revenue from home-based services for the year ended December 31, 2009 was $469.5 million, an increase of $143.5 million, or 44.0%, from $326.0 million for the year ended December 31, 2008. Total admissions increased 43.3% to 81,166 during the 2009, versus 56,630 for the same period in 2008. Average home-based patient census for the year ended December 31, 2009 increased 33.5% to 28,721 patients as compared with 21,519 patients for the year ended December 31, 2008.
49
Table of Contents
As detailed in the tables below, the increase in revenue in 2009 resulted from both organic growth and the growth from our acquisitions during the year ended December 31, 2009.
Organic growth includes growth in “same store” locations, or those locations owned for greater than 12 months, and growth from “de novo” locations. We calculate organic growth by dividing organic growth generated in a period by total revenue generated in the same period of the prior year. Revenue from acquired agencies contributes to organic growth beginning with the thirteenth month after acquisition.
The following tables detail the home-based services revenue growth and percentages for organic and total growth (amounts in thousands, except statistical data):
| Year Ending December 31, 2009 | |||||||||||||||||||||
| Same Store(1) | De Novo(2) | Organic(3) | Organic Growth% |
Acquired(4) | Total | Total Growth % |
|||||||||||||||
| Revenue |
$ | 413,017 | $ | 2,579 | $ | 415,596 | 27.5 | % | $ | 53,874 | $ | 469,470 | 44.0 | % | |||||||
| Revenue Medicare |
$ | 345,610 | $ | 2,245 | $ | 347,855 | 27.2 | % | $ | 40,307 | $ | 388,162 | 42.0 | % | |||||||
| Average Census |
24,357 | 496 | 24,853 | 15.5 | % | 3,868 | 28,721 | 33.5 | % | ||||||||||||
| Average Medicare Census |
19,924 | 426 | 20,350 | 17.3 | % | 2,644 | 22,994 | 32.5 | % | ||||||||||||
| Admissions |
65,666 | 647 | 66,313 | 17.1 | % | 14,853 | 81,166 | 43.3 | % | ||||||||||||
| Medicare Admissions |
46,947 | 488 | 47,435 | 13.7 | % | 9,581 | 57,016 | 36.7 | % | ||||||||||||
| Episodes |
144,247 | 1,583 | 145,830 | 24.2 | % | 13,395 | 159,225 | 35.6 | % | ||||||||||||
| (1) | Same store – location that has been in service with the Company for greater than 12 months. |
| (2) | De Novo – internally developed location that has been in service with the Company for 12 months or less. |
| (3) | Organic – combination of same store and de novo. |
| (4) | Acquired – purchased location that has been in service with the Company for 12 months or less. |
| Year Ending December 31, 2008 | |||||||||||||||||||||
| Same Store(1) |
De Novo(2) | Organic(3) | Organic Growth % |
Acquired(4) | Total | Total Growth % |
|||||||||||||||
| Revenue |
$ | 286,342 | $ | 2,879 | $ | 289,221 | 18.5 | % | $ | 36,820 | $ | 326,041 | 33.6 | % | |||||||
| Revenue Medicare |
$ | 239,627 | $ | 2,431 | $ | 242,058 | 21.9 | % | $ | 31,375 | $ | 273,433 | 37.7 | % | |||||||
| Average Census |
17,228 | 341 | 17,569 | 5.6 | % | 3,950 | 21,519 | 29.4 | % | ||||||||||||
| Average Medicare Census |
14,099 | 277 | 14,376 | 14.5 | % | 2,979 | 17,355 | 38.2 | % | ||||||||||||
| Admissions |
47,150 | 689 | 47,839 | 9.4 | % | 8,791 | 56,630 | 29.5 | % | ||||||||||||
| Medicare Admissions |
34,502 | 495 | 34,997 | 13.8 | % | 6,714 | 41,711 | 35.6 | % | ||||||||||||
| Episodes |
105,712 | 1,323 | 107,035 | 34.4 | % | 10,412 | 117,447 | 47.4 | % | ||||||||||||
| (1) | Same store – location that has been in service with the Company for greater than 12 months. |
| (2) | De Novo – internally developed location that has been in service with the Company for 12 months or less. |
| (3) | Organic – combination of same store and de novo. |
| (4) | Acquired – purchased location that has been in service with the Company for 12 months or less. |
Facility-Based Services. Net service revenue from facility-based services for the year ended December 31, 2009 was $62.5 million, an increase of $5.9 million, or 10.4%, compared with $56.6 million for the year ended December 31, 2008. The increase in net service revenue primarily relates to the additional revenue from our LTACH acquired in 2009.
Cost of Service Revenue
Our cost of service revenue consists of expenses incurred by our clinical and clerical personnel in our agencies and facilities. Cost of service revenue for the year ended December 31, 2009 was $270.5 million, an increase of
50
Table of Contents
$84.2 million, or 45.2%, from $186.3 million for the year ended December 31, 2008. Cost of service revenue represented approximately 50.9% and 48.7% of our net service revenue for the years ended December 31, 2009 and 2008, respectively.
Home-Based Services. Cost of service revenue from home-based services for the year ended December 31, 2009 was $234.1 million, an increase of $79.7 million, or 51.6%, from $154.4 million for the year ended December 31, 2008. The following table summarizes cost of service revenue (amounts in thousands).
| Year Ended December 31, | ||||||||||||
| 2009 | 2008 | |||||||||||
| Salaries, wages and benefits |
$ | 200,401 | 42.7 | %(1) | $ | 131,452 | 40.3 | %(1) | ||||
| Transportation, primarily mileage reimbursement |
16,441 | 3.5 | 11,803 | 3.6 | ||||||||
| Supplies and services |
17,289 | 3.7 | 11,121 | 3.4 | ||||||||
| Total |
$ | 234,131 | 49.9 | % | $ | 154,376 | 47.3 | % | ||||
| (1) | Percentage of Home-Based net service revenue |
The increase in salaries, wages and benefits as a percentage of net service revenue for the year ended December 31, 2009 compared to the same period in 2008 relates to an increase in visits per episode for both registered nurses and physical therapists.
Facility-Based Services. Cost of service revenue from facility-based services for the year ended December 31, 2009 was $36.4 million, an increase of $4.5 million, or 14.1%, from $31.9 million for the year ended December 31, 2008, as detailed in the following table (amounts in thousands).
| Year Ended December 31, | ||||||||||||
| 2009 | 2008 | |||||||||||
| Salaries, wages and benefits |
$ | 22,488 | 36.0 | %(1) | $ | 20,131 | 35.6 | %(1) | ||||
| Transportation |
150 | 0.2 | 260 | 0.5 | ||||||||
| Supplies and services |
13,746 | 22.0 | 11,487 | 20.3 | ||||||||
| Total |
$ | 36,384 | 58.2 | % | $ | 31,878 | 56.4 | % | ||||
| (1) | Percentage of Facility-Based net service revenue |
The increase in facility-based cost of service revenue relates primarily to the increase in supplies and services as a percentage of net service revenue. The increase in supplies and services relates to an increase in patient acuity throughout 2009 compared to 2008.
Provision for Bad Debts
Provision for bad debts for the year ended December 31, 2009 was $4.7 million compared to $11.8 million for the year ended December 31, 2008. For the years ended December 31, 2009 and 2008, the provision for bad debts was approximately 0.9% and 3.1% of net service revenue, respectively. Throughout 2009, we increased collection efforts, including those related to commercial claims, which increased cash collections and reduced overall receivables and days sales outstanding at year end and resulted in lower bad debt expense as a percentage of net service revenue.
General and Administrative Expenses
General and administrative expenses consist primarily of the following expenses incurred by our home office and administrative field personnel:
| • | Home office and field administration: |
| • | salaries and related benefits; |
| • | insurance; |
| • | costs associated with advertising and other marketing activities; and |
| • | rent and utilities. |
| • | Supplies and services: |
| • | accounting, legal and other professional services; and |
| • | office supplies. |
| • | Depreciation; |
51
Table of Contents
| • | Other: |
| • | advertising and marketing expenses; |
| • | recruitment; |
| • | operating locations rent; and |
| • | taxes. |
General and administrative expenses for the year ended December 31, 2009 were $171.7 million, an increase of $47.6 million, or 38.4%, from $124.1 million for the year ended December 31, 2008. General and administrative expenses represented approximately 32.3% and 32.4% of our net service revenue for the years ended December 31, 2009 and 2008, respectively.
Home-Based Services. General and administrative expenses from the home-based services for the year ended December 31, 2009 were $155.7 million, an increase of $45.8 million, or 41.7%, from $109.9 million for the year ended December 31, 2008. General and administrative expenses remained relatively consistent at 33.2% and 33.7% of our net service revenue during the years ended December 31, 2009 and 2008, respectively.
Facility-Based Services. General and administrative expenses from facility-based services for the year ended December 31, 2009 were $16.0 million, an increase of $1.8 million, or 12.7%, from $14.2 million for the year ended December 31, 2008. General and administrative expenses in the facility-based segment were 25.6% and 25.0% of net service revenue for the years ended December 31, 2009 and December 31, 2008, respectively.
Gain (loss) on the sale of assets and entities and Non-operating income
For the year ended December 31, 2009, we had a non-operating loss of $261,000 compared to non-operating income of $1.4 million for the year ended December 31, 2008. The loss during 2009 primarily relates to a $542,000 impairment expense on two provider numbers which were purchased in 2008. In February 2009, CMS denied the Company’s change of ownership for the provider numbers because the agency locations had been moved outside of the allowed service area. The Company has since received new provider numbers for these home health agencies. However, the purchased provider numbers no longer have value and were written off in 2009.
The non-operating income for the year ended December 31, 2008 primarily consists of a gain of $624,000 for the exchange of a minority ownership in two of the Company’s entities for a majority ownership in an acquired entity and a $315,000 gain on the sale of the Company’s aircraft.
Income Tax Expense
The effective tax rates for the years ended December 31, 2009 and 2008 were 37.8% of income from continuing operations attributable to LHC Group, Inc.
Net Income Attributable to Noncontrolling Interest
Net income attributable to noncontrolling interest was $14.0 million and $11.7 million for the years ended December 31, 2009 and 2008, respectively. Noncontrolling interest represented 2.6% and 3.1% of net service revenue for the years ended December 31, 2009 and 2008, respectively.
Discontinued Operations
The following table provides financial results of discontinued operations for the years ended December 31, 2009 and 2008 (amounts in thousands):
| 2009 | 2008 | |||||||
| Net service revenue |
$ | 402 | $ | 756 | ||||
| Costs of services and G&A expenses |
(543 | ) | (1,722 | ) | ||||
| Loss from discontinued operations before noncontrolling interest and income taxes |
(141 | ) | (966 | ) | ||||
| Income tax benefit |
55 | 190 | ||||||
| Loss from discontinued operations net of income tax benefit |
(86 | ) | (776 | ) | ||||
| Less loss from discontinued operations attributable to noncontrolling interest |
— | (123 | ) | |||||
| Loss from discontinued operations attributable to LHC Group Inc.’s common stockholders |
$ | (86 | ) | $ | (653 | ) | ||
52
Table of Contents
In September 2009, the Company sold its outpatient rehabilitation clinic and recognized a loss of $22,000. The results of operations related to the clinic and the loss are included in discontinued operations in the Company’s consolidated statements of income for the years ended December 31, 2009 and 2008.
Discontinued operations for the year ended December 31, 2008 also includes a home health pharmacy, which was closed on September 30, 2007 and a critical access hospital, which was sold on July 1, 2007. There is no activity related to these two locations for the year ended December 31, 2009.
Year Ended December 31, 2008 Compared to Year Ended December 31, 2007
Net Service Revenue
Net service revenue for the year ended December 31, 2008 was $382.6 million, an increase of $85.6 million or 28.8%, from $297.0 million for the same period ending December 31, 2007. The growth in the home-based services net service revenue contributed $81.9 million of the increase in consolidated net service revenue between December 31, 2008 and 2007. Net service revenue was comprised of the following for the periods ending December 31:
| 2008 | 2007 | |||||
| Home-based services |
85.2 | % | 82.2 | % | ||
| Facility-based services |
14.8 | 17.8 | ||||
| 100.0 | % | 100.0 | % | |||
Revenue derived from Medicare represented 83.2% and 81.7% of consolidated net service revenue for the years ended December 31, 2008 and 2007, respectively.
Home-Based Services. Net service revenue from home-based services for the year ended December 31, 2008 was $326.0 million, an increase of $81.9 million, or 33.6%, from $244.1 million for the year ended December 31, 2007. Total admissions increased 29.5% to 56,630 during 2008, versus 43,736 for the same period in 2007. Average home-based patient census for the year ended December 31, 2008 increased 29.4% to 21,519 patients as compared with 16,635 patients for the year ended December 31, 2007.
As detailed in the table below, the increase in revenue in 2008 is explained by both organic growth and the growth from our acquisitions during the year ended December 31, 2008.
53
Table of Contents
The following table details the home-based services revenue growth and percentages for organic and total growth (amounts in thousands, except statistical data):
| Year Ending December 31, 2008 | |||||||||||||||||||||
| Same Store(1) |
De Novo(2) | Organic(3) | Organic Growth % |
Acquired(4) | Total | Total Growth % |
|||||||||||||||
| Revenue |
$ | 286,342 | $ | 2,879 | $ | 289,221 | 18.5 | % | $ | 36,820 | $ | 326,041 | 33.6 | % | |||||||
| Revenue Medicare |
$ | 239,627 | $ | 2,431 | $ | 242,058 | 21.9 | % | $ | 31,375 | $ | 273,433 | 37.7 | % | |||||||
| Average Census |
17,228 | 341 | 17,569 | 5.6 | % | 3,950 | 21,519 | 29.4 | % | ||||||||||||
| Average Medicare Census |
14,099 | 277 | 14,376 | 14.5 | % | 2,979 | 17,355 | 38.2 | % | ||||||||||||
| Admissions |
47,150 | 689 | 47,839 | 9.4 | % | 8,791 | 56,630 | 29.5 | % | ||||||||||||
| Medicare Admissions |
34,502 | 495 | 34,997 | 13.8 | % | 6,714 | 41,711 | 35.6 | % | ||||||||||||
| Episodes |
105,712 | 1,323 | 107,035 | 34.4 | % | 10,412 | 117,447 | 47.4 | % | ||||||||||||
| (1) | Same store – location that has been in service with the Company for greater than 12 months. |
| (2) | De Novo – internally developed location that has been in service with the Company for 12 months or less. |
| (3) | Organic – combination of same store and de novo. |
| (4) | Acquired – purchased location that has been in service with the Company for 12 months or less. |
Facility-Based Services. Net service revenue from facility-based services for the year ended December 31, 2008 was $56.6 million, an increase of $3.7 million, or 7.0%, compared with $52.9 million for the year ended December 31, 2007. Organic growth made up the total growth in this service sector during 2008. The increase in net service revenue primarily relates to an increase in patient acuity throughout the year. Patient days increased to 46,190 in the year ended December 31, 2008, from 45,818 in the year ended December 31, 2007.
Cost of Service Revenue
Cost of service revenue for the year ended December 31, 2008 was $186.3 million, an increase of $36.3 million, or 24.2%, from $150.0 million for the year ended December 31, 2007. Cost of service revenue represented approximately 48.7% and 50.5% of our net service revenue for the years ended December 31, 2008 and 2007, respectively.
Home-Based Services. Cost of service revenue from home-based services for the year ended December 31, 2008 was $154.4 million, an increase of $37.4 million, or 32.0%, from $117.0 million for the year ended December 31, 2007. The following table summarizes cost of service revenue (amounts in thousands):
| Year Ended December 31, | ||||||||||||
| 2008 | 2007 | |||||||||||
| Salaries, wages and benefits |
$ | 131,452 | 40.3 | %(1) | $ | 99,446 | 40.7 | %(1) | ||||
| Transportation, primarily mileage reimbursement |
11,803 | 3.6 | 8,589 | 3.5 | ||||||||
| Supplies and services |
11,121 | 3.4 | 8,927 | 3.7 | ||||||||
| Total |
$ | 154,376 | 47.3 | % | $ | 116,962 | 47.9 | % | ||||
| (1) | Percentage of Home-Based net service revenue |
Facility-Based Services. Cost of service revenue from facility-based services for the year ended December 31, 2008 was $31.9 million, a decrease of $1.2 million, or 3.6%, from $33.1 million for the year ended December 31, 2007, as detailed in the following table (amounts in thousands);
| Year Ended December 31, | ||||||||||||
| 2008 | 2007 | |||||||||||
| Salaries, wages and benefits |
$ | 20,131 | 35.6 | %(1) | $ | 20,266 | 38.3 | %(1) | ||||
| Transportation |
260 | 0.5 | 325 | 0.6 | ||||||||
| Supplies and services |
11,487 | 20.3 | 12,485 | 23.6 | ||||||||
| Total |
$ | 31,878 | 56.4 | % | $ | 33,076 | 62.5 | % | ||||
| (1) | Percentage of Facility-Based net service revenue |
54
Table of Contents
The decrease in cost of facility-based service revenue as a percentage of facility-based net service revenue for the year ended December 31, 2008 relates primarily to a decrease in salary, wages and benefits as a percentage of net service revenue. The decrease is the result of cost management at the facilities and increased acuity of the patients receiving treatment, resulting in higher net service revenue without increased patient days. Additionally during 2008, management renegotiated several contracts with its major suppliers. As a result of the renegotiations, the Company saw reductions in the dollar amount of cost of supplies and as a percentage of net service revenue, throughout the year.
Provision for Bad Debts
Provision for bad debts for the year ended December 31, 2008 was $11.8 million compared to $12.2 million for the year ended December 31, 2007. For the years ended December 31, 2008 and 2007, the provision for bad debts was approximately 3.1% and 4.1% of net service revenue, respectively. In the fourth quarter of 2007, we increased bad debt expense by $3.9 million to reflect collection difficulties, primarily with commercial claims. Prior to that increase, we had been recording bad debt expense of approximately 2.9% of net service revenue. During 2008, we increased collection efforts, including those related to commercial claims, increased cash collections and reduced overall receivables and days sales outstanding at year end, which resulted in lower bad debt expense as a percentage of net service revenue.
General and Administrative Expenses
General and administrative expenses for the year ended December 31, 2008 were $124.1 million, an increase of $28.1 million, or 29.3%, from $96.0 million for the year ended December 31, 2007. General and administrative expenses represented approximately 32.4% and 32.3% of our net service revenue for the years ended December 31, 2008 and 2007, respectively.
Home-Based Services. General and administrative expenses from home-based services for the year ended December 31, 2008 were $109.9 million, an increase of $29.3 million, or 36.4%, from $80.6 million for the year ended December 31, 2007. General and administrative expenses were 33.7% and 33.0% of our net service revenue during the year ended December 31, 2008 and 2007, respectively. This increase as a percentage of net service revenue was in part caused by higher general and administrative expenses in agencies acquired in 2008. In addition, investment in our billing and collections department and growth and development in other departments which support the Company’s growth increased these costs throughout 2008.
Facility-Based Services. General and administrative expenses from the facility-based services for the year ended December 31, 2008 were $14.2 million, a decrease of $1.2 million, or 7.8%, from $15.4 million for the year ended December 31, 2007.
General and administrative expenses in the facility-based segment for the year ended December 31, 2008 represented 25.0% of our net service revenue compared to 29.0% during the year ended December 31, 2007.
Gain (loss) on the sale of assets and entities and Non-operating income
Non-operating income for the year ended December 31, 2008 was $1.4 million compared to $1.1 million for the year ended December 31, 2007. During 2008, the Company recorded a gain of $624,000 for the exchange of a minority ownership in two of the Company’s entities for a majority ownership in an acquired entity. Also, during 2008, the Company recognized a gain of $315,000 related to the sale of the Company’s aircraft.
Income Tax Expense
The effective tax rates for the years ended December 31, 2008 and 2007 were 37.8% and 35.7%, of income from continuing operations attributable to LHC Group, Inc., respectively. The increase is related to the effect of higher state tax rates and the related mix of taxable income in those states and a lower credit in 2008 related to the Gulf Opportunity Act.
Net Income Attributable to Noncontrolling Interest
Net income attributable to noncontrolling interest was $11.7 million for the year ended December 31, 2008, or 3.1% of net service revenue, an increase of $6.4 million, compared to $5.3 million, or 1.8% of net service revenue
55
Table of Contents
for the year ended December 31, 2007. Between June 30, 2007 and December 31, 2007, the Company entered into seven joint venture agreements. These joint ventures contributed to noncontrolling interest expense for a 12 month period ending December 31, 2008 versus only a few months of the preceding year. Further, during 2008, the Company entered into 13 additional joint venture agreements. These new joint venture acquisitions contributed $3.7 million to the increase in noncontrolling interest for the year ended December 31, 2008. The remaining increase relates to the increase in income from operations related to all of our joint ventures.
Discontinued Operations
The following table provides financial results of discontinued operations for the years ended December 31, 2008 and 2007 (amounts in thousands):
| 2008 | 2007 | |||||||
| Net service revenue |
$ | 756 | $ | 3,994 | ||||
| Costs of services and G&A expenses |
(1,722 | ) | (6,699 | ) | ||||
| Loss from discontinued operations before noncontrolling interest and income taxes |
(966 | ) | (2,705 | ) | ||||
| Income tax benefit |
190 | 289 | ||||||
| Loss from discontinued operations net of income tax benefit |
(776 | ) | (2,416 | ) | ||||
| Less loss from discontinued operations attributable to noncontrolling interest |
(123 | ) | (672 | ) | ||||
| Loss from discontinued operations attributable to LHC Group Inc.’s common stockholders |
$ | (653 | ) | $ | (1,744 | ) | ||
In September 2009, the Company sold its outpatient rehabilitation clinic and recognized a loss of $22,000. The results of operations related to the clinic and the loss are included in discontinued operations in the Company’s consolidated statements of income for the years ended December 31, 2008 and 2007.
Discontinued operations for the year ended December 31, 2008 and 2007 also include a home health pharmacy, which was closed on September 30, 2007, and a critical access hospital, which was sold on July 1, 2007.
Liquidity and Capital Resources
Cash at December 31, 2009 decreased by $3.1 million, to $394,000 from $3.5 million at December 31, 2008. Based on our current plan of operations, including acquisitions, we believe this amount, when combined with expected cash flows from operations and amounts available under our revolving line of credit, will be sufficient to fund our growth strategy to meet our anticipated operating expenses, capital expenditures and debt service obligations for at least the next 12 months.
Liquidity
Our principal source of liquidity for our operating activities is the collection of our accounts receivable, most of which are collected from governmental and third-party commercial payors. Our reported cash flows from operating activities are impacted by various external and internal factors, including the following:
| • | Operating Results — Our net income has a significant impact on our operating cash flows. Any significant increase or decrease in our net income could have a material impact on our operating cash flows. |
| • | Timing of Acquisitions — We use our operating cash flows to purchase home health and hospice agencies. When the acquisitions occur at or near the end of a period, our cash outflows significantly increase. |
| • | Start-Up Costs — Following the completion of an acquisition, we suspend billing Medicare and Medicaid claims until we receive the change of ownership and electronic funds transfer approvals. We also generally incur substantial start-up costs in order to implement our business strategy. There is generally a delay between our expenditure start-up costs and the increase in net service revenue and subsequent cash collections, which adversely affects our cash flows from operating activities. |
56
Table of Contents
| • | Timing of Payroll — Our employees are paid bi-weekly on Fridays; therefore, operating cash flows decline in reporting periods that end on a Friday. Conversely, for those reporting periods ending on a day other than Friday, our cash flows are higher because we have not yet paid our payroll. |
| • | Medical Insurance Plan Funding — We are self-funded for medical insurance purposes. Any significant changes in the amount of insurance claims submitted could have a direct impact on our operating cash flows. |
| • | Medical Supplies — A significant expense associated with our business is the cost of medical supplies. Any increase in the cost of medical supplies, or in the use of medical supplies by our patients, could have a material impact on our operating cash flows. |
Cash used in investing activities is primarily for acquisitions of home nursing and hospice agencies, while cash used by financing activities relates to payments on outstanding debt agreements and payments to our noncontrolling interest partners.
The following table summarizes changes in cash flows (amounts in thousands):
| Year Ended December 31, |
||||||||
| 2009 | 2008 | |||||||
| Cash provided by operating activities |
$ | 49,192 | $ | 85,504 | ||||
| Cash used in investing activities |
(41,663 | ) | (75,876 | ) | ||||
| Cash used in financing activities |
(10,646 | ) | (7,272 | ) | ||||
| Change in cash |
(3,117 | ) | 2,356 | |||||
| Cash and cash equivalents at beginning of period |
3,511 | 1,155 | ||||||
| Cash and cash equivalents at end of period |
$ | 394 | $ | 3,511 | ||||
Operating activities during the year ended December 31, 2009 provided $49.2 million in cash compared to $85.5 million for year ended December 31, 2008. Net income provided $57.8 million of operating cash flow in 2009. At December 31, 2009, working capital was $48.4 million compared to $32.1 million at December 31, 2008, an increase of $16.3 million. The decrease in cash provided by operating activities and the change in working capital in 2009 primarily relates to tax payments. As a result of Hurricanes Ike and Gustav, estimated 2008 federal tax payments, as well as those for most states, including Louisiana, were deferred until January 2009. The Company paid $8.5 million on January 3, 2009 related to these deferred payments which reduced operating cash flows in 2009.
Investing activities used $41.7 million and $75.9 million in cash for the years ended December 31, 2009 and 2008, respectively. Cash outflows for the year ending December 31, 2009 included $33.4 million for acquisitions, compared to $69.9 million for acquisitions for the year ending December 31, 2008.
Financing activities used $10.6 million and $7.3 million in cash in the years ended December 31, 2009 and 2008, respectively. During 2008, noncontrolling interest distributions increased $4.6 million. This increase was offset by the $5.7 million outstanding on the line of credit as of December 31, 2009.
Days sales outstanding (“DSO”) for the year ended December 31, 2009 was 48 days compared to 51 days for the same period in 2008.
Indebtedness
Our total long-term indebtedness was $10.2 million at December 31, 2009 and $5.1 million at December 31, 2008, including the current portions of $415,000 and $583,000, respectively. At December 31, 2009, long-term debt included $5.7 million outstanding on the revolving line of credit.
57
Table of Contents
Credit Facility
The Company’s Credit Facility with Capital One, National Association, which was amended on June 15, 2009, provides for a maximum aggregate principal borrowing of $75.0 million. The Credit Facility, which is scheduled to expire on June 15, 2011, is unsecured and has a letter of credit sublimit of $2.5 million. In September 2009, the company issued a $700,000 letter of credit as collateral on the Company’s workers’ compensation insurance. The annual facility fee is 0.25% of the total availability. The interest rate for borrowings under the Credit Facility is a function of the prime rate (Base Rate) subject to a floor or the Eurodollar rate (Eurodollar) subject to a floor, as elected by the Company, plus the applicable margin based on the Leverage Ratio as defined in the Credit Facility. At December 31, 2009, $5.7 million and the letter of credit were outstanding under the Credit Facility. At December 31, 2008, no amounts were outstanding under the Credit Facility.
The interest rate for borrowings under the Credit Facility is a function of the prime rate (Base Rate) or the Eurodollar rate (Eurodollar), as elected by the Company, plus the applicable margin as set forth below:
| Leverage Ration | Eurodollar Margin |
Base Rate Margin |
||||
| < 1.00:1.00 |
2.25 | % | 0.50 | % | ||
| ³ 1.00:1.00 < 1.50:100 |
2.50 | % | 0.75 | % | ||
| ³ 1.50:1.00 < 2.00:1.00 |
2.75 | % | 1.00 | % | ||
| ³ 2.00:1.00 |
3.00 | % | 1.25 | % |
The Company’s Credit Facility contains customary affirmative, negative and financial covenants. For example, the Company is restricted in incurring additional debt, disposing of assets, making investments, allowing fundamental changes to the Company’s business or organization, and making certain payments in respect of stock or other ownership interests, such as dividends and stock repurchases. Under the Credit Facility, the Company is also required to meet certain financial covenants with respect to minimum fixed charge coverage, consolidated net worth, leverage and minimum asset coverage ratios. At December 31, 2009, the Company was in compliance with all covenants and we expect to be in compliance with all covenants throughout 2010.
The Company’s Credit Facility also contains customary events of default, including bankruptcy and other insolvency events, cross-defaults to other debt agreements, a change in control involving the Company or any subsidiary guarantor, and the failure to comply with certain covenants.
Long-Term Debt
On February 28, 2008, the Company paid its promissory note with Bancorp Equipment Finance, Inc. in full. The note was collateralized by the Company’s previous aircraft, which was sold in February 2008 for $3.1 million. The sale resulted in a gain of $315,000.
In February 2008, the Company entered into a loan agreement with Capital One for a term note in the amount of $5.1 million for the purchase of a 1999 Cessna 560 aircraft. The aircraft serves as collateral for the term note, which is payable in 83 monthly installments of principal plus interest commencing on March 6, 2008 followed by one balloon installment of $2.7 million on February 6, 2015. The term note bears interest at the LIBOR rate (adjusted monthly) plus the Applicable Margin (as defined in the term note) of 1.9% (2.14% at December 31, 2009).
58
Table of Contents
Commitments
The following table discloses aggregate information about our contractual obligations and the periods in which payments are due as of December 31, 2009:
| Payment due by period | |||||||||||||||
| Contractual Cash Obligation |
Total | Less Than 1 Year |
1-3 Years | 3-5 Years | More Than 5 Years | ||||||||||
| (In thousands) | |||||||||||||||
| Long-term debt |
$ | 4,483 | $ | 387 | $ | 1,010 | $ | 1,010 | $ | 2,076 | |||||
| Capital lease obligations |
45 | 28 | 17 | — | — | ||||||||||
| Operating leases |
29,380 | 11,062 | 15,925 | 2,120 | 273 | ||||||||||
| Total contractual cash obligations |
$ | 33,908 | $ | 11,477 | $ | 16,952 | $ | 3,130 | $ | 2,349 | |||||
Off-Balance Sheet Arrangements
We do not currently have any off-balance sheet arrangements with unconsolidated entities, financial partnerships or entities often referred to as structured finance or special purpose entities, which would have been established for the purpose of facilitating off-balance sheet arrangements or other contractually narrow or limited purposes. In addition, we do not engage in trading activities involving non-exchange traded contracts. As such, we are not materially exposed to any financing, liquidity, market or credit risk that could arise if we had engaged in these relationships.
The following discussions describe our critical accounting policies, which we believe require the most significant judgments and estimates used in the preparation of our consolidated financial statements.
Critical Accounting Policies
The preparation of financial statements in conformity with U.S. generally accepted accounting principles requires management to make estimates and assumptions that affect the reported amounts of assets and liabilities and disclosure of contingent assets and liabilities at the date of the financial statements and the reported revenue and expenses during the reported period. Actual results could differ from those estimates. Changes in the accounting estimates are reasonably likely to occur from period to period. Accordingly, actual results could differ materially from our estimates. To the extent that there are material differences between these estimates and actual results, our financial condition or results of operations will be affected. We base our estimates on past experience and other assumptions that we believe are reasonable under the circumstances and we evaluate these estimates on an ongoing basis.
The following discussions describe our critical accounting policies, which we believe require the most significant judgments and estimates used in the preparation of our consolidated financial statements.
Principles of Consolidation
The consolidated financial statements include all subsidiaries and entities controlled by the Company. We define control as ownership of a majority of the voting interest of an entity. The consolidated financial statements include entities in which the Company has the obligation to absorb losses of the entities or the right to receive benefits from the entities and has voting control over the entities or both, as a result of ownership, contractual or other financial interests in the entities.
The following table summarizes the percentage of net service revenue earned by type of ownership or relationship the Company had with the operating entity:
| 2009 | 2008 | 2007 | |||||||
| Equity joint ventures |
51.4 | % | 49.6 | % | 43.7 | % | |||
| Wholly owned subsidiaries |
44.6 | 46.6 | 46.4 | ||||||
| License leasing arrangements |
2.5 | 2.1 | 7.8 | ||||||
| Management services |
1.5 | 1.7 | 2.1 | ||||||
| 100.0 | % | 100.0 | % | 100.0 | % | ||||
59
Table of Contents
The change in the percentage of revenue earned by license leasing arrangements and the equity joint ventures relates, in part, to the conversion of one of the Company’s license leasing arrangements to a joint venture on October 1, 2007.
All significant inter-company accounts and transactions have been eliminated in consolidation. Business combinations accounted for as purchases have been included in the consolidated financial statements from the respective dates of acquisition.
The following describes the Company’s consolidation policy with respect to its various ventures excluding wholly owned subsidiaries:
Equity Joint Ventures
The Company’s joint ventures are structured as limited liability companies in which the Company typically owns a majority equity interest ranging from 51% to 99%. Each member of all but one of the Company’s equity joint ventures participates in profits and losses in proportion to their equity interests. The Company has one joint venture partner whose participation in losses is limited. The Company consolidates these entities as the Company has the obligation to absorb losses of the entities and the right to receive benefits from the entities and has voting control over the entities.
License Leasing Arrangements
The Company, through wholly owned subsidiaries, leases home health licenses necessary to operate certain of its home nursing agencies. As with wholly owned subsidiaries, the Company owns 100% of the equity of these entities and consolidates them based on such ownership, as well as the Company’s obligation to absorb losses of the entities and the right to receive benefits from the entities.
Management Services
The Company has various management services agreements under which the Company manages certain operations of agencies and facilities. The Company does not consolidate these agencies or facilities, as the Company does not have an ownership interest and does not have an obligation to absorb losses of the entities or the right to receive the benefits from the entities.
Revenue Recognition
The Company reports net service revenue at the estimated net realizable amount due from Medicare, Medicaid, commercial insurance, managed care payors, patients and others for services rendered. All payors contribute to both the home-based services and facility-based services.
The following table sets forth the percentage of net service revenue earned by category of payor for the years ending December 31:
| 2009 | 2008 | 2007 | |||||||
| Payor: |
|||||||||
| Medicare |
81.7 | % | 83.2 | % | 81.7 | % | |||
| Medicaid |
3.5 | 4.6 | 5.5 | ||||||
| Other |
14.8 | 12.2 | 12.8 | ||||||
| 100.0 | % | 100.0 | % | 100.0 | % | ||||
60
Table of Contents
The percentage of net service revenue contributed from each reporting segment was as follows for the years ending December 31:
| 2009 | 2008 | 2007 | |||||||
| Home-based services |
88.2 | % | 85.2 | % | 82.2 | % | |||
| Facility-based services |
11.8 | 14.8 | 17.8 | ||||||
| 100.0 | % | 100.0 | % | 100.0 | % | ||||
Medicare
Home-Based Services
Home Nursing Services. The Company’s home nursing Medicare patients are classified into one of 153 home health resource groups prior to receiving services. Based on this home health resource group, the Company is entitled to receive a standard prospective Medicare payment for delivering care over a 60-day period referred to as an episode. The Company recognizes revenue based on the number of days elapsed during an episode of care within the reporting period.
Final payments from Medicare may reflect one of four retroactive adjustments to ensure the adequacy and effectiveness of the total reimbursement: (a) an outlier payment if the patient’s care was unusually costly; (b) a low utilization adjustment if the number of visits totaled fewer than five; (c) a partial payment if the patient transferred to another provider before completing the episode; or (d) a payment adjustment based upon the level of therapy services required in the population base. Management estimates the impact of these payment adjustments based on historical experience and records this estimate during the period the services are rendered. The Company’s payment is also adjusted for differences in local prices using the hospital wage index. In calculating the Company’s reported net service revenue from home nursing services, the Company adjusts the prospective Medicare payments by an estimate of the adjustments. The adjustments are calculated using a historical average of prior adjustments.
Hospice Services. The Company is paid by Medicare under a per diem payment system. The Company receives one of four predetermined daily or hourly rates based upon the level of care the Company furnished. The Company records net service revenue from hospice services based on the daily or hourly rate and recognizes revenue as hospice services are provided.
Hospice payments are also subject to two caps. One relates to individual programs receiving more than 20% of its total Medicare reimbursement from inpatient care services and the second relates to individual programs receiving reimbursements in excess of a “cap amount” calculated by multiplying the number of beneficiaries during the period by a statutory amount indexed for inflation. The determination for each cap is made annually based on the 12-month period ending on October 31 of each year. This limit is computed on a program-by-program basis. We have not received notification that any of our hospices have exceeded the cap on inpatient care services during 2009. None of the Company’s hospices exceeded either cap during the years ended December 31, 2008, or 2007.
Facility-Based Services
Long-Term Acute Care Services. The Company is reimbursed by Medicare for services provided under the LTACH prospective payment system, which was implemented on October 1, 2002. Each patient is assigned a long-term care diagnosis-related group. The Company is paid a predetermined fixed amount applicable to that particular group. This payment is intended to reflect the average cost of treating a Medicare patient classified in that particular long-term care diagnosis-related group. For selected patients, the amount may be further adjusted based on length of stay and facility-specific costs, as well as in instances where a patient is discharged and subsequently readmitted, among other factors. The Company calculates the adjustment based on a historical average of these types of adjustments for claims paid. Similar to other Medicare prospective payment systems, the rate is also adjusted for geographic wage differences. Revenue is recognized as services are provided for the Company’s LTACHs.
Medicaid, managed care and other payors
The Company’s Medicaid reimbursement is based on a predetermined fee schedule applied to each service provided. Therefore, revenue is recognized for Medicaid services as services are provided based on this fee
61
Table of Contents
schedule. The Company’s managed care payors reimburse the Company in a manner similar to either Medicare or Medicaid. Accordingly, the Company recognizes revenue from managed care payors in the same manner as the Company recognizes revenue from Medicare or Medicaid.
Management Services
The Company records management services revenue as services are provided in accordance with the various management services agreements to which the Company is a party. As described in the agreements, the Company provides billing, management and other consulting services suited to and designed for the efficient operation of the applicable home nursing agency or inpatient rehabilitation facility. The Company is responsible for the costs associated with the locations and personnel required for the provision of services. The Company is compensated based on a percentage of cash collections, a flat fee or is reimbursed for operating expenses and compensated based on a percentage of operating net income.
Accounts Receivable and Allowances for Uncollectible Accounts
The Company reports accounts receivable net of estimated allowances for uncollectible accounts and adjustments. Accounts receivable are uncollateralized and primarily consist of amounts due from third-party payors and patients. To provide for accounts receivable that could become uncollectible in the future, the Company establishes an allowance for uncollectible accounts to reduce the carrying amount of such receivables to their estimated net realizable value. The credit risk for other concentrations of receivables is limited due to the significance of Medicare as the primary payor. The Company does not believe that there are any other significant concentrations of receivables from any particular payor that would subject it to any significant credit risk in the collection of accounts receivable.
The amount of the provision for bad debts is based upon the Company’s assessment of historical and expected net collections, business and economic conditions, trends in government reimbursement and other collection indicators. Uncollectible accounts are written off when the Company has determined the account will not be collected.
A portion of the estimated Medicare prospective payment system reimbursement from each submitted home nursing episode is received in the form of a request for accelerated payment (“RAP”). The Company submits a RAP for 60% of the estimated reimbursement for the initial episode at the start of care. The full amount of the episode is billed after the episode has been completed. The RAP received for that particular episode is deducted from the final payment. If a final bill is not submitted within the greater of 120 days from the start of the episode, or 60 days from the date the RAP was paid, any RAPs received for that episode will be recouped by Medicare from any other Medicare claims in process for that particular provider. The RAP and final claim must then be resubmitted. For subsequent episodes of care contiguous with the first episode for a particular patient, the Company submits a RAP for 50% instead of 60% of the estimated reimbursement. The remaining 50% reimbursement is requested upon completion of the episode. The Company has earned net service revenue in excess of billings rendered to Medicare.
Our Medicare population is paid at a prospectively set amount that can be determined at the time services are rendered. Our Medicaid reimbursement is based on a predetermined fee schedule applied to each individual service we provide. Our managed care contracts are structured similar to either the Medicare or Medicaid payment methodologies. Because of our payor mix, we are able to calculate our actual amount due at the patient level and adjust the gross charges down to the actual amount at the time of billing. This negates the need for an estimated contractual allowance to be booked at the time we report net service revenue for each reporting period.
At December 31, 2009, our allowance for uncollectible accounts, as a percentage of patient accounts receivable, was approximately 10.1%, or $8.3 million, compared to 14.0%, or $10.0 million, at December 31, 2008.
62
Table of Contents
The following table sets forth, as of December 31, 2009, the aging of accounts receivable (based on the billing date) and the total allowance for uncollectible accounts, expressed as a percentage of the related aged accounts receivable (amounts in thousands):
| Payor |
0-90 | 91-180 | 180-365 | Over 365 | Total | |||||||||||||||
| Medicare |
$ | 40,228 | $ | 9,404 | $ | 6,853 | $ | 1,238 | $ | 57,723 | ||||||||||
| Medicaid |
2,861 | 767 | 942 | 163 | 4,733 | |||||||||||||||
| Other |
14,121 | 3,162 | 2,150 | 24 | 19,457 | |||||||||||||||
| Total |
$ | 57,210 | $ | 13,333 | $ | 9,945 | $ | 1,425 | $ | 81,913 | ||||||||||
| Allowance as a percentage of receivables |
3.4 | % | 9.9 | % | 27.0 | % | 97.2 | % | 10.1 | % | ||||||||||
For home-based services, we calculate the allowance for uncollectible accounts as a percentage of total patient receivables. The percentage changes depending on the payor and increases as the patient receivables age. For facility-based services, we calculate the allowance for uncollectible accounts based on a claim by claim review. As a result, the allowance percentages presented in the table above vary between the aging categories because of the mix of claims in each category.
The following table sets forth as of December 31, 2008, the aging of accounts receivable (based on the billing date) and the total allowance for uncollectible accounts expressed as a percentage of the related aged accounts receivable (amounts in thousands):
| Payor |
0-90 | 91-180 | 180-365 | Over 365 | Total | |||||||||||||||
| Medicare |
$ | 41,772 | $ | 6,806 | $ | 2,678 | $ | 1,305 | $ | 52,561 | ||||||||||
| Medicaid |
2,807 | 1,081 | 1,108 | 946 | 5,942 | |||||||||||||||
| Other |
7,656 | 3,239 | 1,219 | 883 | 12,997 | |||||||||||||||
| Total |
$ | 52,235 | $ | 11,126 | $ | 5,005 | $ | 3,134 | $ | 71,500 | ||||||||||
| Allowance as a percentage of receivables |
6.9 | % | 15.8 | % | 33.0 | % | 94.3 | % | 14.0 | % | ||||||||||
The following table summarizes the activity and ending balances in the allowance for uncollectible accounts (amounts in thousands):
| Beginning of Year Balance |
Additions and Expenses |
Deductions | End of Year Balance | |||||||||
| Year ended December 31: |
||||||||||||
| 2009 |
$ | 9,976 | $ | 4,724 | $ | 6,438 | $ | 8,262 | ||||
| 2008 |
8,953 | 12,463 | 11,440 | 9,976 | ||||||||
| 2007 |
5,769 | 13,817 | 10,633 | 8,953 | ||||||||
Goodwill and Intangible Assets
Goodwill and other intangible assets with indefinite lives are reviewed annually for impairment or more frequently if circumstances indicate impairment may have occurred. If the carrying value of goodwill or an indefinite-lived intangible asset exceeds its fair value, an impairment loss is recognized. The evaluation of impairment involves comparing the current fair value of each of the Company’s reporting units to their recorded value, including goodwill. Components of the Company’s home-based segment are generally represented by individual subsidiaries or joint ventures with individual licenses to conduct specific operations within geographic markets as limited by the terms of each license. Components of the Company’s facility-based services are represented by individual operating entities. Management aggregates the components of these two segments into two reporting units for purposes of evaluating impairment.
63
Table of Contents
The Company estimates the fair value of its identified reporting units using the discounted cash flow method and the market multiple analysis method. These valuations require management to make estimates and assumptions regarding industry economic factors and the profitability of future business strategies. Management considers historical experience and all available information at the time the fair values of its reporting units are estimated. For each of the reporting units, the estimated fair value is determined based on a formula that considers 50% of the estimated value based on a multiple of earnings before interest, taxes, depreciation and amortization plus 50% of the estimated value using recent sales of comparable facilities. A change in the weight assigned to each methodology would not have changed the conclusion that no impairment charge is necessary during the year ending December 31, 2009. The Company has not recognized goodwill impairment charges in 2009, 2008 or 2007.
Included in intangible assets, net are definite-lived assets subject to amortization such as software licenses and non-compete agreements. Amortization of the definite-lived intangible assets is calculated on a straight-line basis over the estimated useful lives of the related assets. Software licenses are amortized over a three year period and non-compete agreements are amortized over the life of the agreement, usually ranging from three to five years.
The Company also has indefinite-lived assets that are not subject to amortization expense such as trade names and certificates of need. The Company has concluded that trade names and certificates of need have indefinite lives, as management has determined that there are no legal, regulatory, contractual, economic or other factors that would limit the useful life of these intangible assets and the Company intends to renew and operate the licenses and use these trade names indefinitely. The Company performs an annual impairment test on the trade names using the relief-from royalty method. Under this method, the fair value of the intangible asset is determined by calculating the present value of the after-tax cost savings associated with owning the trade names and therefore not having to pay royalties for its use for the remainder of its estimated useful lives. The certificates of need are tested annually for impairment using the cost approach. Under this method, assumptions are made about the cost to replace the certificates of need.
In 2008, the Company purchased two home health agency provider numbers in Ohio for $542,000 and obtained approval from the State of Ohio to move the provider numbers to a new service area. In February 2009, the CMS denied the Company’s change of ownership for the provider numbers because the agency locations were moved outside of the allowed service area. Although the Company has re-applied for and received the new provider numbers for these home health agencies, the purchased provider numbers no longer have value. Therefore, the Company recognized a $542,000 impairment expense on the Home-Health segment in other non-operating (loss) income on the Company’s Condensed Consolidated Statements of Income for the year ended December 31, 2009.
Adoption of New Accounting Standards
In June 2009, the Financial Accounting Standards Board (the “FASB”) issued authoritative guidance that replaced the previous hierarchy of GAAP and established the FASB Codification as the single source of authoritative U.S. GAAP recognized by the FASB to be applied by nongovernmental entities. Its primary purpose is to improve clarity and use of existing standards by grouping authoritative literature under common topics. The FASB will no longer issue new standards in the form of Statements, FASB Staff Positions or Emerging Issues Task Force Abstracts. Instead, it will issue Accounting Standards Updates which will serve to update the Codification, provide background information about the guidance and provide the basis for conclusions on the changes to the Codification. The Codification is effective for financial statements issued for interim and annual periods ending after September 15, 2009. The Codification does not change or alter existing GAAP and did not have a material effect on the Company’s condensed financial condition, results of operations, or cash flows.
In April 2009, the FASB issued authoritative guidance requiring publicly-traded entities to disclose in the body or in the accompanying notes of its summarized financial information for interim reporting periods and in its financial statements for annual reporting periods, the fair value of all financial instruments for which it is practicable to estimate that value, whether recognized or not recognized in the statement of financial position, as required by other authoritative guidance. The guidance is effective for interim and annual reporting periods ending after June 15, 2009. The adoption of the new disclosure requirements did not have a material effect on the Company’s condensed financial condition, results of operations, or cash flows.
In May 2009, the FASB issued authoritative guidance establishing general standards of accounting for and disclosing subsequent events that occur after the balance sheet date but before financial statements are issued or are available to be issued. In particular, the guidance sets forth the period after the balance sheet date during which management of the Company should evaluate events or transactions that may occur for potential recognition or disclosure in the financial statements, the circumstances under which the Company should recognize events or transactions occurring after the balance sheet date in its financial statements, and the disclosures that the Company
64
Table of Contents
should make about events or transactions that occurred after the balance sheet date. Because the guidance only introduces the concept of financial statements being available to be issued, the adoption of this guidance did not result in significant changes in the subsequent events that the Company reports, either through recognition or disclosure, in its consolidated financial statements.
On January 1, 2009, the Company prospectively adopted the FASB’s guidance on business combinations. The authoritative guidance changes the accounting treatment and disclosure for certain specific items in a business combination. According to the guidance, an acquiring entity is required to recognize all the assets acquired and liabilities assumed in a transaction at the acquisition-date fair value with limited exceptions. This includes the fair values of the noncontrolling interest acquired. Under previous guidance, the noncontrolling interest (minority interest) was recorded at the minority owner’s historical balance. Contingent consideration arrangements are also now measured and recorded at fair value at the acquisition date. Under previous guidance contingent consideration was not recognized until paid or settled. Other changes include the treatment of acquisition-related costs, which, with the exception of debt or equity issuance costs, are to be recognized as an expense in the period that the costs are incurred and the services are received. The Company capitalized acquisition-related costs under previous guidance. Further, any adjustments during the measurement period to the provisional amounts recognized as part of the purchase price allocation are treated retrospectively as of the acquisition date.
In April 2009, the FASB further issued an update on accounting for assets acquired and liabilities assumed in a business combination that arise from contingencies. The update addresses application issues on initial recognition and measurement, subsequent measurement and accounting, and disclosure of assets and liabilities arising from contingencies in a business combination. The update required that all contractual contingencies and all noncontractual contingencies that are more likely than not to give rise to an asset or liability be recognized at their acquisition date fair value. All noncontractual contingencies that do not meet the more-likely-than not criterion as of the acquisition date would be accounted for in accordance with other U.S. GAAP. The guidance requires that when new information is obtained, a liability be measured at the higher of its acquisition-date fair value and the amount that would be recognized under other authoritative guidance. Further, an acquirer shall recognize at fair value, at the acquisition date, an asset acquired or a liability assumed in a business combination that arises from a contingency if the acquisition-date fair value of that asset or liability can be determined during the measurement period. The Company has adopted the provisions of this guidance effective January 1, 2009.
The Company also adopted the FASB’s guidance on noncontrolling interests in consolidated financial statements on January 1, 2009. The guidance establishes new accounting and reporting standards for the noncontrolling interest, previously known as minority interest. Noncontrolling interest in consolidated subsidiaries is presented in the consolidated balance sheet within stockholders’ equity as a separate component from the parent’s equity. Consolidated net income includes earnings attributable to both the parent and the noncontrolling interest. Earnings per share, which is not affected by the guidance, is based on earnings attributable only to the parent company. The guidance explains the accounting for changes in the parent’s ownership interest in a subsidiary, including transactions where control is retained and where control is relinquished. The guidance requires additional disclosure information related to amounts attributable to the parent for income from continuing operations, discontinued operations and extraordinary items and reconciliations of the parent and noncontrolling interests’ equity in subsidiaries.
| Item 7A. | Quantitative and Qualitative Disclosures about Market Risk. |
As of December 31, 2009, we had $394,000 in cash. Cash in excess of requirements are deposited in highly liquid money market instruments with maturities less than 90 days. Because of the short maturities of these instruments, we would not expect our operating results or cash flows to be materially affected by the effect of a sudden change in market interest rates on our portfolio. At times, the Company’s cash in banks exceeds the Federal Insurance Deposit Corporation (“FDIC”) insurance limit. The Company has not experienced any loss as a result of those deposits and does not expect any in the future.
Our exposure to market risk relates to changes in interest rates for borrowings under the Credit Facility we entered into in February 2008 and amended on June 19, 2009. A hypothetical 100 basis point increase in interest rates on the average daily amounts outstanding under the Credit Facility would have increased interest expense by $10,000 for the year ended December 31, 2009.
65
Table of Contents
| Item 8. | Financial Statements and Supplementary Data. |
The consolidated financial statements and financial statement schedules in Part IV, Item 15 of this Annual Report on Form 10-K are incorporated by reference into this Item 8.
| Item 9. | Changes In and Disagreements with Accountants on Accounting and Financial Disclosure. |
On August 20, 2008, the Audit Committee of the Company’s Board of Directors dismissed Ernst & Young LLP (“Ernst & Young”) as our independent registered public accounting firm. The reports of Ernst & Young on the financial statements of the Company for the past two fiscal years contained no adverse opinion or disclaimer of opinion and were not qualified or modified as to uncertainty, audit scope or accounting principles.
During our two most recent fiscal years and subsequent interim period through August 20, 2008, there were no disagreements with Ernst & Young on any matter of accounting principles or practices, financial statement disclosure, or auditing scope or procedure, which disagreements if not resolved to the satisfaction of Ernst & Young would have caused it to make reference to the subject matter of such disagreements in their reports on the financial statements for such years.
| Item 9A. | Controls and Procedures. |
Evaluation of Disclosure Control and Procedures
The Company maintains disclosure controls and procedures that are designed to ensure that information required to be disclosed by the company in the reports it files or submits under the Exchange Act of 1934 is recorded, processed, summarized and reported within the time periods specified in the SEC’s rules and forms, and that such information is accumulated and communicated to the Company’s management, including its Chief Executive Officer and Chief Financial Officer, as appropriate to allow timely decisions regarding required disclosure.
Under the supervision and with the participation of the Company’s management, including its Chief Executive Officer and Chief Financial Officer, management evaluated the effectiveness of the Company’s disclosure controls and procedures as of December 31, 2009. Based on that evaluation, the Company’s Chief Executive Officer and its Chief Financial Officer concluded that the Company’s disclosure controls and procedures (as such term is defined under Rule 13a-15(e) promulgated under the Securities Exchange Act of 1934, as amended) were effective as of December 31, 2009.
Management’s Report on Internal Control Over Financial Reporting
The Company’s management is responsible for establishing and maintaining adequate internal control over financial reporting, as that term is defined in Exchange Act Rule 13a-15(f). Under the supervision and with the participation of the Company’s management, including the Chief Executive Officer and Chief Financial Officer, the Company conducted an evaluation of its internal control over financial reporting based on the framework in Internal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission. Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
Based on management’s testing and evaluation under the framework in Internal Control-Integrated Framework, management concluded that our internal control over financial reporting was effective as of December 31, 2009.
The attestation report of KPMG, the independent registered public accounting firm, is included herein.
Changes in Internal Control Over Financial Reporting
There have not been any changes in the Company’s internal control over financial reporting, as such term is defined in Rule 13a-15(f) under the Exchange Act, during the Company’s fiscal quarter ended December 31, 2009 that have materially affected, or are reasonably likely to materially affect, the Company’s internal control over financial reporting.
66
Table of Contents
Report of Independent Registered Public Accounting Firm
The Board of Directors and Stockholders
LHC Group, Inc.
We have audited LHC Group, Inc.’s internal control over financial reporting as of December 31, 2009, based on criteria established in Internal Control – Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (COSO). LHC Group, Inc.’s (the Company) management is responsible for maintaining effective internal control over financial reporting and for its assessment of the effectiveness of internal control over financial reporting, included in the accompanying Management’s Report on Internal Control over Financial Reporting. Our responsibility is to express an opinion on the Company’s internal control over financial reporting based on our audit.
We conducted our audit in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether effective internal control over financial reporting was maintained in all material respects. Our audit included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, and testing and evaluating the design and operating effectiveness of internal control based on the assessed risk. Our audit also included performing such other procedures as we considered necessary in the circumstances. We believe that our audit provides a reasonable basis for our opinion.
A company’s internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with U.S. generally accepted accounting principles. A company’s internal control over financial reporting includes those policies and procedures that (1) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with U.S. generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company’s assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
In our opinion, LHC Group, Inc. maintained, in all material respects, effective internal control over financial reporting as of December 31, 2009, based on criteria established in Internal Control – Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States), the consolidated balance sheet of LHC Group, Inc. and subsidiaries as of December 31, 2009, and the related consolidated statements of income, changes in equity, and cash flows for the year then ended, and our report dated March 15, 2010 expressed an unqualified opinion on those consolidated financial statements.
| /s/ KPMG LLP |
| Baton Rouge, Louisiana March 15, 2010 |
67
Table of Contents
| Item 9B. | Other Information. |
None.
| Item 10. | Directors, Executive Officers and Corporate Governance. |
The information required by this Item with respect to directors and executive officers is incorporated by reference from the information contained under the headings “Directors and Executive Officers” and “Corporate Governance” in our definitive Proxy Statement relating to the Company’s 2010 Annual Meeting of Stockholders.
The information required by this Item regarding compliance with Section 16(a) of the Exchange Act is incorporated by reference from the section entitled “Directors and Executive Officers” in the definitive Proxy Statement relating to the Company’s 2010 Annual Meeting of Stockholders.
The information required by this Item with respect to corporate governance is incorporated by reference from the information contained under the heading “The Board of Directors and Corporate Governance” in the definitive Proxy Statement for the Company’s 2010 Annual Meeting of Stockholders.
Code of Conduct and Ethics
We have adopted a code of ethics that applies to all of our directors, officers and employees. This code is publicly available in the investor relations area of our website at www.lhcgroup.com. This code of ethics is not incorporated in this report by reference. Copies of our code of ethics may also be requested in print by writing to Investor Relations at LHC Group, Inc., 420 West Pinhook Road, Suite A, Lafayette, Louisiana, 70503.
| Item 11. | Executive Compensation. |
The information required by this Item is incorporated by reference from the section entitled “Executive Compensation” in the definitive Proxy Statement relating to the Company’s 2010 Annual Meeting of Stockholders.
| Item 12. | Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters. |
The information required by this Item is incorporated by reference to the sections entitled “Security Ownership of Certain Beneficial Owners and Management” in the definitive Proxy Statement relating to the Company’s 2010 Annual Meeting of Stockholders.
Equity Compensation Plan Information
| (a) | (b) | (c) | |||||
| Plan Category |
Number of Shares to be Issued Upon Exercise of Outstanding Options, Warrants, and Rights |
Weighted-Average Exercise Price of Outstanding Price of Outstanding Rights |
Number of Shares Remaining Available for Future Issuance Under Equity Compensation Plans (Excluding Securities Reflected in Column (a)) | ||||
| Equity compensation plans approved by Stockholders: |
19,000 | $ | 17.20 | 415,723 | |||
| Equity compensation plans not approved by Stockholders: |
— | — | — | ||||
| Total |
19,000 | $ | 17.20 | 415,723 | |||
68
Table of Contents
| Item 13. | Certain Relationships and Related Transactions, and Director Independence. |
The information required by this Item is incorporated by reference from the section entitled “Certain Relationships and Related Transactions” in the definitive Proxy Statement relating to the Company’s 2010 Annual Meeting of Stockholders.
| Item 14. | Principal Accounting Fees and Services. |
The information required by this Item is incorporated by reference from the section entitled “Principal Accounting Fees and Services” in the definitive Proxy Statement relating to the Company’s 2010 Annual Meeting of Stockholders.
69
Table of Contents
| Item 15. | Exhibits, Financial Statement Schedules. |
(a) Documents to be filed with Form 10-K:
(1) Financial Statements
| F-1 | ||
| Consolidated Balance Sheets as of December 31, 2009 and 2008 |
F-3 | |
| For each of the three years in the period ended December 31, 2009, 2008 and 2007 |
||
| F-4 | ||
| F-5 | ||
| F-6 | ||
| F-7 |
(2) Financial Statement Schedules
There are no financial statement schedules included in this report.
(3) Exhibits
The Exhibits are listed in the Index of Exhibits required by Item 601 of Regulation S-K included herewith, which is incorporated by reference
Table of Contents
Report of Independent Registered Public Accounting Firm
The Board of Directors and Stockholders
LHC Group, Inc.:
We have audited the accompanying consolidated balance sheets of LHC Group, Inc. and subsidiaries (the Company) as of December 31, 2009 and 2008, and the related consolidated statements of income, changes in equity, and cash flows for the years then ended. These consolidated financial statements are the responsibility of the Company’s management. Our responsibility is to express an opinion on these consolidated financial statements based on our audits.
We conducted our audits in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement. An audit includes examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements. An audit also includes assessing the accounting principles used and significant estimates made by management, as well as evaluating the overall financial statement presentation. We believe that our audits provide a reasonable basis for our opinion.
In our opinion, the consolidated financial statements referred to above present fairly, in all material respects, the financial position of LHC Group, Inc. and subsidiaries as of December 31, 2009 and 2008, and the results of their operations and their cash flows for the years then ended, in conformity with U.S. generally accepted accounting principles.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States), LHC Group, Inc.’s internal control over financial reporting as of December 31, 2009, based on criteria established in Internal Control – Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (COSO), and our report dated March 15, 2010 expressed an unqualified opinion on the effectiveness of the LHC Group, Inc.’s internal control over financial reporting.
/s/ KPMG LLP
Baton Rouge, Louisiana
March 15, 2010
F-1
Table of Contents
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
The Board of Directors and Stockholders
LHC Group, Inc. and subsidiaries
We have audited the accompanying consolidated statements of income, changes in equity, and cash flows of LHC Group, Inc. and subsidiaries (the Company) for the year ended December 31, 2007. These financial statements are the responsibility of the Company’s management. Our responsibility is to express an opinion on these financial statements based on our audit.
We conducted our audits in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement. An audit includes examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements. An audit also includes assessing the accounting principles used and significant estimates made by management, as well as evaluating the overall financial statement presentation. We believe that our audits provide a reasonable basis for our opinion.
In our opinion, the financial statements referred to above present fairly, in all material respects, the consolidated results of operations and cash flows of LHC Group, Inc. and subsidiaries for the year ended December 31, 2007, in conformity with U.S. generally accepted accounting principles.
As discussed in Note 2 to the consolidated financial statements, effective January 1, 2007 the Company adopted FASB Interpretation No. 48, Accounting for Uncertainty in Income Taxes — an Interpretation of FASB Statement No. 109 .
/s/ Ernst & Young LLP
New Orleans, Louisiana
March 14, 2008,
except for Notes 2 and 3, as to which the date is
March 15, 2010
F-2
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
CONSOLIDATED BALANCE SHEETS
(Amounts in thousands, except share data)
| As of December 31, | ||||||||
| 2009 | 2008 | |||||||
| ASSETS | ||||||||
| Current assets: |
||||||||
| Cash |
$ | 394 | $ | 3,511 | ||||
| Receivables: |
||||||||
| Patient accounts receivable, less allowance for uncollectible accounts of $8,262 and $9,976, respectively |
73,651 | 61,524 | ||||||
| Other receivables |
3,850 | 2,317 | ||||||
| Amounts due from governmental entities |
1,184 | 2,434 | ||||||
| Total receivables, net |
78,685 | 66,275 | ||||||
| Deferred income taxes |
4,370 | 4,959 | ||||||
| Prepaid income taxes |
3,131 | — | ||||||
| Prepaid expenses and other current assets |
8,798 | 6,464 | ||||||
| Total current assets |
95,378 | 81,209 | ||||||
| Property, building and equipment, net |
21,361 | 16,348 | ||||||
| Goodwill |
139,474 | 112,572 | ||||||
| Intangible assets, net |
46,851 | 29,975 | ||||||
| Other assets |
3,169 | 3,296 | ||||||
| Total assets |
$ | 306,233 | $ | 243,400 | ||||
| LIABILITIES AND STOCKHOLDERS’ EQUITY | ||||||||
| Current liabilities: |
||||||||
| Accounts payable and other accrued liabilities |
$ | 20,873 | $ | 15,497 | ||||
| Salaries, wages and benefits payable |
22,521 | 16,400 | ||||||
| Amounts due to governmental entities |
3,208 | 6,023 | ||||||
| Income taxes payable |
— | 10,682 | ||||||
| Current portion of long-term debt |
387 | 508 | ||||||
| Total current liabilities |
46,989 | 49,110 | ||||||
| Deferred income taxes |
12,475 | 5,718 | ||||||
| Revolving Credit Facility |
5,723 | — | ||||||
| Long-term debt, less current portion |
4,096 | 4,483 | ||||||
| Other long-term obligations |
1,567 | 145 | ||||||
| Noncontrolling interest-redeemable |
13,823 | 6,682 | ||||||
| Stockholders’ equity: |
||||||||
| Common stock — $0.01 par value: 40,000,000 shares authorized; 20,967,418 and 20,853,463 shares issued and 17,990,685 and 17,895,832 shares outstanding, respectively |
179 | 179 | ||||||
| Treasury stock — 2,976,733 and 2,957,631 shares at cost, respectively |
(3,513 | ) | (3,072 | ) | ||||
| Additional paid-in capital |
86,310 | 85,404 | ||||||
| Retained earnings |
138,196 | 94,310 | ||||||
| Total LHC Group, Inc. stockholders’ equity |
221,172 | 176,821 | ||||||
| Noncontrolling interest—non-redeemable |
388 | 441 | ||||||
| Total equity |
221,560 | 177,262 | ||||||
| Total liabilities and stockholders’ equity |
$ | 306,233 | $ | 243,400 | ||||
See accompanying Notes to the Consolidated Financial Statements
F-3
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF INCOME
(Amounts in thousands, except share and per share data)
| For the Year Ended of December 31, | ||||||||||||
| 2009 | 2008 | 2007 | ||||||||||
| Net service revenue |
$ | 531,980 | $ | 382,591 | $ | 297,017 | ||||||
| Cost of service revenue |
270,515 | 186,254 | 150,038 | |||||||||
| Gross margin |
261,465 | 196,337 | 146,979 | |||||||||
| Provision for bad debts |
4,724 | 11,771 | 12,248 | |||||||||
| General and administrative expenses |
171,695 | 124,074 | 95,950 | |||||||||
| Operating income |
85,046 | 60,492 | 38,781 | |||||||||
| Interest expense |
(142 | ) | (458 | ) | (357 | ) | ||||||
| Gain (loss) on the sale of assets and entities |
(22 | ) | 967 | (108 | ) | |||||||
| Non-operating (loss) income |
(239 | ) | 461 | 1,167 | ||||||||
| Income from continuing operations before income taxes and noncontrolling interest |
84,643 | 61,462 | 39,483 | |||||||||
| Income tax expense |
26,743 | 18,808 | 12,197 | |||||||||
| Income from continuing operations |
57,900 | 42,654 | 27,286 | |||||||||
| Loss from discontinued operations (net of income tax benefit of $55, $190 and $289, respectively) |
(86 | ) | (776 | ) | (2,416 | ) | ||||||
| Gain on sale of discontinued operations (net of income taxes of $20) |
— | — | 31 | |||||||||
| Net income |
57,814 | 41,878 | 24,901 | |||||||||
| Less net income attributable to noncontrolling interest |
13,973 | 11,676 | 5,312 | |||||||||
| Net income attributable to LHC Group, Inc. |
43,841 | 30,202 | 19,589 | |||||||||
| Redeemable noncontrolling interests |
45 | 31 | 193 | |||||||||
| Net income available to LHC Group, Inc.’s common stockholders |
$ | 43,886 | $ | 30,233 | $ | 19,782 | ||||||
| Earnings per share — basic: |
||||||||||||
| Income from continuing operations attributable to LHC Group, Inc. |
$ | 2.44 | $ | 1.73 | $ | 1.24 | ||||||
| Loss from discontinued operations attributable to LHC Group, Inc. |
— | (0.04 | ) | (0.14 | ) | |||||||
| Net income attributable to LHC Group, Inc. |
2.44 | 1.69 | 1.10 | |||||||||
| Redeemable noncontrolling interest |
— | — | 0.01 | |||||||||
| Net income attributable to LHC Group, Inc.’s common stockholders |
$ | 2.44 | $ | 1.69 | $ | 1.11 | ||||||
| Earnings per share — diluted: |
||||||||||||
| Income from continuing operations attributable to LHC Group, Inc. |
$ | 2.43 | $ | 1.73 | $ | 1.23 | ||||||
| Loss from discontinued operations attributable to LHC Group, Inc. |
— | (0.04 | ) | (0.13 | ) | |||||||
| Net income attributable to LHC Group, Inc. |
2.43 | 1.69 | 1.10 | |||||||||
| Redeemable noncontrolling interest |
— | — | 0.01 | |||||||||
| Net income attributable to LHC Group, Inc.’s common stockholders |
$ | 2.43 | $ | 1.69 | $ | 1.11 | ||||||
| Weighted average shares outstanding: |
||||||||||||
| Basic |
17,960,376 | 17,855,634 | 17,760,432 | |||||||||
| Diluted |
18,069,897 | 17,899,087 | 17,827,444 | |||||||||
See accompanying Notes to the Consolidated Financial Statements
F-4
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF CHANGES IN EQUITY
(Amounts in thousands, except share data)
| LHC Group, Inc. | ||||||||||||||||||||||||||||||||
| Common Stock | Non- | |||||||||||||||||||||||||||||||
| Issued | Treasury | Additional | Noncontrolling | Controlling | ||||||||||||||||||||||||||||
| Paid-In | Retained | Interest - Non- | Interest - | |||||||||||||||||||||||||||||
| Amount | Shares | Amount | Shares | Capital | Earnings | redeemable | Total Equity | Redeemable | Net Income | |||||||||||||||||||||||
| Balance at December 31, 2006 |
$ | 177 | 20,682,317 | $ | (2,856 | ) | 2,950,059 | $ | 80,273 | $ | 44,295 | $ | 387 | $ | 122,276 | 3,243 | ||||||||||||||||
| Net income |
— | — | — | — | — | 19,589 | 1,131 | 20,720 | 4,181 | 24,901 | ||||||||||||||||||||||
| Noncontrolling interest distributions |
— | — | — | — | — | — | (1,045 | ) | (1,045 | ) | (4,509 | ) | ||||||||||||||||||||
| Exercise of stock options |
— | 527 | — | — | — | — | — | — | — | |||||||||||||||||||||||
| Nonvested stock compensation |
— | — | — | — | 1,125 | — | — | 1,125 | — | |||||||||||||||||||||||
| Issuance of vested restricted stock |
— | 25,976 | — | — | 62 | — | — | 62 | — | |||||||||||||||||||||||
| Treasury shares redeemed to pay income tax |
— | — | (10 | ) | 370 | — | — | — | (10 | ) | — | |||||||||||||||||||||
| Excess tax benefit—vesting of nonvested stock |
— | — | — | — | 104 | — | — | 104 | — | |||||||||||||||||||||||
| Issuance of common stock under Employee Stock Purchase Plan |
— | 16,893 | — | — | 419 | — | — | 419 | — | |||||||||||||||||||||||
| Recording noncontrolling interest in joint venture at redemption value |
— | — | — | — | — | 193 | — | 193 | — | |||||||||||||||||||||||
| Balances at December 31, 2007 |
$ | 177 | 20,725,713 | $ | (2,866 | ) | 2,950,429 | $ | 81,983 | $ | 64,077 | $ | 473 | $ | 143,844 | $ | 2,915 | |||||||||||||||
| Net income |
— | — | — | — | — | 30,202 | 1,463 | 31,665 | 10,213 | 41,878 | ||||||||||||||||||||||
| Noncontrolling interest distributions |
— | — | — | — | — | — | (1,495 | ) | (1,495 | ) | (8,307 | ) | ||||||||||||||||||||
| Purchase of additional noncontrolling interest |
— | — | — | — | — | — | — | — | 1,861 | |||||||||||||||||||||||
| Issuance of common stock to joint venture partners in exchange for a portion of their minority ownership |
1 | 51,736 | — | — | 1,033 | — | — | 1,034 | — | |||||||||||||||||||||||
| Nonvested stock compensation |
— | — | — | — | 1,935 | — | — | 1,935 | — | |||||||||||||||||||||||
| Issuance of vested restricted stock |
— | 53,026 | — | — | — | — | — | — | — | |||||||||||||||||||||||
| Treasury shares redeemed to pay income tax |
— | — | (206 | ) | 7,202 | — | — | — | (206 | ) | — | |||||||||||||||||||||
| Tax shortfall from issuance of vesting stock |
— | — | — | — | (39 | ) | — | — | (39 | ) | — | |||||||||||||||||||||
| Issuance of common stock under Employee Stock Purchase Plan |
1 | 22,988 | — | — | 492 | — | — | 493 | — | |||||||||||||||||||||||
| Recording noncontrolling interest in joint venture at redemption value |
— | — | — | — | — | 31 | — | 31 | — | |||||||||||||||||||||||
| Balances at December 31, 2008 |
$ | 179 | 20,853,463 | $ | (3,072 | ) | 2,957,631 | $ | 85,404 | $ | 94,310 | $ | 441 | $ | 177,262 | $ | 6,682 | |||||||||||||||
| Net income |
— | — | — | — | — | 43,841 | 1,554 | 45,395 | 12,419 | 57,814 | ||||||||||||||||||||||
| Transfer of noncontrolling interest |
— | — | — | — | 181 | — | — | 181 | 1,228 | |||||||||||||||||||||||
| Purchase of additional controlling interest |
— | — | — | — | (2,286 | ) | — | — | (2,286 | ) | — | |||||||||||||||||||||
| Acquired noncontrolling interest |
— | — | — | — | — | — | — | — | 5,858 | |||||||||||||||||||||||
| Noncontrolling interest distributions |
— | — | — | — | — | — | (1,607 | ) | (1,607 | ) | (12,364 | ) | ||||||||||||||||||||
| Nonvested stock compensation |
— | — | — | — | 2,393 | — | — | 2,393 | — | |||||||||||||||||||||||
| Issuance of vested restricted stock |
— | 89,163 | — | — | — | — | — | — | — | |||||||||||||||||||||||
| Treasury shares redeemed to pay income tax |
— | — | (441 | ) | 19,102 | — | — | — | (441 | ) | — | |||||||||||||||||||||
| Issuance of common stock under Employee Stock Purchase Plan |
— | 24,792 | — | — | 618 | — | — | 618 | — | |||||||||||||||||||||||
| Recording noncontrolling interest in joint venture at redemption value |
— | — | — | — | — | 45 | — | 45 | — | |||||||||||||||||||||||
| Balances at December 31, 2009 |
$ | 179 | 20,967,418 | $ | (3,513 | ) | 2,976,733 | $ | 86,310 | $ | 138,196 | $ | 388 | $ | 221,560 | $ | 13,823 | |||||||||||||||
See accompanying Notes to the Consolidated Financial Statements
F-5
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF CASH FLOWS
(Amounts in thousands)
| For the Year Ended December 31, | ||||||||||||
| 2009 | 2008 | 2007 | ||||||||||
| Operating activities |
||||||||||||
| Net income |
$ | 57,814 | $ | 41,878 | $ | 24,901 | ||||||
| Adjustments to reconcile net income to net cash provided by operating activities: |
||||||||||||
| Depreciation and amortization expense |
4,831 | 3,740 | 3,026 | |||||||||
| Provision for bad debts |
4,724 | 12,463 | 13,817 | |||||||||
| Stock based compensation expense |
2,393 | 1,935 | 1,187 | |||||||||
| Deferred income taxes |
4,646 | 462 | 129 | |||||||||
| Loss on impairment of intangible assets |
542 | — | — | |||||||||
| Gain on sale of assets and partial sale of entity |
— | (967 | ) | — | ||||||||
| Changes in operating assets and liabilities, net of acquisitions: |
||||||||||||
| Receivables |
(17,896 | ) | (597 | ) | (31,109 | ) | ||||||
| Prepaid expenses, other assets |
(4,747 | ) | 4,155 | (1,446 | ) | |||||||
| Accounts payable and accrued expenses |
(1,550 | ) | 20,549 | 1,570 | ||||||||
| Net amounts due from governmental entities |
(1,565 | ) | 1,886 | (61 | ) | |||||||
| Net cash provided by operating activities |
49,192 | 85,504 | 12,014 | |||||||||
| Investing activities |
||||||||||||
| Cash paid for acquisitions, primarily goodwill, intangible assets and advance payment on acquisitions |
(33,427 | ) | (69,898 | ) | (28,935 | ) | ||||||
| Purchases of property, building and equipment |
(8,236 | ) | (8,550 | ) | (3,346 | ) | ||||||
| Proceeds from sale of property and equipment |
— | 3,094 | — | |||||||||
| Purchase of certificate of deposit |
— | (522 | ) | — | ||||||||
| Net cash used in investing activities |
(41,663 | ) | (75,876 | ) | (32,281 | ) | ||||||
| Financing activities |
||||||||||||
| Proceeds from line of credit |
69,206 | 32,850 | — | |||||||||
| Payments on line of credit |
(63,483 | ) | (32,850 | ) | — | |||||||
| Proceeds from debt issuance |
— | 5,050 | — | |||||||||
| Principal payments on debt |
(508 | ) | (3,339 | ) | (199 | ) | ||||||
| Payment of deferred financing fees |
(263 | ) | (75 | ) | — | |||||||
| Payments on capital leases |
(80 | ) | (101 | ) | (207 | ) | ||||||
| Excess tax benefits from vesting of restricted stock |
121 | 91 | 104 | |||||||||
| Proceeds from issuance of common stock under ESPP |
618 | 493 | 419 | |||||||||
| Purchase of additional controlling interest |
(2,286 | ) | — | — | ||||||||
| Noncontrolling interest distributions |
(13,971 | ) | (9,391 | ) | (5,572 | ) | ||||||
| Net cash used in financing activities |
(10,646 | ) | (7,272 | ) | (5,455 | ) | ||||||
| Change in cash |
(3,117 | ) | 2,356 | (25,722 | ) | |||||||
| Cash at beginning of period |
3,511 | 1,155 | 26,877 | |||||||||
| Cash at end of period |
$ | 394 | $ | 3,511 | $ | 1,155 | ||||||
| Supplemental disclosures of cash flow information |
||||||||||||
| Interest paid |
$ | 142 | $ | 456 | $ | 376 | ||||||
| Income taxes paid |
$ | 35,869 | $ | 8,937 | $ | 12,052 | ||||||
Supplemental disclosure of non-cash transactions:
In February 2009, the Company acquired a 75% interest in Southeast Louisiana HomeCare, LLC in exchange for $7.5 million of cash and a noncontrolling interest in three of the Company’s home health agencies. Also, during 2009, the Company acquired a majority ownership in 11 entities and recorded $7.1 million of noncontrolling interest related to the acquisitions.
During the year ended December 31, 2008, the Company issued common stock valued at $1.0 million to several joint venture partners upon the acquisition of a portion of their noncontrolling interest. Also, in October 2008, the Company sold a minority ownership interest in two of its entities as consideration to purchase a majority ownership in an entity. The Company recognized a gain of $624,000 on the partial acquisition.
See accompanying Notes to the Consolidated Financial Statements
F-6
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS
1. Organization
LHC Group, Inc. (the “Company”) is a health care provider specializing in the post-acute continuum of care primarily for Medicare beneficiaries. The Company provides home-based services, primarily through home nursing agencies and hospices and facility-based services, primarily through long-term acute care hospitals. The Company, through its wholly and majority-owned subsidiaries, equity joint ventures and controlled affiliates, currently operates in Louisiana, Mississippi, Arkansas, Alabama, Texas, Kentucky, Florida, Tennessee, Georgia, Virginia, West Virginia, Ohio, Missouri, Maryland, Washington, Oklahoma, Oregon and North Carolina.
2. Summary of Significant Accounting Policies
Immaterial Correction of an Error
During the fourth quarter of 2009, the Company identified an immaterial error in the accounting for and presentation of noncontrolling interest- redeemable. Previously, all noncontrolling interest was presented in equity in the consolidated balance sheet and statement of changes in equity. Noncontrolling interest is generally required to be classified as equity. However, some of the Company’s noncontrolling interest agreements have certain redemption features that are not solely within the control of the Company. Classification of these noncontrolling interests outside of permanent equity is required. Therefore, the Company corrected the classification by presenting certain noncontrolling interest which contains a redemption feature, outside of permanent equity.
The unaudited balance sheets included in the Company’s 2009 interim financial statements presented noncontrolling interest - redeemable as a component of stockholders’ equity, rather than outside of permanent equity. In accordance with authoritative guidance, the Company evaluated the materiality of the error from both a qualitative and quantitative perspective, and concluded the error was immaterial to the current and prior periods. This immaterial error had no effect on our income statement or statement of cash flows for the years ending December 31, 2009, 2008 or 2007, including, no impact on earnings per share, net service revenue or in the manner in which we determine net income attributable to non-controlling interests. Noncontrolling interest - redeemable as of December 31, 2008, March 31, 2009, June 30, 2009 and September 31, 2009 should have been $6.7 million, $11.6 million, $13.2 million, and $13.5 million, respectively.
Use of Estimates
The preparation of financial statements in conformity with U.S. generally accepted accounting principles (“US GAAP”) requires management to make estimates and assumptions that affect the reported amounts of assets and liabilities and disclosure of contingent assets and liabilities at the date of the financial statements and the reported revenue and expenses during the reported period. Actual results could differ from those estimates.
Principles of Consolidation
The consolidated financial statements include all subsidiaries and entities controlled by the Company. Control is defined by the Company as ownership of a majority of the voting interest of an entity. The consolidated financial statements include entities in which the Company has the obligation to absorb losses of the entities or the right to receive benefits from the entities and generally has voting control over the entities or both, as a result of ownership, contractual or other financial interests in the entities. Third party equity interests in the consolidated joint ventures are reflected as noncontrolling interests in the Company’s consolidated financial statements.
The following table summarizes the percentage of net service revenue earned by type of ownership or relationship the Company had with the operating entity for the periods presented:
| 2009 | 2008 | 2007 | |||||||
| Equity joint ventures |
51.4 | % | 49.6 | % | 43.7 | % | |||
| Wholly owned subsidiaries |
44.6 | 46.6 | 46.4 | ||||||
| License leasing arrangements |
2.5 | 2.1 | 7.8 | ||||||
| Management services |
1.5 | 1.7 | 2.1 | ||||||
| 100.0 | % | 100.0 | % | 100.0 | % | ||||
The changes in the percentages of revenue earned by license leasing arrangements and by the equity joint ventures relate, in part, to the conversion of one of the Company’s license leasing arrangements to a joint venture on October 1, 2007.
All significant inter-company accounts and transactions have been eliminated in consolidation. Business combinations accounted for as purchases have been included in the consolidated financial statements from the respective dates of acquisition.
The following discussion describes the Company’s consolidation policy with respect to its various ventures excluding wholly owned subsidiaries:
Equity Joint Ventures
The Company’s joint ventures are structured as limited liability companies in which the Company typically owns a majority equity interest ranging from 51% to 99%. Each member of all but one of the Company’s equity joint ventures participates in profits and losses in proportion to their equity interests. The Company has one joint venture partner whose participation in losses is limited. The Company consolidates these entities as the Company has the obligation to absorb losses of the entities and the right to receive benefits from the entities and generally has voting control over the entities.
F-7
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
License Leasing Arrangements
The Company, through wholly owned subsidiaries, leases home health licenses necessary to operate certain of its home nursing agencies. As with wholly owned subsidiaries, the Company owns 100% of the equity of these entities and consolidates them based on such ownership, as well as the Company’s obligation to absorb losses of the entities and the right to receive benefits from the entities.
Management Services
The Company has various management services agreements under which the Company manages certain operations of agencies and facilities. The Company does not consolidate these agencies or facilities, as the Company does not have an ownership interest and does not have an obligation to absorb losses of the entities or the right to receive the benefits from the entities.
Revenue Recognition
The Company reports net service revenue at the estimated net realizable amount due from Medicare, Medicaid, commercial insurance, managed care payors, patients and others for services rendered. All payors contribute to both the home-based services and facility-based services.
The following table sets forth the percentage of net service revenue earned by category of payor for the years ending December 31:
| 2009 | 2008 | 2007 | |||||||
| Payor: |
|||||||||
| Medicare |
81.7 | % | 83.2 | % | 81.7 | % | |||
| Medicaid |
3.5 | 4.6 | 5.5 | ||||||
| Other |
14.8 | 12.2 | 12.8 | ||||||
| 100.0 | % | 100.0 | % | 100.0 | % | ||||
The percentage of net service revenue contributed from each reporting segment was as follows for the years ending December 31:
| 2009 | 2008 | 2007 | |||||||
| Home-based services |
88.2 | % | 85.2 | % | 82.2 | % | |||
| Facility-based services |
11.8 | 14.8 | 17.8 | ||||||
| 100.0 | % | 100.0 | % | 100.0 | % | ||||
Medicare
Home-Based Services
Home Nursing Services. The Company’s home nursing Medicare patients are classified into one of 153 home health resource groups prior to receiving services. Based on this home health resource group, the Company is entitled to receive a standard prospective Medicare payment for delivering care over a 60-day period, referred to as an episode. The Company recognizes revenue based on the number of days elapsed during an episode of care within the reporting period.
Final payments from Medicare may reflect one of four retroactive adjustments to ensure the adequacy and effectiveness of the total reimbursement: (a) an outlier payment if the patient’s care was unusually costly; (b) a low utilization adjustment if the number of visits totaled fewer than five; (c) a partial payment if the patient transferred to another provider before completing the episode; or (d) a payment adjustment based upon the level of therapy services required in the population base. Management estimates the impact of these payment adjustments based on historical experience and records this estimate during the period the services are rendered. The Company’s payment is also adjusted for differences in local prices using the hospital wage index. In calculating the Company’s reported net service revenue from home nursing services, the Company adjusts the prospective Medicare payments by an estimate of the adjustments. The adjustments are calculated using a historical average of prior adjustments.
Hospice Services. The Company is paid by Medicare under a per diem payment system. The Company receives one of four predetermined daily or hourly rates based upon the level of care the Company furnished. The Company records net service revenue from hospice services based on the daily or hourly rate and recognizes revenue as hospice services are provided.
F-8
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Hospice payments are also subject to two caps. One relates to individual programs receiving more than 20% of its total Medicare reimbursement from inpatient care services and the second relates to individual programs receiving reimbursements in excess of a “cap amount,” calculated by multiplying the number of beneficiaries during the period by a statutory amount that is indexed for inflation. The determination for each cap is made annually based on the 12-month period ending on October 31 of each year. This limit is computed on a program-by-program basis. The Company has not received notification that any of its hospices have exceeded the cap on inpatient care services during 2009. None of the Company’s hospices exceeded either cap during the years ended December 31, 2008, or 2007.
Facility-Based Services
Long-Term Acute Care Services (“LTACHs”). The Company is reimbursed by Medicare for services provided under LTACH prospective payment system, which was implemented on October 1, 2002. Each patient is assigned a long-term care diagnosis-related group, and the Company is paid a predetermined fixed amount applicable to that particular group. This payment is intended to reflect the average cost of treating a Medicare patient classified in that particular long-term care diagnosis-related group. For selected patients, the amount may be further adjusted based on length of stay and facility-specific costs, as well as in instances where a patient is discharged and subsequently readmitted, among other factors. Similar to other Medicare prospective payment systems, the rate is also adjusted for geographic wage differences. Revenue is recognized as services are provided for the Company’s LTACHs.
Medicaid, managed care and other payors
The Company’s Medicaid reimbursement is based on a predetermined fee schedule applied to each service provided. Therefore, revenue is recognized for Medicaid services as services are provided based on this fee schedule.
The Company’s managed care payors reimburse the Company in a manner similar to either Medicare or Medicaid. Accordingly, the Company recognizes revenue from managed care payors in the same manner as the Company recognizes revenue from Medicare or Medicaid.
Management Services
The Company records management services revenue as services are provided in accordance with the various management services agreements to which the Company is a party. As described in the agreements, the Company provides billing, management and other consulting services suited to and designed for the efficient operation of the applicable home nursing agency or inpatient rehabilitation facility. The Company is responsible for the costs associated with the locations and personnel required for the provision of services. The Company is compensated based on a percentage of cash collections, a flat fee or is reimbursed for operating expenses and compensated based on a percentage of operating net income.
Accounts Receivable and Allowances for Uncollectible Accounts
The Company reports accounts receivable net of estimated allowances for uncollectible accounts and adjustments. Accounts receivable are uncollateralized and primarily consist of amounts due from third-party payors and patients. To provide for accounts receivable that could become uncollectible in the future, the Company establishes an allowance for uncollectible accounts to reduce the carrying amount of such receivables to their estimated net realizable value. The credit risk for other concentrations of receivables is limited due to the significance of Medicare as the primary payor. The Company does not believe that there are any other significant concentrations of receivables from any particular payor that would subject it to any significant credit risk in the collection of accounts receivable.
The amount of the provision for bad debts is based upon the Company’s assessment of historical and expected net collections, business and economic conditions and trends in government reimbursement. Uncollectible accounts are written off when the Company has determined the account will not be collected.
A portion of the estimated Medicare prospective payment system reimbursement from each submitted home nursing episode is received in the form of a request for accelerated payment (“RAP”). The Company receives a RAP payment for 60% of the estimated reimbursement for the initial episode at the start of care. The full amount of the episode is billed after the episode has been completed. The RAP received for that particular episode is deducted from the final payment. If a final bill is not submitted within the greater of 120 days from the start of the episode, or 60 days from the date the RAP was paid, any RAPs received for that episode will be recouped by Medicare from any other Medicare claims in process for that particular provider. The RAP and final claim must then be resubmitted. For subsequent episodes of care contiguous with the first episode for a particular patient, the Company submits a RAP for 50% instead of 60% of the estimated reimbursement. The remaining 50% reimbursement is requested upon completion of the episode. The Company has earned net service revenue in excess of billings rendered to Medicare.
F-9
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The Company’s Medicare population is paid at a prospectively set amount that can be determined at the time services are rendered. The Company’s Medicaid reimbursement is based on a predetermined fee schedule applied to each individual service the Company provides. The Company’s managed care contracts are structured similar to either the Medicare or Medicaid payment methodologies. Because of the Company’s payor mix, it is able to calculate actual amounts due at the patient level and adjust the gross charges down to the actual amount at the time of billing. This negates the need for an estimated contractual allowance to be booked at the time it reports net service revenue for each reporting period.
Business Combination
The Company accounts for business combinations using the acquisition method. The assets acquired in the Company’s acquisition consist primarily of a Medicare license, certificate or need and/or a noncompete agreement. The assets acquired and liabilities assumed, if any, are measured at fair value on the acquisition date using the appropriate valuation method. The noncontrolling interest associated with joint venture acquisitions is also measured and recorded at fair value as of the acquisition date. The residual purchase price is recorded as goodwill. The operations are the acquisitions are included in the consolidated financial statements from their respective dates of acquisition.
Goodwill and Intangible Assets
Goodwill and other intangible assets with indefinite lives are reviewed annually for impairment or more frequently if circumstances indicate impairment may have occurred. An impairment loss is recognized if the carrying value of goodwill or an indefinite-lived intangible asset exceeds its fair value. The evaluation of impairment involves comparing the current fair value of each of the Company’s reporting units to their recorded value, including goodwill. Components of the Company’s home -based services segment are generally represented by individual subsidiaries or joint ventures with individual licenses to conduct specific operations within geographic markets as limited by the terms of each license. Components of the Company’s facility-based services are represented by individual operating entities. Management aggregates the components of these two segments into two reporting units for purposes of evaluating impairment.
The Company estimates the fair value of its identified reporting units using the discounted cash flow method and the market multiple analysis method. These valuations require management to make estimates and assumptions regarding industry economic factors and the profitability of future business strategies. Management considers historical experience and all available information at the time the fair values of its reporting units are estimated. For each of the reporting units, the estimated fair value is determined based on a formula that considers 50% of the estimated value based on a multiple of earnings before interest, taxes, depreciation and amortization plus 50% of the estimated value using recent sales of comparable facilities. A change in the weight assigned to each methodology would not have changed the conclusion that no impairment charge is necessary during the year ending December 31, 2009. The Company has not recognized goodwill impairment charges in 2009, 2008 or 2007.
Included in intangible assets, net, are definite-lived assets subject to amortization such as non-compete agreements. Amortization of definite-lived intangible assets is calculated on a straight-line basis over the estimated useful lives of the related assets.
The Company also has indefinite-lived assets that are not subject to amortization expense such as trade names and certificates of need. The Company has concluded that trade names and certificates of need have indefinite lives, as management has determined that there are no legal, regulatory, contractual, economic or other factors that would limit the useful life of these intangible assets and the Company intends to renew and operate the licenses and use these trade names indefinitely. The Company performs an annual impairment test on the trade names using the relief-from royalty method. Under this method, the fair value of the intangible asset is determined by calculating the present value of the after-tax cost savings associated with owning the trade names and, therefore, not having to pay royalties for its use for the remainder of its estimated useful lives. The certificates of need are tested annually for impairment using the cost approach. Under this method assumptions are made about the cost to replace the certificates of need.
Due to/from Governmental Entities
The Company’s LTACHs are reimbursed for certain activities based on tentative rates. The amounts recorded in due to/from governmental entities on the Company’s consolidated balance sheet relate to settled and open cost reports that are subject to the completion of audits and the issuance of final assessments. Final reimbursement is determined based on submission of annual cost reports and audits by the fiscal intermediary. Adjustments are accrued on an estimated basis in the period the related services were rendered and further adjusted as final settlements are determined. These adjustments are accounted for as changes in estimates. There have been no significant changes in estimates during the years ended December 31, 2009 and 2008.
Property, Building and Equipment
Property, building and equipment are stated at cost. Depreciation is computed using the straight-line method over the estimated useful lives of the individual assets. Estimated useful lives for buildings is 39 years and ranges from 3 to 10 years for transportation equipment and furniture and other equipment. The useful life for leasehold improvements is the lesser of the lease term or the expected life of the leasehold improvement. Routine repairs and maintenance are expensed when incurred.
Property, building and equipment is reviewed whenever events or changes in circumstances occur that indicate possible impairment. There were no impairments recognized during the periods ended December 31, 2009, 2008 or 2007.
F-10
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The following table describes the Company’s components of property, building and equipment:
| December 31, | ||||||
| 2009 | 2008 | |||||
| (In thousands) | ||||||
| Land |
$ | 667 | $ | 342 | ||
| Building and improvements |
4,385 | 3,719 | ||||
| Transportation equipment and major moveables |
5,697 | 5,496 | ||||
| Furniture and other equipment |
25,643 | 17,695 | ||||
| 36,392 | 27,252 | |||||
| Less accumulated depreciation and amortization |
15,031 | 10,904 | ||||
| $ | 21,361 | $ | 16,348 | |||
Depreciation expense for the years ended December 31, 2009, 2008 and 2007 was $4.8 million, $3.7 million and $3.0 million, respectively.
Noncontrolling Interest
The nonredeemable interest held by third parties in subsidiaries owned or controlled by the Company is reported on the consolidated balance sheets as noncontrolling interest as a component of stockholders’ equity. Redeemable interest held by third parties in subsidiaries owned or controlled by the Company is reported on the consolidated balance sheets outside permanent equity. All noncontrolling interest reported in the consolidated statements of income reflects the respective interests in the income or loss after income taxes of the subsidiaries attributable to the other parties, the effect of which is removed from the net income available to LHC Group, Inc.
Stock-Based Employee Compensation
The Company grants restricted stock or restricted stock units to employees and members of its Board of Directors as a form of compensation. The expense for such awards is based on the grant date fair value of the award and is recognized on a straight-line basis over the requisite service period. See Note 7 to these consolidated financial statements.
Earnings Per Share
Basic per share information is computed by dividing the item by the weighted-average number of shares outstanding during the period, under the treasury stock method. Diluted per share information is computed by dividing the item by the weighted-average number of shares outstanding plus dilutive potential shares. The dilutive share calculation at December 31, 2009 included 29,043 contingent shares related to one of the Company’s acquisitions. See Note 3 to these consolidated financial statements.
The following table sets forth shares used in the computation of basic and diluted per share information for the years ended December 31, 2009, 2008 and 2007:
| 2009 | 2008 | 2007 | ||||
| Weighted average number of shares outstanding for basic per share calculation |
17,960,376 | 17,855,634 | 17,760,432 | |||
| Effect of dilutive potential shares: |
||||||
| Options |
6,158 | 5,705 | 6,461 | |||
| Nonvested restricted stock |
74,320 | 37,748 | 60,551 | |||
| Contingent shares |
29,043 | — | — | |||
| Adjusted weighted average shares for diluted per share calculation |
18,069,897 | 17,899,087 | 17,827,444 | |||
Subsequent Events
The Company evaluated all events or transactions that occurred from December 31, 2009 through the date the financial statements were issued. During this period, the Company did not have any material recognizable subsequent events.
F-11
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Adoption of New Accounting Standards
In June 2009, the Financial Accounting Standards Board (the “FASB”) issued authoritative guidance that replaced the previous hierarchy of GAAP and established the FASB Codification as the single source of authoritative U.S. GAAP recognized by the FASB to be applied by nongovernmental entities. Its primary purpose is to improve clarity and use of existing standards by grouping authoritative literature under common topics. The FASB will no longer issue new standards in the form of Statements, FASB Staff Positions or Emerging Issues Task Force Abstracts. Instead, it will issue Accounting Standards Updates which will serve to update the Codification, provide background information about the guidance and provide the basis for conclusions on the changes to the Codification. The Codification is effective for financial statements issued for interim and annual periods ending after September 15, 2009. The Codification does not change or alter existing GAAP and did not have a material effect on the Company’s condensed financial condition, results of operations, or cash flows.
In April 2009, the FASB issued authoritative guidance requiring publicly-traded entities to disclose in the body or in the accompanying notes of its summarized financial information for interim reporting periods and in its financial statements for annual reporting periods, the fair value of all financial instruments for which it is practicable to estimate that value, whether recognized or not recognized in the statement of financial position, as required by other authoritative guidance. The guidance is effective for interim and annual reporting periods ending after June 15, 2009. The adoption of the new disclosure requirements did not have a material effect on the Company’s financial condition, results of operations, or cash flows.
In 2009, the Company adopted the FASB authoritative guidance establishing general standards of accounting for and disclosing subsequent events that occur after the balance sheet date but before financial statements are issued or are available to be issued. In particular, the guidance sets forth the period after the balance sheet date during which management should evaluate events or transactions that may occur for potential recognition or disclosure in the financial statements, the circumstances under which the Company should recognize events or transactions occurring after the balance sheet date in its financial statements, and the disclosures that the Company should make about events or transactions that occurred after the balance sheet date. Because the guidance only introduces the concept of financial statements being available to be issued, adoption of this guidance did not result in significant changes in the subsequent events that the Company reports, either through recognition or disclosure, in its consolidated financial statements.
On January 1, 2009, the Company prospectively adopted FASB’s guidance on business combinations. The authoritative guidance changes the accounting treatment and disclosure for certain specific items in a business combination. According to the guidance, an acquiring entity is required to recognize all the assets acquired and liabilities assumed in a transaction at the acquisition-date fair value with limited exceptions. This includes the fair values of the noncontrolling interest acquired. Under previous guidance, the noncontrolling interest (minority interest) was recorded at the minority owner’s historical balance. Contingent consideration arrangements are also now measured and recorded at fair value at the acquisition date. Under previous guidance contingent consideration was not recognized until paid or settled. Other changes include the treatment of acquisition-related costs, which, with the exception of debt or equity issuance costs, are to be recognized as an expense in the period that the costs are incurred and the services are received. The Company capitalized acquisition-related costs under previous guidance. Further, any adjustments during the measurement period to the provisional amounts recognized as part of the purchase price allocation are treated retrospectively as of the acquisition date.
In April 2009, the FASB further issued an update on accounting for assets acquired and liabilities assumed in a business combination that arise from contingencies. The update addresses application issues on initial recognition and measurement, subsequent measurement and accounting, and disclosure of assets and liabilities arising from contingencies in a business combination. The update required that all contractual contingencies and all noncontractual contingencies that are more likely than not to give rise to an asset or liability be recognized at their acquisition date fair value. All noncontractual contingencies that do not meet the more-likely-than not criterion as of the acquisition date would be accounted for in accordance with other U.S. GAAP. The guidance requires that when new information is obtained, a liability be measured at the higher of its acquisition-date fair value or the amount that would be recognized under other authoritative guidance. Further, an acquirer shall recognize at fair value, at the acquisition date, an asset acquired or a liability assumed in a business combination that arises from a contingency if the acquisition-date fair value of that asset or liability can be determined during the measurement period. The Company has adopted the provisions of this guidance effective January 1, 2009, which did not have a material effect on the operating results, financial position, or liquidity of the Company.
The Company also adopted the FASB’s guidance on noncontrolling interests in consolidated financial statements on January 1, 2009. The guidance establishes new accounting and reporting standards for the noncontrolling interest, previously known as minority interest. Noncontrolling interest in consolidated subsidiaries is presented in the consolidated balance sheet within stockholders’ equity as a separate component from the parent’s equity. Consolidated net income includes earnings attributable to both the parent and the noncontrolling interest. Earnings per share, which is not affected by the guidance, is based on earnings attributable only to the parent
F-12
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
company. The guidance explains the accounting for changes in the parent’s ownership interest in a subsidiary, including transactions where control is retained and where control is relinquished. The guidance requires additional disclosure information related to amounts attributable to the parent for income from continuing operations, discontinued operations and extraordinary items and reconciliations of the parent and noncontrolling interests’ equity in subsidiaries.
3. Acquisitions and Divestitures
Pursuant to the Company’s strategy of becoming the leading provider of post-acute health care services in the United States, the Company acquired one LTACH, 13 homecare entities and two hospice entities during 2009. As a result of these acquisitions, the Company maintains an ownership interest in the entities set forth below.
| Acquired Entity |
Ownership Percentage |
State of Operations |
Acquisition Date | ||||
| Southeast Louisiana HomeCare, LLC |
75 | % | Louisiana | February 1, 2009 | |||
| Hospice of Central Arkansas, LLC |
67 | % | Arkansas | April 1, 2009 | |||
| Marion Regional HomeCare, LLC |
67 | % | Alabama | April 1, 2009 | |||
| Louisiana Extended Care Hospital of Kenner, LLC |
75 | % | Louisiana | May 1, 2009 | |||
| Central Basin HomeCare and Hospice, LLC |
100 | % | Washington | May 1, 2009 | |||
| East Alabama Medical Center HomeCare, LLC |
75 | % | Alabama | June 1, 2009 | |||
| Kentucky HomeCare of Henderson, LLC |
67 | % | Kentucky | June 1, 2009 | |||
| Coosa Valley HomeCare, LLC |
75 | % | Alabama | August 1, 2009 | |||
| Northeast Washington Home Health, Inc. |
80.1 | % | Washington | August 1, 2009 | |||
| LHCG XV, LLC |
100 | % | Louisiana | September 1, 2009 | |||
| Three Rivers HomeCare, LLC |
75 | % | Oregon | September 1, 2009 | |||
| Camden HomeCare, LLC |
100 | % | Alabama | October 1, 2009 | |||
| Feliciana Home Health, LLC |
100 | % | Louisiana | November 1,2009 | |||
| Twin Lakes Home Health Agency, LLC |
75 | % | Kentucky | November 1, 2009 | |||
| Woods Memorial Home Health, LLC |
75 | % | Tennessee | December 1, 2009 |
Each of the acquisitions was accounted for under the acquisition method of accounting, and, accordingly, the accompanying consolidated financial statements include the results of operations of each acquired entity from the date of acquisition.
2009 Acquisitions
Home-Based
The total purchase price of home-based acquisitions was $33.2 million, which was paid primarily in cash. The purchase prices were determined based on the Company’s analysis of comparable acquisitions and the target market’s potential future cash flows. The purchase price for Southeast Louisiana HomeCare, LLC included a transfer of a 25% noncontrolling interest in three of the Company’s wholly owned home health agencies. The transfer of the noncontrolling interest in the Company’s existing home health agencies was accounted for as an equity transaction, resulting in the Company recognizing additional paid in capital of $181,000.
The purchase price for Feliciana Home Health, LLC provided for up to $2.5 million in contingent consideration to be paid to the seller if certain financial measurements are achieved. The fair value of the contingent consideration recognized on the acquisition date was $1.7 million. The fair value of the contingent consideration was estimated using an income approach based on financial projections for the acquired company. The projected cash flows were discounted using a discount rate of LIBOR plus 100 basis points, which the Company believes is appropriate and is representative of a market participant assumption. The fair value measurement is based on significant inputs not observable in the market and thus represents a Level 3 fair value measurement.
The Company recognized goodwill of $22.0 million, including $3.2 million of goodwill attributable to noncontrolling interests, related to acquisitions made in 2009. The Company expects its portion of goodwill to be fully tax deductible.
During 2009, the Company purchased additional ownership interests in five of its joint ventures. The total purchase price for the additional ownership interests was $2.3 million and was accounted for as an equity transaction, resulting in the Company recognizing additional paid in capital of $2.3 million.
F-13
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
In 2008, one of the Company’s acquisitions contained contingent consideration to the seller, a portion of which may be settled in shares of the Company’s stock one year after the acquisition date. The number of shares that may be issued is contingent upon the acquired company achieving certain financial measurements in the year after the acquisition. During the three months ended September 30, 2009, the Company recorded $1.9 million of additional purchase price related to the contingent consideration as the acquired company achieved the required financial measurements. Of the contingent consideration, $950,000 was paid in cash during 2009. The remaining $950,000 is recorded as a liability as of December 31, 2009, however the number of the shares to be issued was not determinable beyond a reasonable doubt.
During 2009, the Company settled the working capital amounts acquired on several 2008 acquisitions. An additional $349,000 was paid in cash in 2009 related to the settlements. An additional $2.7 million was recognized as goodwill and a deferred tax liability related to the finalization of acquisition accounting.
On December 31, 2009, the Company paid $1.2 million in cash for two acquisitions with January 1, 2010 acquisition dates. Control was not assumed until January 1, 2010; therefore, the $1.2 million cash payment is recorded in other assets on the balance sheet as of December 31, 2009.
Facility-Based
The total purchase price of the facility-based acquisitions was $1.2 million, which was paid primarily in cash. The purchase price was determined based on the Company’s analysis of comparable acquisitions and the target market’s potential future cash flows.
The Company recognized goodwill of $86,000, including $22,000 of noncontrolling goodwill, related to the acquisitions. The Company expects its portion of goodwill to be fully tax deductible.
In conjunction with the redemption by certain noncontrolling interest holders of their interest in one of the Company’s joint ventures, $15,000 of goodwill, which is not deductible for income tax purposes, was recognized in the facility-based services segment.
The following table summarizes the consideration paid for the 2009 acquisitions and the amounts of the assets acquired and liabilities assumed at the acquisition dates, as well as the fair value at the acquisition dates of the noncontrolling interest acquired for both the home-based and facility-based acquisitions.
| 2009 | |||
| Consideration (in thousands) |
|||
| Cash |
$ | 30,905 | |
| Contingent consideration |
1,726 | ||
| Equity instruments (the Company exchanged a noncontrolling ownership interest in three of its entities) |
1,409 | ||
| Working capital adjustment |
337 | ||
| Fair value of total consideration transferred |
$ | 34,377 | |
| Acquisition-related costs (included in general and administrative expenses in the Company’s statement of income.) |
$ | 672 | |
| Recognized amounts of identifiable assets acquired and liabilities assumed |
|||
| Property, plant and equipment |
$ | 888 | |
| Trade name |
12,949 | ||
| Certificate of need/License |
3,532 | ||
| Other identifiable intangible assets |
797 | ||
| Total identifiable assets |
$ | 18,166 | |
| Noncontrolling interest |
$ | 5,858 | |
| Goodwill, including noncontrolling interest of ($3.3 million) |
$ | 22,069 | |
Trade names and certificates of need are indefinite-lived assets and, therefore, not subject to amortization. The other identifiable assets include non-compete agreements and other contracts that are amortized over the life of the agreements or contracts, ranging from two to five years. The fair value of the acquired intangible assets is preliminary pending the final valuation of those assets.
F-14
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The acquisitions during the year, individually, were immaterial to the Company’s consolidated financial statements; however, when aggregated, total acquisitions were material. The following table contains unaudited pro forma consolidated income statement information assuming the acquisitions closed January 1, 2008 for 2009 acquisitions (amounts in thousands):
| 2009 | 2008 | |||||
| Net service revenue |
$ | 553,315 | $ | 427,127 | ||
| Operating income |
86,833 | 29,670 | ||||
| Net income |
45,222 | 29,590 | ||||
| Basic earnings per share |
2.52 | 1.67 | ||||
| Diluted earnings per share |
2.50 | 1.66 | ||||
To provide financial information that is more representative of the combined results of the Company as if the acquisitions had occurred January 1, 2008, the pro forma disclosure in the table above includes adjustments for depreciation expense, amortization of intangible assets, income tax expense and an estimate of additional costs to provide administrative services for these locations. This pro forma information is presented for illustrative purposes only and may not be indicative of the results of operations that would have actually occurred. In addition, future results may vary significantly from the results reflected in the pro forma information.
2008 Acquisitions
Home-Based
During the year ended December 31, 2008, the Company acquired the existing operations of 11 entities operating a total of 43 agencies and a majority ownership in 12 entities operating a total of 17 agencies. The total purchase price for the acquisitions was $63.7 million, including $2.0 million of acquisition-related costs. Goodwill of $47.2 million and other intangibles of $14.9 million were assigned to the home-based services segment related to the acquisitions. Goodwill of $23.5 million is not deductible for income tax purposes.
In October 2008, the Company purchased a majority ownership in an entity with three agencies in exchange for a minority ownership interest in two of the Company’s entities. Noncontrolling interest of $1.9 million was recorded in the Company’s consolidated balance sheet as of December 31, 2008 related to the noncontrolling ownership transferred as consideration. The Company recognized a gain of $624,000 on the purchase. Goodwill of $2.4 million and other intangibles of $485,000 were assigned to the home-based services segment related to the acquisition.
Facility-Based
In 2008, the Company also acquired an additional ownership interest in one of its majority-owned hospitals for $1.0 million, paid by issuing 51,736 shares of its common stock. Goodwill of $1.0 million related to this acquisition, which is nondeductible for income tax purposes, was assigned to the facility-based services segment.
In conjunction with the redemption by certain noncontrolling interest holders of their interest in one of the Company’s joint ventures, $89,000 of goodwill, which is not deductible for income tax purposes, was recognized in the facility-based services segment.
2007 Acquisitions
During the year ended December 31, 2007, the Company acquired the existing operations of 11 locations and a majority ownership interest in the existing operations of 12 locations for $26.0 million in cash, and $2.4 million in acquisition costs. Goodwill of $21.9 million and other intangibles of $5.8 million were assigned to the home-based services segment.
2009 Divestitures
In September 2009, the Company sold its outpatient rehabilitation clinic. The sale generated a loss of $22,000, which was recognized in the third quarter of 2009. The results of operations related to the clinic are included in discontinued operations in the Company’s condensed consolidated statements of income for the years ending December 31, 2009, 2008 and 2007.
2007 Divestitures
During the year ended December 31, 2007, the Company sold its critical access hospital for $180,000 and recognized a gain of $31,000, net of tax of $20,000. There was no goodwill related to this hospital. Additionally, the Company closed a home health pharmacy location in the year ended December 31, 2007. The assets related to the home health pharmacy are classified as assets held for sale on the balance sheet. The Company retired goodwill of $48,000 related to the termination of its private duty business.
F-15
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The following table provides financial results of discontinued operations for the years ending December 31, 2009, 2008 and 2007 (amounts in thousands):
| 2009 | 2008 | 2007 | ||||||||||
| Net service revenue |
$ | 402 | $ | 756 | $ | 3,994 | ||||||
| Costs of services and general and administrative expenses |
(543 | ) | (1,722 | ) | (6,699 | ) | ||||||
| Loss from discontinued operations before noncontrolling interest and income taxes |
(141 | ) | (966 | ) | (2,705 | ) | ||||||
| Income tax benefit |
55 | 190 | 289 | |||||||||
| Loss from discontinued operations net of income tax benefit |
(86 | ) | (776 | ) | (2,416 | ) | ||||||
| Less loss from discontinued operations attributable to noncontrolling interest |
— | (123 | ) | (672 | ) | |||||||
| Loss from discontinued operations attributable to LHC Group Inc.’s common stockholders |
$ | (86 | ) | $ | (653 | ) | $ | (1,744 | ) | |||
4. Goodwill and Other Intangibles, Net
The following table summarizes the changes in goodwill by segment:
| 2009 | 2008 | ||||||
| (In Thousands) | |||||||
| Home-based services segment: |
|||||||
| Balances at beginning of period |
$ | 107,108 | $ | 57,885 | |||
| Goodwill from acquisitions |
18,735 | 49,223 | |||||
| Goodwill related to noncontrolling interest |
3,248 | — | |||||
| 2008 acquisition adjustments |
(654 | ) | — | ||||
| Deferred tax liability on 2008 acquisitions |
2,700 | — | |||||
| Consideration settlement of 2008 acquisition |
2,772 | — | |||||
| Home-based balance at end of period |
133,909 | 107,108 | |||||
| Facility-based services segment: |
|||||||
| Balances at beginning of period |
$ | 5,464 | $ | 4,342 | |||
| Goodwill from acquisitions |
64 | — | |||||
| Goodwill related to noncontrolling interest |
22 | — | |||||
| Goodwill acquired during the period from redemption of noncontrolling interest |
15 | 1,122 | |||||
| Facility-based balance at end of period |
5,565 | 5,464 | |||||
| Consolidated balance at end of period |
$ | 139,474 | $ | 112,572 | |||
In 2008, the Company purchased two home health agency provider numbers in Ohio for $542,000 and obtained approval from the State of Ohio to move the provider numbers to a new service area. In February 2009, the Centers for Medicare and Medicaid Services (“CMS”) denied the Company’s change of ownership for the provider numbers because the agency locations were moved outside of the allowed service area. Although the Company has re-applied for and received the new provider numbers for these home health agencies, the purchased provider numbers no longer have value. Therefore, the Company has recognized a $542,000 impairment expense on the home-based services segment in other non-operating (loss) income on the Company’s condensed consolidated statements of income for the year ended December 31, 2009.
F-16
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The following table summarizes the changes in other intangibles, net during 2009, which all related to the home-based services segment (amounts in thousands):
| Trade Names |
License and Certificates of Need |
Other Intangibles |
Total | ||||||||||||
| Balance at December 31, 2008 |
$ | 27,233 | $ | 2,001 | $ | 741 | $ | 29,975 | |||||||
| Additions |
12,949 | 3,532 | 797 | 17,278 | |||||||||||
| 2008 acquisition adjustments |
123 | 542 | — | 665 | |||||||||||
| License impairment |
— | (542 | ) | — | (542 | ) | |||||||||
| Amortization |
— | — | (525 | ) | (525 | ) | |||||||||
| Balance at December 31, 2009 |
$ | 40,305 | $ | 5,533 | $ | 1,013 | $ | 46,851 | |||||||
Other intangible assets of $45.9 million, net of accumulated amortization, related to the home-based services segment and $992,000 related to the facility-based services segment as of December 31, 2009.
5. Income Taxes
The Company accounts for income taxes using the liability method. Under the liability method, deferred taxes are determined based on differences between the financial reporting and tax bases of assets and liabilities and are measured using the enacted tax laws that will be in effect when the differences are expected to reverse. Management provides a valuation allowance for any net deferred tax assets when it is more likely than not that a portion of such net deferred tax assets will not be recovered.
As discussed in Note 3 to these consolidated financial statements, during 2009, the Company finalized the acquisition accounting for three of the Company’s 2008 acquisitions and recorded a $2.7 million net deferred tax liability. Significant components of the Company’s deferred tax assets and liabilities as of December 31, 2009 and 2008 were as follows:
| 2009 | 2008 | |||||||
| (In Thousands) | ||||||||
| Deferred tax assets: |
||||||||
| Allowance for uncollectible accounts |
$ | 2,746 | $ | 3,503 | ||||
| Accrued employee benefits |
2,293 | 1,679 | ||||||
| Stock compensation |
897 | 742 | ||||||
| Accrued self-insurance |
1,185 | 796 | ||||||
| Acquisition Costs |
372 | — | ||||||
| Book losses not deductible for taxes |
76 | — | ||||||
| Net operating loss carry forward |
652 | 644 | ||||||
| Valuation allowance |
(652 | ) | (689 | ) | ||||
| Deferred tax assets |
$ | 7,569 | $ | 6,675 | ||||
| Deferred tax liabilities: |
||||||||
| Amortization of intangible assets |
(10,247 | ) | (4,733 | ) | ||||
| Tax depreciation in excess of book depreciation |
(3,005 | ) | (1,683 | ) | ||||
| Prepaid expenses |
(866 | ) | (364 | ) | ||||
| Non-accrual experience accounting method |
(918 | ) | (654 | ) | ||||
| Conversion from cash basis accounting |
(638 | ) | — | |||||
| Deferred tax liabilities |
(15,674 | ) | (7,434 | ) | ||||
| Net deferred tax liability |
$ | (8,105 | ) | $ | (759 | ) | ||
F-17
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Based on the Company’s historical pattern of taxable income, the Company believes it will produce sufficient income in the future to realize its deferred income tax assets. A valuation allowance is established for any portion of a deferred income tax asset for which the Company believes it is more likely than not that the Company will not be able to realize the benefits or portions of a deferred income tax asset. At December 31, 2008 management had a valuation allowance primarily related to the tax net operating losses and deferred tax assets on the Company’s home health pharmacy, which was included in discontinued operations for the years ending December 31, 2008 and 2007. During 2009, the net operating losses were fully utilized; therefore, management released the valuation allowance. Management established a valuation allowance during purchase accounting related to the tax net operating losses acquired during 2008 in one the Company’s stock acquisitions.
The components of the Company’s income tax expense from continuing operations, less noncontrolling interest, were as follows:
| 2009 | 2008 | 2007 | |||||||
| (In Thousands) | |||||||||
| Current: |
|||||||||
| Federal |
$ | 19,026 | $ | 15,928 | $ | 10,585 | |||
| State |
3,071 | 2,418 | 1,483 | ||||||
| 22,097 | 18,346 | 12,068 | |||||||
| Deferred: |
|||||||||
| Federal |
4,001 | 401 | 111 | ||||||
| State |
645 | 61 | 18 | ||||||
| 4,646 | 462 | 129 | |||||||
| Total provision for income taxes |
$ | 26,743 | $ | 18,808 | $ | 12,197 | |||
A reconciliation of the differences between income taxes expense, computed at the federal statutory rate and provisions for income taxes for each period is as follows:
| 2009 | 2008 | 2007 | ||||||||||
| (In Thousands) | ||||||||||||
| Income taxes computed at federal statutory tax rate |
$ | 24,734 | $ | 17,270 | $ | 11,730 | ||||||
| State income taxes, net of federal benefit |
2,480 | 1,730 | 1,001 | |||||||||
| Work Opportunity Act tax credit |
(525 | ) | (518 | ) | (662 | ) | ||||||
| Valuation allowance reduction |
(689 | ) | — | — | ||||||||
| Nondeductible expenses |
743 | 326 | 128 | |||||||||
| Total provision for income taxes |
$ | 26,743 | $ | 18,808 | $ | 12,197 | ||||||
As of December 31, 2009, the Company has no unrecognized tax benefits. The Company recognizes interest and penalties related to uncertain tax positions, if applicable, in interest expense and general and administrative expenses, respectively. During the years ended December 31, 2009, 2008 and 2007, the Company did not recognize any interest or penalties in its consolidated financial statements, nor has it recorded an accrued liability of interest or penalty payments related to uncertain tax positions.
The Company is subject to both federal and state income tax for jurisdictions within which it operates. Within these jurisdictions, the Company is open to examination for tax years ended after December 31, 2006.
F-18
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
6. Credit Arrangements
Long-Term Debt
Long-term debt consisted of the following:
| December 31, | ||||||
| 2009 | 2008 | |||||
| (In thousands) | ||||||
| Due in monthly installments of $28,056 through February 2015 at LIBOR plus 1.90% (2.14% at December 31,2009) plus a balloon payment of $2.7 million |
$ | 4,433 | $ | 4,769 | ||
| Due in August 2010 at 6.25% |
50 | 100 | ||||
| Due in November 2009 at 5.78% |
— | 122 | ||||
| 4,483 | 4,991 | |||||
| Less current portion of long-term debt |
387 | 508 | ||||
| $ | 4,096 | $ | 4,483 | |||
In February 2008, the Company entered into a loan agreement with Capital One, National Association (“Capital One”) for a term note in the amount of $5.1 million for the purchase of a 1999 Cessna 560 aircraft. The aircraft serves as collateral for the term note, which is payable in 83 monthly installments of principal plus interest followed by one balloon installment on February 6, 2015 of $2.7 million. The term note bears interest at the LIBOR Rate (adjusted monthly) plus the Applicable Margin of 1.9%.
Certain of the Company’s loan agreements contain restrictive covenants, including limitations on indebtedness and the maintenance of certain financial ratios. The Company was in compliance with all covenants at December 31, 2009 and 2008.
The scheduled principal payments on long-term debt are as follows for each of the next five years following December 31, 2009 (in thousands):
| 2010 |
$ | 387 | |
| 2011 |
337 | ||
| 2012 |
337 | ||
| 2013 |
337 | ||
| 2014 |
337 | ||
| Thereafter |
2,748 | ||
| $ | 4,483 | ||
Credit Facility
The Company’s Credit Facility with Capital One, which was amended on June 15, 2009, provides for a maximum aggregate principal borrowing of $75.0 million. The Credit Facility, which is scheduled to expire on June 15, 2011, is unsecured and has a letter of credit sublimit of $2.5 million. In September 2009, the company issued a $700,000 letter of credit as collateral on the Company’s workers’ compensation insurance. The annual facility fee is 0.25% of the total availability. The interest rate for borrowings under the Credit Facility is a function of the prime rate (Base Rate) subject to a floor or the Eurodollar rate (Eurodollar) subject to a floor, as elected by the Company, plus the applicable margin based on the Leverage Ratio as defined in the Credit Facility. The Company paid $477,000 of credit fees on the Credit Facility during 2009. At December 31, 2009, $5.7 million and the letter of credit were outstanding under the Credit Facility. At December 31, 2008 no amounts were outstanding under the Credit Facility.
The Company’s Credit Facility contains customary affirmative, negative and financial covenants. For example, the Company is restricted in incurring additional debt, disposing of assets, making investments, allowing fundamental changes to the Company’s business or organization, and making certain payments in respect of stock or other ownership interests, such as dividends and stock repurchases. Under the Credit Facility, the Company is also required to meet certain financial covenants with respect to minimum fixed charge coverage, consolidated net worth, leverage and minimum asset coverage ratios. At December 31, 2009, the Company was in compliance with all covenants.
The Company’s Credit Facility also contains customary events of default. These include bankruptcy and other insolvency events, cross-defaults to other debt agreements, a change in control involving the Company or any subsidiary guarantor, and the failure to comply with certain covenants.
F-19
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
7. Stockholders’ Equity
Equity Based Awards
On January 20, 2005, the Board of Directors and stockholders of the Company approved the 2005 Long Term Incentive Plan (the “Incentive Plan”). The Incentive Plan, which is administered by the Compensation Committee of the Company’s Board of Directors, provides for 1,000,000 shares of common stock that may be issued or transferred pursuant to awards made under the plan. A variety of discretionary awards for employees, officers, directors and consultants are authorized under the Incentive Plan, including restricted stock and incentive or non-qualified statutory stock options. All awards must be evidenced by a written award certificate that will include the provisions specified by the Compensation Committee of the Board of Directors. The Incentive Plan provides that shares of common stock subject to awards granted become available again for issuance if such awards are canceled or forfeited.
The Compensation Committee determines the exercise price for non-statutory stock options. The exercise price for any option cannot be less than the fair market value of the Company’s common stock as of the date of grant.
In the event of a change of control as defined in the Incentive Plan, all restricted periods and restrictions imposed on non-performance based restricted stock awards will lapse and outstanding options will become immediately exercisable in full.
Share Based Compensation
Stock Options
The following table represents stock options activity for the year ended December 31, 2009:
| Number of Shares |
Weighted Average Exercise Price |
Average Remaining Contractual Term |
Aggregate Instrinsic Value | |||||||
| Options outstanding at January 1, 2009 |
19,000 | $ | 17.20 | 7.0 years | $ | 357,275 | ||||
| Options granted |
— | — | — | — | ||||||
| Options exercised |
— | — | — | — | ||||||
| Options forfeited or expired |
— | — | — | — | ||||||
| Options outstanding at December 31, 2009 |
19,000 | $ | 17.20 | 6.0 years | $ | 311,865 | ||||
| Options exercisable at December 31, 2009 |
19,000 | $ | 17.20 | 6.0 years | $ | 311,865 | ||||
All options are fully vested and exercisable at December 31, 2009. No options were exercised in the year ended December 31, 2009 or 2008. There were 2,000 options exercised in the year ended December 31, 2007 with a total intrinsic value of $14,120. There were no options granted during 2009, 2008 or 2007. No compensation expense related to stock option grants was recorded in the years ended December 31, 2009, 2008 or 2007.
Non-vested Stock
The Company issues stock-based compensation to employees in the form of restricted stock, which is an award of common stock subject to certain restrictions. The awards, which the Company calls nonvested shares, generally vest over a five year period, conditioned on continued employment for the full incentive period. Compensation expense for the restricted stock is recognized for the awards that are expected to vest. The expense is based on the fair value of the awards on the date of grant recognized on a straight-line basis over the requisite service period, which generally relates to the vesting period.
During 2009, 2008 and 2007, respectively, 238,028, 149,095 and 181,071 non-vested shares were granted to employees pursuant to the 2005 Long-Term Incentive Plan. These shares vest over a five year period.
The Company also issues restricted stock to its non-employee members of the Company’s Board of Directors. During 2009, 2008 and 2007, respectively, 14,000, 16,100 and 16,100 non-vested shares of stock were granted to the Company’s independent directors under the 2005 Director Compensation Plan. New non-employee directors receive an initial grant of non-vested shares in which one third of these shares vest immediately and the remaining vest over the two year period following the grant date. Additionally, the 2005 Director Compensation Plan provides for annual grants of non-vested shares to non-employee directors in which the full amount of shares vests at the one year anniversary of the grant date.
The fair value of non-vested shares is determined based on the closing trading price of the Company’s shares on the grant date. The weighted average grant date fair values of non-vested shares granted during the years ended December 31, 2009, 2008 and 2007 were $20.49, $18.67 and $27.83, respectively.
F-20
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The following table represents the non-vested stock activity for the year ended December 31, 2009:
| Number of Shares |
Weighted Average Grant Date Fair Value | |||||
| Non-vested shares outstanding at January 1, 2009 |
306,406 | $ | 22.56 | |||
| Granted |
252,028 | $ | 20.40 | |||
| Vested |
(89,163 | ) | $ | 21.62 | ||
| Forfeited |
(3,138 | ) | $ | 19.60 | ||
| Non-vested shares outstanding at December 31, 2009 |
466,133 | $ | 21.88 | |||
As of December 31, 2009, there was $8.1 million of total unrecognized compensation cost related to non-vested shares granted. That cost is expected to be recognized over the weighted average period of 3.4 years. The total fair value of shares vested in the years ended December 31, 2009, 2008 and 2007 were $1.9 million, $1.3 million and $468,000, respectively. The Company records compensation expense related to non-vested share awards at the grant date for shares that are awarded fully vested and over the vesting term on a straight line basis for shares that vest over time. The Company has recorded $2.4 million, $1.9 million and $1.2 million in compensation expense related to non-vested stock grants in the years ended December 31, 2009, 2008 and 2007, respectively.
Employee Stock Purchase Plan
In 2006, the Company adopted the Employee Stock Purchase Plan allowing eligible employees to purchase the Company’s common stock at 95% of the market price on the last day of each calendar quarter. There were 250,000 shares reserved for the plan. During 2008 and 2007, the Company issued 22,988 shares and 16,893 shares, respectively. The Company issued 24,792 shares of common stock under the plan at a weighted average per share price of $24.97 during the year ended December 31, 2009. At December 31, 2009 there were 178,231 shares available for future issuance.
Treasury Stock
In conjunction with the vesting of the non-vested shares of stock, recipients incur withholding tax liabilities. The Company allows the holders to turn in shares of common stock to satisfy those tax obligations. The Company redeemed 19,102, 7,202 and 370 shares of common stock related to these tax obligations at December 31, 2009, 2008 and 2007, respectively.
Issuance of Common Stock
As discussed in Note 3 to these consolidated financial statements, during 2008, the Company issued 51,736 shares of common stock to purchase an additional ownership percentage in one of its majority-owned hospitals. The stock was valued as of May 14, 2008, the effective date of the acquisition.
8. Leases
In certain instances, state laws may prohibit the sale of a home nursing agency or hospitals may be reluctant to sell their home health agencies. In these instances, the Company, through its wholly owned subsidiaries, enters into a lease agreement for a Medicare and Medicaid license, as well as the associated provider number to provide home health or hospice services. As of December 31, 2009, the Company had four license lease arrangements to operate five home nursing agencies and three hospice agencies.
Two of the leases were entered into in 2007 and expire in 2017. Expense related to these leases was $260,000 in 2009 and 2008. Payments due under these leases are $270,000 in 2010.
Two of the leases were entered into in 2005 and expire in 2010. Expense related to these leases was $215,123 in 2009 and $186,000 in 2008. The lease payments associated with these leases are based on a percentage of net quarterly profits; therefore, the future payments will vary with the future profits.
The Company leases office space and equipment at its various locations. Many of the leases contain renewal options with varying terms and conditions. Management expects that in the normal course of business, expiring leases will be renewed or, upon making a decision to relocate, replaced by leases for new locations. Operating lease terms range from three to ten years. Rent expense includes
F-21
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
insurance, maintenance, and other costs as required by the lease. Total rental expense was approximately $13.8 million in 2009, $10.6 million in 2008 and $8.1 million in 2007. Future minimum rental commitments under non-cancelable operating leases are as follows (in thousands):
| 2010 |
$ | 11,062 | |
| 2011 |
7,223 | ||
| 2012 |
5,152 | ||
| 2013 |
3,550 | ||
| 2014 |
1,406 | ||
| Thereafter |
987 | ||
| $ | 29,380 | ||
As of December 31, 2009, future minimum payments by year and in the aggregate, under non-cancelable capital leases with initial terms of one year or more, consisted of the following (in thousands):
| 2010 |
$ | 28 | |
| 2011 |
17 | ||
| 2012 |
— | ||
| 2013 |
— | ||
| 2014 |
— | ||
| Thereafter |
— | ||
| Total minimum lease payments |
45 | ||
| Current portion of capital lease obligations |
28 | ||
| Capital lease obligations, long-term |
$ | 17 | |
The cost of assets held under capital leases was $531,000 at both December 31, 2009 and 2008. The related accumulated amortization was $456,000 at December 31, 2009 and 2008.
9. Employee Benefit Plan
Defined Contribution Plan
The Company sponsors a 401(k) plan to all eligible full-time employees. The plan allows participants to contribute up to 15% of their compensation and allows discretionary Company contributions as determined by the Company’s Board of Directors. Effective January 1, 2006, the Company implemented a discretionary match of up to two percent of participating employee contributions. The employer contribution will vest 20% after two years and 20% each additional year until it is fully vested in year six. Contribution expense to the Company was $2.2 million, $1.4 million and $1.1 million in 2009, 2008 and 2007.
10. Commitments and Contingencies
Contingencies
The Company is involved in various legal proceedings arising in the ordinary course of business. Although the results of litigation cannot be predicted with certainty, management believes the outcome of pending litigation will not have a material adverse effect, after considering the effect of the Company’s insurance coverage, on the Company’s consolidated financial statements.
Joint Venture Buy/Sell Provisions
Several of the Company’s joint ventures include a buy/sell option that grants to the Company and its joint venture partners the right to require the other joint venture party to either purchase all of the exercising member’s membership interests or sell to the exercising member all of the non-exercising member’s membership interest, at the non-exercising member’s option, within 30 days of the receipt of notice of the exercise of the buy/sell option. In some instances, the purchase price is based on a multiple of the historical or future earnings before income taxes and depreciation and amortization of the equity joint venture at the time the buy/sell option is exercised. In other instances, the buy/sell purchase price will be negotiated by the partners and subject to a fair market valuation process. The Company has not received notice from any joint venture partners of their intent to exercise the terms of the buy/sell agreement nor has the Company notified any joint venture partners of its intent to exercise the terms of the buy/sell agreement.
Noncontrolling Interest- Redeemable
A majority of the Company’s joint venture agreements include a provision that requires the Company to purchase the noncontrolling partner’s interest upon the occurrence of certain triggering events, such as death or bankruptcy of the partner or the partner’s exclusion from the Medicare or Medicaid programs. These triggering events and the related repurchase provisions are specific to each individual joint venture; if the repurchase provision is triggered in any one joint venture, the remaining joint ventures would not be impacted. Upon the occurrence of a triggering event, the Company would be required to purchase the noncontrolling partner’s interest at either the fair value or the book value at the time of purchase as stated in the agreement. Historically, no triggering event has occurred, and we believe the likelihood of a triggering event occurring is remote. The Company has never been required to purchase the noncontrolling interest of any of its joint venture partners. According to authoritative guidance, redeemable noncontrolling interests must be reported outside of permanent equity on the consolidated balance sheet in instances where there is a repurchase provision with a triggering event that is outside the control of the Company. The Company had 51 joint venture agreements with these repurchase provisions resulting in total noncontrolling interests - redeemable of $13.8 million and $6.7 million at December 31, 2009 and 2008, respectively.
Compliance
The laws and regulations governing the Company’s operations, along with the terms of participation in various government programs, regulate how the Company does business, the services offered and interactions with patients and the public. These laws and regulations and their interpretations are subject to frequent change. Changes in existing laws or regulations, or their interpretations, or the enactment of new laws or regulations could materially and adversely affect the Company’s operations and financial condition.
F-22
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The Company is subject to various routine and non-routine governmental reviews, audits and investigations. In recent years, federal and state civil and criminal enforcement agencies have heightened and coordinated their oversight efforts related to the health care industry, including with respect to referral practices, cost reporting, billing practices, joint ventures and other financial relationships among health care providers. Violation of the laws governing the Company’s operations, or changes in the interpretation of those laws, could result in the imposition of fines, civil or criminal penalties, the termination of the Company’s rights to participate in federal and state-sponsored programs and the suspension or revocation of the Company’s licenses.
If the Company’s LTACHs fail to meet or maintain the standards for Medicare certification as LTACHs, such as average minimum length of patient stay, they will receive payments under the prospective payment system applicable to general acute care hospitals rather than payment under the system applicable to LTACHs. Payments at rates applicable to general acute care hospitals would likely result in the Company receiving less Medicare reimbursement than currently received for patient services. Moreover, all but one of the Company’s long-term acute care hospitals are subject to additional Medicare criteria because they operate as separate hospitals located in space leased from and located in, a general acute care hospital, known as a host hospital. This is known as a “hospital within a hospital” model. These additional criteria include requirements concerning financial and operational separateness from the host hospital.
The Company anticipates there may be changes to the standard episode-of-care payment from Medicare in the future. Due to the uncertainty of the revised payment amount, the Company cannot estimate the impact that changes in the payment rate, if any, will have on its future financial statements.
The Company believes that it is in material compliance with all applicable laws and regulations. As previously reported, the Company received an administrative subpoena from the Inspector General of the Office of Personnel Management (“OPM”). OPM is an administrative agency responsible for overseeing the Federal Employees Health Benefit Program (“FEHBP”). Although the subpoena was issued by OPM, the Company learned on July 9, 2009 that the scope of the review is not limited to the FEHBP, but also extends to services provided to Medicare beneficiaries. The focus of the review is on third-party quality improvement audits performed on the Company’s behalf by a third party consultant from 2005 to present. The Company will continue to cooperate and provide responsive information for the OPM review.
As previously reported, the Company has a qui tam lawsuit filed in Tennessee entitled United States of America ex rel Sally Christine Summers v. LHC Group, Inc. which alleged a violation of the False Claims Act at a single agency. The Company has received the district court’s order dismissing the case. The plaintiff is now appealing the court’s dismissal, and the Company continues to respond as necessary and appropriate.
Except as discussed in the preceding paragraphs, the Company is not aware of any pending or threatened investigations involving allegations of potential wrongdoing. While no such regulatory inquiries have been made, compliance with such laws and regulations can be subject to future government review and interpretation as well as significant regulatory action, including fines, penalties and exclusion from the Medicare program.
11. Segment Information
The Company’s segments consist of (a) home-based services and (b) facility-based services. Home-based services include home nursing services and hospice services. Facility-based services include long-term acute care services. The accounting policies of the segments are the same as those described in the summary of significant accounting policies.
F-23
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
| Year Ended December 31, 2009 | ||||||||||||
| Home-Based Services |
Facility-Based Services |
Total | ||||||||||
| (In thousands) | ||||||||||||
| Net service revenue |
$ | 469,470 | $ | 62,510 | $ | 531,980 | ||||||
| Cost of service revenue |
234,131 | 36,384 | 270,515 | |||||||||
| Provision for bad debts |
4,199 | 525 | 4,724 | |||||||||
| General and administrative expenses |
155,670 | 16,025 | 171,695 | |||||||||
| Operating income |
75,470 | 9,576 | 85,046 | |||||||||
| Interest expense |
(126 | ) | (16 | ) | (142 | ) | ||||||
| Non operating (loss) income, including gain on sale of assets |
(299 | ) | 38 | (261 | ) | |||||||
| Income from continuing operations before income taxes and noncontrolling interest |
75,045 | 9,598 | 84,643 | |||||||||
| Income tax expense |
24,082 | 2,661 | 26,743 | |||||||||
| Income from continuing operations |
50,963 | 6,937 | 57,900 | |||||||||
| Noncontrolling interest |
12,527 | 1,446 | 13,973 | |||||||||
| Total assets |
$ | 279,416 | $ | 26,817 | $ | 306,233 | ||||||
| Year Ended December 31, 2008 | ||||||||||||
| Home-Based Services |
Facility-Based Services |
Total | ||||||||||
| (In thousands) | ||||||||||||
| Net service revenue |
$ | 326,041 | $ | 56,550 | $ | 382,591 | ||||||
| Cost of service revenue |
154,376 | 31,878 | 186,254 | |||||||||
| Provision for bad debts |
10,208 | 1,563 | 11,771 | |||||||||
| General and administrative expenses |
109,917 | 14,157 | 124,074 | |||||||||
| Operating income |
51,540 | 8,952 | 60,492 | |||||||||
| Interest expense |
(377 | ) | (81 | ) | (458 | ) | ||||||
| Non operating income, including gain on sale of assets |
1,246 | 182 | 1,428 | |||||||||
| Income from continuing operations before income taxes and noncontrolling interest |
52,409 | 9,053 | 61,462 | |||||||||
| Income tax expense |
16,029 | 2,779 | 18,808 | |||||||||
| Income from continuing operations |
36,380 | 6,274 | 42,654 | |||||||||
| Noncontrolling interest |
10,219 | 1,457 | 11,676 | |||||||||
| Total assets |
$ | 220,822 | $ | 22,578 | $ | 243,400 | ||||||
F-24
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
| Year Ended December 31, 2007 | ||||||||||||
| Home-Based Services |
Facility-Based Services |
Total | ||||||||||
| (In thousands) | ||||||||||||
| Net service revenue |
$ | 244,107 | $ | 52,910 | $ | 297,017 | ||||||
| Cost of service revenue |
116,962 | 33,076 | 150,038 | |||||||||
| Provision for bad debts |
9,426 | 2,822 | 12,248 | |||||||||
| General and administrative expenses |
80,595 | 15,355 | 95,950 | |||||||||
| Operating income |
37,124 | 1,657 | 38,781 | |||||||||
| Interest expense |
(250 | ) | (107 | ) | (357 | ) | ||||||
| Non operating income, including gain on sale of assets |
746 | 313 | 1,059 | |||||||||
| Income from continuing operations before income taxes and noncontrolling interest |
37,620 | 1,863 | 39,483 | |||||||||
| Income tax expense |
8,219 | 3,978 | 12,197 | |||||||||
| Income from continuing operations |
29,401 | (2,115 | ) | 27,286 | ||||||||
| Noncontrolling interest |
5,177 | 135 | 5,312 | |||||||||
| Total assets |
$ | 151,540 | $ | 23,445 | $ | 174,985 | ||||||
12. Fair Value of Financial Instruments
The carrying value of the Company’s long-term debt is based on the current interest rates on the Company’s variable debt and approximates its fair value. The carrying amounts of the Company’s cash, receivables, accounts payable and accrued liabilities approximate their fair values because of their short maturity.
13. Allowance for Uncollectible Accounts
The following table summarizes the activity and ending balances in the allowance for uncollectible accounts:
| Beginning of Year Balance |
Additions and Expenses |
Deductions | End of Year Balance | |||||||||
| (In thousands) | ||||||||||||
| Year ended December 31: |
||||||||||||
| 2009 |
$ | 9,976 | $ | 4,724 | $ | 6,438 | $ | 8,262 | ||||
| 2008 |
8,953 | 12,463 | 11,440 | 9,976 | ||||||||
| 2007 |
5,769 | 13,817 | 10,633 | 8,953 | ||||||||
14. Concentration of Risk
The Company’s Louisiana facilities accounted for approximately 34.0%, 41.9% and 50.9% of net service revenue during the years ended December 31, 2009, 2008 and 2007 respectively. Any material change in the current economic or competitive conditions in Louisiana could have a disproportionate effect on the Company’s overall business results.
F-25
Table of Contents
LHC GROUP, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
15. Unaudited Summarized Quarterly Financial Information
The following table presents the Company’s audited quarterly results of operations (amounts in thousands, except share data):
| First Quarter 2009 | Second Quarter 2009 | Third Quarter 2009 | Fourth Quarter 2009 | |||||||||
| (In thousands) | ||||||||||||
| Net service revenue |
$ | 124,457 | $ | 133,175 | $ | 132,856 | $ | 141,492 | ||||
| Gross margin |
62,362 | 66,136 | 63,331 | 69,636 | ||||||||
| Net income attributable to LHC Group, Inc. |
11,081 | 10,262 | 9,832 | 12,666 | ||||||||
| Net income available to common stockholders |
11,109 | 10,282 | 9,829 | 12,666 | ||||||||
| Basic earnings per share |
||||||||||||
| Net income attributable to LHC Group, Inc. |
$ | 0.62 | $ | 0.57 | $ | 0.55 | $ | 0.70 | ||||
| Diluted earnings per share |
||||||||||||
| Net income attributable to LHC Group, Inc. |
$ | 0.62 | $ | 0.57 | $ | 0.54 | $ | 0.70 | ||||
| Weighted average shares outstanding |
||||||||||||
| Basic |
17,924,238 | 17,959,823 | 17,971,352 | 17,985,169 | ||||||||
| Diluted |
17,991,618 | 18,030,373 | 18,116,984 | 18,169,052 | ||||||||
| First Quarter 2008 | Second Quarter 2008 | Third Quarter 2008 | Fourth Quarter 2008 | |||||||||
| (In thousands) | ||||||||||||
| Net service revenue |
$ | 83,281 | $ | 89,934 | $ | 97,990 | $ | 111,386 | ||||
| Gross margin |
42,162 | 45,159 | 50,783 | 58,233 | ||||||||
| Net income attributable to LHC Group, Inc. |
5,338 | 6,334 | 8,032 | 10,498 | ||||||||
| Net income available to common stockholders |
5,439 | 6,298 | 8,003 | 10,493 | ||||||||
| Basic and Diluted earnings per share |
||||||||||||
| Net income attributable to LHC Group, Inc. |
$ | 0.30 | $ | 0.35 | $ | 0.45 | $ | 0.58 | ||||
| Net income available to common shareholders |
$ | 0.31 | $ | 0.35 | $ | 0.45 | $ | 0.58 | ||||
| Weighted average shares outstanding |
||||||||||||
| Basic |
17,800,066 | 17,849,820 | 17,881,228 | 17,891,426 | ||||||||
| Diluted |
17,813,967 | 17,883,964 | 17,976,305 | 17,993,815 | ||||||||
Because of the method used to calculate per share amounts, quarterly per share amounts may not necessarily total to the per share amounts for the entire year.
F-26
Table of Contents
Pursuant to the requirements of Section 13 or 15 (d) of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned thereunto duly authorized.
| LHC GROUP, INC. |
| /S/ KEITH G. MYERS |
| Keith G. Myers |
| President and Chief Executive Officer |
Date March 15, 2010
KNOW ALL MEN BY THESE PRESENTS, that each person whose signature appears below constitutes and appoints Keith G. Myers and Peter J. Roman and either of them (with full power in each to act alone) as true and lawful attorneys-in-fact with full power of substitution, for him and in his name, place and stead, in any and all capacities, to sign any and all amendments to this Annual Report on Form 10-K and to file the same, with all exhibits thereto and other documents in connection therewith, with the Securities and Exchange Commission, hereby ratifying and confirming all that said attorneys-in-fact, or their substitute or substitutes, may lawfully do or cause to be done by virtue hereof.
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed by the following persons on behalf of the registrant and in the capacities and on the dates indicated.
| Signature |
Title |
Date | ||||
| /S/ KEITH G. MYERS | Chief Executive Officer, President and Chairman of the Board of Directors |
March 15, 2010 | ||||
| Keith G. Myers | ||||||
| /S/ PETER J. ROMAN | Executive Vice President, Chief Financial Officer |
March 15, 2010 | ||||
| Peter J. Roman | ||||||
| /S/ JOHN L. INDEST | Director | March 15, 2010 | ||||
| John L. Indest | ||||||
| /S/ DAN S. WILFORD | Director | March 15, 2010 | ||||
| Dan S. Wilford | ||||||
| /S/ RONALD T. NIXON | Director | March 15, 2010 | ||||
| Ronald T. Nixon | ||||||
| /S/ TED W. HOYT | Director | March 15, 2010 | ||||
| Ted W. Hoyt | ||||||
| /S/ GEORGE A. LEWIS | Director | March 15, 2010 | ||||
| George A. Lewis | ||||||
| /S/ JOHN B. BREAUX | Director | March 15, 2010 | ||||
| John B. Breaux | ||||||
| /S/ MONICA F. AZARE | Director | March 15, 2010 | ||||
| Monica F. Azare | ||||||
| /S/ W.J. “BILLY” TAUZIN | Director | March 15, 2010 | ||||
| W.J. “Billy” Tauzin | ||||||
| /S/ KENNETH E. THORPE | Director | March 15, 2010 | ||||
| Kenneth E. Thorpe | ||||||
Table of Contents
| Exhibit Number |
Description of Exhibits | |
| 3.1 | Certificate of Incorporation of LHC Group, Inc. (previously filed as an exhibit to the Form S-1/A (File No. 333-120792) on February 14, 2005). | |
| 3.2 | Bylaws of LHC Group, Inc., as amended on December 3, 2007 (previously filed as Exhibit 3.2 to the Form 10-Q on May 9, 2008) | |
| 3.3 | Certificate of Designations (previously filed as Exhibit B to Exhibit 4.1 to the Form 8-A12B on March 11, 2008). | |
| 4.1 | Specimen Stock Certificate of LHC’s Common Stock, par value $0.01 per share (previously filed as an exhibit to the Form S-1/A (File No. 333-120792) on February 14, 2005). | |
| 4.2 | Reference is made to Exhibits 3.1 and 3.2 (previously filed as an exhibit to the Form S-1/A (File No. 333-120792) on February 14, 2005 and May 9, 2005, respectively). | |
| 4.3 | Stockholder Protection Rights Agreement, Dated March 10, 2008 by and between LHC Group, Inc. and Computershare Trust Company, N.A., as rights agent (previously filed as Exhibit 4.1 to the Form 8-A12B on March 11, 2008). | |
| 10.1 | LHC 2003 Key Employee Equity Participation Plan (previously filed as an exhibit to the Form S-1/A (File No. 333-120792) on November 26, 2004).+ | |
| 10.2 | LHC Group, Inc. 2005 Long-Term Incentive Plan (previously filed as an exhibit to the Form S-1/A (File No. 333-120792) on February 14, 2005). + | |
| 10.3 | Form of Award under LHC Group, Inc. 2005 Director Compensation Plan. (previously filed as an exhibit to the Form S-1/A (File No. 333-120792) on February 14, 2005). + | |
| 10.4 | Form of Indemnity Agreement between LHC Group and directors and certain officers (previously filed as an exhibit to the Form S-1/A (File No. 333-120792) on February 14, 2005). + | |
| 10.5 | LHC Group, Inc. 2005 Director Compensation Plan (previously filed as an exhibit to the Form S-1/A (File No. 333-120792) on February 14, 2005). + | |
| 10.6 | Amendment to LHC Group, Inc. 2005 Director Compensation Plan (previously filed as Exhibit 99.1 to the Form 8-K on June 12, 2006). | |
| 10.7 | LHC Group, Inc. 2006 Employee Stock Purchase Plan (previously filed as Exhibit 99.2 to the Form 8-K on June 12, 2006). + | |
| 10.8 | Severance and Consulting Agreement by and between LHC Group, Inc. and Barry E. Stewart, dated August 15, 2007 (previously filed as Exhibit 10.1 to the Form 8-K on August 15, 2007). | |
| 10.9 | Employment Agreement by and between LHC Group, Inc. and Don Stelly, dated October 22, 2007 (previously filed as Exhibit 10.1 to the Form 8-K on October 30, 2007). + | |
| 10.10 | Employment Agreement between LHC Group, Inc. and Keith G. Myers dated January 1, 2008 (previously filed as Exhibit 10.1 to the Form 8-K on January 4, 2008 ). + | |
| 10.11 | Employment Agreement between LHC Group, Inc. and John L. Indest dated January 1, 2008 (previously filed as Exhibit 10.2 to the Form 8-K on January 4, 2008). + | |
| 10.12 | Employment Agreement by and between LHC Group, Inc. and Peter Roman, dated January 1, 2008 (previously filed as Exhibit 10.3 to the Form 8-K on January 4, 2008). + | |
Table of Contents
| Exhibit Number |
Description of Exhibits | |
| 10.13 | Employment Agreement between LHC Group, Inc. and Daryl Doise dated January 1, 2008 (previously filed as Exhibit 10.4 to the Form 8-K on January 4, 2008). + | |
| 10.14 | Loan Agreement by and between LHC Group, Inc., Palmetto Express, L.L.C. and Capital One, National Association dated February 6, 2008 (previously filed as Exhibit 10.1 to the Form 8-K on February 13, 2008). | |
| 10.15 | Amended and Restated Credit Agreement by and among LHC Group, Inc., Capital One, National Association, First Tennessee Bank, N.A. and Brand Banking and Trust Company, dated June 12, 2008 (previously filed as Exhibit 10.1 to the Form 8-K on June 17, 2008). | |
| 10.16 | First Amendment to Amended and Restated Credit Agreement by and among LHC Group, Inc., Capital One, National Association, Capital One Corporation, First Tennessee Bank, N.A. and Brand Banking and Trust Company, dated June 15, 2009 (previously filed as Exhibit 10.1 to the Form 8-K on June 18, 2009). | |
| 10.17 | Employment Agreement by and between LHC Group, Inc. and John L. Indest dated September 14, 2009 (previously filed as Exhibit 10.1 to the Form 10-Q on November 4, 2009).+ | |
| 10.18 | Employment Agreement by and between LHC Group, Inc. and Pete C. November dated July 25, 2008. + | |
| 10.19 | Amendment to the LHC Group, Inc. 2005 Non-Employee Directors Compensation Plan dated January 1, 2010. + | |
| 21.1 | Subsidiaries of the Registrant. | |
| 23.1 | Consent of Ernst & Young LLP. | |
| 23.2 | Consent of KPMG LLP. | |
| 31.1 | Certification of Keith G. Myers, Chief Executive Officer pursuant to Rule 13a- 14(a)/15d-14(a), as adopted pursuant to Section 302 of the Sarbanes-Oxley Act of 2002. | |
| 31.2 | Certification of Peter J. Roman, Chief Financial Officer pursuant to Rule 13a- 14(a)/15d-14(a), as adopted pursuant to Section 302 of the Sarbanes-Oxley Act of 2002. | |
| 32.1* | Certification of the Chief Executive Officer and Chief Financial Officer pursuant to 18 U.S.C. Section 1350, as adopted pursuant to Section 906 of the Sarbanes-Oxley Act of 2002. | |
| * | This exhibit is furnished to the SEC as an accompanying document and is not deemed to be “filed” for purposes of Section 18 of the Securities Exchange Act of 1934 or otherwise subject to the liabilities of that Section, and the document will not be deemed incorporated by reference into any filing under the Securities Act of 1933. |
| + | Indicates a management contract or compensatory plan. |
