Attached files
Table of Contents
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
FORM 10-K
(Mark one)
| x | ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the fiscal year ended December 31, 2009.
OR
| ¨ | TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the transition period from to
Commission file number: 001-33930
IPC THE HOSPITALIST COMPANY, INC.
(Exact name of registrant as specified in its charter)
| Delaware | 95-4562058 | |
| (State or other jurisdiction of incorporation or organization) | (I.R.S. Employer Identification No.) | |
| 4605 Lankershim Boulevard, Suite 617 North Hollywood, California |
91602 | |
| (Address of principal executive offices) | (Zip code) | |
Registrant’s telephone number, including area code: (888) 447-2362
Securities registered pursuant to Section 12(b) of the Act:
| Title of Each Class |
Name of Each Exchange on Which Registered | |
| Common Stock, $0.001 par value | NASDAQ Global Market |
Securities registered pursuant to Section 12(g) of the Act: None
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes ¨ No x
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act. Yes ¨ No x
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes x No ¨
Indicate by check mark if disclosure of delinquent filers pursuant to Item 405 of Regulation S-K is not contained herein, and will not be contained, to the best of registrant’s knowledge, in definitive proxy or information statements incorporated by reference in Part III of this Form 10-K or amendment to this Form 10-K. x
Indicate by checkmark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer or a smaller reporting company. See the definitions of “large accelerated filer,” “accelerated filer” and “smaller reporting company” in Rule 12b-2 of the Exchange Act. (Check one)
| Large accelerated filer ¨ |
Accelerated filer x | Non-accelerated filer ¨ | Smaller reporting company | ¨ |
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Act). Yes ¨ No x
The aggregate market value of the voting common stock held by non-affiliates of the registrant was approximately $412,003,841, computed by reference to the closing price on the NASDAQ Global Market of $26.69 per share of Common Stock on June 30, 2009. For the purpose of the foregoing calculation only, all directors and executive officers of the registrant and owners of more than 5% of the registrant’s common stock are assumed to be affiliates of the registrant. This determination of affiliate status is not necessarily conclusive for any other purpose.
As of February 17, 2010, there were 16,222,298 shares of the registrant’s common stock, $0.001 par value, outstanding.
DOCUMENTS INCORPORATED BY REFERENCE:
The registrant has incorporated by reference into Part III of this Form 10-K, portions of its Proxy Statement for its 2010 Annual Meeting of Stockholders, to be filed no later than 120 days after the close of the registrant’s fiscal year ended December 31, 2009.
Table of Contents
IPC The Hospitalist Company, Inc.
FORM 10-K
ANNUAL REPORT
TABLE OF CONTENTS
| PART I | ||||
| Item 1 | 1 | |||
| Item 1A | 21 | |||
| Item 1B | 33 | |||
| Item 2 | 33 | |||
| Item 3 | 33 | |||
| Item 4 | 33 | |||
| PART II | ||||
| Item 5 | 34 | |||
| Item 6 | 37 | |||
| Item 7 | Management’s Discussion and Analysis of Financial Condition and Results of Operations |
39 | ||
| Item 7A | 51 | |||
| Item 8 | 51 | |||
| Item 9 | Changes in and Disagreements with Accountants on Accounting and Financial Disclosure |
75 | ||
| Item 9A | 75 | |||
| Item 9B | 77 | |||
| PART III | ||||
| Item 10 | 78 | |||
| Item 11 | 78 | |||
| Item 12 | Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters |
78 | ||
| Item 13 | Certain Relationships and Related Transactions, and Director Independence |
78 | ||
| Item 14 | 78 | |||
| PART IV | ||||
| Item 15 | 79 | |||
| 79 | ||||
| 82 | ||||
Table of Contents
In this Annual Report on Form 10-K (the “Report”), unless otherwise expressly stated or the context otherwise requires, “IPC,” “we,” “us” and “our” refer to IPC The Hospitalist Company, Inc., a Delaware corporation, and its wholly-owned subsidiaries, together with IPC’s affiliated professional corporations and limited liability companies (“affiliated professional organizations”). Our affiliated professional organizations are separate legal entities that provide physician services in certain states and with which we have management agreements. For financial reporting purposes we consolidate the revenues and expenses of all our practice groups that we own or manage because we have a controlling financial interest in these practices based on applicable accounting rules and as described in our accompanying financial statements. Also, unless otherwise expressly stated or the context otherwise requires, “our affiliated hospitalists” refer to physicians, nurse practitioners and physician assistants employed or contracted by either our wholly-owned subsidiaries or our affiliated professional organizations. References to “practices” or “practice groups” refer to our affiliated professional organizations and the wholly-owned subsidiaries of IPC that provide medical services, unless otherwise expressly stated or the context otherwise requires.
Forward-Looking Statements
This Report including “Management’s Discussion and Analysis of Financial Condition and Results of Operations” in Item 7 contains forward-looking statements within the meaning of the Private Securities Litigation Reform Act of 1995 regarding future events and the future results of IPC that are based on management’s current expectations, estimates, projections, and assumptions about our business. Words such as “may,” “will,” “could,” “should,” “target,” “potential,” “project,” “expects,” “anticipates,” “intends,” “plans,” “believes,” “sees,” “estimates” and variations of such words and similar expressions are intended to identify such forward-looking statements. These statements are not guarantees of future performance and involve risks, uncertainties and assumptions that are difficult to predict. Therefore, actual outcomes and results may differ materially from what is expressed or forecasted in such forward-looking statements due to numerous factors, including, but not limited to, those discussed in the “Risk Factors” in Item 1A, “Management’s Discussion and Analysis of Financial Condition and Results of Operations” in Item 7, and elsewhere in this Report as well as those discussed from time to time in our other Securities and Exchange Commission filings and reports. In addition, such statements could be affected by general industry and market conditions. Such forward-looking statements speak only as of the date of this Report or, in the case of any document incorporated by reference, the date of that document, and we do not undertake any obligation to update any forward-looking statement to reflect events or circumstances after the date of this Report, or for changes made to this document by wire services or Internet service providers. If we update or correct one or more forward-looking statements, investors and others should not conclude that we will make additional updates or corrections with respect to other forward-looking statements.
| ITEM 1. | BUSINESS |
Company Overview
We are a leading provider of hospitalist services in the United States. Hospitalist medicine is organized around inpatient care, primarily delivered in hospitals, and is focused on providing, managing and coordinating the care of hospitalized patients. We believe we are the largest dedicated hospitalist company in the United States based on revenues, patient encounters and number of affiliated hospitalists. As of December 31, 2009, our 1,036 affiliated hospitalists, including physicians, nurse practitioners and physician assistants, provide hospitalist solutions at over 475 hospitals and other inpatient facilities in 21 states. We have had more than 8.2 million patient encounters since the beginning of 2007. Collectively, our affiliated hospitalists work with more than 33,000 referring physicians and 3,100 health plans. Our early entry into the emerging hospitalist industry has permitted us to establish a reputation and leadership position that we believe is closely identified with hospitalist medicine.
1
Table of Contents
We began operating our first physician practice in 1998 and have increased the number of our practice groups to over 180 as of December 31, 2009. Since the beginning of 2007, we have acquired 27 practice groups and successfully integrated them into IPC and onto IPC-Link®, our proprietary technology-based management system. Our affiliated hospitalists are primarily full-time employees of our wholly-owned subsidiaries or our affiliated professional organizations, and we also employ over 450 other physicians and non-physician providers and contract with over 200 independent contractors, who provide episodic care as needed.
We assist hospitals and payors in improving quality of care, increasing operating efficiencies and reducing costs. Through our affiliated hospitalists, we provide, manage and coordinate the care of hospitalized patients and serve as the inpatient partner of primary care physicians and specialists, allowing them to focus their time and resources on their office based practices or their specialties. We also provide our affiliated hospitalists with the infrastructure, information management systems, specialized training programs and administrative support necessary to perform these services. We believe we are an attractive employer to hospitalists, whether practicing as individuals or in groups, because our administrative services help reduce the burden associated with managing a physician practice. Likewise, we believe hospitalists choose to affiliate with us because of our leadership position, financial resources, technology-based infrastructure, commitment to training and development, and our performance-based compensation. We provide a comprehensive solution of clinical and management experience, proprietary technology and high quality of care to healthcare constituents, which we believe provides us with a sustained competitive advantage to capitalize on the rapid growth in demand for hospitalists.
Industry Overview
Hospitalist medicine is an emerging specialty. Hospitalists focus on a patient’s care from the time of admission to discharge, working in close consultation with primary care physicians, other referring physicians and medical providers to coordinate the inpatient care delivery system and manage the entire inpatient episode of care. Hospitalists receive medical training generally in primary care, with many having experience in internal medicine, family practice or other medical specialties. Hospitalists differ from primary care physicians and specialists by treating patients only in a non-office based setting. By focusing exclusively on inpatient medicine, a hospitalist develops practice expertise in both the diagnosis and treatment of common conditions that require hospitalization and the optimization of patient care within a hospital. We believe hospitalists serve a necessary and critical role in coordinating, managing and communicating with the different healthcare constituents within the inpatient care and post-hospital settings. According to a study published in the December 20, 2007 issue of the New England Journal of Medicine, patients cared for by a hospitalist had their average length of stay shortened by 12%, or nearly half a day, compared with patients not under the care of a hospitalist. Also, according to a study published in a 2008 issue of Human Resource Management, the hospitalist model lowers the risk of patient re-admissions by 41.8%.
Hospitalists practice in inpatient facilities, including acute care hospitals, long-term acute care facilities, specialty hospitals, psychiatric facilities, rehabilitation hospitals and skilled nursing facilities. Acute care hospitals represent the largest component of inpatient facilities in which hospitalists practice. According to a survey conducted by the American Hospital Association in 2008, there are approximately 5,800 registered hospitals in the United States with approximately 37.5 million patient admissions. In 2007 the average length of stay was approximately 5.5 days. In 2007, total U.S. spending on hospital care was $697 billion and is expected to grow at a compound annual growth rate of approximately 7.0% to $1,374 billion in 2018 according to the Centers for Medicare and Medicaid Services.
Hospitalists assume the inpatient care responsibilities that are otherwise provided by the primary care physician or attending physician and are reimbursed by third parties using the same visit-based or procedural billing codes as would be used by the primary care physician or attending physician. By practicing each day in the same facility, hospitalists perform consistent functions, interact regularly with the same healthcare
2
Table of Contents
professionals and become highly accustomed to specific facility processes, which can result in greater efficiency, less process variability and better patient outcomes. We believe hospitalists are better able to achieve these results because of their exclusive focus on inpatient care without the inherent distraction of balancing both inpatient and outpatient care responsibilities. Likewise, we believe hospitalists generate operating and cost efficiencies by managing the treatment of a large number of patients with similar clinical needs.
According to the Society of Hospitalist Medicine (SHM), the number of hospitalists has grown from an estimated 800 in the mid-1990s to approximately 30,000 in 2010, making it one of the fastest-growing medical disciplines in the United States. A study by the American Hospital Association released in 2008 indicates that over 50% of all hospitals have formal hospitalist programs and we believe based on our operational experience that a greater number of hospitals have hospitalists practicing within their facilities.
We believe the growing demand for hospitalists is primarily driven by five significant changes in the healthcare delivery system:
| • | The primary care physician’s role in hospital care is decreasing due to the increasingly specialized nature of hospital care, the demands of treating higher acuity patients in an outpatient setting and the desire to reduce on-call obligations; |
| • | Hospitals have a greater need for consistent on-site physician availability, due to the need to admit patients from the emergency room, the increasing severity of illness required to justify hospital admissions and external pressures to decrease the length of inpatient stays; |
| • | Specialists have an increased desire to limit their practice to their medical specialty; |
| • | National residency accreditation organizations have established limitations on the number of hours that resident physicians in training may practice; and |
| • | Health plans are seeking alternative mechanisms to appropriately control the substantial increase in inpatient expenditures. |
Our Company and Our Solution
We seek to provide high-quality professional medical care for patients while reducing the cost of care for inpatient facilities and payors. Either through our wholly-owned subsidiaries or our affiliated professional organizations, as of December 31, 2009 we employ or currently affiliate with 1,036 hospitalists, including physicians, nurse practitioners and physician assistants, who are organized into traditional medical group practices to provide hospitalist services. To enhance the efficiency of these operations, we offer our affiliated hospitalists specialized training programs, information management systems and the administrative support necessary to effectively manage these nationally integrated practice group organizations. We have entered into long-term management contracts with our affiliated professional organizations in those states where business entities, as opposed to physicians, are prohibited by statute from practicing medicine and include these entities in our consolidated financial statements.
We generate approximately 94% of our net revenues through our affiliated hospitalists’ patient encounters at hospitals and other inpatient facilities including acute, sub-acute and long-term care settings. Patients are referred to our affiliated hospitalists through their community medical providers, emergency departments, payors and hospitals, in the same manner as many other medical professionals receive referrals. Third party payors and patients pay for our services in the same manner as they would pay the primary care physicians and other medical professionals who otherwise would be furnishing this direct patient care. The remainder of our revenues is substantially comprised of contracts with hospitals and other inpatient facilities to provide hospitalist services.
We believe each major constituent of the healthcare delivery system, including patients, primary care physicians, specialists, acute care hospitals, alternative sites of inpatient care, and health plans, can benefit from better coordinated inpatient care. We are positioned to assist each of these constituents in finding solutions to many of the challenges associated with patient care at inpatient facilities.
3
Table of Contents
Patients
Patients frequently experience medical conditions at unpredictable times and may require admission to a hospital when their primary care physician is unavailable or patients may not have a primary care physician. The quality or the perception of the care received by the patient may suffer as a result of the limited availability of dedicated physicians in the inpatient setting to answer patient questions and provide continuity throughout the inpatient experience. Uncoordinated communication between healthcare providers, patients and family members often negatively affects the inpatient experience and may also impact patient outcomes.
In addition to providing medical services, our affiliated hospitalists are trained to serve as team leaders in coordinating inpatient care and providing a consistent, single point of contact for patients, family members and medical professionals. Our affiliated hospitalists facilitate the communication of patient information in the inpatient setting and, after the patient is discharged, often assist with the transition to outpatient or other post-hospital care by communicating with the outpatient physician provider. In the event a patient does not have a primary care physician, our hospitalists refer the patient to physicians or clinics in the area.
Primary Care Physicians
Primary care physicians are typically focused on treating patients in an office-based setting, not an inpatient facility. The time spent making hospital rounds may reduce the time available for primary care physicians to treat patients in their offices, which can result in lower earnings for the physician. In addition, an inpatient’s medical needs may be unpredictable and require the primary care physician to provide off-hour attention and unscheduled care. Even within the confines of the provision of office-based services, the burden on primary care physicians is increasing because of the continuing reduction in the average length of inpatient stays and the corresponding increase in the acuity of patients treated in an outpatient setting.
We train and support our affiliated hospitalists to manage the care of hospitalized patients, enabling them to assume the inpatient care responsibilities that were previously provided by the primary care physician. As a result of our services, primary care physicians have the opportunity to spend more time treating office-based patients, which may increase their earnings. Our hospitalist programs result in reduced on-call time for primary care physicians and relieve practice demands during evenings and weekends. Our affiliated hospitalists also coordinate the discharge and transition of inpatients to outpatient care by communicating with patients’ primary care physicians after discharge from an inpatient facility. We believe that this communication also enhances patients’ continuity of care.
Specialists
Specialist physicians are trained to focus on specific procedures or medical conditions. As a result, specialists often desire to limit their practice to their medical specialty. Hospitalized patients, however, frequently experience multiple medical conditions that require consideration and coordination among several specialists and other care providers. For example, an orthopedic surgeon treating an elderly patient must consider the patient’s other medical conditions, such as diabetes or hypertension, which can be treated by our affiliated hospitalists or other healthcare providers.
Our affiliated hospitalists focus on the needs of hospitalized patients, thereby relieving specialists of primary responsibility for certain unrelated clinical issues in the inpatient setting and providing these specialists with an opportunity to focus on their specialty. We believe that this enhances the productivity of specialists. Our affiliated hospitalists also serve as a liaison between specialists and patients, primary care physicians, other care providers, and family members.
Acute Care Hospitals
Acute care hospitals must provide consistent and reliable care despite potentially having hundreds of admitting physicians who each have their own methods of care, preferences for medications and differing utilization and review processes. The resulting process variability can lead to an increased number of clinical
4
Table of Contents
errors, higher medical costs and deficiencies in medical record documentation which can lead to reimbursement and regulatory issues. Additionally, acute care hospitals may experience difficulty finding available physicians because of the reluctance of some medical staff members to assume the care of unassigned patients. This is further complicated by the statutory and organizational limitations on intern and resident duty hours. Acute care hospitals also face the challenge of providing medical care to indigent patients. Finally, acute care hospitals can often face emergency department overcrowding caused by large numbers of unassigned patients seeking admission to the hospital through the emergency department.
Our hospitalist programs are structured to provide acute care hospitals with a consistent on-site physician presence that typically results in fewer admitting physicians overseeing patients in the hospital, thereby reducing process variability and enhancing the ability to implement standardized practices. We believe our affiliated hospitalists’ consistent presence in the facilities leads to more efficient processes within the acute care hospitals, which can improve clinical outcomes, decrease average length of inpatient stay and lower costs per day. By concentrating the care of more patients with relatively fewer physicians, hospitals can more easily implement new initiatives and enhance compliance with protocols. We believe our hospitalist training programs lead to improved medical record documentation, which can improve hospital reimbursement and result in better regulatory compliance. Overall, through our hospitalist programs, we provide acute care hospitals with increased patient coverage, rapid response times, efficient management of care for insured and indigent patients and increased emergency department throughput.
Alternative Sites of Inpatient Care
Alternative sites of inpatient care, such as long-term acute care facilities, specialty hospitals, psychiatric facilities, rehabilitation hospitals and skilled nursing facilities, face many of the same challenges as acute care hospitals. Alternative sites of inpatient care may face additional challenges related to the narrow breadth of physician coverage that is typically available at such sites.
Our affiliated hospitalists provide alternative sites of inpatient care with consistent on-site physician availability and experience, which we believe benefits the alternative site of inpatient care by providing a single point of contact and enhances regular communication with other healthcare constituents outside the site of care. By coordinating inpatient care at such facilities, we believe our affiliated hospitalists manage the appropriate utilization of patient care to the benefit of both the facility and the patient.
Health Plans
Health plans face significant increases in costs caused by inconsistent healthcare practices, redundant diagnostic tests, inefficient discharge coordination between hospitals and outpatient physician providers and process variability. In addition, health plans can incur additional costs when their members are admitted to hospitals by physicians who are not credentialed by their plan.
Health plans contract with our credentialed affiliated hospitalists to provide in-network coverage for hospitalized members. We believe our affiliated hospitalists provide consistent healthcare practices, coordinate ordering of diagnostic tests with outpatient physician providers and reduce process variability, resulting in reduced medical costs for health plans while promoting quality of care.
Our Services
We provide our affiliated hospitalists with administrative and professional services to support their practice of medicine, reduce their administrative burden and improve their operating efficiencies.
Information Management System. We provide our affiliated hospitalists with access to IPC-Link® through our web-based “Virtual Office” portal to support their clinical, administrative and communications needs. IPC-Link® is distinctive in its ability to capture the results of each doctor-patient encounter and organize these
5
Table of Contents
results into a searchable database. IPC-Link® enables our affiliated hospitalists to view and record important patient data, and allows hospitalists in a practice group to share patient information as needed. Additionally, the technology enables our affiliated hospitalists to communicate directly and securely to our clinical call center, risk management, and compliance departments. IPC-Link® operates via a secure, HIPAA-compliant web interface, which allows us to assume responsibility for billing, collection and reimbursement for services rendered by our affiliated hospitalists.
Transition Management. We use IPC-Link® to create customized surveys for patients who are discharged to home from an inpatient facility. To assist in monitoring and documenting the patient’s discharge or transition to outpatient care, IPC-Link® provides our call center with patient information and follow-up instructions. Our system provides for our dedicated call center staff of patient representatives and nurses to contact the discharged patient, usually within 48 hours of discharge to home, to discuss the patient’s ability to understand post-discharge instructions, obtain prescribed medication, schedule an appointment with a primary care physician, and fulfill other health-related post-discharge needs. Our system enables us to identify a patient’s post-discharge medical issues on a near real-time basis, coordinate care with the appropriate care provider, improve outcomes, lower the re-admission rate into inpatient facilities, and decrease our medical malpractice risk.
Regional Management. Each of our operating regions is led by an experienced executive director and team of marketing and administrative staff that is responsible for the overall non-clinical management of our affiliated practice groups within a region, as well as coordinating hospitalist recruitment, monitoring financial performance and contracting with facilities and payors. Our regional executive directors and their staffs provide our affiliated hospitalists with direct, day-to-day access to an experienced management team that is familiar with the opportunities and challenges faced by hospitalists in a particular region.
Recruiting. As a national company, we have greater resources to commit to recruiting hospitalists than small practice groups do. We have a dedicated staff of recruiting professionals who are regionally assigned to source, screen and provide candidates to each of our local markets. Our recruiting strategy includes advertising in national physician publications and websites, exhibiting at professional association meetings, establishing a regular presence at select residency programs and leveraging our existing hospitalist relationships.
Training. We have developed extensive training programs and tools for our newly hired hospitalists and our tenured affiliated hospitalists. Our newly hired hospitalists are required to enroll in our comprehensive new-hire training program prior to treating patients. The new-hire training program emphasizes the role of the hospitalist in leading the clinical care team and provides training on billing and medical record documentation, compliance, risk management and other related topics regarding hospitalist practices. Newly hired hospitalists are also paired with experienced local hospitalists as part of the new hire training program. We provide continuing medical education programs for our existing affiliated hospitalists that are designed to enhance the skills of our affiliated hospitalists in key areas, including clinical, risk management and compliance. We sponsor local and national retreats for our affiliated hospitalists to foster better communication and learning and enhance their professional practices. Additionally, we use the automated reporting capabilities of IPC-Link® to allow our affiliated hospitalists to compare and benchmark performance metrics. This information provides positive feedback to our affiliated hospitalists when strong performance is achieved and helps to identify specific areas for improvement.
Financial Reporting. Each month we provide our practice groups with a detailed financial statement that enables each of our affiliated hospitalists to see the financial performance of their respective practices. Our incentive compensation plan is based on these financial statements and provides transparency regarding bonus compensation to our affiliated hospitalists.
Billing and Collections. We assume responsibility for all billing, reimbursement and collection processes relating to hospitalist services provided by our affiliated hospitalists and practice groups. To address the increasingly complex and time-consuming process for obtaining reimbursement for medical services, we have invested in both the technical and human resources necessary to create an efficient billing and reimbursement
6
Table of Contents
process. We provide extensive training to our affiliated hospitalists that emphasizes detailed documentation and proper coding protocol for services provided and procedures performed.
Risk Management. We provide risk management and quality management programs to our affiliated hospitalists. We take a proactive role in promoting early reporting, evaluation and resolution of incidents that may evolve into medical claims. Our risk management program includes hospitalist education and a sophisticated claims management program. The collection and analysis of claims data enables us to identify loss patterns and trends to better target risk management intervention and proactively address potential liability. Risk management education is included in our core orientation program for newly hired hospitalists, and advanced risk management topics are offered to our tenured affiliated hospitalists.
Compliance. Compliance programs are an important part of our business that permit us and our affiliated hospitalists to respond to new regulations and legislation as they arise. We have invested significant resources in developing and enhancing our compliance program, including proprietary compliance issue tracking databases, routine checks of the U.S. Department of Health and Human Services Office of the Inspector General (OIG) list of Excluded Persons or Entities, automated monitoring of key claims management processes and facility contract analysis and monitoring. We also provide comprehensive monitoring and internal auditing processes by both internal staff and third-party coding specialists. Compliance education is an important component of our new-hire training program for our entire staff.
Our Operating Structure
We are a national hospitalist group practice consisting of over 180 local practice groups operating in 16 different regions as of December 31, 2009. The practice groups within each region generally consist of all of our affiliated hospitalists that practice at a specific inpatient facility. These practice groups are supported by both dedicated local professional management teams and clinical leadership.
Operational Management Teams. Our 16 regions are each organized around a regional executive director and a small staff of marketing/practice management and administrative personnel. These management teams are responsible for strategic planning, coordinating with our national staff to recruit hospitalists, managing hospital and payor relationships and contracts, monitoring financial performance, marketing to new referral sources, credentialing with hospitals and payors, identifying new facilities in markets where we may expand our presence and managing the day-to-day non-clinical practice activities.
Clinical Leadership. Each practice group has a practice group leader who is involved in the management of the practice group, including staffing and scheduling, monitoring quality of care and financial performance, and new business initiatives. Each practice group leader is a practicing hospitalist and is part of a regional council that advises the region’s executive director, contributes to clinical leadership for the region, and engages in the planning process for the region. Each regional council appoints a representative to serve on our national advisory board, which advises our chief medical officer. We also support the regional and local clinical leadership structure with our corporate medical affairs department, which monitors company-wide clinical performance and benchmarks, develops programs and coordinates our clinical research activities.
Development and Acquisition Program
We have a dedicated development and acquisition team whose role is to execute our growth strategy by identifying and capitalizing on complementary facility contract and acquisition opportunities in new markets. In existing markets, our development and acquisition team assists the executive director for the region with growth opportunities by identifying and capitalizing on acquisitions of other local practice groups or contracting with new facilities within the region or obtaining contracts with facilities where our affiliated hospitalists are already practicing. In new markets, our development and acquisition team identifies acquisition and contract opportunities and coordinates the due diligence, negotiation and execution of these acquisitions and hospital contracts.
7
Table of Contents
Technology-Based Management System
IPC-Link® is a fully-integrated technology-based management system that supports the clinical, administrative and communication needs of our affiliated hospitalists. Our system contains proprietary software, sophisticated databases and rules engines, automated billing interfaces and extensive web-based reporting tools. We began developing the system internally more than ten years ago and have designed this system to accommodate significant future growth in our business.
Our affiliated hospitalists access IPC-Link® through our web-based “Virtual Office” portal, which can be accessed through a web browser running on any internet connected computer. This portal into the system provides our dispersed workforce with extensive resources and information content and serves as a centralized contact point for our affiliated hospitalists. The “Virtual Office” provides regional and company-wide news, clinical reference materials, an on-line library, practice schedules, access to clinical and business reports related to the practice groups, web-based continuing medical education, patient feedback, access to employee benefits plan information and a secure e-mail system with all of our employees. Our affiliated hospitalists must utilize this portal to access their clinical information and bill for their services.
Our affiliated hospitalists use IPC-Link® to record each patient encounter and are personally responsible for entering data into the system to reduce chances for error or misinterpretation by a nurse or assistant. Our system audits the billing information entered by our affiliated hospitalists for completeness and accuracy and creates an electronic billing file for automated submission to payors. IPC-Link® is distinctive in its ability to capture the results of each clinician-patient encounter and organize these results into a searchable database.
IPC-Link® technology enables our affiliated hospitalists to communicate directly and securely with referring physicians and other healthcare constituents in addition to our clinical call center, risk management and compliance departments. For example, based on information entered directly by the hospitalist, our system produces concise admission, progress and discharge notes and faxes this information to referring physicians and other healthcare constituents. Our faxed discharge notes contain key patient information for use following discharge such as diagnoses, medical tests and studies performed, consultants used, medications prescribed, home care ordered and follow-up care recommendations. IPC-Link® also alerts our call center when a patient has been discharged from the hospital to home and generates a tailored post-discharge survey that we administer to that patient by phone. IPC-Link® compiles call center findings and interventions and faxes a summary to the patient’s outpatient physician.
We also use IPC-Link® to monitor our financial and clinical performance. We create customized, web-based reports based on near real-time data to track important operating metrics, including length of stay, patient volumes and physician productivity, referral sources and trends, readmission rates, physician billings, clinical quality indicators, patient satisfaction and patient post-discharge survey results.
In addition to our intellectual property rights related to IPC-Link®, we also own certain copyrights, trademarks and trade secrets.
Contracts with Inpatient Facilities
Our affiliated hospitalists, in general, provide services in any inpatient facility where they have credentials, called privileges, regardless of whether we have entered into a contract with the inpatient facility. When we contract with hospitals and other inpatient facilities, we typically provide various professional services, including supporting the emergency department, assisting in bed allocation, planning patient discharge, coordinating with ancillary departments, cooperating with facility management, developing facility policies and procedures, training facility personnel and developing call schedules. We believe our facility contracts benefit the inpatient facility by establishing a stable and consistent provider of hospitalist services to that facility, while we benefit by having our affiliated hospitalists obtain unassigned patients through the emergency department, expand the base
8
Table of Contents
of the referral relationships within the facility and strengthen our contractual revenue base. In these contracted facilities, billings to third-party payors for direct patient care constitute the most significant source of our revenue.
The term of these contracts varies between facilities, but they typically can be terminated with cause for various reasons and usually contain provisions allowing for termination without cause by either party upon 90 days notice. Agreements with the inpatient facilities typically contain confidentiality provisions and requirements that the facilities maintain their own insurance.
Contracts with Health Plans
Our regional management teams negotiate health plan contracts on behalf of our affiliated hospitalists in their local markets. These agreements vary from plan to plan and payment is typically a negotiated fee per service. Our regional management teams assist our affiliated hospitalists with any required credentialing with these plans, provide ongoing contract management and maintain the relationships with the health plans. We believe that these health plan contracts can enhance our practices by capturing additional patient volumes as well as promoting prompt payment for services.
Affiliated Hospitalists and Practice Groups
Our practice groups and affiliated hospitalists are responsible for the provision of medical care to patients. Our affiliated hospitalists are employees of either our wholly-owned subsidiaries or affiliated professional organizations. Our affiliated professional organizations are separate legal entities, comprised of corporations, limited liability companies and limited partnerships. For financial reporting purposes, we consolidate the revenues and expenses of all our practice groups that we own or manage because we have a controlling financial interest in these practices based on applicable accounting rules as described in our accompanying financial statements. We provide all of the non-medical, administrative and management services necessary for the operations of each of our affiliated professional organizations under comprehensive long-term management agreements. Under the terms of these agreements, we are paid for the provision of these non-medical management services based upon either the financial performance of the applicable practice group or a fixed fee. Each agreement is for a term of 20 years with 10 year automatic renewal periods, which we may terminate at any time, with or without cause, with 30 days prior written notice to the affiliated professional organization. Agreements with our affiliated professional organizations contain a confidentiality provision and a power of attorney appointing our company as its attorney-in-fact.
Each affiliated professional organization is organized or qualified to do business in a state where only a physician-owned professional entity may provide medical services, and each affiliated professional organization is owned by our Chief Medical Officer, who is a physician. To ensure our continued affiliation with and management of the affiliated professional organizations, we have entered into a succession agreement with each affiliated professional organization and physician owner that prohibits the sale or transfer of the ownership interests of the affiliated professional organization to non-physicians and provides for the repurchase of such ownership interests by the affiliated professional organization for a nominal amount upon the occurrence of certain events.
Our affiliated hospitalists are employed under contracts which typically have one-year employment terms with automatic extensions. The contracts can be terminated with cause for various reasons, and generally contain provisions allowing for termination without cause by either party upon 30 to 60 days notice. Agreements with our affiliated hospitalists generally contain a confidentiality provision and a non-compete and/or non-solicitation provision. The scope and enforceability of these provisions varies from state to state.
Our affiliated hospitalists generally are paid a competitive fixed base salary, and most are eligible to participate in our physician incentive compensation plan, which provides varying bonuses based upon productivity and practice group profitability. We typically provide professional liability and workers compensation coverage, along with vacation, sick leave, continuing medical education, health, disability and 401(k) benefits.
9
Table of Contents
We also utilize the services of independent contractors for certain of our health plan contracts. The independent contractors are paid on a per case basis.
Competition
The healthcare industry is highly competitive, and the market for hospitalists within this industry is highly fragmented. We believe we are the largest dedicated hospitalist company in the United States based on revenues, patient encounters and number of affiliated hospitalists. In each of our local markets and throughout the United States, there are hospitalist groups of varying sizes, as well as privately-owned hospitalist companies, with which our practice groups compete.
Companies in other segments of the healthcare industry, such as emergency department service companies, also provide hospitalist services. Competitors of this nature on a national basis include companies such as Team Health and EmCare, each of which may have greater financial and other resources available to them, including greater access to physicians and greater access to potential customers.
In addition, because of the fragmented nature of the hospitalist market and the ability of physicians to provide services in any hospital where they have certain credentials, competition for growth in existing and expanding markets is not limited to our large competitors with substantial financial resources available to them. We also compete against local physician groups for qualified physicians, and sometimes with hospitals themselves to provide hospitalist services.
We are also dependent on our affiliated hospitalists to provide services and generate revenue. Competition for qualified physicians to act as hospitalists is intense. We compete with many types of healthcare providers, including teaching, research and government institutions, hospitals and other practice groups, for the services of such physicians.
Geographic Coverage
We currently provide services in the following 21 states: Arizona, California, Colorado, Connecticut, Delaware, Florida, Georgia, Illinois, Massachusetts, Michigan, Missouri, Nevada, New Hampshire, New Jersey, North Carolina, Ohio, Oklahoma, Pennsylvania, Rhode Island, Tennessee, and Texas. During 2009, approximately 69% of our net revenue was generated by operations in Arizona, Florida, Michigan, Missouri and Texas. In particular, Texas accounted for approximately 24% of our net revenue for 2009. Our growth strategy contemplates that we will continue to grow our business, in part, by expanding into new markets outside of the 21 states in which we currently operate.
Professional Liability and Other Insurance Coverage
Our business has an inherent risk of claims of medical malpractice against our affiliated physicians and us. We contract and pay premiums for third-party professional liability insurance that indemnifies us and our affiliated hospitalists on a claims-made basis for losses incurred related to medical malpractice litigation. Professional liability coverage is required in order for our affiliated hospitalists to maintain hospital privileges. We record in our consolidated financial statements estimates for our liabilities for self-insured deductibles and claims incurred but not reported based on actuarial loss projections using historical loss patterns. Liabilities for claims incurred but not reported are not discounted. Because many factors can affect historical and future loss patterns, the determination of an appropriate reserve involves complex, subjective judgment, and actual results may vary significantly from estimates. If the deductibles and other amounts that we are actually required to pay materially exceed our estimates, our financial condition and results of operations could be materially adversely affected.
Unlike our claims-made policy in effect prior to 2009 that contained a self-insurance retention, our 2009 claims-made policy provided first dollar coverage up to our policy limits on new claims reported in 2009. In December 2009, we renewed our annual professional liability insurance policy for 2010, effective January 1, 2010, under the same terms as our 2009 policy. There can be no assurance that we will obtain substantially similar coverage as is provided under the 2010 policy at acceptable costs and on favorable terms upon expiration.
10
Table of Contents
During the first quarter of 2010, we reached a preliminary agreement to settle a disputed professional liability claim for a prior year that is in excess of our insurance policy limit. The settlement remains subject to definitive documentation and is contingent upon receiving applicable court approval. We recorded our portion of the settlement of $0.8 million in the fourth quarter of 2009.
We believe that our insurance coverage is appropriate based upon our claims experience and the nature and risks of our business. In addition to the known incidents that have resulted in the assertion of claims, we cannot be certain that our insurance coverage will be adequate to cover liabilities arising out of claims asserted against us, our affiliated professional organizations or our affiliated hospitalists in the future where the outcomes of such claims are unfavorable. We believe that the ultimate resolution of all pending claims, including liabilities in excess of our insurance coverage, will not have a material adverse effect on our financial position, results of operations or cash flows; however, there can be no assurance that future claims will not have such a material adverse effect on our business.
We also maintain general liability, casualty, worker’s compensation, director and officer, and other third-party insurance coverage subject to deductibles and other restrictions in accordance with industry standards. We believe that our insurance coverage is appropriate based upon our claims experience and the nature and risks of our business. However, we cannot assure that any pending or future claim will not be successful or if successful will not exceed the limits of available insurance coverage.
Employees
The following is an approximate break-down of the affiliated hospitalists and non-clinical staff employed or contracted by our wholly-owned subsidiaries or our affiliated professional organizations by job classification as of December 31, 2008 and 2009:
| Job Description |
2008 | 2009 | ||
| Employed physicians |
580 | 703 | ||
| Nurse practitioners and physician assistants |
79 | 105 | ||
| Independent contracted physicians |
122 | 228 | ||
| Non-clinical employees |
369 | 415 | ||
| Total |
1,150 | 1,451 | ||
In addition to the full-time and part-time employees and independent contractors included above, we have employment agreements with over 450 other physicians and non-physician providers, who provide episodic care as needed. All of our employees and independent contractors are located in the United States. None of our employees are covered by collective bargaining agreements. We have had no labor-related work stoppages, and we believe we have positive relations with our employees.
Legal Proceedings
In the ordinary course of our business, we become involved in pending and threatened legal actions and proceedings, most of which involve claims of medical malpractice related to medical services provided by our affiliated hospitalists. We may also become subject to other lawsuits which could involve significant claims and/or significant defense costs. During the first quarter of 2010, we reached a preliminary agreement to settle a disputed professional liability claim for a prior year that is in excess of our insurance policy limit. The settlement remains subject to definitive documentation and is contingent upon receiving applicable court approval. We recorded our portion of the settlement of $0.8 million in the fourth quarter of 2009.
We believe, based upon our review of pending actions and proceedings, that the outcome of such legal actions and proceedings will not have a material adverse effect on our business. The outcome of such actions and proceedings, however, cannot be predicted with certainty and an unfavorable resolution of one or more of them could have a material adverse effect on our business in a future period.
11
Table of Contents
Company Information
Founded in 1995 by Chairman and Chief Executive Officer, Adam D. Singer, M.D., we were incorporated in Delaware in January 1998. Our principal executive offices are located at 4605 Lankershim Boulevard, Suite 617, North Hollywood, California 91602. Our telephone number is (888) 4IPC-DOC (888-447-2362). We maintain a website at www.hospitalist.com.
Available Information
Our internet website address is www.hospitalist.com. Our Annual Report on Form 10-K, Quarterly Reports on Form 10-Q, Current Reports on Form 8-K and amendments to those reports filed or furnished pursuant to Section 13 or 15(d) of the Securities Exchange Act of 1934 are available through our internet website as soon as reasonably practicable after we electronically file such material with, or furnish it to, the Securities and Exchange Commission. Our internet website and the information contained therein or connected thereto is not a part of, and is not incorporated by reference into, this Report.
REGULATORY MATTERS
Significant Federal and State Healthcare Laws Governing Our Business
As a healthcare company, our operations and relationships with healthcare providers such as hospitals, other healthcare facilities, and healthcare professionals are subject to extensive and increasing regulation by numerous federal, state, and local government entities. These laws and regulations often are interpreted broadly and enforced aggressively by multiple government agencies, including OIG, the U.S. Department of Justice, and various state authorities. We have included brief descriptions of some, but not all, of the laws and regulations that affect our business.
A finding that claims for services were not covered or not payable, or the imposition of sanctions associated with a violation of any of these healthcare laws and regulations, could have a material adverse effect on our business, financial condition and results of operations. We cannot guarantee that our arrangements or business practices will not be subject to government scrutiny or be found to violate certain healthcare laws. Government audits, investigations and prosecutions, even if we ultimately are found to be without fault, can be costly and disruptive to our business. Moreover, changes in healthcare legislation or government regulation may restrict our existing operations, limit the expansion of our business or impose additional compliance requirements and costs, any of which could have a material adverse affect on our business, financial condition and results of operations.
False Claims Acts
The federal civil False Claims Act imposes civil liability on individuals or entities that knowingly submit false or fraudulent claims for payment to the federal government. The False Claims Act provides, in part, that the federal government may bring a lawsuit against any person or entity that it believes has knowingly or recklessly presented, or caused to be presented, a false or fraudulent request for payment from the federal government, or has made a false statement or used a false record material to a false claim. Private parties may initiate qui tam whistleblower lawsuits against any person or entity under the False Claims Act in the name of the government and may share in the proceeds of a successful suit.
The federal government has used the False Claims Act to prosecute a wide variety of alleged false claims and fraud allegedly perpetrated against Medicare and state healthcare programs (Medicaid). By way of illustration, these prosecutions may be based upon alleged coding errors, billing for services not rendered, billing services at a higher payment rate than appropriate, and billing for care that is not considered medically necessary. The government and a number of courts also have taken the position that claims presented in violation of certain other statutes, including the federal Anti-Kickback Statute or the Stark Law, can be considered a violation of the False Claims Act based on the theory that a provider impliedly certifies compliance with all applicable laws, regulations, and other rules when submitting claims for reimbursement.
12
Table of Contents
Penalties for False Claims Act violations include fines ranging from $5,500 to $11,000 (as adjusted for inflation) for each false claim, plus up to three times the amount of damages sustained by the government. A False Claims Act violation may provide the basis for the imposition of administrative penalties as well as exclusion from participation in governmental healthcare programs, including Medicare and Medicaid (or, in lieu of exclusion, a Corporate Integrity Agreement entered into with OIG). In addition to the provisions of the False Claims Act, which provide for civil enforcement, the federal government also can use several criminal statutes to prosecute persons who are alleged to have submitted false or fraudulent claims for payment to the federal government.
The Fraud Enforcement and Recovery Act (FERA) of 2009 was enacted on May 20, 2009, and among other things, amends and broadens the federal civil False Claims Act. Significantly, FERA expands the government’s potential legal claims against providers and their subcontractors for failing to timely repay obligations, which under the language of the statute would generally include known overpayments. In addition, FERA clarifies that the False Claims Act applies even to claims not submitted directly to the federal government, such as provider claims to Medicaid, Medicare HMOs, or Medicaid HMOs which are submitted through Medicare contractors. FERA also facilitates increased cooperation between and enforcement efforts by various components of the federal government, co-prosecuting state agencies, and whistleblowers by allowing increased sharing of information, and significantly increasing federal funding for fraud detection and prosecution.
A number of states have enacted false claims acts that are similar to the federal False Claims Act. Even more states are expected to do so in the future because Section 6031 of the Deficit Reduction Act of 2005 (DRA) amended the federal law to encourage these types of changes, along with a corresponding increase in state initiated false claims enforcement efforts. Under the DRA, if a state enacts a false claims act that is at least as stringent as the federal statute and that also meets certain other requirements, the state will be eligible to receive a greater share of any monetary recovery obtained pursuant to certain actions brought under the state’s false claims act. The OIG, in consultation with the Attorney General of the United States, is responsible for determining if a state’s false claims act complies with the statutory requirements. Currently, 31 states and the District of Columbia have some form of state false claims acts. As of January 2010, the OIG has reviewed 20 of these and determined that fourteen of these satisfy the DRA standards, and we anticipate this figure will continue to increase. The 14 states are: California, Georgia, Hawaii, Illinois, Indiana, Massachusetts, Michigan, Nevada, New York, Rhode Island, Tennessee, Texas, Virginia and Wisconsin. Of the 21 states in which we currently operate, the following seventeen states have some form of a state false claims act : California, Colorado, Delaware, Florida, Georgia, Illinois, Massachusetts, Michigan, Missouri, Nevada, New Hampshire, New Jersey, North Carolina, Oklahoma, Rhode Island, Tennessee and Texas.
Anti-Kickback Statutes
The federal Anti-Kickback Statute contained in the Social Security Act prohibits the knowing and willful offer, payment, solicitation or receipt of any form of remuneration in return for, or to induce, (1) the referral of a beneficiary of Medicare, Medicaid or other federal healthcare programs, (2) the furnishing or arranging for the furnishing of items or services reimbursable under Medicare, Medicaid or other federal healthcare programs or (3) the purchase, lease, or order or arranging or recommending the purchasing, leasing or ordering of any item or service reimbursable under Medicare, Medicaid or other federal healthcare programs. Some courts and the OIG interpret the statute to cover any arrangement where even one purpose of the remuneration is to induce referrals. A violation of the Anti-Kickback Statute is a felony punishable by imprisonment, criminal fines of up to $25,000, civil fines of up to $50,000 per violation and three times the amount of the unlawful remuneration. A violation also can result in exclusion from Medicare, Medicaid or other federal healthcare programs.
Due to the breadth of the Anti-Kickback Statute’s broad prohibition, there are a number of statutory exceptions that protect various common business transactions and arrangements from prosecution. In addition, the OIG has published safe harbor regulations that outline arrangements that also are deemed protected from prosecution under the Anti-Kickback Statute, provided all applicable criteria are met. The failure of an activity to
13
Table of Contents
meet all of the applicable safe harbor criteria does not necessarily mean that the particular arrangement violates the Anti-Kickback Statute, but these arrangements may be subject to scrutiny by enforcement agencies.
Some states have enacted statutes and regulations similar to the Anti-Kickback Statute, but which may be applicable regardless of the payor source for the patient. These state laws may contain exceptions and safe harbors that are different from and/or more limited than those of the federal law and that may vary from state to state.
Federal Stark Law
The federal Stark Law, also known as the physician self-referral law, generally prohibits a physician from referring Medicare and Medicaid patients to an entity (including hospitals) providing “designated health services,” if the physician or a member of the physician’s immediate family has a “financial relationship” with the entity, unless a specific exception applies, and further prohibits the entity from billing for any services that arise out of such prohibited referrals. Designated health services include, among other services, inpatient and outpatient hospital services, clinical laboratory services, certain imaging services, and other items or services that our affiliated physicians may order. The prohibition applies regardless of the reasons for the financial relationship and the referral; and therefore, unlike the federal Anti-Kickback Statute, intent to violate the law is not required. Like the Anti-Kickback Statute, the Stark Law contains a number of statutory and regulatory exceptions intended to protect certain types of transactions and business arrangements from penalty. Compliance with all elements of the applicable Stark Law exception is mandatory.
The penalties for violating the Stark Law include the denial of payment for services ordered in violation of the statute, mandatory refunds of any sums paid for such services and civil penalties of up to $15,000 for each violation, and possible exclusion from future participation in the governmental healthcare programs. A person who engages in a scheme to circumvent the Stark Law’s prohibitions may be fined up to $100,000 for each applicable arrangement or scheme.
Some states have enacted statutes and regulations similar to the Stark Law, but which may be applicable to the referral of patients regardless of their payor source and which may apply to different types of services. These state laws may contain statutory and regulatory exceptions that are different from those of the federal law and that may vary from state to state.
Health Information Privacy and Security Standards
Among other directives, the Administrative Simplification Provisions of the Health Insurance Portability and Accountability Act of 1996 (HIPAA) required the federal Department of Health and Human Services (HHS) to adopt standards to protect the privacy and security of certain health-related information. The HIPAA privacy regulations contain detailed requirements concerning the use and disclosure of certain individually identifiable protected health information (PHI) by “HIPAA covered entities,” which include entities like IPC, our affiliated hospitalists, and practice groups.
In addition to the privacy requirements, HIPAA covered entities must implement certain administrative, physical, and technical security standards to protect the integrity, confidentiality and availability of certain electronic PHI received, maintained, or transmitted. HIPAA also implemented the use of standard transaction code sets and standard identifiers that covered entities must use when submitting or receiving certain electronic healthcare transactions, including activities associated with the billing and collection of healthcare claims.
The American Recovery and Reinvestment Act enacted on February 18, 2009, included the Health Information Technology for Economic and Clinical Health Act (HITECH) which modified the HIPAA legislation significantly. Pursuant to HITECH, certain provisions of the HIPAA privacy and security regulations become directly applicable to “HIPAA business associates,” which include IPC when we are working on behalf of our practice groups.
14
Table of Contents
Violations of the HIPAA privacy and security standards may result in civil and criminal penalties. Historically, these included: (1) civil money penalties of $100 per incident, to a maximum of $25,000, per person, per year, per standard violated and (2) depending upon the nature of the violation, fines of up to $250,000 and imprisonment for up to ten years. The passage of HITECH significantly modified the enforcement structure, creating a tiered system of civil money penalties that range from $100 to $50,000 per violation, with a cap of $1.5 million per year for identical violations. We must also comply with the recently promulgated “breach notification” regulations, which implement certain provisions of HITECH. Under these regulations, in addition to reasonable remediation, covered entities must promptly notify affected individuals in the case of a breach of “unsecured PHI,” which is defined by HHS guidance, as well as the HHS Secretary and the media in cases where a breach affects more than 500 individuals. Breaches affecting fewer than 500 individuals must be reported to the HHS Secretary on an annual basis. The regulations also require business associates of covered entities to notify the covered entity of breaches at or by the business associate. Formal enforcement of the new breach notification regulations will begin as of February 22, 2010 and we are taking reasonable steps to reduce the amount of unsecured PHI we handle and retain.
In light of HITECH, we expect increased federal and state HIPAA privacy and security enforcement efforts. State Attorney Generals now have the right to prosecute HIPAA violations committed against residents of their states. In addition, HITECH mandates that the Secretary of HHS conduct periodic compliance audits of HIPAA covered entities and their business associates. It also tasks HHS with establishing a methodology whereby harmed individuals who were the victims of breaches of unsecured PHI may receive a percentage of the Civil Monetary Penalty fine paid by the violator. This methodology for compensation to harmed individuals must be in place by February 17, 2012.
Many states in which we operate also have laws that protect the privacy and security of confidential, personal information. These laws may be similar to or even more protective than the federal provisions. Not only may some of these state laws impose fines and penalties upon violators, but some may afford private rights of action to individuals who believe their personal information has been misused.
Financial Information and Privacy Standards
In addition to privacy and security laws focused on health care data, multiple other federal and state laws regulate the use and disclosure of consumer’s financial information (Personal Information). Many of these laws also require administrative, technical, and physical safeguards to prevent unauthorized use or disclosure of Personal Information, including mandated processes and timeframes for notification of possible or actual breaches of Personal Information to the affected individual. The Federal Trade Commission primarily oversees compliance with the federal laws relevant to us, while state laws are addressed by the state attorney general or other accountable state agency. As with HIPAA, enforcement of laws protecting financial information is increasing. Examples of relevant federal laws include the Fair Credit Reporting Act, the Electronic Communications Privacy Act, and the Computer Fraud and Abuse Act.
Fee-Splitting and Corporate Practice of Medicine
Some states have laws that prohibit business entities, such as IPC, from practicing medicine, employing physicians to practice medicine, exercising control over medical decisions by physicians, also known collectively as the corporate practice of medicine, or engaging in certain arrangements, such as fee-splitting, with physicians. In some states these prohibitions are expressly stated in a statute or regulation, while in other states the prohibition is a matter of judicial or regulatory interpretation. Of the 21 states in which we currently operate, we believe that the following thirteen states prohibit the corporate practice of medicine: California, Colorado, Georgia, Illinois, Massachusetts, Michigan, Nevada, New Hampshire, North Carolina, Ohio, Pennsylvania, Tennessee and Texas.
In states that prohibit the corporate practice of medicine, we operate by maintaining long-term management contracts with affiliated professional organizations, which are each owned and operated by physicians and which
15
Table of Contents
employ or contract with additional physicians to provide hospitalist services. Under these arrangements, we perform only non-medical administrative services, do not represent that we offer medical services, and do not exercise influence or control over the practice of medicine by the physicians or the affiliated professional organizations.
For financial reporting purposes, however, we consolidate the revenues and expenses of all our practice groups that we own or manage because we have a controlling financial interest in these practices based on applicable accounting rules and as described in our accompanying financial statements. In states where fee-splitting is prohibited between physicians and non-physicians, the fees that we receive through our management contracts have been established on a basis that we believe complies with the applicable state laws.
Some of the relevant laws, regulations, and agency interpretations in the states in which we operate have been subject to limited judicial and regulatory interpretation. Moreover, state laws are subject to change and regulatory authorities and other parties, including our affiliated physicians, may assert that, despite these arrangements, we are engaged in the prohibited corporate practice of medicine or that our arrangements constitute unlawful fee-splitting. If this occurred, we could be subject to civil or criminal penalties, our contracts could be found legally invalid and unenforceable (in whole or in part), or we could be required to restructure our contractual arrangements.
Deficit Reduction Act of 2005
Among other mandates, the DRA created a new Medicaid Integrity Program designed to enhance federal and state efforts to detect Medicaid fraud, waste and abuse. Additionally, section 6032 of the DRA requires entities that make or receive annual Medicaid payments of $5.0 million or more from any one state to provide their employees, contractors and agents with written policies and employee handbook materials on federal and state False Claims Acts and related statues. At this time, we are not required to comply with section 6032 because we receive less than $5.0 million in Medicaid payments annually from any one state. However, we will likely be required to comply in the future as our Medicaid billings increase, but we cannot predict when that will occur. We also cannot predict what new state statutes or enforcement efforts may emerge from the DRA and what impact they may have on our operations.
Other Federal Healthcare Fraud and Abuse Laws
We are also subject to other federal healthcare fraud and abuse laws. Under HIPAA, there are two additional federal crimes that could have an impact on our business: “Health Care Fraud” and “False Statements Relating to Health Care Matters.” The Health Care Fraud statute prohibits any person from knowingly and recklessly executing a scheme or artifice to defraud any healthcare benefit program. Healthcare benefit programs include both government and private payors. A violation of this statute is a felony and may result in fines, imprisonment and/or exclusion from governmental healthcare programs.
The False Statements Relating to Health Care Matters statute prohibits knowingly and willfully falsifying, concealing or covering a material fact by any trick, scheme or device or making any materially false, fictitious or fraudulent statement in connection with the delivery of or payment for healthcare benefits, items or services. A violation of this statute is a felony and may result in fines and/or imprisonment.
The OIG may impose administrative sanctions or civil monetary penalties against any person or entity that knowingly presents or causes to be presented a claim for payment to a governmental healthcare program for services that were not provided as claimed, is fraudulent, is for a service by an unlicensed physician, or is for medically unnecessary services. Violations may result in penalties of up to $10,000 per claim, treble damages, and exclusion from governmental healthcare funded programs, such as Medicare and Medicaid. In addition, the OIG may impose administrative sanctions against any physician who knowingly accepts payment from a hospital as an inducement to reduce or limit services provided to Medicare and Medicaid program beneficiaries.
16
Table of Contents
Other State Fraud and Abuse Provisions
In addition to the state laws previously described, we also are subject to other state fraud and abuse statutes and regulations. Many of the states in which we operate have adopted a form of anti-kickback law, self-referral prohibition, and false claims and insurance fraud prohibition. The scope of these laws and the interpretations of them vary from state to state and are enforced by state courts and regulatory authorities, each with broad discretion. Generally, state laws reach to all healthcare services and not just those covered under a governmental healthcare program. A determination of liability under any of these laws could result in fines and penalties and restrictions on our ability to operate in these states. We cannot assure that our arrangements or business practices will not be subject to government scrutiny or be found to violate applicable fraud and abuse laws.
Fair Debt Collection Practices Act
Some of our operations may be subject to compliance with certain provisions of the Fair Debt Collection Practices Act and comparable statutes in many states. Under the Fair Debt Collection Practices Act, a third-party collection company is restricted in the methods it uses to contact consumer debtors and elicit payments with respect to placed accounts. Requirements under state collection agency statutes vary, with most requiring compliance similar to that required under the Fair Debt Collection Practices Act.
U.S. Sentencing Guidelines
The U.S. Sentencing Guidelines are used by federal judges in determining sentences in federal criminal cases. The guidelines are advisory, not mandatory. With respect to corporations, the guidelines state that having an effective ethics and compliance program may be a relevant mitigating factor in determining sentencing. To comply with the guidelines, the compliance program must be reasonably designed, implemented, and enforced such that it is generally effective in preventing and detecting criminal conduct. The guidelines also state that a corporation should take certain steps such as periodic monitoring and appropriately responding to detected criminal conduct. OIG has followed the model of the Sentencing Guidelines in issuing its Compliance Guidances (which also are advisory, not mandatory). While we have attempted to develop and implement our corporate compliance program to be consistent with these guidelines, we cannot be certain that a court (or the OIG) would agree.
Licensing, Certification, Accreditation and Related Laws and Guidelines
Our clinical personnel are subject to numerous federal, state and local licensing laws and regulations, relating to, among other things, professional credentialing and professional ethics. Since we perform services at hospitals and other types of healthcare facilities, we may indirectly be subject to laws applicable to those entities as well as ethical guidelines and operating standards of professional trade associations and private accreditation commissions, such as the American Medical Association and the Joint Commission. There are penalties for non-compliance with these laws and standards, including loss of professional license, civil or criminal fines and penalties, loss of hospital admitting privileges, and exclusion from participation in various governmental and other third-party healthcare programs.
Professional Licensing Requirements
Our affiliated hospitalists must satisfy and maintain their professional licensing in the states where they practice medicine. Activities that qualify as professional misconduct under state law may subject them to sanctions, or to even lose their license and could, possibly, subject us to sanctions as well. Some state boards of medicine impose reciprocal discipline, that is, if a physician is disciplined for having committed professional misconduct in one state where he or she is licensed, another state where he or she is also licensed may impose the same discipline even though the conduct occurred in another state. Professional licensing sanctions may also result in exclusion from participation in governmental healthcare programs, such as Medicare and Medicaid, as well as other third-party programs.
17
Table of Contents
RELATIONSHIPS WITH THIRD-PARTY PAYORS
Medicare, Medicaid and Other Governmental Programs
We derive a significant portion of our revenue from services rendered to beneficiaries of Medicare, Medicaid and other governmental healthcare programs. Participation in these programs requires compliance with stringent and often complex enrollment and reimbursement requirements. The applicable standards are subject to statutory and regulatory changes, administrative rulings, and new interpretations of policy that may be difficult to predict and that may require significant changes to our operations.
Our reimbursement typically is conditioned on our affiliated hospitalists providing the correct procedure and diagnosis codes and properly documenting both the service itself and the medical necessity for the service. Incorrect or incomplete documentation and billing information, or the incorrect selection of codes for the level and type of service provided, could result in non-payment for services rendered or lead to allegations of billing fraud.
Direct and indirect cost containment efforts at the state and federal level may materially impact reimbursement for our services. We believe these trends in cost containment will continue. The Medicare program reimburses for our services based upon the rates in its Physician Fee Schedule, and each year, the Medicare program updates the Physician Fee Schedule reimbursement rates. Many private payors use the Medicare fee schedule to determine their own reimbursement rates. The current Medicare fee schedule methodology has significantly reduced the overall reimbursement rates for physician services because it relies upon, in part, a target-setting formula system called the Sustainable Growth Rate (SGR). The SGR is a target rate of growth in spending for physician services which is intended to control the growth of Medicare expenditures for physicians’ services. The annual fee schedule update is adjusted to reflect the comparison of actual expenditures to target expenditures. Because one of the factors for calculating the SGR system is linked to the growth in the U.S. gross domestic product (GDP), the SGR formula may result in a negative payment update if growth in Medicare beneficiaries’ use of services exceeds GDP growth, a situation which has occurred in the past and whose reoccurrence we cannot predict.
While Congress has intervened in the past few years to mitigate the negative reimbursement impact associated with the SGR formula, there is no guarantee that Congress will continue to do so in the future. Moreover, the existing methodology may result in significant yearly fluctuations in the Medicare Physician Fee Schedule amounts, which may be unrelated to changes in the actual costs of providing physician services. Unless there is a change in the Medicare Physician Fee Schedule methodology, the uncertainty regarding reimbursement rates and fluctuation will continue to exist. See Item 7 “Management’s Discussion and Analysis of Financial Condition and Results of Operations—Factors Affecting Operating Results—Rate Changes by Government Sponsored Programs.”
Because governmental healthcare programs generally reimburse us on a fee schedule basis rather than on a charge-related basis, we generally cannot increase our revenues from these programs by increasing the amount we charge for our services. If our costs increase, we may not be able to recover our increased costs from these programs. Government and private payors have taken and may continue to take steps to control the cost, eligibility for, use and delivery of healthcare services as a result of budgetary constraints, cost containment pressures and other reasons. These cost containment measures and other market changes have generally restricted our ability to recover, or shift to non-governmental payors, any increased costs that we experience. Our business model and financial operations may be materially affected by these developments. Governmental healthcare programs, and other third-party payors, may disallow, in whole or in part, our requests for reimbursement based on determinations that certain amounts are not reimbursable, they were for services provided that were not medically necessary, there was a lack of sufficient supporting documentation, or for a number of other reasons. Additional factors that could complicate our billing include, but are not limited to:
| • | disputes between payors as to which party is responsible for payment; |
18
Table of Contents
| • | the difficulty of adherence to specific compliance requirements, diagnosis coding and various other procedures mandated by the government; and |
| • | failure to obtain proper physician credentialing and documentation in order to bill governmental payors. |
We also are subject to governmental reviews and audits of our bills and claims for reimbursement. These reviews can occur before we are paid for services (pre-payment review) or after we have already received payment (post-payment review). Pre-payment reviews can lead to delays in reimbursement. In the context of post-payment reviews, we may be required to make retroactive adjustments to amounts previously paid to us if a finding is made that we were incorrectly reimbursed. The results of any of these types of reviews may cause us to lose eligibility for certain programs in the event of certain types of non-compliance or subject us to other fines or penalties. Also, some of our affiliated hospitalists may have to participate in payor re-education programs. These governmental healthcare programs are subject to statutory and regulatory changes, administrative rulings, interpretations and determinations, all of which may materially increase or decrease the payments we receive for our services as well as affect the cost of providing services.
Our business could be adversely affected by reductions in or limitations of reimbursement amounts or rates under the governmental healthcare programs, reductions in funding of these programs or elimination of coverage for certain individuals or treatments under these programs. Other delays and uncertainties in the reimbursement process may adversely affect our level of accounts receivable, increase the overall cost of collection, adversely affect our working capital and cause us to incur additional borrowing costs. Unfavorable resolutions of future regulatory reviews or investigations, either individually or in the aggregate, could have a material adverse effect on our business, financial condition and results of operations.
Commercial Payors
We also receive compensation from non-governmental healthcare programs, or commercial payors. As with government payors, the manner and timing with which commercial payors reimburse us for our services may adversely affect our operations. We may be subject to, among other things, reductions or limitations in the reimbursement amounts or rates we receive, disallowances for services provided, pre-payment and post-payment audits, delays in payment, and delays or restrictions in our ability to credential new physicians.
Some of our relationships are pursuant to contracts with commercial payors that offer a wide variety of health insurance products, such as Health Maintenance Organizations, Preferred Provider Organizations, and Exclusive Provider Organizations. These organizations are subject to various state laws and regulations, including federal Employment Retirement Income Security Act of 1974 (ERISA) requirements. We try to secure mutually agreeable contracts with payors that enable our affiliated hospitalists to be listed as in-network participants within the payors’ provider networks. Subject to applicable laws and regulations, the terms, conditions and compensation rates of our contracts with commercial third-party payors are negotiated and often vary widely across markets and among payors.
In some cases, our contracts with commercial payors typically provide for discounted fee-for-service arrangements and grant each party the right to terminate the contracts without cause upon prior written notice. If we do not have a contractual relationship with a health insurance payor, we generally bill the payor our full usual and customary charges. If payment is less than our full usual and customary charges, we bill the balance to the patient, subject to state and federal billing practice laws and regulations. Although we maintain standard billing and collections procedures with appropriate discounts for prompt payment, we also provide discounts in certain hardship situations where patients and their families do not have financial resources necessary to pay the amount due for services rendered. Any amounts written-off related to self-pay patients are based on the specific facts and circumstances related to each individual patient account. We cannot guarantee that the rates of payment we receive will cover the costs of our services.
19
Table of Contents
Industry Operating Environment
Political, economic and regulatory influences are subjecting the healthcare industry in the United States to fundamental change. We anticipate that Congress and state legislatures may continue to review and assess alternative healthcare delivery and payment systems and may in the future propose and adopt legislation effecting fundamental changes in the healthcare delivery system. Congress and state legislatures have adopted and may further consider statutory changes affecting healthcare reform. There can be no assurance as to the ultimate content, timing or effect of any healthcare reform legislation, nor is it possible at this time to estimate the impact of any potential legislation. It is possible that the changes to governmental healthcare program reimbursements may serve as precedent to possible changes in other payors’ reimbursement policies in a manner adverse to us. Similarly, changes in private payor reimbursements could lead to adverse changes in Medicare and other governmental healthcare programs which could have a material adverse effect on our business, financial condition or results of operations.
Corporate Compliance Program
We are committed to complying with applicable state and federal laws and regulations governing the provision of healthcare services. In order to encourage a culture of compliance, we have operated a formal corporate compliance program since 1999. Our compliance officer and executive compliance committee are essential to implementation of our program. The members of the executive compliance committee include our senior officers and our compliance officer. All individuals affiliated with our organization (including the members of our board of directors) are bound by our compliance program.
Our compliance program is modeled after compliance guidance provided by the OIG, with specific attention to the OIG Compliance Program Guidance for Third-Party Medical Billing Companies (1998) and the OIG Compliance Program Guidance for Individual and Small Physician Practices (2000). The primary compliance program components the OIG has recommended, all of which we have implemented, include:
| • | development of a written Code of Conduct; |
| • | development of extensive written compliance policies and procedures, based upon the regulatory risks of our business; |
| • | the designation of a compliance officer and compliance committee; |
| • | the development and implementation of regular training programs; |
| • | open lines of communication for compliance questions and concerns; |
| • | a process for responding appropriately to detected misconduct; |
| • | regular auditing and other internal monitoring techniques; and |
| • | a system of discipline and accountability, including the development of corrective action to address detected offenses. |
We regularly monitor updates from government enforcement entities and all payors that may pertain to the operation of our Compliance Program and our business. We adjust our compliance materials and company policies and procedures accordingly.
The goal of our Compliance Program is to prevent, detect, mitigate, respond to, and resolve regulatory risks. Nevertheless, we cannot assure you that our program will detect and rectify all compliance issues in all markets and for all time periods.
As with other healthcare companies that operate corporate compliance programs, from time to time we identify practices that may have resulted in Medicare or Medicaid overpayments or other regulatory and payment issues. In such cases, it is our practice to disclose the issue to the respective programs and, if appropriate, to
20
Table of Contents
refund any resulting overpayments. While such disclosures and repayments are usually accepted without further action, it is possible that such disclosures and repayments will result in allegations that we have violated applicable laws, regulations, or payor guidance, leading to investigations and possible civil or criminal enforcement actions.
| ITEM 1A. | RISK FACTORS |
The following are important factors that could cause actual results or events to differ materially from those contained in any forward-looking statements made by or on behalf of the Company. In addition, the risks and uncertainties described below are not the only ones we face. Unforeseen risks could arise and problems or issues that we now view as minor could become more significant. If we are unable to adequately respond to these risks and uncertainties, our business, financial condition and results of operations could be materially adversely affected. Additionally, we cannot be certain or give any assurances that any actions taken to reduce known risks and uncertainties will be effective.
The healthcare industry is complex and intensely regulated at the federal, state, and local levels and government authorities may determine that we have failed to comply with applicable laws or regulations.
As a company involved in the provision of healthcare services, we are subject to a myriad of federal, state, and local laws and regulations. There are significant costs involved in complying with these laws and regulations. Moreover, if we are found to have violated any applicable laws or regulations, we could be subject to civil and/or criminal damages, fines, sanctions, or penalties, including exclusion from participation in governmental healthcare programs, such as Medicare and Medicaid. We may also be required to change our method of operations. These consequences could be the result of current conduct or even conduct that occurred a number of years ago. We also could incur significant costs merely if we become the subject of an investigation or legal proceeding alleging a violation of these laws and regulations. We cannot predict whether a federal, state, or local government will determine that we are not operating in accordance with law, or whether the laws will change in the future and impact our business. Any of these actions could have a material adverse effect on our business, financial condition and results of operations.
The following is a non-exhaustive list of some of the more significant healthcare laws and regulations that affect us:
| • | federal laws, including the federal False Claims Act, that provide for penalties against entities and individuals which knowingly or recklessly make claims to Medicare, Medicaid, and other governmental healthcare programs, as well as third-party payors, that contain or are based upon false or fraudulent information; |
| • | a provision of the federal Social Security Act, commonly referred to as the “anti-kickback” statute, that prohibits the knowing and willful offering, payment, solicitation or receipt of any bribe, kickback, rebate or other remuneration, in cash or in kind, in return for the referral or recommendation of patients for items and services covered, in or in part, by federal healthcare programs such as Medicare and Medicaid; |
| • | a provision of the Social Security Act, commonly referred to as the Stark Law or physician self-referral law, that (subject to limited exceptions) prohibits physicians from referring Medicare and Medicaid patients to an entity for the provision of certain “designated health services” if the physician or a member of such physician’s immediate family has a direct or indirect financial relationship with the entity, and prohibits the entity from billing for services arising out of such prohibited referrals; |
| • | a provision of the Social Security Act that provides for criminal penalties on healthcare providers who fail to disclose known overpayments; |
| • | state law provisions pertaining to anti-kickback, self-referral and false claims issues, which typically are not limited to relationships involving governmental payors; |
21
Table of Contents
| • | provisions of, and regulations relating to, the Health Insurance Portability and Accountability Act of 1996 (HIPAA) that provides penalties for knowingly and willfully executing a scheme or artifice to defraud a healthcare benefit program or falsifying, concealing or covering up a material fact or making any material false, fictitious or fraudulent statement in connection with the delivery of or payment for healthcare benefits, items or services; |
| • | provisions of HIPAA and Health Information Technology for Economic and Clinical Health Act (HITECH) limiting how healthcare providers and HIPAA business associates may use and disclose individually identifiable protected health information (PHI) and the security measures taken in connection with protecting that information and related systems, as well as similar or more stringent state laws; |
| • | federal and state laws that provide penalties for providers for billing and receiving payment from a governmental healthcare program for services unless the services are medically necessary and reasonable, adequately and accurately documented, and billed using codes that accurately reflect the type and level of services rendered; |
| • | federal laws that provide for administrative sanctions, including civil monetary penalties for, among other violations, inappropriate billing of services to federal healthcare programs, payments by hospitals to physicians for reducing or limiting services to Medicare or Medicaid patients , or employing or contracting with individuals or entities who/which are excluded from participation in federal healthcare programs; |
| • | federal and state laws and policies that require healthcare providers to enroll in the Medicare and Medicaid programs before submitting any claims for services, to promptly report certain changes in their operations to the agencies that administer these programs, and to re-enroll in these programs when changes in direct or indirect ownership occur or in response to revalidation requests from Medicare and Medicaid; |
| • | state laws that prohibit general business entities from practicing medicine, controlling physicians’ medical decisions or engaging in certain practices, such as splitting fees with physicians; |
| • | laws in some states that prohibit non-domiciled entities from owning and operating medical practices in their states; |
| • | provisions of the Social Security Act (emanating from the Deficit Reduction Act of 2005) that require entities that make or receive annual Medicaid payments of $5 million or more from a single Medicaid program to provide their employees, contractors and agents with written policies and employee handbook materials on federal and state false claims acts and related statutes; that establish a new Medicaid Integrity Program designed to enhance federal and state efforts to detect Medicaid fraud, waste, and abuse; and that increase financial incentives for both states and individuals to bring fraud and abuse claims against healthcare companies; and |
| • | federal and state laws and regulations restricting the techniques that may be used to collect past due accounts from consumers, such as our patients, for services provided to the consumer. |
Providers in the healthcare industry are the subject of federal and state investigations, as well as payor audits.
Due to our participation in government and private healthcare programs, we are sometimes involved in inquiries, reviews, audits and investigations by governmental agencies and private payors of our business practices, including assessments of our compliance with coding, billing and documentation requirements. Federal and state government agencies have active civil and criminal enforcement efforts that include investigations of healthcare companies, and their executives and managers. Under certain circumstances, these investigations can also be initiated by private individuals under whistleblower provisions which may be incentivized by the possibility for private recoveries. The Deficit Reduction Act of 2005 revised federal law to further encourage these federal, state and individually-initiated investigations against healthcare companies.
22
Table of Contents
Responding to these audit and enforcement activities can be costly and disruptive to our business operations, even when the allegations are without merit. If we are subject to an audit or investigation and a finding is made that we were incorrectly reimbursed, we may be required to repay these agencies or private payors, or we may be subjected to pre-payment reviews, which can be time-consuming and result in non-payment or delayed payment for the services we provide. We also may be subject to other financial sanctions or be required to modify our operations.
Our revenue may be negatively impacted by the failure of our affiliated hospitalists to appropriately document services they provide.
We rely upon our affiliated hospitalists to appropriately and accurately complete necessary medical record documentation and assign appropriate reimbursement codes for their services. Reimbursement to us is conditioned on our affiliated hospitalists providing the correct procedure and diagnosis codes and properly documenting the services themselves, including the level of service provided, and the medical necessity for the services. If our affiliated hospitalists have provided incorrect or incomplete documentation or selected inaccurate reimbursement codes, this could result in nonpayment for services rendered or lead to allegations of billing fraud. This could subsequently lead to civil and criminal penalties, including exclusion from government healthcare programs, such as Medicare and Medicaid. In addition, third-party payors may disallow, in whole or in part, requests for reimbursement based on determinations that certain amounts are not covered, services provided were not medically necessary, or supporting documentation was not adequate. Retroactive adjustments may change amounts realized from third-party payors and result in recoupments or refund demands, affecting revenue already received.
Compliance with federal and state privacy laws is expensive, and we may be subject to government or private actions due to privacy and security breaches.
We must comply with numerous federal and state laws and regulations governing the collection, dissemination, access, use, security and confidentiality of patient-identifiable protected health information, including HIPAA and HITECH. As part of our medical record keeping, third-party billing, and other services, we collect and maintain patient health information in paper and electronic format. This portion of our IPC-Link ® platform relies solely on the electronic exchange of patient-identifiable healthcare information. New patient health information standards, whether implemented pursuant to federal or state action, could have a significant effect on the manner in which we handle healthcare-related data and communicate with payors, and compliance with these standards could impose significant costs on us or limit our ability to offer services, thereby negatively impacting the business opportunities available to us. Despite our efforts to prevent security and privacy breaches, they may still occur, especially with IPC-Link®. If our non-compliance with existing or new laws and regulations related to patient health information results in privacy or security breaches, we could be subject to monetary fines, civil suits, civil penalties or criminal sanctions.
As a result of the expanded scope of HIPAA through HITECH, we may incur significant costs in order minimize the amount of PHI we handle and retain that is considered “unsecured PHI” by HHS guidance or to implement improved administrative, technical or physical barriers to protect PHI. We may incur significant costs in order to evaluate whether or not a breach of unsecured PHI has occurred, which individual’s information was breached, and whether or not the potential for harm to the individual exists as a result of the breach. We may incur significant costs to notify the relevant individuals and entities in the event of a breach and to provide appropriate remediation and monitoring to mitigate the possible damage done by the breach.
Providers must be properly enrolled in governmental healthcare programs, such as Medicare and Medicaid, before they can receive reimbursement for providing services, and there may be delays in the enrollment process.
Each time a new affiliated hospitalist joins us, we must enroll the affiliated hospitalist under our applicable group identification number for Medicare or Medicaid programs and for certain managed care and private insurance programs before we can receive reimbursement for services the hospitalist renders to beneficiaries of
23
Table of Contents
those programs. The estimated time to receive approval for the enrollment is sometimes difficult to predict and, in recent years, the Medicare program carriers often have not issued these numbers to our affiliated hospitalists in a timely manner. These practices result in delayed reimbursement that may adversely affect our cash flow and revenues.
We may face malpractice and other lawsuits that may not be covered by insurance.
Malpractice lawsuits are common in the healthcare industry. The medical malpractice legal environment varies greatly by state. The status of tort reform, availability of non-economic damages or the presence or absence of other statutes, such as elder abuse or vulnerable adult statutes, influence the incidence and severity of malpractice litigation. We may also be subject to other types of lawsuits which may involve large claims and significant defense costs. Many states have joint and several liability for all healthcare providers who deliver care to a patient and are at least partially liable. As a result, if one healthcare provider is found liable for medical malpractice for the provision of care to a particular patient, all other healthcare providers who furnished care to that same patient, including possibly our affiliated hospitalists, may also share in the full liability which may be substantial. We currently maintain liability insurance coverage to cover professional liability and other claims. We cannot be certain that our insurance coverage will be adequate to cover liabilities arising out of claims asserted against us, our affiliated professional organizations or our affiliated hospitalists. During the first quarter of 2010, we reached a preliminary agreement to settle a disputed professional liability claim for a prior year that is in excess of our insurance policy limit. The settlement remains subject to definitive documentation and is contingent upon receiving applicable court approval. We recorded our portion of the settlement of $0.8 million in the fourth quarter of 2009. We cannot assure this will not occur again in the future and we cannot provide assurance that any future liabilities will not have a material adverse impact on our results of operations, cash flows or financial position. Liabilities in excess of our insurance coverage, including coverage for professional liability and other claims, could have a material adverse effect on our business, financial condition, and results of operations. In addition, our professional liability insurance coverage generally must be renewed annually and may not continue to be available to us in future years at acceptable costs and on favorable terms.
We have established reserves for potential medical malpractice liability losses which are subject to inherent uncertainties and a deficiency in the established reserves may lead to a reduction in our net income.
Our medical malpractice policies are written on a claims-made basis. Unlike our claims-made policy in effect in 2008 that contained self-insurance retention, the 2009 and 2010 claims-made policies provide first dollar coverage up to our policy limits on new claims reported in 2009 and 2010. We record reserves for our self-insurance retention and an estimate of our liabilities, on an undiscounted basis, for claims incurred but not reported during the policy period, based upon actuarial loss projections using our historical loss experience. These insurance reserves are inherently subject to uncertainty as they could be significantly affected if current and future occurrences differ from historical claim trends and expectations. While claims are monitored closely when estimating reserves, the complexity of the claims and wide range of potential outcomes often hampers timely adjustments to the assumptions used in these estimates. The unpredictable nature of the reporting of claims could result in significant fluctuations in the loss estimate from period to period. It is possible that actual losses and related expenses may differ, perhaps substantially, from the reserve estimates reflected in our financial statements.
In the fourth quarters of 2007 and 2008, we recorded reductions of $0.8 million and $1.0 million, respectively, in our claims and professional liability reserves because our final 2007 and 2008 year end actuarial loss projections were less than the interim actuarial loss projections for the year due to favorable trends in the ratio of claims to our number of encounters and reductions in the estimates of the ultimate costs per claim. If subsequent actual paid claims exceed our estimated reserves, we may be required to increase reserves, which would lead to a reduction in our future net income. Our annual provision for medical malpractice claims as a percentage of net revenues for the years ended December 31, 2007, 2008 and 2009 were 1.4%, 1.1% and 0.4%, respectively. The decline to 0.4% in 2009 as compared to 1.1% in 2008 is the result of changing to first dollar coverage up to our policy limits effective with our 2009 policy.
24
Table of Contents
Competition for hospitalists is intense, and we may not be able to hire and retain hospitalists to provide services.
We are dependent on our affiliated hospitalists to provide services and generate revenue. We compete with many types of healthcare providers, including teaching, research and government institutions, hospitals and other practice groups, for the services of clinicians. The limited number of residents entering the job market each year and the limited number of other licensed providers seeking to change employers makes it challenging to meet our hiring needs and may require us to increase hospitalist compensation in a manner that decreases our profit margins. The limited number of residents and other licensed providers also impacts our ability to recruit new hospitalists with the expertise necessary to provide services within our business and our ability to renew contracts with existing hospitalists on acceptable terms. If we do not do so, our ability to provide services could be adversely affected. Our employed affiliated hospitalist turnover rate in 2008 and 2009 were 21% and 15%, respectively. If this turnover rate were to increase significantly, our recruiting efforts could be over-extended, our growth could be impeded, the consistency of our services could be negatively affected, and our reputation in the healthcare community could be adversely impacted.
We may be unable to enforce the non-competition covenants of departed affiliated hospitalists.
We usually enter into employment agreements with our affiliated hospitalists which typically can be terminated without cause by either party upon prior written notice. Substantially all of our affiliated hospitalists have agreed not to compete within a specified geographic area and at specific facilities for a one year period after termination of employment. The law governing enforcement of non-compete agreements and other forms of restrictive covenants varies from state to state.
Although we believe that the non-competition and other restrictive covenants of our affiliated hospitalists are reasonable in scope and duration and therefore enforceable under applicable state law, courts and arbitrators in some states are reluctant to strictly enforce non-compete agreements and restrictive covenants applicable to physicians. If a substantial number of our affiliated hospitalists leave and we are unable to enforce the non-competition covenants in the employment agreements, our business, financial condition and results of operations could be materially adversely affected. We cannot predict whether a court or arbitration panel would enforce these covenants and it could be costly to enforce such covenants.
Restrictions on immigration may affect our ability to compete for and provide services to our clients, which could adversely affect our ability to meet growth and revenue targets.
While all of our affiliated hospitalists have completed residencies in the United States, as of December 31, 2009, approximately 17.2% of our employed hospitalists were not U.S. citizens. The ability of these affiliated hospitalists to work in the United States depends on our ability to obtain the necessary work visas and work permits. Existing and proposed limitations on, and eligibility restrictions for, these visas could have a significant impact on our ability to recruit hospitalists. Further, in response to recent global political events, the level of scrutiny in granting visas has increased. New security procedures may delay the issuance of visas and affect our ability to hire hospitalists in a timely manner.
Our reliance on work visas for a number of our affiliated hospitalists makes us particularly vulnerable to legislative changes and strict enforcement of new national security procedures, as it affects our ability to hire hospitalists who are not U.S. citizens. If we are not able to obtain a sufficient number of visas for these affiliated hospitalists or encounter delays or additional costs in obtaining or maintaining such visas, our ability to meet our growth and revenue targets could be adversely affected.
25
Table of Contents
We may not make appropriate acquisitions, may fail to integrate them into our business, and/or these acquisitions may alter our current payor mix.
Our business is partially dependent on locating and acquiring or partnering with medical practices or individual physicians to provide hospitalist services. As part of our acquisition strategy, we regularly review potential acquisition opportunities. We believe that there continue to be a number of acquisition opportunities that would be complimentary to our business. We currently have no binding commitments to acquire any specific business or other material assets. We cannot predict whether we will be successful in pursuing such acquisition opportunities or what the consequences of any such acquisition would be. If we are not successful in finding attractive acquisition candidates that we can acquire on satisfactory terms, or if we cannot complete those acquisitions that we identify, we will not be able to realize the benefit of this part of our growth strategy. Furthermore, our acquisition strategy involves a number of risks and uncertainties, including:
| • | We may not be able to identify suitable acquisition candidates or strategic opportunities or successfully implement or realize the expected benefits of any suitable opportunities. In addition, we compete for acquisitions with other potential acquirers, some of which may have greater financial or operational resources than we do. This competition may intensify due to the ongoing consolidation in the healthcare industry, which may increase our acquisition costs. |
| • | We may be unable to successfully integrate completed acquisitions, including our recently completed acquisitions and such acquisitions may fail to achieve the financial results we expected. Integrating completed acquisitions into our existing operations involves numerous short-term and long-term risks, including diversion of our management’s attention, failure to retain key personnel, failure to retain payor contracts and failure of the acquired entity to be financially successful. |
| • | We cannot be certain of the extent of any unknown or contingent liabilities of any acquired business, including liabilities for failure to comply with applicable laws. We may incur material liabilities for past activities of acquired businesses. Also, depending on the location of the acquisition, we may be required to comply with laws and regulations that may differ from those of the states in which our operations are currently conducted. |
| • | We may acquire individual or group medical practices that operate with lower profit margins as compared with our current or expected profit margins or which have a different payor mix than our other practice groups, which would reduce our profit margins. Depending upon the nature of the local healthcare market, we may not be able to implement our business model, which may negatively impact our revenues and profitability. |
| • | If we finance acquisitions by issuing equity securities or securities convertible into equity securities, our existing stockholders could be diluted, which, in turn, could adversely affect the market price of our stock. If we finance an acquisition with debt, it could result in higher leverage and interest costs. As a result, if we fail to evaluate and execute acquisitions properly, we might not achieve the anticipated benefits of these acquisitions, and we may increase our acquisition costs. |
Changes in the rates or methods of third-party reimbursements may adversely affect our operations.
We derive the majority of our revenue from direct billings to governmental healthcare programs, such as Medicare and Medicaid, and private health insurance companies. As a result, any negative changes in the rates or methods of reimbursement for the services we provide would have a significant adverse impact on our revenue and financial results. Government funding for healthcare programs, in particular, is subject to unpredictable statutory and regulatory changes, administrative rulings, interpretations of policy and determinations by intermediaries, and governmental funding restrictions, all of which could materially impact program coverage and reimbursements for our services.
The Medicare program reimburses for our services based upon the rates in its Physician Fee Schedule. Each year on January 1st, the Medicare program updates the Physician Fee Schedule reimbursement rates. Many private payors use the Medicare Physician Fee Schedule to determine their own reimbursement rates. While
26
Table of Contents
Congress has intervened in the past few years to mitigate the impact of this, there is no guarantee that Congress will continue to do so in the future. Moreover, the existing methodology may result in significant yearly fluctuations in the Physician Fee Schedule amounts, which may be unrelated to changes in the actual costs of providing physician services. Unless there is a change in the Medicare Physician Fee Schedule methodology, the uncertainty regarding reimbursement rates and fluctuation will continue to exist. In December 2009, Congress passed a stay of the negative update to the Sustainable Growth Rate (SGR) for a two month period of January and February 2010. Based on current data, the Center for Medicare and Medicaid Services (CMS) is projecting a rate reduction of approximately 21% for 2010, if Congress does not take further legislative action as they have done in prior years.
In December 2009, CMS finalized several changes to refine Medicare payments to physicians effective January 1, 2010, which increased payment rates for primary care services. The proposals include an update to the practice expense component of physician fees which is to be implemented over four years. CMS also ceased payments for consultation codes, which are typically billed by specialists, including our physicians, and were paid at a higher rate than equivalent evaluation and management (E/M) services. Practitioners will use existing E/M service codes when providing these services instead. Resulting savings were redistributed to increase payments for the existing E/M services. In addition, CMS refined how Medicare recognizes the cost of professional liability insurance in its payment system. Also, effective January 1, 2010, the Geographic Practice Cost Indices floor of 1.0 expired which resulted in a decrease in payments to any geographic area with an index of less than 1.0. These changes, taken together with the stay in the negative update to the SGR, resulted in an estimated 1% - 2% increase in Medicare reimbursement rates for the codes applicable to the services performed by our affiliated hospitalists and an overall estimated increase of less than 1% in our net patient revenue per encounter.
Because governmental healthcare programs generally reimburse on a fee schedule basis rather than on a charge-related basis, we generally cannot increase our revenues from these programs by increasing the amount we charge for our services. If our costs increase, we may not be able to recover our increased costs from these programs. Government and private payors have taken and may continue to take steps to control the cost, eligibility for, use and delivery of healthcare services as a result of budgetary constraints, cost containment pressures and other reasons. We believe that these trends in cost containment will continue. These cost containment measures and other market changes in non-governmental insurance plans have generally restricted our ability to recover, or shift to non-governmental payors, any increased costs that we experience. Our business and financial operations may be materially affected by these developments.
If we inadvertently employ or contract with an excluded person, we may face government sanctions.
Individuals and entities can be excluded from participating in the Medicare and Medicaid programs for violating certain laws and regulations, or for other reasons such as the loss of a license in any state, even if the individual retains other licensure. This means that they (and all others) are prohibited from receiving payment for their services rendered to Medicare or Medicaid beneficiaries, and if the excluded individual is a physician, all services ordered (not just provided) by such physician are also non-covered and non-payable. Entities which employ or contract with excluded individuals are prohibited from billing the Medicare or Medicaid programs for the excluded individual’s services, and are subject to civil monetary penalties if they do. The U.S. Department of Health and Human Services Office of the Inspector General (OIG) maintains a list of excluded individuals and entities. Although we have instituted policies and procedures through our Compliance Program to minimize the risks, there can be no assurance that we will not inadvertently hire or contract with an excluded person, or that any of our current employees or contracts will not become excluded in the future without our knowledge. If this occurs, we may be subject to substantial repayments and civil penalties and the hospitals at which we furnish services also may be subject to repayments and sanctions, for which they may seek recovery from us.
27
Table of Contents
The hospitalist industry is competitive.
There are other companies and individuals currently providing hospitalist services. We compete directly with national, regional and local providers of inpatient healthcare, and other companies could enter the market in the future and divert some or all of our business. On a national basis our competitors include Team Health and EmCare, each of which may have greater financial and other resources available to them. We also compete with hospitalist groups and privately-owned hospitalist companies in each of our local markets. Existing or future competitors also may seek to compete with us for acquisitions, which could have the effect of increasing the price and reducing the number of suitable acquisitions, which would have an adverse impact on our growth strategy. Since there are virtually no capital expenditures required to enter the industry, there are few financial barriers to entry. Individual physicians, physician groups and companies in other healthcare industry segments, including hospitals with which we have contracts, some of which have greater financial, marketing and staffing resources, may become competitors in providing hospitalist services and this competition may have a material adverse effect on our business operations and financial position.
Because patients do not typically select their hospitalists, we are completely reliant on referrals from third parties.
Our business is based on referrals for our services. We receive referrals from community medical providers, emergency departments, payors, and hospitals in the same manner as other medical professionals receive patient referrals. We do not provide compensation or other remuneration to our referral sources for referring patients to us. A decrease in these referrals due to competition, concerns about the quality of our services, and other factors could result in a significant decrease in our revenues and adversely impact our financial condition. Similarly, we cannot assure that we will be able to obtain or maintain preferred provider status with significant third-party payors in the communities where we operate. If we are unable to maintain our referral base or our preferred provider status with significant third-party payors, it may negatively impact our revenues and our financial performance.
Hospitals may terminate their agreements with us or reduce the fees they pay us.
We currently derive approximately 6% of our net revenue from contracts directly with hospitals for hospitalist services. Our current partner hospitals may decide not to renew our contracts, introduce unfavorable terms, or reduce fees paid to us. Any of these events may impact the ability of our practice groups to operate at such hospitals, which would negatively impact our revenue and profitability.
Some of the hospitals where our affiliated hospitalists provide services may have their medical staffs closed to non-contracted hospitalists.
In general, our affiliated hospitalists may only provide services in a hospital where they have certain credentials, called privileges, that are granted by the medical staff and controlled by legally binding medical staff bylaws of the hospital. The medical staff decides who will receive privileges, and the medical staff of the hospitals where we currently provide services or wish to provide services could decide that non-contracted hospitalists can no longer receive privileges to practice there. Such a decision would limit our ability to furnish services in a hospital, decrease the number of our affiliated hospitalists who could provide services, or preclude us from entering new hospitals. In addition, hospitals may attempt to enter into exclusive contracts for hospitalist services, which would exclude our affiliated hospitalists who are not part of the contracting group from providing services at that facility or reduce access to certain populations of patients within the hospital.
Many states prohibit business entities from owning or controlling medical practices.
The laws in many of the states in which we operate, or may operate in the future, prohibit business entities from practicing medicine and from exercising control over or employing physicians who practice medicine. This corporate practice of medicine prohibition is intended to prevent unlicensed persons from interfering with or
28
Table of Contents
inappropriately influencing the physician’s professional judgment. These and other laws may also prevent fee-splitting, which is the sharing of professional service income with non-professional or business interests. The interpretation and enforcement of these laws vary significantly from state to state. There is a risk that state authorities or courts may find that our relationships with our affiliated hospitalists and our practice groups violate state corporate practice of medicine and fee-splitting prohibitions. In addition, authorities or courts could determine that we have not complied with new laws which may be enacted, rendering our arrangements illegal. If any of these events occur, we may be subject to fines and penalties, and changes in our business model may be required.
We may be impacted by eligibility changes to government and private insurance programs.
Due to potential decreased availability of healthcare through private employers, the number of patients who are uninsured or participate in governmental programs may increase. A shift in payor mix from managed care and other private payors to government payors or the uninsured may result in a reduction in our rates of reimbursement or an increase in our uncollectible receivables or uncompensated care, with a corresponding decrease in our net revenue. Changes in the eligibility requirements for governmental programs also could increase the number of patients who participate in such programs or the number of uninsured patients. Even for those patients who remain with private insurance, changes in those programs could increase patient responsibility amounts, resulting in a greater risk for us of uncollectible receivables. These factors and events could have a material adverse effect on our business, financial condition and results of operations.
We may have difficulty collecting payments from third-party payors in a timely manner.
We derive significant revenue from third-party payors, and delays in payment or audits leading to refunds to payors may impact our net revenue. We assume the financial risks relating to uncollectible and delayed payments. In the current healthcare environment, payors are continuing their efforts to control expenditures for healthcare, including proposals to revise coverage and reimbursement policies. We may experience difficulties in collecting our revenue because third-party payors may seek to reduce or delay payment to which we believe we are entitled. If we are not paid fully and in a timely manner for such services or there is a finding that we were incorrectly paid, our revenues, cash flows, and financial condition could be materially adversely affected.
Certain federal and state laws may limit our effectiveness at collecting monies owed to us from patients.
We utilize third parties to collect from patients any co-payments and other payments for services that our hospitalists provide to the patients. The federal Fair Debt Collection Practices Act restricts the methods that third-party collection companies may use to contact and seek payment from consumer debtors regarding past due accounts. State laws vary with respect to debt collection practices, although most state requirements are similar to those under the Fair Debt Collection Practices Act. If our collection practices or those of our collection agencies are inconsistent with these standards, we may be subject to actual damages and penalties. These factors and events could have a material adverse effect on our business, financial condition and results of operations.
Unfavorable changes or conditions could occur in the states where our operations are concentrated.
Approximately 69% of our net revenue in 2009 was generated by our operations in five states. Arizona, Florida, Michigan, Missouri and Texas accounted for approximately 16%, 16%, 7%, 6%, and 24%, respectively, of our revenue in 2009. Adverse changes or conditions affecting these states where our operations are concentrated, such as healthcare reforms, changes in laws and regulations, reduced Medicaid reimbursements and government investigations, may have a material adverse effect on our business, financial condition and results of operations.
29
Table of Contents
If we are unable to effectively adapt to changes in the healthcare industry, our business may be harmed.
Due to the importance of the healthcare industry in the lives of all Americans, federal, state, and local legislative bodies frequently pass legislation and promulgate regulations relating to healthcare reform. It is reasonable to believe that there may be increased federal oversight and regulation of the healthcare industry in the future. We cannot assure you as to the ultimate content, timing or effect of any healthcare reform legislation, nor is it possible at this time to estimate the impact of potential legislation on our business. It is possible that future legislation enacted by Congress or state legislatures could adversely affect our business or could change the operating environment of our targeted customers. It is possible that the changes to the Medicare or other governmental healthcare program reimbursements may serve as precedent to possible changes in other payors’ reimbursement policies in a manner adverse to us. Similarly, changes in private payor reimbursements could lead to adverse changes in Medicare and other governmental healthcare programs which could have a material adverse effect on our business, financial condition and results of operations.
Our business model depends on numerous complex management information systems, and any failure to successfully maintain these systems or implement new systems could materially harm our operations and result in potential violations of healthcare laws and regulations.
We depend on a complex, specialized, integrated management information system and standardized procedures for operational and financial information, as well as for our billing operations. We may be unable to enhance our existing management information systems or implement new management information systems where necessary. Additionally, we may experience unanticipated delays, complications, or expenses in implementing, integrating, and operating our systems. Our management information systems may require modifications, improvements, or replacements that may require both substantial expenditures as well as interruptions in operations. Our ability to implement these systems is subject to the availability of information technology and skilled personnel to assist us in creating and implementing these systems. Our failure to successfully implement and maintain all of our systems could have a material adverse effect on our business, financial condition and results of operations. Further, our failure to successfully operate our billing systems could lead to potential violations of healthcare laws and regulations.
We may incur significant costs if we are required to adopt certain provisions under the Health Information Technology for Economic and Clinical Health Act.
HITECH was enacted into law on February 17, 2009 as part of the American Recovery and Reinvestment Act of 2009. Among the many provisions of HITECH, are those relating to the implementation and use of certified Electronic Health Records (EHRs). Our patient medical records are maintained and under the custodianship of the healthcare facilities in which we operate. However, if we are required to adopt the use of EHRs utilized by these healthcare facilities, or comply with any related provisions of HITECH, we may incur significant costs which could have a material adverse effect on our business operations and financial position.
We are dependent upon our key management personnel for our future success.
Our success depends to a significant extent on the continued contributions of our key management personnel, including our Chairman and Chief Executive Officer, Adam D. Singer, M.D., for the management of our business and implementation of our business strategy. We have entered into employment agreements with Dr. Singer as well as our other named executive officers. Our agreement with Dr. Singer has a three year term and the agreements with our other named executive officers have one year terms, in each case, subject to automatic renewals. We maintain key man life insurance on Dr. Singer in the amount of $3.0 million and IPC is the designated beneficiary of such policy. The loss of Dr. Singer or other key management personnel could have a material adverse effect on our business, financial condition and results of operations.
30
Table of Contents
We may not be able to effectively manage our growth.
We have experienced significant growth in our business and personnel over the years which we expect to continue. For example, from 2007 to 2009 our annual patient encounters increased from 2,153,000 to 3,291,000 and we increased our number of hospitalists from 546 to 1,036. We have managed this growth by augmenting the staff of our corporate office and the staff of our 16 operating regions. However, we may be unable to effectively manage this growth going forward with respect to appropriate hiring, training and oversight of personnel, or appropriate integration into our systems. These events could materially adversely impact our business, financial condition and results of operations.
Our intellectual property rights are valuable, and if we are unable to protect them or are subject to intellectual property rights claims, our business may be harmed.
Our intellectual property rights, including those rights related to IPC-Link® and certain trademarks, copyrights and trade secrets, are important assets for us. We do not hold any patents protecting our intellectual property. Various events outside of our control pose a threat to our intellectual property rights as well as to our business. For example, we may be subject to third-party intellectual property rights claims, and our technologies may not be able to withstand any such claims. Regardless of the merits of the claims, any intellectual property claims could be time-consuming and expensive to litigate or settle. In addition, if any claims against us are successful, we may have to pay substantial monetary damages or discontinue any of our practices that are found to be in violation of another party’s rights. We also may have to seek a license to continue such practices, which may significantly increase our operating expenses or may not be available to us at all. Also, the efforts we have taken to protect our proprietary rights may not be sufficient or effective. Any significant impairment of our intellectual property rights could harm our business or our ability to compete.
The recent economic and credit crisis could have an adverse effect on our business, financial condition and results of operations.
The recent economic and credit crisis has reduced the availability of liquidity and credit to fund the continuation and expansion of many business operations nationally. This shortage of liquidity and credit, combined with recent substantial losses in equity markets, could lead to an extended national economic recession and result in an adverse effect on our business, financial condition and results of operations. Our ability to access the capital markets may be severely restricted at such time when we would like, or need, to access those markets, which could have a negative impact on our growth plans and the flexibility to react to changing economic and business conditions. Although we are unable to determine the specific impact of the current economic conditions on our business at this time, further deterioration or a prolonged period of recession could have an adverse impact on our operations and could impact not only the healthcare decisions of patients, but also the solvency of third-party insurance payors.
We might need to raise additional capital, which might not be available.
We may require additional equity or debt financing for additional working capital for expansion, to consummate acquisitions or if we suffer significant losses. In the event of additional financing is unavailable to us, we may be unable to expand or make acquisitions and the price of our common stock may decline.
The terms of our debt agreement could restrict our operations, particularly our ability to respond to changes in our business or to take specified actions.
Our existing secured debt agreement contains, and any future indebtedness would likely contain, a number of restrictive covenants that impose significant operating and financial restrictions on us, including restrictions on our ability to take actions that may be in our best interests. Our existing debt agreement includes covenants, including requirements that:
| • | generally do not allow us to borrow additional amounts without the approval of our lenders; |
31
Table of Contents
| • | require us to notify our lender of, and grant security interests in, newly-acquired companies; |
| • | allow us to dispose of assets only in accordance with the terms of our existing secured debt; |
| • | restrict our ability to pay dividends without the approval of our lenders; |
| • | we do not impair our lenders’ security interests in our assets; and |
| • | require us to maintain minimum cash balances. |
We may write off intangible assets, such as goodwill.
Our intangible assets, which consist primarily of goodwill related to our acquisitions, are subject to annual impairment testing. Under current accounting standards, goodwill is tested for impairment on an annual basis and we may be subject to impairment losses as circumstances change after an acquisition. If we record an impairment loss related to our goodwill, it could have a material adverse effect on our results of operations for the year in which the impairment is recorded. The amount of goodwill recorded at December 31, 2009 is $91.7 million as compared to stockholders’ equity of $145.1 million.
Our quarterly results will likely fluctuate from period to period, which could increase the volatility in the price of our common stock.
We have historically experienced and expect to continue to experience quarterly fluctuations in revenue and net income. Absent the impact and timing of acquisitions, our net revenue has historically been higher in the first and fourth quarters of the year primarily due to the following factors:
| • | the number of physicians we have on staff during the quarter, which may fluctuate based upon the timing of hires due to the end of the academic year for graduating resident physicians and the schedule of the Internal Medicine Board exams and terminations in our existing practices; and |
| • | fluctuations in patient encounters, which are impacted by hospital census, which can be volatile, physician productivity and seasonality due to the higher occurrence of illnesses such as flu and pneumonia in patient populations in the first quarter. |
As a result of the fluctuations caused by these factors and due to the timing of acquisitions, our results of operations for any quarter are not indicative of results of operations for any future period or full year. These variations in our results of operations could contribute to volatility in the price of our common stock. In addition, we have significant fixed operating costs, including physician practice salaries and benefits and, as a result, are highly dependent on patient encounters and the productivity of our affiliated hospitalists to sustain profitability.
Provisions in our charter documents could limit another party’s ability to acquire us and deprive our investors of the opportunity to obtain a takeover premium for their securities.
Our amended and restated certificate of incorporation and our bylaws contain several provisions that may make it substantially more difficult for a third-party to acquire us. This may make it more difficult or expensive for a third-party to acquire a majority of our outstanding common stock. These provisions also may delay, prevent or deter a merger, acquisition, tender offer, proxy contest or other transaction that might otherwise result in our stockholders receiving a premium over the market price for their common stock.
Our ability to designate the rights and preferences of undesignated preferred stock could result in the issuance of stock with rights and preferences that are superior to those of your shares, which could reduce the value of your investment.
Our amended and restated certificate of incorporation authorizes our board of directors to designate by resolution, different classes and/or series of stock from the 15,000,000 shares of preferred stock authorized. Our board of directors is also empowered to fix the relative rights, preferences, privileges and limitations of each
32
Table of Contents
class or series of preferred stock. This means that our board of directors may issue shares of preferred stock with rights and preferences, including, among other things, dividend, liquidation, redemption and voting rights that are superior to the rights, preferences and privileges of the shares of our common stock. In addition, we may issue other securities, such as convertible promissory notes, that may have rights and preferences that are superior to those of the shares of our common stock. In addition, our board of directors has the ability, without further stockholder approval, to issue additional shares of our common stock and securities exercisable for, convertible into or exchangeable for shares of our authorized capital stock. The ability of our board of directors to designate the rights and preferences of the preferred stock could impede or deter an unsolicited tender offer, merger or takeover of our business, or make a change of control of our company difficult to accomplish. In addition, the issuance of shares of our common stock or other securities having rights and preferences superior to those of the shares of common stock being offered could reduce the value of our common stock.
We do not intend to pay cash dividends on our common stock, which means that capital appreciation, if any, of our common stock will be our stockholders’ only source of gain.
We do not intend to pay cash dividends on our common stock. We currently intend to retain all available funds and any future earnings for use in the operation and expansion of our business and do not anticipate paying any cash dividends in the foreseeable future. In addition, the terms of our current, as well as any future, financing agreements may preclude us from paying any dividends. As a result, capital appreciation, if any, of our common stock will be our stockholders’ sole source of potential gain for the foreseeable future.
| ITEM 1B. | UNRESOLVED STAFF COMMENTS |
None.
| ITEM 2. | PROPERTIES |
We lease office space in North Hollywood, California for our corporate headquarters. The lease will expire on June 30, 2011. In addition, we lease a number of administrative offices in connection with our regional offices in particular markets. We believe our present facilities are adequate to meet our current and projected needs. We do not view any of these leases or locations for administrative offices as material to our business. We expect to be able to renew each of our leases or lease comparable facilities on terms commercially acceptable to us.
| ITEM 3. | LEGAL PROCEEDINGS |
In the ordinary course of our business, we become involved in pending and threatened legal actions and proceedings, most of which involve claims of medical malpractice related to medical services provided by our affiliated hospitalists. We may also become subject to other lawsuits which could involve significant claims and/or significant defense costs.
We believe, based upon our review of pending actions and proceedings, that the outcome of such legal actions and proceedings will not have a material adverse effect on our business. The outcome of such actions and proceedings, however, cannot be predicted with certainty and an unfavorable resolution of one or more of them could have a material adverse effect on our business in a future period.
| ITEM 4. | SUBMISSION OF MATTERS TO A VOTE OF SECURITY HOLDERS |
None.
33
Table of Contents
| ITEM 5. | MARKET FOR REGISTRANT’S COMMON EQUITY, RELATED STOCKHOLDER MATTERS AND ISSUER PURCHASES OF EQUITY SECURITIES |
Market Information
Our common stock has been traded on the NASDAQ Global Market since January 25, 2008, the date of our initial public offering, under the symbol “IPCM.” On such date, we sold 3,300,000 shares of common stock and the selling stockholders sold 1,900,000 shares of common stock. The underwriters had an option to purchase a maximum of 705,000 additional shares from the selling stockholders to cover over-allotments of shares, which they exercised on January 28, 2008. Prior to our initial public offering, there had been no public market for our common stock. The initial public offering price of our common stock on January 25, 2008 was $16.00 per share. After the offering, there were 14,844,934 shares of our common stock outstanding.
On July 21, 2008, we closed a follow-on public offering for the sale of 4,025,000 shares of our common stock at a price of $18.50 per share. Of these shares 1,135,231 shares were newly issued shares sold by us, and 2,889,769 were shares sold by existing stockholders, including 525,000 shares pursuant to an exercise by the underwriters of their over-allotment option. After the offering, there were 16,017,237 shares of our common stock outstanding.
Following is a table presenting the closing sales prices on the NASDAQ Global Market for a share of our common stock by fiscal quarter for fiscal years 2009 and 2008:
| High | Low | |||||
| 2009 | ||||||
| 4th Quarter |
$ | 34.09 | $ | 30.21 | ||
| 3rd Quarter |
$ | 33.75 | $ | 25.87 | ||
| 2nd Quarter |
$ | 28.92 | $ | 16.89 | ||
| 1st Quarter |
$ | 20.22 | $ | 14.07 | ||
| 2008 | ||||||
| 4th Quarter |
$ | 24.59 | $ | 13.46 | ||
| 3rd Quarter |
$ | 28.11 | $ | 18.73 | ||
| 2nd Quarter |
$ | 23.84 | $ | 18.82 | ||
| 1st Quarter (beginning January 25, 2008) |
$ | 22.48 | $ | 16.57 | ||
Holders
As of February 17, 2010, we had 118 holders of record of our common stock, and the closing price on that date for our common stock was $38.25 per share. Because our shares of common stock are held by brokers and other institutions on behalf of stockholders, we are unable to estimate the total number of beneficial owners represented by these stockholders of record.
Dividend Policy
We have never declared or paid cash dividends on our capital stock. The payment of dividends is within the discretion of our board of directors and will depend on our earnings, capital requirements and operating and financial position, among other factors. We expect to retain all of our earnings to finance the expansion and development of our business, and we currently have no plans to pay dividends in the foreseeable future. In addition, our existing credit facility limits, and any future debt agreements may restrict, our ability to pay dividends.
34
Table of Contents
Performance Graph
The following graph illustrates a comparison of the total cumulative stockholder return on our common stock since January 25, 2008, which is the date our common stock first began trading on the NASDAQ Global Market, to two indices: NASDAQ Healthcare Index and Russell 2000 Index Total Return. The graph assumes an initial investment of $100 on January 25, 2008. The comparisons in the graph are required by the Securities and Exchange Commission (SEC) and are not intended to forecast or be indicative of possible future performance of our common stock.
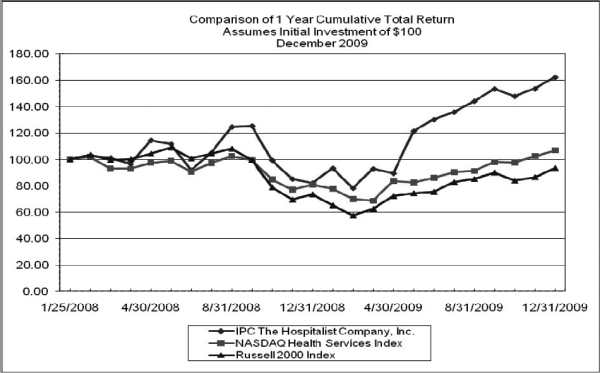
Note 1: Data complete through last fiscal year.
Note 2: Peer group indices use beginning of period market capitalization weighting.
Note 3: Calculated (or derived) based from CRSP NASDAQ Health Services, Center for Research in Security Prices (CRSP®), Graduate Copyright Zacks, Investment Research, Inc. 2009. Used with permission. All rights reserved.
35
Table of Contents
Use of Proceeds from Sales of Registered Securities
On January 30, 2008, we closed an initial public offering of our common stock consisting of 5,905,000 shares of common stock. Of these shares, 3,300,000 were newly issued shares sold by us and 2,605,000 were existing shares sold by the selling stockholders, including 705,000 shares pursuant to an exercise by the underwriters of their over-allotment option. The offering was effected pursuant to a Registration Statement on Form S-1 (File No. 333-145850), which the SEC declared effective on January 24, 2008. Credit Suisse and Jefferies & Company acted as lead underwriters.
The public offering price was $16.00 per share and $94.5 million in the aggregate. Underwriting discounts and commissions were $1.12 per share and $6.6 million in the aggregate. Proceeds after expenses to us were $13.99 per share and $46.2 million in the aggregate. Proceeds after expenses to the selling stockholders were $14.88 per share and $38.8 million in the aggregate.
On July 21, 2008, we closed a follow-on public offering for the sale of 4,025,000 shares of our common stock. Of these shares 1,135,231 shares were newly issued shares sold by us, and 2,889,769 were shares sold by existing stockholders, including 525,000 shares pursuant to an exercise by the underwriters of their over-allotment option. The offering was effected pursuant to a Registration Statement on Form S-1 (File No. 333-151722), which the SEC declared effective on July 16, 2008. Credit Suisse and Jefferies & Company acted as lead underwriters.
The follow-on public offering price was $18.50 per share and $74.5 million in the aggregate. Underwriting discounts and commissions were $1.0175 per share and $4.1 million in the aggregate. Proceeds after expenses to us were $16.72 per share and $19.0 million in the aggregate. Proceeds after expenses to the selling stockholders were $17.4825 per share and $50.5 million in the aggregate.
We did not receive any of the proceeds from the sale of shares by selling stockholders or on any exercise of the underwriters’ over-allotment option. The net proceeds received by us in the initial public offering were $46.2 million and in the follow-on offering were $19.0 million as follows:
| Initial Public Offering |
Follow-On Public Offering | |||||
| Aggregate offering proceeds to the Company |
$ | 52,800,000 | $ | 21,002,000 | ||
| Underwriting discounts and commissions |
3,696,000 | 1,155,000 | ||||
| Offering expenses |
2,940,000 | 865,000 | ||||
| Net proceeds to the Company |
$ | 46,164,000 | $ | 18,982,000 | ||
We used the net proceeds of the initial public offering to repay $14.1 million of our debt outstanding under our revolving credit facility and intend to continue to use the balance from the initial public offering and follow-on offering for general corporate purposes, including the acquisition of physician practices and working capital.
Securities Authorized for Issuance under Equity Participation Plans
Information required by this item with respect to our equity compensation plans will be contained in our definitive proxy statement for the 2010 Annual Meeting of Stockholders to be filed with the SEC and is hereby incorporated by reference.
Recent Sales of Unregistered Securities
None.
Purchases of Equity Securities by the Issuer and Affiliated Purchasers
None.
36
Table of Contents
| ITEM 6. | SELECTED FINANCIAL DATA |
We derived the following selected consolidated financial data for the five years ended December 31, 2009 from our audited consolidated financial statements. You should read the data in conjunction with Item 7 “Management’s Discussion and Analysis of Financial Condition and Results of Operations,” our consolidated financial statements, related notes and other financial information included herein. Historical results of operations and financial position are not necessarily indicative of the results that may be expected for future periods.
| Year Ended December 31, | ||||||||||||||||||||
| 2005 | 2006 | 2007 | 2008 | 2009 | ||||||||||||||||
| (dollars in thousands, except for per share data) | ||||||||||||||||||||
| Consolidated Statements of Operations Data: |
||||||||||||||||||||
| Net revenue |
$ | 110,883 | $ | 148,098 | $ | 190,002 | $ | 251,179 | $ | 310,521 | ||||||||||
| Operating expenses: |
||||||||||||||||||||
| Cost of services—physician practice salaries, benefits and other |
78,966 | 109,332 | 136,960 | 181,850 | 225,801 | |||||||||||||||
| General and administrative |
27,587 | 32,330 | 37,874 | 44,701 | 51,338 | |||||||||||||||
| Depreciation and amortization |
671 | 1,098 | 1,396 | 2,146 | 2,295 | |||||||||||||||
| Litigation loss and professional liability settlements(1),(2),(3) |
3,025 | 1,377 | — | — | 750 | |||||||||||||||
| Total operating expenses |
110,249 | 144,137 | 176,230 | 228,697 | 280,184 | |||||||||||||||
| Income from operations |
634 | 3,961 | 13,772 | 22,482 | 30,337 | |||||||||||||||
| Investment income |
342 | 233 | 397 | 604 | 84 | |||||||||||||||
| Interest expense |
(309 | ) | (1,313 | ) | (1,691 | ) | (868 | ) | (293 | ) | ||||||||||
| Loss on fair value of preferred stock warrant liabilities(4) |
(90 | ) | (690 | ) | (8,781 | ) | — | — | ||||||||||||
| Income before income taxes and cumulative effect of change in accounting principle |
577 | 2,191 | 3,697 | 22,218 | 30,128 | |||||||||||||||
| Income tax (benefit) provision(5) |
(4,009 | ) | 413 | 4,564 | 8,664 | 11,501 | ||||||||||||||
| Net income (loss) before cumulative effect of change in accounting principle |
4,586 | 1,778 | (867 | ) | 13,554 | 18,627 | ||||||||||||||
| Cumulative effect of change in accounting principle |
(941 | ) | — | — | — | — | ||||||||||||||
| Net income (loss) |
3,645 | 1,778 | (867 | ) | 13,554 | 18,627 | ||||||||||||||
| Accretion of redeemable convertible preferred stock(4) |
(248 | ) | (271 | ) | (229 | ) | — | — | ||||||||||||
| Income allocable to preferred stockholders |
(3,397 | ) | (1,507 | ) | — | (696 | ) | — | ||||||||||||
| Net (loss) income attributable to common stockholders |
$ | — | $ | — | $ | (1,096 | ) | $ | 12,858 | $ | 18,627 | |||||||||
| Per share data: |
||||||||||||||||||||
| Net (loss) income per share attributable to common stockholders—historical(6): |
||||||||||||||||||||
| Basic |
$ | — | $ | — | $ | (0.64 | ) | $ | 0.88 | $ | 1.16 | |||||||||
| Diluted |
$ | — | $ | — | $ | (0.64 | ) | $ | 0.87 | $ | 1.14 | |||||||||
| Net income (loss) per share attributable to common stockholders— pro forma(7): |
||||||||||||||||||||
| Basic |
$ | 0.36 | $ | 0.17 | $ | (0.08 | ) | $ | 0.89 | N/A | ||||||||||
| Diluted |
$ | 0.35 | $ | 0.16 | $ | (0.08 | ) | $ | 0.88 | N/A | ||||||||||
| Other Operating Data: |
||||||||||||||||||||
| Number of patient encounters (in thousands) |
1,302 | 1,747 | 2,153 | 2,790 | 3,294 | |||||||||||||||
| Hospitalists at end of the year |
421 | 432 | 546 | 781 | 1,036 | |||||||||||||||
| Other Financial Information: |
||||||||||||||||||||
| Net cash provided by (used in) operating activities |
$ | 1,415 | $ | (4,768 | ) | $ | 1,442 | $ | 14,368 | $ | 23,484 | |||||||||
| Net cash (used in) provided by investing activities |
(18,931 | ) | 754 | (13,729 | ) | (31,460 | ) | (22,112 | ) | |||||||||||
| Net cash provided by (used in) financing activities |
8,758 | 3,239 | 13,317 | 47,510 | 7,293 | |||||||||||||||
| Net (decrease) increase in cash and cash equivalents |
(8,758 | ) | (775 | ) | 1,030 | 30,418 | (5,921 | ) | ||||||||||||
| Consolidated Balance Sheet Data: |
||||||||||||||||||||
| Cash and cash equivalents |
$ | 6,721 | $ | 5,946 | $ | 6,976 | $ | 37,394 | $ | 31,473 | ||||||||||
| Total assets |
63,187 | 76,029 | 97,376 | 162,691 | 188,212 | |||||||||||||||
| Total debt including current portion of long-term debt |
11,458 | 14,451 | 26,822 | 8,839 | — | |||||||||||||||
| Redeemable convertible preferred stock |
42,731 | 43,002 | — | — | — | |||||||||||||||
| Total stockholders’ (deficit) equity |
(12,796 | ) | (11,014 | ) | 43,017 | 122,947 | 145,077 | |||||||||||||
37
Table of Contents
| (1) | In 2005, we recorded $3.0 million as a litigation loss related to a judgment resulting from an action brought by a former non-physician independent contractor. In December 2007, the judgment and accrued interest were paid in full. |
| (2) | During 2006, we settled a professional liability claim in excess of our insurance policy limit. We recorded the settlement at the net present value of $1.3 million of which we paid $0.8 million during 2006 and the balance was paid in 2007. We also recorded additional legal fees related to the appeal of the judgment in connection with the action brought by a former non-physician independent contractor in 2005. |
| (3) | During the first quarter of 2010, we reached a preliminary agreement to settle a disputed professional liability claim for a prior year that is in excess of our insurance policy limit. The settlement remains subject to definitive documentation and is contingent upon receiving applicable court approval. We recorded our portion of the settlement of $0.8 million in the fourth quarter of 2009. |
| (4) | On October 29, 2007, our certificate of incorporation was amended to remove the redemption feature of our preferred stock. On such date, our redeemable convertible preferred stock was no longer redeemable and the warrants to purchase such stock were reclassified to permanent equity. Upon completion of our initial public offering, warrants held by our preferred stockholders were automatically converted into 609,197 shares of our common stock in a cashless exchange using the treasury stock method and the remaining warrants exercisable into 86,458 common shares, were classified as permanent equity. All remaining warrants were exercised as of October 2008. |
| (5) | During 2005, our income tax valuation allowance, primarily related to net operating losses was partially reversed based on historical earnings and expected future income from operations adequate to recognize a significant portion of our deferred tax assets. During 2006, the remaining valuation allowance for consolidated entities that file consolidated tax returns was reversed for the same reasons as for 2005. |
| (6) | All per share data has been adjusted to reflect a 1-for-6.4 reverse stock split which was completed in January 2008. |
| (7) | Pro forma earnings per share data assumes the conversion of preferred shares to common stock on the first day of such period at a ratio of 6.4:1 as well as a cashless exchange of warrants held by our preferred stockholders using the treasury stock method. |
38
Table of Contents
| ITEM 7. | MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS |
The following discussion highlights the principal factors that have affected our financial condition and results of operations as well as our liquidity and capital resources for the periods described. This discussion should be read in conjunction with our consolidated financial statements and the related notes included in this Report. This discussion contains forward-looking statements that are subject to known and unknown risks. Actual results and the timing of events may differ significantly from those expressed or implied in such forward-looking statements due to a number of factors, including those set forth in the section entitled “Risk Factors” and elsewhere in this Report. The operating results for the periods presented were not significantly affected by inflation.
Company Overview and Recent Developments
We are a leading provider of hospitalist services in the United States. Hospitalist medicine is organized around inpatient care, primarily delivered in hospitals, and is focused on providing, managing and coordinating the care of hospitalized patients. We believe we are the largest dedicated hospitalist company in the United States based on revenues, patient encounters and number of affiliated hospitalists. As of December 31, 2009, either through our wholly-owned subsidiaries or our affiliated professional organizations, we employ or affiliate with 1,036 hospitalists who provide hospitalist services at over 475 hospitals and medical facilities in 21 states. We have had more than 8.2 million patient encounters since the beginning of 2007. Our early entry into the emerging hospitalist industry has permitted us to establish a reputation and leadership position that we believe is closely identified with hospitalist medicine.
We began operating our first hospitalist practice in 1998 and have increased the number of our practice groups to over 180. Since the beginning of 2007, we have acquired 27 practice groups and successfully integrated them into IPC and onto IPC-Link®, our proprietary technology-based management system. Our affiliated hospitalists are primarily full-time employees of our wholly-owned subsidiaries or our affiliated professional organizations, and we also employ over 450 other physicians and non-physician providers and contract with over 200 independent contractors, who provide episodic care as needed.
Subsequent to December 31, 2009, we completed the acquisition of the assets of one hospitalist physician practice.
During the first quarter of 2010, we reached a preliminary agreement to settle a disputed professional liability claim for a prior year that is in excess of our insurance policy limit. The settlement remains subject to definitive documentation and is contingent upon receiving applicable court approval. We recorded our portion of the settlement of $0.8 million in the fourth quarter of 2009.
Initial Public Offering and Follow-On Public Offering
On January 30, 2008, we completed our initial public offering (IPO) for the sale of 5,905,000 shares of our common stock at a price of $16.00 per share. Of these shares 3,300,000 were newly issued shares sold by us, and 2,605,000 were shares sold by existing stockholders. We received net proceeds of $46,164,000 after deducting underwriting discounts and commissions of $3,696,000 and other fees and expenses of $2,940,000. Upon completion of our IPO, all of our preferred stock, and a majority of our warrants converted to common stock. Immediately after the offering, and including the conversion of the preferred stock and warrants, there were 14,844,934 shares of our common stock outstanding.
On July 21, 2008, we closed a follow-on public offering for the sale of 4,025,000 shares of our common stock at a price of $18.50 per share. Of these shares 1,135,231 shares were newly issued shares sold by us, and 2,889,769 were shares sold by certain of our existing stockholders. We received net proceeds of $18,982,000 after deducting underwriters’ discounts and commissions of $1,155,000 and fees and expenses of $865,000. Immediately after the offering, there were 16,017,237 shares of our common stock outstanding.
39
Table of Contents
Practice Acquisitions
During the year ended December 31, 2009, we acquired the assets of eight hospitalist physician practices for a total estimated purchase price of $24,294,000. In connection with these acquisitions, we recorded goodwill of $23,519,000, furniture and equipment of $6,000 and other identifiable intangible assets of $769,000 consisting of physician, payor and hospital agreements. We also recorded $4,289,000 of additional goodwill related to contingent consideration pertaining to acquisitions that occurred prior to 2009. Total transaction costs of $82,000 for 2009 acquisitions were expensed as incurred.
Key Performance Indicators
We manage our business by monitoring certain key performance indicators that impact our revenue and profitability. The most important key performance indicators for our business are:
| • | Patient encounters — billable encounters generated by our affiliated hospitalists. Typically we have one billable encounter per patient per day although our affiliated hospitalists may have several interactions with a patient during a twenty-four hour period. |
| • | Revenue per encounter — net revenue from patient billings divided by patient encounters. |
| • | Average encounters per hospitalist per day — the number of patient encounters for a day divided by the number of hospitalists, adjusted for full or part-time status, measured for the same period. We use this metric to monitor our affiliated hospitalists’ productivity. |
Geographic Coverage and Revenue
During 2007, 2008 and 2009 approximately 71%, 67% and 69%, respectively, of our net revenue was generated by operations in five states: Arizona, Florida, Michigan, Missouri and Texas. Over those same periods, our operations in Texas accounted for approximately, 27%, 26% and 24% of our net revenue. Although we continue to seek to diversify the geographic scope of our operations, primarily through acquisitions of physician group practices or by recruiting new hospitalists or entering into new hospital contracts, we may not be able to successfully implement or realize the expected benefits of any of these initiatives. Adverse changes or conditions affecting states in which our operations are concentrated, such as healthcare reforms, changes in laws and regulations, reduced Medicaid reimbursements, or government investigations, may have a material adverse effect on our business, financial condition and results of operations.
We generate approximately 94% of our net revenue primarily from billings to third-party payors such as Medicare, Medicaid, managed care organizations and insurance companies. We generate the remaining 6% of our net revenue from hospitals and other inpatient facilities for organizing and managing hospitalist programs, providing medical directorships and providing coverage for patients admitted from the emergency department who otherwise have no assigned admitting physician.
Our affiliated hospitalists generally document and submit billing codes daily through the use of IPC-Link®. IPC-Link® captures all our patient demographic and clinical information for billing and submits this data electronically after a series of automated edits and manual review of any exceptions. Our automated edit procedures follow specific business rules to correct billing errors. We utilize a sophisticated tracking and monitoring system to obtain receipt of appropriate reimbursement from our payors and identify billing issues and trends early in the reimbursement process. Our monitoring system is able to identify when we are reimbursed less than what we are contracted to receive and report when we have not received appropriate payment or other issues have developed. Based on the information from our monitoring system, our collection department contacts third party payors to resolve billing issues and to expedite our collections. If we have a contractual relationship with the payor, we pursue the collection until the issue is resolved. If we are unable to collect from third-party payors and we do not have a contractual relationship with the payor, we bill the patient for the unpaid balance. We use outside service organizations to invoice and collect co-payments and/or deductibles from insured patients and discounted fees from uninsured, or self-pay, patients. After 120 days of internal collection efforts, we write off the unpaid accounts and send them to an outside collection agency.
40
Table of Contents
We determine our net revenue from patient billings based on our estimate of collections from payors. Our fee schedule is the same for all parties regardless of geography or party responsible for paying the bill for our services. We are reimbursed by Medicare and Medicaid at government established rates, by managed care and insurance organizations at contracted rates or other discounted rates and have various arrangements with other third-party insurers. In addition, patients may be personally responsible for a deductible or co-payment under their third-party payor coverage. We may provide discounted or free services to self-pay patients who require hospital admission when we are providing admission coverage for emergency departments, if our collection attempts are unsuccessful. Due to the uncertainty regarding collectability of charges associated with services we provide to uninsured patients and patients with co-pay or deductible balances, our net revenue recognition for these patients is based on our expected cash collections.
With respect to our revenue generated from billings to third-party payors, the table below summarizes our approximate payor mix as a percentage of patient encounters for the periods indicated:
| Year Ended December 31, | ||||||
| 2007 | 2008 | 2009 | ||||
| Medicare |
46% | 45% | 43% | |||
| Medicaid |
4% | 5% | 5% | |||
| Other third parties |
40% | 43% | 45% | |||
| Self-pay patients |
10% | 7% | 7% | |||
| 100% | 100% | 100% | ||||
The decrease in the percentage of our self-pay patients from 2007 to 2008 reflects better identification of sources of reimbursement for patient encounters and reduction in coverage of emergency departments in certain cases. The percentage of our net revenue related to self-pay patients is a significantly smaller percentage of our net revenues as much of these services are uncompensated.
Seasonality and Quarterly Fluctuations
We have historically experienced and expect to continue to experience quarterly fluctuations in net revenue and income from operations. Absent the impact and timing of acquisitions, our net revenue has historically been higher in the first and fourth quarters of the year primarily due to the following factors:
| • | the number of physicians we have on staff during the quarter, which may fluctuate based upon the timing of hires due to the end of the academic year for graduating resident physicians, the schedule of the Internal Medicine Board exams and terminations in our existing practices; and |
| • | fluctuations in patient encounters, which are impacted by hospital census, which can be volatile, and physician productivity and often reflect seasonality due to the higher occurrence of illnesses such as flu and pneumonia in patient populations in the first quarter. |
We have significant fixed operating costs, including physician practice salaries and benefits and, as a result, are highly dependent on patient encounters and the productivity of our hospitalists to sustain profitability. Additionally, quarterly results may be affected by the timing of acquisitions and the hiring and termination of our affiliated hospitalists.
Factors Affecting Operating Results
Rate Changes by Government Sponsored Programs
The Medicare program reimburses for our services based upon the rates in its Physician Fee Schedule, and each year the Medicare program updates the Physician Fee Schedule reimbursement rates based on a formula approved by Congress in the Balanced Budget Act of 1997. Many private payors use the Medicare fee schedule to determine their own reimbursement rates. Effective January 1, 2009, the Medicare update resulted in an estimated overall 4.6% weighted average increase in Medicare reimbursement rates for the codes applicable to
41
Table of Contents
the services performed by our affiliated hospitalists and an estimated overall 2.6% increase in our net patient revenue per encounter.
The Medicare law requires the Centers for Medicare and Medicaid Services (CMS) to adjust the Medicare Physician Fee Schedule payment rates annually based on an update formula which includes application of the Sustainable Growth Rate (SGR) that was adopted in the Balanced Budget Act of 1997. This formula has yielded negative updates every year beginning in 2002, although CMS was able to take administrative steps to avoid a reduction in 2003, and Congress has taken a series of legislative actions to prevent reductions each year from 2004 to 2009. In December 2009, Congress passed a stay of the negative update to the SGR for a two month period of January and February 2010. Based on current data, CMS is projecting a rate reduction of approximately 21% for 2010 if Congress does not take further legislative action as they have done in prior years.
In December, 2009, CMS finalized several changes to refine Medicare payments to physicians effective January 1, 2010, which increased payment rates for primary care services. The proposals include an update to the practice expense component of physician fees which is to be implemented over four years. CMS also ceased payments for consultation codes, which are typically billed by specialists, including our physicians, and were paid at a higher rate than equivalent evaluation and management (E/M) services. Practitioners will use existing E/M service codes when providing these services instead. Resulting savings were redistributed to increase payments for the existing E/M services. In addition, CMS refined how Medicare recognizes the cost of professional liability insurance in its payment system. Also, effective January 1, 2010, the Geographic Practice Cost Indices floor of 1.0 expired which resulted in a decrease in payments to any geographic area with an index of less than 1.0. These changes, taken together with the stay in the negative update to the SGR, resulted in an estimated 1% - 2% increase in Medicare reimbursement rates for the codes applicable to the services performed by our affiliated hospitalists and an overall estimated increase of less than 1% in our net patient revenue per encounter
While Congress has intervened in the past few years to mitigate projected CMS rate reductions, there is no guarantee that Congress will continue to do so in the future Similarly, no assurance can be provided as to the ultimate content, timing or effect of any other healthcare reform legislation being considered by Congress, nor is it possible at this time to estimate the impact of any potential healthcare reform legislation on our business.
Professional Liability Rates
Medical malpractice insurance premium rates are affected by a variety of factors both internal, including our own loss experience and the associated defense costs, and external such as medical malpractice loss experience for internal medicine physicians which varies greatly across different regions. Other factors include varying state laws covering tort reform, the local climate for large jury awards, the rate of investment income and reinsurance costs, all of which can result in wide variations in premium rates not only from region to region, but also from year to year. Although our malpractice premium rates have remained relatively stable over the last three years, the factors discussed above could lead to variations in future costs.
Principles of Consolidation
Our consolidated financial statements include the accounts of IPC The Hospitalist Company, Inc. and its wholly owned subsidiaries and consolidated professional medical corporations managed under long-term management agreements (the Professional Medical Corporations). Some states have laws that prohibit business entities, such as IPC, from practicing medicine, employing physicians to practice medicine, exercising control over medical decisions by physicians (collectively known as the corporate practice of medicine), or engaging in certain arrangements with physicians, such as fee-splitting. In states that have these restrictions, we operate by maintaining long-term management contracts with the Professional Medical Corporations, which are each owned and operated by physicians, and which employ or contract with additional physicians to provide hospitalist services. Under the management agreements, we provide and perform all non-medical management and administrative services, including financial management, information systems, marketing, risk management and administrative support. The management agreements have an initial term of 20 years and are automatically renewable for successive 10-year periods unless terminated by either party for cause. The management
42
Table of Contents
agreements are not terminable by the Professional Medical Corporations, except in the case of gross negligence, fraud, or other illegal acts by us, or bankruptcy of IPC.
Through the management agreements and our relationship with the stockholders of the Professional Medical Corporations, we have exclusive authority over all non-medical decision making related to the ongoing business operations of the Professional Medical Corporations. Further, our rights under the management agreements are unilaterally salable or transferable. Based on the provisions of the agreements, we have determined that the Professional Medical Corporations are variable interest entities (VIE’s), and that we are the primary beneficiary because we have controls over the operations of these VIE’s. Consequently, we consolidate the revenue and expenses of the Professional Medical Corporations from the date of execution of the agreements. All intercompany balances and transactions have been eliminated in consolidation.
Critical Accounting Estimates
The preparation of financial statements requires management to make estimates and assumptions relating to the reporting of results of operations, financial condition and related disclosure of contingent assets and liabilities at the date of the financial statements. Actual results may differ from those estimates under different assumptions or conditions. The following are our most critical accounting estimates, which are those that require management’s most difficult, subjective and complex judgments, requiring the need to make estimates about the effect of matters that are inherently uncertain and may change in subsequent periods.
The following discussion is not intended to represent a comprehensive list of our accounting estimates. For a detailed discussion of the application of these and other accounting policies, see Note 1 to our audited consolidated financial statements included in this Report.
Revenues
Net revenue primarily consists of fees for medical services provided by our affiliated hospitalists under fee-for-service and other professional fee arrangements with various payors including Medicare, Medicaid, managed care organizations, insurance companies and hospitals.
We report net revenue in the period in which services are provided, at rates that reflect the amount expected to be collected. Although we have standard billing rates in our system, we do not use these standard billing rates for recording the amount of revenue we expect to collect. Some providers of medical services record revenue at their standard billing rates with an allowance for contractual discounts. The process of estimating the ultimate amount of revenue to be collected is highly subjective and requires the application of judgment based on many factors, including contractual reimbursement rates, the payor mix, age of receivables, historical cash collection experience and other relevant information. Revenue related to patient responsibility accounts, including both deductible and co-pays for insured patients and discounted fees for uninsured patients, is recorded at amounts reasonably assured of collection.
The evaluation of these factors, as well as the interpretation of governmental regulations and private insurance contract provisions, involves complex, subjective judgments. As a result of the inherent complexity of these calculations, our actual revenues and net income, and our accounts receivable, could vary from the amounts reported.
Accounts Receivable
Accounts receivable primarily consists of amounts due from third-party payors, including governmental programs, such as Medicare and Medicaid, managed care organizations, insurance companies, hospitals and amounts due from patients. Accounts receivable are stated at the amount expected to be collected, net of reserves for amounts estimated by management to be uncollectible. We write off uncollectible accounts receivable after reasonable collection efforts have been exhausted. We also regularly analyze the ultimate collectability of accounts receivable after certain stages of the collection cycle using a look-back analysis to determine the amount of receivables subsequently collected and adjustments are recorded when necessary.
43
Table of Contents
Goodwill and Other Intangible Assets
We record acquired assets and liabilities and additional future consideration at their acquisition-date fair values, and expense all transaction related costs under the acquisition method of accounting. Goodwill represents the excess of cost over the fair value of the net assets acquired. Other intangible assets primarily represent the fair value of hospital service contract agreements and non-compete agreements acquired in connection with certain asset purchase agreements. Goodwill and other indefinite-lived intangible assets are not amortized. Separable identified intangible assets that have finite lives are amortized over their useful lives.
In addition to the initial consideration paid at the close of each business combination, the asset purchase agreements for certain completed practice acquisitions provide for additional future consideration to be paid, which is generally based upon the achievement of certain operating results of the acquired practices as of certain measurement dates. Pursuant to new GAAP, the estimated fair value of additional future consideration related to transactions that are completed on or after January 1, 2009, is accrued at the acquisition-date. Subsequent changes, if any, to the acquisition-date fair value of transactions that occurred after January 1, 2009 are recognized as part of on-going operations.
We review and evaluate goodwill and other intangible assets for impairment on an annual basis, as well as when events or changes in business conditions suggest potential impairment, at the entity level since we operate in only one line of business. The testing for impairment is completed using a two step test. The first step compares the fair value of our Company with its carrying amount, including goodwill. If the carrying amount of the entity exceeds its fair value, a second step is performed to determine the amount of any impairment loss. During 2007, 2008 and 2009, no impairment indicators were present and no impairment was recognized.
Claims Liability and Professional Liability Reserves
For 2008 and prior years, we were self-insured up to certain limits for costs associated with professional liability claims. Reserves are evaluated regularly for such self-insurance retention. As of January 1, 2009, our professional liability insurance was changed to first dollar coverage up to our policy limits. Our malpractice policies are on a claims-made basis; consequently, we establish reserves on an undiscounted basis for estimates of the loss that we will ultimately incur on claims that have been incurred but not reported. These reserves are based upon actuarial loss projections, which are updated semi-annually. The actuarial loss projections consider a number of factors, including historical claim payment patterns and changes in case reserves and the assumed rate of increase in healthcare costs. Historical experience and recent trends in the historical experience are the most significant factors in the determination of these reserves. We believe the use of actuarial methods to account for these reserves provides a consistent and effective way to measure these subjective accruals. However, given the magnitude of the claims involved and the length of time until the ultimate cost is known, the use of any estimation technique in this area is inherently sensitive and subject to change when actual paid claims information becomes known. Accordingly, our recorded reserves could differ from our ultimate costs related to these claims due to changes in our incident reporting, claims payment and settlement practices or claims reserve practices, as well as differences between assumed and future cost increases.
Recently Adopted and New Accounting Pronouncements
See Note 1 to the Consolidated Financial Statements for information regarding recently adopted and new accounting principles.
44
Table of Contents
Results of Operations and Operating Data
Consolidated Results
The following table sets forth operating data and selected consolidated statements of operations information stated as a percentage of net revenue:
| Year Ended December 31, | ||||||
| 2007 | 2008 | 2009 | ||||
| Operating data—patient encounters |
2,153,000 | 2,790,000 | 3,294,000 | |||
| Net revenue |
100.0% | 100.0% | 100.0% | |||
| Operating expenses: |
||||||
| Cost of services-physician practice salaries, benefits and other |
72.1% | 72.4% | 72.7% | |||
| General and administrative |
19.9% | 17.8% | 16.5% | |||
| Depreciation and amortization |
0.7% | 0.8% | 0.8% | |||
| Professional liability settlement |
0.0% | 0.0% | 0.2% | |||
| Total operating expenses |
92.7% | 91.0% | 90.2% | |||
| Income from operations |
7.3% | 9.0% | 9.8% | |||
| Investment income |
0.2% | 0.2% | 0.0% | |||
| Interest expense |
(0.9)% | (0.4)% | (0.1)% | |||
| Loss on fair value of preferred stock warrant liabilities |
(4.6)% | 0.0% | 0.0% | |||
| Income before income taxes |
2.0% | 8.8% | 9.7% | |||
| Income tax provision |
2.4% | 3.4% | 3.7% | |||
| Net income (loss) |
(0.4)% | 5.4% | 6.0% | |||
Year ended December 31, 2009 compared to year ended December 31, 2008
Our patient encounters for 2009 increased 18.1% to 3,294,000, compared to 2,790,000 for 2008. Net revenue for 2009 was $310.5 million, an increase of $59.3 million, or 23.6%, from $251.2 million for 2008. Of this $59.3 million increase, $45.8 million or 77.2% was attributable to same-market area growth and $13.5 million was attributable to revenue generated from acquisitions which enabled us to enter new markets. We entered one of these new markets through an acquisition in the third quarter of 2008 and two new markets through acquisitions in 2009. Same-market areas are those geographic areas in which we have had operations for the entire current period and the entire comparable prior period. Because in-market area acquisitions are often small practice groups which become subsumed within existing practice groups and are managed by our existing regional management staff, we consider these as part of our same-market area growth. Same-market area net revenue increased 18.7% primarily as the result of a 13.5% increase in patient encounters and a 3.8% increase in patient revenue per encounter, with the remainder due to an increase in hospital contract revenue. The increase in patient revenue per encounter was partially due to a 2.6% net increase in Medicare reimbursement rates effective January 1, 2009 for the codes applicable to the services performed by our affiliated hospitalists and the remainder is a result of improvements in our billing processes and collections.
Physician practice salaries, benefits and other expenses for 2009 were $225.8 million or 72.7% of net revenue compared to $181.9 million or 72.4% of net revenue for 2008. These costs increased by $43.9 million or 24.2%. Same-market area physician costs increased a total of $34.3 million, of which $30.8 million was from costs of net new hires or acquired physician practices in the same-market area. Costs related to existing physicians increased by $3.5 million. In addition, $9.6 million of the $43.9 million overall cost increase is attributable to physician costs associated with new market openings and new market acquisitions. Physician costs as a percentage of net revenue increased slightly as a result of practices under development.
45
Table of Contents
General and administrative expenses increased $6.6 million, or 14.8%, to $51.3 million, or 16.5% of net revenue, for 2009, as compared to $44.7 million, or 17.8% of net revenue for 2008. The increase in expense is the result of increased stock based compensation, an increase in the number of national physician meetings and increased costs to support the continuing growth of our operations, including a new regional office to support a new market acquisition, additional corporate development, and finance and information technology expenses. General and administrative expenses decreased as a percentage of net revenue as we continue to leverage these costs over a larger revenue base.
During the first quarter of 2010, we reached a preliminary agreement to settle a disputed professional liability claim for a prior year that is in excess of our insurance policy limit. The settlement remains subject to definitive documentation and is contingent upon receiving applicable court approval. We recorded our portion of the settlement of $0.8 million in the fourth quarter of 2009.
Income from operations increased $7.8 million, or 34.9%, to $30.3 million, as compared to $22.5 million for 2008. Our operating margin increased to 9.8% for 2009 from 9.0% for 2008. The increase in operating margin percentage is directly attributable to the reduction in general and administrative expenses as a percentage of net revenue.
We recorded interest expense of $0.3 million for 2009, as compared to $0.9 million for 2008. The decrease in interest expense is primarily attributable to the lower term-loan balances during 2009 compared to 2008 and the payoff of the balances outstanding on our term-loan and equipment loans in June 2009.
Our effective tax rate for the year ended December 31, 2009 was 38.2% compared to 39.0% for the year ended December 31, 2008. The 2009 effective tax rate differs from 2008 primarily due to an increase in state enterprise zone tax credits. The effective tax rate differs from the statutory U.S. federal rate of 35.0% due primarily to state income taxes. We expect our 2010 effective income tax rate to be approximately 39.0%.
Net income increased to $18.6 million for 2009, as compared to $13.6 million for 2008, and our net income margin increased to 6.0% from 5.4% for the same period in the prior year. The net income margin increase to 6.0 % is primarily the result of leveraging our general and administrative expenses over a larger revenue base as we grow our practices and acquire new practices.
Year ended December 31, 2008 compared to year ended December 31, 2007
Our patient encounters for 2008 increased 29.6% to 2,790,000, compared to 2,153,000 for 2007. Net revenue for the year ended December 31, 2008 was $251.2 million, an increase of $61.2 million, or 32.2%, from $190.0 million for the year ended December 31, 2007. Of this $61.2 million increase, $36.3 million, or 59.3% was attributable to same-market area growth and $24.9 million was attributable to revenue generated from completed acquisitions during 2008 and 2007. Same-market area net revenue increased 20.1% primarily as the result of a 16.6% increase in patient encounters. Overall net revenue per encounter increased by 2.1%, primarily as a result of an increase in revenue from hospital contracts and increases in net patient revenue per encounter primarily as a result of improvements in our billing processes and collections.
Physician practice salaries, benefits and other expenses for the year ended December 31, 2008 were $181.9 million or 72.4% of net revenue compared to $137.0 million or 72.1% of net revenue for the year ended December 31, 2007. These costs increased by $44.9 million or 32.8%. Same-market area physician costs increased a total of $26.6 million, or 20.3% of which $6.4 million was primarily the result of increased salaries, practice bonuses and other costs related to an increase in existing hospitalists’ productivity and $20.2 million was from costs of net new hires or acquired physicians in the same-market area practices. The remaining increased cost of $18.3 million is attributable to physician costs associated with new market acquisitions. Physician costs as a percentage of net revenue increased slightly as a result of lower physician productivity in new practices under development.
46
Table of Contents
General and administrative expenses increased $6.8 million, or 17.9%, to $44.7 million, or 17.8% of net revenue, for the year ended December 31, 2008, as compared to $37.9 million, or 19.9% of net revenue for the year ended December 31, 2007. The increase is the result of a combination of increased costs as a public company, increased stock compensation expense and increased costs to support the continuing growth of our operations, and our acquisitions, including the addition of new regional offices to support our geographic expansion. General and administrative expenses decreased as a percentage of net revenue as we continue to leverage these costs over a larger revenue base.
Income from operations increased $8.7 million, or 63.0% to $22.5 million for the year ended December 31, 2008, as compared to $13.8 million for the same period in the prior year. Our operating margin increased to 9.0% for the year ended December 31, 2008 from 7.3% for the year ended December 31, 2007. The increase in operating margin percentage is directly attributable to the reduction in general and administrative expenses as a percentage of net revenue.
We recorded interest expense of $0.9 million for the year ended December 31, 2008, as compared to interest expense of $1.7 million for the year ended December 31, 2007. The decrease in interest expense is primarily attributable to the pay-off of balances outstanding on our revolving credit agreement with proceeds from our initial public offering in January 2008.
Our effective tax rate for the year ended December 31, 2008 was 39.0% compared to 42.0% for the year ended December 31, 2007, excluding the nondeductible loss of $8.8 million we incurred related to the change in the fair value preferred stock warrant liabilities in 2007, a benefit from utilization of net operating losses that were subject to a valuation allowance from separate tax filing entities, and a rate change benefit applicable to federal deferred tax assets. The 2008 effective tax rate includes a state enterprise zone tax credit, which reduced the 2008 state effective tax rate by approximately 2.0%. The effective tax rate differs from the statutory U.S. federal rate of 35.0% due primarily to state income taxes.
Net income increased to $13.6 million for the year ended December 31, 2008, as compared to a net loss of $0.9 million for the year ended December 31, 2007 and our net income margin increased to 5.4% from a negative 0.5% for the same period in the prior year. During 2007, we recorded a loss of $8.8 million related to the change in the fair value of preferred stock warrant liabilities. Excluding such loss in 2007, our net income margin was 4.2%. The net income margin increase to 5.4% is primarily the result of leveraging our general and administrative expenses over a larger revenue base as we grow our practices and acquire new practices.
Liquidity and Capital Resources
In January 2008, we completed our initial public offering which resulted in net proceeds of $46.2 million to us after payment of underwriting discounts and commissions and offering expenses. We used part of the proceeds to pay off the outstanding balance of $14.1 million under the revolving portion of our credit agreement.
On July 21, 2008, we closed a follow-on public offering for the sale of 4,025,000 shares of our common stock at a price of $18.50 per share. Of these shares 1,135,231 shares were newly issued shares sold by us, and 2,889,769 were shares sold by existing stockholders. We received net proceeds of $18,982,000 after deducting underwriters’ discounts and commissions of $1,155,000 and fees and expenses of $865,000. Immediately after the offering, there were 16,017,237 shares of our common stock outstanding. At December 31, 2008, we had outstanding borrowings of $8.8 million on our term loan and other financings, a letter of credit of $0.1 million outstanding under our $30.0 million revolving credit agreement and $37.4 million in cash and cash equivalents.
In June 2009, we paid off all remaining debt of $7.3 million under our term loan and our equipment financing loans. At December 31, 2009, we had $31.5 million in cash and cash equivalents.
47
Table of Contents
Year ended December 31, 2009 compared to year ended December 31, 2008
Net cash provided by operating activities for 2009 increased to $23.5 million compared to $14.4 million for 2008. Accounts receivable increased by $3.8 million during 2009. However, on a days sales outstanding (DSO) basis, which we use to measure the effectiveness of our collections, DSO decreased to 54 DSO as of December 31, 2009 compared to 60 DSO as of December 31, 2008. We calculate our DSO using a three-month rolling average of net revenues. Accrued compensation increased $3.8 million for 2009 compared to a decrease of $1.2 million for 2008 due to the timing of our bi-weekly payroll in relation to the period ending date of December 31. Prepaid expenses increased by $0.5 million for 2009 compared to a decrease of $2.1 million for 2008. The 2008 decrease in prepaid expenses was higher than the 2009 decrease because of prepaid costs related to our initial public offering in early 2008.
Net cash used in investing activities was $22.1 million for 2009, compared to $31.5 million for 2008. Cash of $20.2 million was used in 2009 for physician practice acquisitions and earn-out payments on prior acquisitions compared to $29.9 million used in 2008. The remainder of cash used in investing activities was for purchases of computer hardware and software, and office furnishings.
For 2009, net cash used in financing activities was $7.3 million, compared to $47.5 million provided by financing activities for 2008. In January 2008, we completed our initial public offering which resulted in aggregate net proceeds of $46.2 million to us after payment of underwriting discounts and commissions and offering expenses. We used part of the proceeds of our initial public offering to pay off the outstanding balance of $14.1 million under the revolving portion of our Credit Facility in January 2008, and in late June 2009 we paid off all remaining debt of $7.3 million under our term loan and our equipment financing loans. In July 2008, we completed a follow-on public offering which resulted in aggregate net proceeds of $19.0 million to us after payment of underwriting discounts and commissions and offering expenses. We intend to continue to use the net proceeds of the initial and follow-on public offerings for general corporate purposes, including the acquisitions of physician practices and working capital.
Year ended December 31, 2008 compared to year ended December 31, 2007
Net cash provided by operating activities for the year ended December 31, 2008 was $14.4 million compared to $1.4 million provided by operations for the same period of 2007. Operating cash flow from changes in working capital for the year ended December 31, 2008 increased by $7.2 million. Accounts receivable increased by $5.0 million during the year ended December 31, 2008. However, DSO decreased to 60 DSO as of December 31, 2008 compared to 69 DSO as of December 31, 2007. Prepaid expenses decreased by $2.1 million for the 2008 period compared to an increase of $3.2 million for the 2007 period. The decrease was primarily the result of funding of $1.8 million in prepaid IPO costs from our public stock offering in January 2008.
Net cash used in investing activities was $31.5 million for the year ended December 31, 2008, compared to net cash used in investing activities of $13.7 million for the same period in 2007. Cash of $29.9 million was used in 2008 for acquisitions of physician practices and earn-out payments on 2008 and prior years acquisitions compared to $15.3 million in the same period of the prior year. The remainder of cash used in investing activities was for purchases of computer hardware and software and office furnishings.
For the year ended December 31, 2008, net cash provided by financing activities was $47.5 million, compared to $13.3 million for the year ended December 31, 2007. During 2008, we completed our initial public offering and a follow-on offering which resulted in aggregate net proceeds of $65.2 million to us after payment of underwriting discounts and commissions and offering expenses. These proceeds were offset by debt payments of $18.0 million, of which $14.1 million paid off the outstanding balance under the revolving portion of our credit agreement shortly after our initial public offering in January 2008.
48
Table of Contents
Credit Facility and Liquidity
Our Credit Facility provides a revolving line of credit of $30.0 million, with a sublimit of $5.0 million for the issuance of letters of credit, plus a term loan in an original amount of $10.0 million. The Credit Facility has a maturity date of September 15, 2011. We use the Credit Facility for working capital, practice acquisitions and capital expenditures. The outstanding principal balance under the term loan portion of the Credit Facility was zero and $8.8 million as of December 31, 2009 and 2008, respectively. In June 2009, we paid off all outstanding debt under the term loan and our equipment financing loans. At December 31, 2009, we had a letter of credit of $100,000 outstanding and $29.9 million available under the revolving line of credit.
The revolving line of credit is limited by a formula based on a certain multiple times the trailing twelve months of earnings before interest, taxes, depreciation, amortization, and certain non-cash items. Borrowings under the Credit Facility bear interest at a rate based on either LIBOR plus 1.5% to 2.0%, or the lender’s prime rate, as selected by us for each advance. We pay an unused commitment fee equal to 0.25% per annum on the difference between the revolving line capacity and the average balance outstanding for each quarter. Outstanding amounts advanced to us under the revolving line of credit are repayable on or before the maturity date. The Credit Facility is secured by all of our current and future personal and intellectual property assets, except those held subject to purchase money loans and capital leases. The Credit Facility includes various customary financial covenants and restrictions, as well as customary remedies for our lenders following an event of default. As of December 31, 2009, we were in compliance with such financial covenants and restrictions.
We anticipate that funds generated from operations, together with our current cash on hand and funds available under our revolving credit agreement will be sufficient to finance our working capital requirements and fund anticipated acquisitions, contingent acquisition consideration and capital expenditures.
Contractual Obligations and Reserves
The table below summarizes by maturity our significant contractual obligations and reserves, including interest, as of December 31, 2009:
| Due in Years Ending December 31, | |||||||||||||||||||||
| 2010 | 2011 | 2012 | 2013 | 2014 | Thereafter | Total | |||||||||||||||
| Operating lease obligations |
$ | 1,881 | $ | 1,125 | $ | 516 | $ | 222 | $ | 189 | $ | 99 | $ | 4,032 | |||||||
| Acquisition earn-out payments(1) |
7,622 | 3,117 | — | — | — | — | 10,739 | ||||||||||||||
| Accrued professional liability settlement(2) |
750 | — | — | — | — | — | 750 | ||||||||||||||
| Medical malpractice reserves—self-insured retention(3) |
467 | 109 | 36 | 24 | 11 | 12 | 659 | ||||||||||||||
| Sub-total contractual obligations |
10,720 | 4,351 | 552 | 246 | 200 | 111 | 16,180 | ||||||||||||||
| Medical malpractice reserve—claims-made basis(3) |
239 | 1,420 | 2,704 | 2,748 | 1,864 | 2,515 | 11,490 | ||||||||||||||
| Total contractual obligations and reserves |
$ | 10,959 | $ | 5,771 | $ | 3,256 | $ | 2,994 | $ | 2,064 | $ | 2,626 | $ | 27,670 | |||||||
| (1) | In February 2010, we paid $0.9 million of additional consideration that was accrued at December 31, 2009, related to the acquisition of various hospitalist physician practices in 2008. In addition to the initial consideration paid pursuant to certain other asset purchase agreements entered into during the year ended December 31, 2009, additional future consideration is to be paid based upon the achievement of certain operating results of the acquired practices as of certain measurement dates. These additional payments are estimated to be approximately $10.7 million and the majority of such payments are expected to be made during 2010, with the remaining amounts to be paid in early 2011. Such additional consideration is not contingent upon the future employment of the sellers. |
49
Table of Contents
| (2) | During the first quarter of 2010, we reached a preliminary agreement to settle a disputed professional liability claim for a prior year that is in excess of our insurance policy limit. The settlement remains subject to definitive documentation and is contingent upon receiving applicable court approval. We recorded our portion of the settlement of $0.8 million in the fourth quarter of 2009. |
| (3) | We were self-insured up to certain limits for costs associated with professional liability claims reported prior to January 1, 2009. Effective January 1, 2009, we are fully insured up to our policy limits through third party malpractice insurance policies. We establish reserves that we expect to pay for the self-insurance retention. Our malpractice policies are on a claims-made basis, consequently, we establish reserves on an undiscounted basis for estimates of the loss that we will ultimately incur on claims that have been incurred but not reported. These reserves and the timing of payment of such amounts are estimated based upon actuarial loss projections, which are updated semi-annually. So long as we maintain third party malpractice insurance policies, the claims in excess of self-insured retention will be covered by such third party policy up to the policy limits. |
Off-Balance Sheet Arrangements
As of December 31, 2009, we had no off-balance sheet arrangements.
50
Table of Contents
| ITEM 7A. | QUANTITATIVE AND QUALITATIVE DISCLOSURES ABOUT MARKET RISK |
We are exposed to changes in interest rate as a result of our Credit Facility. At our option, the interest rate on outstanding borrowings under our Credit Facility is either LIBOR plus 1.5% to 2.0% or the base rate plus the applicable margin as defined in the agreements. The base rate is a daily floating rate based on most recently announced by our lender, as its “prime rate,” whether or not such announced rate is the lowest rate available from our lender. LIBOR is either the 30, 60, 90 or 180 day LIBOR. Historically, we have chosen not to use interest rate derivatives to manage our exposure to changes in interest rates.
We had no outstanding borrowings under the term loan portion of our Credit Facility at December 31, 2009.
Investments in both fixed rate and floating rate interest earning instruments carry a degree of interest rate risk. Fixed rate securities may have their fair market value adversely impacted due to a rise in interest rates, while floating rate securities with shorter maturities may produce less income if interest rates fall. As of December 31, 2009, all of our short-term investments were invested in money market funds with less than 90-day maturities.
| ITEM 8. | FINANCIAL STATEMENTS AND SUPPLEMENTARY DATA |
The consolidated financial statements and supplementary data are as set forth in the “Index to Consolidated Financial Statements” on page 52.
51
Table of Contents
IPC THE HOSPITALIST COMPANY, INC.
INDEX TO CONSOLIDATED FINANCIAL STATEMENTS
52
Table of Contents
Report of Independent Registered Public Accounting Firm
Board of Directors
IPC The Hospitalist Company, Inc.
We have audited the accompanying consolidated balance sheets of IPC The Hospitalist Company, Inc. (the “Company”) as of December 31, 2008 and 2009 and the related consolidated statements of operations, stockholders’ equity and cash flows for each of the three years in the period ended December 31, 2009. Our audits also included the financial statement schedule listed in the index at Item 15(a). These financial statements and schedule are the responsibility of the Company’s management. Our responsibility is to express an opinion on these financial statements and schedule based on our audits.
We conducted our audits in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement. An audit includes examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements. An audit also includes assessing the accounting principles used and significant estimates made by management, as well as evaluating the overall financial statement presentation. We believe that our audits provide a reasonable basis for our opinion.
In our opinion, the financial statements referred to above present fairly, in all material respects, the consolidated financial position of IPC The Hospitalist Company, Inc. at December 31, 2008 and 2009 and the consolidated results of its operations and its cash flows for each of the three years in the period ended December 31, 2009, in conformity with U.S. generally accepted accounting principles. Also, in our opinion, the related financial statement schedule, when considered in relation to the basic financial statements taken as a whole, presents fairly in all material respects the information set forth therein.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States), IPC The Hospitalist Company, Inc.’s internal control over financial reporting as of December 31, 2009, based on criteria established in Internal Control-Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission and our report dated February 22, 2010 expressed an unqualified opinion thereon.
As discussed in Note 1 to the consolidated financial statements, the Company changed its method of accounting for business combinations with the adoption of the guidance originally in FASB Statement No. 141(R), Business Combinations (coded in FASB ASC Topic 805, Business Combinations) effective January 1, 2009.
| /s/ Ernst & Young LLP |
Los Angeles, California
February 22, 2010
53
Table of Contents
IPC The Hospitalist Company, Inc.
Consolidated Balance Sheets
(in thousands, except for share data)
| As of December 31, | ||||||
| 2008 | 2009 | |||||
| Assets |
||||||
| Current assets: |
||||||
| Cash and cash equivalents |
$ | 37,394 | $ | 31,473 | ||
| Accounts receivable, net |
44,474 | 48,276 | ||||
| Prepaid expenses and other current assets |
8,081 | 8,531 | ||||
| Total current assets |
89,949 | 88,280 | ||||
| Furniture and equipment, net |
2,452 | 3,011 | ||||
| Goodwill |
63,893 | 91,701 | ||||
| Other intangible assets, net |
2,905 | 2,776 | ||||
| Deferred tax assets, net |
3,492 | 2,444 | ||||
| Total assets |
$ | 162,691 | $ | 188,212 | ||
| Liabilities |
||||||
| Current liabilities: |
||||||
| Accounts payable and accrued liabilities |
$ | 4,664 | $ | 4,083 | ||
| Accrued compensation |
11,232 | 15,017 | ||||
| Payables for practice acquisitions |
2,476 | 10,739 | ||||
| Medical malpractice and self-insurance reserves, current portion |
539 | 706 | ||||
| Accrued professional liability settlement |
— | 750 | ||||
| Deferred tax liabilities |
481 | 134 | ||||
| Short-term debt and current portion of long-term debt |
3,471 | — | ||||
| Total current liabilities |
22,863 | 31,429 | ||||
| Long-term debt, less current portion |
5,368 | — | ||||
| Medical malpractice and self-insurance reserves, less current portion |
11,220 | 11,443 | ||||
| Other long-term liabilities |
293 | 263 | ||||
| Total liabilities |
39,744 | 43,135 | ||||
| Stockholders’ equity: |
||||||
| Preferred stock, $0.001 par value, 15,000,000 shares authorized, none issued |
— | — | ||||
| Common stock, $0.001 par value, 50,000,000 shares authorized, 16,068,835 and 16,161,813 shares issued and outstanding at December 31, 2008 and 2009, respectively |
16 | 16 | ||||
| Additional paid-in capital |
122,024 | 125,527 | ||||
| Retained earnings |
907 | 19,534 | ||||
| Total stockholders’ equity |
122,947 | 145,077 | ||||
| Total liabilities and stockholders’ equity |
$ | 162,691 | $ | 188,212 | ||
The accompanying notes are an integral part of these consolidated financial statements.
54
Table of Contents
IPC The Hospitalist Company, Inc.
Consolidated Statements of Operations
(dollars in thousands, except for per share data)
| Years Ended December 31, | ||||||||||||
| 2007 | 2008 | 2009 | ||||||||||
| Net revenue |
$ | 190,002 | $ | 251,179 | $ | 310,521 | ||||||
| Operating expenses: |
||||||||||||
| Cost of services—physician practice salaries, benefits and other |
136,960 | 181,850 | 225,801 | |||||||||
| General and administrative |
37,874 | 44,701 | 51,338 | |||||||||
| Depreciation and amortization |
1,396 | 2,146 | 2,295 | |||||||||
| Professional liability settlement |
— | — | 750 | |||||||||
| Total operating expenses |
176,230 | 228,697 | 280,184 | |||||||||
| Income from operations |
13,772 | 22,482 | 30,337 | |||||||||
| Investment income |
397 | 604 | 84 | |||||||||
| Interest expense |
(1,691 | ) | (868 | ) | (293 | ) | ||||||
| Loss on fair value of preferred stock warrant liabilities |
(8,781 | ) | — | — | ||||||||
| Income before income taxes |
3,697 | 22,218 | 30,128 | |||||||||
| Income tax provision |
4,564 | 8,664 | 11,501 | |||||||||
| Net (loss) income |
(867 | ) | 13,554 | 18,627 | ||||||||
| Accretion of redeemable convertible preferred stock |
(229 | ) | — | — | ||||||||
| Income allocable to preferred stockholders |
— | (696 | ) | — | ||||||||
| Net (loss) income attributable to common stockholders |
$ | (1,096 | ) | $ | 12,858 | $ | 18,627 | |||||
| Per share data: |
||||||||||||
| Net (loss) income per share attributable to common stockholders—historical: |
||||||||||||
| Basic |
$ | (0.64 | ) | $ | 0.88 | $ | 1.16 | |||||
| Diluted |
$ | (0.64 | ) | $ | 0.87 | $ | 1.14 | |||||
| Net (loss) income per share attributable to common stockholders—pro forma: |
||||||||||||
| Basic |
$ | (0.08 | ) | $ | 0.89 | N/A | ||||||
| Diluted |
$ | (0.08 | ) | $ | 0.88 | N/A | ||||||
The accompanying notes are an integral part of these consolidated financial statements.
55
Table of Contents
Consolidated Statements of Stockholders’ Equity
(dollars in thousands, except for per share data)
| Series A | Series B | Series C | Series D | (Accumulated Deficit) Retained Earnings |
||||||||||||||||||||||||||||||||||||||||||
| Common Stock | Preferred Stock | Preferred Stock | Preferred Stock | Preferred Stock | Additional Paid-in Capital |
Total | ||||||||||||||||||||||||||||||||||||||||
| Shares | Amount | Shares | Amount | Shares | Amount | Shares | Amount | Shares | Amount | |||||||||||||||||||||||||||||||||||||
| Balance at December 31, 2006 |
1,244,257 | $ | 1 | — | $ | — | — | $ | — | — | $ | — | — | $ | — | $ | 27 | $ | (11,042 | ) | $ | (11,014 | ) | |||||||||||||||||||||||
| Issuance of common stock |
637,458 | 1 | — | — | — | — | — | — | — | — | 499 | — | 500 | |||||||||||||||||||||||||||||||||
| Repurchase of common stock |
(3,333 | ) | — | — | — | — | — | — | — | — | — | (9 | ) | — | (9 | ) | ||||||||||||||||||||||||||||||
| Tax benefits from stock options |
— | — | — | — | — | — | — | — | — | — | 455 | — | 455 | |||||||||||||||||||||||||||||||||
| Stock-based compensation expense |
— | — | — | — | — | — | — | — | — | — | 91 | — | 91 | |||||||||||||||||||||||||||||||||
| Reclassification of convertible preferred stock |
— | — | 10,318,866 | 10 | 17,893,968 | 18 | 11,139,850 | 11 | 18,408,551 | 18 | 43,173 | — | 43,230 | |||||||||||||||||||||||||||||||||
| Warrant fair value |
— | — | — | — | — | — | — | — | — | — | 11,369 | — | 11,369 | |||||||||||||||||||||||||||||||||
| Adjustment to initially apply accounting for uncertain tax positions |
— | — | — | — | — | — | — | — | — | — | — | (509 | ) | (509 | ) | |||||||||||||||||||||||||||||||
| Accretion of redeemable convertible preferred stock |
— | — | — | — | — | — | — | — | — | — | — | (229 | ) | (229 | ) | |||||||||||||||||||||||||||||||
| Net loss |
— | — | — | — | — | — | — | — | — | — | — | (867 | ) | (867 | ) | |||||||||||||||||||||||||||||||
| Balance at December 31, 2007 |
1,878,382 | 2 | 10,318,866 | 10 | 17,893,968 | 18 | 11,139,850 | 11 | 18,408,551 | 18 | 55,605 | (12,647 | ) | 43,017 | ||||||||||||||||||||||||||||||||
| Initial public offering of common stock, net of $6,636 of offering costs |
3,300,000 | 3 | — | — | — | — | — | — | — | — | 46,161 | — | 46,164 | |||||||||||||||||||||||||||||||||
| Conversion of preferred stock to common stock in connection with initial public offering |
9,025,195 | 9 | (10,318,866 | ) | (10 | ) | (17,893,968 | ) | (18 | ) | (11,139,850 | ) | (11 | ) | (18,408,551 | ) | (18 | ) | — | — | (48 | ) | ||||||||||||||||||||||||
| Issuance of common stock for warrants exercised on a cashless basis in connection with initial public offering |
641,340 | 1 | — | — | — | — | — | — | — | — | — | — | 1 | |||||||||||||||||||||||||||||||||
| Follow-on public offering of common stock, net of $2,020 of offering costs |
1,135,231 | 1 | — | — | — | — | — | — | — | — | 18,981 | — | 18,982 | |||||||||||||||||||||||||||||||||
| Issuance of common stock |
88,687 | — | — | — | — | — | — | — | — | — | (58 | ) | — | (58 | ) | |||||||||||||||||||||||||||||||
| Tax benefits from stock options |
— | — | — | — | — | — | — | — | — | — | 454 | — | 454 | |||||||||||||||||||||||||||||||||
| Stock-based compensation expense |
— | — | — | — | — | — | — | — | — | — | 881 | — | 881 | |||||||||||||||||||||||||||||||||
| Net income |
— | — | — | — | — | — | — | — | — | — | — | 13,554 | 13,554 | |||||||||||||||||||||||||||||||||
| Balance at December 31, 2008 |
16,068,835 | 16 | — | — | — | — | — | — | — | — | 122,024 | 907 | 122,947 | |||||||||||||||||||||||||||||||||
| Issuance of common stock |
92,978 | — | — | — | — | — | — | — | — | — | 736 | — | 736 | |||||||||||||||||||||||||||||||||
| Tax benefits from stock options |
— | — | — | — | — | — | — | — | — | — | 810 | — | 810 | |||||||||||||||||||||||||||||||||
| Stock-based compensation expense |
— | — | — | — | — | — | — | — | — | — | 1,957 | — | 1,957 | |||||||||||||||||||||||||||||||||
| Net income |
— | — | — | — | — | — | — | — | — | — | — | 18,627 | 18,627 | |||||||||||||||||||||||||||||||||
| Balance at December 31, 2009 |
16,161,813 | $ | 16 | — | $ | — | — | $ | — | — | $ | — | — | $ | — | $ | 125,527 | $ | 19,534 | $ | 145,077 | |||||||||||||||||||||||||
The accompanying notes are an integral part of these consolidated financial statements.
56
Table of Contents
IPC The Hospitalist Company, Inc.
Consolidated Statements of Cash Flows
(dollars in thousands)
| Years Ended December 31, | ||||||||||||
| 2007 | 2008 | 2009 | ||||||||||
| Operating activities |
||||||||||||
| Net (loss) income |
$ | (867 | ) | $ | 13,554 | $ | 18,627 | |||||
| Adjustments to reconcile net (loss) income to net cash provided by operating activities: |
||||||||||||
| Depreciation and amortization |
1,396 | 2,146 | 2,295 | |||||||||
| Stock-based compensation expense |
91 | 881 | 1,957 | |||||||||
| Tax liability reduction for uncertain tax positions |
— | (7 | ) | (30 | ) | |||||||
| Deferred income taxes |
1,336 | (103 | ) | 701 | ||||||||
| Change in acquisition fair value |
— | — | (158 | ) | ||||||||
| Revaluation of preferred stock warrant liabilities |
8,781 | — | — | |||||||||
| Changes in assets and liabilities: |
||||||||||||
| Accounts receivable |
(7,976 | ) | (4,980 | ) | (3,802 | ) | ||||||
| Prepaid expenses and other current assets |
(3,382 | ) | 2,122 | (450 | ) | |||||||
| Accounts payable and accrued liabilities |
(344 | ) | (3 | ) | (581 | ) | ||||||
| Accrued compensation |
4,159 | (1,150 | ) | 3,785 | ||||||||
| Medical malpractice and self-insurance reserves |
1,846 | 1,908 | 390 | |||||||||
| Accrued professional liability settlement |
(3,598 | ) | — | 750 | ||||||||
| Net cash provided by operating activities |
1,442 | 14,368 | 23,484 | |||||||||
| Investing activities |
||||||||||||
| Acquisitions of physician practices |
(15,303 | ) | (29,921 | ) | (20,162 | ) | ||||||
| Purchase of furniture and equipment |
(926 | ) | (1,539 | ) | (1,950 | ) | ||||||
| Elimination of cash restriction by lender |
2,500 | — | — | |||||||||
| Net cash used in investing activities |
(13,729 | ) | (31,460 | ) | (22,112 | ) | ||||||
| Financing activities |
||||||||||||
| Proceeds from (repayments of) long-term debt and capital leases, net |
12,371 | (17,986 | ) | (8,839 | ) | |||||||
| Net proceeds from issuance of common stock |
491 | 65,042 | 736 | |||||||||
| Excess tax benefits from stock-based compensation |
455 | 454 | 810 | |||||||||
| Net cash provided by (used in) financing activities |
13,317 | 47,510 | (7,293 | ) | ||||||||
| Net increase (decrease) in cash and cash equivalents |
1,030 | 30,418 | (5,921 | ) | ||||||||
| Cash and cash equivalents, beginning of year |
5,946 | 6,976 | 37,394 | |||||||||
| Cash and cash equivalents, end of year |
$ | 6,976 | $ | 37,394 | $ | 31,473 | ||||||
| Supplemental disclosure of cash flow information |
||||||||||||
| Cash paid for: |
||||||||||||
| Interest |
$ | 2,021 | $ | 827 | $ | 314 | ||||||
| Income taxes |
$ | 4,234 | $ | 7,764 | $ | 9,338 | ||||||
| Acquisitions of physician practices consisted of the following: |
||||||||||||
| Acquired assets: |
||||||||||||
| Goodwill and intangible assets |
$ | 13,429 | $ | 31,987 | $ | 28,577 | ||||||
| Furniture and equipment |
— | 118 | 6 | |||||||||
| Accrued consideration |
1,874 | (2,184 | ) | (8,421 | ) | |||||||
| Net cash paid for acquisitions |
$ | 15,303 | $ | 29,921 | $ | 20,162 | ||||||
| Accretion of redeemable convertible preferred stock |
$ | (229 | ) | $ | — | $ | — | |||||
| Reclassification of convertible preferred stock to equity |
$ | 43,231 | $ | — | $ | — | ||||||
The accompanying notes are an integral part of these consolidated financial statements.
57
Table of Contents
IPC THE HOSPITALIST COMPANY, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS
December 31, 2009
1. Operations and Significant Accounting Policies
Business
IPC The Hospitalist Company, Inc. and its subsidiaries (the “Company,” “IPC,” “we,” “us,” and “our”) is a national physician group practice company that operates and manages full-time hospitalist practices. Hospitalists are acute-care physician specialists, who focus on a patient’s hospital care from time of admission to discharge and have no outpatient responsibilities. Hospitalists practice exclusively in hospitals or other inpatient facilities, including acute, sub-acute and long-term care settings. The physicians are primarily full-time employees of our subsidiaries or consolidated Professional Medical Corporations, although part-time and temporary physicians are also employed or contracted on an as-needed basis.
Reverse Stock Split and Amended and Restated Certificate of Incorporation
In January 2008, we completed a 1-for-6.4 reverse stock split of our outstanding common stock. The accompanying financial statements and notes to the financial statements give retroactive effect to the reverse stock split for all periods presented. In addition, the reverse stock split resulted in an adjustment in the number of shares of common stock issuable upon conversion of our convertible preferred stock to a 6.4:1 ratio. In addition, we adopted an Amended and Restated Certificate of Incorporation, which provides that our authorized capital stock consists of 50 million shares of common stock, $0.001 par value per share, and 15 million shares of preferred stock, $0.001 par value per share.
Initial Public Offering and Follow-On Public Offering
On January 30, 2008, we completed our initial public offering (IPO) for the sale of 5,905,000 shares of our common stock at a price of $16.00 per share. Of these shares 3,300,000 were newly issued shares sold by us, and 2,605,000 were shares sold by existing stockholders. We received net proceeds of $46,164,000 after deducting underwriting discounts and commissions of $3,696,000 and other fees and expenses of $2,940,000. As discussed further in Note 8, upon completion of our IPO, all of our preferred stock, and a majority of our warrants converted to common stock. Immediately after the offering, and including the conversion of the preferred stock and warrants, there were 14,844,934 shares of our common stock outstanding.
On July 21, 2008, we closed a follow-on public offering for the sale of 4,025,000 shares of our common stock at a price of $18.50 per share. Of these shares 1,135,231 shares were newly issued shares sold by us, and 2,889,769 were shares sold by certain of our existing stockholders. We received net proceeds of $18,982,000 after deducting underwriters’ discounts and commissions of $1,155,000 and fees and expenses of $865,000. Immediately after the offering, there were 16,017,237 shares of our common stock outstanding.
Principles of Consolidation
Our consolidated financial statements include the accounts of IPC The Hospitalist Company, Inc. and its wholly owned subsidiaries and consolidated Professional Medical Corporations managed under long-term management agreements. Some states have laws that prohibit business entities, such as IPC, from practicing medicine, employing physicians to practice medicine, exercising control over medical decisions by physicians (collectively known as the corporate practice of medicine), or engaging in certain arrangements with physicians, such as fee-splitting. In states that have these restrictions, we operate by maintaining long-term management contracts with affiliated professional organizations, which are each owned and operated by physicians, and which employ or contract with additional physicians to provide hospitalist services. Under the management agreements,
58
Table of Contents
IPC THE HOSPITALIST COMPANY, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
we provide and perform all non-medical management and administrative services, including financial management, information systems, marketing, risk management and administrative support. The management agreements have an initial term of 20 years and are automatically renewable for successive 10-year periods unless terminated by either party for cause. The management agreements are not terminable by the Professional Medical Corporations, except in the case of gross negligence, fraud, or other illegal acts by us, or bankruptcy of IPC.
Through the management agreements and our relationship with the stockholders of the Professional Medical Corporations, we have exclusive authority over all non-medical decision making related to the ongoing business operations of the Professional Medical Corporations. Further, our rights under the management agreements are unilaterally salable or transferable. Based on the provisions of the agreements, we have determined that the Professional Medical Corporations are variable interest entities (VIE’s), and that we are the primary beneficiary because we have controls over the operations of these VIE’s. Consequently, we consolidate the revenue and expenses of the Professional Medical Corporations from the date of execution of the agreements. All intercompany balances and transactions have been eliminated in consolidation.
Segment Reporting
We operate in a regional operating structure. The results of our regional operations are aggregated into a single reportable segment for purposes of presenting financial information.
Revenue
Net revenue consists of fees for medical services provided by our affiliated hospitalists under fee-for-service, case rate and other professional fee arrangements with various payors including Medicare, Medicaid, managed care organizations, insurance companies, and hospitals. Net revenue is reported on the accrual basis in the period in which services are provided, at rates that reflect the amount expected to be collected. The process of estimating the ultimate amount of revenue to be collected is highly subjective and requires the application of our judgment based on many factors, including contractual reimbursement rates, payor mix, age of receivables, historical cash collection experience and other relevant information. Revenue related to patient responsibility accounts is recorded at amounts reasonably assured of collection, which is net of a provision for uncollectible accounts. During 2007, 2008 and 2009, we recorded a provision for uncollectible accounts of $6,649,000, $8,498,000, and $10,054,000, respectively. We write off uncollectible accounts receivable after reasonable collection efforts have been exhausted.
During 2007, 2008 and 2009, approximately 50%, 50% and, 48%, respectively, of our patient volume was from Medicare and Medicaid programs.
Use of Estimates
The preparation of financial statements in conformity with U.S. generally accepted accounting principles requires us to make estimates and assumptions that affect the reported amounts of assets, liabilities, revenues and expenses at the date and for the periods that the financial statements are prepared. Significant estimates include the estimated net realizable value of accounts receivable, estimated liabilities for claims incurred but not reported (IBNR) related to our medical malpractice coverage, fair value of contingent consideration related to business combinations and the analysis of goodwill for impairment.
The process of estimating the net realizable value of accounts receivable, the IBNR liabilities, fair value of contingent consideration related to business combinations and the analysis of goodwill for impairment involves judgment decisions, which are subject to an inherent degree of uncertainty. Actual results could differ from those estimates.
59
Table of Contents
IPC THE HOSPITALIST COMPANY, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Fair Value of Financial Instruments
We disclose fair value information about financial instruments for which it is practical to estimate that value. Our consolidated balance sheet as of December 31, 2009 included the following financial instruments: cash and cash equivalents, accounts receivable and accounts payable and accrued liabilities. We consider the carrying amounts of current assets and liabilities to approximate their fair value because of the relatively short period of time between the origination of these instruments and their expected realization.
Cash and Cash Equivalents
Our cash and cash equivalents consist of bank deposits, money market accounts and short-term securities with maturities of three months or less.
Accounts Receivable and Concentrations of Credit Risk
Accounts receivable primarily consists of amounts due from third-party payors, including government sponsored Medicare and Medicaid programs, and insurance companies, and amounts due from hospitals, and patients. Accounts receivable are stated at the amount expected to be collected, net of reserves for amounts estimated to be uncollectible. At December 31, 2008 and 2009, we recorded an allowance for uncollectible accounts of $3,323,000, and $2,702,000, respectively. Except with respect to the Medicare and Medicaid programs, concentrations of credit risk, which consist primarily of accounts receivable, is limited due to the large number of payors comprising our diverse payor mix and patient base. Receivables from Medicare and Medicaid programs made up approximately 35% and 32% of the net accounts receivable at December 31, 2008 and 2009, respectively.
Furniture and Equipment
Furniture and equipment are stated on the basis of cost or fair value on the date of practice acquisition. Repairs and maintenance are charged to expense as incurred. Depreciation is provided using the straight-line method over the estimated useful lives of the assets. Amortization of items under capital leases is provided using the straight-line method. The depreciable life is generally three years for equipment and software, seven years for furniture, and the lesser of the useful life or lease period for leasehold improvements.
At December 31, furniture and equipment consisted of the following (dollars in thousands):
| 2008 | 2009 | |||||||
| Furniture |
$ | 1,432 | $ | 1,617 | ||||
| Computer equipment and software |
6,592 | 8,205 | ||||||
| Office equipment |
1,535 | 1,609 | ||||||
| Leasehold improvements |
331 | 415 | ||||||
| 9,890 | 11,846 | |||||||
| Less: Accumulated depreciation and amortization |
(7,438 | ) | (8,835 | ) | ||||
| $ | 2,452 | $ | 3,011 | |||||
Depreciation and amortization expense for furniture and equipment was $1,042,000, $1,395,000 and $1,397,000 for 2007, 2008 and 2009, respectively.
60
Table of Contents
IPC THE HOSPITALIST COMPANY, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Goodwill and Other Intangible Assets
We record acquired assets and liabilities and additional future consideration at their acquisition-date fair values, and expense all transaction related costs under the acquisition method of accounting. Goodwill represents the excess of cost over the fair value of the net assets acquired. Other intangible assets primarily represent the fair value of hospital service contract agreements and non-compete agreements acquired in connection with certain asset purchase agreements. Goodwill and other indefinite-lived intangible assets are not amortized. Separable identified intangible assets that have finite lives are amortized over their useful lives.
In addition to the initial consideration paid at the close of each business combination, the asset purchase agreements for certain completed practice acquisitions provide for additional future consideration to be paid, which is generally based upon the achievement of certain operating results of the acquired practices as of certain measurement dates. Pursuant to new GAAP, the estimated fair value of additional future consideration related to transactions that are completed on or after January 1, 2009, is accrued at the acquisition-date. Subsequent changes, if any, to the acquisition-date fair value of transactions that occurred after January 1, 2009 are recognized as part of on-going operations.
We review and evaluate goodwill and other intangible assets for impairment on an annual basis at the entity level since we operate in only one line of business. The testing for impairment is completed using a two step test. The first step compares the fair value of the Company with its carrying amount, including goodwill. If the carrying amount of the entity exceeds its fair value, a second step is performed to determine the amount of any impairment loss. During 2007, 2008 and 2009, no impairment indicators were present and no impairment was recognized.
Medical Malpractice Liability Insurance
We maintain medical malpractice insurance coverage that indemnifies us and our employed health care professionals on a claims-made basis. Claims-made coverage covers only those claims reported during the policy period. Unlike our claims-made policy in effect in 2008 that contained self-insurance retention, our 2009 claims-made policy provided first dollar coverage up to our policy limits on new claims reported in 2009. In December 2009, we renewed our annual professional liability insurance policy for 2010 effective January 1, 2010 under the same terms as our 2009 policy. We expect to be able to continue to obtain coverage in future years; however, there can be no assurance that we will obtain substantially similar coverage as is provided under the 2010 policy at acceptable costs and on favorable terms upon expiration.
We record reserves for self-insurance retention related to the policy plan of 2008 and prior years and an estimate of our liabilities, on an undiscounted basis, for claims incurred but not reported based upon actuarial loss projections using our historical loss experience. At December 31, 2008 and 2009, our accrual for potential future uninsured claims, including a provision for IBNR not covered under our claims-made insurance policy was $11,759,000 and $12,149,000, respectively.
Stock-Based Compensation
At December 31, 2009, we had three stock-based employee compensation plans, which are described more fully in Note 6 to the Consolidated Financial Statements. Compensation cost recognized in 2007, 2008 and 2009 includes amounts for awards granted after December 31, 2005 and for awards outstanding on December 31, 2005 that are subsequently modified, based on the estimated grant-date fair value.
61
Table of Contents
IPC THE HOSPITALIST COMPANY, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Reclassifications
Certain prior year amounts have been reclassified to conform to the current year presentation.
Recently Adopted Accounting Pronouncements
In June 2009, the Financial Accounting Standards Board (FASB) issued a new pronouncement which establishes the single source of authoritative U.S. generally accepted accounting principles for all nongovernmental entities, superseding existing accounting literature and pronouncements by the FASB, the American Institute of Certified Public Accountants and the Emerging Issues Task Force, and other related accounting literature. This new pronouncement reorganizes all U.S. generally accepted accounting principles into approximately 90 accounting topics, displays them using a consistent structure, and includes relevant Securities and Exchange Commission (SEC) guidance organized using the same topical structure in separate sections. After adopting this new pronouncement on September 30, 2009, we have ceased the use of reference to specific FASB Statements of Financial Accounting Standards or other accounting literature in our disclosures as we did in our previous SEC filings, and use the term “GAAP” to refer to any and all authoritative U.S. generally accepted accounting principles established by this new pronouncement. This pronouncement does not change GAAP; therefore, our adoption of this pronouncement did not have any impact on our financial position, results of operations or cash flows.
On January 1, 2009, we adopted newly issued GAAP related to business combinations which introduces significant changes in the accounting for and reporting of business acquisitions. This new GAAP changes how business acquisitions are accounted for and impacts financial statements at the acquisition date and in subsequent periods. An acquiring entity is required to recognize all of the assets acquired and liabilities assumed in a transaction at the acquisition-date fair value, with limited exceptions, and all transaction related costs are expensed. Subsequent changes, if any, to the acquisition-date fair value that are the result of facts and circumstances that did not exist as of the acquisition date are recognized as part of on-going operations. Its provisions are effective for business combinations for which the acquisition date is on or after January 1, 2009. The impact of this new GAAP on our consolidated financial statements depends on the nature, terms and size of our business combinations that occur after the effective date.
On January 1, 2008, we adopted revised GAAP related to fair value measures for our financial assets and liabilities. In February 2008, the FASB deferred the effective date of this revised GAAP for certain nonfinancial assets and nonfinancial liabilities to our fiscal 2009. This revised GAAP defines fair value and provides a framework for measuring fair value. It also requires expanded disclosure requirements which include the methods and assumptions used to measure fair value and the effect of fair value measures on earnings. This revised GAAP applies to any GAAP that requires or permits fair value measurements. The adoption of this revised GAAP on January 1, 2009 for nonfinancial assets and liabilities did not have a material impact on our financial position, results of operations or cash flows.
On April 1, 2009, we adopted revised GAAP which provides additional guidance for estimating fair value when the volume and level of activity for an asset or liability has significantly decreased. The adoption of this GAAP did not have a material impact on our financial position, results of operations or cash flows.
On April 1, 2009, we adopted newly issued GAAP which requires that a public company evaluate subsequent events through the date when it issues its financial statements and disclose the date and any material nonrecognized subsequent events. The adoption of this GAAP did not have a material impact on our financial position, results of operations or cash flows.
62
Table of Contents
IPC THE HOSPITALIST COMPANY, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
New Accounting Principles
In June 2009, the FASB issued revised GAAP which amends the existing GAAP on VIE’s and changes the consolidation guidance applicable to a VIE. The revised GAAP requires the use of a qualitative analysis rather than a quantitative analysis to determine whether an enterprise is the primary beneficiary of a VIE, and is, therefore, required to consolidate the VIE. The revised GAAP also requires continuous reassessments of whether an enterprise is the primary beneficiary of a VIE, while the existing GAAP only requires reconsideration of the primary beneficiary of a VIE when specific events occur. Enhanced disclosures about an enterprise’s involvement with a VIE will also be required. This revised GAAP will be effective for interim and annual reporting periods beginning after November 15, 2009. The adoption of this revised GAAP will not have a material impact on our financial position, results of operations or cash flows.
2. Practice Acquisitions
For acquisitions closed on or after January 1, 2009, we recognize all of the assets acquired, liabilities assumed and future additional consideration at the acquisition-date fair value and expense all transaction related costs.
During 2009, in connection with the acquisition of assets of eight hospitalist physician practices, we recorded goodwill and other identifiable intangible assets consisting of physician and hospital agreements. Amounts recorded as goodwill and identifiable intangible assets are amortized for tax purposes over 15 years. The results of operations of these acquisitions are included in the consolidated financial statements from the respective dates of acquisition. In addition to the initial consideration paid at the close of each transaction, the asset purchase agreements for six of the completed acquisitions provide for future consideration to be paid, which is generally based upon the achievement of certain operating results of the acquired practices as of certain measurement dates. These additional payments are not contingent upon the future employment of the sellers. The estimated fair value of additional future consideration related to transactions that occurred in 2009 is recognized at the acquisition-date, while additional consideration amounts related to transactions that occurred prior to 2009 are recorded on their respective measurement dates as additional goodwill. Subsequent changes, if any, to the acquisition-date fair value of transactions that occurred after January 1, 2009 are recognized as part of on-going operations. We evaluated the carrying value of future consideration for all 2009 acquisitions as of December 31, 2009, and determined that the fair value of future consideration was $158,000 less than its carrying value. Such reduction is reflected in general and administration expenses.
We estimate the fair value of additional future considerations to be paid based on discounted projected earnings of the acquired practices as of certain measurement dates. The discount rate that we use consists of a risk-free U.S. Treasury bond yield plus a company credit risk rate which we believe is acceptable by willing market participants.
63
Table of Contents
IPC THE HOSPITALIST COMPANY, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The following table summarizes the total amounts recorded during 2009, related to the acquisition of hospitalist practices (dollars in thousands):
| Goodwill | Intangible Assets |
Furniture and Equipment |
Total | ||||||||||
| Acquired assets—paid and accrued: |
|||||||||||||
| 2009 transactions |
$ | 23,519 | $ | 769 | $ | 6 | $ | 24,294 | |||||
| Addition to prior year transactions |
4,289 | — | — | 4,289 | |||||||||
| Total acquired assets |
27,808 | 769 | 6 | 28,583 | |||||||||
| Cash paid for acquisitions: |
|||||||||||||
| 2009 transactions |
13,934 | 769 | 6 | 14,709 | |||||||||
| Prior year transactions |
5,453 | — | — | 5,453 | |||||||||
| Total cash paid for acquisitions |
19,387 | 769 | 6 | 20,162 | |||||||||
| Accrued consideration |
$ | 8,421 | $ | — | $ | — | 8,421 | ||||||
| Change in fair value of additional future consideration |
(158 | ) | |||||||||||
| Net increase in payable for practice acquisitions |
$ | 8,263 | |||||||||||
At December 31, other intangible assets consist of the following (dollars in thousands):
| 2008 | 2009 | |||||||
| Non-compete agreements |
$ | 1,059 | $ | 1,305 | ||||
| Hospital contracts |
3,238 | 3,761 | ||||||
| 4,297 | 5,066 | |||||||
| Less: Accumulated amortization |
(1,392 | ) | (2,290 | ) | ||||
| $ | 2,905 | $ | 2,776 | |||||
Other intangible assets are being amortized over their estimated useful lives which range from three to six years and have a weighted average remaining useful life of 1.9 years at December 31, 2009. Amortization expense for identifiable intangible assets was $353,000, $751,000 and $898,000 for the years ended December 31, 2007, 2008, and 2009, respectively.
Future estimated aggregate amortization expenses are as follows (dollars in thousands):
| 2010 |
$ | 938 | |
| 2011 |
712 | ||
| 2012 |
477 | ||
| 2013 |
445 | ||
| 2014 |
204 | ||
| $ | 2,776 | ||
3. Debt
Our amended and restated loan agreement (Credit Facility), as further amended through October 2007, provides a revolving line of credit of $30,000,000, with a sublimit of $5,000,000 for the issuance of letters of credit, and a term loan in an original amount of $10,000,000. The Credit Facility has a maturity date of September 15, 2011. The Credit Facility is used for working capital and to fund practice acquisitions and capital expenditures.
64
Table of Contents
IPC THE HOSPITALIST COMPANY, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The revolving line is limited by a formula based on a certain multiple times the trailing twelve months of earnings before interest, depreciation, taxes, amortization and certain other non-cash items. Borrowings under the Credit Facility bear interest at a rate, based on either LIBOR plus 1.5% to 2.0%, or the lender’s prime rate, as selected by us for each advance. We pay an unused commitment fee equal to 0.25% per annum on the difference between the revolving line capacity and the average balance outstanding during the year. Outstanding amounts advanced to us under the revolving line of credit are repayable on or before the maturity date.
The Credit Facility is secured by all of our current and future personal and intellectual property assets, except those held subject to purchase money loans and capital leases. The facility includes various customary financial covenants and restrictions, as well as customary remedies for our lenders following an event of default. As of December 31, 2009, we were in compliance with such financial covenants and restrictions.
As of December 31, 2008, our principal balance under the term loan portion of the Credit Facility was $7,813,000. In June 2009, we paid off all outstanding debt under the term loan and our equipment financing loans. At December 31, 2009, we had a letter of credit of $100,000 outstanding and $29,900,000 available under the revolving line of credit.
At December 31, 2008, debt consisted of the following (dollars in thousands):
| Term loan, secured by personal property with interest at rates ranging from 2.91% to 6.43%, due on September 15, 2011 |
$ | 7,813 | ||
| Loan agreements, secured by personal property, payable in monthly installments through December 2010, with interest at rates ranging from 6.51% to 8.51% |
1,026 | |||
| 8,839 | ||||
| Less: Current portion |
(3,471 | ) | ||
| Long-term debt, long-term portion |
$ | 5,368 | ||
Interest costs and unused commitment fees for the years ended December 31 are comprised of the following (dollars in thousands):
| 2007 | 2008 | 2009 | |||||||
| Interest costs |
$ | 1,642 | $ | 796 | $ | 217 | |||
| Unused commitment fees |
49 | 72 | 76 | ||||||
| Total interest expenses |
$ | 1,691 | $ | 868 | $ | 293 | |||
4. Income Taxes
We use the liability method of accounting for income taxes pursuant to GAAP. Under this method, deferred taxes are determined based on the difference between the financial statement and tax basis of assets and liabilities using enacted tax rates in effect in the years in which the differences are expected to reverse. Deferred tax assets are recognized and measured based on the likelihood of realization of the related tax benefit in the future.
65
Table of Contents
IPC THE HOSPITALIST COMPANY, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The income tax provision for the years ended December 31, is comprised of the following (dollars in thousands):
| 2007 | 2008 | 2009 | |||||||||
| Current: |
|||||||||||
| Federal |
$ | 2,292 | $ | 7,398 | $ | 9,101 | |||||
| State |
936 | 1,374 | 1,699 | ||||||||
| Total current |
3,228 | 8,772 | 10,800 | ||||||||
| Deferred: |
|||||||||||
| Federal |
1,004 | (100 | ) | 858 | |||||||
| State |
332 | (8 | ) | (157 | ) | ||||||
| Total deferred |
1,336 | (108 | ) | 701 | |||||||
| Total provision |
$ | 4,564 | $ | 8,664 | $ | 11,501 | |||||
The 2007, 2008 and 2009 current tax provisions include $455,000, $454,000 and $810,000, respectively, of tax benefit from stock compensation recorded to additional paid-in capital.
Certain of our consolidated Professional Medical Corporations are not consolidated for tax return purposes. Included in the table below are the related effects of the separate return filing requirements. A reconciliation of the provision for income taxes compared with U.S. statutory tax rates for the years ended December 31 is shown below:
| 2007 | 2008 | 2009 | ||||
| Statutory federal tax provision |
35.00 % | 35.00 % | 35.00 % | |||
| Increase (decrease) in taxes resulting from: |
||||||
| State taxes net of federal benefit |
23.00 % | 3.97 % | 3.40 % | |||
| Change in valuation allowance |
(7.67)% | (0.12)% | (0.56)% | |||
| Change in federal deferred rate |
(4.47)% | — | — | |||
| Fair value of preferred stock warrants |
80.76 % | — | — | |||
| Permanent differences and other |
2.52 % | 0.18 % | 0.43 % | |||
| Recognition of tax benefits for uncertain tax positions |
(5.69)% | (0.03)% | (0.10)% | |||
| Income tax provision |
123.45 % | 39.00 % | 38.17 % | |||
During 2007, the valuation allowance on consolidated Professional Medical Corporations that file separate tax returns was partially reversed based on the historical and current year earnings and expected future earnings. This reduction of valuation allowance combined with the adjustment to the federal rate applicable to deferred tax assets reduced our 2007 effective tax rate. However, our 2007 effective tax rate was unfavorably impacted by the nondeductible expense from recording the change in fair value of preferred stock warrant liabilities. The state tax impact of this unfavorable item in 2007 was reported in the state rate.
In 2009 there was an increase in state tax credits recognized which reduced the state rate and the overall effective tax rate when compared to 2008.
66
Table of Contents
IPC THE HOSPITALIST COMPANY, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Deferred income taxes reflect the net tax effect of temporary differences between the carrying amounts of assets and liabilities for financial reporting purposes and the amounts used for income tax purposes. At December 31, the significant components of our deferred tax assets and liabilities consisted of the following (dollars in thousands):
| 2008 | 2009 | |||||||
| Deferred tax assets: |
||||||||
| Net operating loss (NOL) carryforwards |
$ | 870 | $ | 519 | ||||
| Allowance for uncollectible accounts |
1,429 | 1,121 | ||||||
| Compensation accruals |
444 | 852 | ||||||
| Accrued IBNR claims |
5,057 | 5,042 | ||||||
| Stock based compensation |
367 | 1,007 | ||||||
| State taxes and credits |
170 | 425 | ||||||
| Other |
11 | 363 | ||||||
| Total deferred tax assets |
8,348 | 9,329 | ||||||
| Less: Valuation allowance |
(329 | ) | (128 | ) | ||||
| Deferred tax assets, net |
$ | 8,019 | $ | 9,201 | ||||
| Deferred tax liabilities: |
||||||||
| Prepaid insurance |
(2,235 | ) | (2,444 | ) | ||||
| Depreciation and amortization |
(2,773 | ) | (4,447 | ) | ||||
| Total deferred tax liabilities |
(5,008 | ) | (6,891 | ) | ||||
| Total net deferred tax asset |
$ | 3,011 | $ | 2,310 | ||||
We evaluate the recoverability of our deferred tax assets based on operations. The remaining valuation allowance relates to consolidated Professional Medical Corporations that file separate tax returns for which the realization of the deferred tax asset is not more likely than not to be utilized.
As of December 31, 2009 we have federal NOL carryforwards of $1,394,000, which begin to expire in 2020, and state NOL carryforwards of $464,000, which begin to expire in 2014. Federal NOLs of $1,367,000 incurred before 2000 are subject to an annual change of ownership limitation of approximately $195,000 per Internal Revenue Code Section 382 and applicable state statutes, which may limit our ability to utilize a portion of these losses.
As of December 31, 2009 we have California enterprise zone credit carryforwards of $316,000, which do not expire.
At December 31, 2009 we had $281,000 of gross unrecognized tax benefits (UTB), of which $215,000 would reduce the effective tax rate if recognized. Unrecognized tax benefits of approximately $227,000 related to intercompany interest charges are expected to decrease in the next 12 months due to the close of the statute of limitations.
Following is a tabular reconciliation of the gross UTB activity during 2009 (dollars in thousands):
| Reconciliation of Gross Unrecognized Tax Benefits |
|||
| Balance at December 31, 2008 excluding interest and penalties of $76 |
$ | 325 | |
| Increases—tax positions taken in prior years |
— | ||
| Decreases—tax provisions taken in prior years |
— | ||
| Current year tax positions |
— | ||
| Settlements |
— | ||
| Lapse of statute of limitations |
(44) | ||
| Balance at December 31, 2009 excluding interest and penalties of $88 |
$ | 281 | |
67
Table of Contents
IPC THE HOSPITALIST COMPANY, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Our accounting policy is to include interest and penalties related to uncertain tax positions in income tax expense. As of December 31, 2009 we have accrued a total of $88,000 of interest and penalties related to uncertain tax positions.
The tax years 2005 to 2008 remain open to examination by the major taxing jurisdictions to which we are subject. The statute for tax years 1997 to 2004 is closed, except that the tax years 1997 to 2002 are subject to adjustment of net operating losses by the Internal Revenue Service. We are subject to taxation in the United States and various state jurisdictions. We are not aware of any notices of examination by any taxing authorities.
5. Defined Contribution Plan
Substantially all of our employees are eligible to participate in the IPC The Hospitalist Company, Inc. 401(k) Plan (the Plan) During 2007 the Plan was amended to increase the amount we contribute to 50% of the first 7% of the participant’s contributions, and effective July 1, 2007 to reduce the vesting period to one year. In January 2008 we further amended the Plan to provide for automatic enrollment of all new hires and existing employees not enrolled and to change the eligibility date to 60 days following an employee’s date of hire. Employees that are automatically enrolled have 60 days to opt out of the Plan and to receive a refund of any contributions made in that period. We fund contributions as accrued. Expense recognized in connection with our contributions amounted to approximately $2,422,000, $3,597,000 and $4,094,000 for the years ended December 31, 2007, 2008 and 2009, respectively.
6. Stock-Based Compensation
At December 31, 2009, we had three stock-based employee compensation plans, for which we reserved a total of 2,593,611 common shares for issuance. Starting in 2007, we only issue shares from our 2007 Equity Participation Plan (2007 Plan). For each calendar year until 2013, the number of shares authorized for issuance under the 2007 Plan will increase in an amount equal to 2.5% of the total number of shares of our common stock outstanding at the close of the first trading day of each year. The number of shares available for issuance under the 2007 Plan will also be increased by any shares granted pursuant to the other two equity participation plans, which are subsequently forfeited by the participants. As of December 31, 2009, 152,652 shares of our common stock were available for issuance under our stock-based employee compensation plans. Pursuant to the 2007 Plan, the available shares of our common stock for issuance were increased by 405,247 on January 4, 2010.
The options under the three plans generally vest over a four-year period from date of grant, and unrestricted options terminate on the 10th anniversary of the agreement date.
All options granted during the year ended December 31, 2007 and all options granted in January 2008 prior to our IPO on January 25, 2008, were issued with exercise prices equal to the fair value of shares at the date of the grant, as determined contemporaneously with the grants. As a result of our IPO, we revised our estimate of the fair value of common stock for financial accounting purposes for options granted in November 2007, based upon the offering price, after giving effect to a discount for lack of marketability. Our stock-based compensation expense for the year ended December 31, 2007 includes consideration of the revised fair value of common stock for the options granted in November 2007. Subsequent to our IPO, all options granted have been issued with exercise prices equal to the closing price of our common stock on the NASDAQ Global Market on the dates of the grant.
Stock-based compensation expense for the year ended December 31, 2007, 2008 and 2009 was $91,000, $881,000 and $1,957,000, respectively, and such expense is included in general and administrative expenses. As of December 31, 2009, there was $3,424,000 of total unrecognized compensation cost related to non-vested share-based compensation arrangements granted under the plans, which is expected to be recognized over a weighted-average period of 2.7 years.
68
Table of Contents
IPC THE HOSPITALIST COMPANY, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The fair value of each option grant is estimated on the date of the grant using the Black-Scholes option-pricing model based on the following weighted-average assumptions:
| Year Ended December 31, 2007 |
Year Ended December 31, 2008 |
Year Ended December 31, 2009 |
|||||||
| Risk-free interest rate |
4.05 – 4.94 | % | 2.33 | % | 2.21 | % | |||
| Expected volatility |
37.0 | % | 37.0 | % | 40.0 | % | |||
| Expected option life (in years) |
6.25 | 6.20 | 6.00 | ||||||
| Expected dividend yield |
0.0 | % | 0.0 | % | 0.0 | % |
The risk-free interest rate is based on the implied yield currently available on U.S. Treasury zero coupon issues. The expected volatility is primarily based on historical volatility levels of our public company peer group. The expected option life of each award granted was calculated using the “simplified method” in accordance with GAAP.
The following table summarizes activity in our three stock-based employee compensation plans during the year ended December 31, 2009 (dollars in thousands, except for per share data):
| Shares | Weighted-Average Exercise Price |
Weighted- Average Remaining Contractual Term (years) |
Aggregate Intrinsic Value |
Weighted Average Fair Value | ||||||||||
| Options outstanding at December 31, 2008 |
678,432 | $ | 10.71 | $ | 4.64 | |||||||||
| Changes during year: |
||||||||||||||
| Granted |
450,960 | 15.81 | 6.90 | |||||||||||
| Exercised |
(74,796 | ) | 6.37 | 2.69 | ||||||||||
| Forfeited |
(12,762 | ) | 9.73 | 5.02 | ||||||||||
| Options outstanding at December 31, 2009 |
1,041,834 | $ | 13.24 | 8.14 | $ | 20,843 | $ | 5.75 | ||||||
| Options exercisable at December 31, 2009 |
392,786 | $ | 10.38 | 7.29 | $ | 8,981 | $ | 4.32 | ||||||
The total intrinsic value of stock options exercised during the year ended December 31, 2009 was $1,599,000.
See Note 8 for information on warrants issued to purchase Preferred Stock.
7. Employee Stock Purchase Plan
In March 2008, our board of directors adopted the amended and restated IPC The Hospitalist Company, Inc. Nonqualified Employee Stock Purchase Plan (ESPP), which we implemented on July 1, 2008. The plan authorizes the issuance of up to an aggregate of 156,250 shares of our common stock to eligible employees who meet the service requirements. At the end of each annual offering period under the plan, an automatic purchase of our common stock is made on behalf of the plan’s participants. Eligible employees may purchase common stock through payroll deductions in amounts from $500 to $10,000 per year. Employees may reduce or suspend deductions during the year or withdraw from the plan during the year and receive a refund of their deductions. For 2008, the offering period was six months and the annual deduction limits were reduced by 50%. Stock purchases are made at a price equal to 85% of the fair market value (i.e., closing price of our common stock on
69
Table of Contents
IPC THE HOSPITALIST COMPANY, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
the NASDAQ Global Market) of a share of our common stock on the first or last day of the offering period, whichever is less. For the years ended December 31, 2008 and 2009, share based expense relating to the ESPP was $77,000 and $195,000, respectively, and is included in general and administrative expenses.
8. Redeemable Convertible Preferred Stock
Upon consummation of our IPO in January 2008, all preferred stock shares converted into 9,025,195 shares of common stock and warrants held by our preferred stockholders automatically converted into 609,197 shares of our common stock in a cashless exercise using the treasury stock method. Warrants held by a certain lender also converted at the completion of our IPO into 32,143 shares of common stock in a cashless exchange using the treasury method. All remaining warrants were exercised as of October 2008.
9. Earnings Per Share
Prior to our initial public offering (IPO), we had issued securities other than common stock that contractually entitled the holder to participate in dividends and earnings of our company. Upon the completion of our IPO on January 30, 2008, all of our securities other than our common stock were converted into shares of our common stock (see Note 8 for further discussion). As a result, we were required to use the Two-Class Method to compute earnings per share for all periods prior to the completion of our IPO. Under the Two-Class Method, we allocate earnings attributable to common stockholders for the period, after deduction of preferred stock dividends, to be allocated between the common and preferred stockholders based on their respective rights to receive dividends. Basic net income per share is then calculated by dividing income attributable to common stockholders (including the reduction for any undeclared, preferred stock dividends assuming current income for the period had been distributed) by the weighted-average number of common shares outstanding, net of shares subject to repurchase by us, during the period. We do not present basic and diluted net income per share for securities other than common stock; therefore, the following net income per share amounts only pertain to our common stock. We calculate diluted net income per share under the if-converted method unless the conversion of the preferred stock is anti-dilutive to basic net income per share. To the extent preferred stock is anti-dilutive, we calculate diluted net income per share under the Two-Class Method.
The calculations of basic and diluted net (loss) income per share attributable to common stockholders for the years ended December 31, 2007, 2008 and 2009 are as follows (dollars in thousands, except for per share data):
| 2007 | 2008 | 2009 | ||||||||
| Basic: |
||||||||||
| Net (loss) income attributable to common stockholders |
$ | (1,096 | ) | $ | 12,858 | $ | 18,627 | |||
| Weighted average number of common shares outstanding |
1,706,682 | 14,544,722 | 16,115,993 | |||||||
| Basic net (loss) income per share attributable to common stockholders |
$ | (0.64 | ) | $ | 0.88 | $ | 1.16 | |||
| Diluted: |
||||||||||
| Net (loss) income attributable to common stockholders |
$ | (1,096 | ) | $ | 12,858 | $ | 18,627 | |||
| Weighted average number of common shares outstanding |
1,706,682 | 14,544,722 | 16,115,993 | |||||||
| Weighted average number of dilutive common equivalents from options to purchase common stock and preferred stock warrants |
— | 247,245 | 251,113 | |||||||
| Weighted average number of common shares and common share equivalents |
1,706,682 | 14,791,967 | 16,367,106 | |||||||
| Diluted net (loss) income per share attributable to common stockholders |
$ | (0.64 | ) | $ | 0.87 | $ | 1.14 | |||
70
Table of Contents
IPC THE HOSPITALIST COMPANY, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
In 2007, 9,025,193 shares of our convertible preferred stock are excluded from the calculation of diluted net income per share attributable to common stockholders because to do so would be anti-dilutive. Outstanding stock options with an exercise price above market, are excluded from our diluted computation as their effect would be anti-dilutive. At December 31, 2008 and 2009, there were approximately 29,718 and 310 outstanding stock options with an exercise price above the average annual market price for 2008 and 2009, respectively.
The following pro forma of basic and diluted net (loss) income per share attributable to common stockholders in 2007 and 2008 assumes the conversion of preferred shares to common stock at a ratio of 6.4:1 as well as a cashless exchange of warrants held by our preferred stockholders using the treasury stock method (dollars in thousands, except per share data):
| 2007 | 2008 | ||||||
| Basic: |
|||||||
| Net (loss) income attributable to common stockholders—historical |
$ | (1,096 | ) | $ | 12,858 | ||
| Accretion of redeemable convertible preferred stockholders |
229 | — | |||||
| Income allocable to preferred stockholders |
— | 696 | |||||
| Net (loss) income attributable to common stockholders—pro forma |
$ | (867 | ) | $ | 13,554 | ||
| Weighted average number of common shares outstanding—historical |
1,706,682 | 14,544,722 | |||||
| Add number of preferred shares and warrants converted to common shares |
9,511,089 | 631,763 | |||||
| Common shares outstanding—pro forma |
11,217,771 | 15,176,485 | |||||
| Basic net (loss) income per share attributable to common stockholders—pro forma |
$ | (0.08 | ) | $ | 0.89 | ||
| Diluted: |
|||||||
| Net (loss) income attributable to common stockholders—historical |
$ | (1,096 | ) | $ | 12,858 | ||
| Accretion of redeemable convertible preferred stockholders |
229 | — | |||||
| Income allocable to preferred stockholders |
— | 696 | |||||
| Net (loss) income attributable to common stockholders—pro forma |
$ | (867 | ) | $ | 13,554 | ||
| Weighted average number of common shares outstanding—historical |
1,706,682 | 14,544,722 | |||||
| Add: number of preferred shares and warrants converted to common shares |
9,511,089 | 631,763 | |||||
| Add: weighted average number of dilutive common equivalent shares |
— | 207,298 | |||||
| Common shares outstanding—pro forma |
11,217,771 | 15,383,783 | |||||
| Diluted net (loss) income per share attributable to common stockholders—pro forma |
$ | (0.08 | ) | $ | 0.88 | ||
71
Table of Contents
IPC THE HOSPITALIST COMPANY, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
10. Commitments and Contingencies
Leases
We lease certain buildings and equipment under operating leases. Certain building leases contain renewal options. Future minimum rental payments required under operating leases that have initial or remaining noncancelable leases as of December 31, 2009, are as follows (dollars in thousands):
| 2010 |
$ | 1,881 | |
| 2011 |
1,125 | ||
| 2012 |
516 | ||
| 2013 |
222 | ||
| 2014 |
189 | ||
| Thereafter |
99 | ||
| Total |
$ | 4,032 | |
Rent expense for 2007, 2008 and 2009 was approximately $1,787,000, $1,963,000 and $2,303,000, respectively.
Regulatory Matters
Laws and regulations governing the Medicare and Medicaid programs are complex and subject to interpretation. We believe that we are in compliance with all applicable laws and regulations, and we are not aware of any pending or threatened investigations involving allegations of potential wrongdoing. While no such regulatory inquiries have been made, compliance with such laws and regulations can be subject to future government review and interpretation as well as significant regulatory action including fines, penalties, and exclusion from the Medicare and Medicaid programs.
We operate in certain states regulated under corporate practice of medicine laws and we believe that we are in compliance with all such laws.
Legal
In the ordinary course of our business, we become involved in pending and threatened legal actions and proceedings, most of which involve claims of medical malpractice related to medical services provided by our affiliated physicians. We may also become subject to other lawsuits, which could involve significant claims and/or significant defense costs.
We believe, based upon our review of pending actions and proceedings that the outcome of such legal actions and proceedings will not have a material adverse effect on our business, financial condition, results of operations, or cash flows. The outcome of such actions and proceedings, however, cannot be predicted with certainty and an unfavorable resolution of one or more of them could have a material adverse effect on our business, financial condition, results of operations, or cash flows in a future period.
Liability Insurance
Although we currently maintain liability insurance policies on a claims-made basis, which are intended to cover malpractice liability and certain other claims, the coverage must be renewed annually, and may not continue to be available to us in future years at acceptable costs, and on favorable terms. In addition to the known incidents occurring through December 31, 2009 that have resulted in the assertion of claims, we cannot be certain that our insurance coverage will be adequate to cover liabilities arising out of claims asserted against us in the
72
Table of Contents
IPC THE HOSPITALIST COMPANY, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
future where the outcomes of such claims are unfavorable. During the first quarter of 2010, we reached a preliminary agreement to settle a disputed professional liability claim for a prior year that is in excess of our insurance policy limit. The settlement remains subject to definitive documentation and is contingent upon receiving applicable court approval. We recorded the excess amount of $750,000 as professional liability settlement expense in our consolidated statement of operations for 2009 and accrued professional liability settlement in the current liabilities of our balance sheet as of December 31, 2009.
We believe that the ultimate resolution of all pending claims, including liabilities in excess of our insurance coverage, will not have a material adverse effect on our financial position, results of operations or cash flows; however, there can be no assurance that future claims will not have a material adverse effect on our business.
11. Fair Value Measurement
Fair value is defined as the price that would be received to sell an asset or paid to transfer a liability in an orderly transaction between market participants at the measurement date (an exit price). The established fair value hierarchy distinguishes between market participant assumptions based on market data obtained from sources independent of the reporting entity (Levels 1 and 2) and the reporting entity’s own assumptions about market participant assumptions (Level 3). This hierarchy is used to measure fair value as follows:
| • | Level 1 inputs utilize quoted prices in active markets for identical assets or liabilities. |
| • | Level 2 inputs include quoted prices for similar assets and liabilities in active markets; quoted prices in markets that are not active; and other inputs that are observable or can be corroborated by observable market data for the asset or liability. |
| • | Level 3 inputs are unobservable inputs for the asset or liability that are supported by little or no market activity. |
The following table presents our liabilities measured at fair value on a recurring basis as of December 31, 2009 (dollars in thousands):
| Fair Value Measurement at December 31, 2009 | ||||||||||||
| Quoted Prices In Active Markets for Identical Instruments (Level 1) |
Significant Other Observable Inputs (Level 2) |
Significant Unobservable Inputs (Level 3) |
Total Balance | |||||||||
| Payable for practice acquisitions |
$ | — | $ | — | $ | 9,407 | $ | 9,407 | ||||
The following table presents a reconciliation for our liabilities measured at fair value on a recurring basis using significant unobservable inputs (level 3) for 2009 (dollars in thousands):
| Payable for Practice Acquisition |
||||
| Beginning balance at December 31, 2008 |
$ | — | ||
| Addition through acquisition—2009 transactions |
9,565 | |||
| Change in fair value realized |
(158 | ) | ||
| Ending balance at December 31, 2009 |
$ | 9,407 | ||
The change in fair value $158,000 is included in general and administration expenses.
The fair value of our payable for practice acquisitions that occur after January 1, 2009 is determined using widely accepted valuation techniques, which include the estimation of future consideration to be paid based on
73
Table of Contents
IPC THE HOSPITALIST COMPANY, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
projected earnings of the acquired practices as of certain measurement dates. The earnings projections and the related fair value of our payable for practice acquisitions are reassessed on a quarterly basis.
We measure certain assets including goodwill and other intangible assets at fair value on a nonrecurring basis. Those assets are written down to fair value when they are deemed to be impaired. During 2007, 2008 and 2009, we did not recognize any impairment on such assets.
12. Quarterly Results of Operations (unaudited)
Following is a summary of our quarterly results of operations for the years ended December 31, 2008 and 2009 (dollars in thousands, except for per share data):
| Mar 31, 2008 |
Jun 30, 2008 |
Sep 30, 2008 |
Dec 31, 2008 |
Mar 31, 2009 |
Jun 30, 2009 |
Sep 30, 2009 |
Dec 31, 2009 |
|||||||||||||||||||||||||
| Net revenue |
$ | 60,559 | $ | 59,154 | $ | 63,164 | $ | 68,302 | $ | 76,057 | $ | 74,783 | $ | 77,521 | $ | 82,160 | ||||||||||||||||
| Income from operations |
5,427 | 4,803 | 5,389 | 6,863 | 7,567 | 7,019 | 7,433 | 8,318 | ||||||||||||||||||||||||
| Investment income |
164 | 144 | 186 | 110 | 41 | 24 | 13 | 6 | ||||||||||||||||||||||||
| Interest expense |
(385 | ) | (194 | ) | (144 | ) | (145 | ) | (79 | ) | (169 | ) | (23 | ) | (22 | ) | ||||||||||||||||
| Income before income taxes |
5,206 | 4,753 | 5,431 | 6,828 | 7,529 | 6,874 | 7,423 | 8,302 | ||||||||||||||||||||||||
| Income tax provision |
2,186 | 1,997 | 2,281 | 2,200 | 3,012 | 2,749 | 2,804 | 2,936 | ||||||||||||||||||||||||
| Net income |
$ | 3,020 | $ | 2,756 | $ | 3,150 | $ | 4,628 | $ | 4,517 | $ | 4,125 | $ | 4,619 | $ | 5,366 | ||||||||||||||||
| Per share data: |
||||||||||||||||||||||||||||||||
| Net income per share attributable to common stockholders—historical: |
||||||||||||||||||||||||||||||||
| Price per share(1): |
||||||||||||||||||||||||||||||||
| Basic |
$ | 0.20 | $ | 0.19 | $ | 0.20 | $ | 0.29 | $ | 0.28 | $ | 0.26 | $ | 0.29 | $ | 0.33 | ||||||||||||||||
| Diluted |
$ | 0.20 | $ | 0.18 | $ | 0.20 | $ | 0.28 | $ | 0.28 | $ | 0.25 | $ | 0.28 | $ | 0.32 | ||||||||||||||||
| Weighted average shares: |
||||||||||||||||||||||||||||||||
| Basic |
11,434,588 | 14,873,501 | 15,784,261 | 16,059,982 | 16,089,357 | 16,101,969 | 16,122,506 | 16,149,409 | ||||||||||||||||||||||||
| Diluted |
11,831,936 | 15,087,795 | 15,987,343 | 16,239,765 | 16,258,950 | 16,297,917 | 16,455,740 | 16,532,069 | ||||||||||||||||||||||||
| Net income per share attributable to common stockholders—pro forma: |
||||||||||||||||||||||||||||||||
| Price per share(1): |
||||||||||||||||||||||||||||||||
| Basic |
$ | 0.22 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |||||||||||||||||||||||
| Diluted |
$ | 0.21 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |||||||||||||||||||||||
| Weighted average shares: |
||||||||||||||||||||||||||||||||
| Basic |
13,975,526 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | ||||||||||||||||||||||||
| Diluted |
14,212,207 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | ||||||||||||||||||||||||
| (1) | Earnings per share are computed independently for each of the quarters presented and therefore may not sum to the total for the year. |
13. Subsequent Events
We have evaluated our subsequent events through February 22, 2010, the date of issuance of our 2009 annual consolidated financial statements. During the first quarter of 2010, we reached a preliminary agreement to settle a disputed professional liability claim for a prior year that is in excess of our insurance policy limit. The settlement remains subject to definitive documentation and is contingent upon receiving applicable court approval. We recorded the settlement amount of $750,000 as professional liability settlement expense in our consolidated statement of operations for 2009 and accrued professional liability settlement in the current liabilities of our balance sheet as of December 31, 2009.
74
Table of Contents
| ITEM 9. | CHANGES IN AND DISAGREEMENTS WITH ACCOUNTANTS ON ACCOUNTING AND FINANCIAL DISCLOSURE |
None.
| ITEM 9A. | CONTROLS AND PROCEDURES |
Evaluation of Disclosure Controls and Procedures
We maintain controls and procedures designed to ensure that we are able to collect the information we are required to disclose in the reports we file with the Securities and Exchange Commission, and to process, summarize and disclose this information within the time periods specified in the rules of the Securities and Exchange Commission. Our management, with the participation of our Chief Executive Officer and our Chief Financial Officer, has conducted an evaluation of the design and operation of our “disclosure controls and procedures” as defined in Rule 13a-15(e) and 15d-15(e) under the Security Exchange Act of 1934 (Exchange Act). Based on this evaluation, our Chief Executive Officer and our Chief Financial Officer have concluded that our disclosure controls and procedures are effective as of the end of the period covered by this report to ensure that information required to be disclosed in the reports that we file or submit under the Exchange Act is recorded, processed, summarized and reported within the time periods specified in the Securities and Exchange Commission’s rules and forms.
Internal Control over Financial Reporting
Management’s Report on Internal Control over Financial Reporting
Our management is responsible for establishing and maintaining adequate internal control over financial reporting as defined in Rule 13a-15(f) or 15d-15(f) promulgated under the Exchange Act. Those rules define internal control over financial reporting as a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with accounting principles generally accepted in the United States of America (GAAP), and includes those policies and procedures that:
| • | pertain to the maintenance of records that in reasonable detail accurately and fairly reflect the transactions and dispositions of the assets of the company; |
| • | provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with GAAP, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company: and |
| • | provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use or disposition of the company’s assets that could have a material effect on the financial statements. |
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate, because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
Our management assessed the effectiveness of our internal control over financial reporting as of December 31, 2009. In making this assessment, our management used the criteria established in Internal Control-Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (COSO). Based on their assessment and those criteria, management believes that as of December 31, 2009, our internal control over financial reporting is effective.
There was no change in our internal control over financial reporting that occurred during the three months ended December 31, 2009 that has materially affected, or is reasonably likely to materially affect, our internal control over financial reporting.
The effectiveness of our internal control over financial reporting has been audited by Ernst & Young, LLP, an independent registered public accounting firm, as stated in their report appearing on the page immediately following, which expresses an unqualified opinion on the effectiveness of our internal control over financial reporting as of December 31, 2009.
75
Table of Contents
Report of Independent Registered Public Accounting Firm
Board of Directors
IPC The Hospitalist Company, Inc.
We have audited IPC The Hospitalist Company, Inc.’s (the “Company’s”) internal control over financial reporting as of December 31, 2009, based on criteria established in Internal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (the COSO criteria). The Company’s management is responsible for maintaining effective internal control over financial reporting, and for its assessment of the effectiveness of internal control over financial reporting included in the accompanying management’s report on internal control over financial reporting. Our responsibility is to express an opinion on the Company’s internal control over financial reporting based on our audit.
We conducted our audit in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether effective internal control over financial reporting was maintained in all material respects. Our audit included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, testing and evaluating the design and operating effectiveness of internal control based on the assessed risk, and performing such other procedures as we considered necessary in the circumstances. We believe that our audit provides a reasonable basis for our opinion.
A company’s internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company’s internal control over financial reporting includes those policies and procedures that (1) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company’s assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
In our opinion, IPC The Hospitalist Company, Inc. maintained, in all material respects, effective internal control over financial reporting as of December 31, 2009, based on the COSO criteria.
We have also audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States), the consolidated balance sheets of IPC The Hospitalist Company, Inc. as of December 31, 2008 and 2009, and the related consolidated statements of operations, stockholders’ equity, and cash flows for each of the three years in the period ended December 31, 2009 and our report dated February 22, 2010 expressed an unqualified opinion thereon.
/s/ Ernst & Young LLP
Los Angeles, California
February 22, 2010
76
Table of Contents
| ITEM 9B. | OTHER INFORMATION |
Not applicable.
77
Table of Contents
| ITEM 10. | DIRECTORS, EXECUTIVE OFFICERS AND CORPORATE GOVERNANCE |
Information required by this item will be contained in our definitive Proxy Statement with respect to the 2010 Annual Meeting of Stockholders to be filed with the Securities and Exchange Commission (the “2010 Proxy Statement”) and is hereby incorporated by reference.
| ITEM 11. | EXECUTIVE COMPENSATION |
Information required by this item will be contained in the 2010 Proxy Statement and is hereby incorporated by reference.
| ITEM 12. | SECURITY OWNERSHIP OF CERTAIN BENEFICIAL OWNERS AND MANAGEMENT AND RELATED STOCKHOLDER MATTERS |
Information required by this item will be contained in the 2010 Proxy Statement and is hereby incorporated by reference.
| ITEM 13. | CERTAIN RELATIONSHIPS AND RELATED TRANSACTIONS, AND DIRECTOR INDEPENDENCE |
Information required by this item will be contained in the 2010 Proxy Statement and is hereby incorporated by reference.
| ITEM 14. | PRINCIPAL ACCOUNTANT FEES AND SERVICES |
Information required by this item will be contained in the 2010 Proxy Statement and is hereby incorporated by reference.
78
Table of Contents
| ITEM 15. | EXHIBITS AND FINANCIAL STATEMENT SCHEDULES |
(a)(1) Financial Statements
The financial statements filed as part of this report are listed on the index to financial statements on page 52.
(a)(2) Financial Statement Schedules
The following schedule is filed as part of this Report:
IPC THE HOSPITALIST COMPANY, INC.
SCHEDULE II: VALUATION AND QUALIFYING ACCOUNTS
| Years Ended December 31, | ||||||||||||
| 2007 | 2008 | 2009 | ||||||||||
| (dollars in thousands) | ||||||||||||
| Allowance for uncollectible accounts were as follows: |
||||||||||||
| Balance at beginning of year |
$ | 1,810 | $ | 2,972 | $ | 3,323 | ||||||
| Amount charged against operating revenue |
6,649 | 8,498 | 10,054 | |||||||||
| Accounts receivable write-offs (net of recoveries) |
(5,487 | ) | (8,147 | ) | (10,675 | ) | ||||||
| Balance at end of year |
$ | 2,972 | $ | 3,323 | $ | 2,702 | ||||||
No other schedules are included because the required information is inapplicable, not required or are presented in the financial statements or the related notes thereto.
(a)(3) Exhibits
| Exhibit Number |
Description of Document | |
| 3.1* | Amended and Restated Certificate of Incorporation of IPC The Hospitalist Company, Inc. | |
| 3.2* | Amended and Restated Bylaws of IPC The Hospitalist Company, Inc. | |
| 4.1* | Form of Common Stock Certificate | |
| 10.1*† | IPC The Hospitalist Company, Inc. 2007 Equity Participation Plan, dated July 19, 2007, and the forms of agreements used thereunder | |
| 10.2*† | Form of Indemnification Agreement between IPC The Hospitalist Company, Inc. and each of its directors and executive officers | |
| 10.3* | Form of Management Agreement between a subsidiary of IPC The Hospitalist Company, Inc. and each of its affiliated professional organizations | |
| 10.3.1 | Form of Amendment to Management Agreement between a subsidiary of IPC The Hospitalist Company, Inc. and each of its affiliated professional organizations | |
| 10.4* | Second Amended and Restated Loan and Security Agreement, dated as of August 31, 2005, by and between Comerica Bank and IPC The Hospitalist Company, Inc. (f/k/a InPatient Consultants Management, Inc.) | |
| 10.5* | LIBOR Addendum to Second Amended and Restated Loan and Security Agreement, dated as of August 31, 2005, by and between Comerica Bank and IPC The Hospitalist Company, Inc. (f/k/a InPatient Consultants Management, Inc.) | |
79
Table of Contents
| Exhibit Number |
Description of Document | |
| 10.6* | First Amendment to Second Amended and Restated Loan and Security Agreement, dated as of March 30, 2006 by and between Comerica Bank and IPC The Hospitalist Company, Inc. (f/k/a InPatient Consultants Management, Inc.) | |
| 10.7* | Second Amendment to Second Amended and Restated Loan and Security Agreement, dated as of January 31, 2007 by and between Comerica Bank and IPC The Hospitalist Company, Inc. (f/k/a InPatient Consultants Management, Inc.) | |
| 10.8* | Third Amendment to Second Amended and Restated Loan and Security Agreement, dated as of October 22, 2007, by and between Comerica Bank and IPC The Hospitalist Company, Inc. (f/k/a InPatient Consultants Management, Inc.) | |
| 10.9* | Master Security Agreement, dated as of September 26, 2007, by and between General Electric Capital Corporation and IPC The Hospitalist Company, Inc. | |
| 10.11† | Second Amended and Restated Employment Agreement, effective August 5, 2009, between Adam D. Singer, M.D. and IPC The Hospitalist Company, Inc. (incorporated by reference to Exhibit 10.1 to the Registrant’s Form 10-Q (File No. 200-90806) filed on August 6, 2009) | |
| 10.12† | Second Amended and Restated Employment Agreement, effective August 5, 2009, between R. Jeffrey Taylor and IPC The Hospitalist Company, Inc. (incorporated by reference to Exhibit 10.2 to the Registrant’s Form 10-Q (File No. 200-90806) filed on August 6, 2009) | |
| 10.13† | Second Amended and Restated Employment Agreement, effective August 5, 2009, between Devra G. Shapiro and IPC The Hospitalist Company, Inc. (incorporated by reference to Exhibit 10.3 to the Registrant’s Form 10-Q (File No. 200-90806) filed on August 6, 2009) | |
| 10.14† | Second Amended and Restated Employment Agreement, effective August 5, 2009, between Richard G. Russell and IPC The Hospitalist Company, Inc. (incorporated by reference to Exhibit 10.4 to the Registrant’s Form 10-Q (File No. 200-90806) filed on August 6, 2009) | |
| 10.15† | IPC The Hospitalist Company, Inc. Nonqualified Employee Stock Purchase Plan amended and restated effective as of March 19, 2008 (incorporated by reference to Exhibit 10.1 to the Registrant’s Form 10-Q (File No. 001-33930) filed on May 14, 2008) | |
| 10.16*† | IPC The Hospitalist Company, Inc. Executive Change of Control Plan | |
| 10.17*† | 2002 Equity Participation Plan of IPC The Hospitalist Company, Inc. (f/k/a InPatient Consultants Management, Inc.) and the form of stock option agreement used thereunder | |
| 10.18*† | Written Consent of InPatient Consultants Management, Inc. dated January 31, 2007 amending the 2002 Equity Participation Plan | |
| 10.19*† | 1997 Equity Participation Plan of IPC The Hospitalist Company, Inc. (f/k/a InPatient Consultants Management, Inc.) and the form of stock option agreement used thereunder | |
| 10.20*† | Amendment No. 1 to the 1997 Equity Participation Plan of InPatient Consultants Management, Inc. dated April 29, 1998 | |
| 10.21*† | Amendment No. 2 to the 1997 Equity Participation Plan of InPatient Consultants Management, Inc. dated April 28, 1999 | |
| 10.22*† | Amendment No. 3 to the 1997 Equity Participation Plan of InPatient Consultants Management, Inc. dated October 10, 2000 | |
| 10.23* | Form of Succession Agreement between an affiliated entity of IPC The Hospitalist Company, Inc. and its founding doctor | |
80
Table of Contents
| Exhibit Number |
Description of Document | |
| 10.24* | Second Amended and Restated Registration Rights Agreement, dated October 7, 2002, by and between IPC The Hospitalist Company, Inc. (f/k/a InPatient Consultants Management, Inc.), the founding stockholders signatory thereto and the investors signatory thereto | |
| 21.1 | Subsidiaries of IPC The Hospitalist Company, Inc. | |
| 23.1 | Consent of Independent Registered Public Accounting Firm | |
| 31.1 | Certification of the Chief Executive Officer pursuant to Rule 13a-14(a) or Rule 15d-14(a) of the Securities Exchange Act of 1934 as adopted pursuant to Section 302 of the Sarbanes Oxley Act. | |
| 31.2 | Certification of the Chief Financial Officer pursuant to Rule 13a-14(a) or Rule 15d-14(a) of the Securities Exchange Act of 1934 as adopted pursuant to Section 302 of the Sarbanes Oxley Act. | |
| 32.1 | Certification of the Chief Executive Officer pursuant to 18 U.S.C. Section 1350 as adopted pursuant to Section 906 of the Sarbanes-Oxley Act. | |
| 32.2 | Certification of the Chief Financial Officer pursuant to 18 U.S.C. Section 1350 as adopted pursuant to Section 906 of the Sarbanes-Oxley Act. | |
| * | Incorporated herein by reference to IPC The Hospitalist Company, Inc.’s Registration Statement on Form S-1 (File No. 333-145850). |
| † | Management contracts or compensation plans, contracts or arrangements |
81
Table of Contents
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the Registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized on the 22nd day of February 2010.
| IPC THE HOSPITALIST COMPANY, INC. (Registrant) | ||
| By: |
/s/ ADAM D. SINGER, M.D. | |
| Adam D. Singer, M.D. | ||
| Chief Executive Officer | ||
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed below by the following persons on behalf of the Registrant and in the capacities indicated on February 22, 2010.
| Signature |
Title | |
| /s/ ADAM D. SINGER, M.D. Adam D. Singer, M.D. |
Chief Executive Officer, Chairman and Director (Principal Executive Officer) | |
| /s/ R. JEFFREY TAYLOR R. Jeffrey Taylor |
President, Chief Operating Officer and Director | |
| /s/ DEVRA G. SHAPIRO Devra G. Shapiro |
Chief Financial Officer (Principal Financial Officer) | |
| /s/ FERNANDO J. SARRIA Fernando J. Sarria |
Chief Accounting Officer (Principal Accounting Officer) | |
| /s/ MARK J. BROOKS Mark J. Brooks |
Director | |
| /s/ THOMAS P. COOPER, M.D. Thomas P. Cooper, M.D. |
Director | |
| /s/ FRANCESCO FEDERICO, M.D. Francesco Federico, M.D. |
Director | |
| /s/ WOODRIN GROSSMAN Woodrin Grossman |
Director | |
| /s/ PATRICK G. HAYS Patrick G. Hays |
Director | |
| /s/ C. THOMAS SMITH C. Thomas Smith |
Director | |
| /s/ CHUCK TIMPE Chuck Timpe |
Director | |
82
